Sepsis and septic shock Sir Run Shaw Hospital



























- Slides: 78
Sepsis and septic shock Sir Run Shaw Hospital, 3 rd floor of critical care medicine Zhejiang university school of medicine Jian-cang Zhou M. D.
Sepsis and Septic Shock • Definitions • Epidemiology • Pathogenesis • Principles of management
Definition - SIRS • Systemic Inflammatory Response Syndrome – Manifested by 2 or more of the following: • • Temperature > 38°C (100. 4 F) or < 36°C (96. 8 F) HR > 90 BPM RR > 20/min or Pa. CO 2 < 32 mm Hg WBC 12, 000 or >10% bands Systemic
Definition - Sepsis • Sepsis – SIRS PLUS a documented infection • • Positive CXR Positive U/A Cellulitis /Abscess Positive Blood Culture
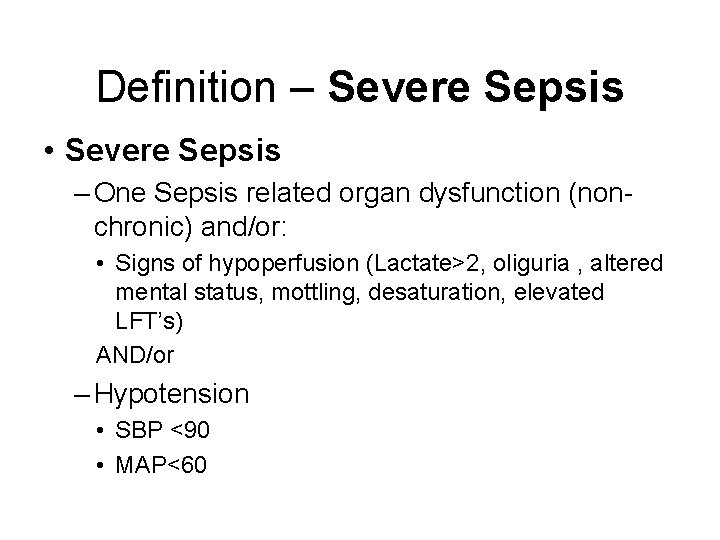
Definition – Severe Sepsis • Severe Sepsis – One Sepsis related organ dysfunction (nonchronic) and/or: • Signs of hypoperfusion (Lactate>2, oliguria , altered mental status, mottling, desaturation, elevated LFT’s) AND/or – Hypotension • SBP <90 • MAP<60
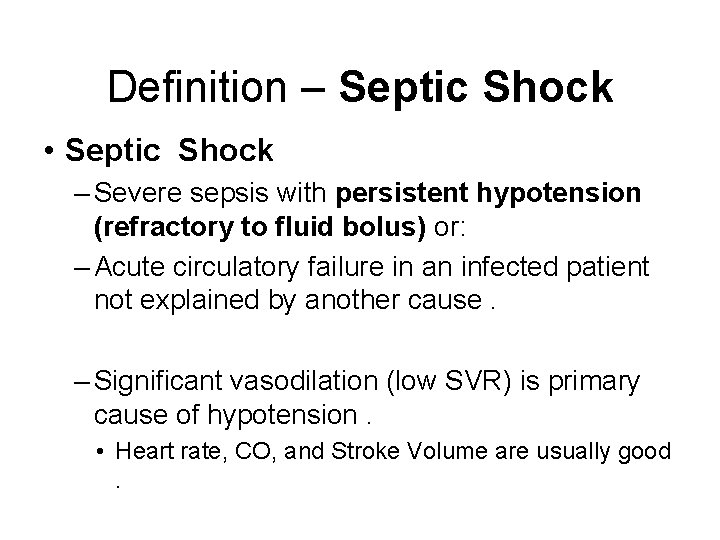
Definition – Septic Shock • Septic Shock – Severe sepsis with persistent hypotension (refractory to fluid bolus) or: – Acute circulatory failure in an infected patient not explained by another cause. – Significant vasodilation (low SVR) is primary cause of hypotension. • Heart rate, CO, and Stroke Volume are usually good.
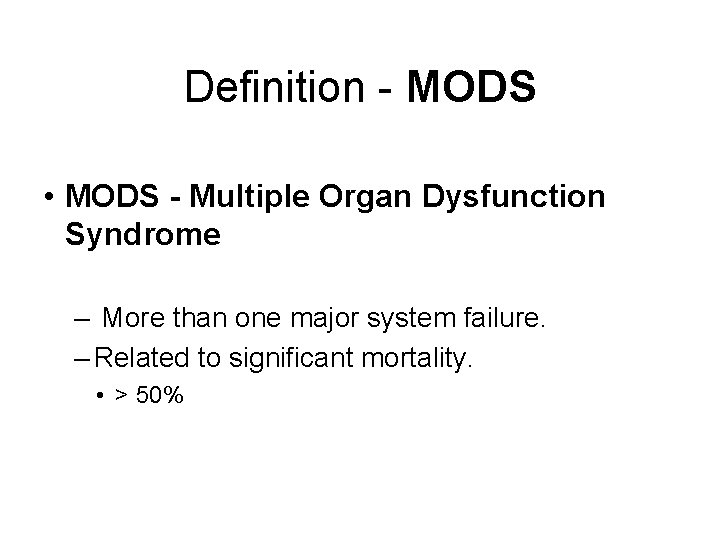
Definition - MODS • MODS - Multiple Organ Dysfunction Syndrome – More than one major system failure. – Related to significant mortality. • > 50%

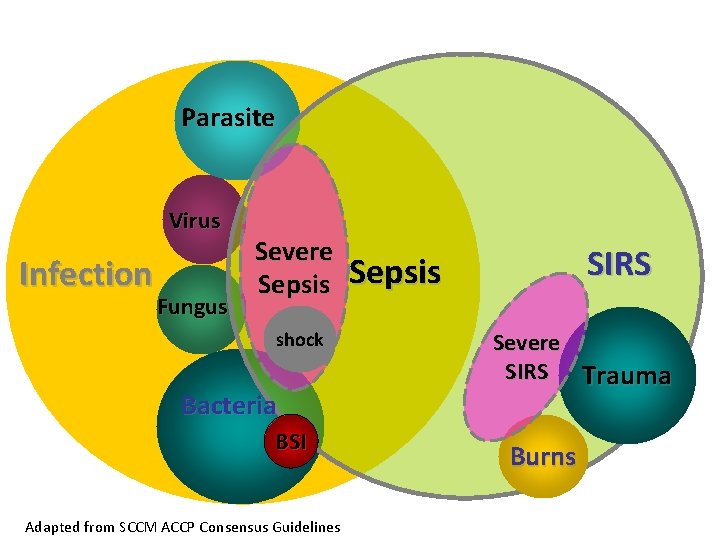
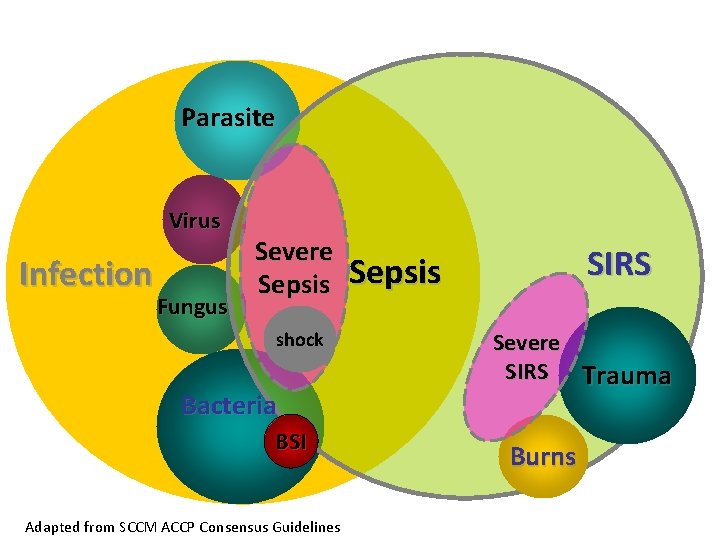
Parasite Virus Infection Fungus Severe Sepsis shock Bacteria BSI Adapted from SCCM ACCP Consensus Guidelines SIRS Sepsis Severe SIRS Trauma Burns
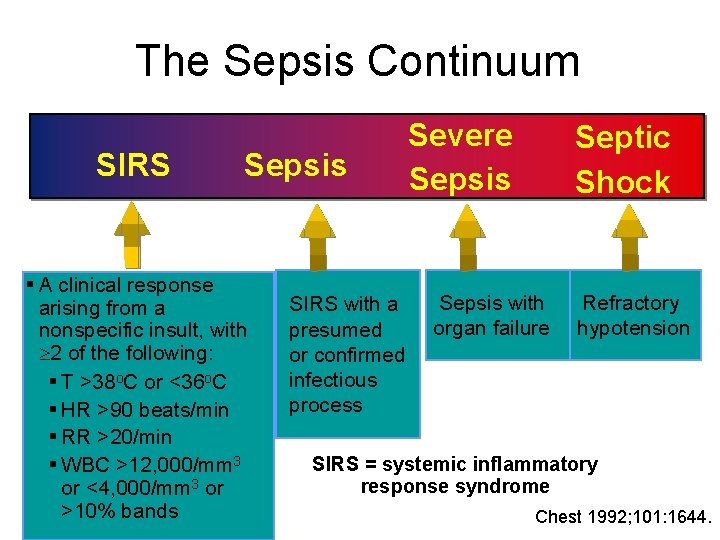
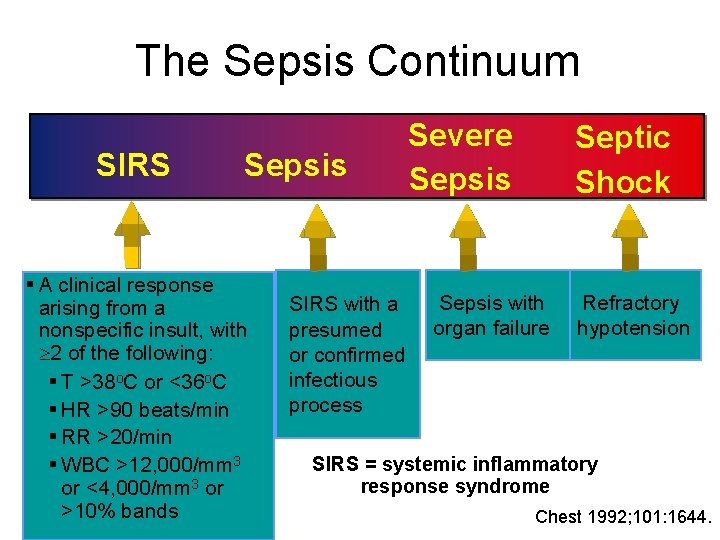
The Sepsis Continuum SIRS Sepsis § A clinical response arising from a nonspecific insult, with 2 of the following: § T >38 o. C or <36 o. C § HR >90 beats/min § RR >20/min § WBC >12, 000/mm 3 or <4, 000/mm 3 or >10% bands SIRS with a presumed or confirmed infectious process Severe Sepsis Septic Shock Sepsis with organ failure Refractory hypotension SIRS = systemic inflammatory response syndrome Chest 1992; 101: 1644.
Epidemiology

Comparable Global Epidemiology • 95 cases per 100, 000 – 2 week surveillance – 206 French ICUs • 95 cases per 100, 000 – 3 month survey – 23 Australian/New Zealand ICUs • 51 cases per 100, 000 – England, Wales and Northern Ireland.
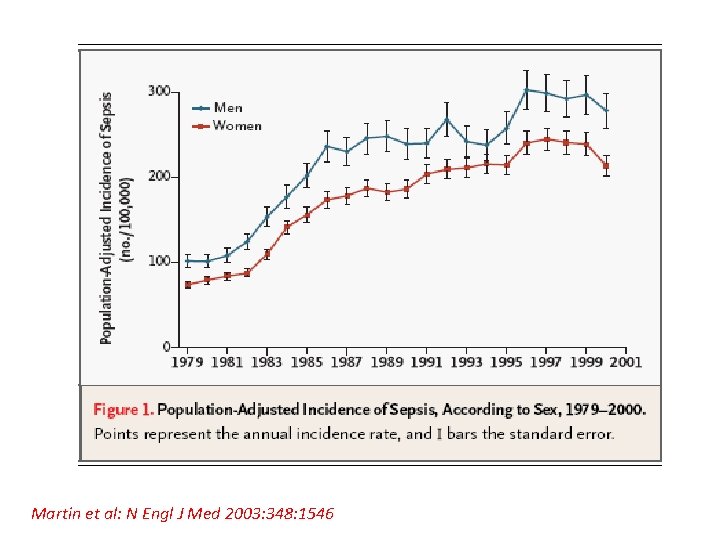
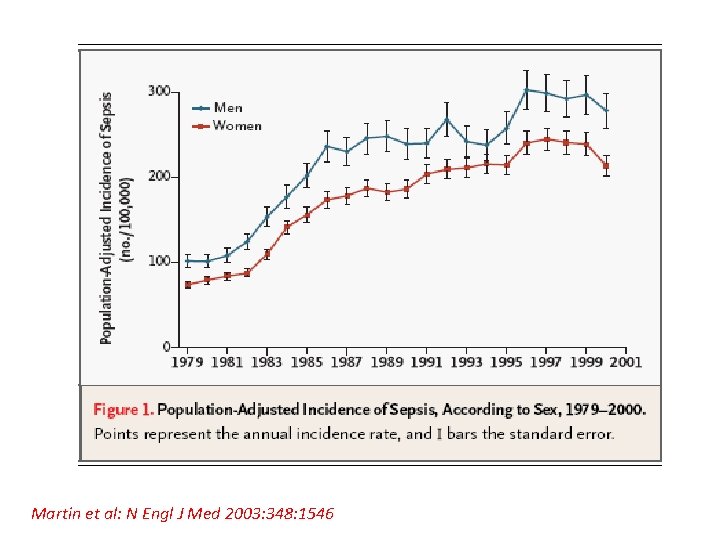
Martin et al: N Engl J Med 2003: 348: 1546
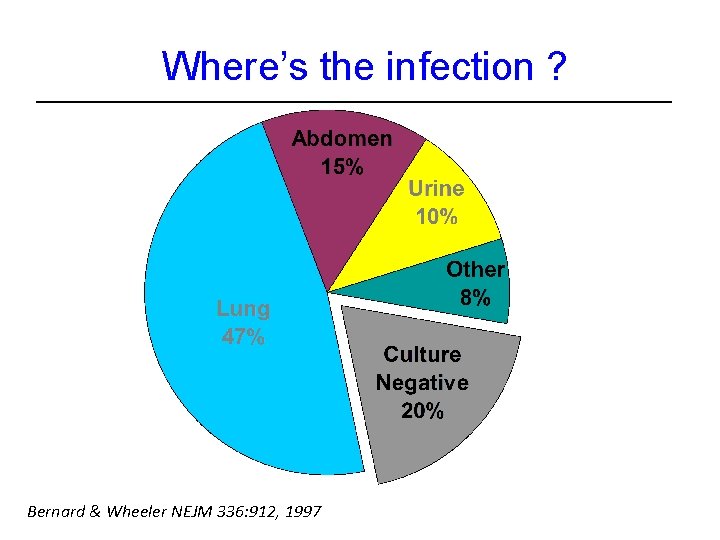
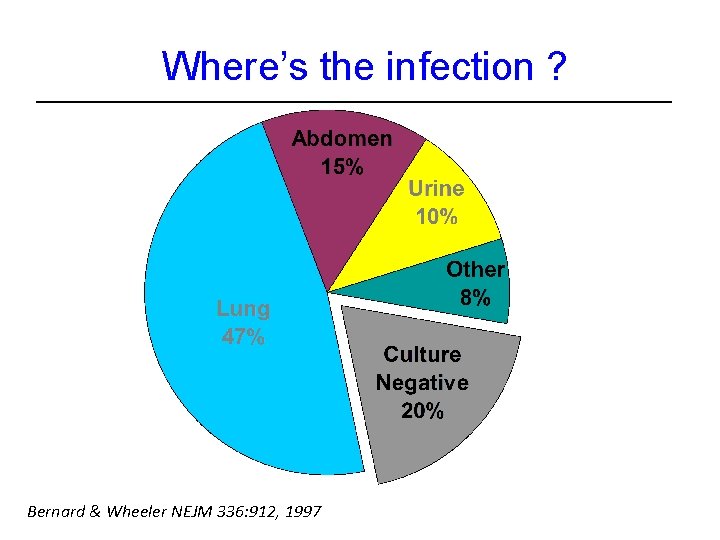
Where’s the infection ? Bernard & Wheeler NEJM 336: 912, 1997
Pathogenesis

Sepsis and septic shock Bacterial infection Excessive host response Host factors lead to cellular damage Organ damage Death
Why sepsis is important?
