CHAPTER 19 Nursing Care of the Family During




- Slides: 49
CHAPTER 19 Nursing Care of the Family During Labor and Birth Copyright © 2016 by Elsevier Inc. All rights reserved.
LEARNING OBJECTIVES * Describe the ongoing assessment of maternal progress during the first, second, third, and fourth stages of labor. • Recognize the physical and psychosocial findings indicative of maternal progress during labor. • Describe fetal assessment during labor.
LEARNING OBJECTIVES (CONT. ) • Incorporate evidence-based nursing interventions into a comprehensive plan of care relevant to each stage of labor. • Understand how The Safe Deliveries Roadmap put out by the Washington State Hospital Association adopts evidenced-based practices to ensure safe deliveries and healthy babies. • Recognize the importance of support (family, partner, doula, nurse) in fostering maternal confidence and facilitating the progress of labor and birth.
LEARNING OBJECTIVES (CONT. ) • Analyze the influence of cultural and religious beliefs and practices on the process of labor and birth. • Evaluate the effect of perineal trauma on the woman’s reproductive and sexual health. • Identify the other P’s in the labor process: Position, Psychological • Understand how the development of the Friedman Curve guided practice and why people are questioning it today.
First Stage of Labor Begins with regular uterine contractions Ends with full cervical effacement and dilation Obstetric triage Prenatal data Ø The nurse reviews the prenatal record to identify the woman’s individual needs and risks Copyright © 2016 by Elsevier Inc. All rights reserved. 5
FIRST STAGE OF LABOR (CONT. ) • Three phases of the first stage of labor • Latent phase (up to 6 cm of dilation) • Active phase (4 to 7 cm of dilation) • Transition phase (8 to 10 cm of dilation)
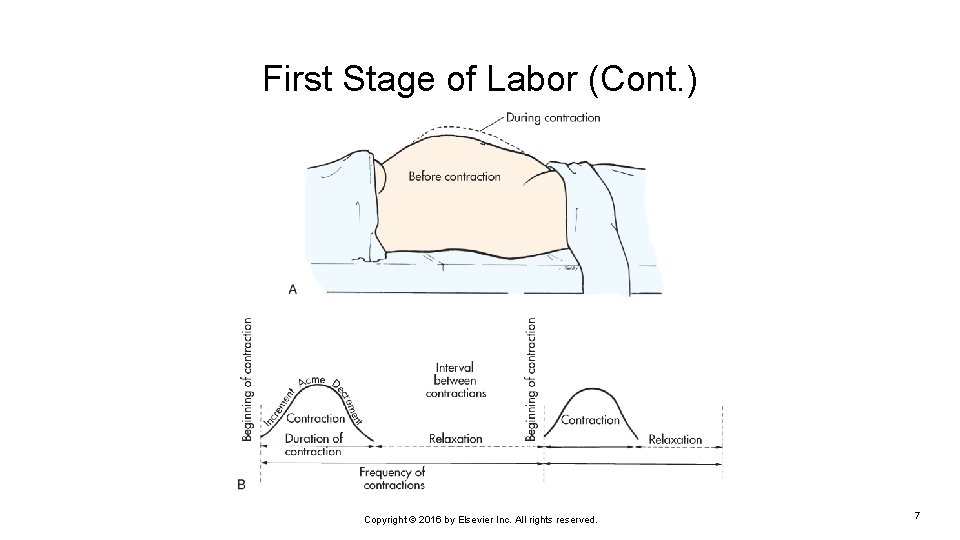
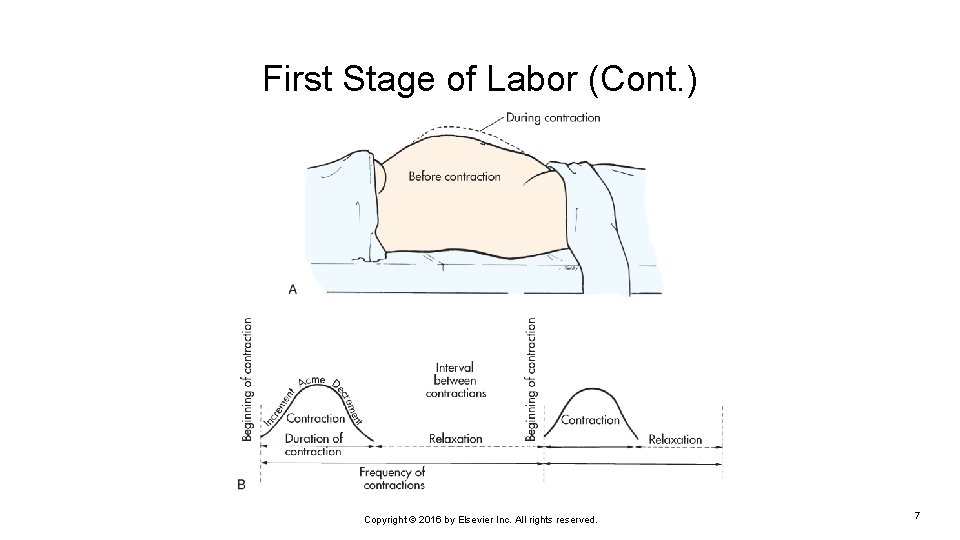
First Stage of Labor (Cont. ) Copyright © 2016 by Elsevier Inc. All rights reserved. 7
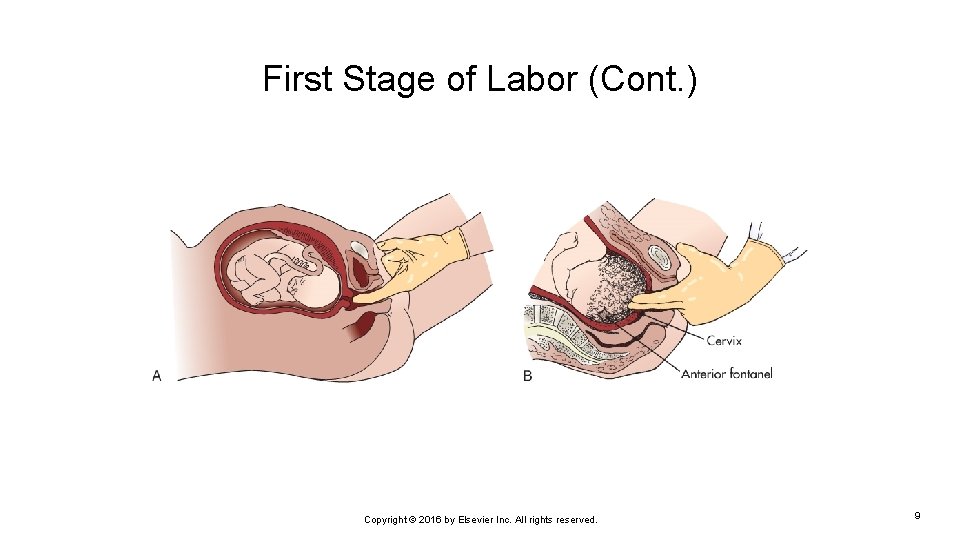
FIRST STAGE OF LABOR (CONT. ) • Assessment and nursing diagnosis • Determination of whether the woman is in labor • Contractions • Cervix • Fetus
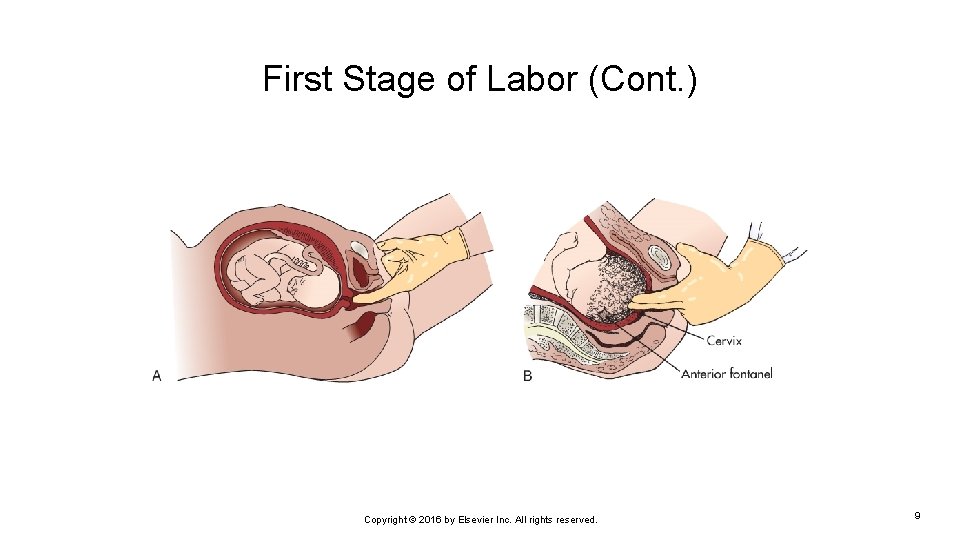
First Stage of Labor (Cont. ) Copyright © 2016 by Elsevier Inc. All rights reserved. 9
FIRST STAGE OF LABOR (CONT. ) • Assessment and nursing diagnosis • Admission to the labor unit • Admission data • Prenatal data • Interview • Spontaneous rupture of membranes • Bloody or pink show • Psychosocial factors (P) • Women with history of sexual abuse • Other vaginal trauma (FGM) • Obstetrical History • Support • Stress in labor
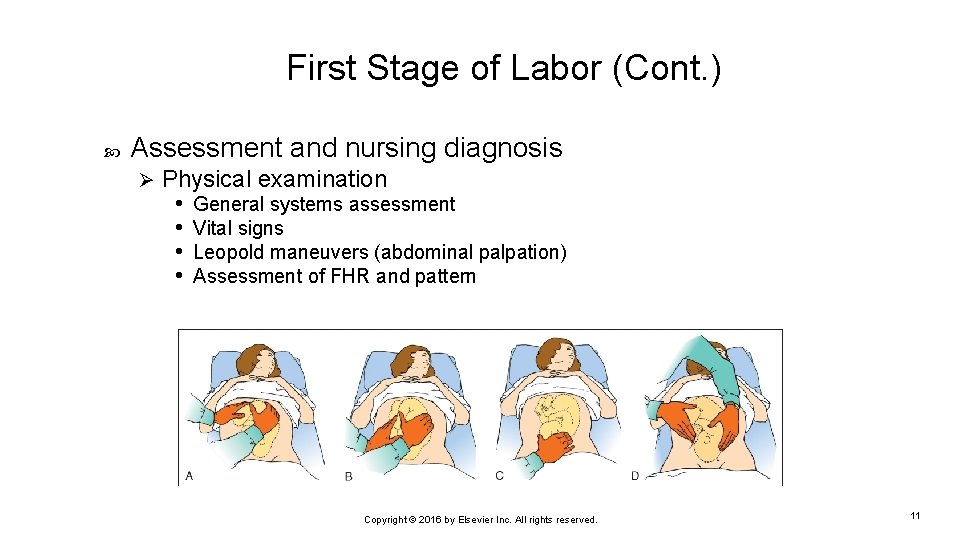
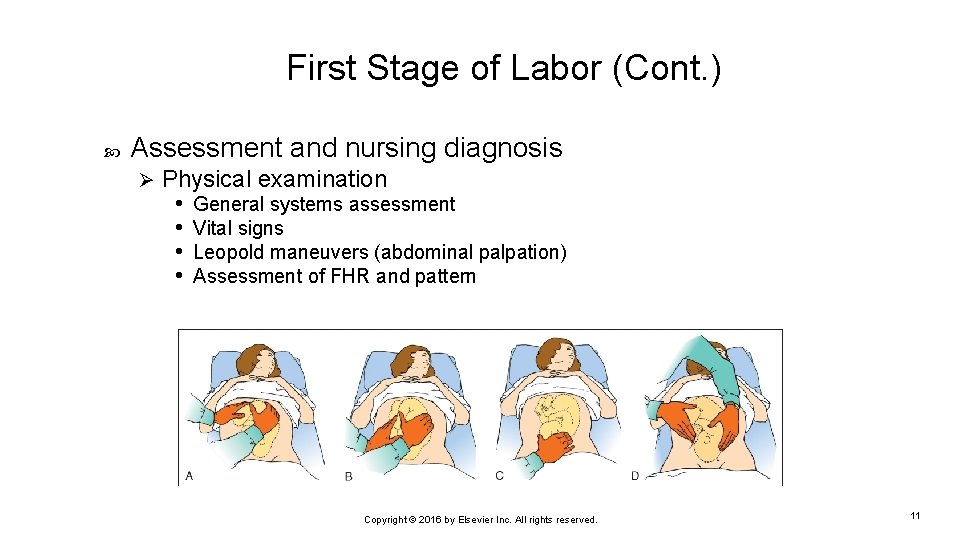
First Stage of Labor (Cont. ) Assessment and nursing diagnosis Ø Physical examination • General systems assessment • Vital signs • Leopold maneuvers (abdominal palpation) • Assessment of FHR and pattern Copyright © 2016 by Elsevier Inc. All rights reserved. 11
FIRST STAGE OF LABOR (CONT. ) • Assessment and nursing diagnosis • Physical examination • Assessment of uterine contractions • Frequency • Intensity • Mild, moderate, or strong • Duration • Resting tone • Vaginal examination • Cervical effacement, dilation, fetal descent
FIRST STAGE OF LABOR (CONT. ) • Assessment and nursing diagnosis • Laboratory and diagnostic tests • Analysis of urine specimen • Blood tests • Complete blood count (CBC) • Type and screen • Assessment of amniotic membranes and fluid • Other tests • If GBS status unknown, rapid test can be performed • Signs of potential problems
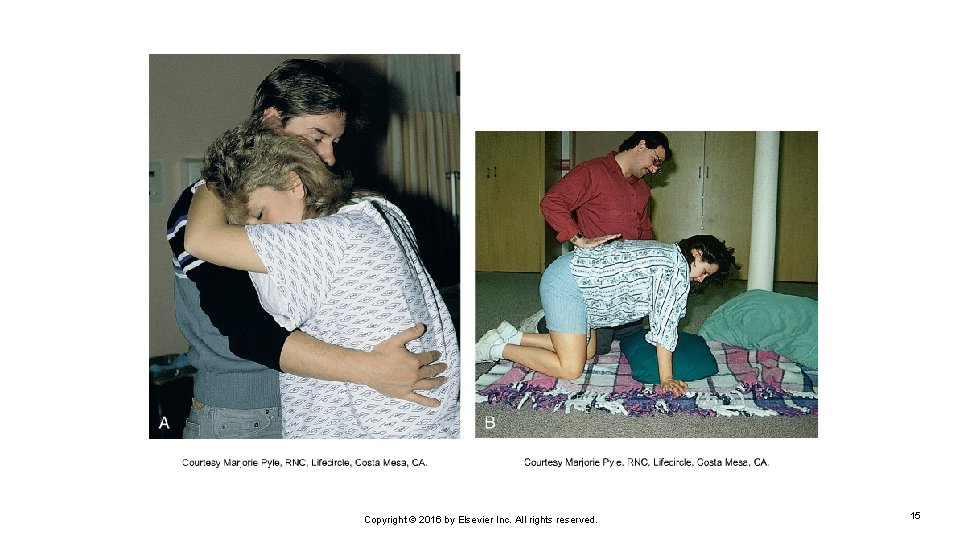
FIRST STAGE OF LABOR (CONT. ) • Plan of care and interventions • Standards of care • Physical nursing care during labor • General hygiene • Nutrient and fluid intake • Oral intake • Intravenous intake • Elimination • Voiding: at least every 2 hours • Catheterization • Bowel elimination • Ambulation and positioning
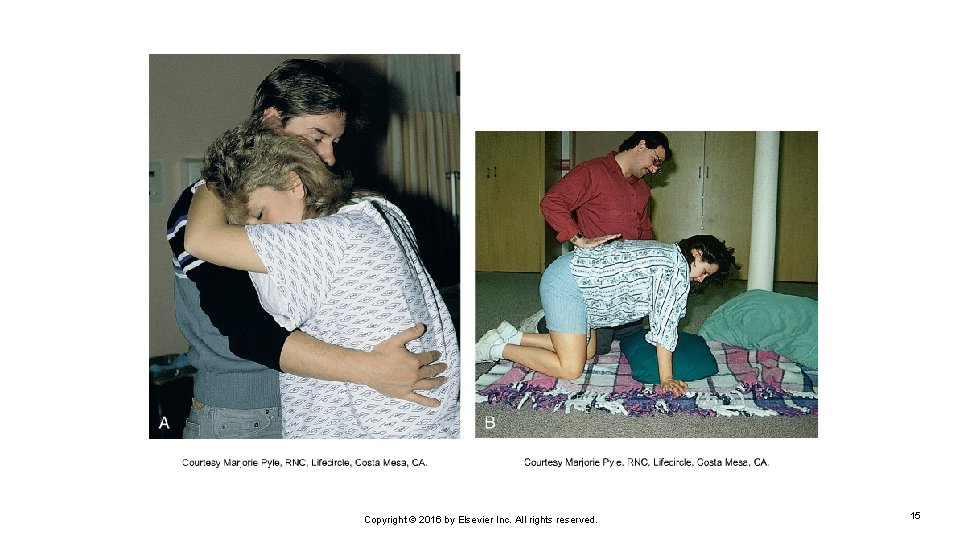
Copyright © 2016 by Elsevier Inc. All rights reserved. 15
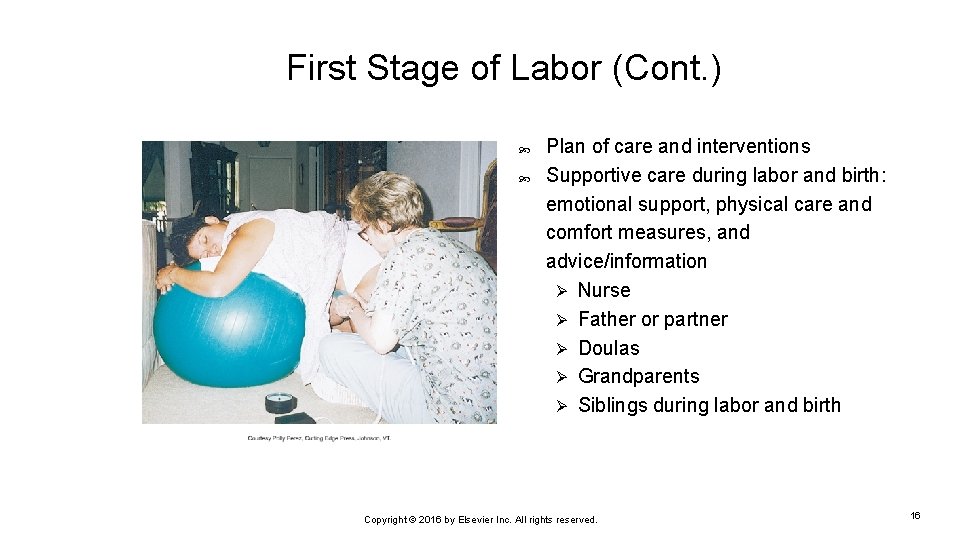
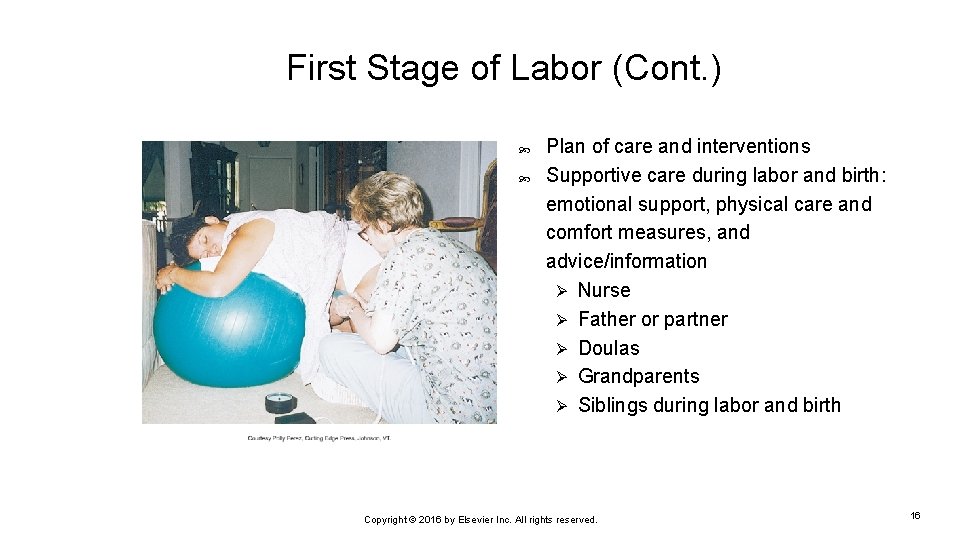
First Stage of Labor (Cont. ) Plan of care and interventions Supportive care during labor and birth: emotional support, physical care and comfort measures, and advice/information Ø Nurse Ø Father or partner Ø Doulas Ø Grandparents Ø Siblings during labor and birth Copyright © 2016 by Elsevier Inc. All rights reserved. 16
CASE STUDY A 22 -year-old woman presents to your maternity triage area. When you ask her reason for seeking care, she states, “I keep changing my underwear, but then it gets wet again. ” • What other information do you need to gather? • What can you do to figure out whether or not her bag of waters (BOW) is ruptured?
CASE STUDY (CONT. ) • Her bag of waters (BOW) is not broken. What should you do next? • Your patient is 2 cm/50%/-2. What stage and phase of labor is she in? What is your next assessment/intervention?
CASE STUDY (CONT. ) You receive orders to send the patient home. She states, “I can’t believe you’re sending me home when I’m so crampy! How am I supposed to sleep tonight? ” • What comfort measures will you suggest? • What teaching do you need to do?
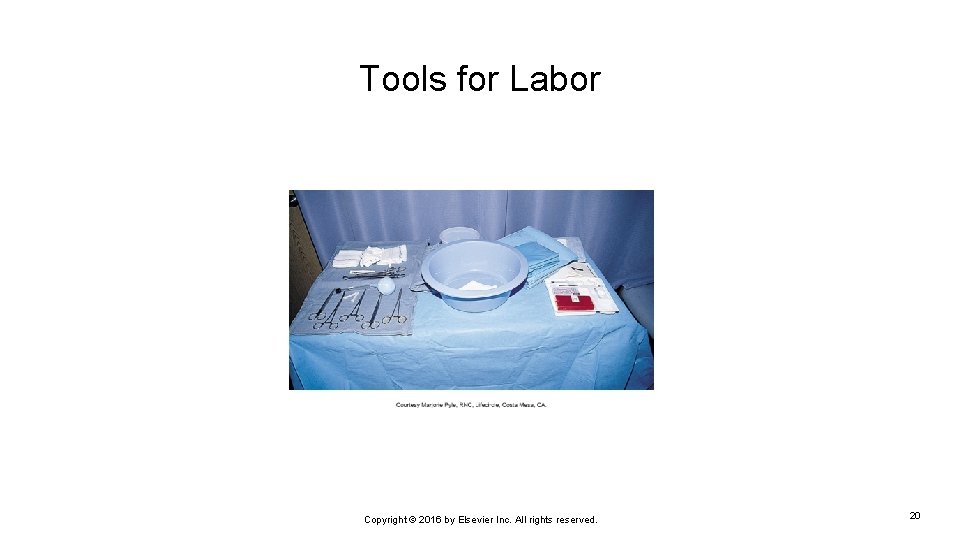
Tools for Labor Copyright © 2016 by Elsevier Inc. All rights reserved. 20
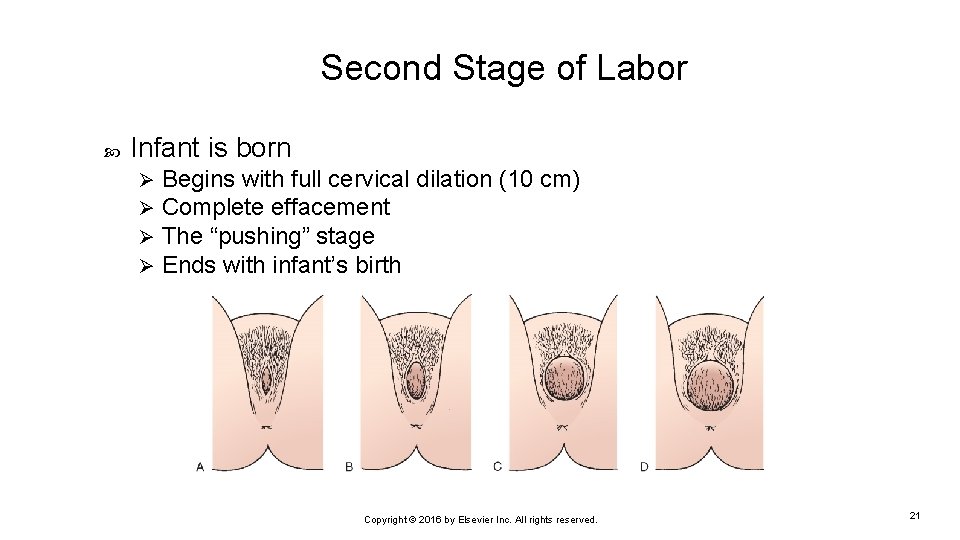
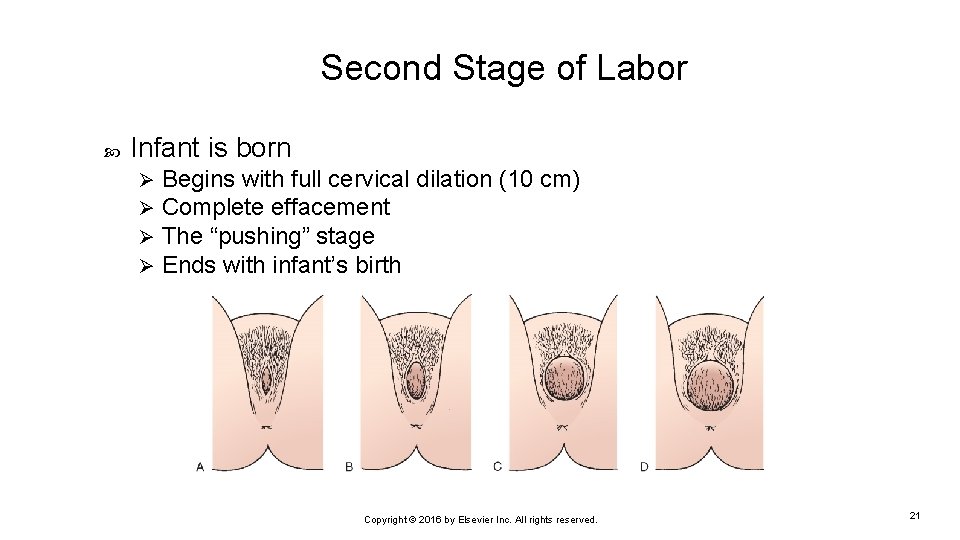
Second Stage of Labor Infant is born Ø Ø Begins with full cervical dilation (10 cm) Complete effacement The “pushing” stage Ends with infant’s birth Copyright © 2016 by Elsevier Inc. All rights reserved. 21
SECOND STAGE OF LABOR (CONT. ) • Two phases • Latent: relatively calm with passive descent of baby through birth canal (laboring down) • Active: pushing and urge to bear down • Ferguson reflex: the urge to “bear down”
CARE MANAGEMENT • Preparing for birth • Maternal position: Supine, semirecumbent, or lithotomy positions are still widely used in Western societies despite evidence that an upright position shortens labor. • Bearing-down efforts • Valsalva maneuver • Fetal heart rate and pattern • Support of father or partner • Supplies, instruments, and equipment
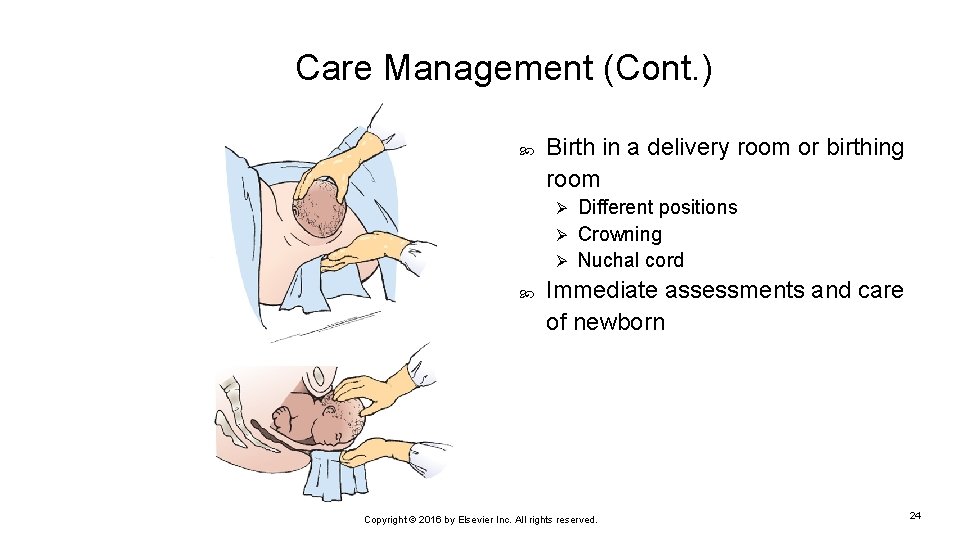
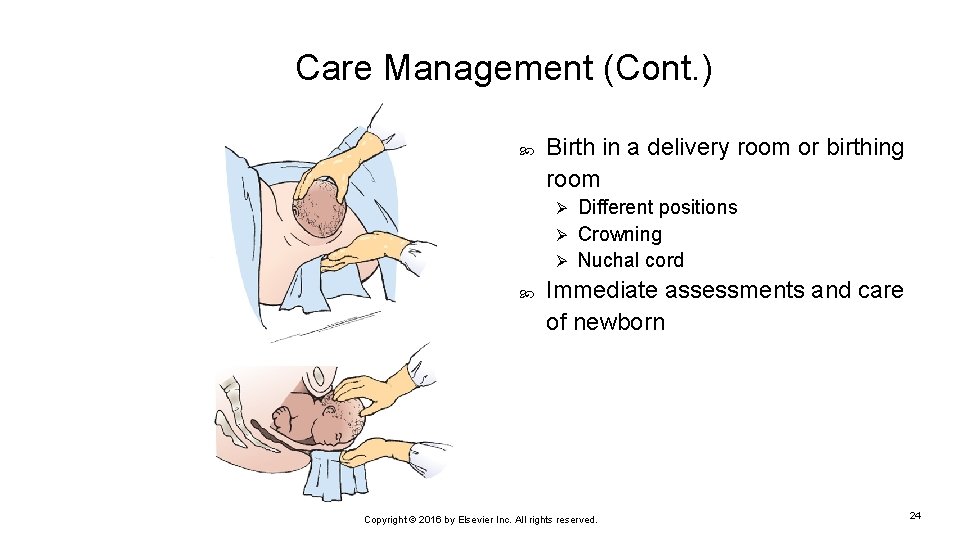
