Implementation of the Surviving Sepsis Campaign Guidelines Keys
- Slides: 50
Implementation of the Surviving Sepsis Campaign Guidelines: Keys to Success Tom Ahrens, DNS RN CCNS FAAN Research Scientist/Clinical Specialist Barnes-Jewish Hospital St. Louis, MO tsa 2109@bjc. org
Keys to Success • Who are the champions – Administrative – Clinical • Physician • Nurse • Pharmacy – Coders • Education of staff – Can sepsis be recognized • ED • ICU • Floors – How to educate • Need mass, effective and rapid education • Traditional methods will not be most effective – Limited reach – Limited effectiveness due to lack of engagement • Web based, virtual reality – Documentation • Physician and APN education on key words in sepsis/severe sepsis documentation
Can your staff recognize sepsis? Sepsis can be subtle until it is so obvious you can’t miss it
62 year old admitted to hospital with hip infection • On admission – T – 38. 5 – RR – 24 – P – 104 – WBC – 19, 000 • Where should he be admitted?
36 hours post admission Urine output drops – What should be done?
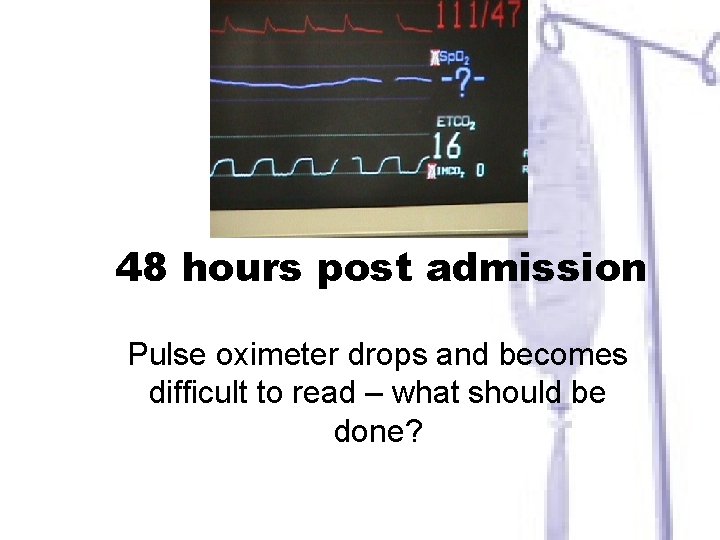
48 hours post admission Pulse oximeter drops and becomes difficult to read – what should be done?
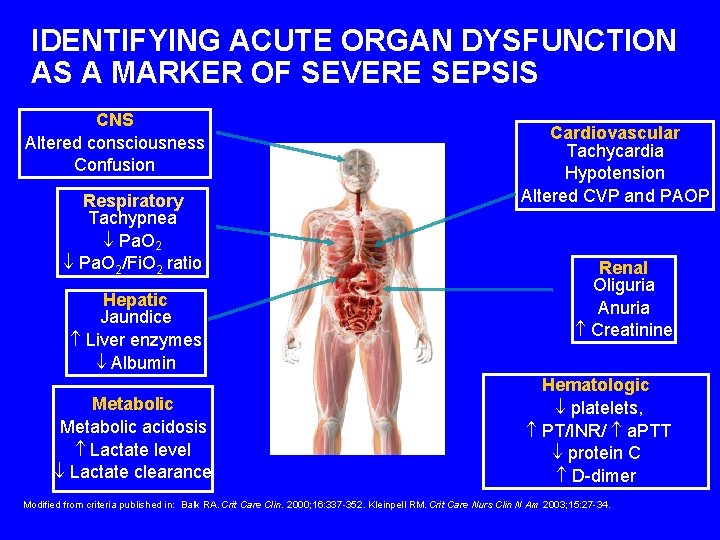
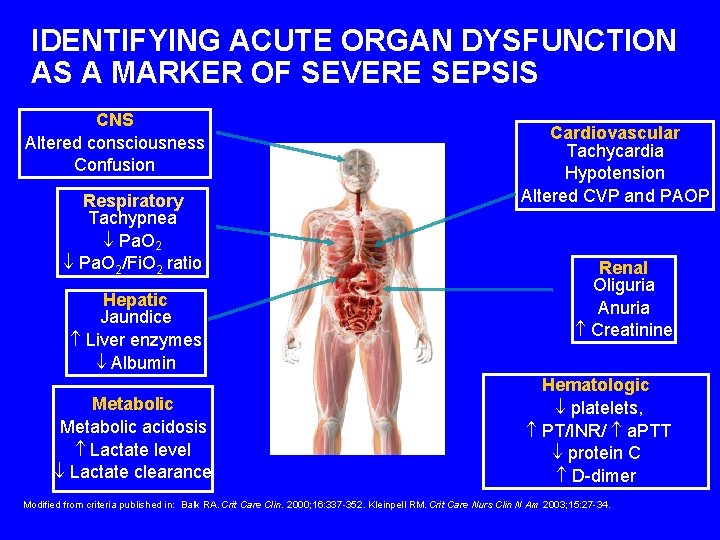
IDENTIFYING ACUTE ORGAN DYSFUNCTION AS A MARKER OF SEVERE SEPSIS CNS Altered consciousness Confusion Respiratory Tachypnea Pa. O 2/Fi. O 2 ratio Hepatic Jaundice Liver enzymes Albumin Metabolic acidosis Lactate level Lactate clearance Cardiovascular Tachycardia Hypotension Altered CVP and PAOP Renal Oliguria Anuria Creatinine Hematologic platelets, PT/INR/ a. PTT protein C D-dimer Modified from criteria published in: Balk RA. Crit Care Clin. 2000; 16: 337 -352. Kleinpell RM. Crit Care Nurs Clin N Am 2003; 15: 27 -34.
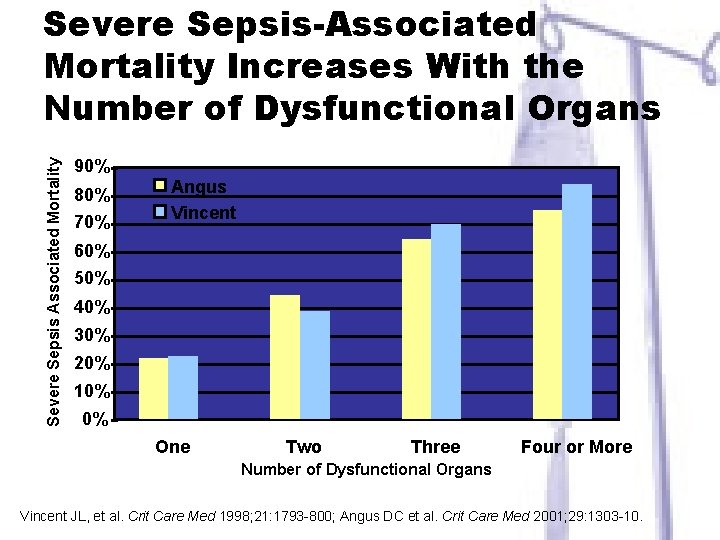
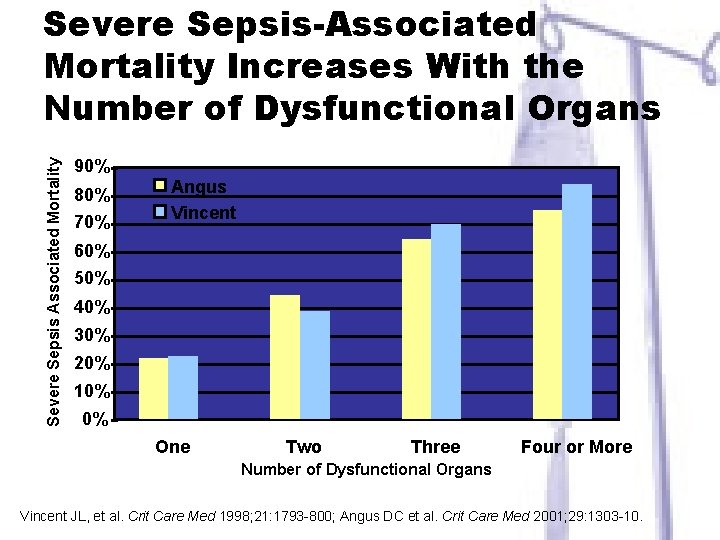
Severe Sepsis Associated Mortality Severe Sepsis-Associated Mortality Increases With the Number of Dysfunctional Organs 90% 80% 70% Angus Vincent 60% 50% 40% 30% 20% 10% 0% One Two Three Four or More Number of Dysfunctional Organs Vincent JL, et al. Crit Care Med 1998; 21: 1793 -800; Angus DC et al. Crit Care Med 2001; 29: 1303 -10.
1) Which one of the following are signs of the systemic inflammatory response syndrome? A. B. C. D. Respiratory acidosis Pain Hypotension Tachypnea
2) What is the definition of sepsis? A. Infection plus multi organ system dysfunction B. Inflammation with a high white blood cell count C. Infection as the cause of the systemic inflammatory response D. Presence of positive blood cultures
4) When is POC Lactate indicated in Patient Assessment? A. When a patient’s blood pressure is low B. If the patient has an infection and signs of SIRS C. A rapid response call to a patient with a decreased LOC D. Before giving a vasopressor
“Our arsenals for fighting off bacteria are so powerful, and involve so many different defense mechanisms, that we are more in danger from them than from the invaders. “We live in the midst of explosive devices; we are mined!” Lewis Thomas - 1972 Germs, New England Journal Of Medicine DR 32708 3000093662 1204. 5 Copyright © 2004, Eli Lilly and Company. All rights reserved. Xigris is a registered trademark of Eli Lilly and Company.
“Except on few occasions, the patient appears to die from the body's response to infection rather than from it. ” Sir William Osler – 1904 The Evolution of Modern Medicine
History of Treating Severe Sepsis Antibiotics, fluids, vasopressors - Have they been successful? Have we searched for better treatments?
Key to Success Rapid Identification • Nursing’s role in identifying and helping in the treatment of sepsis is more important than ever before • Implementing protocols on the floor, ED and ICU • Physician and coder’s working together to improve documentation
Hemodynamics of Sepsis • Concept of early resuscitation – Establishing urgency – use of Lactate – Normal 1 -2 mmol – > 4 mmol with metabolic acidosis suggests tissue hypoxia • Fluids with a goal – The role of mixed venous oxyhemoglobin (Scv. O 2) 16
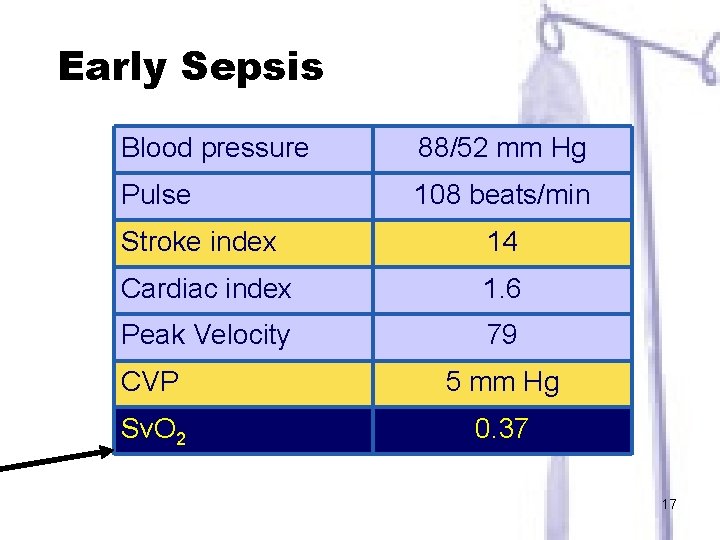
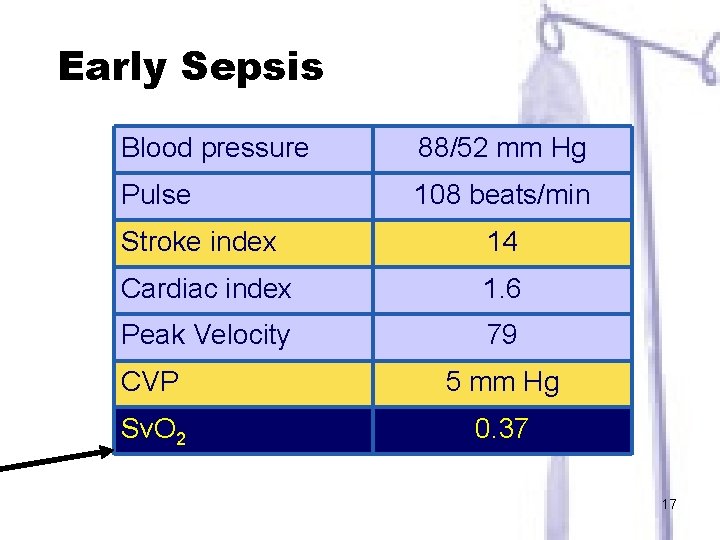
Early Sepsis Blood pressure 88/52 mm Hg Pulse 108 beats/min Stroke index 14 Cardiac index 1. 6 Peak Velocity 79 CVP 5 mm Hg Sv. O 2 0. 37 17
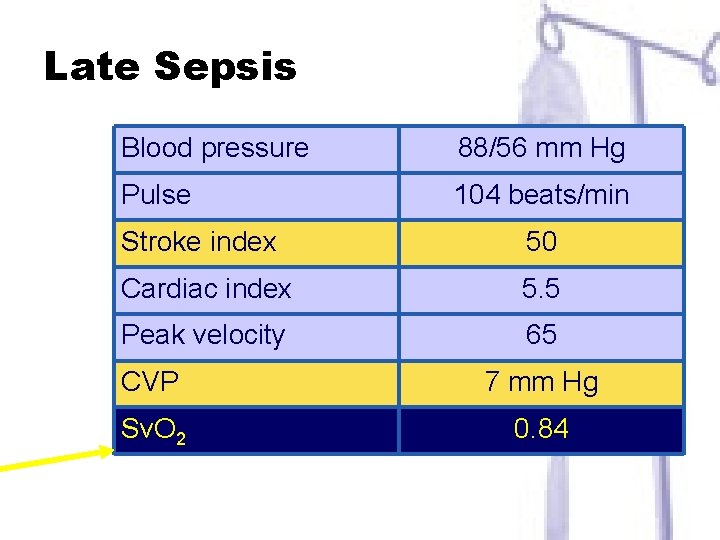
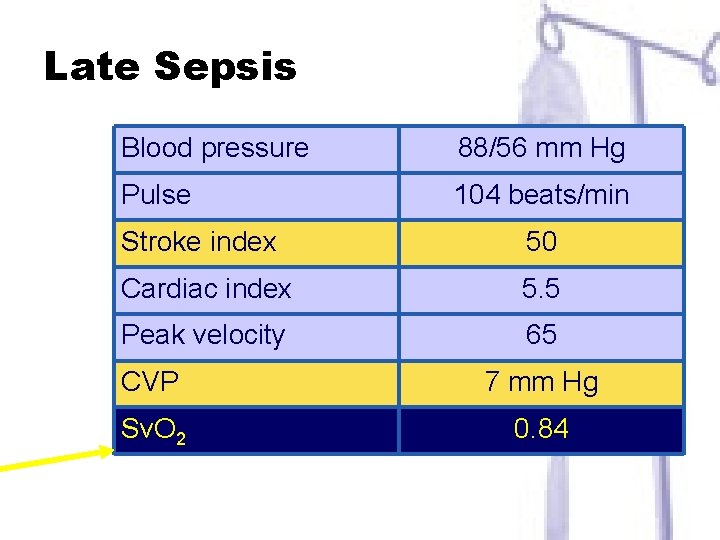
Late Sepsis Blood pressure 88/56 mm Hg Pulse 104 beats/min Stroke index 50 Cardiac index 5. 5 Peak velocity 65 CVP 7 mm Hg Sv. O 2 0. 84
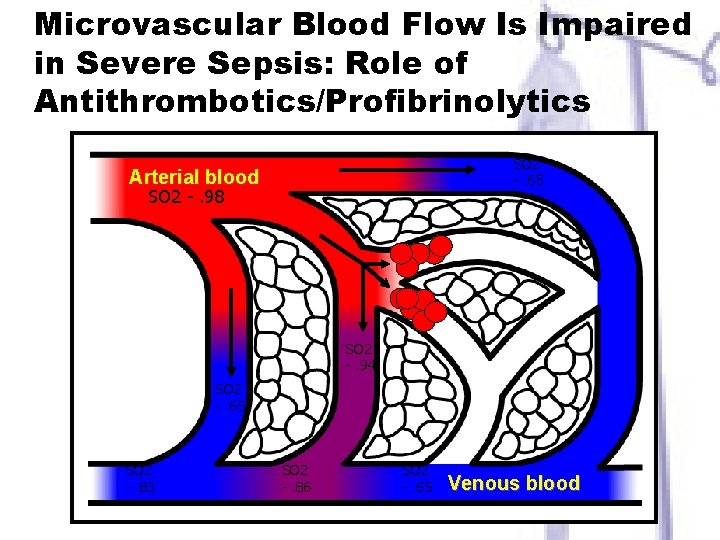
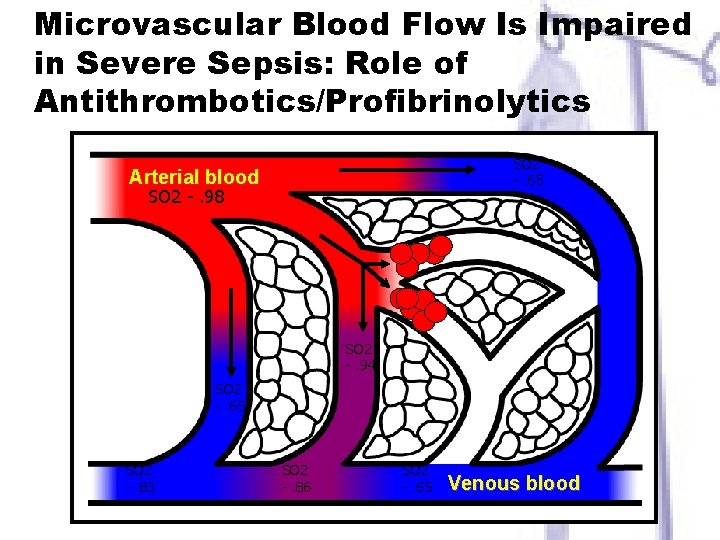
Microvascular Blood Flow Is Impaired in Severe Sepsis: Role of Antithrombotics/Profibrinolytics SO 2 -. 65 Arterial blood SO 2 -. 98 SO 2 -. 94 SO 2 -. 65 SO 2 -. 83 SO 2 -. 86 SO 2 -. 65 Venous blood
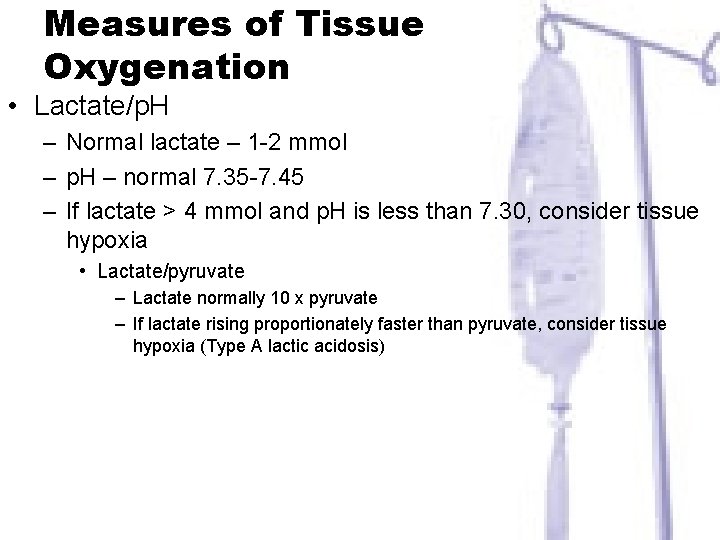
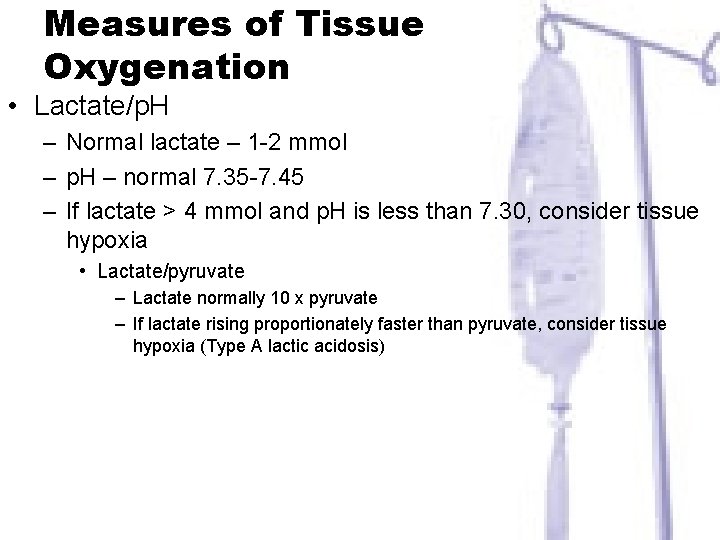
Measures of Tissue Oxygenation • Lactate/p. H – Normal lactate – 1 -2 mmol – p. H – normal 7. 35 -7. 45 – If lactate > 4 mmol and p. H is less than 7. 30, consider tissue hypoxia • Lactate/pyruvate – Lactate normally 10 x pyruvate – If lactate rising proportionately faster than pyruvate, consider tissue hypoxia (Type A lactic acidosis)
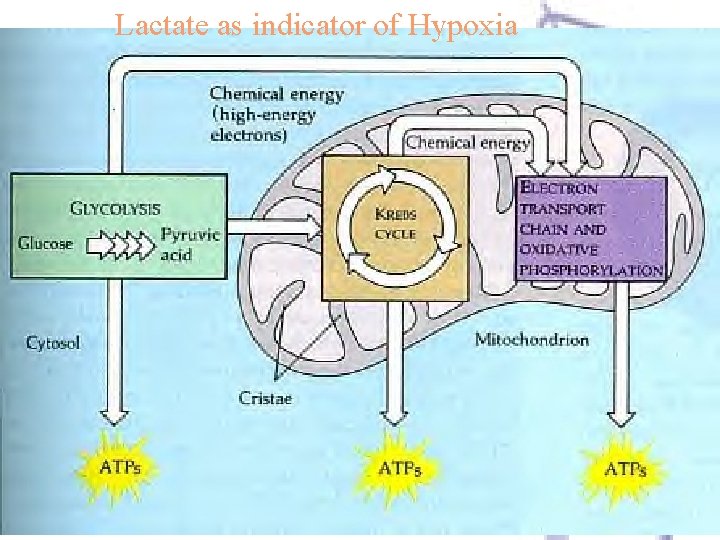
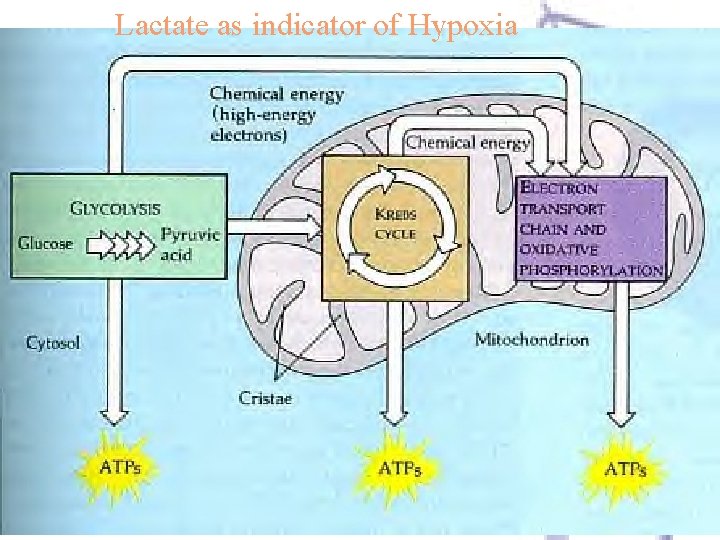
Lactate as indicator of Hypoxia
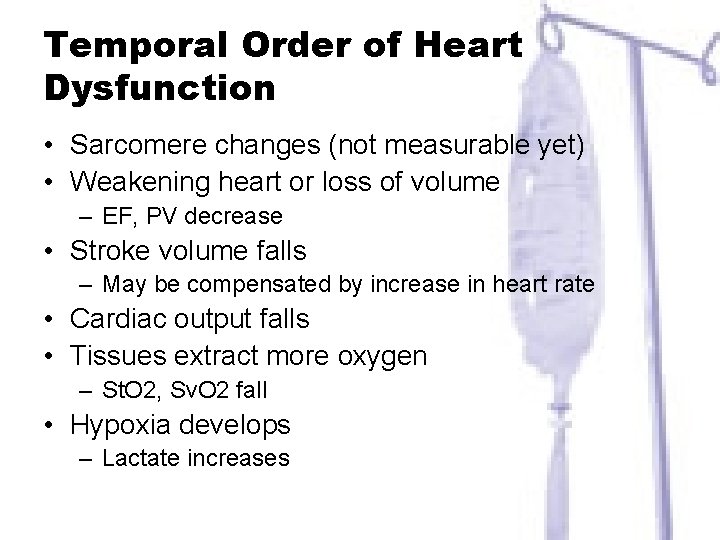
