BRS Renal Tutorial Kalyan Vemulapalli kvv 16ic ac
BRS Renal Tutorial Kalyan Vemulapalli kvv 16@ic. ac. uk
• The amount of content you need to know has decreased compared to last year • But I still want to test your understanding and knowledge of the content throughout • Therefore I will be asking you questions that you don’t need to learn in terms of content • But you should be able to derive the answer through what you are meant to know
Learning Outcomes • Genitourinary structure and function: Describe the structural and cellular organisation of the kidney, bladder, and prostate and relate this to function. • Genitourinary specialist cells: Summarise the cell types of the kidney and genitourinary tract and their function. • Genitourinary disorders: • Summarise the pathology and pathophysiology of genitourinary disorders. • Describe the clinical features and treatment options of genitourinary disorders.
Kidney Function • Overall, the kidney functions as a regulator of homeostasis • Excretion of waste products (from metabolic processes) • Regulation of body fluids, salts, acid-base balance • Blood Pressure control • Hormone secretion (EPO, renin) • What do EPO and renin do?
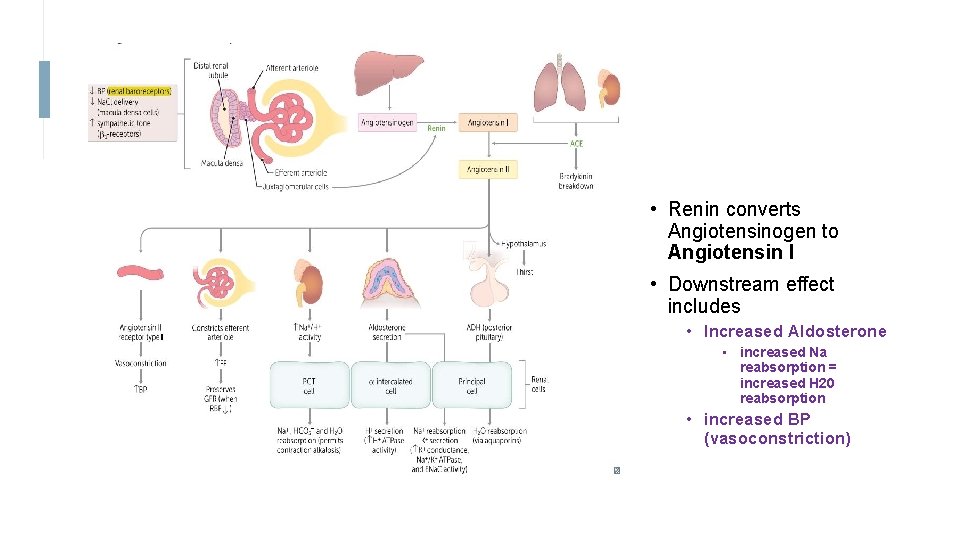
• Renin converts Angiotensinogen to Angiotensin I • Downstream effect includes • Increased Aldosterone • increased Na reabsorption = increased H 20 reabsorption • increased BP (vasoconstriction)
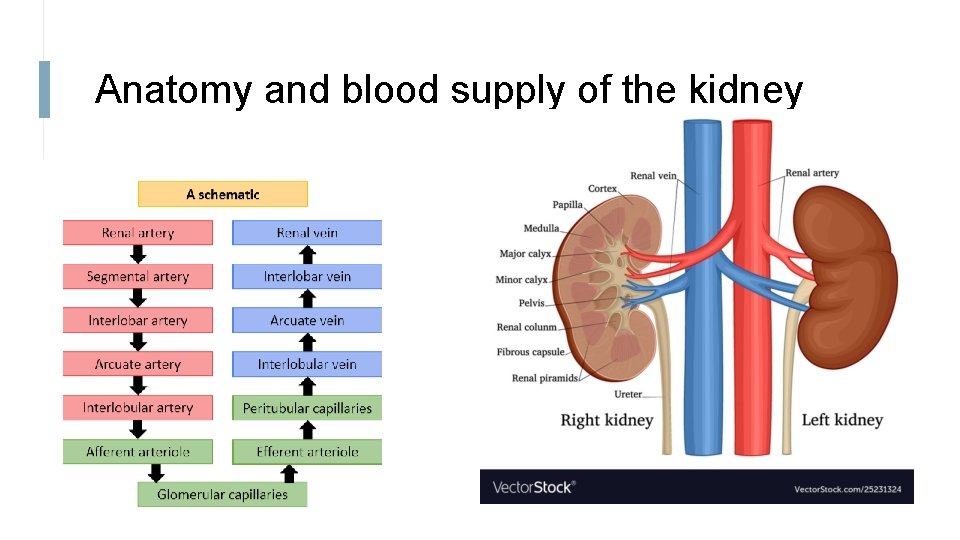
Anatomy and blood supply of the kidney
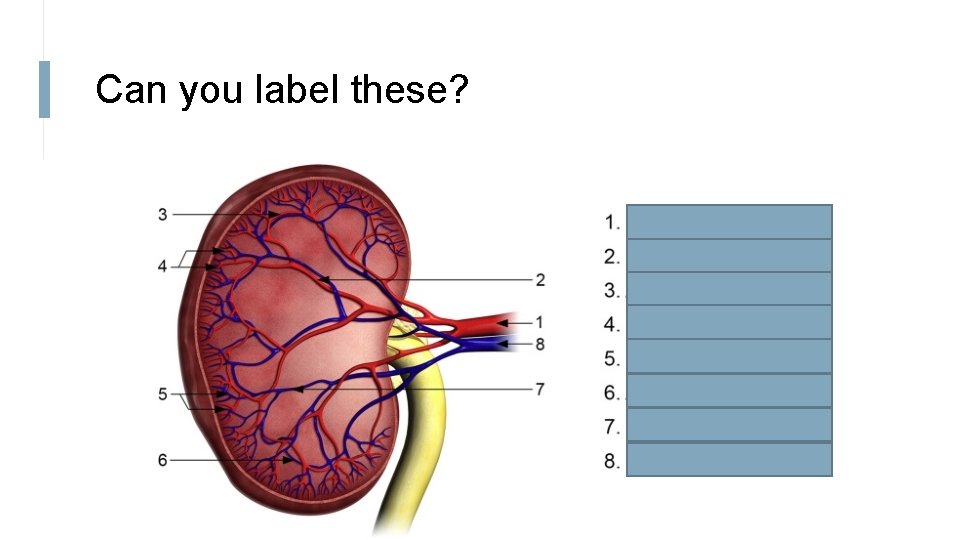
Can you label these?