Care Management (Cont. ) Birth in a delivery room or birthing room Different positions Ø Crowning Ø Nuchal cord Ø Immediate assessments and care of newborn Copyright © 2016 by Elsevier Inc. All rights reserved. 24
CARE MANAGEMENT: PERINEAL TRAUMA RELATED TO CHILDBIRTH • Perineal lacerations • First degree: laceration that extends through the skin and vaginal mucous membrane but not the underlying fascia and muscle • Second degree: laceration that extends through the fascia and muscles of the perineal body, but not the anal sphincter • Third degree: laceration that involves the external anal sphincter • Fourth degree: laceration that extends completely through the rectal mucosa, disrupting both the external and internal anal sphincters
CARE MANAGEMENT: PERINEAL TRAUMA RELATED TO CHILDBIRTH (CONT. ) • Vaginal and urethral lacerations • Cervical injuries • Episiotomy • An incision in the perineum used to enlarge the vaginal outlet • Has steadily declined in recent years due to a lack of sound, rigorous research to support its benefits
EXAMPLE OF EVIDENCE-BASED PRACTICE • Cochrane Review published October 2015: Pushing methods for the second stage of labor • Review of randomized controlled trials including: • 7 trials (815 women) comparing the types of pushing: spontaneous vs. directed pushing with or without epidural anesthesia • 13 trials (2879 women) comparing timing of pushing: delayed pushing versus immediate pushing with epidural anesthesia.
EVIDENCE-BASED PRACTICE (CONT’D) • Results: • For type of pushing: (spontaneous vs. active pushing) • No clear difference in the duration of second stage • No clear difference in perineal lacerations and episiotomies • No difference in the mode of birth ( spontaneous vaginal delivery, instrumental delivery or c-section) • No difference in outcomes of baby in terms of apgar scores or admission to NICU
EVIDENCE-BASED PRACTICE (CONT’D) • Results: • For the timing of pushing: (delayed pushing vs. immediate pushing – all women with an epidural) • Delayed pushing was associated with an increase in the duration of the second stage by about 54 minutes. • No difference in terms of perineal lacerations and episiotomies • No difference in neonatal outcomes in terms of Apgar scores and NICU admission • Delayed pushing reduced the duration of pushing by about 20 minutes and slightly increased the rate of spontaneous vaginal delivery • Delayed pushing was associated with an increased incidence of low umbilical cord p. H
EVIDENCE-BASED PRACTICE (CONT’D) How would you use this evidence? What is your clinical bottom line? Citation: http: //www. cochrane. org/CD 009124/PREG_pushing-methods-second-stage-labour

THIRD STAGE OF LABOR • Birth of the baby until the placenta is expelled • The third stage is generally by far the shortest stage of labor • Usually expelled within 10 to 15 minutes after the birth; may be problematic if >30 minutes • Active management of the third stage (Pitocin, gentle traction of the cord) • Sudden gush of dark blood from the introitus • Apparent lengthening of the umbilical cord • Vaginal fullness • Placental examination and disposal • Cultural preferences
VIDEOS
CHALLENGING FRIEDMAN’S CURVE


FOURTH STAGE OF LABOR • Care management • First 1 to 2 hours after birth • Assessment of maternal physical status • Physiologic changes to prepregnancy status • Signs of potential problems • Excessive blood loss • Alterations in vital signs and consciousness • Care of the new mother and post anesthesia/analgesia care • Care of the family • Family-newborn relationships

THE SAFE DELIVERIES ROADMAP • This collaboration is led by the Washington State Hospital Association to adopt evidenced-based practices to ensure safe deliveries and healthy babies. This initiative is undertaken in partnership with leading organizations, and builds upon the successful effort to reduce early elective deliveries.
VIDEO OF ROADMAP
SUMMARY OF LABOR AND DELIVERY RECOMMENDATIONS • First Stage: Delay Admission to Labor Unit * Cervix less than 4 cm * Membranes intact * Reactive NST/ FHR Category 1 confirmed by two practitioners * Pain control adequate with appropriate outpatient interventions as needed
SUMMARY OF L&D RECOMMENDATIONS (CONTINUED) • First Stage: Consider Discharge Home or Further Observation * Cervix 4 -5 cm without change x 2 -4 hours * Less than 80% effacement * Membranes intact * Reactive NST/ FHR Cat 1 * Contractions less than 3/ 10 minutes
SUMMARY OF L&D RECOMMENDATIONS (CONTINUED) • First Stage: Consider Artificial Rupture of Membranes * Cervix 4 -5 cm without change x 2 -4 hours * 90 -100% effacement * Membranes intact * Reactive NST/ FHR Cat 1 * Contractions less than 3 / 10 minutes
SUMMARY OF L&D RECOMMENDATIONS (CONTINUED) First Stage: Consider Cesarean Delivery * Cervix 6 cm or greater * Membranes ruptured (if feasible) * Arrest of cervical dilation and uterine activity Second Stage: Assessment of Descent and Position of Presenting Part * At least every 1 -2 hours
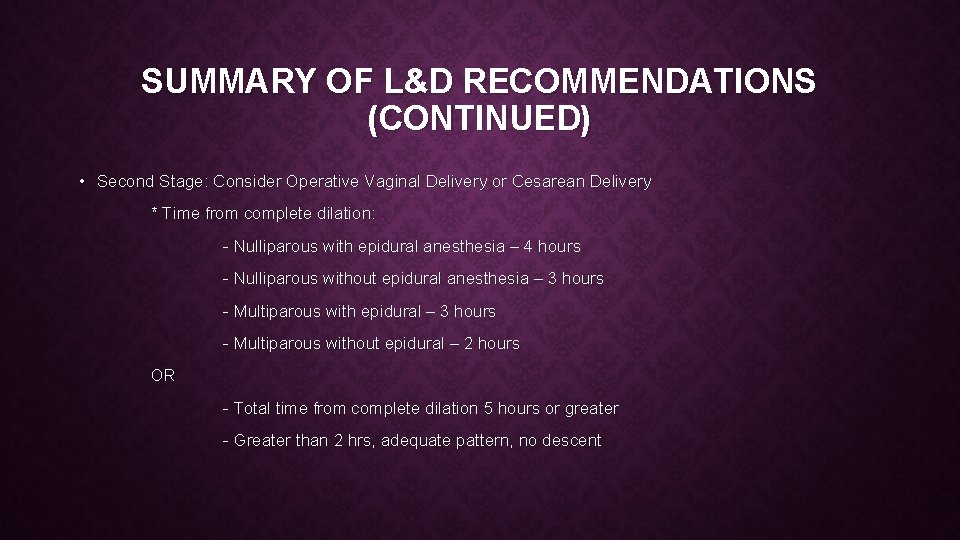
SUMMARY OF L&D RECOMMENDATIONS (CONTINUED) • Second Stage: Consider Operative Vaginal Delivery or Cesarean Delivery * Time from complete dilation: - Nulliparous with epidural anesthesia – 4 hours - Nulliparous without epidural anesthesia – 3 hours - Multiparous with epidural – 3 hours - Multiparous without epidural – 2 hours OR - Total time from complete dilation 5 hours or greater - Greater than 2 hrs, adequate pattern, no descent
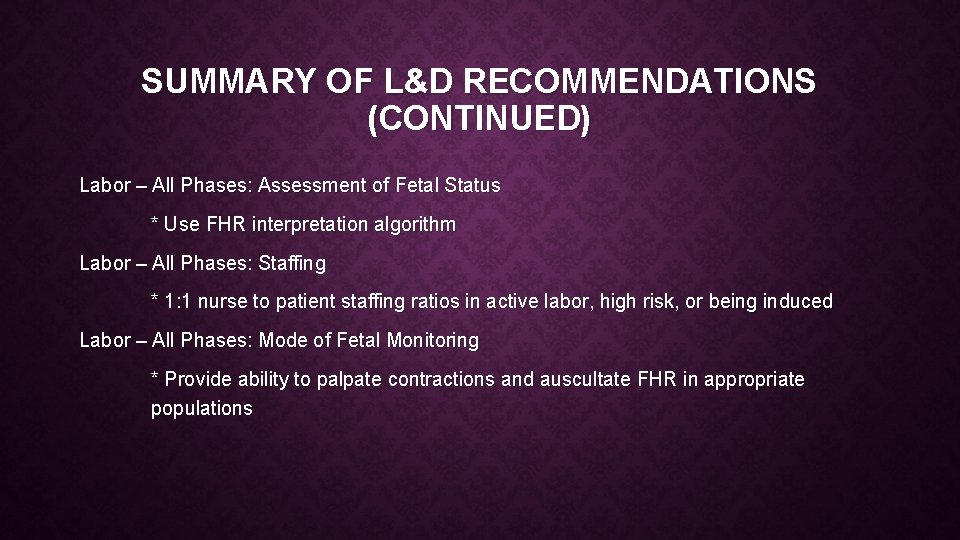
SUMMARY OF L&D RECOMMENDATIONS (CONTINUED) Labor – All Phases: Assessment of Fetal Status * Use FHR interpretation algorithm Labor – All Phases: Staffing * 1: 1 nurse to patient staffing ratios in active labor, high risk, or being induced Labor – All Phases: Mode of Fetal Monitoring * Provide ability to palpate contractions and auscultate FHR in appropriate populations
KEY POINTS • The familiar environment of her home is most often the ideal place for a woman during the latent/early phase of the first stage of labor. • The nurse assumes much of the responsibility for assessing the progress of labor and for keeping the nurse-midwife or physician informed about that progress and deviations from expected findings.
KEY POINTS (CONT. ) • The fetal heart rate and pattern reveal the fetal response to the stress of the labor process. • Regardless of the actual labor and birth experience, the woman’s or couple’s perception of the birth experience is most likely to be positive when events and performances are consistent with expectations, especially in terms of maintaining control and adequacy of pain relief.
KEY POINTS (CONT. ) • The woman’s level of anxiety may increase when she does not understand what is being said to her about her labor because of the medical terminology used or because of a language barrier. • Coaching, emotional support, and comfort measures assist the woman to use her energy constructively in relaxing and working with the contractions.
KEY POINTS (CONT. ) • The progress of labor is enhanced when a woman changes her position frequently during the first stage of labor. • The cultural beliefs and practices of a woman and her significant others, including her partner, can have a profound influence on their approach to labor and birth. • Women with a history of sexual abuse or vaginal trauma often experience profound stress and anxiety during childbirth.
KEY POINTS (CONT. ) • Practice changes based on new evidence, and as practitioners we must keep up with what our guiding organizations are advising and what the new standards of practice are in order to deliver safe healthcare to our patients and promote healthy outcomes.
 Family care plan in community health nursing
Family care plan in community health nursing Ocd nursing care plan pdf
Ocd nursing care plan pdf Cataract nursing care plan
Cataract nursing care plan Levels of care primary secondary tertiary
Levels of care primary secondary tertiary Chapter 7 nursing management of pain during labor and birth
Chapter 7 nursing management of pain during labor and birth Chapter 14 nursing management during labor and birth
Chapter 14 nursing management during labor and birth Chapter 41 rehabilitation and restorative nursing care
Chapter 41 rehabilitation and restorative nursing care Nurse charting examples
Nurse charting examples The nursing assistant and the care team
The nursing assistant and the care team Chapter 2 foundations of resident care
Chapter 2 foundations of resident care Family guy is not appropriate to watch during school
Family guy is not appropriate to watch during school Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Tư thế worm breton
Tư thế worm breton Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Các môn thể thao bắt đầu bằng tiếng đua
Các môn thể thao bắt đầu bằng tiếng đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính thế năng
Công thức tính thế năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Phép trừ bù
Phép trừ bù Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thế nào là giọng cùng tên?
Thế nào là giọng cùng tên? Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Fecboak
Fecboak Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot Số.nguyên tố
Số.nguyên tố Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Hổ sinh sản vào mùa nào
Hổ sinh sản vào mùa nào Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập