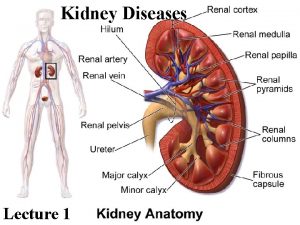
Nutrition in Kidney Diseases Functions of Kidney n


- Slides: 35
Nutrition in Kidney Diseases
Functions of Kidney n Excrete waste material: end products of protein metabolism (urea, uric acid, creatinine, ammonia, and sulfates), excess water and nutrients, dead renal cells, and toxic substances n Electrolyte balance n Hormonal regulation n Blood pressure regulation n Glucose homeostatis
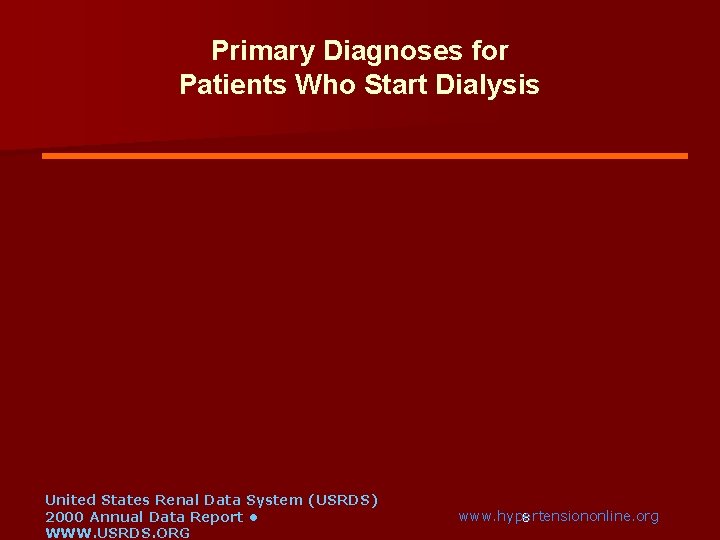
ETIOLOGY n n n Diabetes mellitus (28%) Hypertension (25%) Glomerulonephritis (21%) Polycystic Kidney Diease (4%) Other (23%): Obstruction, infection, etc.
Primary Diagnoses for Patients Who Start Dialysis Other 10% Diabetes Glomerulonephritis 50% 13% Hypertension 27% United States Renal Data System (USRDS) 2000 Annual Data Report • WWW. USRDS. ORG www. hypertensiononline. org 8
Chronic Renal Failure Develops slowly, number of functioning nephrons constantly diminishing. Uremia is a result Symptoms: nausea, headache, coma, convulsions. Severe renal failure will result in death unless dialysis used. 9