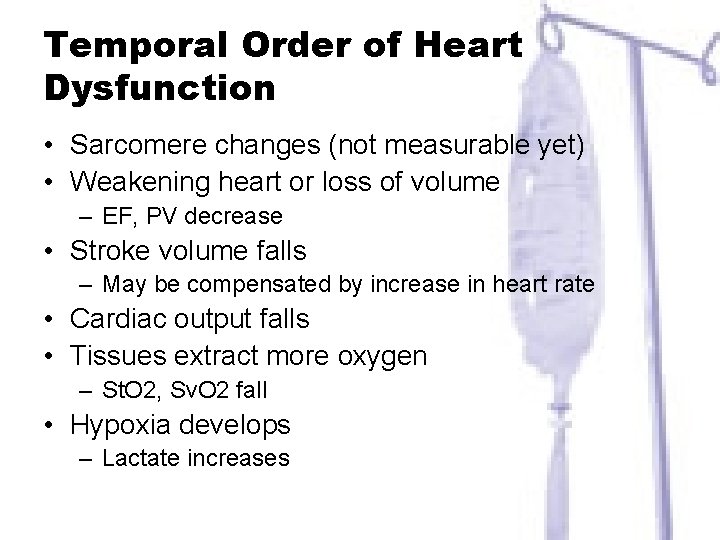
Temporal Order of Heart Dysfunction • Sarcomere changes (not measurable yet) • Weakening heart or loss of volume – EF, PV decrease • Stroke volume falls – May be compensated by increase in heart rate • Cardiac output falls • Tissues extract more oxygen – St. O 2, Sv. O 2 fall • Hypoxia develops – Lactate increases
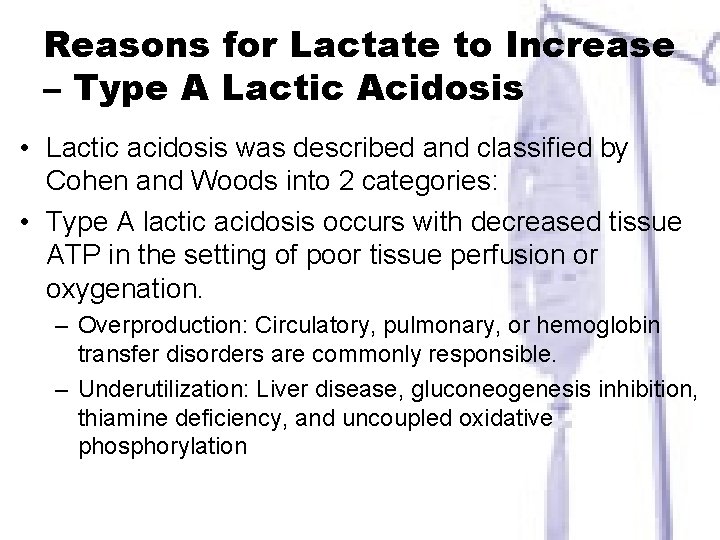
Reasons for Lactate to Increase – Type A Lactic Acidosis • Lactic acidosis was described and classified by Cohen and Woods into 2 categories: • Type A lactic acidosis occurs with decreased tissue ATP in the setting of poor tissue perfusion or oxygenation. – Overproduction: Circulatory, pulmonary, or hemoglobin transfer disorders are commonly responsible. – Underutilization: Liver disease, gluconeogenesis inhibition, thiamine deficiency, and uncoupled oxidative phosphorylation
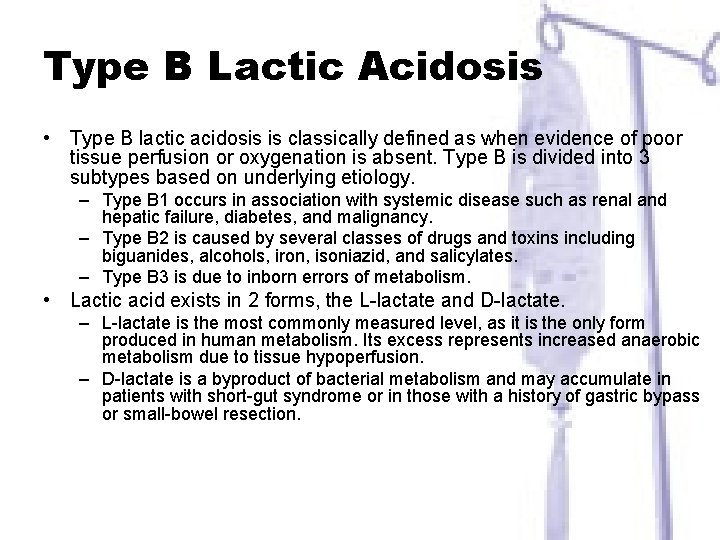
Type B Lactic Acidosis • Type B lactic acidosis is classically defined as when evidence of poor tissue perfusion or oxygenation is absent. Type B is divided into 3 subtypes based on underlying etiology. – Type B 1 occurs in association with systemic disease such as renal and hepatic failure, diabetes, and malignancy. – Type B 2 is caused by several classes of drugs and toxins including biguanides, alcohols, iron, isoniazid, and salicylates. – Type B 3 is due to inborn errors of metabolism. • Lactic acid exists in 2 forms, the L-lactate and D-lactate. – L-lactate is the most commonly measured level, as it is the only form produced in human metabolism. Its excess represents increased anaerobic metabolism due to tissue hypoperfusion. – D-lactate is a byproduct of bacterial metabolism and may accumulate in patients with short-gut syndrome or in those with a history of gastric bypass or small-bowel resection.
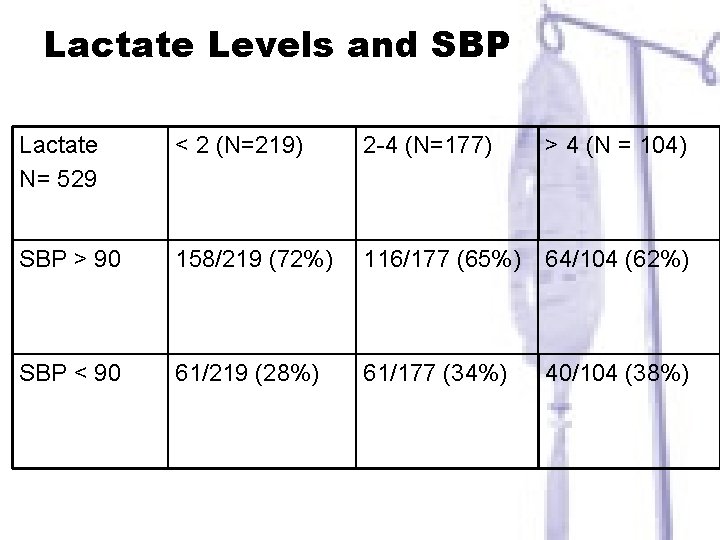
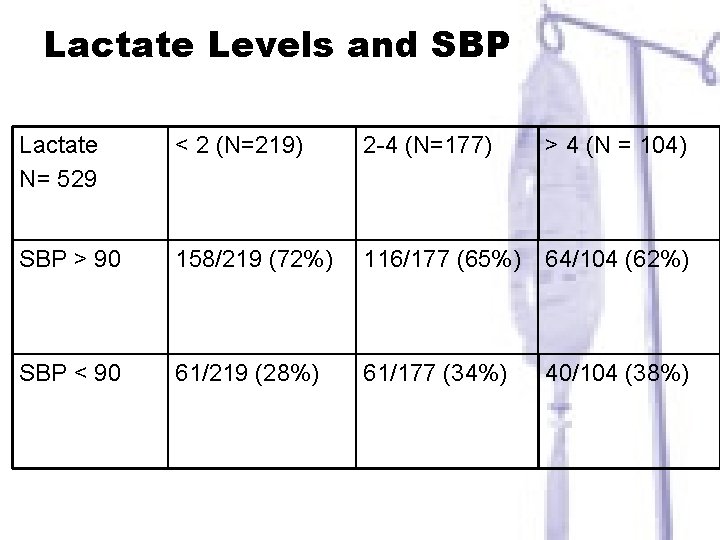
Lactate Levels and SBP Lactate N= 529 < 2 (N=219) 2 -4 (N=177) > 4 (N = 104) SBP > 90 158/219 (72%) 116/177 (65%) 64/104 (62%) SBP < 90 61/219 (28%) 61/177 (34%) 40/104 (38%)
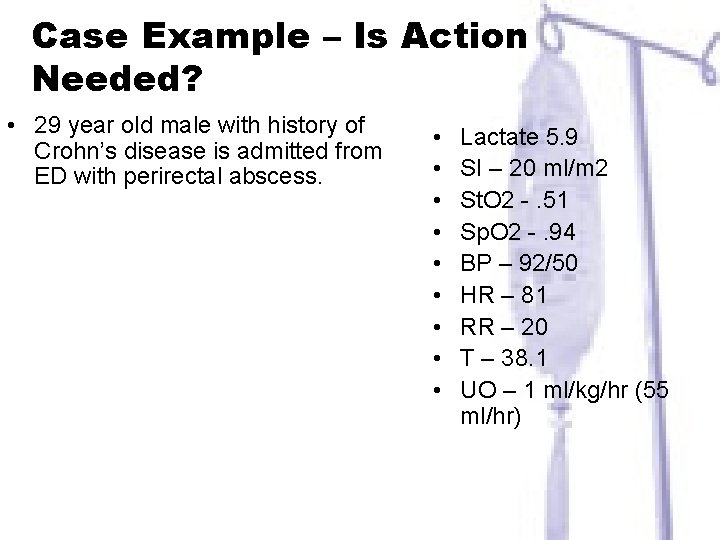
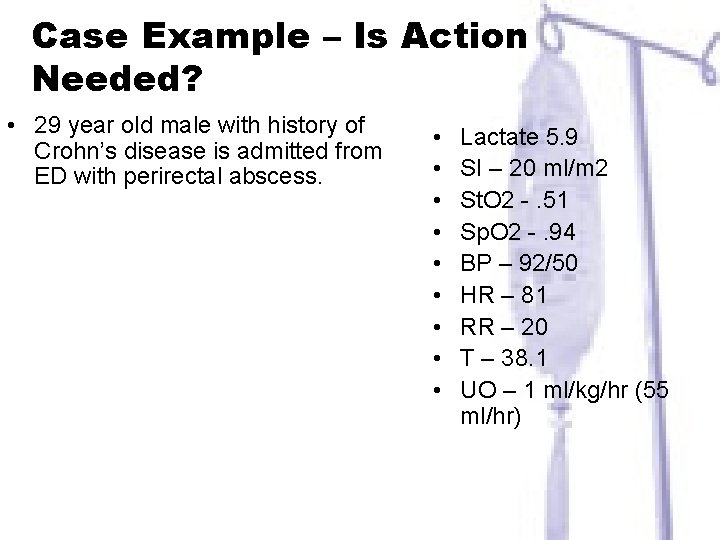
Case Example – Is Action Needed? • 29 year old male with history of Crohn’s disease is admitted from ED with perirectal abscess. • • • Lactate 5. 9 SI – 20 ml/m 2 St. O 2 -. 51 Sp. O 2 -. 94 BP – 92/50 HR – 81 RR – 20 T – 38. 1 UO – 1 ml/kg/hr (55 ml/hr)
Sepsis often progresses when the host cannot contain the primary infection • a problem most often related to – characteristics of the microorganism, • such as a high burden of infection • the presence of superantigens and other virulence factors, • resistance to opsonization and phagocytosis, • antibiotic resistance.
Cell dysoxia • Epithelial cells have diminished oxygen consumption – due to a depletion of nicotinamide adenine dinucleotide (NAD) • Concept of cell stunning or hibernation
Pathophysiology of Sepsis What do we need to know
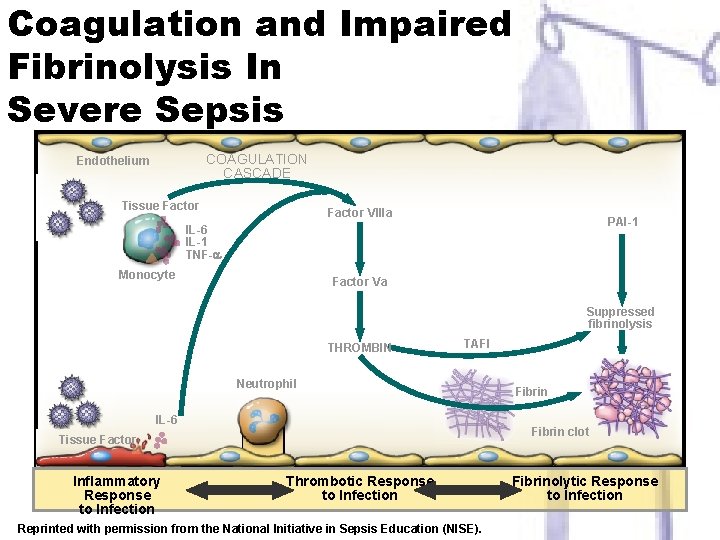
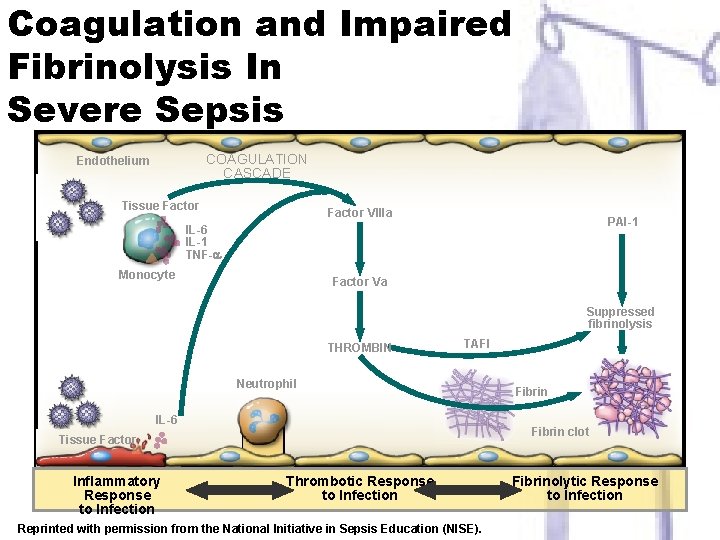
Coagulation and Impaired Fibrinolysis In Severe Sepsis COAGULATION CASCADE Endothelium Tissue Factor VIIIa PAI-1 IL-6 IL-1 TNF- Monocyte Factor Va Suppressed fibrinolysis THROMBIN TAFI Neutrophil IL-6 Fibrin clot Tissue Factor Inflammatory Response to Infection Fibrin Thrombotic Response to Infection Reprinted with permission from the National Initiative in Sepsis Education (NISE). Fibrinolytic Response to Infection
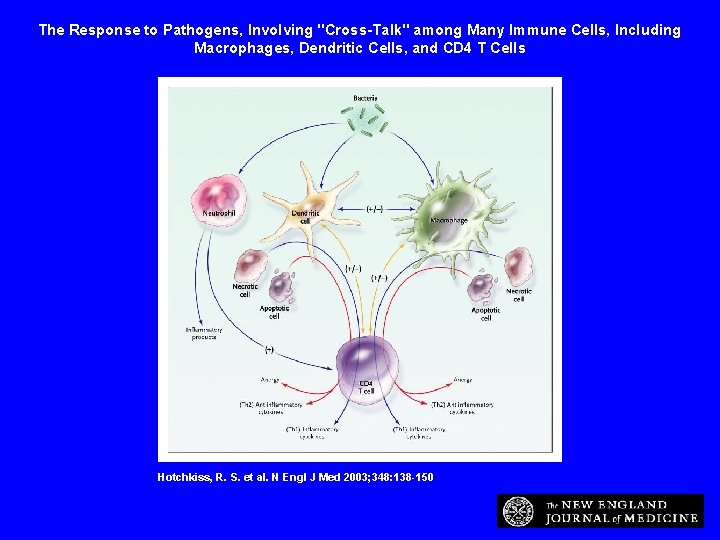
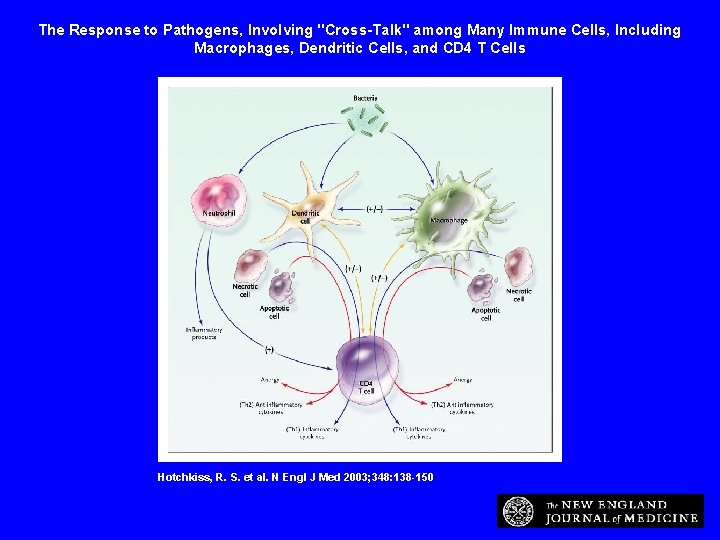
The Response to Pathogens, Involving "Cross-Talk" among Many Immune Cells, Including Macrophages, Dendritic Cells, and CD 4 T Cells Hotchkiss, R. S. et al. N Engl J Med 2003; 348: 138 -150
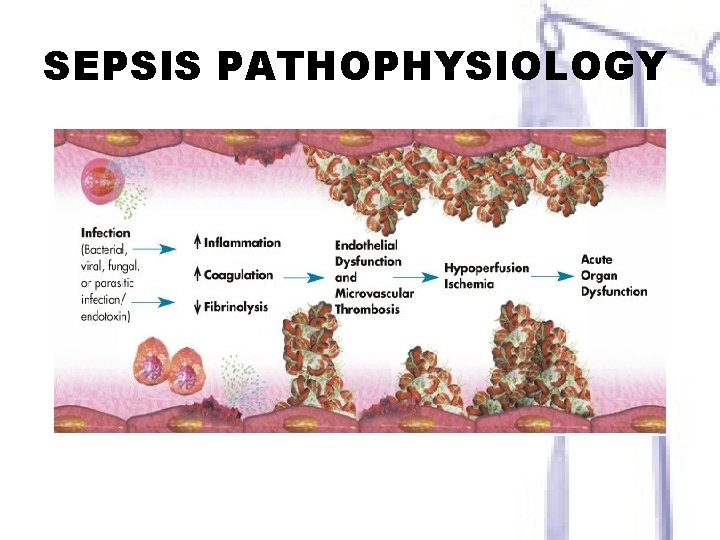
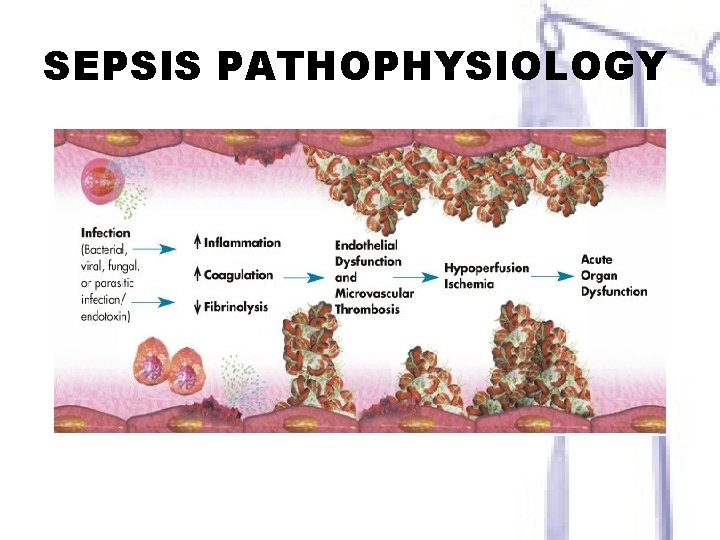
SEPSIS PATHOPHYSIOLOGY
Identification and Management of Severe Sepsis Potential Biomarkers
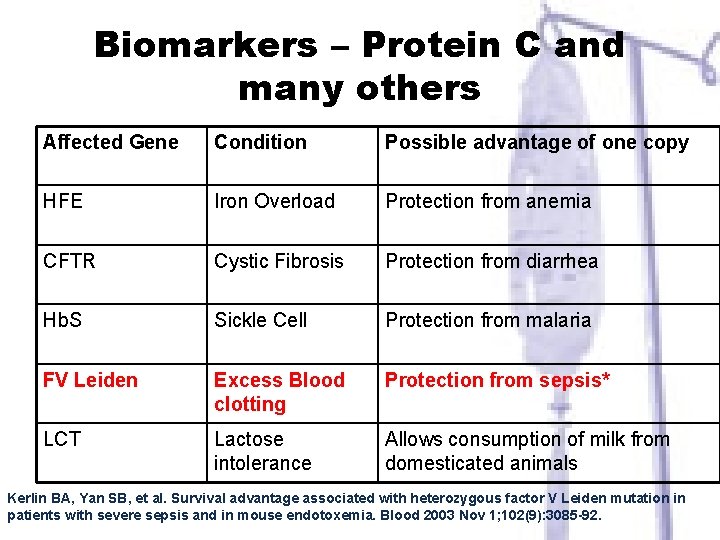
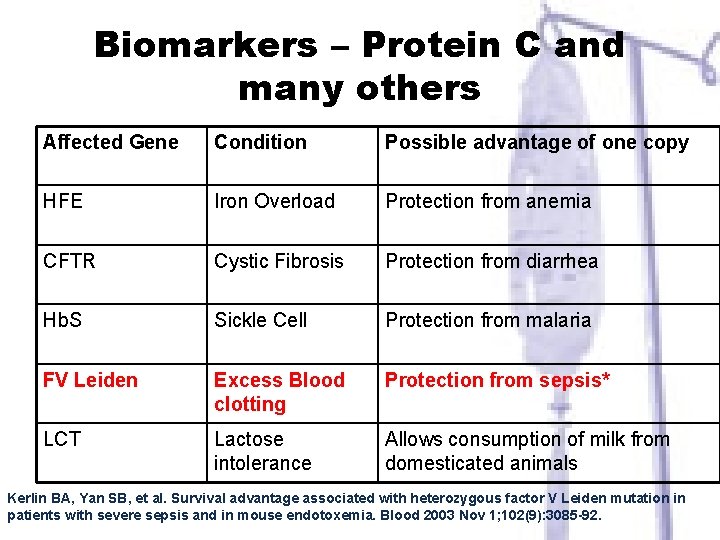
Biomarkers – Protein C and many others Affected Gene Condition Possible advantage of one copy HFE Iron Overload Protection from anemia CFTR Cystic Fibrosis Protection from diarrhea Hb. S Sickle Cell Protection from malaria FV Leiden Excess Blood clotting Protection from sepsis* LCT Lactose intolerance Allows consumption of milk from domesticated animals Kerlin BA, Yan SB, et al. Survival advantage associated with heterozygous factor V Leiden mutation in patients with severe sepsis and in mouse endotoxemia. Blood 2003 Nov 1; 102(9): 3085 -92.
How do We Identify Sepsis Now? In absence of biomarkers, must rely on crude physical indicators
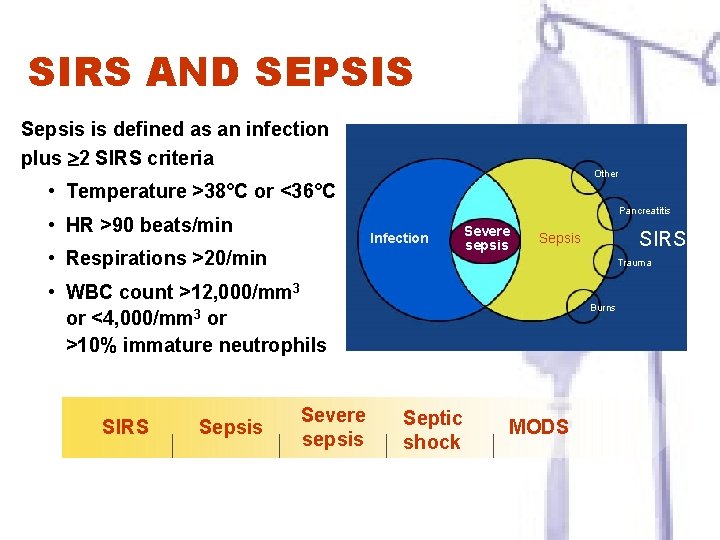
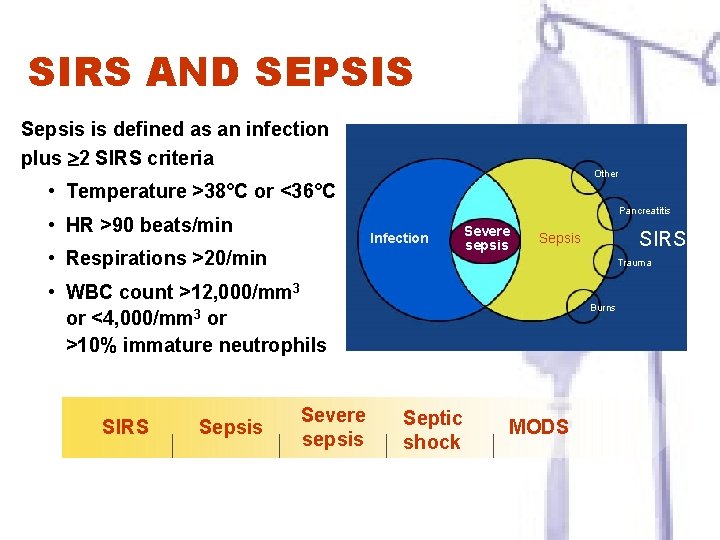
SIRS AND SEPSIS Sepsis is defined as an infection plus 2 SIRS criteria Other • Temperature >38°C or <36°C Pancreatitis • HR >90 beats/min Infection • Respirations >20/min Severe sepsis Trauma • WBC count >12, 000/mm 3 or <4, 000/mm 3 or >10% immature neutrophils SIRS Sepsis Severe sepsis Levy MM, et al. Crit Care Med. 2003; 31: 1250 -1256. Burns Septic shock MODS
• Reduce mortality in severe sepsis by 25% over the next five years (Fall 2002): Barcelona Declaration • Surviving Sepsis Campaign Guidelines for Management of Severe Sepsis and Septic Shock – Crit Care Med 2008: 36(1) 296 -327 • www. survivingsepsis. org
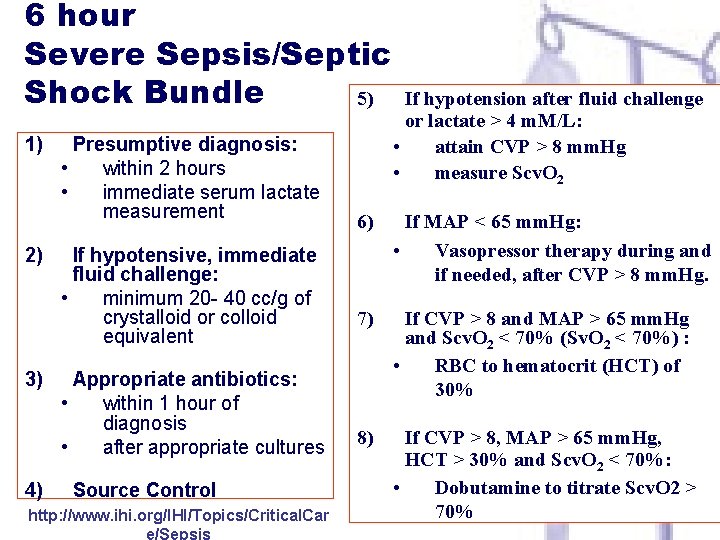
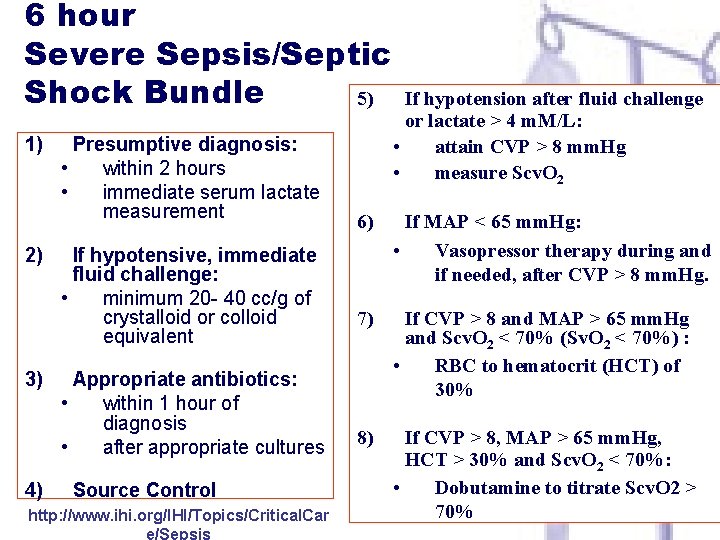
6 hour Severe Sepsis/Septic Shock Bundle 5) 1) 2) 3) 4) Presumptive diagnosis: • within 2 hours • immediate serum lactate measurement If hypotensive, immediate fluid challenge: • minimum 20 - 40 cc/g of crystalloid or colloid equivalent Appropriate antibiotics: • within 1 hour of diagnosis • after appropriate cultures Source Control http: //www. ihi. org/IHI/Topics/Critical. Car e/Sepsis If hypotension after fluid challenge or lactate > 4 m. M/L: • attain CVP > 8 mm. Hg • measure Scv. O 2 6) If MAP < 65 mm. Hg: • Vasopressor therapy during and if needed, after CVP > 8 mm. Hg. 7) If CVP > 8 and MAP > 65 mm. Hg and Scv. O 2 < 70% (Sv. O 2 < 70%) : • RBC to hematocrit (HCT) of 30% 8) If CVP > 8, MAP > 65 mm. Hg, HCT > 30% and Scv. O 2 < 70%: • Dobutamine to titrate Scv. O 2 > 70%
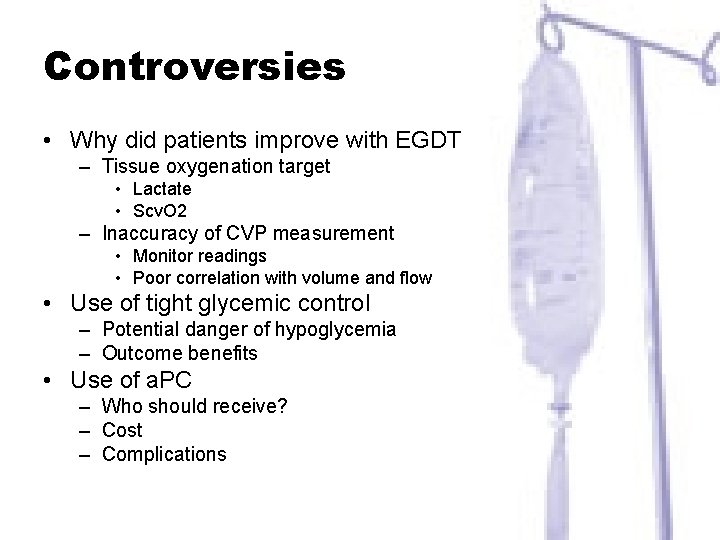
Controversies • Why did patients improve with EGDT – Tissue oxygenation target • Lactate • Scv. O 2 – Inaccuracy of CVP measurement • Monitor readings • Poor correlation with volume and flow • Use of tight glycemic control – Potential danger of hypoglycemia – Outcome benefits • Use of a. PC – Who should receive? – Cost – Complications
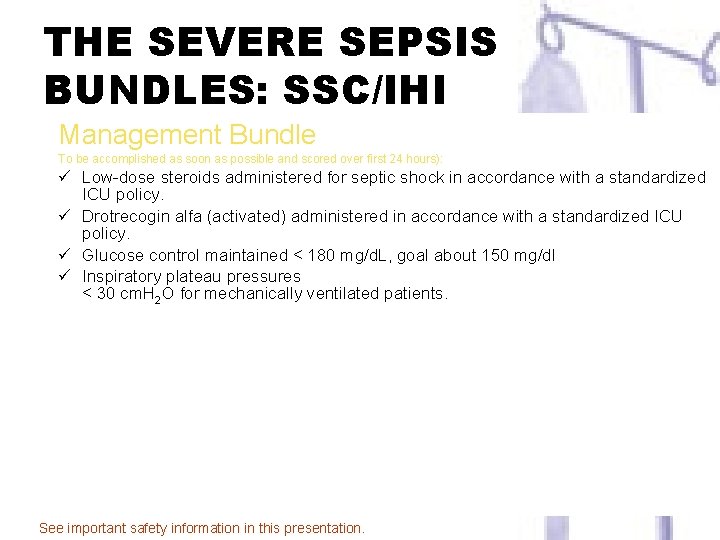
THE SEVERE SEPSIS BUNDLES: SSC/IHI Management Bundle To be accomplished as soon as possible and scored over first 24 hours): ü Low-dose steroids administered for septic shock in accordance with a standardized ICU policy. ü Drotrecogin alfa (activated) administered in accordance with a standardized ICU policy. ü Glucose control maintained < 180 mg/d. L, goal about 150 mg/dl ü Inspiratory plateau pressures < 30 cm. H 2 O for mechanically ventilated patients. http: //www. ihi. org Accessed 3/23/05. See important safety information in this presentation.
Improving Outcomes in Severe Sepsis & Septic Shock: A Prospective Multi-Center Collaborative Study Before and After Implementation of an Early Sepsis Initiative The Multi-Center Severe Sepsis & Septic Shock Collaborative Group Chad M. Cannon, MD, FAAEM, FACEP Assistant Clinical Professor Department of Emergency Medicine University of Kansas Hospital Kansas City, Kansas ccannon@kumc. edu
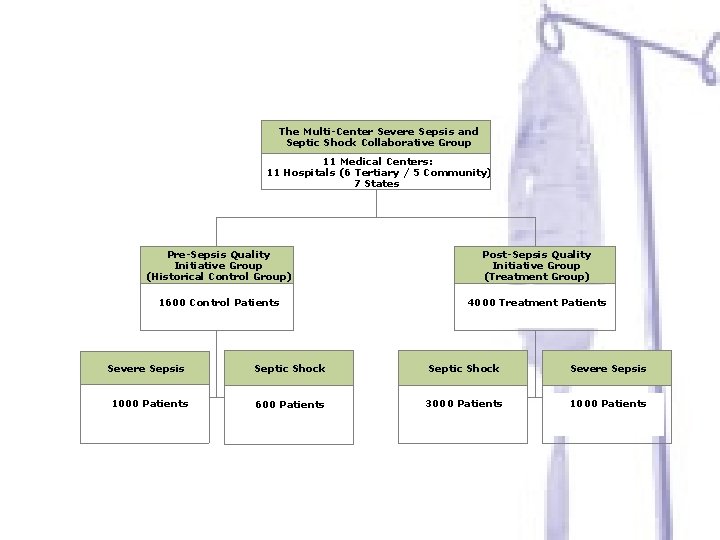
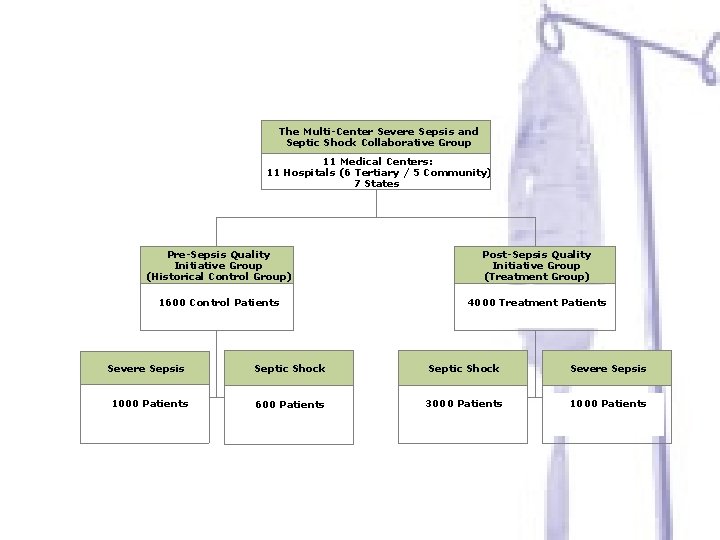
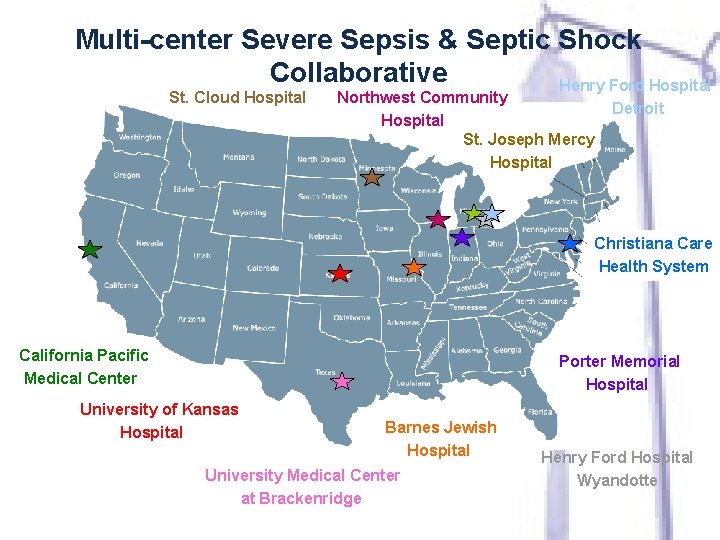
The Multi-Center Severe Sepsis and Septic Shock Collaborative Group 11 Medical Centers: 11 Hospitals (6 Tertiary / 5 Community) 7 States Pre-Sepsis Quality Initiative Group (Historical Control Group) Post-Sepsis Quality Initiative Group (Treatment Group) 1600 Control Patients 4000 Treatment Patients Severe Sepsis 1000 Patients Septic Shock Severe Sepsis 600 Patients 3000 Patients 1000 Patients
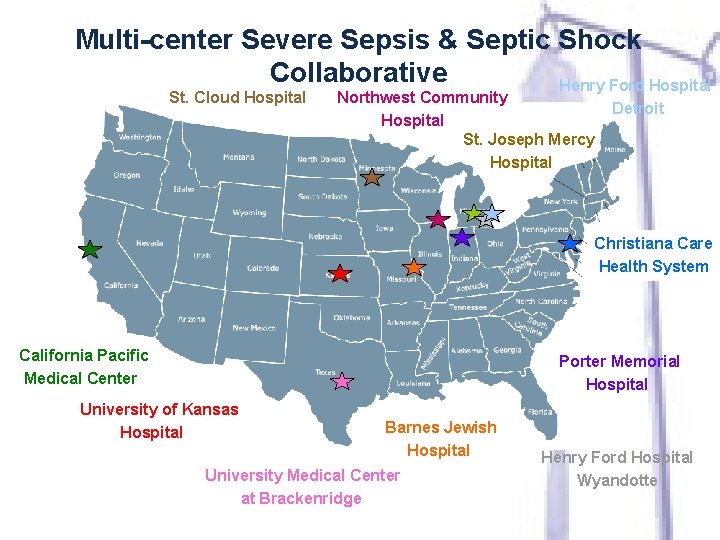
Multi-center Severe Sepsis & Septic Shock Collaborative Henry Ford Hospital St. Cloud Hospital Northwest Community Hospital St. Joseph Mercy Hospital Detroit Christiana Care Health System California Pacific Medical Center Porter Memorial Hospital University of Kansas Hospital Barnes Jewish Hospital University Medical Center at Brackenridge Henry Ford Hospital Wyandotte
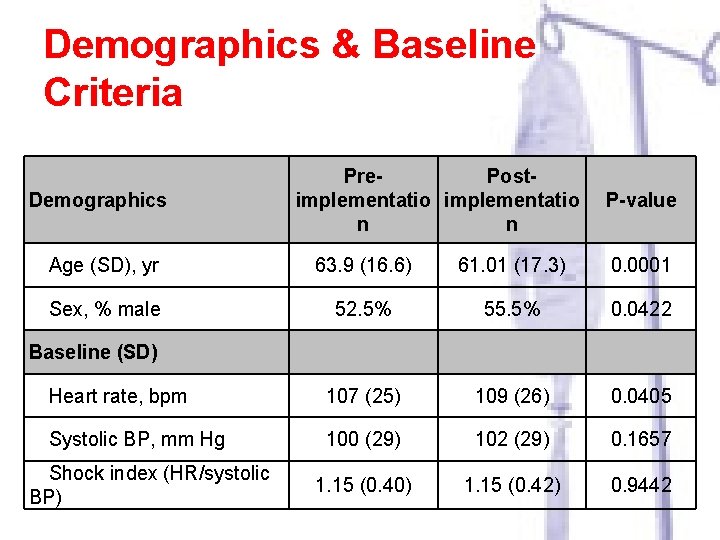
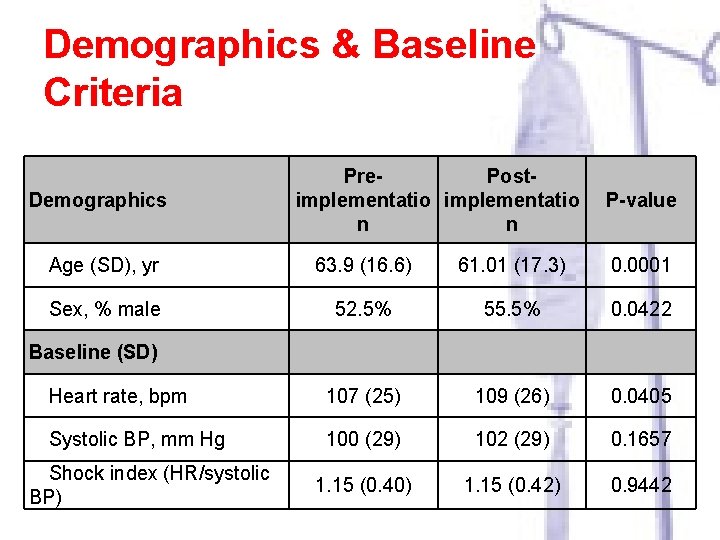
Demographics & Baseline Criteria Demographics Pre. Postimplementatio n n P-value Age (SD), yr 63. 9 (16. 6) 61. 01 (17. 3) 0. 0001 Sex, % male 52. 5% 55. 5% 0. 0422 107 (25) 109 (26) 0. 0405 100 (29) 102 (29) 0. 1657 1. 15 (0. 40) 1. 15 (0. 42) 0. 9442 Baseline (SD) Heart rate, bpm Systolic BP, mm Hg Shock index (HR/systolic BP)
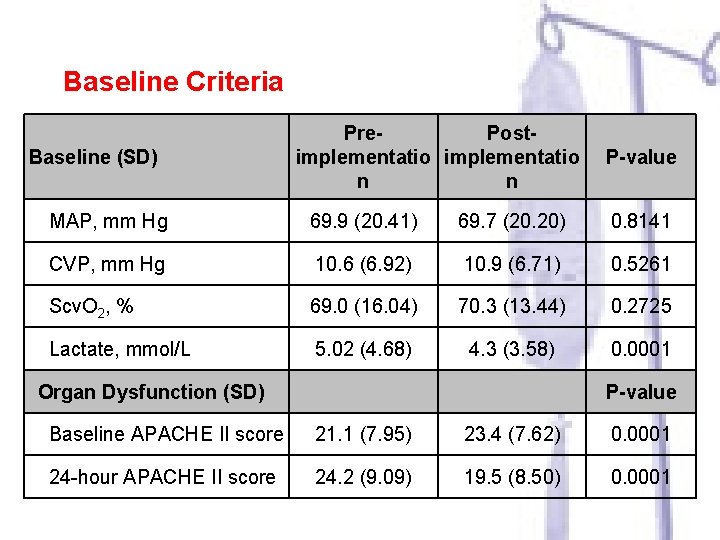
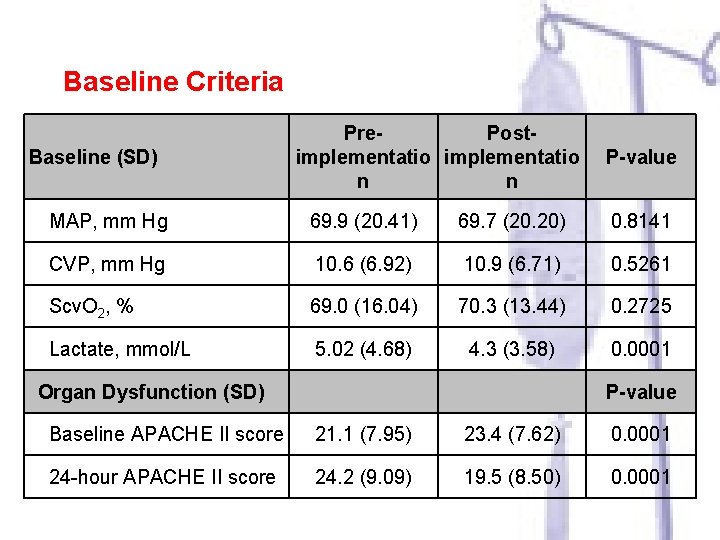
Baseline Criteria Baseline (SD) Pre. Postimplementatio n n P-value MAP, mm Hg 69. 9 (20. 41) 69. 7 (20. 20) 0. 8141 CVP, mm Hg 10. 6 (6. 92) 10. 9 (6. 71) 0. 5261 Scv. O 2, % 69. 0 (16. 04) 70. 3 (13. 44) 0. 2725 Lactate, mmol/L 5. 02 (4. 68) 4. 3 (3. 58) 0. 0001 Organ Dysfunction (SD) P-value Baseline APACHE II score 21. 1 (7. 95) 23. 4 (7. 62) 0. 0001 24 -hour APACHE II score 24. 2 (9. 09) 19. 5 (8. 50) 0. 0001
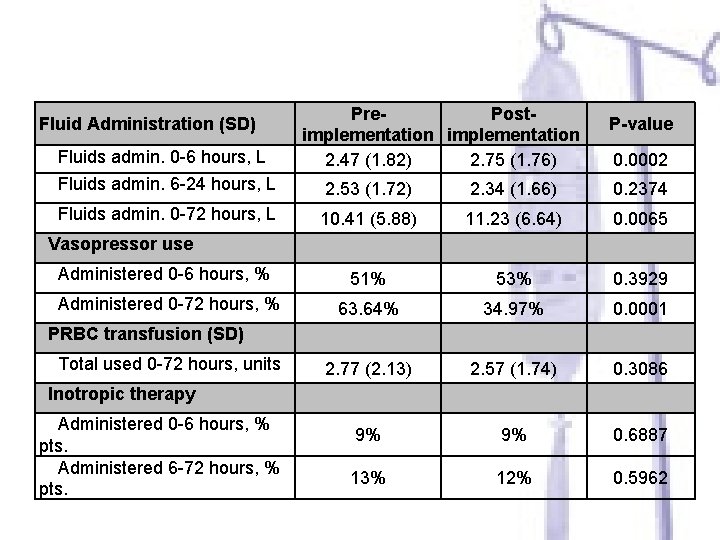
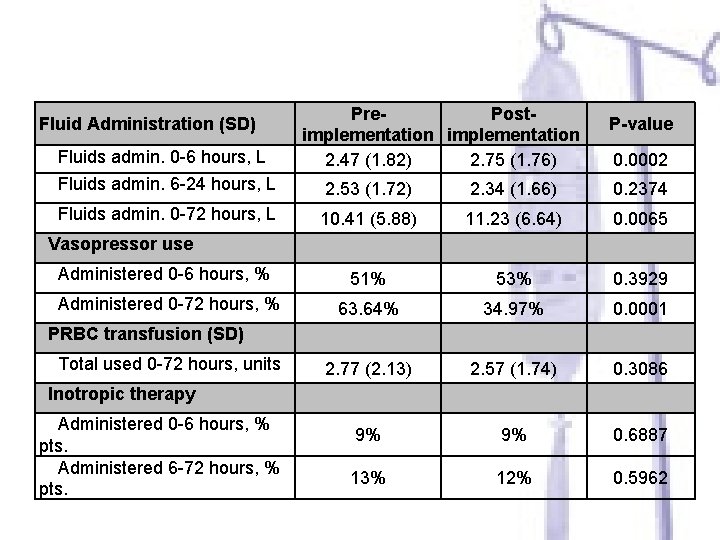
Fluid Administration (SD) Fluids admin. 0 -6 hours, L Pre. Postimplementation 2. 47 (1. 82) 2. 75 (1. 76) P-value 0. 0002 Fluids admin. 6 -24 hours, L 2. 53 (1. 72) 2. 34 (1. 66) 0. 2374 Fluids admin. 0 -72 hours, L 10. 41 (5. 88) 11. 23 (6. 64) 0. 0065 Administered 0 -6 hours, % 51% 53% 0. 3929 Administered 0 -72 hours, % 63. 64% 34. 97% 0. 0001 2. 77 (2. 13) 2. 57 (1. 74) 0. 3086 9% 9% 0. 6887 13% 12% 0. 5962 Vasopressor use PRBC transfusion (SD) Total used 0 -72 hours, units Inotropic therapy Administered 0 -6 hours, % pts. Administered 6 -72 hours, % pts.
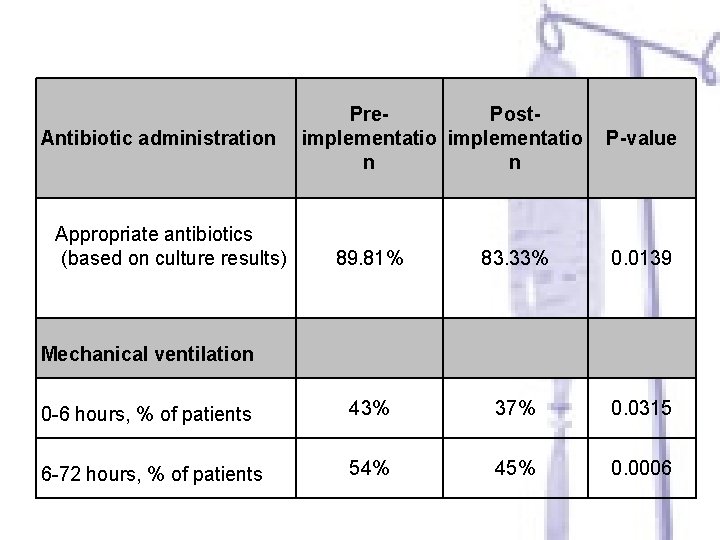
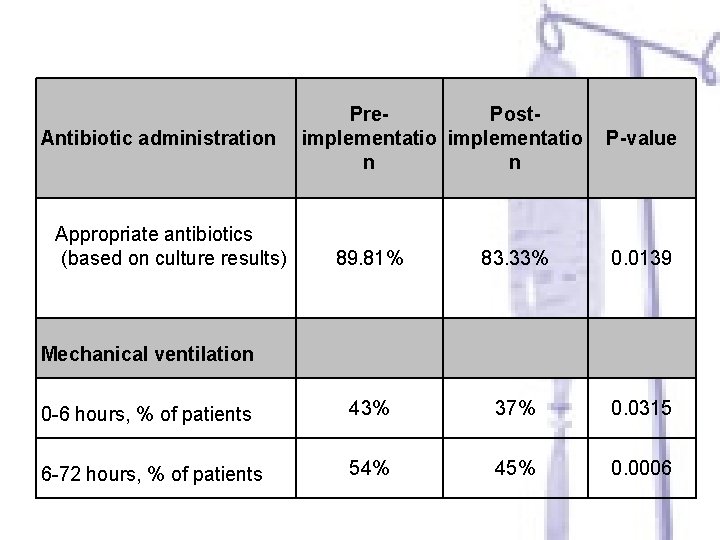
Antibiotic administration Pre. Postimplementatio n n Appropriate antibiotics (based on culture results) 89. 81% P-value 83. 33% 0. 0139 Mechanical ventilation 0 -6 hours, % of patients 43% 37% 0. 0315 6 -72 hours, % of patients 54% 45% 0. 0006
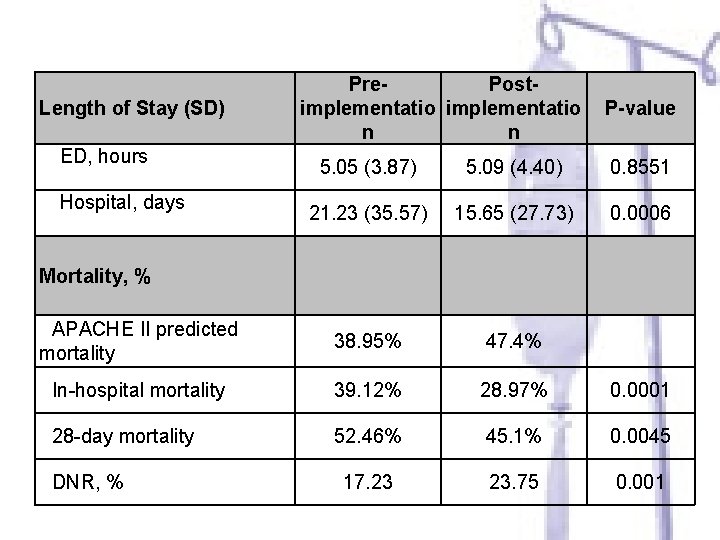
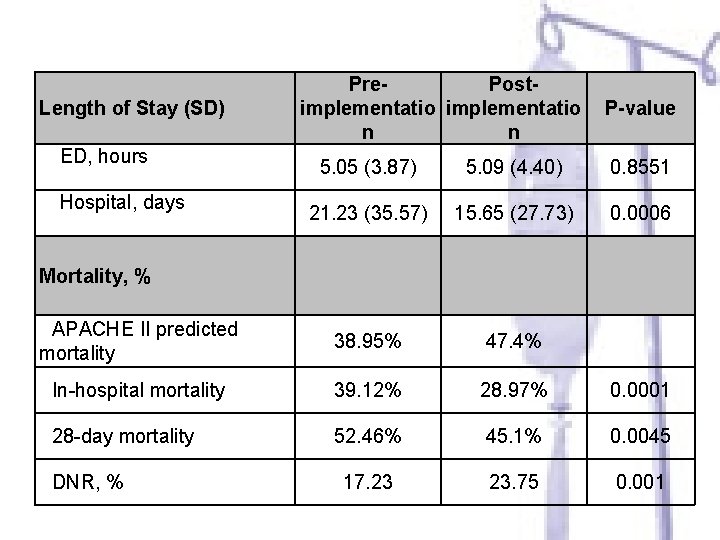
Length of Stay (SD) ED, hours Pre. Postimplementatio n n P-value 5. 05 (3. 87) 5. 09 (4. 40) 0. 8551 21. 23 (35. 57) 15. 65 (27. 73) 0. 0006 APACHE II predicted mortality 38. 95% 47. 4% In-hospital mortality 39. 12% 28. 97% 0. 0001 28 -day mortality 52. 46% 45. 1% 0. 0045 17. 23 23. 75 0. 001 Hospital, days Mortality, % DNR, %
Case Studies
Implementation of Evidenced Based Practice/Protocols • Every day, every shift, make sure each patient is screened for the following – Does the patient have severe sepsis? If so, • Is it documented properly • Has the sepsis protocols been implemented • Measure results – Have good baseline data – Evaluate impact of protocol and documentation implementation
 Surviving sepsis definition
Surviving sepsis definition Quick sofa
Quick sofa Keys to content writing
Keys to content writing Priesthood keys restored in kirtland temple
Priesthood keys restored in kirtland temple Campaign management implementation guide
Campaign management implementation guide Heorot pronunciation
Heorot pronunciation Wolfgang amadeus mozart was the only surviving
Wolfgang amadeus mozart was the only surviving Surviving a flood
Surviving a flood Surviving in an estuary answers
Surviving in an estuary answers The most ancient surviving seed plants are the
The most ancient surviving seed plants are the 7 wonders of the world map
7 wonders of the world map Folk examples
Folk examples Ann marie cotton
Ann marie cotton Oldest surviving greek drama
Oldest surviving greek drama Bjarni geir viðarsson
Bjarni geir viðarsson Sepsis hour 1 bundle
Sepsis hour 1 bundle Sepsis pp respiratorio
Sepsis pp respiratorio Sepsis significado
Sepsis significado Puerperal sepsis
Puerperal sepsis Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Dr ali hieatt
Dr ali hieatt Sepsis care near palo alto
Sepsis care near palo alto Puerperal sepsis
Puerperal sepsis Pae sepsis neonatal
Pae sepsis neonatal Give 3 take 3 sepsis
Give 3 take 3 sepsis Sepsis
Sepsis Sepsis 6 bundle
Sepsis 6 bundle Sofa escala
Sofa escala Riesgo de sepsis nanda
Riesgo de sepsis nanda Criterios de gibbs
Criterios de gibbs Sepsis bundle
Sepsis bundle Sepsis
Sepsis Lady neck
Lady neck Hora dorada sepsis
Hora dorada sepsis Hypotensis
Hypotensis Neonatal sepsis symptoms
Neonatal sepsis symptoms What is sepsis disease
What is sepsis disease Sepsis dietary management
Sepsis dietary management Neonatarum
Neonatarum Driver diagram example
Driver diagram example Accefluid
Accefluid Dental sepsis
Dental sepsis Gdp sepsis decision support tool
Gdp sepsis decision support tool Sepsis definition
Sepsis definition Stages of sepsis
Stages of sepsis Neonatal sepsis nelson pediatrics
Neonatal sepsis nelson pediatrics Hemodynamics
Hemodynamics Prevention of puerperal sepsis
Prevention of puerperal sepsis Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau