Chronic Kidney Disease in Kidney Cancer Patients Anthony







- Slides: 52
Chronic Kidney Disease in Kidney Cancer Patients Anthony Chang, MD University of Chicago Medical Center
Outline • Non-Neoplastic Kidney Diseases in Kidney Cancer – – – • Harmful Common Underappreciated Review common medical renal diseases associated with renal cancer
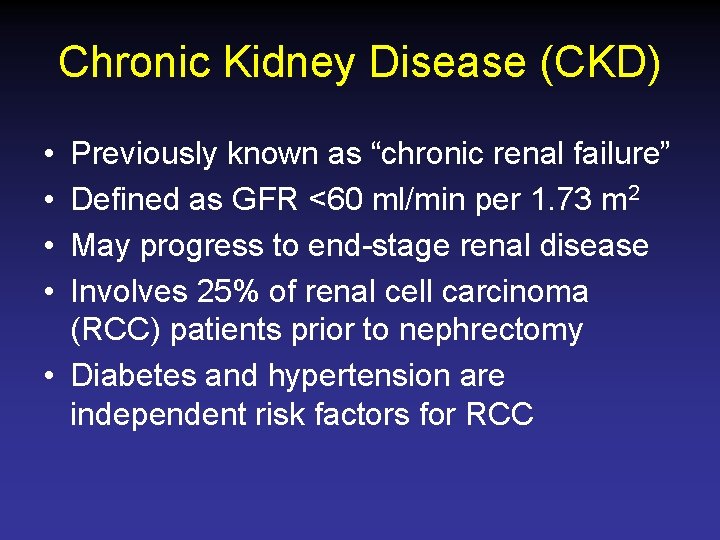
Chronic Kidney Disease (CKD) • • Previously known as “chronic renal failure” Defined as GFR <60 ml/min per 1. 73 m 2 May progress to end-stage renal disease Involves 25% of renal cell carcinoma (RCC) patients prior to nephrectomy • Diabetes and hypertension are independent risk factors for RCC
Chronic Kidney Disease (CKD) • ↑ risk of CKD after radical compared with partial nephrectomy • ↑ risk of cardiovascular and noncardiovascular death
American Urological Association • 2009 - T 1 tumors (<7 cm) should be treated with partial nephrectomy • Emerging data that T 2 tumors should also be treated with nephron sparing surgery
“Despite mounting evidence that PN is an effective and preferable approach to the T 1 renal mass, it remains markedly underutilized in the USA and abroad. The overzealous use of radical nephrectomy for T 1 tumors must now be considered detrimental to the long term health of the kidney tumor patient. ”
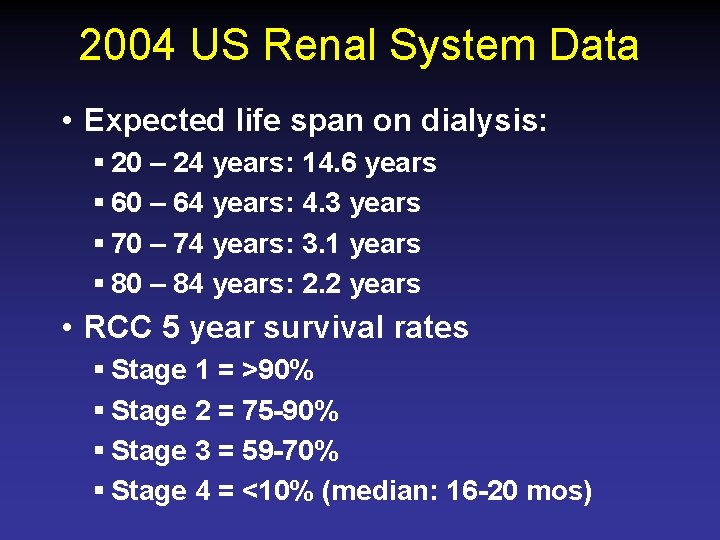
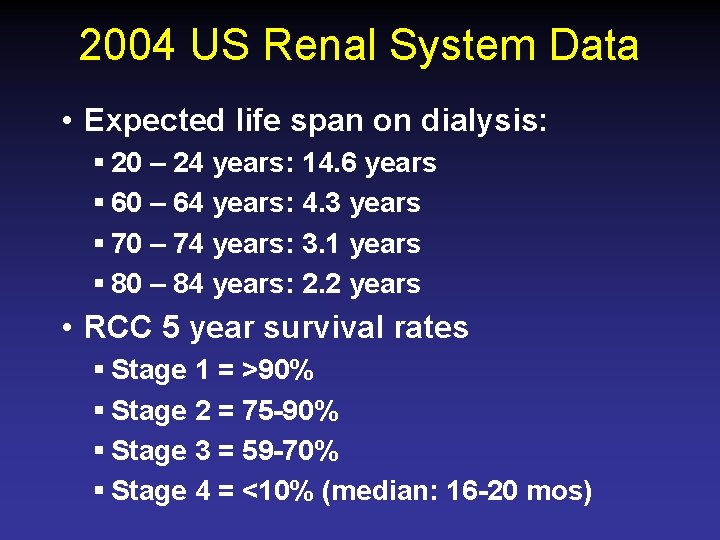
2004 US Renal System Data • Expected life span on dialysis: § 20 – 24 years: 14. 6 years § 60 – 64 years: 4. 3 years § 70 – 74 years: 3. 1 years § 80 – 84 years: 2. 2 years • RCC 5 year survival rates § Stage 1 = >90% § Stage 2 = 75 -90% § Stage 3 = 59 -70% § Stage 4 = <10% (median: 16 -20 mos)
