Nursing Care of the Family During Pregnancy Chapter





- Slides: 62
Nursing Care of the Family During Pregnancy Chapter 14
Learning Objectives Describe strategies for confirming pregnancy and estimating the date of birth. Summarize the physical, psychosocial, and behavioral changes that usually occur as the expectant mother and other family members adapt to pregnancy. Evaluate the benefits of prenatal care and problems of accessibility for some women. Outline the patterns of health care used to assess maternal and fetal health status at initial and follow-up visits during pregnancy.
Learning Objectives (Cont. ) Select the typical nursing assessments, diagnoses, interventions, and methods of evaluation in providing care for the pregnant woman. Plan education needed by pregnant women to understand manage physical discomforts related to pregnancy and to recognize signs and symptoms of potential complications. Evaluate the effect of culture, age, parity, and number of fetuses on the response of the family to the pregnancy and on the prenatal care provided. Compare the options for health care providers and birth setting choices that are available.
Nursing Care during Pregnancy Prenatal period Period of physical and psychologic preparation for birth and parenthood Opportunity for nurses and members of health care team to influence family health Healthy Health women seek care and guidance promotion interventions can affect well-being of woman, child, and rest of family
Nursing Care during Pregnancy Spans 9 months 10 lunar months of 28 days (280 days total) Trimesters First: weeks 1 through 13 Second: weeks 14 through 26 Third: weeks 27 through 40
Diagnosis of Pregnancy Signs and symptoms Presumptive Missed Home indicators menstrual period pregnancy test positive Amenorrhea, nausea, vomiting, breast tenderness, urinary frequency, fatigue (morning sickness) Quickening (perception of fetal movement)
Diagnosis of Pregnancy Signs and symptoms (cont’d) Probable indicators Uterine enlargement Braxton Hicks contractions Uterine souffle Ballotement Positive pregnancy test
Diagnosis of Pregnancy Signs and symptoms (cont’d) Positive indicators Presence Fetal of fetal heartbeat distinct from mother’s movement felt by someone other than mother Visualization (e. g. , ultrasound examination)
Estimating Date of Birth Estimated date of birth (EDB) Older terms Estimated date of delivery (EDD) Estimated date of confinement (EDC) Ultrasound Standard procedure for determining the gestational age of the fetus Naegele’s rule to calculate EDB Assumes that the woman has a 28 -day cycle and that fertilization occurs on the 14 th day After determining the first day of the LMP, subtract 3 calendar months and add 7 days
Adaptation to Pregnancy Maternal adaptation Accepting the pregnancy Identifying with the mother role Reordering personal relationships Establishing relationship with fetus: attachment process of the mother Phase 1: She accepts the biologic fact of pregnancy Phase 2: She accepts the growing fetus as distinct from herself Phase 3: She prepares realistically for the birth and parenting of the child Preparing for childbirth

Adaptation to Pregnancy (Cont. ) Paternal adaptation Accepting the pregnancy Couvade syndrome Developmental tasks experienced by the expectant father Announcement phase Moratorium phase Focusing phase Identifying with the father role Reordering personal relationships Establishing relationship with the fetus Preparing for birth
Adaptation to Pregnancy (Cont. ) Adaptation to parenthood for the nonpregnant partner Sibling adaptation Depends on age and dependency needs Grandparent adaptation
Sibling Adaptation Sharing the spotlight with a new brother or sister may be the first major crisis for a child Older child often experiences a sense of loss or feels jealous at being “replaced” by the new baby Factors that influence the child’s response are age, the parent’s attitudes, the father’s role, the length of separation from the mother, the hospital’s visitation policy, and how the child has been prepared for the change Mother with other children must devote time and energy to reorganizing her relationship with these children She needs to prepare siblings for the birth of the baby
Grandparent Adaptation Expectant grandparenthood can represent a maturational milestone for the parent of an expectant parent Grandparents describe having a grandchild as the best thing that ever happen to them Grandparents, when the mother is a young adolescent or for other reasons such as substance-abusing mother; the grandchild may mean assuming care and raising another child when they thought childrearing was over Grandparent is the historian who transmits the family history Role model and support person
Care Management Purpose of prenatal care is to identify existing risk factors and other deviations from normal Emphasis on preventive care and optimal self-care Prenatal care is sought routinely by women of middle or high socioeconomic status
Care Management Women in poverty or lacking health insurance may not have access to public or private care Lack of culturally sensitive care and communication interferes with access to care Immigrant women may not seek prenatal care Birth outcomes are less positive, with higher rates of maternal and newborn complications Problems with LBW and infant mortality associated with inadequate prenatal care
Care Management Barriers to obtaining prenatal care include: Inadequate numbers of providers Unpleasant facilities or procedures Inconvenient clinic hours Distance to facilities Lack of transportation Fragmentation of services Inadequate finances Personal and cultural attitudes
Care Management Effectiveness of home visiting by nurses during pregnancy has been validated Current model of prenatal care used for more than a century Model is being questioned, and tendency to fewer visits with women at low risk for complications
Care Management Initial visit Prenatal interview Reason for seeking care Current pregnancy Childbearing Health and female reproductive history Nutritional history History of drug and herbal preparation use Family history Social, experiential, occupational history
Schedule of Prenatal Visits 1 X a month until 28 th week Every 2 weeks until 36 th week Weekly from 37 th until delivery
Lab Tests PPD Hepatitis B Cervical cytology and screening for infection - Chlamydia gonorrhea RPR/VDRL – HIV recommended CBC, Blood type and Rh-factor, antibody screen. Tests for sickle cell, Folacin levels, Rubella
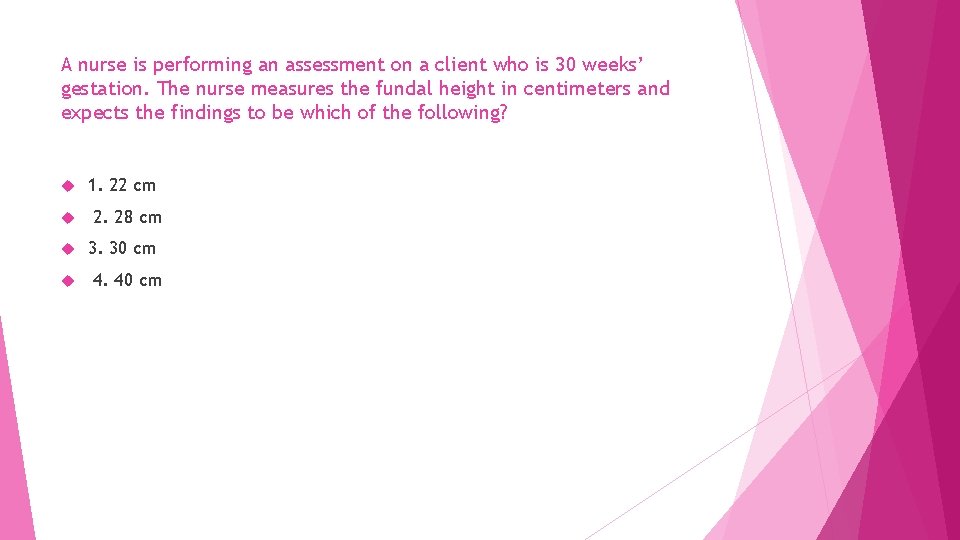
Fundal Height Measurement of the height of the uterus above the symphysis pubis, is used as one indicator of fetal growth Measurement also provides a gross estimate of the duration of pregnancy Second and third trimester (weeks 18 to 30) the height of the in centimeters is approximately the same as the number of weeks gestation Measurement of fundal height may aid in the identification of high risk factors Stable or decreased fundal height may indicate the presence of IUGR Excessive increase could indicate the presence of multifetal, gestation, or hydramnios

Care Management Assessment (cont’d) Follow-up visits Interview Physical examination Fetal assessment Fundal height Gestational age Health status
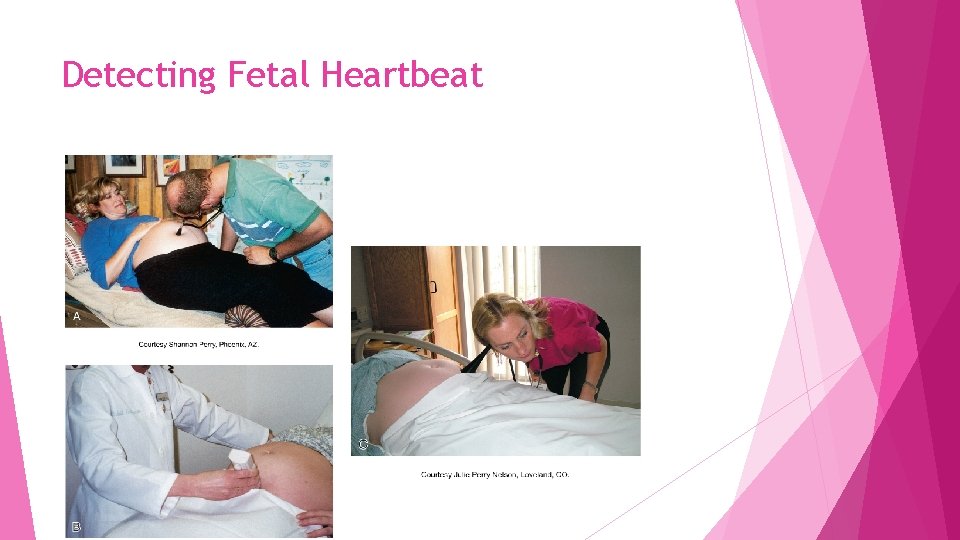
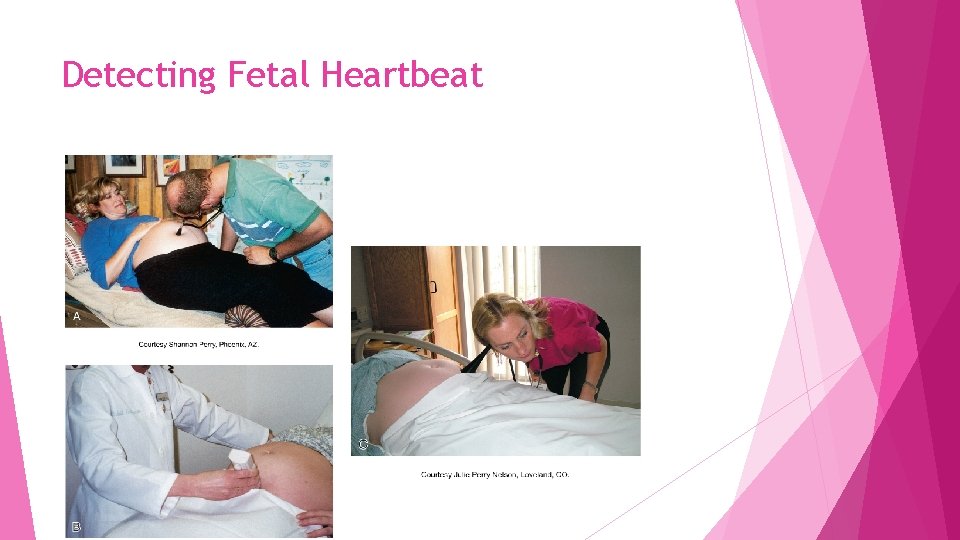
Detecting Fetal Heartbeat
Gestational Age Determined from the menstrual history, contraceptive history, and pregnancy results Findings obtained from the clinical evaluation: First uterine size estimate, date and size Fetal heart rate first heard: date, method (Doppler, stethoscope, fetoscope) Date of quickening
Gestational Age Current fundal height, estimated fetal weight (EFW) Current week of gestation by history of LMP or ultrasound examination (or both) Ultrasound examination: date, week of gestation, biparietal diameter (BPD) Reliability of dates
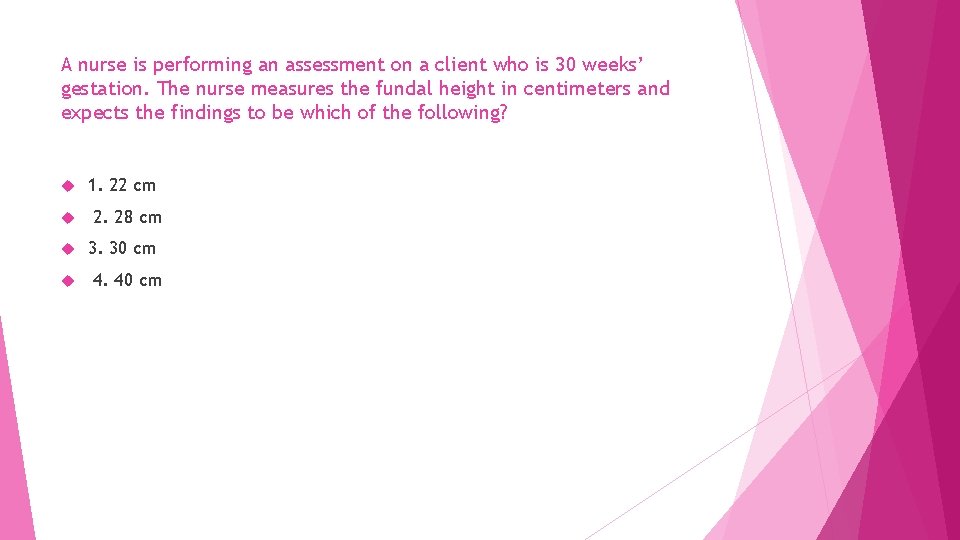
A nurse is performing an assessment on a client who is 30 weeks’ gestation. The nurse measures the fundal height in centimeters and expects the findings to be which of the following? 1. 22 cm 2. 28 cm 3. 30 cm 4. 40 cm
Care Management Assessment Follow-up visits (cont’d) Fetal assessment Laboratory tests Multiple-marker Other or triple-screen blood tests (RPR/VDRL, CBC, anti-Rh) tests Ultrasonography Amniocentesis
Care Management Plan of care and implementation Care paths Education for self-care Nutrition Personal hygiene Prevention Kegel of urinary tract infections exercises Preparation Dental for breastfeeding newborn health
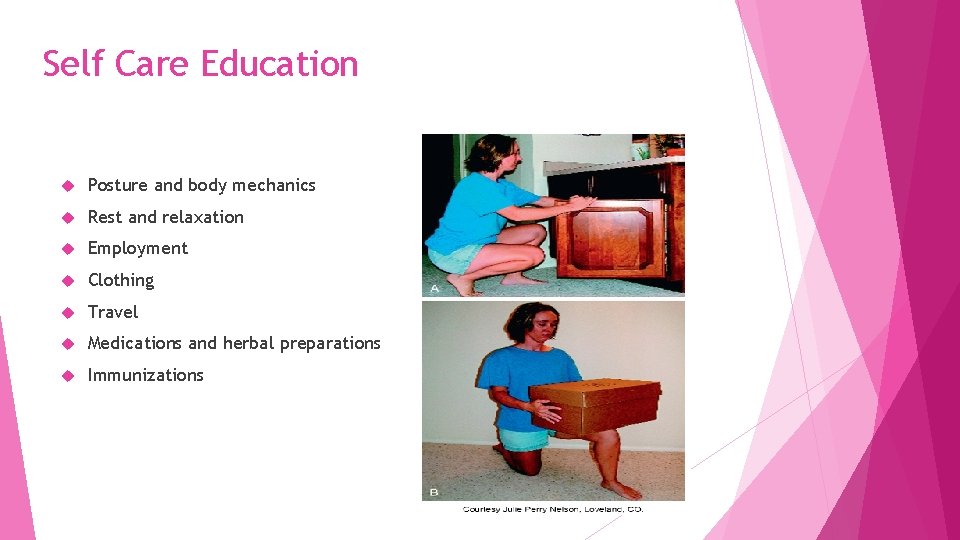
Self Care Education Nutrition Personal hygiene Prevention of Urinary tract Infections Kegal exercises Dental Care Posture and body mechanics Exercise Rest and relaxation
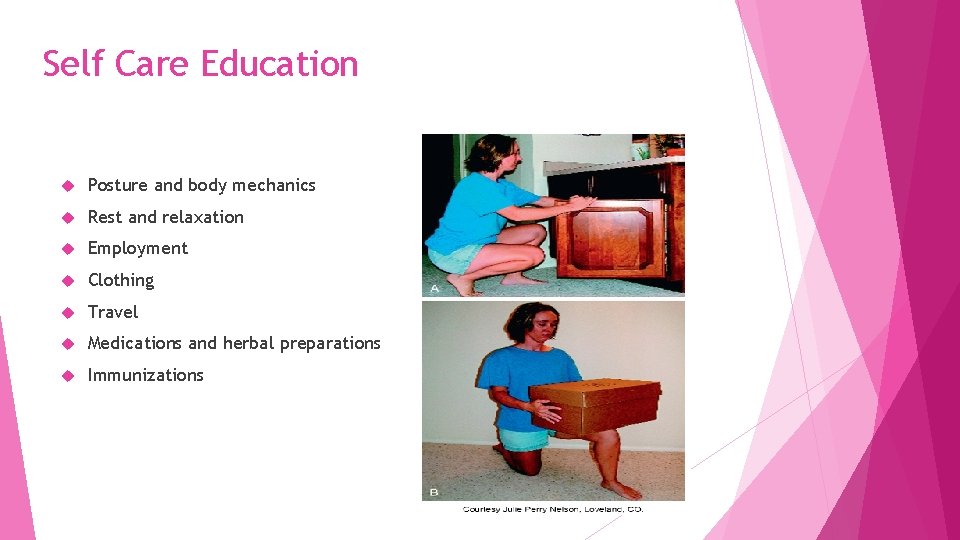
Self Care Education Posture and body mechanics Rest and relaxation Employment Clothing Travel Medications and herbal preparations Immunizations

Danger Signs in Pregnancy Vaginal Bleeding or drainage Abdominal Pain Headache/Blurred vision Edema of hands or face Excessive Nausea and vomiting Excessive weight gain Excessive or Decreased fetal activity
Rest, recreation and Sleep Napping for 30 min in am and pm. Beneficial
Breast Care Colostrum secreted early in pregnancy Bathe breasts with clean washcloth and warm water Avoid- Soap. Alcohol and other drying cleansers Breast Support Well-fitted bra cup large enough to cover all breast tissue Large breasts - wide cotton shoulder straps
Bowel Habits Prevent Constipation by Drinking large amounts of fluid Diet containing fresh fruit raw veg, and whole grain breads and bran Citracel Stool or Metamucil add bulk to stool softeners MOM dioctyl sodium sulfosuccinate
Hemorrhoids Prevent If constipation protruding gently push back into rectum Knee chest position Icebag or cold compresses with witch hazel or Epsom salts Sitz bathes Kegel Exercise
Travel Avoid if any hx of vag. Bleeding, PIH, multiple gestations, or last weeks of pregnancy Flying recommended for -Long distances Drink plenty of fluids Automobile Take rest periods every hour Seat belts Lap belt Under abdomen shoulder belt - above the uterus and below the neck

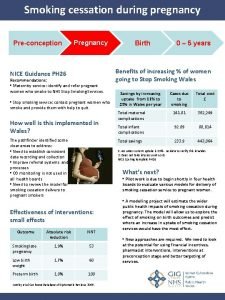
Care Management Plan of care and implementation Care paths Education for self-care (cont’d) Immunizations Alcohol, Normal cigarettes, and other substances discomforts Recognizing Printed potential complications list of signs and symptoms Emergency telephone numbers
Immunizations Tetanus-diphtheria-acellular-pertussis (TDAP)-should be administered between 27 and 36 weeks of pregnancy Recombinant hepatitis B Influenza (inactivated) vaccine-all women who are pregnant during the influenza season (November through March) should be offered the influenza vaccine
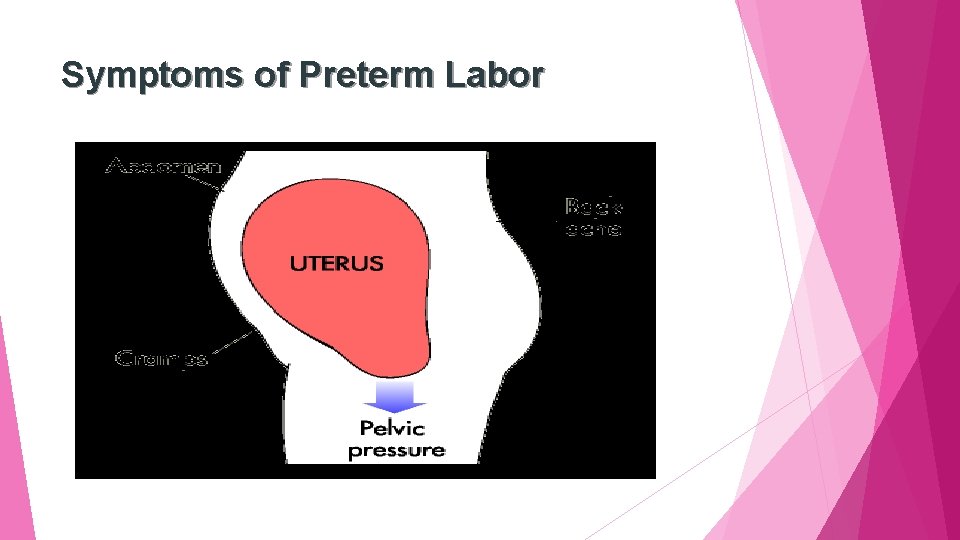
Care Management Assessment Education for self-care (cont’d) Recognizing After preterm labor the 20 th week Before 37 th week of pregnancy Uterine contractions, if untreated, cause cervix to open earlier, with resulting preterm birth
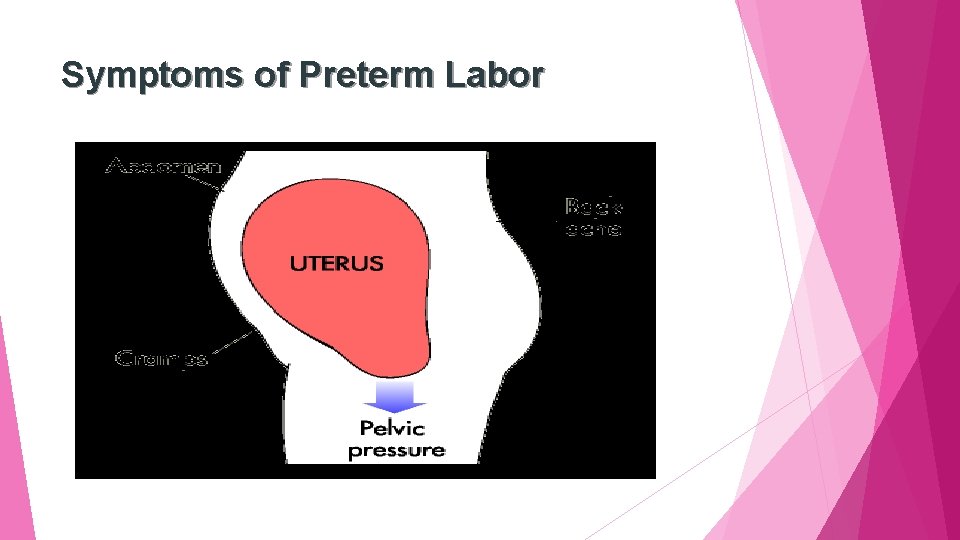
Symptoms of Preterm Labor
Variations in Prenatal Care Cultural influences Emotional response Clothing Physical Sexual Diet activity and rest activity
Variations in Prenatal Care Age Adolescents Much less likely than older women to receive adequate prenatal care Women older than 35 years Multiparous women Nulliparous women
Variations in Prenatal Care Multifetal Twin pregnancy pregnancies often end in prematurity Rupture of membranes before term common Congenital malformations twice as common in monozygotic twins as in singletons No increase in incidence of congenital anomalies in dizygotic twins
Variations in Prenatal Care Multifetal pregnancy (cont’d) Multifetal pregnancy probability increased by: History of dizygous twins in female lineage Use of fertility drugs Rapid uterine growth for weeks of gestation Hydramnios Palpation expected of more small or large parts than
Variations in Prenatal Care Multifetal pregnancy (cont’d) Multifetal pregnancy probability increased by: Asynchronous fetal heartbeats or more than one fetal electrocardiographic tracing Ultrasonographic fetus evidence of more than one
Variations in Prenatal Care Multifetal pregnancy (cont’d) Prenatal care given women with multifetal pregnancies includes changes in: Pattern of care Amount of weight gained Nutritional Uterine intake observed distention cause severe backache
Variations in Prenatal Care Multifetal pregnancy (cont’d) Multiple newborns may place strain on: Finances Space Workload Woman’s and family’s ability to cope Lifestyle changes may be necessary Parents need help in planning for care
Childbirth and Perinatal Education Perinatal education goals Establish lifestyle behaviors for optimal health Prepare psychologically for pregnancy and the responsibilities that come with parenthood Identify, Screen Get minimize, and treat risk factors health hazards in workplace and home genetic counseling for inherited diseases Compare perinatal care options available
Perinatal Education Goal is to help individuals and family members to make informed and safe decisions about pregnancy, birth, infant care, and early parenthood Classes for expectant parents Education programs consist of a menu of class series and activities from preconception through the early months of parenting.

Perinatal Care Choices Physicians Midwives Certified Direct nurse-midwives (CNMs) entry midwives or certified midwives (CMs) Traditional Doulas Birth plans or lay midwives
Birth Setting Choices Hospital Labor, delivery, recovery rooms (LDRs) Labor, delivery, recovery, postpartum rooms (LDRPs) Birth centers Home birth Remains a controversial topic in American health care
Key Points The prenatal period is a preparatory one both physically, in terms of fetal growth and parental adaptations, and psychologically, in terms of anticipation of parenthood. Pregnancy affects parent-child, sibling-child, and grandparent-child relationships. Discomforts and changes of pregnancy can cause anxiety for the woman and her family and require sensitive attention and a plan for teaching selfmanagement measures.
Key Points (Cont. ) Education about safety during activity and exercise is essential, given maternal anatomic and physiologic responses to pregnancy. Important components of the initial prenatal visit include detailed and carefully documented findings from the interview, a comprehensive physical examination, and selected laboratory tests. Follow-up visits are shorter than the initial visit and are important for monitoring the health of the mother and fetus and providing anticipatory guidance as needed.
Key Points (Cont. ) Even in normal pregnancy the nurse must remain alert to hazards such as supine hypotension, signs and symptoms of potential complications, and signs of family maladaptations. Blood pressure is evaluated on the basis of absolute values and length of gestation and is interpreted in light of modifying factors. Each pregnant woman needs to know how to recognize and report signs of potential complications such as preterm labor.
Key Points (Cont. ) There is an increased incidence of physical, mental, and verbal abuse during pregnancy. Culture, age, parity, and multifetal pregnancy can have a significant effect on the course and outcome of the pregnancy. Nurses must ask pregnant women and their families about preferences, practices, and customs related to childbearing to provide culturally sensitive care.
Key Points (Cont. ) Childbirth education teaches tuning in to the body’s inner wisdom and coping strategies that enhance women’s ability to cope effectively with labor and birth. Perinatal education strives to promote healthier pregnancies and family lifestyles. Nurses can help pregnant women and their families to make informed decisions about care providers, birth settings, and labor support.
Question 1. With regard to follow-up visits and the physical examination for women receiving prenatal care, nurses should be aware that : a. The interview portions become more intensive as the visits become more frequent over the course of the pregnancy. b. Monthly visits are scheduled for the first trimester, every 2 weeks for the second trimester, and weekly for the third trimester. c. During the abdominal examination, the nurse should be alert for supine hypotension. d. For pregnant women, a systolic blood pressure (BP) of 130 mm Hg and a diastolic BP of 80 mm Hg is sufficient to be considered hypertensive
 Pictures of spotting during pregnancy
Pictures of spotting during pregnancy 30 / 4
30 / 4 Prenatal care and adaptations to pregnancy
Prenatal care and adaptations to pregnancy Chapter 4 prenatal care and adaptations to pregnancy
Chapter 4 prenatal care and adaptations to pregnancy Bacteria
Bacteria Hormones during pregnancy
Hormones during pregnancy Normal cervical length
Normal cervical length Role of nurse in reproductive health ppt
Role of nurse in reproductive health ppt Components of weight gain during pregnancy
Components of weight gain during pregnancy Sajda during pregnancy
Sajda during pregnancy Feeling like periods in early pregnancy
Feeling like periods in early pregnancy Flovent safe during pregnancy
Flovent safe during pregnancy Family care plan in community health nursing
Family care plan in community health nursing Nursing interventions for obsessive compulsive disorder
Nursing interventions for obsessive compulsive disorder Nursing care plan on cataract
Nursing care plan on cataract Primary care secondary care tertiary care
Primary care secondary care tertiary care Nursing theories related to teenage pregnancy
Nursing theories related to teenage pregnancy Multiple pregnancy nursing diagnosis
Multiple pregnancy nursing diagnosis Chapter 7 nursing management of pain during labor and birth
Chapter 7 nursing management of pain during labor and birth Nursing responsibilities during labor
Nursing responsibilities during labor Chapter 41 rehabilitation and restorative nursing care
Chapter 41 rehabilitation and restorative nursing care Pie documentation nursing
Pie documentation nursing The nursing assistant and the care team chapter 2
The nursing assistant and the care team chapter 2 Chapter 2 the nursing assistant and the care team
Chapter 2 the nursing assistant and the care team Chapter 20 reproduction and pregnancy
Chapter 20 reproduction and pregnancy Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Chapter 5 reproducible master a pregnancy vocabulary
Chapter 5 reproducible master a pregnancy vocabulary The xbox came out before the wii fact or opinion
The xbox came out before the wii fact or opinion Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Tư thế worm breton là gì
Tư thế worm breton là gì Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Môn thể thao bắt đầu bằng chữ f
Môn thể thao bắt đầu bằng chữ f Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính thế năng
Công thức tính thế năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V cc cc
V cc cc Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot Số nguyên tố là số gì
Số nguyên tố là số gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates