Chronic Kidney Disease Acute Kidney Injury Samantha Mikesic






- Slides: 95
Chronic Kidney Disease & Acute Kidney Injury Samantha Mikesic Dietetic Intern
Clinical Site: Conemaugh Memorial Medical Center • More than 600 licensed acute, rehab and long-term beds. 1 • Vision: Excellence, Every Patient, Every Time. 1
Overview of disease Kidney’s function What is CKD? Etiology/ signs and symptoms Pathophysiology of CKD Classifications of CKD Diagnosis and Treatment MNT of CKD MNT with and without Dialysis Hemodialysis vs. Peritoneal Dialysis vs. CRRT Significant lab values in CKD Patient review ADIME notes Summary
Kidneys The kidneys are powerful chemical factories that perform the following functions: 2 Remove waste products from the body Balance the body's fluids and electrolytes Release hormones that regulate blood pressure Acid-base balance Endocrine Control the production of red blood cells
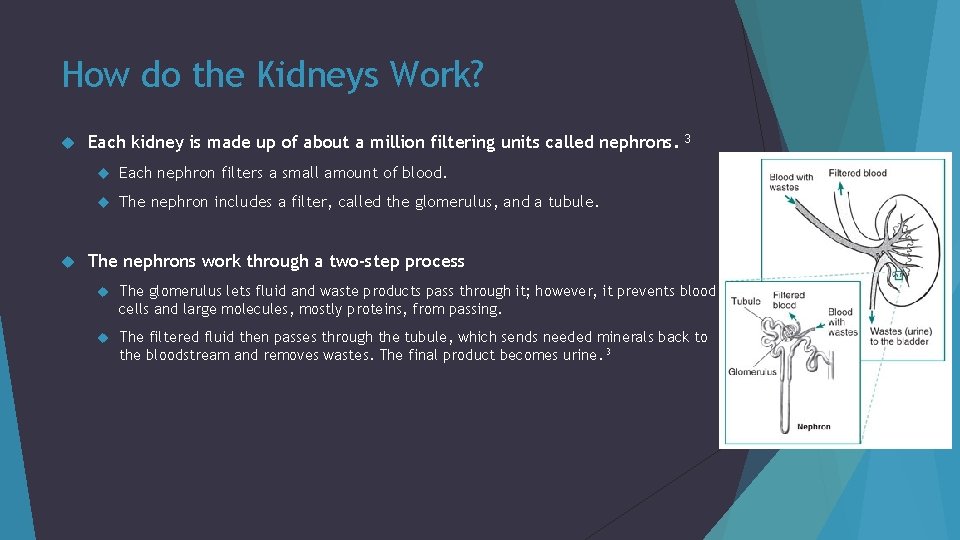
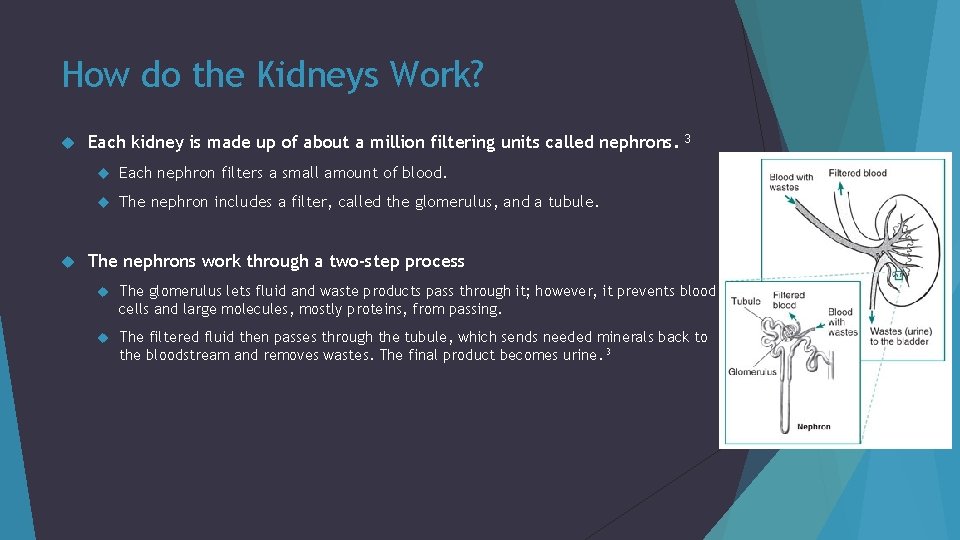
How do the Kidneys Work? Each kidney is made up of about a million filtering units called nephrons. Each nephron filters a small amount of blood. The nephron includes a filter, called the glomerulus, and a tubule. 3 The nephrons work through a two-step process The glomerulus lets fluid and waste products pass through it; however, it prevents blood cells and large molecules, mostly proteins, from passing. The filtered fluid then passes through the tubule, which sends needed minerals back to the bloodstream and removes wastes. The final product becomes urine. 3
What is CKD? Chronic kidney disease describes the gradual loss of kidney function Irreversible renal dysfunction that will progress over months to years 5 CKD includes conditions that damage your kidneys and decrease their ability to keep you healthy 2 CKD is kidney damage for ≥ 3 months, defined by structural or functional abnormalities of the kidney, with or without decreased glomerular filtration rate (GFR) 2, 5, 6
Facts about CKD 26 million American adults have CKD and millions of others are at increased risk. 2 People with CKD have significantly higher rates of morbidity, mortality, hospitalization, and healthcare utilization. The prevalence of CKD stages 2 -5 have continued to increase since 1988. 2
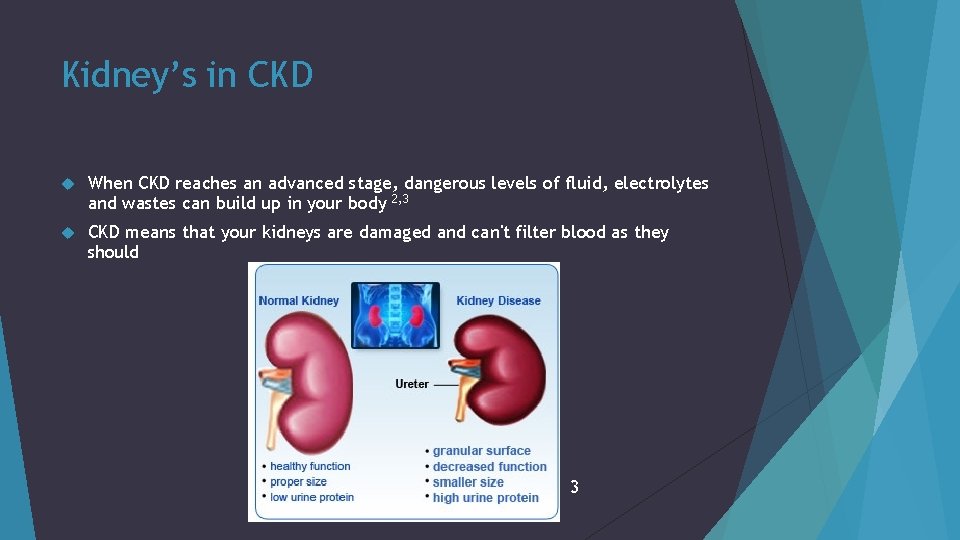
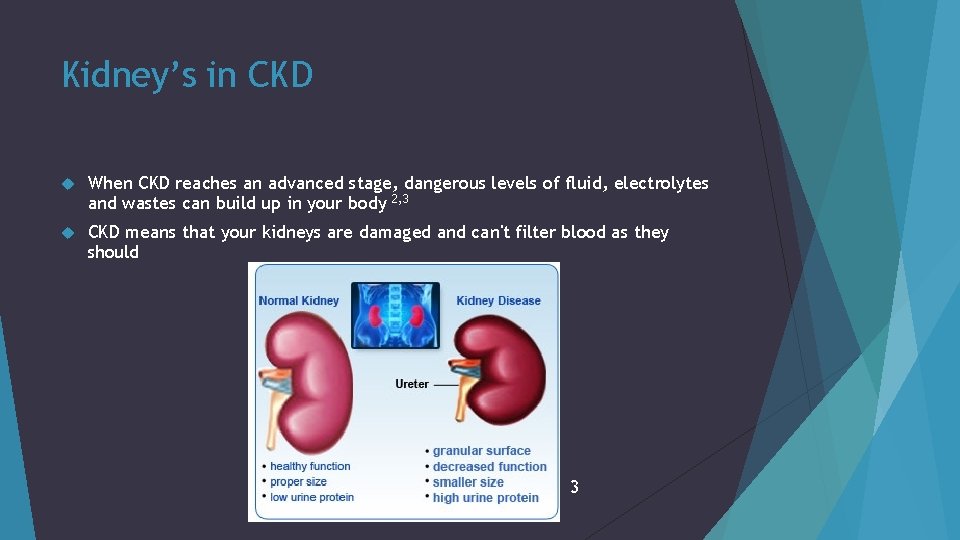
