Chronic Kidney Disease Chapter 46 Chronic Kidney Disease



- Slides: 73
Chronic Kidney Disease Chapter 46
Chronic Kidney Disease (CKD) • Involves progressive, irreversible loss of kidney function • More than 26 million American adults have CKD • Over half a million Americans are receiving treatment for ESRD
Chronic Kidney Disease • Defined as one of the following: • Kidney damage • Pathologic abnormalities • Markers of damage • Blood, urine, imaging tests • Low glomerular filtration rate (GFR) • <60 m. L/min for longer than 3 months
Chronic Kidney Disease • Leading causes • Diabetes- 50% • Hypertension- 25% • Individuals with CKD are frequently asymptomatic • Results in CKD being underdiagnosed and untreated
Chronic Kidney Disease • Disease staging based on decrease in GFR • Normal GFR: 125 m. L/min, which is reflected by urine creatinine clearance • Last stage of kidney failure • End-stage renal disease (ESRD) occurs when GFR <15 m. L/min
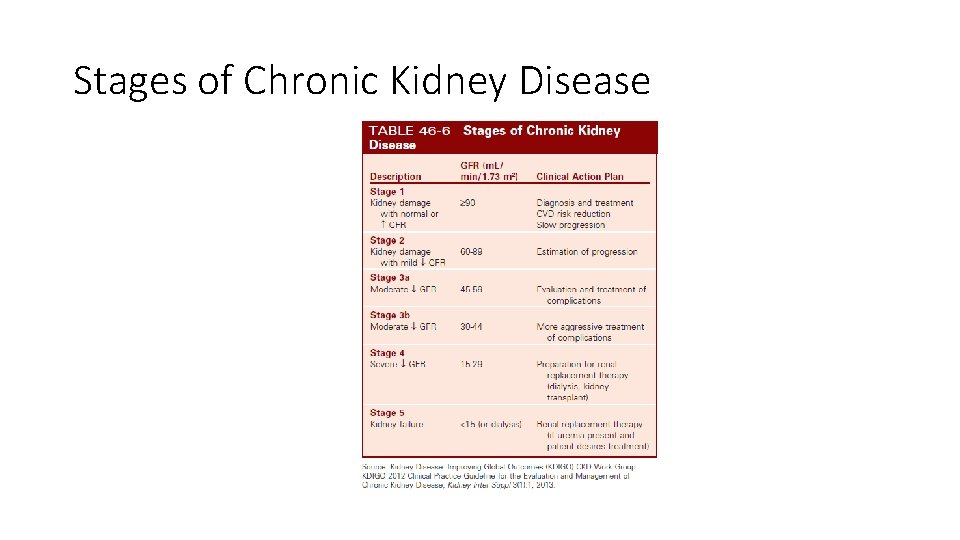
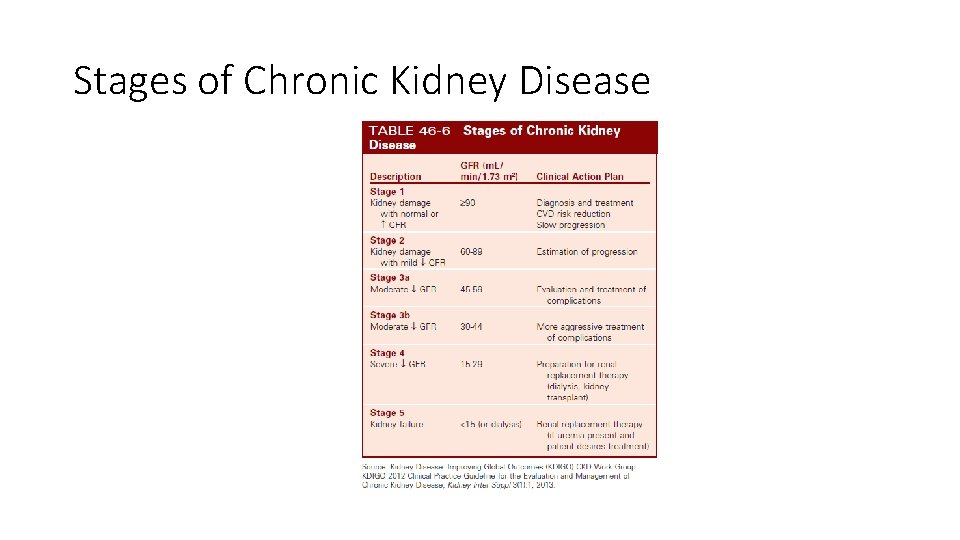
Stages of Chronic Kidney Disease
Case Study (©Purestock/Thinkstock) • K. W. , a 35 -year-old man, began to notice weakness with activities such as walking distances or running. • He also had tingling all over his body, particularly in his hands and feet.
Case Study (©Purestock/Thinkstock) • At age 5, K. W. was admitted to the hospital for hematuria, and acute glomerulonephritis was diagnosed. • At age 11, he was admitted to the same hospital, and recurring acute glomerulonephritis was diagnosed. • K. W. has had no further follow-up until this admission.
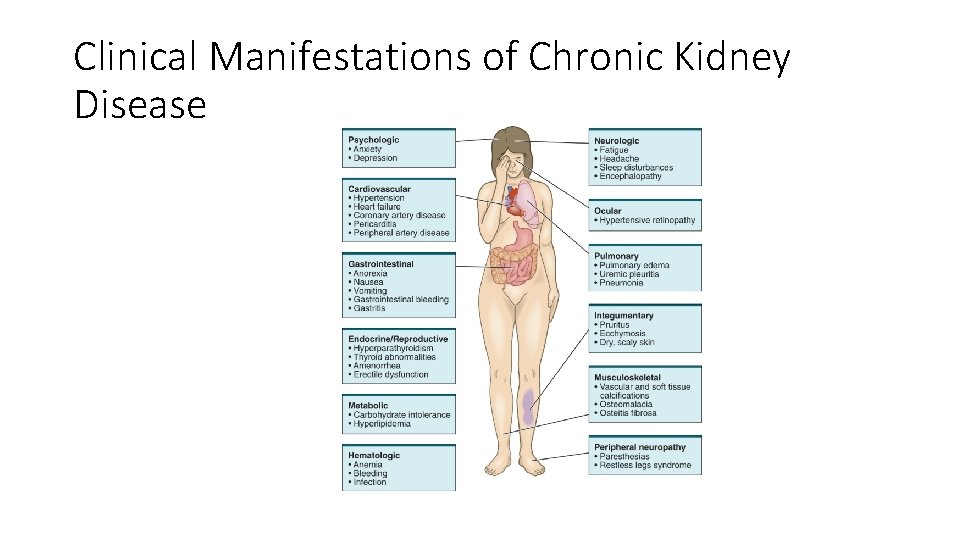
Clinical Manifestations • Result of retained substances • • • Urea Creatinine Phenols Hormones Electrolytes Water
Clinical Manifestations • Uremia • Syndrome in which kidney function declines to the point that symptoms occur in multiple body systems • Often occurs when GFR is ≤ 15 m. L/min
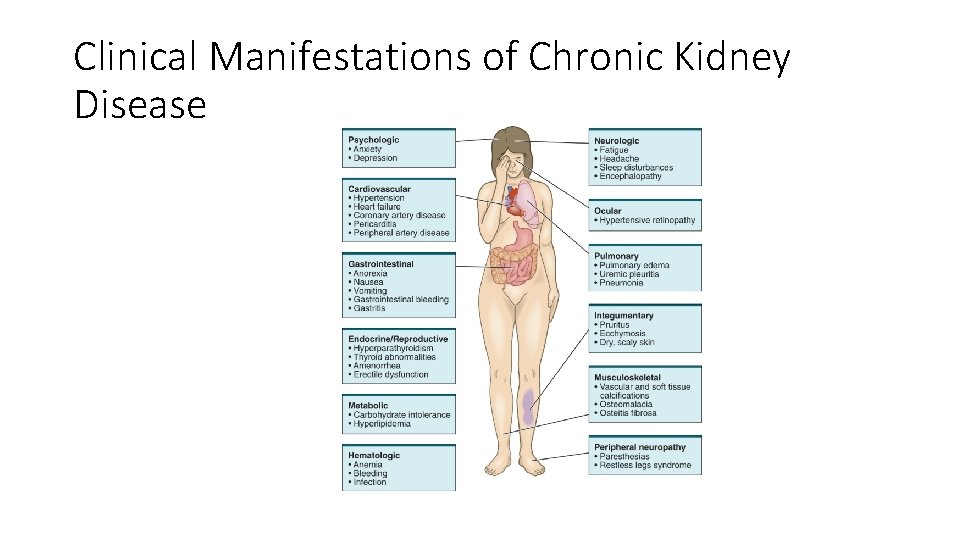
Clinical Manifestations of Chronic Kidney Disease
Case Study (©Purestock/Thinkstock) • K. W. says he had an increase in urine production several months ago and was concerned about the possibility of diabetes. • History reveals grandmother and aunt have diabetes; no family history of renal disease.
Case Study (©Purestock/Thinkstock) • He states that he has recently developed a severe decrease in urine output.
Clinical Manifestations Urinary System • Early stages • No change in urine output • Polyuria may be present related to diabetes. • As CKD progresses patients have increasing fluid retention • After a period on dialysis, patients may become anuric
Clinical Manifestations Urinary System • Early stages • No change in urine output • Polyuria may be present related to diabetes. • As CKD progresses patients have increasing fluid retention • After a period on dialysis, patients may become anuric
Clinical Manifestations Metabolic Disturbances • Altered carbohydrate metabolism • Caused by impaired glucose metabolism • From cellular insensitivity to normal action of insulin
Clinical Manifestations Metabolic Disturbances • Defective carbohydrate metabolism • Patients with diabetes who develop uremia may require less insulin than before the onset of CKD • Excretion of insulin dependent on kidneys • Insulin dosing must be individualized
Clinical Manifestations Metabolic Disturbances • Elevated triglycerides • Hyperinsulinemia stimulates hepatic production of triglycerides • Altered lipid metabolism • ↓ Levels of enzyme lipoprotein lipase • Important in breakdown of lipoproteins
Clinical Manifestations Metabolic Disturbances • Elevated triglycerides • Hyperinsulinemia stimulates hepatic production of triglycerides • Altered lipid metabolism • ↓ Levels of enzyme lipoprotein lipase • Important in breakdown of lipoproteins
Clinical Manifestations Electrolyte/Acid-Base Imbalances • Potassium • Hyperkalemia • Most serious electrolyte disorder in kidney disease • Fatal dysrhythmias • When serum potassium level reaches 7 to 8 m. Eq/L (7 to 8 mmol/L) When serum potassium level
Clinical Manifestations Electrolyte/Acid-Base Imbalances • Sodium • May be elevated, normal, or low • Because of impaired excretion, sodium along with water is retained • Dilutional hyponatremia may occur • Edema • Hypertension • HF
Clinical Manifestations Electrolyte/Acid-Base Imbalances • Calcium and phosphate alterations • Magnesium alterations • Hypermagnesemia • Related to ingestion of magnesium • Can result in absence of reflexes, decreased mental status, cardiac dysrhythmias, hypotension, respiratory failure
Clinical Manifestations Electrolyte/Acid-Base Imbalances • Metabolic acidosis • Results from • Kidneys’ impaired ability of to excrete excess acid (primary ammonia) • Defective reabsorption and regeneration of bicarbonate • Plasma bicarbonate level usually falls to approximately 16 to 20 m. Eq/L (16 to 20 mmol/L)
Clinical Manifestations Hematologic System • Anemia • Due to ↓ production of erythropoietin • From ↓ of functioning renal tubular cells • Also decreased iron stores • Folic acid lost in dialysis • Bleeding tendencies • Defect in platelet function
Clinical Manifestations Hematologic System • Infection • Changes in WBC function • Altered immune response and function • Hyperglycemia and external trauma
Clinical Manifestations Cardiovascular System • CV disease and CKD closely linked • Traditional CV risk factors • Hypertension • Elevated lipids • Nontraditional CV risk factors • Vascular calcification • Arterial stiffness
Clinical Manifestations Cardiovascular System • Calcium deposits associated with stiffness of blood vessels • Vascular smooth muscle cells change • Chondrocytes or osteoblastlike cells • High calcium and phosphate totals • Impaired renal excretion • Drug therapies to treat bone disease
Clinical Manifestations Cardiovascular System • Hypertension • Both a cause and a consequence of CKD • Aggravated by sodium and water retention • Increased renin production may contribute • Lead to left ventricular hypertrophy and HF
Clinical Manifestations Cardiovascular System • Hypertension • Both a cause and a consequence of CKD • Aggravated by sodium and water retention • Increased renin production may contribute • Lead to left ventricular hypertrophy and HF
Clinical Manifestations Gastrointestinal System • Every part of GI system is affected • Cause: excessive urea • • • Stomatitis with ulcerations Uremic fetor (urinous odor of breath) Gastrointestinal system Diabetic gastroparesis GI bleeding Constipation
Clinical Manifestations Neurologic System • Expected as kidney disease progresses • Result of • • ↑ Nitrogenous waste products Electrolyte imbalances Metabolic acidosis Atrophy and demyelination of nerve fibers
Clinical Manifestations Neurologic System • CNS depression • • Lethargy, apathy Decreased ability to concentrate Fatigue, irritability Altered mental ability Seizures Coma Hypertensive encephalopathy
Clinical Manifestations Neurologic System • Slowing of nerve conduction • Restless legs syndrome • Paresthesias • Motor involvement • • Foot drop Muscle weakness and atrophy Loss of deep tendon reflexes Peripheral neuropathy
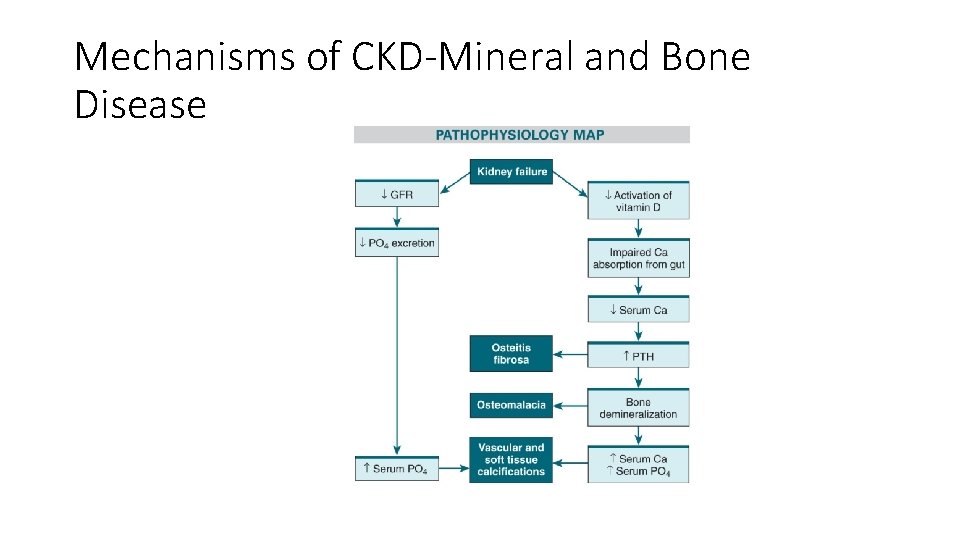
Clinical Manifestations Musculoskeletal System • CKD mineral and bone disorder • Systemic disorder of mineral and bone metabolism • Results in • Skeletal complications (osteomalacia, osteitis fibrosa) • Soft tissue complications (vascular calcifications)
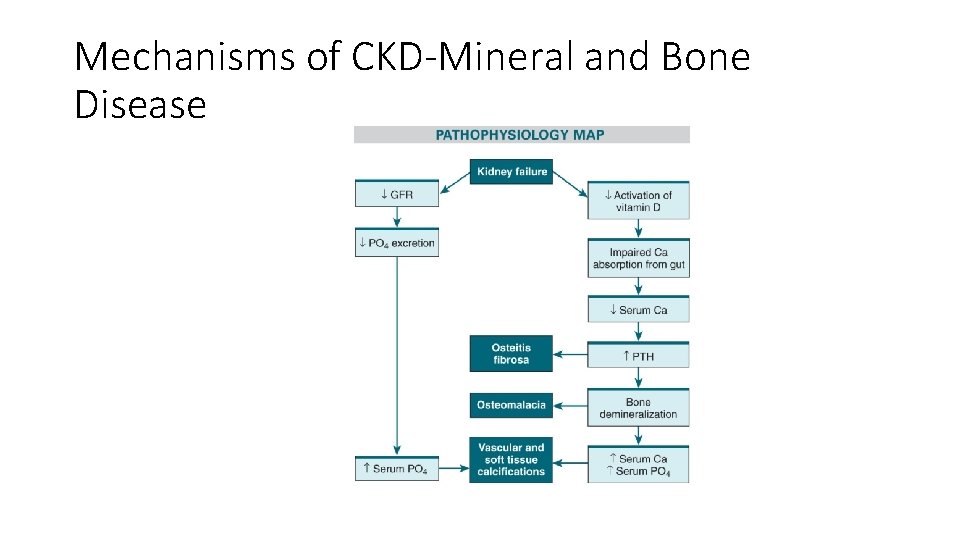
Mechanisms of CKD-Mineral and Bone Disease
Clinical Manifestations Integumentary System • Pruritus • Itching may be intense • Leads to bleeding or infection • Uremic frost • Urea crystalizes on skin

Clinical Manifestations Reproductive System • Infertility and decreased libido • Experienced by both sexes • Low sperm counts • Sexual dysfunction • Pregnancy poses significant risk to mother and infant
Clinical Manifestations Psychologic Changes • Personality and behavioral changes • Emotional lability • Withdrawal • Depression
Case Study (©Purestock/Thinkstock) • K. W. states that he has had difficulty with itchy skin and assumed that it was simply related to winter dryness. • He also recently received a diagnosis of restless legs syndrome.
Diagnostic Studies • History and physical examination • Dipstick evaluation of protein • Urinalysis • Renal ultrasound/ biopsy • Albumin-to-creatinine ratio (first morning void) • GFR
Interprofessional Care • Overall Goals • • Preserve existing kidney function Reduce risks of CV disease Prevent complications Provide for patient’s comfort
Case Study (©Purestock/Thinkstock) • K. W. undergoes a renal biopsy, which shows severe damage of nephrons. • His BP is 154/88. • He receives a diagnosis of chronic glomerulonephritis. • He has stage 4 chronic kidney disease and begins conservative therapy.
Interprofessional Care Conservative Therapy • Correction of extracellular fluid volume overload or deficit • Nutritional therapy • Erythropoietin therapy • Calcium supplementation, phosphate binders
Interprofessional Care Conservative Therapy • Antihypertensive therapy • Measures to lower potassium • Adjustment of drug dosages to degree of renal function
Interprofessional Care Drug Therapy • Hyperkalemia • • • Restriction of high-potassium foods and drugs IV glucose and insulin IV 10% calcium gluconate
Interprofessional Care Drug Therapy • Hyperkalemia • • • Restriction of high-potassium foods and drugs IV glucose and insulin IV 10% calcium gluconate
Interprofessional Care Drug Therapy • Hypertension • • Weight loss (if indicated) Therapeutic lifestyle changes Diet recommendations (DASH Diet) Administration of antihypertensive drugs
Interprofessional Care Drug Therapy • Hypertension • Antihypertensive drugs • ACE inhibitors • ARB agents
Interprofessional Care Drug Therapy • CKD-Mineral and bone disease (MBD) • Phosphate not restricted until patient requires renal replacement therapy • Phosphate intake then restricted to < 1 g/day

Interprofessional Care Drug Therapy • CKD-MBD • Phosphate binders • Calcium acetate (Phos. Lo) • Calcium carbonate (Caltrate) • Bind phosphate in bowel and then excreted • Sevelamer hydrochloride (Renagel) • Lowers cholesterol and LDL levels
Interprofessional Care Drug Therapy • CKD-MBD • Phosphate binders • Should be administered with each meal • Side effect: constipation
Interprofessional Care Drug Therapy • CKD-MBD • Avoid aluminum preparations • Supplementing vitamin D • Calcitriol • Serum phosphate level must be lowered before calcium or vitamin D is administered
Interprofessional Care Drug Therapy • CKD-MBD • Controlling secondary hyperparathyroidism • Calcimimetic agents • Cinacalcet (Sensipar) • ↑ Sensitivity of calcium receptors in parathyroid glands • Subtotal or total parathyroidectomy
Interprofessional Care Drug Therapy • Anemia • Erythropoietin (EPO) • • • Epoetin alfa (Epogen, Procrit) Darbepoeitin alfa (Aranesp) Administered IV or subcutaneously Increased hemoglobin and hematocrit in 2 to 3 weeks Side effects: thromboembolism, hypertension
Interprofessional Care Drug Therapy • Anemia • Iron supplements • If plasma ferritin level is <100 ng/m. L • Side effects: gastric irritation, constipation • May make stool dark in color
Interprofessional Care Drug Therapy • Anemia • Folic acid supplements • Needed for RBC formation • Removed by dialysis • Avoid blood transfusions • Increase the development of antibodies • May lead to iron overload
Interprofessional Care Drug Therapy • Dyslipidemia • Statins (HMG-Co. A reductase inhibitors) • Most effective for lowering LDL level • atorvastatin (Lipitor) • Fibrates (fibric acid derivitives) • Used to lower triglyceride levels • gemfibrozil
Interprofessional Care Drug Therapy • Complications • Drug toxicity • • Digoxin Diabetic agents Antibiotics Opioid medications
Case Study (©Purestock/Thinkstock) • K. W. is started on the following medications: • • Darbepoetin alfa (Aranesp) weekly HCTZ 25 mg PO daily Captopril 25 mg PO bid Calcium carbonate 600 mg PO bid
Interprofessional Care Nutritional Therapy • Designed to maintain good nutrition • Monitor laboratory parameters • Protein intake • Normal for HD patient • Increased for PD patient • Fluid restriction • Intake depends on daily urine output
Interprofessional Care Nutritional Therapy • Sodium restriction • Diets vary from 2 to 4 g/day • Salt substitutes should be avoided because they contain potassium chloride
Interprofessional Care Nutritional Therapy • Potassium restriction • Limit: 2 to 3 g • High-potassium foods should be avoided
Interprofessional Care Nutritional Therapy • Phosphate restriction in ESRD • Limit: 1 g/day • Foods high in phosphate • Meat • Dairy products • Most foods high in phosphate are also high in protein • Phosphate binders essential
Nursing Management Nursing Assessment • Complete history of any existing kidney disease, family history • Long-term health problems • Drugs and herbal preparations • Dietary habits • Support systems
Nursing Management Nursing Diagnoses • Excess fluid volume • Risk for electrolyte imbalance • Risk for injury • Imbalanced nutrition: less than body requirements
Nursing Management Planning • Overall Goals • • Demonstrate knowledge and ability to comply with therapeutic regimen Participate in decision making Demonstrate effective coping strategies Continue with activities of daily living within physiologic limitations
Nursing Management Nursing Implementation • Health Promotion • Identify individuals at risk for CKD • • Diabetes mellitus Hypertension History or family history of kidney disease Repeated urinary tract infection • Regular checkups and changes in urinary appearance, frequency, and volume should be reported
Nursing Management Nursing Implementation • Acute Care • Most care for CKD occurs on an outpatient basis • In-hospital care required for management of complications and for kidney transplantation
Nursing Management Nursing Implementation • Ambulatory Care • Teach patient and caregiver about • Diet • Drugs • Common side effects • Pill organizer • Avoid over-the-counter drugs • Take daily BP • Identify signs of fluid overload, electrolyte imbalances
Nursing Management Nursing Implementation • Ambulatory Care • Patient can complete evaluation for kidney transplant • Explain what is involved in PD or HD, home dialysis modalities, transplantation, palliative care
Case Study (©Purestock/Thinkstock) • K. W. ’s condition stabilizes, and he is ready for discharge. • Peritoneal dialysis versus hemodialysis is discussed with him as a possibility in the future. • He begins asking if kidney transplantation will cure his chronic kidney disease.

Nursing Management Evaluation • The patient with CKD will maintain • Fluid and electrolyte levels within normal ranges • An acceptable weight with no more than a 10% weight loss
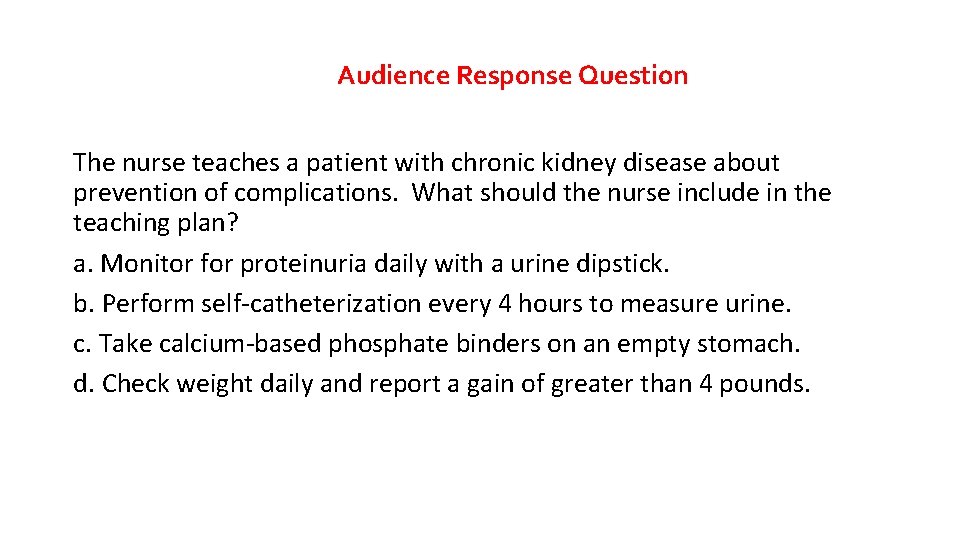
Audience Response Question The nurse teaches a patient with chronic kidney disease about prevention of complications. What should the nurse include in the teaching plan? a. Monitor for proteinuria daily with a urine dipstick. b. Perform self-catheterization every 4 hours to measure urine. c. Take calcium-based phosphate binders on an empty stomach. d. Check weight daily and report a gain of greater than 4 pounds.
 Nephrology near atwater
Nephrology near atwater Carlee oakley
Carlee oakley Low potassium diet nemo
Low potassium diet nemo Sighns of kidney disease
Sighns of kidney disease Resonium por
Resonium por Albumin kidney disease
Albumin kidney disease Albumin kidney disease
Albumin kidney disease Symptomatic polycystic kidney disease
Symptomatic polycystic kidney disease Chronic granulomatous disease
Chronic granulomatous disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Jewish chronic disease study
Jewish chronic disease study Stigmata of portal hypertension
Stigmata of portal hypertension Stigmata of chronic liver disease
Stigmata of chronic liver disease Nonalcoholic fatty liver disease
Nonalcoholic fatty liver disease Kate lorig stanford
Kate lorig stanford Developed by ed
Developed by ed Chronic disease
Chronic disease Nursing management of cirrhosis of liver
Nursing management of cirrhosis of liver Chronic disease
Chronic disease Dohányos tüdő
Dohányos tüdő Chronic rheumatic heart disease
Chronic rheumatic heart disease Bharathi viswanathan
Bharathi viswanathan Chapter 18 common chronic and acute conditions
Chapter 18 common chronic and acute conditions Pathophysiology of kidney stones
Pathophysiology of kidney stones Bellinior
Bellinior What are the three regions of the kidney
What are the three regions of the kidney Kidney infection
Kidney infection Interpolar region of kidney
Interpolar region of kidney Kidneys location and structure figure 15-2
Kidneys location and structure figure 15-2 Mesangial
Mesangial Figure 15-4 is a diagram of a nephron
Figure 15-4 is a diagram of a nephron Artery kidney
Artery kidney Meetslk
Meetslk Kidney pathology
Kidney pathology Gfr rumus
Gfr rumus Urinary tract obstruction
Urinary tract obstruction Coverings of kidney
Coverings of kidney Arenesp
Arenesp Kidney function test
Kidney function test Hyaline arteriolosclerosis
Hyaline arteriolosclerosis Hyperplastic arteriolitis
Hyperplastic arteriolitis Kidney agenesis
Kidney agenesis Uric acid kidney stone
Uric acid kidney stone Urineferous
Urineferous Oviduct frog
Oviduct frog Biologymad kidney
Biologymad kidney Kidney epithelial tissue
Kidney epithelial tissue Space of disse liver
Space of disse liver Hydrogen secretion in kidney
Hydrogen secretion in kidney Basinlike area of the kidney continuous with the ureter
Basinlike area of the kidney continuous with the ureter Vertebrocostal angle
Vertebrocostal angle Cell shape
Cell shape Kidney is a retroperitoneal organ
Kidney is a retroperitoneal organ Endive oxalate
Endive oxalate Topper learning.com
Topper learning.com Renal tubule
Renal tubule Midpole of the left kidney
Midpole of the left kidney Erythrocytopenia prefix and suffix
Erythrocytopenia prefix and suffix Filtration membrane
Filtration membrane Ain kidney
Ain kidney Kidney
Kidney Dr. santhosh thomas
Dr. santhosh thomas Kidney week abstract submission
Kidney week abstract submission Kidney diagram
Kidney diagram Kidney
Kidney Kidney
Kidney Bladder male
Bladder male Kidney
Kidney Kidney
Kidney Tubulus proximalis
Tubulus proximalis Kidney model labeled
Kidney model labeled Kidney slide
Kidney slide Disadvantage of kidney transplant
Disadvantage of kidney transplant Fish kidney
Fish kidney