“As I spoke, the family seemed to relax visibly, and began to break into smiles. “Oh, that’s wonderful news, wonderful news!” I smiled too, automatically, although I did not think my news—a biopsy finding of advanced glomerulosclerosis, irreversible kidney failure— had been so wonderful. It was true that this particular kidney biopsy had been done because of heavy proteinuria and newly diagnosed kidney failure in a man with a lung nodule; the working diagnosis had been a paraneoplastic membranous nephropathy, and the specter of lung cancer had been hanging over the scene for the last few days. My news made the possibility of cancer recede. The nodule eventually was found to be benign, and we were left to deal with the aftermath of the not-cancer diagnosis, the good news that wasn’t. If the one-year mortality for new end-stage kidney failure exceeds that for most new cancer diagnoses, why is it that this family, like many others, dreaded the latter more than the former? ”

“I became very close with the patient who reacted with such relief to the diagnosis of advanced kidney disease rather than cancer. I saw him progress, quickly and inexorably, to dialysis-requiring kidney failure. I watched him suffer with infections, fatigue, confusion, and cramps. He lost his appetite, and became weak and bedbound. He died less than a year after I met him. To the end, I don’t think that he or his family ever understood that the news I had brought was bad, or that kidney failure itself had been the final blow to his fragile health. Perhaps it was for the best that they did not really understand. Then again, that’s what oncologists used to say, in whispers, outside the rooms of patients who were pretending not to listen. ” Dena E. Rifkin, MD, MS La Jolla, California
Non-Neoplastic Renal Diseases & Kidney Cancer
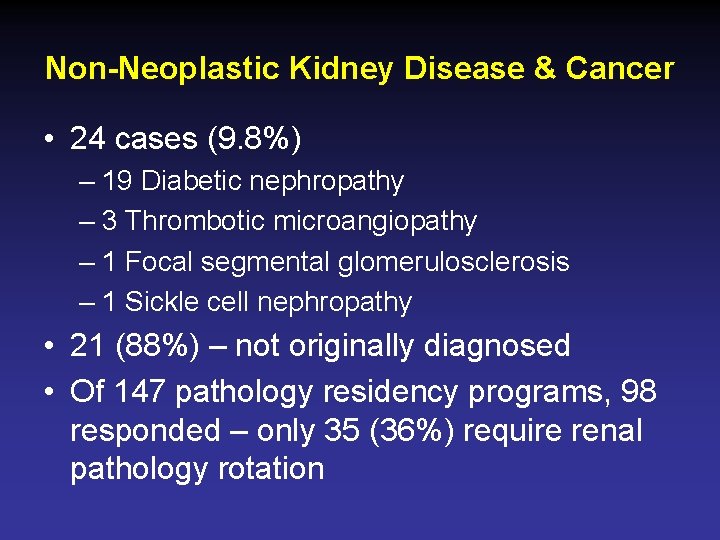