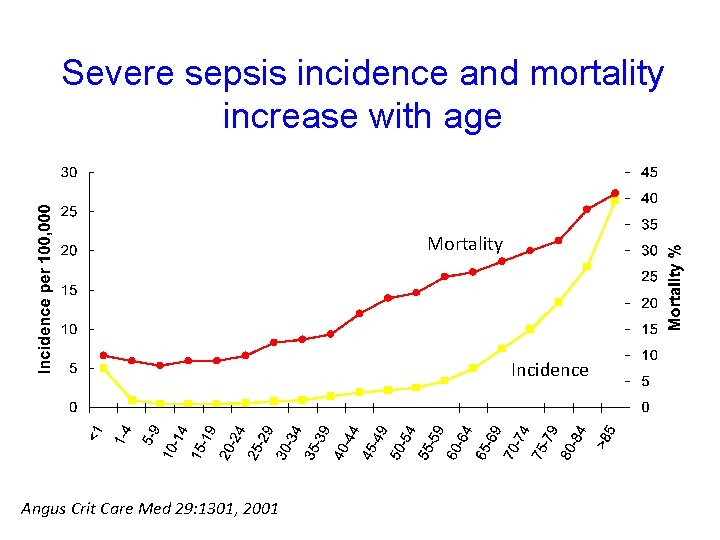
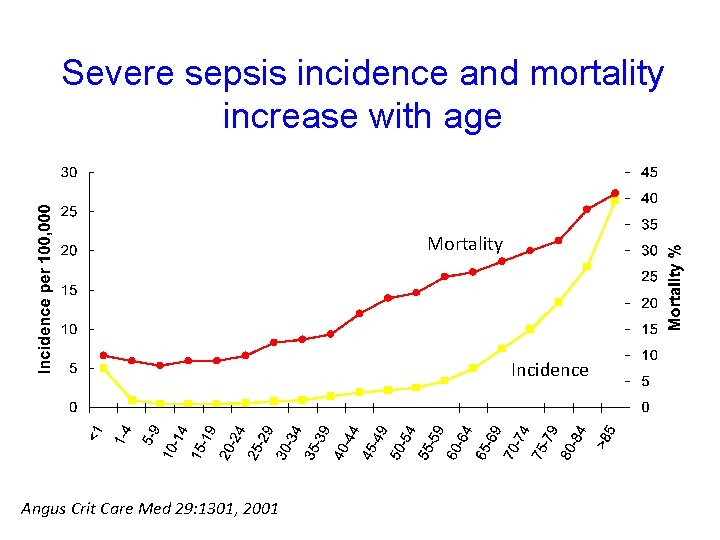
Severe sepsis incidence and mortality increase with age Mortality Incidence Angus Crit Care Med 29: 1301, 2001
Severe Sepsis • Major cause of morbidity and mortality worldwide. • Leading cause of death in noncoronary ICU. • 11 th leading cause of death overall. • More than 750, 000 cases of severe sepsis in US annually. • In the US, more than 500 patients die of severe sepsis daily.
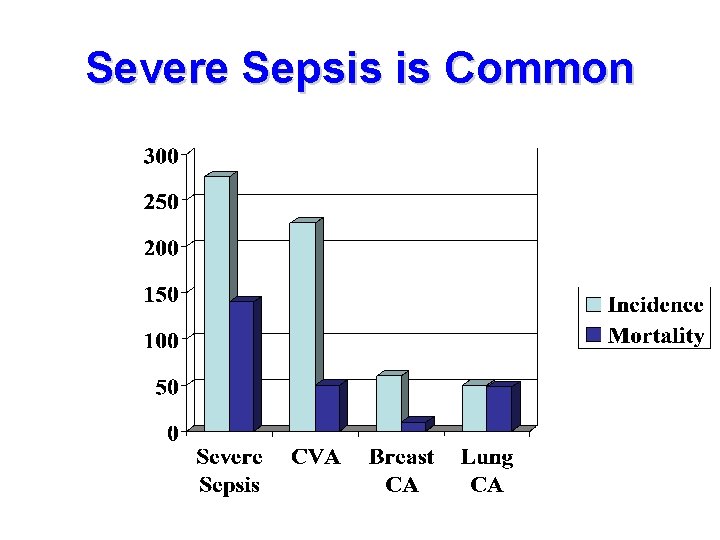
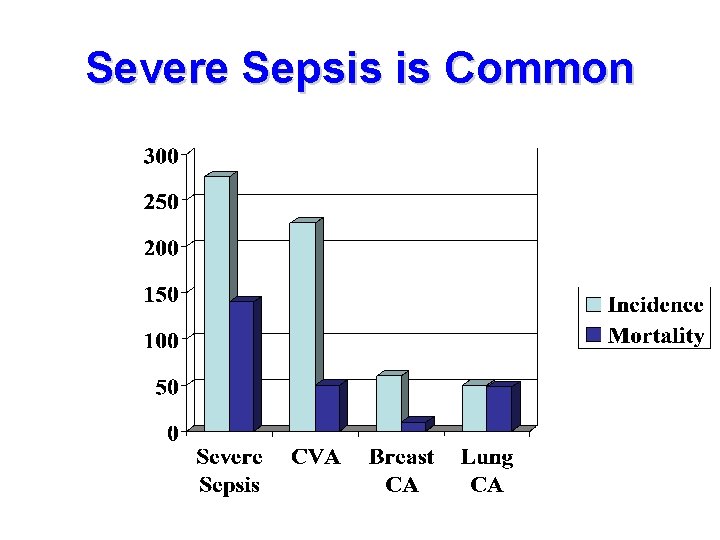
Severe Sepsis is Common
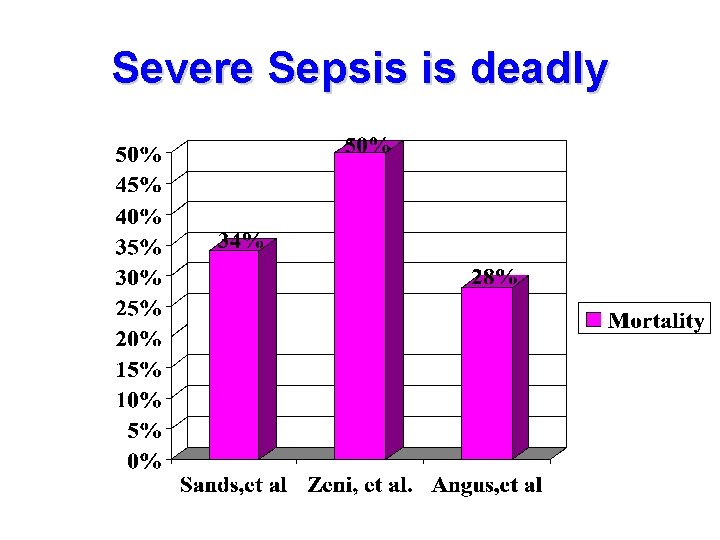
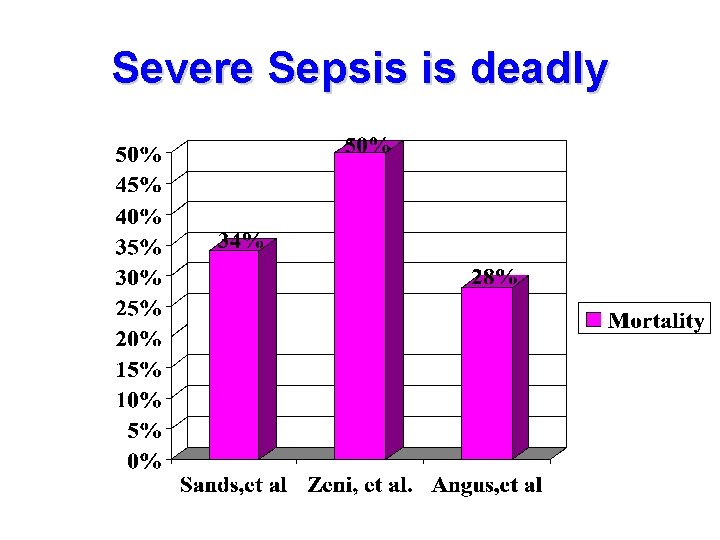
Severe Sepsis is deadly
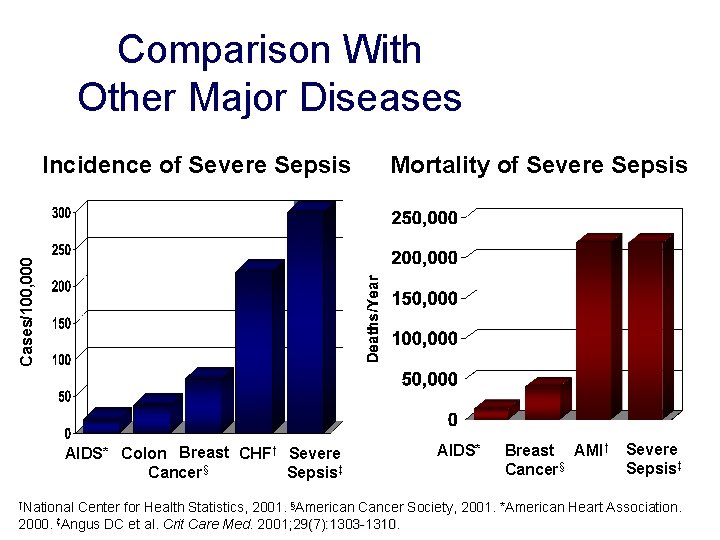
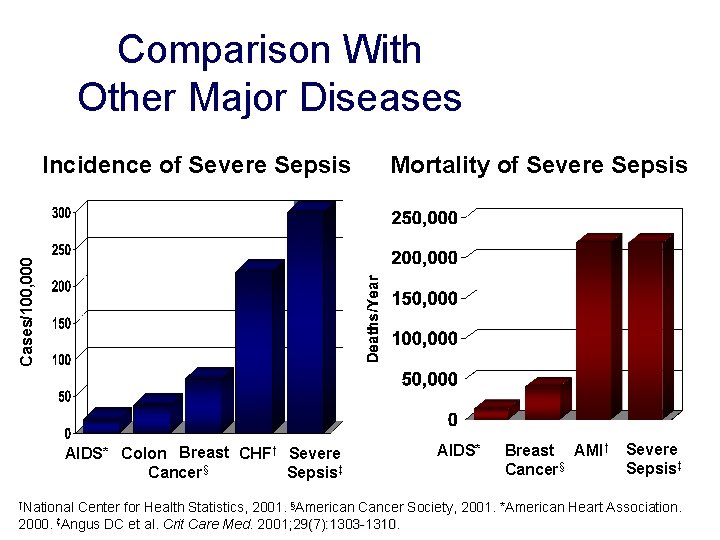
Comparison With Other Major Diseases Mortality of Severe Sepsis Cases/100, 000 Incidence of Severe Sepsis AIDS* Colon Breast CHF† Severe Cancer§ Sepsis‡ †National AIDS* Breast AMI† Cancer§ Severe Sepsis‡ Center for Health Statistics, 2001. §American Cancer Society, 2001. *American Heart Association. 2000. ‡Angus DC et al. Crit Care Med. 2001; 29(7): 1303 -1310
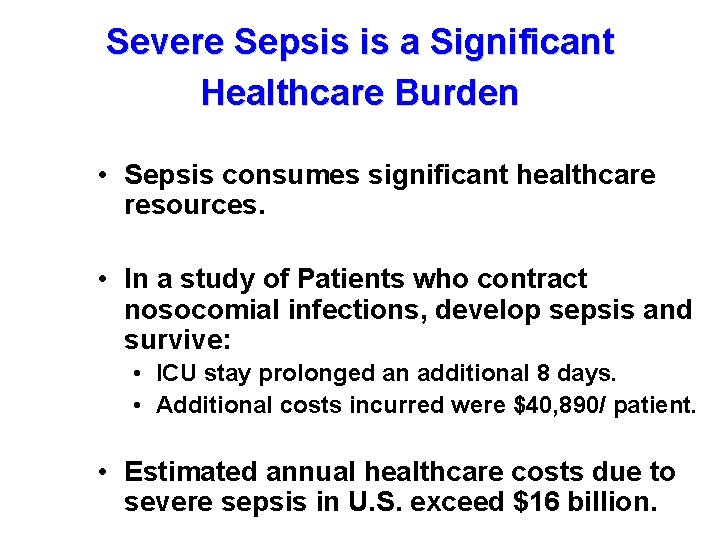
Severe Sepsis is a Significant Healthcare Burden • Sepsis consumes significant healthcare resources. • In a study of Patients who contract nosocomial infections, develop sepsis and survive: • ICU stay prolonged an additional 8 days. • Additional costs incurred were $40, 890/ patient. • Estimated annual healthcare costs due to severe sepsis in U. S. exceed $16 billion.
