Part 2 Mechanical Properties of the Lung and




- Slides: 46
Part 2 Mechanical Properties of the Lung and Chest Wall: Static and Dynamic 1
Section I STATIC LUNG MECHNICS: The mechanical properties of a lung whose volume is not changing with time 2
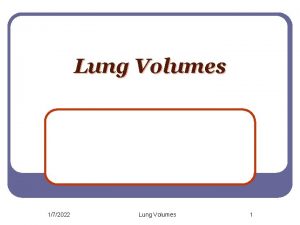
1. Pulmonary Volume and Capacity 3
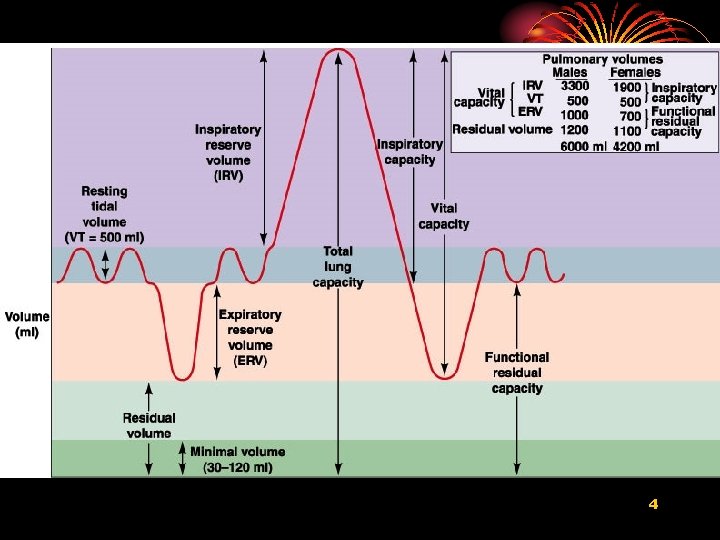
4
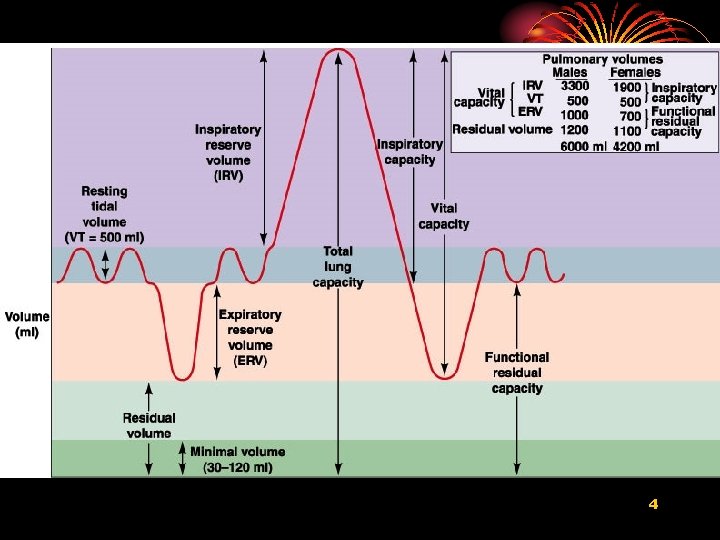
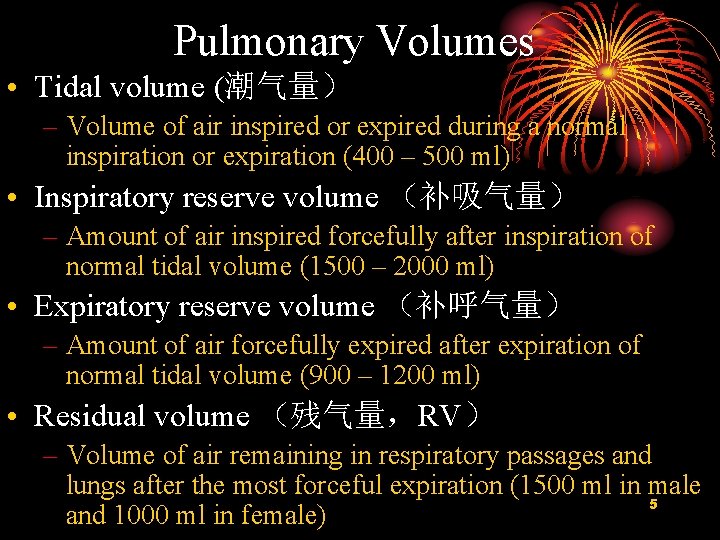
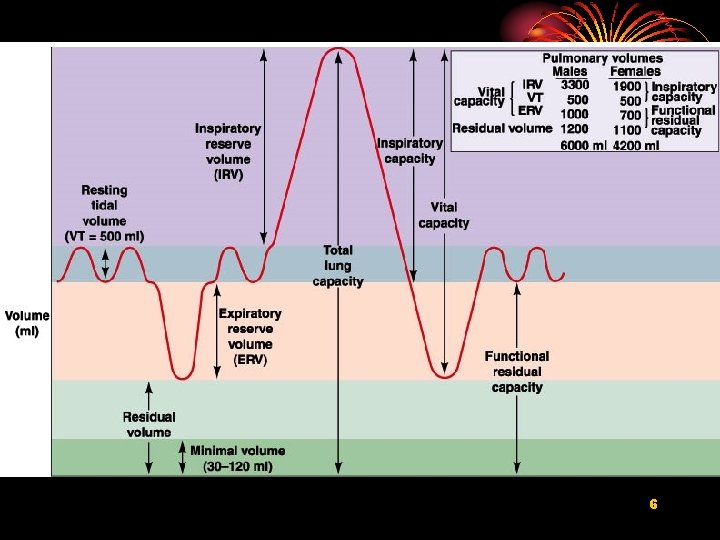
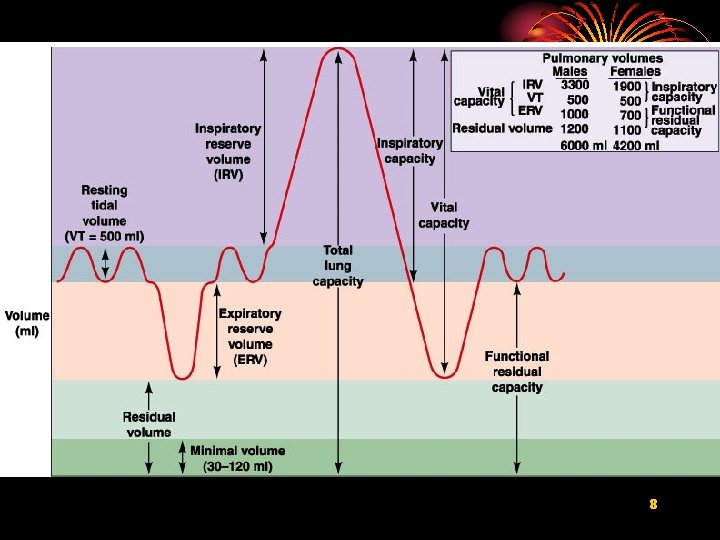
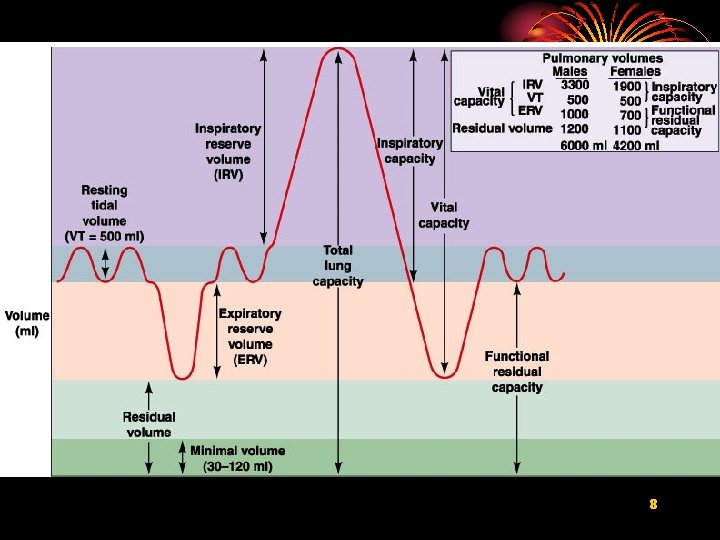
Pulmonary Volumes • Tidal volume (潮气量) – Volume of air inspired or expired during a normal inspiration or expiration (400 – 500 ml) • Inspiratory reserve volume (补吸气量) – Amount of air inspired forcefully after inspiration of normal tidal volume (1500 – 2000 ml) • Expiratory reserve volume (补呼气量) – Amount of air forcefully expired after expiration of normal tidal volume (900 – 1200 ml) • Residual volume (残气量,RV) – Volume of air remaining in respiratory passages and lungs after the most forceful expiration (1500 ml in male 5 and 1000 ml in female)
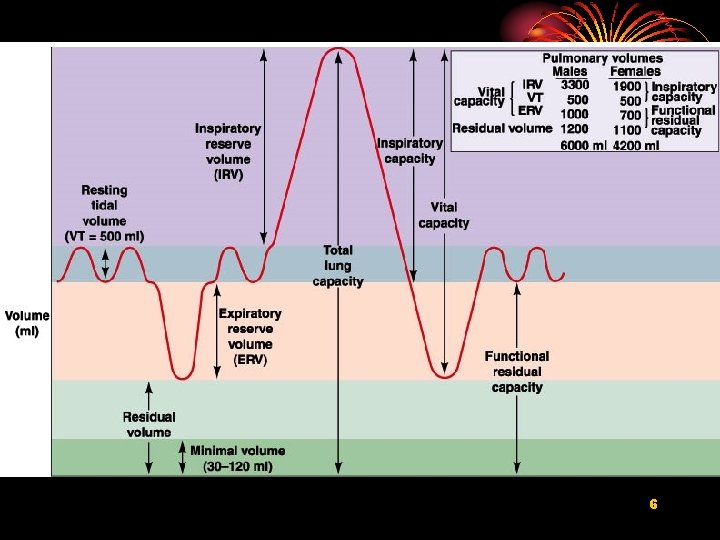
6
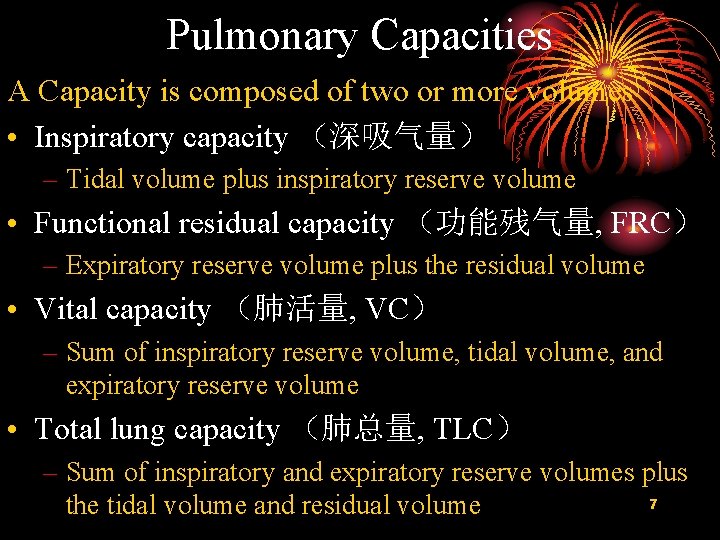
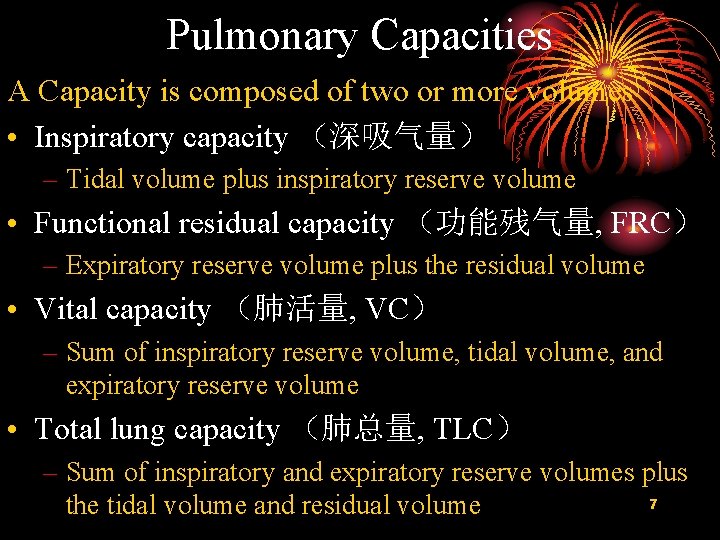
Pulmonary Capacities A Capacity is composed of two or more volumes • Inspiratory capacity (深吸气量) – Tidal volume plus inspiratory reserve volume • Functional residual capacity (功能残气量, FRC) – Expiratory reserve volume plus the residual volume • Vital capacity (肺活量, VC) – Sum of inspiratory reserve volume, tidal volume, and expiratory reserve volume • Total lung capacity (肺总量, TLC) – Sum of inspiratory and expiratory reserve volumes plus 7 the tidal volume and residual volume