Non-Neoplastic Kidney Disease & Cancer • 24 cases (9. 8%) – 19 Diabetic nephropathy – 3 Thrombotic microangiopathy – 1 Focal segmental glomerulosclerosis – 1 Sickle cell nephropathy • 21 (88%) – not originally diagnosed • Of 147 pathology residency programs, 98 responded – only 35 (36%) require renal pathology rotation
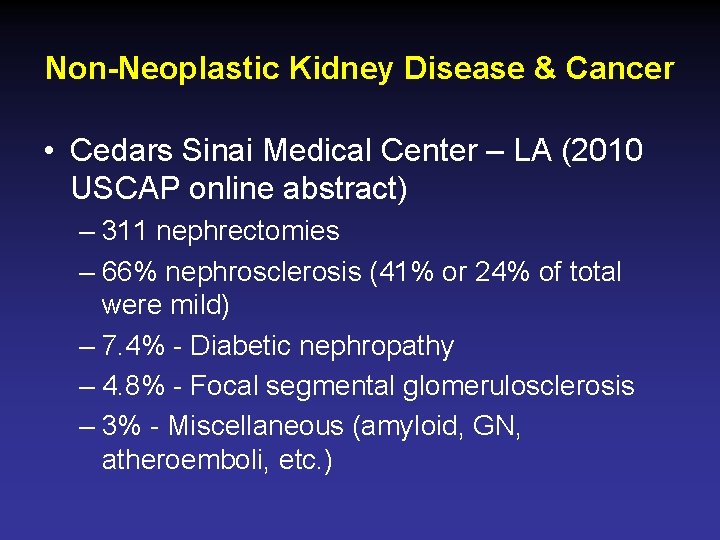
Non-Neoplastic Kidney Disease & Cancer • Cedars Sinai Medical Center – LA (2010 USCAP online abstract) – 311 nephrectomies – 66% nephrosclerosis (41% or 24% of total were mild) – 7. 4% - Diabetic nephropathy – 4. 8% - Focal segmental glomerulosclerosis – 3% - Miscellaneous (amyloid, GN, atheroemboli, etc. )

Non-Neoplastic Kidney Disease & Cancer • Weill Cornell Medical College (2011 USCAP abstract) – 216 nephrectomy cases – 47 (21. 7%) new pathologic diagnoses • • • 21 – diabetic nephropathy 11 – hypertensive nephropathy 6 – focal segmental glomerulosclerosis 2 – collapsing glomerulopathy Arteriolar sclerosis predictive of renal function decline
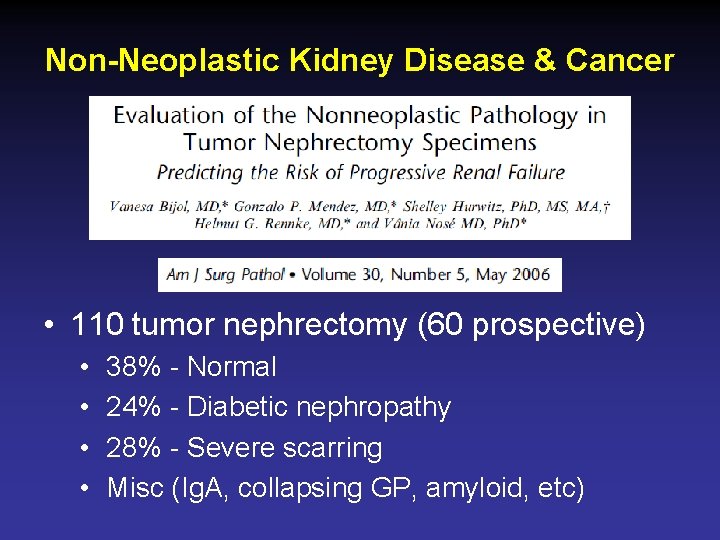
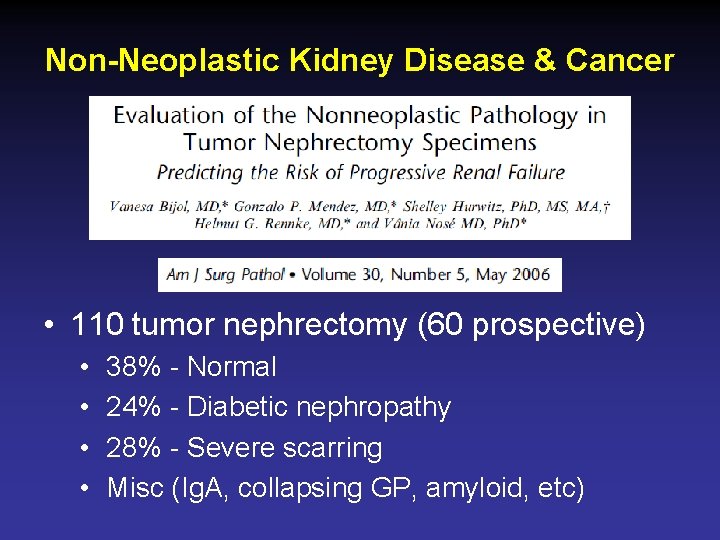
Non-Neoplastic Kidney Disease & Cancer • 110 tumor nephrectomy (60 prospective) • • 38% - Normal 24% - Diabetic nephropathy 28% - Severe scarring Misc (Ig. A, collapsing GP, amyloid, etc)
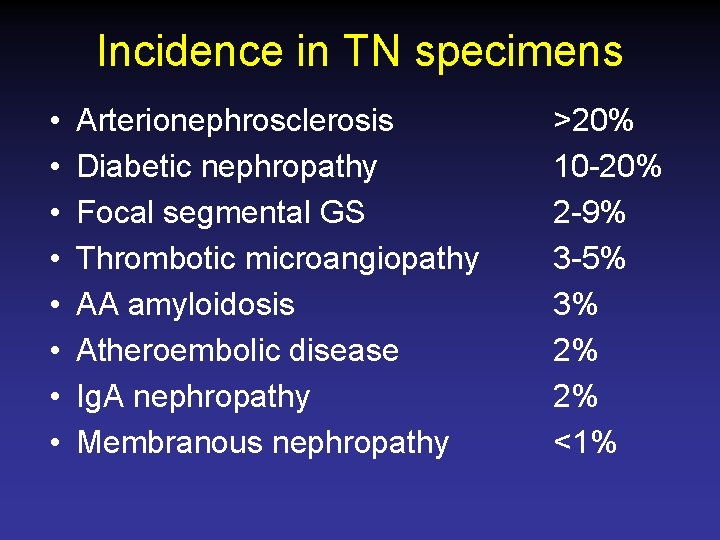
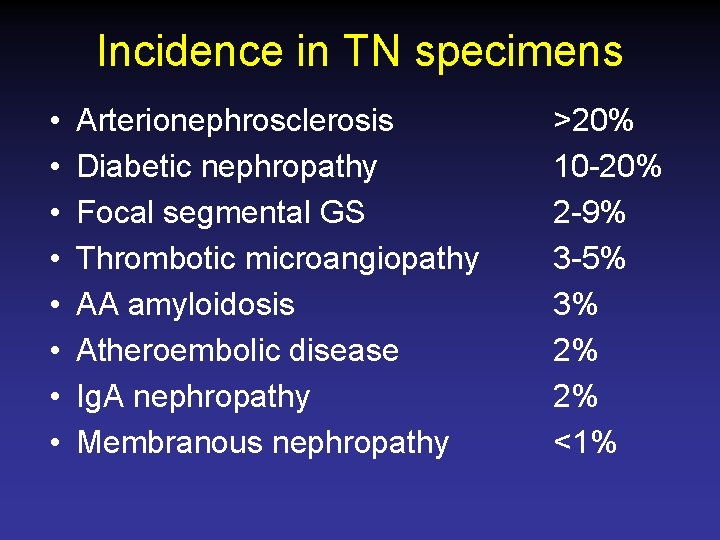
Incidence in TN specimens • • Arterionephrosclerosis Diabetic nephropathy Focal segmental GS Thrombotic microangiopathy AA amyloidosis Atheroembolic disease Ig. A nephropathy Membranous nephropathy >20% 10 -20% 2 -9% 3 -5% 3% 2% 2% <1%
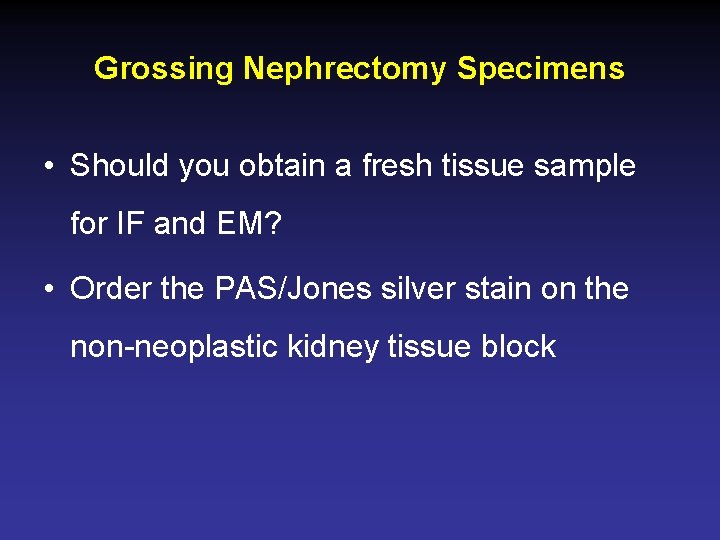
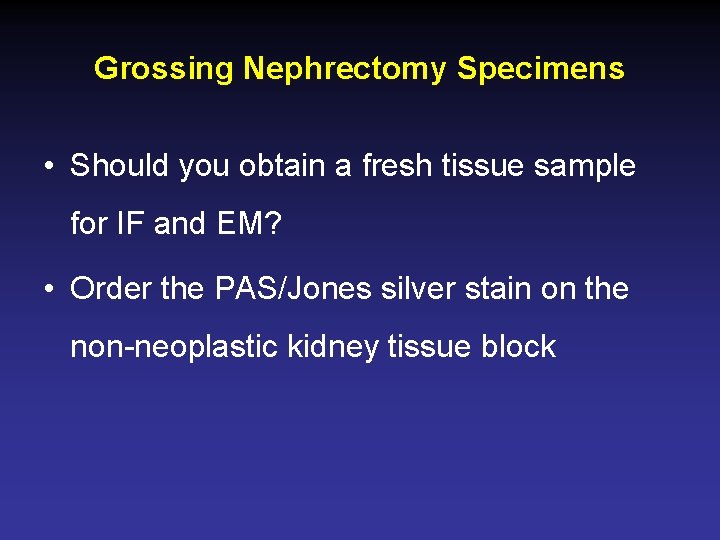
Grossing Nephrectomy Specimens • Should you obtain a fresh tissue sample for IF and EM? • Order the PAS/Jones silver stain on the non-neoplastic kidney tissue block
