Acute Kidney Injury Outline Acute Kidney Injury I




![Estimated Baseline SCr Age (Years) 36 Black Males (mg/d. L [μmol/L]) Other Males (mg/d. Estimated Baseline SCr Age (Years) 36 Black Males (mg/d. L [μmol/L]) Other Males (mg/d.](https://slidetodoc.com/presentation_image/3397c7e71ad258886721007bd48510a5/image-36.jpg)


- Slides: 65
Acute Kidney Injury
Outline: Acute Kidney Injury I. Anatomy II. Epidemiology III. Mortality & Cost IV. Diagnosis, Assessment, & Management V. Treatment VI. Limitations and Unmet Clinical Needs 2

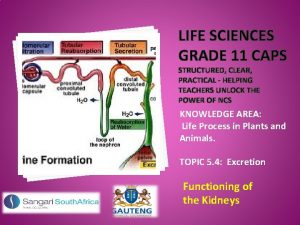
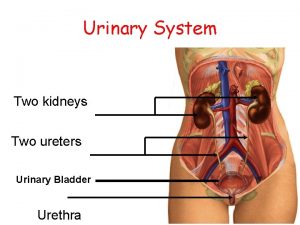
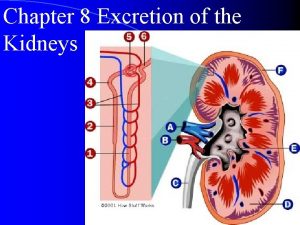
Anatomy 3
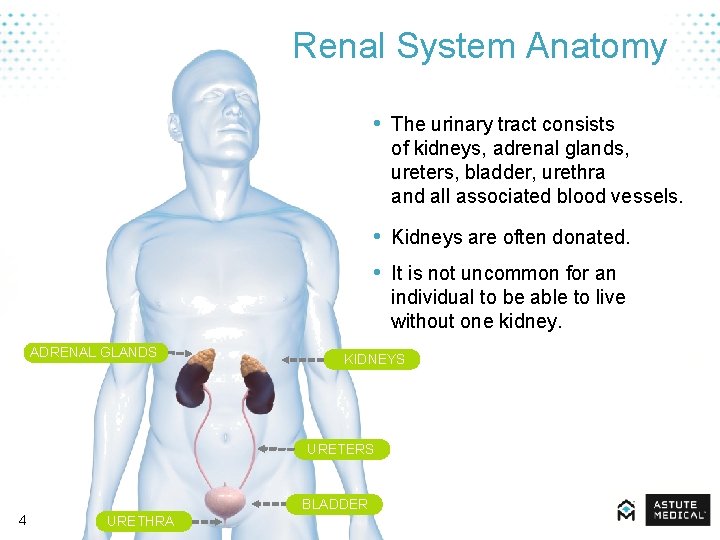
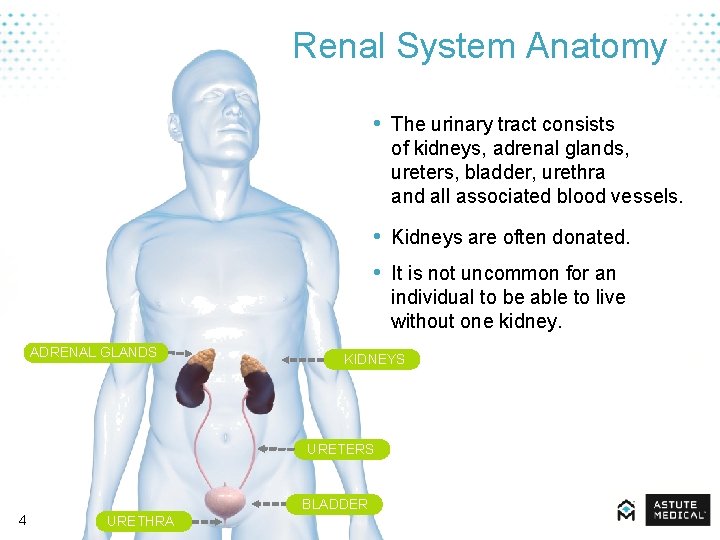
Renal System Anatomy • The urinary tract consists of kidneys, adrenal glands, ureters, bladder, urethra and all associated blood vessels. • Kidneys are often donated. • It is not uncommon for an individual to be able to live without one kidney. ADRENAL GLANDS KIDNEYS URETERS 4 BLADDER URETHRA
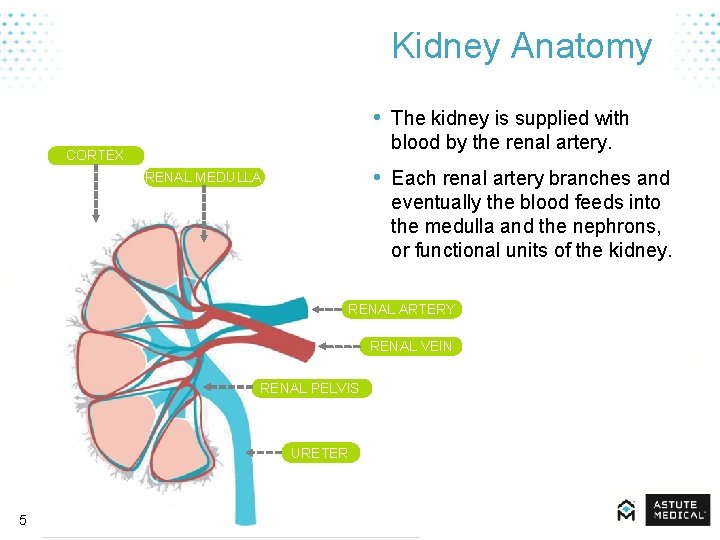
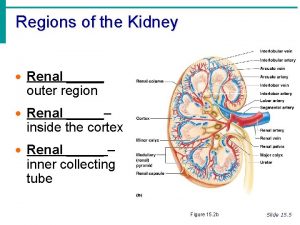
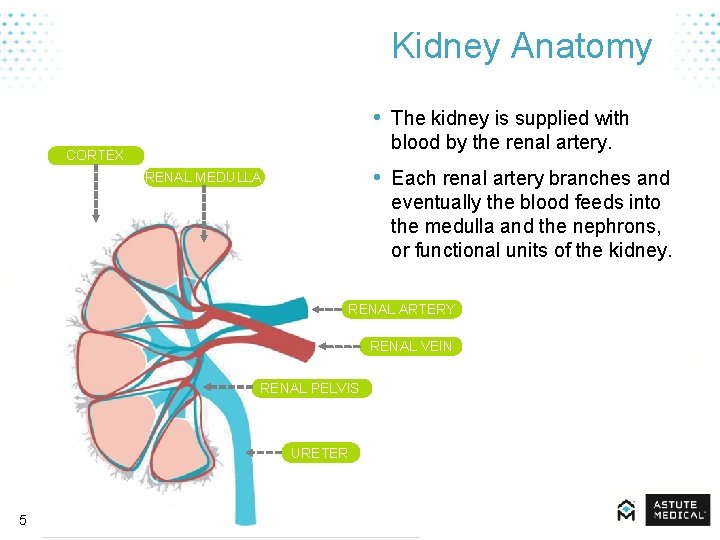
Kidney Anatomy • The kidney is supplied with blood by the renal artery. CORTEX • Each renal artery branches and RENAL MEDULLA eventually the blood feeds into the medulla and the nephrons, or functional units of the kidney. RENAL ARTERY RENAL VEIN RENAL PELVIS URETER 5
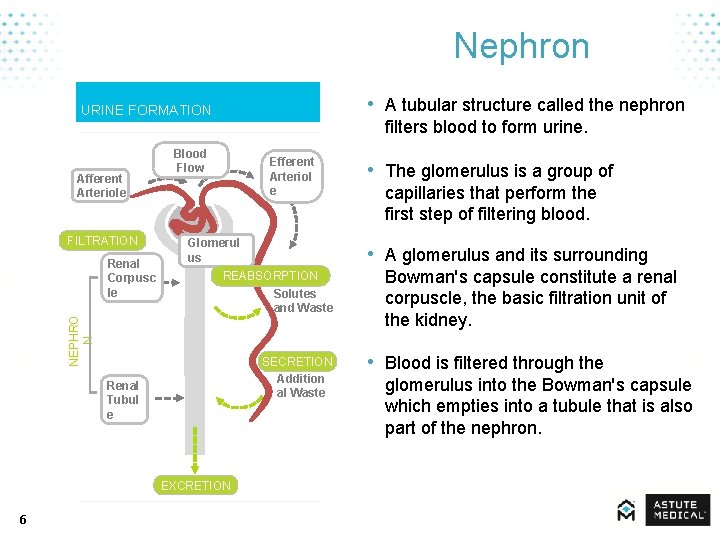
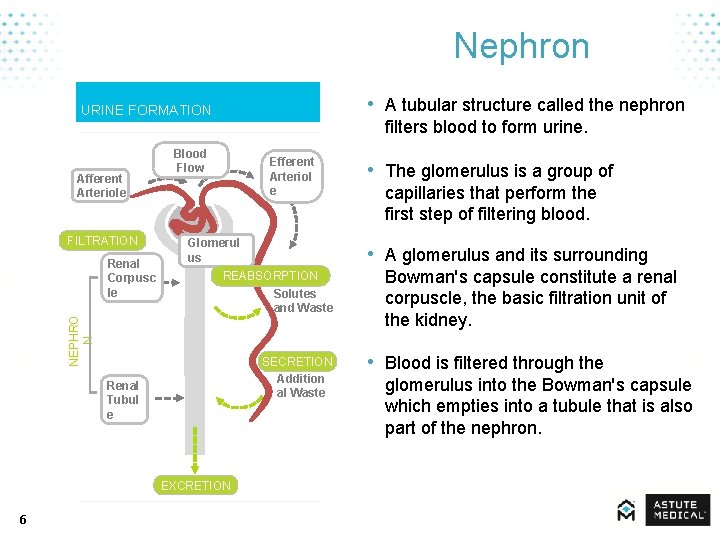
Nephron • A tubular structure called the nephron URINE FORMATION Afferent Arteriole FILTRATION Blood Flow Efferent Arteriol e Glomerul us SECRETION Addition al Waste Renal Tubul e EXCRETION 6 • The glomerulus is a group of capillaries that perform the first step of filtering blood. • A glomerulus and its surrounding REABSORPTION Solutes and Waste NEPHRO N Renal Corpusc le filters blood to form urine. Bowman's capsule constitute a renal corpuscle, the basic filtration unit of the kidney. • Blood is filtered through the glomerulus into the Bowman's capsule which empties into a tubule that is also part of the nephron.

Epidemiology 7
Acute Kidney Injury • Acute kidney injury (AKI) is a rapid loss of kidney function including: – Rapid time course (less than 48 hours) – Rise in serum creatinine – Reduction in urine output (oliguria) 8 Mehta RL, Kellum JA, Shah SV et al. Crit Care. 2007; 11(2): R 31.
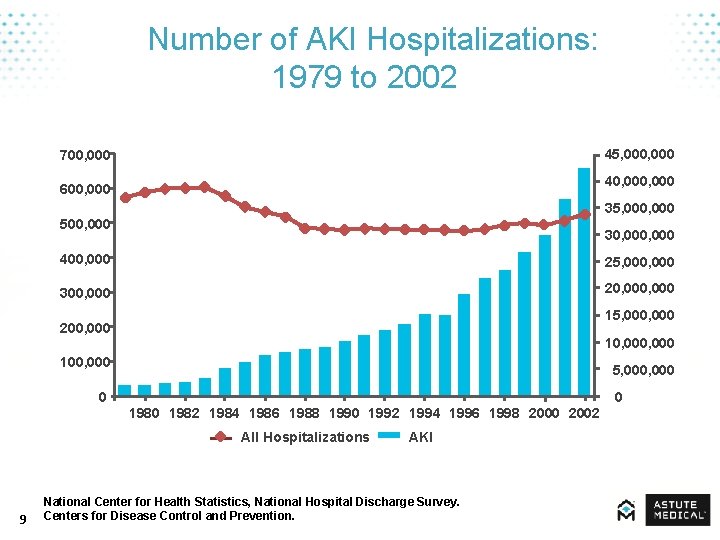
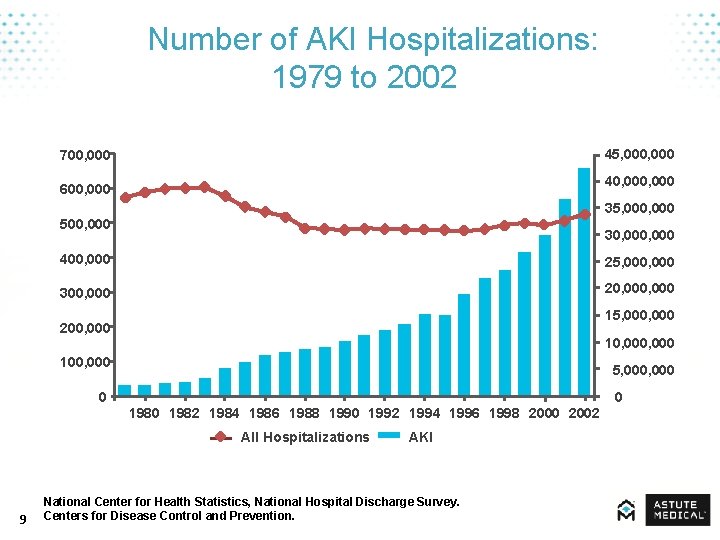
Number of AKI Hospitalizations: 1979 to 2002 45, 000 700, 000 40, 000 600, 000 500, 000 35, 000 400, 000 30, 000 25, 000 300, 000 20, 000 15, 000 200, 000 100, 000 10, 000 5, 000 0 1982 1984 1986 1988 1990 1992 1994 1996 1998 2000 2002 All Hospitalizations AKI National Center for Health Statistics, National Hospital Discharge Survey. Centers for Disease Control and Prevention. 9 0
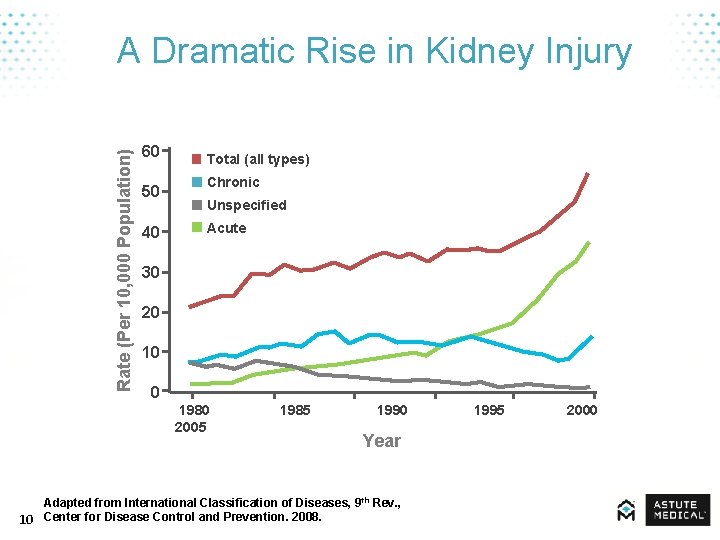
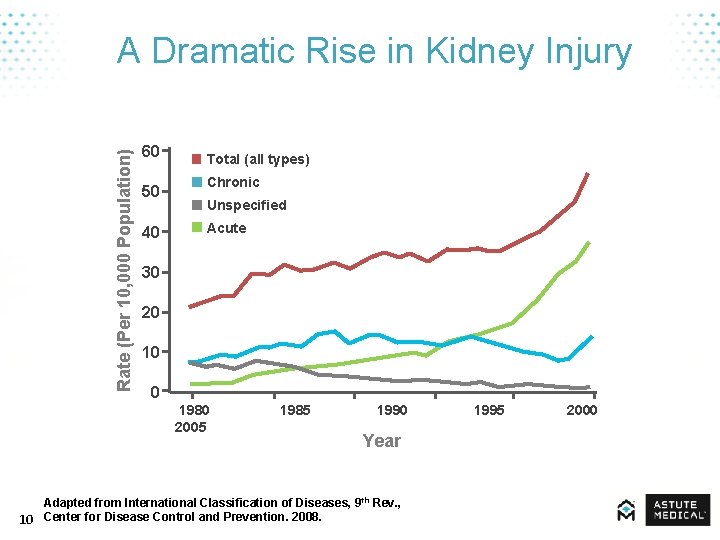
Rate (Per 10, 000 Population) A Dramatic Rise in Kidney Injury 60 50 40 Total (all types) Chronic Unspecified Acute 30 20 10 0 1980 1985 1990 1995 2000 2005 Year Adapted from International Classification of Diseases, 9 th Rev. , 10 Center for Disease Control and Prevention. 2008.
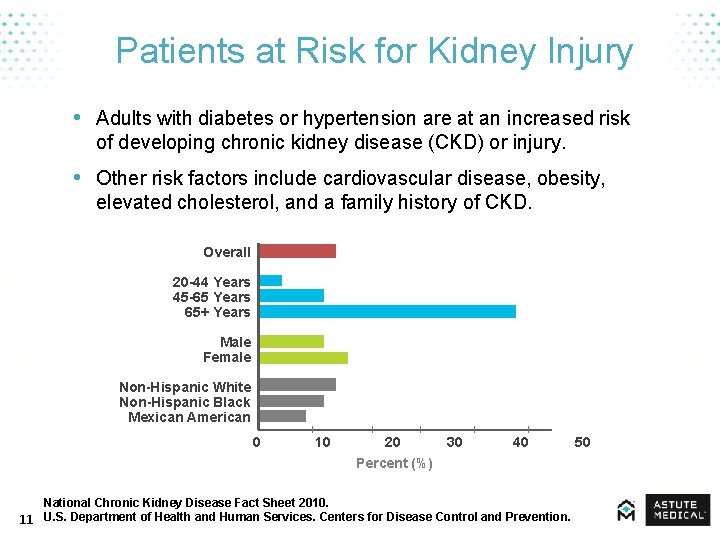
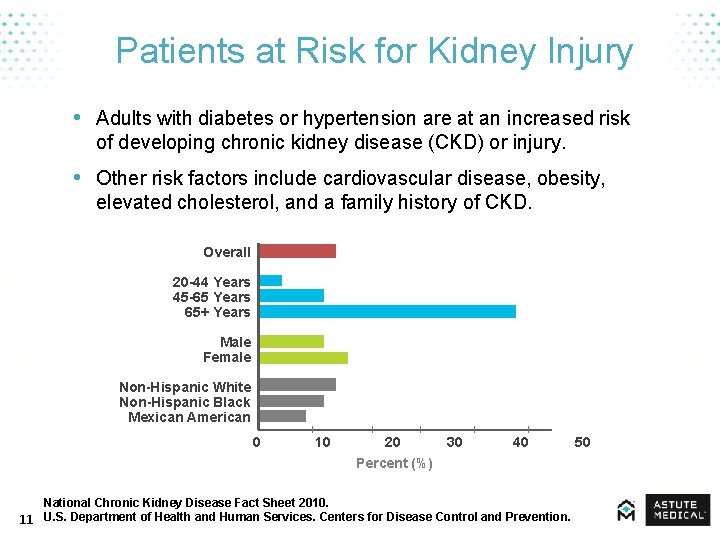
Patients at Risk for Kidney Injury • Adults with diabetes or hypertension are at an increased risk of developing chronic kidney disease (CKD) or injury. • Other risk factors include cardiovascular disease, obesity, elevated cholesterol, and a family history of CKD. Overall 20 -44 Years 45 -65 Years 65+ Years Male Female Non-Hispanic White Non-Hispanic Black Mexican American 0 10 20 30 40 50 Percent (%) National Chronic Kidney Disease Fact Sheet 2010. 11 U. S. Department of Health and Human Services. Centers for Disease Control and Prevention.
AKI Risk Factors • • • 12 Sepsis Age > 65 years Presence of infection Low cardiac output Major surgery Trauma Cancer Hypervolemia (fluid overload) Cirrhosis Certain medications Dennen P, Douglas IS, Anderson R. Crit Care Med. 2010; 38: 261 -75. Kidney Disease: Improving Global Outcomes (KDIGO). 2008.
