Rejection of the Kidney Allograft N Engl J


- Slides: 46
Rejection of the Kidney Allograft N Engl J Med 2010; 363: 1451 -62. R 3 박세윤
CLINICAL FEATURES OF ALLOGRAFT REJECTION
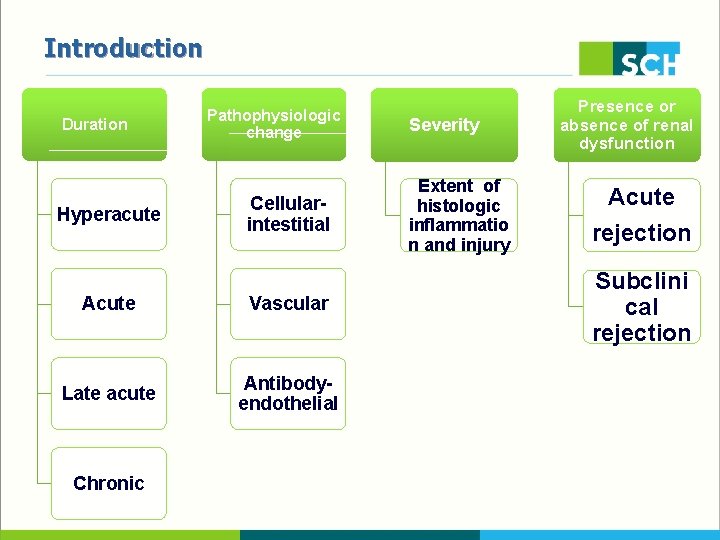
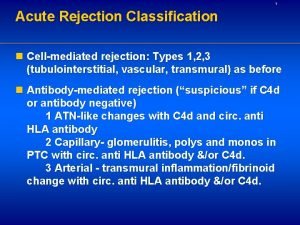
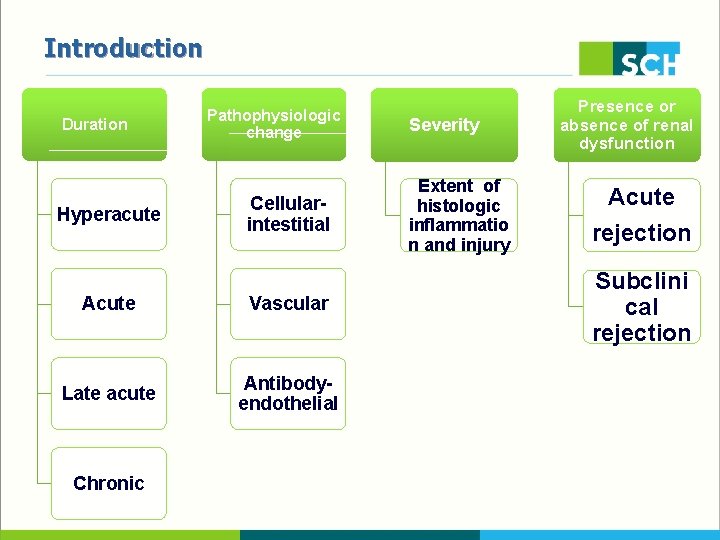
Introduction Duration Hyperacute Pathophysiologic change Cellularintestitial Acute Vascular Late acute Antibodyendothelial Chronic Severity Extent of histologic inflammatio n and injury Presence or absence of renal dysfunction Acute rejection Subclini cal rejection
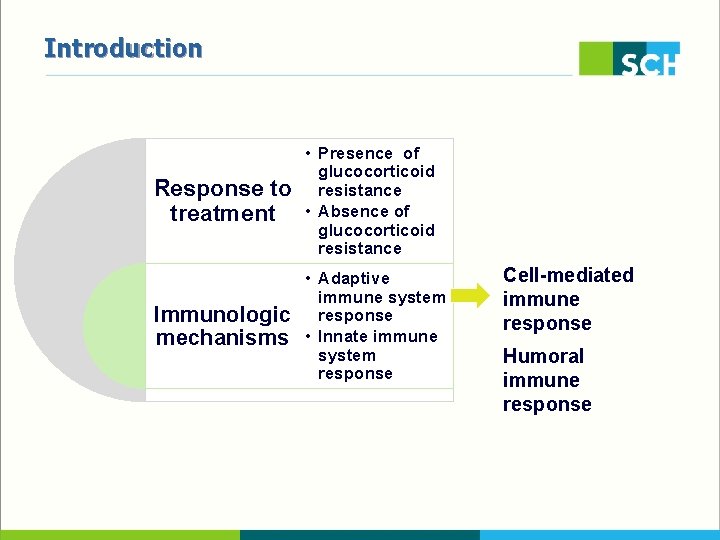
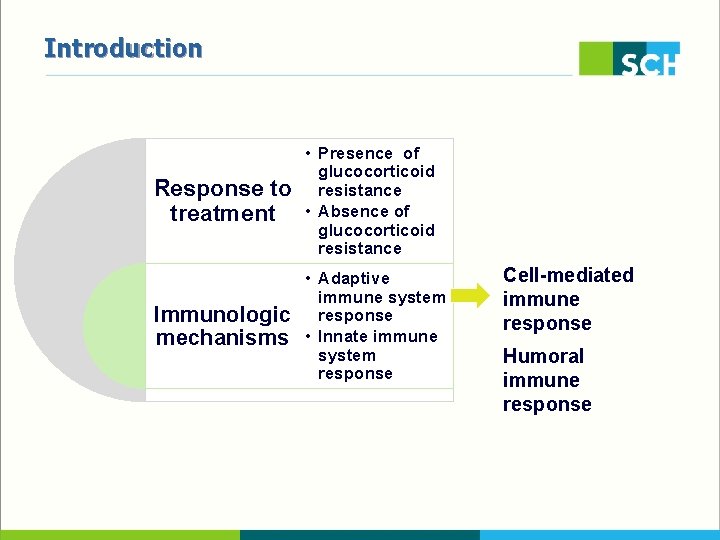
Introduction Response to treatment • Presence of glucocorticoid resistance • Absence of glucocorticoid resistance Immunologic mechanisms • Adaptive immune system response • Innate immune system response Cell-mediated immune response Humoral immune response
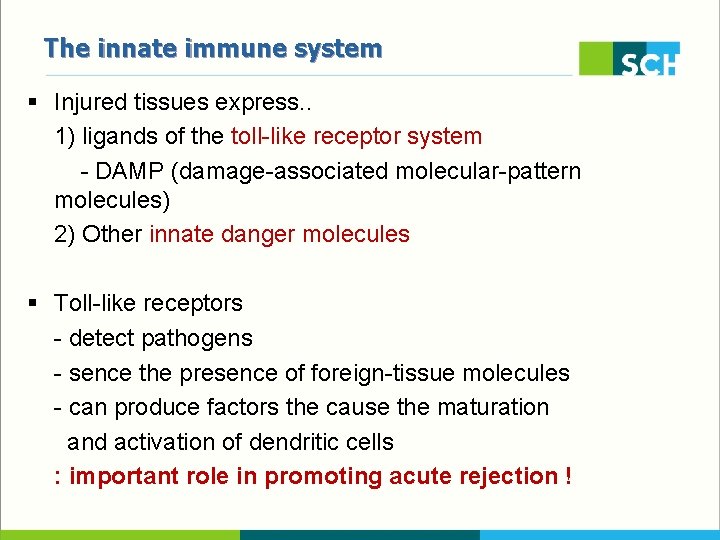
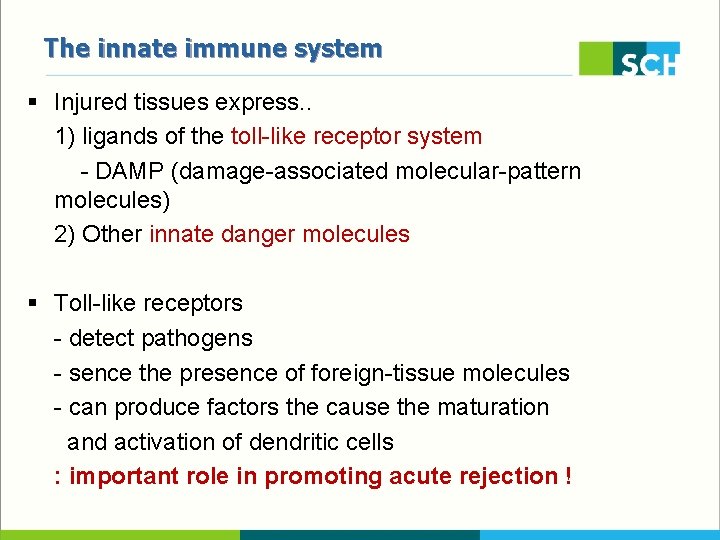
The innate immune system § Injured tissues express. . 1) ligands of the toll-like receptor system - DAMP (damage-associated molecular-pattern molecules) 2) Other innate danger molecules § Toll-like receptors - detect pathogens - sence the presence of foreign-tissue molecules - can produce factors the cause the maturation and activation of dendritic cells : important role in promoting acute rejection !
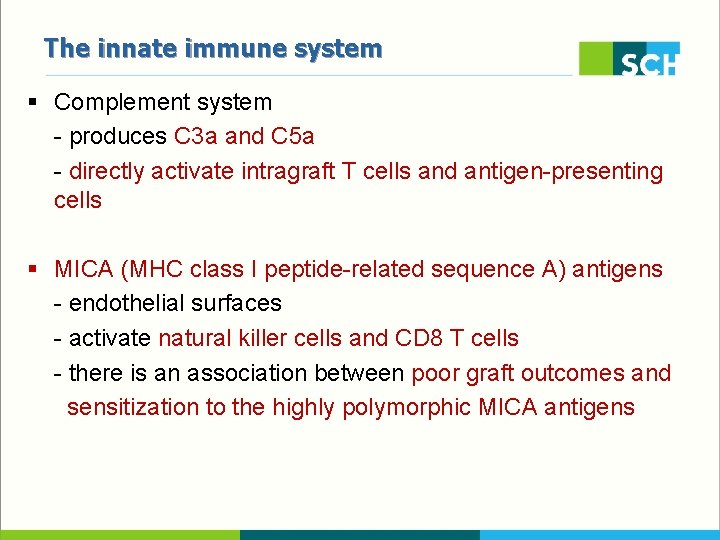
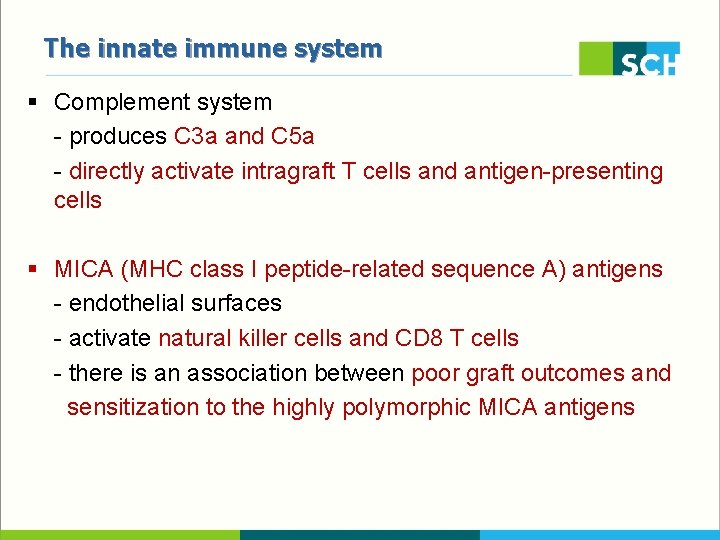
The innate immune system § Complement system - produces C 3 a and C 5 a - directly activate intragraft T cells and antigen-presenting cells § MICA (MHC class I peptide-related sequence A) antigens - endothelial surfaces - activate natural killer cells and CD 8 T cells - there is an association between poor graft outcomes and sensitization to the highly polymorphic MICA antigens
ANTIBODY-MEDIATED REJECTION HLA molecules Endothelial-cell antigens ABO blood-group antigens on endothelial cells and red cells
Antibodies against blood-group antigens § ABO-incompatible kidneys successfully transplanted : with use of an experimental protocol entails perioperative removal of antibodies from the recipient by means of plasmapheresis or immunoadsorption § After they have been removed, anti-blood-groop antibodies can rise to pretreatment levels after transplantation -> adhere to the microvasculature activate complement but they generally do not injure the endothelium ‘accommodation’ but mechanism is unknown
Hyperacute Rejection § Rejection of the renal graft that occurs almost immediately after release of the vascular cross clamps is classified as hyperacute. § The kidney appears flaccid and mottled : reflecting the deposition of antibodies against HLA antigens expressed on the endothelium of the glomeruli and microvasculature § Activation of the classic complement cascade within the graft, endothelial necrosis, platelet deposition, local coagulation
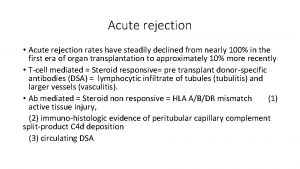
Acute Antibody-Mediated Rejection § Antibody-mediated rejection often begins within days after trasnplantation (or within weeks, if antilymphocyte antibody therapy was given) § The main feature is rapid graft dysfunction due to inflammation § Agonistic angiotensin II type 1 (AT 1)–receptor antibodies § associated with corticosteroid-resistant vascular rejection accompanied by malignant hypertension § pathogenic role remains unclear
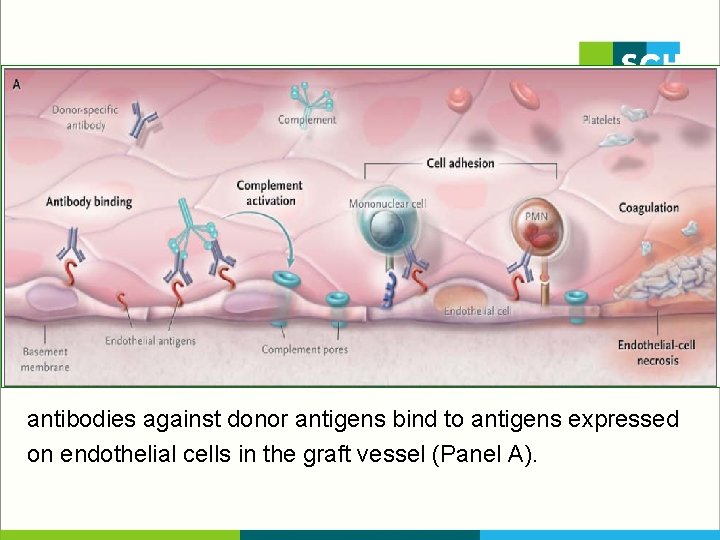
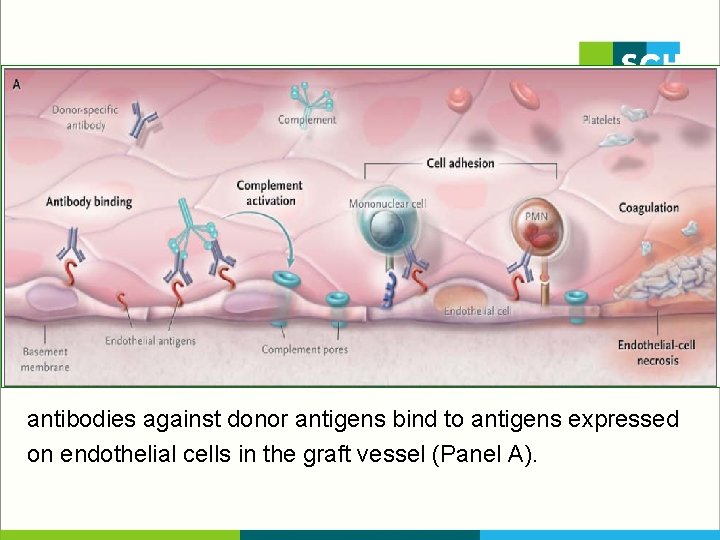
antibodies against donor antigens bind to antigens expressed on endothelial cells in the graft vessel (Panel A).
Acute Antibody-Mediated Rejection § Promote platelet aggregation § Von Willebrand factor § P-selectin § Cause leukocytes to adhere to glomeruli (glomerulitis) or to dilated peritubular capillaries (margination) § Interleukin-1α § Interleukin-8 § Chemokine (C-C motif) ligand 2 (CCL 2) § Chemoattractants C 3 a and C 5 a
Acute Antibody-Mediated Rejection § C 4 d, a marker of classic complement activation, is frequently found in peritubular capillaries § C 5 b triggers the assembly of the membrane-attack complex (C 5 b–C 9) § causes localized endothelial necrosis and apoptosis § detachment of endothelial cells from the basement membrane § Microthrombi, with hemorrhage and arterial-wall necrosis and infartion, occur in severe cases
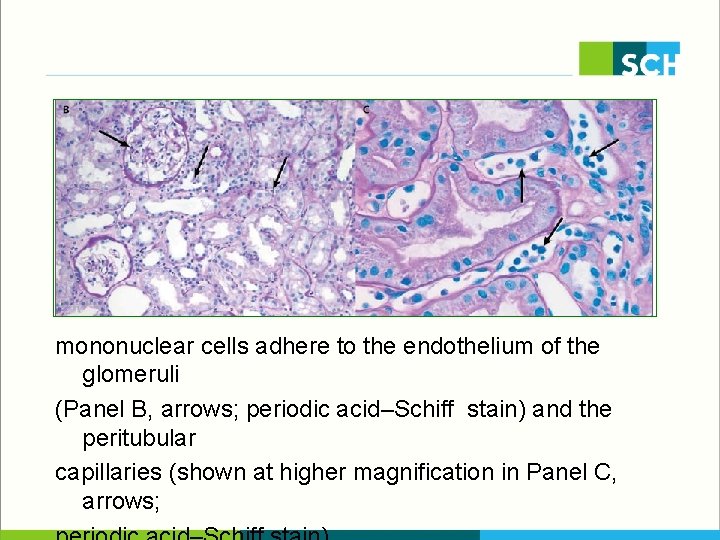
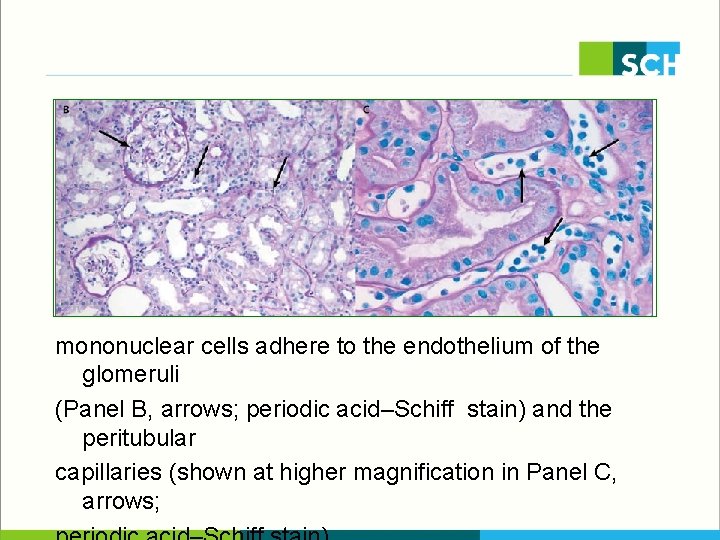
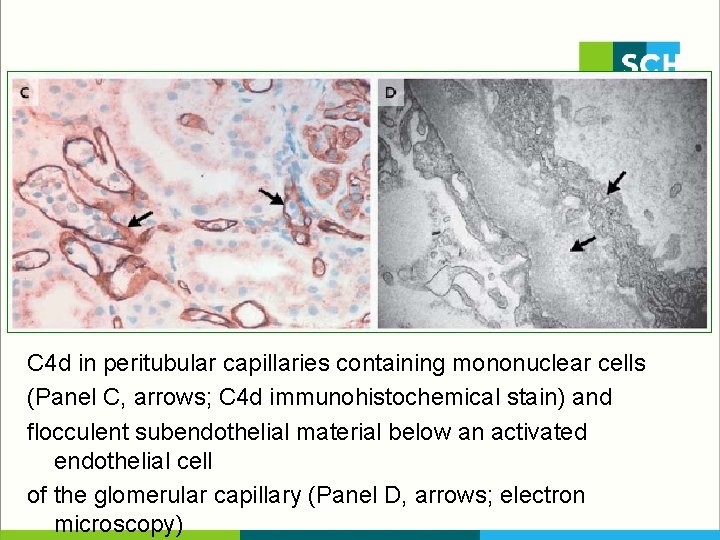
mononuclear cells adhere to the endothelium of the glomeruli (Panel B, arrows; periodic acid–Schiff stain) and the peritubular capillaries (shown at higher magnification in Panel C, arrows;
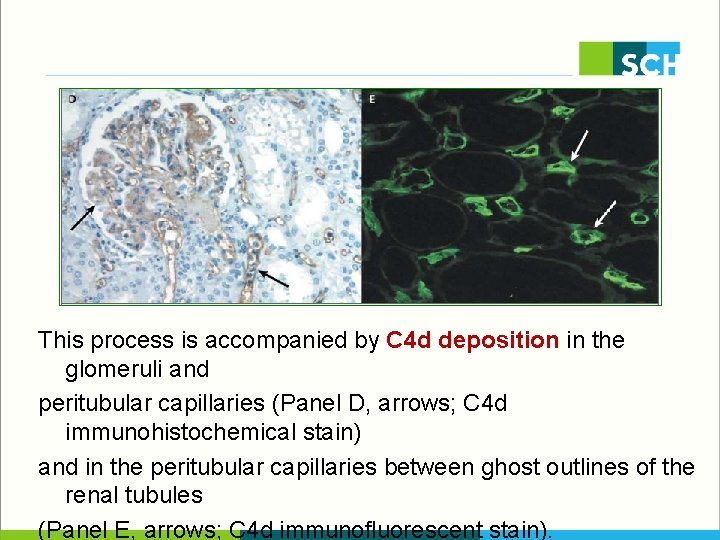
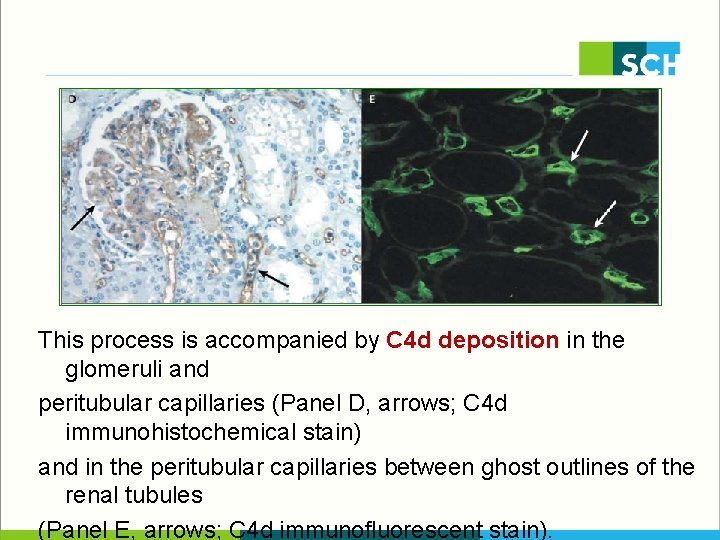
This process is accompanied by C 4 d deposition in the glomeruli and peritubular capillaries (Panel D, arrows; C 4 d immunohistochemical stain) and in the peritubular capillaries between ghost outlines of the renal tubules (Panel E, arrows; C 4 d immunofluorescent stain).
Acute Antibody-Mediated Rejection § Early diagnosis and treatment are essential for salvaging grafts § Treatments include removal of antibodies § § § plamapheresis immunoadsorption high-dose pulses of glucocorticoids intravenous immune globulin antiproliferative agents
Acute Antibody-Mediated Rejection § Supplementary therapies § rituximab § antilymphocyte antibody § New, investigational agents § Eculizumab (a monoclonal antibody that inhibits the cleavage of C 5) § Bortezomib (a proteasome inhibitor that can inhibit plasma cells)

T-CELL-MEDIATED REJECTION
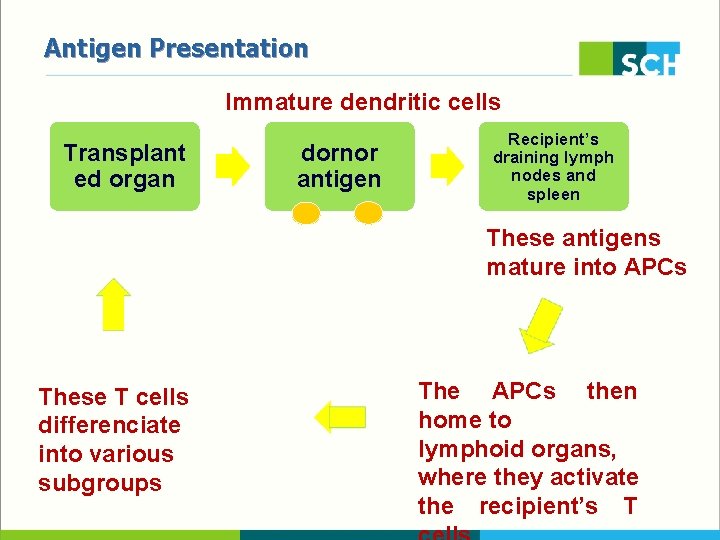
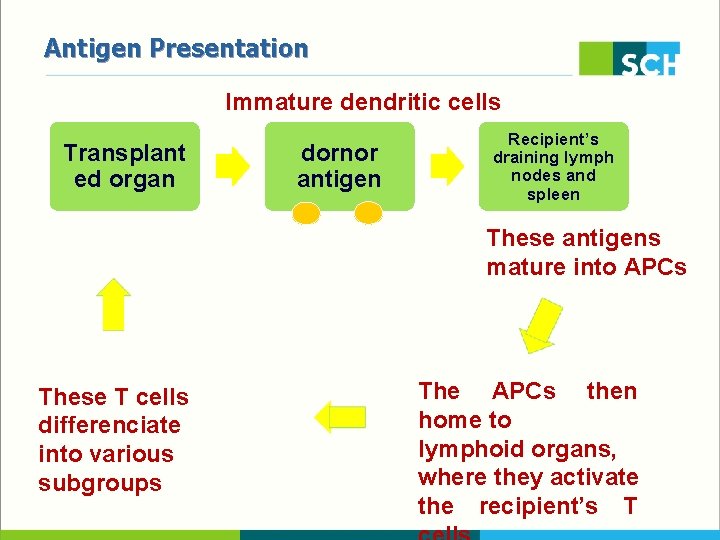
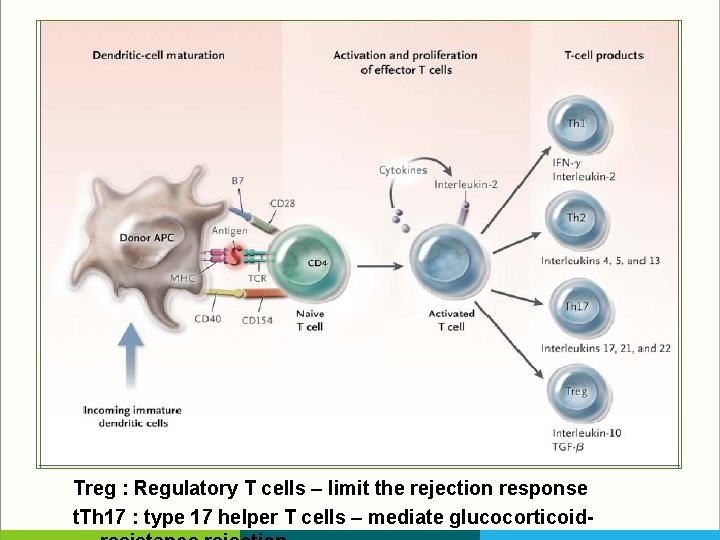
Antigen Presentation Immature dendritic cells Transplant ed organ dornor antigen Recipient’s draining lymph nodes and spleen These antigens mature into APCs These T cells differenciate into various subgroups The APCs then home to lymphoid organs, where they activate the recipient’s T
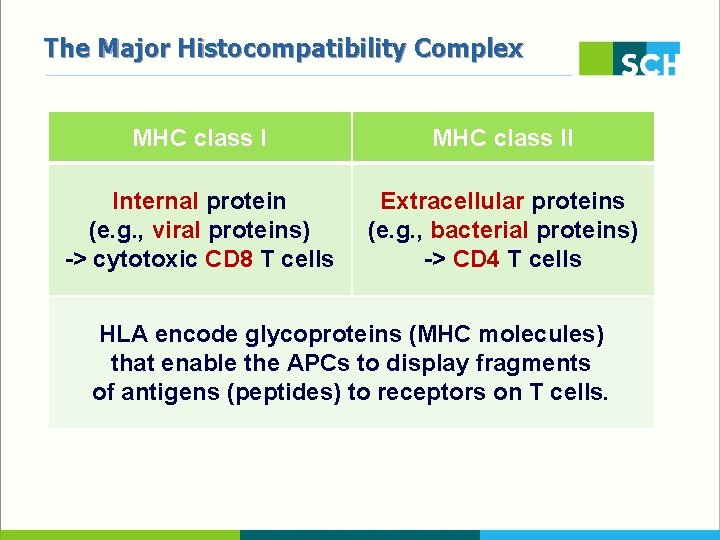
The Major Histocompatibility Complex § HLA class I - HLA-A. -B, -C § HLA class II - DP, -DQ, -DR § HLA class III - Complement system, Cytokine, Heat shock proein
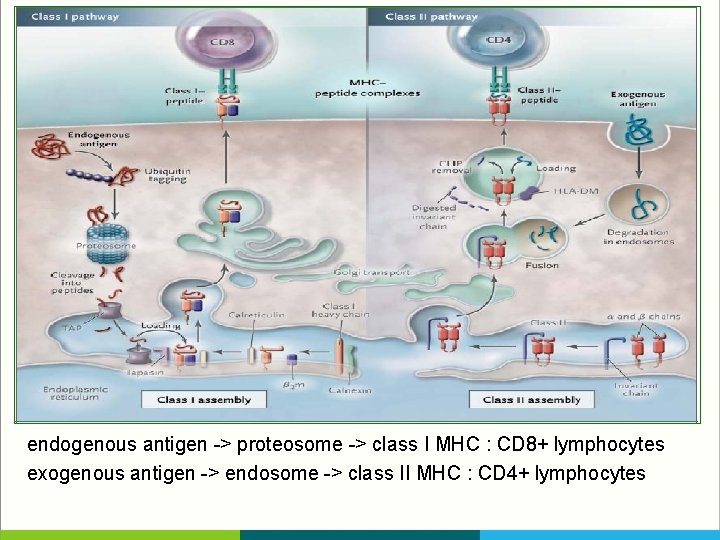
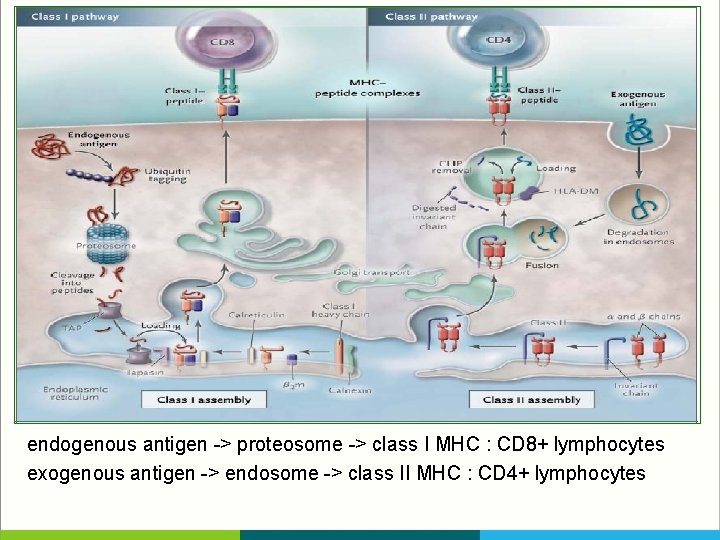
endogenous antigen -> proteosome -> class I MHC : CD 8+ lymphocytes exogenous antigen -> endosome -> class II MHC : CD 4+ lymphocytes
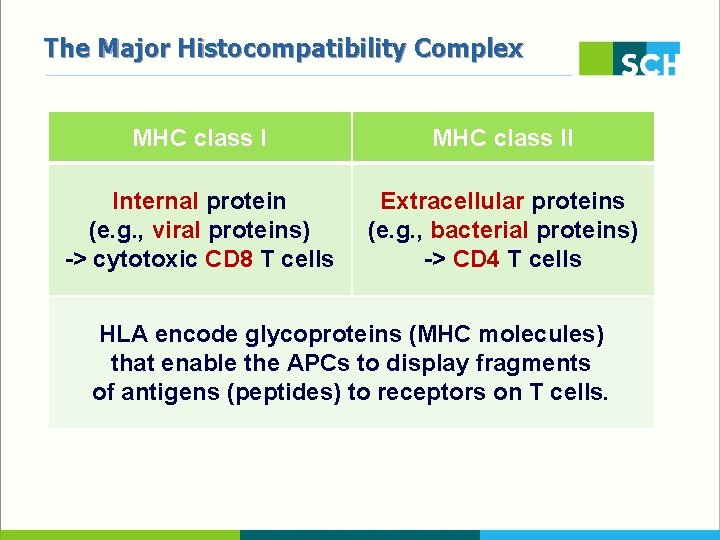
The Major Histocompatibility Complex MHC class II Internal protein (e. g. , viral proteins) -> cytotoxic CD 8 T cells Extracellular proteins (e. g. , bacterial proteins) -> CD 4 T cells HLA encode glycoproteins (MHC molecules) that enable the APCs to display fragments of antigens (peptides) to receptors on T cells.