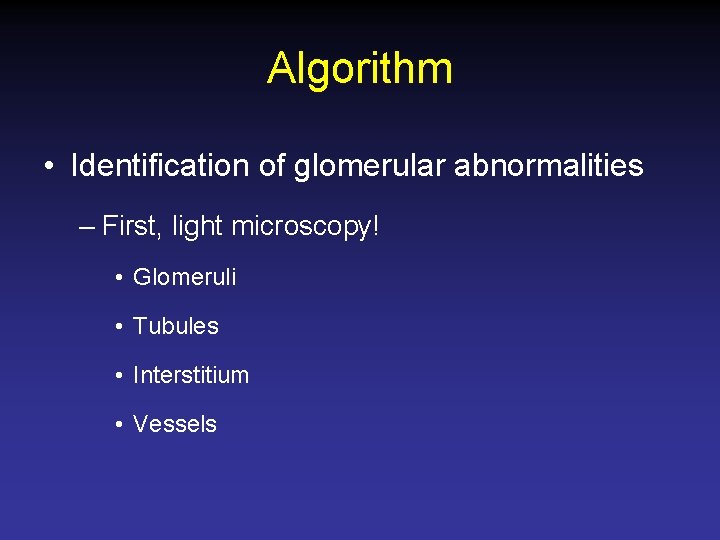
Algorithm • Identification of glomerular abnormalities – First, light microscopy! • Glomeruli • Tubules • Interstitium • Vessels
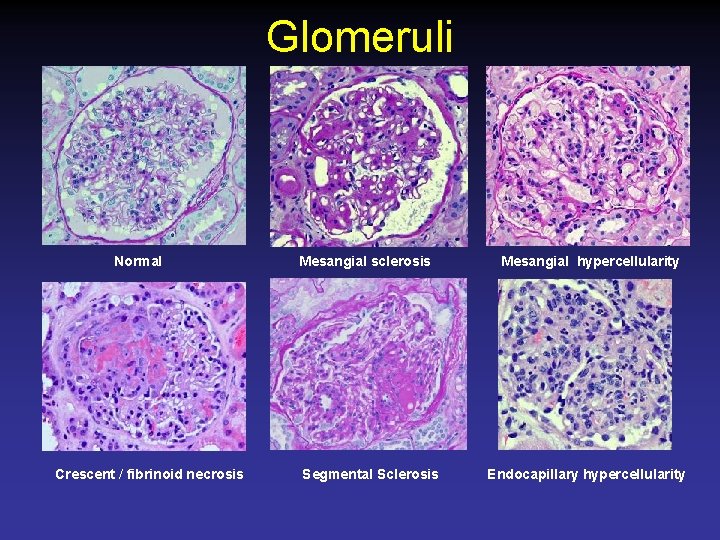
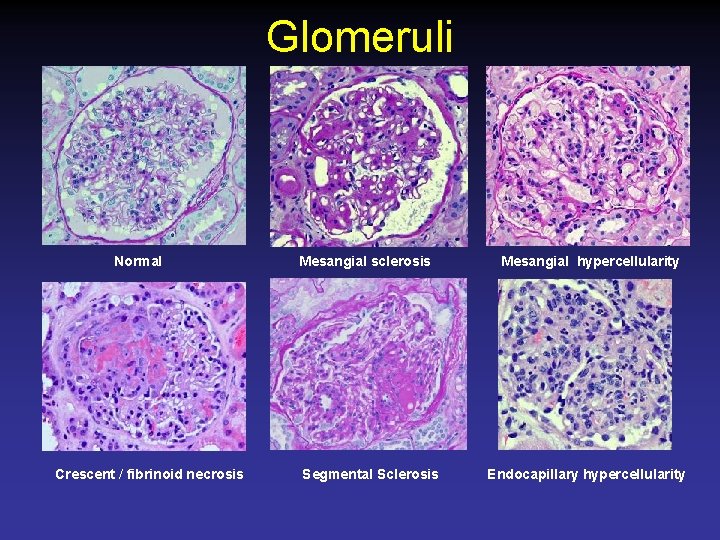
Glomeruli Normal Crescent / fibrinoid necrosis Mesangial sclerosis Segmental Sclerosis Mesangial hypercellularity Endocapillary hypercellularity

Algorithm • If glomerular abnormalities present, – Consider Congo red – Immunofluorescence microscopy (Ig. G, Ig. A, Ig. M, kappa/lambda light chains, albumin) on paraffin tissue sections • Decreased sensitivity compared with frozen tissue – Immunohistochemistry – Electron microscopy from paraffin block • Preservation/processing artifact

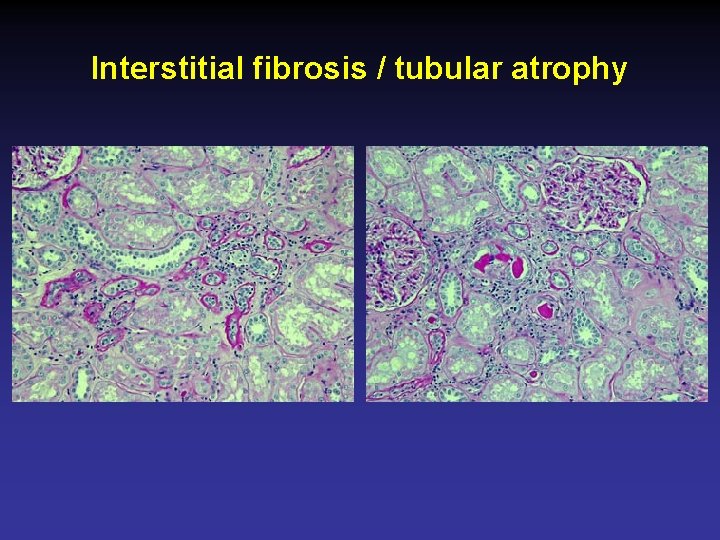
Tubules / Interstitium Normal Interstitial inflammation Interstitial fibrosis / tubular atrophy Acute tubular injury
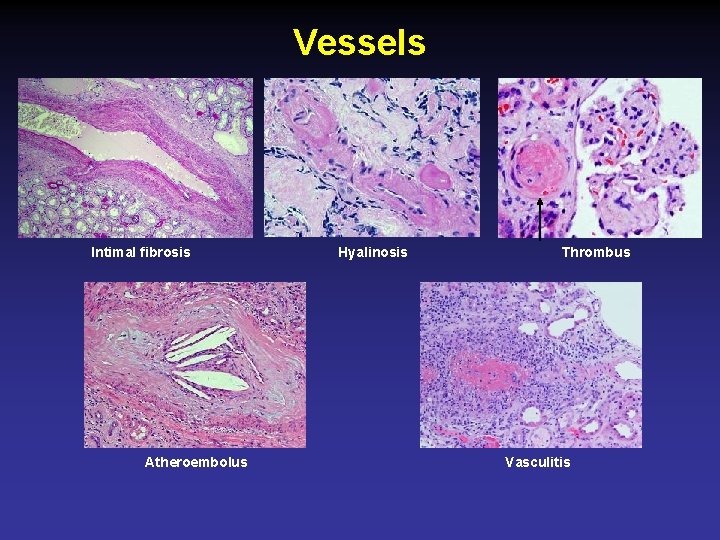
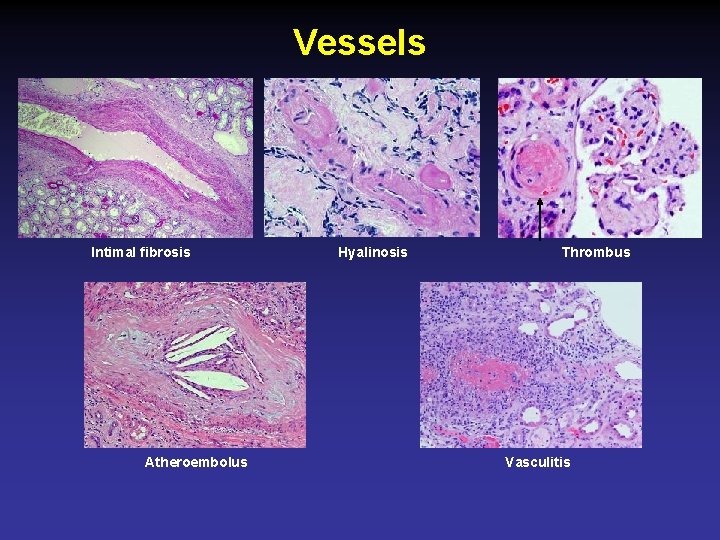
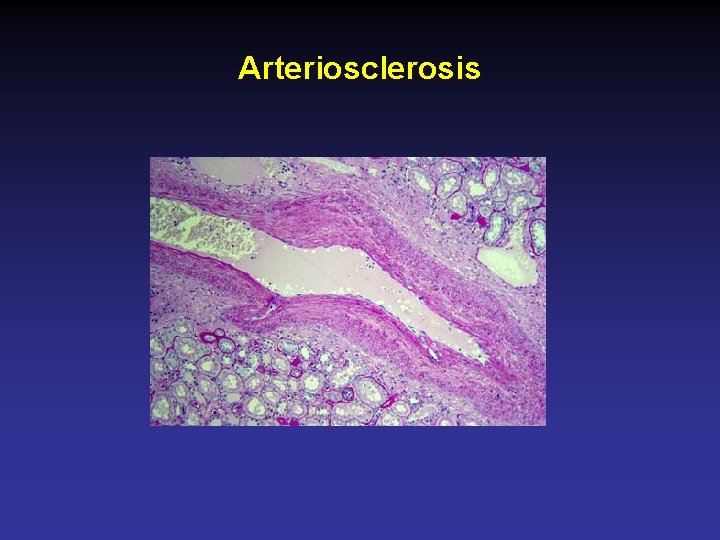
Vessels Intimal fibrosis Atheroembolus Hyalinosis Thrombus Vasculitis

Diabetic Nephropathy • • • Diabetes is a risk factor for RCC 8% of American adults c diabetes 10 -20% of RCC patients have diabetes DN in up to 8 -20% of TN specimens Diabetic nodular glomerulosclerosis predicts progression of CKD • Treatment: Strict blood glucose control
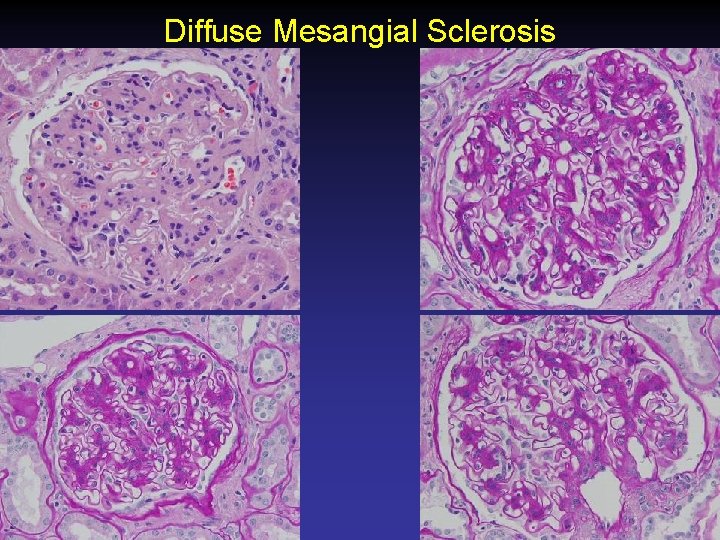
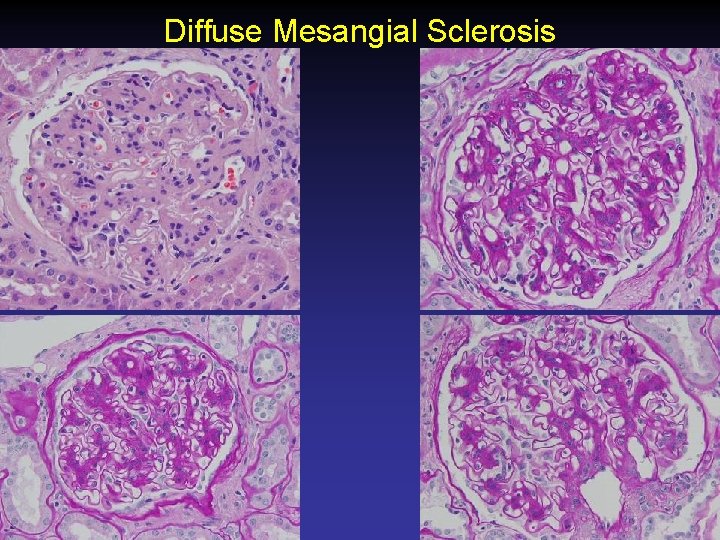
Diffuse Mesangial Sclerosis
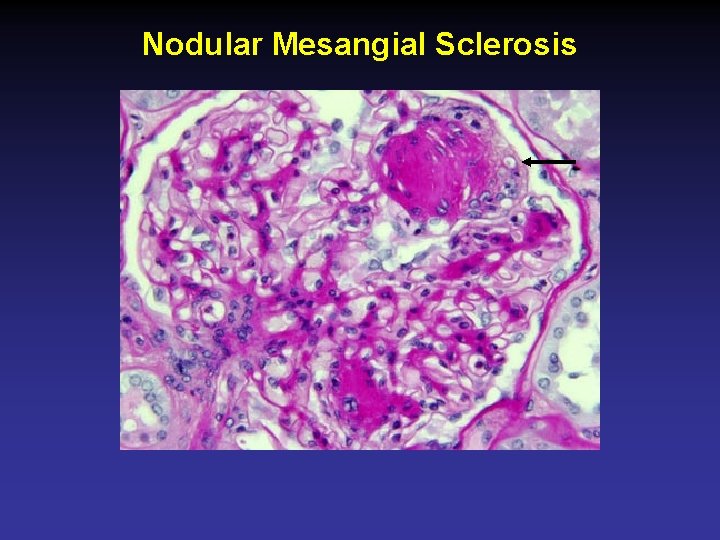
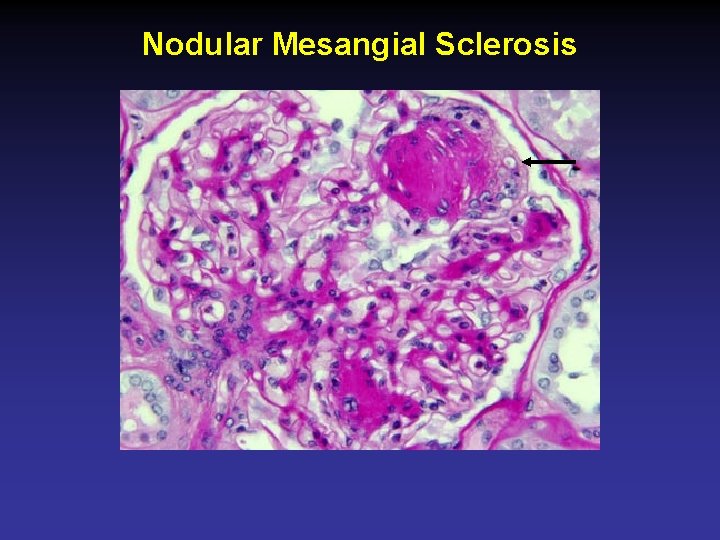
Nodular Mesangial Sclerosis
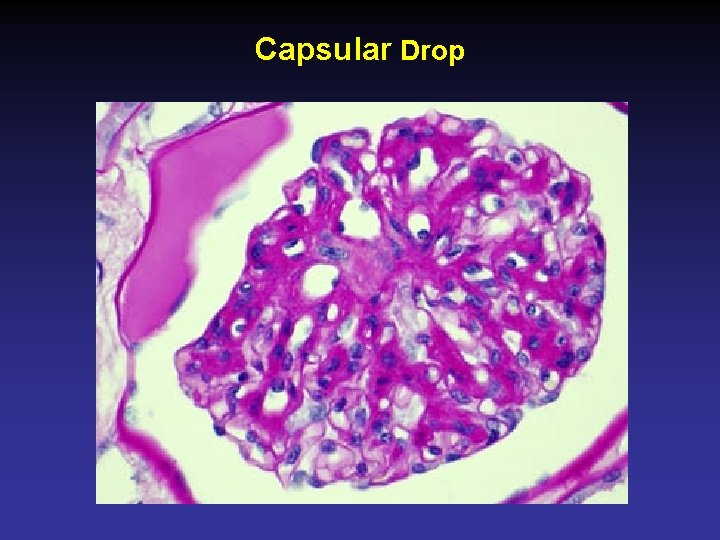
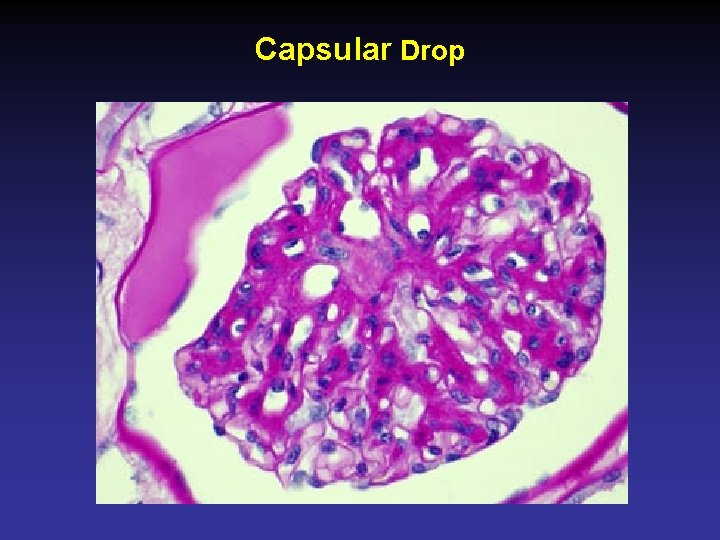
Capsular Drop
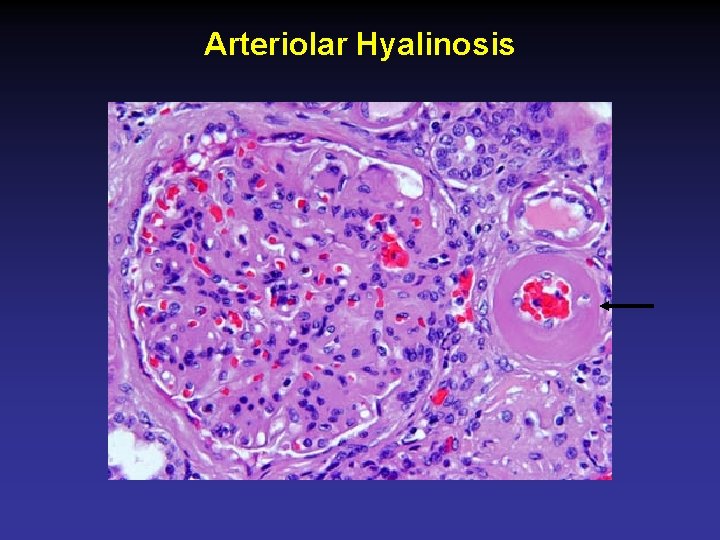
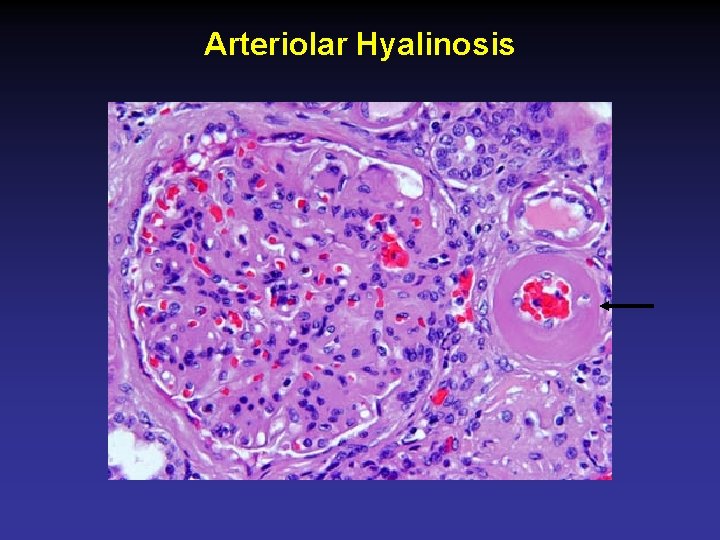
Arteriolar Hyalinosis
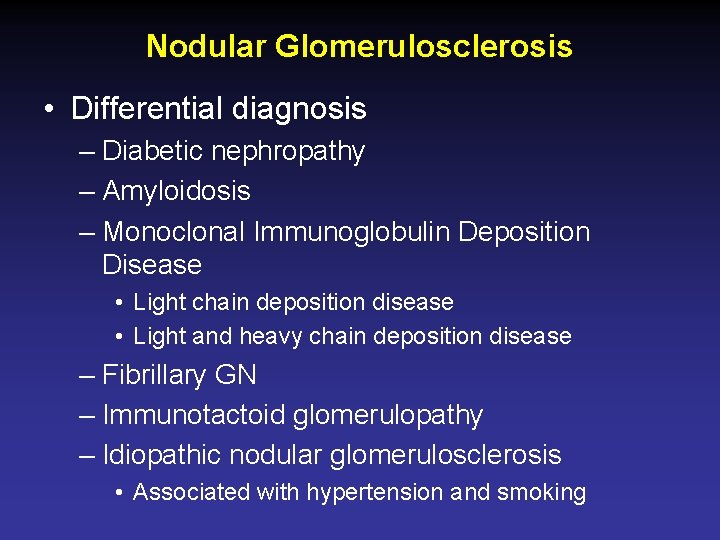
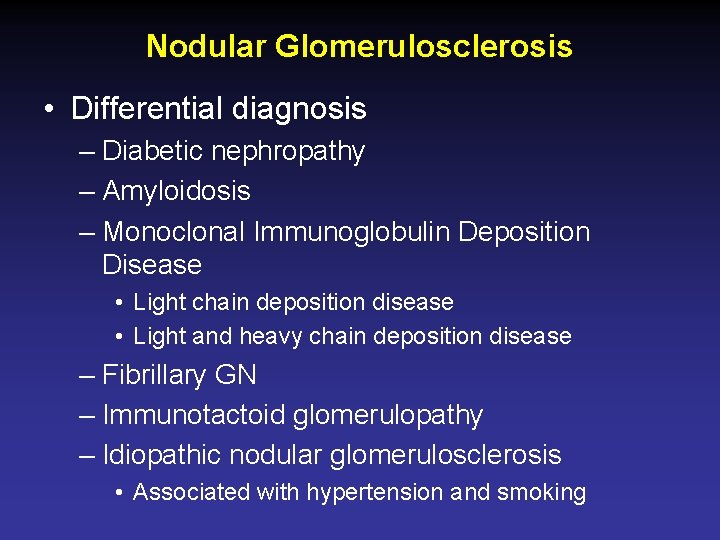
Nodular Glomerulosclerosis • Differential diagnosis – Diabetic nephropathy – Amyloidosis – Monoclonal Immunoglobulin Deposition Disease • Light chain deposition disease • Light and heavy chain deposition disease – Fibrillary GN – Immunotactoid glomerulopathy – Idiopathic nodular glomerulosclerosis • Associated with hypertension and smoking
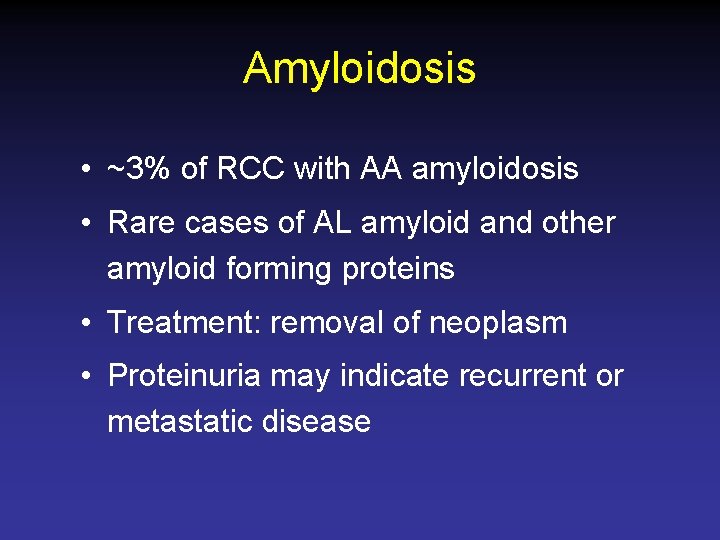
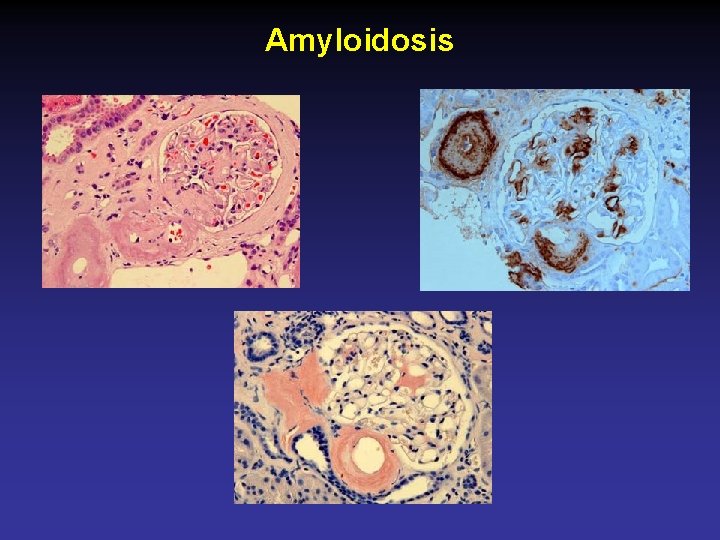
Amyloidosis • ~3% of RCC with AA amyloidosis • Rare cases of AL amyloid and other amyloid forming proteins • Treatment: removal of neoplasm • Proteinuria may indicate recurrent or metastatic disease
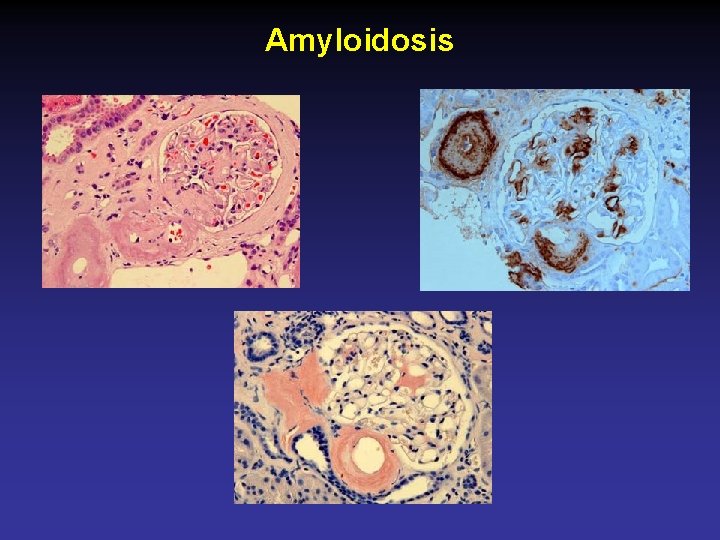
Amyloidosis

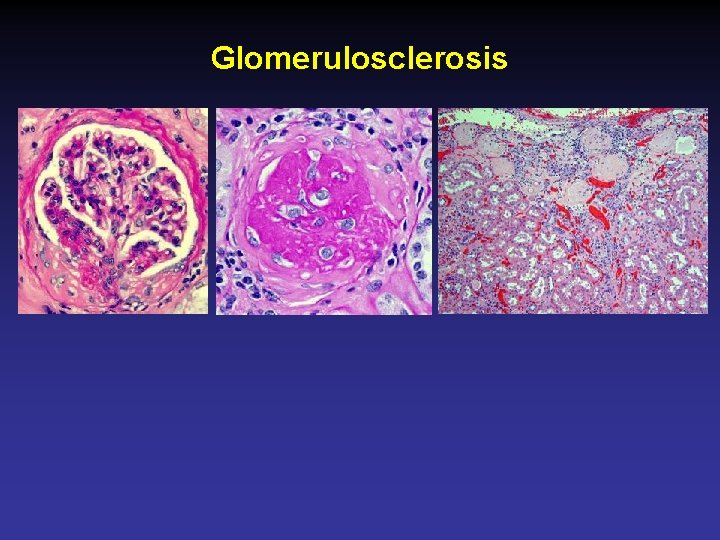
Arterionephrosclerosis • AKA Hypertensive nephropathy / nephrosclerosis • Hypertension in 25 -60% of RCC pts • Tumor nephrectomy (TN) specimens – 40% with arteriosclerosis and no TI scarring – 20% with arteriosclerosis and TI scarring • >20% global glomerulosclerosis predicts progression of CKD
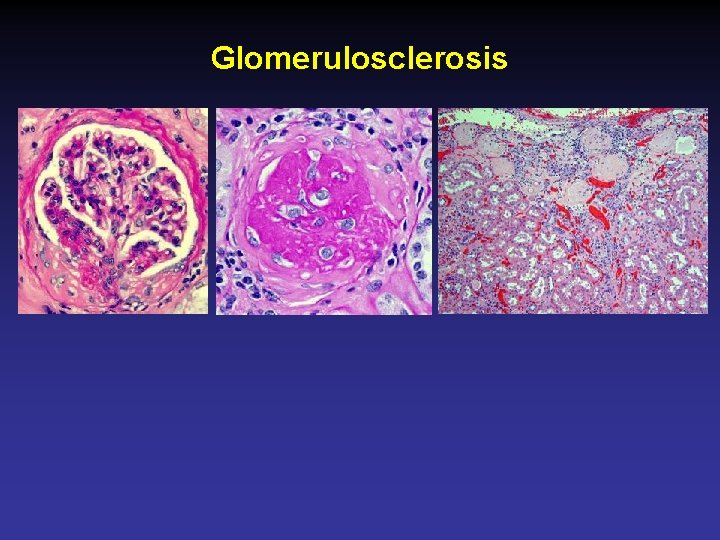
Glomerulosclerosis
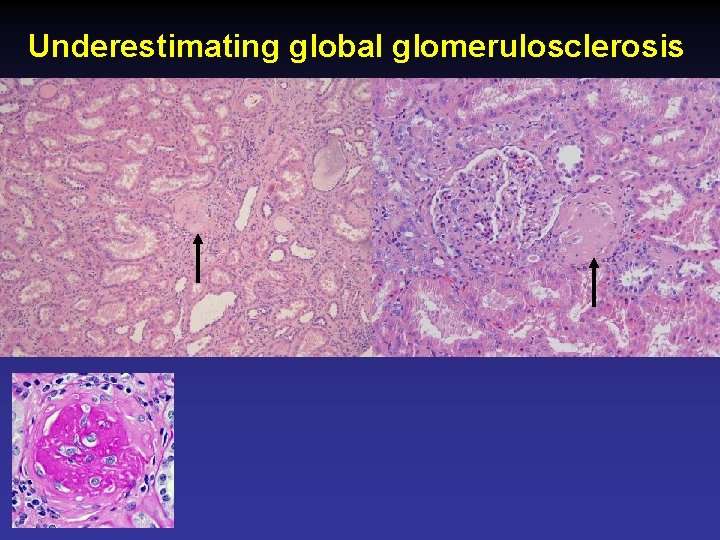
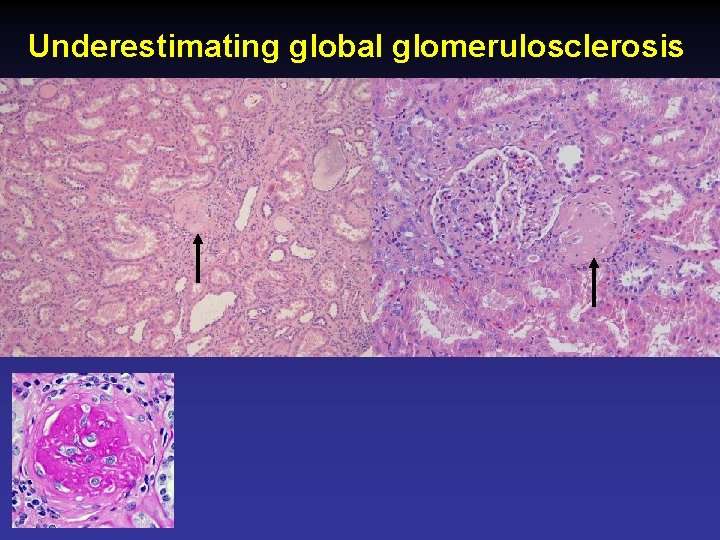
Underestimating global glomerulosclerosis
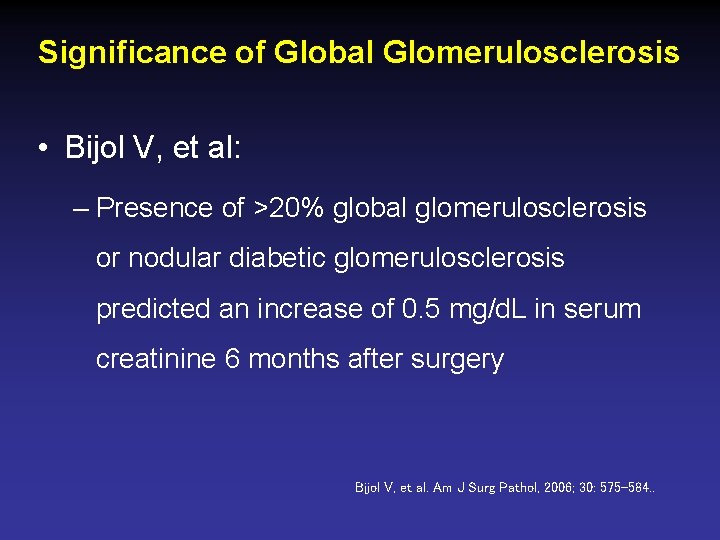
Significance of Global Glomerulosclerosis • Bijol V, et al: – Presence of >20% global glomerulosclerosis or nodular diabetic glomerulosclerosis predicted an increase of 0. 5 mg/d. L in serum creatinine 6 months after surgery Bijol V, et al. Am J Surg Pathol, 2006; 30: 575 -584. .
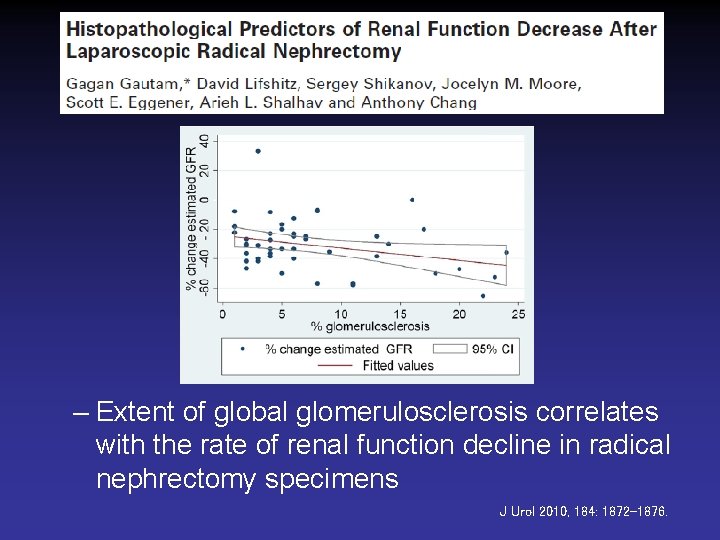
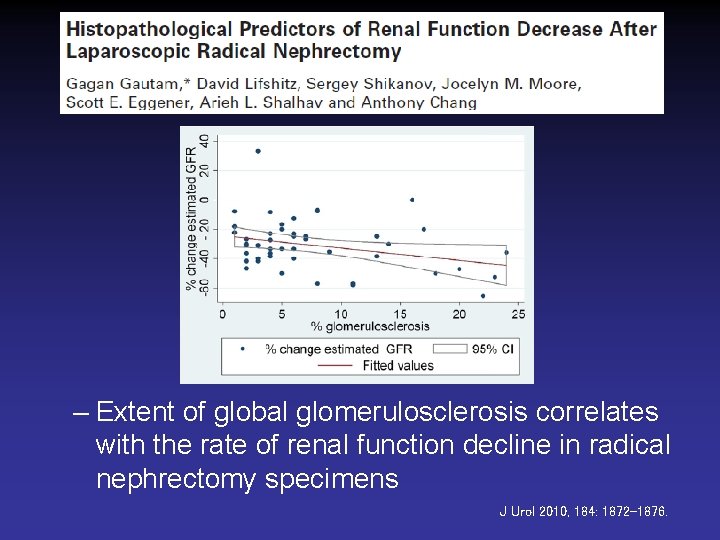
– Extent of global glomerulosclerosis correlates with the rate of renal function decline in radical nephrectomy specimens J Urol 2010, 184: 1872 -1876.
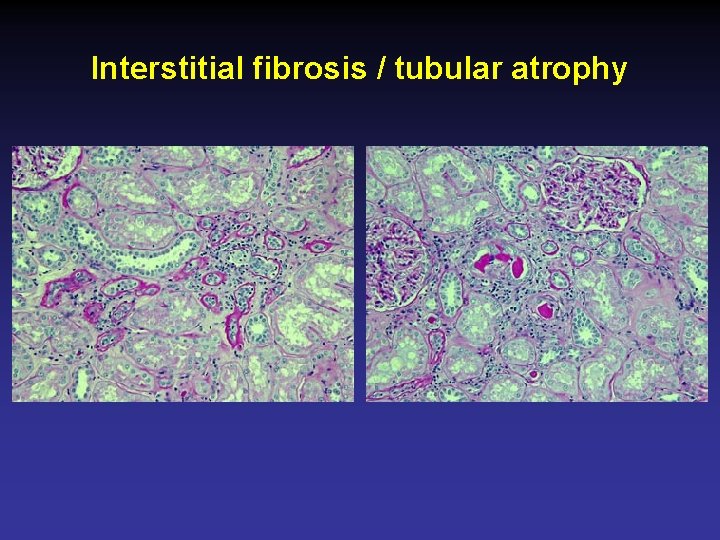
Interstitial fibrosis / tubular atrophy
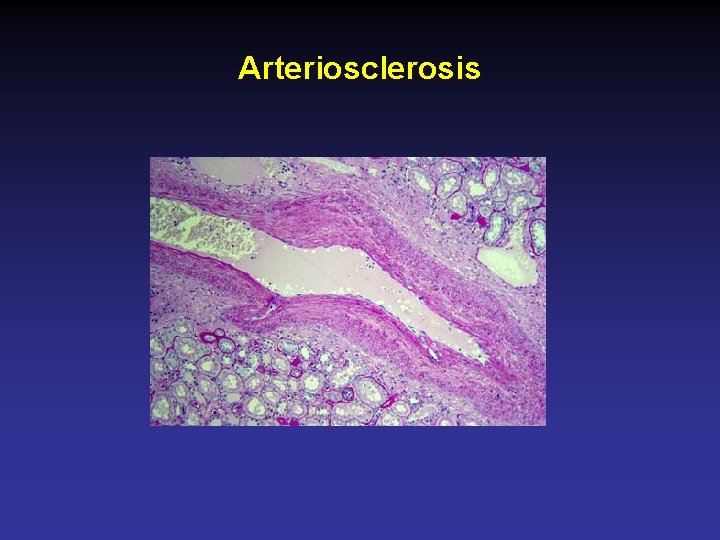
Arteriosclerosis
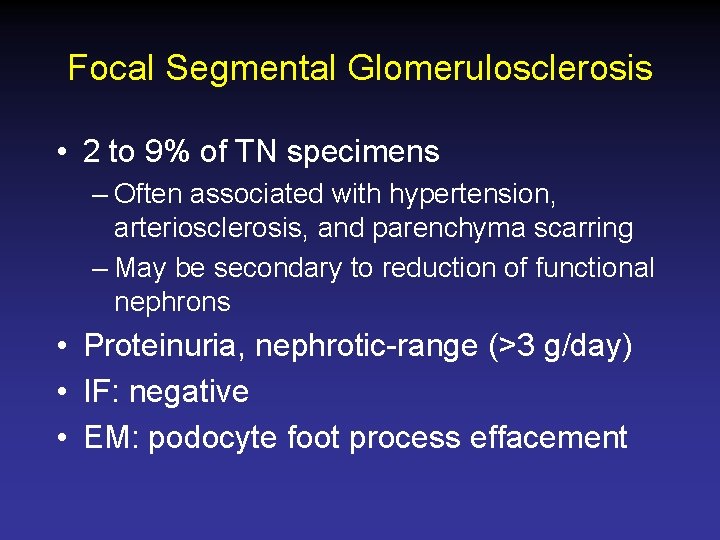
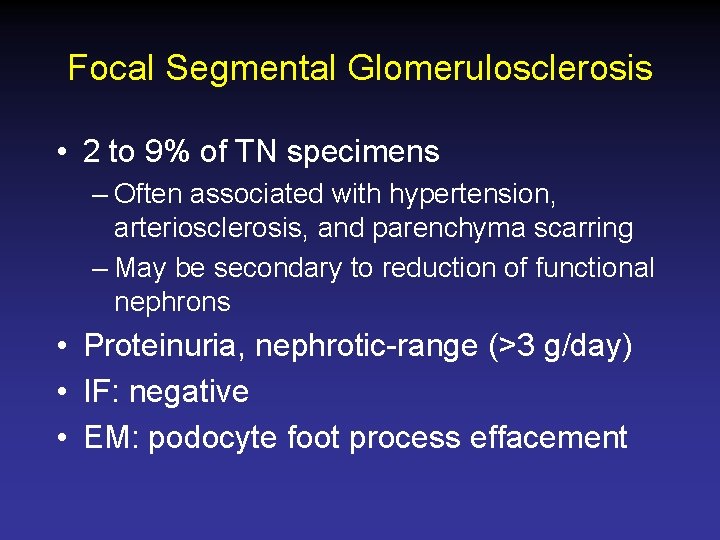
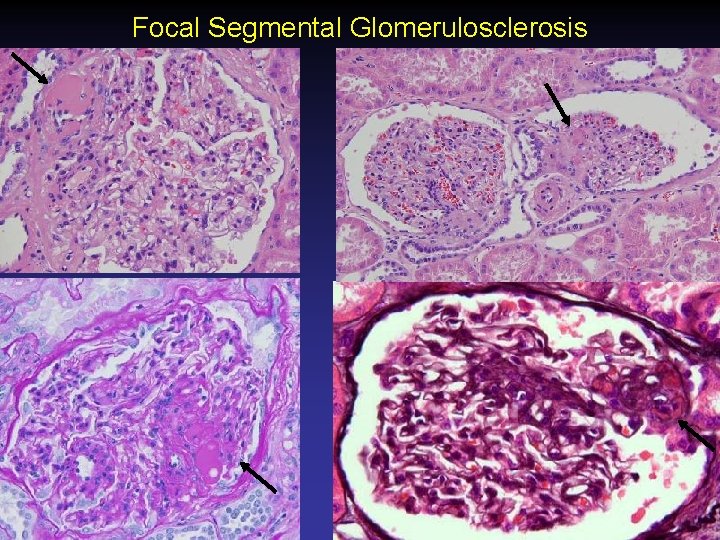
Focal Segmental Glomerulosclerosis • 2 to 9% of TN specimens – Often associated with hypertension, arteriosclerosis, and parenchyma scarring – May be secondary to reduction of functional nephrons • Proteinuria, nephrotic-range (>3 g/day) • IF: negative • EM: podocyte foot process effacement
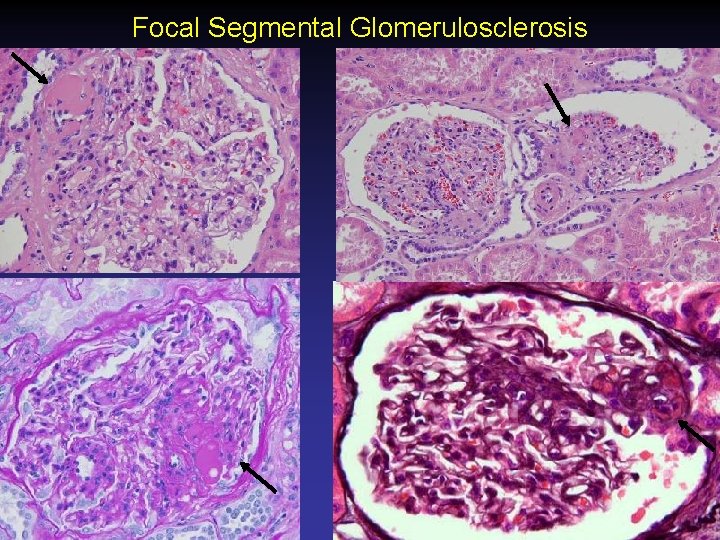
Focal Segmental Glomerulosclerosis
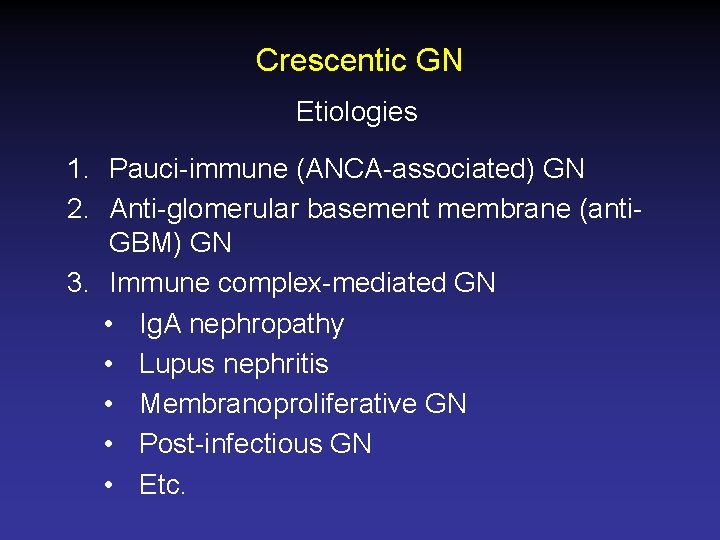
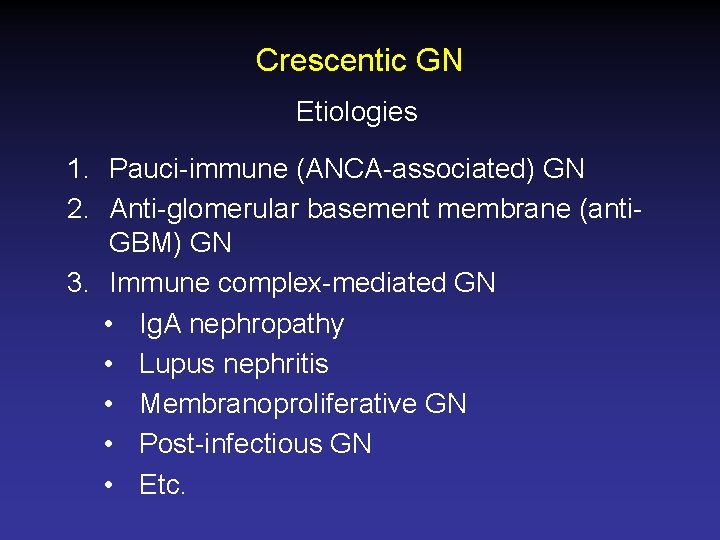
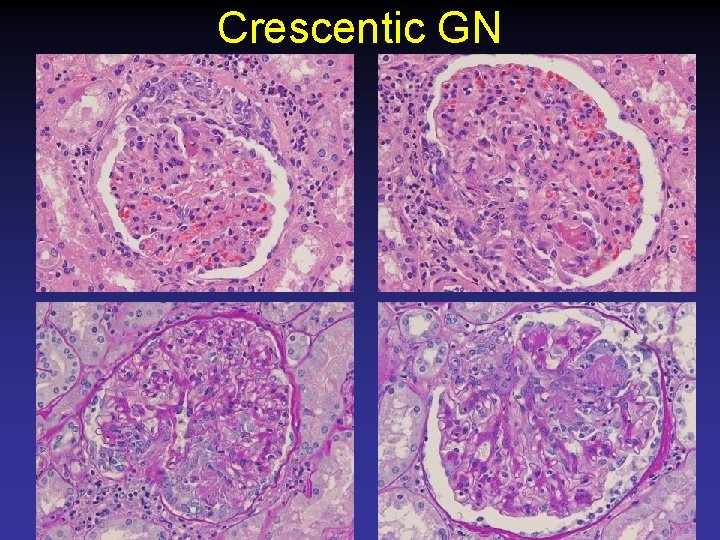
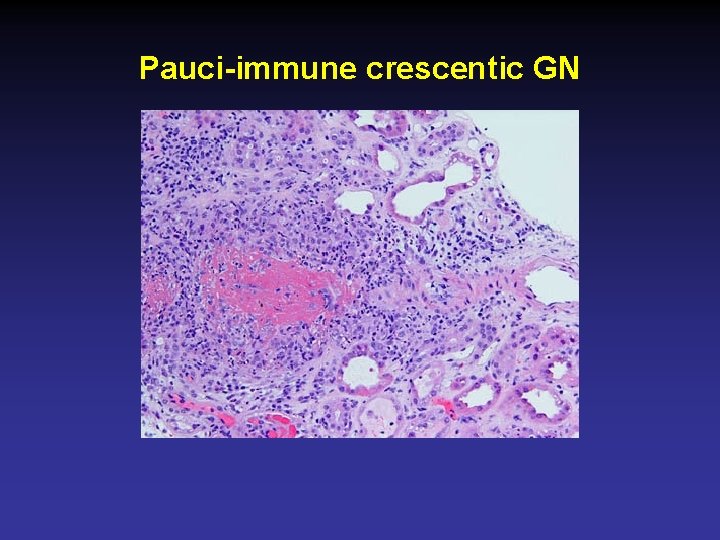
Crescentic GN Etiologies 1. Pauci-immune (ANCA-associated) GN 2. Anti-glomerular basement membrane (anti. GBM) GN 3. Immune complex-mediated GN • Ig. A nephropathy • Lupus nephritis • Membranoproliferative GN • Post-infectious GN • Etc.
