Chapter 14 Nursing Management During Labor and Birth
Chapter 14: Nursing Management During Labor and Birth
Nursing Management of Laboring Women • Assessment • Comfort measures • Emotional support • Information and instruction • Advocacy • Support for the partner Copyright © 2017 Wolters Kluwer · All Rights Reserved
Maternal Assessment During Labor and Birth • Maternal status (vital signs, pain, prenatal record review) – Vaginal examination (cervical dilation, effacement, membrane status, fetal descent and presentation) – Rupture of membranes – Uterine contractions – Leopold maneuvers Copyright © 2017 Wolters Kluwer · All Rights Reserved
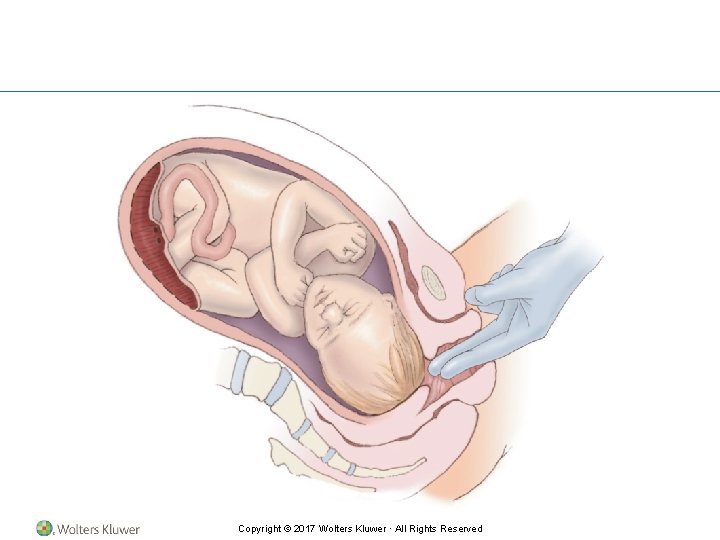
Copyright © 2017 Wolters Kluwer · All Rights Reserved
Fetal Assessment During Labor and Birth • Amniotic fluid analysis • Fetal heart rate monitoring – Handheld versus electronic; intermittent versus continuous; external versus internal • Fetal heart rate patterns – Baseline, baseline variability, periodic changes (see Table 14. 1) • Other assessment methods – Fetal scalp sampling, pulse oximetry, stimulation Copyright © 2017 Wolters Kluwer · All Rights Reserved
Guidelines for Assessing Fetal Heart Rate • Initial 10 - to 20 -minute continuous FHR assessment on entry into labor/birth area • Completion of a prenatal and labor risk assessment on all clients • Intermittent auscultation every 30 minutes during active labor for low-risk women and every 15 minutes for highrisk women • During second stage of labor intermittent auscultation every 15 minutes for low-risk women and every 5 minutes for high-risk women Copyright © 2017 Wolters Kluwer · All Rights Reserved
Question According to the ACOG, ICSI, and AWHONN guidelines, how often should the fetal heart rate be assessed for a high-risk laboring woman during the second stage of labor? a. Every 5 minutes b. Every 10 minutes c. Every 15 minutes d. Every 20 minutes Copyright © 2017 Wolters Kluwer · All Rights Reserved
Answer a. Every 5 minutes During the second stage of labor, intermittent auscultation should be done every 5 minutes for the high-risk woman and every 15 minutes for the low-risk woman. (ACOG, ICSI, AWHONN guidelines) Copyright © 2017 Wolters Kluwer · All Rights Reserved
Continuous Electronic Fetal Monitoring • Uses a machine to produce a continuous tracing of the FHR • Produce a graphic record of the FHR pattern • Primary objective – To provide information about fetal oxygenation and prevent fetal injury from impaired oxygenation – To detect fetal heart rate changes early before they are prolonged and profound Copyright © 2017 Wolters Kluwer · All Rights Reserved
Copyright © 2017 Wolters Kluwer · All Rights Reserved
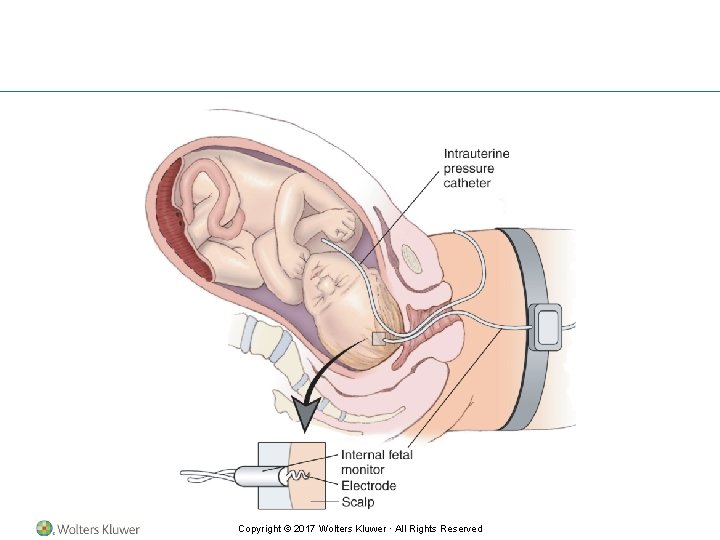
Criteria for Using Continuous Internal Monitoring of the FHR • Ruptured membranes • Cervical dilation of at least 2 cm • Present fetal part low enough to allow placement of the scalp electrode • Skilled practitioner available to insert spiral electrode Copyright © 2017 Wolters Kluwer · All Rights Reserved
Four Categories of Baseline Variability • Absent: fluctuation range undetectable • Minimal: fluctuation range observed at <5 beats per minute • Moderate: (normal) fluctuation range from 6 to 25 beats per minute • Marked: fluctuation range >25 beats per minute Copyright © 2017 Wolters Kluwer · All Rights Reserved
Nursing Interventions • Average FHR 110 to 160 beats per minute • Fetal bradycardia • Fetal tachycardia • FHR variability an indicator of fetal status Copyright © 2017 Wolters Kluwer · All Rights Reserved
Typical Periodic Baseline Changes • Accelerations • Decelerations – Early – Late – Variable – Prolonged Copyright © 2017 Wolters Kluwer · All Rights Reserved
Fetal Assessment • Nurse’s role • Additional methods to validate FHR – Fetal scalp sampling – Fetal pulse oximetry – Fetal stimulation Copyright © 2017 Wolters Kluwer · All Rights Reserved
Comfort and Pain Management • Pain as universal experience; intensity highly variable • Mandate for pain assessment in all clients admitted to health care facility • Numerous nonpharmacologic and pharmacologic choices available Copyright © 2017 Wolters Kluwer · All Rights Reserved
Nonpharmacologic Measures for Pain Management • Continuous labor support • Hydrotherapy • Ambulation and position changes • Acupuncture and acupressure • Attention focusing and imagery • Therapeutic touch and massage; effleurage • Breathing techniques (e. g. , patterned-paced breathing) Copyright © 2017 Wolters Kluwer · All Rights Reserved
Question Is the following statement True or False? Pain experienced by a woman in labor is fairly intense. a. True b. False Copyright © 2017 Wolters Kluwer · All Rights Reserved
Answer b. False Pain during labor is a universal experience, but the intensity varies. Copyright © 2017 Wolters Kluwer · All Rights Reserved
Pharmacologic Measures • Systemic analgesia • Regional or local anesthesia • Neuraxial analgesia/anesthesia techniques: use of analgesic or anesthetic, continuously or intermittently into epidural or intrathecal space • Shift in pain management: woman as an active participant during labor Copyright © 2017 Wolters Kluwer · All Rights Reserved
Systemic Analgesia • Route: typically administered parenterally through existing IV line • Drugs – Opioids (butorphanol, nalbuphine, meperidine, fentanyl) – Ataractics (hydroxyzine, promethazine) – Benzodiazepines (diazepam, midazolam) Copyright © 2017 Wolters Kluwer · All Rights Reserved
Regional Analgesia/Anesthesia • Epidural block: continuous infusion or intermittent injection; usually started when dilation >5 cm • Combined spinal–epidural block (“walking epidural”) • Patient-controlled epidural • Local infiltration (usually for episiotomy or laceration repair) • Pudendal block (usually for second stage, episiotomy, or operative vaginal birth) • Intrathecal (spinal) analgesia/anesthesia (during labor and cesarean birth) Copyright © 2017 Wolters Kluwer · All Rights Reserved
General Anesthesia • Emergency cesarean birth or woman with contraindication to use of regional anesthesia • IV injection, inhalation, or both • Commonly, first thiopental IV to produce unconsciousness • Next, muscle relaxant • Then intubation, followed by administration of nitrous oxide and oxygen; volatile halogenated agent also possible to produce amnesia Copyright © 2017 Wolters Kluwer · All Rights Reserved
Neuraxial Analgesia/Anesthesia • Rise in use • Does not interfere with progress of labor • Allows the woman to be an active participant in labor Copyright © 2017 Wolters Kluwer · All Rights Reserved
First Stage of Labor: Phone Assessment • Estimated date of birth • Fetal movement; frequency in past few days • Other premonitory signs of labor experienced • Parity, gravida, and previous childbirth experiences • Time frame in previous labors • Characteristics of contractions • Bloody show and membrane status (whether ruptured or intact) • Presence of supportive adult in household or if she is alone Copyright © 2017 Wolters Kluwer · All Rights Reserved
Nursing Care During First Stage of Labor • General measures – Obtain admission history – Check results of routine laboratory tests and any special tests – Ask about childbirth plan – Complete a physical assessment • Initial contact either by phone or in person Copyright © 2017 Wolters Kluwer · All Rights Reserved
First Stage of Labor: Admission Assessment • Maternal health history • Physical assessment (body systems, vital signs, heart and lung sounds, height and weight) – Fundal height measurement – Uterine activity, including contraction frequency, duration, and intensity – Status of membranes (intact or ruptured) – Cervical dilation and degree of effacement – Fetal heart rate, position, station – Pain level Copyright © 2017 Wolters Kluwer · All Rights Reserved
First Stage of Labor: Admission Assessment (cont. ) • Fetal assessment • Lab studies – Routine: urinalysis, CBC – Syphilis screening, Hbs. Ag screening, GBS, HIV (with woman’s consent), and possible drug screening if not included in prenatal history • Assessment of psychological status Copyright © 2017 Wolters Kluwer · All Rights Reserved
Question Is the following statement True or False? If a pregnant woman in labor calls the health care facility, the nurse should strongly advise the woman to come to the facility to be evaluated. a. True b. False Copyright © 2017 Wolters Kluwer · All Rights Reserved
Answer b. False If the initial contact is made by phone, the nurse needs to ask the woman about her signs and symptoms and what she is experiencing. The nurse would then instruct the woman to remain at home or come to the facility based on the woman’s responses. Copyright © 2017 Wolters Kluwer · All Rights Reserved
First Stage of Labor: Continuing Assessment • Woman’s knowledge, experience, and expectations • Vital signs • Vaginal examinations • Uterine contractions • Pain level • Coping ability • FHR • Amniotic fluid Copyright © 2017 Wolters Kluwer · All Rights Reserved
Nursing Management: Second Stage • Assessment – Typical signs of second stage – Contraction frequency, duration, intensity – Maternal vital signs – Fetal response to labor via FHR – Amniotic fluid with rupture of membranes – Coping status of woman and partner Copyright © 2017 Wolters Kluwer · All Rights Reserved
Question During the second stage of labor, assessment would include which of the following? a. Complaints of rectal or perineal pressure b. Estimated date of birth c. Fundal height d. Fetal position Copyright © 2017 Wolters Kluwer · All Rights Reserved
Answer a. Complaints of rectal or perineal pressure During the second stage of labor, the nurse would assess for signs typical for this stage, such as complaints of rectal or perineal pressure. Assessment of estimated date of birth, fundal height, and fetal position are assessments for the first stage of labor. Copyright © 2017 Wolters Kluwer · All Rights Reserved
Nursing Management: Second Stage • Interventions – Supporting woman and partner in active decision -making – Supporting involuntary bearing-down efforts; encouraging no pushing until strong desire or until descent and rotation of fetal head well advanced – Providing instructions, assistance, pain relief – Using maternal positions to enhance descent and reduce pain – Preparing for assisting with delivery Copyright © 2017 Wolters Kluwer · All Rights Reserved
Nursing Management: Second Stage (cont. ) • Interventions with birth – Cleansing of perineal area and vulva – Assisting with birth, suctioning of newborn, and umbilical cord clamping – Providing immediate care of newborn • Drying • Apgar score • Identification Copyright © 2017 Wolters Kluwer · All Rights Reserved
Nursing Management: Third Stage • Assessment – Placental separation; placenta and fetal membranes examination; perineal trauma; episiotomy; lacerations • Interventions – Instructing to push when separation apparent; giving oxytocin if ordered; assisting woman to comfortable position; providing warmth; applying ice to perineum if episiotomy; explaining assessments to come; monitoring mother’s physical status; recording birthing statistics; documenting birth in birth book Copyright © 2017 Wolters Kluwer · All Rights Reserved
Nursing Management: Fourth Stage • Assessment – Vital signs, fundus, perineal area, comfort level, lochia, bladder status • Interventions – Support and information – Fundal checks; perineal care and hygiene – Bladder status and voiding – Comfort measures – Parent–newborn attachment – Teaching Copyright © 2017 Wolters Kluwer · All Rights Reserved
- Slides: 38