Kidney Transplantation Committee Spring 2015 Revised Kidney Allocation



- Slides: 28
Kidney Transplantation Committee Spring 2015
Revised Kidney Allocation System § Implemented Dec. 4, 2014 § 6 month data will be shared at Aug-Oct regional meetings § Monitoring community feedback to determine where clarification and tweaks may be needed in policy and UNet℠
How will KAS be monitored? 17+ data analyses, including: § Longevity matching: are fewer age or longevitymismatched transplants occurring? § Access: are high CPRA and blood type B patients getting more offers and transplants? What is the distribution of transplants by recipient age? § Utilization: have kidney discard rates decreased, in particular for high KDPI kidneys?
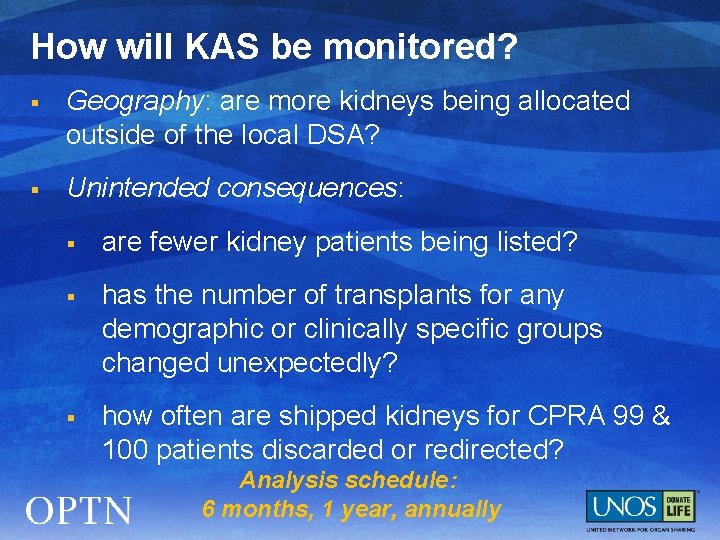
How will KAS be monitored? § Geography: are more kidneys being allocated outside of the local DSA? § Unintended consequences: § are fewer kidney patients being listed? § has the number of transplants for any demographic or clinically specific groups changed unexpectedly? § how often are shipped kidneys for CPRA 99 & 100 patients discarded or redirected? Analysis schedule: 6 months, 1 year, annually
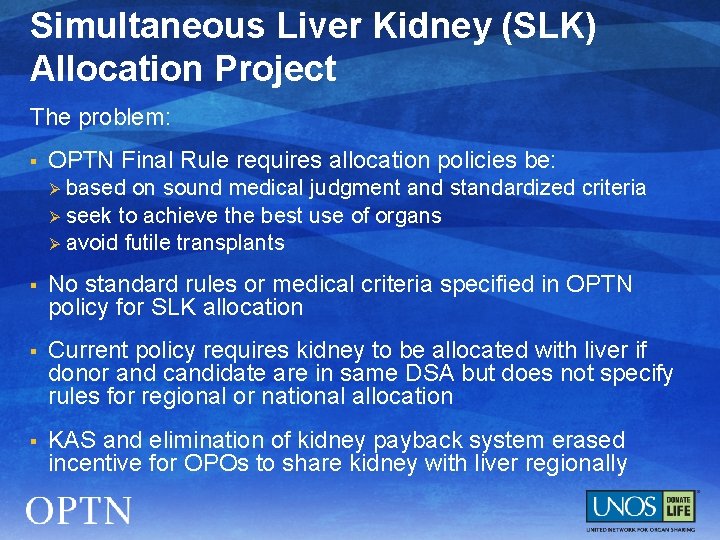
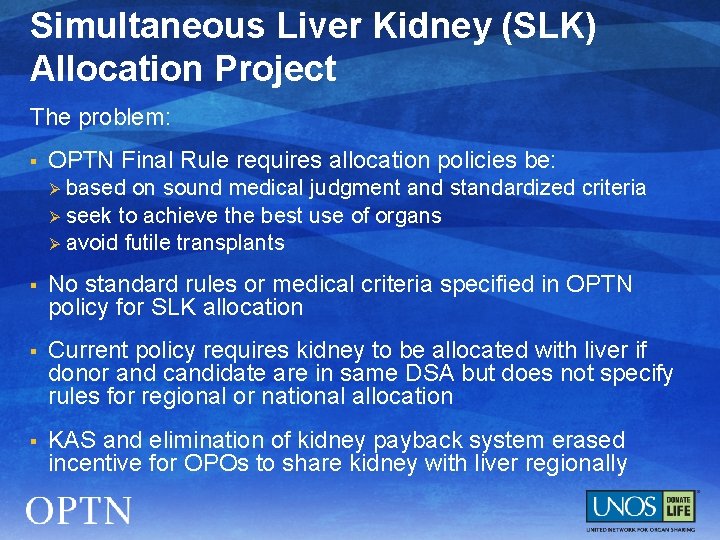
Simultaneous Liver Kidney (SLK) Allocation Project The problem: § OPTN Final Rule requires allocation policies be: based on sound medical judgment and standardized criteria Ø seek to achieve the best use of organs Ø avoid futile transplants Ø § No standard rules or medical criteria specified in OPTN policy for SLK allocation § Current policy requires kidney to be allocated with liver if donor and candidate are in same DSA but does not specify rules for regional or national allocation § KAS and elimination of kidney payback system erased incentive for OPOs to share kidney with liver regionally
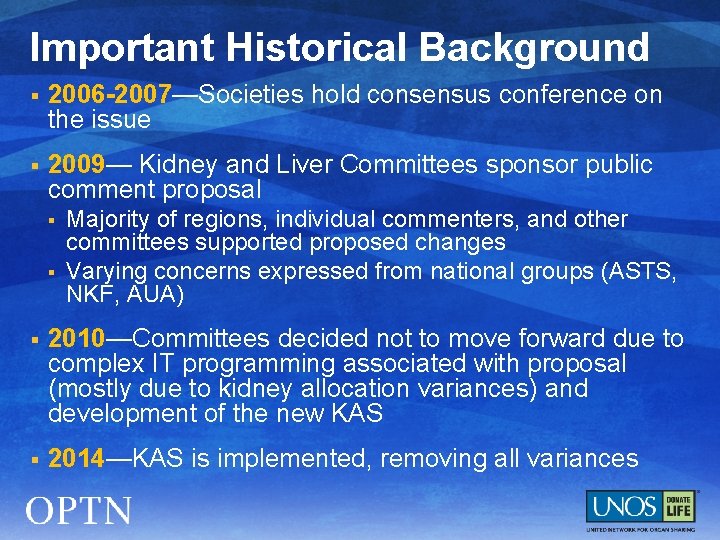
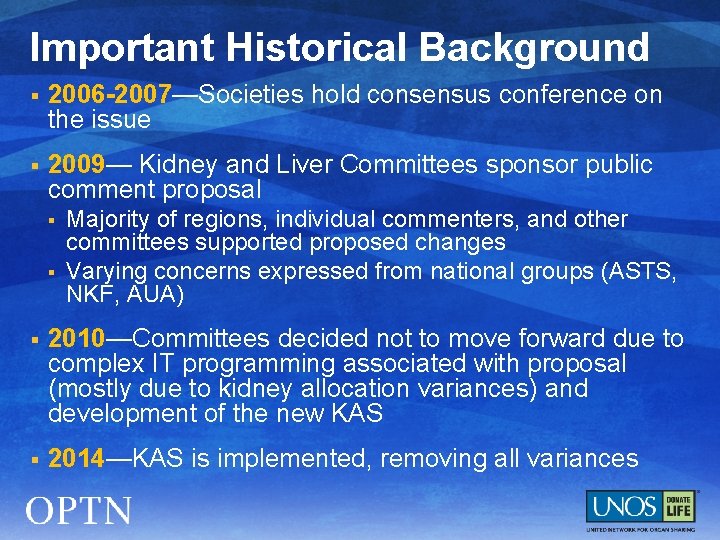
Important Historical Background § 2006 -2007—Societies hold consensus conference on the issue § 2009— Kidney and Liver Committees sponsor public comment proposal § § Majority of regions, individual commenters, and other committees supported proposed changes Varying concerns expressed from national groups (ASTS, NKF, AUA) § 2010—Committees decided not to move forward due to complex IT programming associated with proposal (mostly due to kidney allocation variances) and development of the new KAS § 2014—KAS is implemented, removing all variances
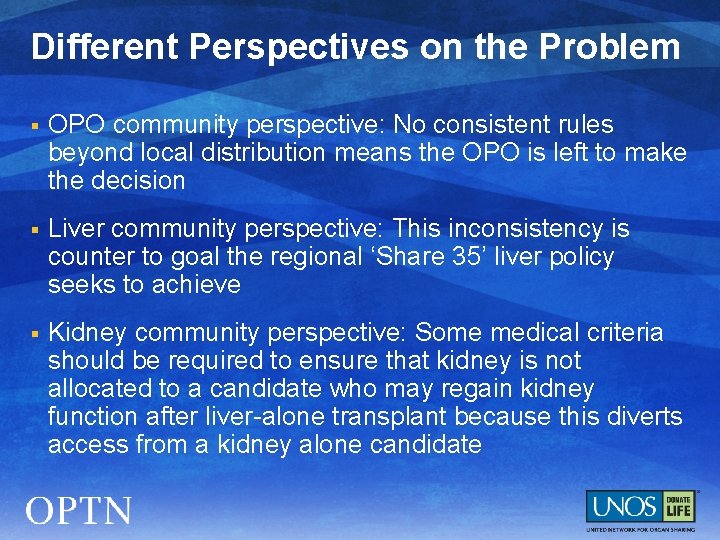
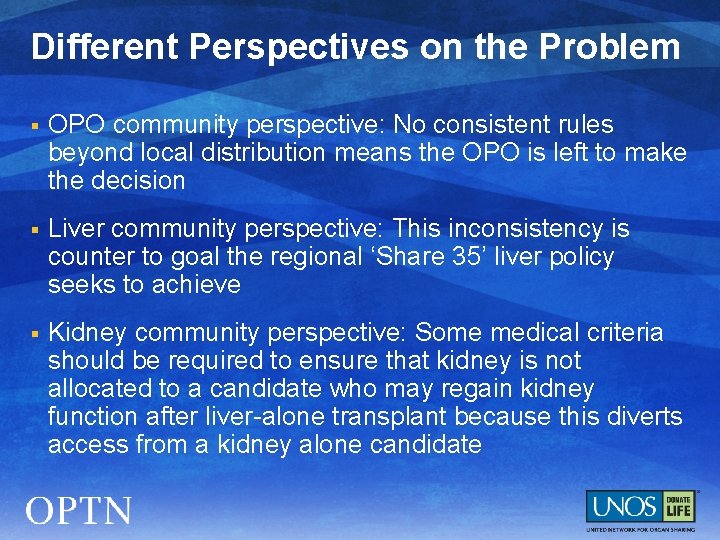
Different Perspectives on the Problem § OPO community perspective: No consistent rules beyond local distribution means the OPO is left to make the decision § Liver community perspective: This inconsistency is counter to goal the regional ‘Share 35’ liver policy seeks to achieve § Kidney community perspective: Some medical criteria should be required to ensure that kidney is not allocated to a candidate who may regain kidney function after liver-alone transplant because this diverts access from a kidney alone candidate
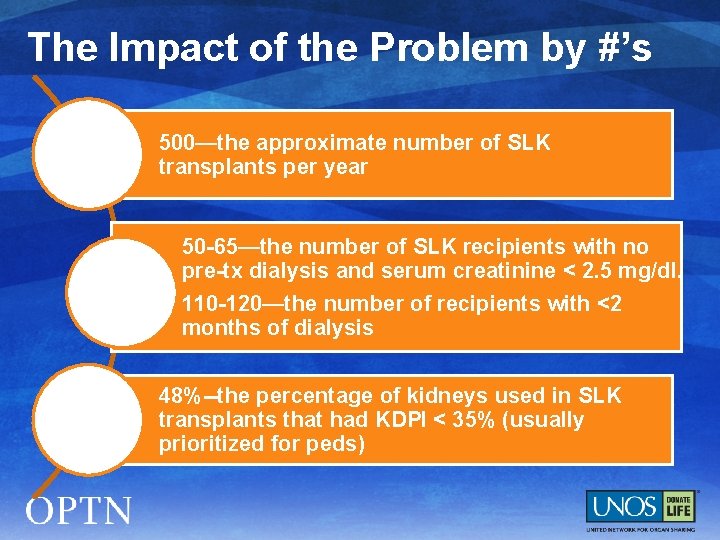
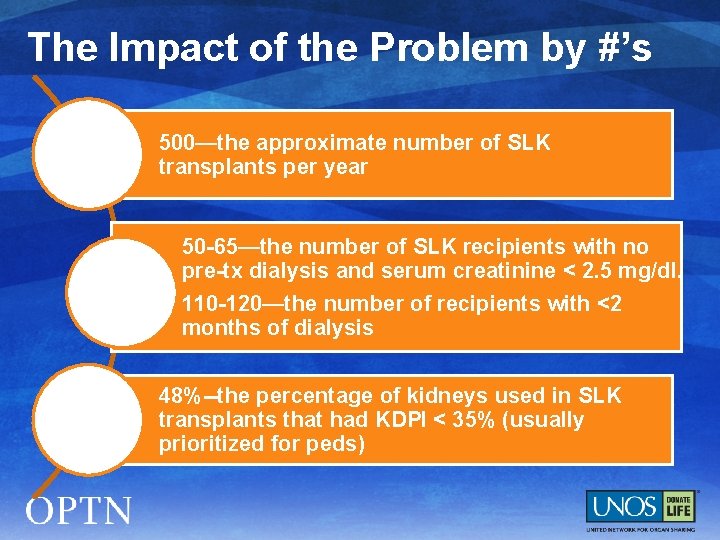
The Impact of the Problem by #’s 500—the approximate number of SLK transplants per year 50 -65—the number of SLK recipients with no pre-tx dialysis and serum creatinine < 2. 5 mg/dl. 110 -120—the number of recipients with <2 months of dialysis 48%--the percentage of kidneys used in SLK transplants that had KDPI < 35% (usually prioritized for peds)
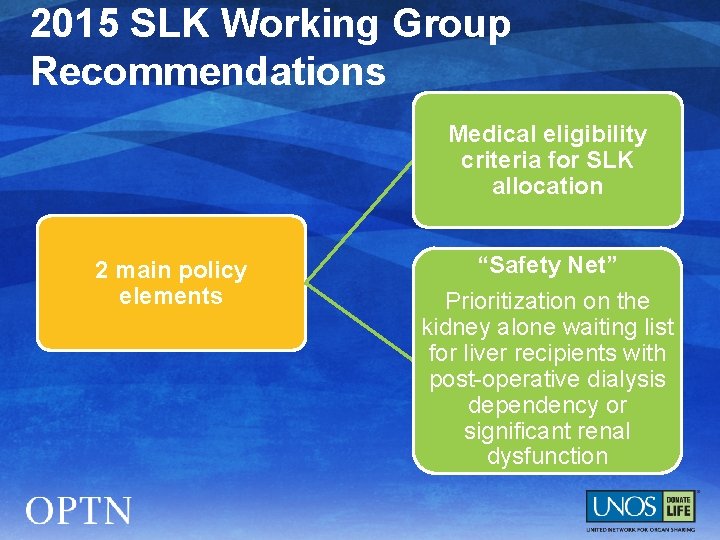
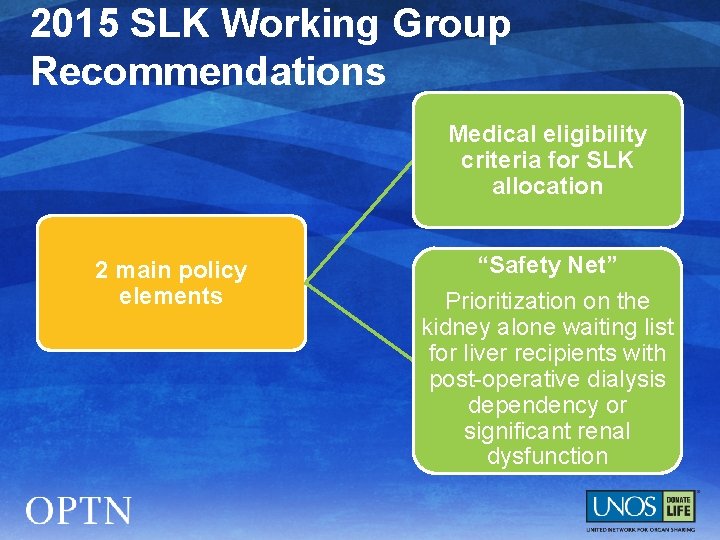
2015 SLK Working Group Recommendations Medical eligibility criteria for SLK allocation 2 main policy elements “Safety Net” Prioritization on the kidney alone waiting list for liver recipients with post-operative dialysis dependency or significant renal dysfunction
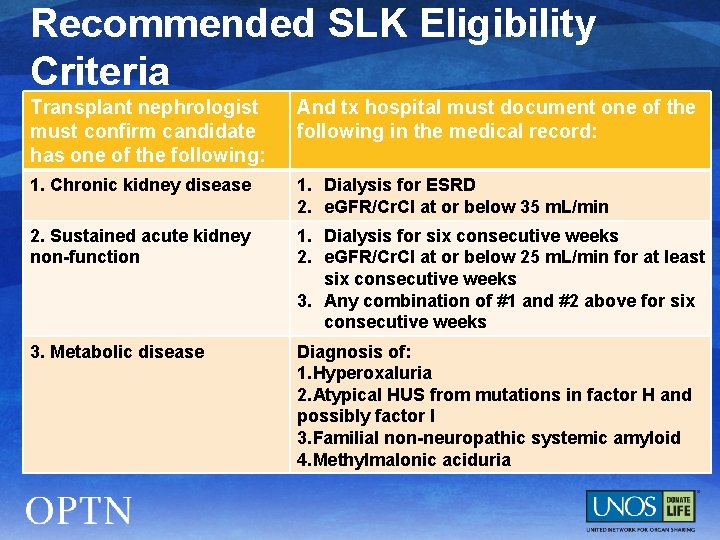
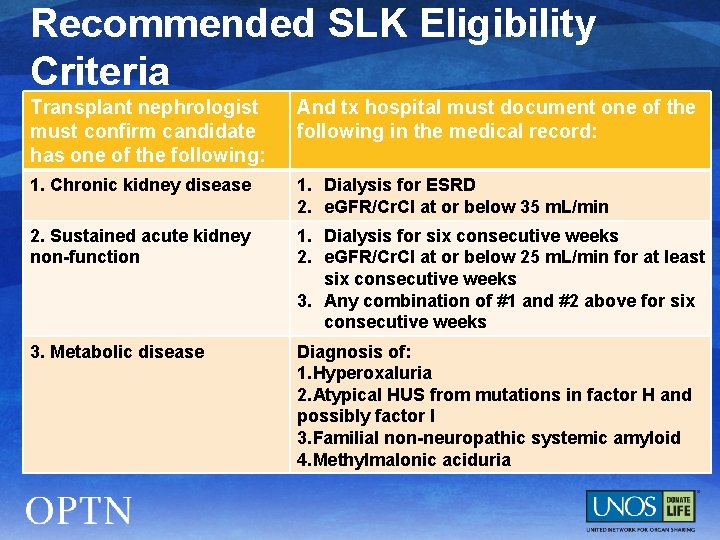
Recommended SLK Eligibility Criteria Transplant nephrologist must confirm candidate has one of the following: And tx hospital must document one of the following in the medical record: 1. Chronic kidney disease 1. Dialysis for ESRD 2. e. GFR/Cr. Cl at or below 35 m. L/min 2. Sustained acute kidney non-function 1. Dialysis for six consecutive weeks 2. e. GFR/Cr. Cl at or below 25 m. L/min for at least six consecutive weeks 3. Any combination of #1 and #2 above for six consecutive weeks 3. Metabolic disease Diagnosis of: 1. Hyperoxaluria 2. Atypical HUS from mutations in factor H and possibly factor I 3. Familial non-neuropathic systemic amyloid 4. Methylmalonic aciduria