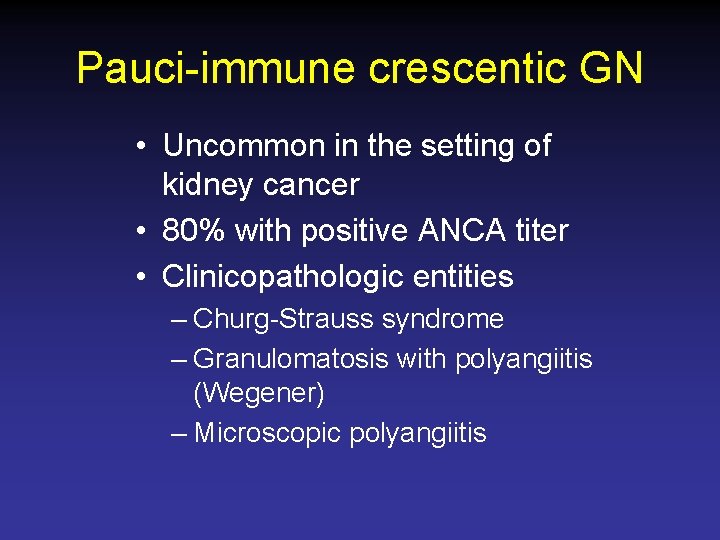
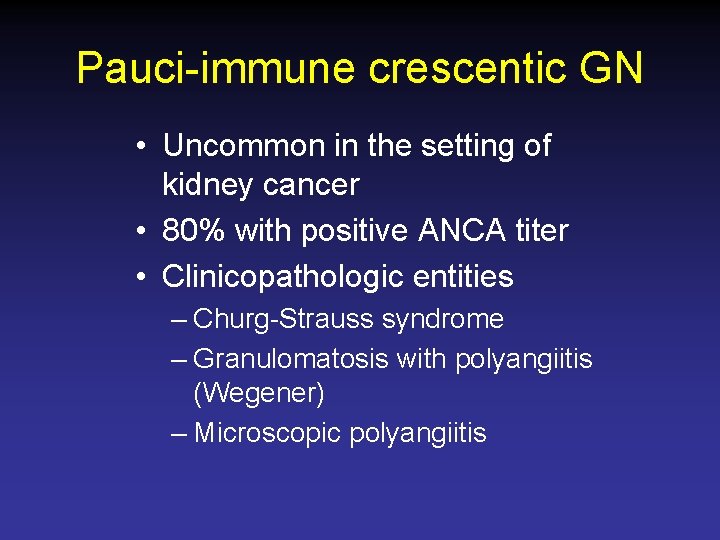
Pauci-immune crescentic GN • Uncommon in the setting of kidney cancer • 80% with positive ANCA titer • Clinicopathologic entities – Churg-Strauss syndrome – Granulomatosis with polyangiitis (Wegener) – Microscopic polyangiitis
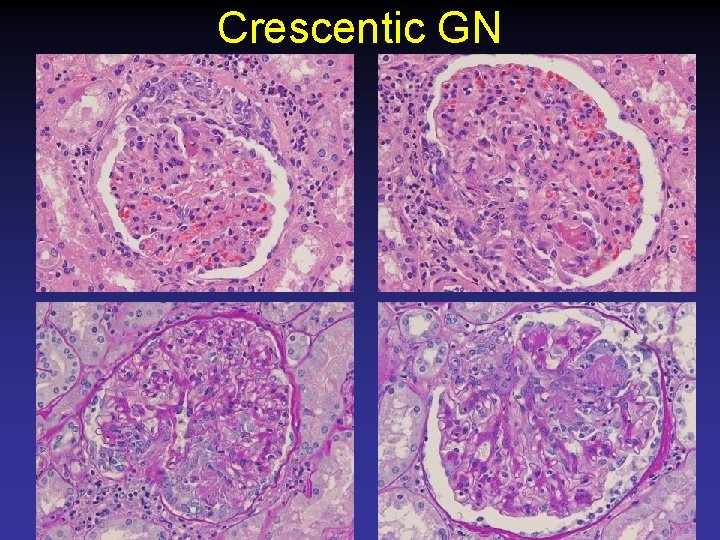
Crescentic GN
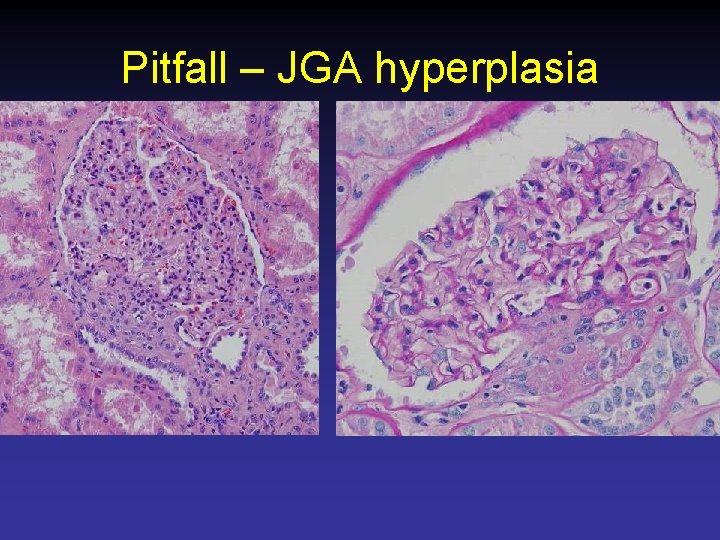
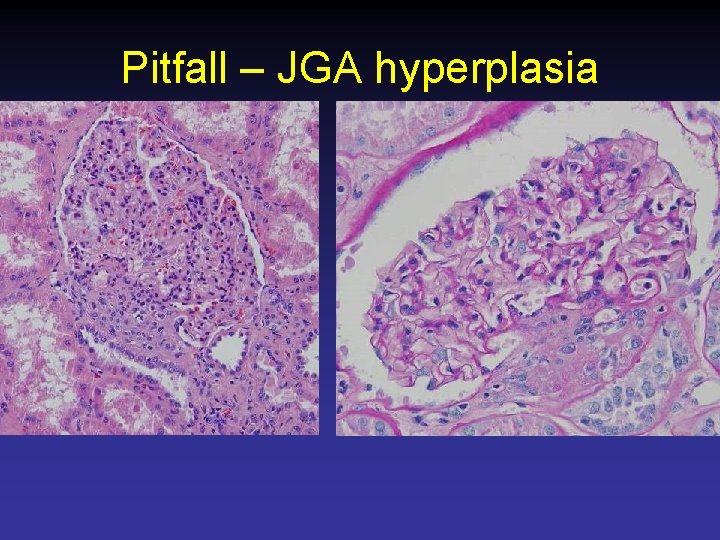
Pitfall – JGA hyperplasia
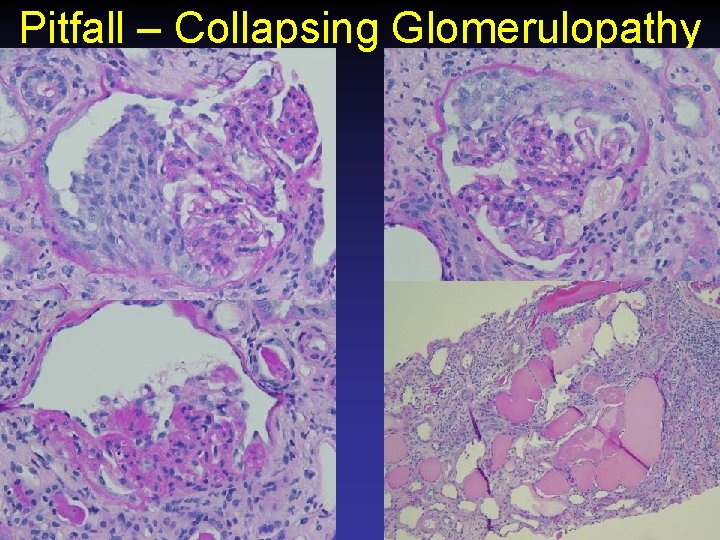
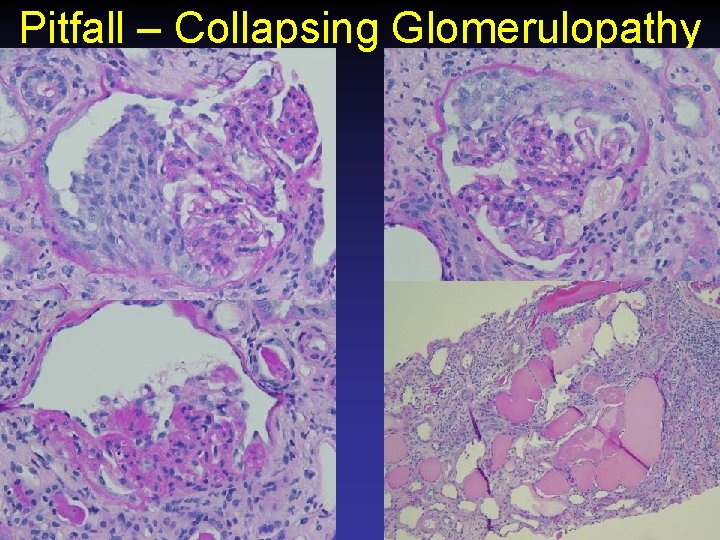
Pitfall – Collapsing Glomerulopathy
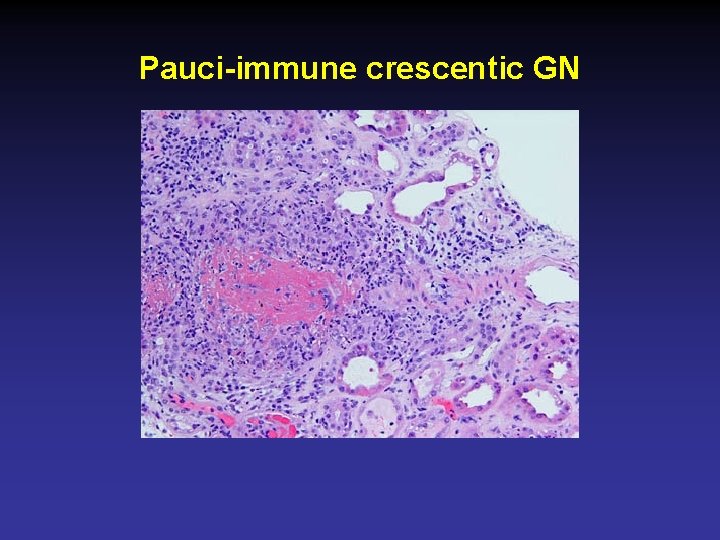
Pauci-immune crescentic GN

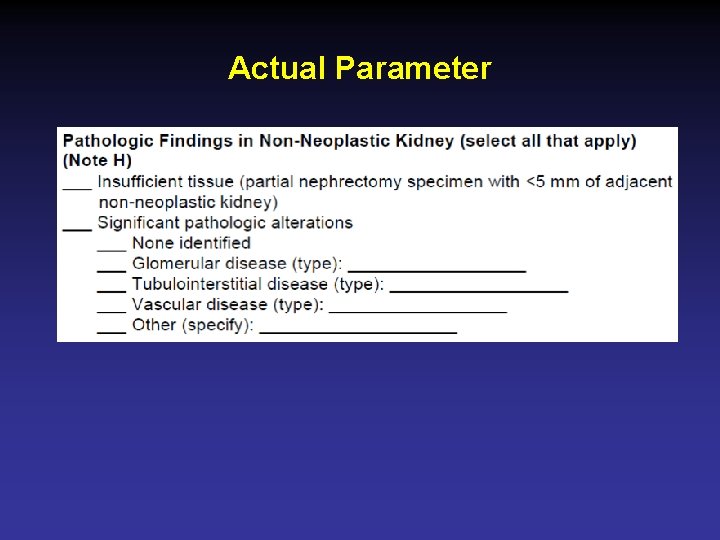
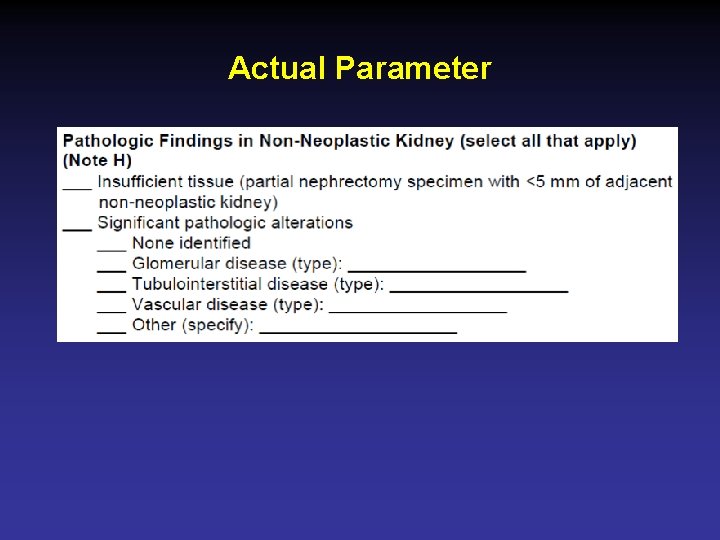
Actual Parameter
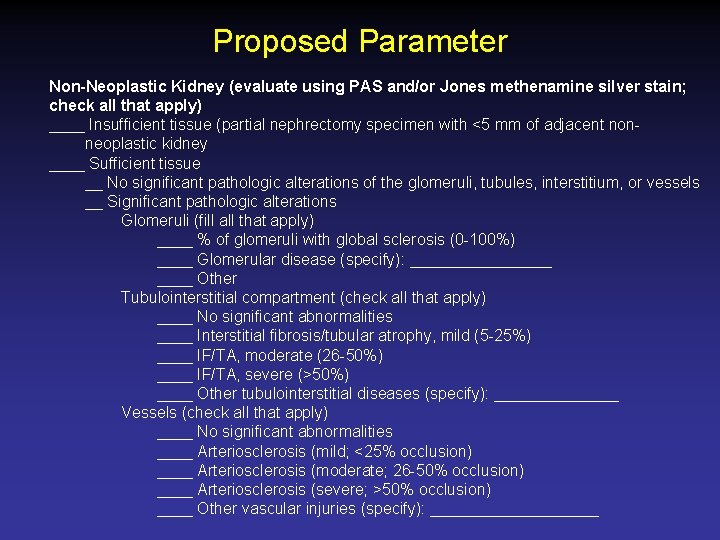
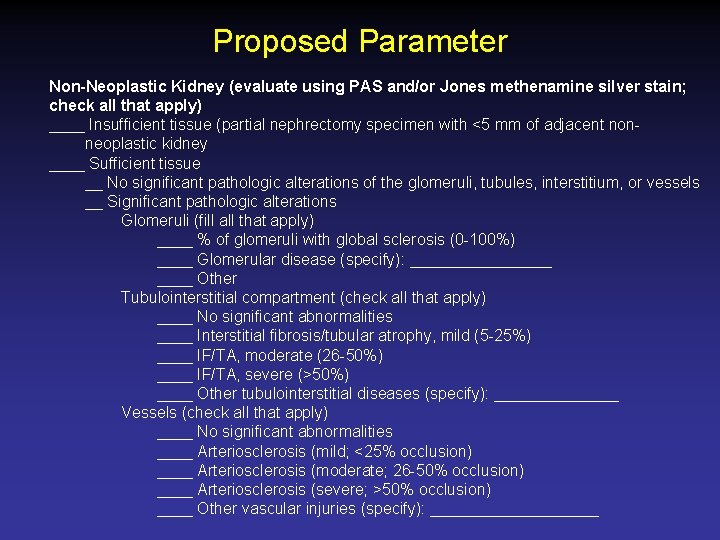
Proposed Parameter Non-Neoplastic Kidney (evaluate using PAS and/or Jones methenamine silver stain; check all that apply) ____ Insufficient tissue (partial nephrectomy specimen with <5 mm of adjacent nonneoplastic kidney ____ Sufficient tissue __ No significant pathologic alterations of the glomeruli, tubules, interstitium, or vessels __ Significant pathologic alterations Glomeruli (fill all that apply) ____ % of glomeruli with global sclerosis (0 -100%) ____ Glomerular disease (specify): ________ Other Tubulointerstitial compartment (check all that apply) ____ No significant abnormalities ____ Interstitial fibrosis/tubular atrophy, mild (5 -25%) ____ IF/TA, moderate (26 -50%) ____ IF/TA, severe (>50%) ____ Other tubulointerstitial diseases (specify): _______ Vessels (check all that apply) ____ No significant abnormalities ____ Arteriosclerosis (mild; <25% occlusion) ____ Arteriosclerosis (moderate; 26 -50% occlusion) ____ Arteriosclerosis (severe; >50% occlusion) ____ Other vascular injuries (specify): __________
Future Directions • Improve coordinated care between urologists and nephrologists • Refine therapeutic implications of pathologic parameters of the non-neoplastic kidney – % Global glomerulosclerosis – Severity of interstitial fibrosis / tubular atrophy – Severity of arteriosclerosis or arteriolosclerosis
Summary • Chronic Kidney Disease / End-stage renal disease is important • Non-neoplastic renal diseases are common – Diabetic nephropathy – Arterionephrosclerosis • Examine the non-neoplastic kidney carefully, especially with benign tumors! • Order PAS/Jones silver stains
Questions?
 Chronic kidney disease near atwater
Chronic kidney disease near atwater Nih score
Nih score Nursing care plan of cancer patients ppt
Nursing care plan of cancer patients ppt Seer kidney cancer
Seer kidney cancer Stomach cancer symptons
Stomach cancer symptons Wagner model of chronic disease management
Wagner model of chronic disease management Chronic granulomatous disease
Chronic granulomatous disease Vijaya's echo criteria
Vijaya's echo criteria Peripheral stigmata of cld
Peripheral stigmata of cld Chronic disease
Chronic disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Chronic disease
Chronic disease Stages of cirrhosis of the liver
Stages of cirrhosis of the liver Jewish chronic disease hospital study
Jewish chronic disease hospital study Kate lorig chronic disease self-management
Kate lorig chronic disease self-management Copd full form
Copd full form Features of cld
Features of cld Albumin kidney disease
Albumin kidney disease Low potassium diet nemo
Low potassium diet nemo Albumin kidney disease
Albumin kidney disease Sighns of kidney problems
Sighns of kidney problems Symptomatic polycystic kidney disease
Symptomatic polycystic kidney disease Choronic kidney disease
Choronic kidney disease Cancer burden of disease
Cancer burden of disease Bharathi viswanathan
Bharathi viswanathan Chronic inflammation
Chronic inflammation Chronic care solutions
Chronic care solutions Circulatory disturbances pathology
Circulatory disturbances pathology Definition of chronic toxicity
Definition of chronic toxicity Wagner chronic care model 1998
Wagner chronic care model 1998 Cbti program
Cbti program Pbc vs psc
Pbc vs psc Myalgic encephalomyelitis
Myalgic encephalomyelitis Endolaser dcr
Endolaser dcr O que é isso
O que é isso Chronic rejection
Chronic rejection Chronic inducible urticaria
Chronic inducible urticaria Chronic care
Chronic care Chronic pancreatitis guideline
Chronic pancreatitis guideline Mycloblast
Mycloblast Chronic care solutions
Chronic care solutions Mouse nibbled appearance of vocal cord is seen in
Mouse nibbled appearance of vocal cord is seen in Errosive gastritis
Errosive gastritis Mild persistent asthma
Mild persistent asthma Chronic
Chronic Basement membrane stain
Basement membrane stain Hemolysis symptoms
Hemolysis symptoms Chronic hepatitis
Chronic hepatitis Flinders model of chronic health disorders
Flinders model of chronic health disorders Leukemoid reaction
Leukemoid reaction Periapical granuloma vs abscess
Periapical granuloma vs abscess Cml stages
Cml stages