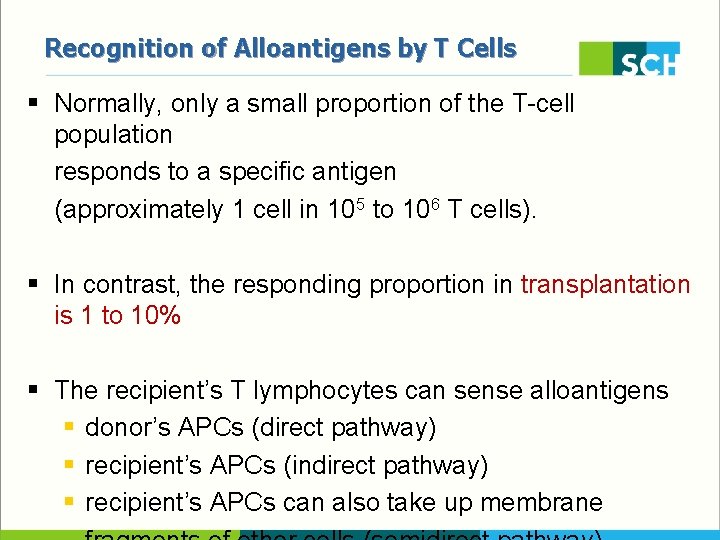
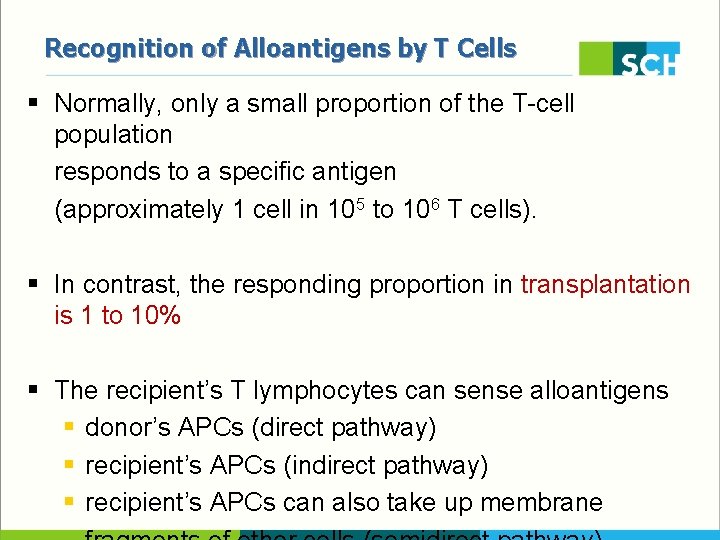
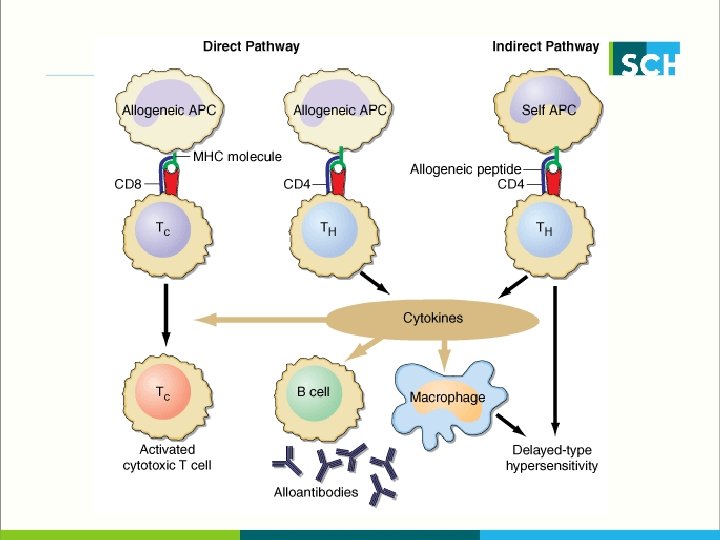
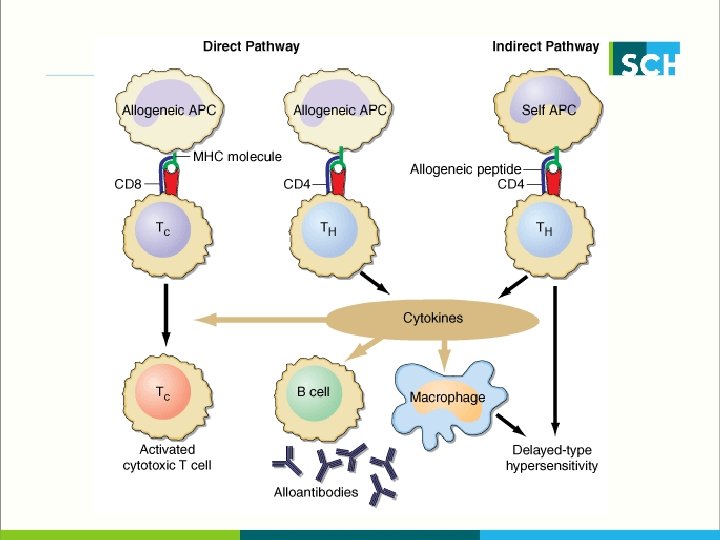
Recognition of Alloantigens by T Cells § Normally, only a small proportion of the T-cell population responds to a specific antigen (approximately 1 cell in 105 to 106 T cells). § In contrast, the responding proportion in transplantation is 1 to 10% § The recipient’s T lymphocytes can sense alloantigens § donor’s APCs (direct pathway) § recipient’s APCs (indirect pathway) § recipient’s APCs can also take up membrane
T-Cell Subgroups § CD 4 T cells produce inflammatory cytokines interferon-γ and interleukin-2 : drive a cellular response interleukin-4, interleukin-5, and interleukin-13, : produce a humoral response § CD 8 T cells mediate cytotoxicity, their effector functions overlap
T-Cell Subgroups § type 1 helper T (Th 1) cells drive the cellular immune response § type 2 helper T (Th 2) cells produce the humoral immune response § can reject grafts, using pathways that involve eosinophils
T-Cell Subgroups § Regulatory T (Treg) cells § express the transcription factor forkhead box P 3 (FOXP 3) § The number of Treg cells correlates with markers of T-cell rejection, including interstitial inflammation, tubulitis, and cytotoxic gene expression, but not with the graft outcome, suggesting that FOXP 3 -positive cells aid in stabilizing inflammation within the graft
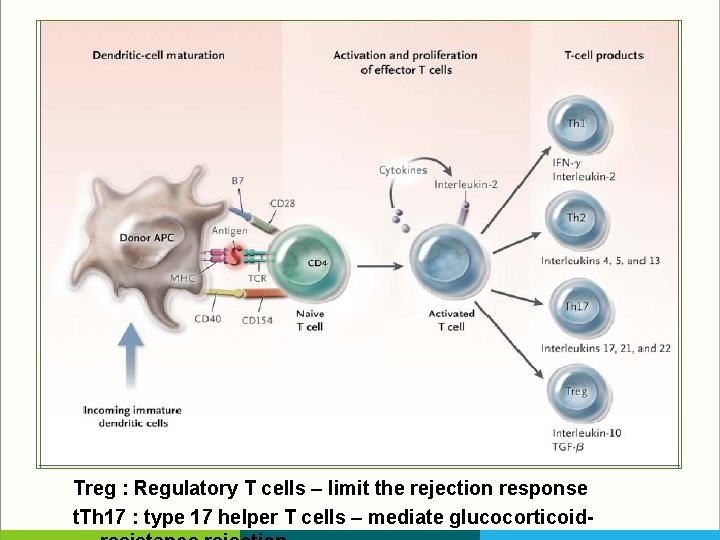
Treg : Regulatory T cells – limit the rejection response t. Th 17 : type 17 helper T cells – mediate glucocorticoid-
Costimulation § T-cell activation requires signals other than those engendered by the MHC–peptide complex, termed costimulatory signals § T cells become anergic when presented with an antigen in the absence of these signals, and agents that block these signals are under development § CD 80 (B 7 -1) and CD 86 (B 7 -2) ; these two B 7 molecules are ligands for two T-cell– membrane receptors, CD 28 (stimulate) and CTLA-4 (inhibitory)
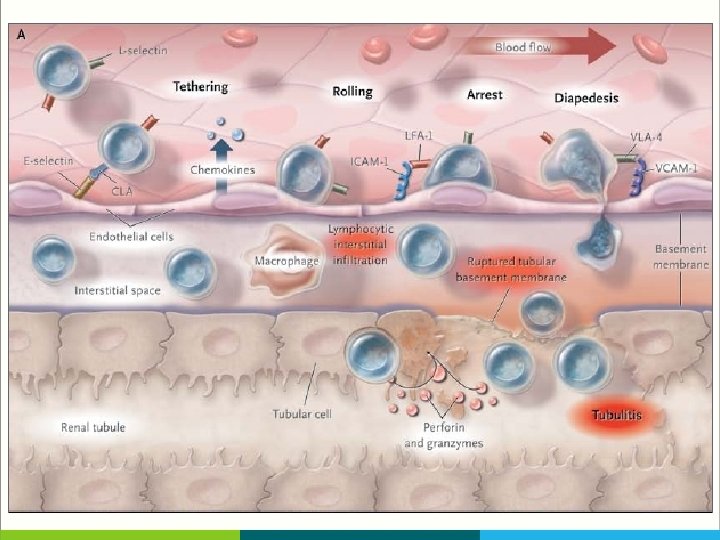
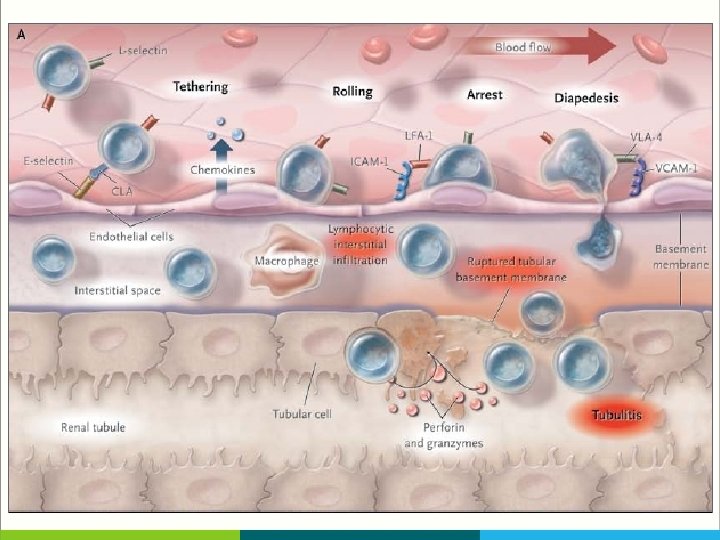
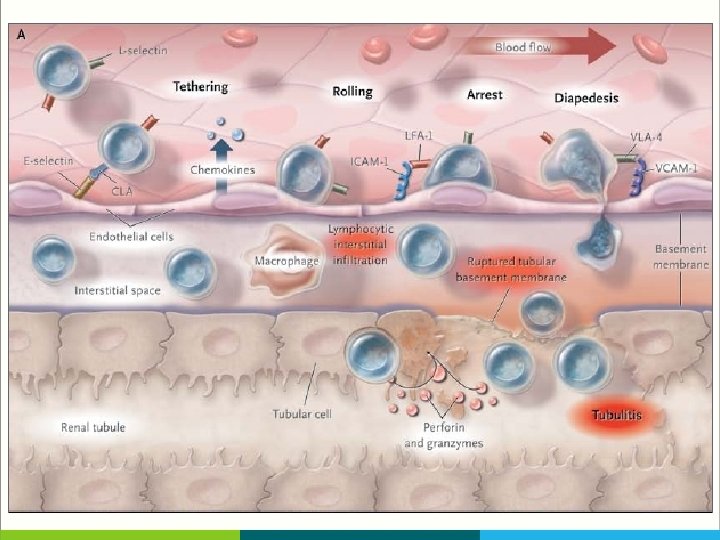
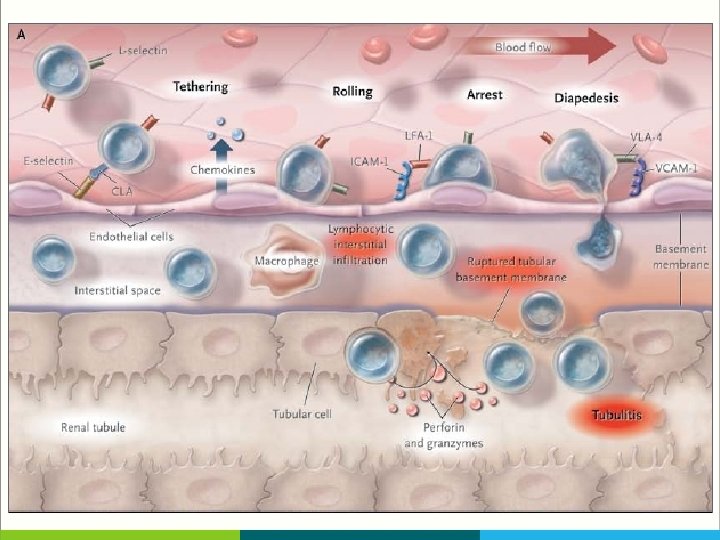
T-Cell Movement in The Allograft § T cells use adhesion molecules, including leukocyte-function–associated antigen 1 (LFA 1) to roll along and tether to endothelium, migrate across peritubular capillaries, and enter the graft § Fingolimod, a small molecule that blocks the egress of T cells from lymph nodes, and anti–LFA-1 agents block such T-cell movement, but until now they have had a limited clinical effect in transplantation
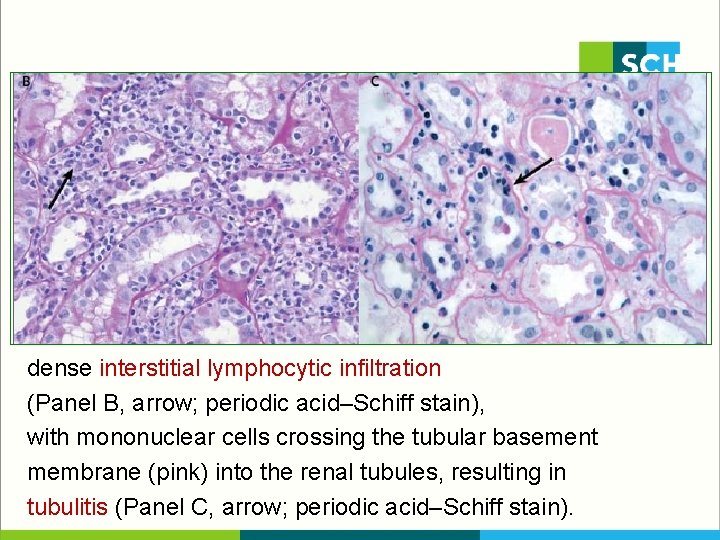
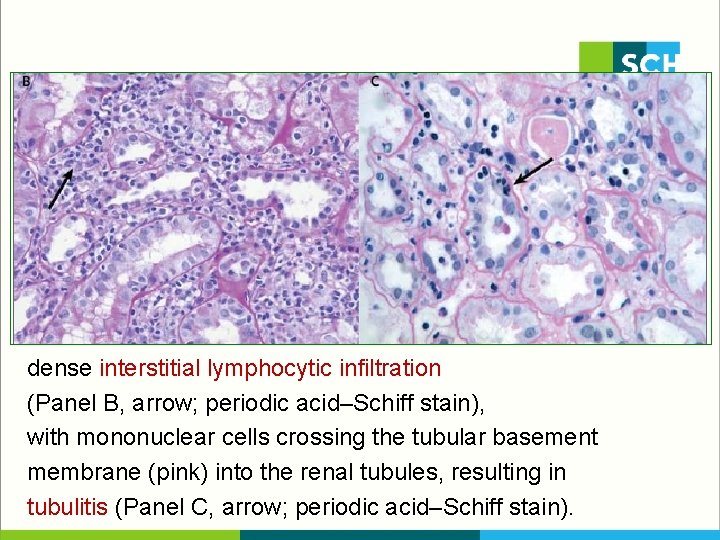
dense interstitial lymphocytic infiltration (Panel B, arrow; periodic acid–Schiff stain), with mononuclear cells crossing the tubular basement membrane (pink) into the renal tubules, resulting in tubulitis (Panel C, arrow; periodic acid–Schiff stain).
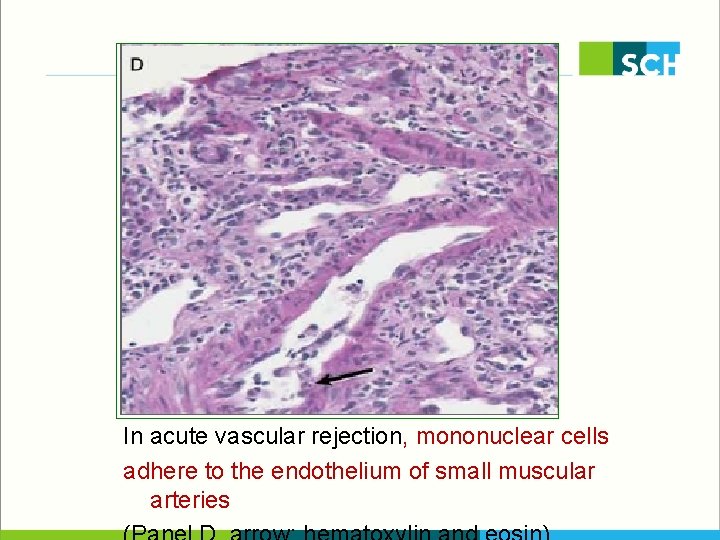
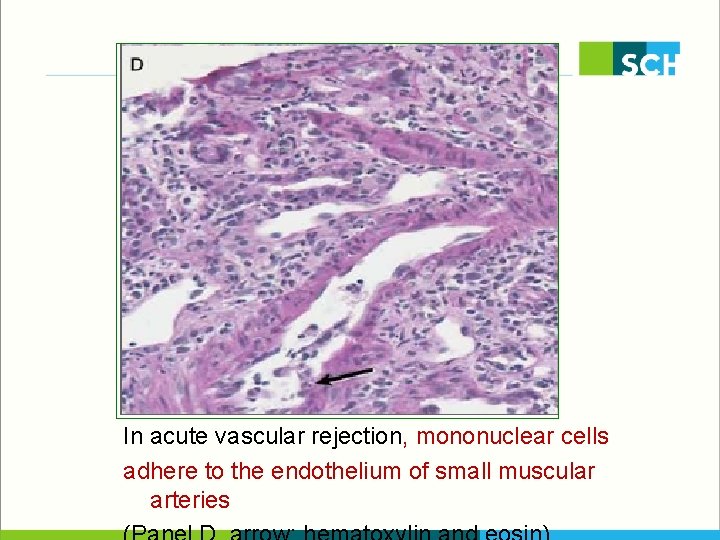
In acute vascular rejection, mononuclear cells adhere to the endothelium of small muscular arteries
Effector T Cells § CD 8 T cells release perforin, which perforates target-cell membranes, and granzymes A and B, which enter cells and induce caspase-mediated apoptosis. § The Fas ligand on cytotoxic T cells activates Fas, a receptor on cells of the graft, and this interaction also induces caspase-mediated apoptosis
Effector T Cells § CD 4 T cells can attack grafted cells expressing minor MHC antigens and can also secrete TNF-α and tumor necrosis factor β (TNF-β), which bind to TNF receptors on endothelial or tubular cells, causing them to undergo apoptosis § In animals, blockade of TNF by antibody or knockout of TNF-receptor genes prolongs allograft survival.
OTHER PATTERNS OF REJECTION Vascular rejection Late actue rejection Chronic rejection
Vascular Rejection § CD 4 and CD 8 T cells and macrophages invade the subendothelium and intima of muscular arteries by means of intercellular adhesion molecule 1 (ICAM-1) or vascular-cell adhesion molecules (VCAM) on activated endothelium and by means of chemokine (e. g. , CCL 4, CCL 5, and CXCL 8) gradients. § Experimental evidence suggests that anti-MHC antibodies, T-cell– mediated immunity to minor MHC antigens, Natural killer cells, and interferon-γ all play a role in the invasion of vessels.

Vascular Rejection § Vascular rejection is a severe condition that does not respond to glucocorticoid therapy and instead requires potent antilymphocyte- antibody therapy (muromonab-CD 3 [Orthoclone OKT 3, Ortho Biotech] or antithymocyte globulin).
Lacte Acute Rejection § Severe and difficult to reverse, with a high risk of subsequent graft loss § Its main features are active immune inflammation and chronic tubulointerstitial damage, which frequently involves graft-directed antibody.
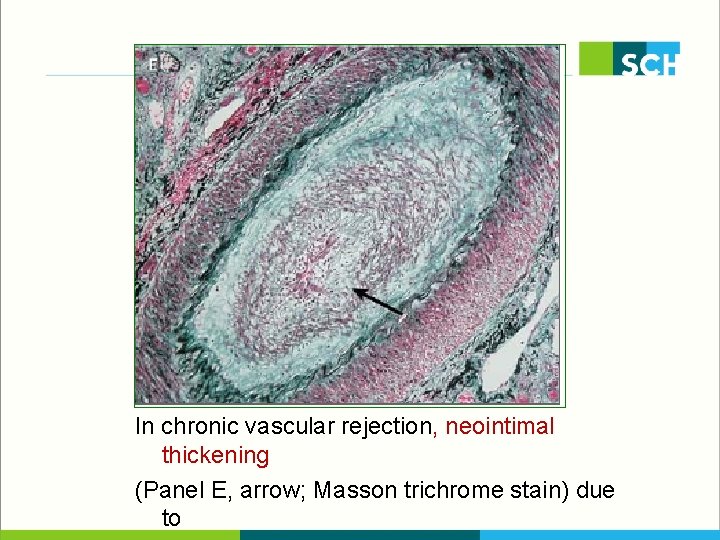
Chronic Rejection § Chronic allograft rejection — ongoing immune injury to the graft — is due to a failure to maintain sufficient immunosuppression to control residual antigraft lymphocytes or antibodies § Its features include a progressive decline in renal function, Invasion of the renal parenchyma by T cells, and persistent infiltration of the interstitium by T cells and macrophages § Occasionally, one also sees smooth-muscle proliferation and hyperplasia in vessels, forming a neointima; focal destruction
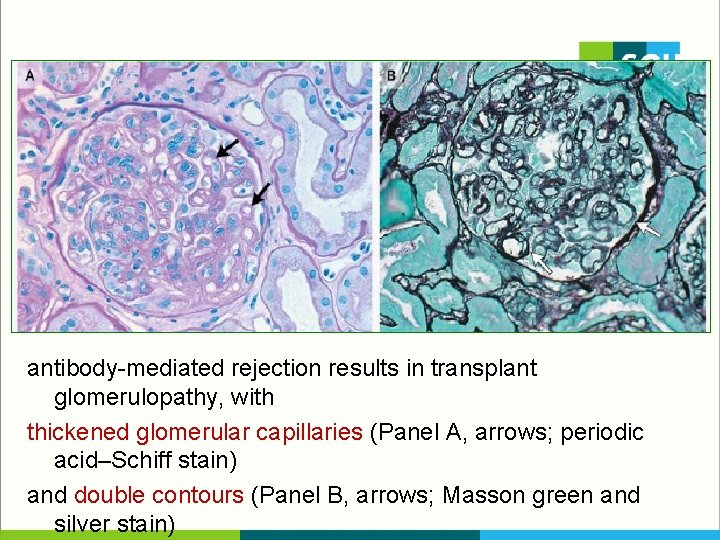
Chronic Rejection § In chronic antibody-mediated rejection, undetected preexisting donor-specific antibodies or antibodies generated after transplantation deposit on the capillary endothelium § Endothelial injury to glomerular and peritubular capillaries causes cellular hypertrophy, subendothelial deposition of fibrillary material, expansion and duplication of the glomerular basement membrane, or mesangial- cell interposition
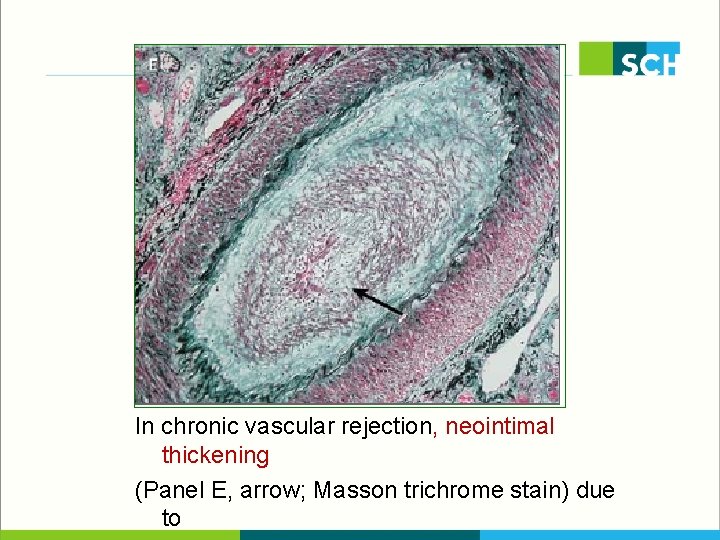
In chronic vascular rejection, neointimal thickening (Panel E, arrow; Masson trichrome stain) due to
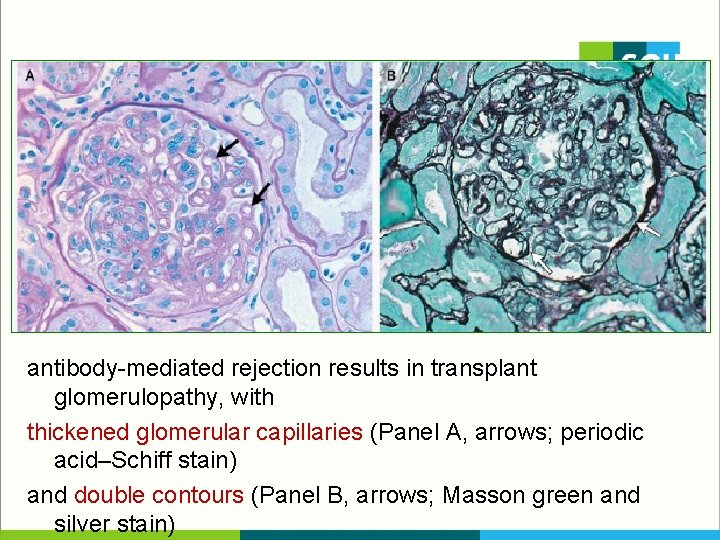
antibody-mediated rejection results in transplant glomerulopathy, with thickened glomerular capillaries (Panel A, arrows; periodic acid–Schiff stain) and double contours (Panel B, arrows; Masson green and silver stain)
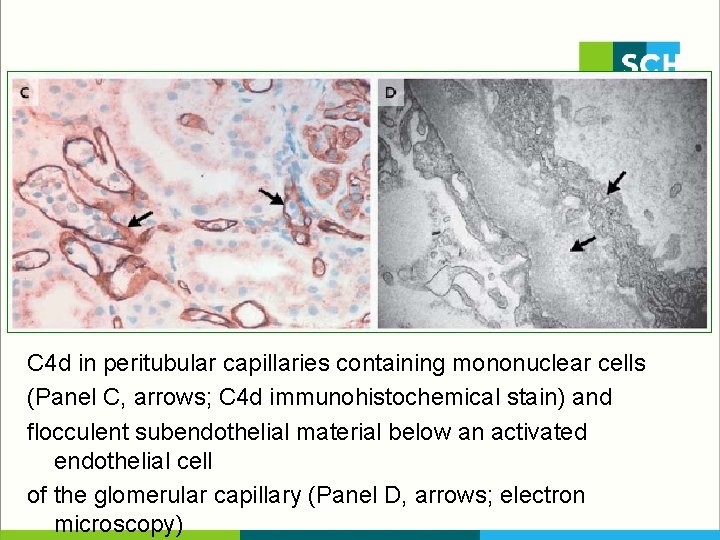
C 4 d in peritubular capillaries containing mononuclear cells (Panel C, arrows; C 4 d immunohistochemical stain) and flocculent subendothelial material below an activated endothelial cell of the glomerular capillary (Panel D, arrows; electron microscopy)
 Dfdba bone graft
Dfdba bone graft Autogenous vs allograft
Autogenous vs allograft Engl 5440u class notes
Engl 5440u class notes Engl 214
Engl 214 Jessica mehr
Jessica mehr Edmund engl
Edmund engl Theories of fashion movement
Theories of fashion movement Refifs
Refifs Luke 4 rejection at nazareth
Luke 4 rejection at nazareth Rejection attachment
Rejection attachment Elishagoodman
Elishagoodman Chronic rejection
Chronic rejection Dependency rejection
Dependency rejection Capacity of cooling tower
Capacity of cooling tower Near zone length ultrasound
Near zone length ultrasound Scientific name for sugar glider
Scientific name for sugar glider Chronic rejection
Chronic rejection Sample rejection criteria
Sample rejection criteria Chronic rejection
Chronic rejection Opposite of rejection
Opposite of rejection Sample rejection criteria
Sample rejection criteria Chronic rejection
Chronic rejection Chronic rejection
Chronic rejection Reassurance dalam konseling
Reassurance dalam konseling Test summary reports
Test summary reports Acceptance and rejection region
Acceptance and rejection region Switching overvoltages in ehv and uhv systems
Switching overvoltages in ehv and uhv systems Sample rejection criteria
Sample rejection criteria Rejection sensitive dysphoria
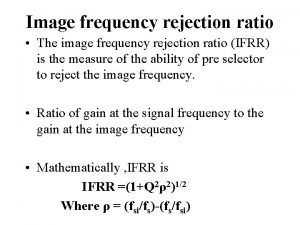
Rejection sensitive dysphoria Image frequency rejection ratio
Image frequency rejection ratio Voltage gain of amplifier
Voltage gain of amplifier Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Hát lên người ơi
Hát lên người ơi Hổ sinh sản vào mùa nào
Hổ sinh sản vào mùa nào Diễn thế sinh thái là
Diễn thế sinh thái là đại từ thay thế
đại từ thay thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Công của trọng lực
Công của trọng lực Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay