Sem Physio 22 Mechanical properties of the lung













- Slides: 35
Sem Physio 22 – Mechanical properties of the lung and chest wall: static and dynamic Prof. dr. Željko Dujić

- Chest wall – rib cage, diaphragm, abdominal cavity, anterior abdominal muscles. - Static mechanics – not changing over time. - Lung Capacity – 2 or more volumes. - FRC – resting lung volume. - RV/TLC ratio – normal less than 0. 25, increased in air trapping (COPD) due to increased RV and TLC (RV more) (obstructive pulmonary disease) or in pulmonary fibrosis (restrictive pulmonary disease) due to TLC reduction


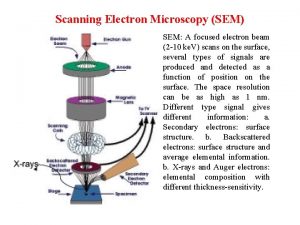
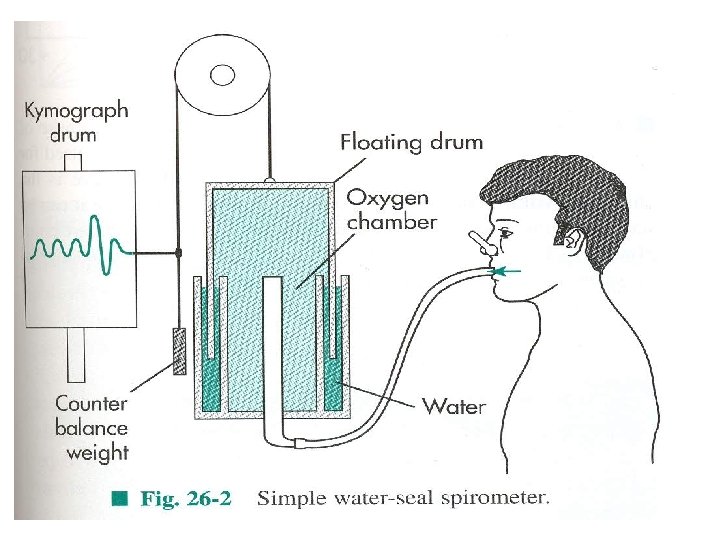
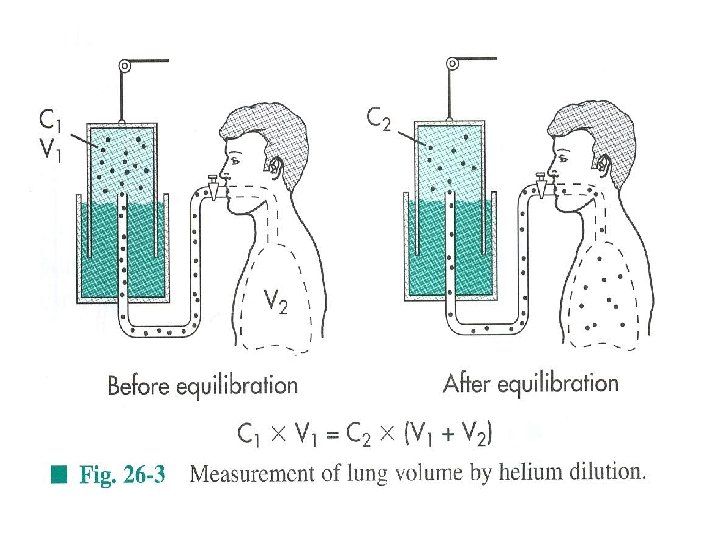
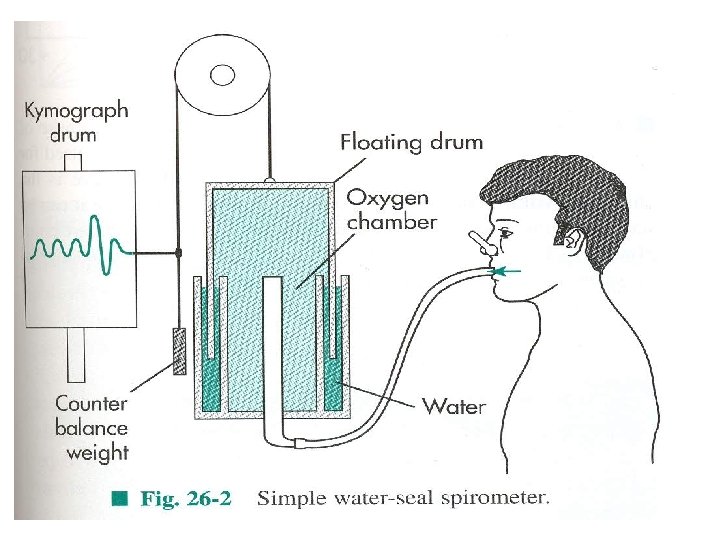
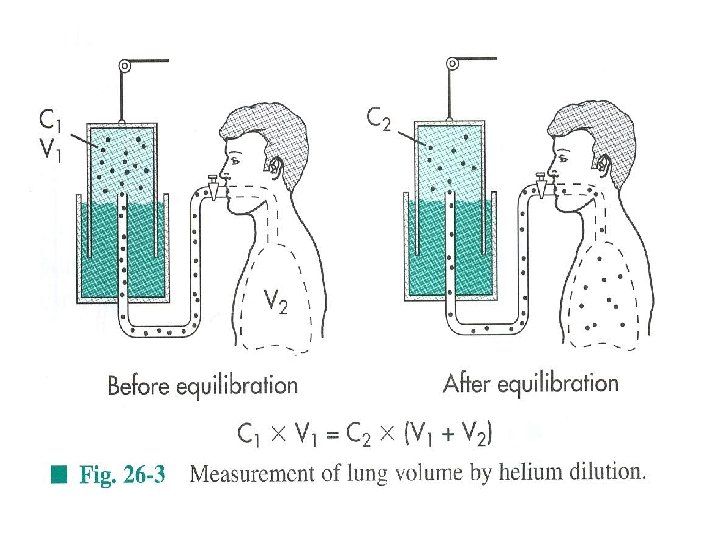