Kidney’s in CKD When CKD reaches an advanced stage, dangerous levels of fluid, electrolytes and wastes can build up in your body 2, 3 CKD means that your kidneys are damaged and can't filter blood as they should 3
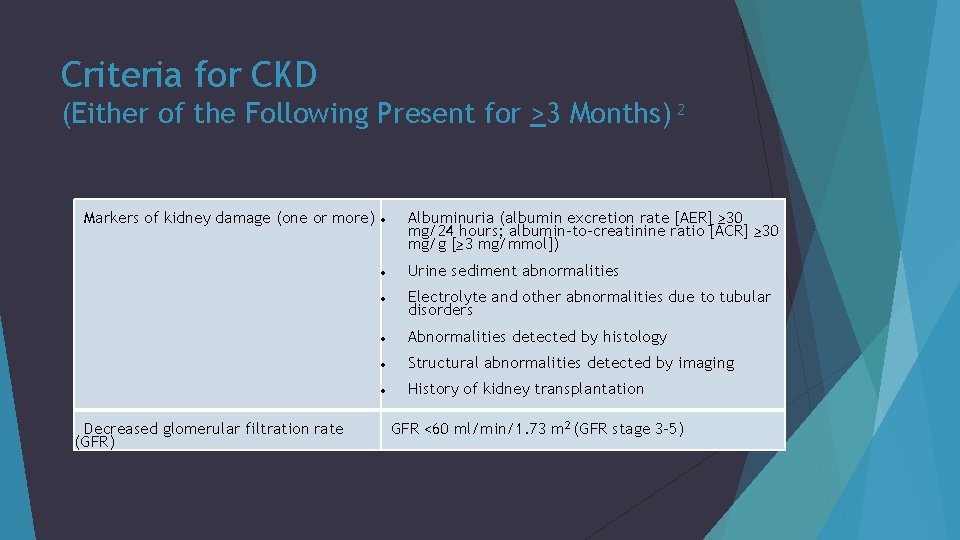
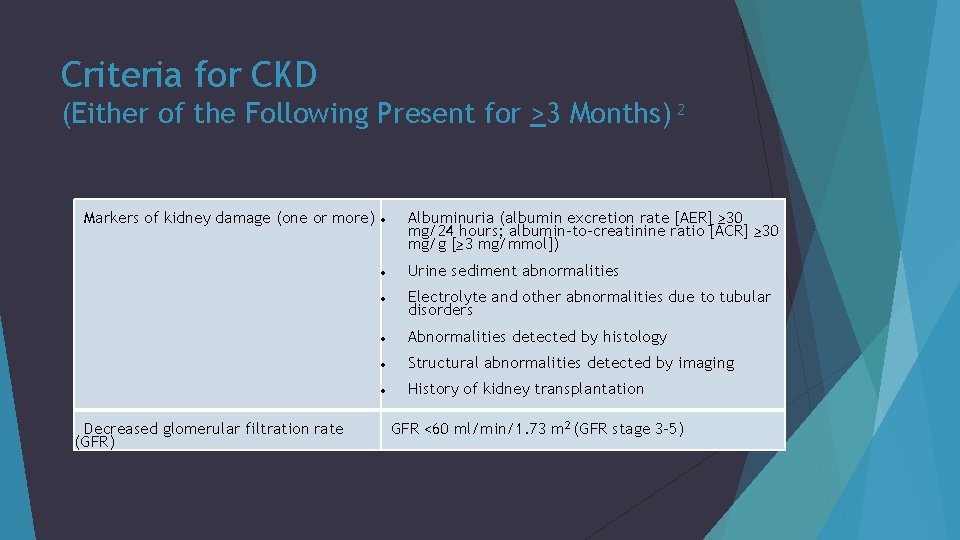
Criteria for CKD (Either of the Following Present for >3 Months) 2 Markers of kidney damage (one or more) Decreased glomerular filtration rate (GFR) Albuminuria (albumin excretion rate [AER] ≥ 30 mg/24 hours; albumin-to-creatinine ratio [ACR] ≥ 30 mg/g [≥ 3 mg/mmol]) Urine sediment abnormalities Electrolyte and other abnormalities due to tubular disorders Abnormalities detected by histology Structural abnormalities detected by imaging History of kidney transplantation GFR <60 ml/min/1. 73 m 2 (GFR stage 3 -5)
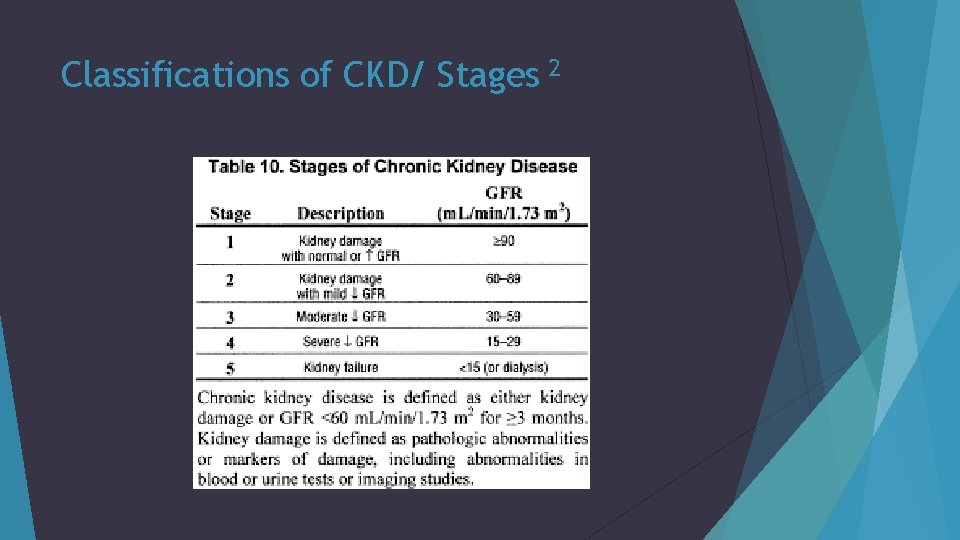
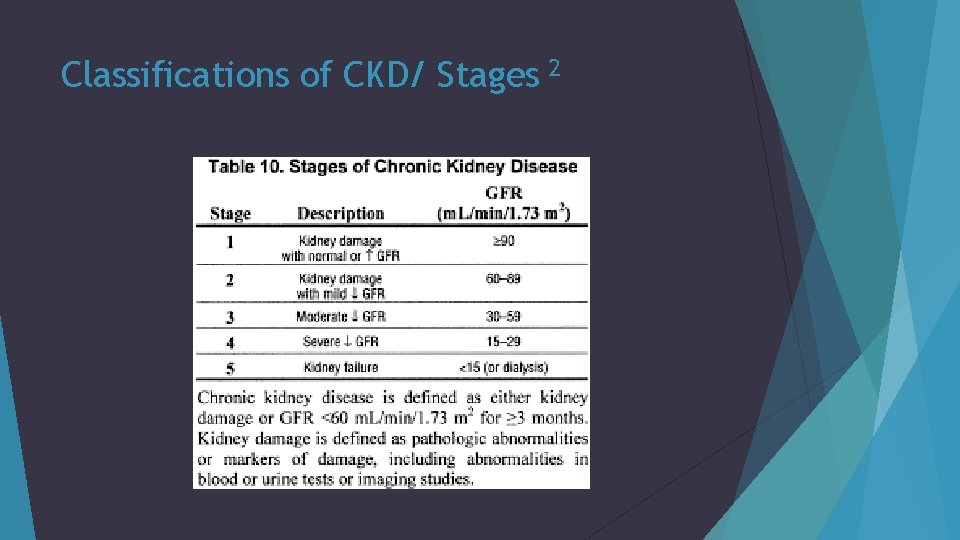
Classifications of CKD/ Stages 2
Symptoms of CKD Most people may not have any severe symptoms until their kidney disease is advanced. 2 Possible symptoms include: feel more tired and have less energy trouble concentrating poor appetite trouble sleeping muscle cramping at night swollen feet and ankles puffiness around your eyes dry, itchy skin urge to urinate more often
Etiology of CKD The two main causes of chronic kidney disease are diabetes and high blood pressure, which are responsible for up to two-thirds of the cases Other factors include 5 Glomerulonephritis Polycystic kidney disease Malformations in babies in the womb Lupus Obstructions caused by things like kidney stones or tumors Repeated urinary infections
Pathophysiology of CKD Kidney disease can affect glomeruli, tubules, interstitial tissue and/or vessels. The kidneys have limited ways of responding to inciting causes of damage 5 prolonged kidney injury promotes infiltration of inflammatory cells and pro-fibrotic cytokine production Fibroblast activation results in the production and deposition of collagen and other extracellular matrix components. 5 Hypoxia is often present due to increased oxidative stress plays a role in the pathogenesis of CKD.
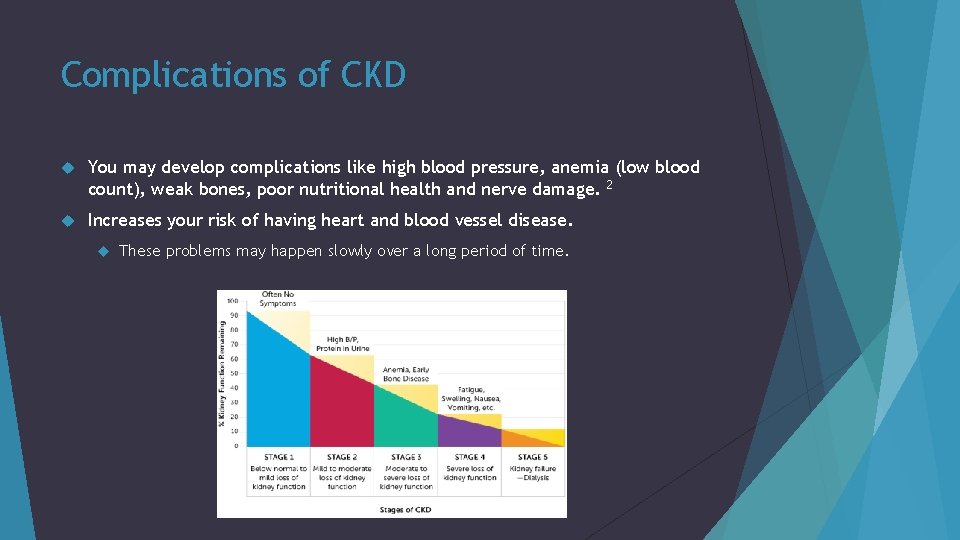
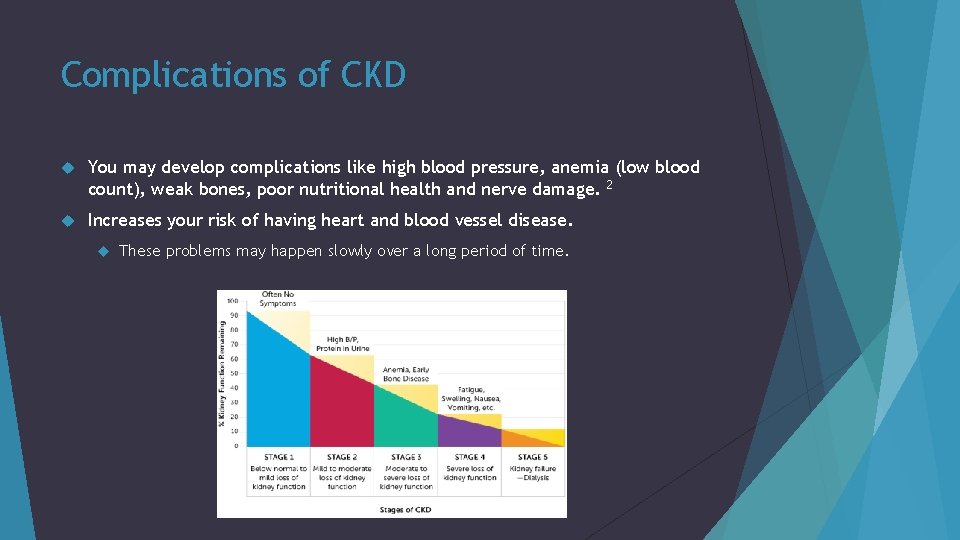
Complications of CKD You may develop complications like high blood pressure, anemia (low blood count), weak bones, poor nutritional health and nerve damage. 2 Increases your risk of having heart and blood vessel disease. These problems may happen slowly over a long period of time.
How do you Diagnose CKD? A urine test can determine if you have CKD Albumin Creatinine Ratio (ACR) Glomerular filtration rate (GFR) is the best estimate of kidney function Two simple tests can detect CKD: 2 blood pressure urine albumin and serum creatinine Kidney biopsy is done in some cases to check for a specific type of kidney disease, and see how much kidney damage has occurred 2

Other Diagnoses Diagnosis: 2 Screening for microalbuminuria Laboratory studies Urine studies for albuminuria Ultrasound imaging
Progression of CKD Fortunately, most patients do no progress from CKD stage 3 to 5 17% of CKD stage 4 patients will progress to stage 5 less than one percent of CKD stage 3 patients will progress to stage 5
Treatment and risk reduction of CKD progression Treatment: 8 Angiotensin converting enzyme inhibitor (ACEI) or an angiotensin receptor blocker (ARB) to prevent or decrease the rate of progression to end stage renal disease Blood pressure control Management of comorbid diabetes and consideration of cardiovascular risk factors Monitoring for CKD complications (anemia, electrolyte abnormalities, abnormal fluid balance, mineral bone disease, and malnutrition) Avoidance of nephrotoxic medications to prevent worsening of renal failure Follow-up Yearly assessment of GFR and albuminuria Referral to nephrology
MNT of CKD MNT prevents and treats protein-energy malnutrition and mineral and electrolyte disorders Minimizes that impact of other co-morbidities on the progression of kidney disease. 7
Assessment The RD should assess food and nutrition-related history of adult with chronic kidney disease (CKD) 7 -8 Food and nutrient intake Medications and dietary supplements Knowledge, beliefs, and attitudes Behavior Factors affecting access to food and nutrition-related supplies The RD should reassess the above at follow-up
Assessment cont. Use ideal body weight to assess nutritional needs Use dry weight or edema-free body weight In Hemodialysis patients: post-dialysis weight Body weight can be difficult to determine, because as the kidney function declines, the ability to regulate fluid balance may be compromised 7 -8 Pts on dialysis gain several kg of fluid between HD treatments If pts gain >5%, may reflect excessive fluid intake, leading to hypertension, edema, ascites, pleural effusion (Interdialytic weight gain) 7 -8
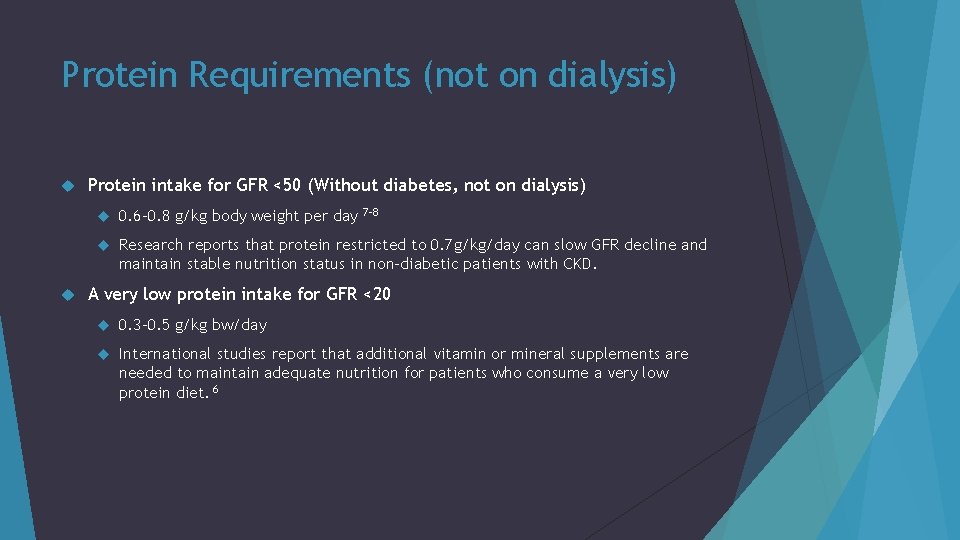
Protein Requirements (not on dialysis) Protein intake for GFR <50 (Without diabetes, not on dialysis) 0. 6 -0. 8 g/kg body weight per day Research reports that protein restricted to 0. 7 g/kg/day can slow GFR decline and maintain stable nutrition status in non-diabetic patients with CKD. 7 -8 A very low protein intake for GFR <20 0. 3 -0. 5 g/kg bw/day International studies report that additional vitamin or mineral supplements are needed to maintain adequate nutrition for patients who consume a very low protein diet. 6
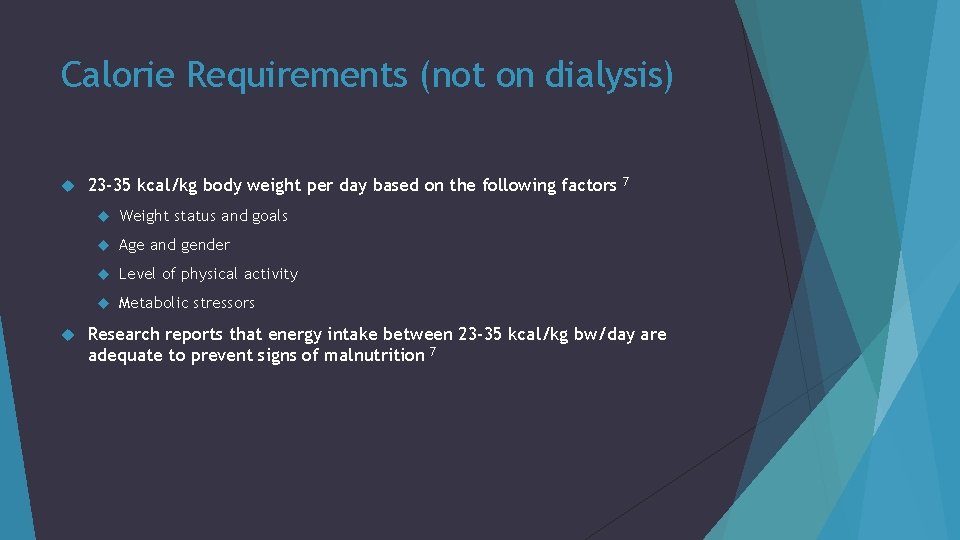
Calorie Requirements (not on dialysis) 23 -35 kcal/kg body weight per day based on the following factors Weight status and goals Age and gender Level of physical activity Metabolic stressors 7 Research reports that energy intake between 23 -35 kcal/kg bw/day are adequate to prevent signs of malnutrition 7
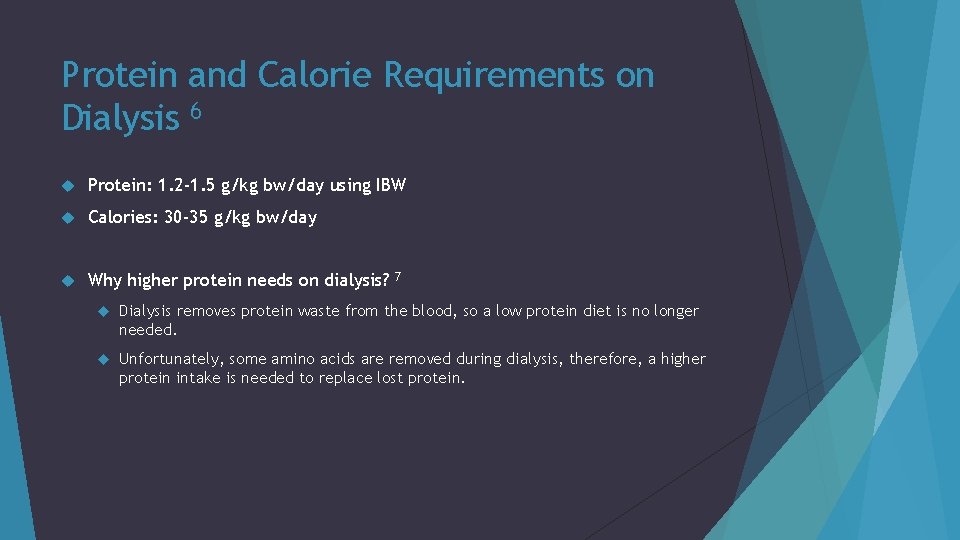
Protein and Calorie Requirements on Dialysis 6 Protein: 1. 2 -1. 5 g/kg bw/day using IBW Calories: 30 -35 g/kg bw/day Why higher protein needs on dialysis? 7 Dialysis removes protein waste from the blood, so a low protein diet is no longer needed. Unfortunately, some amino acids are removed during dialysis, therefore, a higher protein intake is needed to replace lost protein.
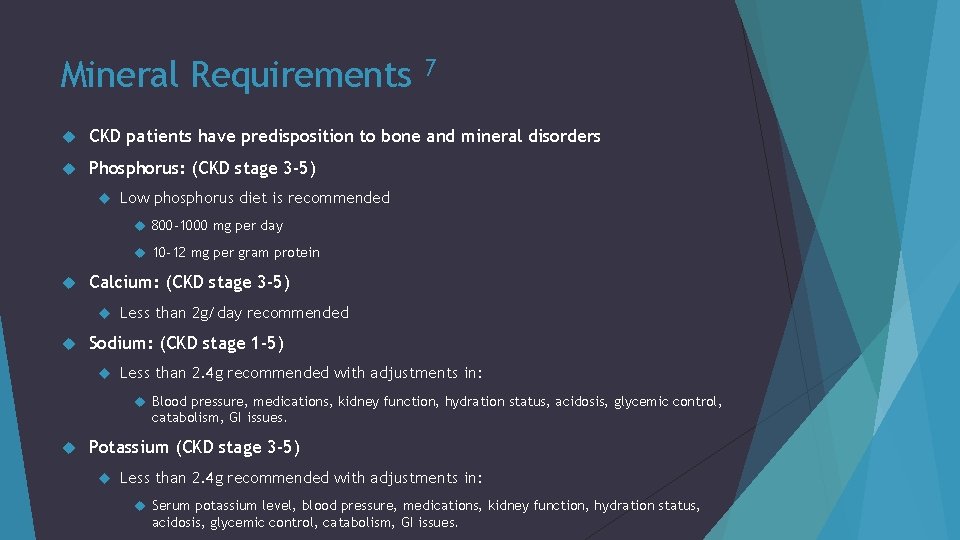
Mineral Requirements 7 CKD patients have predisposition to bone and mineral disorders Phosphorus: (CKD stage 3 -5) Low phosphorus diet is recommended 800 -1000 mg per day 10 -12 mg per gram protein Calcium: (CKD stage 3 -5) Less than 2 g/day recommended Sodium: (CKD stage 1 -5) Less than 2. 4 g recommended with adjustments in: Blood pressure, medications, kidney function, hydration status, acidosis, glycemic control, catabolism, GI issues. Potassium (CKD stage 3 -5) Less than 2. 4 g recommended with adjustments in: Serum potassium level, blood pressure, medications, kidney function, hydration status, acidosis, glycemic control, catabolism, GI issues.
Dialysis What is dialysis? 9, 10 Dialysis is a way of cleaning your blood when your kidneys can no longer do the job. It gets rid of your body's wastes, extra salt and water, and helps to control your blood pressure. Types of Dialysis Hemodialysis Peritoneal Dialysis CRRT
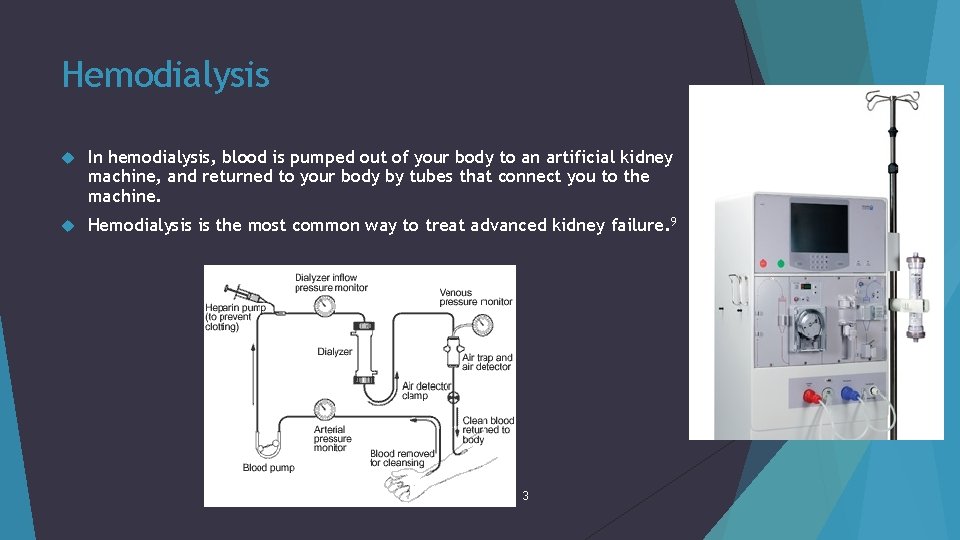
Hemodialysis In hemodialysis, blood is pumped out of your body to an artificial kidney machine, and returned to your body by tubes that connect you to the machine. Hemodialysis is the most common way to treat advanced kidney failure. 9 3
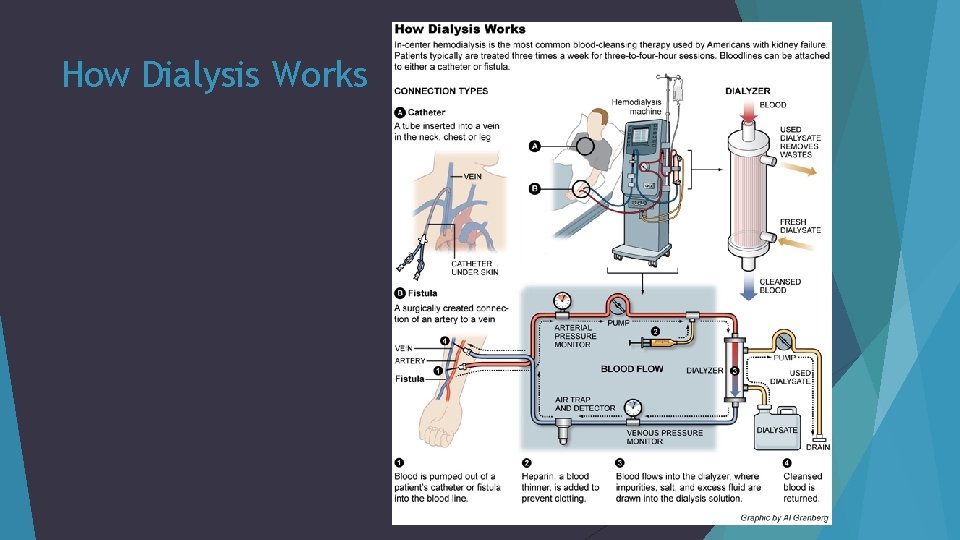
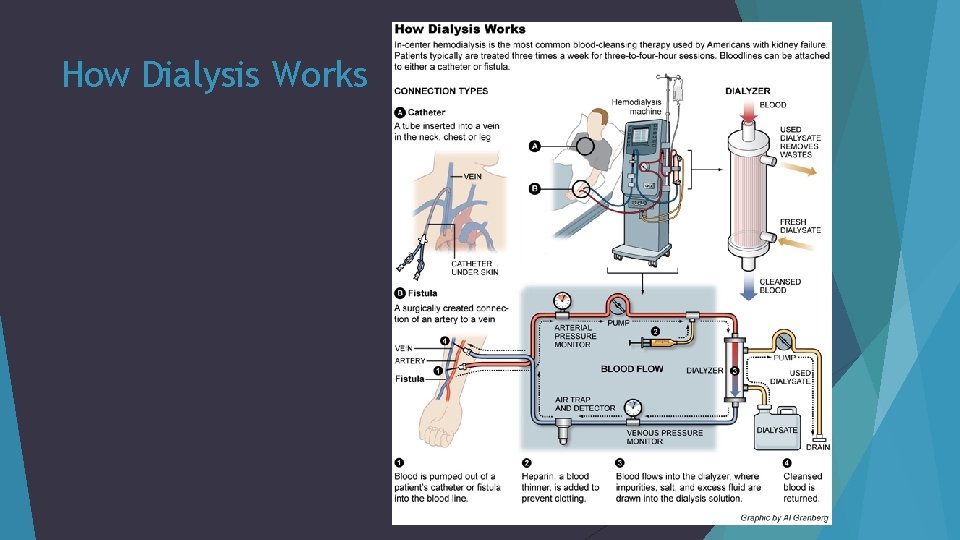
How Dialysis Works
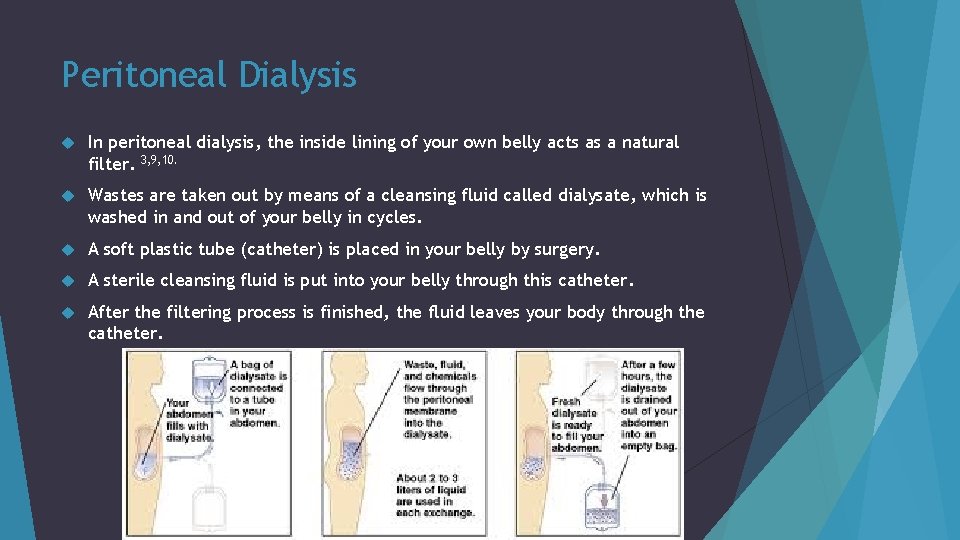
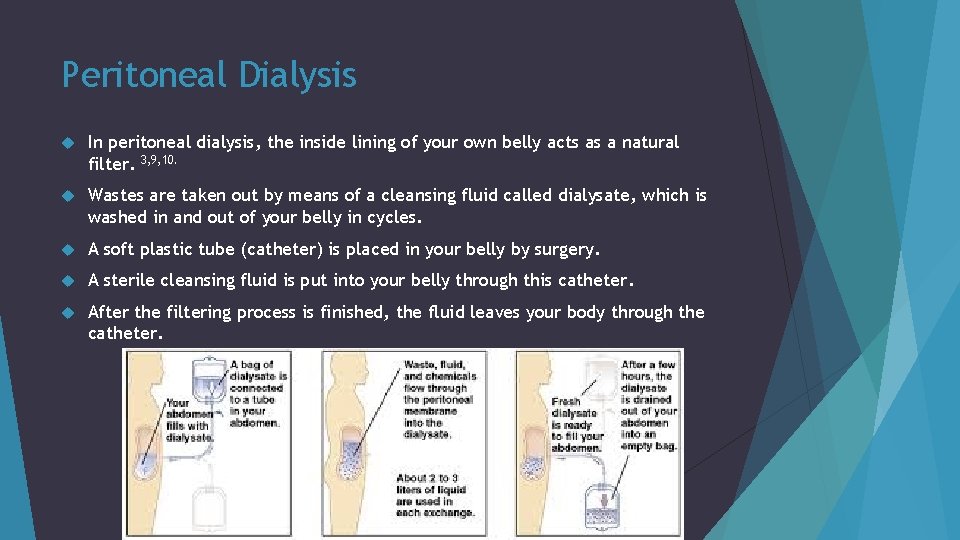
Peritoneal Dialysis In peritoneal dialysis, the inside lining of your own belly acts as a natural filter. 3, 9, 10. Wastes are taken out by means of a cleansing fluid called dialysate, which is washed in and out of your belly in cycles. A soft plastic tube (catheter) is placed in your belly by surgery. A sterile cleansing fluid is put into your belly through this catheter. After the filtering process is finished, the fluid leaves your body through the catheter.
Continuous Renal Replacement Therapy (CRRT) CRRT is a dialysis modality used to treat critically ill, hospitalized patients in the intensive care unit. Intended to be applied for 24 hours per day in an ICU. The major advantage of continuous therapy is the slower rate of solute or fluid removal per unit of time. Thus, CRRT is generally better tolerated than conventional therapy since many of the complications of intermittent hemodialysis are related to the rapid rate of solute and fluid loss. 9, 10
Significant Lab Values in CKD 4, 7, 8, 11, 12 Blood Urea Nitrogen (BUN): Normal range- 7– 22 mg/d. L Urea nitrogen is a normal waste product in your blood that comes from the breakdown of protein from the foods you eat and from your body metabolism. It is normally removed from your blood by your kidneys, but when kidney function slows down, the BUN level rises. BUN can also rise if you eat more protein, and it can fall if you eat less protein. Serum Creatinine: Normal range- 0. 8 to 1. 4 mg/dl Creatinine is a waste product in your blood that comes from muscle activity. It is normally removed from your blood by your kidneys, but when kidney function slows down, the creatinine level rises.
Significant Lab Values in CKD cont. Serum Albumin: normal range- 3. 5 -5. 0 g/dl A low level of albumin in your blood may be caused by not getting enough protein or calories from your diet. Urine Protein: normal range- 6. 0 – 8. 0 g/d. L, < 150 mg/24 hr (urine) When your kidneys are damaged, protein leaks into your urine. A simple test can be done to detect protein in your urine. Persistent protein in the urine is an early sign of chronic kidney disease.
Significant Lab Values in CKD cont. Hematocrit: Females 37– 46%, Males 42 – 52% Your hematocrit is a measure of the red blood cells your body is making. A low hematocrit can mean you have anemia and need treatment with iron and EPO. Hemoglobin: Females- 12. 3 – 15. 7 g/d. L, Males- 14. 0 – 17. 4 g/d. L Hemoglobin is the part of red blood cells that carries oxygen from your lungs to all parts of your body. Your hemoglobin level tells your doctor if you have anemia If you have anemia, you may need treatment with iron supplements and a hormone called erythropoietin (EPO).
Significant Lab Values in CKD cont. Sodium: normal range- 135 – 145 m. Eq/L Calcium: normal range- 8. 7 – 10. 3 mg/d. L Phosphorus: normal range- 2. 5 – 4. 5 mg/d. L High phosphorus level can lead to weak bones. Potassium: normal range-3. 5 – 5. 0 m. Eq/L Potassium is a mineral in your blood that helps your heart and muscles work properly. A potassium level that is too high or too low may weaken muscles and change your heartbeat.
Patient: Admission 1/1/2016 87 year old Caucasian female Chief Complaint: shortness of breath and edema Patient admitted on 1/1/2016 with Acute on Chronic Heart Failure exacerbations, Acute Kidney Injury (AKI), and Hyponatremia
Anthropometrics Ht: 137. 16 cm (54”) patient stated Wt: 68. 1 kg (149. 8 lbs) actual July 2015: 54. 6 kg (13. 5 kg wt gain in 6 months) BMI: 36. 2 BMI indicates pt. is obesity grade II. BMI may be falsely skewed upward due to +1 to +3 pitting edema
Social History Pt. denies tobacco, alcohol, or drug use Pt. lives at home She is on home hospice
Past Medical History Atrial fibrillation Congestive heart failure Systolic with EF 38% in June 2015 End-stage renal disease with stents, not on hemodialysis CKD stage III with hx of AKI multiple episodes including in the setting of solitary functioning kidney ad left-sided hydronephrosis CAD status post stents Hypertension Macular degeneration

Past surgical history Left total knee arthroplasty Pacemaker placement
Medications at home Bumex 1 mg daily It can treat fluid retention (edema) and high blood pressure.
Current Medication Ferrous Sulfate (iron): to treat iron deficiency anemia Famotidine (pepsid): treat heart burn Carvedilol (Coreg): beta blocker Pantoprazole (protonix): proton pump inhibitor Miconazole nitrate: treat skin infection Sodium chloride: to treat low sodium Epoetin alfa: to treat anemia Senna-doc: stool softener and a laxative Oxycodone: opioid pain medication Lasix: Diuretic
Lasix: Furosemide Lasix (furosemide) is a loop diuretic (water pill) that prevents your body from absorbing too much salt, allowing salt to instead be passed in your urine. 11 Furosemide belongs to the class of medications called diuretics. It is used to treat edema that occurs with congestive heart failure and disorders of the liver, kidney, and lung. It is also used to control mild to moderate high blood pressure. It may be used in combination with other medications to treat more severe high blood pressure. Furosemide works by increasing the amount of urine produced and excreted, and by removing excessive water (edema) from the body.
Protonix: pantoprazole Protonix (pantoprazole) is a proton pump inhibitor that decreases the amount of acid produced in the stomach, used to treat gastroesophageal reflux disease (GERD) 14 Proton pump inhibitors are substituted benzimidazole derivatives that inhibit the proton pump (H+/K+ ATPase) in the parietal cells of the stomach. The proton pump is the final common pathway for gastric acid secretion where hydrogen ions are exchanged for potassium ions. Pantoprazole is the only PPI available for intravenous (IV) administration; it is also packaged as 40 mg tablets.
Epoetin alfa Epoetin is indicated for the treatment of anemia associated with chronic renal failure 13 Epoetin alfa is a glycoprotein, produced by recombinant DNA technology, that contains 165 amino acids in a sequence identical to that of endogenous human erythropoietin Endogenous erythropoietin is produced primarily in the kidney. The anemia associated with chronic renal failure is caused primarily by inadequate production of the hormone (EPO) EPO binds to the erythropoietin receptor on the red cell progenitor surface and activates a JAK 2 signaling cascade. High level erythropoietin receptor expression is localized to erythroid progenitor cells.
Diagnosis Impression Acute exacerbation of congestive heart failure Pt. has history of CHF and has bilateral pleural edema with shortness of breath and orthopnea (difficulty breathing when lying down) Kidney function has definitely taken injury (Acute Kidney Injury)
Nephrology Report Dx: CKD stage III, AKI, CHF exacerbation CKD stage III due to solitary functioning kidney, nephrosclerosis Acute on chronic kidney injury in setting of fluid overload improving Hypokalemia in setting of diuretics Metabolic alkalosis in the setting of diuretics and likely due to respiratory acidosis with hx of chronic alkalosis Hx of HTN, controlled
Nephrology Plan Continue with diuretics, Lasix 40 mg IV daily Give IV Diamox in setting of metabolic alkalosis and volume overload Will follow electrolyte, renal function, volume status Monitor weights daily Avoid nephrotoxins
Physical Assessment Pt. is awake, alert, and oriented Pt. appears pale Breathing appears slightly labored but in no apparent distress Significant pedal edema +1 or +2 pitting edema Abdomen is soft, non-tender, and distended Large hernia present Soft and reducible Bowel sounds are present
Initial Assessment 1/6/2016 Moderate Risk (reassess every 5 -6 days) Pt. arrived from home Reason for consult: length of stay Diagnosis: Acute CHF exacerbation, AKI, hyponatremia (No PES at this time)
Anthropometrics Wt. changes: 3. 9 kg wt. loss since admission Wt. loss possibly due to diuretics, pt. on IV furosemide Mental Status: Appears alert Appetite: Good Intake: Varies PO intake varies 25 -75%. Pt states she only eats about half of her meals because they are too large of portions. Observed pt. tray, she was sent waffles, oatmeal, cheerios, and beverages. Pt. did consume 100% of cheerios, 50% of waffle, and bites of oatmeal.
Patient’s needs (ESRD not on dialysis) Ideal Body Weight: Protein: 0. 6 -0. 8 g/kg 45. 5 kg 27 -36 g protein Calories: 25 -30 kcal/kg 1138 -1365 kcal/day
Lab values Glucose high: 131 Blood urea nitrogen (BUN) high: 30 Creatinine high: 3. 1 Sodium (Na+) low: 130 Hemoglobin (Hgb) low: 10. 2 Hematocrit (Hct) low: 32 GFR: 52 (Indicates CKD stage 3)
Medical Tests: Xray of chest: Cardiomegaly with pulmonary vascular congestion Enlarged heart with excessive accumulation of fluid in the lungs, indicating CHF. Blood creatinine test helps to estimate the glomerular filtration rate (GFR) by measuring the level of creatinine in your blood. GFR: 52 (CKD st 3) Creatinine high A blood urea nitrogen (BUN) test measures how much nitrogen from the waste product urea is in your blood. BUN level rises when the kidneys aren't working well enough to remove urea from the blood. BUN high A fasting blood glucose test is done to measure your blood sugar. High blood sugar levels damage blood vessels in the kidneys. Glucose high Blood tests measure levels of waste products and electrolytes in your blood that should be removed by your kidneys. Na+ low
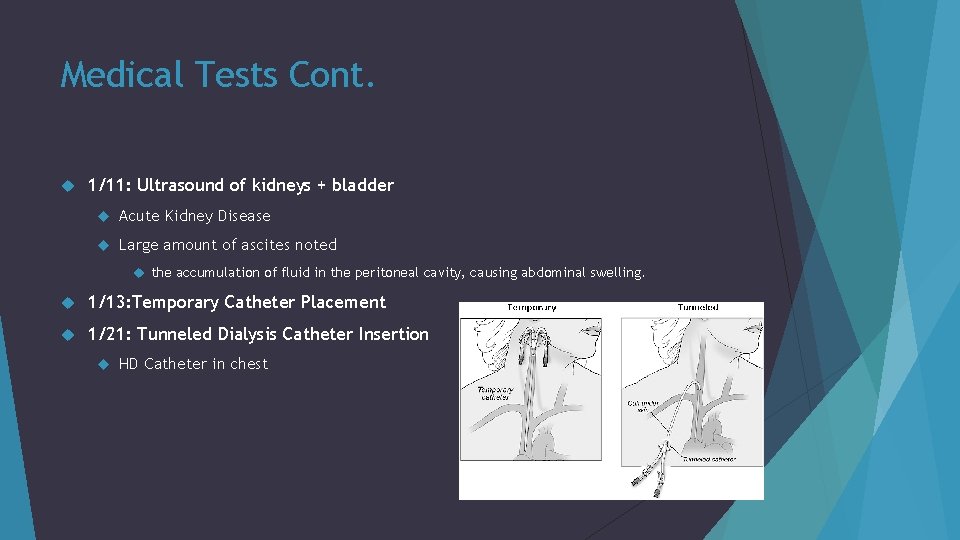
Medical Tests Cont. 1/11: Ultrasound of kidneys + bladder Acute Kidney Disease Large amount of ascites noted the accumulation of fluid in the peritoneal cavity, causing abdominal swelling. 1/13: Temporary Catheter Placement 1/21: Tunneled Dialysis Catheter Insertion HD Catheter in chest
Intervention Intake encouraged Patient contacted Chart reviewed See recommendations Current Diet: Regular (house), 2000 ADA, Na 4 g, Cardiac (low cholesterol, 4 g Na), 1200 cc/day. Recommend change diet to Regular (house), Na 2 g, Cardiac (low cholesterol, 4 g Na) Recommend discontinue (d/c) ADA diet due to no history of diabetes
Intervention cont. Goal: adequate nutrition, adequate intake Goal is to prevent skin breakdown: Reddened areas noted Will not recommend PO supplements at this time, will continue to monitor pts intakes Recommend encourage intake Recommend daily weights

Monitor and Evaluation Will monitor: Intake Appetite Weight Labs Hydration Diet tolerance Nutrition Status No nutrition education indicated at this time
Reassessment 1/12/2016 High Risk (every 3 -4 days) Diagnosis updated: unsuccessful foley catheter attempt Catheter in bladder to drain urine Wt: 72. 1 kg (gain) +1 LE edema noted Mental Status: Appears alert/ question reliability Appetite: poor Intake: varies, nausea, distention PO intake ranges from 0 -75%. Average 30%. Pt complaints of (c/o) nausea RN stated pt. is having some abdominal distention, but continues to have bowel movements (BM)
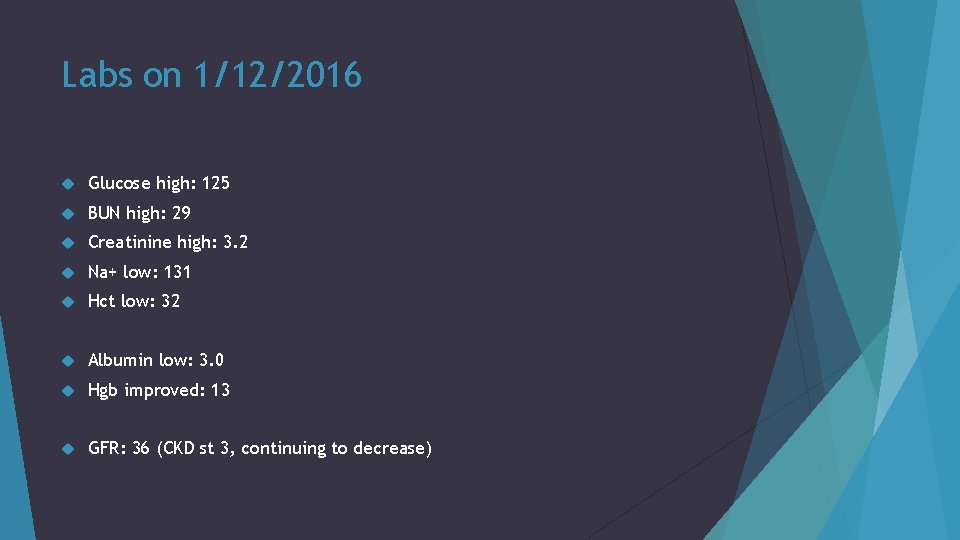
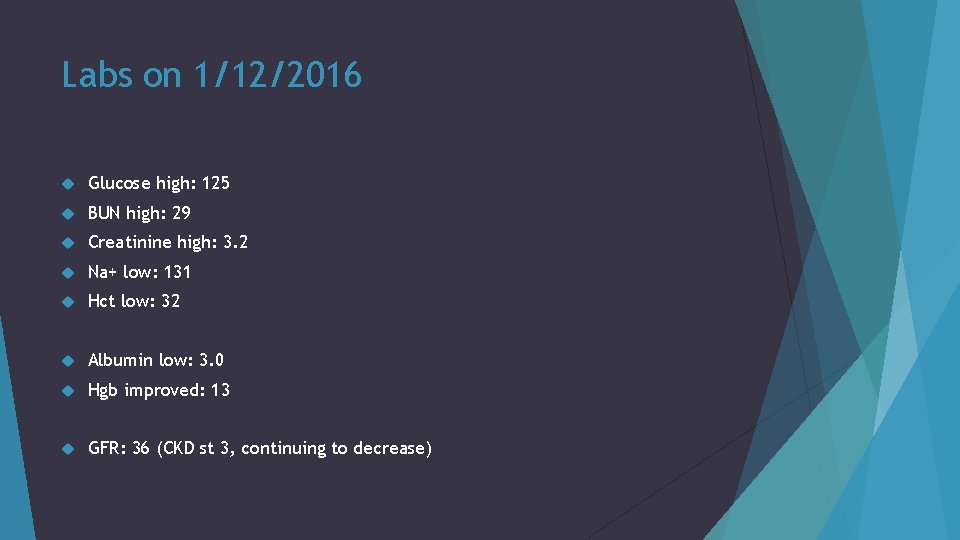
Labs on 1/12/2016 Glucose high: 125 BUN high: 29 Creatinine high: 3. 2 Na+ low: 131 Hct low: 32 Albumin low: 3. 0 Hgb improved: 13 GFR: 36 (CKD st 3, continuing to decrease)
Diagnosis PES #1: Predicted suboptimal energy intake r/t decreased appetite AEB average PO intake of 30%.
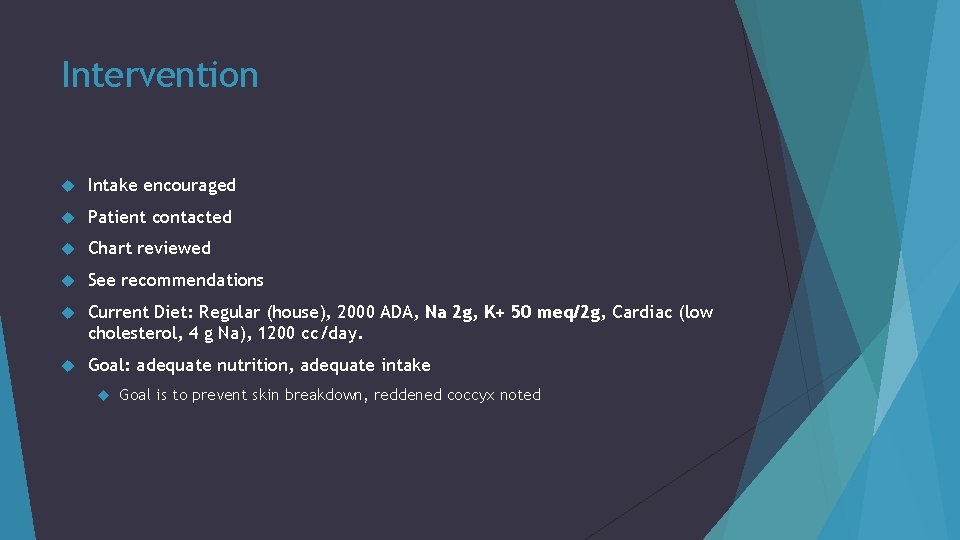
Intervention Intake encouraged Patient contacted Chart reviewed See recommendations Current Diet: Regular (house), 2000 ADA, Na 2 g, K+ 50 meq/2 g, Cardiac (low cholesterol, 4 g Na), 1200 cc/day. Goal: adequate nutrition, adequate intake Goal is to prevent skin breakdown, reddened coccyx noted
Calculating K+ needs K+ (IBW x 40) /39 (45. 5 x 40)/39 = 47 Recommend: K+ 50 meq/2 g
Intervention Cont. Recommend: Change diet Regular, Na 2 g, Cardiac (low cholesterol, 4 g. Na) Recommend Health shakes once daily, and magic cups once daily Health Shake Nutrition: 200 calories, 6 g protein Magic Cup Nutrition: 290 calories, 9 g protein Encourage intake Supplements Daily weights
Monitoring and Evaluation Monitor: Intake Appetite Weights Labs Hydration Diet tolerance Supplement intake Nutrition status
Reassessment 1/14/2016 High Risk (every 3 -4 days) Consult: New start Hemodialysis and Length of stay Diagnosis updated: Pleural effusion, new start Hemodialysis (HD) Wt: 68. 7 kg Pt receiving IV Furosemide Appetite: poor Intake: inadequate PO intake has been 0% at most meals since last encounter
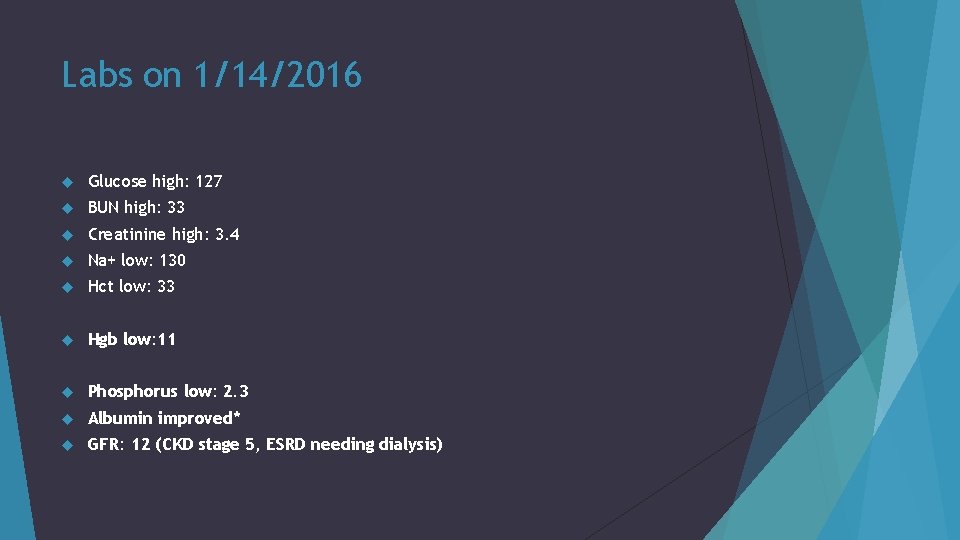
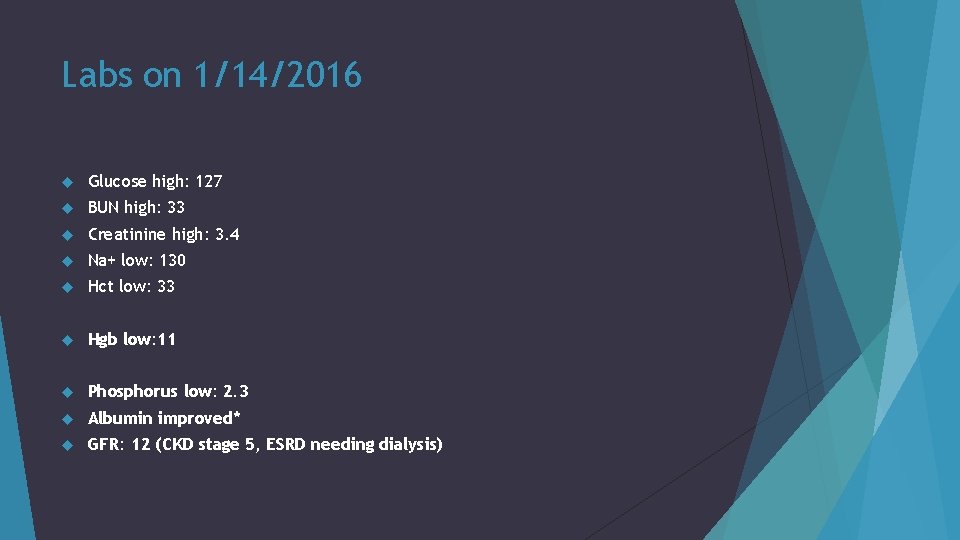
Labs on 1/14/2016 Glucose high: 127 BUN high: 33 Creatinine high: 3. 4 Na+ low: 130 Hct low: 33 Hgb low: 11 Phosphorus low: 2. 3 Albumin improved* GFR: 12 (CKD stage 5, ESRD needing dialysis)
Diagnosis PES #1: Revised Predicted suboptimal energy intake r/t decreased appetite AEB suboptimal meal completion. PES #2: Increased protein-calorie needs r/t increased demand for hemodialysis AEB new start HD, and estimated protein calorie needs.
Patient Needs: ESRD on hemodialysis IBW: 45. 5 kg Protein 1. 2 -1. 5 g/kg bw Calories 30 -35 kcal/kg bw 55 -68 g protein/day 1365 -1593 kcal/day Fluid needs will vary on hemodialysis
Intervention Intake encouraged Patient contacted Chart reviewed See recommendations Current Diet: Regular (house), 2000 ADA, Na 2 g, Cardiac (low cholesterol, 4 g Na), 1200 cc/day. Health shakes once daily, magic cup once daily. Goal: adequate nutrition, adequate intake
Intervention Cont. Recommend diet and supplement changes for dialysis and encourage PO intake: Recommend daily weights Diet change recommendations: Regular (house), 2 g Na, cardiac (low chol, 4 g Na), phosphorus restriction Nepro BID Nutrition: 425 calories, 19. 1 g protein
Monitoring and Evaluation Monitor: Intake Appetite Weights Labs Hydration Diet tolerance Supplement intake Nutrition status

Reassessment 1/18/2016 High Risk (every 3 -4 days) Diagnosis updated: Acute CHF, AKI, pleural effusion, ESRD new start HD. Wt: 63. 6 kg 8. 4 kg loss in 2 weeks BMI 33. 7. BMI indicates pt. is obesity grade I. +2 pitting edema noted. Appetite: poor Intake: Inadequate Pt. is consuming an average of 45% of meals.

Labs 1/18/2016 Glucose high: 137 BUN high: 46 (Increasing) Creatinine high: 3. 4 Na+ low: 135 Hct low: 32 Hgb low: 10. 5 GFR: 13 (CKD stage 5, ESRD needing dialysis)
Diagnosis PES 1 & 2 remain
Intervention Chart reviewed See recommendations Current Diet: Regular (house), 2000 ADA, Na 2 g, phosphorus restriction, cardiac (low cholesterol, 4 g Na), 1200 cc/day, protein 90 g. Nepro BID and Magic cup once daily. Goal: adequate nutrition, promote healing, adequate intake Goal is to promote healing, reddened coccyx and tear in right shin noted
Intervention Cont. Recommend change diet, encourage intake, supplements, daily weights Diet change recommendations: Regular (house), 2 g Na, cardiac (low cholesterol, 4 g Na), protein 70 g. Recommend remove phosphorus restriction, decrease protein requirements from 90 g, and remove 2000 ADA diet. Phosphorus normal at this time, will continue to monitor labs to determine if restrictions are necessary
Monitoring and Evaluation Monitor: Intake Appetite Weights Labs Hydration Diet tolerance Supplement intake Nutrition status
Dietary Teaching 1/19/2016 Discussed Renal diet while on dialysis Talked with pt and family member about the importance of supplements to ensure adequate protein intake. Learning barriers: Physical Pt. seemed lethargic and did not respond to education at this time Family member stated pt. is consuming 50% of supplements Will continue to monitor intake and follow up with education needs
Reassessment 1/21/2016 High Risk (every 3 -4 days) Diagnosis updated: New start HD, ESRD Wt: 62. 8 kg 0. 8 kg loss in one week, wt loss possibly due to edema BMI 33. 3. BMI indicates pt. is obesity grade I. BMI would be inaccurate due to +2 pitting edema Appetite: poor Intake: Inadequate Pt. is consuming an average of 41% of meals.
Labs 1/21/2016 Glucose high: 122 BUN high: 33 Creatinine high: 3. 0 Na+ low: 135 Hgb low: 9. 7 Hct low: 31 GFR: 14 (ESRD)
Diagnosis PES 1 & 2 remain
Intervention Patient contacted Chart reviewed See recommendations Current Diet: Regular (house), 2000 ADA, Na 2 g, phosphorus restriction, cardiac (low cholesterol, 4 g Na), 1200 cc/day, protein 90 g. Nepro BID and Magic cup once daily. Goal: adequate nutrition, promote healing, adequate intake Goal is to promote healing, reddened coccyx and left buttocks noted
Intervention Cont. Recommend change diet, encourage intake, supplements, daily weights Diet change recommendations stand (1/18/2016) Regular (house), 2 g Na, cardiac (low cholesterol, 4 g Na), protein 70 g. Recommend remove phosphorus restriction, decrease protein requirements from 90 g, and remove 2000 ADA diet. If PO intake does not improve will discuss tube feedings with pt. and family. No POLST in chart. No family at bedside at time of visit. Will continue to monitor PO and supplement intake
Monitoring and Evaluation Monitor: Intake Appetite Weights Labs Hydration Diet tolerance Supplement intake Nutrition status
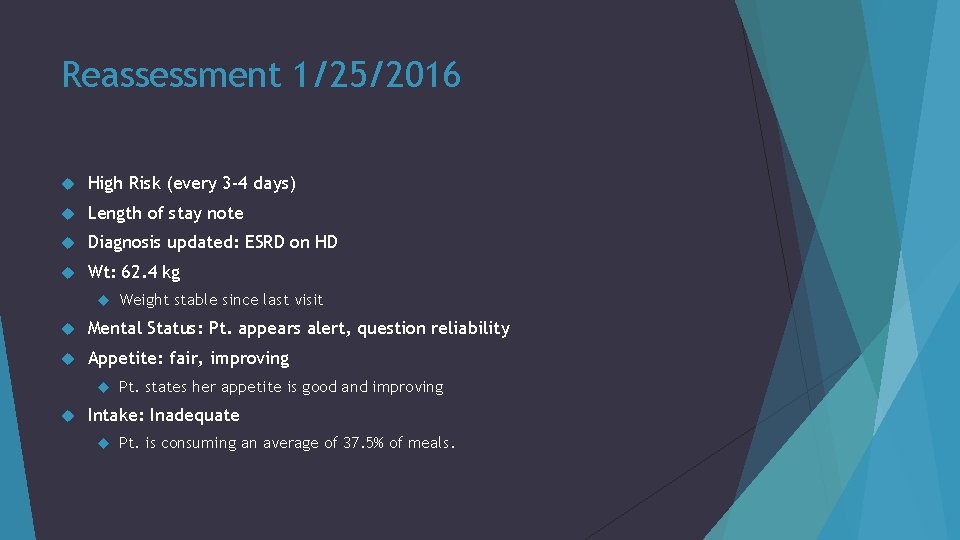
Reassessment 1/25/2016 High Risk (every 3 -4 days) Length of stay note Diagnosis updated: ESRD on HD Wt: 62. 4 kg Weight stable since last visit Mental Status: Pt. appears alert, question reliability Appetite: fair, improving Pt. states her appetite is good and improving Intake: Inadequate Pt. is consuming an average of 37. 5% of meals.
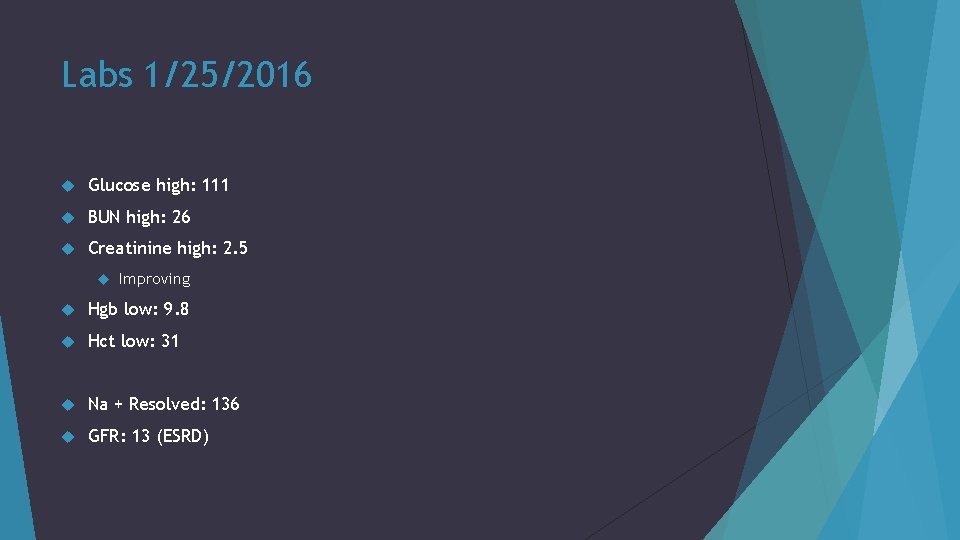
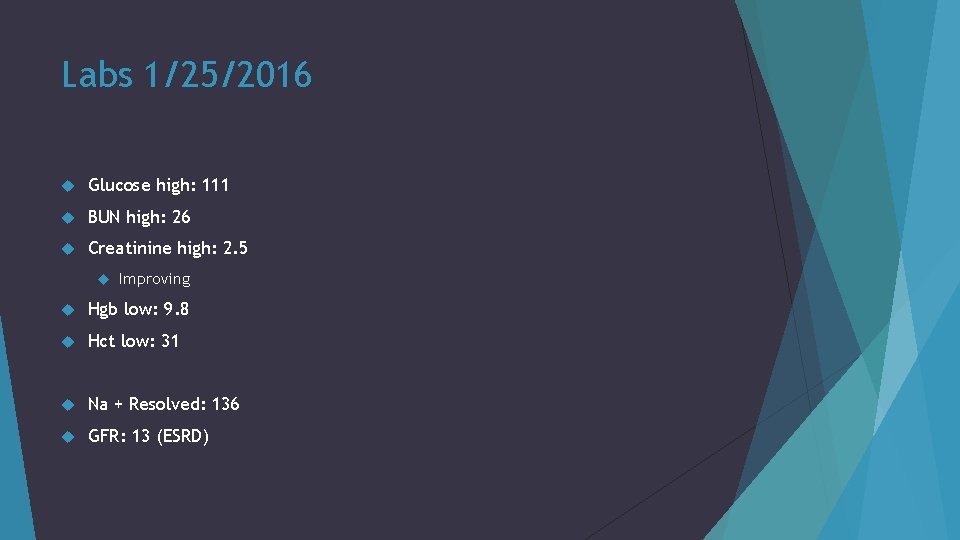
Labs 1/25/2016 Glucose high: 111 BUN high: 26 Creatinine high: 2. 5 Improving Hgb low: 9. 8 Hct low: 31 Na + Resolved: 136 GFR: 13 (ESRD)
Diagnosis PES 1 remains PES 2 revised: Increased protein calorie needs r/t increased demand for wound healing and hemodialysis, AEB impaired skin integrity and new start HD.
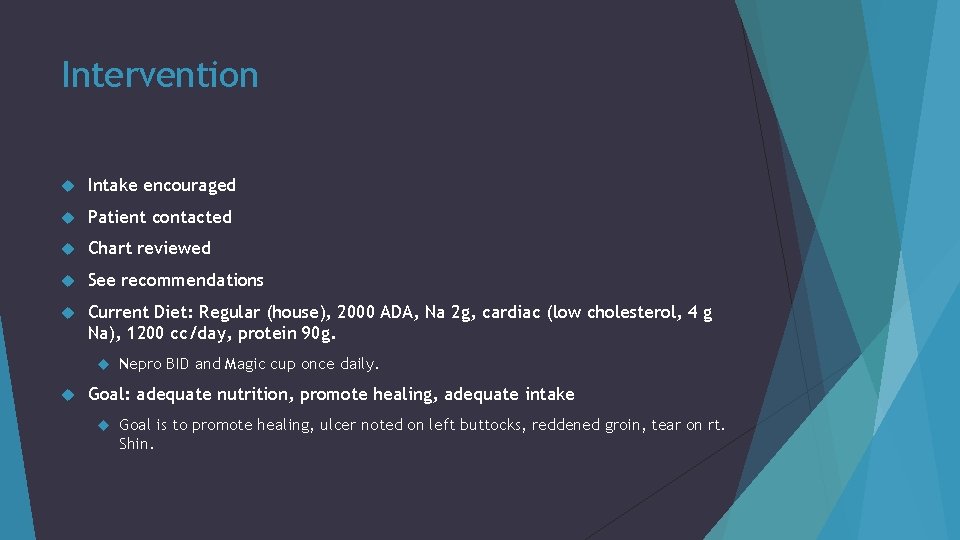
Intervention Intake encouraged Patient contacted Chart reviewed See recommendations Current Diet: Regular (house), 2000 ADA, Na 2 g, cardiac (low cholesterol, 4 g Na), 1200 cc/day, protein 90 g. Nepro BID and Magic cup once daily. Goal: adequate nutrition, promote healing, adequate intake Goal is to promote healing, ulcer noted on left buttocks, reddened groin, tear on rt. Shin.

Intervention Cont. Recommend Continue current plan of care Encourage intake Daily weights
Monitoring and Evaluation Monitor: Intake Appetite Weights Labs Hydration Diet tolerance Supplement intake Nutrition status
Dietary Teaching Learning barriers: Physical and Cognitive Talked with patient about the importance of protein and supplement intake Pt. stated that she would try to consume at least half of her supplements when provided Overall, pt. is stable and maintaining her CKD with hemodialysis and diet
Patient Discharged 1/27/2016 Pt. is discharged to a nursing home Pt. is continuing to come to Conemaugh as an outpatient to receive hemodialysis 3 x per week Discharge Dx: Acute on chronic systolic and diastolic CHF Acute on chronic kidney disease, CKD stage 5 on HD Anasarca (extreme generalized edema) Secondary Dx: Bilateral pleural effusion Volume overload Cirrhosis and ascites
Follow up 2/8/2016 Pt. continuing to get hemodialysis 3 x/week at Conemaugh to maintain CKD Pt. labs on 2/8: Glucose: 127 high BUN: 33 high Creatinine: 3. 5 high Hgb: 10. 2 low Hct: 33 low K+, Phosphorus, and Na+ all normal at this time
References 1. Conemaugh. org. Conemaugh Health System. 2016. Available at: http: //www. conemaugh. org/. 2. The National Kidney Foundation Kidney Disease Outcomes Quality Initiative (NKF KDOQI). 2014. Available at: https: //www. kidney. org/professionals/guidelines. 3. Niddk. nih. gov. The Kidneys and How They Work. 2016. Available at: http: //www. niddk. nih. gov/healthinformation/health-topics/Anatomy/kidneys-how-they-work/Pages/anatomy. aspx. 4. Chronic Kidney Disease: Clinical Practice Recommendations for Primary Care Physicians and Healthcare Providers. Divisions of Nephrology & Hypertension and General Internal Medicine. 2011; 6: 2 -42. Available at: https: /www. asn-online. org/education/training/fellows/HFHS_CKD_V 6. pdf. 5. Bird L, Walker D. Pathophysiology of chronic kidney disease. Companion Animal. 2015; 20(1): 15 -19. doi: 10. 12968/coan. 2015. 20. 1. 15. 6. Ward F, Holian J, Murray P. Drug therapies to delay the progression of chronic kidney disease. Clinical Medicine. 2015; 15(6): 550 -557. doi: 10. 7861/clinmedicine. 15 -6 -550. 7. Guideline. gov. National Guideline Clearinghouse | Management of chronic kidney disease. 2016. Available at: http: //www. guideline. gov/content. aspx? id=47920&search=chronic+kidney+disease.
References Cont. 8. Nutritioncaremanual. org. Public Home Page - Nutrition Care Manual. 2015. Available at: https: //www. nutritioncaremanual. org/topic. cfm? ncm_category_id=1&ncm_toc_id=23081&ncm_heading=Nu trition%20 Care&ncm_content_id=78563#Anthropometric. Measurements. AD. 9. Fluid and dietary restriction's efficacy on chronic kidney disease patients in hemodialysis. Rev Bras Enferm. 2015; 68(6): 842 -50. 10. Dukkipati R, Noori N, Feroze U, Kopple J. Dietary Protein Intake in Patients with Advanced Chronic Kidney Disease and on Dialysis. Seminars in Dialysis. 2010; 23(4): 365 -372. doi: 10. 1111/j. 1525 -139 x. 2010. 00753. x. 11. The National Kidney Foundation. Understanding Your Lab Values. 2014. Available at: https: //www. kidney. org/kidneydisease/understandinglabvalues. 12. Merck Manuals Professional Edition. Chronic Kidney Disease - Genitourinary Disorders. 2016. Available at: http: //www. merckmanuals. com/professional/genitourinary-disorders/chronic-kidneydisease/chronic-kidney-disease. 13. Web. MD. Chronic Kidney Disease-Medications. 2016. Available at: http: //www. webmd. com/a-to-z- guides/chronic-kidney-disease-medications. 14. Der G. An overview of proton pump inhibitors. Gastroenterology Nursing: The Official Journal of the Society of Gastroenterology Nurses and Associates. September 2003; 26(5): 182 -190.