Acute Tubular injury Lecture 5 Acute Tubular Injury
Acute Tubular injury Lecture 5
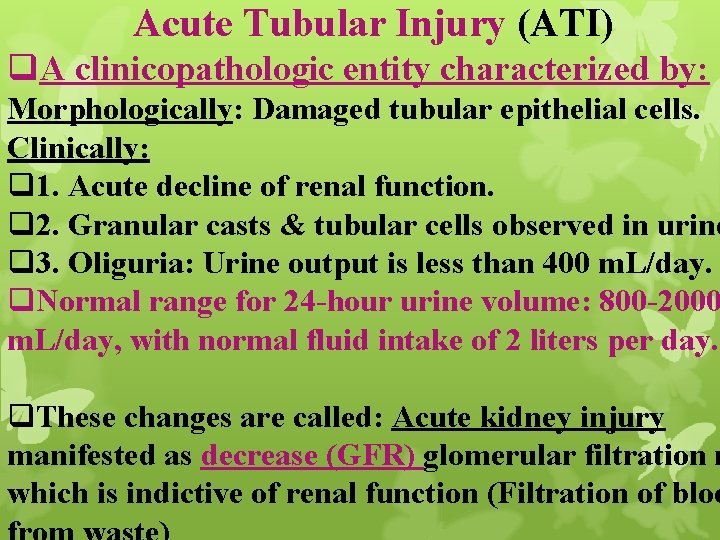
Acute Tubular Injury (ATI) q. A clinicopathologic entity characterized by: Morphologically: Damaged tubular epithelial cells. Clinically: q 1. Acute decline of renal function. q 2. Granular casts & tubular cells observed in urine q 3. Oliguria: Urine output is less than 400 m. L/day. q. Normal range for 24 -hour urine volume: 800 -2000 m. L/day, with normal fluid intake of 2 liters per day. q. These changes are called: Acute kidney injury manifested as decrease (GFR) glomerular filtration r which is indictive of renal function (Filtration of bloo
Causes of acute tubuler injury include: (1) Acute kidney injury. (2) Severe glomerular diseases: Rapidly progressive GN. (3) Diffuse renal vascular diseases: Microscopic polyangitis. (Result from infl. of B. V. ) Thrombotic microangiopathies. (4) Acute drug-induced allergic interstitial nephritis.
(5) Inadequate blood flow to kidney: Ischemic ATI: Generalized or localized decrease in blood flow in: 1. Severe trauma. 2. Acute pancreatitis: By unknown mechanism. Studies showed that systemic inflammation, cytokine & free radicals production & other factors affect microcirculation play a role. 3. Septicemia. 4. Marked hypotension. 5. Shock. 6. Hemolytic crises: Mismatched blood transfusions. Myoglobinuria: Occurs when destruction of muscle lead to elaboration of globin.
6. Nephrotoxic ATI: Caused by poisons: 1. Heavy metals (Mercury). 2. Organic solvent(Carbon tetrachloride). (Cleaning) 3. Drugs: Gentamicin & other antibiotics. 4. Radiographic contrast agents. Tubular epithelial cells are sensitive to: Anoxia & toxins. Persistent severe disturbances in blood flow Diminished oxygen & substrate delivery to tubular cells Cell injury. q ATI is reversible so: q Proper recognition (DIAGNOSIS) & management can make difference between full recovery & death.
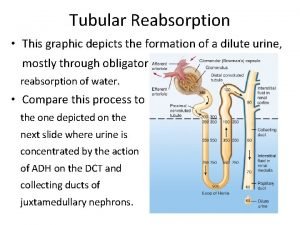
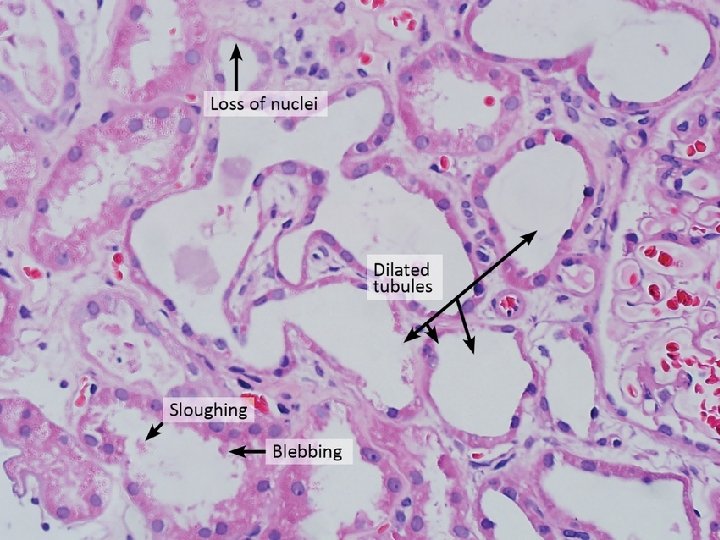
Morphology Ischemic ATI: Tubular injuries include: 1. Attenuation of proximal tubular brush borders. 2. Blebbing & sloughing of brush borders. 3. Vacuolization of cells. 4. Detachment of tubular cells from BM with sloughing of cells into urine. 5. Presence of proteina casts in distal tubules & collecting ducts. 6. Casts contain myoglobin when ATI is caused by crush injuries. 7. Interstitium: Generalized edema with mild infl. infiltrate: Polymorphonuclear leukocytes, lymphocytes & plasma cells.
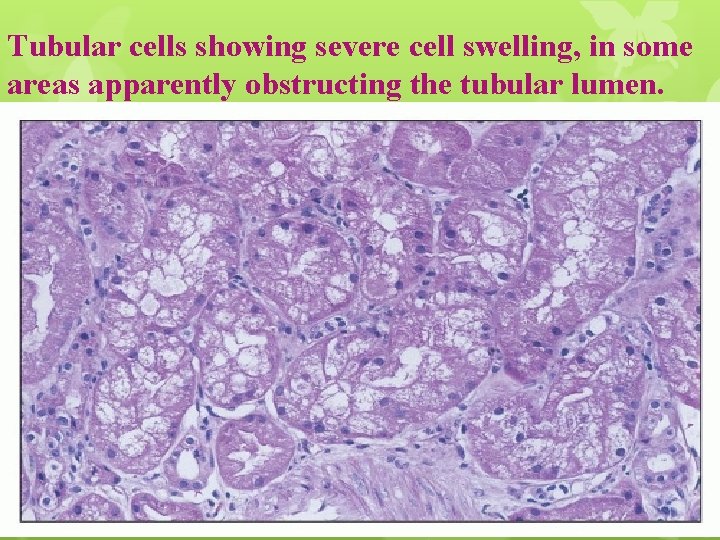
Tubular cells showing severe cell swelling, in some areas apparently obstructing the tubular lumen.
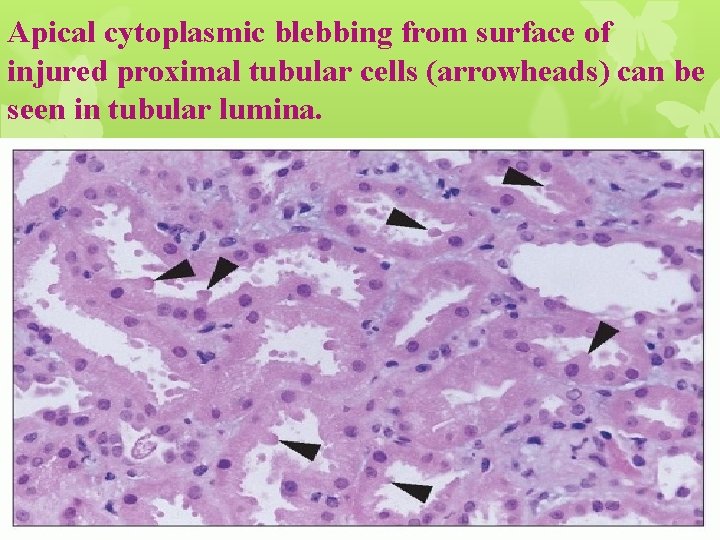
Apical cytoplasmic blebbing from surface of injured proximal tubular cells (arrowheads) can be seen in tubular lumina.
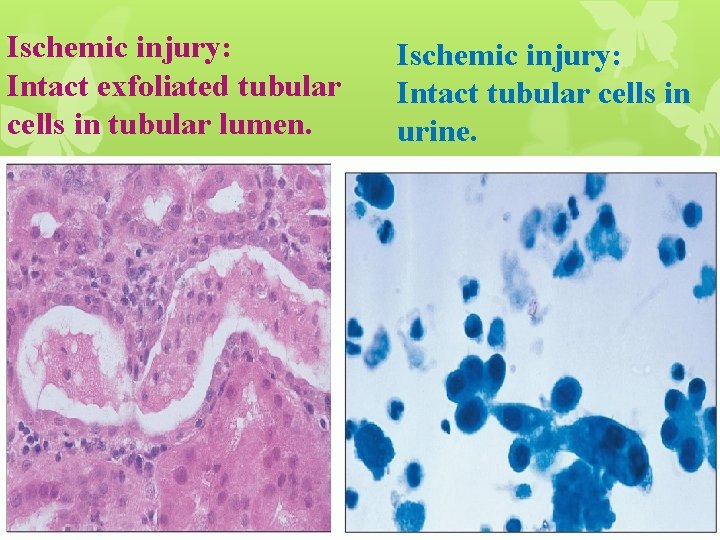
Ischemic injury: Intact exfoliated tubular cells in tubular lumen. Ischemic injury: Intact tubular cells in urine.
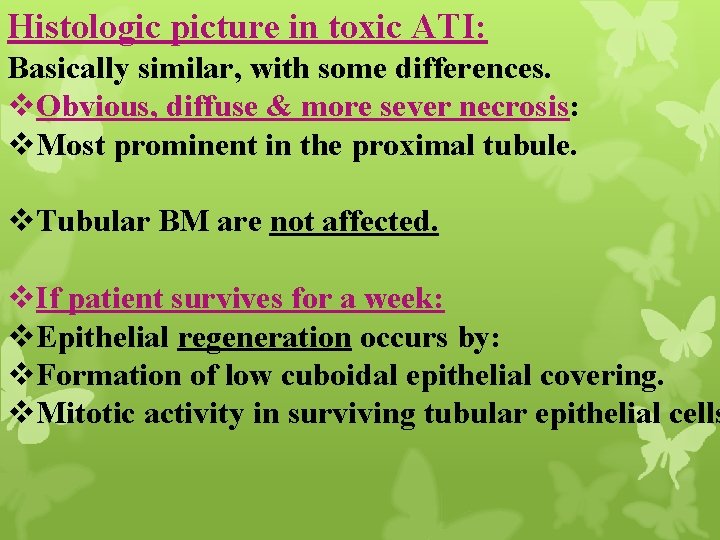
Histologic picture in toxic ATI: Basically similar, with some differences. v. Obvious, diffuse & more sever necrosis: v. Most prominent in the proximal tubule. v. Tubular BM are not affected. v. If patient survives for a week: v. Epithelial regeneration occurs by: v. Formation of low cuboidal epithelial covering. v. Mitotic activity in surviving tubular epithelial cells

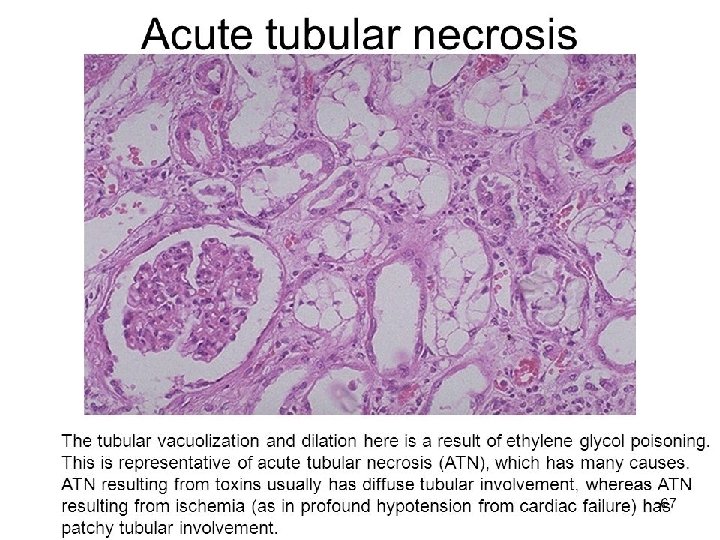

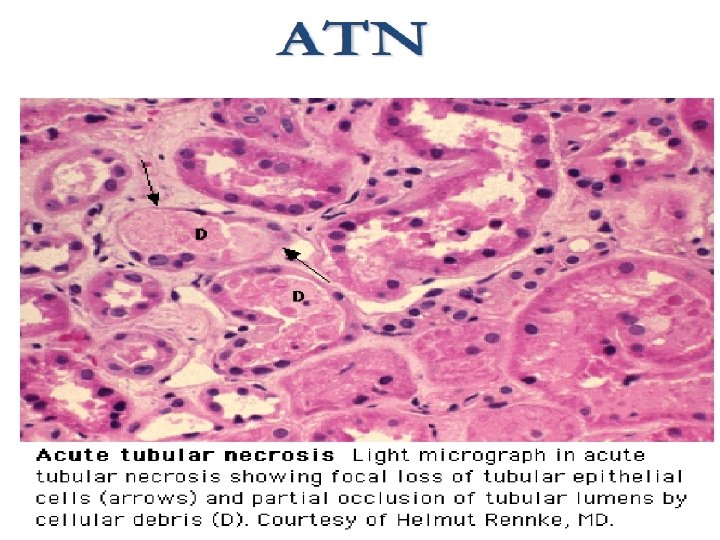
Detached necrotic tubular cells, with pyknotic nuclei in lumen of proximal tubule. B: Granular casts with necrotic cell debris. Flattened tubular epithelium in tubules containing necrotic debris.
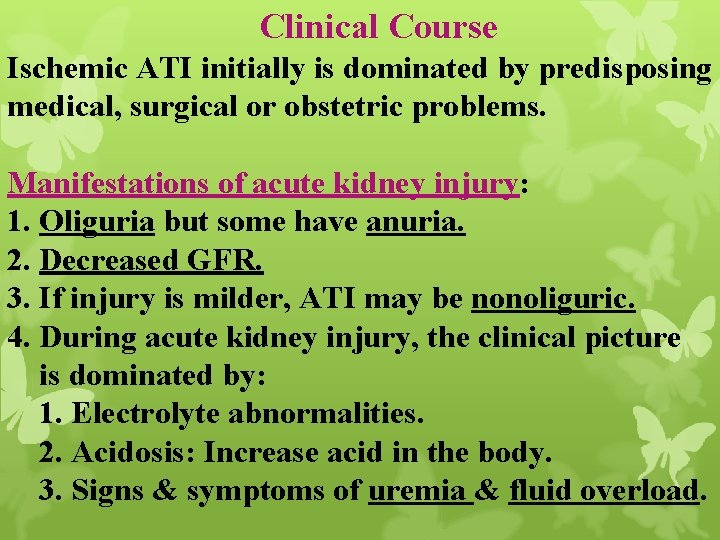
Clinical Course Ischemic ATI initially is dominated by predisposing medical, surgical or obstetric problems. Manifestations of acute kidney injury: 1. Oliguria but some have anuria. 2. Decreased GFR. 3. If injury is milder, ATI may be nonoliguric. 4. During acute kidney injury, the clinical picture is dominated by: 1. Electrolyte abnormalities. 2. Acidosis: Increase acid in the body. 3. Signs & symptoms of uremia & fluid overload.
Prognosis: Varies depending on severity & nature of injury & associated medical conditions. In the absence of careful supportive treatment or dialysis Death. When the cause of acute kidney injury is ATI: Repair & tubular regeneration improvement. Gradual clinical
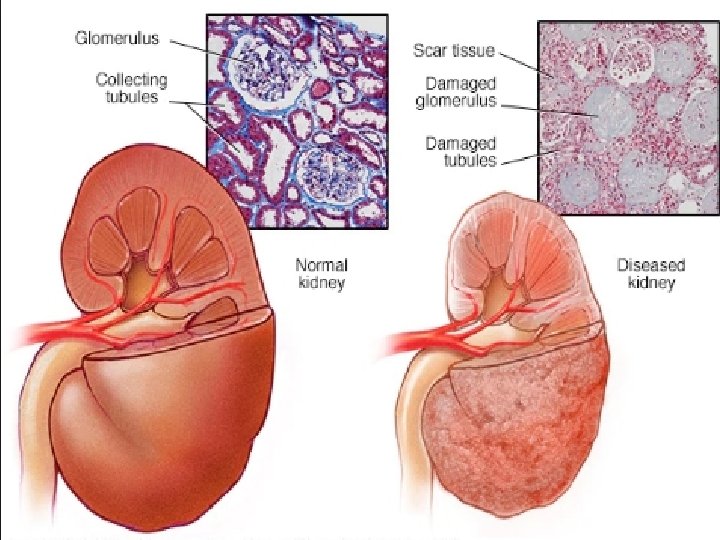
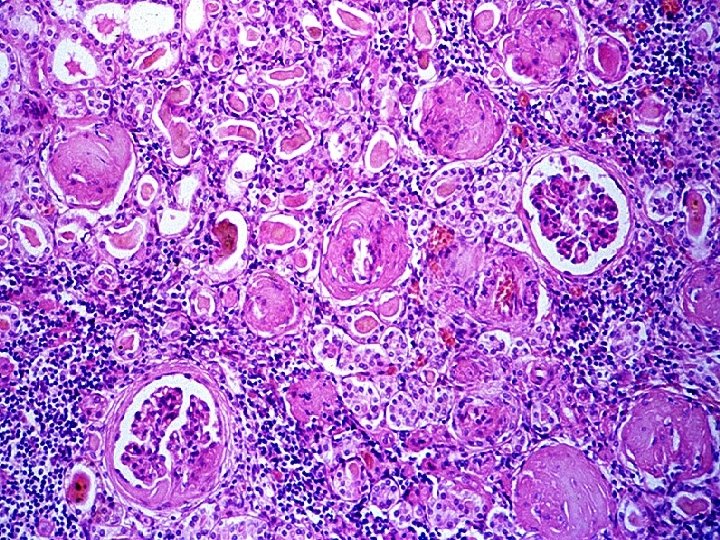
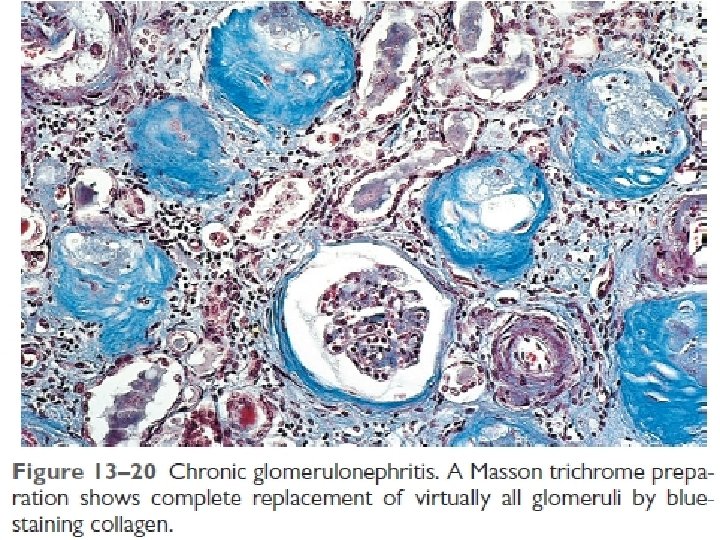
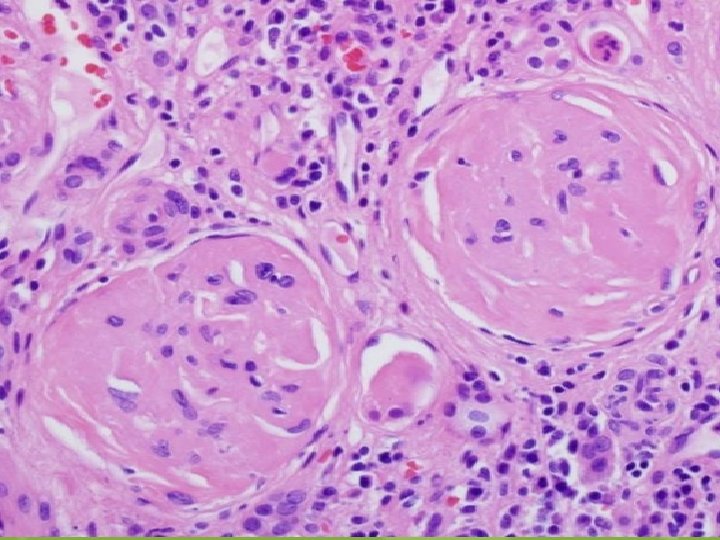
Chronic kidney disease v. Result from progressive scarring that is caused by any type of kidney disease. v. Alterations in function of the remaining intact nephrons are maladaptive & cause further scarring. v. Results in end-stage kidney: v. Glomeruli, tubules, interstitium & vessels, all are sclerosed. v. Unless disorder is treated with dialysis or transplantation, death results from uremia.
Morphology v. Gross: v. Kidneys are symmetrically contracted. v. Surfaces: Red-brown & diffusely granular when disorder affects blood vessels or glomeruli. v. Kidneys damaged by chronic pyelonephritis are unevenly involved & have deep scars. Microscopically: v. Advanced scarring of glomeruli. v. Sometimes complete sclerosis obliterate glomeruli. v. Interstitial fibrosis. v. Atrophy of tubules in cortex.
v. Diminution & loss of portions of peritubular capillary network. v. Thick-walled with narrowed lumina of small & medium-sized arteries secondary to hypertension. v. Lymphocytic infiltrates in fibrotic interstitial tissu v. Damage to all kidney structures: End stage kidneys.
Clinical course v. May develop insidiously & discovered late after the onset of renal insufficiency. v. Renal disease may be detected by routine medical examination: v 1. Proteinuria. v 2. Hypertension. v 3. Azotemia. v. Specific findings precede chronic kidney disease: 1. Some degree of proteinuria is present in all cases. 2. Hypertension: Very common & its effects may dominate the clinical picture.
v 3. In patients with glomeruler disease resulting in nephrotic syndrome Glomeruler sclerosis Closing the way for more protein loss. v. So: Nephrotic syndrome becomes less sever but the kidney will have more advanced disease. v 4. Microscopic hematuria. v. Grossly bloody urine is infrequent at late stage. v. Prognosis is poor without treatment. v. Progression to uremia & death is the rule.
Thank you
- Slides: 27