- Measurement of lung volumes – RV and TLC can not be measured with spirometry, but can with helium dilution and body plethysmography. - Helium dilution – the change of concentration of inert gas is proportional to the new volume in which inert gas has been distributed. - Body plethysmography (body box) – the method uses Boyle’s law in which Px. V=contant. The subject makes panting (shallow inspirations and expirations) against closed mouth piece.
- During expiratory phase the gas in the lung is compressed, with resulting expanding volume in the box leading to P reduction. - In healthy subject FRC measured by helium and body plethy. is the same, however in subject with trapped air, FRC by body plethy. is larger since it measures total lung volume at the end of normal expiration.

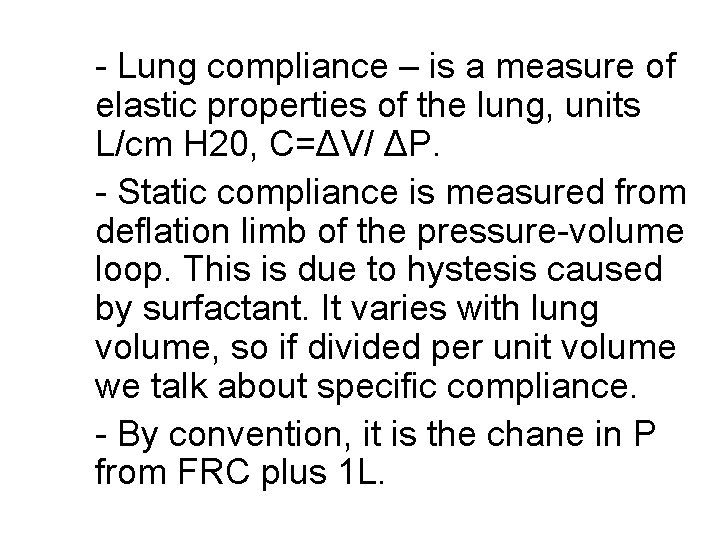
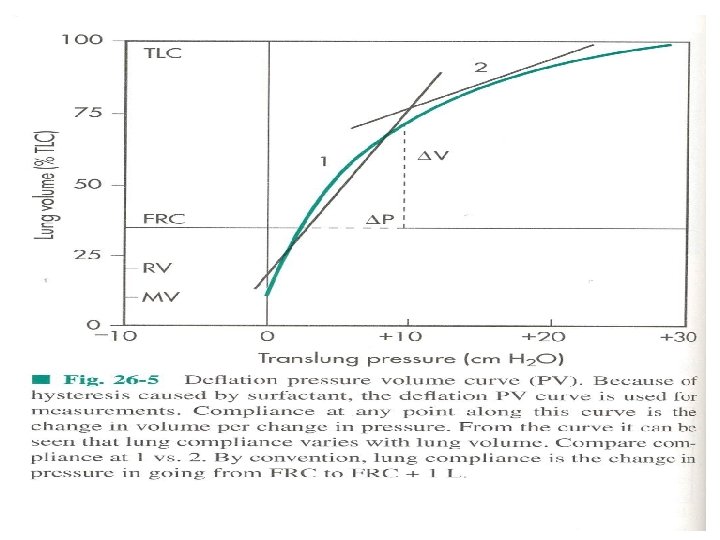
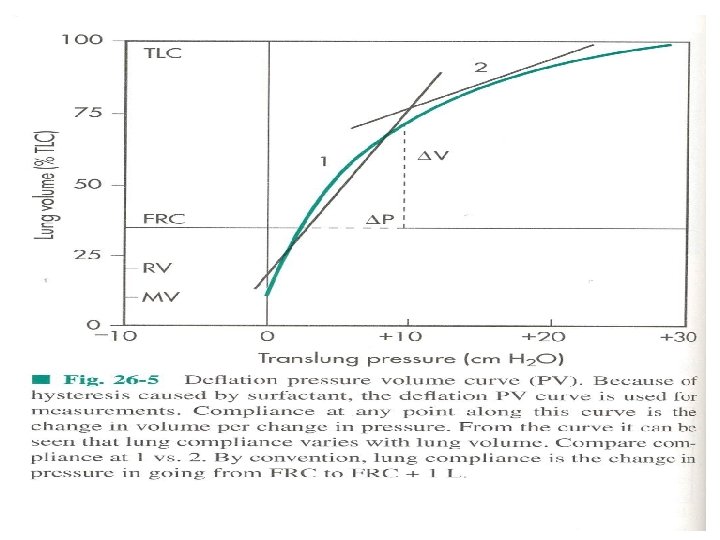
- Lung compliance – is a measure of elastic properties of the lung, units L/cm H 20, C=ΔV/ ΔP. - Static compliance is measured from deflation limb of the pressure-volume loop. This is due to hystesis caused by surfactant. It varies with lung volume, so if divided per unit volume we talk about specific compliance. - By convention, it is the chane in P from FRC plus 1 L.

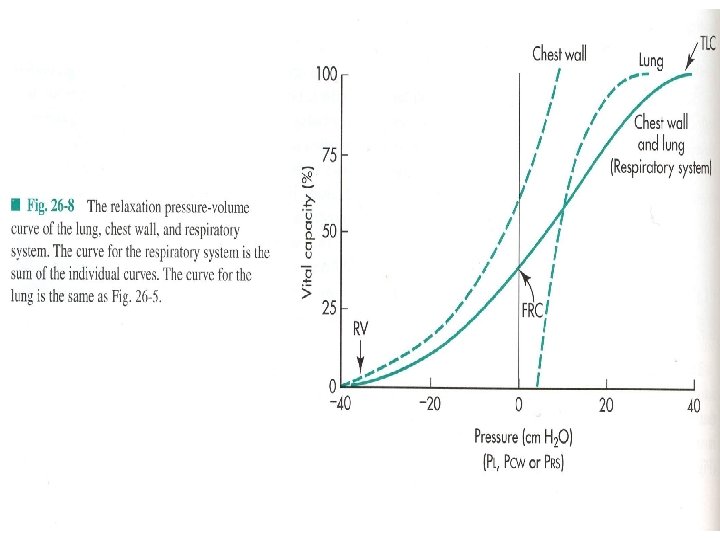
- Lung compliance – is measured with esophageal balloon (Ppl, pleural P), when the lung is not moving (no flow) Ppl is negative (subatmospheric). - Lung-chest interactions – Transmural P (across X), transpulmonary PL=PA-Ppl, the lung requires positive PL to increase volume. - Pw (transmural P across chest wall)=Ppl-Pb (barometric) - Prs (respiratory system)=PL+Pw=PA-Pb - Prs is 0 at FRC, at TLC both the lung and chest wall P are positive, both need transmural distending P.
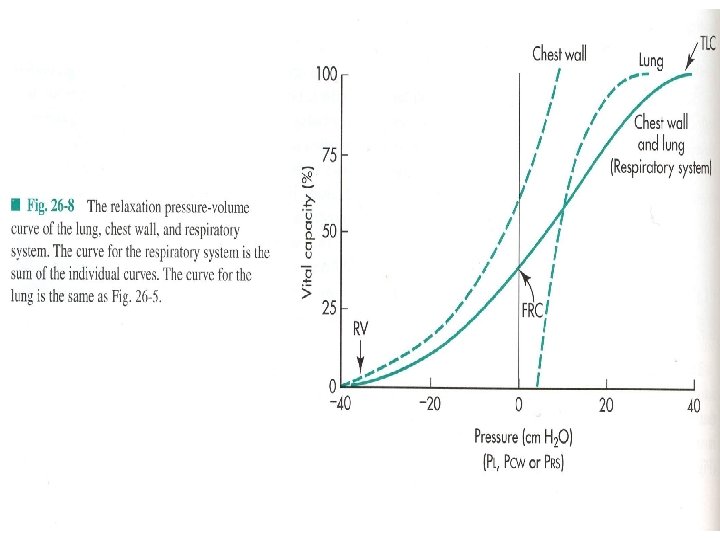
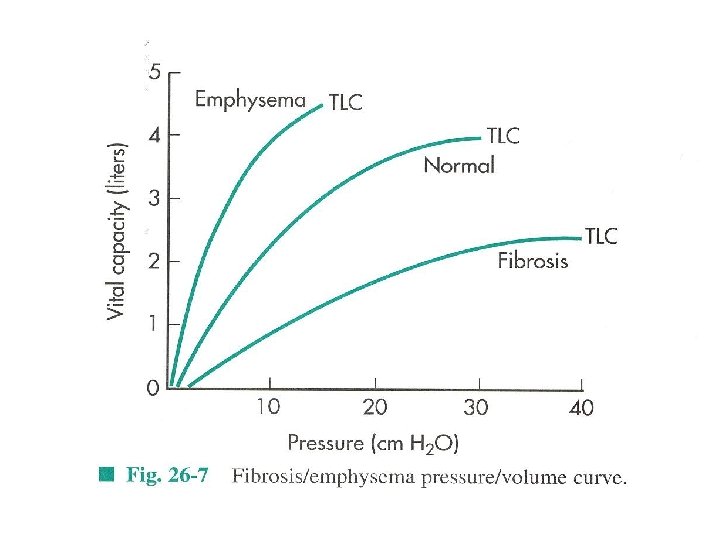
- Resting volume of the chest wall is 60% of TLC, of the lung is 10% TLC. That is above 60% TLC both elastic recoil P reduce lung size. - PL flattens at pressures above 20 cm H 20 because we have reached elastic limits of the lungs (conective tissue limitation, collagen, elastin). - PA is the sum of Ppl and Pelastic recoil pressure of the lung (tends to collapse the lung).

- VE=VTxf (6 L of air=500 m. Lx 12 breaths pm) - PA is 0 at no flow (any time during respiratory cycle), also for Prs (in the absence of airflow the Prs is 0). - DYNAMIC LUNG MECHANICS - Dynamic compliance – a dynamic CL ia calculated as a slope of the line that joints end-inspiratory and endexpiratory points of no flow. - Hysteresis of CL loop is related to lung volume dependent changes in surface tension. - Dyn CL is always less than sta at rest, but is increases during exercise (with larger Vt and P changes, more surfactant molecules are incorporated into air-liquid interface (sighing and yawning are normal physiological means to normalize surface layer). - Dyn and sta Cw are the same.


- Airflow in airways – laminar and turbulent flow - Fully developed laminar flow – the gas in the center of the tube moves twice as fast as the average velocity. - Poiseuille’s law V(flow)= Pπr 4/8ηl, R= 8ηl/πr 4. So R is determined by r. - In turbulent flow gas moves both parallel and perpendicular to the axis of the tube. Overal gas velocity is blunted, because of consumption of energy in creating eddies and chaotic movement. - Re=2 rvd/η, where d is fuid density, v average velocity, r radius, η viscosity.
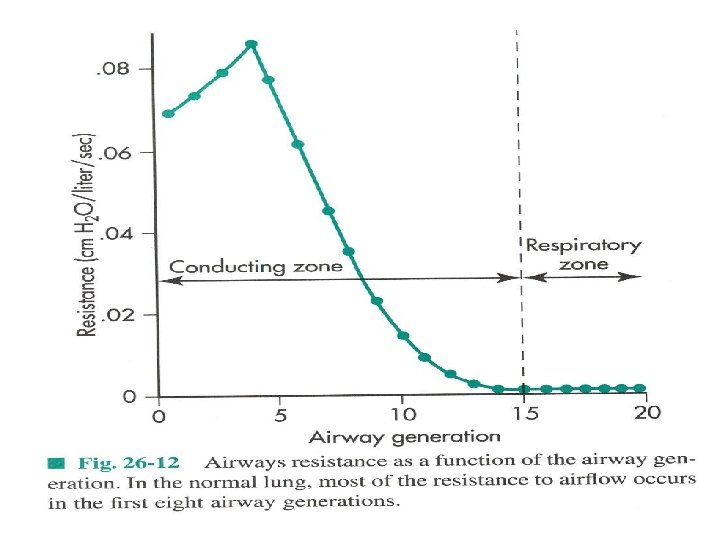
- Turbulent flow is normally present in trachea, large flow, low cross sectional area (CSA), bifurcations, can be heart with auscultation, it is also formed by glottis and vocal cords (irregular structures). - In smaller airways airflow is laminar, can not be heart (silent), we head small airways with mucus secretion or inflammation. - Lung resistance – large (>2 mm), medium (~2 mm, subsegmental bronchi) and small (<2 mm, bronchioles) airways. - The major R are large airways (small CSA, high flow) (80% at normal breathing), small not important (high CSA and paraller arrangement)
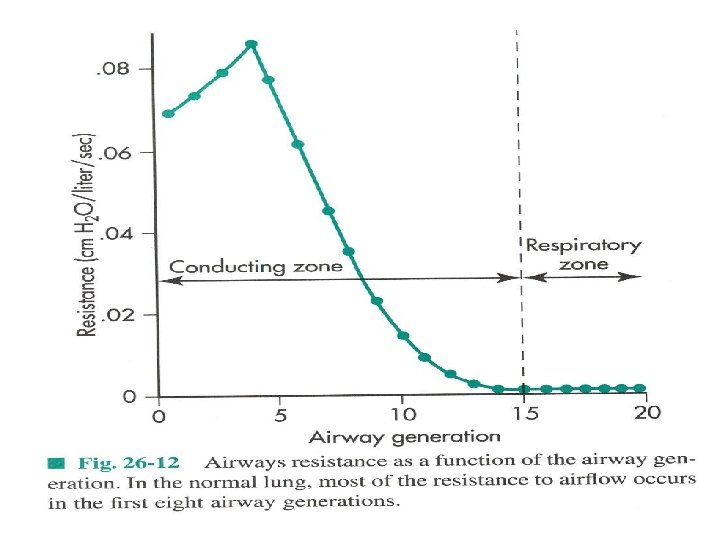
- Factors that contribute to resistance – lung volume, R reduces with increasing LV. If conductance (reciprocal of resitance) is plotted against lung volume the relationship is linear. <othet factors are airway mucus, edema, contraction of bronchial smooth muscle, all decrease the caliber of airways. - Less dense O 2 -helium gas mixture easier breathed during SCUBA or status asthmaticus. - Measured with body box or with esophageal balloon. -R=ΔP/V(flow), normal value 1 -3 cm. H 20/L/sec


- Neurohumoral factors and airways – PNS causes bronchocontriction, SNS bronchdilatation, NANC both. - Agents such as histamine, ACH, thromboxane A 2, prostaglandin F 2, leukotrines (LT B 4, C 4, D 4) are released by various resident and recruited airway cells. - Metacholine provocation and spirometry, hypersensitivity.

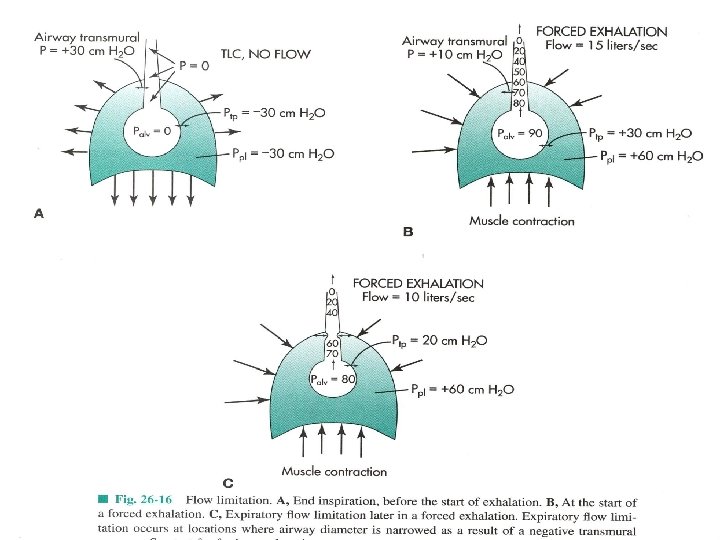
- Three major forces for the maximal inspiratory flow: inspiratory muscles force, static recoil of the lung, reduction of airway resitance with increased LV. Maximal inspiratory flow at the middle between TLC and RV. - Expiratory flow limitation and Equal Pressure Point. This occurs in distensible, collapsable airways, without cartilage. - Two reasons for decreasing transmural pressure during expiration: expiratory airflow resistance and CSA decreases with increasing gas velocity and loss of lateral pressure. - After EPP is achieved no amount of effort will increase the flow further.

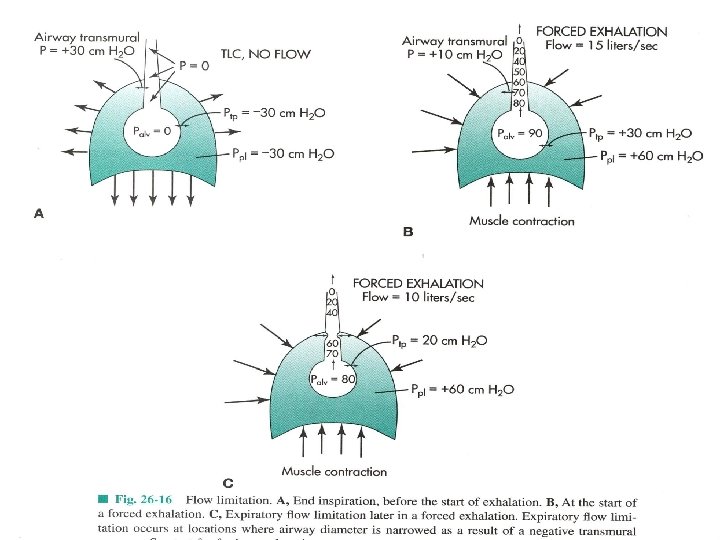
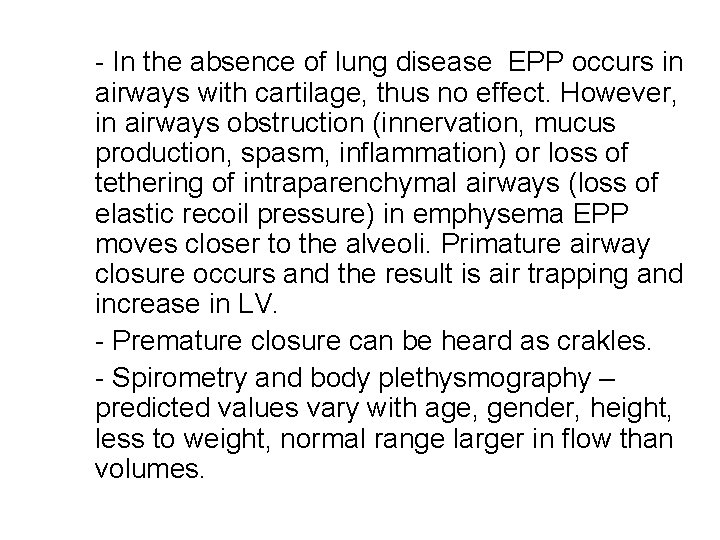
- In the absence of lung disease EPP occurs in airways with cartilage, thus no effect. However, in airways obstruction (innervation, mucus production, spasm, inflammation) or loss of tethering of intraparenchymal airways (loss of elastic recoil pressure) in emphysema EPP moves closer to the alveoli. Primature airway closure occurs and the result is air trapping and increase in LV. - Premature closure can be heard as crakles. - Spirometry and body plethysmography – predicted values vary with age, gender, height, less to weight, normal range larger in flow than volumes.

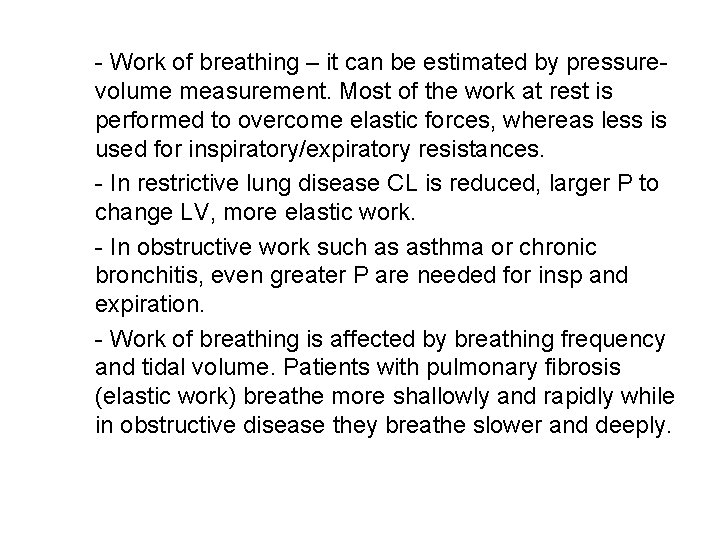
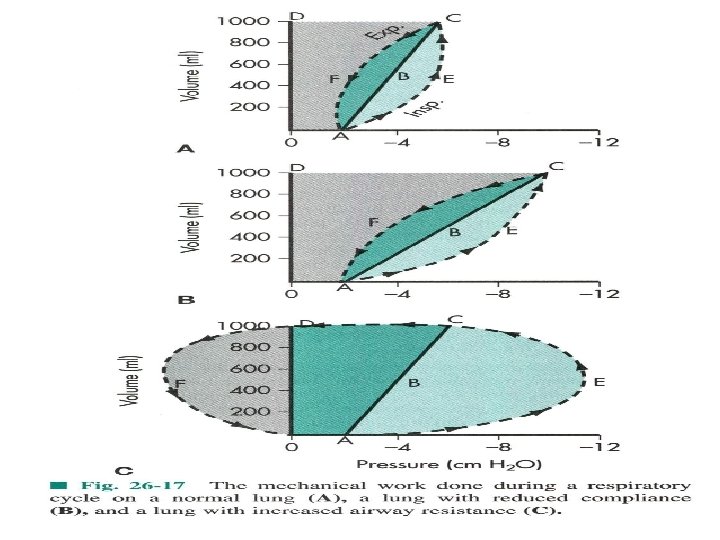
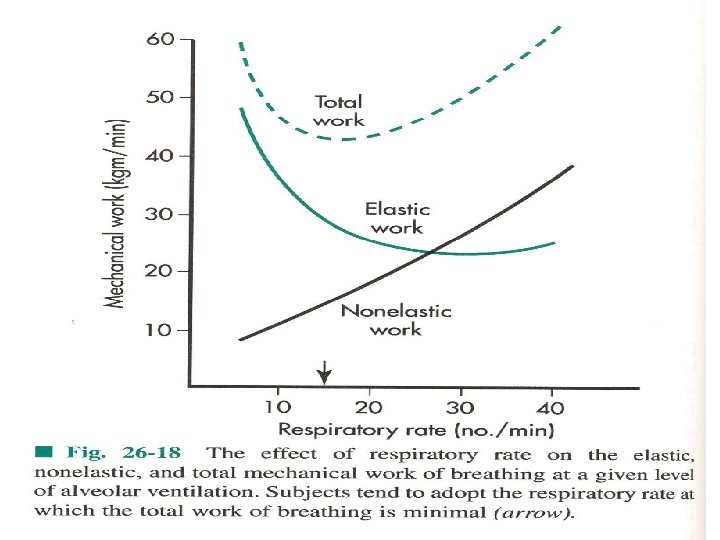
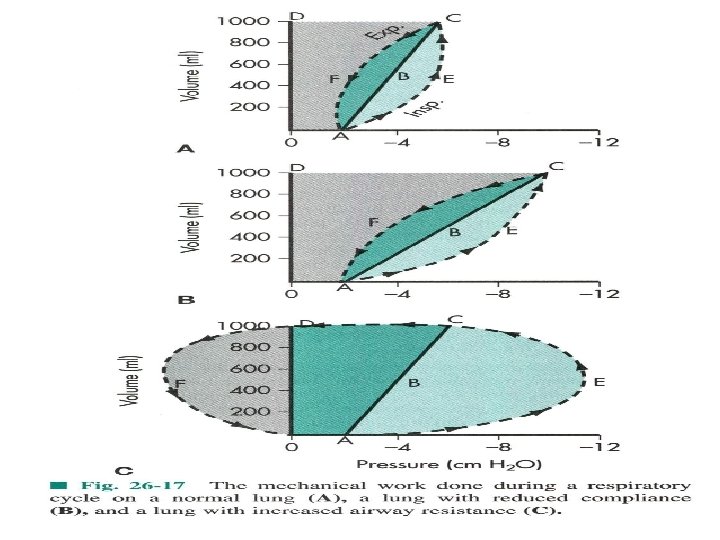
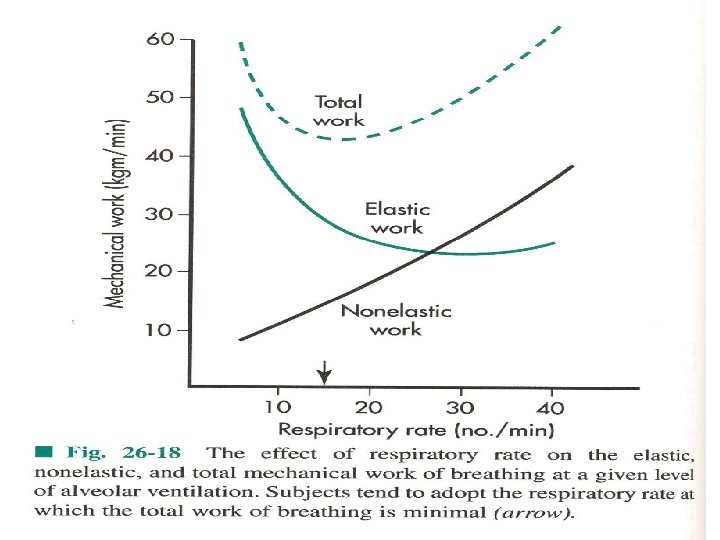
- Work of breathing – it can be estimated by pressurevolume measurement. Most of the work at rest is performed to overcome elastic forces, whereas less is used for inspiratory/expiratory resistances. - In restrictive lung disease CL is reduced, larger P to change LV, more elastic work. - In obstructive work such as asthma or chronic bronchitis, even greater P are needed for insp and expiration. - Work of breathing is affected by breathing frequency and tidal volume. Patients with pulmonary fibrosis (elastic work) breathe more shallowly and rapidly while in obstructive disease they breathe slower and deeply.
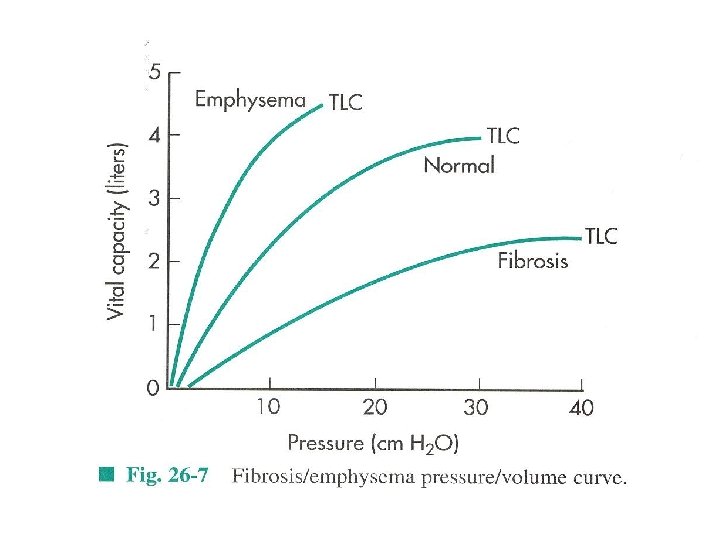
- In emphysema the alveolar and capillary wals are progresively destroyed, increased CL, less tethering causes EPP to move towards alveoli, air trapping and increases in RV, TLC and FRC, Raw is also increased. - In chronic bronchitis EPP also moves closer to alveoli due to inflammation, increases in RV, FRC, TLC, CL normal. - In restrictive pulmonary diseases CL is reduced, flows are not affected, FVC and FEV 1 reduced. - In pregnancy enlarged uterus increases intrabdominal P and reduces dia movement, FRC is decreased, increased Raw.
 Sem sem sem
Sem sem sem Releia voltou a criar histórias agora sem culpa e sem medo
Releia voltou a criar histórias agora sem culpa e sem medo Atividades sobre intertextualidade 6 ano com gabarito
Atividades sobre intertextualidade 6 ano com gabarito Linda constanzo
Linda constanzo Elements of aesthetics
Elements of aesthetics Chris perkins physio
Chris perkins physio Physio rehab centre
Physio rehab centre Physio pleasure
Physio pleasure Marlina mansour
Marlina mansour Physio direct huntingdon
Physio direct huntingdon Signalplant
Signalplant Sim physio
Sim physio Jane ann meehan physio
Jane ann meehan physio Triangle.physiotherapy
Triangle.physiotherapy Caroline white physio
Caroline white physio Varilux physio 360
Varilux physio 360 Actual mechanical advantage vs ideal mechanical advantage
Actual mechanical advantage vs ideal mechanical advantage Crostalline
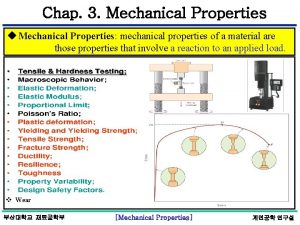
Crostalline Mechanical properties of materials physics
Mechanical properties of materials physics Chemical properties of cardboard
Chemical properties of cardboard What is size-independent measure of load
What is size-independent measure of load Elastic modulus dental materials
Elastic modulus dental materials Properties of mechanical waves
Properties of mechanical waves Hardness of nanomaterials
Hardness of nanomaterials Properties of mechanical waves
Properties of mechanical waves Property of mechanical waves
Property of mechanical waves Intensive vs extensive properties
Intensive vs extensive properties Chemical property of water
Chemical property of water Chúa yêu trần thế
Chúa yêu trần thế Hươu thường đẻ mỗi lứa mấy con
Hươu thường đẻ mỗi lứa mấy con đại từ thay thế
đại từ thay thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay