1 Nursing Management of Pregnancy At Risk Pregnancy









- Slides: 66

1 Nursing Management of Pregnancy At Risk: Pregnancy –Related Complications 11/27/2020
2 11/27/2020
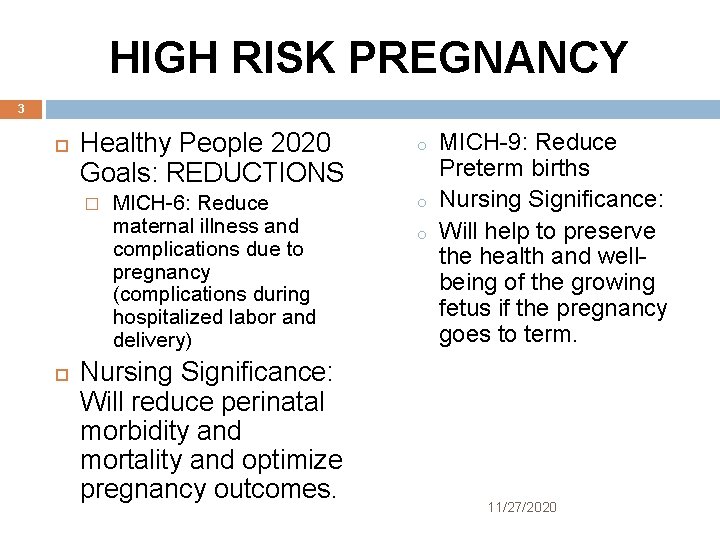
HIGH RISK PREGNANCY 3 Healthy People 2020 Goals: REDUCTIONS o MICH-6: Reduce maternal illness and complications due to pregnancy (complications during hospitalized labor and delivery) o � Nursing Significance: Will reduce perinatal morbidity and mortality and optimize pregnancy outcomes. o MICH-9: Reduce Preterm births Nursing Significance: Will help to preserve the health and wellbeing of the growing fetus if the pregnancy goes to term. 11/27/2020

MATERNAL DEATHS 4 The leading causes of maternal deaths during pregnancy are: � THROMBOEMBOLISM � HEMORRHAGE � INFECTION � HYPERTENSION OF PREGNANCY � ANESTHESIA RELATED COMPLICATIONS � ECTOPIC PREGNANCY � HEART DISEASE 11/27/2020
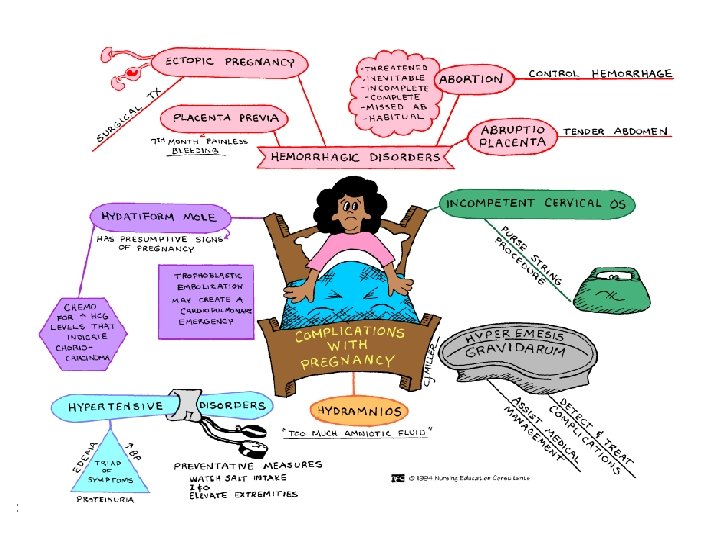
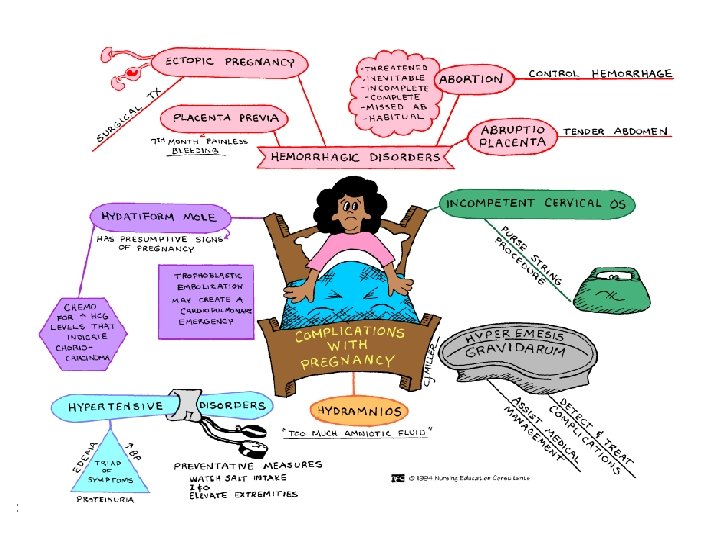
COMPLICATIONS OF BLEEDING 5 Vaginal Bleeding: deviation from normal that may occur at any time during pregnancy. REFER to table 19. 1 p. 629 1 st trimester: threatened, missed, incomplete, or complete abortion /miscarriage. Cause: Unknown, possible chromosomal or uterine abnormalities. 11/27/2020
PREGNANCY COMPLICATIONS 6 Abortion: is defined as any interruption of a pregnancy before the fetus is viable, whether done by medical or surgical means. Miscarriage: interruption of pregnancy that occurs spontaneously. Nonviable pregnancy: fetuses of 20 -24 weeks gestation or weighing 500 gms or less. 11/27/2020
COMPLICATIONS OF ABORTIONS 7 DIC HEMORRHAGE INFECTION (Endometritis) SEPTIC ABORTION ISOIMMUNIZATION 11/27/2020
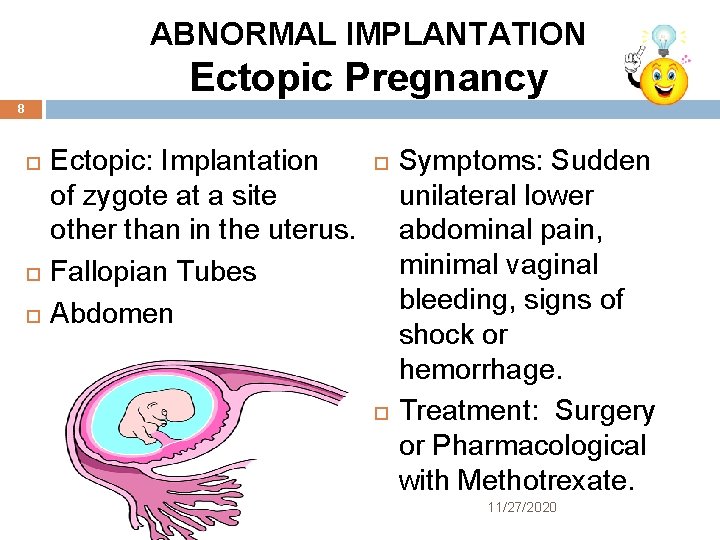
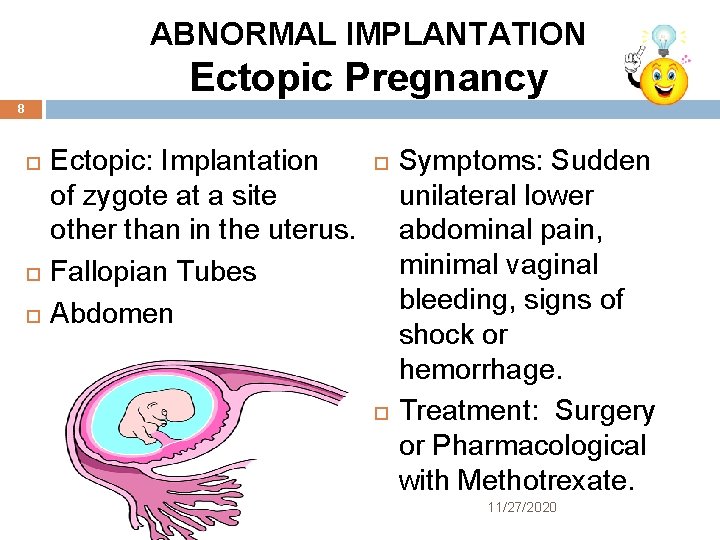
ABNORMAL IMPLANTATION Ectopic Pregnancy 8 Ectopic: Implantation of zygote at a site other than in the uterus. Fallopian Tubes Abdomen Symptoms: Sudden unilateral lower abdominal pain, minimal vaginal bleeding, signs of shock or hemorrhage. Treatment: Surgery or Pharmacological with Methotrexate. 11/27/2020
Ectopic 9 Nursing Assessment Health history and Physical exam. Laboratory � Vital Signs � Observe S/S of hypovolemic shock � Analgesics � Surgical Prep � Serum Beta-h. CG � CBC/Type & RH � Urinalysis Diagnostic testing � Transvaginal ultrasound Nursing Management: Preparation for treatment Emotional Support Education 11/27/2020
HYDATIDIFORM MOLE 10 Gestational Trophoblastic Disease (GTD): Abnormal proliferation of trophoblast tissue; fertilization or division defect Partial (rarely cancerous) Complete(associated with Choriocarcinoma. Assessment: Overgrowth of uterus, highly positive HCG test, no fetus present, bleeding, cyst formation. Treatment: D&C, HCG weekly until non -detectable (3 weeks) then levels monthly for 12 months. Chest x-ray q 6 months, regular pelvic exams 11/27/2020
PREGNANCY: MORBIDITY & MORTALITY DATA 11 11/27/2020

