ECTOPIC PREGNANCY ECTOPIC PREGNANCY In ectopic pregnancy a
- Slides: 46
ECTOPIC PREGNANCY
ECTOPIC PREGNANCY In ectopic pregnancy, a fertilized ovum implants in an area other-than the endometrial lining of the uterus More than 95 o/o of extrauterine Pregnanciesoccuri n the fallopian tube.
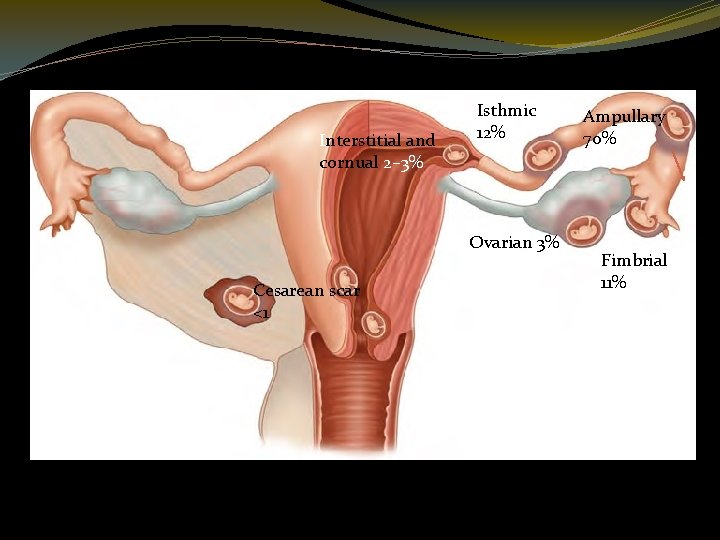
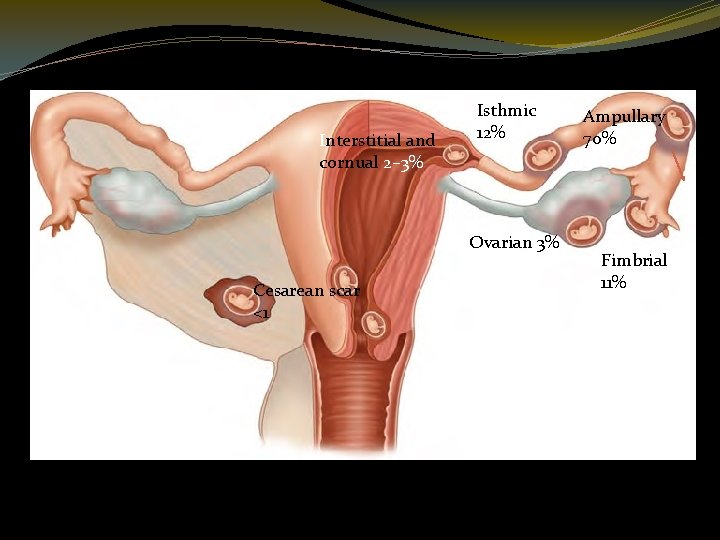
Interstitial and cornual 2– 3% Isthmic 12% Ovarian 3% Cesarean scar <1 Abdominal 1% Cervical <1% Ampullary 70% Fimbrial 11%
incidence �The incidence in the United Kingdom has changed little in the last decade with 9. 6 ectopics per 1000 pregnancies in 1991– 1993 and 11. 0 per 1000 pregnancies in 2000– 2002 This may be due, at least in part, to a higher incidence of salpingitis, an increase in ovularion induction and assisted reproductive technology, and more tubal sterilization
Increasing Ectopic Pregnancy Rates A number of reasons at least partially explain the increased rate of ectopic pregnancies in the United States and many European countries. Some of these include: 1. Increasing prevalence of sexually transmitted infections, especially those caused by Chlamydia trachomatis 2. Identification through earlier diagnosis of some ectopic pregnancies otherwise destined to resorb spontaneously
3. Popularity of contraception that predisposes pregnancy failures to be ectopic 4. Tubal sterilization techniques that with contraceptive failure increase the likelihood of ectopic pregnancy 5. Assisted reproductive technology 6. Tubal surgery, including salpingotomy for tubal pregnancy and tuboplasty for infertility.
Mortality �According to the World Health Organization (2007), ectopic pregnancy is responsible for almost 5 percent of maternal deaths in developed countries.