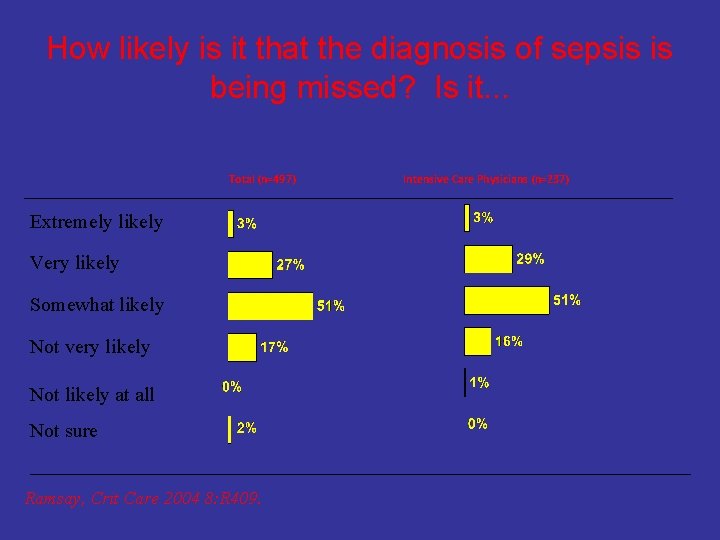
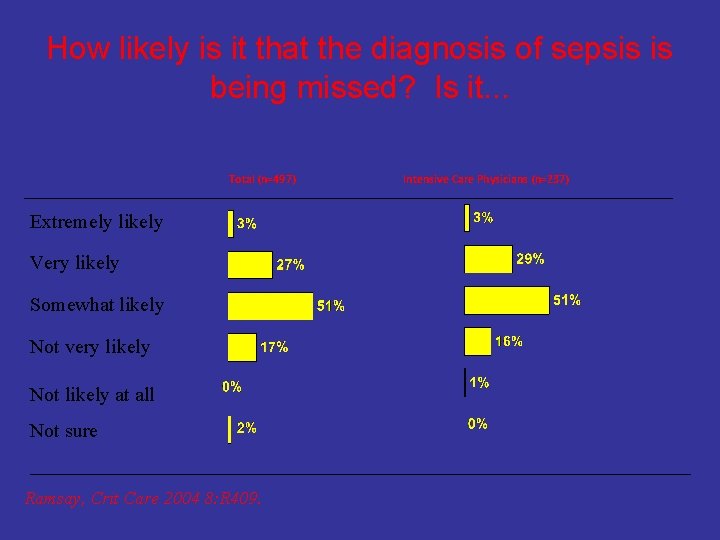
How likely is it that the diagnosis of sepsis is being missed? Is it. . . Total (n=497) Extremely likely Very likely Somewhat likely Not very likely Not likely at all Not sure Ramsay, Crit Care 2004 8: R 409. Intensive Care Physicians (n=237)

Management
Management of Sepsis • Recognition • Supportive care • Source control • Antibiotics • Specific (adjunctive) therapy
Key Components(1) • Fluid resuscitation • Appropriate cultures prior to antibiotic administration • Early targeted antibiotics and source control • Use of vasopressors/inotropes when fluid resuscitation optimized
Key Components(2) • Evaluation for adrenal insufficiency • Stress dose corticosteroid administration • Recombinant human activated protein C (xigris) for severe sepsis • Low tidal volume mechanical ventilation for ARDS • Tight glucose control
Key Components(3): Prevent Complications of Critical Illness ----General • Prophylaxis for DVT • Stress ulcer prophylaxis • Prevention of nosocomial pneumonia by elevation of head to 45 degrees • Facilitate extubation by daily interruption of sedation and early SBT • Narrowing of antibiotic spectrum when appropriate
Treatment of Septic Shock • Initiate broad-spectrumSite specific antibiotics – Goal is administration within three hours of arrival in ED. – Several studies support the concept of “earlier the better” • EarlyAppropriate antibiotics appear to affect outcomes. • Cochrane paper underway on subject
Treatment of Septic Shock • Antibiotic Choices – Base on suspected pathogen information. • Remember previous cultures on your patient! – Adapt to local pathogensantibiotogram. – Consider MRSA coverage • Many institutions routinely include. – Many paths to same destination.
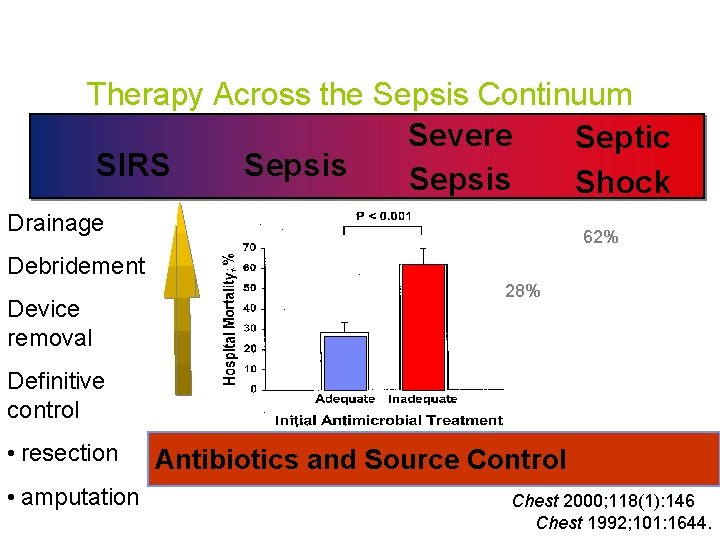
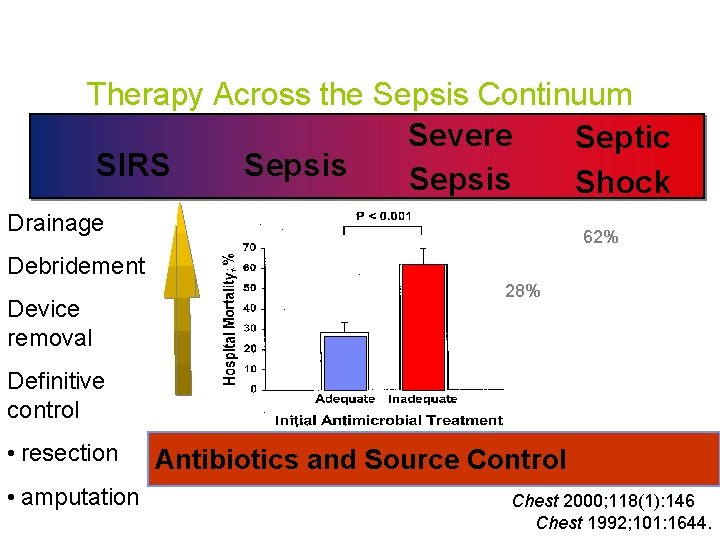
Therapy Across the Sepsis Continuum Severe Septic Sepsis SIRS Sepsis Shock Drainage 62% Debridement Device removal 28% Definitive control • resection • amputation Antibiotics and Source Control Chest 2000; 118(1): 146 Chest 1992; 101: 1644.
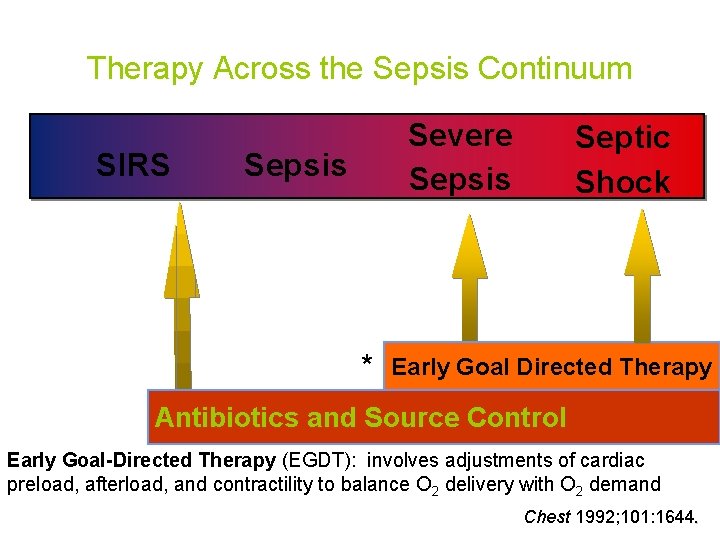
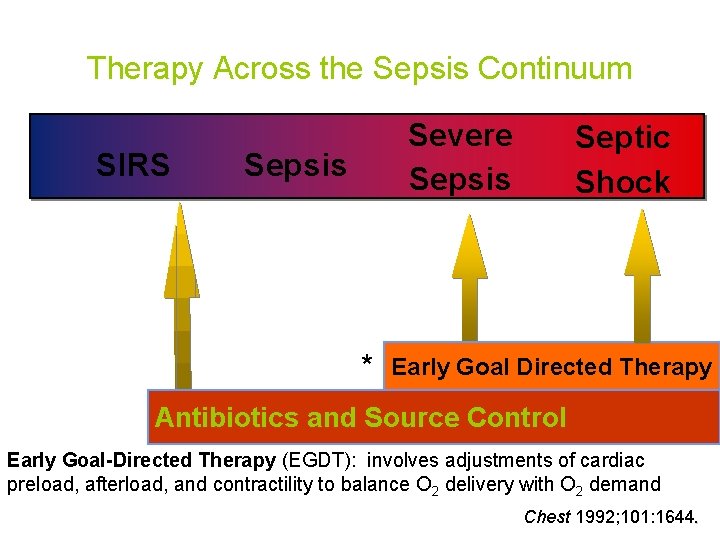
Therapy Across the Sepsis Continuum SIRS Severe Sepsis * Septic Shock Early Goal Directed Therapy Antibiotics and Source Control Early Goal-Directed Therapy (EGDT): involves adjustments of cardiac preload, afterload, and contractility to balance O 2 delivery with O 2 demand Chest 1992; 101: 1644.
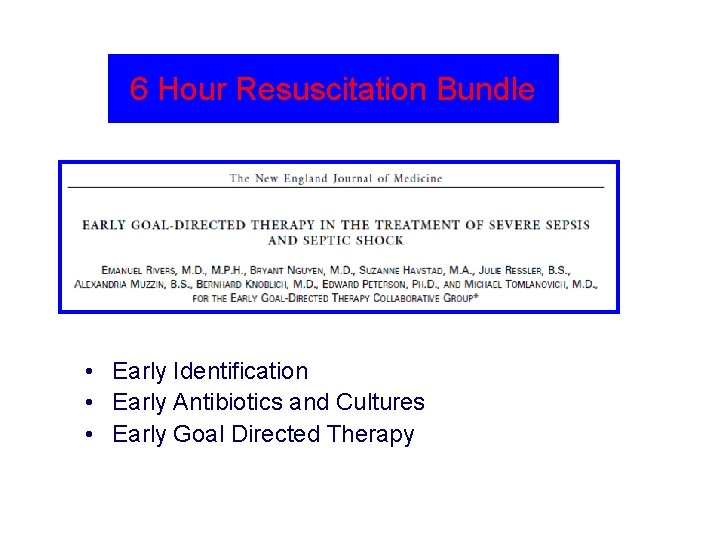
6 Hour Resuscitation Bundle • Early Identification • Early Antibiotics and Cultures • Early Goal Directed Therapy
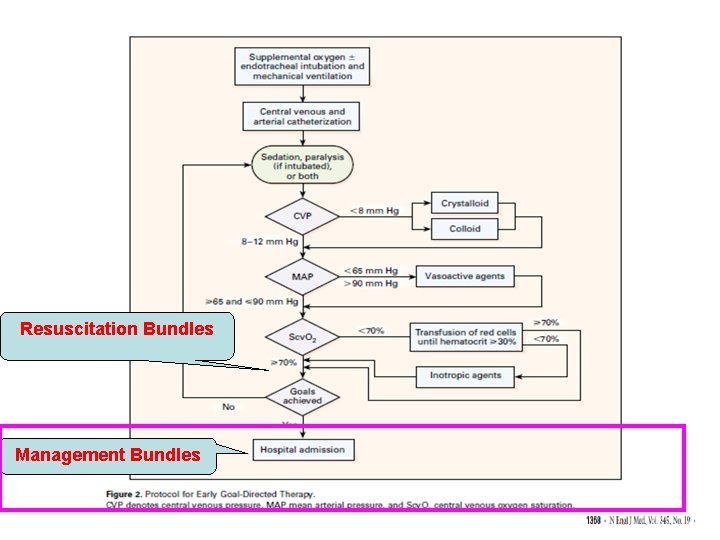
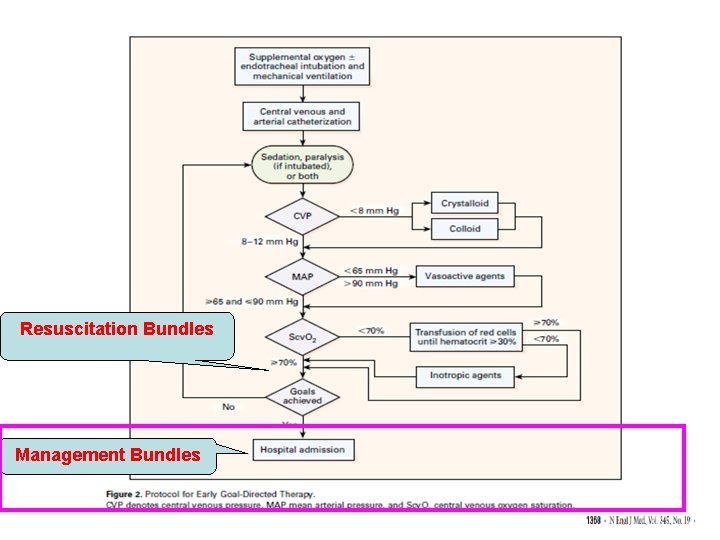
Resuscitation Bundles Management Bundles
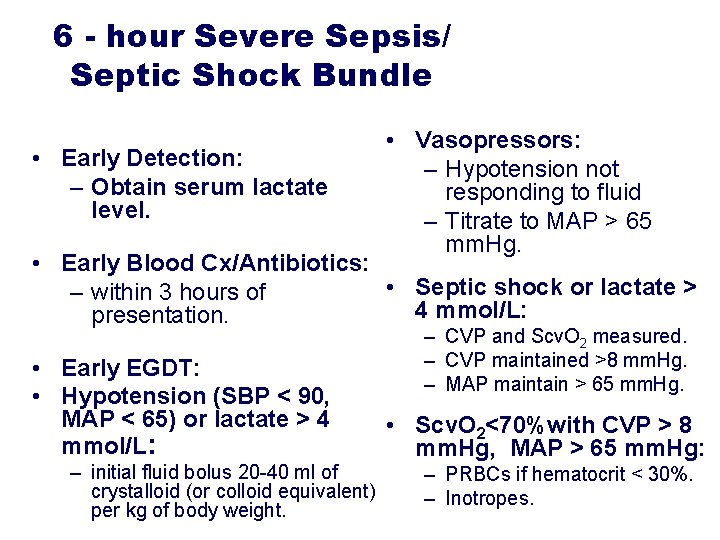
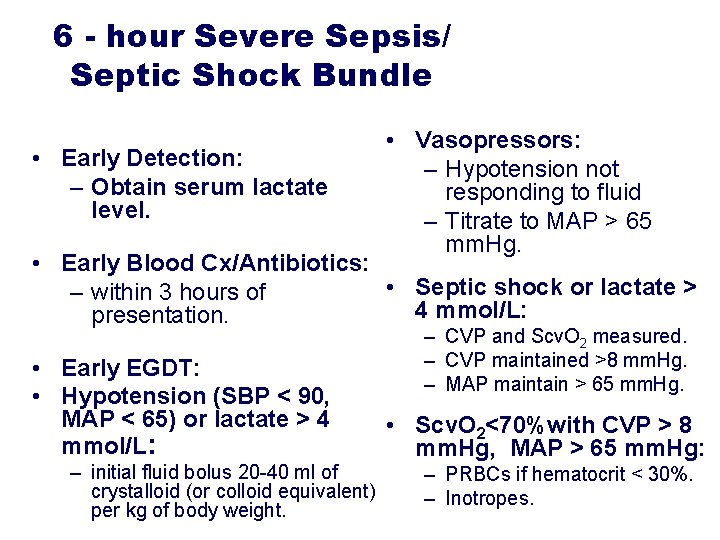
6 - hour Severe Sepsis/ Septic Shock Bundle • Early Detection: – Obtain serum lactate level. • Vasopressors: – Hypotension not responding to fluid – Titrate to MAP > 65 mm. Hg. • Early Blood Cx/Antibiotics: • Septic shock or lactate > – within 3 hours of 4 mmol/L: presentation. • Early EGDT: • Hypotension (SBP < 90, MAP < 65) or lactate > 4 mmol/L: – initial fluid bolus 20 -40 ml of crystalloid (or colloid equivalent) per kg of body weight. – CVP and Scv. O 2 measured. – CVP maintained >8 mm. Hg. – MAP maintain > 65 mm. Hg. • Scv. O 2<70%with CVP > 8 mm. Hg, MAP > 65 mm. Hg: – PRBCs if hematocrit < 30%. – Inotropes.

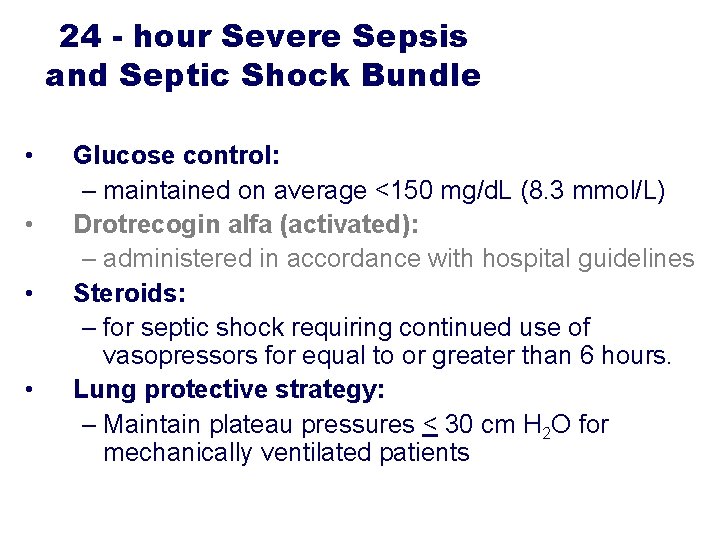
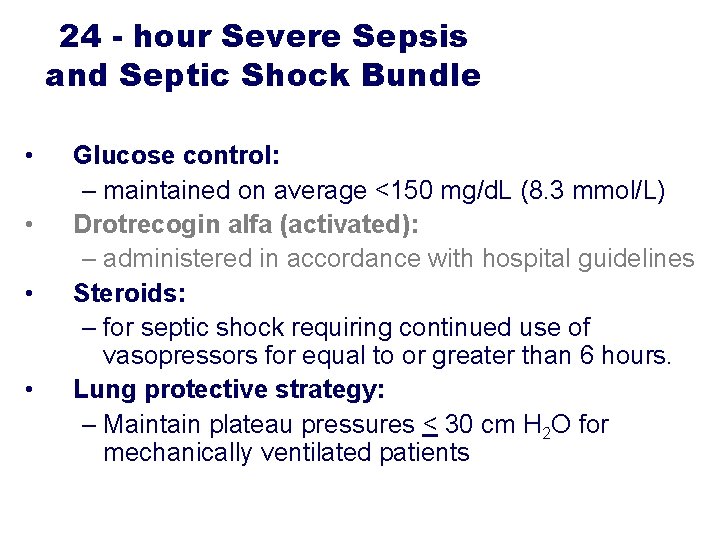
24 - hour Severe Sepsis and Septic Shock Bundle • • Glucose control: – maintained on average <150 mg/d. L (8. 3 mmol/L) Drotrecogin alfa (activated): – administered in accordance with hospital guidelines Steroids: – for septic shock requiring continued use of vasopressors for equal to or greater than 6 hours. Lung protective strategy: – Maintain plateau pressures < 30 cm H 2 O for mechanically ventilated patients
What Pressors for Septic Shock ? • Several non-randomized studies and one small prospective randomized study of dopamine vs norepinephrine for septic shock suggest that survival may be improved with the use of norepinephrine



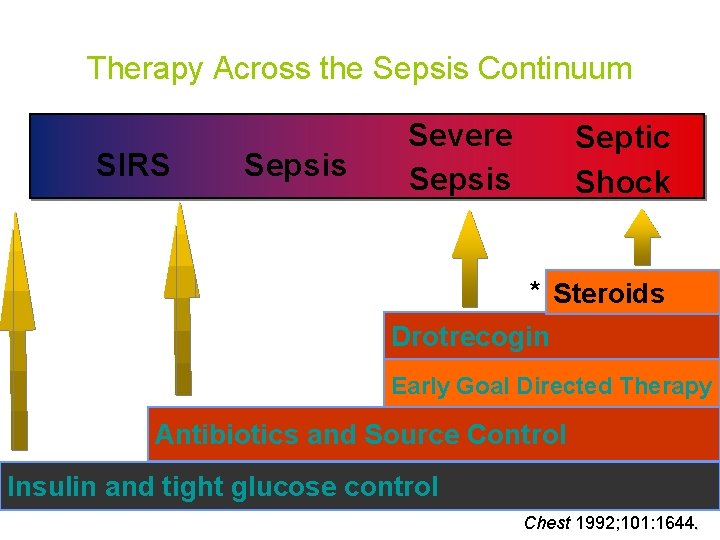
Therapy Across the Sepsis Continuum SIRS Sepsis Severe Sepsis Septic Shock Early Goal Directed Therapy Antibiotics and Source Control * Insulin and tight glucose control Chest 1992; 101: 1644.
Glucose Control: Mechanisms • • Stress hyperglycemia is common in sepsis Glucose has pro-inflammatory effects Insulin resistance is common in sepsis Insulin has an anti-inflammatory effect, possibly via NOS. • Benefit is likely related to both insulin itself and lowering of blood glucose










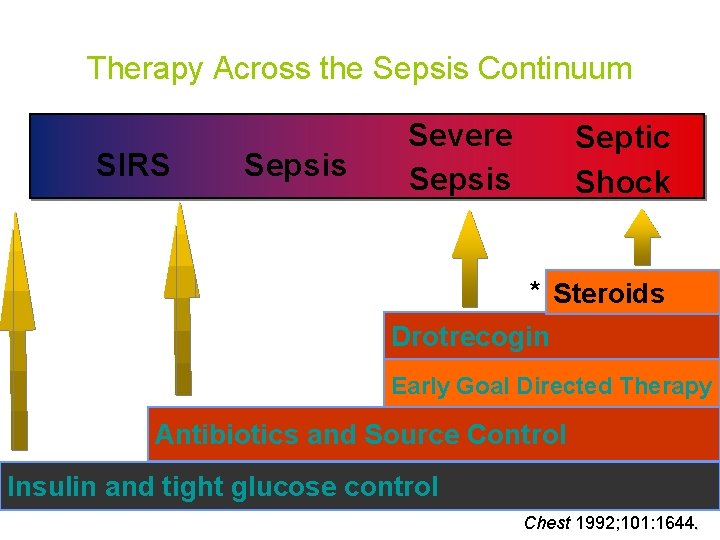
Therapy Across the Sepsis Continuum SIRS Sepsis Severe Sepsis Septic Shock * Steroids Drotrecogin Early Goal Directed Therapy Antibiotics and Source Control Insulin and tight glucose control Chest 1992; 101: 1644.
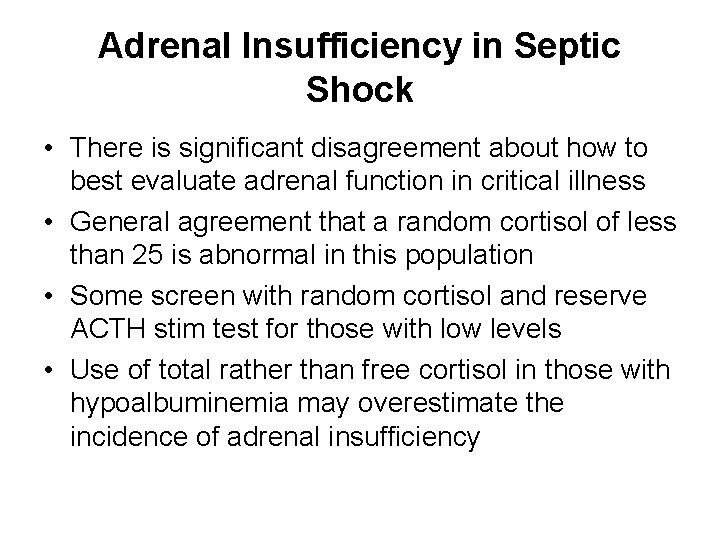
Adrenal Insufficiency in Septic Shock • There is significant disagreement about how to best evaluate adrenal function in critical illness • General agreement that a random cortisol of less than 25 is abnormal in this population • Some screen with random cortisol and reserve ACTH stim test for those with low levels • Use of total rather than free cortisol in those with hypoalbuminemia may overestimate the incidence of adrenal insufficiency
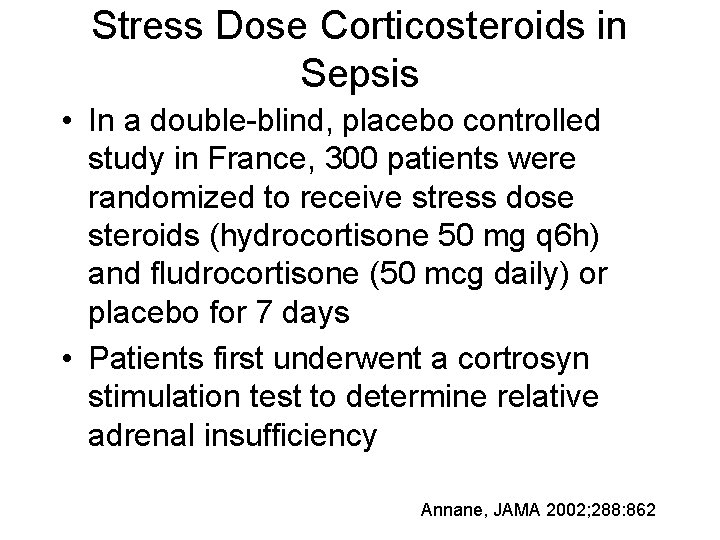
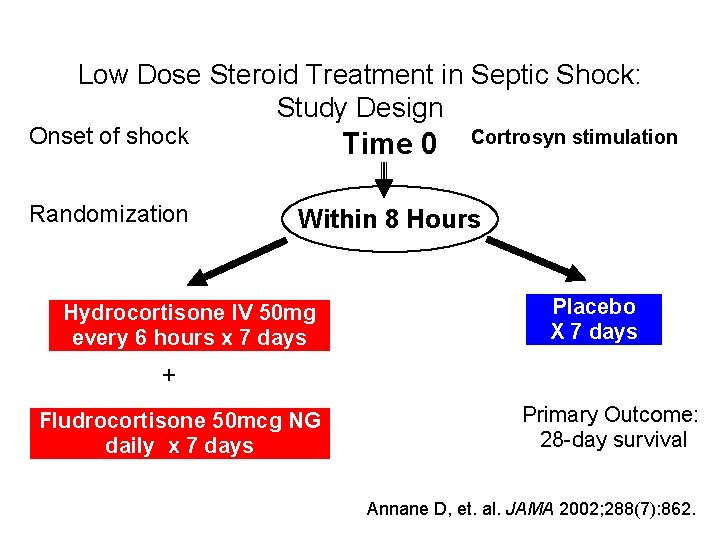
Stress Dose Corticosteroids in Sepsis • In a double-blind, placebo controlled study in France, 300 patients were randomized to receive stress dose steroids (hydrocortisone 50 mg q 6 h) and fludrocortisone (50 mcg daily) or placebo for 7 days • Patients first underwent a cortrosyn stimulation test to determine relative adrenal insufficiency Annane, JAMA 2002; 288: 862
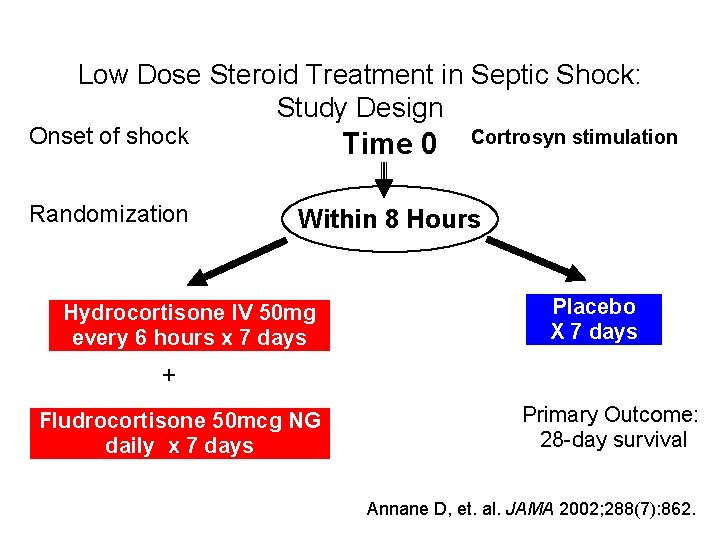
Low Dose Steroid Treatment in Septic Shock: Study Design Onset of shock Time 0 Randomization Within 8 Hours Hydrocortisone IV 50 mg every 6 hours x 7 days Cortrosyn stimulation Placebo X 7 days + Fludrocortisone 50 mcg NG daily x 7 days Primary Outcome: 28 -day survival Annane D, et. al. JAMA 2002; 288(7): 862.
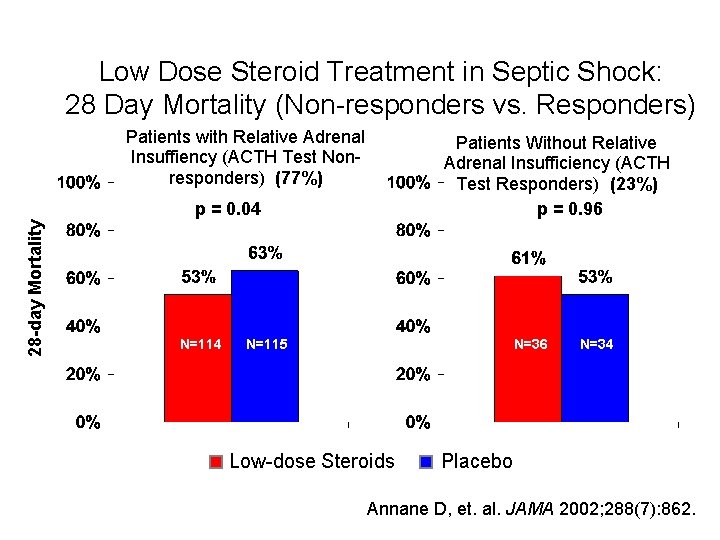
• Relative adrenal insufficiency was defined as a failure to increase serum cortisol by greater than 9 mcg/dl after a 250 mcg ACTH stimulation test. • Using this criteria, 77% of patients in this study were adrenally insufficient
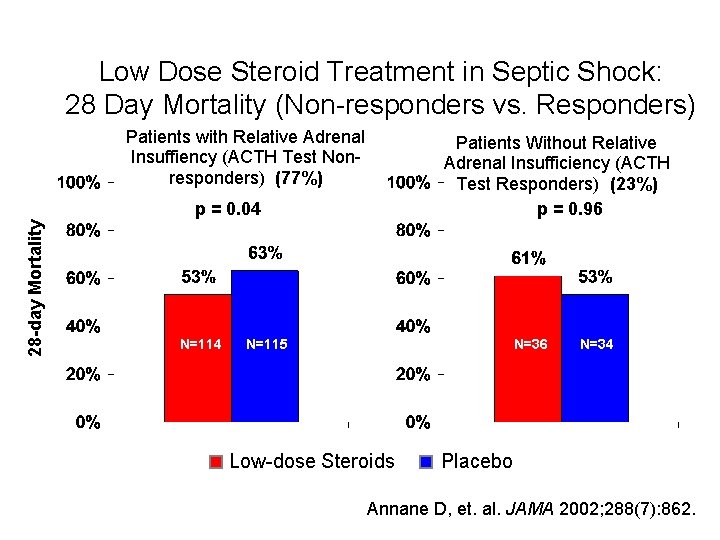
Low Dose Steroid Treatment in Septic Shock: 28 Day Mortality (Non-responders vs. Responders) Patients with Relative Adrenal Insuffiency (ACTH Test Nonresponders) (77%) Patients Without Relative Adrenal Insufficiency (ACTH Test Responders) (23%) p = 0. 96 28 -day Mortality p = 0. 04 N=115 N=36 Low-dose Steroids N=34 Placebo Annane D, et. al. JAMA 2002; 288(7): 862.
Corticosteroids in Sepsis • Obtain a baseline cortisol or ACTH stimulation • Start stress dose steroids (hydrocortisone 200 -300 mg +/- fludrocortisone 50 mcg) • Discontinue if levels are adequate


Case series


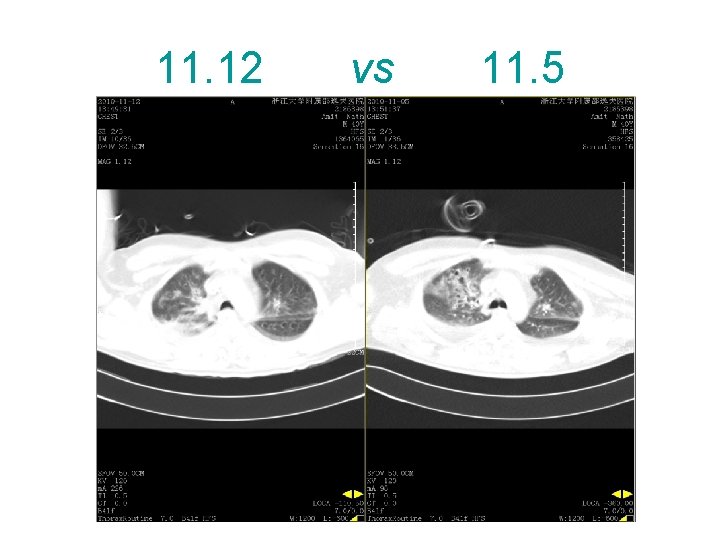
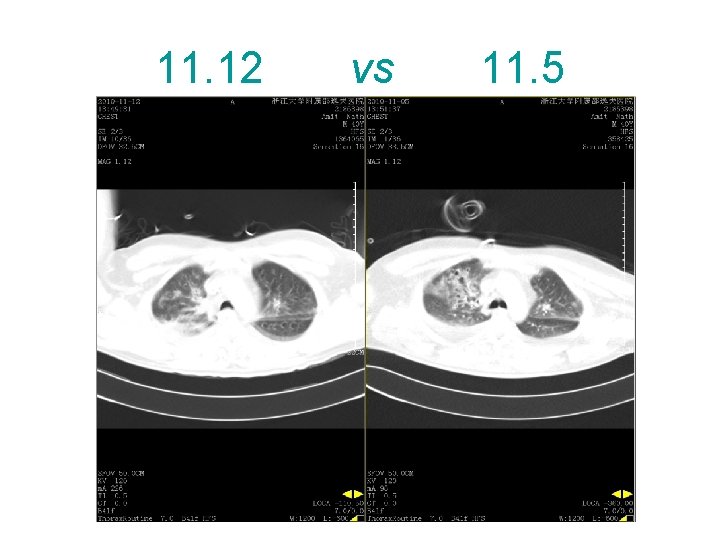
11. 12 vs 11. 5





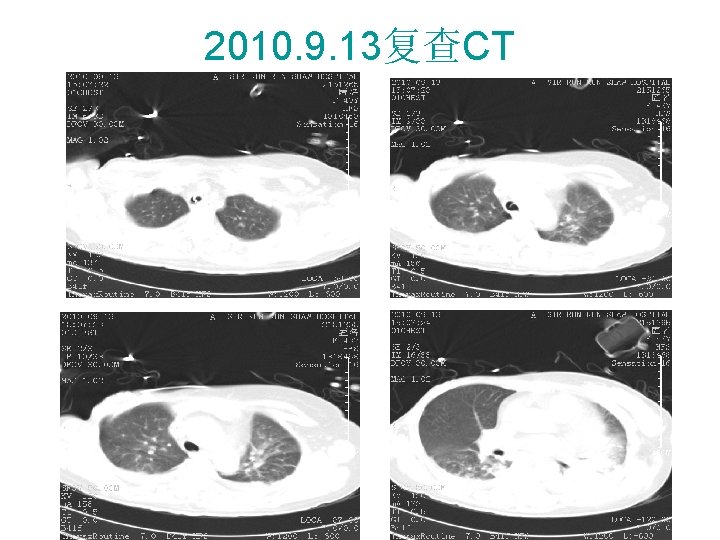
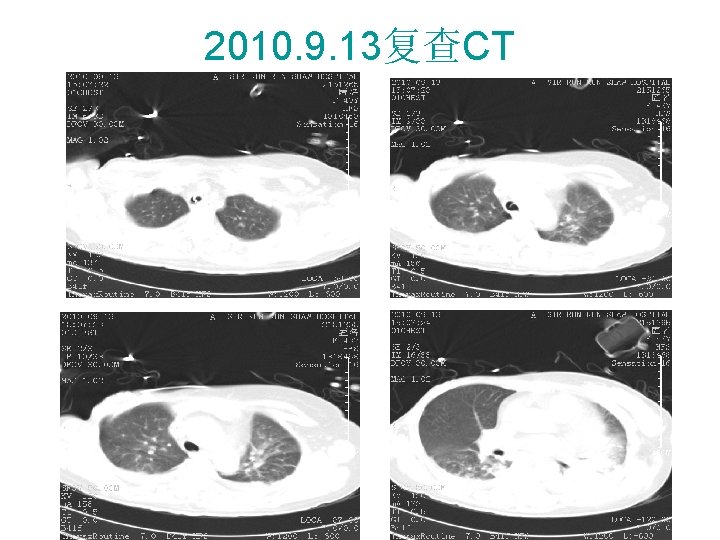
2010. 9. 13复查CT
Summary
SURVIVING SEPSIS • Fluid resuscitation, goal-directed • Appropriate cultures prior to antibiotic administration • Early targeted antibiotics and source control • Use of vasopressors/inotropes when fluid resuscitation optimized
SURVIVING SEPSIS • Evaluation for adrenal insufficiency • Stress dose corticosteroid administration • Recombinant human activated protein C (xigris) for severe sepsis • Insulin drip for tight glucose control • Low tidal volumes (6 cc/kg) for mechanical ventilation in ARDS
PREVENT COMPLICATIONS • • Stress ulcer and DVT prophylaxis Narrow antibiotic spectrum Prevent VAP: 45 degree elevation Facilitate early discontinuation of mechanical ventilation: sedation interruption, early SBT
Thanks for your attention
 Q sofa
Q sofa Cauda equina vs conus medullaris
Cauda equina vs conus medullaris Shok neurogenico
Shok neurogenico Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Subacute combined degeneration of the cord
Subacute combined degeneration of the cord Perfect competition long run equilibrium
Perfect competition long run equilibrium Multirule
Multirule Perfect competition short run
Perfect competition short run Run lola run themes
Run lola run themes Run lola run editing techniques
Run lola run editing techniques Short run vs long run economics
Short run vs long run economics Brigitta olsen
Brigitta olsen Nnlolas
Nnlolas Definition of hospital pharmacy
Definition of hospital pharmacy Jea septic tank phase out
Jea septic tank phase out Septic tank contamination groundwater
Septic tank contamination groundwater Symptoms of gonorrhea
Symptoms of gonorrhea Indianapolis septic tank elimination program
Indianapolis septic tank elimination program Septic squeeze test tonsillitis
Septic squeeze test tonsillitis Advantex ax20 price
Advantex ax20 price Barnstable county septic loan
Barnstable county septic loan Pickwickian syndrome in dogs
Pickwickian syndrome in dogs Septic arthritis complications
Septic arthritis complications Panhandle health septic
Panhandle health septic Septic arthritis antibiotics
Septic arthritis antibiotics Septic arthritis antibiotics
Septic arthritis antibiotics Qqq10
Qqq10 Multiflow septic system
Multiflow septic system Puraflo peat
Puraflo peat Septic arthritis complications
Septic arthritis complications Doc's septic tank cleaning
Doc's septic tank cleaning Enthesitis
Enthesitis Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Haemophilus influenzae
Haemophilus influenzae Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Chemical oxygen demand principle
Chemical oxygen demand principle Septic spleen
Septic spleen Septic arthritis workup
Septic arthritis workup Septic
Septic Summit county septic permit
Summit county septic permit Rock solid septic
Rock solid septic Nitrex
Nitrex Nongonococcal septic arthritis
Nongonococcal septic arthritis Spoken english and broken english
Spoken english and broken english Sepsis care near palo alto
Sepsis care near palo alto Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Sepsis neonatal temprana y tardía
Sepsis neonatal temprana y tardía Neonatarum
Neonatarum Prevention of puerperal sepsis
Prevention of puerperal sepsis Sepsis
Sepsis Hora dorada emergencias
Hora dorada emergencias Gdp sepsis decision support tool
Gdp sepsis decision support tool Vertical y horizontal
Vertical y horizontal Maternal sepsis
Maternal sepsis Neonatal sepsis symptoms
Neonatal sepsis symptoms Neonatal sepsis nelson pediatrics
Neonatal sepsis nelson pediatrics Hoja de balance hidrico en enfermeria
Hoja de balance hidrico en enfermeria Sepsis bundle
Sepsis bundle Example of drivers
Example of drivers Sepsis hour 1 bundle
Sepsis hour 1 bundle Dr alex sepsis
Dr alex sepsis Segurneo guia farmacologica
Segurneo guia farmacologica Sepsis dietary management
Sepsis dietary management Sepsis hour 1 bundle
Sepsis hour 1 bundle Surviving sepsis definition
Surviving sepsis definition Give 3 take 3 sepsis
Give 3 take 3 sepsis Sepsis
Sepsis Sepsis definition
Sepsis definition Puerperal sepsis
Puerperal sepsis Criterios sepsis
Criterios sepsis What is sepsis disease
What is sepsis disease Stages of sepsis
Stages of sepsis Puerperal sepsis
Puerperal sepsis Sepsis
Sepsis Sepsis triangle
Sepsis triangle Sepsis pp respiratorio
Sepsis pp respiratorio David howe ent
David howe ent Emanms
Emanms