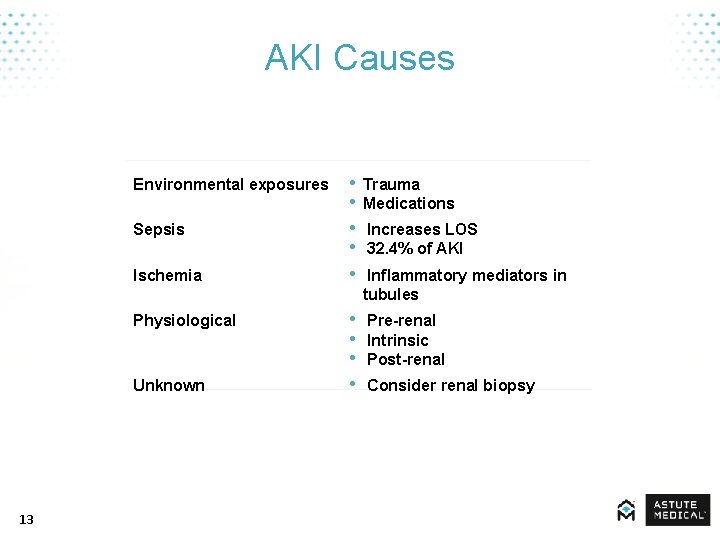
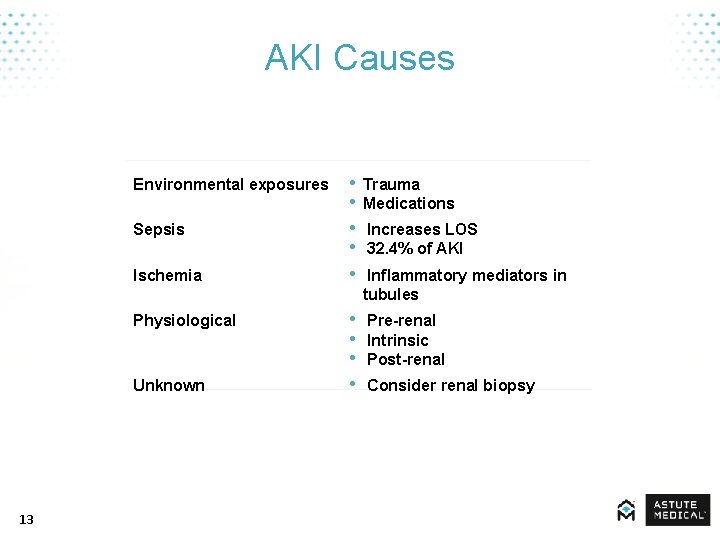
AKI Causes Environmental exposures Sepsis Ischemia Physiological Unknown 13 • • • Trauma Medications • • Pre-renal Intrinsic Post-renal Increases LOS 32. 4% of AKI Inflammatory mediators in tubules Consider renal biopsy
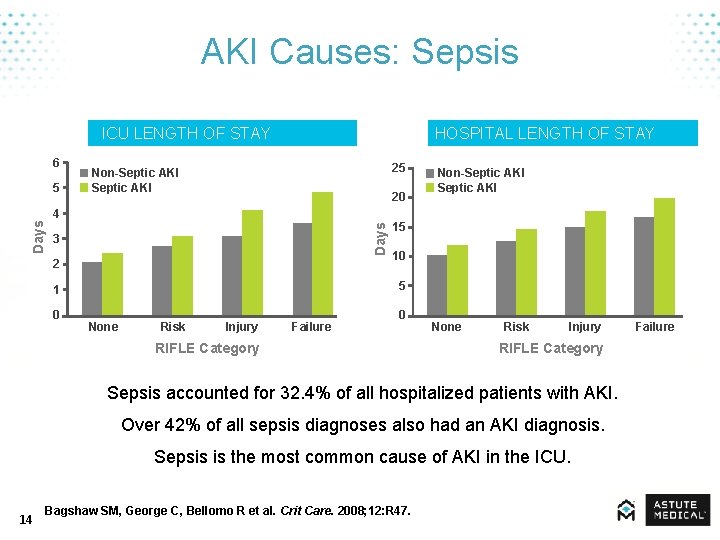
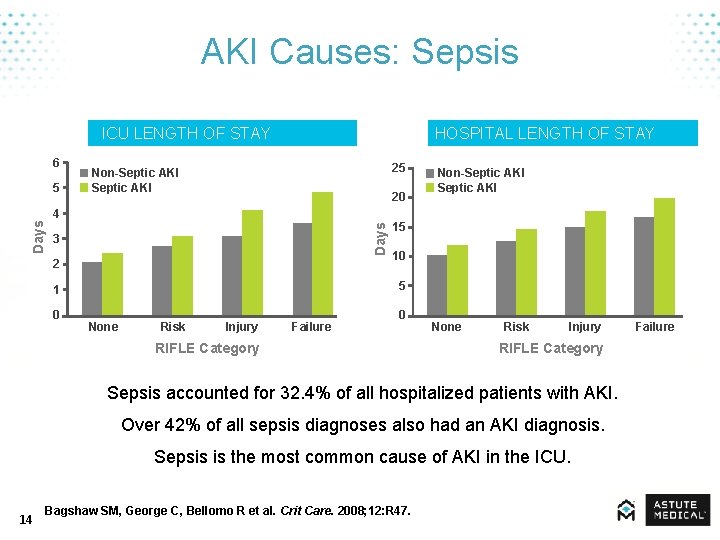
AKI Causes: Sepsis ICU LENGTH OF STAY 6 5 HOSPITAL LENGTH OF STAY 25 Non-Septic AKI 20 Days 4 3 2 15 10 5 1 0 Non-Septic AKI None Risk Injury Failure 0 RIFLE Category None Risk Injury RIFLE Category Sepsis accounted for 32. 4% of all hospitalized patients with AKI. Over 42% of all sepsis diagnoses also had an AKI diagnosis. Sepsis is the most common cause of AKI in the ICU. 14 Bagshaw SM, George C, Bellomo R et al. Crit Care. 2008; 12: R 47. Failure
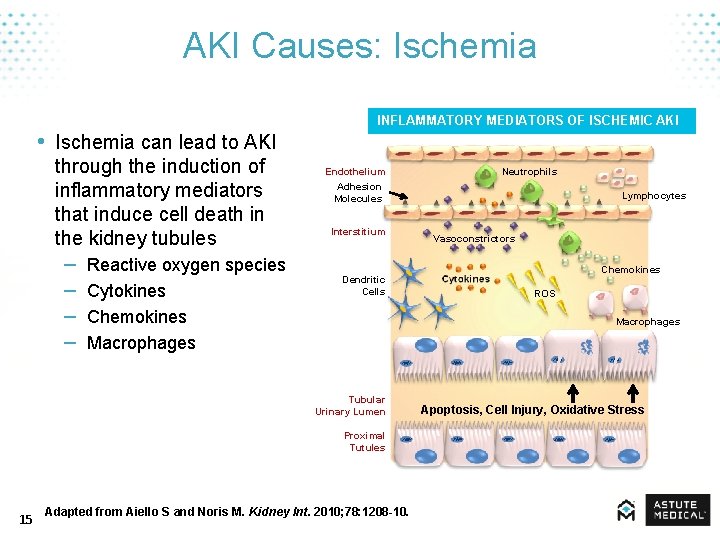
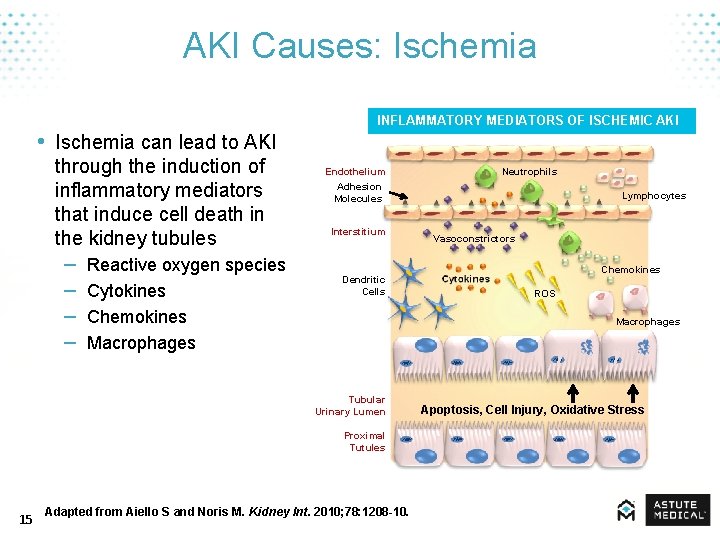
AKI Causes: Ischemia • Ischemia can lead to AKI through the induction of inflammatory mediators that induce cell death in the kidney tubules – – Reactive oxygen species Cytokines Chemokines Macrophages INFLAMMATORY MEDIATORS OF ISCHEMIC AKI Endothelium Adhesion Molecules Interstitium Dendritic Cells Lymphocytes Vasoconstrictors Chemokines ROS Macrophages Tubular Urinary Lumen Proximal Tutules 15 Neutrophils Adapted from Aiello S and Noris M. Kidney Int. 2010; 78: 1208 -10. Apoptosis, Cell Injury, Oxidative Stress
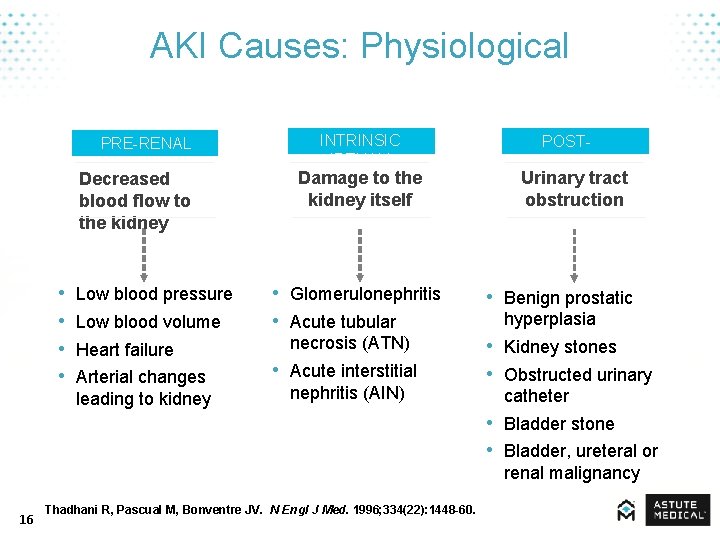
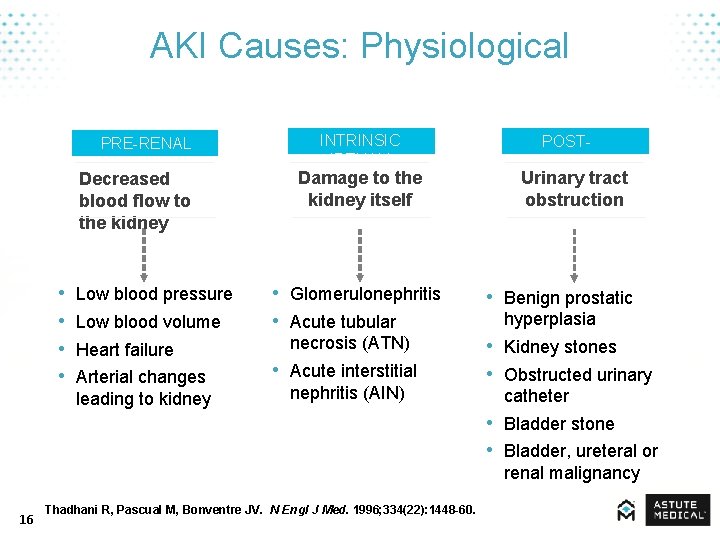
AKI Causes: Physiological PRE-RENAL Decreased blood flow to the kidney • • Low blood pressure Low blood volume Heart failure Arterial changes leading to kidney INTRINSIC (RENAL) Damage to the kidney itself • Glomerulonephritis • Acute tubular necrosis (ATN) • Acute interstitial nephritis (AIN) POSTRENAL Urinary tract obstruction • Benign prostatic hyperplasia • Kidney stones • Obstructed urinary catheter • Bladder stone • Bladder, ureteral or renal malignancy 16 Thadhani R, Pascual M, Bonventre JV. N Engl J Med. 1996; 334(22): 1448 -60.
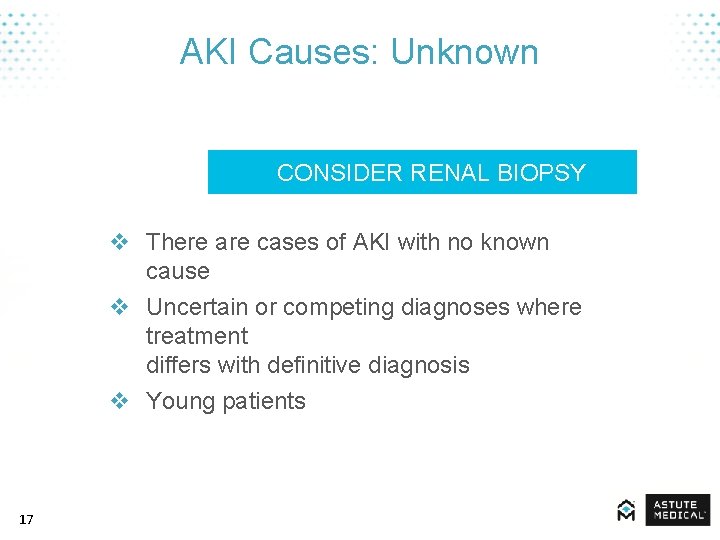
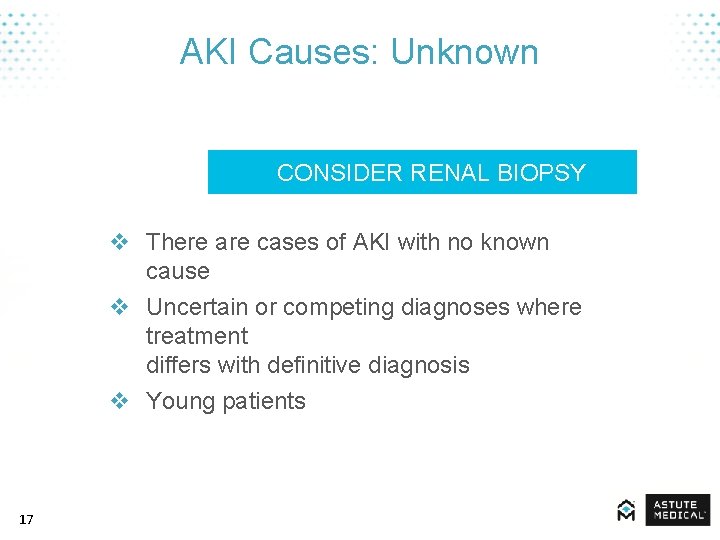
AKI Causes: Unknown CONSIDER RENAL BIOPSY v There are cases of AKI with no known cause v Uncertain or competing diagnoses where treatment differs with definitive diagnosis v Young patients 17
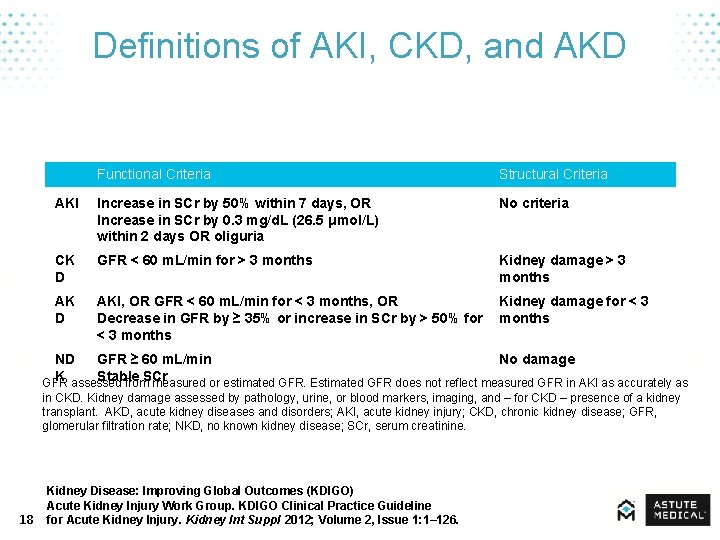
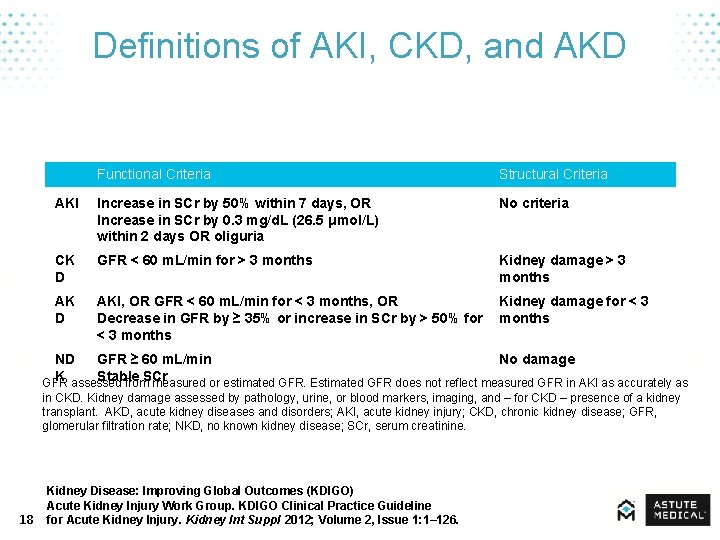
Definitions of AKI, CKD, and AKD Functional Criteria Structural Criteria AKI Increase in SCr by 50% within 7 days, OR Increase in SCr by 0. 3 mg/d. L (26. 5 μmol/L) within 2 days OR oliguria No criteria CK D GFR < 60 m. L/min for > 3 months Kidney damage > 3 months AK D AKI, OR GFR < 60 m. L/min for < 3 months, OR Kidney damage for < 3 Decrease in GFR by ≥ 35% or increase in SCr by > 50% for months < 3 months ND GFR ≥ 60 m. L/min No damage K Stable SCr GFR assessed from measured or estimated GFR. Estimated GFR does not reflect measured GFR in AKI as accurately as in CKD. Kidney damage assessed by pathology, urine, or blood markers, imaging, and – for CKD – presence of a kidney transplant. AKD, acute kidney diseases and disorders; AKI, acute kidney injury; CKD, chronic kidney disease; GFR, glomerular filtration rate; NKD, no known kidney disease; SCr, serum creatinine. 18 Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2012; Volume 2, Issue 1: 1– 126.