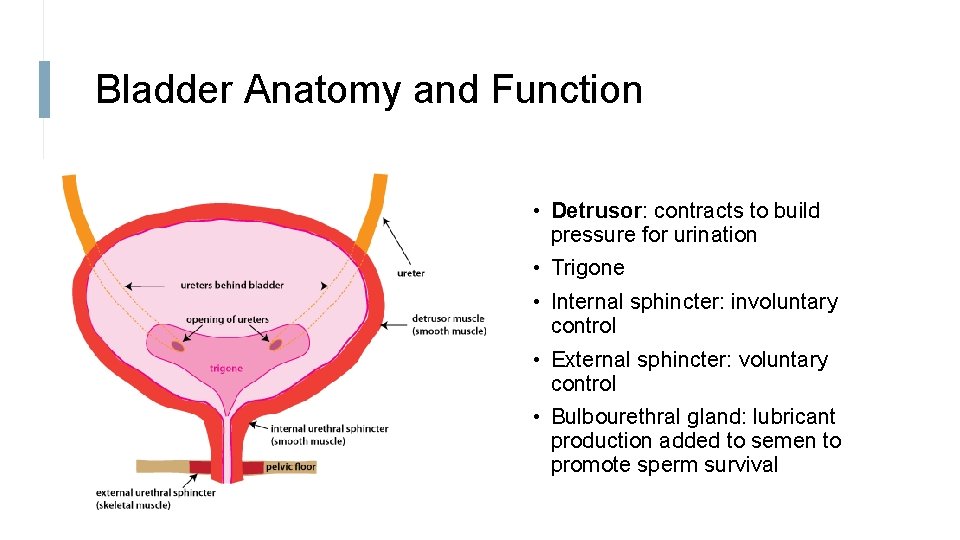
Bladder Anatomy and Function • Detrusor: contracts to build pressure for urination • Trigone • Internal sphincter: involuntary control • External sphincter: voluntary control • Bulbourethral gland: lubricant production added to semen to promote sperm survival
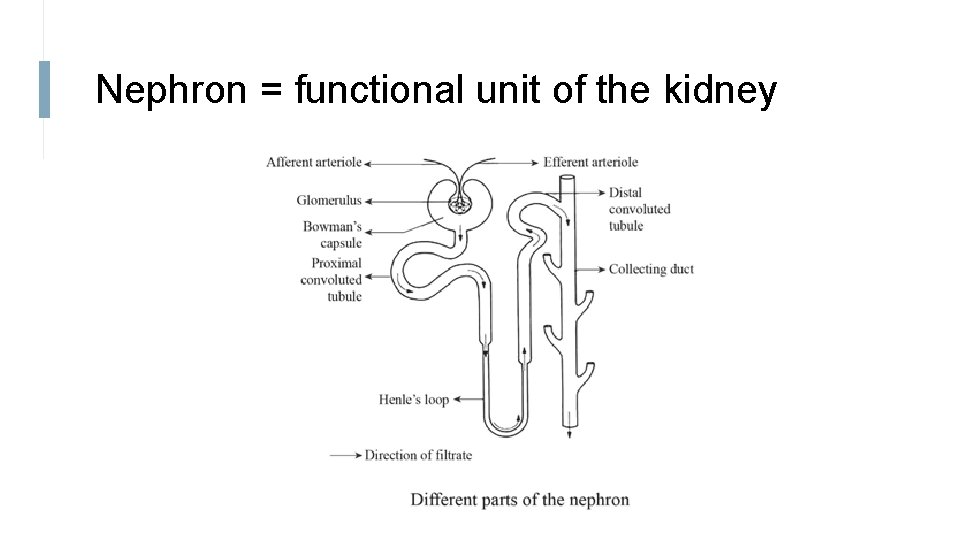
Nephron = functional unit of the kidney
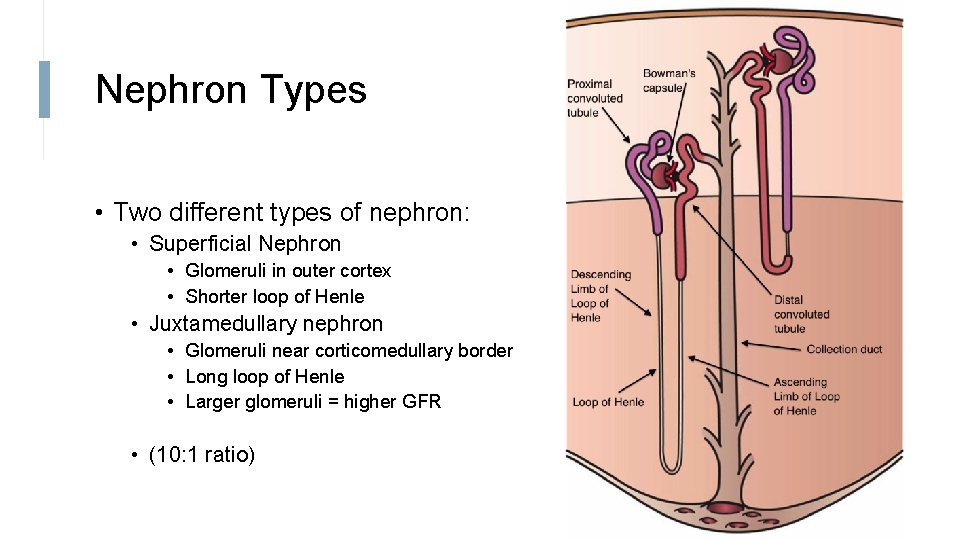
Nephron Types • Two different types of nephron: • Superficial Nephron • Glomeruli in outer cortex • Shorter loop of Henle • Juxtamedullary nephron • Glomeruli near corticomedullary border • Long loop of Henle • Larger glomeruli = higher GFR • (10: 1 ratio)
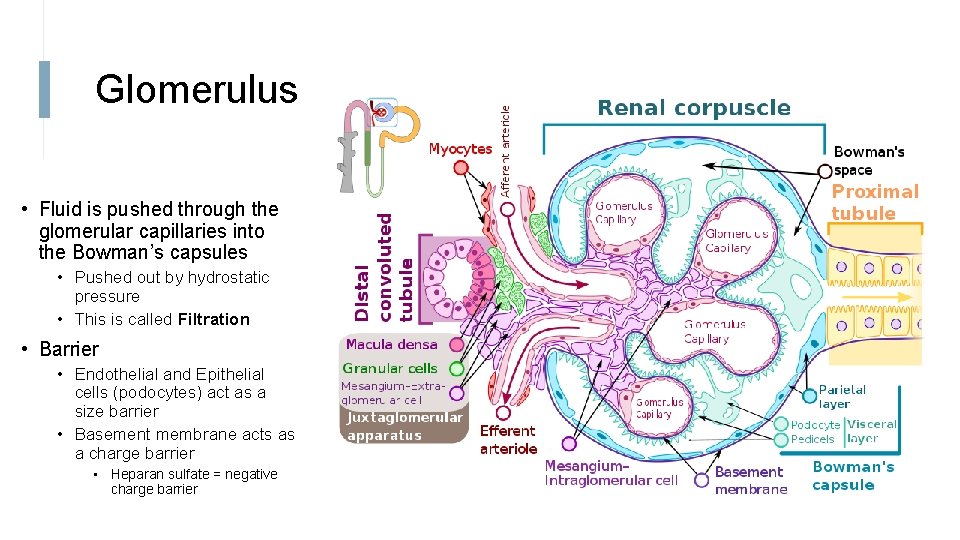
Glomerulus • Fluid is pushed through the glomerular capillaries into the Bowman’s capsules • Pushed out by hydrostatic pressure • This is called Filtration • Barrier • Endothelial and Epithelial cells (podocytes) act as a size barrier • Basement membrane acts as a charge barrier • Heparan sulfate = negative charge barrier
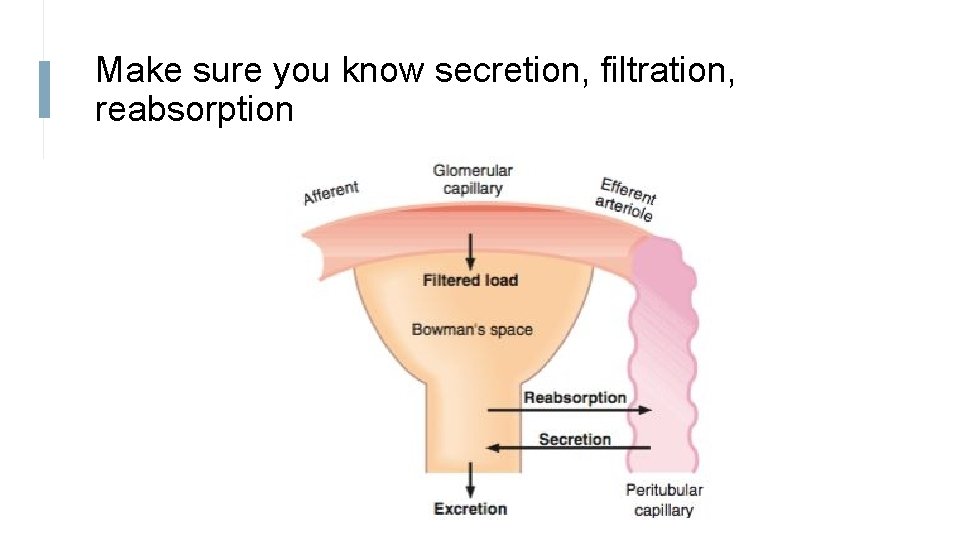
Make sure you know secretion, filtration, reabsorption
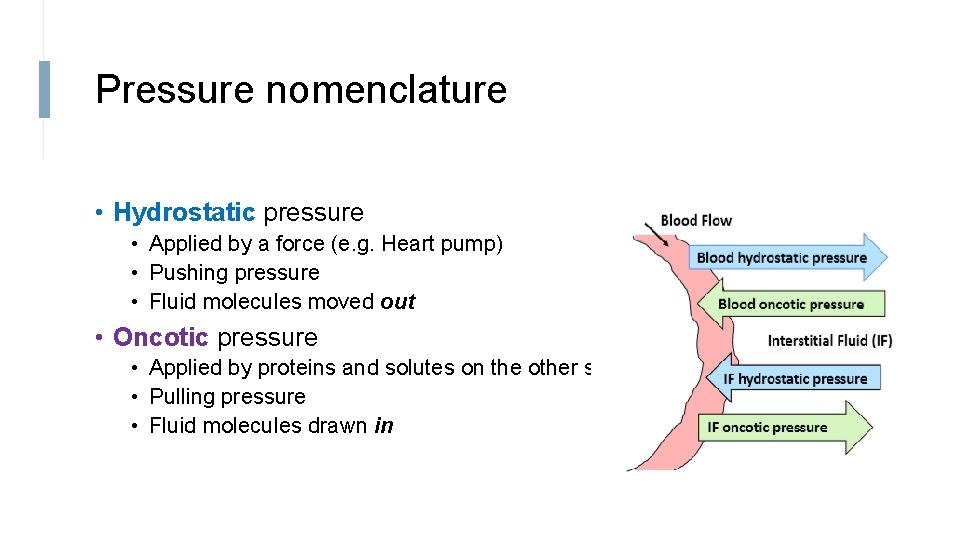
Pressure nomenclature • Hydrostatic pressure • Applied by a force (e. g. Heart pump) • Pushing pressure • Fluid molecules moved out • Oncotic pressure • Applied by proteins and solutes on the other side • Pulling pressure • Fluid molecules drawn in
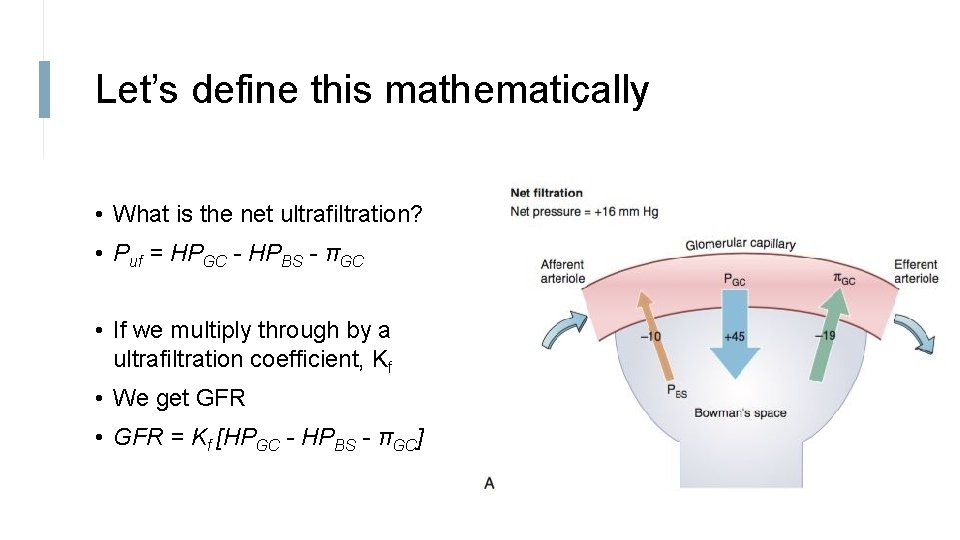
Let’s define this mathematically • What is the net ultrafiltration? • Puf = HPGC - HPBS - πGC • If we multiply through by a ultrafiltration coefficient, Kf • We get GFR • GFR = Kf [HPGC - HPBS - πGC]
Glomerular Filtration Rate • Amount of fluid filtered from glomeruli to Bowman capsule per unit time • Sum of filtration rate for all functioning nephrons • GFR = Puf x Kf • Kf is a coefficient of ultrafiltration • What does this mean? • GFR is normally between 90 -140 ml/min in male and 80 -125 ml/min in female • LOW GFR = RENAL DISEASE
GFR is regulated • Why? • Two methods • Myogenic mechanism • Tubulo-glomerular feedback
Myogenic Mechanism 1. If increased arterial pressure, 2. Afferent arteriole stretches What happens if we stretch a muscle? 3. Arteriole contracts as a reflex What happens if the arteriole contracts? 4. Resistance increases 5. Blood flow decreases 6. GFR is unchanged.
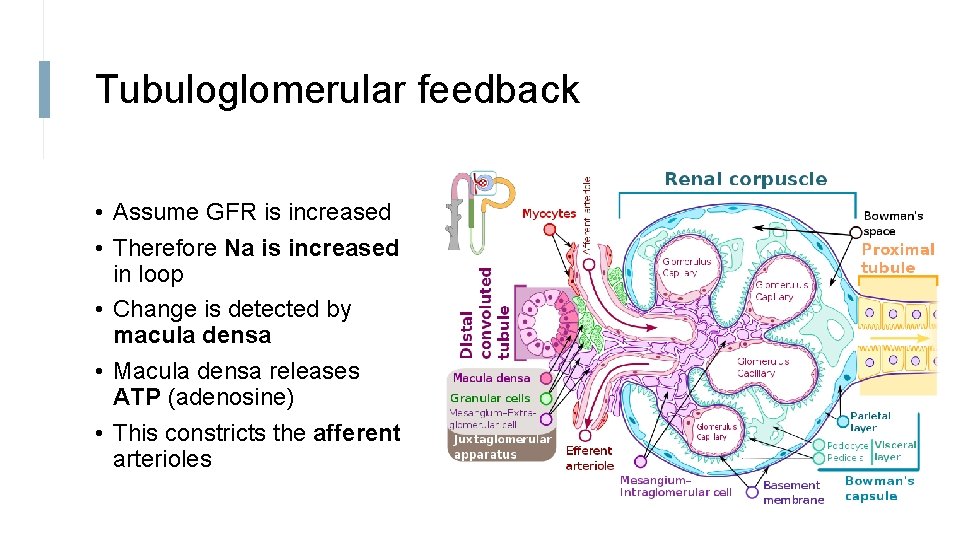
Tubuloglomerular feedback • Assume GFR is increased • Therefore Na is increased in loop • Change is detected by macula densa • Macula densa releases ATP (adenosine) • This constricts the afferent arterioles
GFR is hard to measure, therefore we calculate something called clearance first • Renal clearance is number of litres of plasma that are cleared of a substance per unit time • C = UV/P • So if C = 50 ml/min, 50 ml of plasma is cleared of this substance per minute
But we can’t use any clearance • This is because some materials are completely reabsorbed • Some materials are secreted • Some materials are not filtered • Therefore, we need a material that is freely filtered AND not reabsorbed AND not secreted
So what substances can we use? • Inulin • Creatinine • Slightly overestimates GFR • Why? • So why use creatinine over inulin? • Waste product from muscle metabolism • Low or high creatinine indicates renal failure
Moving on, how can we work out how much blood is going to the kidney? • Renal plasma flow is calculated by finding a molecule that is totally excreted by the kidney • So both filtration, and secretion • The molecule that was found to do this is PAH • The clearance of PAH = the RPF
One last equation…. • Filtration fraction is how much of the plasma was filtered. • So a FF of 20% means 20% of the plasma entering the glomerulus is filtered • FF = GFR/RPF
Maths over! • I’m assuming you know the difference between passive and active transport….
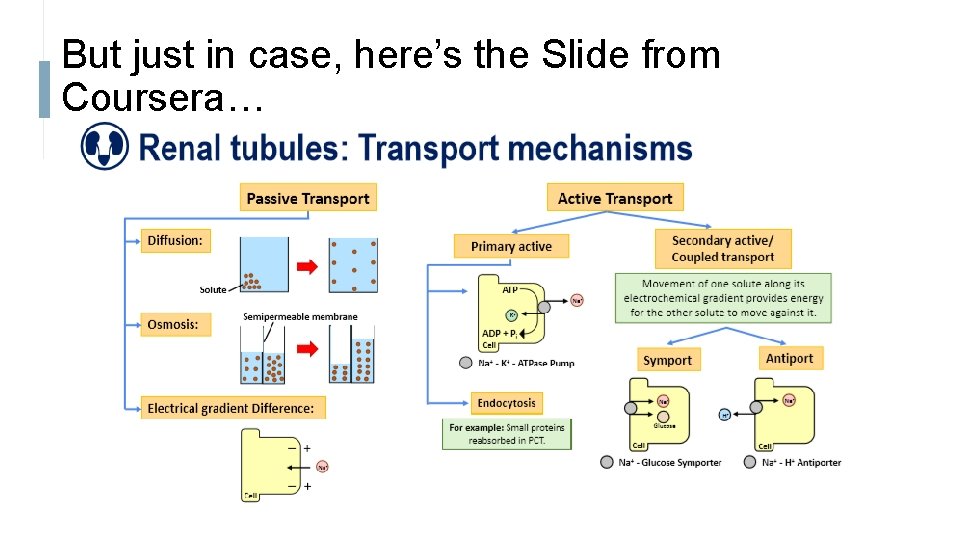
But just in case, here’s the Slide from Coursera…
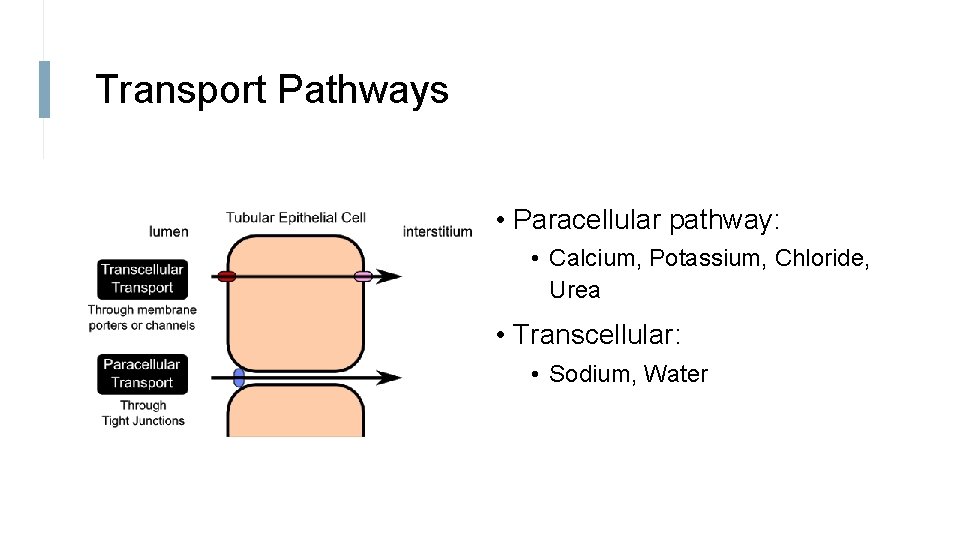
Transport Pathways • Paracellular pathway: • Calcium, Potassium, Chloride, Urea • Transcellular: • Sodium, Water
The diagrams on the next few slides are from your lecture by Paul Kemp
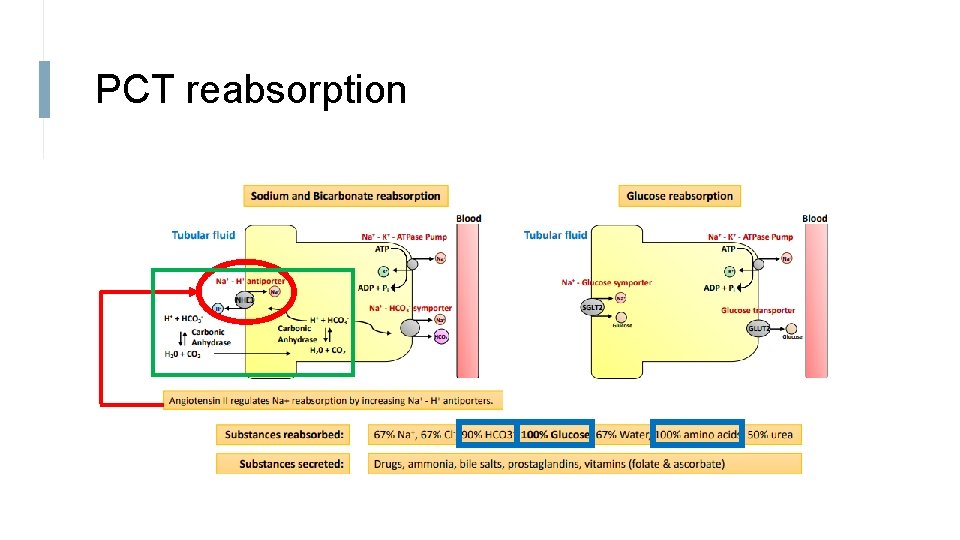
PCT reabsorption
PCT • 90% of Bicarbonate reabsorbed • 100 % of Glucose and Amino Acids are reabsorbed in early PCT • Through Na cotransport
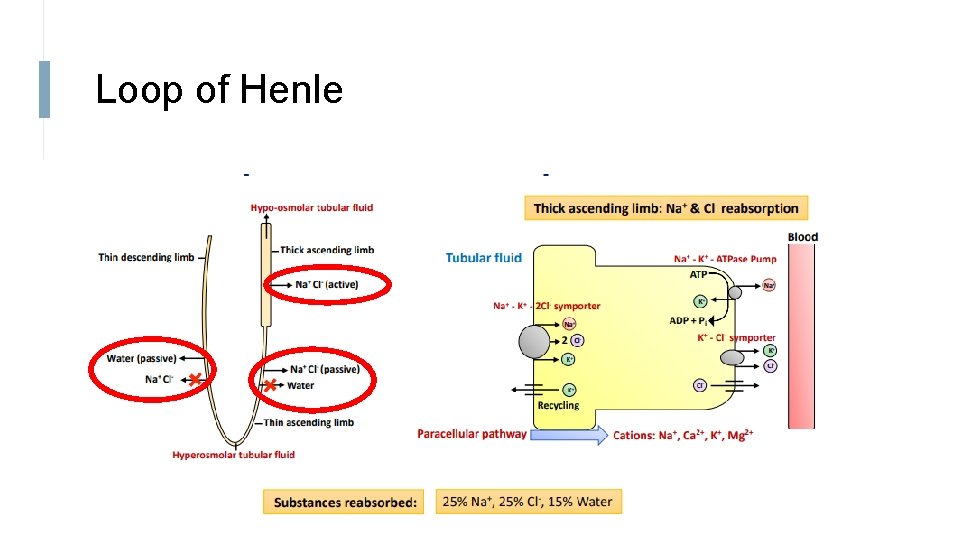
Loop of Henle
Descending Loop of Henle • Permeable to water • Impermeable to Na • Tubular fluid becomes progressively hyper-osmotic as it descends • Meaning the concentration of salts is higher • This is because water is reabsorbed
Thin ascending loop • Permeable to Na (passive) • Impermeable to water
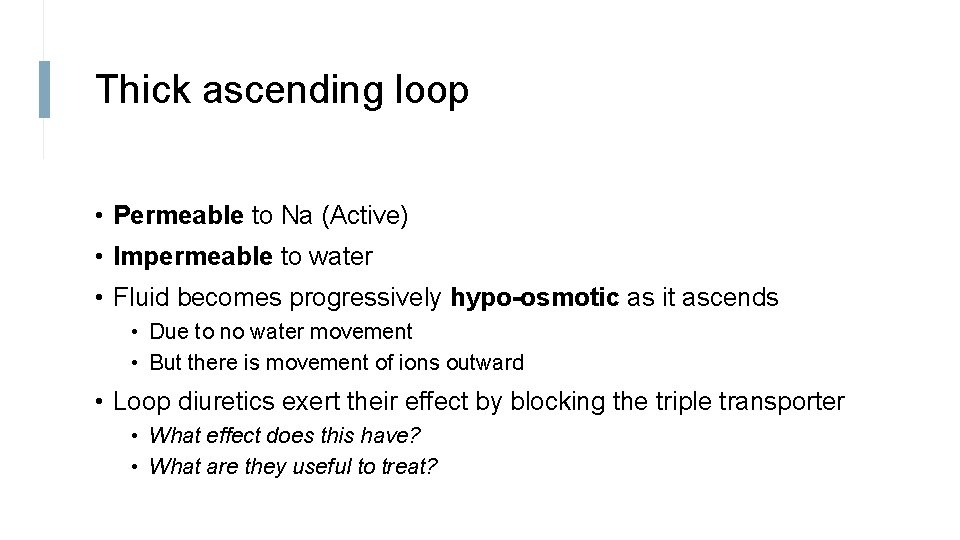
Thick ascending loop • Permeable to Na (Active) • Impermeable to water • Fluid becomes progressively hypo-osmotic as it ascends • Due to no water movement • But there is movement of ions outward • Loop diuretics exert their effect by blocking the triple transporter • What effect does this have? • What are they useful to treat?
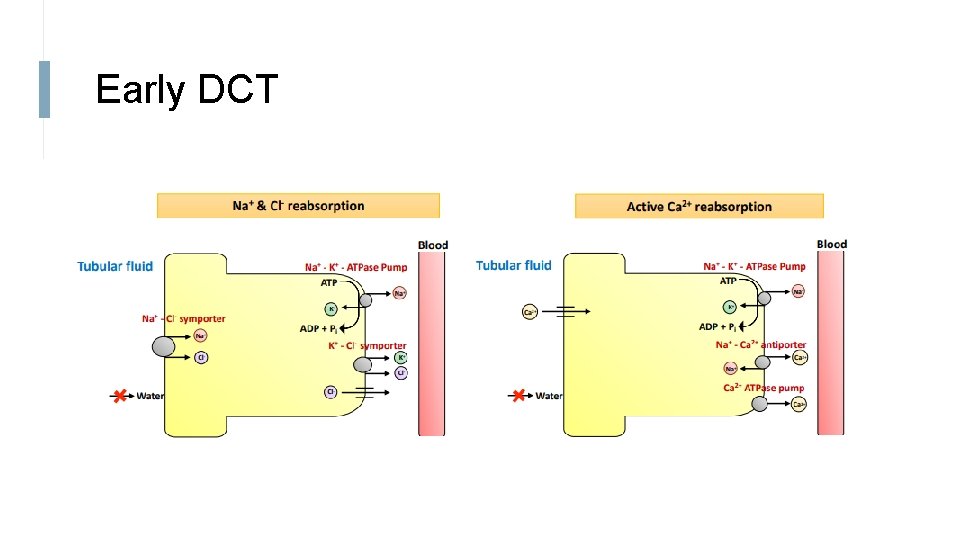
Early DCT
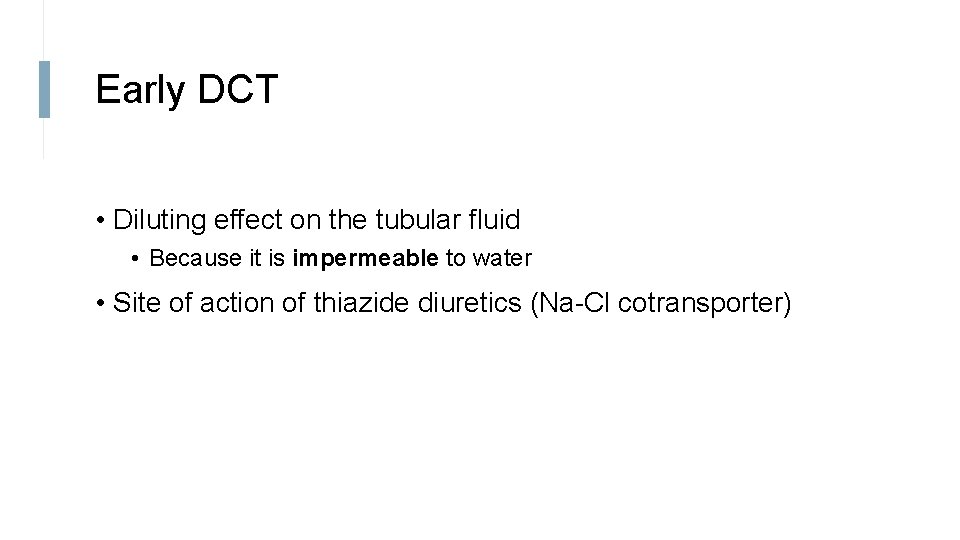
Early DCT • Diluting effect on the tubular fluid • Because it is impermeable to water • Site of action of thiazide diuretics (Na-Cl cotransporter)
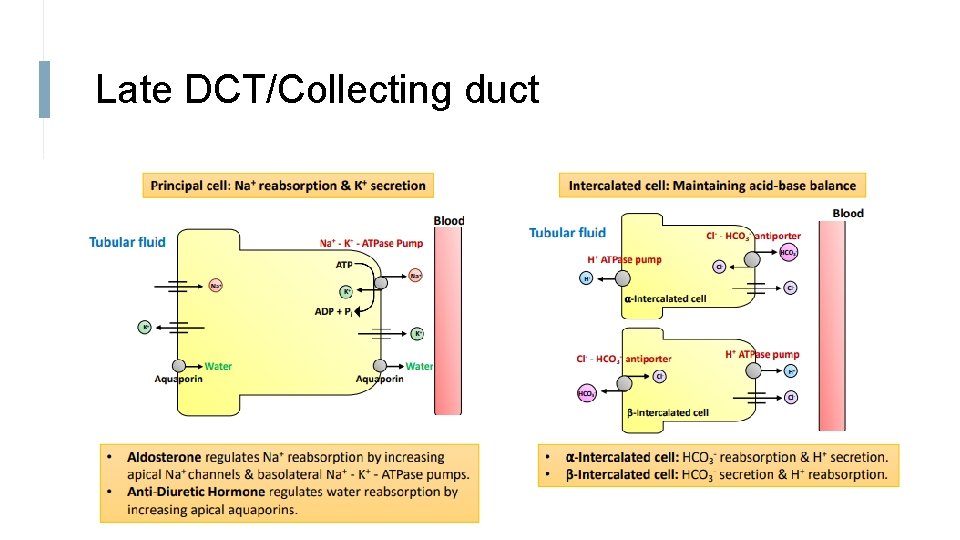
Late DCT/Collecting duct
Late DCT/Collecting Duct • Water reabsorption is regulated by ADH • ADH causes aquaporins on the apical side to increase • What would Syndrome of inappropriate ADH (SIADH) mean for amount of urination?
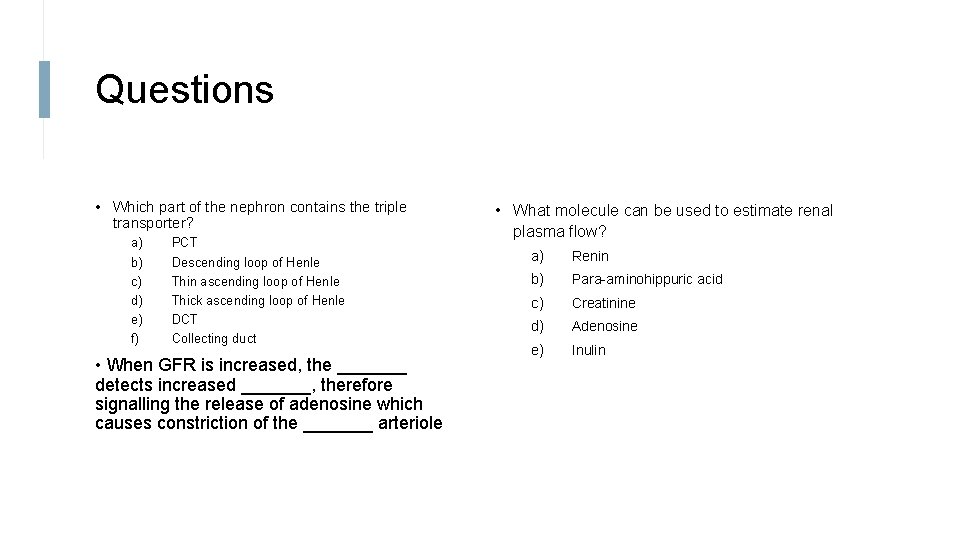
Questions • Which part of the nephron contains the triple transporter? a) b) c) d) e) f) PCT Descending loop of Henle Thin ascending loop of Henle Thick ascending loop of Henle DCT Collecting duct • When GFR is increased, the _______ detects increased _______, therefore signalling the release of adenosine which causes constriction of the _______ arteriole • What molecule can be used to estimate renal plasma flow? a) Renin b) Para-aminohippuric acid c) Creatinine d) Adenosine e) Inulin
Questions • On the following graph, draw the change in concentrations of the following substances: inulin, sodium, glucose, amino acids, water PCT Descending Loop Ascending Loop DCT Collecting Duct
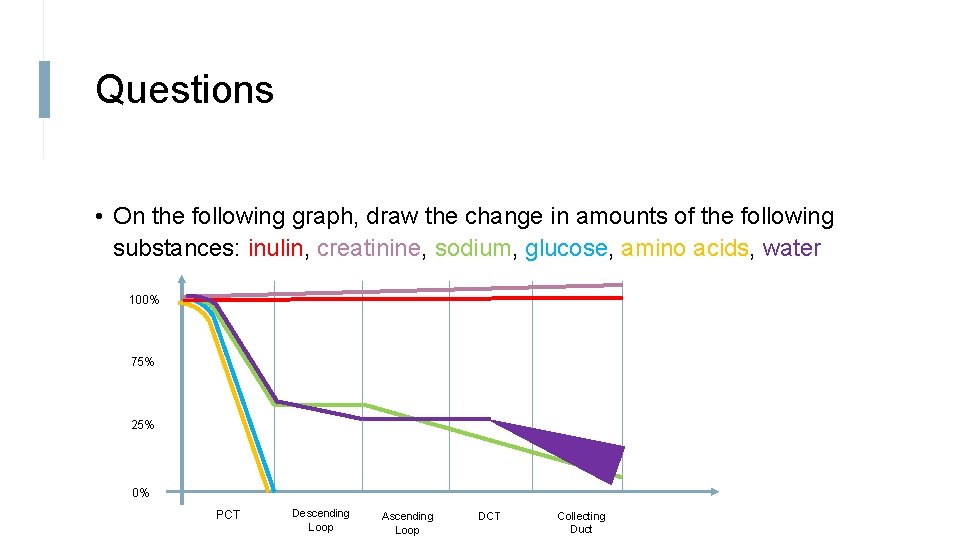
Questions • On the following graph, draw the change in amounts of the following substances: inulin, creatinine, sodium, glucose, amino acids, water 100% 75% 25% 0% PCT Descending Loop Ascending Loop DCT Collecting Duct
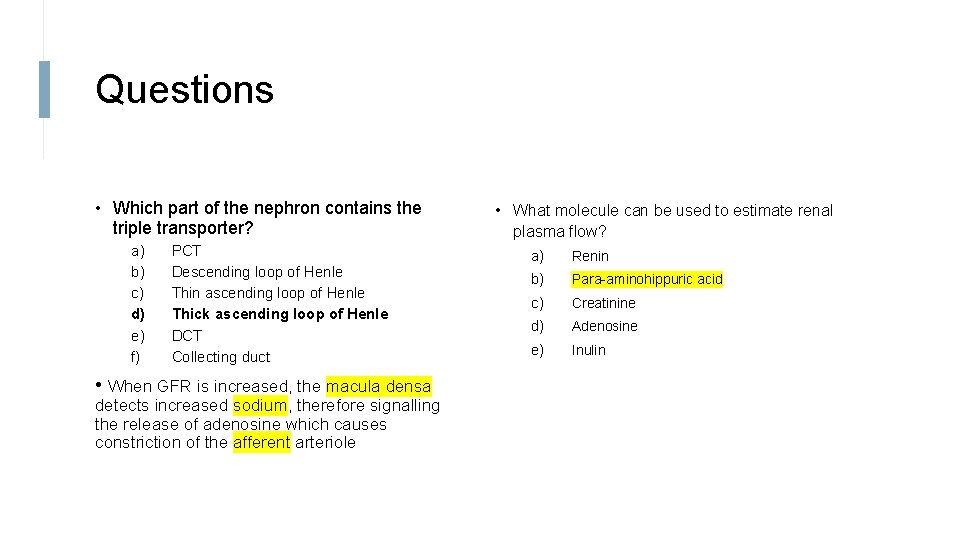
Questions • Which part of the nephron contains the triple transporter? a) b) c) d) e) f) PCT Descending loop of Henle Thin ascending loop of Henle Thick ascending loop of Henle DCT Collecting duct • When GFR is increased, the macula densa detects increased sodium, therefore signalling the release of adenosine which causes constriction of the afferent arteriole • What molecule can be used to estimate renal plasma flow? a) Renin b) Para-aminohippuric acid c) Creatinine d) Adenosine e) Inulin
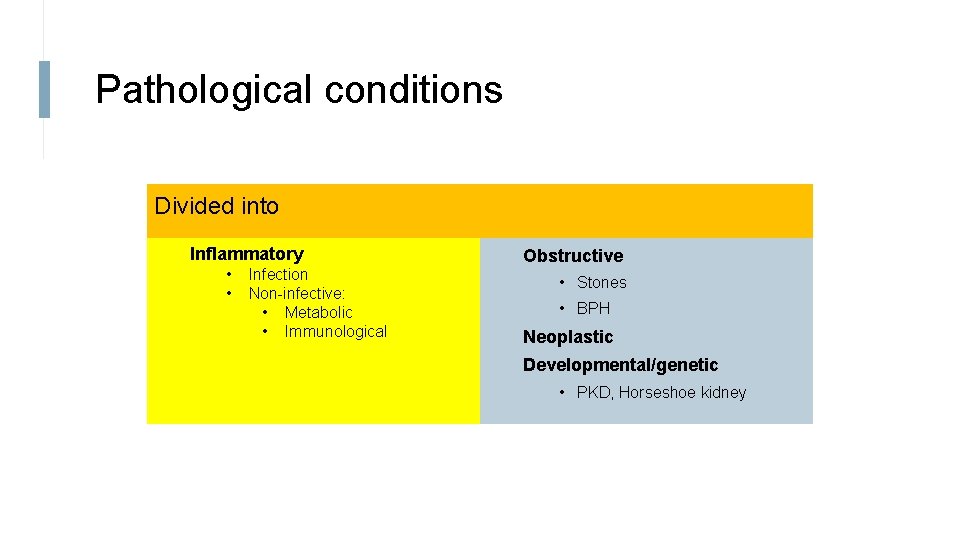
Pathological conditions Divided into Inflammatory • • Infection Non-infective: • Metabolic • Immunological Obstructive • Stones • BPH Neoplastic Developmental/genetic • PKD, Horseshoe kidney
UTIs are very common Inflammatory Most commonly due to an ascending infection Infection of the urethra, bladder, or kidney Known as urethritis, cystitis, pyelonephritis
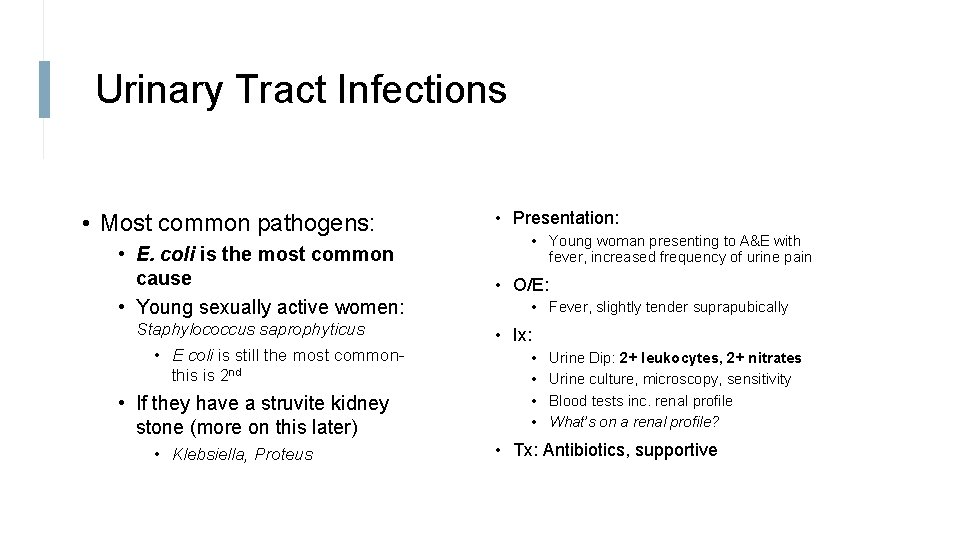
Urinary Tract Infections • Most common pathogens: • E. coli is the most common cause • Young sexually active women: Staphylococcus saprophyticus • E coli is still the most commonthis is 2 nd • If they have a struvite kidney stone (more on this later) • Klebsiella, Proteus • Presentation: • Young woman presenting to A&E with fever, increased frequency of urine pain • O/E: • Fever, slightly tender suprapubically • Ix: • • Urine Dip: 2+ leukocytes, 2+ nitrates Urine culture, microscopy, sensitivity Blood tests inc. renal profile What’s on a renal profile? • Tx: Antibiotics, supportive
Metabolic cause: Diabetic Nephropathy Most common cause of CKD and kidney failure in the west Rx factors: HTN, poor diabetic control, smoking Clinical Ix: • • Microalbuminuria – first sign Glucose in urine Proteinuria Other diabetic complications (retinopathy, neuropathy)
Other Inflammatory causes nephritic syndrome nephrotic syndrome
Nephritic syndrome • Hematuria • Proteinuria (normally less than nephrotic syndrome) • HTN, reduced urine output, increased urea/creatinine • Patient: 35 year old, sore throat for 4 days, red colour in urine • Normal temperature, HTN, normal exam • Ix: Urine dipstick = 3+ blood, 2+ protein • Urine = raised protein to creatinine ratio • Protein is lower than in nephrotic syndrome (Proteinuria < 3. 5 g/day) • Kidney biopsy: Ig. A nephropathy
Ig. A Nephropathy (Type of Nephritic syndrome) • Deposition of Ig. A antibody in the kidney • Ig. A nephropathy typically follows a respiratory or GI tract infection • Why? • Causes inflammation and scarring • Many progress to failure • Tx: • Treat HTN, reduce proteinuria • ARB/ACEi • Reduce Sodium intake • Immunotherapy • Renal Replacement therapy if late stage disease (dialysis, transplantation)

Minimal change most common in children, triggered by recent infection Nephrotic Syndrome Many causes Minimal change disease FSGS Membranous Lupus • cytokine-mediated damage of foot processes and loss of glomerular basement anions (heparan sulphate) Microscopy • Lipids may be seen in proximal tubule cells of the nephron (light microscopy) • Normal light microscopy of glomerulus • Electron microscopy: Podocyte effacement Complication of thrombosis Tx: • Corticosteroids, cyclophosphamide • Tacrolimus (antibody targeting B cell pathway) • Diuretics • Anticoagulation (risk of thrombosis complication)
Goodpasture's disease Organ Specific • Lung and kidney (alpha 3 chain of t. IV collagen) • Called anti-glomerular bsaement membrane SLE (ANA, anti-ds. DNA) Vasculitis (ANCA)
Can form in the kidney, ureter, bladder Obstructive: Stones Presentation: • Extreme pain from the abdomen/flank radiating to the groin • Associated with urinary tract infection Investigations/Findings • • Radio-opaque Different types: mostly calcium oxalate Hx of stones Blood in urine, infection, kidney function normal, XRay, USS, CT
Treatment • Pain control, hydration • Can give a specific treatment depending on size, location, fitness, and on equipment availability • Shockwave Lithotripsy (High energy sound waves to break up stones to smaller ones) • Ureteroscopy • Percutaneous nephrolithotomy
Benign = BPH Neoplastic: Tumour • Can cause lack of urination (FUND HIPS) Malignant • RCC, TCC, Prostatic, Testicular Presentation: asymptomatic, hematuria, pain • RCC: classic triad of hematuria, palpable mass, and flank pain Ix: Imaging, Urine tests, PSA, Biopsy, Stage Tx: remove obstruction, chemo, radio, hormonal, surgery
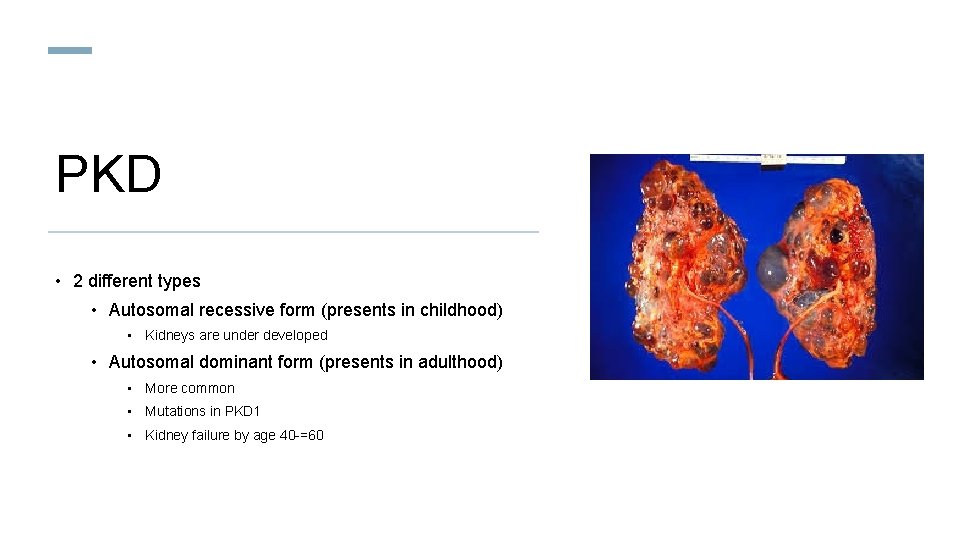
PKD • 2 different types • Autosomal recessive form (presents in childhood) • Kidneys are under developed • Autosomal dominant form (presents in adulthood) • More common • Mutations in PKD 1 • Kidney failure by age 40 -=60
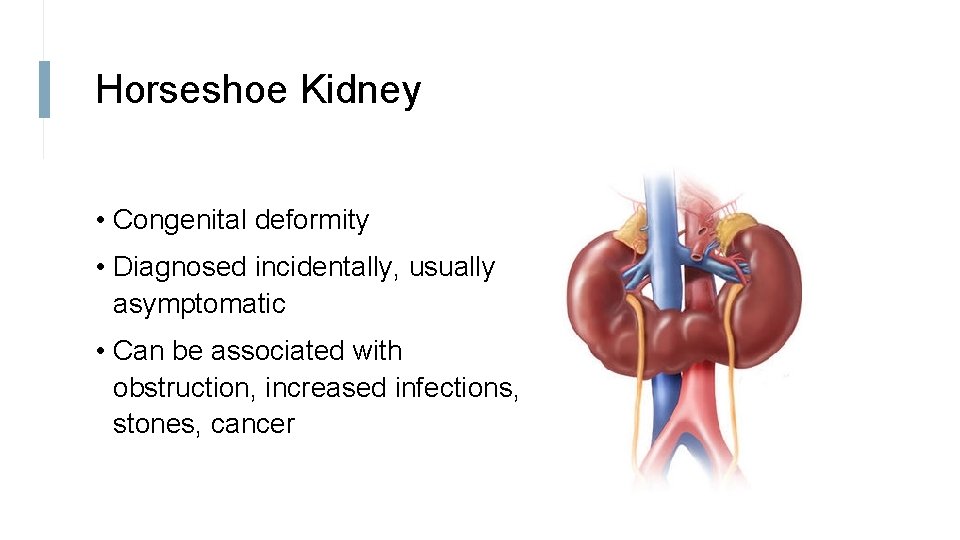
Horseshoe Kidney • Congenital deformity • Diagnosed incidentally, usually asymptomatic • Can be associated with obstruction, increased infections, stones, cancer
Feedback • Please leave feedback by filling out this very short survey! – http: //tiny. cc/tutorialfeedback LO: please insert relevant Learning objective reference here 56
- Slides: 56