Use of oximes in the management of organophosphorus
![Wilson’s work in early 1950 s [BBA 1955] Nicotinohydroxamic acid methiodide 2 pyridine aldoxime Wilson’s work in early 1950 s [BBA 1955] Nicotinohydroxamic acid methiodide 2 pyridine aldoxime](https://slidetodoc.com/presentation_image_h2/2bc3367489b7aad2c77ff369322256bb/image-3.jpg)
![Wilson’s work in early 1950 s [BBA 1955] Lu. H 6 Wilson’s work in early 1950 s [BBA 1955] Lu. H 6](https://slidetodoc.com/presentation_image_h2/2bc3367489b7aad2c77ff369322256bb/image-4.jpg)
![[PAM] 20 mg/L = 75 µMol [PAM] 20 mg/L = 75 µMol](https://slidetodoc.com/presentation_image_h2/2bc3367489b7aad2c77ff369322256bb/image-10.jpg)










- Slides: 48
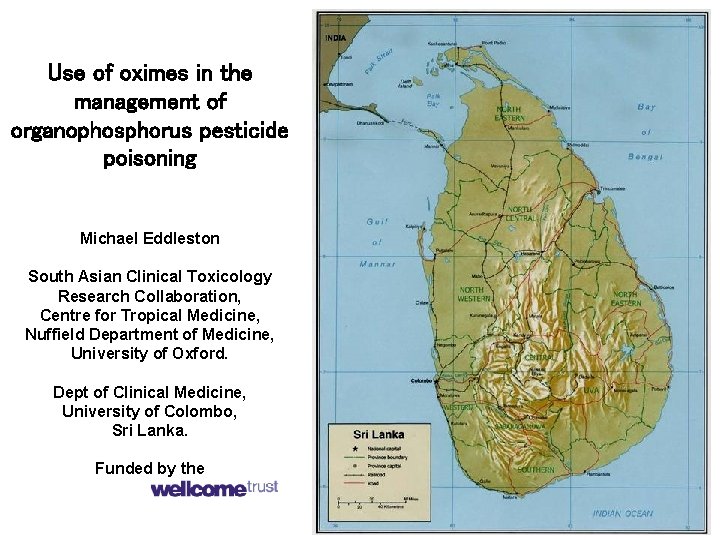
Use of oximes in the management of organophosphorus pesticide poisoning Michael Eddleston South Asian Clinical Toxicology Research Collaboration, Centre for Tropical Medicine, Nuffield Department of Medicine, University of Oxford. Dept of Clinical Medicine, University of Colombo, Sri Lanka. Funded by the
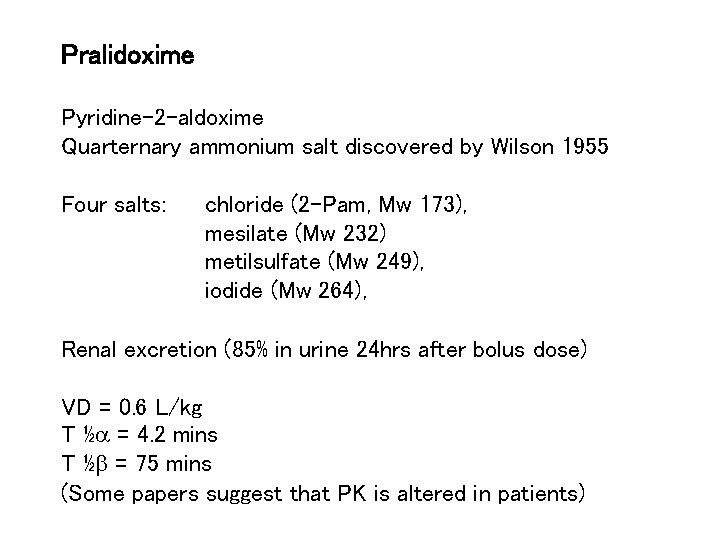
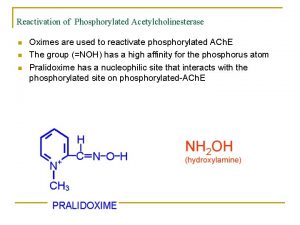
Pralidoxime Pyridine-2 -aldoxime Quarternary ammonium salt discovered by Wilson 1955 Four salts: chloride (2 -Pam, Mw 173), mesilate (Mw 232) metilsulfate (Mw 249), iodide (Mw 264), Renal excretion (85% in urine 24 hrs after bolus dose) VD = 0. 6 L/kg T ½a = 4. 2 mins T ½b = 75 mins (Some papers suggest that PK is altered in patients)
![Wilsons work in early 1950 s BBA 1955 Nicotinohydroxamic acid methiodide 2 pyridine aldoxime Wilson’s work in early 1950 s [BBA 1955] Nicotinohydroxamic acid methiodide 2 pyridine aldoxime](https://slidetodoc.com/presentation_image_h2/2bc3367489b7aad2c77ff369322256bb/image-3.jpg)
Wilson’s work in early 1950 s [BBA 1955] Nicotinohydroxamic acid methiodide 2 pyridine aldoxime methiodide [2 pralidoxime methiodide, 2 -PAM]
![Wilsons work in early 1950 s BBA 1955 Lu H 6 Wilson’s work in early 1950 s [BBA 1955] Lu. H 6](https://slidetodoc.com/presentation_image_h2/2bc3367489b7aad2c77ff369322256bb/image-4.jpg)
Wilson’s work in early 1950 s [BBA 1955] Lu. H 6
Pralidoxime Pyridine-2 -aldoxime Quarternary ammonium salt discovered by Wilson 1955 Four salts: chloride (Mw 173), iodide (Mw 264), metilsulfate (Mw 249), mesilate (Mw 232) Renal excretion (85% in urine 24 hrs after bolus dose) VD = 0. 6 L/kg T ½a = 4. 2 mins T ½b = 75 mins (Some papers suggest that PK is altered in patients)
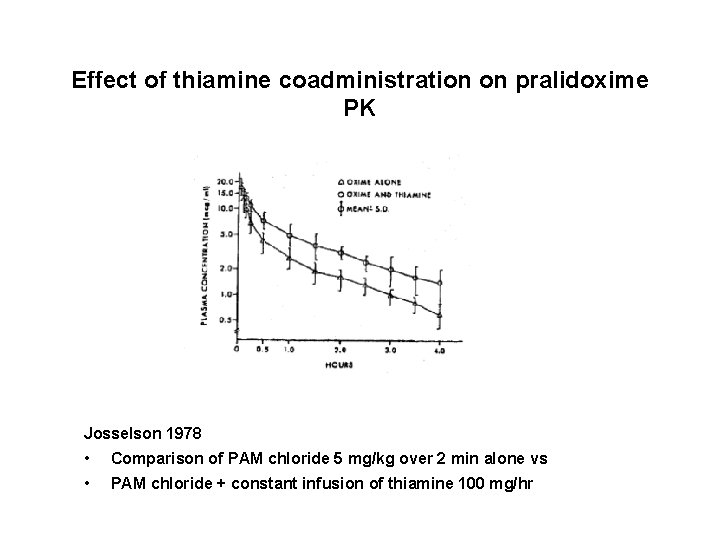
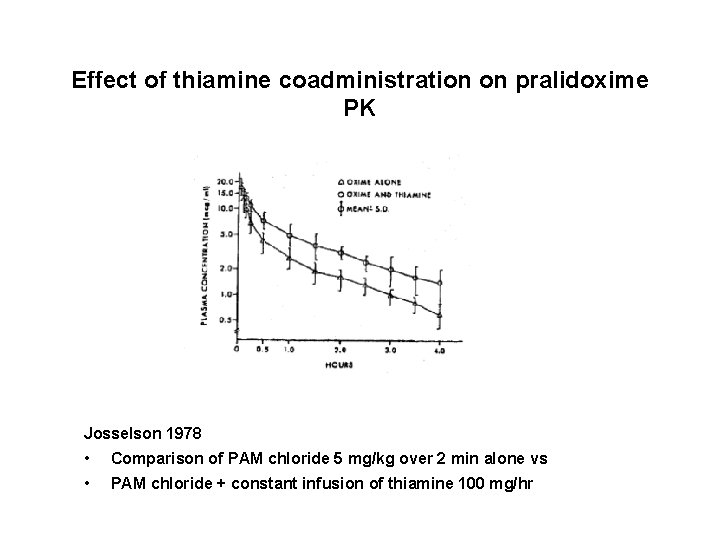
Effect of thiamine coadministration on pralidoxime PK Josselson 1978 • Comparison of PAM chloride 5 mg/kg over 2 min alone vs • PAM chloride + constant infusion of thiamine 100 mg/hr
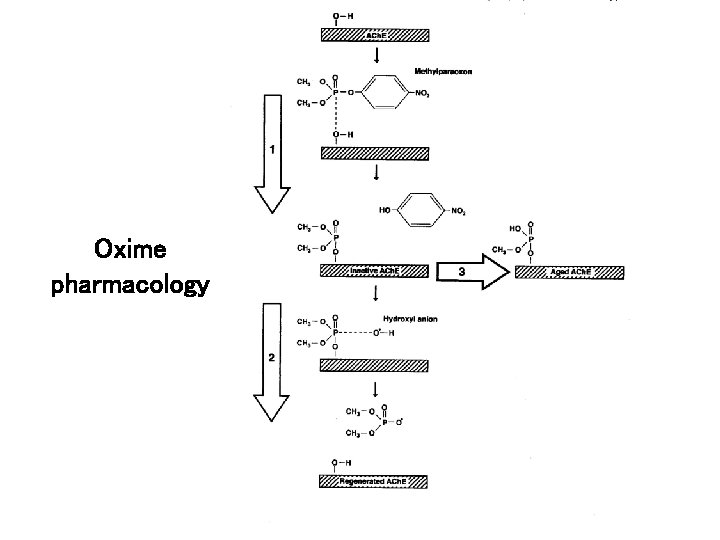
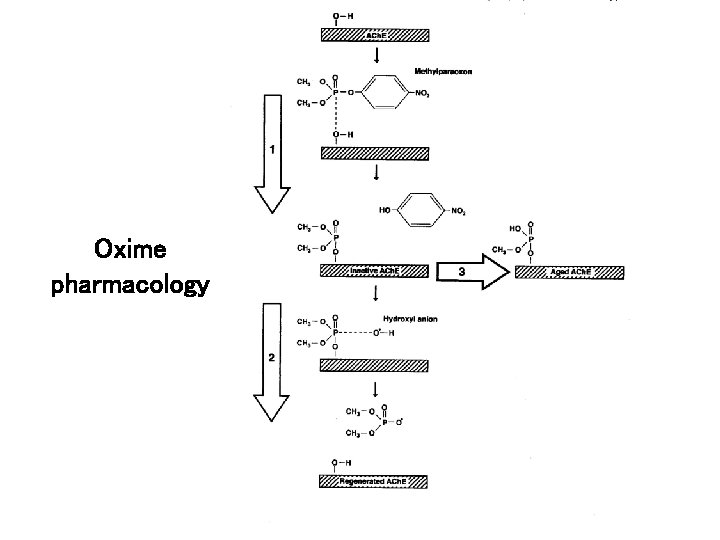
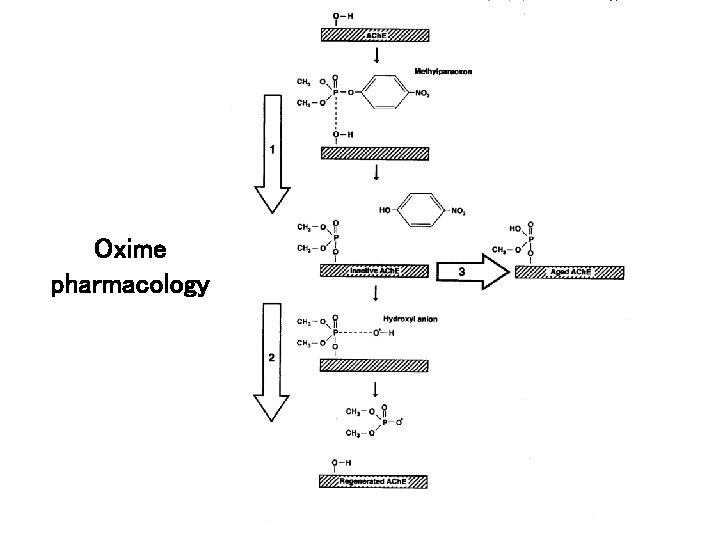
Oxime pharmacology
Pralidoxime First used clinically by Namba in 1956 Most textbooks now recommend a regimen of: 1 g over 5 -20 mins, repeated after 3 -8 hrs. Commonly given for just 24 hrs. However, many Asian clinicians doubt its effectiveness The World Health Organization responds that pralidoxime should be given. But what is the clinical trial evidence?
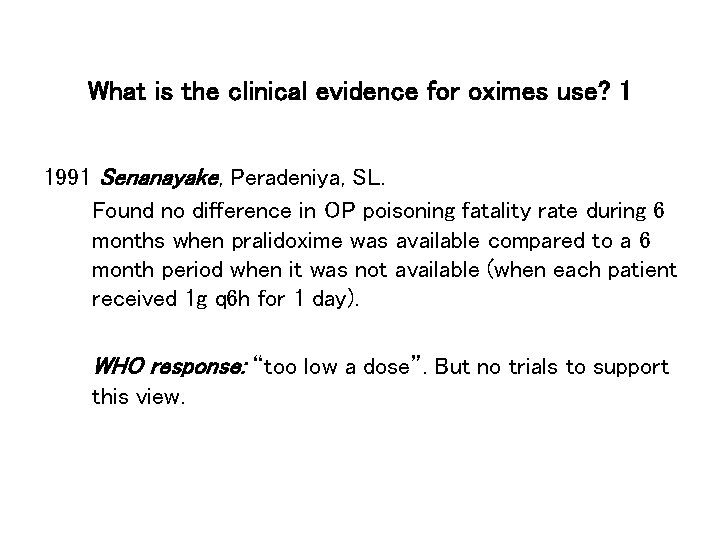
What is the clinical evidence for oximes use? 1 1991 Senanayake, Peradeniya, SL. Found no difference in OP poisoning fatality rate during 6 months when pralidoxime was available compared to a 6 month period when it was not available (when each patient received 1 g q 6 h for 1 day). WHO response: “too low a dose”. But no trials to support this view.
![PAM 20 mgL 75 µMol [PAM] 20 mg/L = 75 µMol](https://slidetodoc.com/presentation_image_h2/2bc3367489b7aad2c77ff369322256bb/image-10.jpg)
[PAM] 20 mg/L = 75 µMol
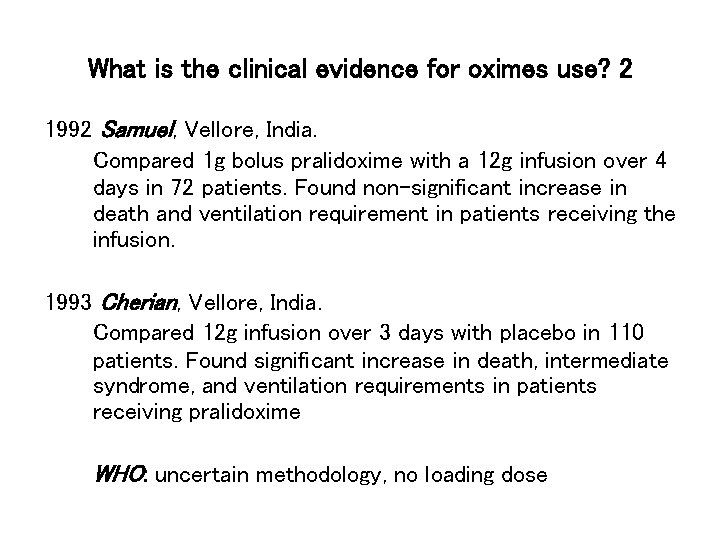
What is the clinical evidence for oximes use? 2 1992 Samuel, Vellore, India. Compared 1 g bolus pralidoxime with a 12 g infusion over 4 days in 72 patients. Found non-significant increase in death and ventilation requirement in patients receiving the infusion. 1993 Cherian, Vellore, India. Compared 12 g infusion over 3 days with placebo in 110 patients. Found significant increase in death, intermediate syndrome, and ventilation requirements in patients receiving pralidoxime WHO: uncertain methodology, no loading dose
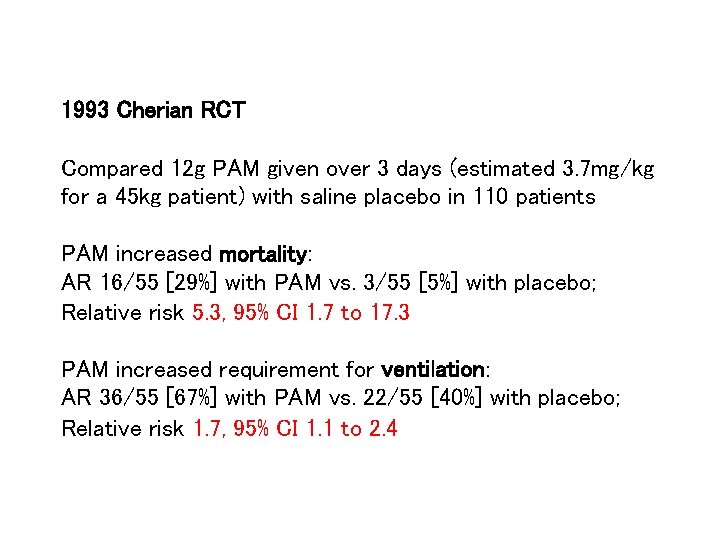
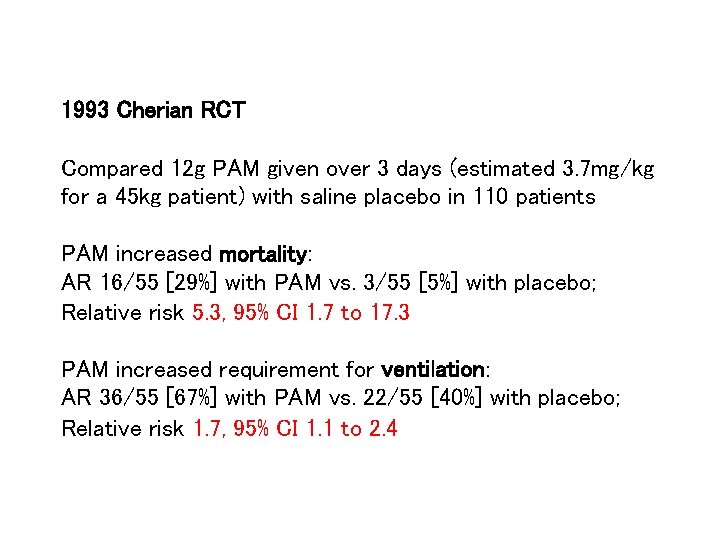
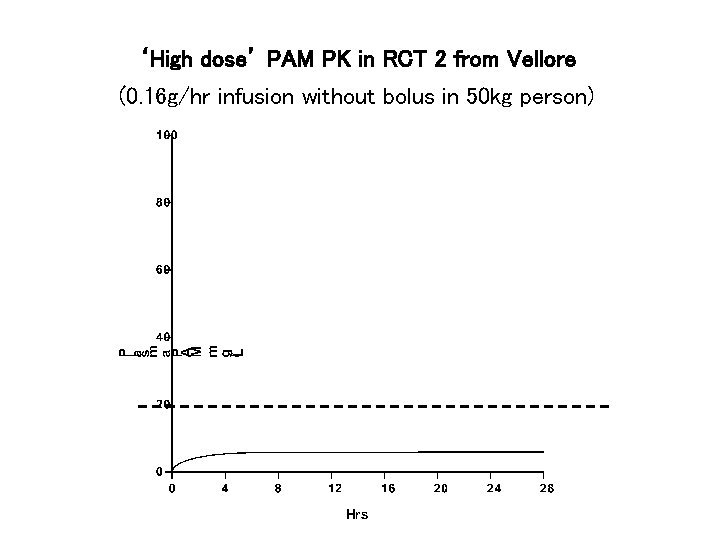
1993 Cherian RCT Compared 12 g PAM given over 3 days (estimated 3. 7 mg/kg for a 45 kg patient) with saline placebo in 110 patients PAM increased mortality: AR 16/55 [29%] with PAM vs. 3/55 [5%] with placebo; Relative risk 5. 3, 95% CI 1. 7 to 17. 3 PAM increased requirement for ventilation: AR 36/55 [67%] with PAM vs. 22/55 [40%] with placebo; Relative risk 1. 7, 95% CI 1. 1 to 2. 4
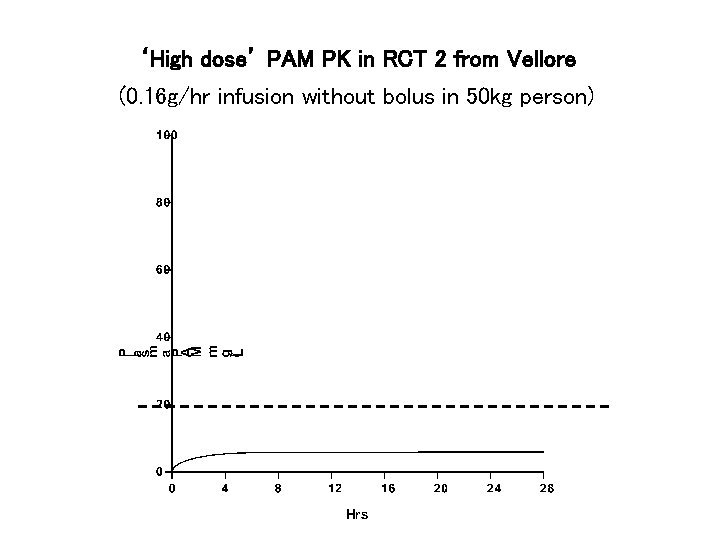
‘High dose’ PAM PK in RCT 2 from Vellore (0. 16 g/hr infusion without bolus in 50 kg person)
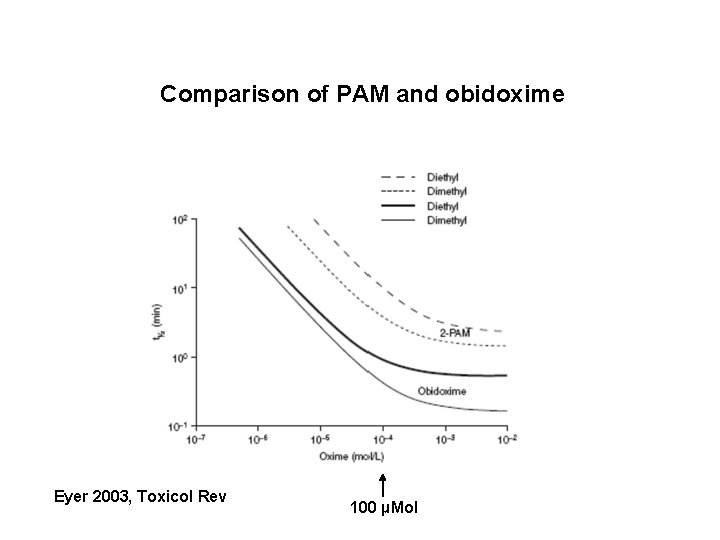
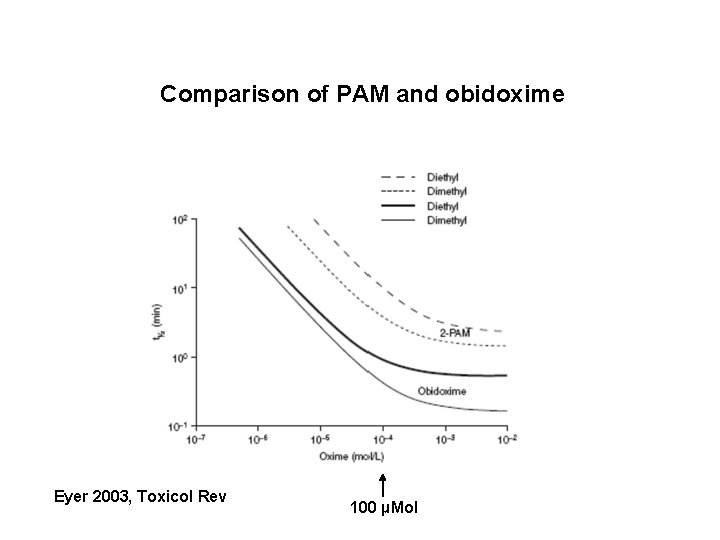
Comparison of PAM and obidoxime Eyer 2003, Toxicol Rev 100 µMol
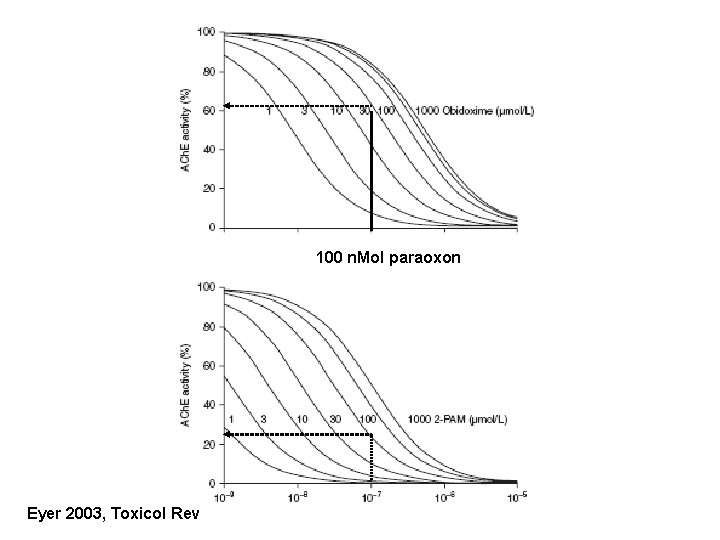
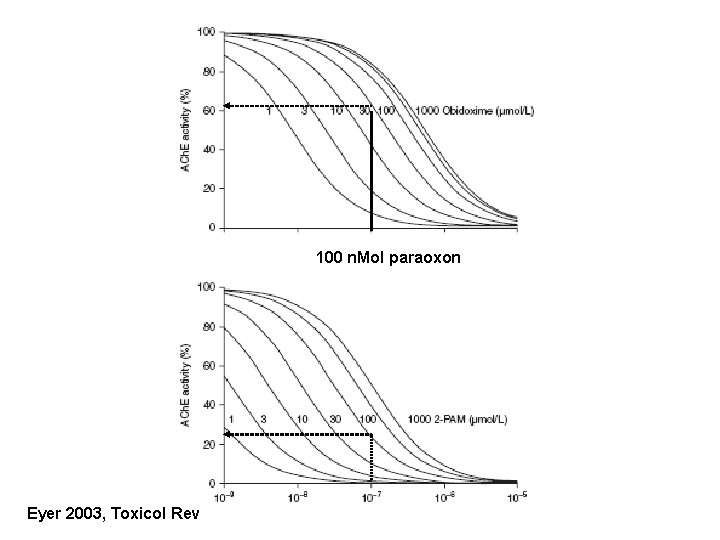
100 n. Mol paraoxon Eyer 2003, Toxicol Rev
There may also be differences between OPs in how they respond to oximes
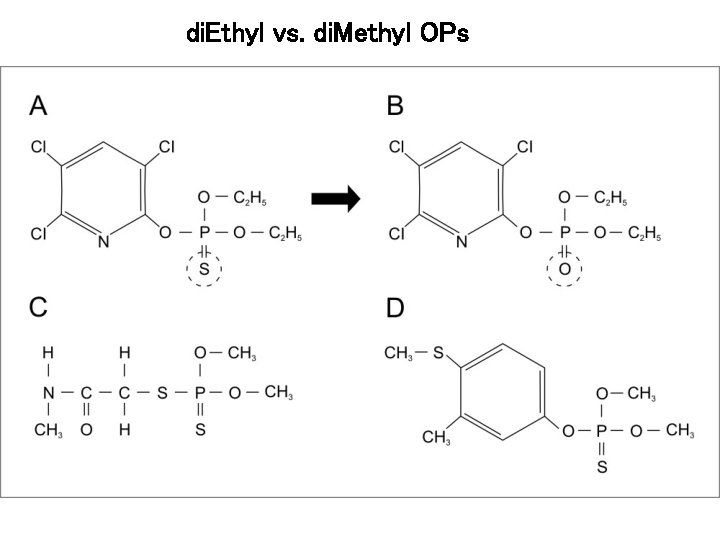
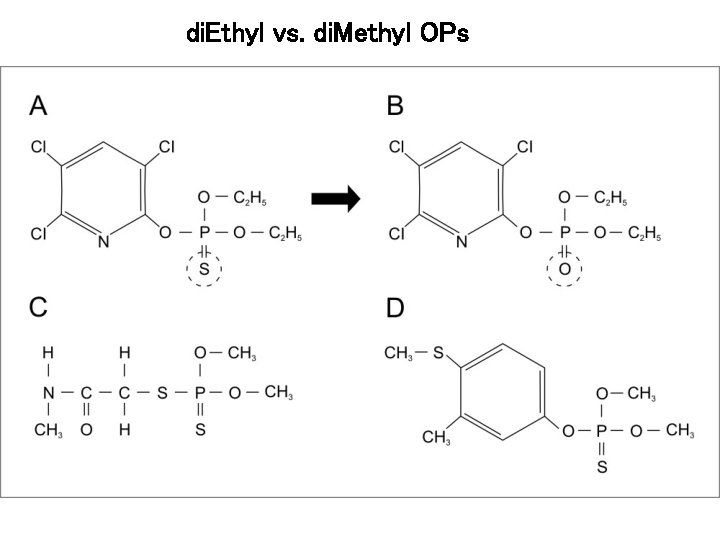
di. Ethyl vs. di. Methyl OPs
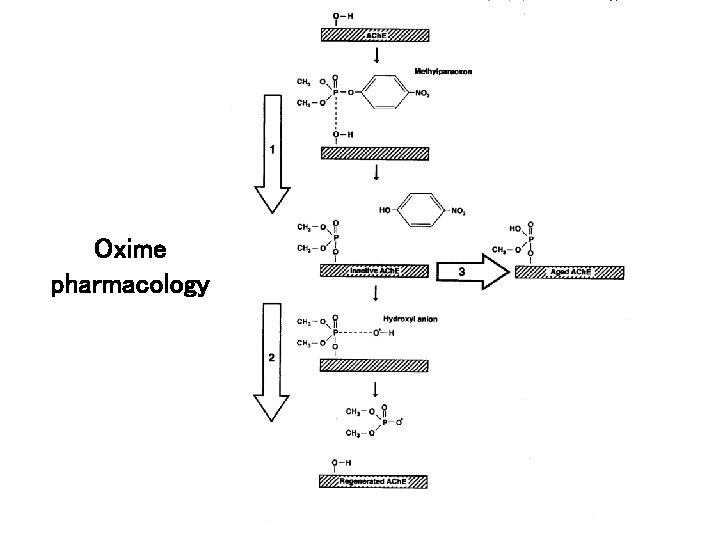
Oxime pharmacology
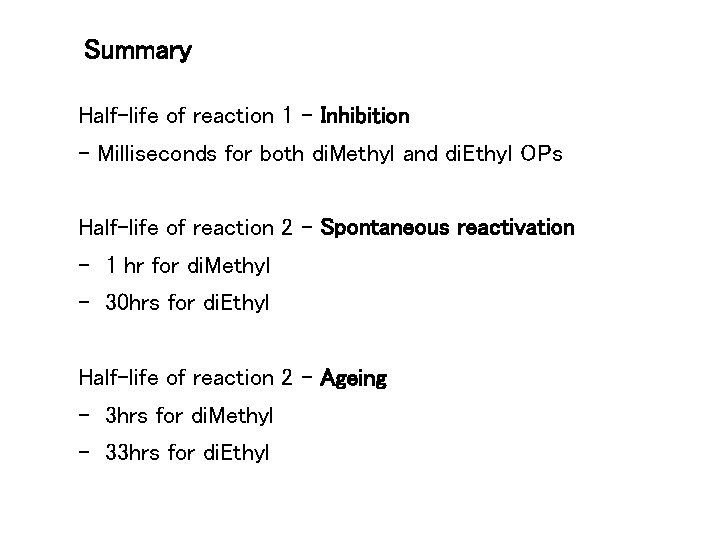
Summary Half-life of reaction 1 - Inhibition - Milliseconds for both di. Methyl and di. Ethyl OPs Half-life of reaction 2 - Spontaneous reactivation - 1 hr for di. Methyl - 30 hrs for di. Ethyl Half-life of reaction 2 - Ageing - 3 hrs for di. Methyl - 33 hrs for di. Ethyl
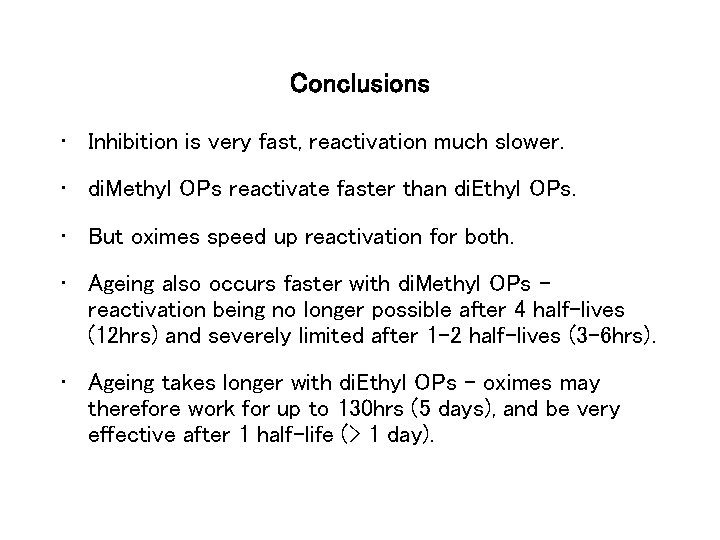
Conclusions • Inhibition is very fast, reactivation much slower. • di. Methyl OPs reactivate faster than di. Ethyl OPs. • But oximes speed up reactivation for both. • Ageing also occurs faster with di. Methyl OPs – reactivation being no longer possible after 4 half-lives (12 hrs) and severely limited after 1 -2 half-lives (3 -6 hrs). • Ageing takes longer with di. Ethyl OPs – oximes may therefore work for up to 130 hrs (5 days), and be very effective after 1 half-life (> 1 day).
Do we see any evidence of this variable response clinically?

Organophosphorus pesticide poisoning

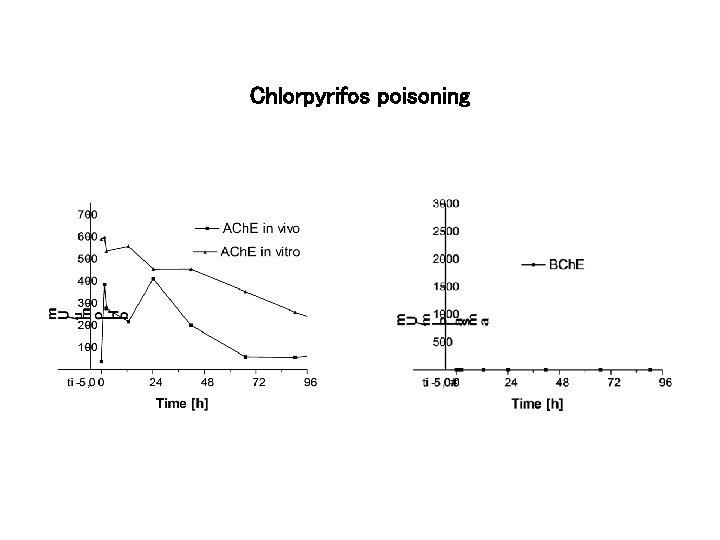
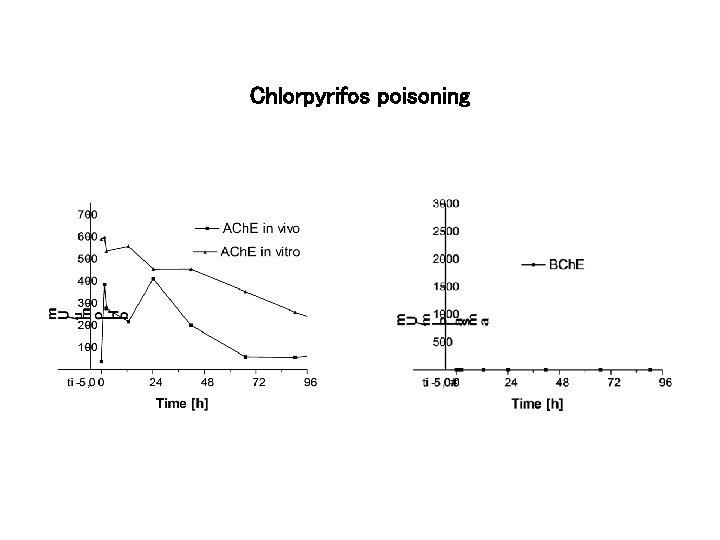
Chlorpyrifos poisoning
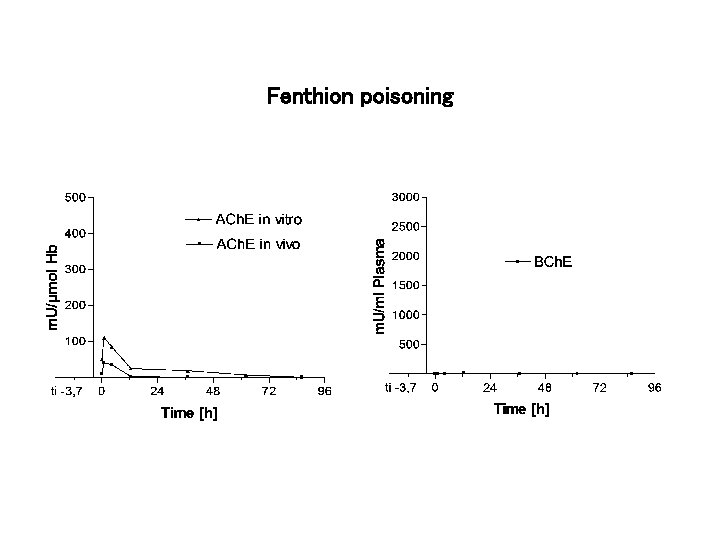