Clinical pathophysioloy n n n n Metabolic acidosis: result in; – Muscle breakdown – Bone dissolving Hyperkalemia Hypertension Negative N balance Insulin resistance Hyperphosphatemia Anemia
Progression of chronic renal failure n Factors causing progression § sustaining primary disease § systemic hypertension § Intraglomerular hypertension § Proteinuria § Nephrocalcinosis § Dyslipidaemia § Imbalance between renal energy demands and supply
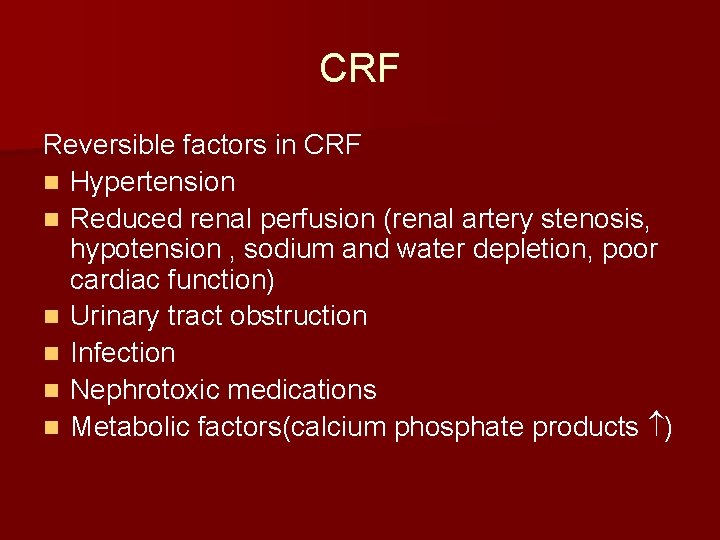
CRF Reversible factors in CRF n Hypertension n Reduced renal perfusion (renal artery stenosis, hypotension , sodium and water depletion, poor cardiac function) n Urinary tract obstruction n Infection n Nephrotoxic medications n Metabolic factors(calcium phosphate products )
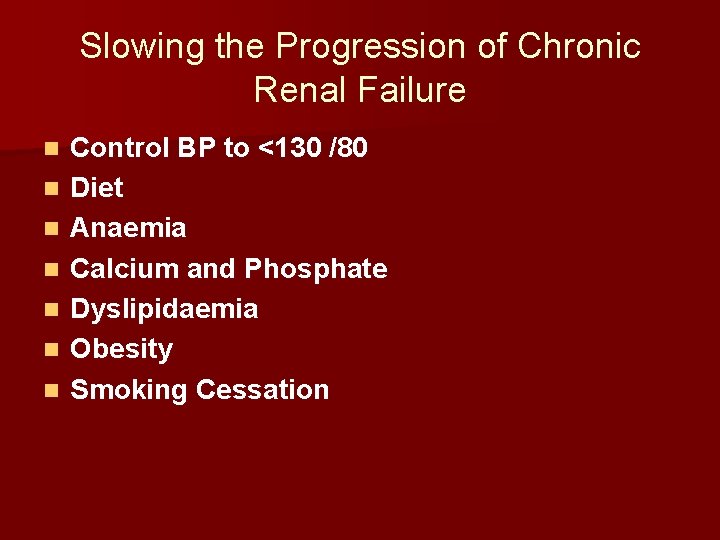
Slowing the Progression of Chronic Renal Failure n n n n Control BP to <130 /80 Diet Anaemia Calcium and Phosphate Dyslipidaemia Obesity Smoking Cessation
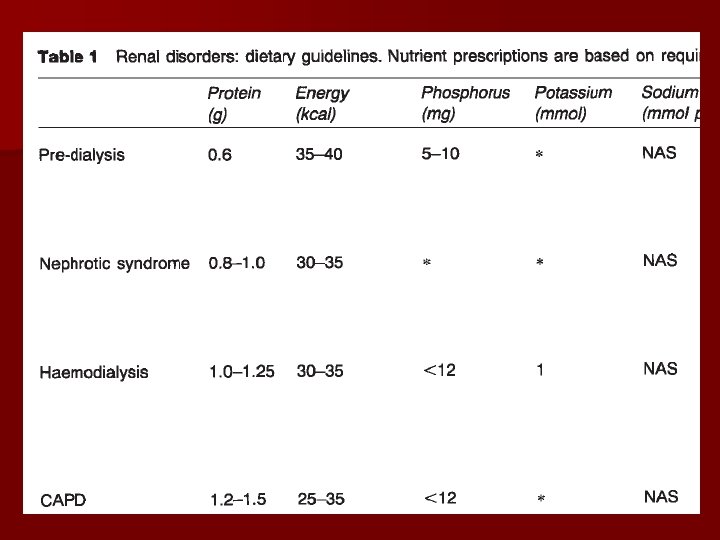
Dietary Treatment of Renal Disease q. Extremely complicated. q. Intended to reduce the amount of excretory work demanded of the kidneys while helping them maintain fluid, acid-base, and electrolyte balance. q. In CRF may have protein, sodium, potassium and phosphorus restricted. 14
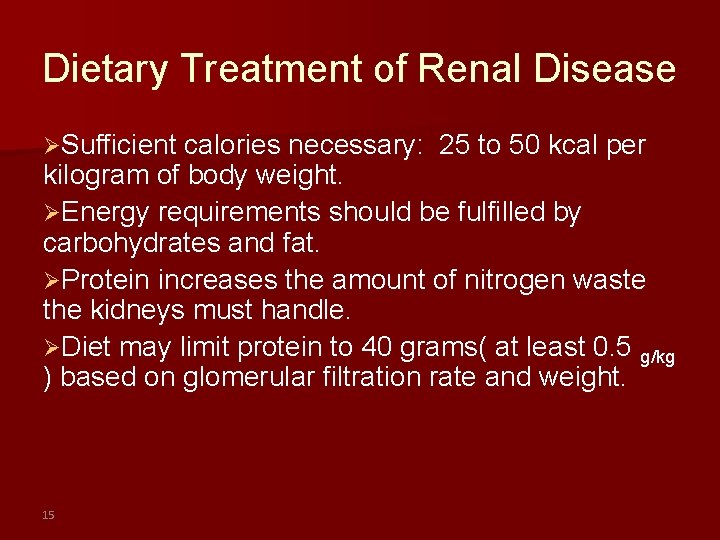
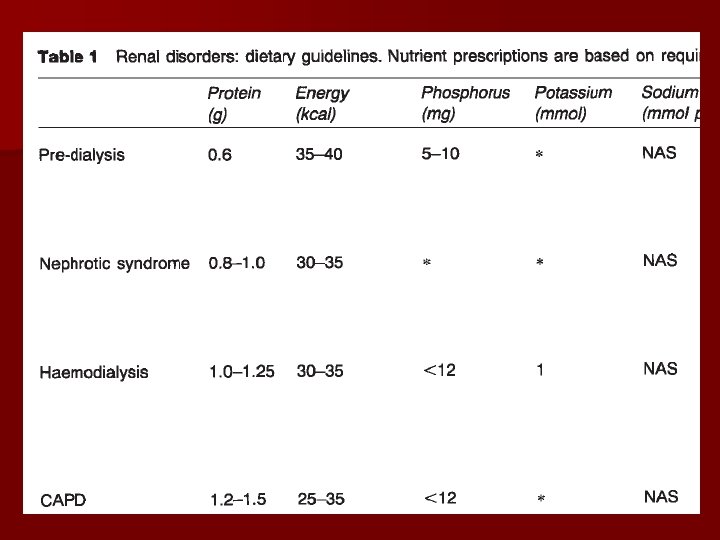
Dietary Treatment of Renal Disease ØSufficient calories necessary: 25 to 50 kcal per kilogram of body weight. ØEnergy requirements should be fulfilled by carbohydrates and fat. ØProtein increases the amount of nitrogen waste the kidneys must handle. ØDiet may limit protein to 40 grams( at least 0. 5 g/kg ) based on glomerular filtration rate and weight. 15
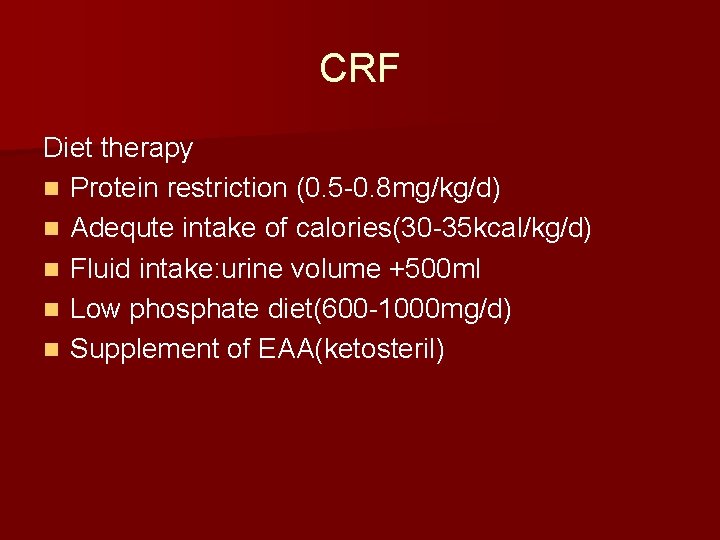
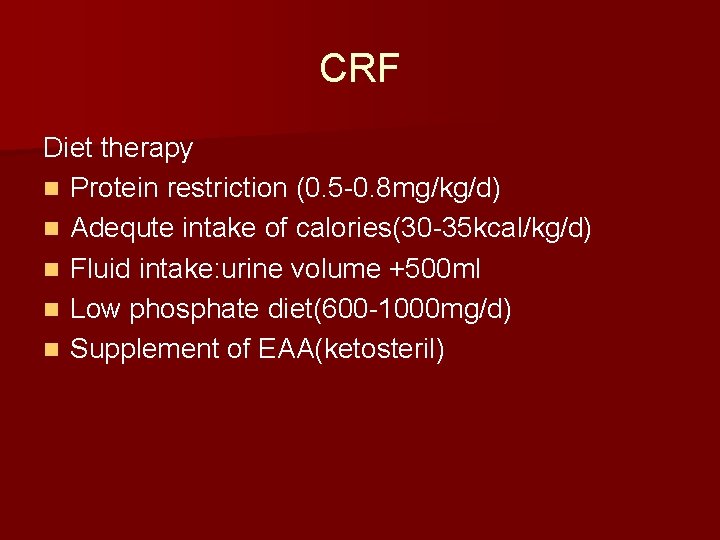
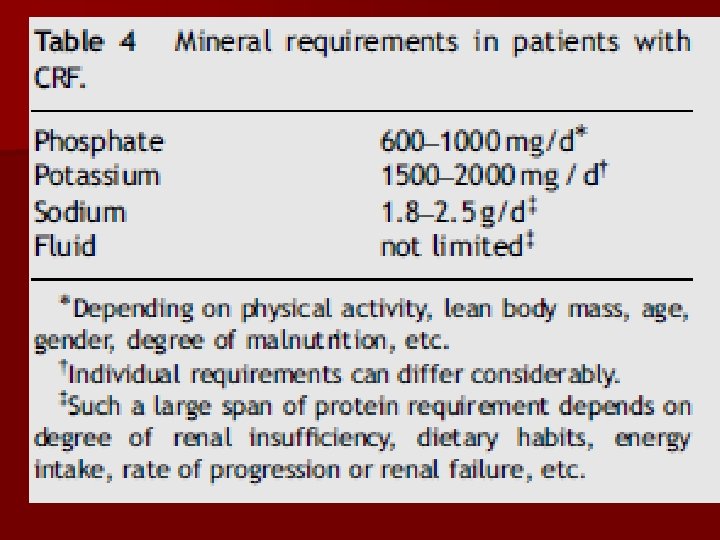
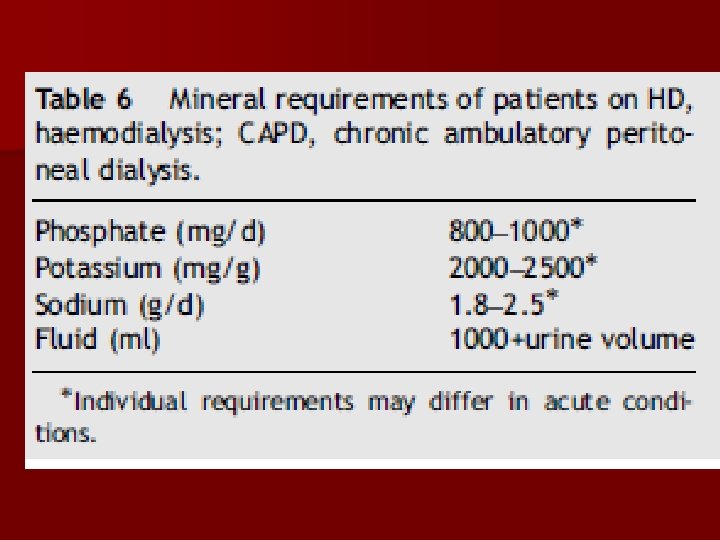
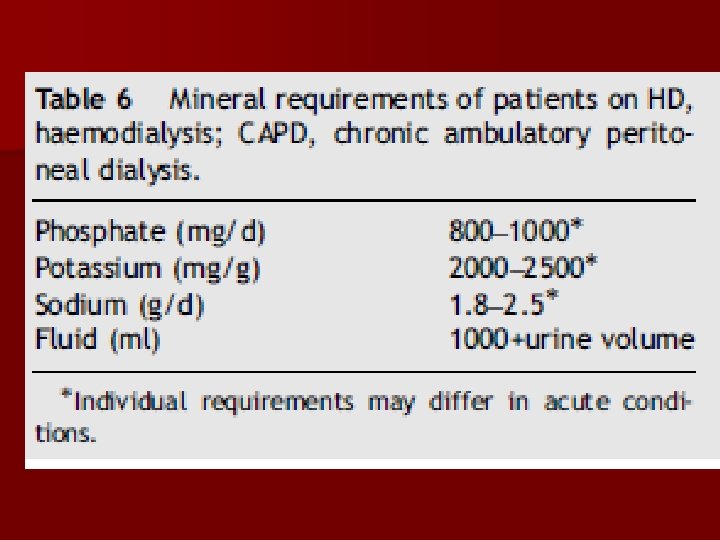
CRF Diet therapy n Protein restriction (0. 5 -0. 8 mg/kg/d) n Adequte intake of calories(30 -35 kcal/kg/d) n Fluid intake: urine volume +500 ml n Low phosphate diet(600 -1000 mg/d) n Supplement of EAA(ketosteril)

Fluid n Unrestricted until urine output declines n Urine output plus 1000 cc/d Evaluate effect on blood pressure and cardiac function
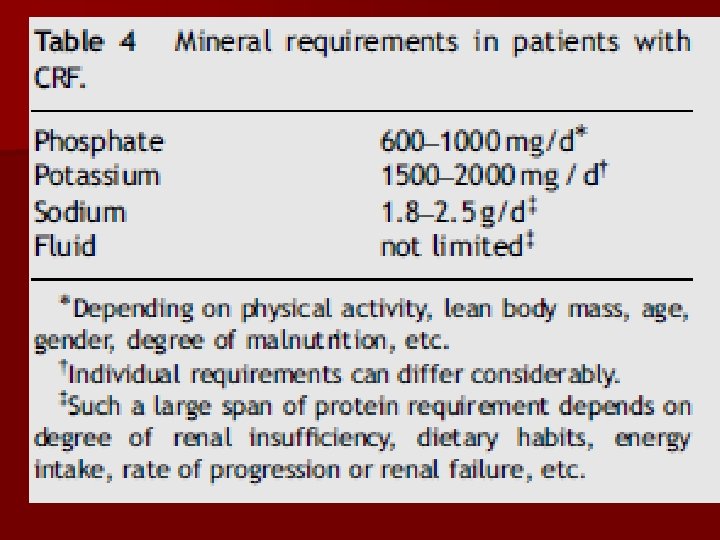
Sodium n 2 -4 g/d (43 m. Eq = 1 g) n Variable with urine output and disease etiology n Evaluate effect on hypertension control and cardiac function
Potassium Accumulates in CKD stage 5 n Hyperkalemia →cardiac danger n Restrict to 2 -4 g/d (26 m. Eq=1 g) n
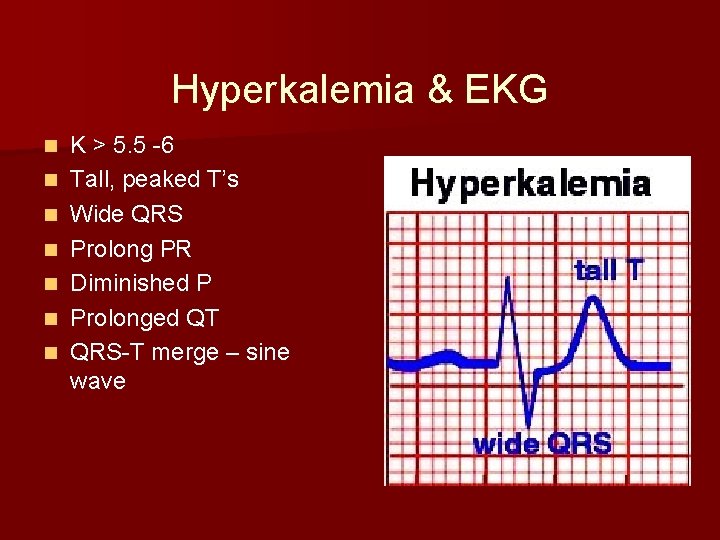
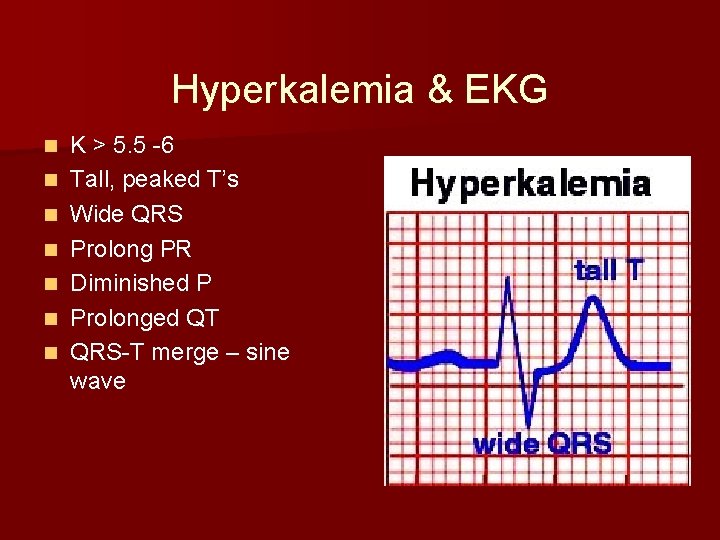
Hyperkalemia & EKG n n n n K > 5. 5 -6 Tall, peaked T’s Wide QRS Prolong PR Diminished P Prolonged QT QRS-T merge – sine wave
Hyperkalemia Symptoms n n n Weakness Lethargy Muscle cramps Paresthesias Hypoactive DTRs Dysrhythmias
Nutrition Implications of ARF n ARF causes anorexia, nausea, vomiting, bleeding n ARF causes rapid nitrogen loss and lean body mass loss (hypercatabolism) n ARF causes ↑ gluconeogenesis with insulin resistance n Dialysis causes loss of amino acids and protein n Uremia toxins cause impaired glucose utilization and protein synthesis
Treatment Goals for Renal Failure n n n n Correct electrolytes Control acidosis Treat significant hyperphosphatemia Treat symptomatic anemia Initiate dialysis for hyperkalemia or acidosis not controlled, fluid overload, ↑ in BUN>20 mg/dl/24 hours or BUN>100 mg/dl Evaluate drugs for renal effect Avoid/treat infection
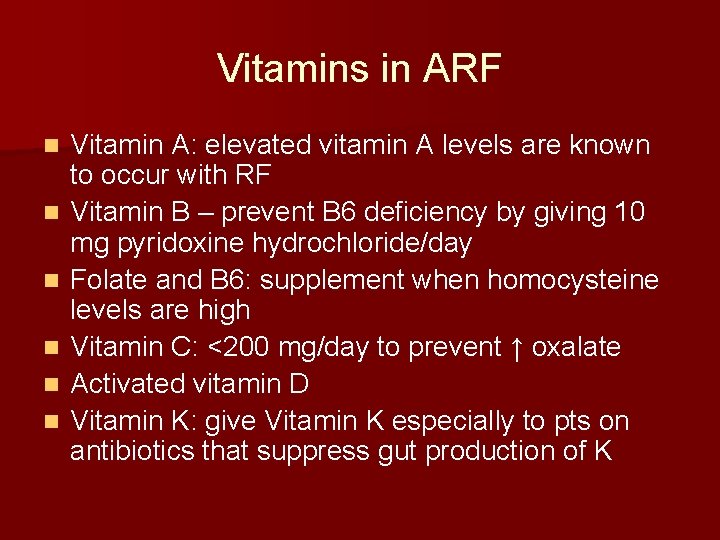
Vitamins in ARF n n n Vitamin A: elevated vitamin A levels are known to occur with RF Vitamin B – prevent B 6 deficiency by giving 10 mg pyridoxine hydrochloride/day Folate and B 6: supplement when homocysteine levels are high Vitamin C: <200 mg/day to prevent ↑ oxalate Activated vitamin D Vitamin K: give Vitamin K especially to pts on antibiotics that suppress gut production of K
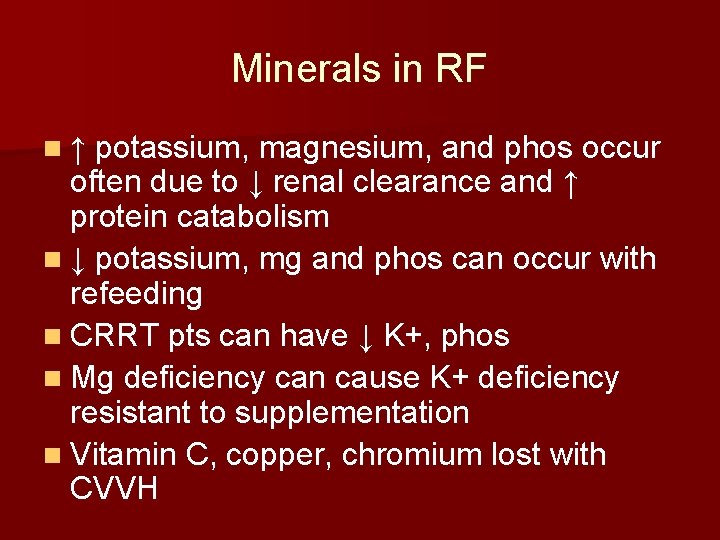
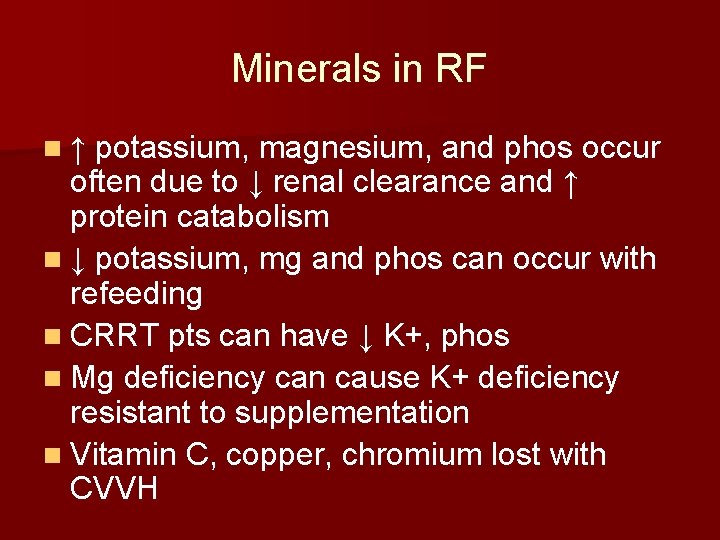
Minerals in RF n ↑ potassium, magnesium, and phos occur often due to ↓ renal clearance and ↑ protein catabolism n ↓ potassium, mg and phos can occur with refeeding n CRRT pts can have ↓ K+, phos n Mg deficiency can cause K+ deficiency resistant to supplementation n Vitamin C, copper, chromium lost with CVVH
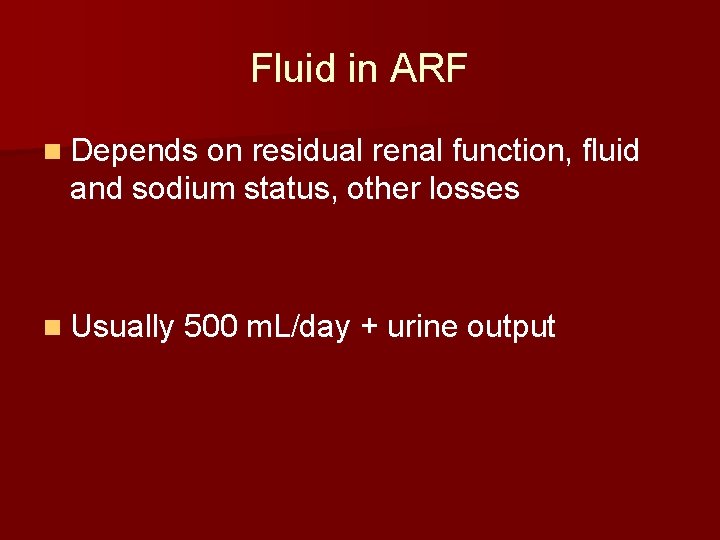
Fluid in ARF n Depends on residual renal function, fluid and sodium status, other losses n Usually 500 m. L/day + urine output
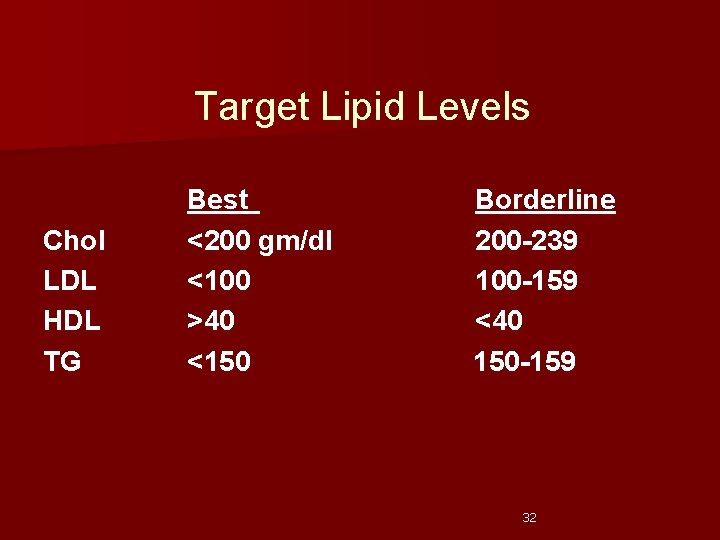
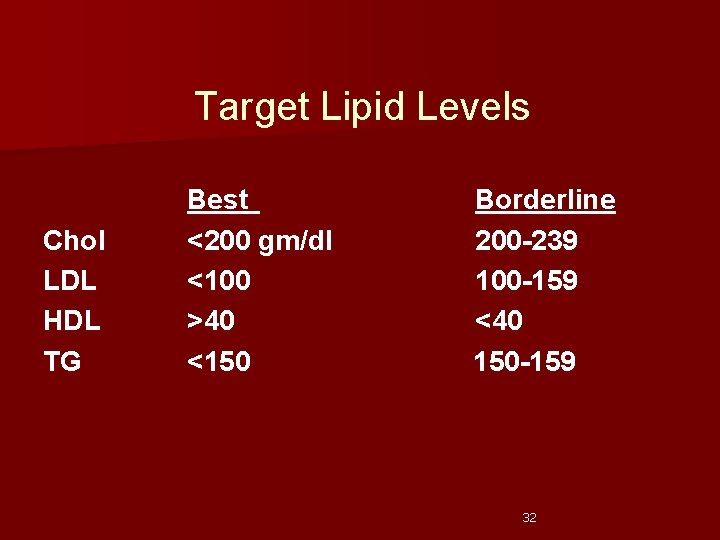
Target Lipid Levels Chol LDL HDL TG Best <200 gm/dl <100 >40 <150 Borderline 200 -239 100 -159 <40 150 -159 32
Dialysis Done be either hemodialysis or peritoneal dialysis. Hemodialysis requires permanent access to the bloodstream through a fistula. Hemodialysis is done 3 times a week for 3 -5 hours at a time. 33
Dialysis Peritoneal dialysis makes use of the peritoneal cavity. Less efficient than hemodialysis. Treatments usually last about 10 to 12 hours a day, 3 times a week. Complications include peritonitis, hypotension, weight gain. 34
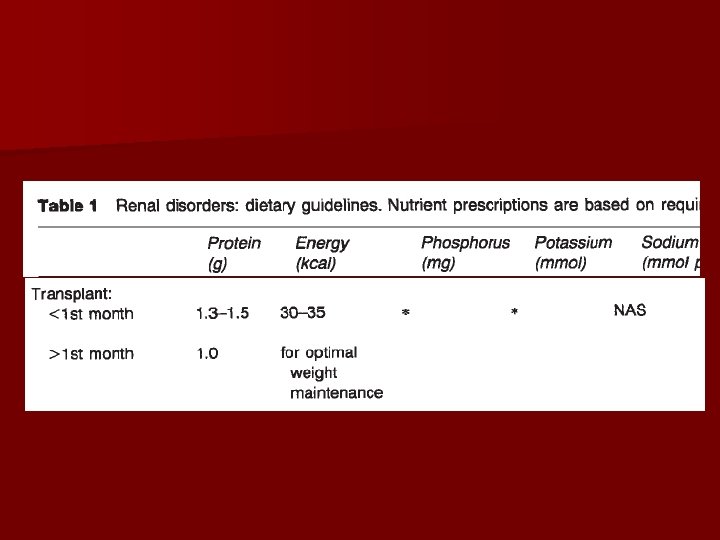
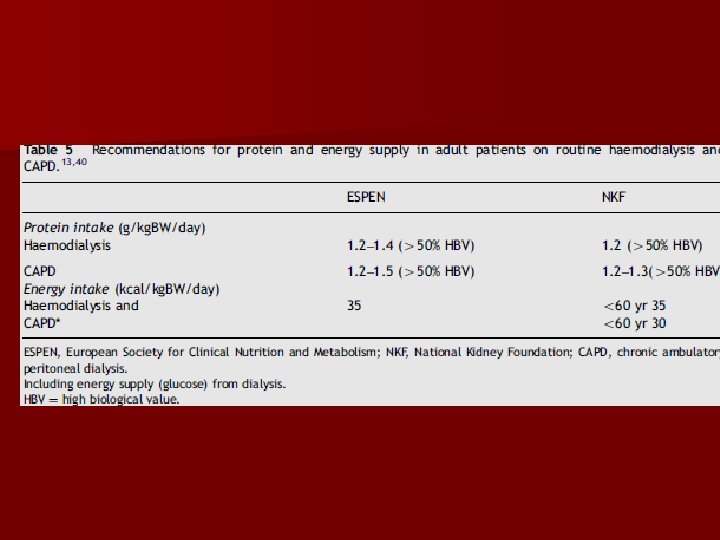
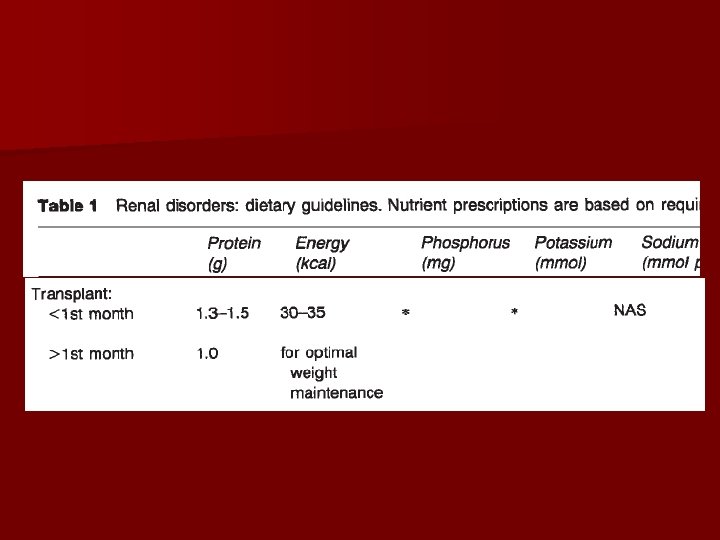
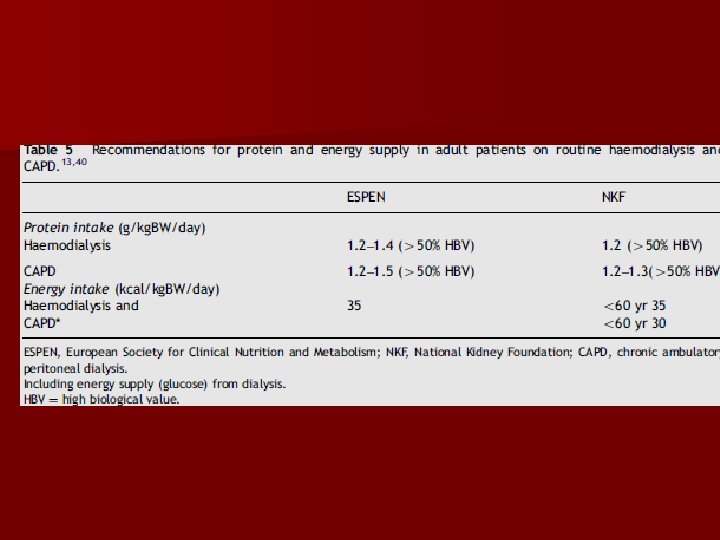
Diet During Dialysis clients may need additional protein. Amount must be carefully controlled. Hemodialysis: 1. 0 to 1. 2 g/kg of protein to make up for losses during dialysis. Peritoneal dialysis: 1. 2 to 1. 5 g/kg protein. 35
Diet During Dialysis 75% of this protein should be high biological value (HBV) protein, found in eggs, meat, fish, poultry, milk, and cheese. Potassium is usually restricted. A typical renal diet could be written as “ 80 -3 -3” which means 80 g protein, 3 g sodium, and 3 g potassium daily. 36

 Kidney function test name
Kidney function test name Kangaroo rat loop of henle
Kangaroo rat loop of henle 7 functions of the kidney
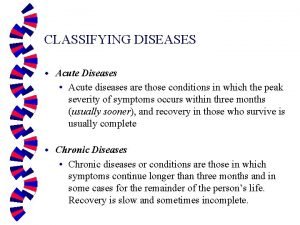
7 functions of the kidney Types of diseases
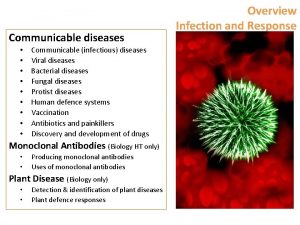
Types of diseases Two quality gurus
Two quality gurus Protein deficiency diseases
Protein deficiency diseases Natural history of diseases
Natural history of diseases Lifestyle modern
Lifestyle modern Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Inflammation of mfa ppt
Inflammation of mfa ppt Iceberg phenomenon of disease
Iceberg phenomenon of disease Human diseases a systemic approach
Human diseases a systemic approach Venn diagram of communicable and noncommunicable diseases
Venn diagram of communicable and noncommunicable diseases Chapter 24 lesson 1 sexually transmitted diseases
Chapter 24 lesson 1 sexually transmitted diseases Classification of periapical diseases
Classification of periapical diseases Section 19-3 diseases caused by bacteria and viruses
Section 19-3 diseases caused by bacteria and viruses Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders Chapter 32 childhood communicable diseases bioterrorism
Chapter 32 childhood communicable diseases bioterrorism Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Chapter 23 lesson 1 understanding communicable diseases
Chapter 23 lesson 1 understanding communicable diseases Chapter 22 genetics and genetically linked diseases
Chapter 22 genetics and genetically linked diseases Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Milady nail diseases and disorders
Milady nail diseases and disorders Chapter 10 lymphatic system diseases and disorders
Chapter 10 lymphatic system diseases and disorders X linked diseases
X linked diseases Whats sex linked
Whats sex linked Helminthic diseases
Helminthic diseases Hyperglyceremia
Hyperglyceremia Nutritional diseases
Nutritional diseases Nutritional diseases
Nutritional diseases King of diseases
King of diseases Retrocuspid papilla
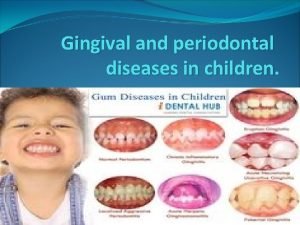
Retrocuspid papilla Non communicable diseases
Non communicable diseases