Health Insurance Adverse Selection Moral Hazard FGS 8



![Risk aversion Expected Value: E [income if heads]=Prb(H)*$2+Prb(T)*0=1 Actuarially fair gamble: is one in Risk aversion Expected Value: E [income if heads]=Prb(H)*$2+Prb(T)*0=1 Actuarially fair gamble: is one in](https://slidetodoc.com/presentation_image_h/2152c7a01308ae31f4df73b58c21bf8b/image-26.jpg)



























- Slides: 153
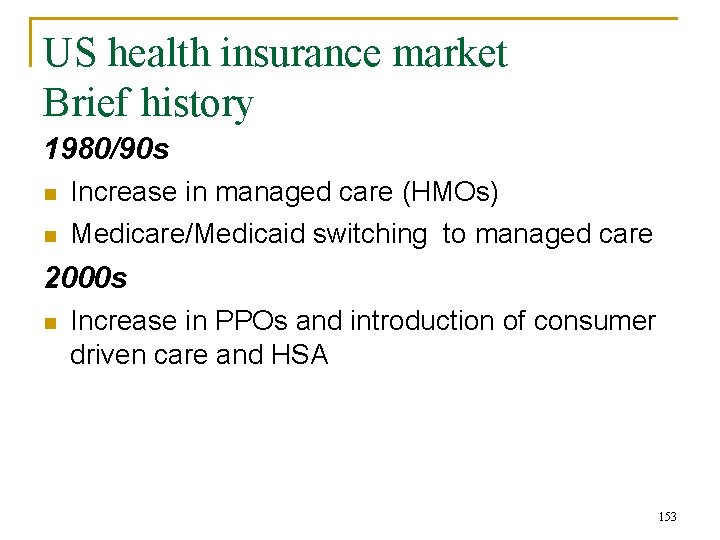
Health Insurance Adverse Selection Moral Hazard FGS 8, 10, 11, 12 Cutler 1994 1
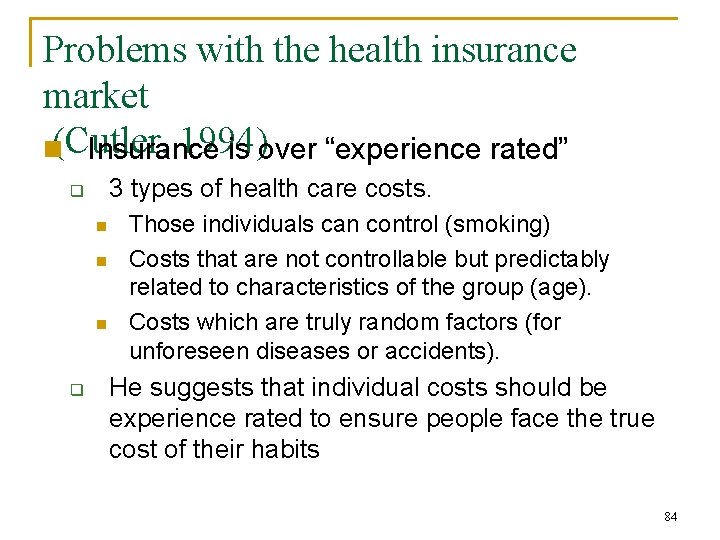
Outline n n Uninsured in the US Demand for Insurance q q n Problems with demand for insurance q q n n Moral hazard Adverse selection Problems with the health insurance market (Cutler) Health insurance features Insurance and demand for medical care Supply of insurance q q q n What is insurance – risk pooling What is risk aversion Demand for insurance Factors affecting demand for insurance Fee-for-service Managed care Consumer-driven health plans and health savings accounts US health insurance market a brief history 2

Uninsured § Uninsured and Underinsured 47 million people uninsured in 2006 (15 % of population) q n n An increase of 8. 6 million from 2000 Majority are employed in small firms (<100) 16 million non-elderly adults (20%) were underinsured q n High out-of-pocket health costs to income ratio 3

Figure 1: 47 million uninsured in 2006; Increase of 8. 6 million since 2000 Number of uninsured, in millions Source: U. S. Census Bureau, March Current Population Survey, 2001– 2007. 4
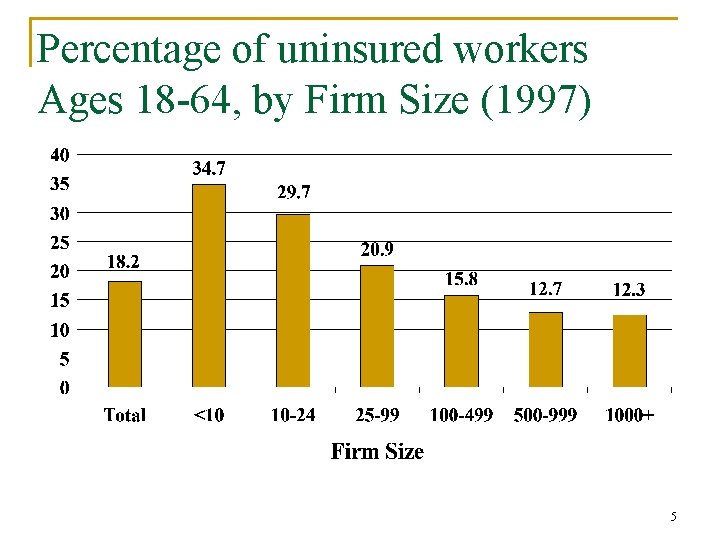
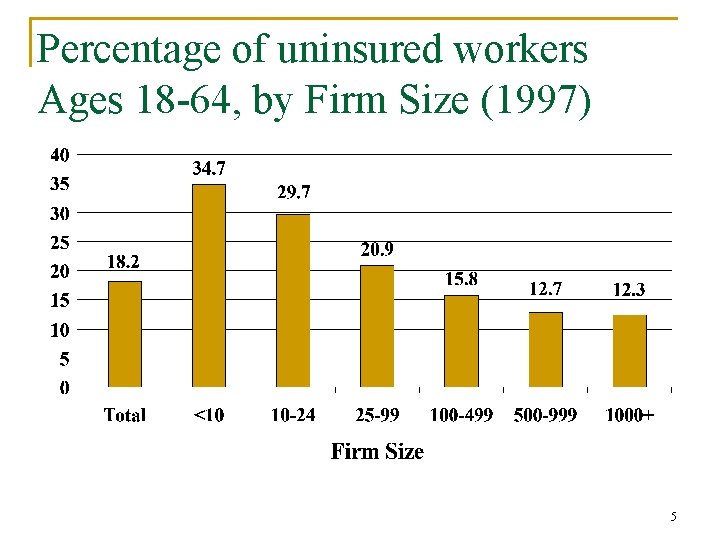
Percentage of uninsured workers Ages 18 -64, by Firm Size (1997) 5
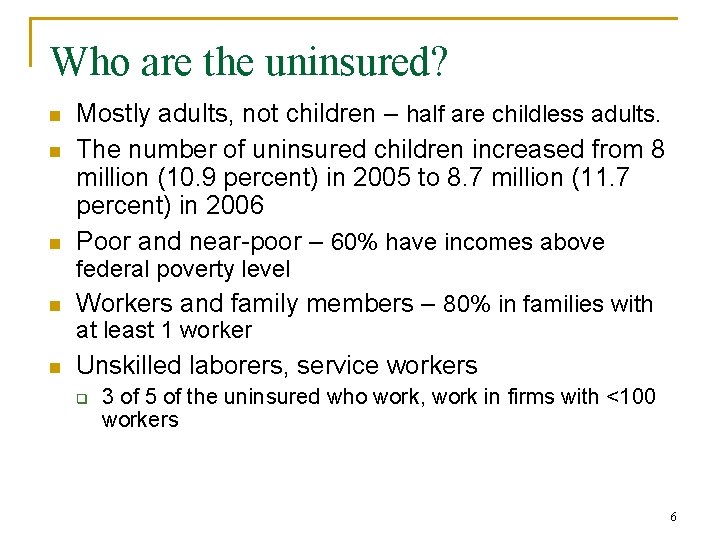
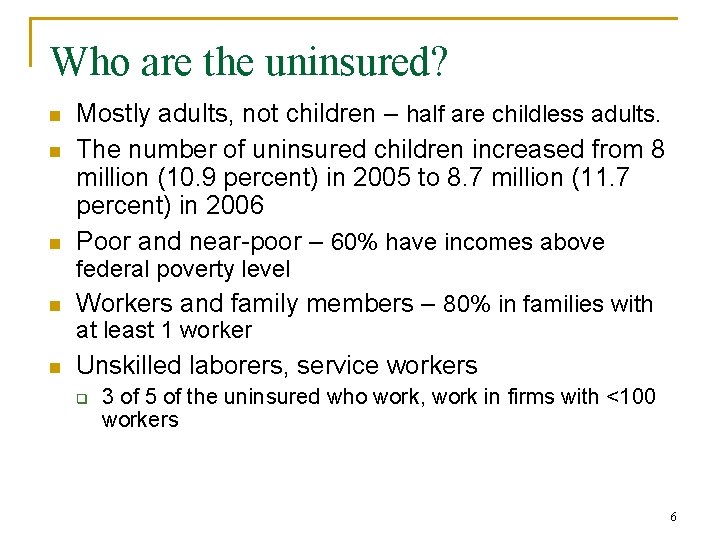
Who are the uninsured? n n n Mostly adults, not children – half are childless adults. The number of uninsured children increased from 8 million (10. 9 percent) in 2005 to 8. 7 million (11. 7 percent) in 2006 Poor and near-poor – 60% have incomes above federal poverty level n Workers and family members – 80% in families with at least 1 worker n Unskilled laborers, service workers q 3 of 5 of the uninsured who work, work in firms with <100 workers 6
Uninsured: Why are they uninsured n Three primary reasons that workers don’t have insurance: q q q The employer does not offer a health plan. Employer offers health plan, but employee is not eligible for the plan because of part-time status or some other rule. Employee doesn’t buy plan because plan too expensive or does not perceive need for plan 7
Uninsured: Why are they uninsured n Uninsured, more likely to: q q q Change jobs Work part-time Work for small firms n n Small-firms pay much higher premiums because their risk is perceived to be large. Why don’t they buy private health insurance q There is no risk pooling with private health insurance and it is expensive n n Average annual cost of family policy in the private market (3, 330) Average annual cost an employee pays out of pocket towards group insurance (2, 700) 8
Uninsured: Impact on health outcomes n Empirical research gives mixed results q Empirically difficult to measure n n Selection bias: Those who choose not to buy health insurance do so because they are healthier Endogeneity: does lack of insurance cause poor health, or does poor health decrease the probability of being insured. (can’t determine direction of causality) Despite inconclusive empirical evidence, the argument that those without insurance experience poor health is powerful. As the number of uninsured grow, policy makers will have an increasingly difficult time ignoring health consequences of the uninsured. 9
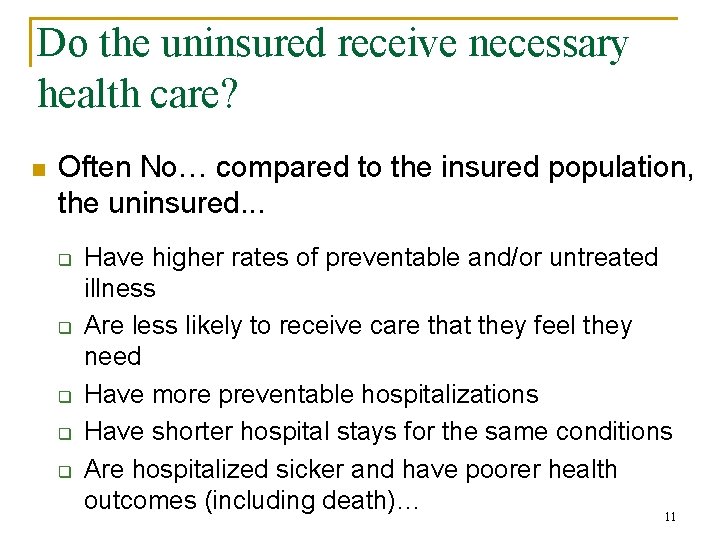
Do the uninsured receive necessary health care? 10
Do the uninsured receive necessary health care? n Often No… compared to the insured population, the uninsured. . . q q q Have higher rates of preventable and/or untreated illness Are less likely to receive care that they feel they need Have more preventable hospitalizations Have shorter hospital stays for the same conditions Are hospitalized sicker and have poorer health outcomes (including death)… 11
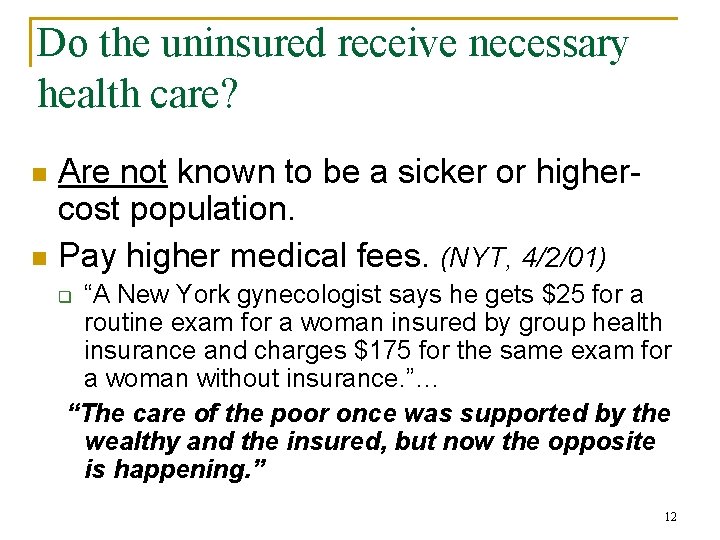
Do the uninsured receive necessary health care? Are not known to be a sicker or highercost population. n Pay higher medical fees. (NYT, 4/2/01) n “A New York gynecologist says he gets $25 for a routine exam for a woman insured by group health insurance and charges $175 for the same exam for a woman without insurance. ”… “The care of the poor once was supported by the wealthy and the insured, but now the opposite is happening. ” q 12
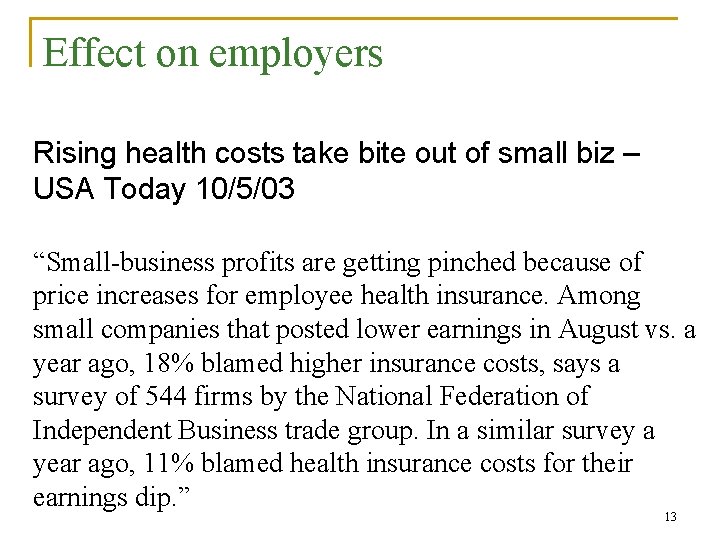
Effect on employers Rising health costs take bite out of small biz – USA Today 10/5/03 “Small-business profits are getting pinched because of price increases for employee health insurance. Among small companies that posted lower earnings in August vs. a year ago, 18% blamed higher insurance costs, says a survey of 544 firms by the National Federation of Independent Business trade group. In a similar survey a year ago, 11% blamed health insurance costs for their earnings dip. ” 13
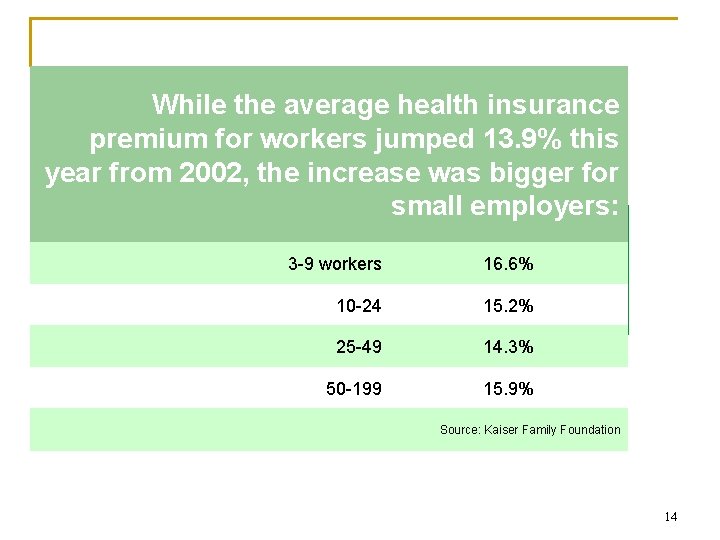
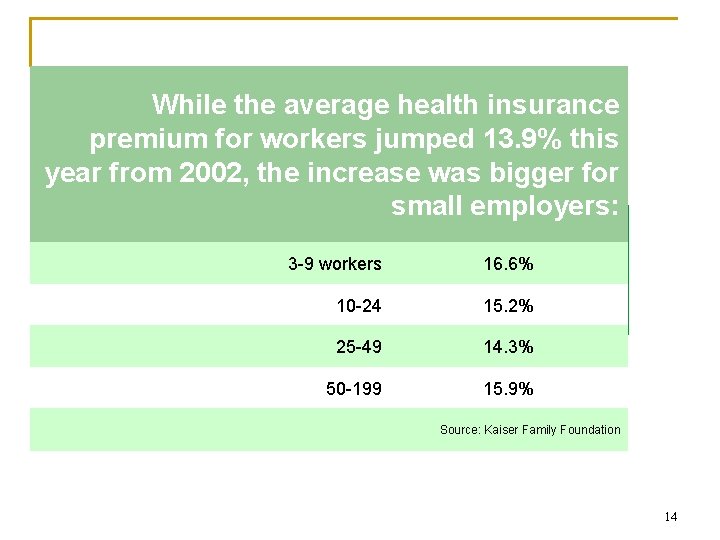
While the average health insurance premium for workers jumped 13. 9% this year from 2002, the increase was bigger for small employers: Ouch! 3 -9 workers 16. 6% 10 -24 15. 2% 25 -49 14. 3% 50 -199 15. 9% Source: Kaiser Family Foundation 14
Outline n n Uninsured in the US Demand for Insurance q q n Problem with demand for insurance q q n n Moral hazard Adverse selection Problems with the health insurance market (Cutler) Health insurance features Insurance and demand for medical care Supply of insurance q q q n What is insurance – risk pooling What is risk aversion Demand for insurance Factors affecting demand for insurance Fee-for-service Managed care Consumer-driven health plans and health savings accounts US health insurance market a brief history 15
What is insurance n n Meant to insure us against random uncertainty. Club of 100 members. On average, each year one member gets sick, it costs $20, 000. It is random who gets sick. This is a lot of money for one person to pay. 16
What is insurance n n Instead, they insure each other and each pay $200 a year. They pay this to avoid the risk of uncertainty that they will have to pay 20, 000. Money put in bank to get interest, and pay out when someone gets sick. Aim of insurance is to reduce the variability in one’s income by pooling risks with a large number of people. 17
What is insurance n n n Outlays for health may be variable for one person, they are fairly predictable for the group. Health insurance would not be necessary if everyone had average needs. But we do not it is variable. Insurance makes it possible to obtain health care without going Bankrupt (new cancer drug $100, 000 a year). 18

What is insurance Desirable characteristics for insurance: 1. The number of insured should be large, and they should be independently exposed to potential risk 2. Losses covered should be definite in time, place, and amount 3. The chance of loss should be measurable 4. The loss should be accidental from view point of person who is insured 19
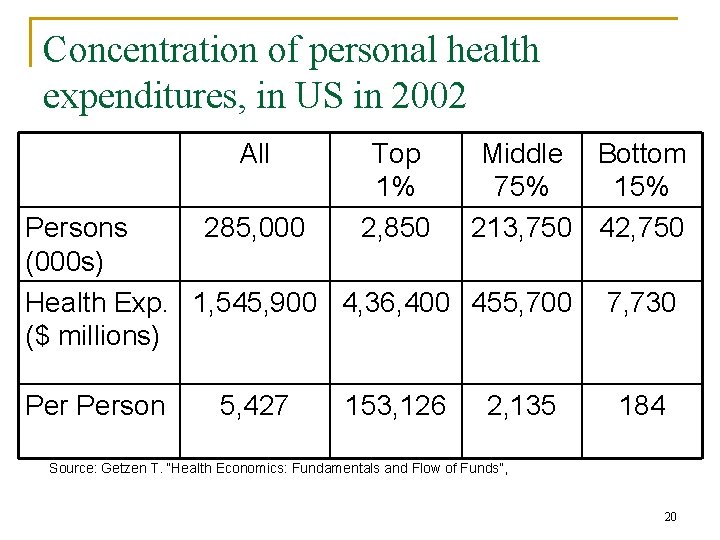
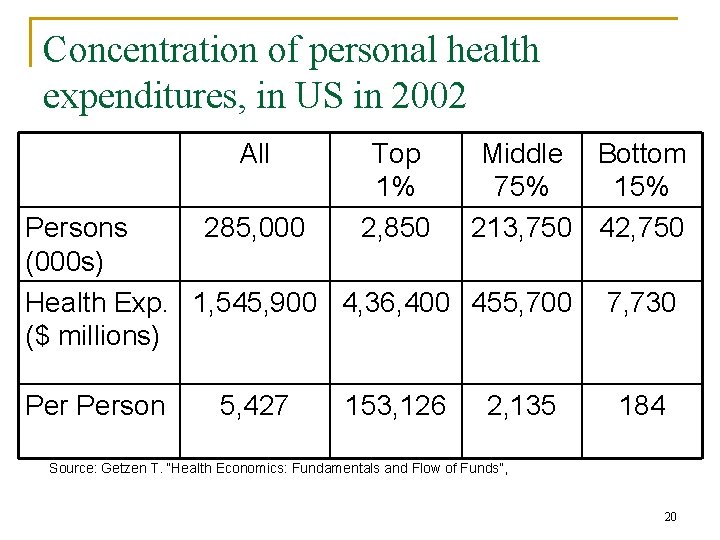
Concentration of personal health expenditures, in US in 2002 All Top 1% 2, 850 Middle Bottom 75% 15% 213, 750 42, 750 Persons 285, 000 (000 s) Health Exp. 1, 545, 900 4, 36, 400 455, 700 ($ millions) Person 5, 427 153, 126 2, 135 7, 730 184 Source: Getzen T. “Health Economics: Fundamentals and Flow of Funds”, 20
Terminology Loading Fee: general costs associated with the insurance company doing business, such as sales, advertising, or profit. Premium: When people buy insurance policies, they typically pay a given premium for a given amount of coverage should the event occur. Should cover average medical care expenses 21
Demand for health insurance n Results of uncertainly q q n Insurance companies pool risk q n Illness and medical expenditures are unpredictable Hospitalizations, serious injury, and rehabilitation and other advanced modern treatments can be very expensive Can save for possible medical expenditures Most households are averse to risk Don’t take on risk, spread risk among many consumers What is risk aversion? 22
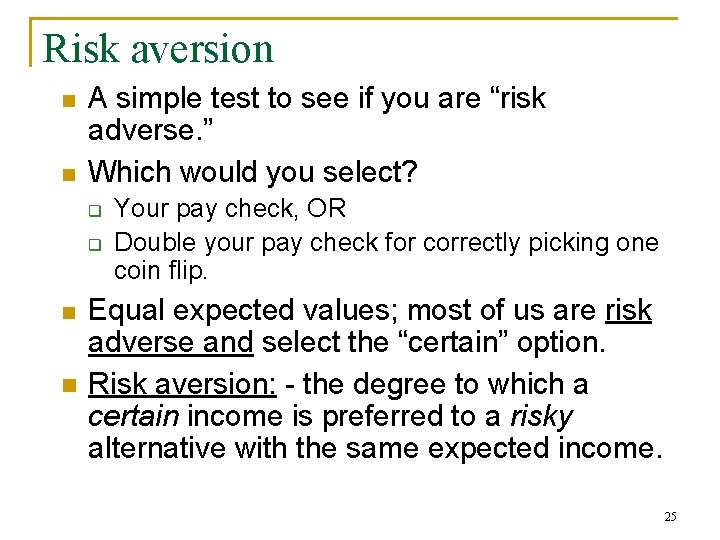
Risk aversion Consider the gambling game: q q n Zan and Forest flip a coin. If it comes up heads, Zan wins a dollar and Forest nothing. If it comes up tails, Forest wills a dollar and Zan nothing. How much should they each be willing to pay to play this game? Expected Return for Zan: P(head)*$2 + P(tails)*0=$1 q Willing to pay $1 cents 23
Risk aversion n n Would you be willing to play this game for $5 get $10 if win, for $10, 000 get $20, 000 if win? The fact that you are less willing to play at larger amounts shows you are risk averse 24
Risk aversion n n A simple test to see if you are “risk adverse. ” Which would you select? q q n n Your pay check, OR Double your pay check for correctly picking one coin flip. Equal expected values; most of us are risk adverse and select the “certain” option. Risk aversion: - the degree to which a certain income is preferred to a risky alternative with the same expected income. 25
![Risk aversion Expected Value E income if headsPrbH2PrbT01 Actuarially fair gamble is one in Risk aversion Expected Value: E [income if heads]=Prb(H)*$2+Prb(T)*0=1 Actuarially fair gamble: is one in](https://slidetodoc.com/presentation_image_h/2152c7a01308ae31f4df73b58c21bf8b/image-26.jpg)
Risk aversion Expected Value: E [income if heads]=Prb(H)*$2+Prb(T)*0=1 Actuarially fair gamble: is one in which the amount you pay for the gamble is equal to the expected value of the gamble. n You paid a $1 to play, and the expected value of the game was $1. 26

Risk aversion n If price of gamble (amount pay to play game) is equal to the expected return, then the gamble is actuarially fair. In health, if expected benefit payment is equal to premiums, the insurance policy is actuarially fair. Now suppose the gamble was instead for $5, 000, would you want to play the game? q If not you are defined as being risk averse, because you do not want to take the actuarially fair gamble. 27
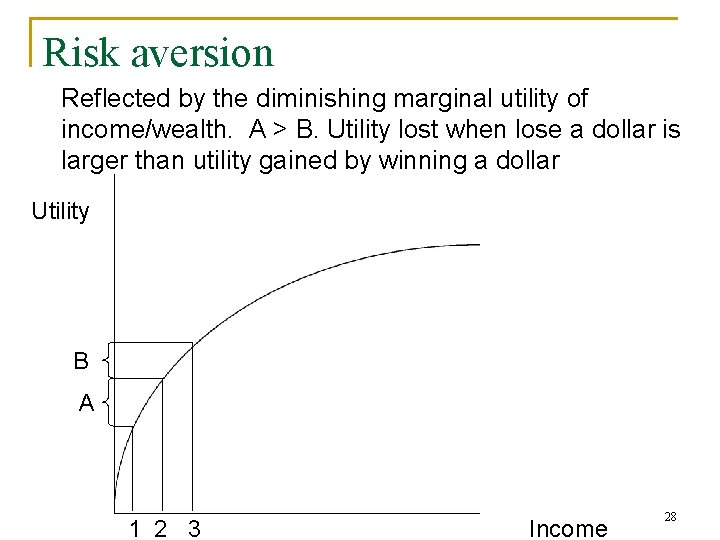
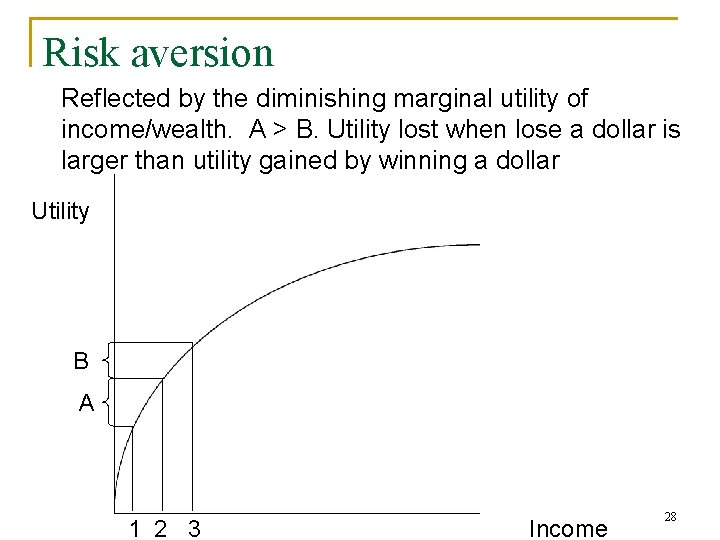
Risk aversion Reflected by the diminishing marginal utility of income/wealth. A > B. Utility lost when lose a dollar is larger than utility gained by winning a dollar Utility B A 1 2 3 Income 28
Risk aversion n Presence of aversion makes consumers willing to pay to spread risk with others. Insurance companies specialize in pricing risks, not in taking risks. Lesson from theory of insurance: the losses that are insured are: large, infrequent, random, and not associated with a large moral hazard. 29

Demand for insurance See notes from black board Factors affecting demand for health insurance: 1. Probability of illness 2. Loading fee 3. Magnitude of loss relative to income (cost of illness) 4. Degree of risk aversion 5. Price: Higher price reduces likelihood that an individual will insure against a given event 30
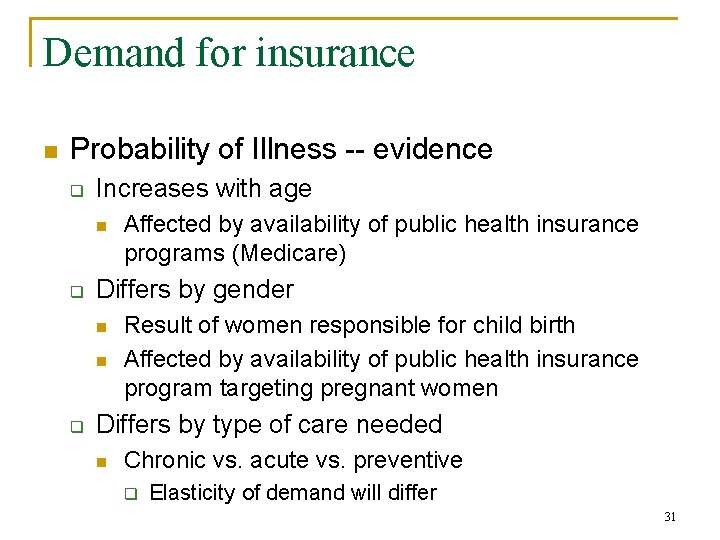
Demand for insurance n Probability of Illness -- evidence q Increases with age n q Differs by gender n n q Affected by availability of public health insurance programs (Medicare) Result of women responsible for child birth Affected by availability of public health insurance program targeting pregnant women Differs by type of care needed n Chronic vs. acute vs. preventive q Elasticity of demand will differ 31
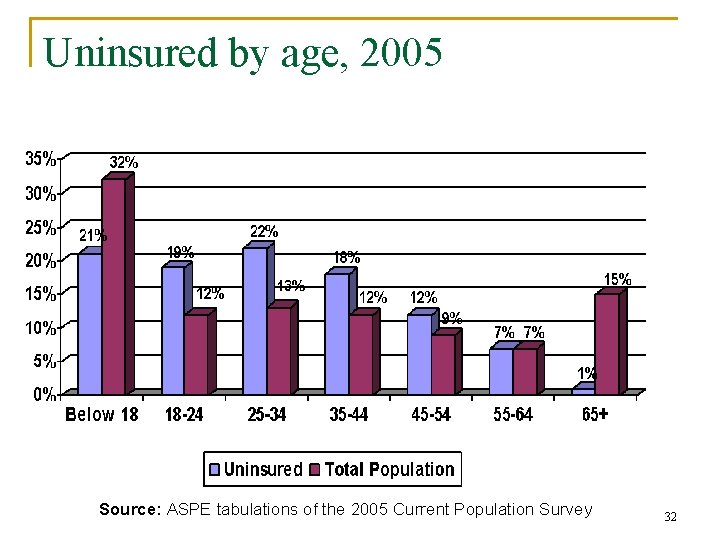
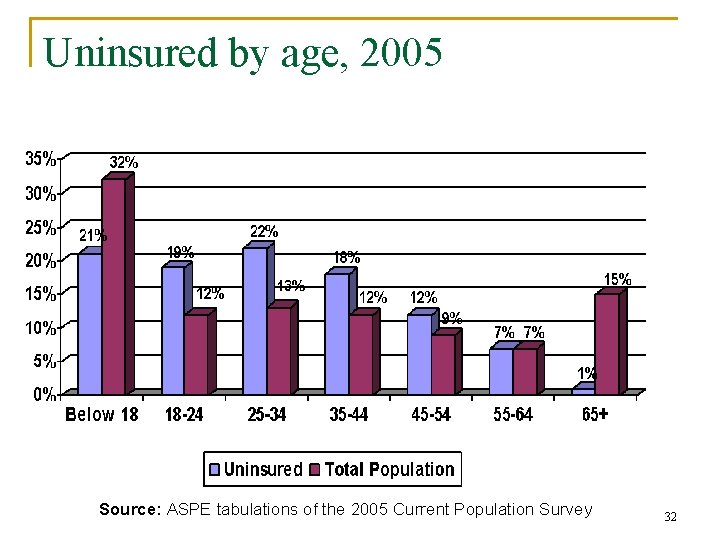
Uninsured by age, 2005 Source: ASPE tabulations of the 2005 Current Population Survey 32
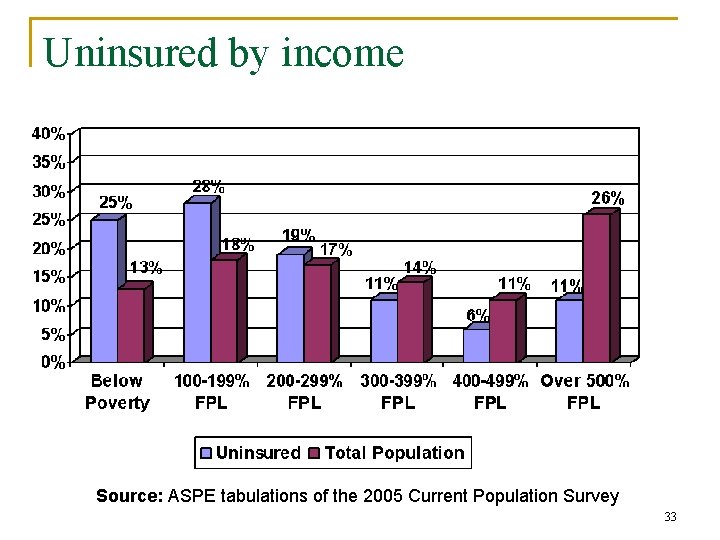
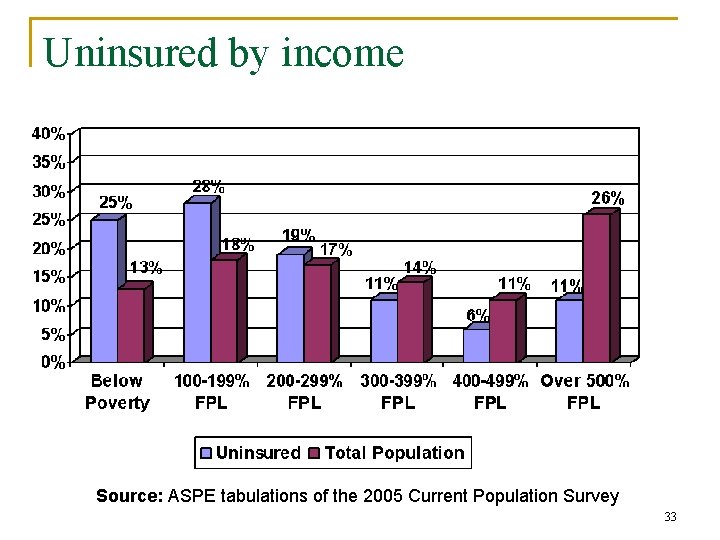
Uninsured by income Source: ASPE tabulations of the 2005 Current Population Survey 33
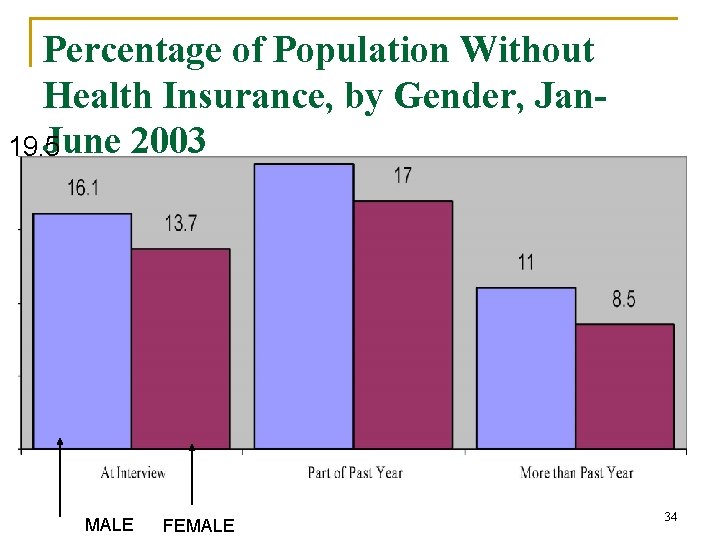
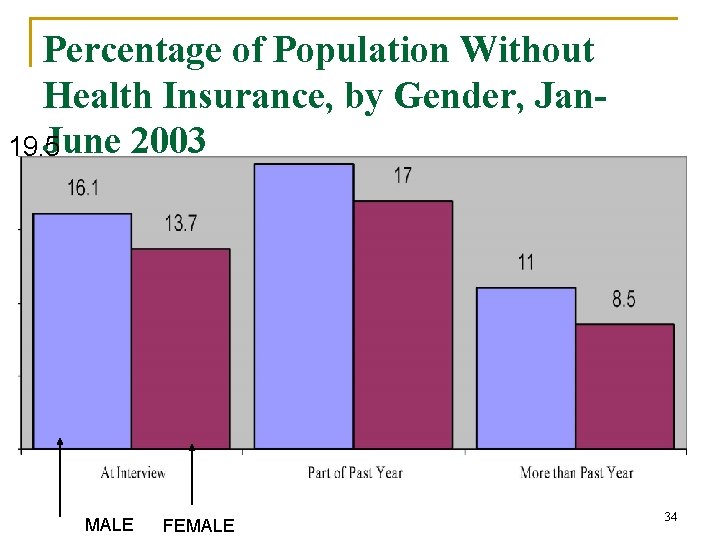
Percentage of Population Without Health Insurance, by Gender, Jan. June 2003 19. 5 MALE FEMALE 34
Outline n n Uninsured in the US Demand for insurance q q n Problems with demand for insurance q q n n Moral hazard Adverse selection Problems with the health insurance market (Cutler) Health insurance features Insurance and demand for medical care Supply of insurance q q q n What is insurance – risk pooling What is risk aversion Demand for insurance Factors affecting demand for insurance Fee-for-service Managed care Consumer-driven health plans and health savings accounts US health insurance market a brief history 35
Problems in demand for insurance Two main problems with demand for insurance 1. Moral hazard: The disincentives created by insurance for individuals to take measures that would reduce the amount of care demanded. OR, additional quantity of health care demanded, resulting from a decrease in the net price of health care attributable to insurance 36
Problems in demand for insurance 2. Adverse selection: A situation often resulting from asymmetric information in which individuals are able to purchase insurance at rates that are below actuarially fair rates plus loading costs - alternatively: occurs when high-risk consumers, who know more about their own health status than insurers do, subcribe to an insured group composed of lower-risk individuals to secure low premiums. 37
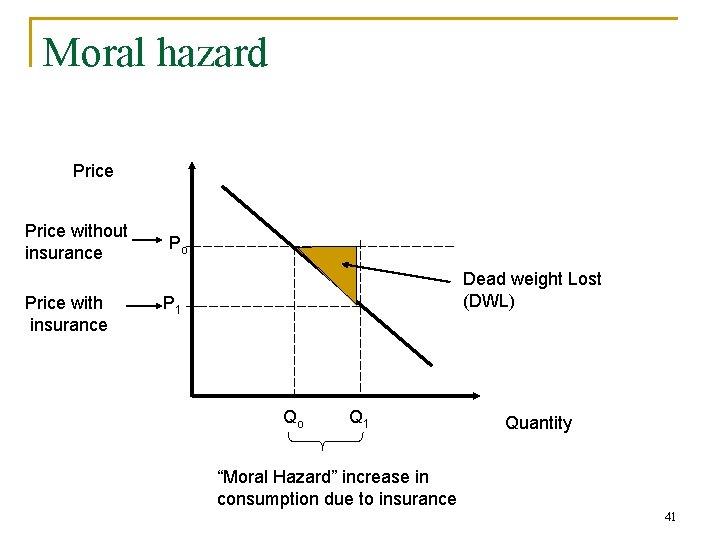
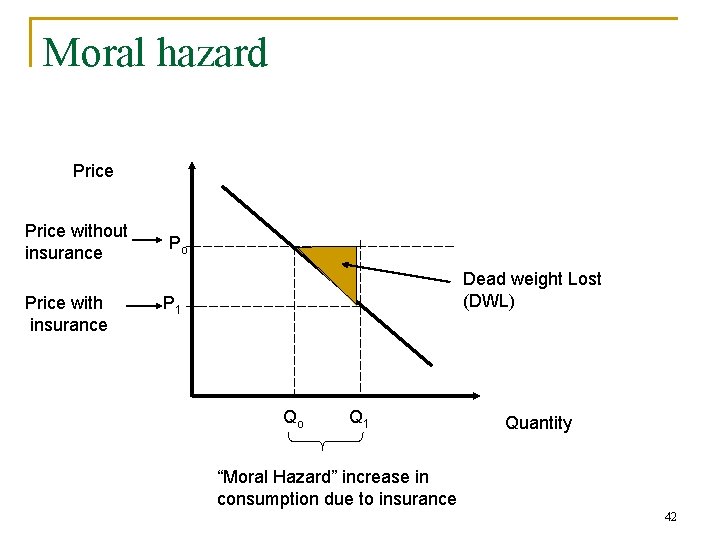
Moral hazard n n n What are the effects of the new price system (with insurance) on demand for insurance. Buying insurance lowers the price per unit of health care service at time it is bought. Person with health insurance is more likely to go to the doctor for a small problem than someone without health insurance q Likely to affect good with higher elasticity of demand such as preventive care. 38

Moral hazard Moral Hazard: refers to the increased usage of services when the pooling of risks lead to decreased marginal costs for services. (i. e. the price is reduced). n It is also used to refer to how one changes behavior when they are insured. q We may take more risks, which could have health care implications when insured rather than not insured. n Learning snow boarding (lot of people break their arms). May not learn if don’t have health insurance. 39
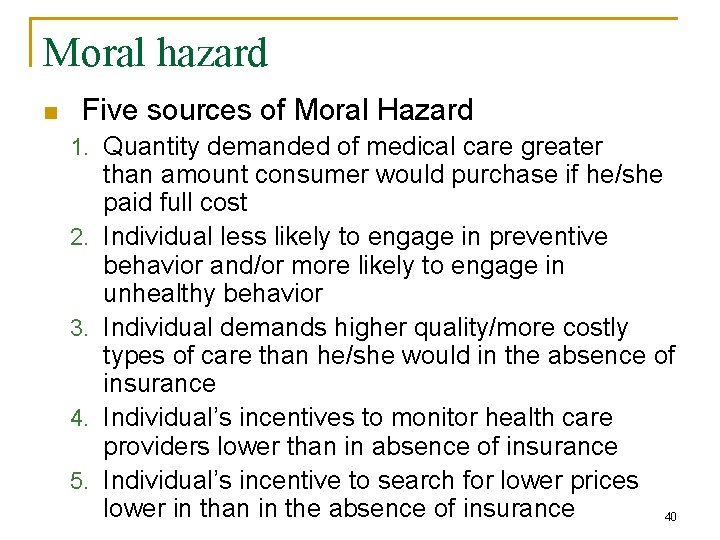
Moral hazard n Five sources of Moral Hazard 1. Quantity demanded of medical care greater 2. 3. 4. 5. than amount consumer would purchase if he/she paid full cost Individual less likely to engage in preventive behavior and/or more likely to engage in unhealthy behavior Individual demands higher quality/more costly types of care than he/she would in the absence of insurance Individual’s incentives to monitor health care providers lower than in absence of insurance Individual’s incentive to search for lower prices lower in than in the absence of insurance 40
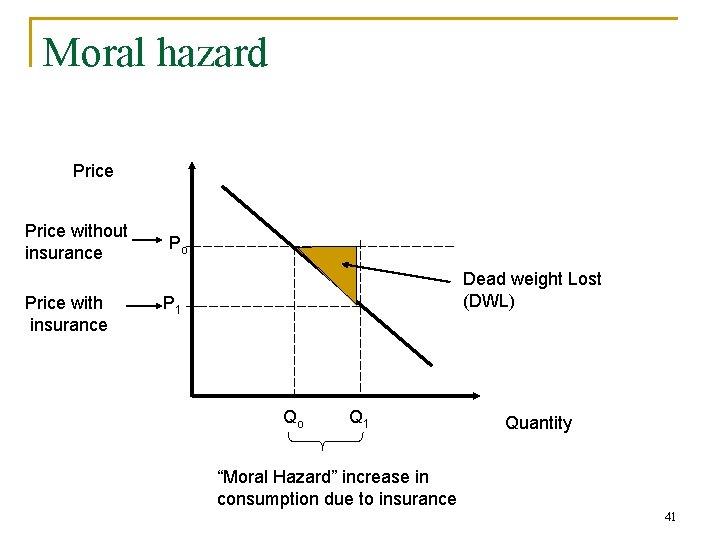
Moral hazard Price without insurance Price with insurance Po Dead weight Lost (DWL) P 1 Qo Q 1 Quantity “Moral Hazard” increase in consumption due to insurance 41
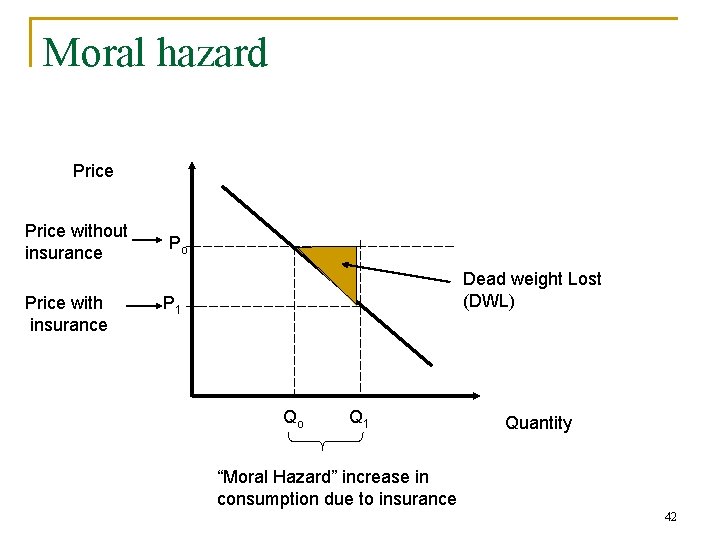
Moral hazard Price without insurance Price with insurance Po Dead weight Lost (DWL) P 1 Qo Q 1 Quantity “Moral Hazard” increase in consumption due to insurance 42

Moral hazard Price without insurance Price with insurance D 1 Moral Hazard: D 2 • decreases when the price becomes more elastic. (i. e. for those goods you want no matter the price. Po DWL P 1 Qo. Q 2 Q 1 Quantity 43
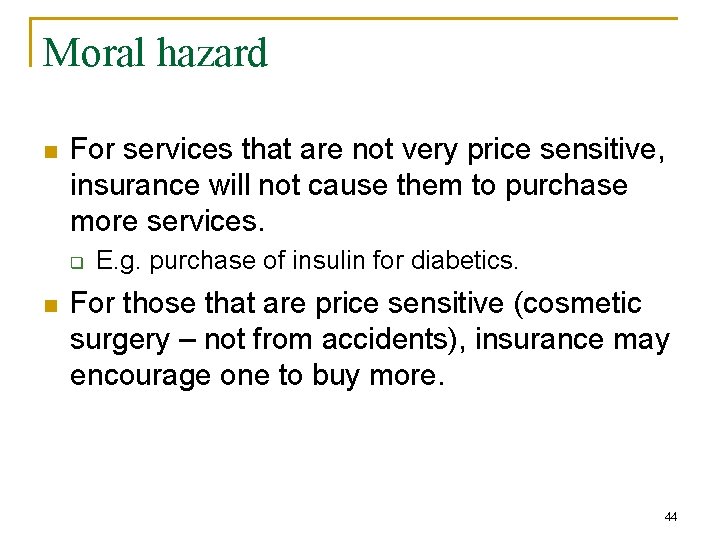
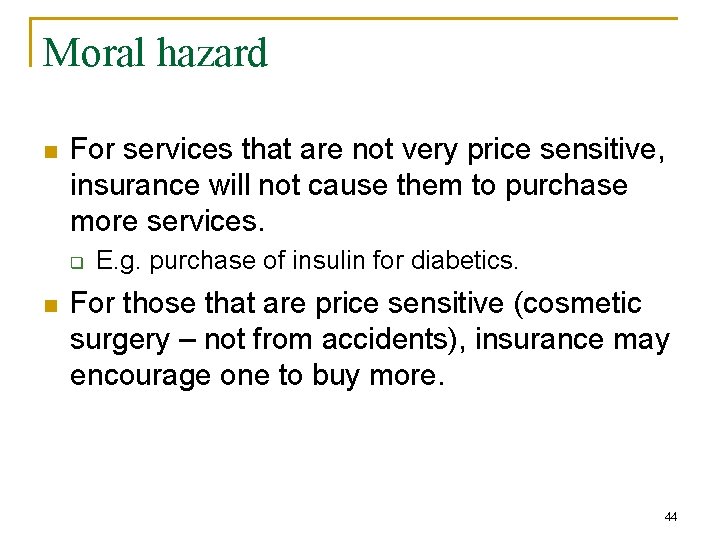
Moral hazard n For services that are not very price sensitive, insurance will not cause them to purchase more services. q n E. g. purchase of insulin for diabetics. For those that are price sensitive (cosmetic surgery – not from accidents), insurance may encourage one to buy more. 44
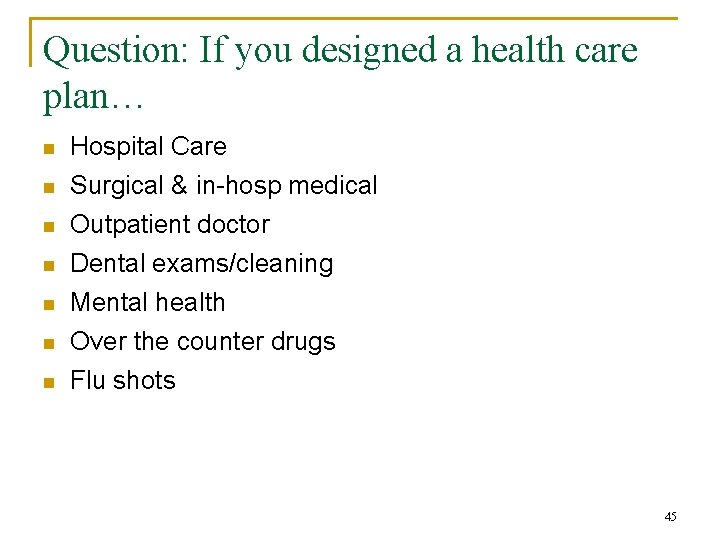
Question: If you designed a health care plan… n Hospital Care n Surgical & in-hosp medical n Outpatient doctor Dental exams/cleaning Mental health Over the counter drugs Flu shots n n 45
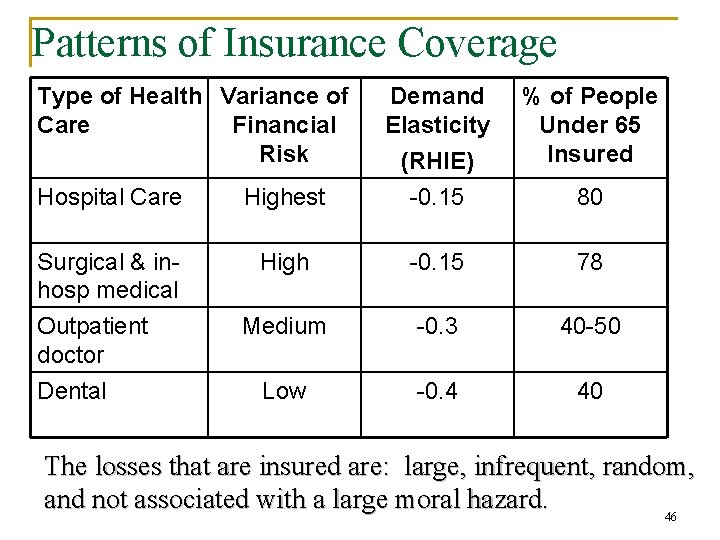
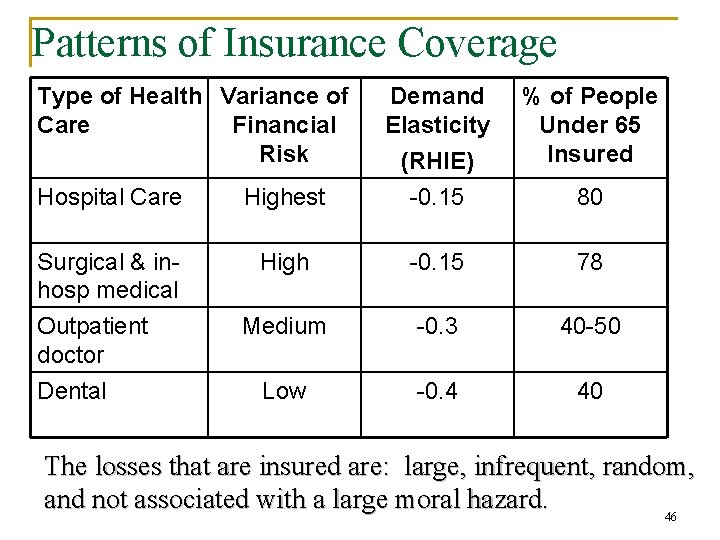
Patterns of Insurance Coverage Type of Health Variance of Care Financial Risk Hospital Care Highest Demand Elasticity (RHIE) -0. 15 Surgical & inhosp medical Outpatient doctor High -0. 15 78 Medium -0. 3 40 -50 Low -0. 4 40 Dental % of People Under 65 Insured 80 The losses that are insured are: large, infrequent, random, and not associated with a large moral hazard. 46

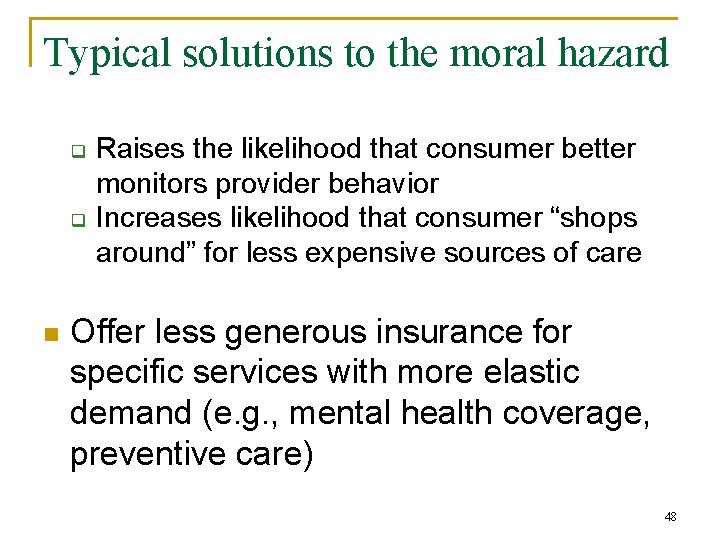
Typical solutions to the moral hazard n Increase cost sharing q q Could do this through co-payments or deductibles Reduce the quantity demanded by increasing price consumer faces Increases preventive behavior/reduces unhealthy behavior since consumer faces part of “costs” from these behaviors Increases the likelihood of consumer choosing less expensive types of medical care 47
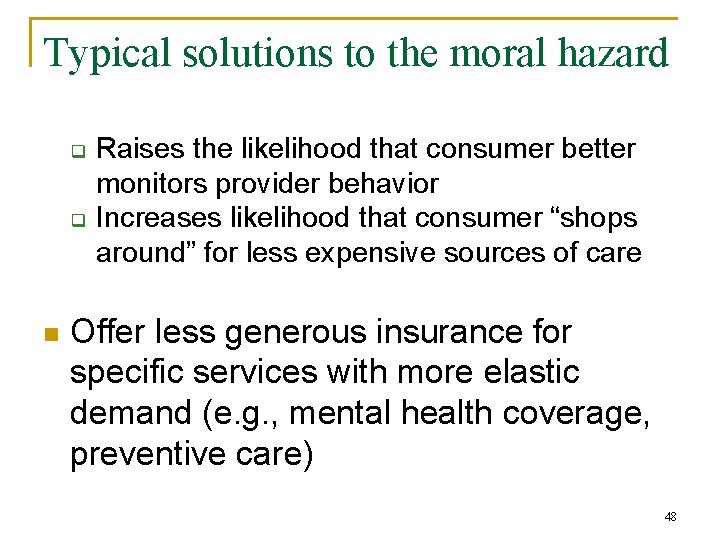
Typical solutions to the moral hazard q q n Raises the likelihood that consumer better monitors provider behavior Increases likelihood that consumer “shops around” for less expensive sources of care Offer less generous insurance for specific services with more elastic demand (e. g. , mental health coverage, preventive care) 48
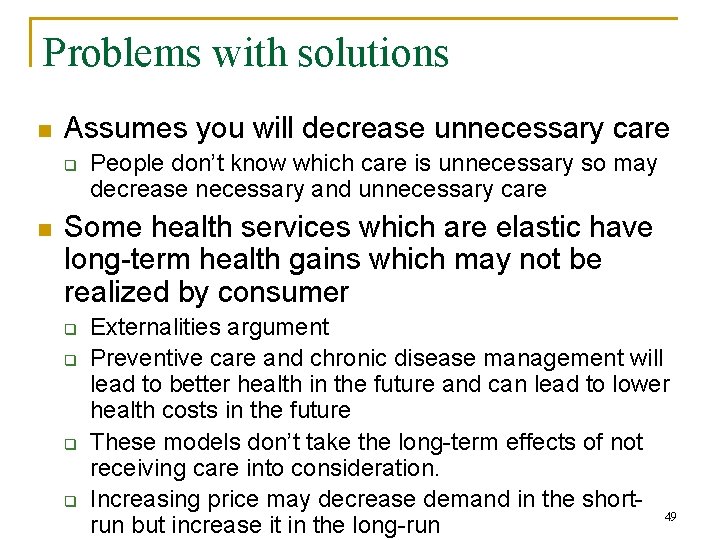
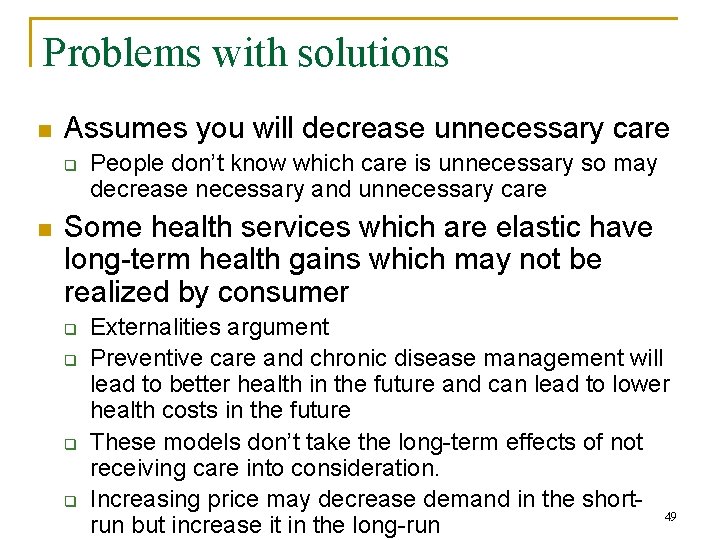
Problems with solutions n Assumes you will decrease unnecessary care q n People don’t know which care is unnecessary so may decrease necessary and unnecessary care Some health services which are elastic have long-term health gains which may not be realized by consumer q q Externalities argument Preventive care and chronic disease management will lead to better health in the future and can lead to lower health costs in the future These models don’t take the long-term effects of not receiving care into consideration. Increasing price may decrease demand in the short 49 run but increase it in the long-run
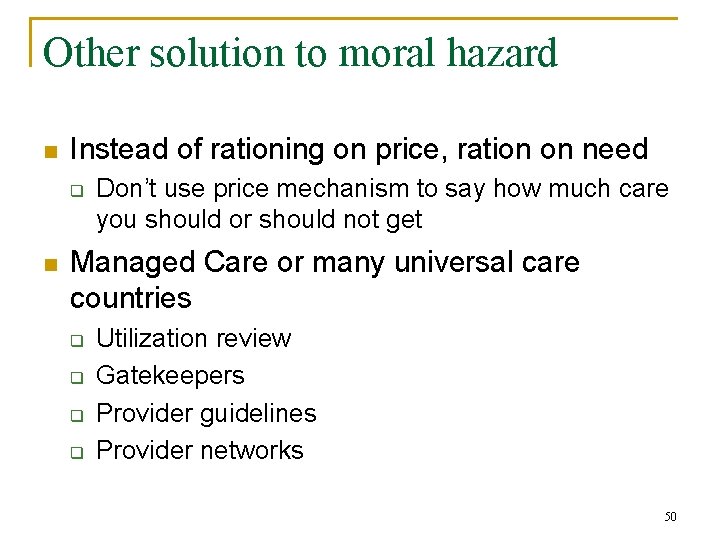
Other solution to moral hazard n Instead of rationing on price, ration on need q n Don’t use price mechanism to say how much care you should or should not get Managed Care or many universal care countries q q Utilization review Gatekeepers Provider guidelines Provider networks 50
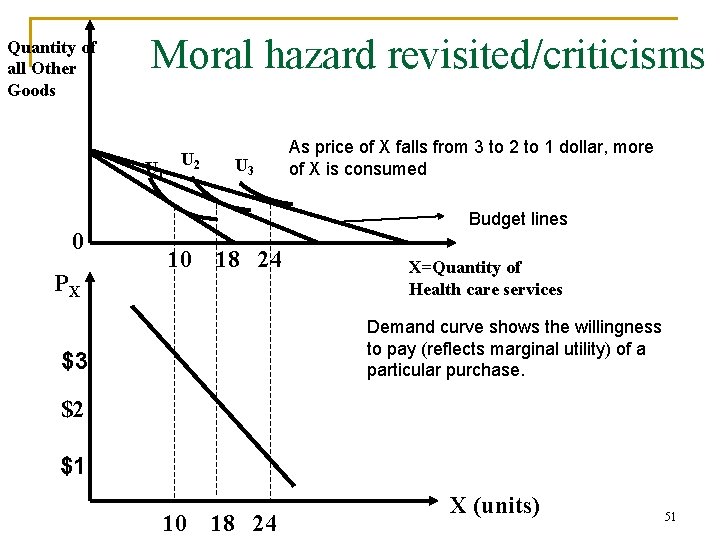
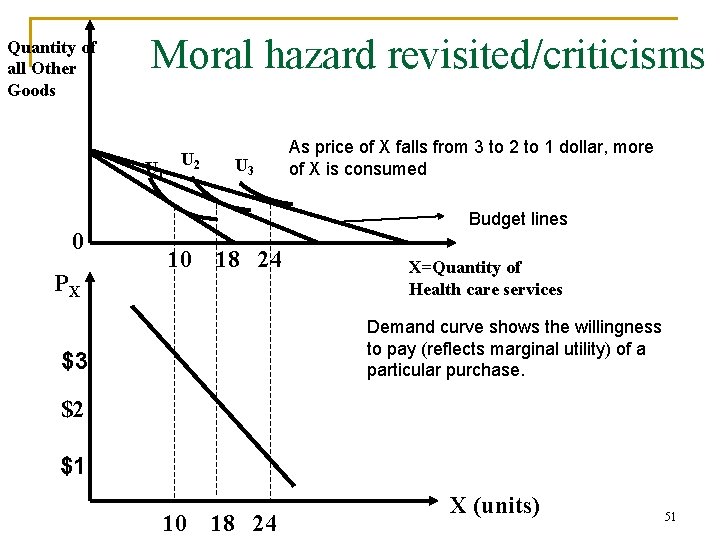
Quantity of all Other Goods Moral hazard revisited/criticisms U 1 0 PX U 2 U 3 As price of X falls from 3 to 2 to 1 dollar, more of X is consumed Budget lines 10 18 24 X=Quantity of Health care services Demand curve shows the willingness to pay (reflects marginal utility) of a particular purchase. $3 $2 $1 10 18 24 X (units) 51

Moral hazard revisited Assumption on consumer preferences that must hold for demand to represent willingness to pay. 1. Consumers must be rational. More of a good always makes them better off. Preferences must exhibit transitivity q q If there are 3 bundles A, B, C A preferred to B, and B preferred to C n n q q Then A must be preferred to C and not the other way round. Consumers must be able to rank any bundle, so which is preferred to which. 52
Moral hazard revisited 2. They must have sufficient information to make good choices. 3. They must know what the result of their consumption decisions will be If these assumptions hold the demand curve shows the willingness to pay for an additional unit of health services 53
Moral hazard revisited Do we meet these assumption? 1. Are consumers rational? n Consumers do not have information on prices and quality to be able to rank/choose different health bundles. q q You can pay a lower price for a health plan but it is not the same product. Do we really know all the differences? n Do people understand the difference between feefor-service and managed care and how the type of payment system might affect care? Are they just picking the least costs without recognizing the potential quality or service differences. 54

Moral hazard revisited n q We have to choose health plans, this is very hard to do when you can’t get information on quality and pricing. n n Infection or complication rates are not provided by hospitals How much you are reimbursed if you have to seek healthcare outside the network when traveling. Is more health care better? q Or are you going to get more services because quality is poor and they can’t figure out the problem. 55
Moral hazard revisited 2. Do consumers know what is best for them? q People can make the wrong tradeoffs. Can be due to need to “show-off” or due to time preferences. n E. g, young tend to think they are invincible q q Who has done things where they think they were lucky? Who has friends that were not so lucky? Wearing helmet when riding bike. Would think differently about the decision if you had an accident and were hurt. 56
Moral hazard revisited 3. Do consumers know the result of their consumption decision? q q q Do we know what would have happened if we had not been treated? The counterfactual. Would the result have been the same if I saw a different doctor? We often do not know if we made the right decision. n E. g. after head injury begin a series of acupuncture. It takes a number of session for acupuncture to work so takes time. Time also helps your head heal. So after a month and a half of acupuncture you feel better. Was it the acupuncture or was it time that 57 healed you?
Moral hazard revisited n Who said the prices reflect the cost of making the good q With monopolies that prices may be too high so we are under consuming care n E. g. prices of the drug for cancer going to go from $20, 000 to $100, 000 58
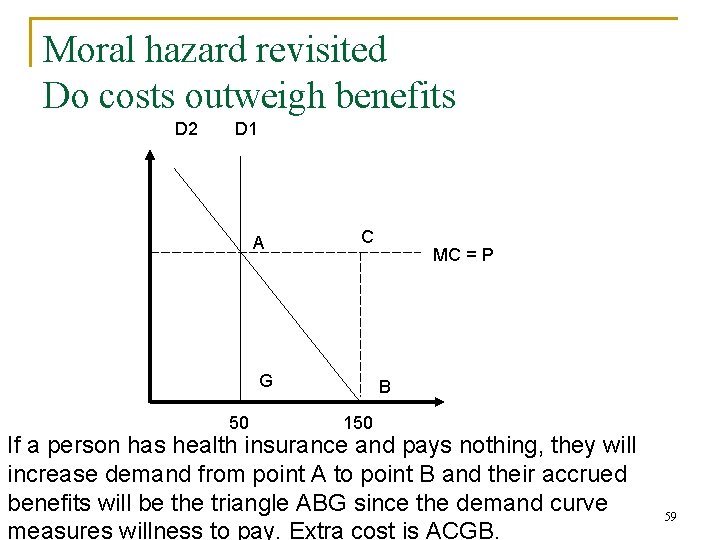
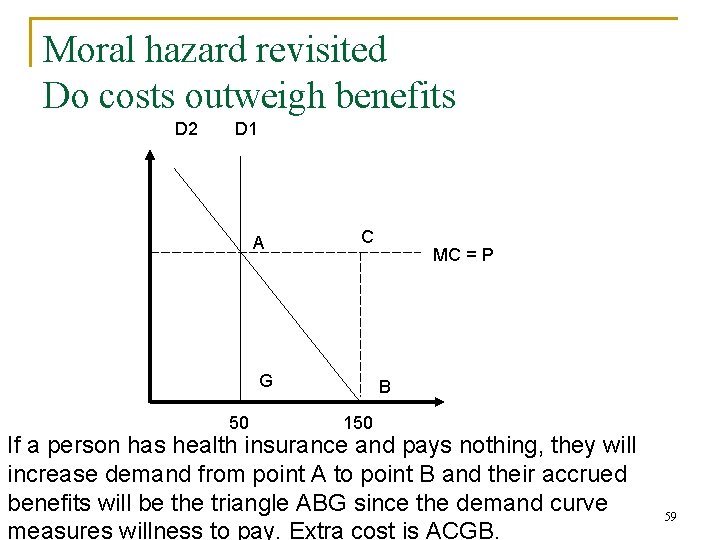
Moral hazard revisited Do costs outweigh benefits D 2 D 1 A C G 50 MC = P B 150 If a person has health insurance and pays nothing, they will increase demand from point A to point B and their accrued benefits will be the triangle ABG since the demand curve measures willness to pay. Extra cost is ACGB. 59
Moral hazard revisited Welfare loss from moral hazard n n Used results from the RAND health insurance experiment (see handout) Found those who paid 95% coinsurance compared to those who paid 0%, had annual expenditures that were 28% less Those who faced a 25% coinsurance spent 18% less than those who faced 0% Willard Manning used these results to show that total welfare loss from moral hazard is between $37 and 60 billion. (represents between 19 and 30 percent of total national health expenditure 60
Moral hazard revisited The problem with welfare calculations n n n These calculations are based on the assumption that the demand curves show the marginal utility a person derives from an additional service. Assumed that the services that were not consumed (when price rose) must have been those that gave them the lowest marginal utility (least effective). Hard to figure out marginal utility consumers receive from different services. 61
Moral hazard revisited The problem with welfare calculations n n n RAND studied grouped services received into categories based on medical effectiveness. Found that cost-sharing was just as likely to lower use of highly effective care as rarely effective care. Cost sharing did not lead to rates of care seeking that were more “appropriate” from a clinic standpoint. 62
Moral hazard revisited n When people try to measure moral hazard they are likely over estimating it. q n Forget to take into account the utility you get from health insurance (that you are risk adverse) You also have to ask if consuming more health care is a bad thing? q Comes back to a value judgment. n n Much of health care private goods. Consuming more preventative care to avoid later large costs would be good thing for society. Yet preventative care is often something an insurance company doesn’t cover (elastic demand – more moral hazard). q e. g. article on providing preventative care for diabetes patients in NY times. 63
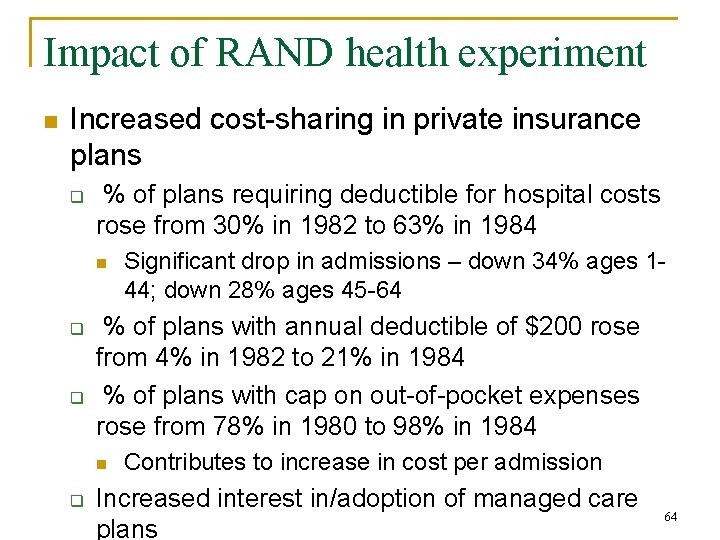
Impact of RAND health experiment n Increased cost-sharing in private insurance plans q % of plans requiring deductible for hospital costs rose from 30% in 1982 to 63% in 1984 n q q % of plans with annual deductible of $200 rose from 4% in 1982 to 21% in 1984 % of plans with cap on out-of-pocket expenses rose from 78% in 1980 to 98% in 1984 n q Significant drop in admissions – down 34% ages 144; down 28% ages 45 -64 Contributes to increase in cost per admission Increased interest in/adoption of managed care plans 64

Adverse selection n This theoretical idea comes from Arrow’s 1963 article. Risk pooling works because everyone in the group is at risk and therefore has an interest in making sure that solid insurance benefits are provided. Suppose the risk was not random, you knew: q q You had a higher chance of lung cancer because smoked all your life – insure You never smoked, eat well, do exercise, so think there is a low chance of getting sick – would not 65 want to pay a lot for health insurance.

Adverse selection n Adverse selection occurs when some factors are known to the insured (i. e. you) by not to the insurer. q n i. e. there is asymmetric information Result of asymmetric information q Two types of consumers: n n q Insurance company observes overall risk in the market not the actual risk for each individual: n q relatively healthy, with low risk of illness (p L) relatively unhealthy, with high risk of illness (p H) p = f(p H)+ (1 -f) (p L); p is probability of illness Sets premium based on observed average risk, you decide to take up health care or not based on your actual risk. Those who are healthier or less risk adverse are more likely to under insure or not insure and those who are sicker and 66 risk adverse will insure
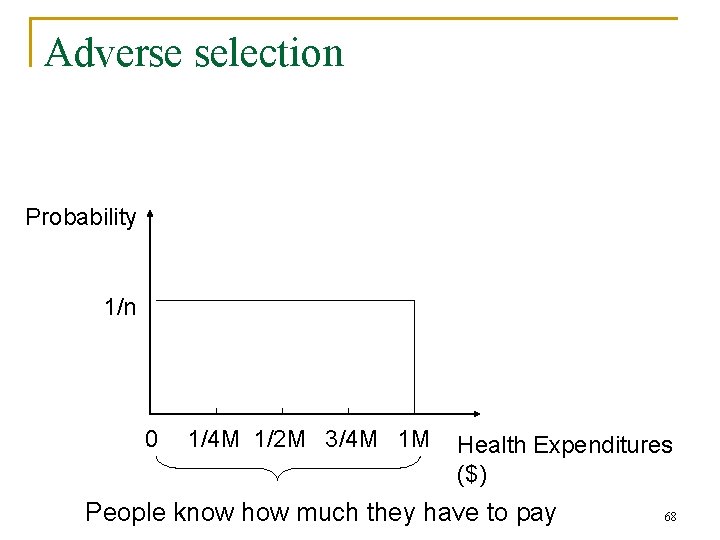
Adverse selection n Example: suppose have n people all with the same demographic characteristics. q Each person knows what they will probably have to pay n q q q So know where they are on the horizontal axis of the next graph. Insurance company knows distribution of health expenditures by person but not which person pays what. People know exactly what they will have to pay. How much should insurance company charge? 67
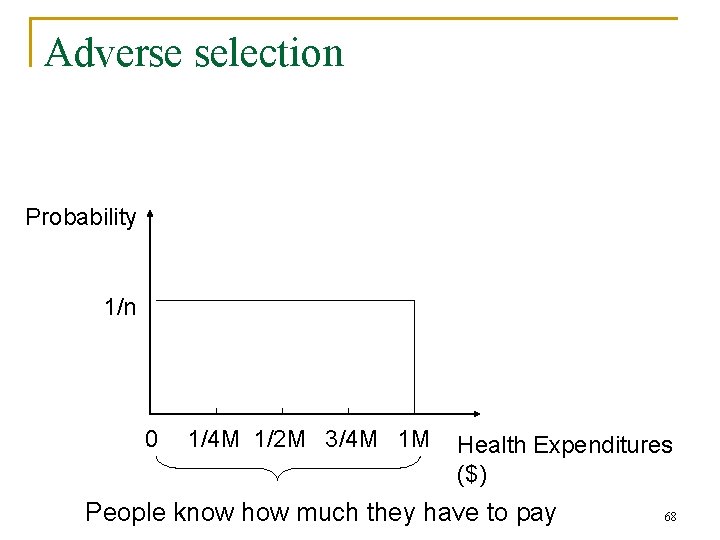
Adverse selection Probability 1/n 0 1/4 M 1/2 M 3/4 M 1 M Health Expenditures ($) People know how much they have to pay 68
Adverse selection n Suppose set price of insurance at $0 q q Everyone will sign up. Insurance company expects to pay out $1/2 M so would be losing money, 69

Adverse selection n So suppose try to set the price of insurance at $1/2 M q q Those who know their expenditures are less than 1/2 M will choose to self-insure and will not sign up for the program. Once they leave the market, the expected amount insurance company will have to pay is $3/4 M, so premium will need to be this much. But then others will drop out of the market. In fact, if adverse selection is very bad, there may be no health insurance offered! 70
Adverse selection n People select into insurance based on their own risk of sickness Adverse selection into the health insurance market will be a problem if insurance companies only know the average risk of the population. To try to mitigate the problem of adverse selection insurance companies need to figure out each person’s actual probability of illness 71
Possible solutions to adverse selection n Waiting periods Pre-existing condition exclusions n Risk rating (underwriting) n q If the high risks are something the insurance company can observe in advance, they can adjust premiums up or down to account for varying risk. n Adjust insurance based on age, gender, behaviors (how much you smoke or drink), BMI, your cholesterol, blood pressure 72
Possible solutions to adverse selection n Insurance that precludes individual selection according to subscribers’ perceptions of their own risk q q Mandate that everyone must purchase health insurance Universal health insurance 73

Adverse selection Alternatively, there are: n Group or Community Ratings: Premiums are based on the average characteristics of a group or community rather than your individual characteristics. q q Old and young in a group pay the same amount. Those with and without chronic conditions pay the same amount 74
Adverse selection n Problems for companies in US: Compare Google to Ford q q Google is full of young workers – so insurance premiums and what the company has to pay might be quite low. Ford has older workers – so their insurance premiums and what the company might pay will be quite high. n q Still can be adverse selection, young workers may not want to buy insurance Google is probably happier than Ford with group ratings used by private health care. Health care unaffordable for some companies 75
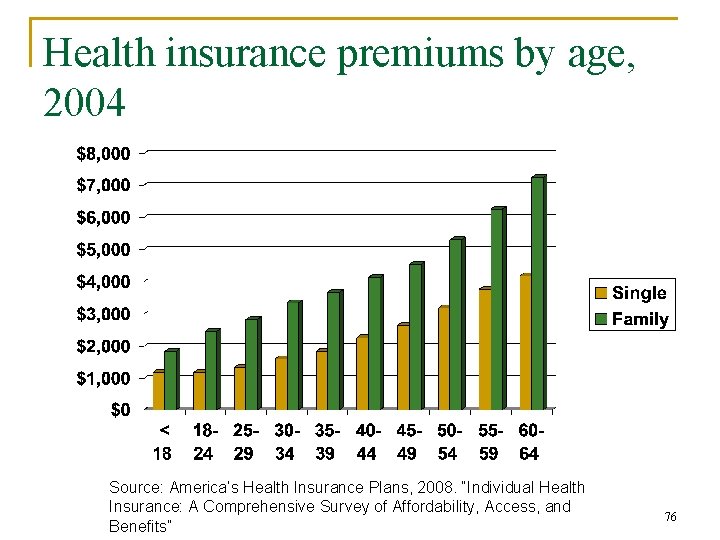
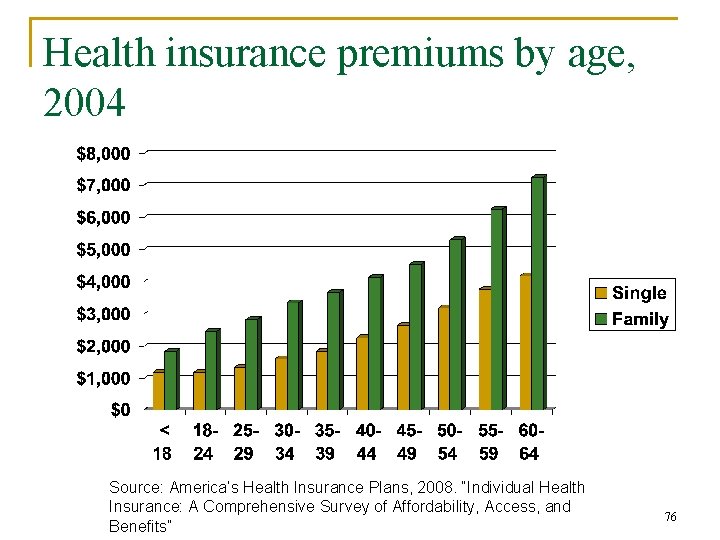
Health insurance premiums by age, 2004 Source: America’s Health Insurance Plans, 2008. “Individual Health Insurance: A Comprehensive Survey of Affordability, Access, and Benefits” 76
Adverse selection: Harvard University Problem: n n 1994, Harvard University was facing a substantial deficit in the employee benefits budget. Offered both HMO plans and a more expensive PPO health insurance plan. Harvard generously subsidized the more expensive, “high-option” PPO plans for employees. Needed to determine how to reduce employee benefits 77

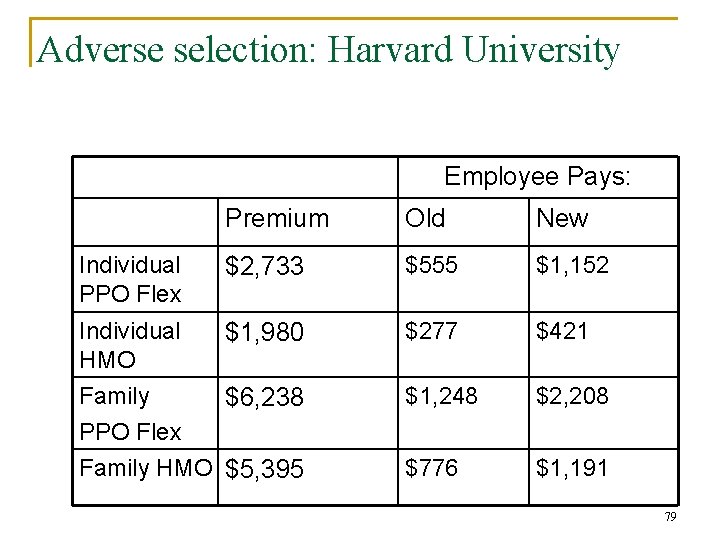
Adverse selection: Harvard University Strategy: n 1995, Harvard decide to contribute the same amount to employee plans regardless of which type they chose n Employee contributions increased for both the HMO and PPO plans, but more severely in the more expensive PPO plans. 78
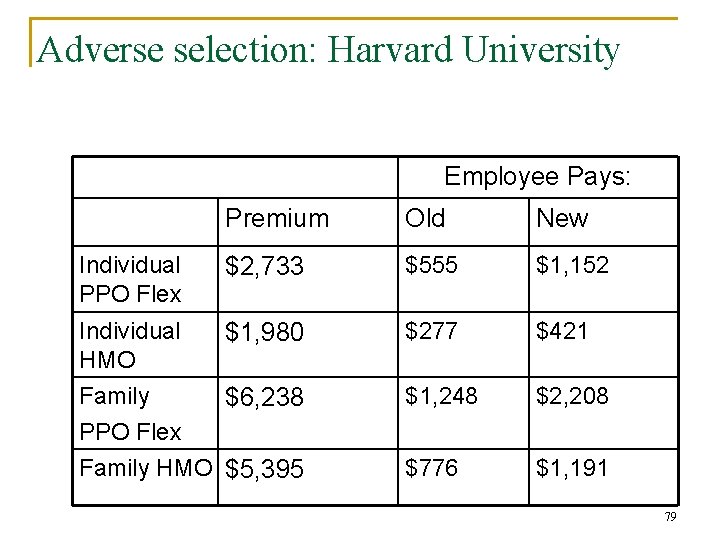
Adverse selection: Harvard University Employee Pays: Premium Old New $2, 733 $555 $1, 152 Individual $1, 980 HMO Family $6, 238 PPO Flex Family HMO $5, 395 $277 $421 $1, 248 $2, 208 $776 $1, 191 Individual PPO Flex 79
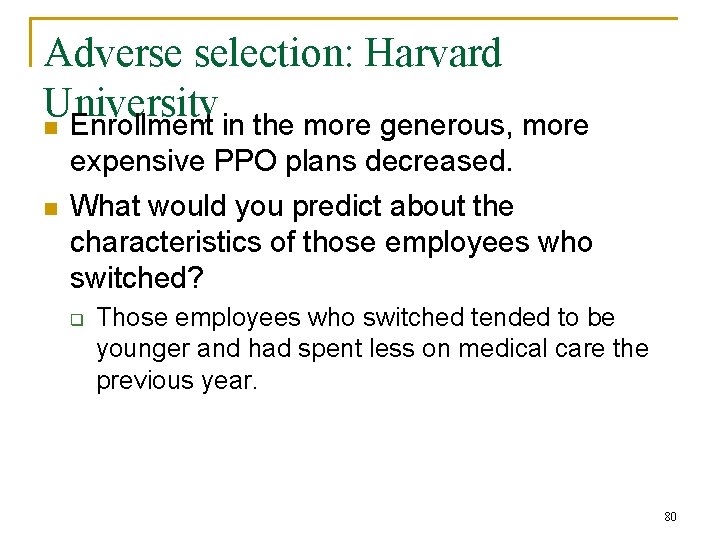
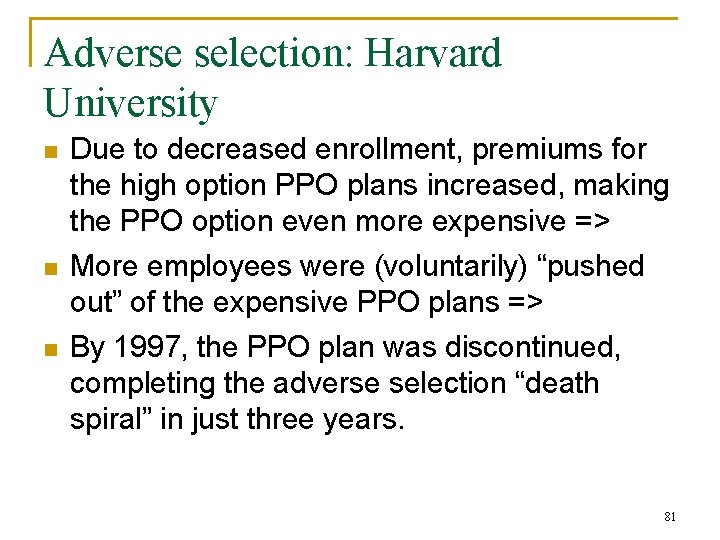
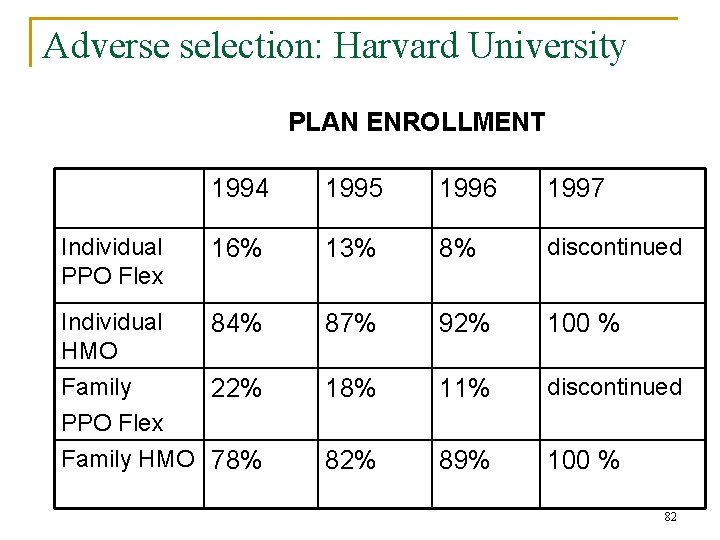
Adverse selection: Harvard University n Enrollment in the more generous, more n expensive PPO plans decreased. What would you predict about the characteristics of those employees who switched? q Those employees who switched tended to be younger and had spent less on medical care the previous year. 80
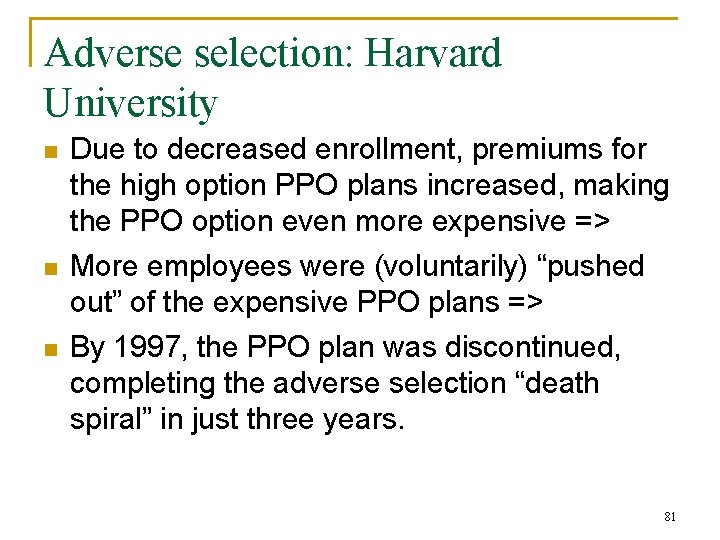
Adverse selection: Harvard University n n n Due to decreased enrollment, premiums for the high option PPO plans increased, making the PPO option even more expensive => More employees were (voluntarily) “pushed out” of the expensive PPO plans => By 1997, the PPO plan was discontinued, completing the adverse selection “death spiral” in just three years. 81
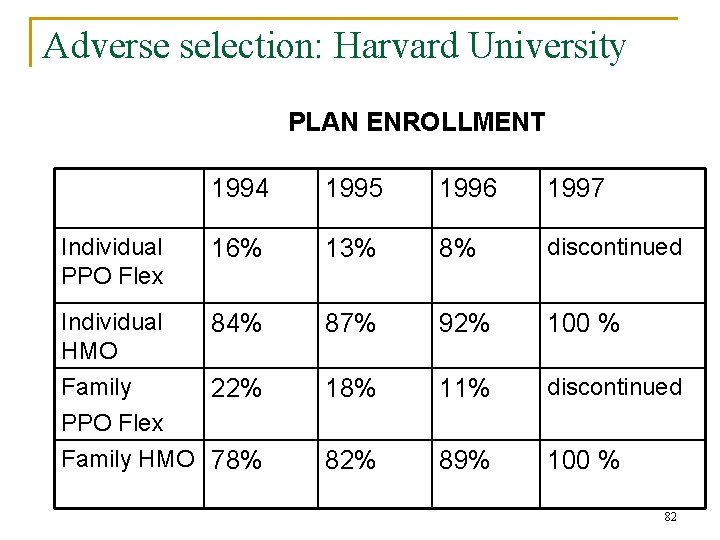
Adverse selection: Harvard University PLAN ENROLLMENT 1994 1995 1996 1997 16% 13% 8% discontinued Individual 84% HMO Family 22% PPO Flex Family HMO 78% 87% 92% 100 % 18% 11% discontinued 82% 89% 100 % Individual PPO Flex 82
Outline n n Uninsured in the US Demand for Insurance q q n Problem with demand for insurance q q n n Moral hazard Adverse selection Problems with the health insurance market (Cutler) Health insurance features Insurance and demand for medical care Supply of insurance q q q n What is insurance – risk pooling What is risk aversion Demand for insurance Factors affecting demand for insurance Fee-for-service Managed care Consumer-driven health plans and health savings accounts US health insurance market a brief history 83
Problems with the health insurance market (Cutler, 1994) n Insurance is over “experience rated” 3 types of health care costs. q n n n q Those individuals can control (smoking) Costs that are not controllable but predictably related to characteristics of the group (age). Costs which are truly random factors (for unforeseen diseases or accidents). He suggests that individual costs should be experience rated to ensure people face the true cost of their habits 84

Problems with the health insurance market (Cutler, 1994) q q For predictable but uncontrollable costs it is essentially a distributional issue (should the young subsidize the old) For random costs, it is natural to pool costs. n For individual or employees of small firms their premiums are large and variable often making them unsustainable. n He argues for community ratings- charge everyone the same rate based on age or location. n But the bigger the pool of people the better, so why stop at community? 85
Question: why is small group health insurance so expensive? n Loading cost: administrative and other costs associated with underwriting insurance policies q n n n Per capita loading costs decrease as firm group size increases Loading costs = (risk premium + administrative costs + marketing costs + profits) Small group purchasers have less bargaining power Risk pool is smaller, and if a sick person less people to spread the costs Adverse selection 86

Typical loading fees by group size As a percent of benefits (Phelps, p. 343) 87
Outline n n Uninsured in the US Demand for Insurance q q n Problem with demand for insurance q q n n Moral hazard Adverse selection Problems with the health insurance market (Cutler) Health insurance features Insurance and demand for medical care Supply of insurance q q q n What is insurance – risk pooling What is risk aversion Demand for insurance Factors affecting demand for insurance Fee-for-service Managed care Consumer-driven health plans and health savings accounts US health insurance market a brief history 88

Health insurance features n Co-insurance q n Deductibles q n Insurer covers all costs until some upper limit is reached Indemnity (Co-pays) q n Patient pays a fixed amount out of pocket, then insurance company pays all additional costs Maxiumum/limit q n Consumer pays a fixed percent of the cost (say 20%) and the insurance company picks up the rest Insurer pays fixed amount per unit of service (e. g. Physician office visit) and patient pays any additional costs Mixed 89
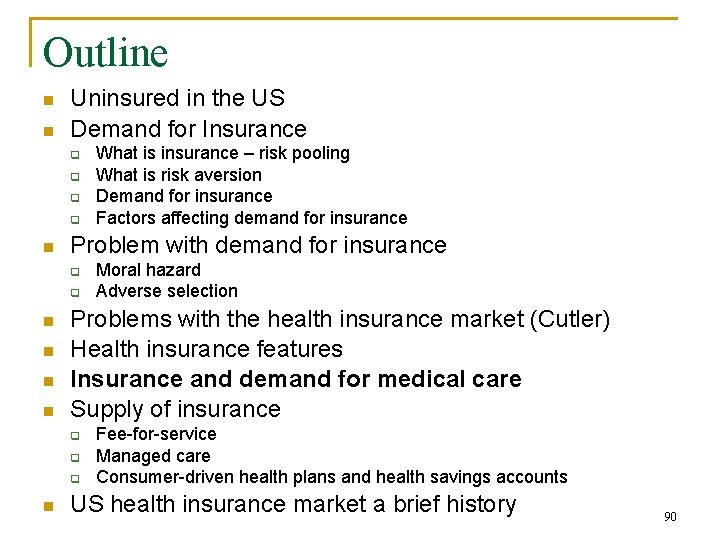
Outline n n Uninsured in the US Demand for Insurance q q n Problem with demand for insurance q q n n Moral hazard Adverse selection Problems with the health insurance market (Cutler) Health insurance features Insurance and demand for medical care Supply of insurance q q q n What is insurance – risk pooling What is risk aversion Demand for insurance Factors affecting demand for insurance Fee-for-service Managed care Consumer-driven health plans and health savings accounts US health insurance market a brief history 90
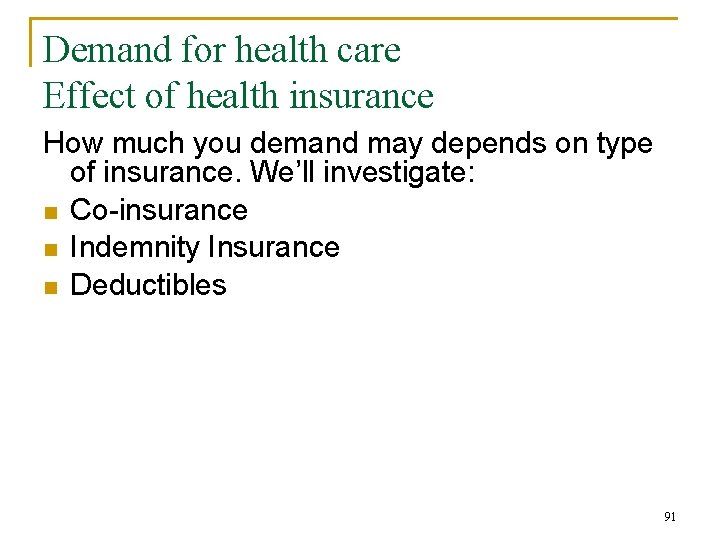
Demand for health care Effect of health insurance How much you demand may depends on type of insurance. We’ll investigate: n Co-insurance n Indemnity Insurance n Deductibles 91

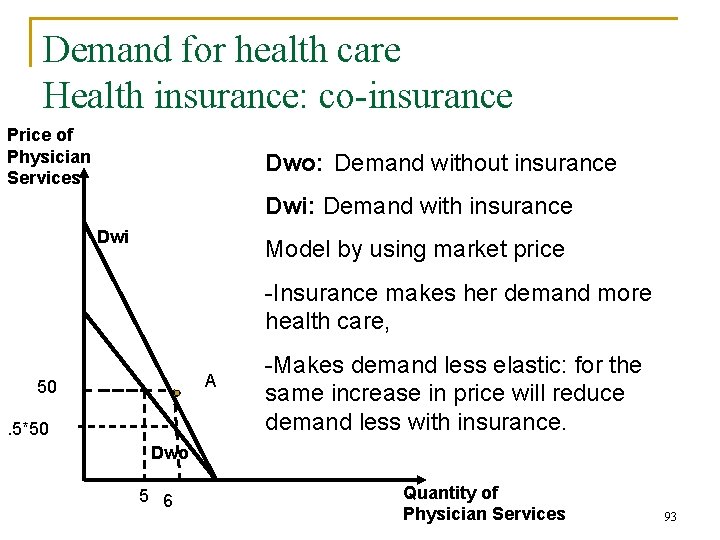
Demand for health care Health insurance: co-insurance Price of Physician Services Dwo: Demand without insurance Effective Price: Amount paid out of pocket Model using DWO curve Assume: . 5 co-insurance Consumer pays without insurance 50 Consumer Pays with insurance . 5*50 Demand increased by one unit Dwo 5 6 Quantity of Physician Services 92
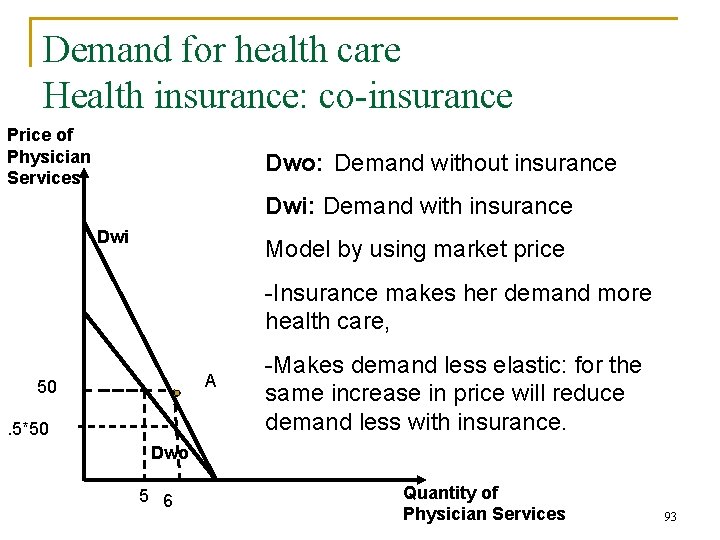
Demand for health care Health insurance: co-insurance Price of Physician Services Dwo: Demand without insurance Dwi: Demand with insurance Dwi Model by using market price -Insurance makes her demand more health care, A 50. 5*50 -Makes demand less elastic: for the same increase in price will reduce demand less with insurance. Dwo 5 6 Quantity of Physician Services 93
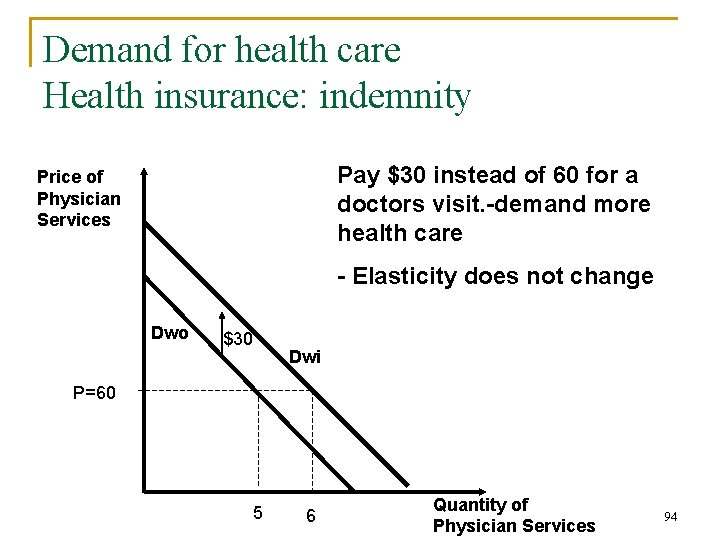
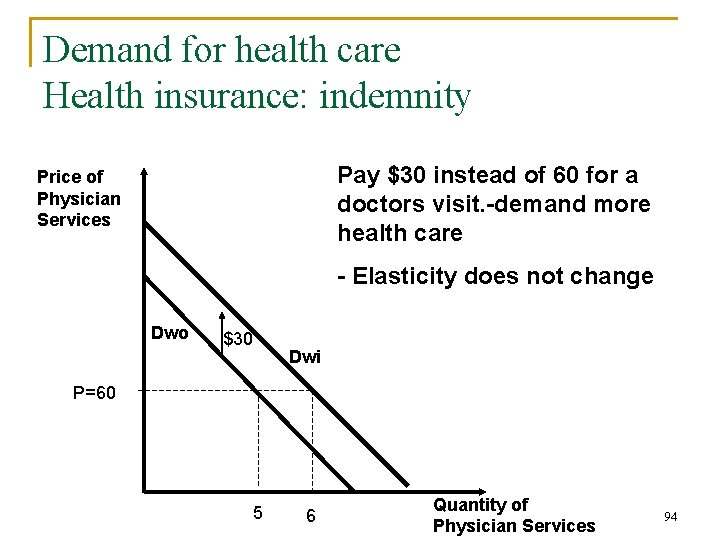
Demand for health care Health insurance: indemnity Pay $30 instead of 60 for a doctors visit. -demand more health care Price of Physician Services - Elasticity does not change Dwo $30 Dwi P=60 5 6 Quantity of Physician Services 94
Demand for health care Health insurance: deductible Purpose of deductible is to lower cost for insurance company 1. Reduce administrative costs because lower number of small claims. 2. May lower demand for medical care q n Depends on cost of the medical episode Small costs small problem may not demand health care, big costs you are more likely to get the health care. 95
Demand for health care Health insurance: deductible cont. q q Time when medical care is demanded n If close to time when deductible is reset, may wait for care n If just after deductible has started more likely to have care Probability of needing additional medical care in the remainder of the deductible period. n If know definitely will meet deductible, won’t wait to go to doctor. 96
Outline n n Uninsured in the US Demand for Insurance q q n Problem with demand for insurance q q n n Moral hazard Adverse selection Problems with the health insurance market (Cutler) Health insurance features Insurance and demand for medical care Supply of insurance q q q n What is insurance – risk pooling What is risk aversion Demand for insurance Factors affecting demand for insurance Fee-for-service Managed care Consumer-driven health plans and health savings accounts US health insurance market a brief history 97
Three important insurance markets Three important insurance types in the US are 1. Fee-for-service 2. Managed care (associated with capitation) 3. Consumer-driven health plans and health savings accounts 98
Fee-For-Service Popular system before the 1990 s § Patients choose medical provider § No gatekeeper: can go to any doctor and ask for any services n Doctors are reimbursed for each service they provide by the insurance company q n n n Physicians have a schedule of fees, and so did insurance companies and the lower of the two would be paid Providers (doctors) had autonomy over what care to prescribe and how to practice medicine Doctors tended to have independent practices Insurer manages the financial risk and pays usual, customary, or reasonable charges 99
Fee-For-Service Problems with fee-for-service: n No restraint on supply-side q With asymmetric information, problem of supplier induced demand. (over prescribing) n q q Doctors know more than patients so prescribe things that patient doesn’t really need No incentives to find most cost-effective way to deliver care. Saw excess supply of hospital beds, nursing staff etc n Could be so doctors had room to maximize income 100
Fee-For-Service n No demand constraint q q n n Often no co-payments Could choose what doctor, hospital, and specialists These two problems lead to over-utilization and high health care costs Policy options q q Gate keepers, must go to primary care physician before go onto specialist Second or third opinions, must seek second opinions before expensive care given (another doctor who would not have the profit motive) Co-payments 101 Managed-care a major response in US
Managed care Key features: 1. Patient care is provided through a network or organization of providers (hospitals, physician, clinics etc). q q Patient must use the preferred providers or will pay more Organization is held clinically and fiscally responsible go the outcomes and health status of the population served 102
Managed care 2. Utilization review: centralized reviews of the appropriateness of provider practices (i. e. doctor told if they are over prescribing or not using the most cost-effective care by administration) q q Doctors don’t like this because they can’t practice how they want to integrate financing and delivery of health care Goal is to provide cost-effective and comprehensive health care 103
Managed care 3. Selective contracting: payers negotiate prices and contract selectively with local providers (physicians and hospitals q Distinguishing characteristic from fee-for-service q Patient must use the preferred providers or will pay more 4. Gatekeeper: must see a primary physician who needs to prescribe any specialty services 104
Managed care 5. Doctors payment: Capitated rate per member per month q n n n q q i. e. doctor paid a set amount per patient, if don’t use it all keep the rest, if use more have to finance themselves Stop loss provision in contract. Specifies the total over the capitation rate per member before must be paid more. Reinsurance again large losses Yearly salary: may be adjusted for patient load Negotiated fee-for services (for some kinds) 105
Managed care These features could lead to lower cost and better quality care Capitation: q Introduce a budget constraint onto the supply side n q q More volume means less profit Creates an incentive to keep people healthy, prevention emphasized Incentive to choose most cost-effective way to provide care 106
Managed care Utilization review: q q Incentive to choose most cost-effective way to provide care Incentive to provide only needed care Gatekeeper: q Introduces a demand constraint Networks: q May provide better quality care since better communication between different doctors looking after case 107
Managed care Competition among hospitals: n 2004, approx. 41% of hospitals reported having revenue from capitated contracts n Managed care organizations often only contract with one hospital in the area q Hospitals compete on price to get these contracts n Note the competition for fee-for-service payment to hospitals increased price as they competed on quality and number of services 108
Managed care Types of Managed Care Organizations (MCOs): 1. Health Maintenance Organizations (HMOs): q q Example Kaiser Provide comprehensive health care. Usually entail few out-of-pocket expenditures. Must use services provided by the HMO doctors or network n q Primary care physician is the gatekeeper n n q Tend to hire all personal and have them as salaried staff. Must see primary care physician and have them authorize any care you get Choose a primary care physician and can’t see others Unauthorized care is not reimbursed 109
Managed care 2. Preferred Provider Organization (PPO) q Consumer given two choices of plans Use in-network providers and have a lower deductible and co-payment Use out of network providers but pay a higher out-of-pocket costs. 1. 2. q q So financial incentives provided to encourage use of network providers. Usually no gatekeeper system 110
Managed care q Organization contracts with physicians and hospitals to provide services at below average cost (i. e. negotiates prices for services). n n q q q These are the people that become in-network providers Usually does not use capitation No guarantee provider will see patients under the plan About half require a mandatory second opinion for recommended surgery. Some kind of utilization review is usually done. 111
Managed care 3. Point-of-service (POS) q q Hybrid of HMO and PPO Like PPO, two tier coverage n q In network much cheaper than out-of-network. Like HMO, each member is assigned to a physician gate-keeper, who must authorize innetwork care in order for the care to be covered on the in-network terms. 112
Growth in managed care n Growth of managed care was slow q Historic opposition by organized medicine groups to managed care n n Took away patient choice of doctor Threatened ability of doctors to earn excess profits q Under fee-for-service can price discriminate § q Charge different fee for the same services Not possible to price discriminate due to capitated or negotiated fees 113

Growth in managed care n HMO Act 1973: q q q n Enabled HMOs to become federally qualified if they provided comprehensive benefits and some other requirement Loan guarantees and grants for startup costs provided Qualified HMOs could require firms in the area with 25 or more employees to offer the HMO as an option Still no real expansion until the 1980 s q q Medicare and Medicaid switching to HMOs Number of HMOs grew from 235 in 1980 to 623 in 1986 114
Growth in managed care n Really expanded in the 1990 s q n 2000 s q n First HMOs expanded n HMOs consolidated n Enrollment in HMOs increased from 33 million in 1990 to 81 million in 2000 HMO enrollments decreased but PPOs are expanding rapidly n Provider greater choice of doctors (more expensive than HMO) See Figure 12 -1 FGS 115
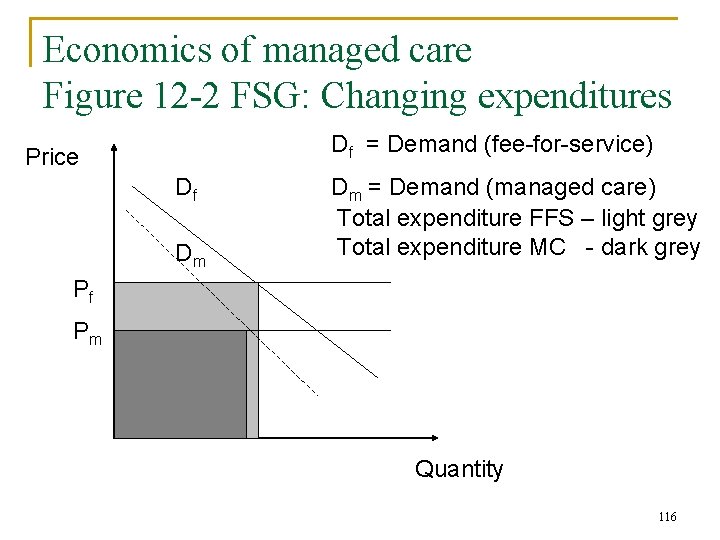
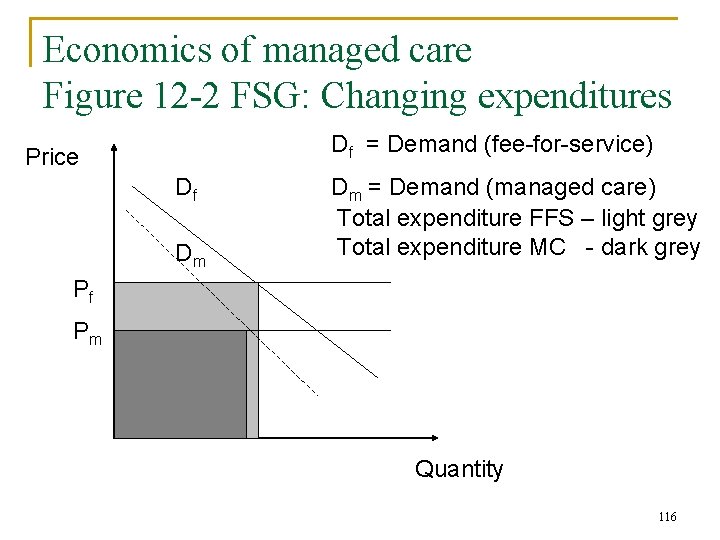
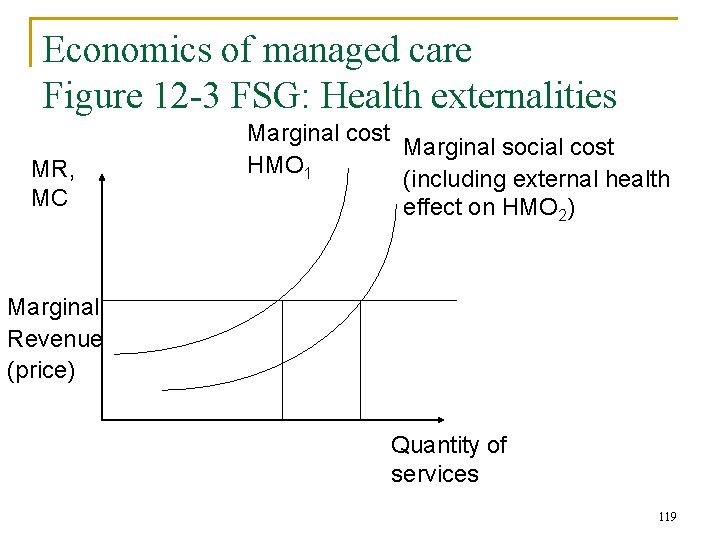
Economics of managed care Figure 12 -2 FSG: Changing expenditures Df = Demand (fee-for-service) Price Df Dm Dm = Demand (managed care) Total expenditure FFS – light grey Total expenditure MC - dark grey Pf Pm Quantity 116

Economics of managed care Predictions using economic theory: 1. Factors leading to a decrease in price q Exerts market power to lower prices from Pf to Pm Only possible when had been earning economic profits 2. Factors leading to the decrease in demand n q q n Reduce inpatient care by keeping patients healthier, using alternatives which are more cost-effective Limiting length of stays Minimizing supplier induced demand Encouraging more cost-effective care though information technology and financial incentives to providers Tradeoff q Constraint on consumer choice of doctors 117
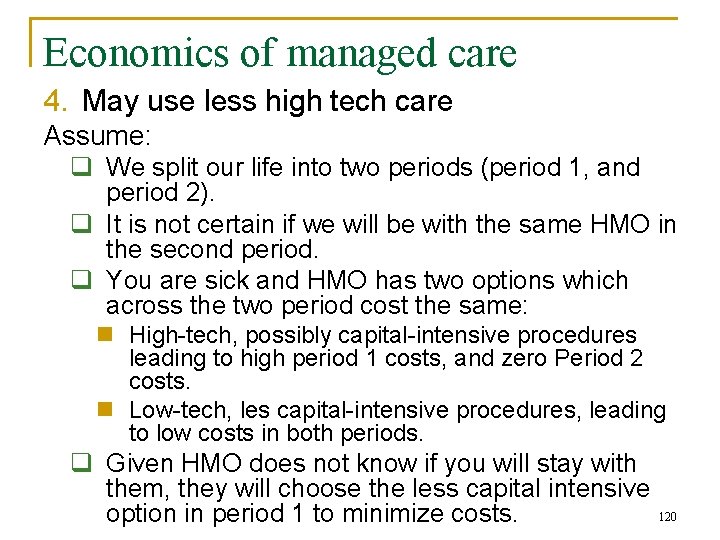
Economics of managed care 3. Amount of care provided by managed care organization may provide less care than is optimal q q We want good health over our life-time HMO wants to minimize costs since receives a constant revenue per patient each year n If they believe their patients will not stay in the HMO for a long period of time q q q Provide cheaper care in the short-term to minimize costs, even if it mean higher long term costs May mean the other HMOs have higher long-term costs if the patient moves to a different HMO This is called a negative externality 118
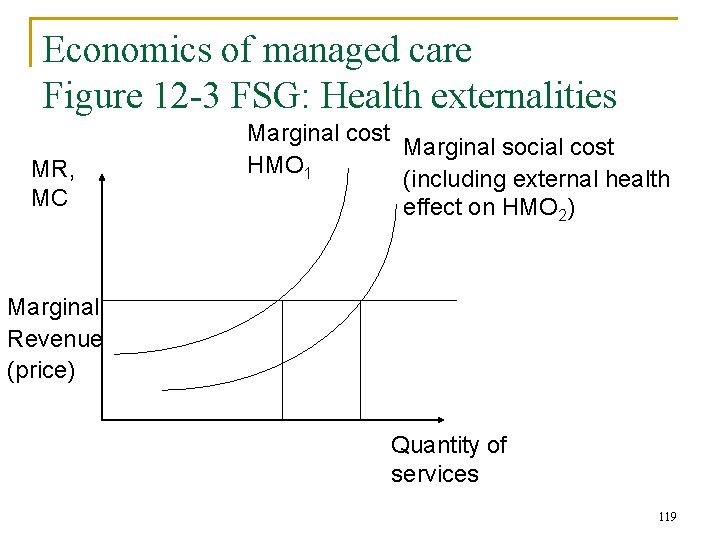
Economics of managed care Figure 12 -3 FSG: Health externalities MR, MC Marginal cost Marginal social cost HMO 1 (including external health effect on HMO 2) Marginal Revenue (price) Quantity of services 119
Economics of managed care 4. May use less high tech care Assume: q We split our life into two periods (period 1, and period 2). q It is not certain if we will be with the same HMO in the second period. q You are sick and HMO has two options which across the two period cost the same: n High-tech, possibly capital-intensive procedures leading to high period 1 costs, and zero Period 2 costs. n Low-tech, les capital-intensive procedures, leading to low costs in both periods. q Given HMO does not know if you will stay with them, they will choose the less capital intensive 120 option in period 1 to minimize costs.
Managed care Potential Problems with MCOs: 1. Dumping: refusing to treat less healthy patients who might use services in excess of their premiums. Say the organization is not equipped to treat certain patients. FFS won’t do this because charge for all services given. q q 2. Creaming: Seeking to attract more healthy patients who will use services costing less than their premiums q FFS may do this if reimbursement rates are not high enough 121
Managed care 3. Skimping: Providing less than optimal quantity of services for any given condition q FFS won’t do this because can charge for each service given 4. Poor Quality: If patients don’t stay in MCO long, may not pay MCO to provide preventative or quality care, since they will not reap the lower future health care costs from these efforts q q FFS may do this if reimbursement rates are not high enough On the flip side MCO may promote more preventive care than under FFS – depends on how fast the rewards are reaped. FFS don’t like to do it because reimbursement rates often low for preventive care. 122

Impact of managed care Recap: Predictions n Theory predicts that MC compared to FFS: q q q n Increase utilization of preventive services Reduce utilization or more costly service (partly by more preventive care) – hospital care Lower health care costs Capitation raises some concerns q Reduced quality/quantity of care: n n n Skimming – provide less than optimal care Use lower technology solutions Could result in poor health outcomes 123
Impact of managed care Recap: Predictions n Adverse selection q q q Healthier patients select into MC given lower costs Riskier select MC due to more comprehensive benefits and community rating Healthier patients due to cream skimming and dumping by plans. What happens in reality? 124
Impact of managed care Methodological issues n Methodologically difficult to find empirical evidence q Could compare health care costs, and quality for all those who are under FFS and all those under managed care. 125

Impact of managed care Methodological issues n Problem 1: q q If utilization decreases is this because the managed care organization is reducing necessary care, or because the population is healthier due to more preventive care therefore not needing as much care altogether. Need to look at outcomes that will separate out these effects. 126
Impact of managed care Methodological issues n Problem 2: SELECTION BIAS q Do the same types of people choose FFS and managed care? q No, sicker people more likely to choose FFS so health care costs for those people will be higher n n Expenditure may be higher not because FFS more expensive, but because they have a sicker population May also find FFS uses more technology. Not because of incentives but because they have a sicker population and more high tech care is more likely to be needed. Very hard to control for how sick someone is. Comparing two very different populations so may not have people with the exact same types of sickness in both groups. 127
Impact of managed care Methodological issues n To do analysis well really need to randomize people into FFS or managed care – or to find a policy experiment where people are forced to move from one to the other due to a mandate 128
Impact of managed care Empirical evidence n Selection q Evidence that the healthier select into managed care plans n n 10 -30% lower utilization prior to switch for nonelderly population Greater differences among Medicare population q n Riley et al (1994) – Medicare patients entering HMO had 37 % lower than average costs while those exiting had 60% higher than average costs Need to worry about selection bias when examining impact on costs, utilization and quality 129
Managed care Empirical evidence n Utilization q Confounded by selection issues n q Evidence on selection means there would be lower utilization due to healthier population in managed care Early studies of HMOs (reviewed by Luft, 1981) n n n Studies are confounded Lower inpatient admission rates Mixed effects on length of stay Overall lower average number of inpatient days Great likelihood of number of outpatient visits 130
Managed care Empirical evidence q Rand Health Experiment (Manning et al. 1984) Randomized experiment n 2, 353 individuals randomly assigned to either: q q q n FFS physician of their choice (431 people) HMO (1, 149) Control group: HMO people who had been in the HMO the year before. The FFS people where then randomized into one of four groups. q q Free care Pay 25% of expenses up to max of $1, 000 out of pocket Pay 95% of expenses up to max of $1, 000 out of pocket 95% co-insurance on outpatient services, up to a max of $150 person or $450 per family 131
Managed care Empirical evidence n n n See Table 12 -3 FSG for results HMO findings consistent with non-experimental findings Less inpatient hospital use More outpatient use Costs: q Rand Health Experiment n n n Lower inpatient costs Higher, but not significantly, outpatient costs Overall costs 28% lower than under “free care” plan 132
Managed care Empirical evidence n Prices q Mixed evidence n Some evidence that managed care plans effective in obtaining lower prices for care q n Tied to monopsony power Other find higher prices q Depends on the market, including monopoly power of hospitals, excess or non-excess capacity of provider in the market 133

Managed care Empirical evidence n Innovation/Adoption of new technology q Mixed evidence n n Early studies found positive association between managed care penetration and use of new technology More recent studies find slower diffusion of new technology where managed care penetration in higher Some find no differences Recent literature on a number of issues q Miller and Luft, 2002 – Table 12 -4 FSG 134
Managed care Empirical evidence Costs: 2 questions a) Do they reduce the level of costs? n n q Use more cost-effective practices so as more people move to managed care the overall health care costs will go down. This is a one time cost decrease Evidence that the overall costs are reduce (Rand health experiment) 135

Managed care Empirical evidence b) Do they reduce the growth in costs (trends) n q q Reduce the percent increase in costs each year. Earlier studies found that growth in costs about the same between FFS and managed care. More recent studies find slower rates of growth under managed care plans (up to 1 percentage point a year) 136

Consumer-driven health plans and health savings accounts n New approach to health insurance n Response to: q q n Renewed growth in health care costs n Move in 2000 s from HMOs to PPOs may be partly responsible for this Continued growth in health insurance premiums Backlash against restricted choice in managed care Growth in information technology Emphasizes q q q Greater consumer control over health care spending Making consumer sensitive to cost of care Allowing consumer to choose provider, but to also pay for 137 the differences in the costs of the providers
Consumer-driven health plans and health savings accounts Consumer Drive Health Care: Typical package n High deductible/catastrophic health insurance plan (typically PPO type) q Individual deductible may be $3, 000, more for families n q Co-insurance: in-network co-insurance much cheaper than out of network. n q Must pay for all care up to $3, 000 after that the insurance company will pay. Even if reach deductible, still have to pay co-insurance Out-of-pocket maximum n n For individual may have a $5, 000 max One pay 5, 000 out-of-pocket don’t need to pay anymore. 138
Consumer-driven health plans and health savings accounts n Health savings account (HSA). Personal savings account used to pay for care q q q Only eligible for HSA if have a high deductible. Account is tax exempt. Don’t pay taxed on the money you contribute and don’t pay taxes when you take the money out Individual or employer may contribute up a fixed amount (e. g. 100 percent of deductible or $2, 700 per individual or $5, 450 per family in 2006). Can’t contribute more. 139
Consumer-driven health plans and health savings accounts q q q Can only take out money to pay for qualified health expenditures. Will pay a penalty if use it for anything else If you don’t spend the money one year it stays in your account and you can grow it through money market funds, mutual funds, CDs etc. Once reach 65, individuals can make nonqualified health withdrawals and only play the appropriate tax rate without any penalties. n n Problem with this is it is being used for tax evasion Used to save money tax free while pay a high tax rate. Then take money out when retired so are paying a low tax rate. Rich benefit more than poor. 140
Consumer-driven health plans and health savings accounts Advocate argue: n Consumers more likely: q q n Insurers: q n n Only get care they need since they have to pay much of the cost out-of-pocket Will choose cheaper or more cost-effective care since pay out-ofpocket Will be more likely to use cheaper drugs This will all lead to decrease in growth in health care costs. Still have incentive to managed costs once high deductible has been reached Benefit people of all risk levels by imposing caps on out-ofpocket spending. More people will insure because the costs of the plans are cheaper 141
Consumer-driven health plans and health savings accounts Opponents argue: n May decrease costs now but lead to higher costs later q People won’t pay for necessary care that keeps them healthy in the future n n May not get necessary preventive care or manage ongoing chronic conditions Leads to higher costs in the future q q n If can switch plan with lower out-of-pocket costs will do so. Otherwise, will be left pay high health care costs Detracts from risk pooling (purpose of insurance) q q Plan likely to attract the healthy Pay: low costs when healthy, high costs when unhealthy 142

Consumer-driven health plans and health savings accounts n n Difficult for individual to measure quality of care due to asymmetric information – not clear how easy it is for them to make the right choices Will not decrease the number of uninsured because they don’t have enough money to pay the high deductibles so no point getting the insurance 143
Consumer-driven health plans and health savings accounts q Choice of provider not really different if not rich n To keep prices down need to use in network provider q q Choice of provider has not changed Costs may go up with choice of provider n Can use out of network provided (choice) but will pay more q q No negotiated prices with out of network providers so they can charge much more If insurance covering costs once the max is hit this choice of providers will cost a lot more to the health care system 144

Consumer-driven health plans and health savings accounts n Early Evidence q q q Little use to date, but growing interest Some evidence that lower risk population more likely to choose this type of health care. n This is called favorable selection (healthier choosing to insure this way) Others suggest greater appeal to high income populations n Tax evasion n Can choose high cost providers and still have insurance pay for it when have expensive years n No trouble paying the 5, 000 or more out-of-pocket n Means there is may be little impact on reaching the uninsured 145
Outline n n Uninsured in the US Demand for Insurance q q n Problem with demand for insurance q q n n Moral hazard Adverse selection Problems with the health insurance market (Cutler) Health insurance features Insurance and demand for medical care Supply of insurance q q q n What is insurance – risk pooling What is risk aversion Demand for insurance Factors affecting demand for insurance Fee-for-service Managed care Consumer-driven health plans and health savings accounts US health insurance market a brief history 146
US health insurance market Brief history n Earliest health insurance dates to 1840 s q Sickness insurance n q n Limited supply of private insurance Some interest in public health insurance in the early 1900 s q q n Provided income during illness Teddy Roosevelt: Progressive party Opposed by American Medical Association and others “socialized medicine” 1920 s/1930 s see increasing demand for and supply of health insurance q Rising health care costs 147
US health insurance market Brief history 1929: Modern private health insurance n Dallas teachers contracted with Baylor University Hospital q q $6 annual payment paid in monthly installments 21 days of hospitalization 148
US health insurance market Brief history 1930 s & depression n Growth in similar prepaid health care plans with hospitals q q n Protect individuals from risk during period of low and falling incomes Guaranteed hospitals a steady income American Hospital Association created and organized several plans, e. g. Blue Cross q q Subscribers free choice of hospitals within a city Pre-paid policies covering fixed amount of hospital care with no deductible/copayments Premiums determined by community ratings Grow from 1, 300 to over 3 million covered from 1929 -1939149

US health insurance market Brief history n Blue Shield plans q Success of Blue Cross plans for hospital care led to the development of Blue Shield plans for physicians care. 1939: California physicians’ service plan n Covered all physician services q Physicians could charge patient above the amount they received from BS plan (cost-sharing) 150

US health insurance market Brief history 1940 s/1950 s n Growth in for-profit insurance companies q q q Success of BC/BS Health care costs increasing Employers offering health insurance as a benefit n n n q Gov’t imposed price and wage controls to curb inflation Only way employers could attract new workers was with fringe benefits. So offered private health insurance. These fringe benefits were not reported to IRS (tax-exempt) IRS eventually asked them to be included in wage bill Workers expressed alarm and congress passed the health insurance could remain tax exempt Use experience rating not community rating so could set lower premiums for some 151
US health insurance market Brief history 1960 s/1970 s n Increase in population covered by private health insurance q n n Most through employers Continued increase in comprehensiveness of policies Fueled by: q q Growth in incomes Tax treatment of insurance benefits n n Don’t pay tax on money going to health insurance Medicare/Medicaid introduced in mid-1960 s q See rise in health care expenditures 152
US health insurance market Brief history 1980/90 s n Increase in managed care (HMOs) n Medicare/Medicaid switching to managed care 2000 s n Increase in PPOs and introduction of consumer driven care and HSA 153
 Icss fgs
Icss fgs Moodle fgs
Moodle fgs Adverse selection
Adverse selection Adverse selection
Adverse selection Adverse selection
Adverse selection Adverse selection
Adverse selection What is adverse selection
What is adverse selection Adverse selection
Adverse selection What is adverse selection
What is adverse selection Tools to help solve adverse selection problems
Tools to help solve adverse selection problems Cartoon message
Cartoon message Moral hazard occurs when
Moral hazard occurs when Selezione avversa
Selezione avversa Moral hazard adalah
Moral hazard adalah Features of fire insurance
Features of fire insurance What happens if we leave afghanistan
What happens if we leave afghanistan Moral individu dan moral kelompok
Moral individu dan moral kelompok Moral de esclavos y moral de señores
Moral de esclavos y moral de señores Bambrough moral scepticism and moral knowledge download
Bambrough moral scepticism and moral knowledge download Balancing selection vs stabilizing selection
Balancing selection vs stabilizing selection Similarities
Similarities K selection r selection
K selection r selection Natural selection vs artificial selection
Natural selection vs artificial selection Difference between continuous and discontinuous variation
Difference between continuous and discontinuous variation Example of sexual selection
Example of sexual selection K selection r selection
K selection r selection Natural selection vs artificial selection
Natural selection vs artificial selection Two way selection and multiway selection
Two way selection and multiway selection Multiway selection in c
Multiway selection in c Procedure of pure line selection
Procedure of pure line selection Health hazard symbol
Health hazard symbol Health hazard
Health hazard Example of hazard
Example of hazard Ttuhsc writing center
Ttuhsc writing center Fau health insurance
Fau health insurance Umms employee benefits
Umms employee benefits Blue cross tonik plan
Blue cross tonik plan Ouhsc student health
Ouhsc student health Raksha health insurance tpa address
Raksha health insurance tpa address Ucf dental insurance
Ucf dental insurance Health insurance market segmentation
Health insurance market segmentation Deloitte health insurance
Deloitte health insurance What is deductible in health insurance
What is deductible in health insurance Health insurance premium payment program ny
Health insurance premium payment program ny Commonwealth health insurance connector authority
Commonwealth health insurance connector authority Chapter 14 health disability and life insurance
Chapter 14 health disability and life insurance Aditya birla nuvo health insurance
Aditya birla nuvo health insurance Uw madison student health insurance
Uw madison student health insurance Statewide health insurance benefits advisors
Statewide health insurance benefits advisors Paramounttpa
Paramounttpa Ceww health insurance consortium
Ceww health insurance consortium Religare health insurance franchise
Religare health insurance franchise Missouri state health insurance assistance program
Missouri state health insurance assistance program Ira b wilson
Ira b wilson Healthscope po box 99006 lubbock tx
Healthscope po box 99006 lubbock tx Pace university health insurance
Pace university health insurance Belgium student insurance
Belgium student insurance Chickasaw nation division of health
Chickasaw nation division of health Panabridge health insurance
Panabridge health insurance Keller isd health insurance
Keller isd health insurance Whirlpool health insurance
Whirlpool health insurance Early arrival student health insurance asu
Early arrival student health insurance asu Small business health insurance delaware
Small business health insurance delaware Delaware health insurance exchange
Delaware health insurance exchange Phi permanent health insurance
Phi permanent health insurance Uib hr portal
Uib hr portal Characteristics of health insurance
Characteristics of health insurance Allianz cern mpa
Allianz cern mpa Travel health insurance association annual conference
Travel health insurance association annual conference Unl student health insurance
Unl student health insurance Paramount prior authorization
Paramount prior authorization Free health insurance
Free health insurance Predictive analytics in health insurance
Predictive analytics in health insurance Wsu health and wellness pharmacy
Wsu health and wellness pharmacy Etsu health insurance
Etsu health insurance Ouhsc health club
Ouhsc health club New mexico medical insurance pool
New mexico medical insurance pool Dchr health insurance
Dchr health insurance Colorado health op
Colorado health op Chapman university health insurance
Chapman university health insurance Unit 2 lesson 3 health insurance and financial planning
Unit 2 lesson 3 health insurance and financial planning Unit 2 lesson 3 health insurance and financial planning
Unit 2 lesson 3 health insurance and financial planning Chip adultbasic health insurance
Chip adultbasic health insurance Ace health insurance
Ace health insurance Adverse reaction definition
Adverse reaction definition Near miss examples
Near miss examples Adverse reaction definition
Adverse reaction definition Adverse reaction definition
Adverse reaction definition Adverse events in hospital
Adverse events in hospital Ir adverse event
Ir adverse event Adverse events in hospital
Adverse events in hospital Paracetamol adverse effects
Paracetamol adverse effects Loop diuretics adverse effects
Loop diuretics adverse effects Paracetamol dose per kg
Paracetamol dose per kg Vildagliptin renal dose adjustment
Vildagliptin renal dose adjustment Azalastyna
Azalastyna Harley nadler
Harley nadler Diuretic classification
Diuretic classification Hayanil drug
Hayanil drug Adverse treatment
Adverse treatment If you are driving under adverse conditions
If you are driving under adverse conditions 5.2 driving in adverse conditions assignment
5.2 driving in adverse conditions assignment Adverse event adalah
Adverse event adalah Fetal warfarin syndrome mnemonic
Fetal warfarin syndrome mnemonic Beta blocker examples
Beta blocker examples Beta adrenergic blockers action
Beta adrenergic blockers action Alpha blockers
Alpha blockers Adverse effect of alpha blockers
Adverse effect of alpha blockers Adverse childhood experiences study
Adverse childhood experiences study Adverse yaw
Adverse yaw Adverse childhood experiences study
Adverse childhood experiences study Adverse event
Adverse event Novartis adverse event reporting
Novartis adverse event reporting Adverse childhood experiences study
Adverse childhood experiences study Adverse
Adverse Adverse yaw
Adverse yaw Unanticipated problem vs adverse event
Unanticipated problem vs adverse event Adverse event crf
Adverse event crf Adverse childhood experiences powerpoint
Adverse childhood experiences powerpoint What are adverse childhood experiences
What are adverse childhood experiences Ae coding
Ae coding Definition of adverse event
Definition of adverse event When your headlights shine into fog, *
When your headlights shine into fog, * Chapter 12 driving in adverse conditions
Chapter 12 driving in adverse conditions Serious adverse event reconciliation
Serious adverse event reconciliation Adverse food reactions
Adverse food reactions Adverse events following immunization (aefi) course answers
Adverse events following immunization (aefi) course answers No adverse remarks meaning
No adverse remarks meaning Ahca adverse incident reporting
Ahca adverse incident reporting Roles of occupational health nurse
Roles of occupational health nurse National health intervention programme for mother and child
National health intervention programme for mother and child Louisiana department of health and hospitals
Louisiana department of health and hospitals Similarities between health education and health promotion
Similarities between health education and health promotion Whole health circle of health
Whole health circle of health Health and social care component 3 health and wellbeing
Health and social care component 3 health and wellbeing Health promotion world health organization
Health promotion world health organization University of central florida health care administration
University of central florida health care administration Chapter 3 health wellness and health disparities
Chapter 3 health wellness and health disparities Health education and propaganda
Health education and propaganda Chapter 1 lesson 2 what affects your health
Chapter 1 lesson 2 what affects your health Chapter 1 health and wellness fundamentals
Chapter 1 health and wellness fundamentals Optimal health in each of the six components of health
Optimal health in each of the six components of health Primary and secondary effects of a tectonic hazard
Primary and secondary effects of a tectonic hazard Four main components of whmis 2015
Four main components of whmis 2015 Good hazard scenarios describe where it is happening
Good hazard scenarios describe where it is happening Hazards of hand tools
Hazards of hand tools Primary and secondary effects of a tectonic hazard
Primary and secondary effects of a tectonic hazard Interim hazard classification
Interim hazard classification Examples physical hazards
Examples physical hazards Hazard management cycle vs park model
Hazard management cycle vs park model Tectonic hazard profile
Tectonic hazard profile Toolbox talk risk assessment
Toolbox talk risk assessment Pictogram physical hazard
Pictogram physical hazard Hazardele geomorfologice
Hazardele geomorfologice