Anatomy Physiology Unit 7 The Urinary System Function








- Slides: 29
Anatomy & Physiology Unit 7: The Urinary System
Function of the Urinary System n n Dispose of excess wastes and ions Regulate blood volume Balance water and electrolytes Regulates acid-base balance
Urinary System n Organs: n Kidneys: n n n 2 - each lie against dorsal wall, retroperitoneally Size of a bar of soap Extend from T 12 to L 3, right lower than left Ureters (2): tubes running from kidneys to bladder Bladder: located in pelvis—retroperitoneally Urethra: tube running from bladder to outside

Kidney Anatomy n n Each kidney is enclosed in a renal capsule and fatty capsule Inside divided into 3 regions: Renal cortex: outer region n Renal medulla: dark-red inside layer n Medullary pyramids: triangular regions— apex of each point toward hilus n n Separated by renal columns
Kidney Anatomy n Renal pelvis: flat, basin-like cavity n n Continuous with ureters leaving hilus Calyces: cup-shaped areas that enclose apex of pyramids n Act to collect urine from pyramids and pass onto the pelvis to be sent out ureters to bladder

Kidney Anatomy n n Blood Supply: ~ ¼ of total blood supply passes through kidneys each minute All vessels exit and enter kidney within the hilus n Renal artery: feeds blood into kidneys n n Branch into arterioles & capillaries inside kidney Renal vein: filtered blood draining from kidneys
Kidney Anatomy n n n Blood Flow Through Nephron Enters afferent arteriole---units with glomerulus —exits efferent arteriole Efferent arteriole smaller in diameter than afferent—so blood “backs up” n n Blood flow slows down—raises blood pressure Moves onto peritubular capillaries n Porous, low blood prssure, permits lots of movement across walls
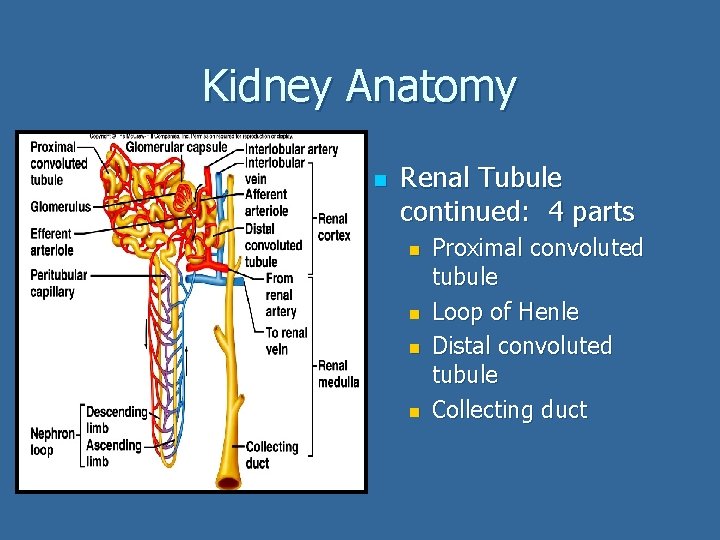
Kidney Anatomy n Nephrons: structural and functional units of kidney ~1 million per kidney n Actually form urine n 2 main structures: n Glomerulus (Bowman’s Capsule): knot of capillaries n Renal tubule: starts at glomerulus then continues as a 3 cm. tubule n
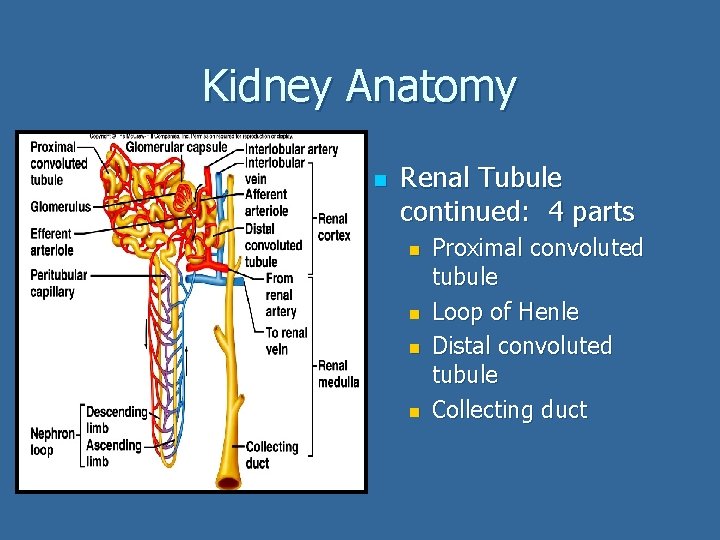
Kidney Anatomy n Renal Tubule continued: 4 parts n n Proximal convoluted tubule Loop of Henle Distal convoluted tubule Collecting duct
Students-Teaching-Students Urine Production Urine is produced within the nephrons of the kidneys in 3 main steps With your table buddy read pages 486 -487 in your text and take notes on urine production. (15 minutes) n List the 3 steps of urine formation. n n Explain what is moving out and in and where in the nephron does this taking place Where does urine go (the pathway) once it’s produced? Write this down in your notebook. (5 minutes)
Kidney Physiology: Urine Formation Occurs in 3 steps: filtration, reabsorption and secretion 1. Filtration: nonselective, passive process n n n Filtrate = blood plasma without proteins & blood cells (too big) Occurs within glomerulus Blood filtered from afferent arterioles due to high blood pressure within tubule Blood from glomerulus drained into efferent arterioles which feed the peritubular capillaries— low in blood pressure—great for absorption

Kidney Physiology: Urine Formation 2. Re-absorption: begins as filtrate enters proximal convoluted tubule—into peritubular capillaries n n Too many “good” things filtered out of blood and need to return—glucose, amino acids, water Water filtered passively (osmosis) Solid particles transported actively via carriers Nitrogenous wastes poorly reabsorbed (no carriers)

Kidney Physiology: Urine Formation 3. Secretion: re-absorption in reverse n n n Last chance to dump out drugs, hydrogen & potassium ions & creatinine Occurs in proximal & distal convoluted tubule Anything entering collecting duct from distal convoluted tubule sent through pyramids to calyces and renal pelvis—out to ureters—this is urine
Urine n Clear to pale to deep yellow n n Urochrome: pigment made from destroyed hemoglobin Sterile, slightly aromatic, slightly acidic Composed of: sodium & potassium ions, urea, uric acid, creatinine, ammonia, bicarbonate ions Should not have: glucose, proteins, RBC’s, hemoglobin, WBC’s and bile n Composition can change based on metabolism and disease
Urinalysis Assignment n n There are several substances that should not be found in urine-so medical professionals use urinalysis as a tool to diagnose injury and illness Using your book, look up the name of the condition and its potential causes if the following are found in urine: a. Glucose b. Proteins c. Pus (WBCs & bacteria) d. Bile pigment e. Hemoglobin f. RBCs
Urinalysis n Glucose---glycosuria n n Proteins: proteinuria n n Bleeding in urinary tract (trauma, stones, infection) Hemoglobin: hemoglobinuria n n Urinary tract infection (UTI) RBCs: hematuria n n Physical exertion, pregnancy, hypertension Pus: pyuria n n Too much sugar or diabetes mellitus Transfusion reaction, hemolytic anemia Bile: bilirubinuria n Hepatitis
Ureters n n Slender tubes, 25 -30 cm long Passageways to carry urine from kidneys to bladder Lined with smooth muscle---peristalsis propels urine Bladder mucosa blocks urine from backflowing out of bladder into ureters
Bladder n n n Smooth, collapsable, muscular sac Temporarily stores urine 3 openings: 2 for ureters, 1 for urethra Can hold 1 pint and up to 2 pints Lined by transitional epithelium—allows bladder to stretch n Not like the stomach, more like a balloon
Urethra n n Thin-walled tube with smooth muscles— for peristalsis 2 sphincters Internal: involuntary n External: voluntary n
Micturition n n aka voiding: the emptying of the bladder Controlled by the sphincters Once 200 ml collects in bladder, stretch receptors are activated—stimulates muscular walls to contract—forces urine passed internal sphincter—FEELS LIKE YOU HAVE TO VOID External sphincter can hold urine if needed The feeling of needing to go will pass until about 300 ml collects—reflex starts again
Fluid, Electrolyte & Acid-Base Balance n Water & Electrolyte Balance Water accounts for 50% of body weight in females/60% in males n Fluid Compartments n Intracellular Fluid (ICF): 2/3 of total body fluid —contained within living cells n Extracellular Fluid (ECF): 1/3 of total body fluid —located outside cells n n Examples: blood plasma, interstitial fluid, CSF

Fluid, Electrolyte & Acid-Base Balance n n n Water & Electrolyte Balance Remember this: WATER FOLLOWS SALT! Small changes in electrolyte balance forces water to move b/n compartments n Alters blood volume and pressure and impairs nerve and muscle cells

Fluid, Electrolyte & Acid-Base Balance n n n Water & Electrolyte Balance Water is gained through food and drink Water is lost through sweat, breathing and predominately urine Electrolytes enter through food and “hard” water Electrolytes leave through sweat, feces and predominately urine
Fluid, Electrolyte & Acid-Base Balance n n Hormonal Control Antidiuretic hormone (ADH) Osmoreceptors in hypothalamus signal release of ADH n This prevents urine loss n n Aldosterone If blood too dilute, water leaves blood stream n Kidneys retain sodium, rids potassium n

Fluid, Electrolyte & Acid-Base Balance n n 1. Maintaining Acid-Base Balance 3 methods: Buffers: a chemical that resists changes in p. H Weak Acids: release H+ in presence of strong base Weak Bases: combine with excess H+ in presence of strong acid

Fluid, Electrolyte & Acid-Base Balance n n 2. Maintaining Acid-Base Balance 3 methods: Respiratory System CO 2 high—too acidic: increase in rate & depth of breathing CO 2 low—too basic: decrease in rate & depth of breathing
Fluid, Electrolyte & Acid-Base Balance n n 3. Maintaining Acid-Base Balance 3 methods: Kidneys If blood is acidic: H+ are secreted & bicarbonate ions reabsorbed If blood too basic: rate of H+ secretion decreases, bicarbonate ions secreted
Urinary Mishaps n n Incontinence: unable to voluntarily control external sphincter Renal Caliculi: kidney stones n n Urine too concentrated—uric acid salts Urinary Tract Infection: bacterial infection of urethra—can lead to kidney infection n More common in women