Recommended SLK Allocation Policy § If candidate meets the eligibility criteria, the OPO must allocate the kidney with the liver if allocation is local or regional before offering the kidney to a kidney-alone candidate
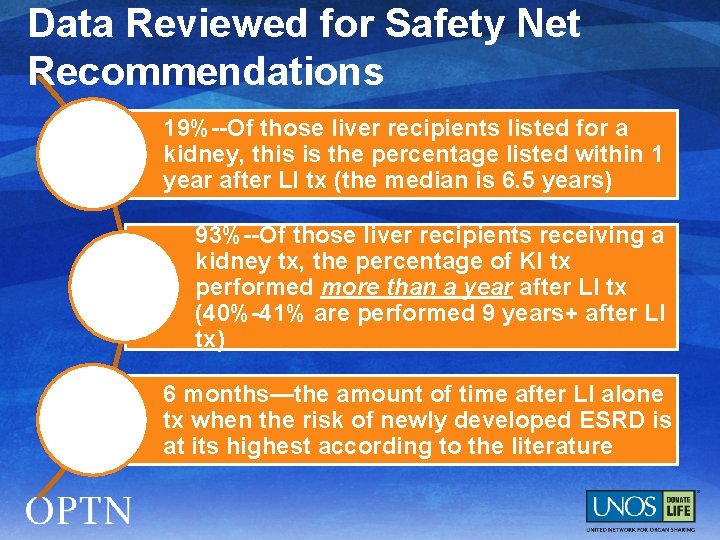
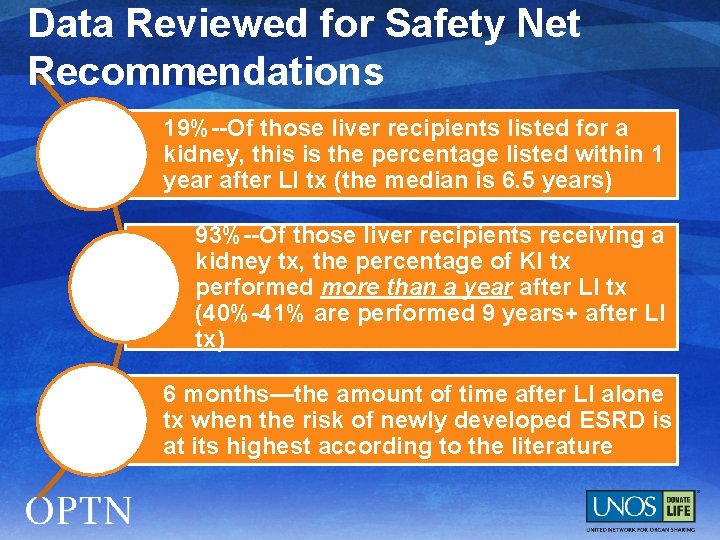
Data Reviewed for Safety Net Recommendations 19%--Of those liver recipients listed for a kidney, this is the percentage listed within 1 year after LI tx (the median is 6. 5 years) 93%--Of those liver recipients receiving a kidney tx, the percentage of KI tx performed more than a year after LI tx (40%-41% are performed 9 years+ after LI tx) 6 months—the amount of time after LI alone tx when the risk of newly developed ESRD is at its highest according to the literature
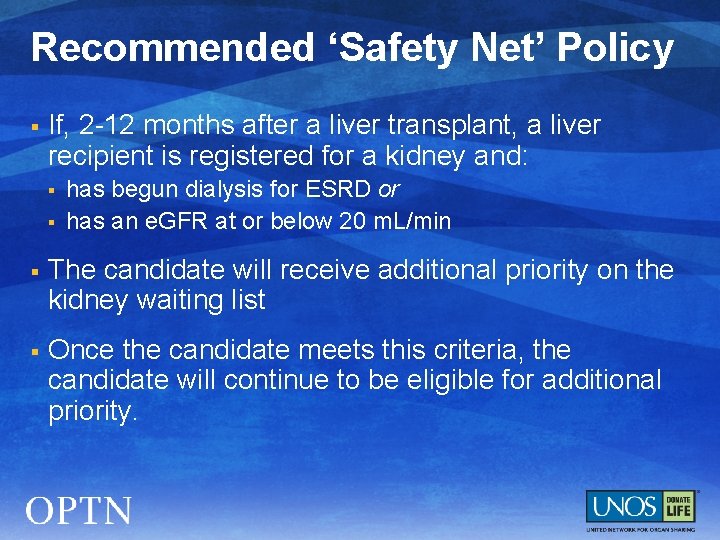
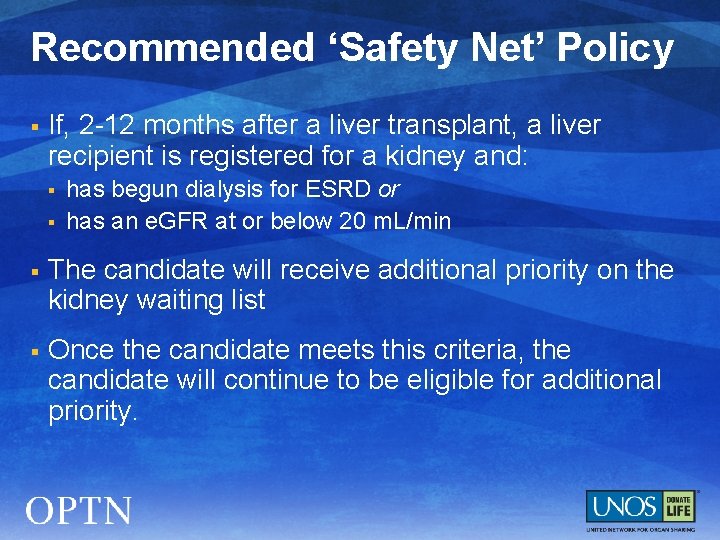
Recommended ‘Safety Net’ Policy § If, 2 -12 months after a liver transplant, a liver recipient is registered for a kidney and: § § has begun dialysis for ESRD or has an e. GFR at or below 20 m. L/min § The candidate will receive additional priority on the kidney waiting list § Once the candidate meets this criteria, the candidate will continue to be eligible for additional priority.
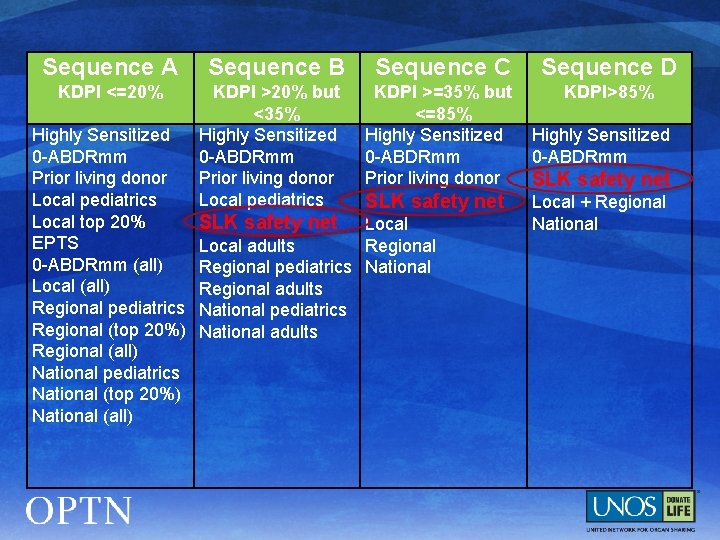
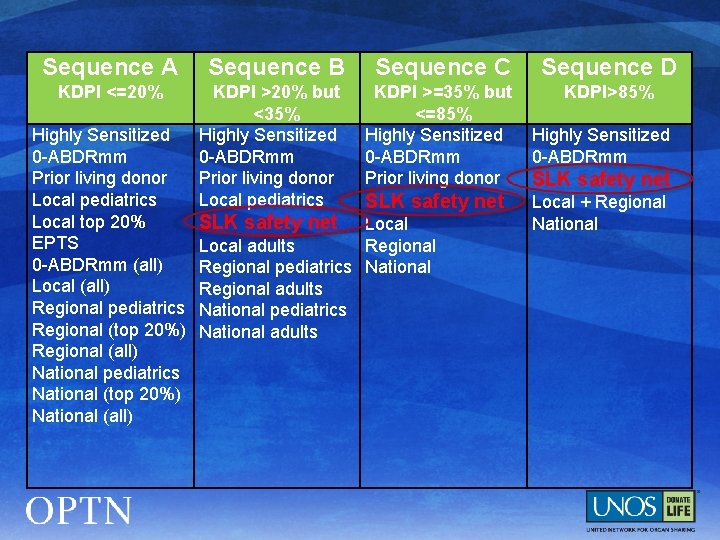
Sequence A KDPI <=20% Highly Sensitized 0 -ABDRmm Prior living donor Local pediatrics Local top 20% EPTS 0 -ABDRmm (all) Local (all) Regional pediatrics Regional (top 20%) Regional (all) National pediatrics National (top 20%) National (all) Sequence B Sequence C Sequence D KDPI >20% but <35% Highly Sensitized 0 -ABDRmm Prior living donor Local pediatrics KDPI >=35% but <=85% Highly Sensitized 0 -ABDRmm Prior living donor KDPI>85% SLK safety net Local adults Regional pediatrics National Regional adults National pediatrics National adults Highly Sensitized 0 -ABDRmm SLK safety net Local + Regional National

Next Steps § Seeking feedback from: § § § Regions Professional transplant societies and national groups Other Committees § Committees will reconvene in Spring to review feedback/finalize a public comment proposal for Fall 2015 § Explore and discuss application of these changes to heart/kidney and lung/kidney allocation
Comments/Questions? § Richard Formica, MD Committee Chair richard. formica@yale. edu § Regional Rep name (RA will complete) Region X Representative email address § Gena Boyle, MPA Committee Liaison gena. boyle@unos. org
Extras
Survival advantage of receiving a KI Purpose: Provide evidence supporting SLK eligibility criteria
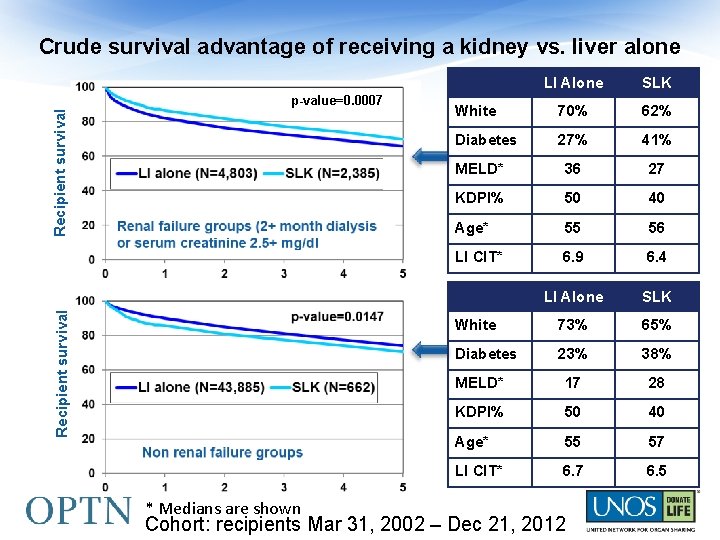
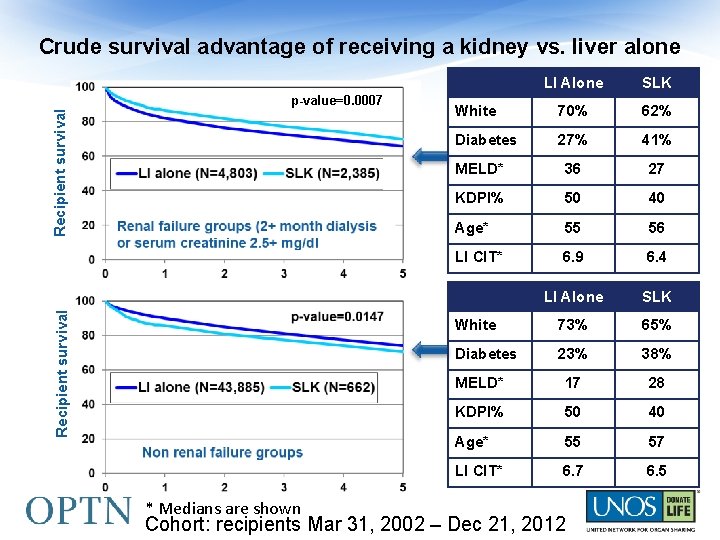
Crude survival advantage of receiving a kidney vs. liver alone Recipient survival p-value=0. 0007 * Medians are shown LI Alone SLK White 70% 62% Diabetes 27% 41% MELD* 36 27 KDPI% 50 40 Age* 55 56 LI CIT* 6. 9 6. 4 LI Alone SLK White 73% 65% Diabetes 23% 38% MELD* 17 28 KDPI% 50 40 Age* 55 57 LI CIT* 6. 7 6. 5 Cohort: recipients Mar 31, 2002 – Dec 21, 2012
KI graft survival for SLK vs. KI alone … and Heart-Kidney Purpose: Assess degree of decrease in kidney graft survival in multi-organ transplants

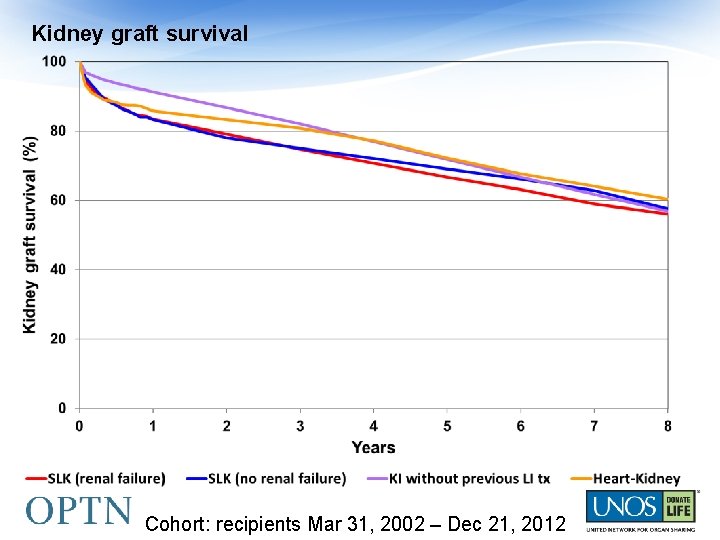
Kidney graft survival White Age (median) Recipient survival SLK (ren. failure) SLK (no ren. failure) KI 62% 65% 45% 56 57 54 Cohort: recipients Mar 31, 2002 – Dec 21, 2012
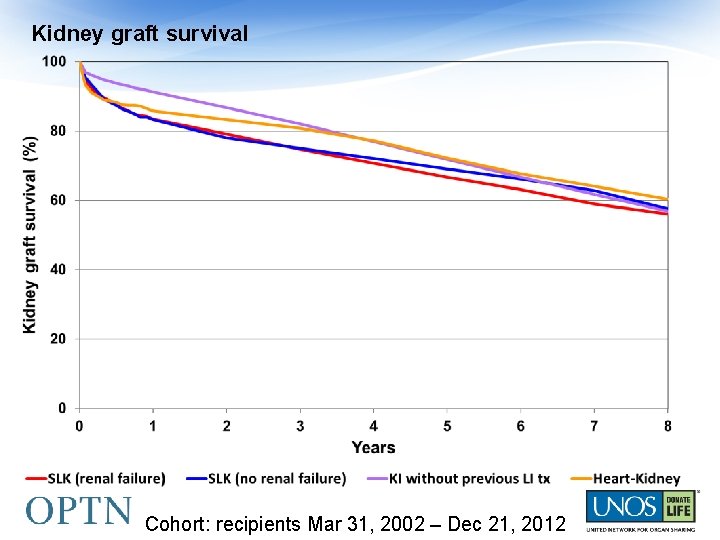
Kidney graft survival Cohort: recipients Mar 31, 2002 – Dec 21, 2012
The effect of a previous LI tx on KI waiting list and recipient survival Purpose: provide evidence supporting the use of the safety net
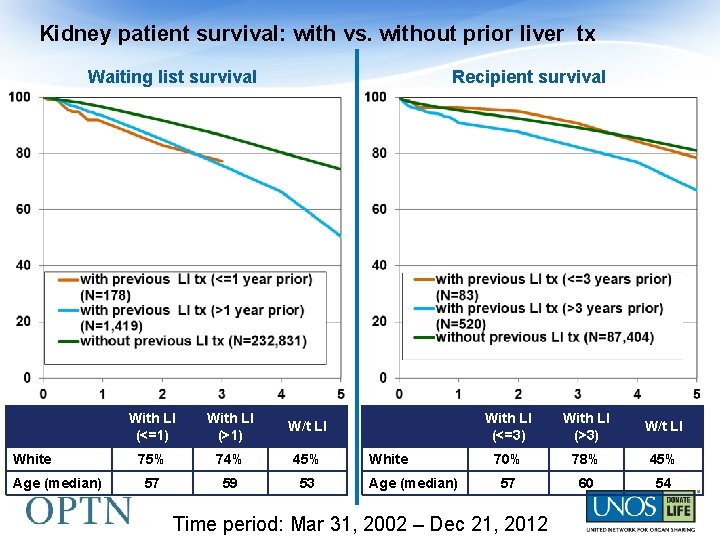
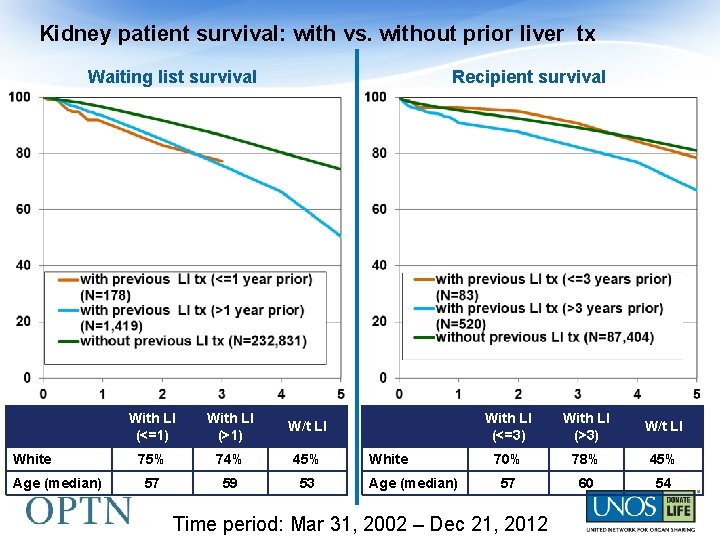
Kidney patient survival: with vs. without prior liver tx Waiting list survival White Age (median) Recipient survival With LI (<=1) With LI (>1) W/t LI 75% 74% 45% 57 59 53 White Age (median) With LI (<=3) With LI (>3) W/t LI 70% 78% 45% 57 60 54 Time period: Mar 31, 2002 – Dec 21, 2012
Summary Eligibility criteria: survival advantage of receiving a KI SLK: lower KI graft survival rates Safety net: KI after LI transplant
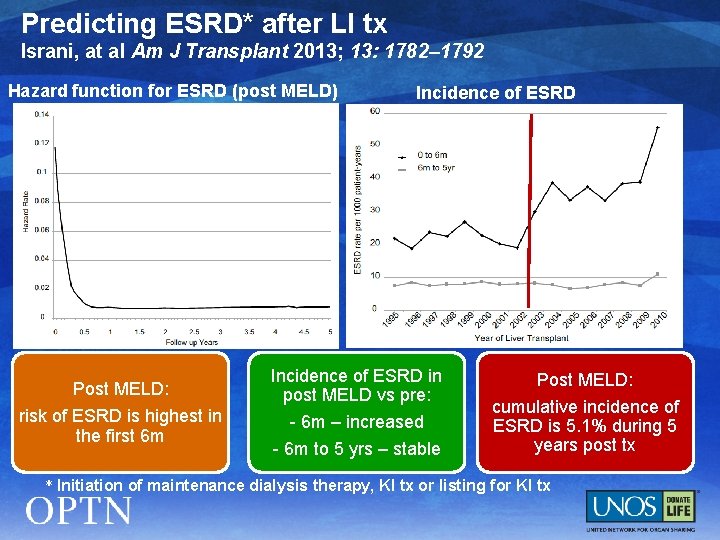
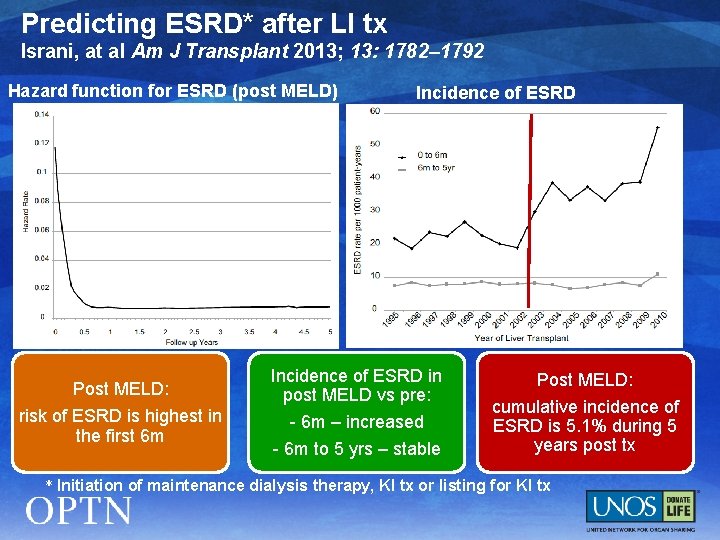
Predicting ESRD* after LI tx Israni, at al Am J Transplant 2013; 13: 1782– 1792 Hazard function for ESRD (post MELD) Post MELD: risk of ESRD is highest in the first 6 m Incidence of ESRD in post MELD vs pre: - 6 m – increased - 6 m to 5 yrs – stable Post MELD: cumulative incidence of ESRD is 5. 1% during 5 years post tx * Initiation of maintenance dialysis therapy, KI tx or listing for KI tx
SLK Working Group § Kidney Transplantation Committee § Liver and Intestinal Organ Transplantation Committee § OPO Committee § Ethics Committee § Minority Affairs Committee § Operations and Safety Committee
Achieving a Balance Access Utility