8
RV/TLC • Normally less than 0. 25 • Increase by the obstructive pulmonary disease (RV) • Increase during the restrictive lung disease (TLC) 9
Minute and Alveolar Ventilation • Minute ventilation: Total amount of air moved into and out of respiratory system per minute • Respiratory rate or frequency: Number of breaths taken per minute • Anatomic dead space: Part of respiratory system where gas exchange does not take place • Alveolar ventilation: How much air per minute enters the parts of the respiratory system in 10 which gas exchange takes place
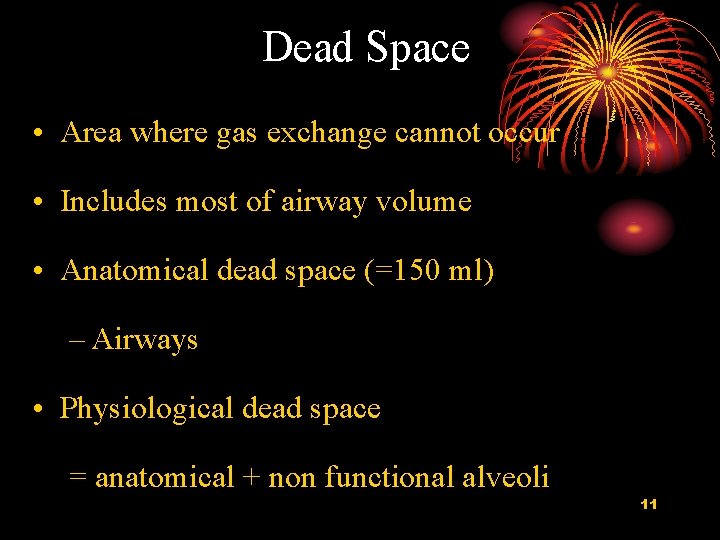
Dead Space • Area where gas exchange cannot occur • Includes most of airway volume • Anatomical dead space (=150 ml) – Airways • Physiological dead space = anatomical + non functional alveoli 11
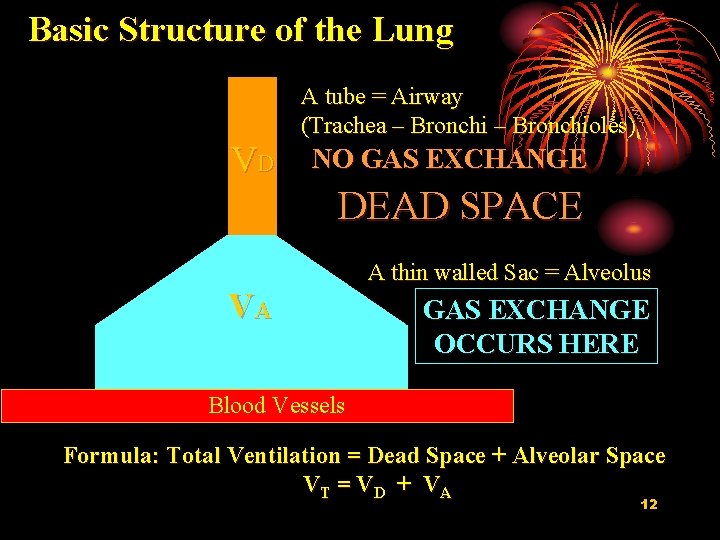
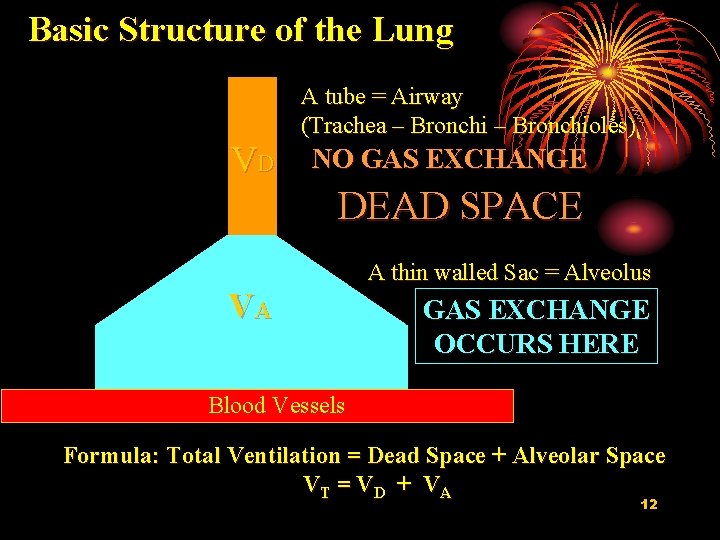
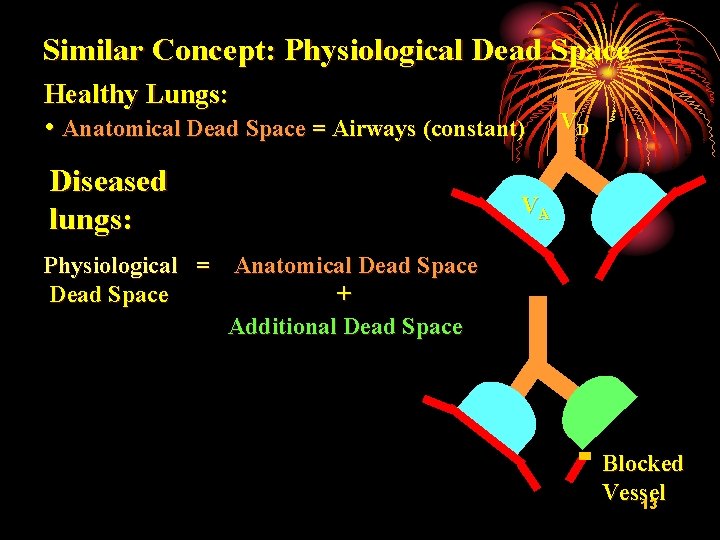
Basic Structure of the Lung A tube = Airway (Trachea – Bronchioles) VD NO GAS EXCHANGE DEAD SPACE VA A thin walled Sac = Alveolus GAS EXCHANGE OCCURS HERE Blood Vessels Formula: Total Ventilation = Dead Space + Alveolar Space VT = V D + V A 12
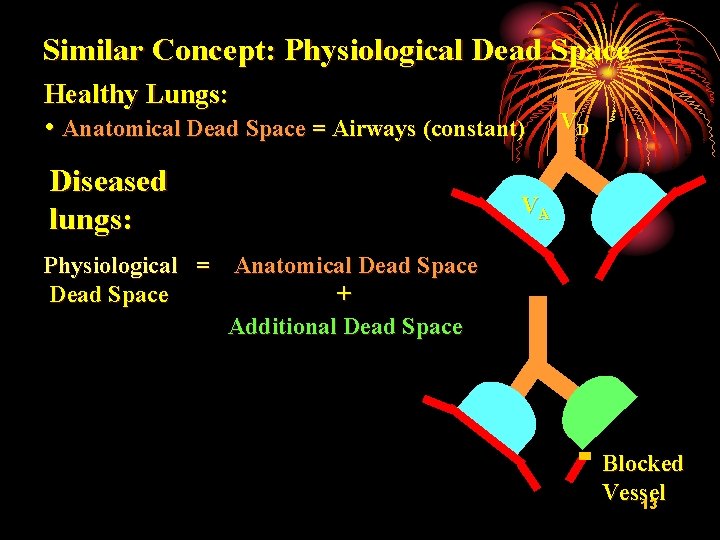
Similar Concept: Physiological Dead Space Healthy Lungs: • Anatomical Dead Space = Airways (constant) Diseased lungs: VD VA Physiological = Anatomical Dead Space + Additional Dead Space Blocked Vessel 13