Risk factors for ectopic pregnancy �History of previous ectopic pregnancy �(IUCD) or sterilization failure �Pelvic inflammatory disease �Chlamydia infection �Early age of intercourse and multiple partners �History of infertility �Previous pelvic surgery �Increased maternal age �Cigarette smoking �Strenuous physical exercise �In utero DES exposure
TUBAL PREGNANCY �The fertilized ovum may lodge in any portion of the oviduct, giving rise to ampullary, isthmic, and interstitial tubal pregnancies In rare instances, the fertilized ovum may implant in the fimbriated extremity. The ampulla is the most frequent site, followed by the isthmus. Interstitial pregnancy accounts for only about 2 percent. From these primary types, secondary forms of tubo-abdominal, tubo-ovarian, and broadligament pregnancies occasionally develop.
Clinical presentation 1 -subacute clinical picture of A. abdominal pain &vaginal bleeding in early pregnancy. Vaginal bleeding is usually dark red, indicative old blood B- abdominal/ pelvic pain may be localized to the iliac fossa. C- sholder tip pain indicative of free blood in the abdominal cavity D- dizzeness (anaemia) Bimanual examination can reveal tenderness in the fornices and there may be cervical excitation 2 - Acute clinical presentation due to rupture ectopic pregnancy with massive intraperitoneal bleeding. They can present with signs of hypovolaemic shock & acute abdomen
Investigation �The following are useful investigation for the diagnosis of ectopic pregnancy � 1 - observations : Bp, pulse , temperatuer � 2 - laboratory investigations: �Haemoglobin. blood group(prepare blood forr cross match) & B-HCG �A B-HCG level of less than 5 m. IU/ml, is considered negative for pregnancy& any thing above 25 m. IU/ml is considered positive for pregnancy �In 85% of pregnancy the B-HCG levels almost double every 48 hours in normally developing intrautrine pregnancy
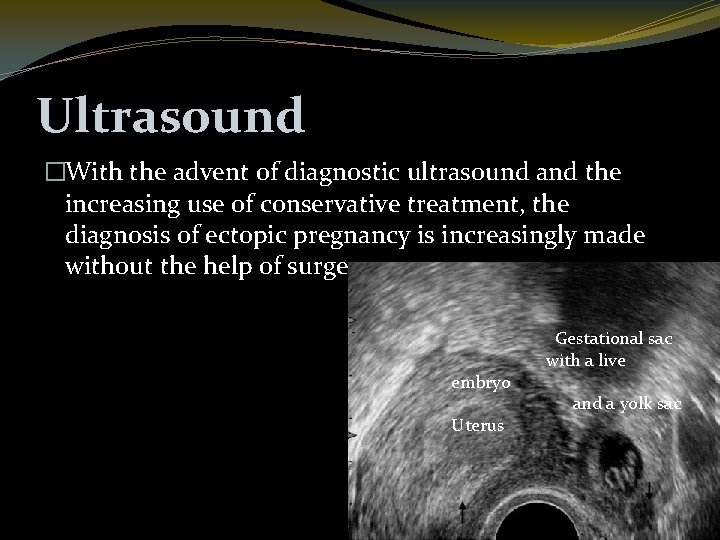
In ectopic pregnancy the rise in B-HCG is suboptimal, . However multiple readings are required for comparison purposes. Transvaginal ultrasound scan (TVS) An intrauterine gestational sac should be visualized at 4. 5 weeks Gestation. the corresponding B-HCG at that gestation is around 1500 m. IU/ml. By the time a gestational sac with fetal heart pulsation is detcted (at around 5 weeks gestation)B-HCGlevel should be around 3000 m. IU/ml Thus , if there were discrepancy betwween B-HCG cocentration and that seen on ultrasound scan(e. g. a high. B-HCG with no intruterine pregnancy on ultrasound scan), the differential diagnosis of an ectopic pregnancy must be made.
�Identification of an intruterine pregnancy(gestational sac, yolk sac, and fetal pole) on TVS effectively excludes the possibility of ectopic pregnancy in most patients except in those patients with rare hterotopic pregnancy. �The presence of free fluid during TVSis suggestive of a ruptured cetopic pregnancy �Lparoscopy: this can be used to diagnose and treat ectopic pregnancy
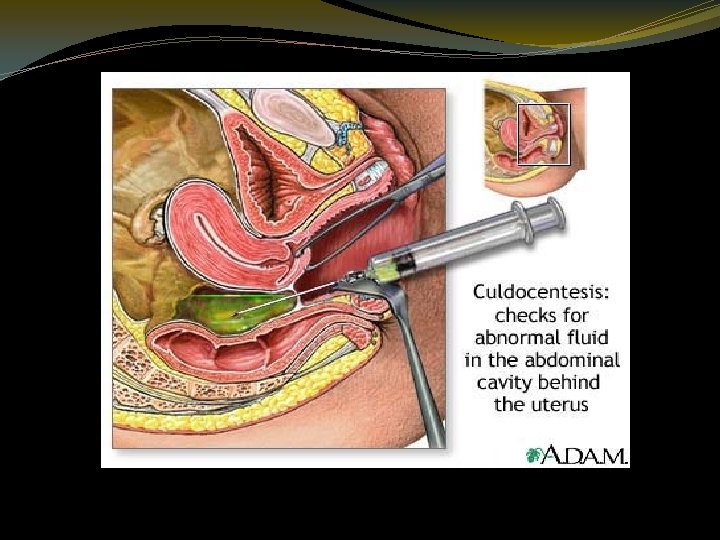
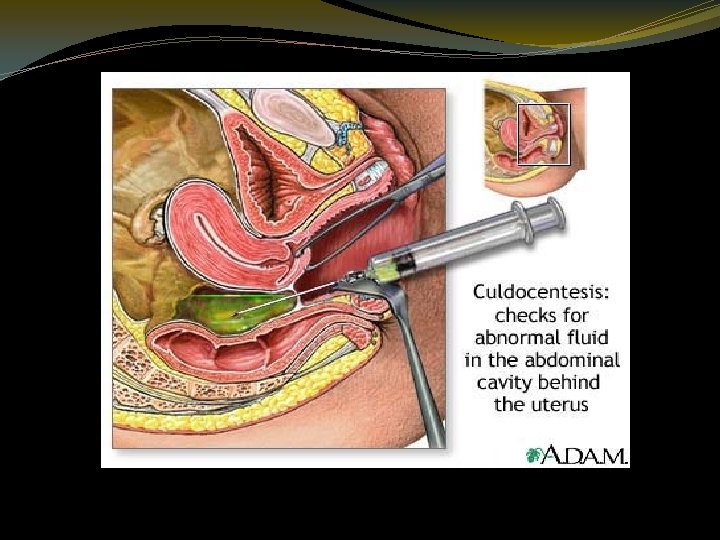
Culdocentesis This simple technique was used commonly in the past to identify hemoperitoneum. The cervix is pulled toward the symphysis with a tenaculum, and a long 16 - or 18 -gauge needle is inserted through the posterior vaginal fornix into the cul-de-sac. If present, fluid can be aspirated, however, failure to do so is interpreted only as unsatisfactory entry into the cul-de-sac and does not exclude an ectopic pregnancy, either ruptured or unruptured. Fluid containing fragments of old clots, or bloody fluid that does not clot, is compatible with the diagnosis of hemoperitoneum resulting from an ectopic pregnancy. If the blood subsequently clots, it may have been obtained from an adjacent blood vessel rather than from a bleeding ectopic pregnancy.
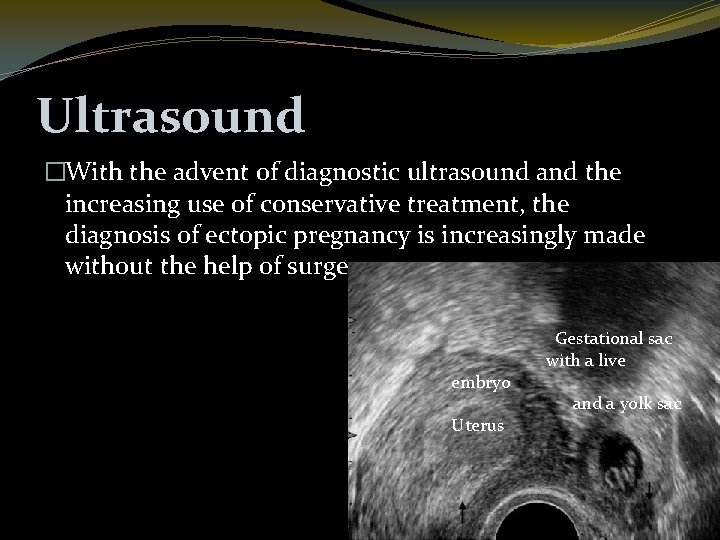
Ultrasound �With the advent of diagnostic ultrasound and the increasing use of conservative treatment, the diagnosis of ectopic pregnancy is increasingly made without the help of surgery. embryo Uterus Gestational sac with a live and a yolk sac
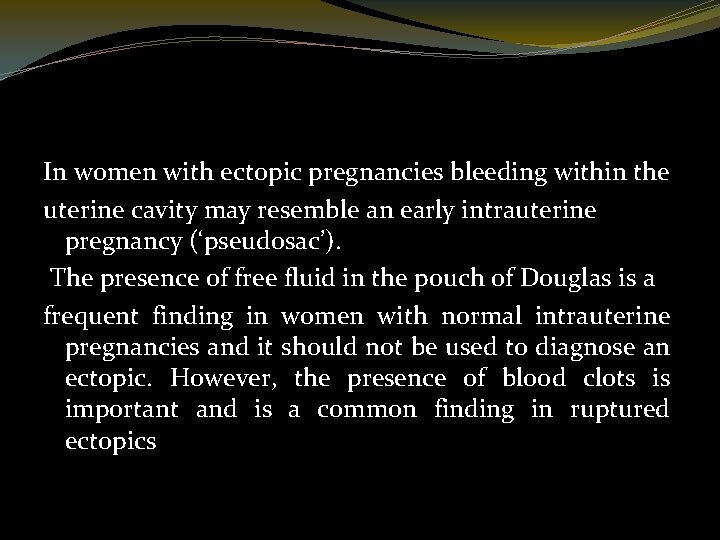
In women with ectopic pregnancies bleeding within the uterine cavity may resemble an early intrauterine pregnancy (‘pseudosac’). The presence of free fluid in the pouch of Douglas is a frequent finding in women with normal intrauterine pregnancies and it should not be used to diagnose an ectopic. However, the presence of blood clots is important and is a common finding in ruptured ectopics
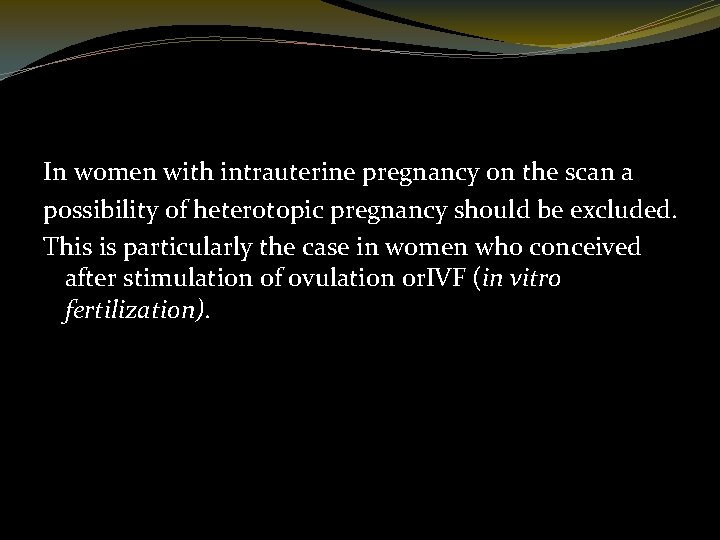
In women with intrauterine pregnancy on the scan a possibility of heterotopic pregnancy should be excluded. This is particularly the case in women who conceived after stimulation of ovulation or. IVF (in vitro fertilization).
Serum Progesterone. A single progesterone measurement can be used to establish with high reliability that there is a normally developing pregnancy. A value exceeding 25 ng/m. L excludes ectopic pregnancy with 92. 5 -percent sensitivity. �Conversely, values below 5 ng/m. L are found in only 0. 3 percent of normal pregnancies. Thus, values 5 ng/m. L suggest either an intrauterine pregnancy with a dead fetus or an ectopic pregnancy. Because in most ectopic pregnancies, progesterone levels range between 10 and 25 ng/m. L, the clinical utility is limited
Novel Serum Markers. A number of preliminary studies have been done to evaluate novel markers to detect ectopic pregnancy. These include vascular endothelial growth factor (VEGF), cancer antigen 125 (CA 125), creatine kinase, fetal fibronectin, and mass spectrometry-based proteomics None of these are in current clinical use.
�Differential diagnosis The diagnosis is from any other acute abdominal catastrophe such as rupture of a viscus or acute peritonitis. The clinical picture is so typical that in most cases diagnosis presents no difficulty. Other diagnoses which may confuse are: • inevitable miscarriage; • bleeding with an ovarian cyst; • pelvic appendicitis; • acute salpingitis.
Management
Expectant management �Expectant management has important advantages over medical treatment as it follows the natural history of the disease and is free from serious side effects of methotrexate. Expectant management requires prolonged follow-up and it may cause anxiety to both women and their carers. However, the main limiting factor in the use of expectant management is the relatively high failure rate and the inability to identify with accuracy the cases that are likely to fail expectant management. To minimize the risk of failure many authors have used very strict selection criteria for expectant management such as the initial h. CG <250 IU
Surgery has been traditionally used both for the diagnosis and treatment of ectopic pregnancy. With recent advances in operative laparoscopy, the minimally invasive approach has also become accepted as the method of choice to treat most tubal ectopic pregnancies. There are important advantages of laparoscopic over open surgery which include less post-operative pain, shorter hospital stay and faster resumption of social activity
Laporatomy In a case of severe haemorrhage in ruptured ectopic pregnancy , the patient must be taken immediately to the operating theatre. Little time should be wasted in attempting resuscitation which can prove useless and may only increase bleeding. An intravenous drip should be set up and a blood transfusion given as soon as possible.
�Surgical Management Laparoscopy is the preferred surgical treatment for ectopic pregnancy unless the woman is hemodynamically unstable �Tubal surgery is considered *conservative when there is tubal salvage. Examples include salpingostomy, salpingotomy, and fimbrial expression of the ectopic pregnancy. �*Radical surgery is defined by salpingectomy.
Laparoscopy techniques exist to: • kill the embryo with a direct injection of methotrexate or mifepristone allowing absorption so requiring no surgery on the tube; • incise the swollen tube over the ectopic pregnancy, aspirate the embryo, and achieve haemostasis (salpingostomy).
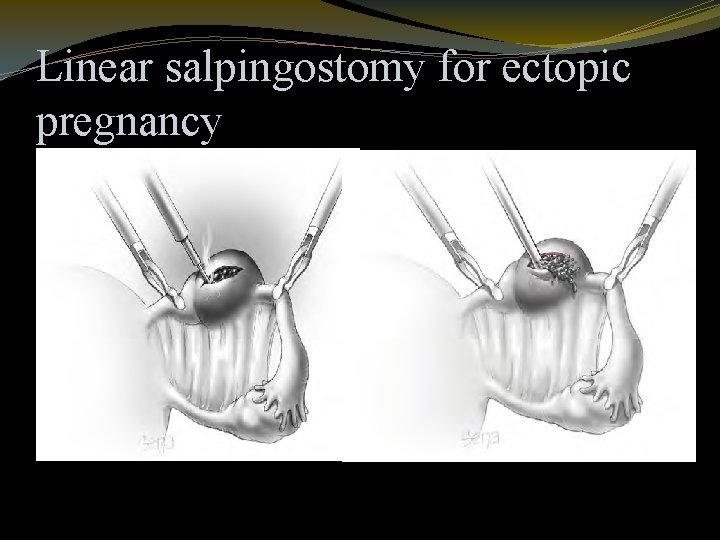
Salpingostomy. This procedure is used to remove a small pregnancy that is usually less than 2 cm in length and located in the distal third of the fallopian tube. A 10 - to 15 - mm linear incision is made with unipolar needle cautery on the antimesenteric border over the pregnancy. The products usually will extrude from the incision and can be carefully removed or flushed out using highpressure irrigation that more thoroughly removes the trophoblastic tissue
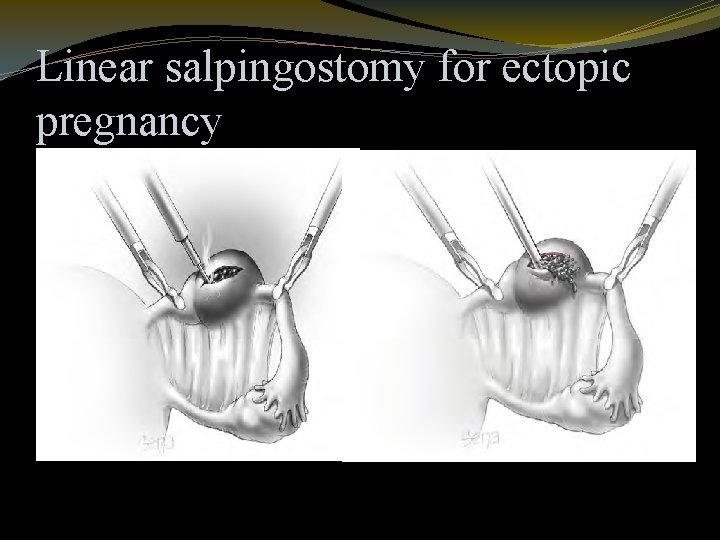
Linear salpingostomy for ectopic pregnancy
�Salpingotomy. Seldom performed today, salpingotomy is essentially the same procedure as salpingostomy except that the incision is closed with delayed-absorbable suture. .
�Salpingectomy. Tubal resection may be used for both ruptured and unruptured ectopic pregnancies. When removing the oviduct, it is advisable to excise a wedge of the outer third (or less) of the interstitial portion of the tube. This so-called cornual resection is done in an effort to minimize the rare recurrence of pregnancy in the tubal stump. Even with cornual resection, however, a subsequent interstitial pregnancy is not always prevented.
Persistent Trophoblast. Incomplete removal of trophoblast may result in persistent ectopic pregnancy. Because of this, administered a “prophylactic” 1 mg/m 2 dose of methotrexate postoperatively. Persistent trophoblast complicates 5 to 20 percent of salpingostomies and can be identified by persistent or rising h. CG levels. Usually h. CG levels fall quickly and are at about 10 percent of preoperative values by day 12. Also, if the postoperative day 1 serum - h. CG value is less than 50 percent of the preoperative value, then persistent trophoblast rarely is a problem
Medical Management with Methotrexate This folic acid antagonist is highly effective against rapidly proliferating trophoblast, and it has been used for more than 40 years to treat gestational trophoblastic disease
Selection criteria for conservative management of ectopic pregnancy 1. Minimal clinical symptoms 2. Certain ultrasound diagnosis of ectopic 3. No evidence of embryonic cardiac activity 4. Size <5 cm 5. No evidence of haematoperitoneum on ultrasound scan 6. Low serum h. CG (methotrexate <3000 IU/l; expectant 7. <1500 IU/l)
�The followin are resonable indications for methotrexate use � 1 -cornual pregnancy � 2 -Prsistant trophoblastic disorders � 3 - patient with one fallopian tubeand fertility desired. � 4 -patient who refuse surgery or whome surgery is risky � 5 -treatment of ectopic pregnancy where trophoblast is adherent to bowel or blood vessel
Contrindications of medical treatment � 1 - chronic liver, renal or haematological disordes � 2 - active infection � 3 -immunodeficency � 4 - breast feeding Side effect of methotrexate nausea. vomiting , stomatitis, cojuctivitis, GI upset, photosensitive skin reaction Abdominal pain Advise the women to take contraception for three months after methotreate. It is also important to avoid alcohol & exposure to sunlight during treatment
�Non-tubal ectopics Interstitial ectopics The implantation of the conceptus in the proximal portion of the Fallopian tube, which is within the muscularwall of the uterus, is called an interstitial pregnancy. The incidence of interstitial ectopic is 1 in 2500– 5000 live births and it accounts for 2– 6% of all ectopic pregnancies
Ruptured interstitial pregnancy usually presents dramatically with severe intra-abdominal bleeding, which requires urgent surgery. Haemostasis can usually be achieved by removing the pregnancy tissue and suturing the rupture site. However, in cases of extreme bleeding a cornual resection or in rare cases a hysterectomy may be necessary to arrest the bleeding.
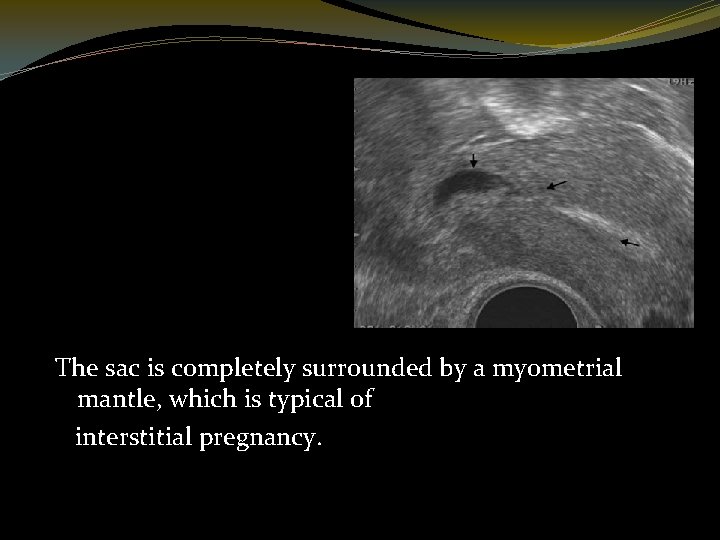
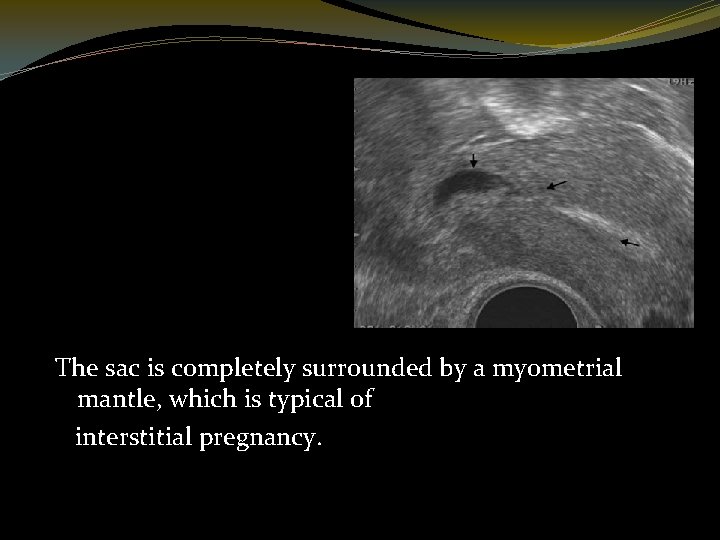
The sac is completely surrounded by a myometrial mantle, which is typical of interstitial pregnancy.
Pregnancies located below the internal os –cervical and Caesarean scar ectopics Cervical pregnancy is defined as the implantation of the conceptus within the cervix, below the level of the internal os. Caesarean scar pregnancy is a novel entity, which refers to a pregnancy implanted into a deficient uterine scar following previous lower segment Caesarean section
�An attempt to remove cervical or Caesarean section pregnancy is likely to cause severe vaginal bleeding and hysterectomy rates of 40% have been described when a D&C was attempted without pre-operative diagnosis of cervical pregnancy
�Ovarian pregnancy is defined as the implantation of the conceptus on the surface of the ovary or inside the ovary, away from the fallopian tubes. The diagnosis of ovarian pregnancy is rarely achieved pre-operatively; hence most women are treated surgically as the diagnosis is reached only at operation
Abdominal pregnancy is a rarity that only a few gynaecologists will encounter during their professional career. Most abdominal pregnancies are the result of reimplantation of ruptured undiagnosed tubal ectopic pregnancies. With the increasing accuracy of first-trimester transvaginal scanning it is likely the prevalence of advanced abdominal pregnancy will decrease even further in the future.
The clinical and ultrasound features of an early abdominal pregnancy are very similar to tubal ectopic pregnancies. However, viable abdominal pregnancies, which progress beyond the first trimester, are typically missed on routine transabdominal scanning. Abdominal pregnancy should be suspected in women with persistent abdominal pain later in pregnancy and in those who complain of painful fetal movements.
Treatment of abdominal pregnancy is surgical. In advanced abdominal pregnancies accompanied by normal fetal development diagnosed in the late second trimester termination of pregnancy may be delayed for a few weeks until the fetus reaches viability. At surgery the gestational sac should be opened carefully avoiding disruption of the placenta. The fetus should be removed, the cord cut short and the placenta should be left in situ.
Any attempt to remove the placenta may result in massive uncontrollable haemorrhage. Adjuvant treatment with methotrexate is not necessary and the residual placental tissue will absorb slowly over a period of many months, sometimes a few years. The placental tissue left in situ may become infected leading to the formation of a pelvic abscess, which may require drainage.