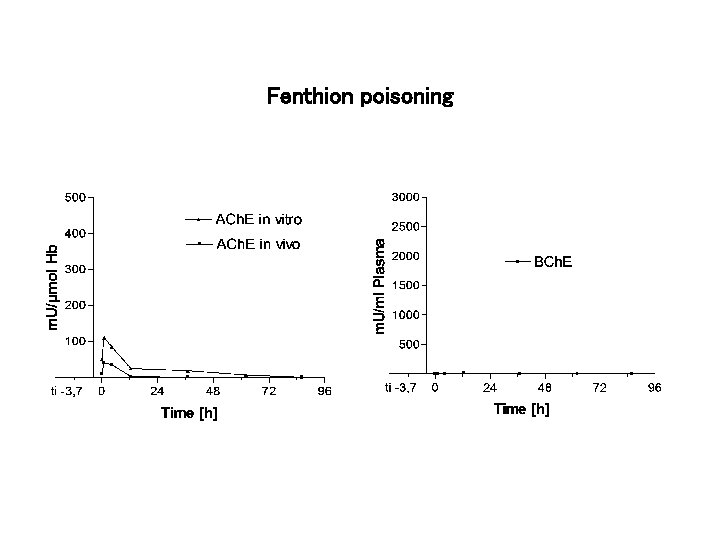
Fenthion poisoning
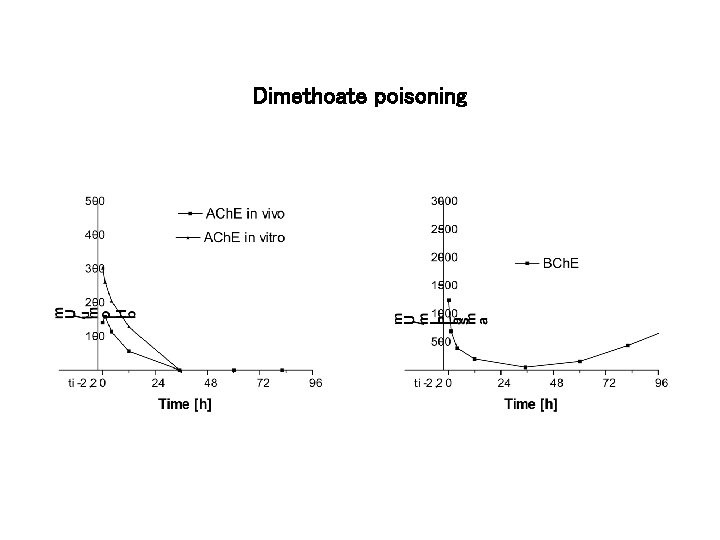
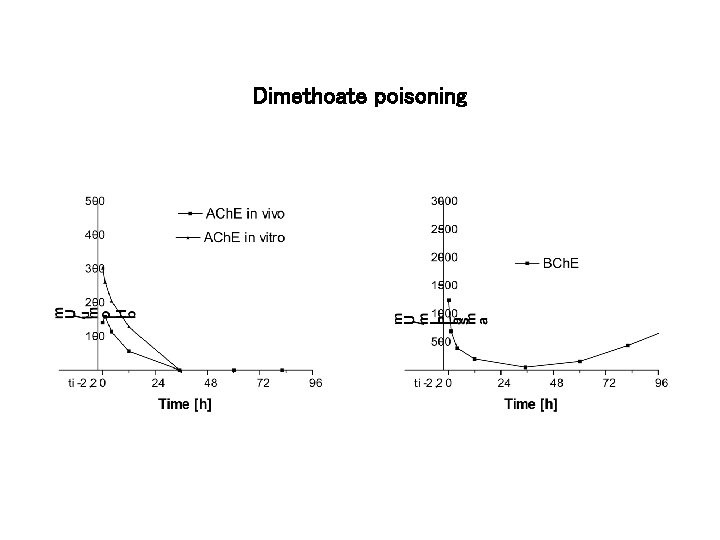
Dimethoate poisoning
Have we got the dose wrong for dimethoate?


Dimethoate poisoning in Munich
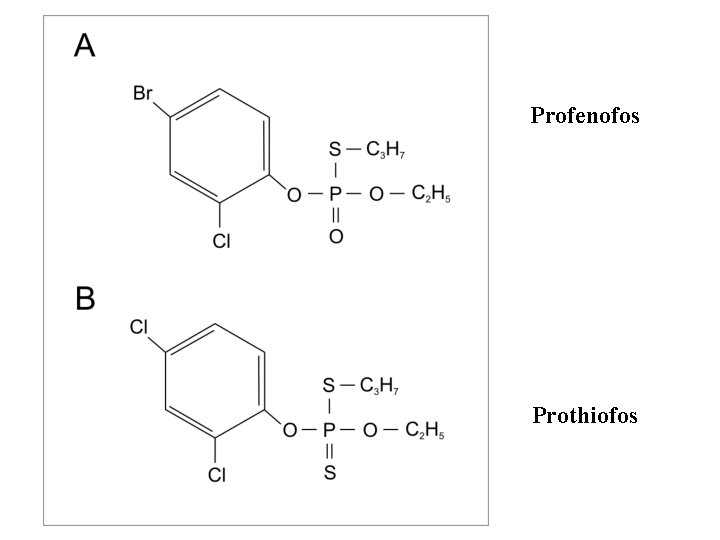
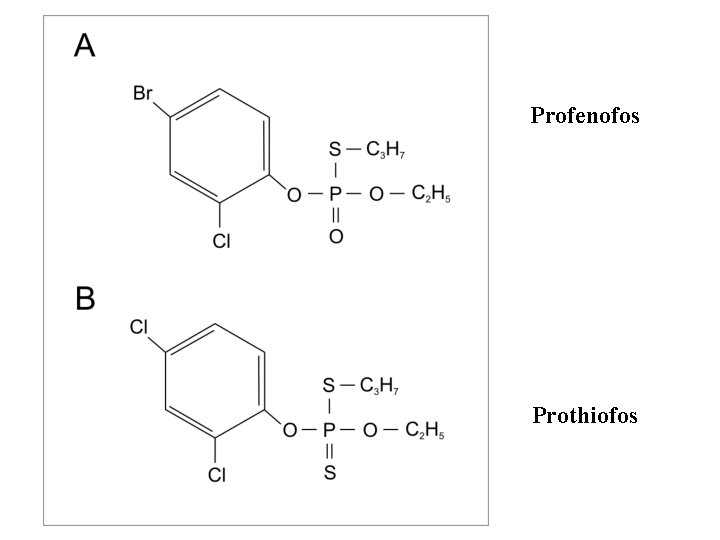
Profenofos Prothiofos
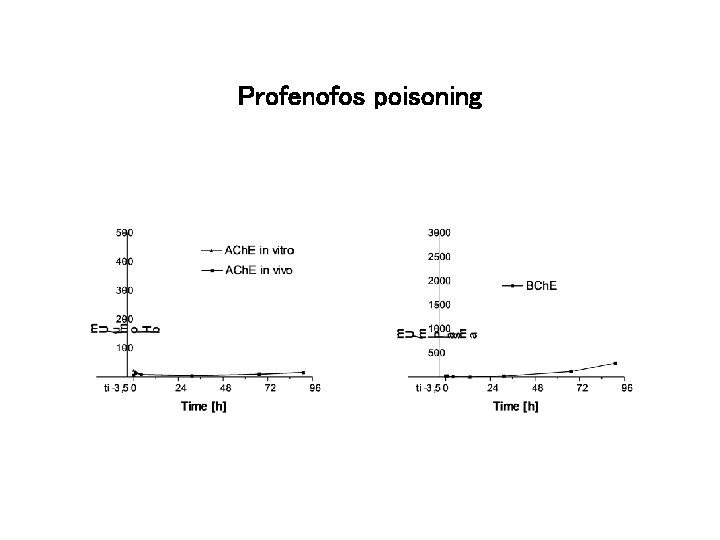
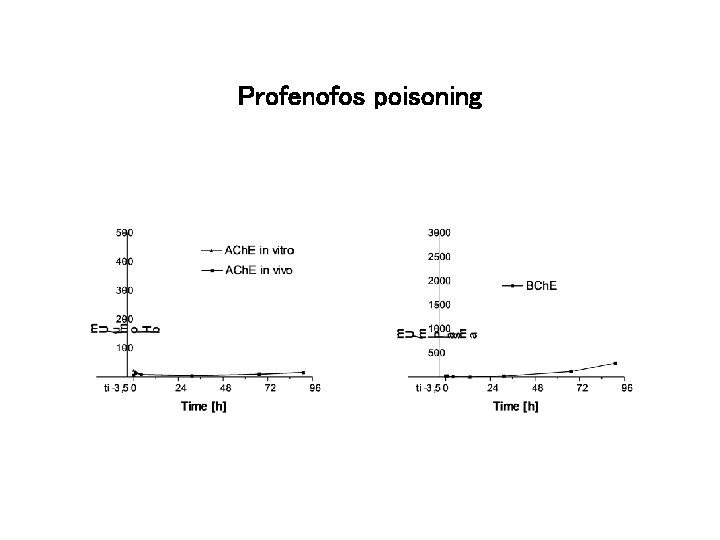
Profenofos poisoning
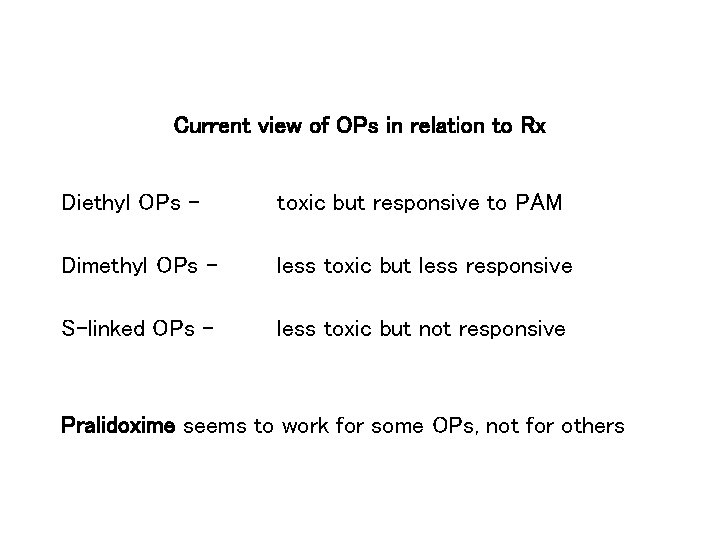
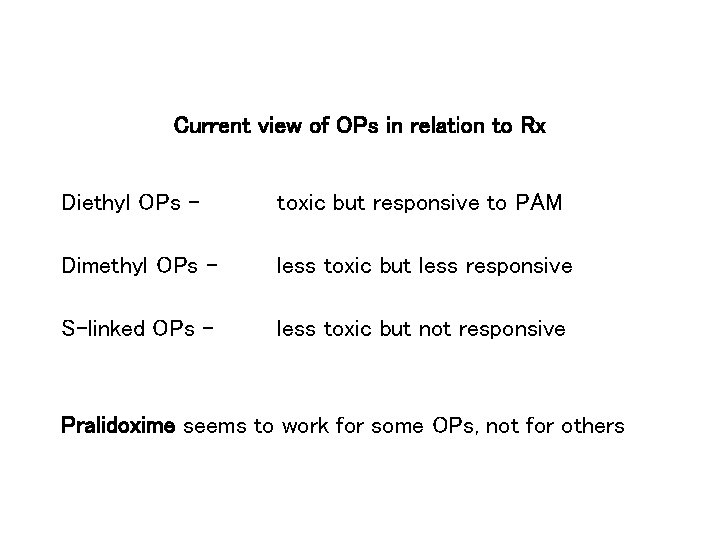
Current view of OPs in relation to Rx Diethyl OPs - toxic but responsive to PAM Dimethyl OPs - less toxic but less responsive S-linked OPs - less toxic but not responsive Pralidoxime seems to work for some OPs, not for others
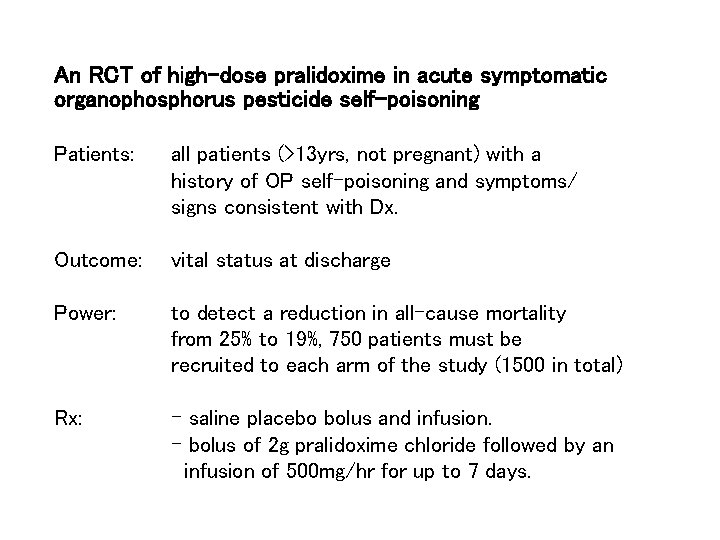
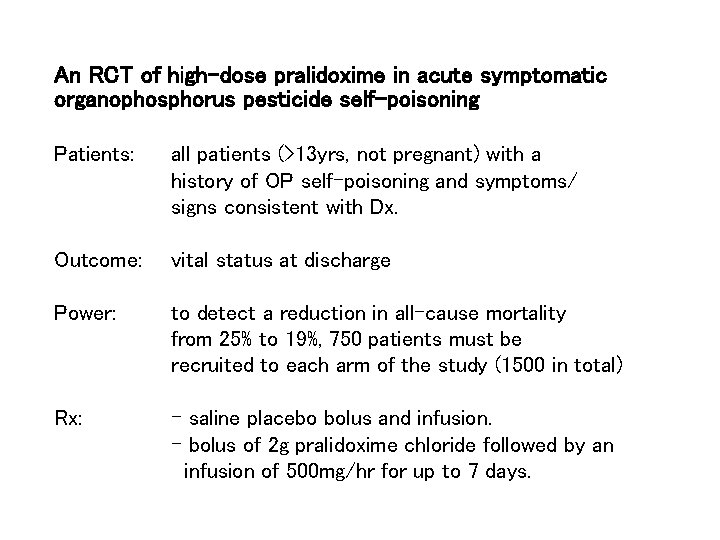
An RCT of high-dose pralidoxime in acute symptomatic organophosphorus pesticide self-poisoning Patients: all patients (>13 yrs, not pregnant) with a history of OP self-poisoning and symptoms/ signs consistent with Dx. Outcome: vital status at discharge Power: to detect a reduction in all-cause mortality from 25% to 19%, 750 patients must be recruited to each arm of the study (1500 in total) Rx: - saline placebo bolus and infusion. - bolus of 2 g pralidoxime chloride followed by an infusion of 500 mg/hr for up to 7 days.




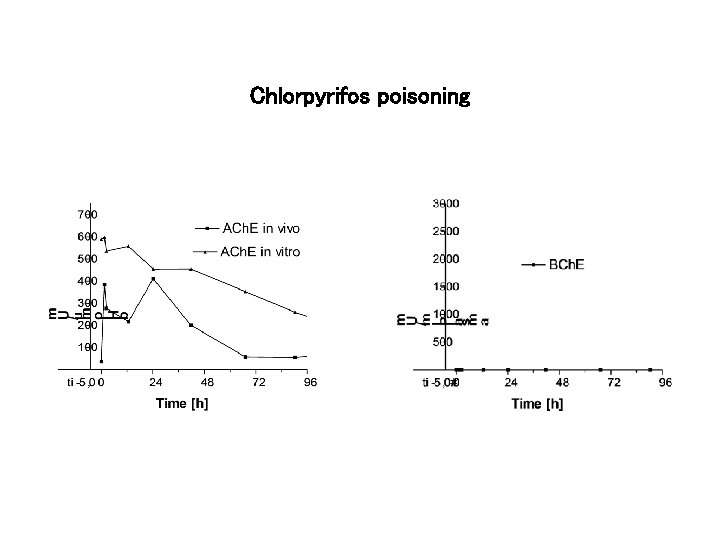
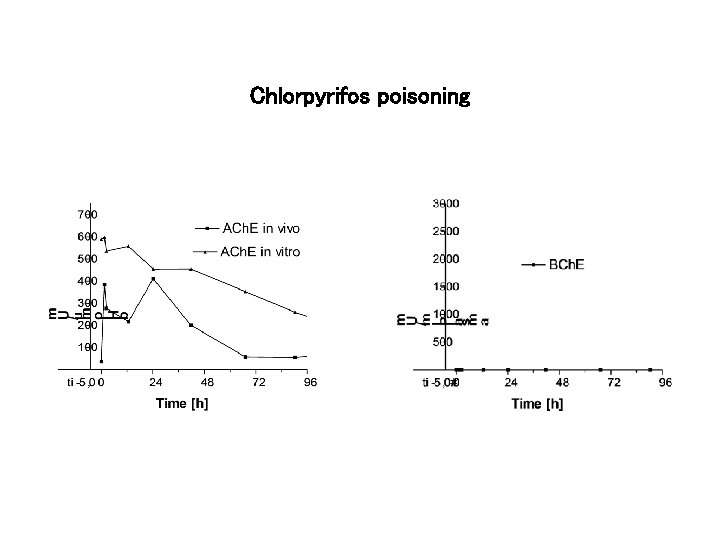
Chlorpyrifos poisoning

Parathion reactivation
Variation between OPs might be the reason why earlier trials did not find benefit from pralidoxime
• Another reason may be time to onset of poisoning • If the patient becomes severely ill SOON after ingestion, they may well lose consciousness and aspirate the pesticide, or stop breathing and suffer hypoxic brain damage, before hospital admission. • In this case, patients will die in hospital from aspiration pneumonia or hypoxic brain damage. • Provision of antidotes including pralidoxime will then be irrelevant.
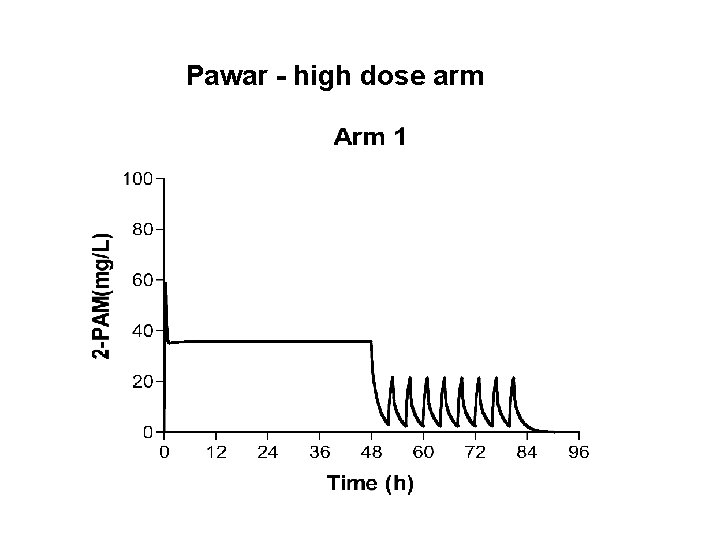
Lancet 368: 2136 • A recent study carried out by S Pawar and colleagues in Baramati, Maharashtra, suggests that very high doses of pralidoxime iodide may benefit many patients with di. Ethyl and di. Methyl OP poisoning who present early • RCT of 200 patients • All received 2 g loading dose, then for 48 hrs either 1 g infused over 1 hr every 1 hr or 1 g infused over 1 hr every 4 hrs followed by 1 g every 4 hours until off ventilator
Pawar - usual dose arm
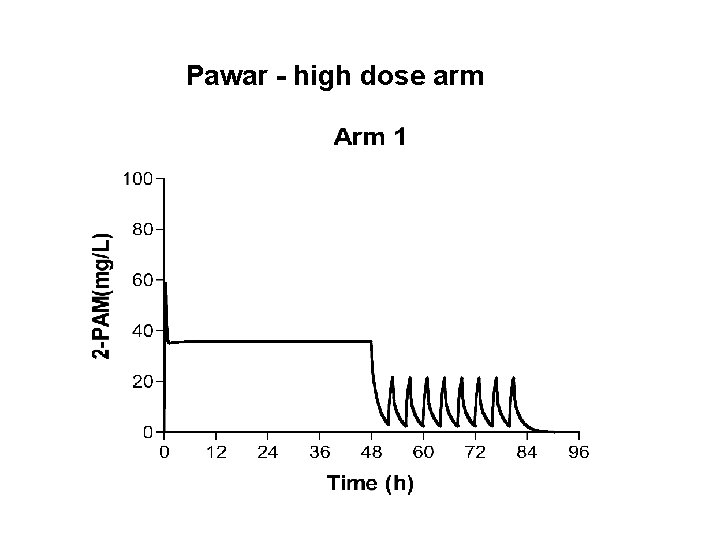
Pawar - high dose arm

Results • Case fatality: 8% in control group 1% in high dose group • Ventilation: median time 10 hrs in control group median time 3 hrs in high dose group • Interestingly, seemed to work for both dimethoate (di. Methyl OP) and chlorpyrifos (di. Ethyl OP). • The patients seem to have been moderately poisoned, with severely poisoned patients excluded. ? Valid for severely poisoned patients?
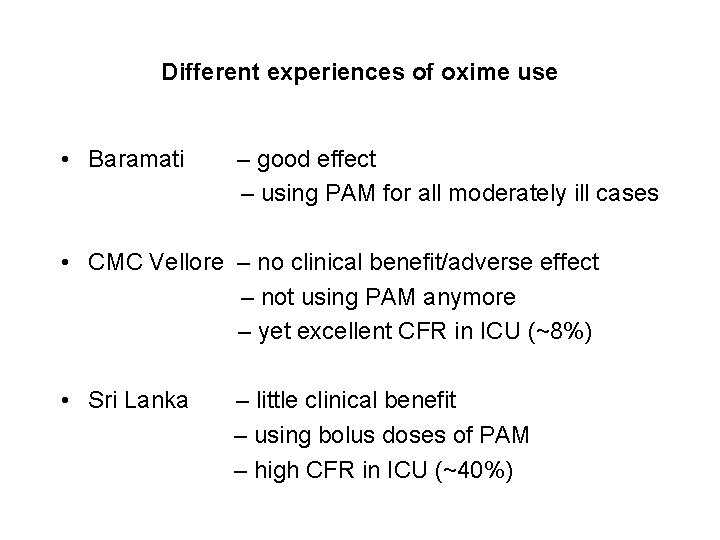
Different experiences of oxime use • Baramati – good effect – using PAM for all moderately ill cases • CMC Vellore – no clinical benefit/adverse effect – not using PAM anymore – yet excellent CFR in ICU (~8%) • Sri Lanka – little clinical benefit – using bolus doses of PAM – high CFR in ICU (~40%)
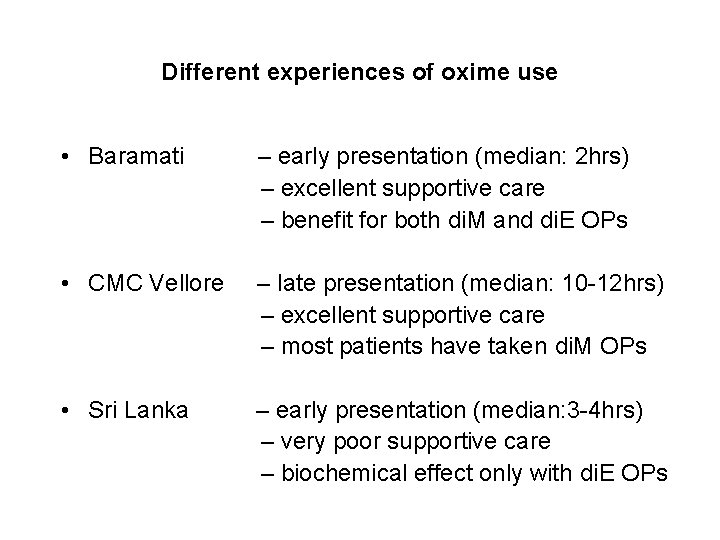
Different experiences of oxime use • Baramati – early presentation (median: 2 hrs) – excellent supportive care – benefit for both di. M and di. E OPs • CMC Vellore – late presentation (median: 10 -12 hrs) – excellent supportive care – most patients have taken di. M OPs • Sri Lanka – early presentation (median: 3 -4 hrs) – very poor supportive care – biochemical effect only with di. E OPs
Conclusions • The ideal regimen is likely to involve high doses and a bolus dose followed by an infusion However • the evidence base for pralidoxime use is weak • There is variable biochemical response to oximes by ACh. E inhibited by different OPs. • Some OPs may not respond at all • The time to presentation will affect whether pralidoxime is effective
 Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Tư thế worm breton là gì
Tư thế worm breton là gì Chúa yêu trần thế
Chúa yêu trần thế Môn thể thao bắt đầu bằng chữ f
Môn thể thao bắt đầu bằng chữ f Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Ví dụ về giọng cùng tên
Ví dụ về giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot Số nguyên là gì
Số nguyên là gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Scientific management
Scientific management Top management middle management first line management
Top management middle management first line management Top management middle management first line management
Top management middle management first line management Yesterday
Yesterday St. marys county land use and zoning lawyer
St. marys county land use and zoning lawyer Hospital management system software engineering
Hospital management system software engineering Use case diagram game
Use case diagram game