2. Lung Compliance • Lung compliance (CL) • is a measure of the elastic properties of the lung, • is a reflection of lung distensibility 14
Elasticity • Tendency to return to initial size after distension. • High content of elastin proteins. – Very elastic and resist distension. • Recoil ability. • Elastic tension increases during inspiration and is reduced by recoil during expiration. 15
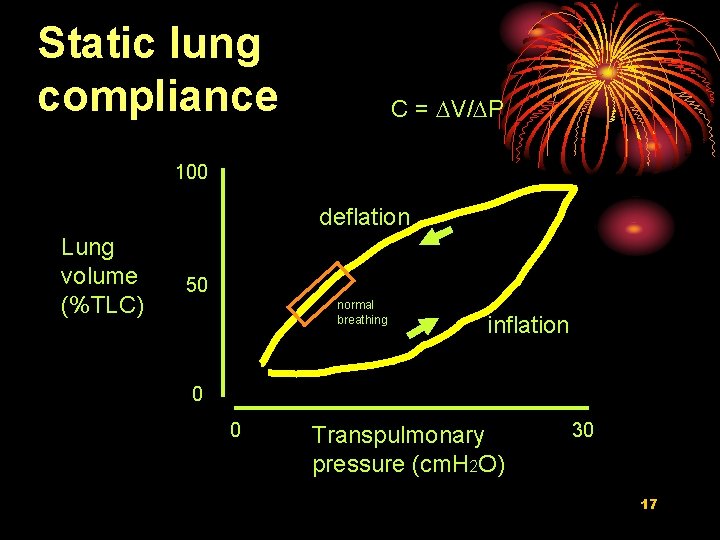
Compliance • Distensibility (stretchability): – Ease with which the lungs can expand. – The compliance is inversely proportional to elastic resistance • Change in lung volume per change in transpulmonary pressure. DV/DP • 100 x more distensible than a balloon. • Specific compliance (比顺应性): the compliance per unit volume 16
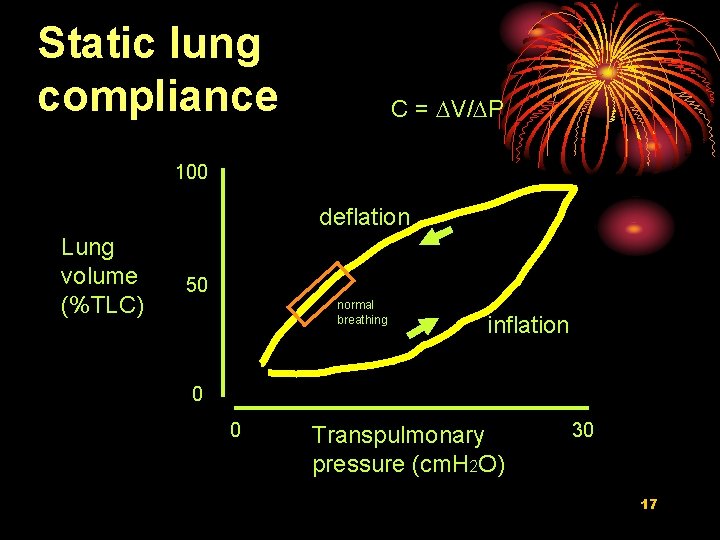
Static lung compliance C = DV/DP 100 deflation Lung volume (%TLC) 50 normal breathing inflation 0 0 Transpulmonary pressure (cm. H 2 O) 30 17
Section II DYNAMIC LUNG MECHANICS Aspects of mechanics that studies the lung in motion 18

1. Dynamic Compliance 19
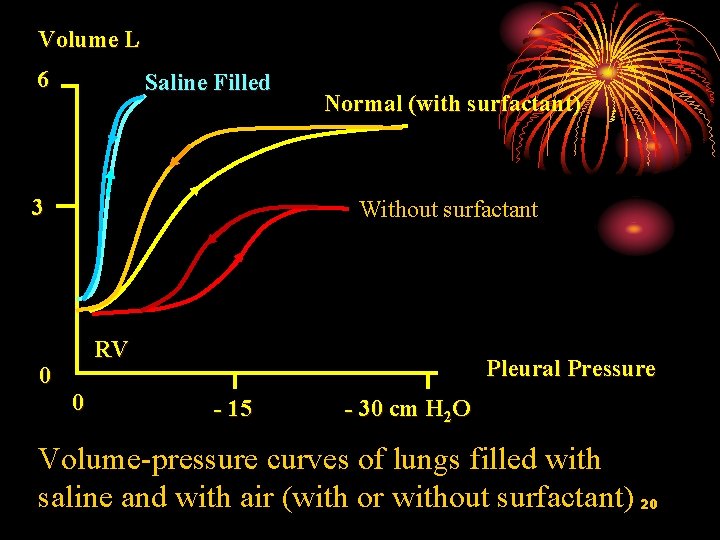
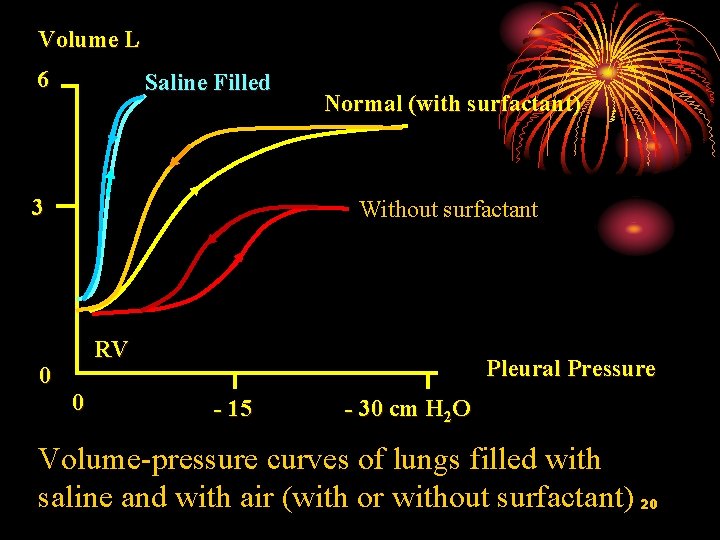
Volume L 6 Saline Filled 3 0 Normal (with surfactant) Without surfactant RV 0 Pleural Pressure - 15 - 30 cm H 2 O Volume-pressure curves of lungs filled with saline and with air (with or without surfactant) 20
Dynamic lung compliance • Is always less than static compliance • Increase during exercise • Increase during sighing and yawning 21

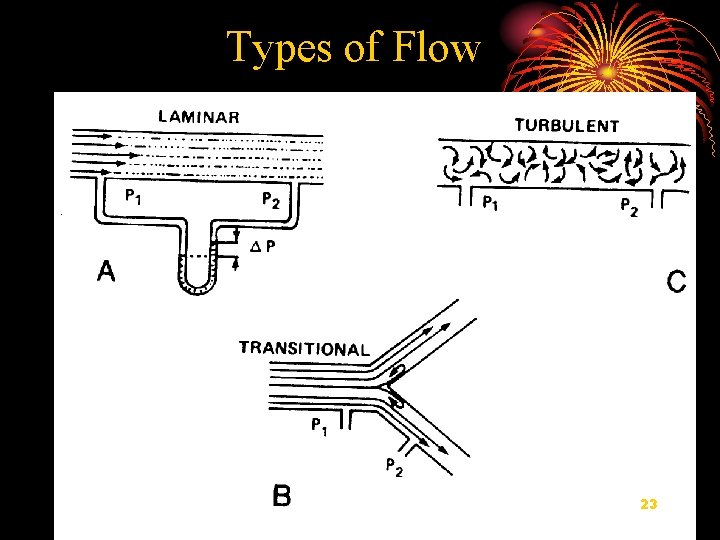
2. Airflow in Airways 22
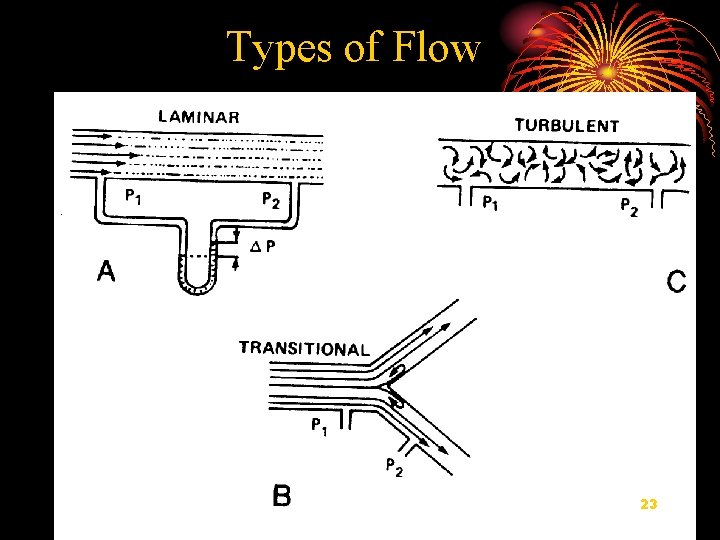
Types of Flow 23
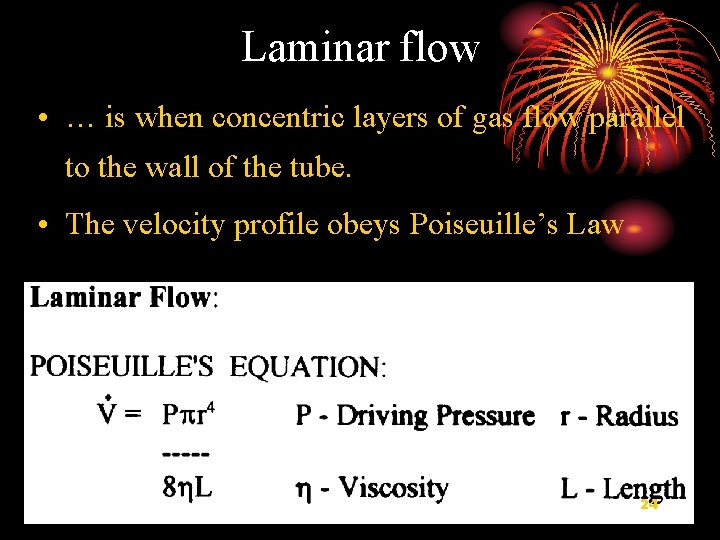
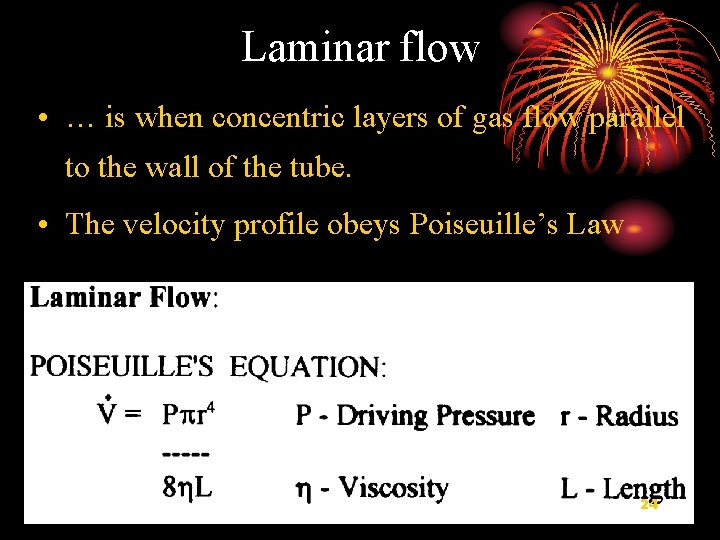
Laminar flow • … is when concentric layers of gas flow parallel to the wall of the tube. • The velocity profile obeys Poiseuille’s Law 24
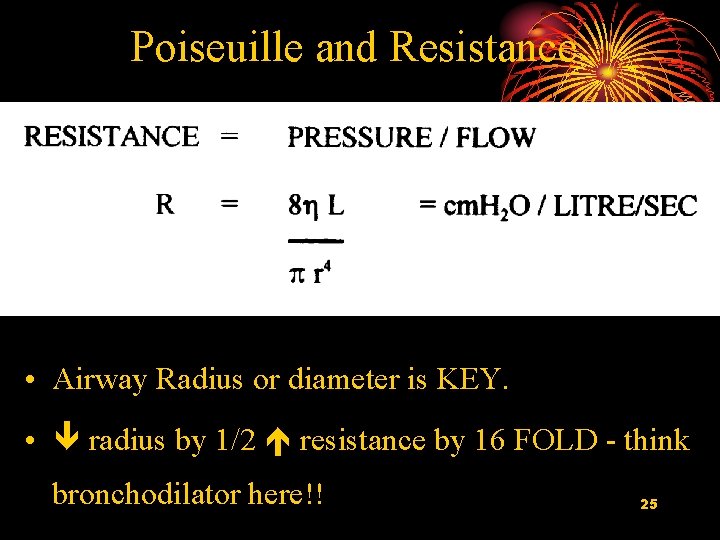
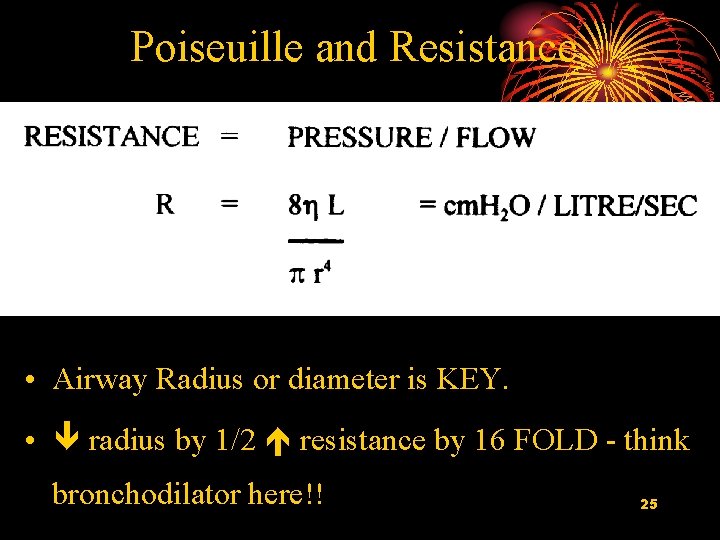
Poiseuille and Resistance • Airway Radius or diameter is KEY. • radius by 1/2 resistance by 16 FOLD - think bronchodilator here!! 25
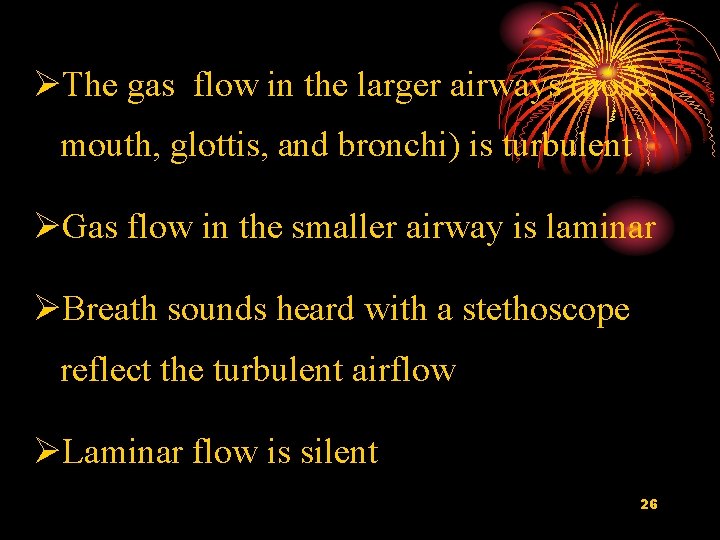
ØThe gas flow in the larger airways (nose, mouth, glottis, and bronchi) is turbulent ØGas flow in the smaller airway is laminar ØBreath sounds heard with a stethoscope reflect the turbulent airflow ØLaminar flow is silent 26
3. Gas Flow Resistance • Elastic Resistance • Inelastic Resistance 27
Elastic Resistance ØCaused by Øthe elastic tissue of the lung and the thoracic wall Ø surface tension of the fluid that lines the inside wall of the alveoli Ø The elastic resistance caused by surface tension Øare much more complex. Øaccounts for about two thirds of the total elastic 28 resistance

Inelastic Resistance Ø comprises 1. airway resistance (friction) 2. pulmonary tissue resistance (viscosity, and inertia). Ø the airway resistance account for 80%-90% of the inelastic resistance Ø the more important both in health and disease. 29
Airway Resistance • Airway resistance is the resistance to flow of air in the airways • due to : 1) internal friction between gas molecules 2)2) friction between gas molecules and the walls of the airways 30
Factors that influence airway resistance • Airway diameter • asthma (哮喘)and parasympathetic stimulation: Narrowing airways. • Emphysema (肺气肿): decreases small airway diameter during forced expiration • Turbulence air flow • Rapid breathing: • Density and viscosity of the inspired gas 31
Control of Airway Smooth Muscle • Neural control – Adrenergic beta receptors causing dilatation – Parasympathetic-muscarinic receptors causing constriction – NANC nerves (non-adrenergic, non-cholinergic) • Inhibitory release VIP and NO bronchodilitation • Stimulatory bronchoconstriction, mucous secretion, vascular hyperpermeability, cough, vasodilation 32 “neurogenic inflammation”
Control of Airway Smooth Muscle • Local factors – histamine binds to H 1 receptors-constriction – histamine binds to H 2 receptors-dilation – slow reactive substance of anaphylaxis (过敏反应) - constriction-allergic response to pollen – Prostaglandins (前列腺速) E series - dilation – Prostaglandins (前列腺素)F series constriction 33
Control of Airway Smooth Muscle (cont) • Environmental pollution – smoke, dust, sulfur dioxide, some acidic elements in smog • Elicit constriction of airways – mediated by: • parasympathetic reflex • local constrictor responses 34

4. Measurement of Expiratory Flow - FVC 35
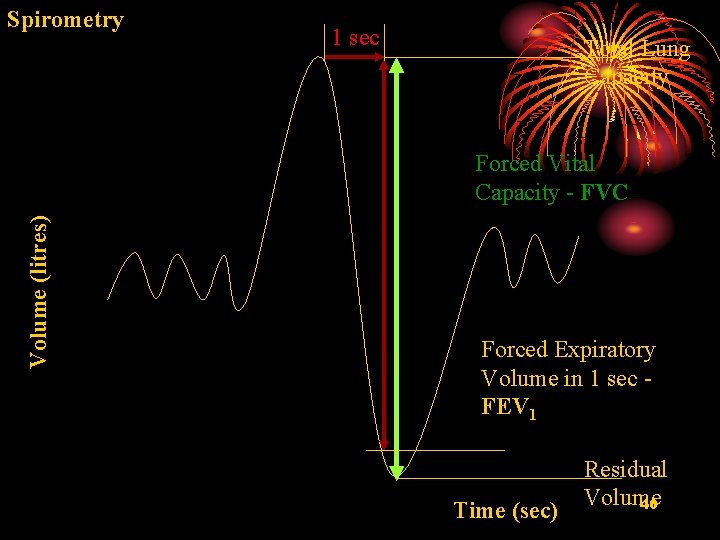