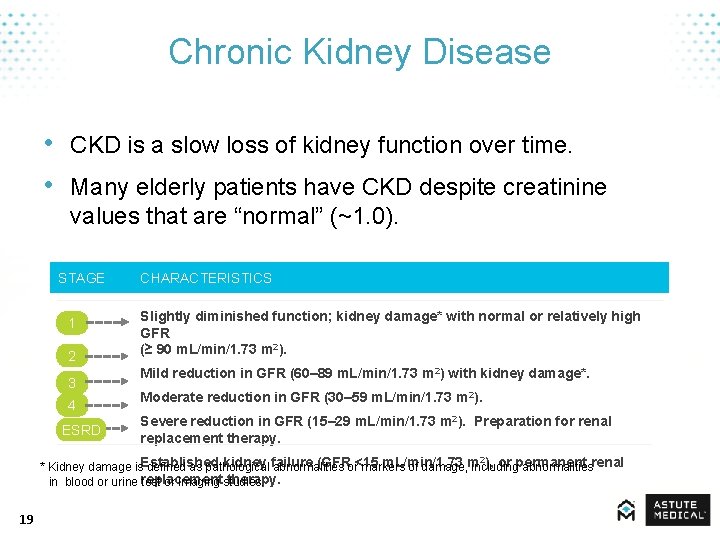
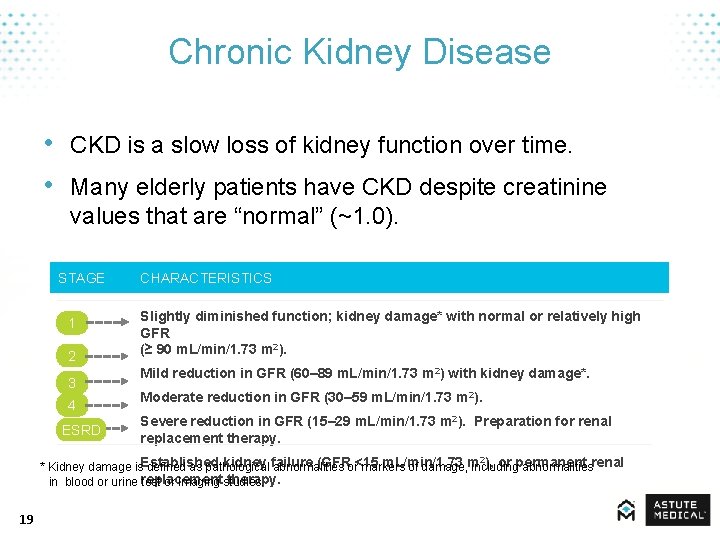
Chronic Kidney Disease • CKD is a slow loss of kidney function over time. • Many elderly patients have CKD despite creatinine values that are “normal” (~1. 0). STAGE 1 2 3 4 ESRD CHARACTERISTICS Slightly diminished function; kidney damage* with normal or relatively high GFR (≥ 90 m. L/min/1. 73 m 2). Mild reduction in GFR (60– 89 m. L/min/1. 73 m 2) with kidney damage*. Moderate reduction in GFR (30– 59 m. L/min/1. 73 m 2). Severe reduction in GFR (15– 29 m. L/min/1. 73 m 2). Preparation for renal replacement therapy. Established kidney failure (GFR <15 m. L/min/1. 73 m ), or permanent renal * Kidney damage is defined as pathological abnormalities or markers of damage, including abnormalities replacement therapy. in blood or urine test or imaging studies. 2 19
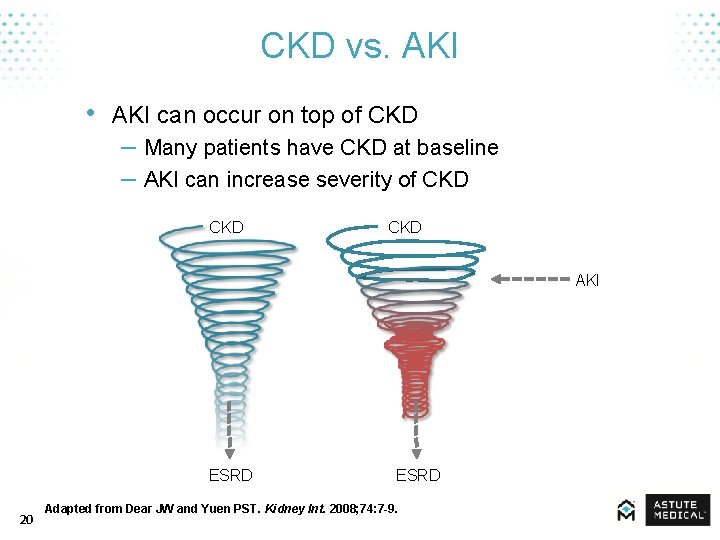
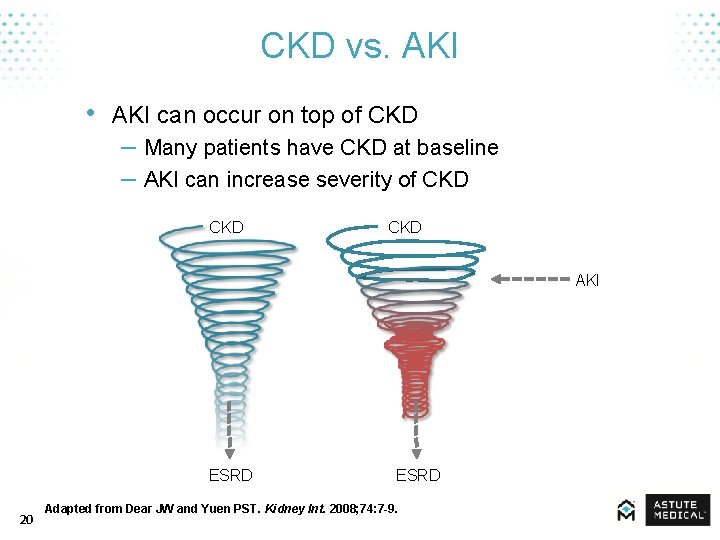
CKD vs. AKI • AKI can occur on top of CKD – Many patients have CKD at baseline – AKI can increase severity of CKD CKD AKI ESRD 20 ESRD Adapted from Dear JW and Yuen PST. Kidney Int. 2008; 74: 7 -9.
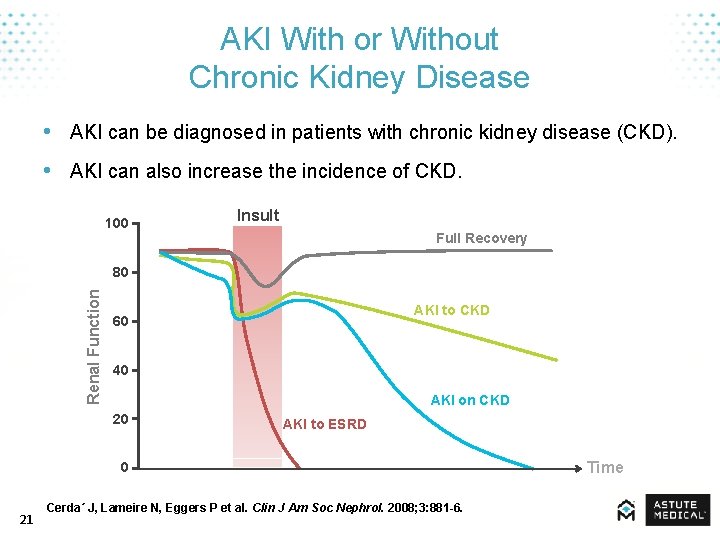
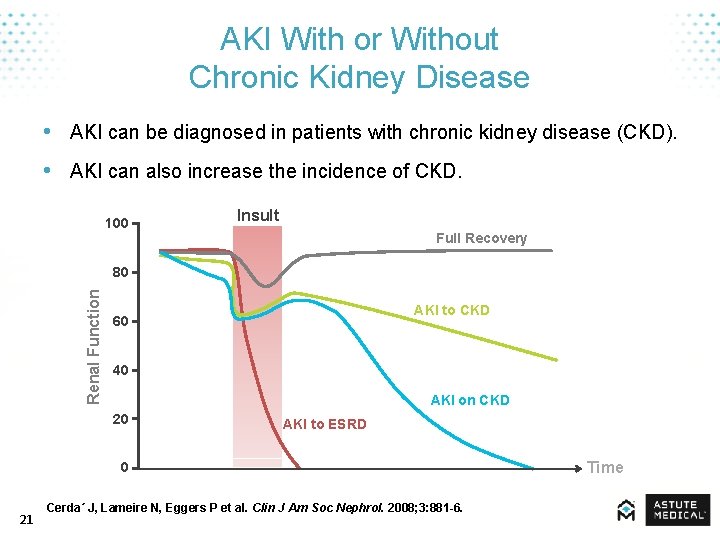
AKI With or Without Chronic Kidney Disease • AKI can be diagnosed in patients with chronic kidney disease (CKD). • AKI can also increase the incidence of CKD. 100 Insult Full Recovery Renal Function 80 AKI to CKD 60 40 AKI on CKD 20 AKI to ESRD 0 21 Cerda´ J, Lameire N, Eggers P et al. Clin J Am Soc Nephrol. 2008; 3: 881 -6. Time
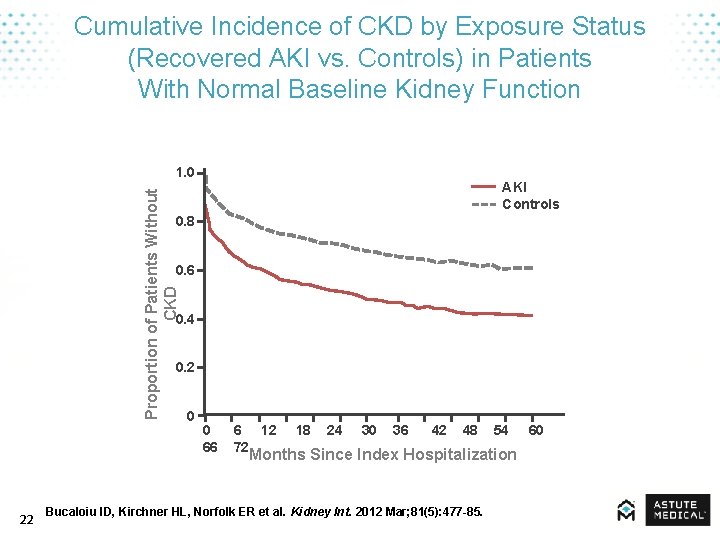
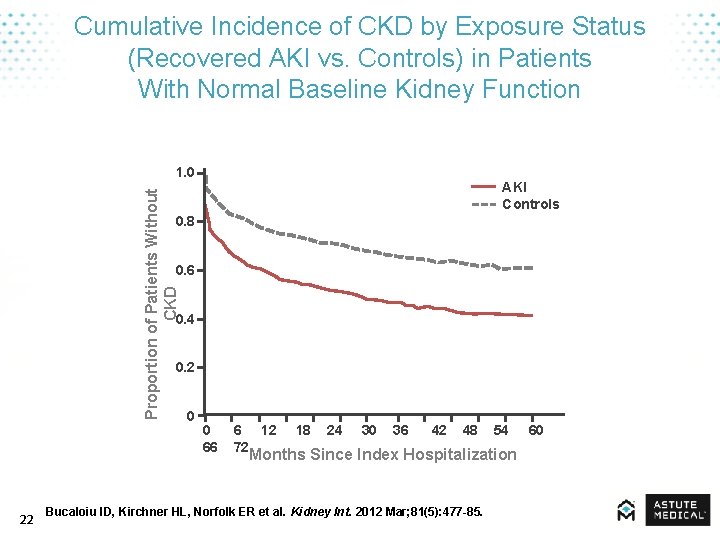
Cumulative Incidence of CKD by Exposure Status (Recovered AKI vs. Controls) in Patients With Normal Baseline Kidney Function Proportion of Patients Without CKD 1. 0 AKI Controls 0. 8 0. 6 0. 4 0. 2 0 0 6 12 18 24 30 36 42 48 54 60 66 72 Months Since Index Hospitalization 22 Bucaloiu ID, Kirchner HL, Norfolk ER et al. Kidney Int. 2012 Mar; 81(5): 477 -85.
Additional Comorbid Pathologies • • Diabetes mellitus Ischemic heart disease Congestive heart failure Hypertension MOST COMORBID CONDITIONS ARE INFLAMMATORY OR CARDIOVASCULAR 23 Bagshaw SM. Nephrol Dial Transplant. 2008; 23(7): 2126 -8.

Mortality & Cost 24
AKI Increases Hospital Length of Stay and Associated Costs AKI = INCREASING COST AND LENGTH OF STAY 25
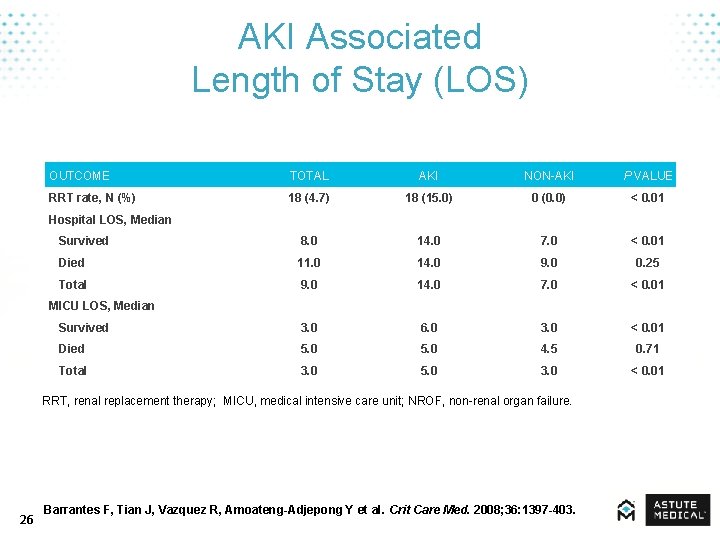
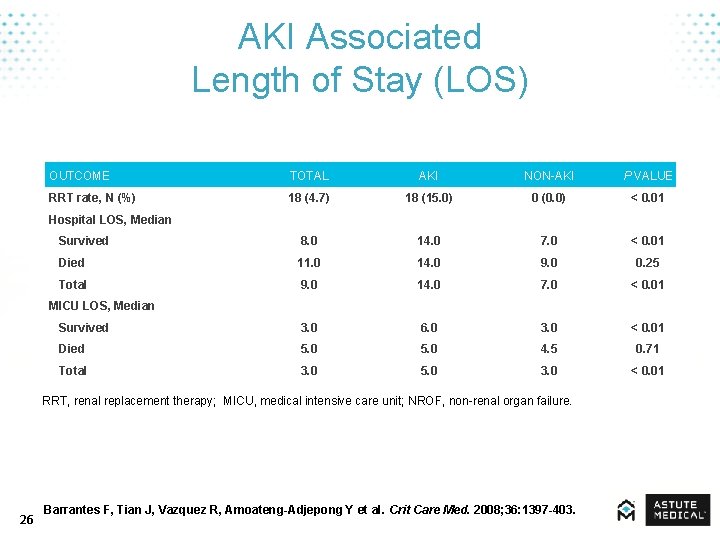
AKI Associated Length of Stay (LOS) OUTCOME TOTAL AKI NON-AKI P VALUE RRT rate, N (%) 18 (4. 7) 18 (15. 0) 0 (0. 0) < 0. 01 Survived 8. 0 14. 0 7. 0 < 0. 01 Died 11. 0 14. 0 9. 0 0. 25 Total 9. 0 14. 0 7. 0 < 0. 01 Survived 3. 0 6. 0 3. 0 < 0. 01 Died 5. 0 4. 5 0. 71 Total 3. 0 5. 0 3. 0 < 0. 01 Hospital LOS, Median MICU LOS, Median RRT, renal replacement therapy; MICU, medical intensive care unit; NROF, non-renal organ failure. 26 Barrantes F, Tian J, Vazquez R, Amoateng-Adjepong Y et al. Crit Care Med. 2008; 36: 1397 -403.
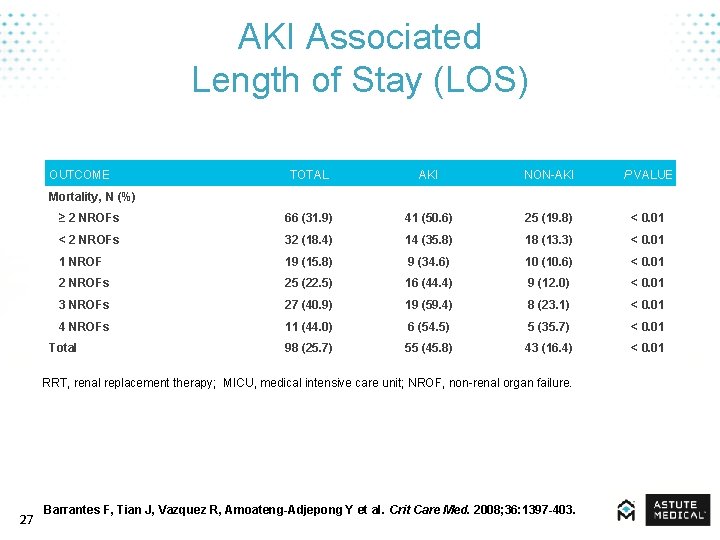
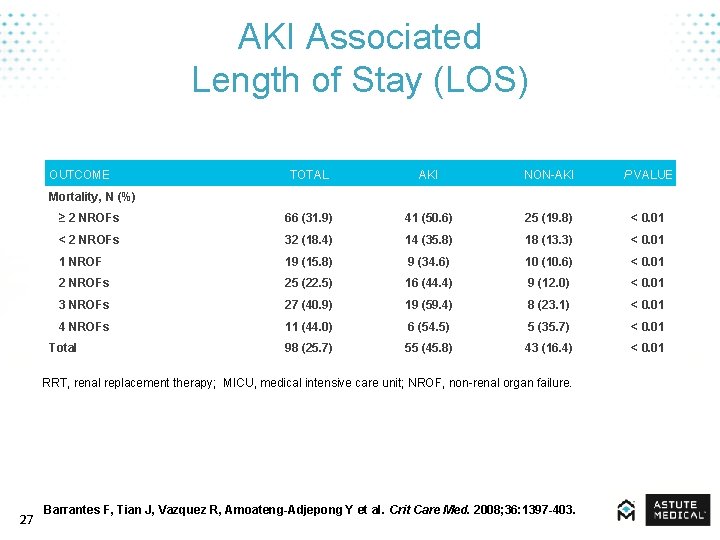
AKI Associated Length of Stay (LOS) OUTCOME TOTAL AKI NON-AKI P VALUE ≥ 2 NROFs 66 (31. 9) 41 (50. 6) 25 (19. 8) < 0. 01 < 2 NROFs 32 (18. 4) 14 (35. 8) 18 (13. 3) < 0. 01 1 NROF 19 (15. 8) 9 (34. 6) 10 (10. 6) < 0. 01 2 NROFs 25 (22. 5) 16 (44. 4) 9 (12. 0) < 0. 01 3 NROFs 27 (40. 9) 19 (59. 4) 8 (23. 1) < 0. 01 4 NROFs 11 (44. 0) 6 (54. 5) 5 (35. 7) < 0. 01 Total 98 (25. 7) 55 (45. 8) 43 (16. 4) < 0. 01 Mortality, N (%) RRT, renal replacement therapy; MICU, medical intensive care unit; NROF, non-renal organ failure. 27 Barrantes F, Tian J, Vazquez R, Amoateng-Adjepong Y et al. Crit Care Med. 2008; 36: 1397 -403.
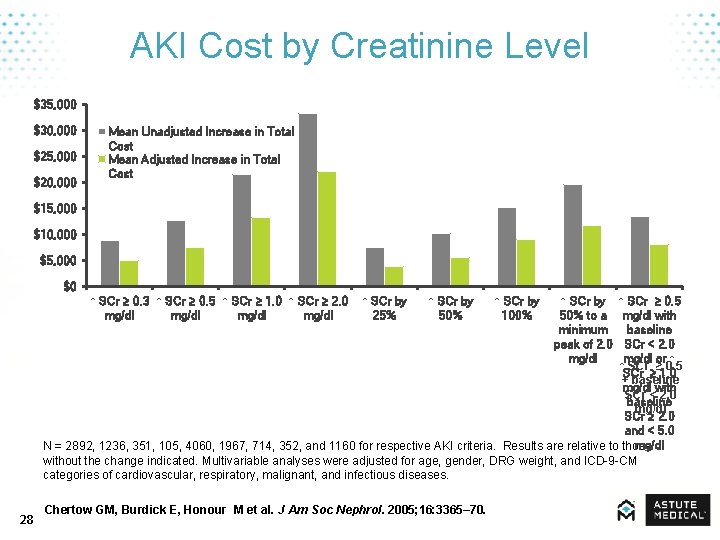
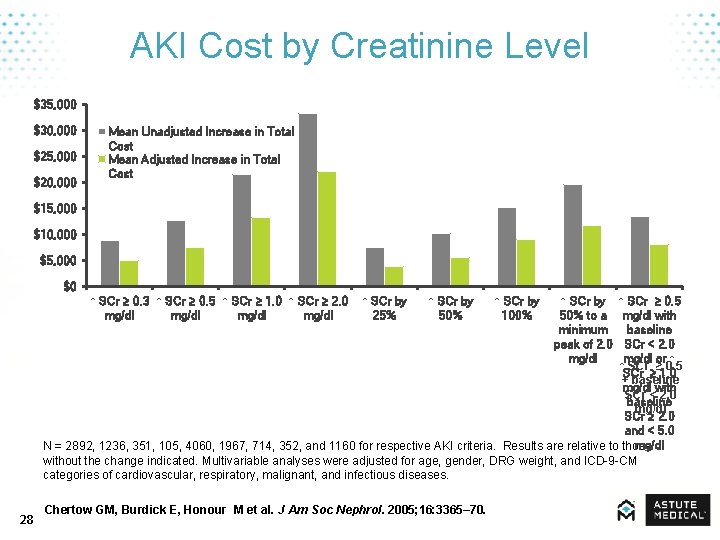
AKI Cost by Creatinine Level $35, 000 $30, 000 $25, 000 $20, 000 Mean Unadjusted Increase in Total Cost Mean Adjusted Increase in Total Cost $15, 000 $10, 000 $5, 000 $0 ↑ SCr ≥ 0. 3 ↑ SCr ≥ 0. 5 ↑ SCr ≥ 1. 0 ↑ SCr ≥ 2. 0 mg/dl ↑ SCr ≥ 0. 5 mg/dl with baseline SCr < 2. 0 mg/dl or ↑ ↑ SCr ≥ 0. 5 SCr ≥ 1. 0 + baseline mg/dl with SCr < 2. 0 baseline mg/dl SCr ≥ 2. 0 and < 5. 0 mg/dl N = 2892, 1236, 351, 105, 4060, 1967, 714, 352, and 1160 for respective AKI criteria. Results are relative to those without the change indicated. Multivariable analyses were adjusted for age, gender, DRG weight, and ICD-9 -CM categories of cardiovascular, respiratory, malignant, and infectious diseases. 28 ↑ SCr by 25% ↑ SCr by 50% Chertow GM, Burdick E, Honour M et al. J Am Soc Nephrol. 2005; 16: 3365– 70. ↑ SCr by 100% ↑ SCr by 50% to a minimum peak of 2. 0 mg/dl
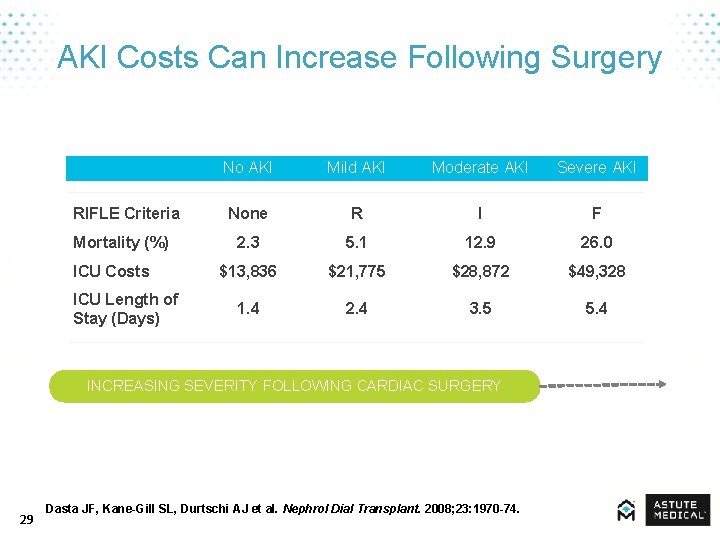
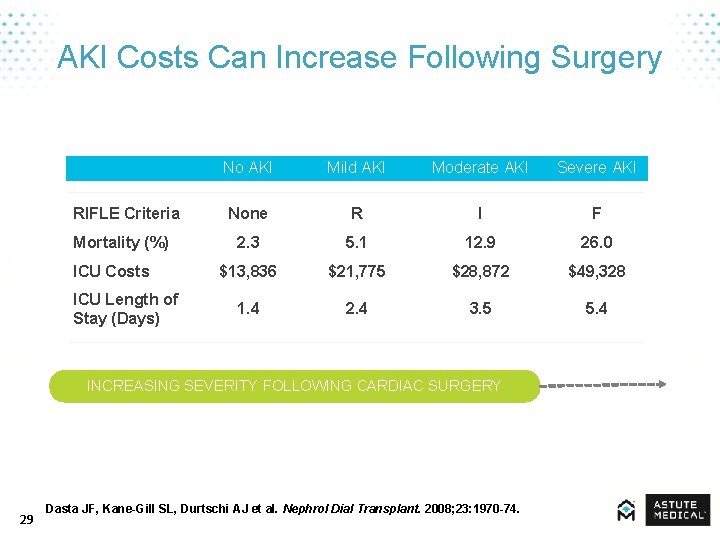
AKI Costs Can Increase Following Surgery RIFLE Criteria Mortality (%) ICU Costs ICU Length of Stay (Days) No AKI Mild AKI Moderate AKI Severe AKI None R I F 2. 3 5. 1 12. 9 26. 0 $13, 836 $21, 775 $28, 872 $49, 328 1. 4 2. 4 3. 5 5. 4 INCREASING SEVERITY FOLLOWING CARDIAC SURGERY 29 Dasta JF, Kane-Gill SL, Durtschi AJ et al. Nephrol Dial Transplant. 2008; 23: 1970 -74.
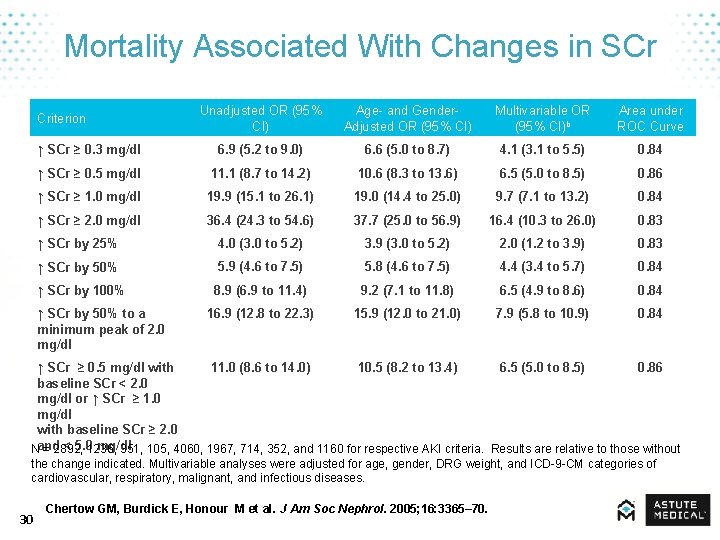
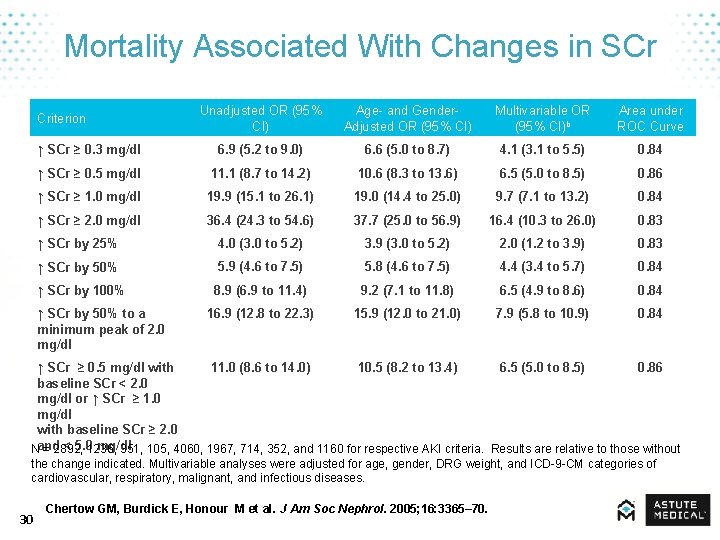
Mortality Associated With Changes in SCr Unadjusted OR (95% CI) Age- and Gender. Adjusted OR (95% CI) Multivariable OR (95% CI)b Area under ROC Curve ↑ SCr ≥ 0. 3 mg/dl 6. 9 (5. 2 to 9. 0) 6. 6 (5. 0 to 8. 7) 4. 1 (3. 1 to 5. 5) 0. 84 ↑ SCr ≥ 0. 5 mg/dl 11. 1 (8. 7 to 14. 2) 10. 6 (8. 3 to 13. 6) 6. 5 (5. 0 to 8. 5) 0. 86 ↑ SCr ≥ 1. 0 mg/dl 19. 9 (15. 1 to 26. 1) 19. 0 (14. 4 to 25. 0) 9. 7 (7. 1 to 13. 2) 0. 84 ↑ SCr ≥ 2. 0 mg/dl 36. 4 (24. 3 to 54. 6) 37. 7 (25. 0 to 56. 9) 16. 4 (10. 3 to 26. 0) 0. 83 ↑ SCr by 25% 4. 0 (3. 0 to 5. 2) 3. 9 (3. 0 to 5. 2) 2. 0 (1. 2 to 3. 9) 0. 83 ↑ SCr by 50% 5. 9 (4. 6 to 7. 5) 5. 8 (4. 6 to 7. 5) 4. 4 (3. 4 to 5. 7) 0. 84 ↑ SCr by 100% 8. 9 (6. 9 to 11. 4) 9. 2 (7. 1 to 11. 8) 6. 5 (4. 9 to 8. 6) 0. 84 16. 9 (12. 8 to 22. 3) 15. 9 (12. 0 to 21. 0) 7. 9 (5. 8 to 10. 9) 0. 84 Criterion ↑ SCr by 50% to a minimum peak of 2. 0 mg/dl ↑ SCr ≥ 0. 5 mg/dl with 11. 0 (8. 6 to 14. 0) 10. 5 (8. 2 to 13. 4) 6. 5 (5. 0 to 8. 5) 0. 86 baseline SCr < 2. 0 mg/dl or ↑ SCr ≥ 1. 0 mg/dl with baseline SCr ≥ 2. 0 and < 5. 0 mg/dl N = 2892, 1236, 351, 105, 4060, 1967, 714, 352, and 1160 for respective AKI criteria. Results are relative to those without the change indicated. Multivariable analyses were adjusted for age, gender, DRG weight, and ICD-9 -CM categories of cardiovascular, respiratory, malignant, and infectious diseases. 30 Chertow GM, Burdick E, Honour M et al. J Am Soc Nephrol. 2005; 16: 3365– 70.
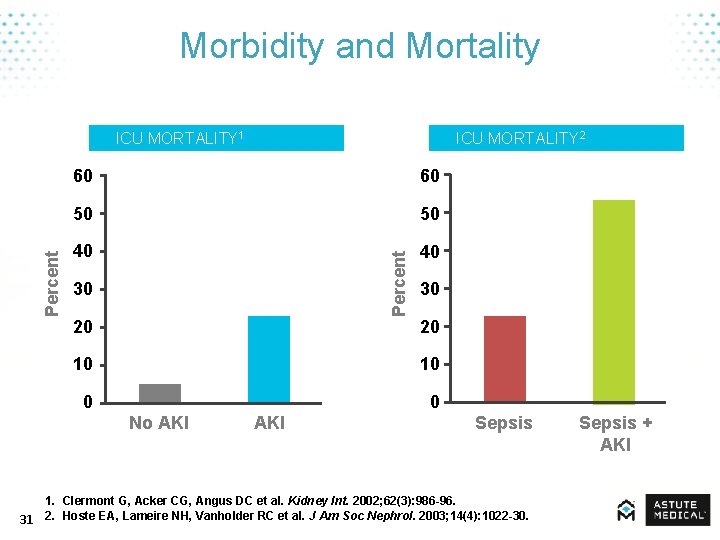
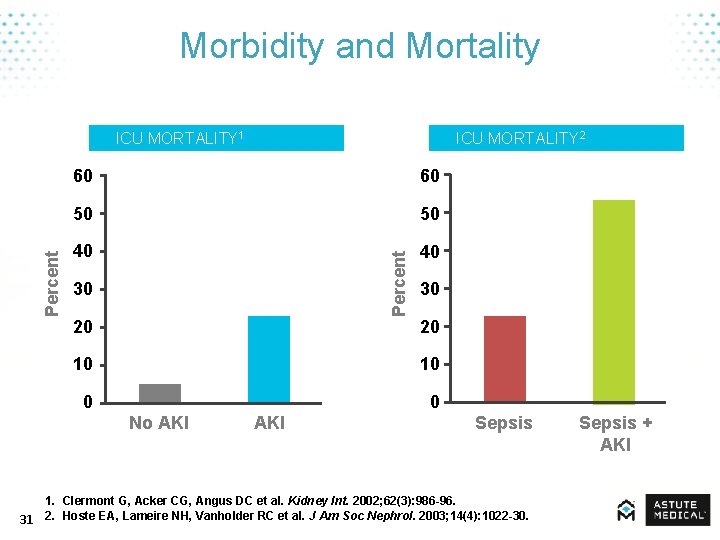
Morbidity and Mortality ICU MORTALITY 2 60 60 50 50 40 40 Percent ICU MORTALITY 1 30 20 10 10 0 0 No AKI Sepsis 1. Clermont G, Acker CG, Angus DC et al. Kidney Int. 2002; 62(3): 986 -96. 31 2. Hoste EA, Lameire NH, Vanholder RC et al. J Am Soc Nephrol. 2003; 14(4): 1022 -30. Sepsis + AKI
Diagnosis, Assessment, & Management 32

Traditional Methods of Measurement 33
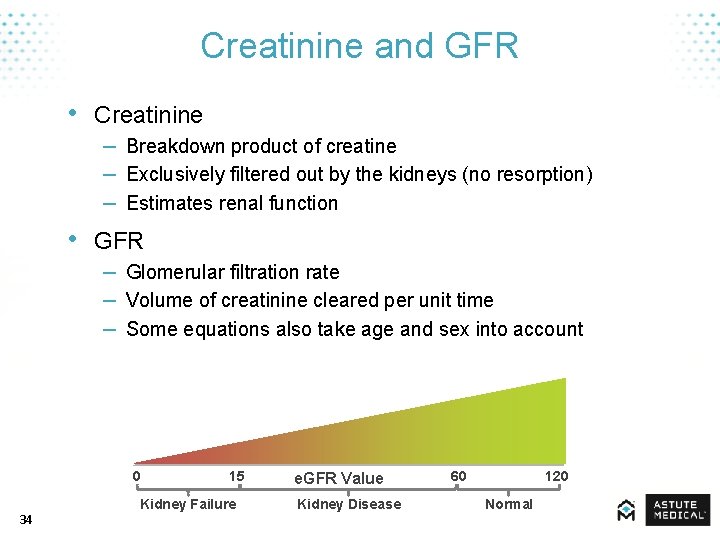
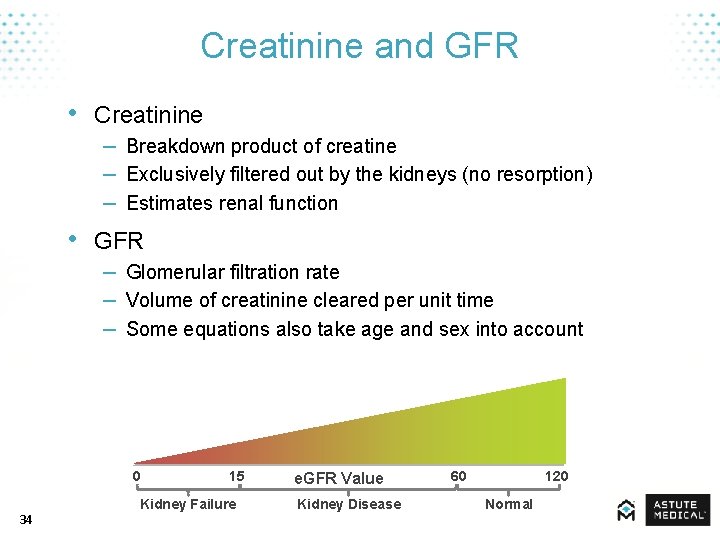
Creatinine and GFR • Creatinine – Breakdown product of creatine – Exclusively filtered out by the kidneys (no resorption) – Estimates renal function • GFR – Glomerular filtration rate – Volume of creatinine cleared per unit time – Some equations also take age and sex into account 0 34 15 Kidney Failure e. GFR Value Kidney Disease 60 120 Normal
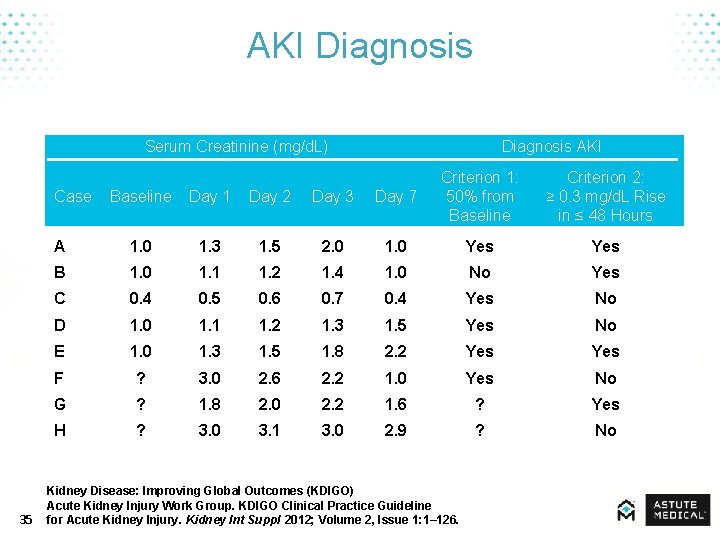
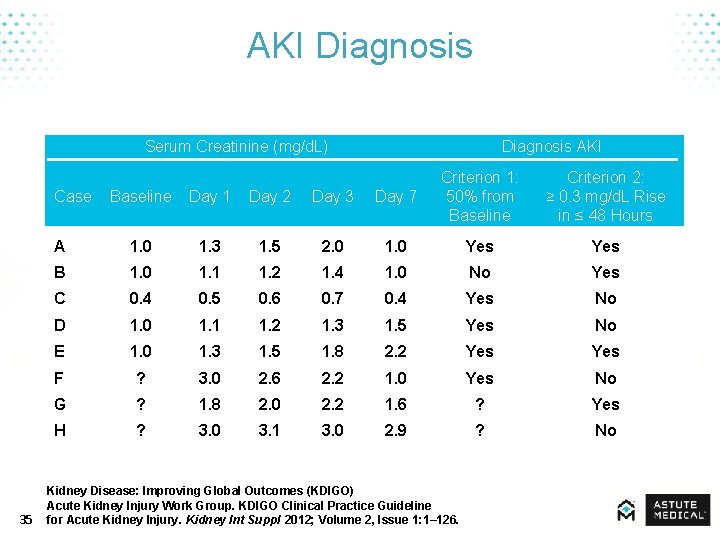
AKI Diagnosis Serum Creatinine (mg/d. L) Baseline Day 1 Day 2 Day 3 Day 7 Criterion 1: 50% from Baseline A 1. 0 1. 3 1. 5 2. 0 1. 0 Yes B 1. 0 1. 1 1. 2 1. 4 1. 0 No Yes C 0. 4 0. 5 0. 6 0. 7 0. 4 Yes No D 1. 0 1. 1 1. 2 1. 3 1. 5 Yes No E 1. 0 1. 3 1. 5 1. 8 2. 2 Yes F ? 3. 0 2. 6 2. 2 1. 0 Yes No G ? 1. 8 2. 0 2. 2 1. 6 ? Yes H ? 3. 0 3. 1 3. 0 2. 9 ? No Case 35 Diagnosis AKI Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2012; Volume 2, Issue 1: 1– 126. Criterion 2: ≥ 0. 3 mg/d. L Rise in ≤ 48 Hours
![Estimated Baseline SCr Age Years 36 Black Males mgd L μmolL Other Males mgd Estimated Baseline SCr Age (Years) 36 Black Males (mg/d. L [μmol/L]) Other Males (mg/d.](https://slidetodoc.com/presentation_image/3397c7e71ad258886721007bd48510a5/image-36.jpg)
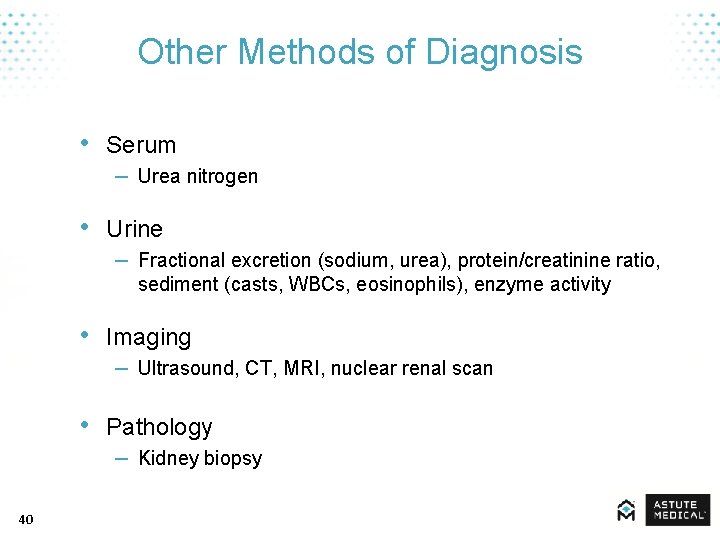
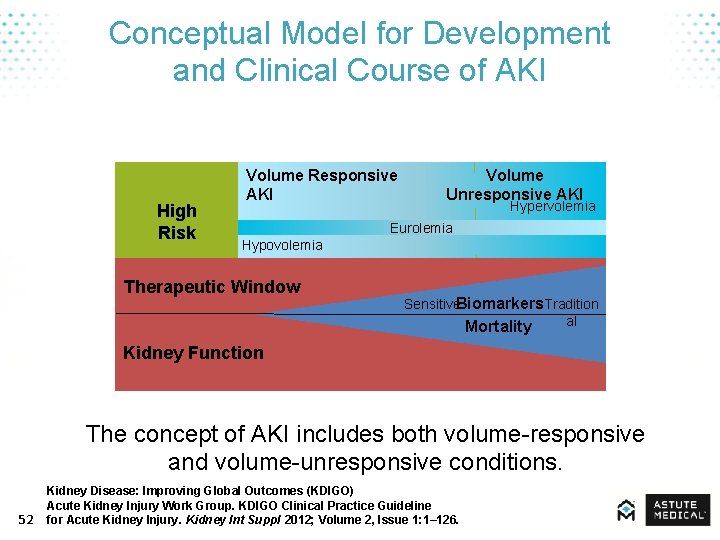
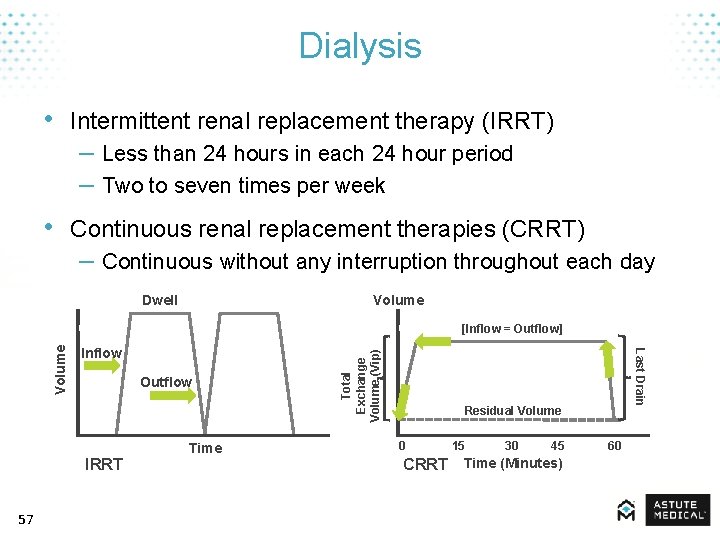
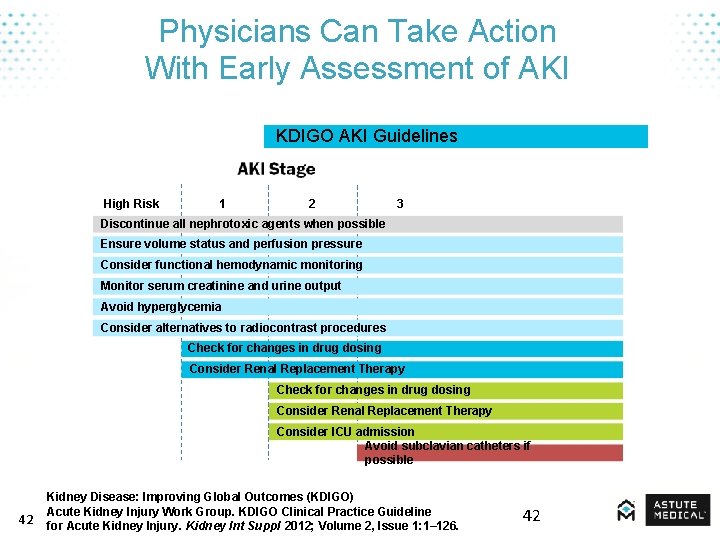
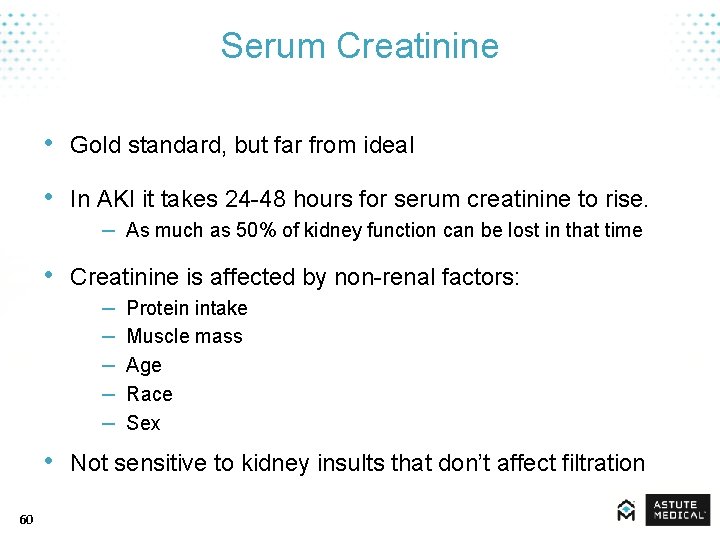
Estimated Baseline SCr Age (Years) 36 Black Males (mg/d. L [μmol/L]) Other Males (mg/d. L [μmol/L]) Black Females (mg/d. L [μmol/L]) Other Females (mg/d. L [μmol/L]) 20 -24 1. 5 (133) 1. 3 (155) 1. 2 (106) 1. 0 (88) 25 -29 1. 5 (133) 1. 2 (106) 1. 1 (97) 1. 0 (88) 30 -39 1. 4 (124) 1. 2 (106) 1. 1 (97) 0. 9 (80) 40 -54 1. 3 (115) 1. 1 (97) 1. 0 (88) 0. 9 (80) 55 -65 1. 3 (155) 1. 1 (97) 1. 0 (88) 0. 8 (71) > 65 1. 2 (106) 1. 0 (88) 0. 9 (80) 0. 8 (71) Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2012; Volume 2, Issue 1: 1– 126.
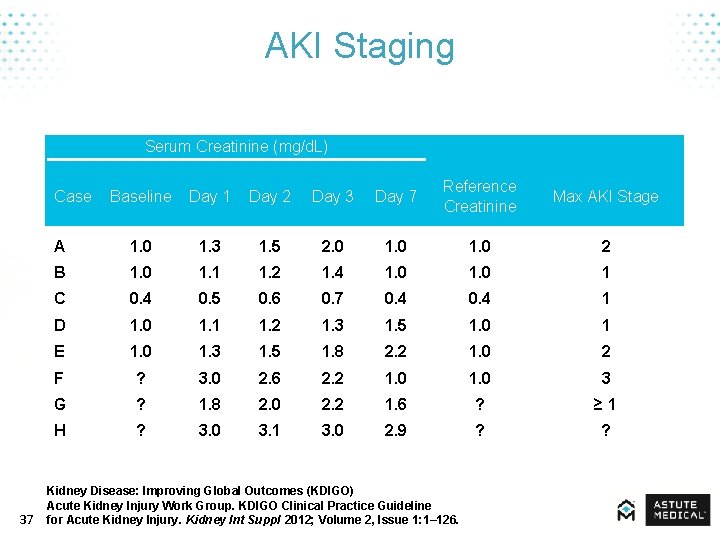
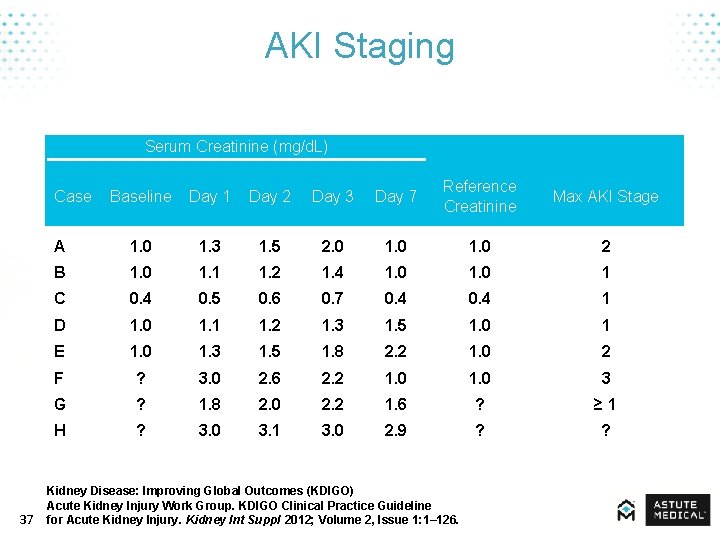
AKI Staging Serum Creatinine (mg/d. L) Baseline Day 1 Day 2 Day 3 Day 7 Reference Creatinine Max AKI Stage A 1. 0 1. 3 1. 5 2. 0 1. 0 2 B 1. 0 1. 1 1. 2 1. 4 1. 0 1 C 0. 4 0. 5 0. 6 0. 7 0. 4 1 D 1. 0 1. 1 1. 2 1. 3 1. 5 1. 0 1 E 1. 0 1. 3 1. 5 1. 8 2. 2 1. 0 2 F ? 3. 0 2. 6 2. 2 1. 0 3 G ? 1. 8 2. 0 2. 2 1. 6 ? ≥ 1 H ? 3. 0 3. 1 3. 0 2. 9 ? ? Case 37 Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2012; Volume 2, Issue 1: 1– 126.
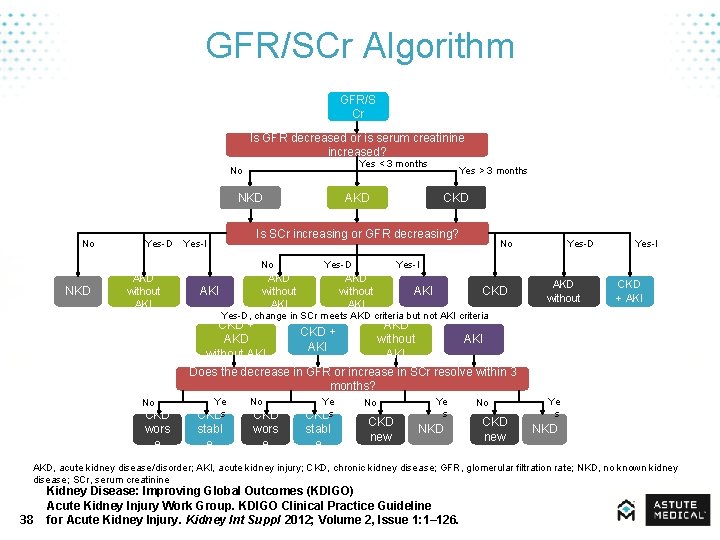
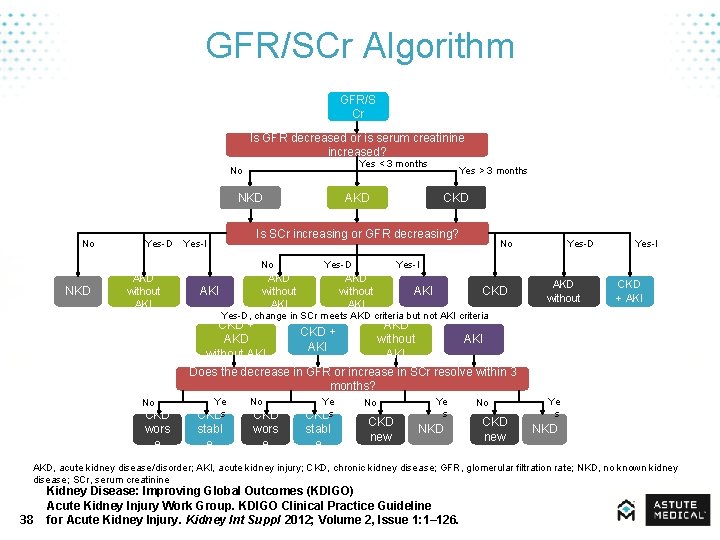
GFR/SCr Algorithm GFR/S Cr Is GFR decreased or is serum creatinine increased? Yes < 3 months No NKD No Yes-D Yes-I NKD AKI CKD Is SCr increasing or GFR decreasing? No AKD without AKI AKD Yes > 3 months Yes-D AKD without AKI No Yes-I AKD without AKI CKD Yes-D, change in SCr meets AKD criteria but not AKI criteria CKD + AKD without AKI CKD + AKI AKD without AKI Yes-D CKD + AKD without AKI Yes-I CKD + AKI Does the decrease in GFR or increase in SCr resolve within 3 months? Ye Ye RRT, renal replacement therapy; MICU, medical intensive care unit; NROF, non-renal organ failure. No No s s CKD CKD s CKD NKD wors stabl new e e AKD, acute kidney disease/disorder; AKI, acute kidney injury; CKD, chronic kidney disease; GFR, glomerular filtration rate; NKD, no known kidney disease; SCr, serum creatinine 38 Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2012; Volume 2, Issue 1: 1– 126.
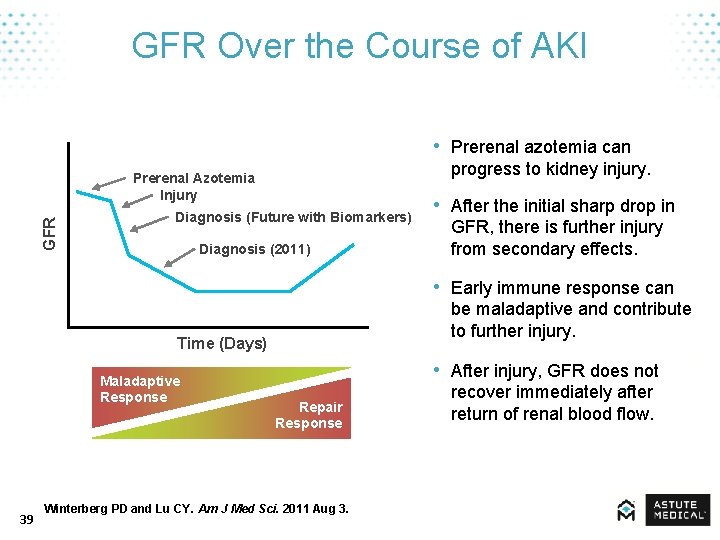
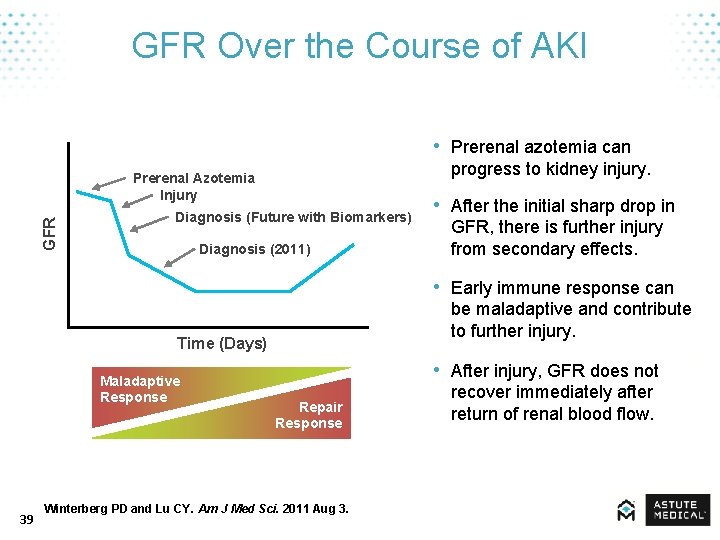
GFR Over the Course of AKI • Prerenal azotemia can progress to kidney injury. GFR Prerenal Azotemia Injury Diagnosis (Future with Biomarkers) Diagnosis (2011) • After the initial sharp drop in GFR, there is further injury from secondary effects. • Early immune response can be maladaptive and contribute to further injury. Time (Days) Maladaptive Response 39 • After injury, GFR does not Repair Response Winterberg PD and Lu CY. Am J Med Sci. 2011 Aug 3. recover immediately after return of renal blood flow.
Other Methods of Diagnosis • Serum – Urea nitrogen • Urine – Fractional excretion (sodium, urea), protein/creatinine ratio, sediment (casts, WBCs, eosinophils), enzyme activity • Imaging – Ultrasound, CT, MRI, nuclear renal scan • Pathology – Kidney biopsy 40
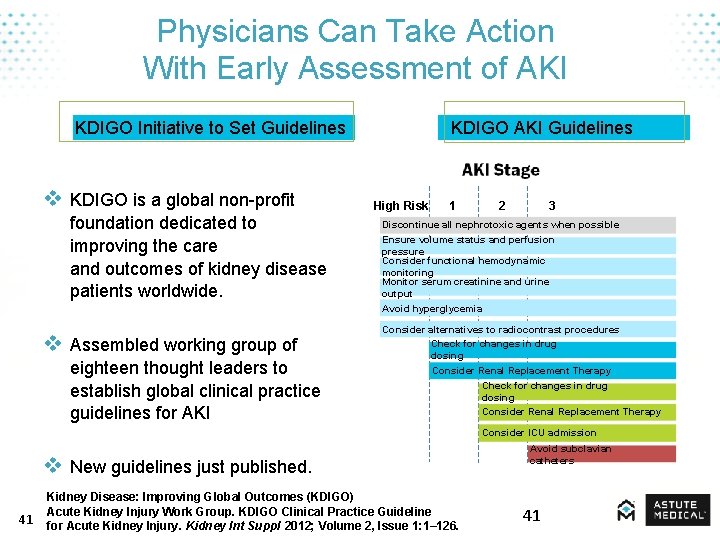
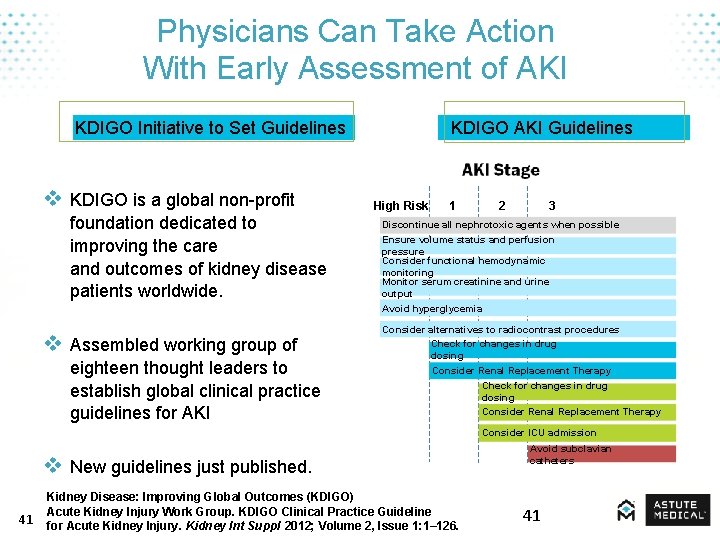
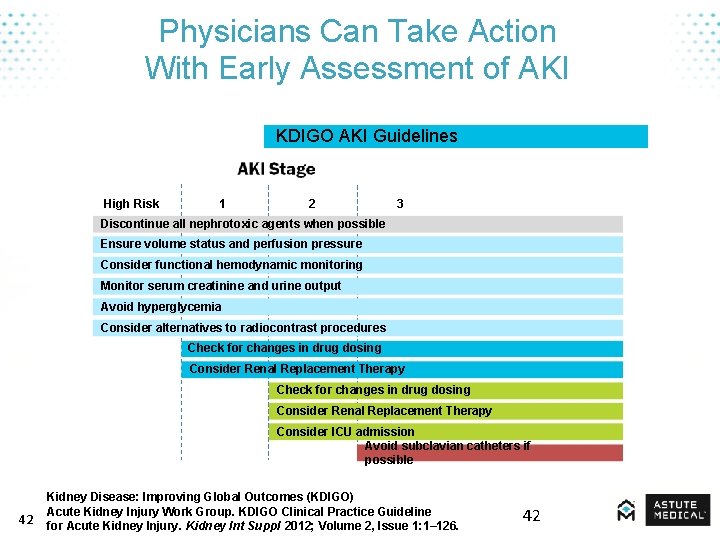
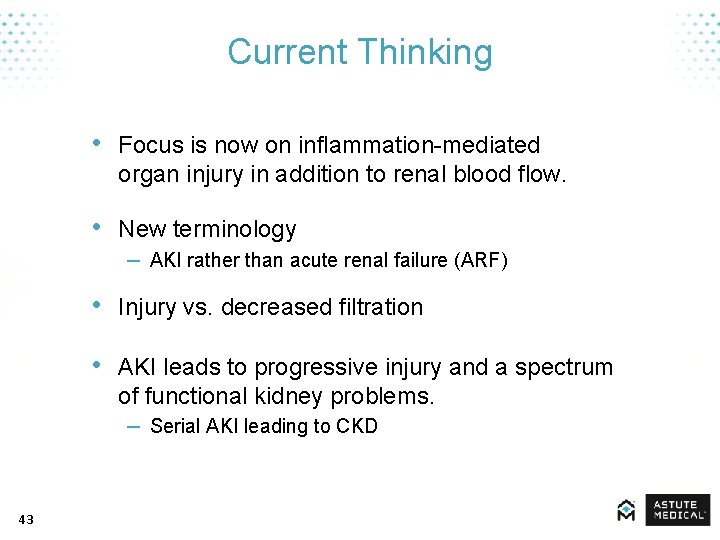
Physicians Can Take Action With Early Assessment of AKI KDIGO Initiative to Set Guidelines v KDIGO is a global non-profit foundation dedicated to improving the care and outcomes of kidney disease patients worldwide. v Assembled working group of eighteen thought leaders to establish global clinical practice guidelines for AKI KDIGO AKI Guidelines High Risk 1 2 3 Discontinue all nephrotoxic agents when possible Ensure volume status and perfusion pressure Consider functional hemodynamic monitoring Monitor serum creatinine and urine output Avoid hyperglycemia Consider alternatives to radiocontrast procedures Check for changes in drug dosing Consider Renal Replacement Therapy Consider ICU admission v New guidelines just published. 41 Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2012; Volume 2, Issue 1: 1– 126. Avoid subclavian catheters 41
Physicians Can Take Action With Early Assessment of AKI KDIGO AKI Guidelines High Risk 1 2 3 Discontinue all nephrotoxic agents when possible Ensure volume status and perfusion pressure Consider functional hemodynamic monitoring Monitor serum creatinine and urine output Avoid hyperglycemia Consider alternatives to radiocontrast procedures Check for changes in drug dosing Consider Renal Replacement Therapy Consider ICU admission Avoid subclavian catheters if possible 42 Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2012; Volume 2, Issue 1: 1– 126. 42
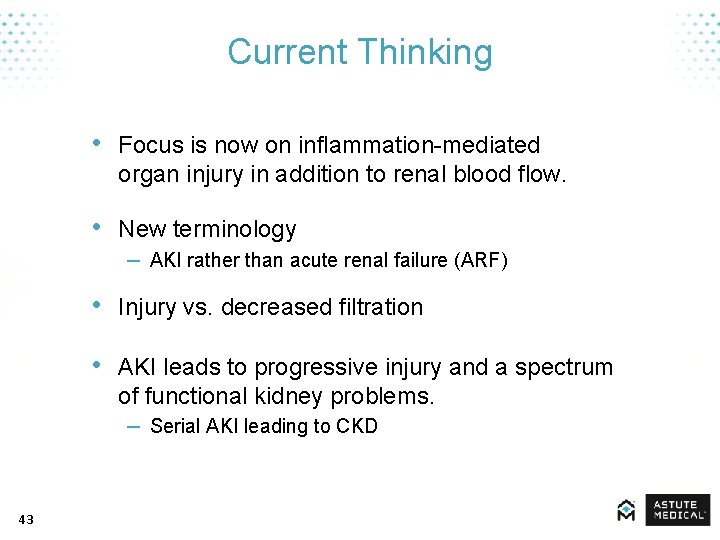
Current Thinking • Focus is now on inflammation-mediated organ injury in addition to renal blood flow. • New terminology – AKI rather than acute renal failure (ARF) • Injury vs. decreased filtration • AKI leads to progressive injury and a spectrum of functional kidney problems. – Serial AKI leading to CKD 43
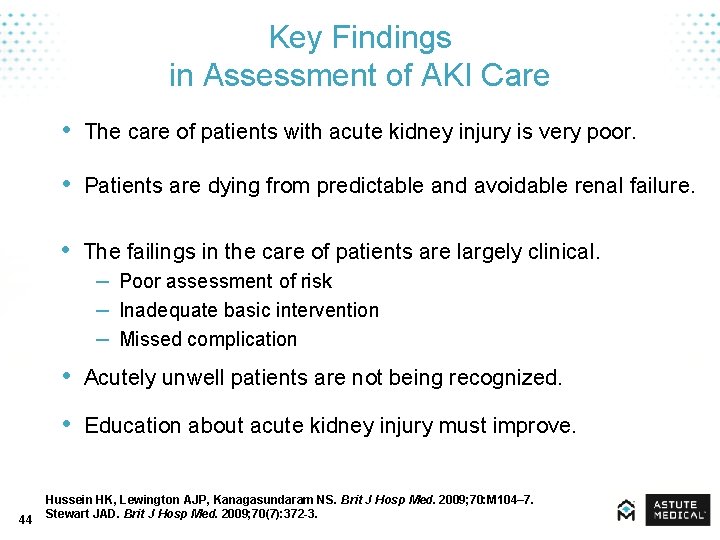
Key Findings in Assessment of AKI Care • The care of patients with acute kidney injury is very poor. • Patients are dying from predictable and avoidable renal failure. • The failings in the care of patients are largely clinical. – Poor assessment of risk – Inadequate basic intervention – Missed complication • Acutely unwell patients are not being recognized. • Education about acute kidney injury must improve. 44 Hussein HK, Lewington AJP, Kanagasundaram NS. Brit J Hosp Med. 2009; 70: M 104– 7. Stewart JAD. Brit J Hosp Med. 2009; 70(7): 372 -3.
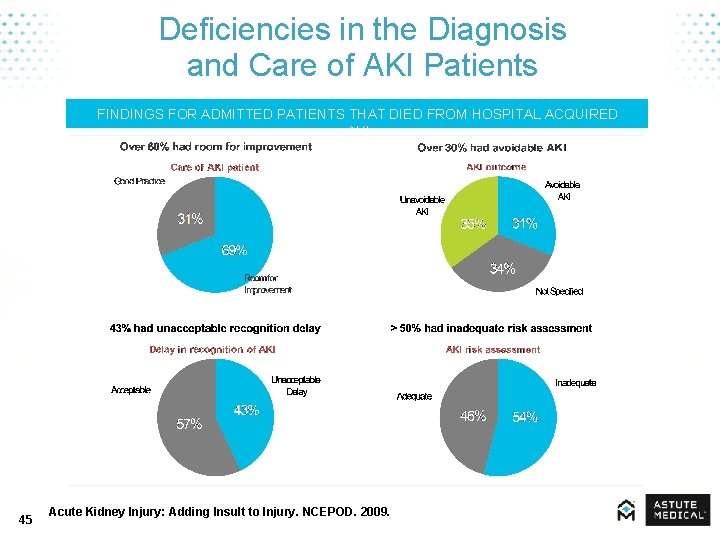
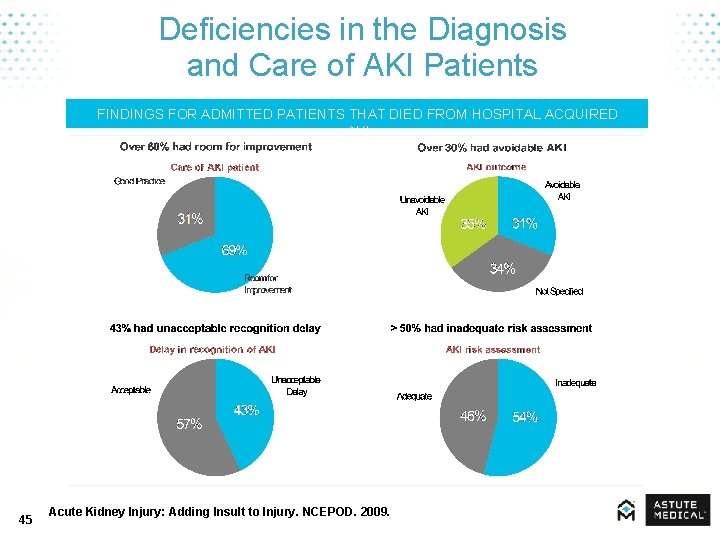
Deficiencies in the Diagnosis and Care of AKI Patients FINDINGS FOR ADMITTED PATIENTS THAT DIED FROM HOSPITAL ACQUIRED AKI 45 Acute Kidney Injury: Adding Insult to Injury. NCEPOD. 2009.
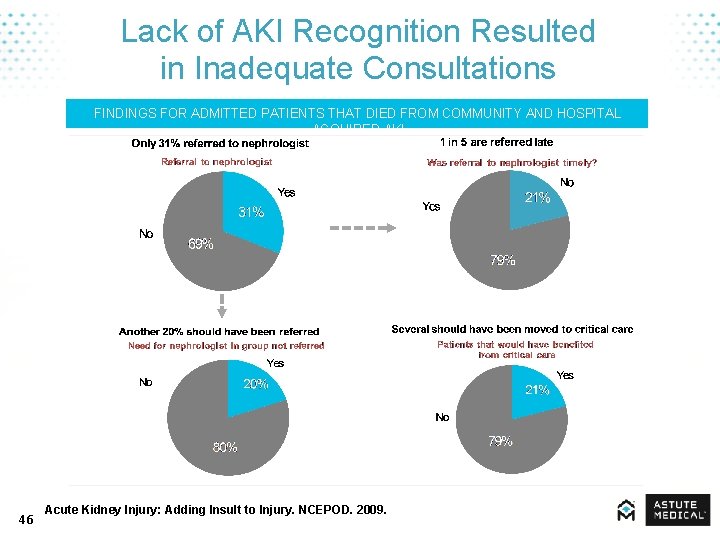
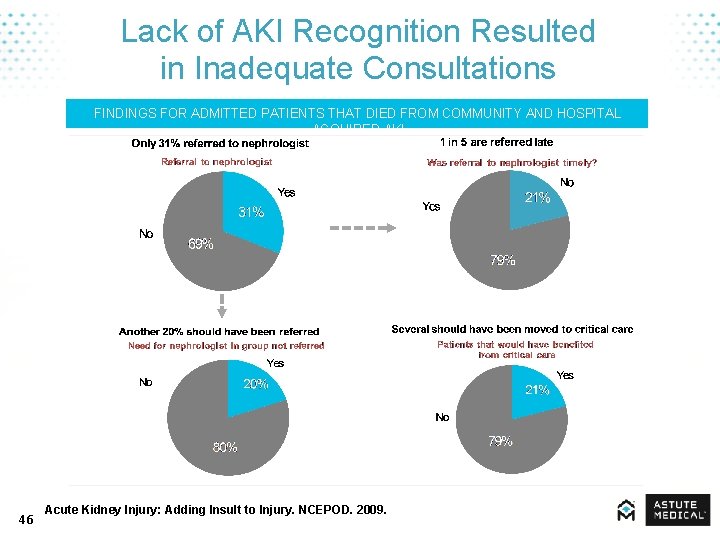
Lack of AKI Recognition Resulted in Inadequate Consultations FINDINGS FOR ADMITTED PATIENTS THAT DIED FROM COMMUNITY AND HOSPITAL ACQUIRED AKI 46 Acute Kidney Injury: Adding Insult to Injury. NCEPOD. 2009.
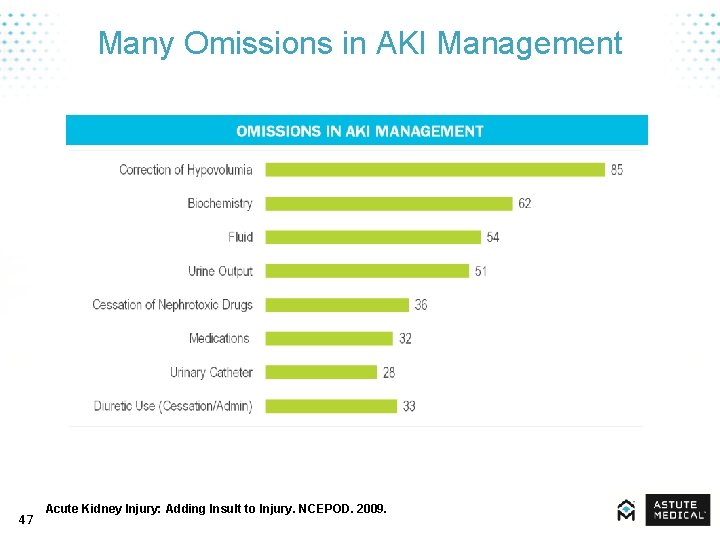
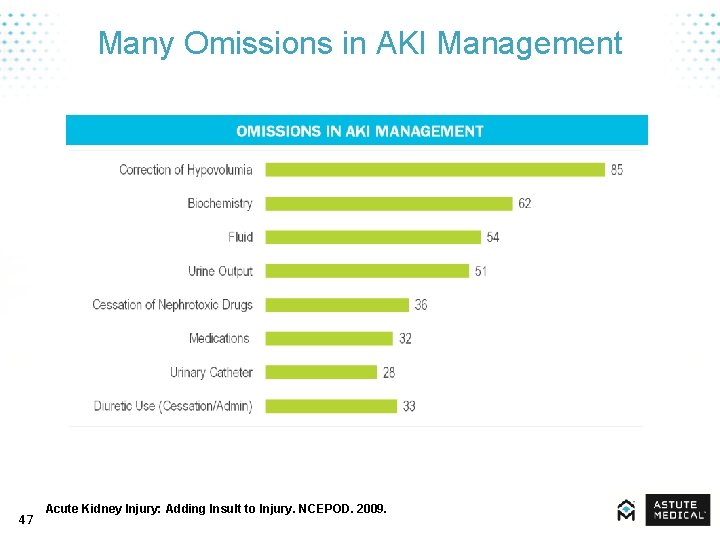
Many Omissions in AKI Management 47 Acute Kidney Injury: Adding Insult to Injury. NCEPOD. 2009.
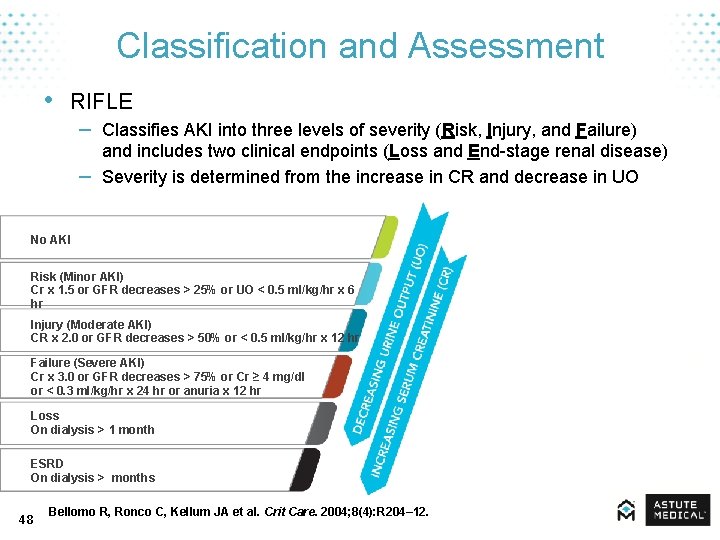
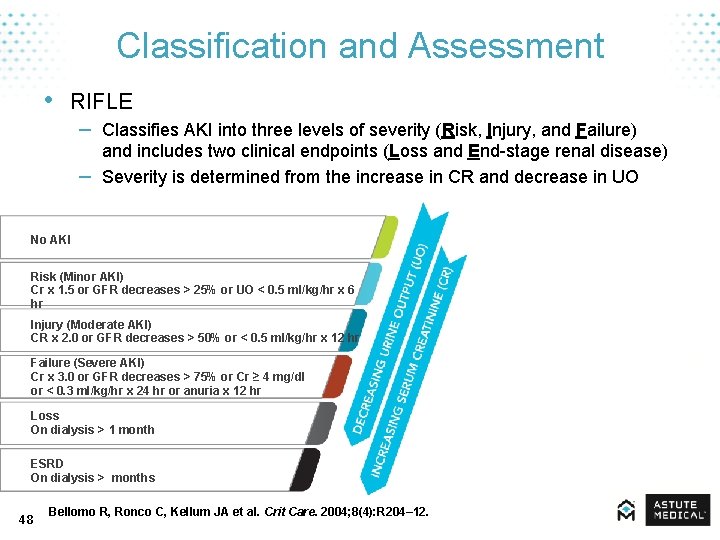
Classification and Assessment • RIFLE – Classifies AKI into three levels of severity (Risk, Injury, and Failure) – and includes two clinical endpoints (Loss and End-stage renal disease) Severity is determined from the increase in CR and decrease in UO No AKI Risk (Minor AKI) Cr x 1. 5 or GFR decreases > 25% or UO < 0. 5 ml/kg/hr x 6 hr Injury (Moderate AKI) CR x 2. 0 or GFR decreases > 50% or < 0. 5 ml/kg/hr x 12 hr Failure (Severe AKI) Cr x 3. 0 or GFR decreases > 75% or Cr ≥ 4 mg/dl or < 0. 3 ml/kg/hr x 24 hr or anuria x 12 hr Loss On dialysis > 1 month ESRD On dialysis > months 48 Bellomo R, Ronco C, Kellum JA et al. Crit Care. 2004; 8(4): R 204– 12.
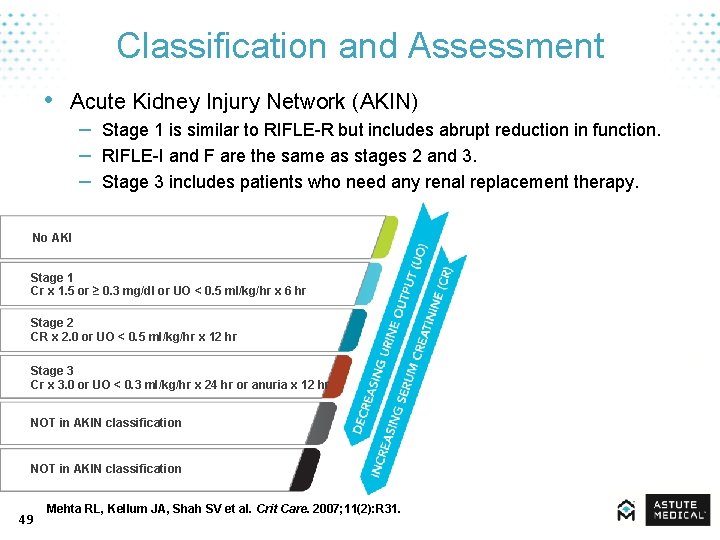
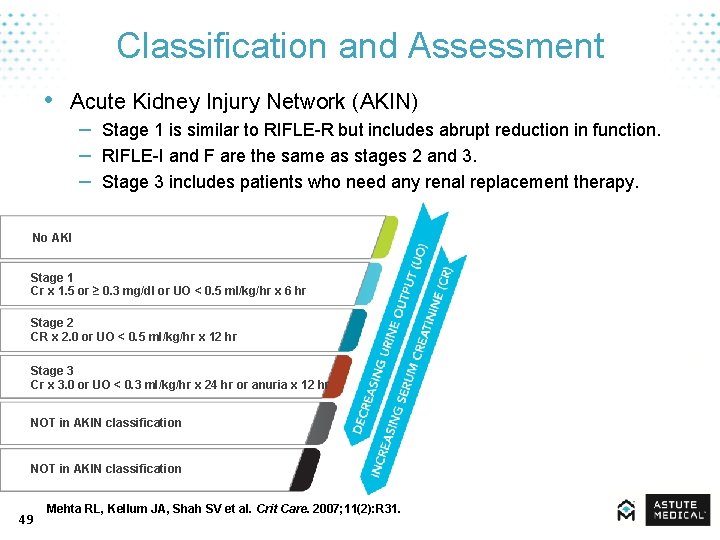
Classification and Assessment • Acute Kidney Injury Network (AKIN) – Stage 1 is similar to RIFLE-R but includes abrupt reduction in function. – RIFLE-I and F are the same as stages 2 and 3. – Stage 3 includes patients who need any renal replacement therapy. No AKI Stage 1 Cr x 1. 5 or ≥ 0. 3 mg/dl or UO < 0. 5 ml/kg/hr x 6 hr Stage 2 CR x 2. 0 or UO < 0. 5 ml/kg/hr x 12 hr Stage 3 Cr x 3. 0 or UO < 0. 3 ml/kg/hr x 24 hr or anuria x 12 hr NOT in AKIN classification 49 Mehta RL, Kellum JA, Shah SV et al. Crit Care. 2007; 11(2): R 31.
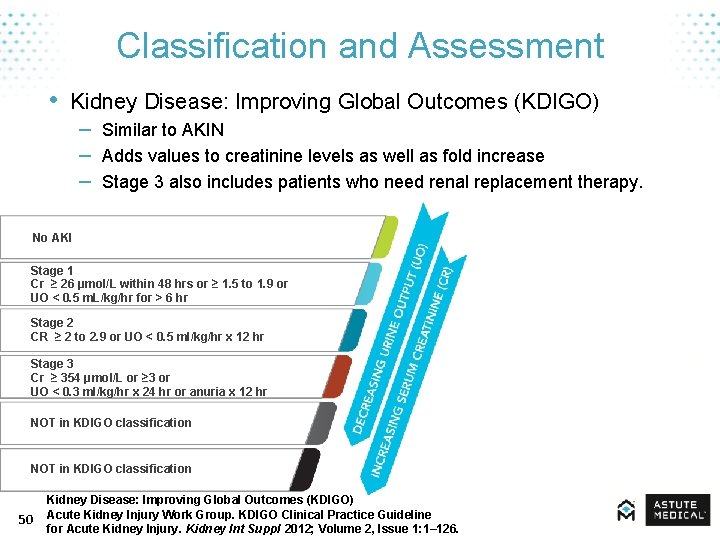
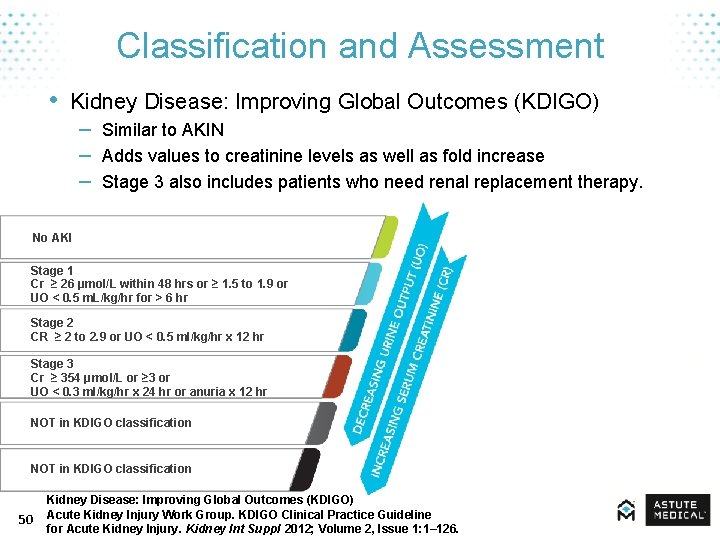
Classification and Assessment • Kidney Disease: Improving Global Outcomes (KDIGO) – Similar to AKIN – Adds values to creatinine levels as well as fold increase – Stage 3 also includes patients who need renal replacement therapy. No AKI Stage 1 Cr ≥ 26 μmol/L within 48 hrs or ≥ 1. 5 to 1. 9 or UO < 0. 5 m. L/kg/hr for > 6 hr Stage 2 CR ≥ 2 to 2. 9 or UO < 0. 5 ml/kg/hr x 12 hr Stage 3 Cr ≥ 354 μmol/L or ≥ 3 or UO < 0. 3 ml/kg/hr x 24 hr or anuria x 12 hr NOT in KDIGO classification 50 Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2012; Volume 2, Issue 1: 1– 126.
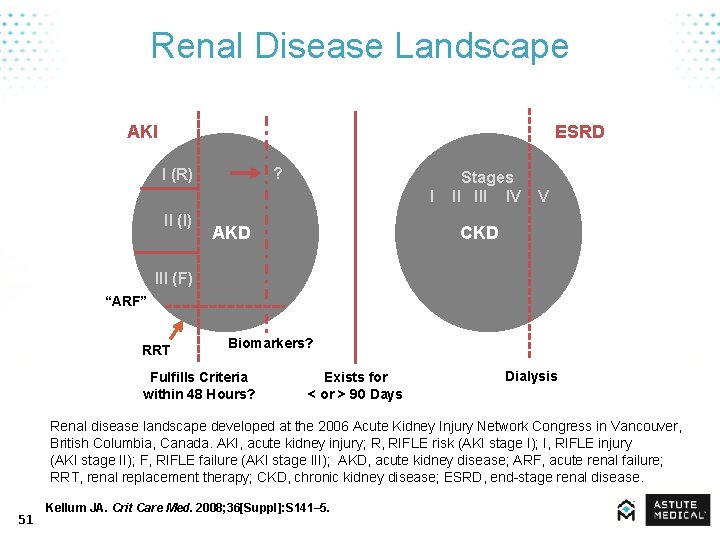
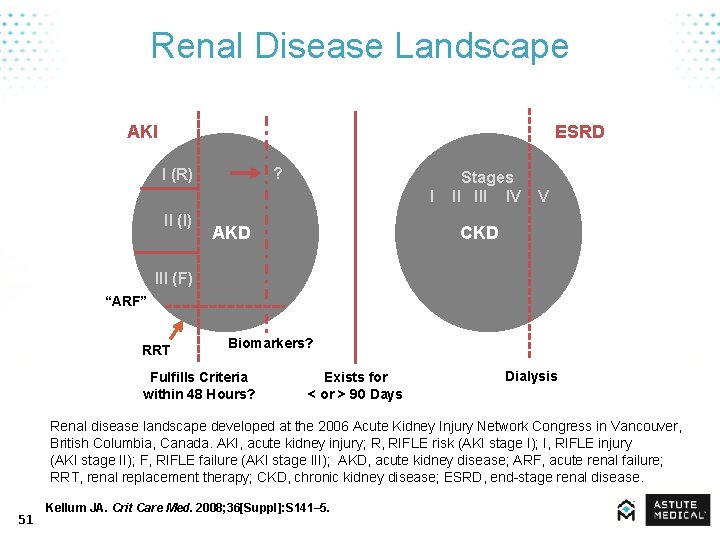
Renal Disease Landscape AKI ESRD ? I (R) II (I) Stages I III IV V AKD CKD III (F) “ARF” RRT Biomarkers? Fulfills Criteria within 48 Hours? Exists for < or > 90 Days Dialysis Renal disease landscape developed at the 2006 Acute Kidney Injury Network Congress in Vancouver, British Columbia, Canada. AKI, acute kidney injury; R, RIFLE risk (AKI stage I); I, RIFLE injury (AKI stage II); F, RIFLE failure (AKI stage III); AKD, acute kidney disease; ARF, acute renal failure; RRT, renal replacement therapy; CKD, chronic kidney disease; ESRD, end-stage renal disease. 51 Kellum JA. Crit Care Med. 2008; 36[Suppl]: S 141– 5.
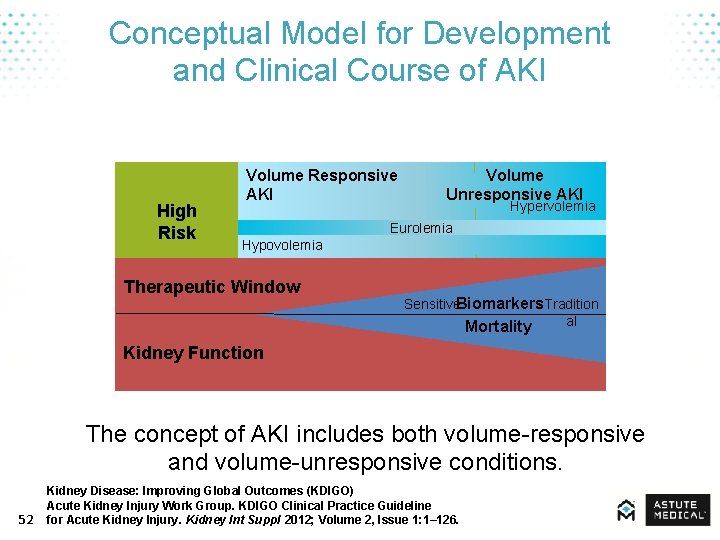
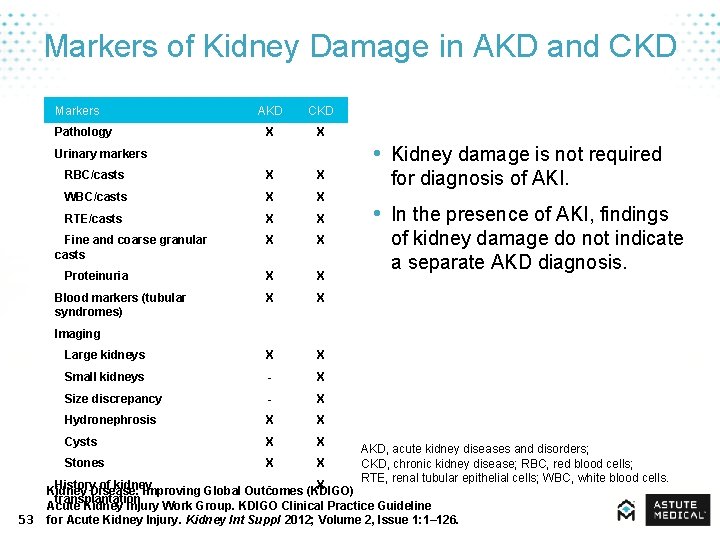
Conceptual Model for Development and Clinical Course of AKI High Risk Volume Responsive AKI Volume Unresponsive AKI Hypervolemia Eurolemia Hypovolemia Therapeutic Window Sensitive. Biomarkers Tradition al Mortality Kidney Function The concept of AKI includes both volume-responsive and volume-unresponsive conditions. 52 Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2012; Volume 2, Issue 1: 1– 126.
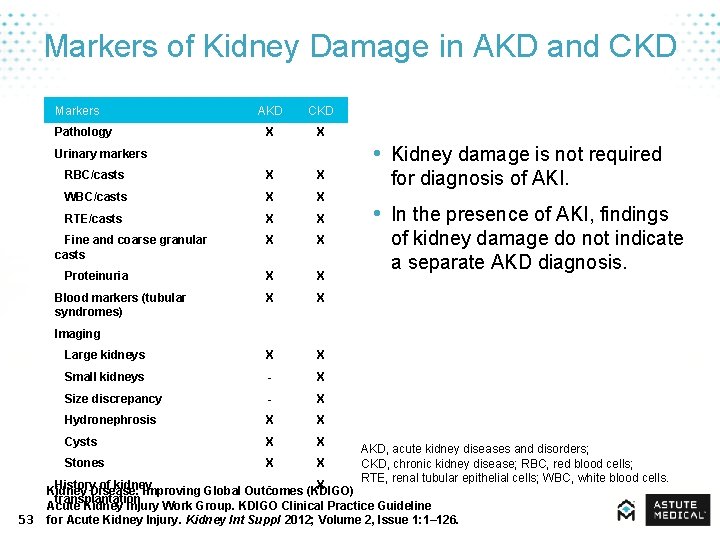
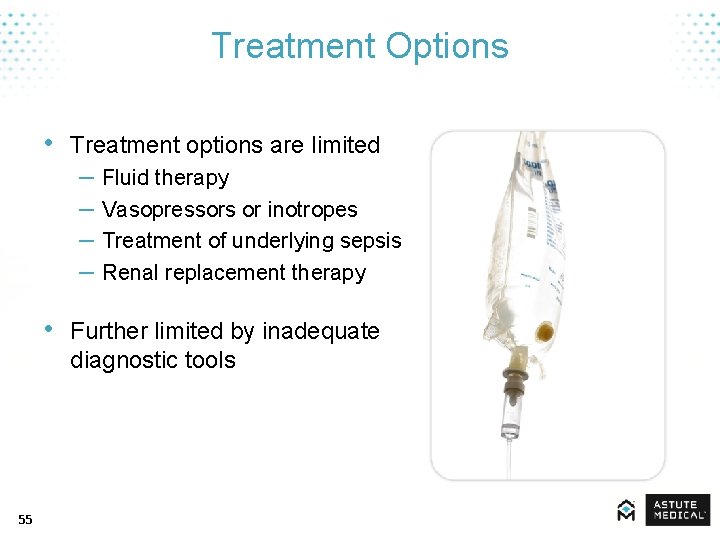
Markers of Kidney Damage in AKD and CKD Markers Pathology AKD CKD X X • Kidney damage is not required Urinary markers RBC/casts X X WBC/casts X X RTE/casts X X Fine and coarse granular casts X X Proteinuria X X Blood markers (tubular syndromes) X X Large kidneys X X Small kidneys - X Size discrepancy - X Hydronephrosis X X Cysts X X Stones X X for diagnosis of AKI. • In the presence of AKI, findings of kidney damage do not indicate a separate AKD diagnosis. Imaging 53 AKD, acute kidney diseases and disorders; CKD, chronic kidney disease; RBC, red blood cells; RTE, renal tubular epithelial cells; WBC, white blood cells. History of kidney X Kidney Disease: Improving Global Outcomes (KDIGO) transplantation Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2012; Volume 2, Issue 1: 1– 126.

Treatment 54
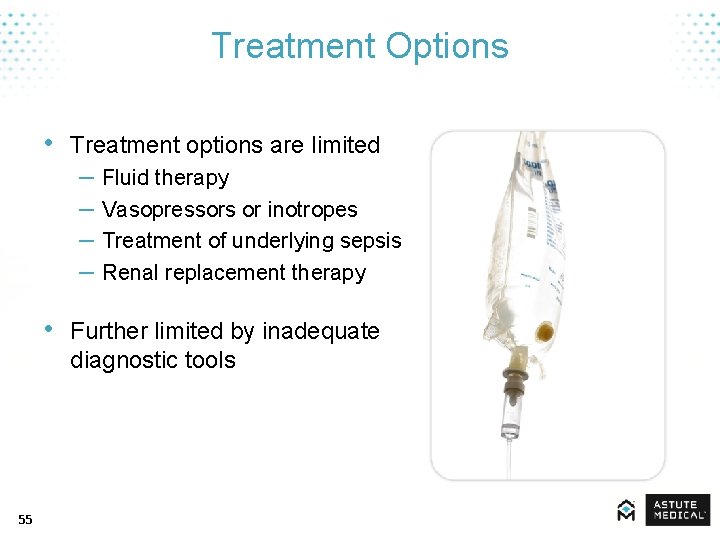
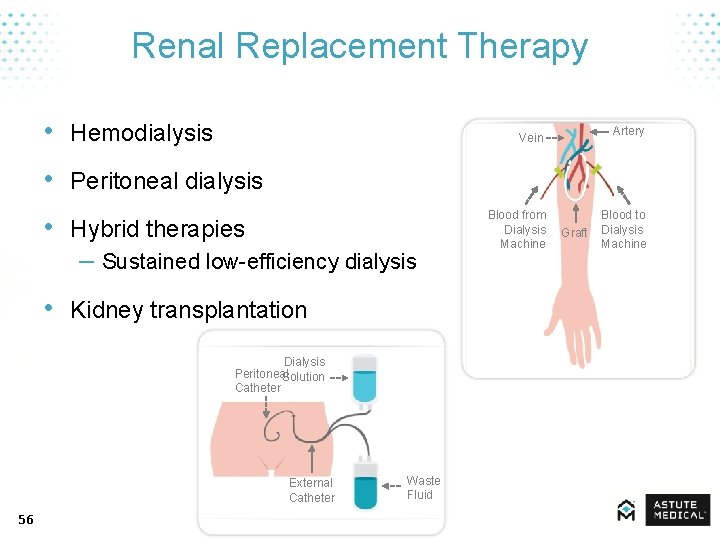
Treatment Options • Treatment options are limited – Fluid therapy – Vasopressors or inotropes – Treatment of underlying sepsis – Renal replacement therapy • Further limited by inadequate diagnostic tools 55
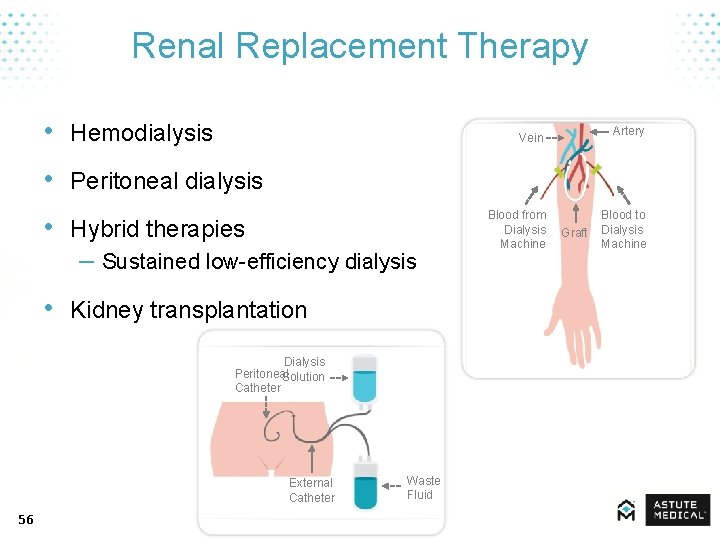
Renal Replacement Therapy • Hemodialysis Artery Vein • Peritoneal dialysis • Hybrid therapies – Sustained low-efficiency dialysis • Kidney transplantation Dialysis Peritoneal Solution Catheter External Catheter 56 Waste Fluid Blood from Dialysis Machine Graft Blood to Dialysis Machine
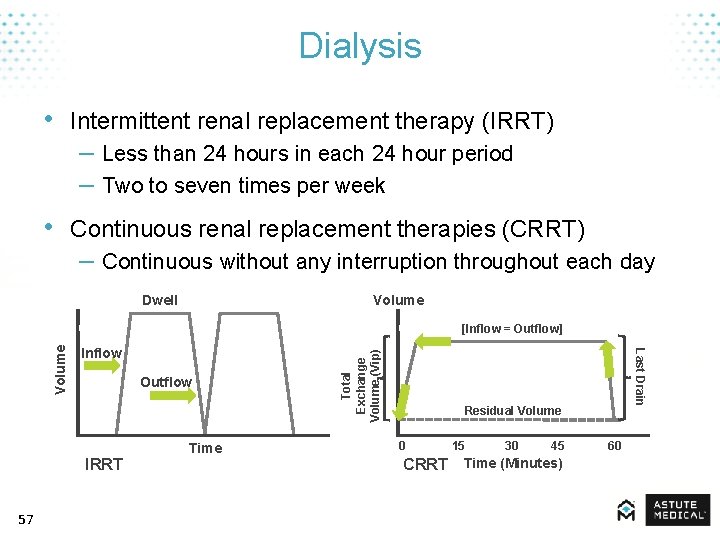
Dialysis • Intermittent renal replacement therapy (IRRT) – Less than 24 hours in each 24 hour period – Two to seven times per week • Continuous renal replacement therapies (CRRT) – Continuous without any interruption throughout each day Volume Dwell Outflow IRRT 57 Time Total Exchange Volume (Vip) Inflow Residual Volume 0 15 30 45 60 CRRT Time (Minutes) Last Drain Volume [Inflow = Outflow]
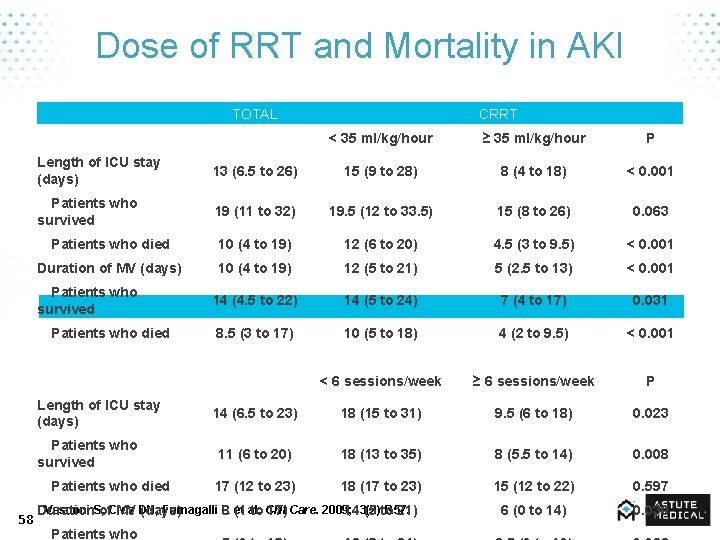
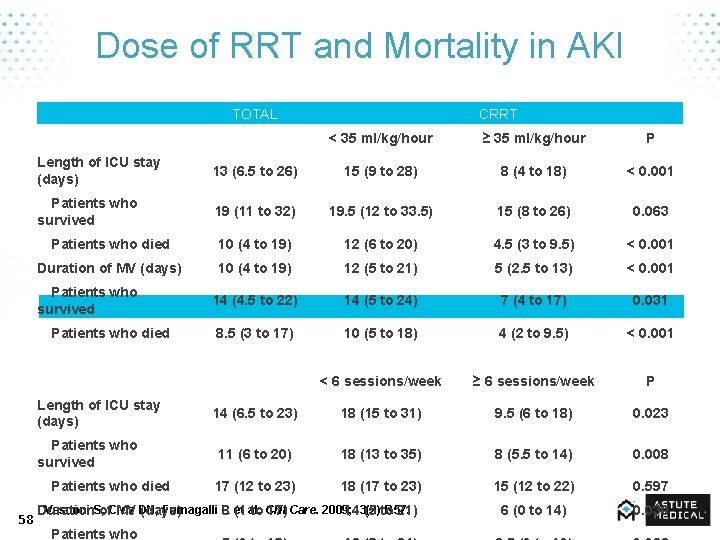
Dose of RRT and Mortality in AKI TOTAL CRRT < 35 ml/kg/hour ≥ 35 ml/kg/hour P Length of ICU stay (days) 13 (6. 5 to 26) 15 (9 to 28) 8 (4 to 18) < 0. 001 Patients who survived 19 (11 to 32) 19. 5 (12 to 33. 5) 15 (8 to 26) 0. 063 Patients who died 10 (4 to 19) 12 (6 to 20) 4. 5 (3 to 9. 5) < 0. 001 Duration of MV (days) 10 (4 to 19) 12 (5 to 21) 5 (2. 5 to 13) < 0. 001 Patients who survived 14 (4. 5 to 22) 14 (5 to 24) 7 (4 to 17) 0. 031 Patients who died 8. 5 (3 to 17) 10 (5 to 18) 4 (2 to 9. 5) < 0. 001 TOTAL < 6 sessions/week ≥ 6 sessions/week P 14 (6. 5 to 23) 18 (15 to 31) 9. 5 (6 to 18) 0. 023 Patients who survived 11 (6 to 20) 18 (13 to 35) 8 (5. 5 to 14) 0. 008 Patients who died 17 (12 to 23) 18 (17 to 23) 15 (12 to 22) 0. 597 6 (0 to 14) 0. 030 Length of ICU stay (days) 58 IRRT Vesconi S, Cruz DN, Fumagalli R et al. Crit Duration of MV (days) 8 (1 to 17) Care. 2009; 13(2): R 57. 14 (5 to 21) Patients who

Limitations & Unmet Needs 59
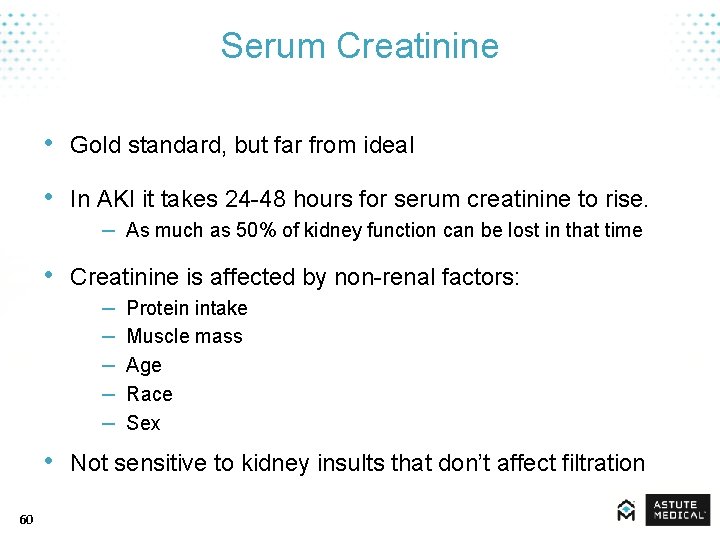
Serum Creatinine • Gold standard, but far from ideal • In AKI it takes 24 -48 hours for serum creatinine to rise. – As much as 50% of kidney function can be lost in that time • Creatinine is affected by non-renal factors: – Protein intake – Muscle mass – Age – Race – Sex • Not sensitive to kidney insults that don’t affect filtration 60
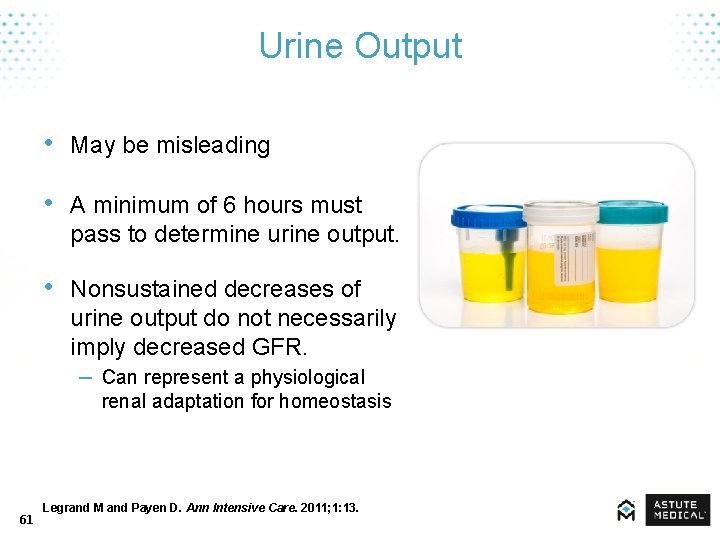
Urine Output • May be misleading • A minimum of 6 hours must pass to determine urine output. • Nonsustained decreases of urine output do not necessarily imply decreased GFR. – Can represent a physiological renal adaptation for homeostasis 61 Legrand M and Payen D. Ann Intensive Care. 2011; 1: 13.
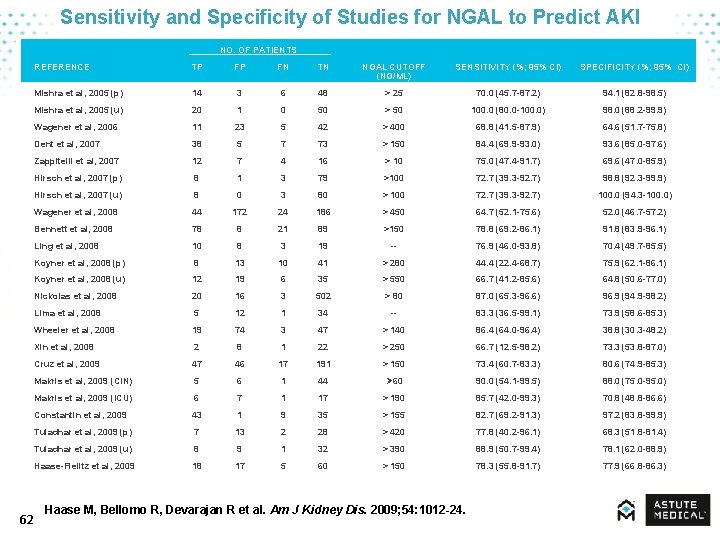
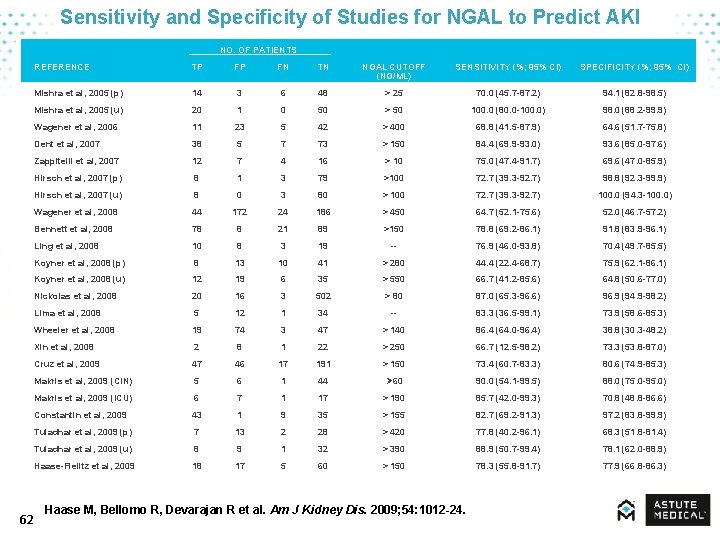
Sensitivity and Specificity of Studies for NGAL to Predict AKI NO. OF PATIENTS 62 REFERENCE TP FP FN TN NGAL CUTOFF (NG/ML) SENSITIVITY (%; 95% CI) SPECIFICITY (%; 95% CI) Mishra et al, 2005 (p) 14 3 6 48 > 25 70. 0 (45. 7 -87. 2) 94. 1 (82. 8 -98. 5) Mishra et al, 2005 (u) 20 1 0 50 > 50 100. 0 (80. 0 -100. 0) 98. 0 (88. 2 -99. 9) Wagener et al, 2006 11 23 5 42 > 400 68. 8 (41. 5 -87. 9) 64. 6 (51. 7 -75. 8) Dent et al, 2007 38 5 7 73 > 150 84. 4 (69. 9 -93. 0) 93. 6 (85. 0 -97. 6) Zappitelli et al, 2007 12 7 4 16 > 10 75. 0 (47. 4 -91. 7) 69. 6 (47. 0 -85. 9) Hirsch et al, 2007 (p) 8 1 3 79 >100 72. 7 (39. 3 -92. 7) 98. 8 (92. 3 -99. 9) Hirsch et al, 2007 (u) 8 0 3 80 > 100 72. 7 (39. 3 -92. 7) 100. 0 (94. 3 -100. 0) Wagener et al, 2008 44 172 24 186 > 450 64. 7 (52. 1 -75. 6) 52. 0 (46. 7 -57. 2) Bennett et al, 2008 78 8 21 89 >150 78. 8 (69. 2 -86. 1) 91. 8 (83. 9 -96. 1) Ling et al, 2008 10 8 3 19 -- 76. 9 (46. 0 -93. 8) 70. 4 (49. 7 -85. 5) Koyner et al, 2008 (p) 8 13 10 41 > 280 44. 4 (22. 4 -68. 7) 75. 9 (62. 1 -86. 1) Koyner et al, 2008 (u) 12 19 6 35 > 550 66. 7 (41. 2 -85. 6) 64. 8 (50. 6 -77. 0) Nickolas et al, 2008 20 16 3 502 > 80 87. 0 (65. 3 -96. 6) 96. 9 (94. 9 -98. 2) Lima et al, 2008 5 12 1 34 -- 83. 3 (36. 5 -99. 1) 73. 9 (58. 6 -85. 3) Wheeler et al, 2008 19 74 3 47 > 140 86. 4 (64. 0 -96. 4) 38. 8 (30. 3 -48. 2) Xin et al, 2008 2 8 1 22 > 250 66. 7 (12. 5 -98. 2) 73. 3 (53. 8 -87. 0) Cruz et al, 2009 47 46 17 191 > 150 73. 4 (60. 7 -83. 3) 80. 6 (74. 9 -85. 3) Makris et al, 2009 (CIN) 5 6 1 44 Ø 60 90. 0 (54. 1 -99. 5) 88. 0 (75. 0 -95. 0) Makris et al, 2009 (ICU) 6 7 1 17 > 190 85. 7 (42. 0 -99. 3) 70. 8 (48. 8 -86. 6) Constantin et al, 2009 43 1 9 35 > 155 82. 7 (69. 2 -91. 3) 97. 2 (83. 8 -99. 9) Tuladhar et al, 2009 (p) 7 13 2 28 > 420 77. 8 (40. 2 -96. 1) 68. 3 (51. 8 -81. 4) Tuladhar et al, 2009 (u) 8 9 1 32 > 390 88. 9 (50. 7 -99. 4) 78. 1 (62. 0 -88. 9) Haase-Fielitz et al, 2009 18 17 5 60 > 150 78. 3 (55. 8 -91. 7) 77. 9 (66. 8 -86. 3) Haase M, Bellomo R, Devarajan R et al. Am J Kidney Dis. 2009; 54: 1012 -24.
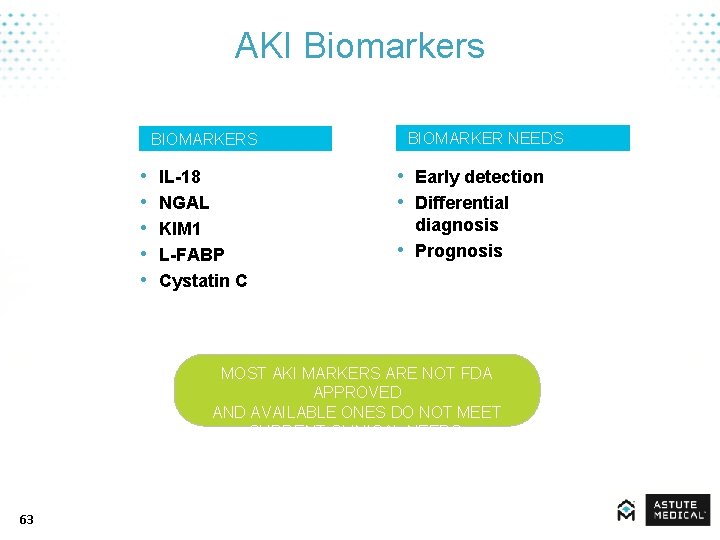
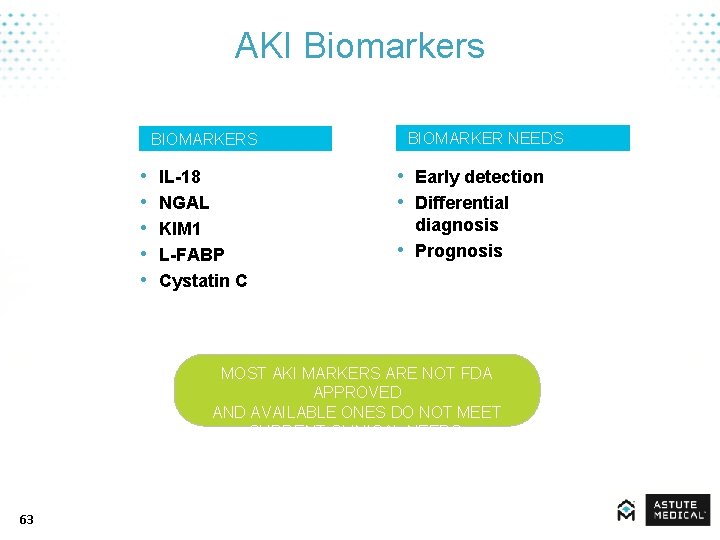
AKI Biomarkers BIOMARKER NEEDS BIOMARKERS • • • IL-18 NGAL KIM 1 L-FABP Cystatin C • Early detection • Differential • diagnosis Prognosis MOST AKI MARKERS ARE NOT FDA APPROVED AND AVAILABLE ONES DO NOT MEET CURRENT CLINICAL NEEDS. 63
Possible Utility of New Biomarkers • Early detection • Differential diagnosis • Prognosis – Predict need for dialysis – Reversibility – Risk of death 64
Unmet Clinical Needs • AKI is difficult to assess. • Mortality is high and it carries a very high cost. • Currently available methodologies and biomarkers are not meeting clinical needs. • New biomarkers are on the horizon to assist with AKI risk assessment. 65
 Aki aki aki
Aki aki aki How to protect yourself from intentional injuries
How to protect yourself from intentional injuries Example of a sentence outline
Example of a sentence outline Cell shape
Cell shape Renal medulla
Renal medulla Tubulus proximalis
Tubulus proximalis Kidney diagram
Kidney diagram Frog bile duct
Frog bile duct World kidney day 2011
World kidney day 2011 7 functions of the kidney
7 functions of the kidney Gfr rumus
Gfr rumus Life science grade 11 kidney practical
Life science grade 11 kidney practical Kaarlo hinkkala
Kaarlo hinkkala Adh feedback
Adh feedback Kidney failure urine color chart
Kidney failure urine color chart 3 layers of the kidney
3 layers of the kidney Kidney hilum
Kidney hilum Fish kidney
Fish kidney Seer kidney cancer
Seer kidney cancer Renal tubule
Renal tubule Adipocyte
Adipocyte Kidney in pelvis
Kidney in pelvis Nemo kidney disease
Nemo kidney disease Kidney biopsy core curriculum
Kidney biopsy core curriculum Hydrogen secretion in kidney
Hydrogen secretion in kidney Urinary system
Urinary system Adpkd
Adpkd Symptomatic polycystic kidney disease
Symptomatic polycystic kidney disease Stomach cancer symptons
Stomach cancer symptons Medulla kidney
Medulla kidney Kidney
Kidney Tubulus intermedius
Tubulus intermedius Bellinior
Bellinior Xenobiotics definition
Xenobiotics definition Ain kidney
Ain kidney Sahaj shankh mudra
Sahaj shankh mudra Collecting duct
Collecting duct Adh role
Adh role Sonia sangha
Sonia sangha Efferent arteriole
Efferent arteriole Wolffian duct
Wolffian duct Kidney
Kidney Excretory system image
Excretory system image Renal function test
Renal function test Albumin kidney disease
Albumin kidney disease Kidney space
Kidney space Ectopia renal
Ectopia renal Nephron structure
Nephron structure Order of urine flow through kidney
Order of urine flow through kidney Diagram of kidney pain
Diagram of kidney pain Dog kidney
Dog kidney Kidney
Kidney Midpole of the left kidney
Midpole of the left kidney Function of nephron slideshare
Function of nephron slideshare Kidney
Kidney Space of disse
Space of disse Cortex medulla pelvis
Cortex medulla pelvis Basinlike area of the kidney continuous with the ureter
Basinlike area of the kidney continuous with the ureter Nursing management of hydronephrosis
Nursing management of hydronephrosis Chapter 15 the urinary system figure 15-3
Chapter 15 the urinary system figure 15-3 Slk kidney
Slk kidney Albumin kidney disease
Albumin kidney disease Urinary tract obstruction
Urinary tract obstruction Hypercalauria
Hypercalauria Bladder apex
Bladder apex What do kidney stones look like
What do kidney stones look like