GTD 12 Nursing Assessment S/S pregnancy Discharge Anemia No fetal heart Ovarian enlargement Severe morning sickness Fluid retention/swelling Enlarged uterine size h. CG levels greatly increased Early development of preeclampsia Expulsion of grapelike vesicles Nursing Management Preparing the client � Providing Emotional Support � � � Surgical Intervention Pregnancy loss Potential Life Threatening condition Spiritual/Cultural Care Educating the Client � � Simple explanations regarding cause of GTD Follow-up care including h. CG levels weekly, need to prevent pregnancy for more than 1 year, contraceptive methods. 11/27/2020
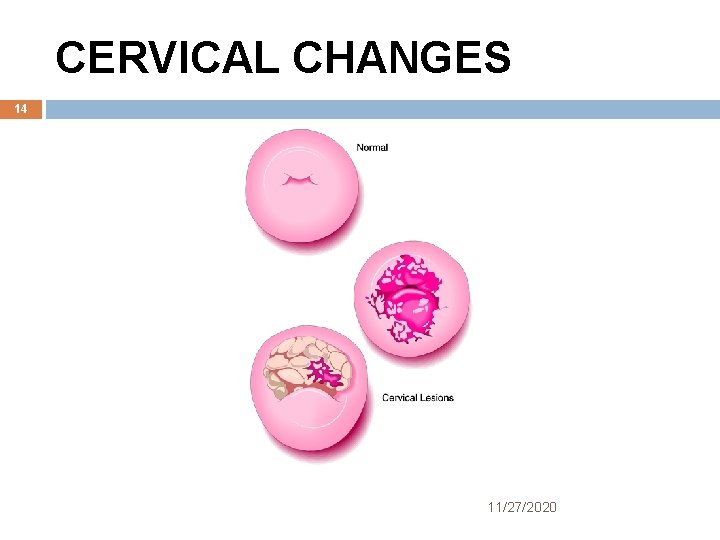
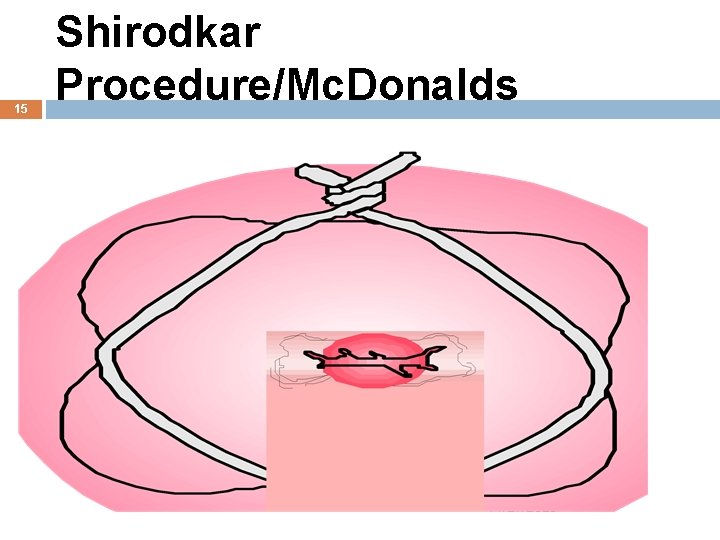
PREMATURE CERVICAL DILATATION 13 Cervical Insufficiency: Cervix that dilates prematurely and therefore, cannot hold a fetus until term. Pregnancy loss usually occurs at 20 wks gestation. Cause generally unknown, but may be related to cervical trauma. Nursing Assessment: H/O Painless bleeding leading to expulsion of fetus, cervical damage, previous loss of pregnancy around 20 wks gestation, vaginal discharge Treatment: Cerclage: sutures inserted into the cervix (Mc. Donald procedure). Or Shirodkar normally performed at 12 -14 wks gestation 11/27/2020
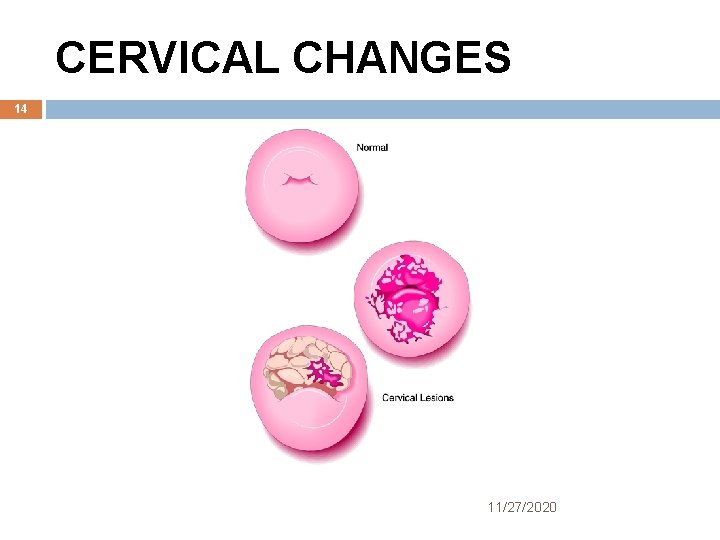
CERVICAL CHANGES 14 11/27/2020
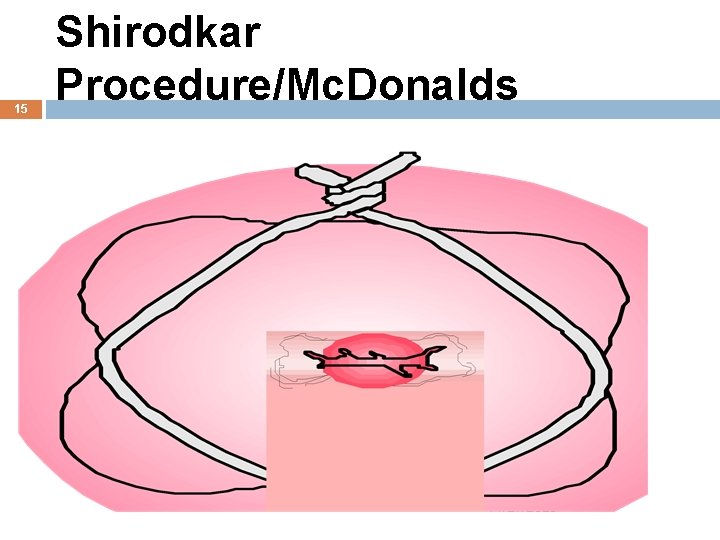
15 Shirodkar Procedure/Mc. Donalds 11/27/2020
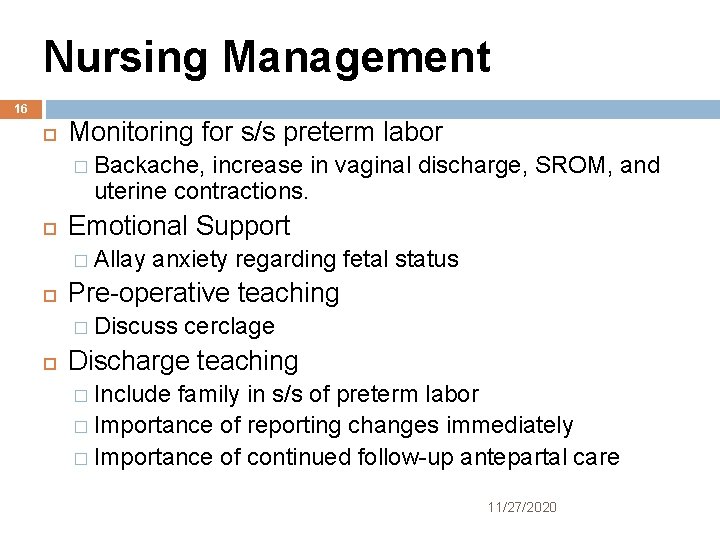
Nursing Management 16 Monitoring for s/s preterm labor � Backache, increase in vaginal discharge, SROM, and uterine contractions. Emotional Support � Allay anxiety regarding fetal status Pre-operative teaching � Discuss cerclage Discharge teaching � Include family in s/s of preterm labor � Importance of reporting changes immediately � Importance of continued follow-up antepartal care 11/27/2020
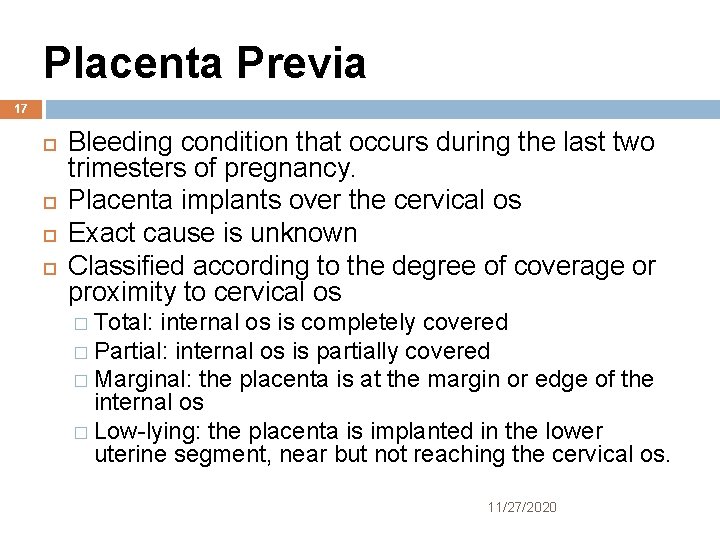
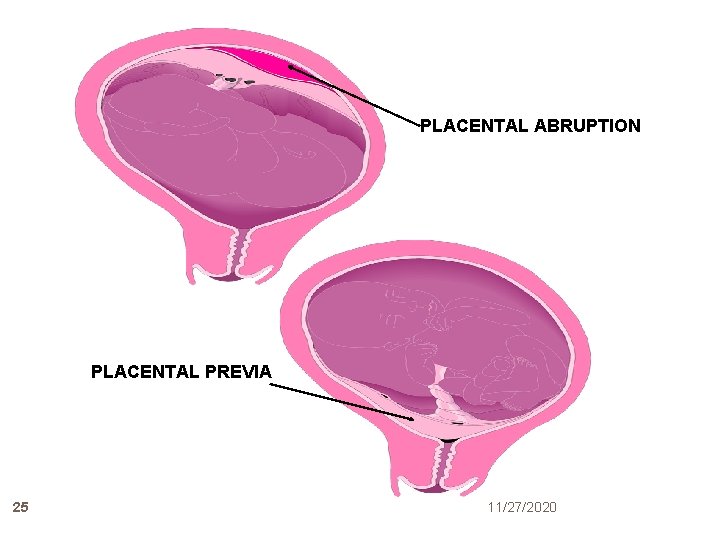
Placenta Previa 17 Bleeding condition that occurs during the last two trimesters of pregnancy. Placenta implants over the cervical os Exact cause is unknown Classified according to the degree of coverage or proximity to cervical os � Total: internal os is completely covered � Partial: internal os is partially covered � Marginal: the placenta is at the margin or edge of the internal os � Low-lying: the placenta is implanted in the lower uterine segment, near but not reaching the cervical os. 11/27/2020
PLACENTAL ABNORMALITIES 18 Frequently associated with: Increased parity � Advanced maternal age � Past cesarean births � Past uterine curettage � Multiple gestation � Cocaine use � Prior previa � Smoking � Infertility treatment � 11/27/2020
PREVIA ASSESSMENT 19 Painless bleeding � Duration � Amount � Presence detect fetal blood in maternal circulation) of pain � Previous bleeds � Fetal Heart Rate Management: Diagnostic ultrasound Kleihauer Betke test (used to Bed Rest No Vaginal Exams Administer Betamethasone (Celestone) 12 mg IM stat and repeated in 24 hrs. and 1 -2 wks. Rhig Workup Cesarean Birth 11/27/2020

Nursing Management 20 Thorough history and physical VS FHR/Contractions Laboratory Support Education 11/27/2020
ABRUPTIO PLACENTA 21 Premature separation of placenta � Partial � Complete Causes: Unknown, associated with hypertension, high parity, short cord, PIH, trauma, drugs and cigarettes. Assessment: � Sharp abdominal pain � uterine tenderness � Vaginal Bleeding � Couvelaire Uterus (concealed hemorrhage) � Maternal shock � Fetal distress � DIC 11/27/2020
ABRUPTIO MANAGEMENT/Obstetrical 22 Emergency Vital Signs Fetal Heart Rate Routine Labs DIC workup IV Therapy Vaginal Delivery or Cesarean Section 11/27/2020
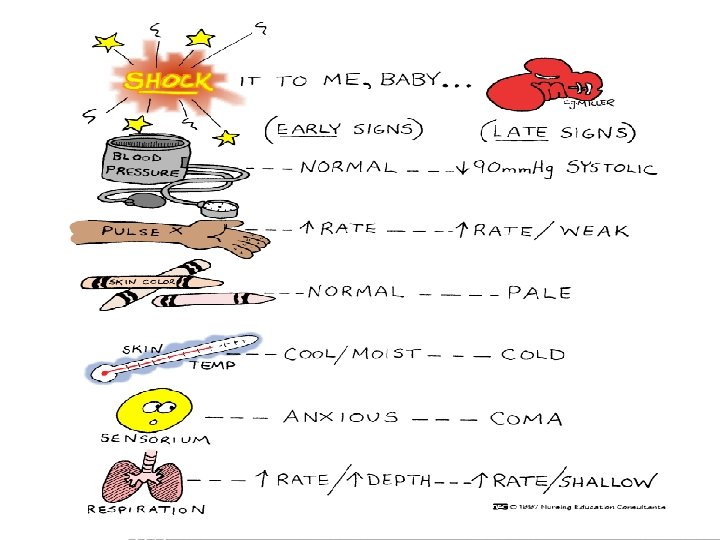
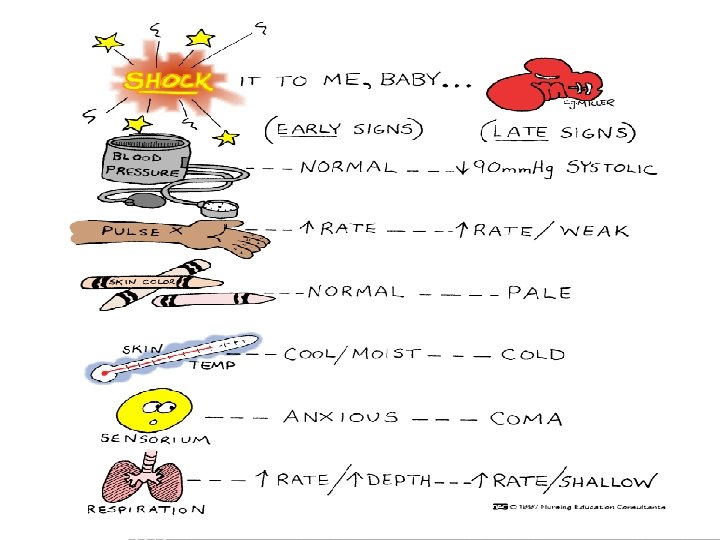
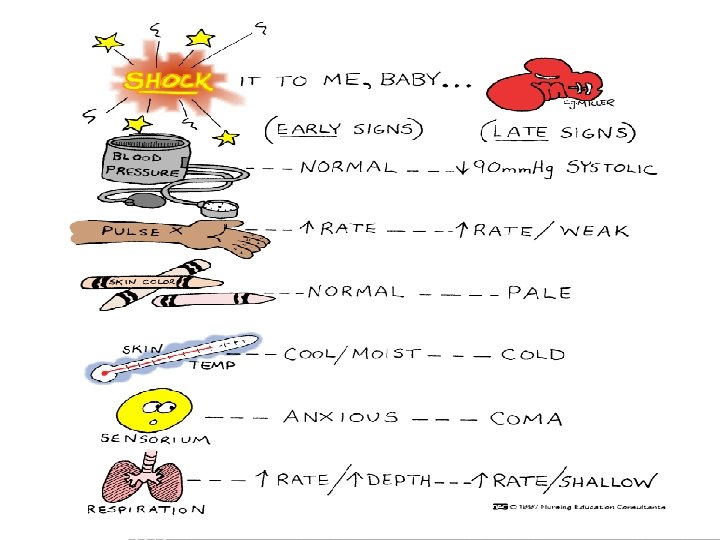
Nursing Management 23 Ensuring adequate tissue perfusion � VS, pulse ox, FHR, Contractions � IV therapy � Strict bed rest � Left lateral position (to prevent vena cava compression) � Oxygen therapy � Indwelling foley cath � Observe for hypovolemic shock, DIC Support and Education 11/27/2020
24 11/27/2020
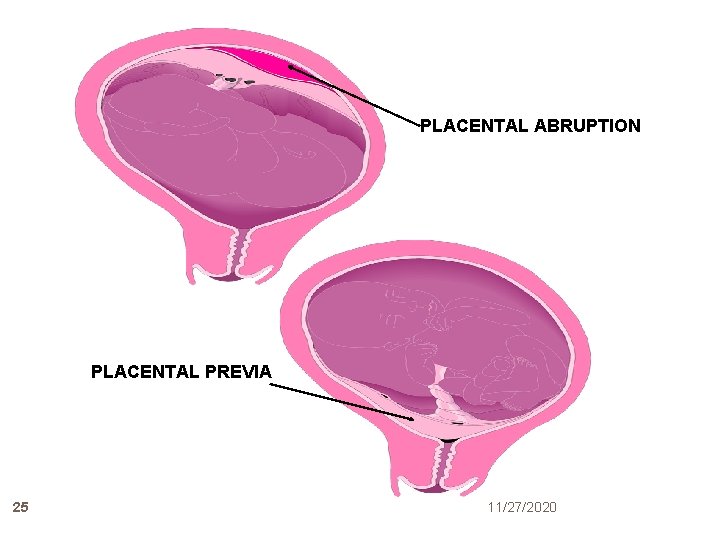
PLACENTAL ABRUPTION PLACENTAL PREVIA 25 11/27/2020
Placenta Accreta 26 Condition in which the placenta attaches itself too deeply into the wall of the uterus but does not penetrate the uterine muscle. Diagnosed after birth when placenta does not separate from the uterine wall. 11/27/2020
Hyperemesis Gravidarum 27 Occurs in 5 out of 1000 pregnancies Defined as persistent vomiting unresponsive to outpatient treatment and is severe enough to cause weight loss and disturbed nutritional status. Related to increasing level of h. CG. Lasts beyond 12 weeks gestation. 11/27/2020
Symptoms Hyperemesis 28 Electrolyte imbalance Dehydration Weight loss Acidosis Alkalosis Ketonuria Hypokalemia 11/27/2020
Therapeutic Management 29 Dietary and lifestyle alterations Hospitalization/ NPO status (24 -36 hours) Oral nutritional supplementation Pharmacologic preparations � Promethazine (Phenergan) � Prochlorperazine (Compazine) � Ondansetron (Zofran) IV vitamin-mineral therapy Parenteral nutrition Enteral tube feedings Supportive psychotherapy 11/27/2020
Nursing Management 30 Health History and Physical Examination Review of antepartal record Lab testing review (LFT’s, CBC, BUN, serum electrolytes, urinalysis, urine specific gravity, ketones, and ultrasound results) Promote Comfort and Nutrition Support and Education 11/27/2020
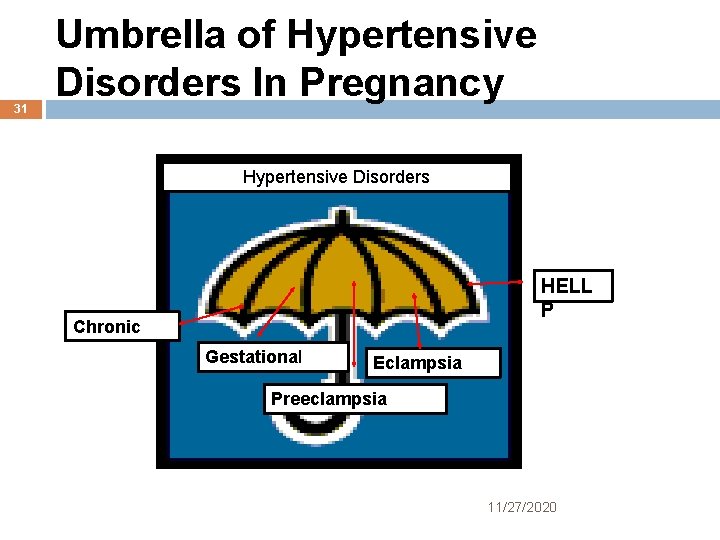
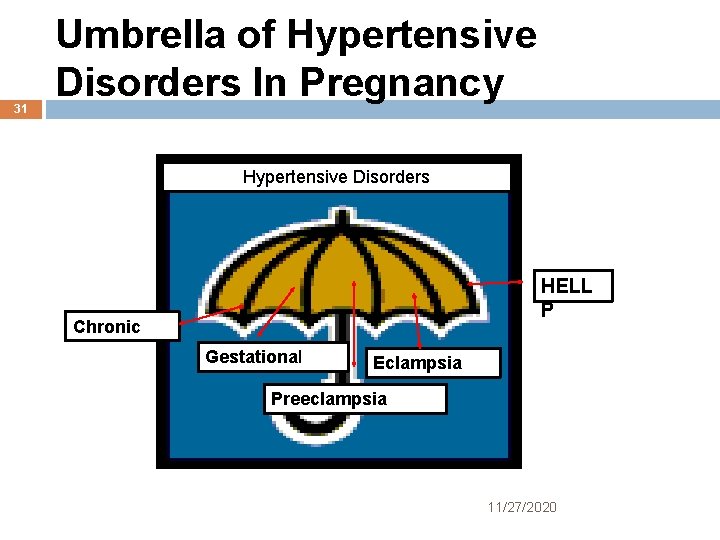
31 Umbrella of Hypertensive Disorders In Pregnancy Hypertensive Disorders HELL P Chronic Gestational Eclampsia Preeclampsia 11/27/2020
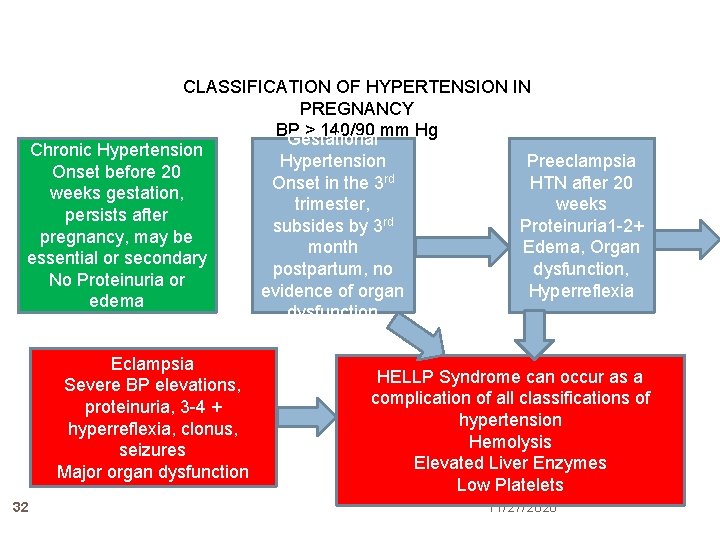
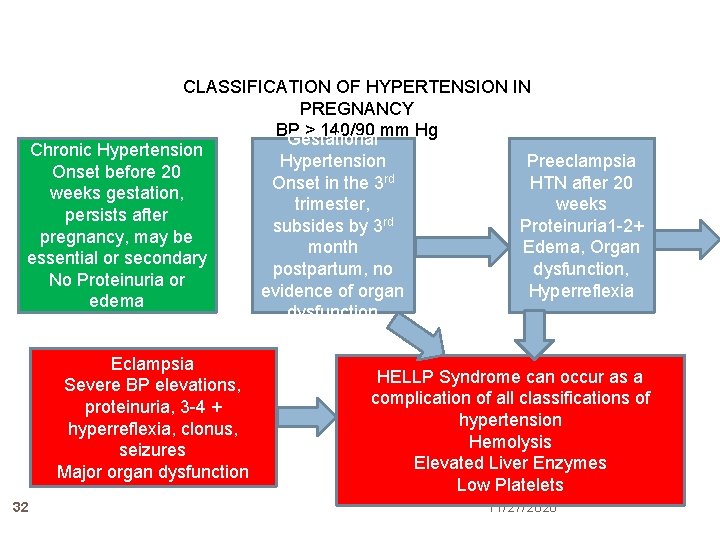
CLASSIFICATION OF HYPERTENSION IN PREGNANCY BP > 140/90 mm Hg Gestational Chronic Hypertension Preeclampsia Hypertension Onset before 20 HTN after 20 Onset in the 3 rd weeks gestation, weeks trimester, persists after Proteinuria 1 -2+ subsides by 3 rd pregnancy, may be Edema, Organ month essential or secondary dysfunction, postpartum, no No Proteinuria or evidence of organ Hyperreflexia edema dysfunction Eclampsia Severe BP elevations, proteinuria, 3 -4 + hyperreflexia, clonus, seizures Major organ dysfunction 32 HELLP Syndrome can occur as a complication of all classifications of hypertension Hemolysis Elevated Liver Enzymes Low Platelets 11/27/2020

Chronic Hypertension 33 Existence of high BP prior to pregnancy or before the 20 th week of gestation Persists beyond 12 weeks postpartum Preconception counseling 11/27/2020 Antihypertensive agents reserved for severe hypertension Systolic > 160 mm. Hg or Diastolic >100 mm/Hg Medication Therapy: Methyldopa (Aldomet) Labetalol (Transdate) Atenolol (Tenormin) Nifedipine (Procardia) 11/27/2020 33
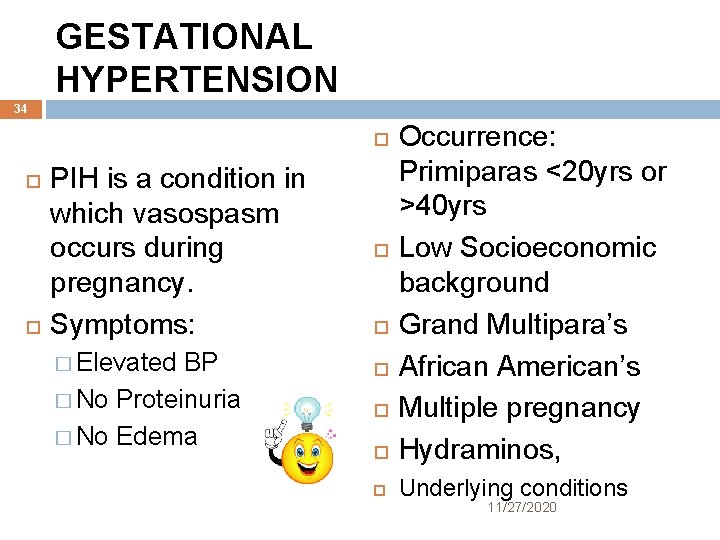
GESTATIONAL HYPERTENSION 34 Occurrence: Primiparas <20 yrs or >40 yrs Low Socioeconomic background Grand Multipara’s African American’s Multiple pregnancy Hydraminos, Underlying conditions PIH is a condition in which vasospasm occurs during pregnancy. Symptoms: � Elevated BP � No Proteinuria � No Edema 11/27/2020
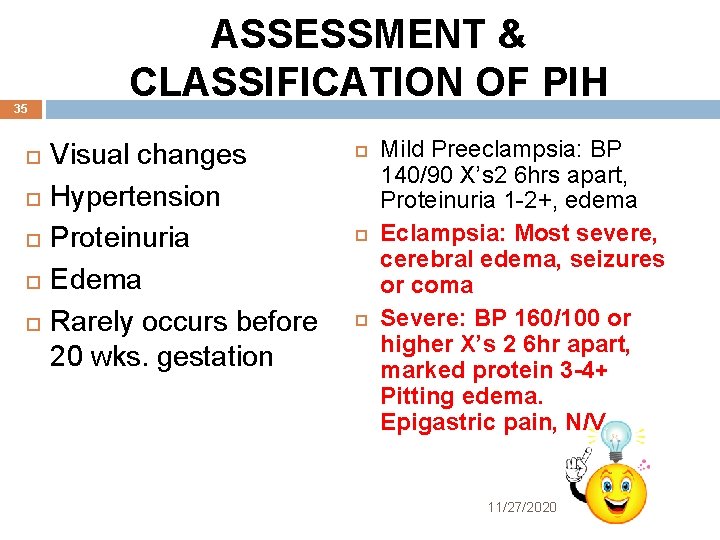
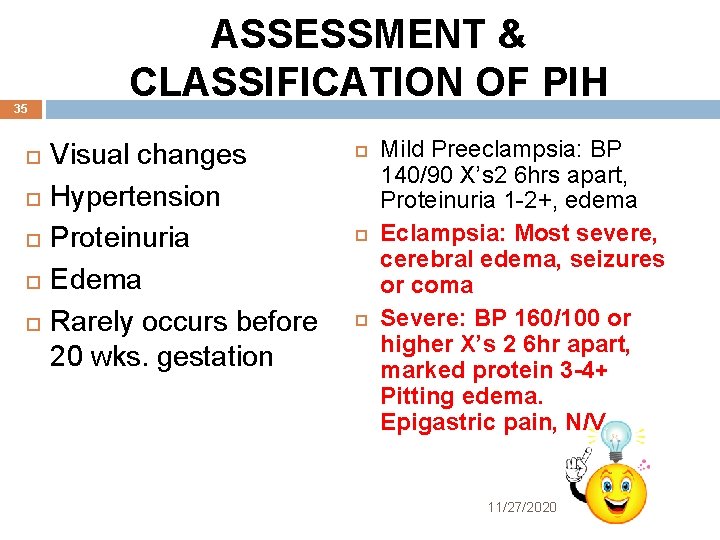
35 ASSESSMENT & CLASSIFICATION OF PIH Visual changes Hypertension Proteinuria Edema Rarely occurs before 20 wks. gestation Mild Preeclampsia: BP 140/90 X’s 2 6 hrs apart, Proteinuria 1 -2+, edema Eclampsia: Most severe, cerebral edema, seizures or coma Severe: BP 160/100 or higher X’s 2 6 hr apart, marked protein 3 -4+ Pitting edema. Epigastric pain, N/V 11/27/2020
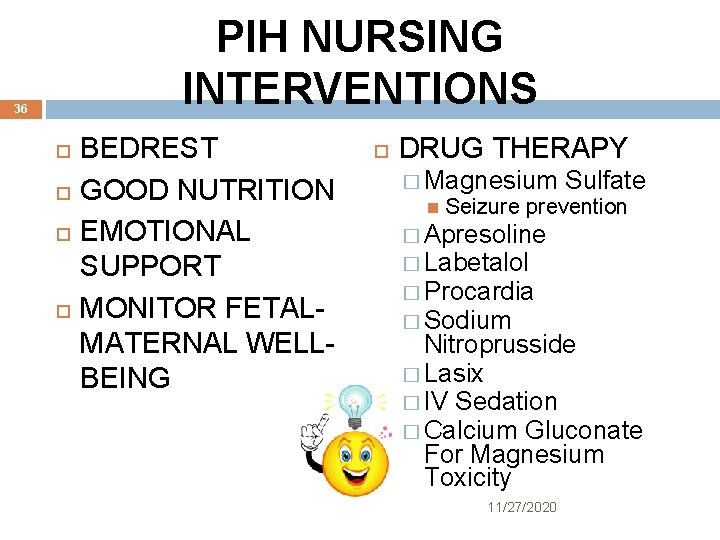
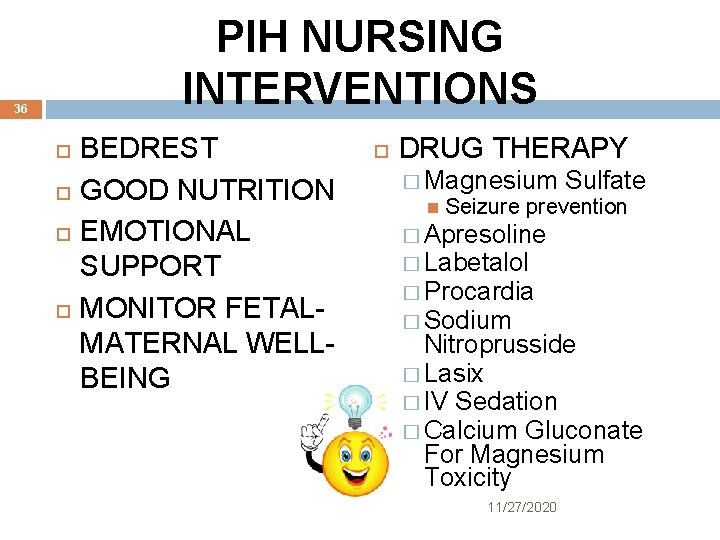
PIH NURSING INTERVENTIONS 36 BEDREST GOOD NUTRITION EMOTIONAL SUPPORT MONITOR FETALMATERNAL WELLBEING DRUG THERAPY � Magnesium Sulfate Seizure prevention � Apresoline � Labetalol � Procardia � Sodium Nitroprusside � Lasix � IV Sedation � Calcium Gluconate For Magnesium Toxicity 11/27/2020
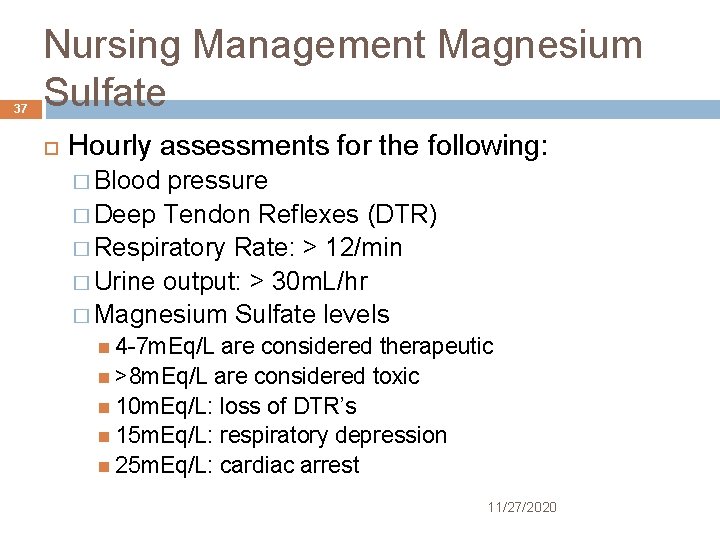
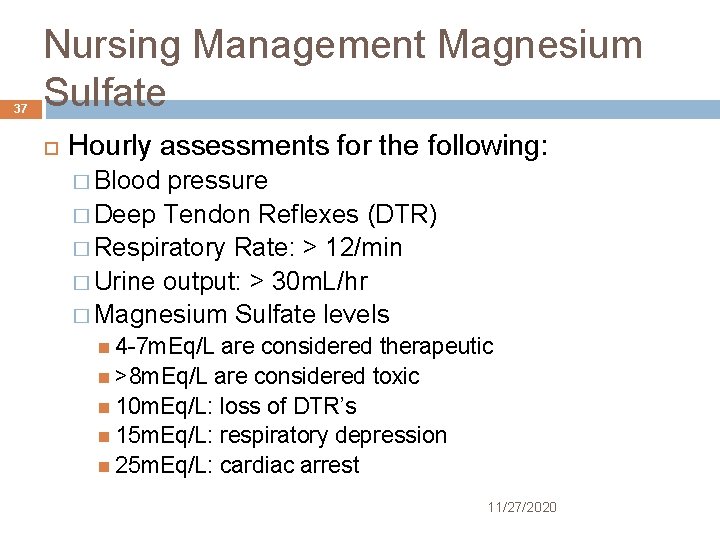
37 Nursing Management Magnesium Sulfate Hourly assessments for the following: � Blood pressure � Deep Tendon Reflexes (DTR) � Respiratory Rate: > 12/min � Urine output: > 30 m. L/hr � Magnesium Sulfate levels 4 -7 m. Eq/L are considered therapeutic >8 m. Eq/L are considered toxic 10 m. Eq/L: loss of DTR’s 15 m. Eq/L: respiratory depression 25 m. Eq/L: cardiac arrest 11/27/2020
38 11/27/2020
HELLP SYNDROME 39 A variation of PIH named for the common symptoms that occur. H-Hemolysis E-Elevated Liver Enzymes L-Low Platelets Maternal Mortality 24% Infant Mortality 35% 11/27/2020
40 11/27/2020
HELLP SYMPTOMS 41 Nausea Epigastric Pain General Malaise Right Upper Quadrant tenderness. Lab Values: � RBC’s- Thrombocytopenia, platelet count <100, 000 � Elevated liver enzymes: ALT/AST 11/27/2020
TREATMENT OF HELLP 42 SUPPORTATIVE THERAPY � Vital Signs � Maternal/Fetal Assessments DELIVERY OF FETUS � Vaginal � Cesarean Section TRANSFUSIONS OF: � Fresh Frozen Plasma � Platelets 11/27/2020
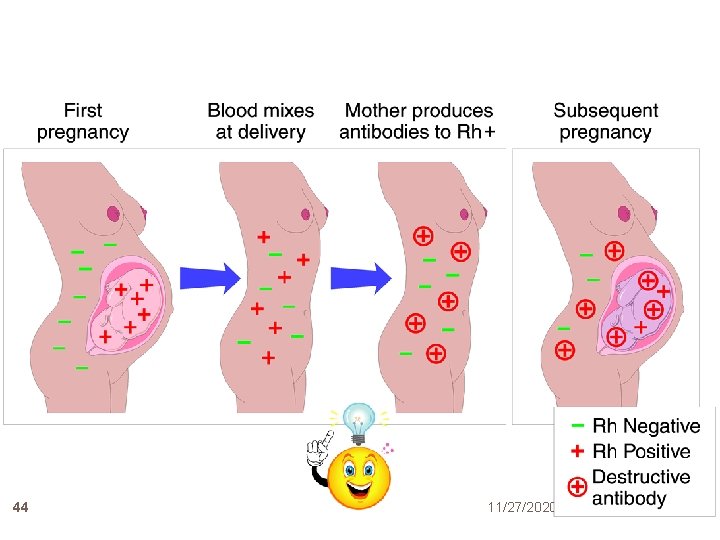
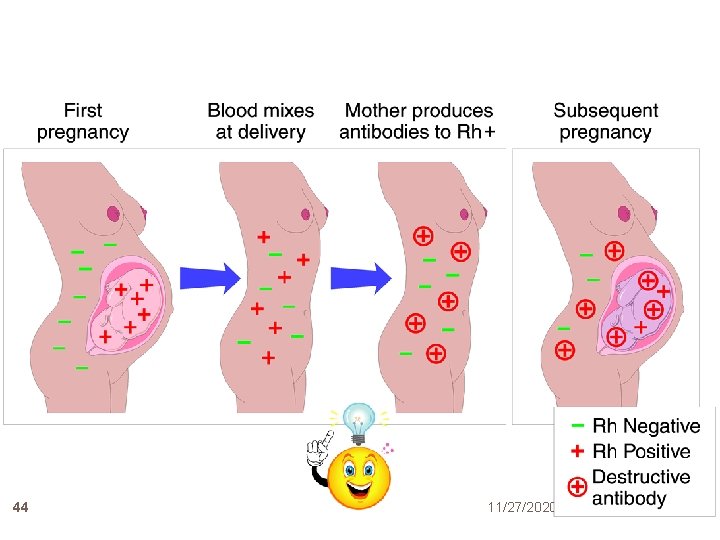
ISOIMMUNIZATION 43 Rh Incompatibility- a blood incompatibility between mother and fetus. Only the fetus is affected. A mixing of maternal and fetal blood. Usually only affects 2 nd or greater pregnancies. Causes: � Amniocentesis � Percutaneous Umbilical Blood sampling � Placental separation 11/27/2020
44 11/27/2020
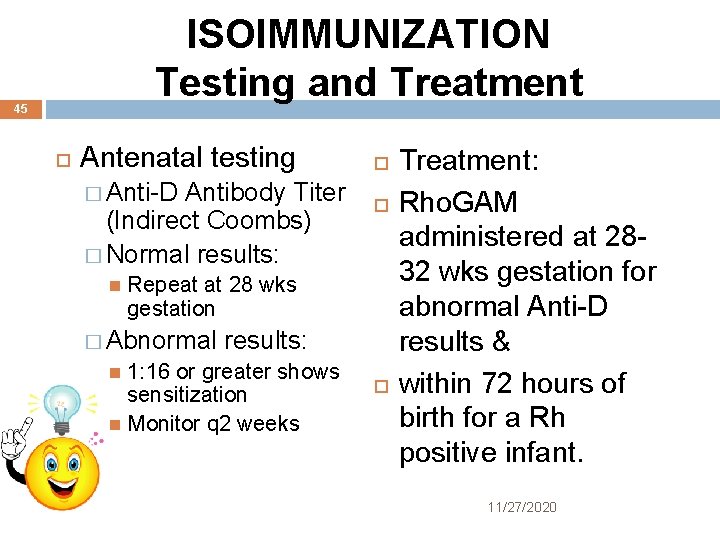
ISOIMMUNIZATION Testing and Treatment 45 Antenatal testing � Anti-D Antibody Titer (Indirect Coombs) � Normal results: Repeat at 28 wks gestation � Abnormal results: 1: 16 or greater shows sensitization Monitor q 2 weeks Treatment: Rho. GAM administered at 2832 wks gestation for abnormal Anti-D results & within 72 hours of birth for a Rh positive infant. 11/27/2020
ABO INCOMPATIBILITY 46 Occurs in 20 to 25% of pregnancies Rarely causes significant hemolysis Type 0 Mother with a type A or B fetus Incompatibility results from the interaction of antibodies present in maternal serum and the antigen sites on the fetal RBC’s No Antepartal treatment necessary Newborn can develop hyperbilirubinemia 11/27/2020

Amniotic fluid Imbalances 47 Amniotic fluid develops from several maternal and fetal structures, including the amnion, chorion, maternal blood, fetal lungs, GI tract, kidneys and skin. Hydraminos (Polyhydraminos) � Excessive Oligohydramnios � Decreased 11/27/2020
HYDRAMINOS 48 Excessive amniotic fluid formation. � Normal: 500 -1000 ml at term � Abnormal: > 2000 ml at term � Amniotic Fluid Index: AFI >24 cm 11/27/2020
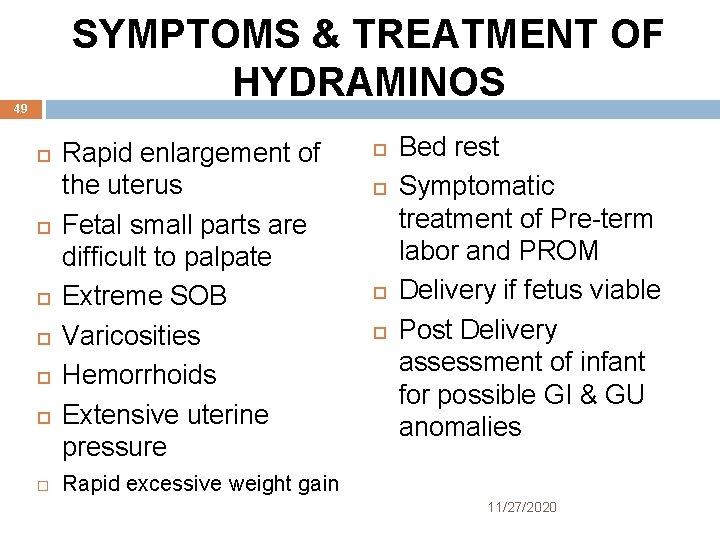
SYMPTOMS & TREATMENT OF HYDRAMINOS 49 Rapid enlargement of the uterus Fetal small parts are difficult to palpate Extreme SOB Varicosities Hemorrhoids Extensive uterine pressure Bed rest Symptomatic treatment of Pre-term labor and PROM Delivery if fetus viable Post Delivery assessment of infant for possible GI & GU anomalies Rapid excessive weight gain 11/27/2020

Complications of Hydramnios 50 Fetal Malpresentation Premature ROM Preterm Labor Fetal anomalies � Anencephaly � Tracheoesophageal Fistula with stenosis � Intestinal obstruction � Hyperglycemia in fetus 11/27/2020
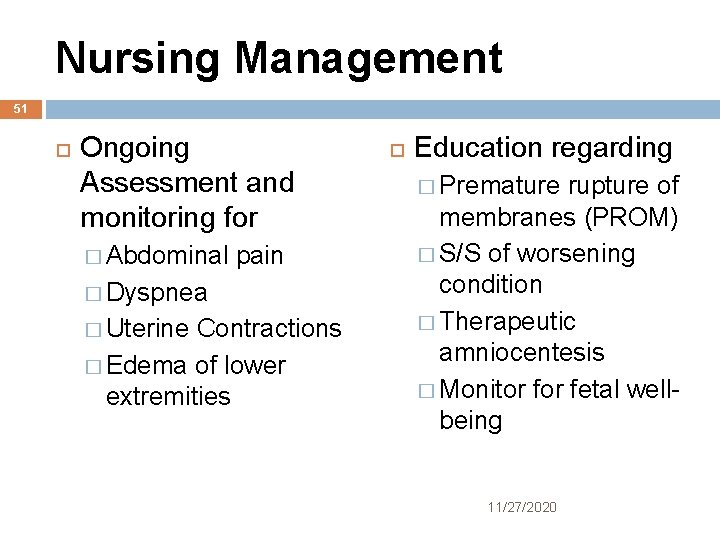
Nursing Management 51 Ongoing Assessment and monitoring for � Abdominal pain � Dyspnea � Uterine Contractions � Edema of lower extremities Education regarding � Premature rupture of membranes (PROM) � S/S of worsening condition � Therapeutic amniocentesis � Monitor fetal wellbeing 11/27/2020
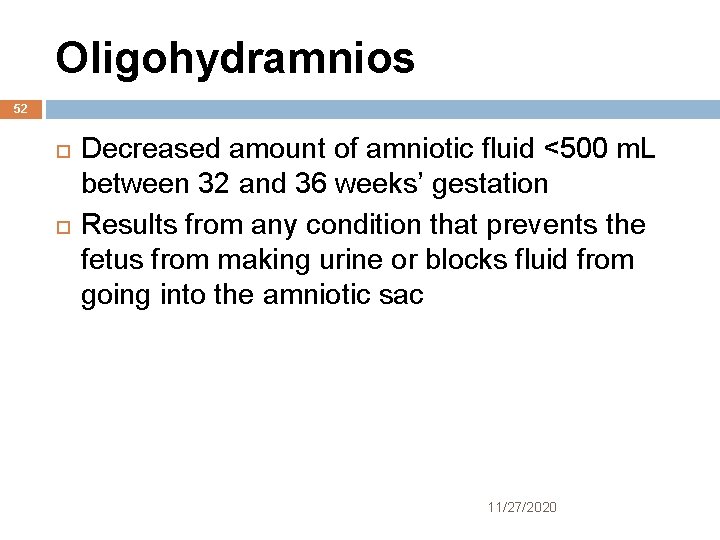
Oligohydramnios 52 Decreased amount of amniotic fluid <500 m. L between 32 and 36 weeks’ gestation Results from any condition that prevents the fetus from making urine or blocks fluid from going into the amniotic sac 11/27/2020
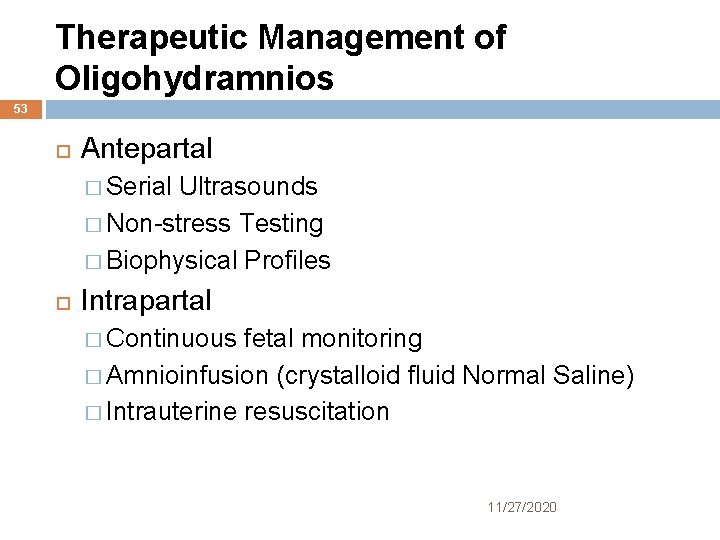
Therapeutic Management of Oligohydramnios 53 Antepartal � Serial Ultrasounds � Non-stress Testing � Biophysical Profiles Intrapartal � Continuous fetal monitoring � Amnioinfusion (crystalloid fluid Normal Saline) � Intrauterine resuscitation 11/27/2020
Nursing Assessment/Management 54 Uteroplacental Insufficiency PROM HTN of Pregnancy Gestational Diabetes IUGR Post-Term Pregnancy Fetal Renal Agenesis Polycystic Kidneys Fetal Urinary Tract Obstructions Continuous monitoring for fetal well-being Non-stress Testing Intrapartum: presence of variable decelerations indicating cord compression Amnioinfusion Comfort measures 11/27/2020
MULTIPLE GESTATIONS 55 Woman’s body must adjust to the effects of more than one fetus. Twinning – 12 per 1000 births Triplets - 1 in 6400 births 4, 5, 6, 7 - Fetus’s may be single ovum conception, multiple ova conception or a combination of both 11/27/2020
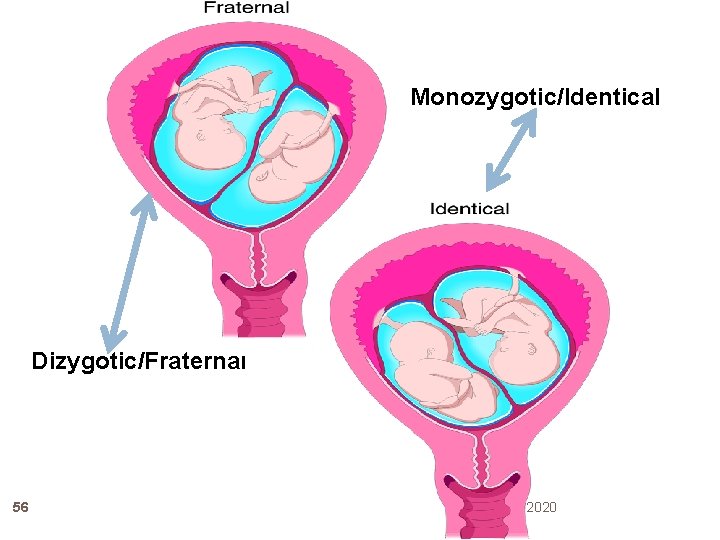
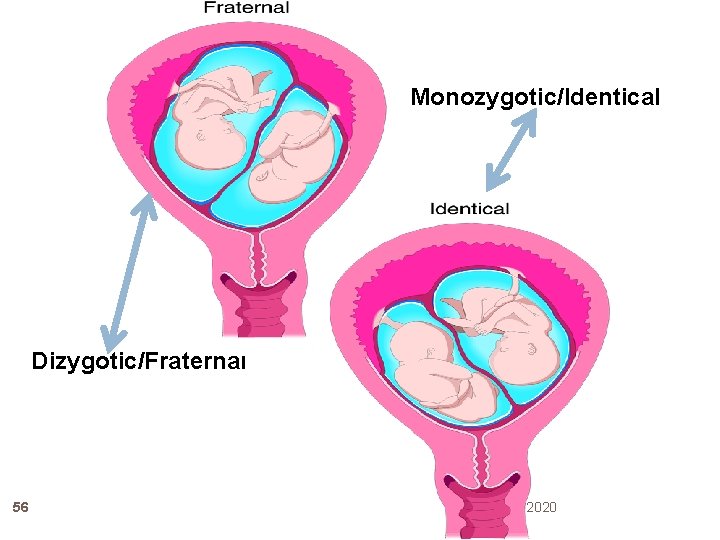
Monozygotic/Identical Dizygotic/Fraternal 56 11/27/2020
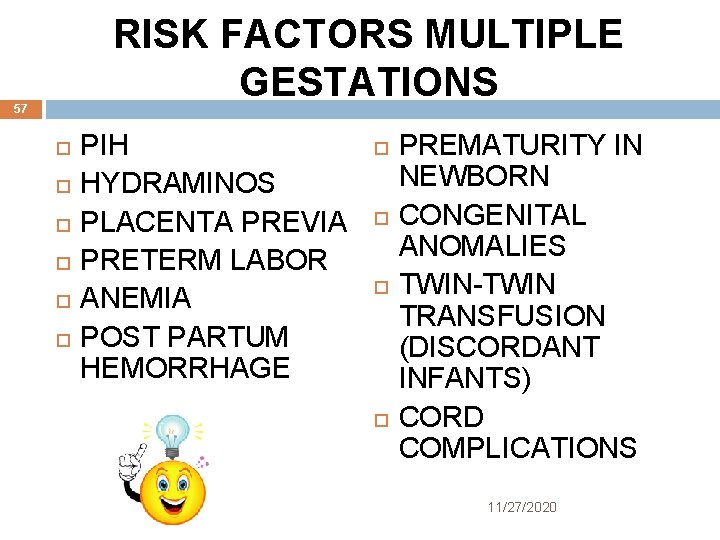
RISK FACTORS MULTIPLE GESTATIONS 57 PIH HYDRAMINOS PLACENTA PREVIA PRETERM LABOR ANEMIA POST PARTUM HEMORRHAGE PREMATURITY IN NEWBORN CONGENITAL ANOMALIES TWIN-TWIN TRANSFUSION (DISCORDANT INFANTS) CORD COMPLICATIONS 11/27/2020
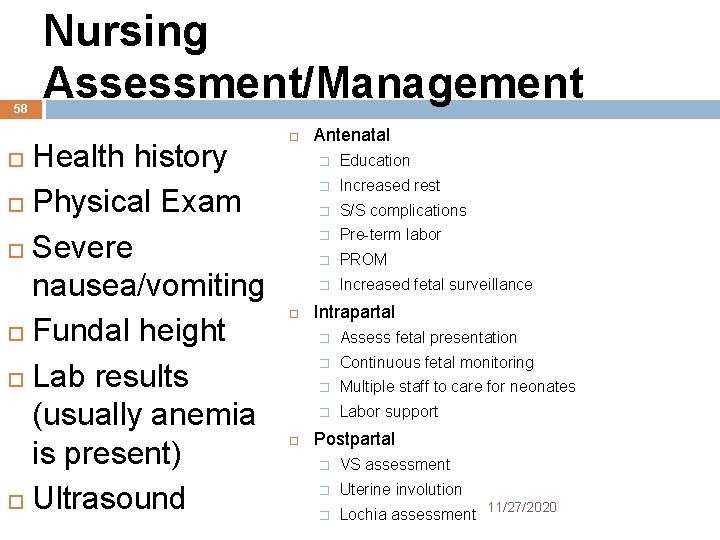
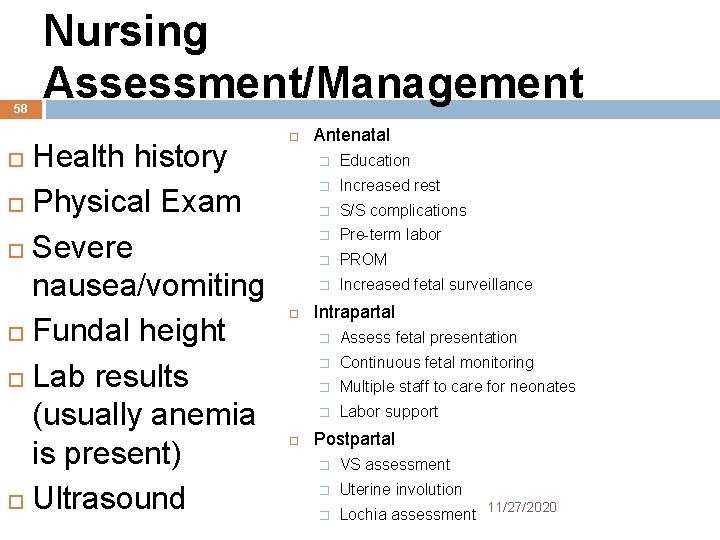
58 Nursing Assessment/Management Health history Physical Exam Severe nausea/vomiting Fundal height Lab results (usually anemia is present) Ultrasound Antenatal � Education � Increased rest � S/S complications � Pre-term labor � PROM � Increased fetal surveillance Intrapartal � Assess fetal presentation � Continuous fetal monitoring � Multiple staff to care for neonates � Labor support Postpartal � VS assessment � Uterine involution � Lochia assessment 11/27/2020
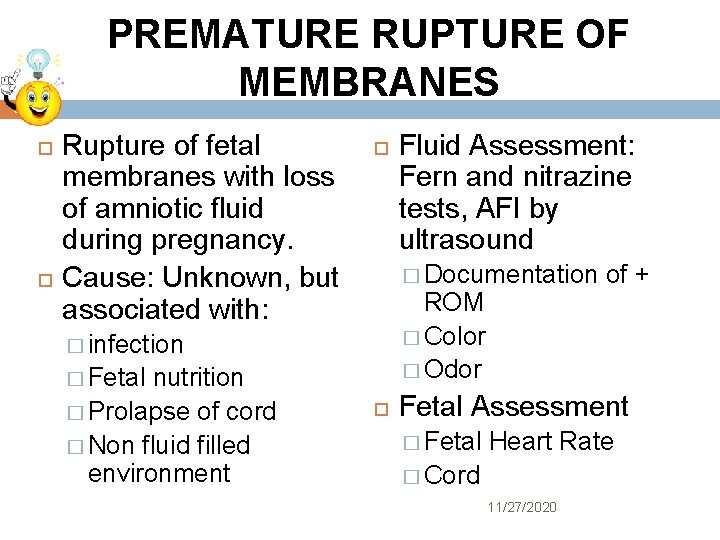
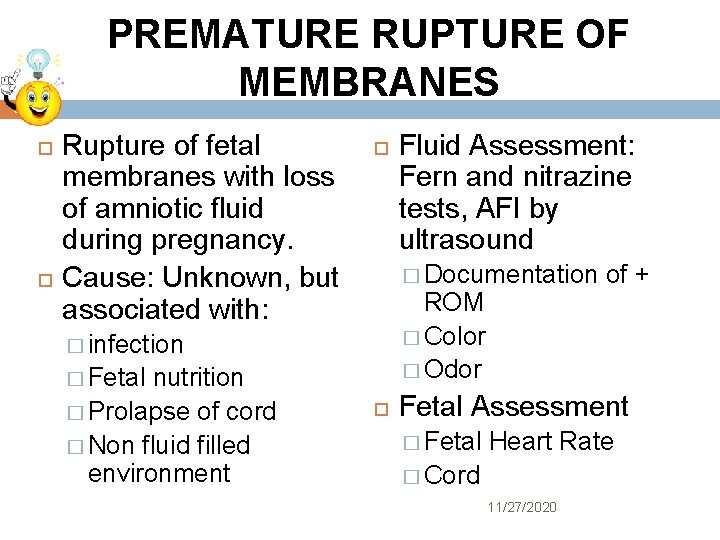
PREMATURE RUPTURE OF MEMBRANES 59 Rupture of fetal membranes with loss of amniotic fluid during pregnancy. Cause: Unknown, but associated with: � Documentation ROM � Color � Odor � infection nutrition � Prolapse of cord � Non fluid filled environment Fluid Assessment: Fern and nitrazine tests, AFI by ultrasound � Fetal of + Fetal Assessment � Fetal Heart Rate � Cord 11/27/2020
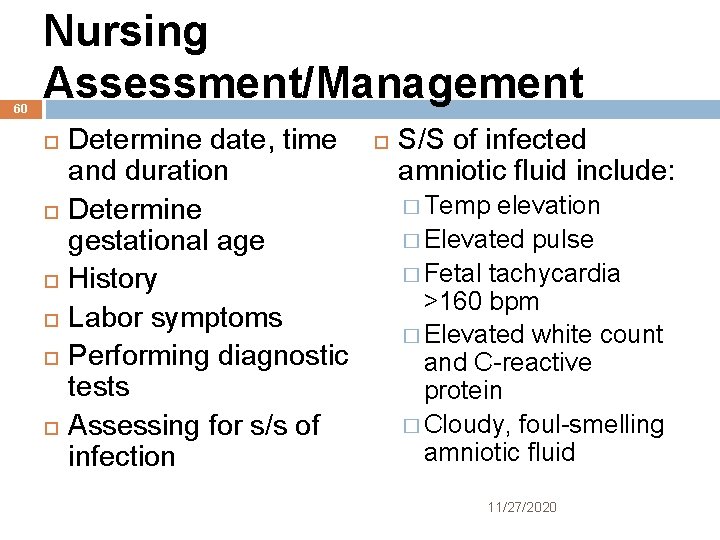
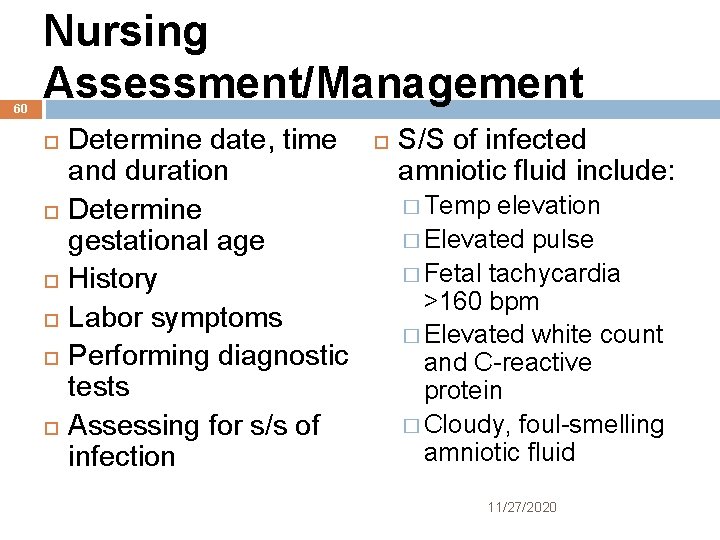
60 Nursing Assessment/Management Determine date, time and duration Determine gestational age History Labor symptoms Performing diagnostic tests Assessing for s/s of infection S/S of infected amniotic fluid include: � Temp elevation � Elevated pulse � Fetal tachycardia >160 bpm � Elevated white count and C-reactive protein � Cloudy, foul-smelling amniotic fluid 11/27/2020
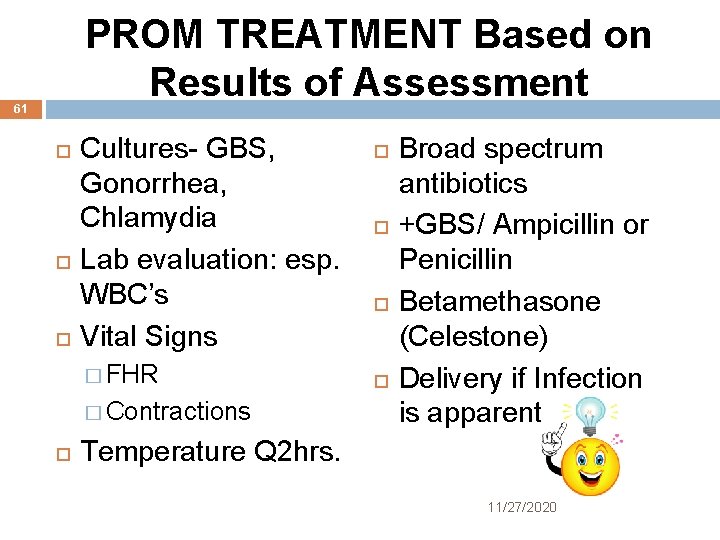
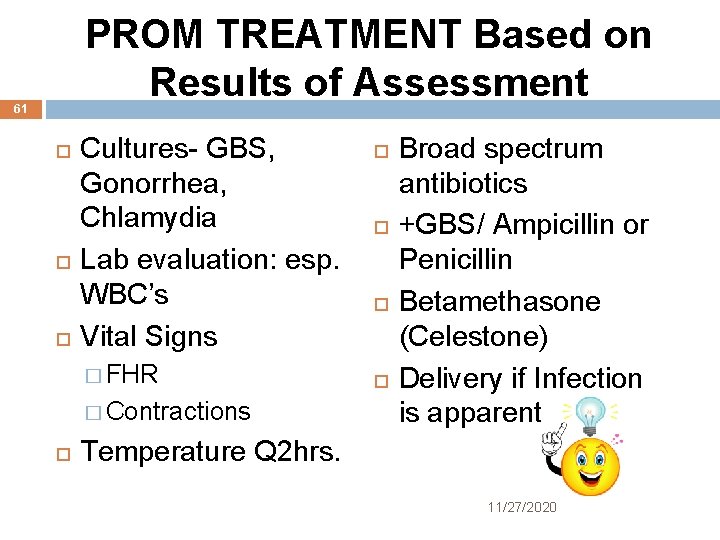
PROM TREATMENT Based on Results of Assessment 61 Cultures- GBS, Gonorrhea, Chlamydia Lab evaluation: esp. WBC’s Vital Signs � FHR � Contractions Broad spectrum antibiotics +GBS/ Ampicillin or Penicillin Betamethasone (Celestone) Delivery if Infection is apparent Temperature Q 2 hrs. 11/27/2020

Questions 62 CLICKERS PLEASE!!! 11/27/2020
A patient, 32 weeks pregnant with severe headache, is admitted to the hospital with preeclampsia. In addition to obtaining baseline vital signs and placing the client on bed rest, the physician ordered the following items. Which of the orders should the nurse perform first? A. Assess deep tendon reflexes B. Obtain complete blood count C. Assess baseline weight D. Obtain routine urinalysis 63 11/27/2020
A woman at 26 -weeks-gestation is diagnosed with severe preeclampsia with HELLP syndrome. The nurse will assess for which of the following signs/symptoms? A. Low serum creatinine B. High serum protein C. Bloody stools D. Epigastric pain 64 11/27/2020
Which of the following findings should the nurse expect when assessing a client, 8 weeks’ gestation with a gestational trophoblastic disease (hydatiform mole)? A. Protracted pain B. Variable fetal heart decelerations C. Dark brown vaginal bleeding D. Suicidal ideations 65 11/27/2020

A woman has been diagnosed with a ruptured ectopic pregnancy. Which of the following signs and symptoms is characteristic of this diagnosis. A. Dark brown rectal bleeding B. Severe nausea and vomiting C. Sharp unilateral abdominal pain D. Marked hyperthermia 66 11/27/2020
 Definition of spotting during pregnancy
Definition of spotting during pregnancy Credit risk market risk operational risk
Credit risk market risk operational risk Key risk indicators for vendor management
Key risk indicators for vendor management Risk map
Risk map Risk management in nursing
Risk management in nursing Nursing theories related to teenage pregnancy
Nursing theories related to teenage pregnancy Multiple pregnancy nursing diagnosis
Multiple pregnancy nursing diagnosis Nursing care plan for anemia slideshare
Nursing care plan for anemia slideshare Preoperative nursing care plan for cataract surgery
Preoperative nursing care plan for cataract surgery Draw rmmm plan
Draw rmmm plan Avoidance risk
Avoidance risk Relative risk calculation
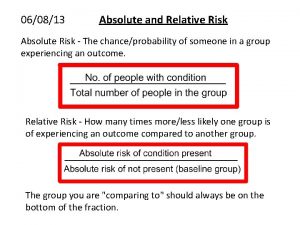
Relative risk calculation Residual risk and secondary risk pmp
Residual risk and secondary risk pmp Inherent risks examples
Inherent risks examples Absolute risk vs relative risk
Absolute risk vs relative risk Thinking algebraically stock market game answer key
Thinking algebraically stock market game answer key Medium-term risk examples
Medium-term risk examples Risk financing transfer dan risk retention
Risk financing transfer dan risk retention The biggest risk is not taking any risks
The biggest risk is not taking any risks Business risk audit
Business risk audit Business risk vs financial risk capital structure
Business risk vs financial risk capital structure Relative risk
Relative risk Population attributable risk formula
Population attributable risk formula Aspiration risk nursing diagnosis
Aspiration risk nursing diagnosis Virchow's triad definition
Virchow's triad definition Team nursing care delivery model
Team nursing care delivery model Nursing intervention for ocd
Nursing intervention for ocd Nursing interventions for neonatal abstinence syndrome
Nursing interventions for neonatal abstinence syndrome Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Top management and middle management
Top management and middle management Top management middle management first line management
Top management middle management first line management Top management middle management first line management
Top management middle management first line management Wvu risk management
Wvu risk management Cook county risk management
Cook county risk management Uaf risk management
Uaf risk management Wharton risk management and decision processes center
Wharton risk management and decision processes center Walt disney company risk management
Walt disney company risk management Ibm smart supply chain
Ibm smart supply chain Data governance and risk management
Data governance and risk management Internal audit definition
Internal audit definition Telecommunications project management
Telecommunications project management Supply chain risk management framework
Supply chain risk management framework Supply chain risk management framework
Supply chain risk management framework Cisco supply chain risk management
Cisco supply chain risk management Risk management einkauf
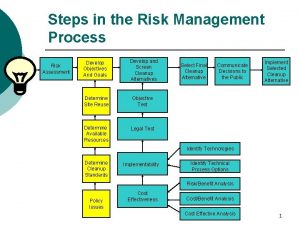
Risk management einkauf Steps in risk management process
Steps in risk management process What is risk in software project management
What is risk in software project management Risk management in software engineering
Risk management in software engineering Clinical risk management in dentistry
Clinical risk management in dentistry Risk management plus online
Risk management plus online What is risk projection
What is risk projection Risk management for water and wastewater utilities
Risk management for water and wastewater utilities Hse risk management policy
Hse risk management policy Civil engineering completed risks insurance
Civil engineering completed risks insurance Risk management for enterprises and individuals
Risk management for enterprises and individuals Risk management in industrial engineering
Risk management in industrial engineering Anz risk management framework
Anz risk management framework Four stages of project risk management
Four stages of project risk management Lister
Lister Pmi risk management definition
Pmi risk management definition Avoidance risk
Avoidance risk Orm worksheet
Orm worksheet Orca risk assessment
Orca risk assessment Orm methodology 4 step process
Orm methodology 4 step process Swot analysis risk management
Swot analysis risk management Certification course in risk management nibm
Certification course in risk management nibm Literature review on enterprise risk management
Literature review on enterprise risk management