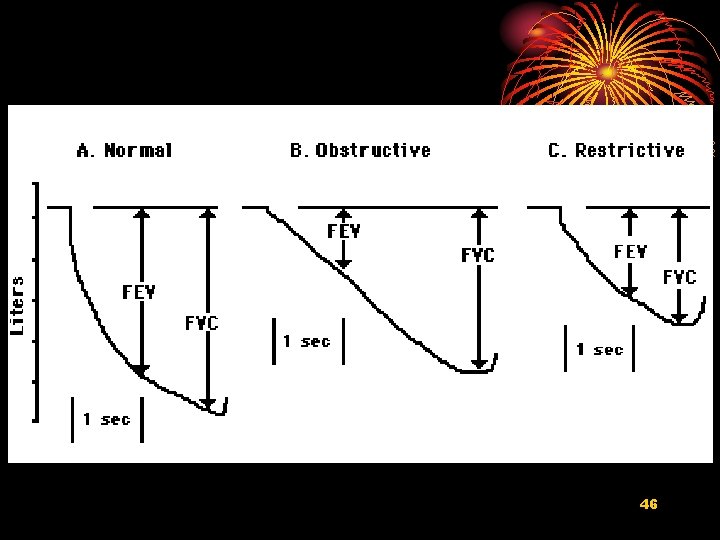
FVC - forced vital capacity • Defines maximum volume of exchangeable air in lung (vital capacity) – forced expiratory breathing maneuver – requires muscular effort and some patient training • Initial (healthy) FVC values approx 4 liters – slowly diminishes with normal aging 36
FVC - forced vital capacity(cont) • Significantly reduced FVC suggests damage to lung tissue – restrictive lung disease (fibrosis,纤维化) – constructive lung disease – loss of functional alveolar tissue • Intra-subject variability factors – age – sex – height – ethnicity 37
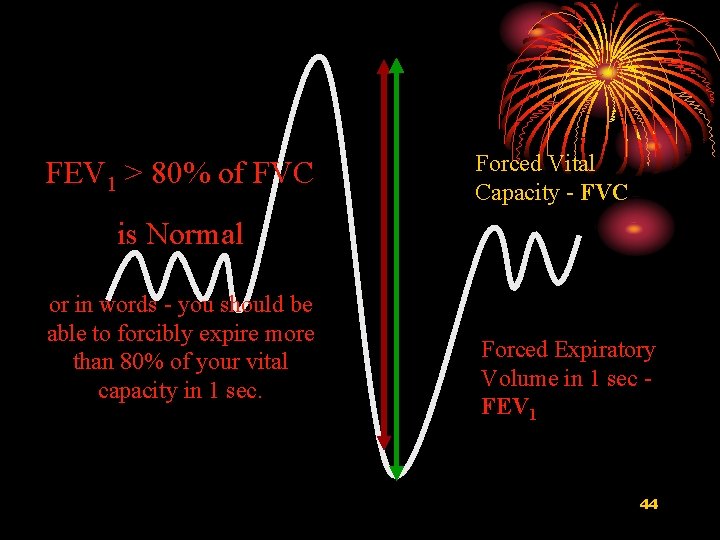
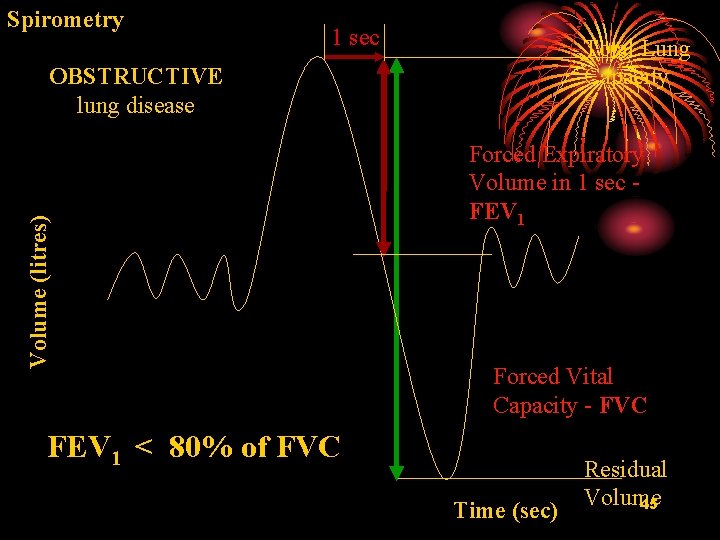
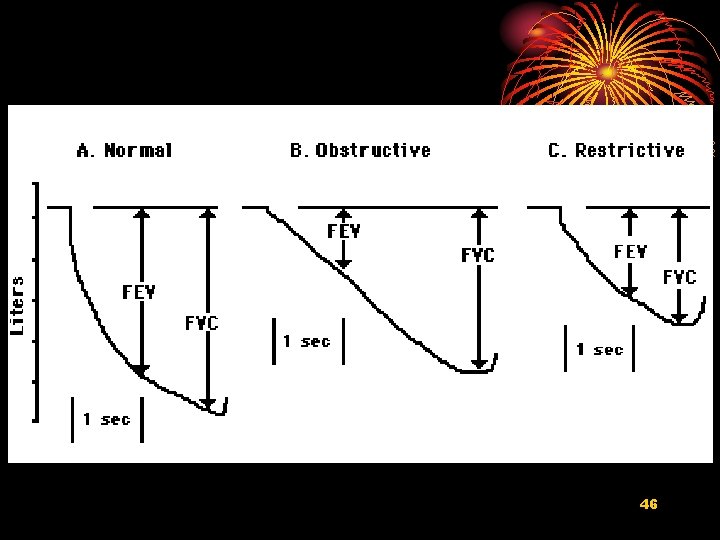
FEV 1 - forced expiratory volume (1 second) • maximum air flow rate out of lung in initial 1 second interval – forced expiratory breathing maneuver – requires muscular effort and some patient training • FEV 1/FVC ratio – normal FEV 1 about 3 liters – FEV 1 needs to be normalized to individual’s vital capacity (FVC) – typical normal FEV 1/FVC ratio = 3 liters/ 4 liters =380. 75
• FEV 1 - forced expiratory volume (1 second) Standard screening measure for obstructive lung disease – FEV 1/FVC reduction trend over time (years) is key indicator – calculate % predicted FEV 1/FVC (age and height normalized) • Reduced FEV 1/FVC suggests obstructive damage to lung airways – episodic, reversible by bronchodilator drugs • probably asthma (哮喘) – continual, irreversible by bronchodilator drugs • probably COPD (chronic obstructive pulmonary 39 disease,慢性阻塞性肺病)
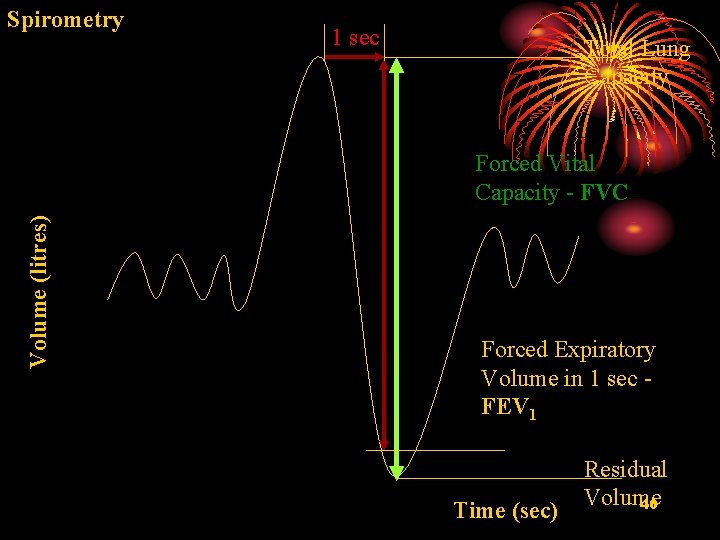
Spirometry 1 sec Total Lung Capacity Volume (litres) Forced Vital Capacity - FVC Forced Expiratory Volume in 1 sec FEV 1 Time (sec) Residual Volume 40
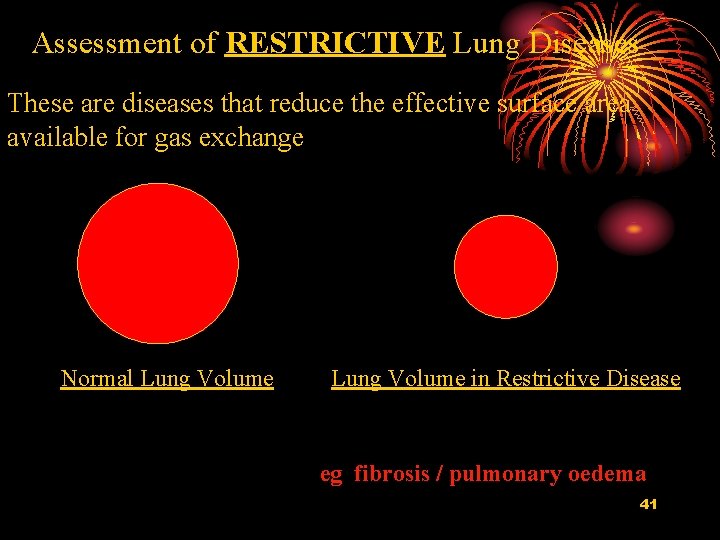
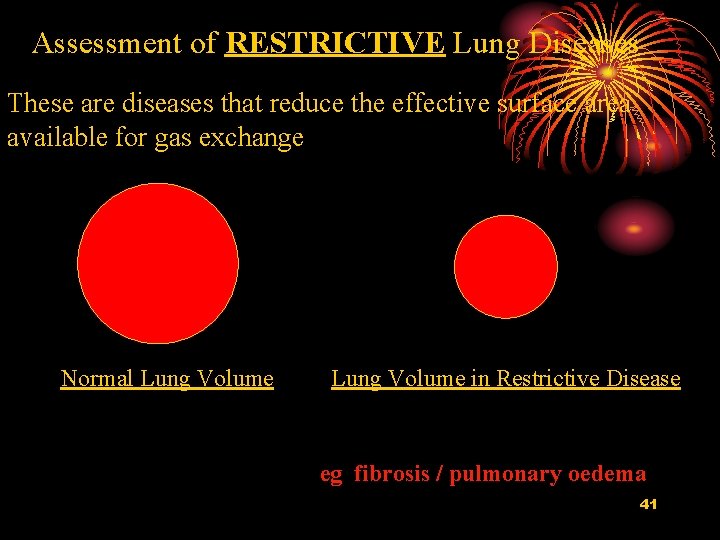
Assessment of RESTRICTIVE Lung Diseases These are diseases that reduce the effective surface area available for gas exchange Normal Lung Volume in Restrictive Disease eg fibrosis / pulmonary oedema 41
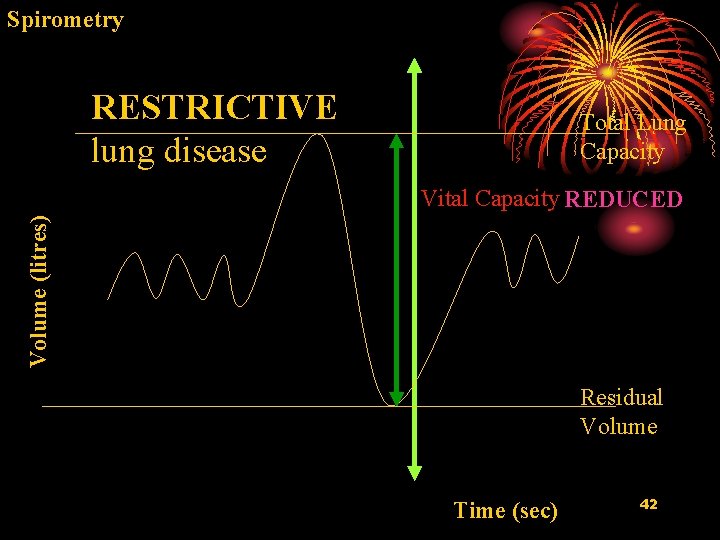
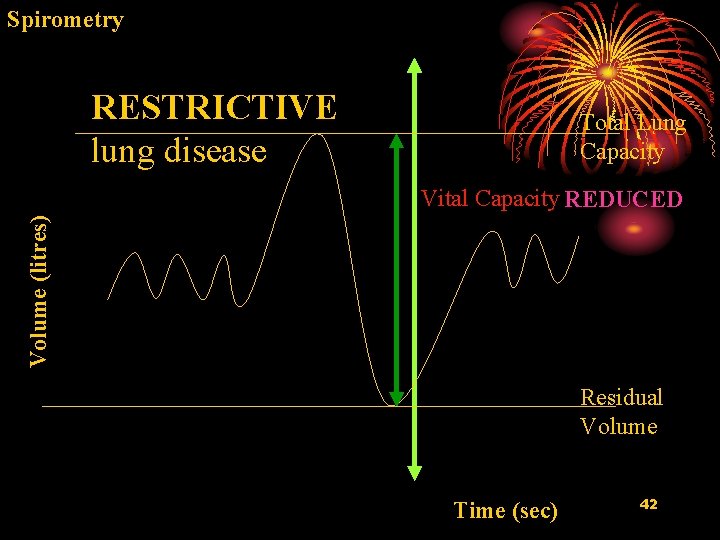
Spirometry RESTRICTIVE lung disease Total Lung Capacity Volume (litres) Vital Capacity REDUCED Residual Volume Time (sec) 42
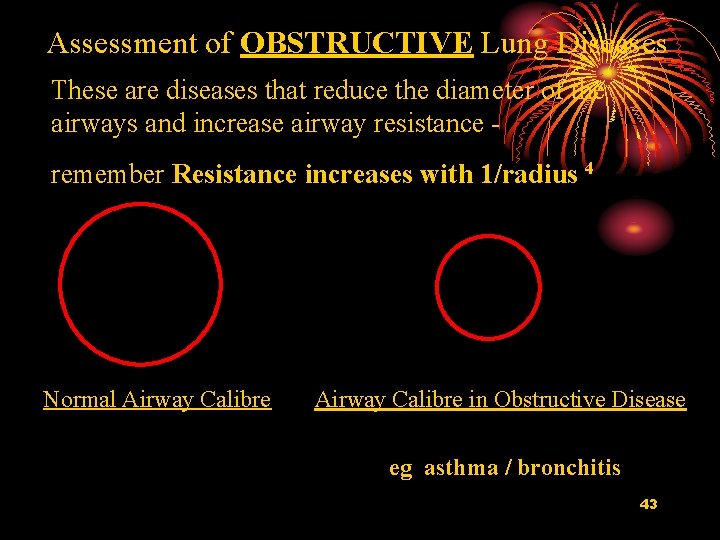
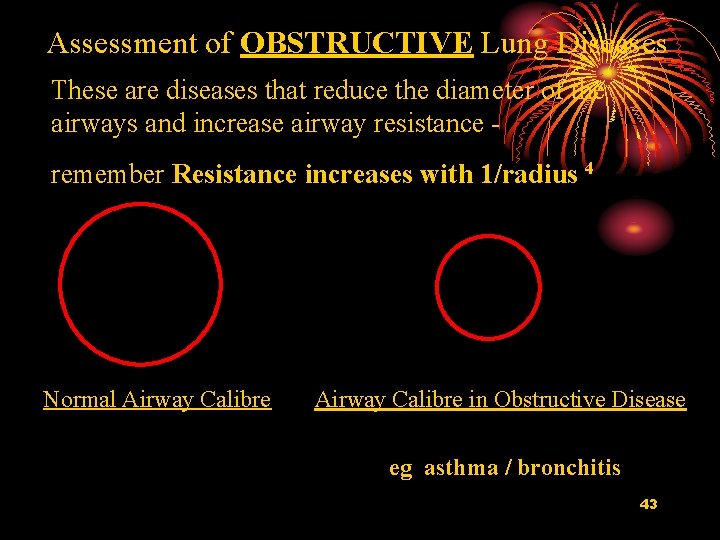
Assessment of OBSTRUCTIVE Lung Diseases These are diseases that reduce the diameter of the airways and increase airway resistance remember Resistance increases with 1/radius 4 Normal Airway Calibre in Obstructive Disease eg asthma / bronchitis 43
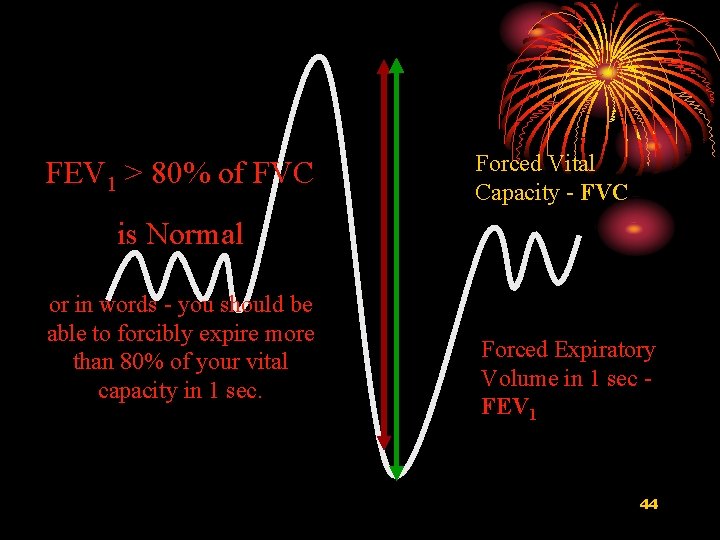
FEV 1 > 80% of FVC Forced Vital Capacity - FVC is Normal or in words - you should be able to forcibly expire more than 80% of your vital capacity in 1 sec. Forced Expiratory Volume in 1 sec FEV 1 44
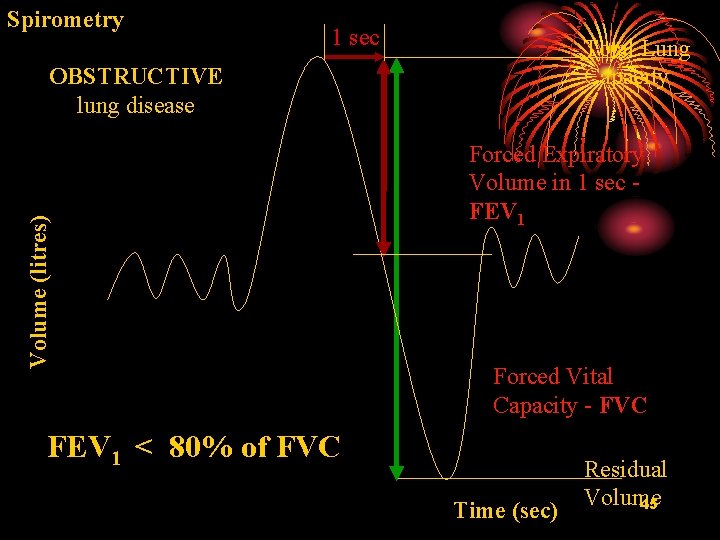
Spirometry 1 sec Total Lung Capacity Volume (litres) OBSTRUCTIVE lung disease Forced Expiratory Volume in 1 sec FEV 1 Forced Vital Capacity - FVC FEV 1 < 80% of FVC Time (sec) Residual Volume 45
46
 Anatomy of the respiratory system
Anatomy of the respiratory system Actual mechanical advantage vs ideal mechanical advantage
Actual mechanical advantage vs ideal mechanical advantage Intensive vs extensive properties
Intensive vs extensive properties Physical properties of ice cube
Physical properties of ice cube Mechanical properties of materials physics
Mechanical properties of materials physics Stress strain curve toughness
Stress strain curve toughness Hardness of nanomaterials
Hardness of nanomaterials Properties of mechanical wave
Properties of mechanical wave Material properties of cardboard
Material properties of cardboard Properties of mechanical waves
Properties of mechanical waves Properties of mechanical waves
Properties of mechanical waves Tensile strength of plastic
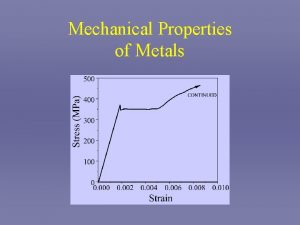
Tensile strength of plastic Mechanical properties of metals ppt
Mechanical properties of metals ppt Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Môn thể thao bắt đầu bằng từ chạy
Môn thể thao bắt đầu bằng từ chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Phép trừ bù
Phép trừ bù Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng xinh xinh thế chỉ nói điều hay thôi
Cái miệng xinh xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V cc
V cc Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Tia chieu sa te
Tia chieu sa te Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot So nguyen to
So nguyen to Tư thế ngồi viết
Tư thế ngồi viết