Simultaneous Liver Kidney SLK Allocation Policy Kidney Transplantation
- Slides: 36
Simultaneous Liver Kidney (SLK) Allocation Policy Kidney Transplantation Committee Fall 2015 1
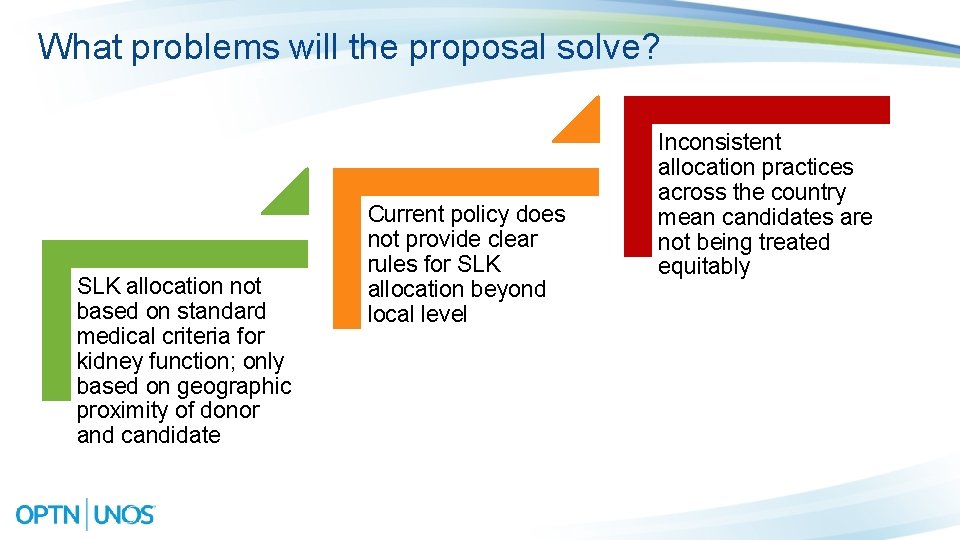
What problems will the proposal solve? SLK allocation not based on standard medical criteria for kidney function; only based on geographic proximity of donor and candidate Current policy does not provide clear rules for SLK allocation beyond local level Inconsistent allocation practices across the country mean candidates are not being treated equitably
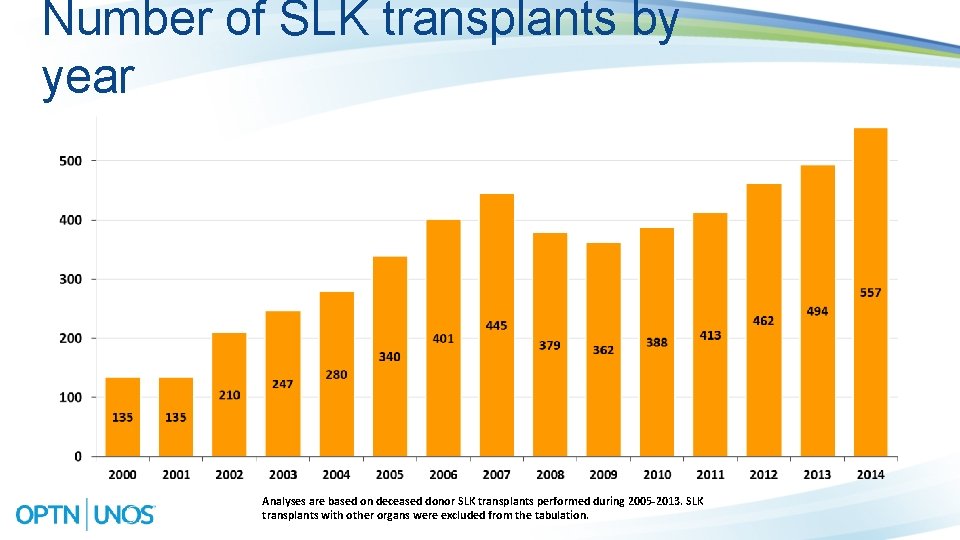
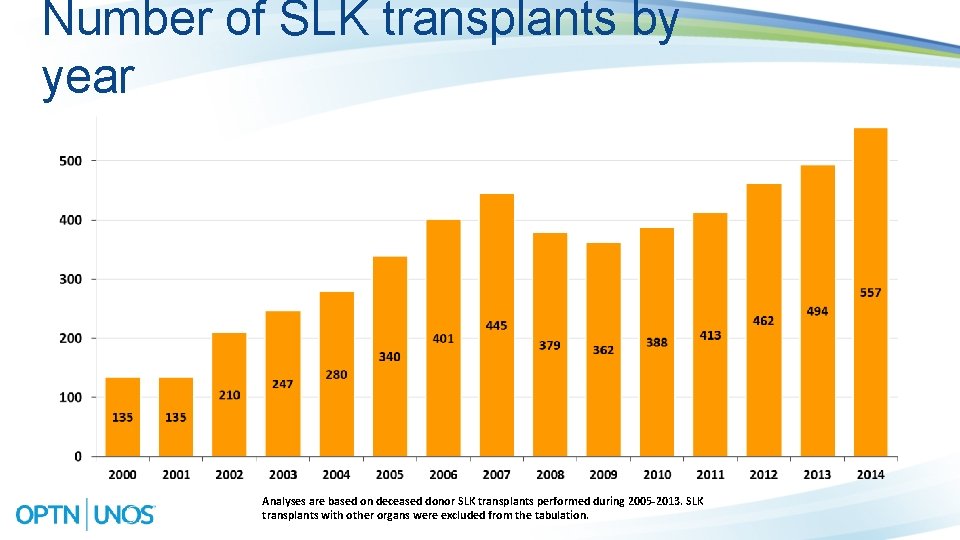
Number of SLK transplants by year Analyses are based on deceased donor SLK transplants performed during 2005 -2013. SLK transplants with other organs were excluded from the tabulation.
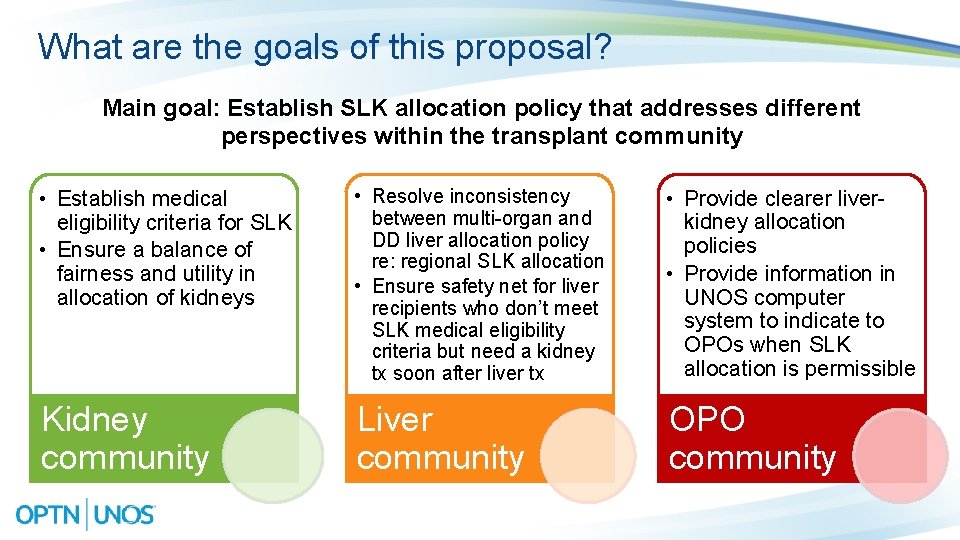
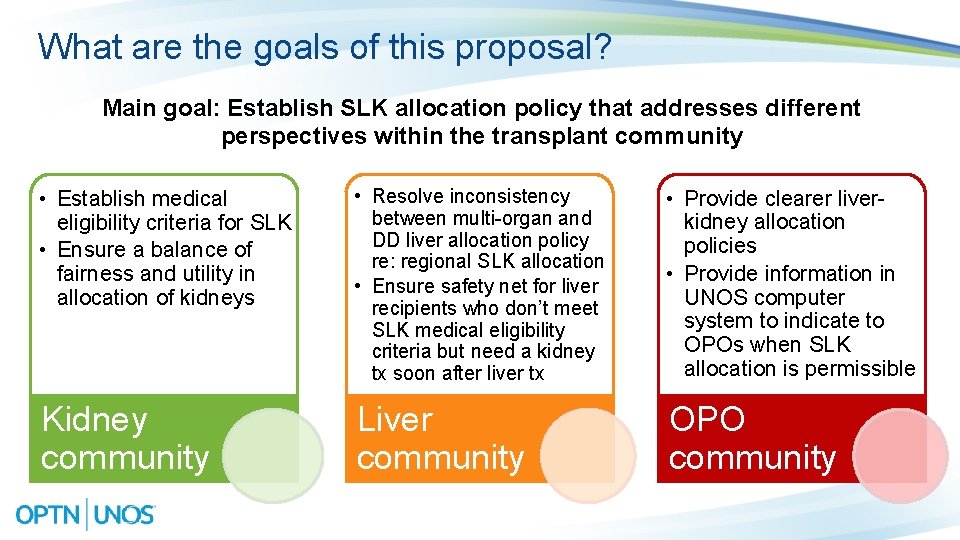
What are the goals of this proposal? Main goal: Establish SLK allocation policy that addresses different perspectives within the transplant community • Establish medical eligibility criteria for SLK • Ensure a balance of fairness and utility in allocation of kidneys • Resolve inconsistency between multi-organ and DD liver allocation policy re: regional SLK allocation • Ensure safety net for liver recipients who don’t meet SLK medical eligibility criteria but need a kidney tx soon after liver tx • Provide clearer liverkidney allocation policies • Provide information in UNOS computer system to indicate to OPOs when SLK allocation is permissible Kidney community Liver community OPO community
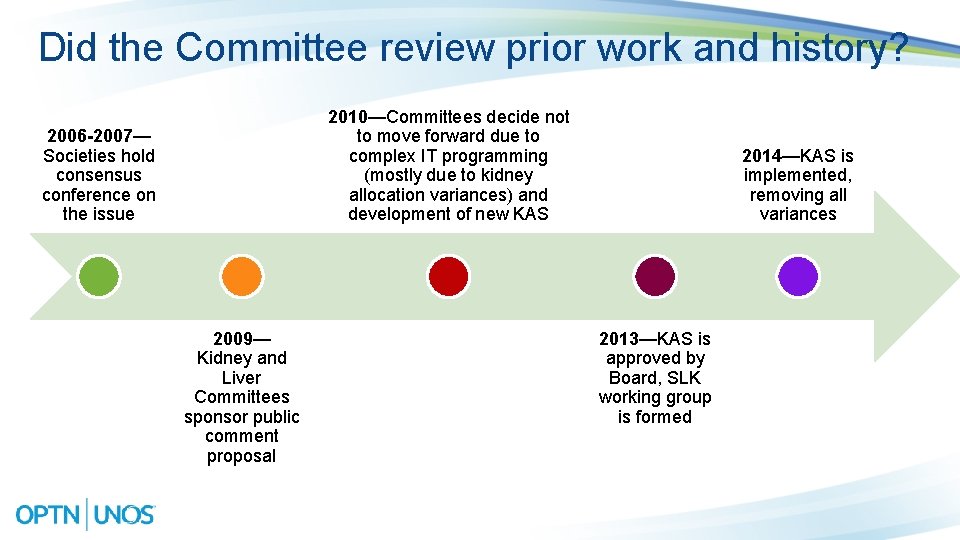
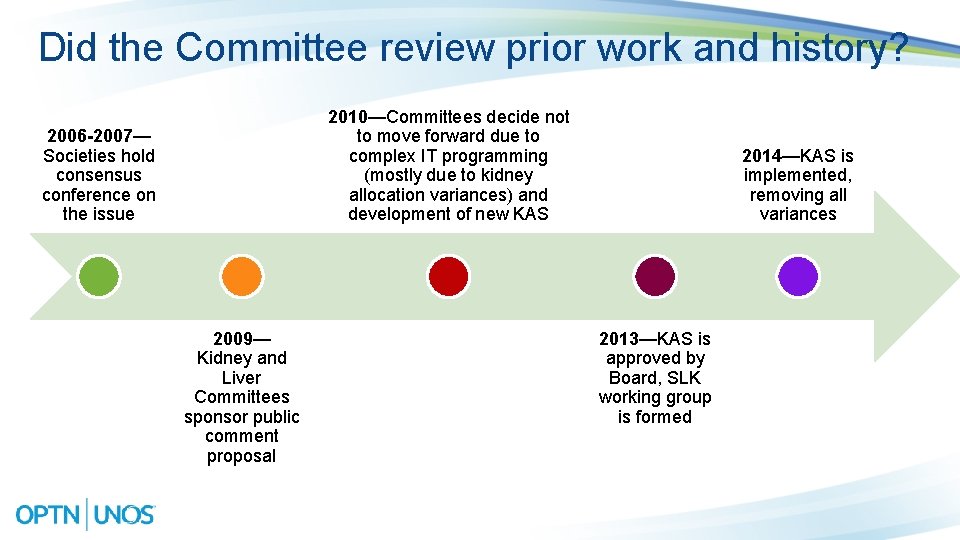
Did the Committee review prior work and history? 2010—Committees decide not to move forward due to complex IT programming (mostly due to kidney allocation variances) and development of new KAS 2006 -2007— Societies hold consensus conference on the issue 2009— Kidney and Liver Committees sponsor public comment proposal 2014—KAS is implemented, removing all variances 2013—KAS is approved by Board, SLK working group is formed
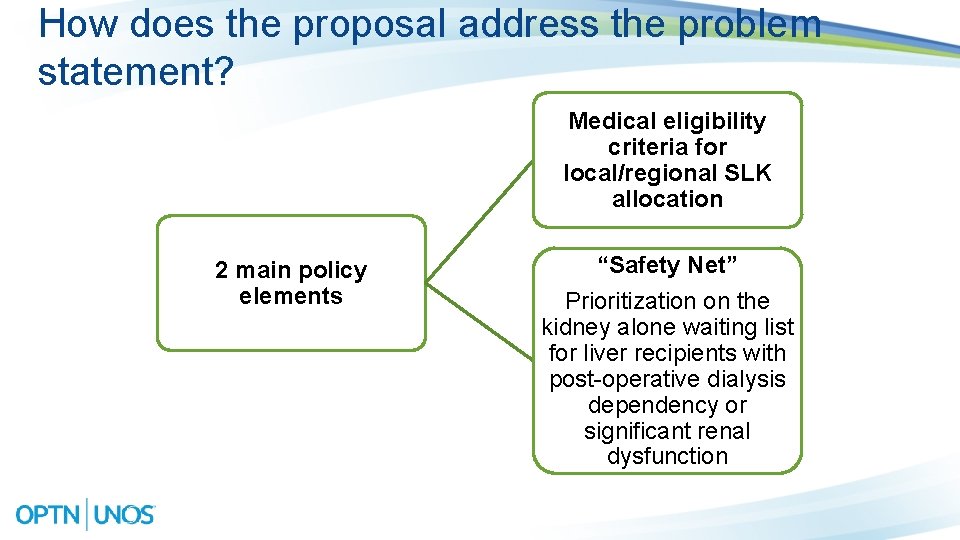
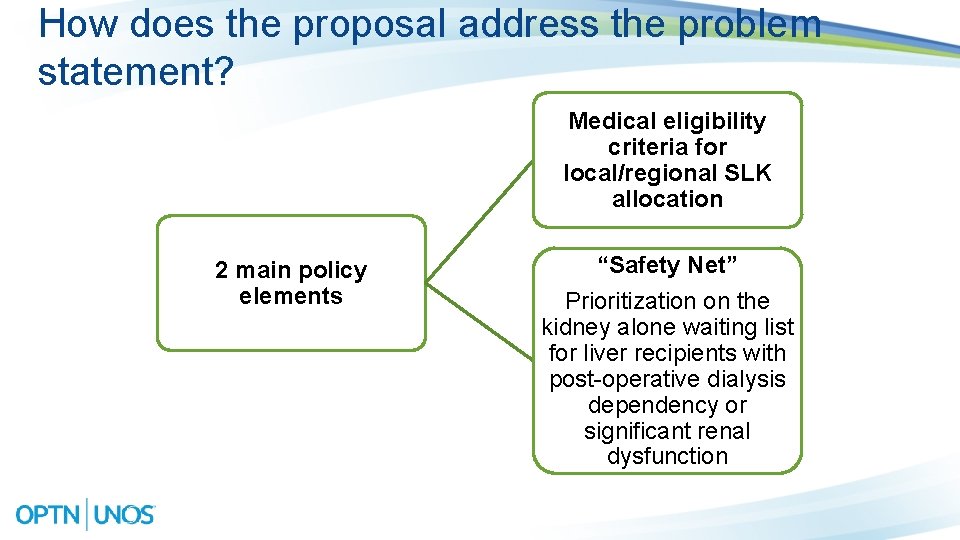
How does the proposal address the problem statement? Medical eligibility criteria for local/regional SLK allocation 2 main policy elements “Safety Net” Prioritization on the kidney alone waiting list for liver recipients with post-operative dialysis dependency or significant renal dysfunction
SLK Medical Eligibility Criteria 7
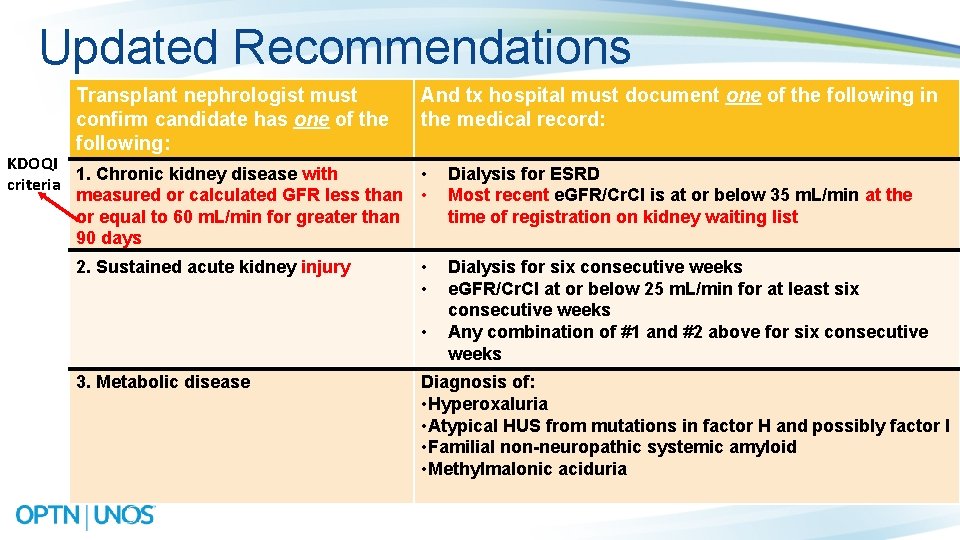
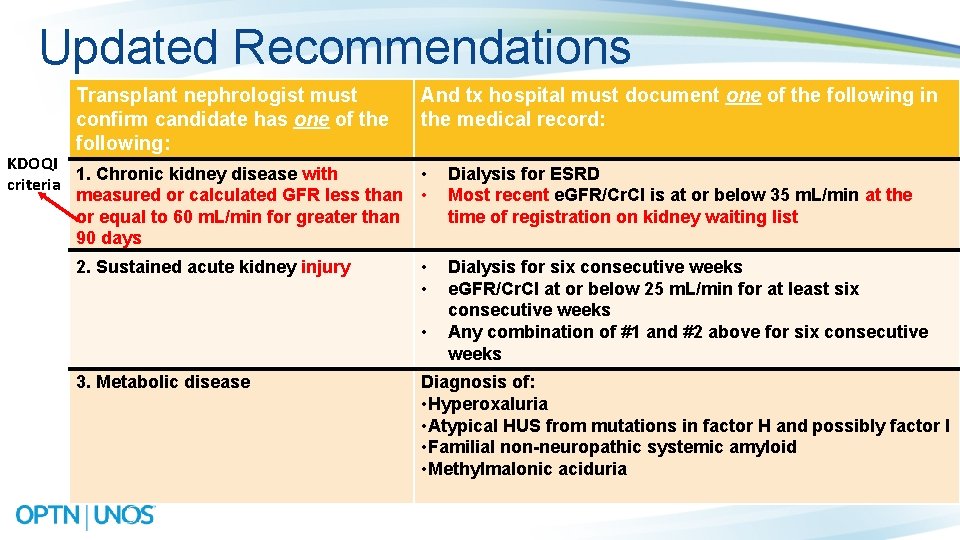
Updated Recommendations Transplant nephrologist must confirm candidate has one of the following: KDOQI 1. Chronic kidney disease with criteria measured or calculated GFR less than or equal to 60 m. L/min for greater than 90 days 2. Sustained acute kidney injury And tx hospital must document one of the following in the medical record: • • Dialysis for ESRD Most recent e. GFR/Cr. Cl is at or below 35 m. L/min at the time of registration on kidney waiting list • • Dialysis for six consecutive weeks e. GFR/Cr. Cl at or below 25 m. L/min for at least six consecutive weeks Any combination of #1 and #2 above for six consecutive weeks • 3. Metabolic disease Diagnosis of: • Hyperoxaluria • Atypical HUS from mutations in factor H and possibly factor I • Familial non-neuropathic systemic amyloid • Methylmalonic aciduria
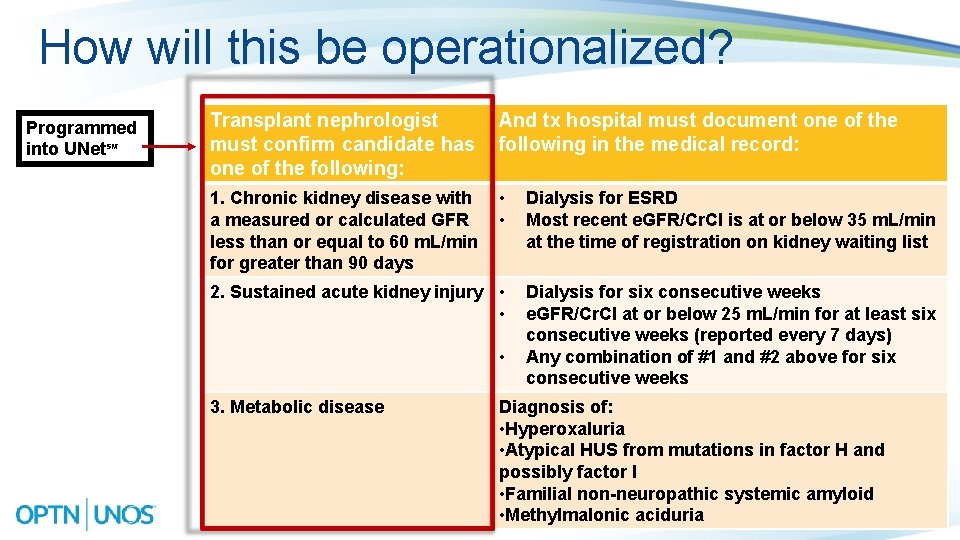
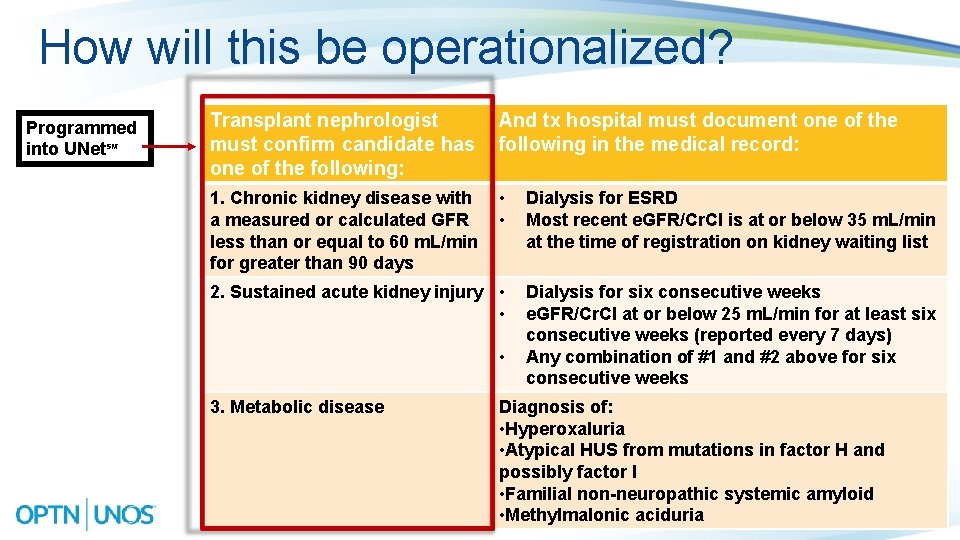
How will this be operationalized? Programmed into UNet℠ Transplant nephrologist must confirm candidate has one of the following: And tx hospital must document one of the following in the medical record: 1. Chronic kidney disease with a measured or calculated GFR less than or equal to 60 m. L/min for greater than 90 days • • Dialysis for ESRD Most recent e. GFR/Cr. Cl is at or below 35 m. L/min at the time of registration on kidney waiting list 2. Sustained acute kidney injury • • Dialysis for six consecutive weeks e. GFR/Cr. Cl at or below 25 m. L/min for at least six consecutive weeks (reported every 7 days) Any combination of #1 and #2 above for six consecutive weeks • 3. Metabolic disease Diagnosis of: • Hyperoxaluria • Atypical HUS from mutations in factor H and possibly factor I • Familial non-neuropathic systemic amyloid • Methylmalonic aciduria
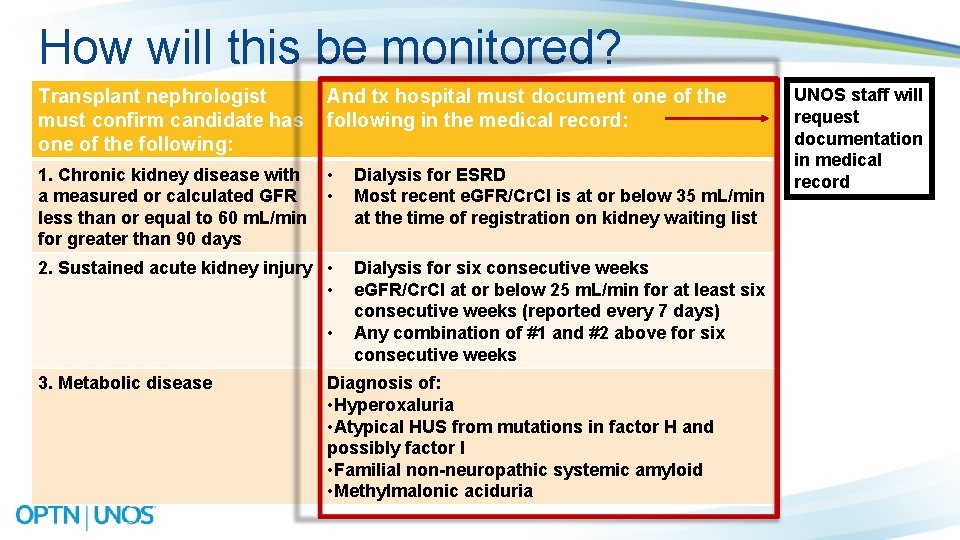
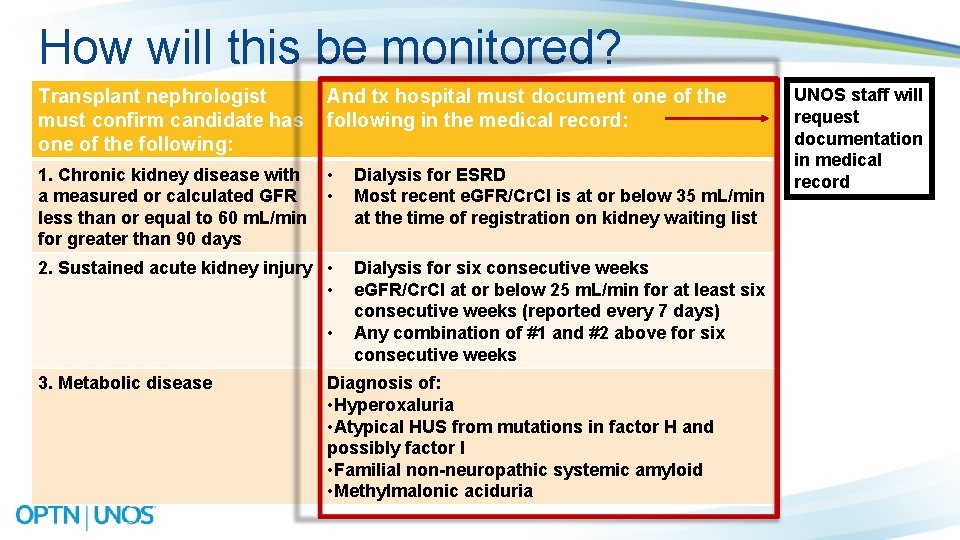
How will this be monitored? Transplant nephrologist must confirm candidate has one of the following: And tx hospital must document one of the following in the medical record: 1. Chronic kidney disease with a measured or calculated GFR less than or equal to 60 m. L/min for greater than 90 days • • Dialysis for ESRD Most recent e. GFR/Cr. Cl is at or below 35 m. L/min at the time of registration on kidney waiting list 2. Sustained acute kidney injury • • Dialysis for six consecutive weeks e. GFR/Cr. Cl at or below 25 m. L/min for at least six consecutive weeks (reported every 7 days) Any combination of #1 and #2 above for six consecutive weeks • 3. Metabolic disease Diagnosis of: • Hyperoxaluria • Atypical HUS from mutations in factor H and possibly factor I • Familial non-neuropathic systemic amyloid • Methylmalonic aciduria UNOS staff will request documentation in medical record
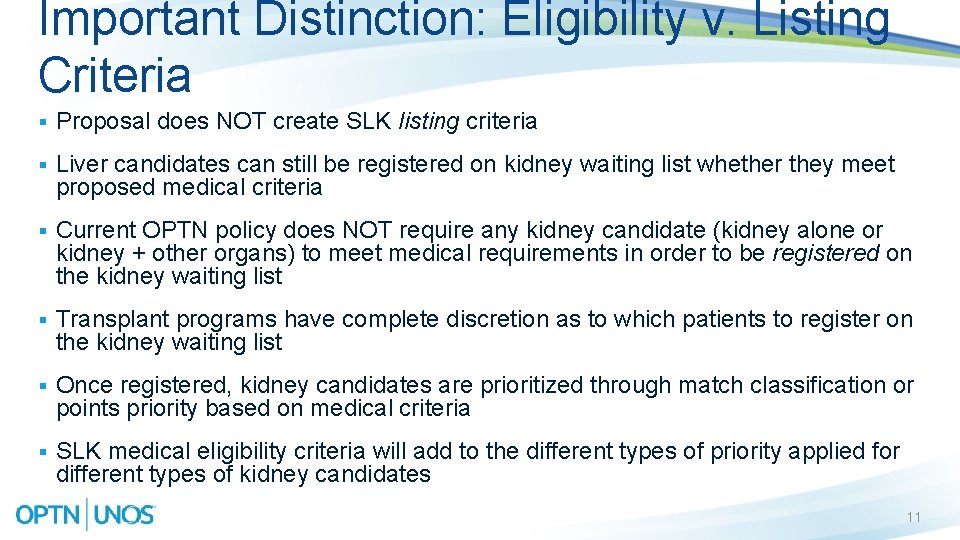
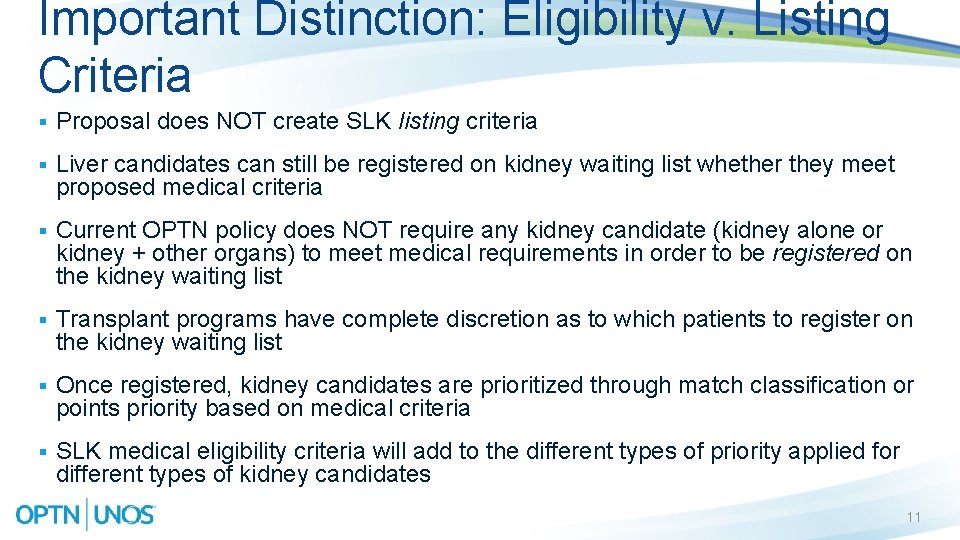
Important Distinction: Eligibility v. Listing Criteria § Proposal does NOT create SLK listing criteria § Liver candidates can still be registered on kidney waiting list whether they meet proposed medical criteria § Current OPTN policy does NOT require any kidney candidate (kidney alone or kidney + other organs) to meet medical requirements in order to be registered on the kidney waiting list § Transplant programs have complete discretion as to which patients to register on the kidney waiting list § Once registered, kidney candidates are prioritized through match classification or points priority based on medical criteria § SLK medical eligibility criteria will add to the different types of priority applied for different types of kidney candidates 11
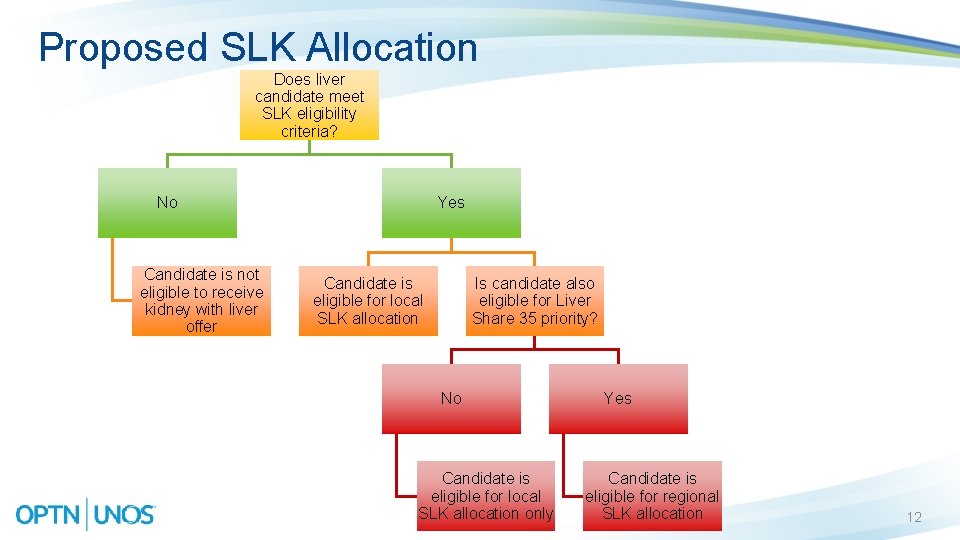
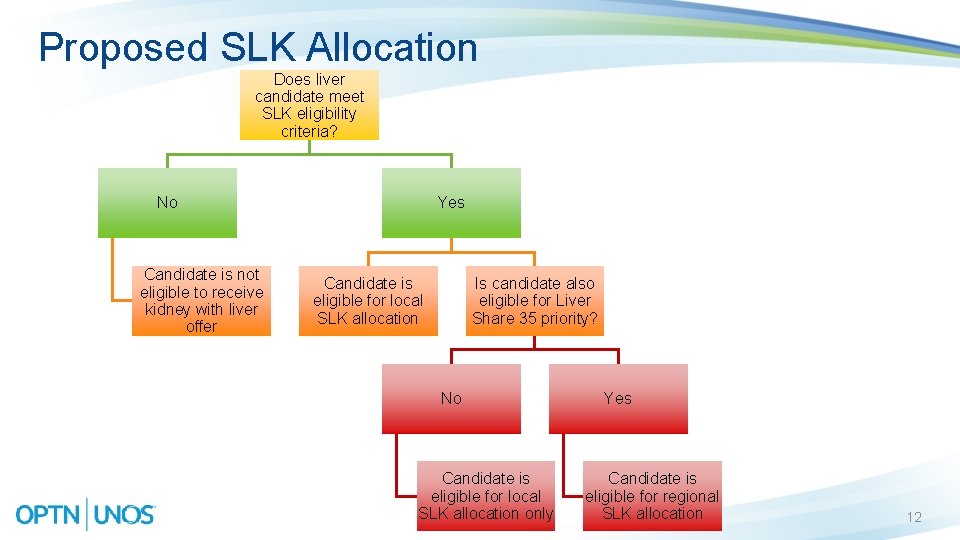
Proposed SLK Allocation Does liver candidate meet SLK eligibility criteria? No Candidate is not eligible to receive kidney with liver offer Yes Candidate is eligible for local SLK allocation Is candidate also eligible for Liver Share 35 priority? No Candidate is eligible for local SLK allocation only Yes Candidate is eligible for regional SLK allocation 12
Anticipated Post-Public Comment Changes—SLK Allocation Due to recent feedback from Liver Committee, the following policy clarifications are actively under construction: • Clarifying that local SLK candidates must only meet medical eligibility criteria in order to be eligible • Amending proposal so that it will not apply to pediatric SLK candidates • Specifying that OPO must extend SLK offers to eligible Share 35 candidates in the host OPO’s region if offering to liver/kidney candidates Specific feedback needed on one element: • Under what circumstances should national SLK candidates receive priority? 13
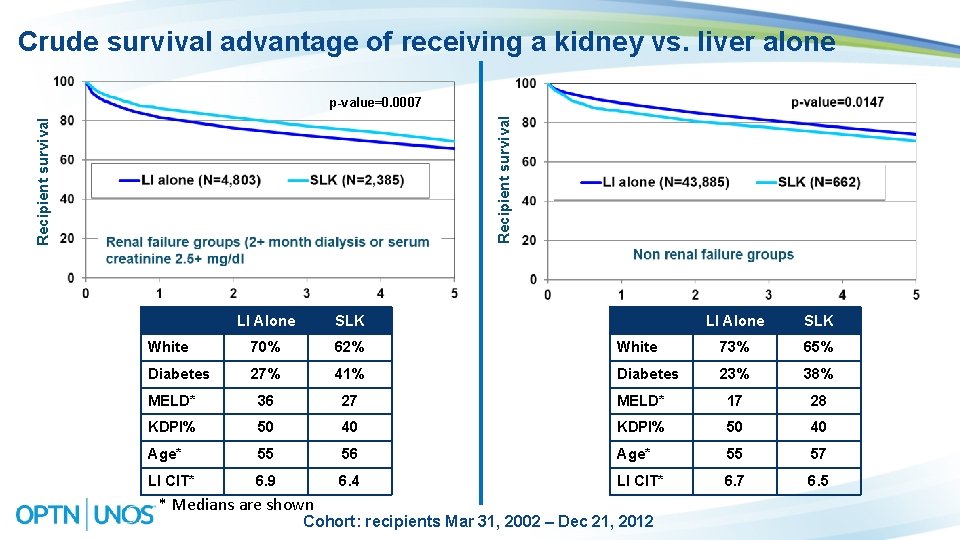
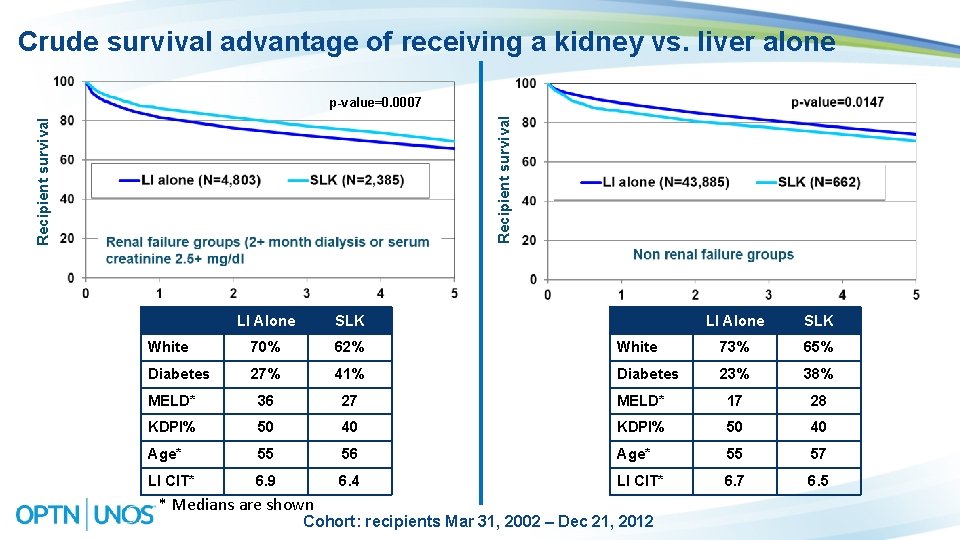
Crude survival advantage of receiving a kidney vs. liver alone Recipient survival p-value=0. 0007 LI Alone SLK White 70% 62% White 73% 65% Diabetes 27% 41% Diabetes 23% 38% MELD* 36 27 MELD* 17 28 KDPI% 50 40 Age* 55 56 Age* 55 57 LI CIT* 6. 9 6. 4 LI CIT* 6. 7 6. 5 * Medians are shown Cohort: recipients Mar 31, 2002 – Dec 21, 2012
How Multi-Organ Involving KI works § If OPO recovers a kidney with liver, heart, lung, or pancreas, must allocate kidney locally as part of local multi-organ combination § OPO has discretion to choose between following combinations: § § Local heart/kidney candidate Local liver/kidney candidate Local lung/kidney candidate Pancreas/kidney candidates (local through regional/national zero mismatch offers) 15
How Multi-Organ Involving KI Will Work if Approved § If OPO recovers a kidney with liver, heart, lung, or pancreas, must allocate kidney locally as part of local multi-organ combination § OPO has discretion to choose between following combinations: § § Local heart/kidney candidate Local liver/kidney candidate (eligible local/regional offers) Local lung/kidney candidate Pancreas/kidney candidates (local through regional/national zero mismatch offers) 16
SLK ‘Safety Net’ Policy 17
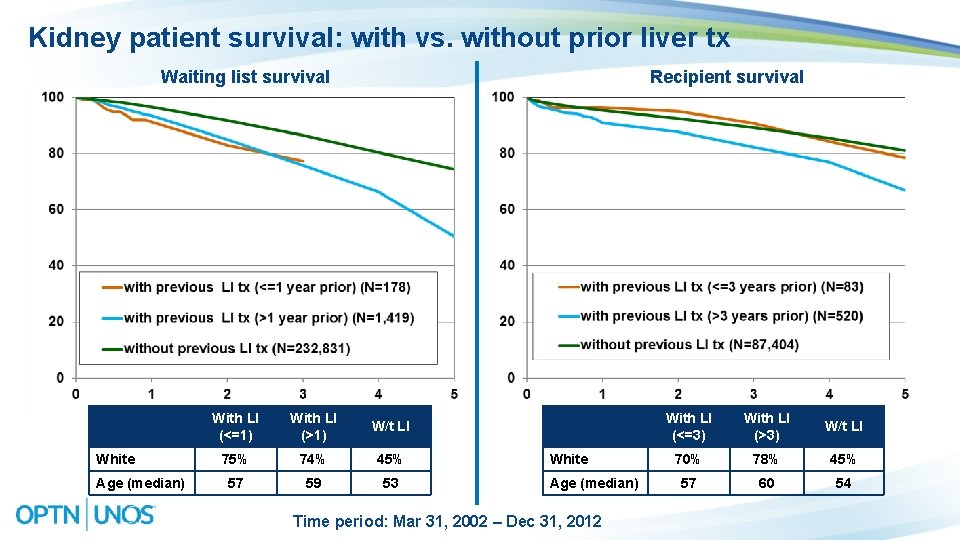
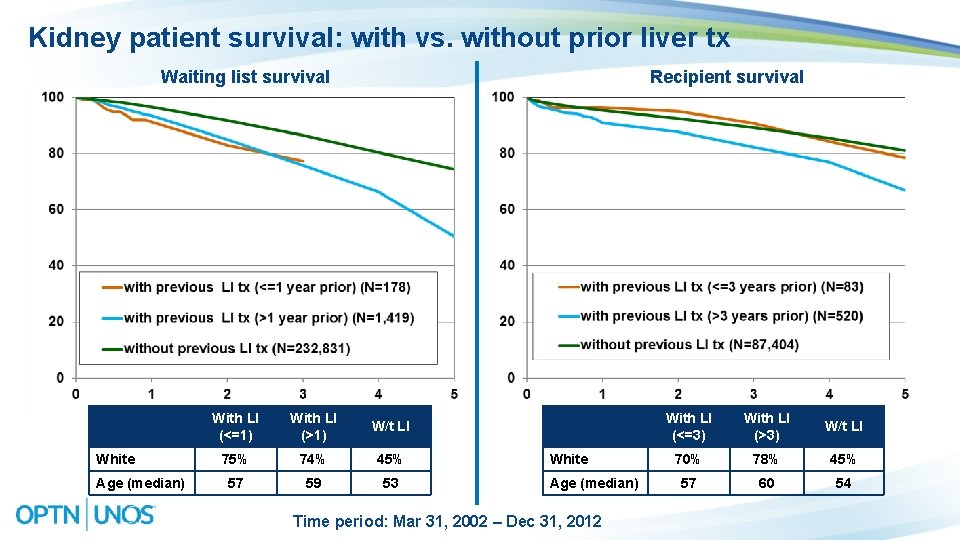
Kidney patient survival: with vs. without prior liver tx Waiting list survival White Age (median) Recipient survival With LI (<=1) With LI (>1) W/t LI 75% 74% 45% 57 59 53 White Age (median) Time period: Mar 31, 2002 – Dec 31, 2012 With LI (<=3) With LI (>3) W/t LI 70% 78% 45% 57 60 54
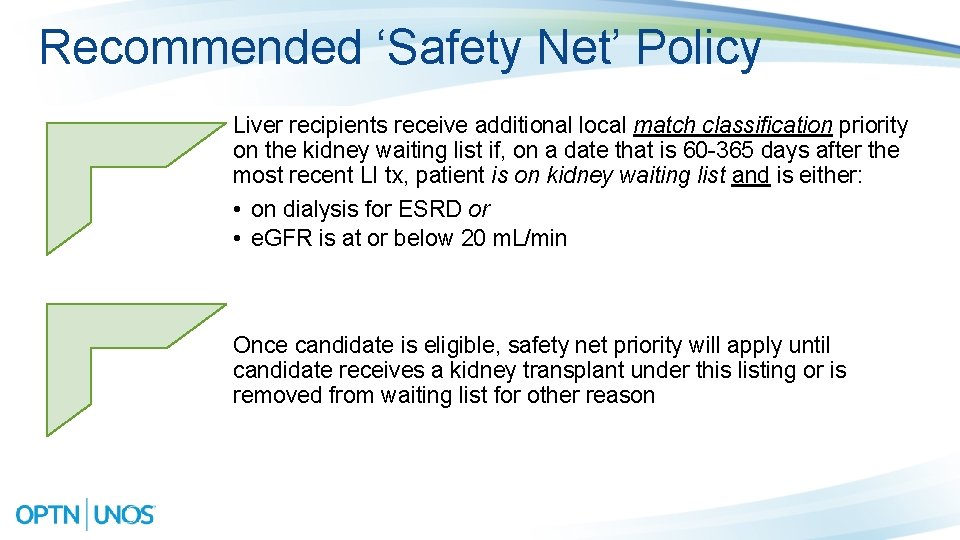
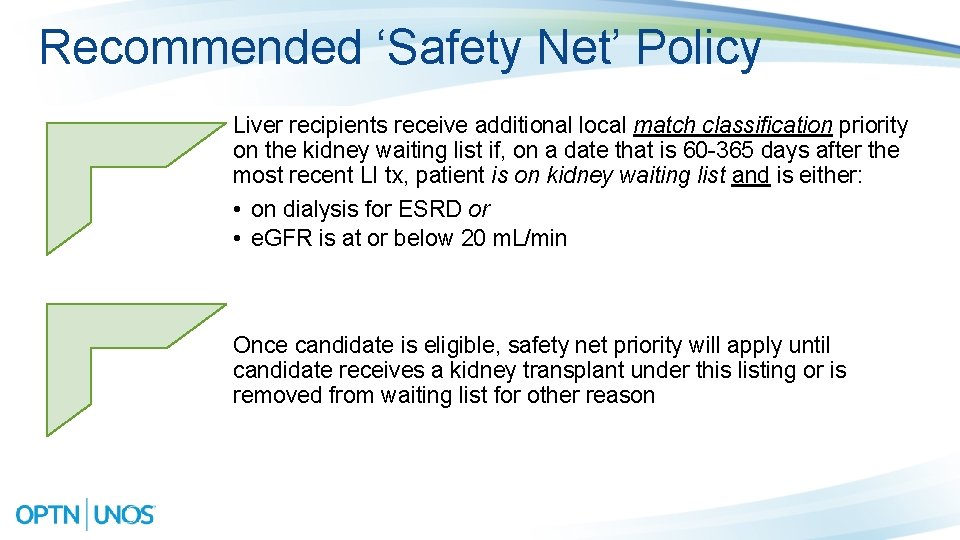
Recommended ‘Safety Net’ Policy Liver recipients receive additional local match classification priority on the kidney waiting list if, on a date that is 60 -365 days after the most recent LI tx, patient is on kidney waiting list and is either: • on dialysis for ESRD or • e. GFR is at or below 20 m. L/min Once candidate is eligible, safety net priority will apply until candidate receives a kidney transplant under this listing or is removed from waiting list for other reason
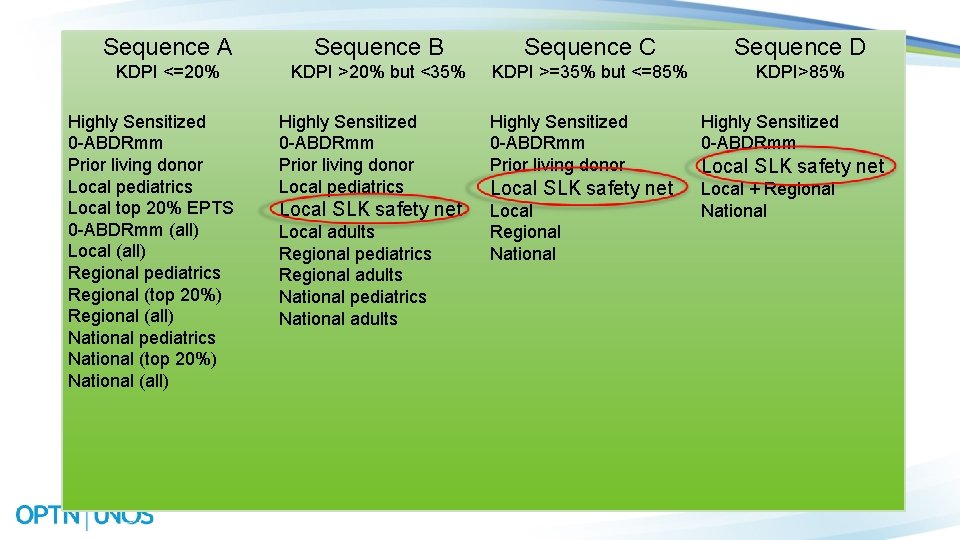
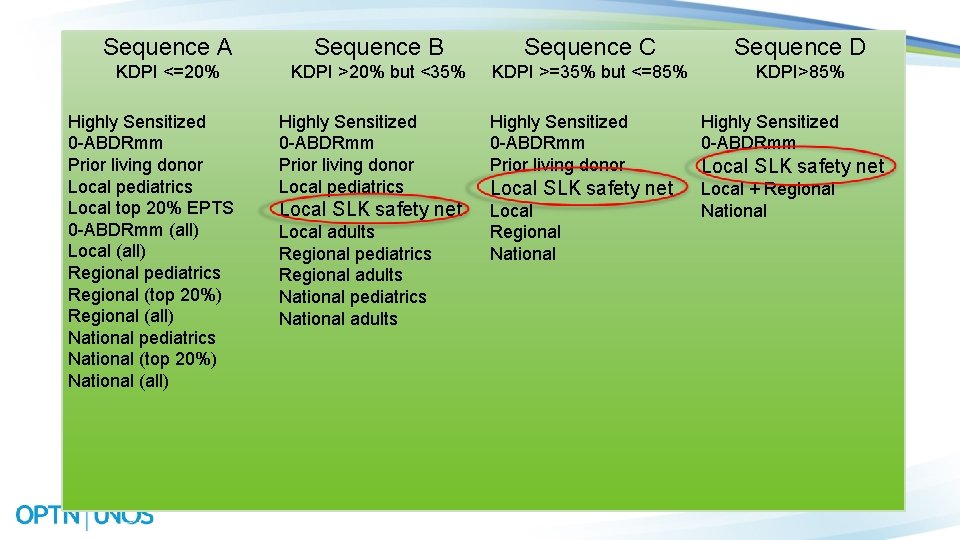
Sequence A Sequence B Sequence C Sequence D KDPI <=20% KDPI >20% but <35% KDPI >=35% but <=85% KDPI>85% Highly Sensitized 0 -ABDRmm Prior living donor Local pediatrics Local top 20% EPTS 0 -ABDRmm (all) Local (all) Regional pediatrics Regional (top 20%) Regional (all) National pediatrics National (top 20%) National (all) Highly Sensitized 0 -ABDRmm Prior living donor Local pediatrics Highly Sensitized 0 -ABDRmm Prior living donor Highly Sensitized 0 -ABDRmm Local SLK safety net Local Regional National Local + Regional National Local adults Regional pediatrics Regional adults National pediatrics National adults Local SLK safety net
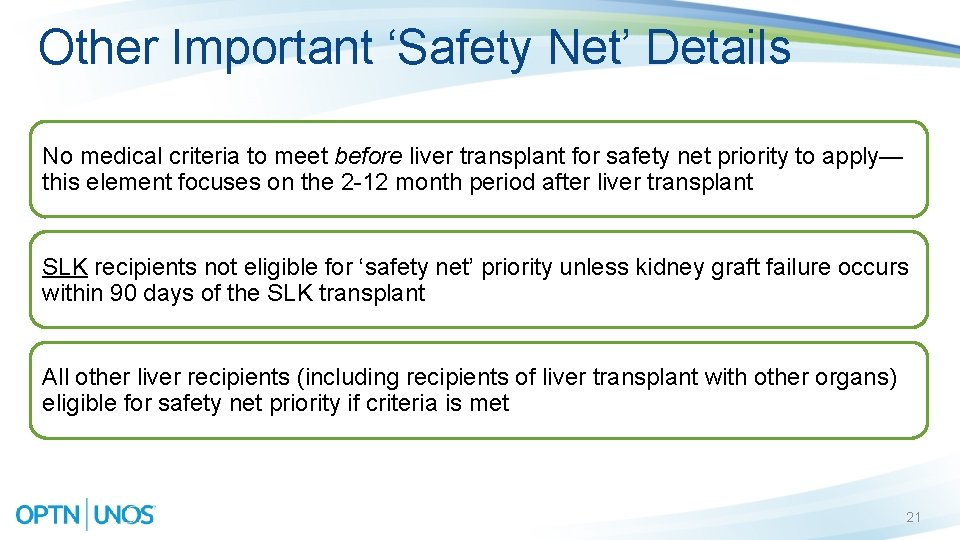
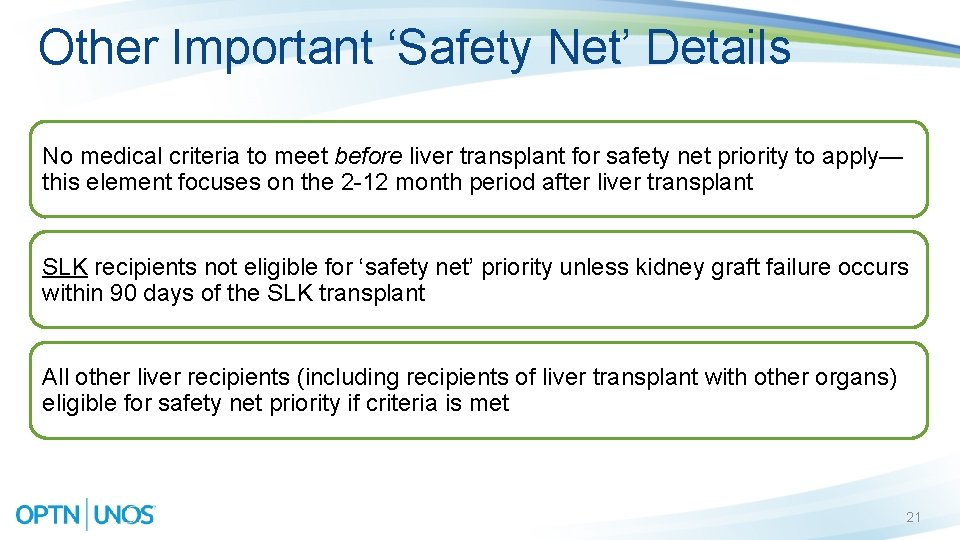
Other Important ‘Safety Net’ Details No medical criteria to meet before liver transplant for safety net priority to apply— this element focuses on the 2 -12 month period after liver transplant SLK recipients not eligible for ‘safety net’ priority unless kidney graft failure occurs within 90 days of the SLK transplant All other liver recipients (including recipients of liver transplant with other organs) eligible for safety net priority if criteria is met 21
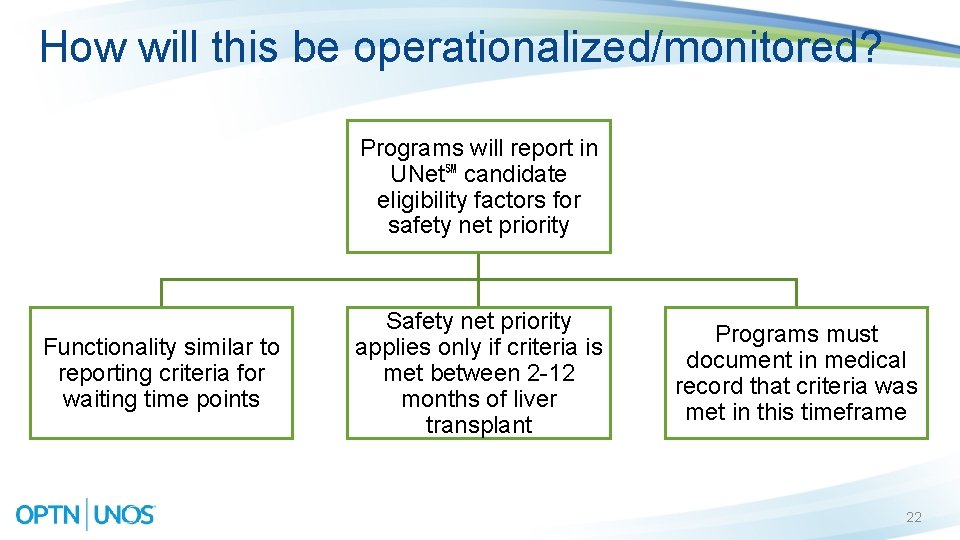
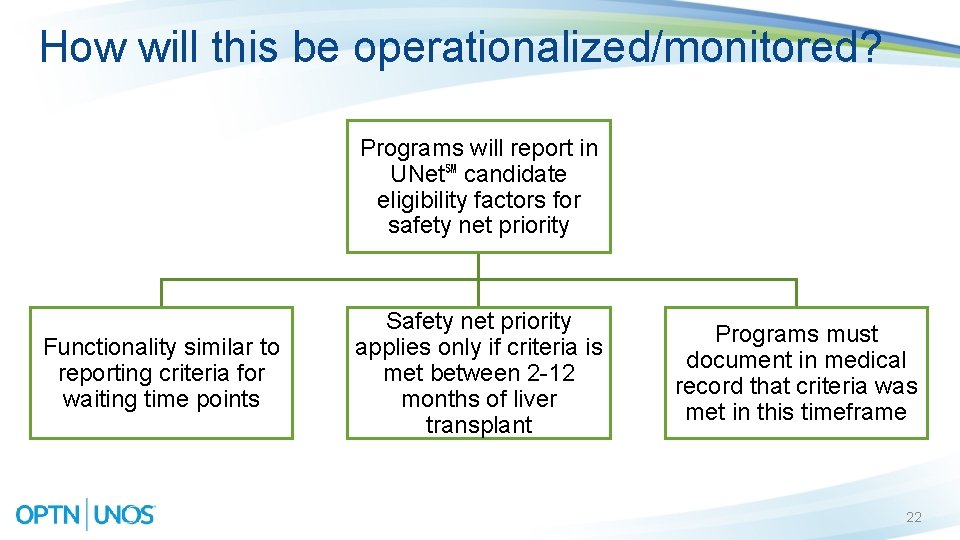
How will this be operationalized/monitored? Programs will report in UNet℠ candidate eligibility factors for safety net priority Functionality similar to reporting criteria for waiting time points Safety net priority applies only if criteria is met between 2 -12 months of liver transplant Programs must document in medical record that criteria was met in this timeframe 22
How does this proposal support the OPTN Strategic Plan? 2015 -2018 OPTN Strategic Plan Goal: Increase equity in access to transplants Objective: Establish clearer rules for allocation of multiple organs to a single candidate, especially liver-kidney candidates 23
Questions? Mark Aeder, MD Committee Chair mark. aeder@uhhospitals. org Gena Boyle Project Liaison gena. boyle@unos. org 24
Extra SLK slides 25
Who did the Committee collaborate with? Ethics, OPO, Liver, Minority Affairs, & Ops and Safety committees OPTN Regions ASTS NKF AUA 26
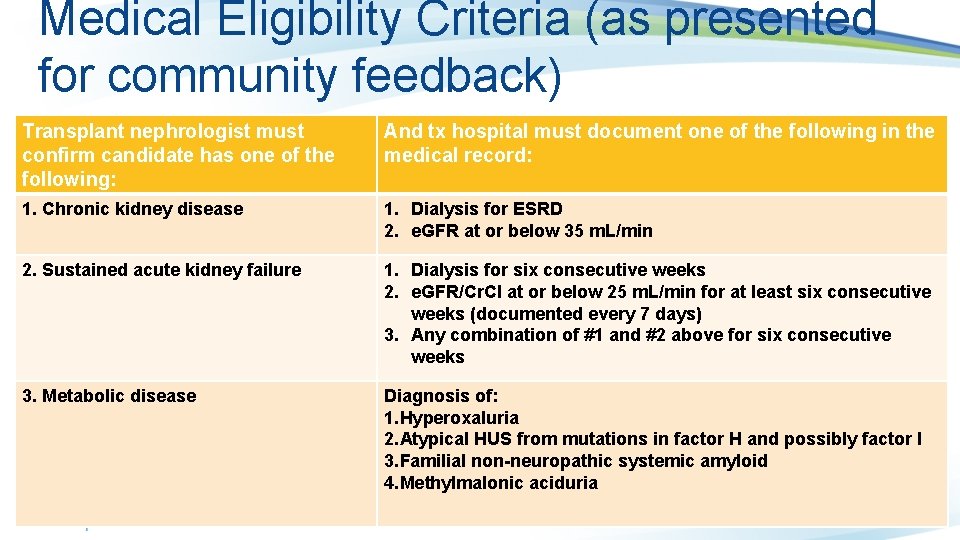
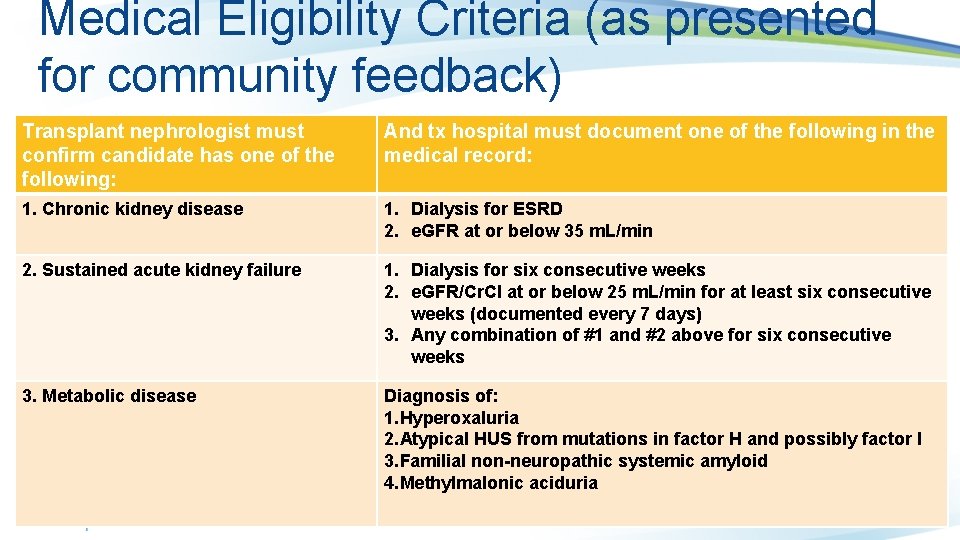
Medical Eligibility Criteria (as presented for community feedback) Transplant nephrologist must confirm candidate has one of the following: And tx hospital must document one of the following in the medical record: 1. Chronic kidney disease 1. Dialysis for ESRD 2. e. GFR at or below 35 m. L/min 2. Sustained acute kidney failure 1. Dialysis for six consecutive weeks 2. e. GFR/Cr. Cl at or below 25 m. L/min for at least six consecutive weeks (documented every 7 days) 3. Any combination of #1 and #2 above for six consecutive weeks 3. Metabolic disease Diagnosis of: 1. Hyperoxaluria 2. Atypical HUS from mutations in factor H and possibly factor I 3. Familial non-neuropathic systemic amyloid 4. Methylmalonic aciduria
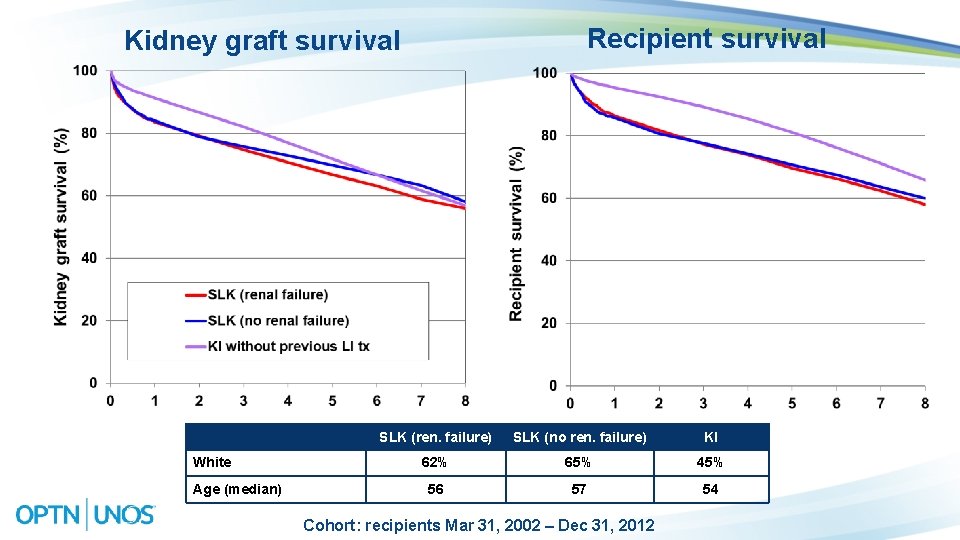
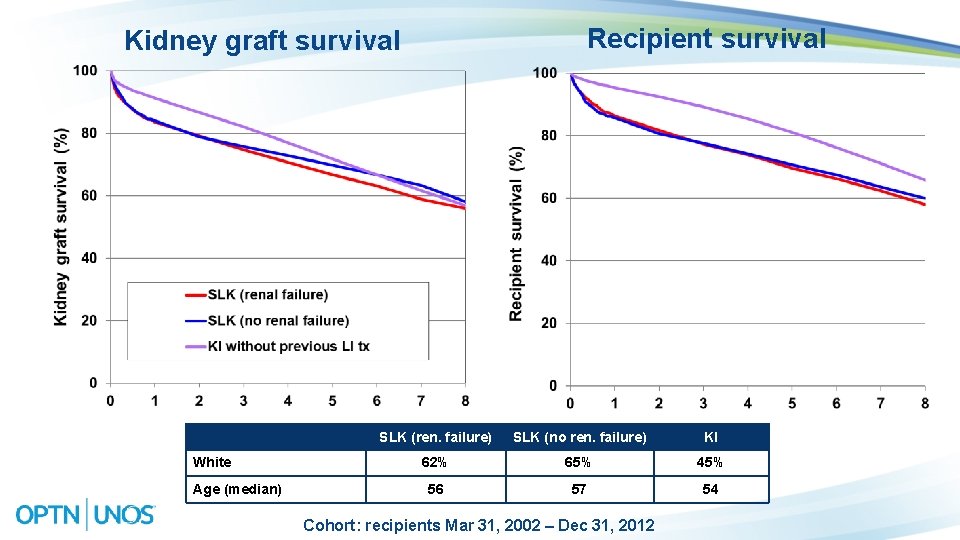
Recipient survival Kidney graft survival White Age (median) SLK (ren. failure) SLK (no ren. failure) KI 62% 65% 45% 56 57 54 Cohort: recipients Mar 31, 2002 – Dec 31, 2012
Regional Feedback (SLK medical eligibility criteria) Medical criteria for CKD needs to be spelled out Specify a duration for GFR Require more than one GFR measurement over a period of time for CKD Require specific GFR measurement to ensure consistency 29
Constituency Group Feedback (SLK medical eligibility criteria) AST • Generally supportive • Concerned CKD definition does not contain time component; suggested adopting NKF KDOQI criteria (90 days) • Requested requiring a consistent method of measuring GFR NKF • Supports updated criteria, especially having nephrologist confirm candidate diagnosis • Remain concerned with category #2 being labeled as ‘kidney failure’, would suggest it be re-labeled AUA • Generally rejected notion that SLK recipients have better outcomes if receiving both organs from the same donor and would encourage use of living donors in this setting instead of SLK 30
Regional Feedback (Safety Net) Several regions supported proposal because of inclusion of safety net Concerns it may be disincentive for liver recipient to find a living KI donor Suggestion to distinguish between medical need for the kidney pre and post liver Tx Suggestion priority should not apply for Sequence B, only for C & D (KDPI greater than 35%) Suggestion to expand priority beyond the local level
Constituency Group Feedback (Safety Net) NKF • Strongly support • Appreciative of the changes made since 2009 proposal AUA • No comments on ‘safety net’ priority AST • Support ‘safety net’ prioritization • Requested Committee consider no priority for sequence B (KDPI 21 -34%) because it could be disincentive for candidate to seek a living donor 32
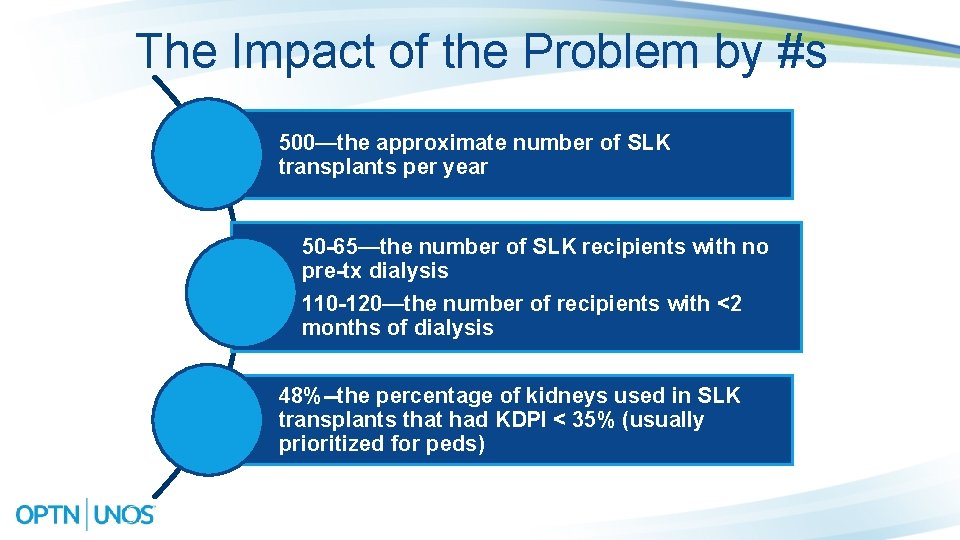
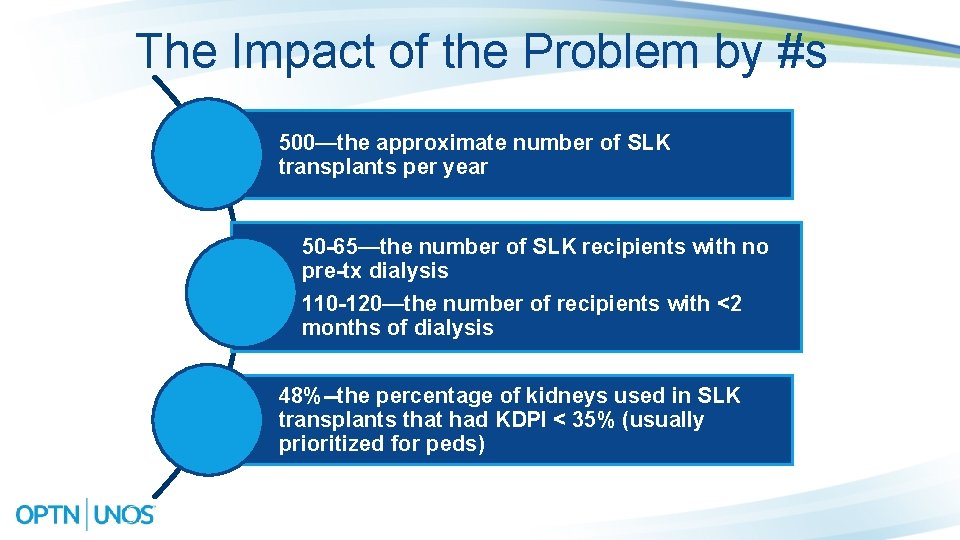
The Impact of the Problem by #s 500—the approximate number of SLK transplants per year 50 -65—the number of SLK recipients with no pre-tx dialysis 110 -120—the number of recipients with <2 months of dialysis 48%--the percentage of kidneys used in SLK transplants that had KDPI < 35% (usually prioritized for peds)
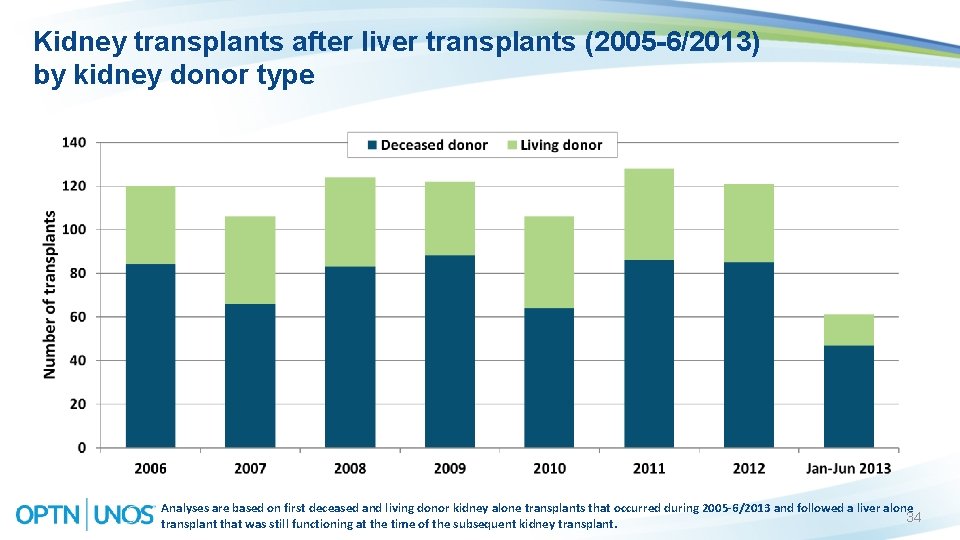
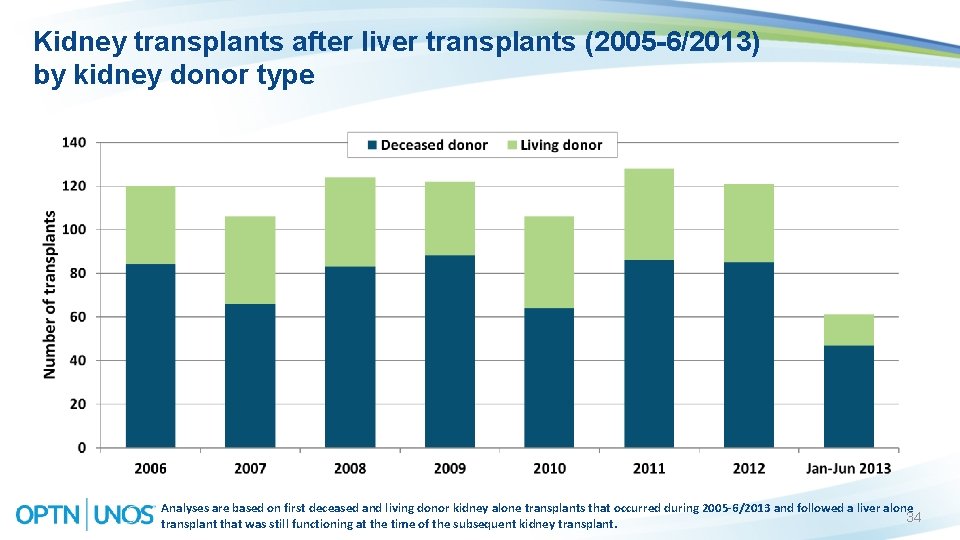
Kidney transplants after liver transplants (2005 -6/2013) by kidney donor type Analyses are based on first deceased and living donor kidney alone transplants that occurred during 2005 -6/2013 and followed a liver alone 34 transplant that was still functioning at the time of the subsequent kidney transplant.
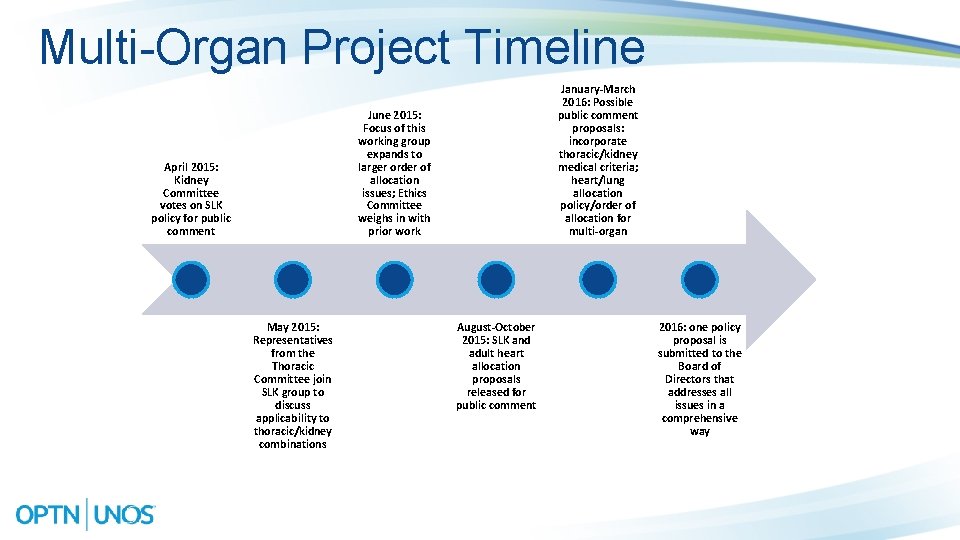
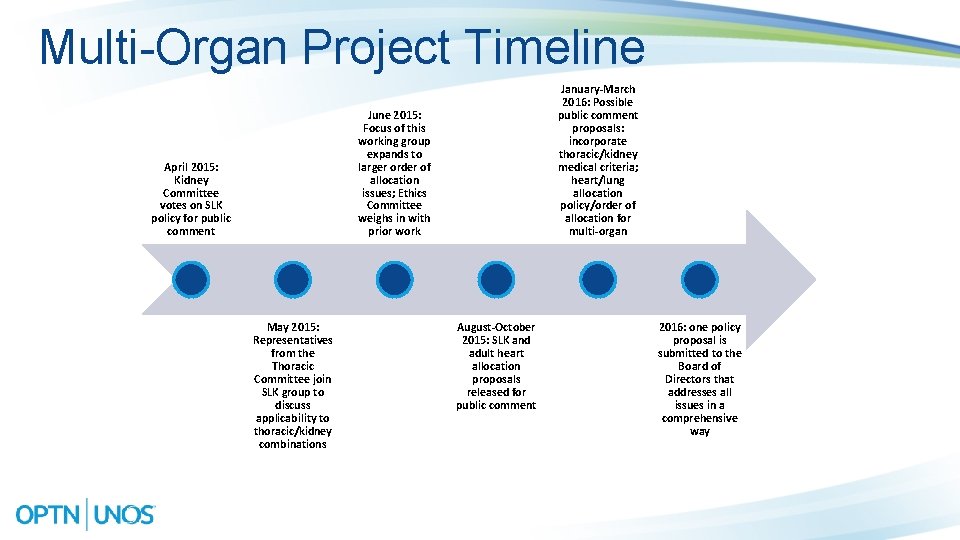
Multi-Organ Project Timeline January-March 2016: Possible public comment proposals: incorporate thoracic/kidney medical criteria; heart/lung allocation policy/order of allocation for multi-organ June 2015: Focus of this working group expands to larger order of allocation issues; Ethics Committee weighs in with prior work April 2015: Kidney Committee votes on SLK policy for public comment May 2015: Representatives from the Thoracic Committee join SLK group to discuss applicability to thoracic/kidney combinations August-October 2015: SLK and adult heart allocation proposals released for public comment 2016: one policy proposal is submitted to the Board of Directors that addresses all issues in a comprehensive way
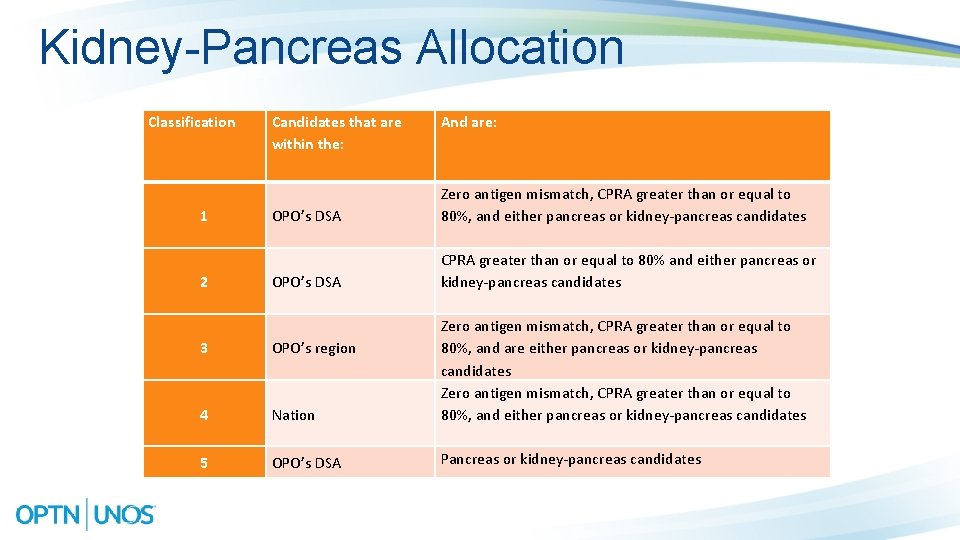
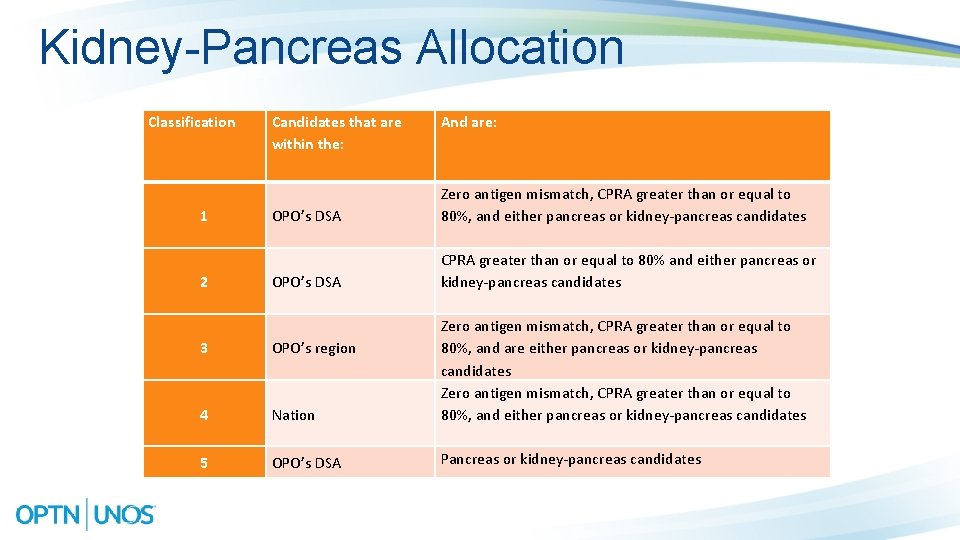
Kidney-Pancreas Allocation Classification 1 2 Candidates that are within the: And are: OPO’s DSA Zero antigen mismatch, CPRA greater than or equal to 80%, and either pancreas or kidney-pancreas candidates OPO’s DSA CPRA greater than or equal to 80% and either pancreas or kidney-pancreas candidates 3 OPO’s region 4 Nation Zero antigen mismatch, CPRA greater than or equal to 80%, and are either pancreas or kidney-pancreas candidates Zero antigen mismatch, CPRA greater than or equal to 80%, and either pancreas or kidney-pancreas candidates 5 OPO’s DSA Pancreas or kidney-pancreas candidates