Characteristics of the U S Health Care System
- Slides: 25
Characteristics of the U. S. Health Care System DRAFT – Private and Confidential
Learning Objectives 4 Understand the importance of health and health care to American life 4 Identify and analyze defining characteristics of the US health care system 4 Identify major issues and concerns with the current system 2
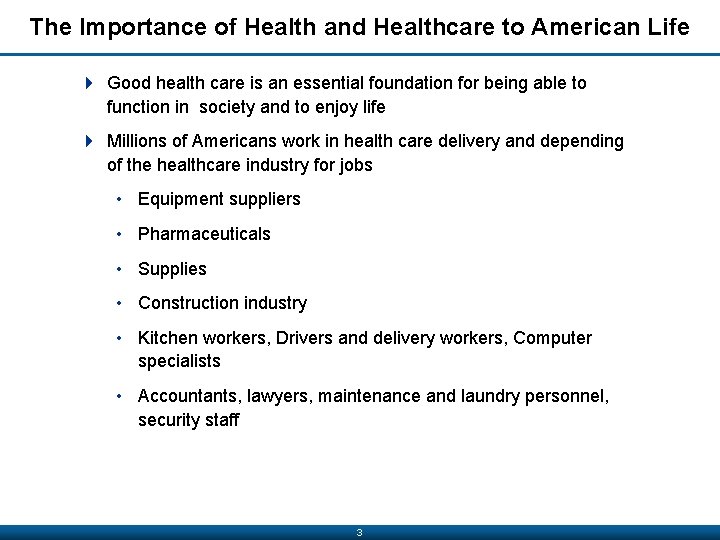
The Importance of Health and Healthcare to American Life 4 Good health care is an essential foundation for being able to function in society and to enjoy life 4 Millions of Americans work in health care delivery and depending of the healthcare industry for jobs • Equipment suppliers • Pharmaceuticals • Supplies • Construction industry • Kitchen workers, Drivers and delivery workers, Computer specialists • Accountants, lawyers, maintenance and laundry personnel, security staff 3
Historical Perspective DRAFT – Private and Confidential
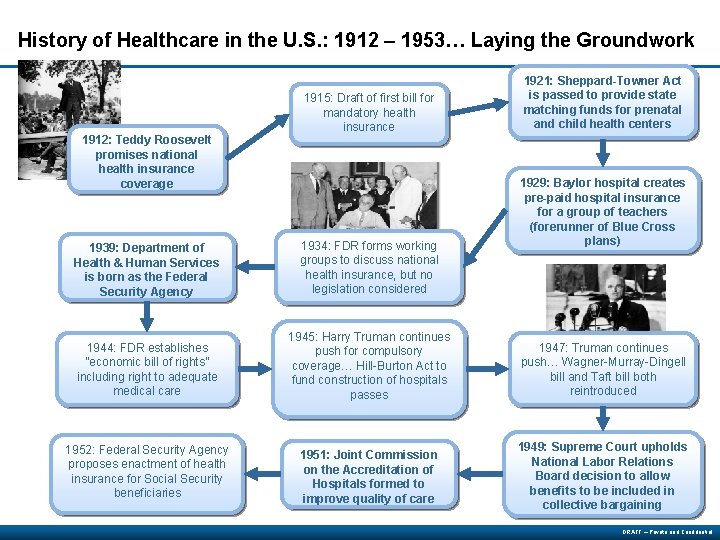
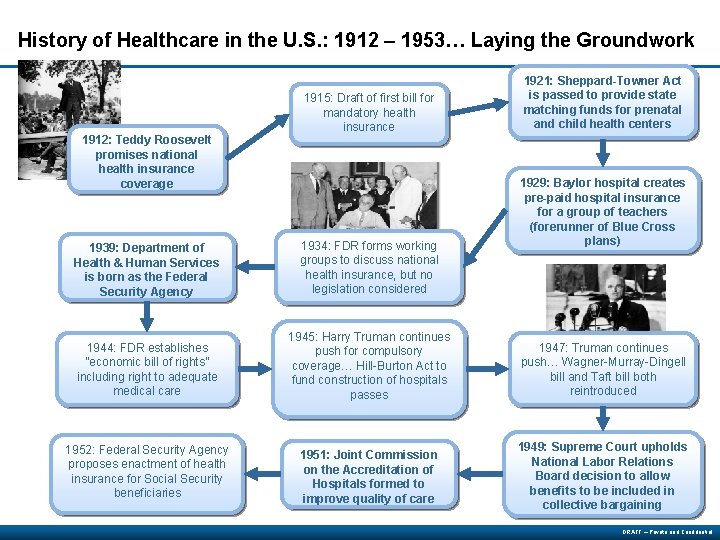
History of Healthcare in the U. S. : 1912 – 1953… Laying the Groundwork 1915: Draft of first bill for mandatory health insurance 1912: Teddy Roosevelt promises national health insurance coverage 1921: Sheppard-Towner Act is passed to provide state matching funds for prenatal and child health centers 1929: Baylor hospital creates pre-paid hospital insurance for a group of teachers (forerunner of Blue Cross plans) 1939: Department of Health & Human Services is born as the Federal Security Agency 1934: FDR forms working groups to discuss national health insurance, but no legislation considered 1944: FDR establishes “economic bill of rights” including right to adequate medical care 1945: Harry Truman continues push for compulsory coverage… Hill-Burton Act to fund construction of hospitals passes 1947: Truman continues push… Wagner-Murray-Dingell bill and Taft bill both reintroduced 1952: Federal Security Agency proposes enactment of health insurance for Social Security beneficiaries 1951: Joint Commission on the Accreditation of Hospitals formed to improve quality of care 1949: Supreme Court upholds National Labor Relations Board decision to allow benefits to be included in collective bargaining DRAFT – Private and Confidential
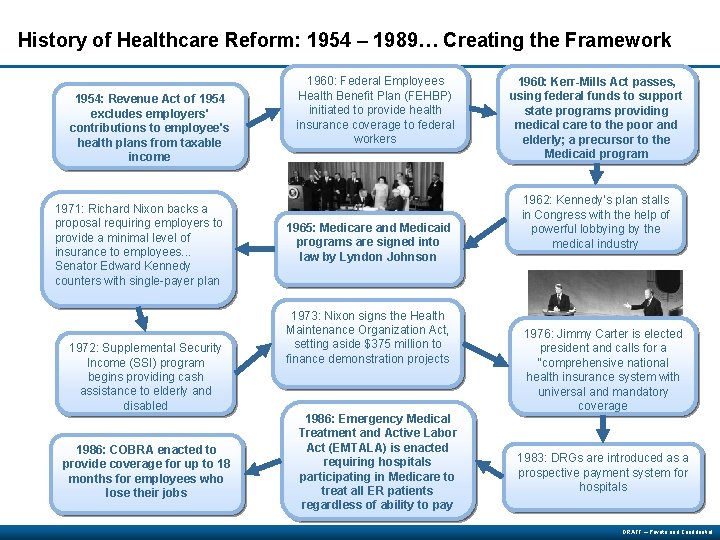
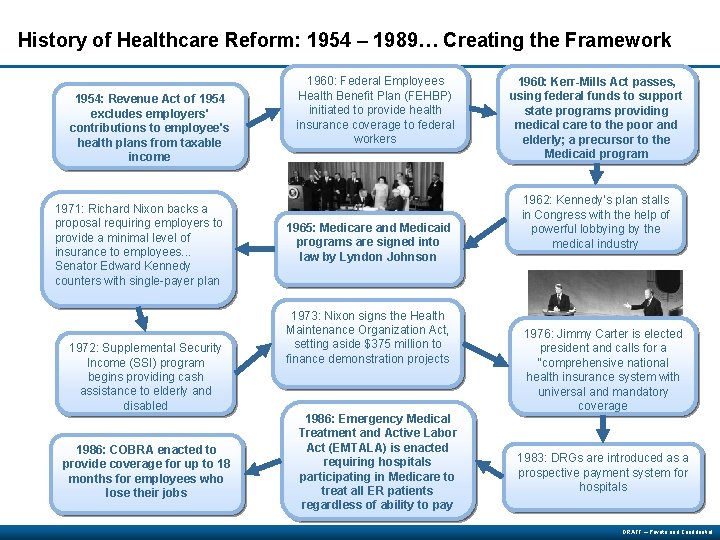
History of Healthcare Reform: 1954 – 1989… Creating the Framework 1954: Revenue Act of 1954 excludes employers' contributions to employee's health plans from taxable income 1971: Richard Nixon backs a proposal requiring employers to provide a minimal level of insurance to employees. . . Senator Edward Kennedy counters with single-payer plan 1972: Supplemental Security Income (SSI) program begins providing cash assistance to elderly and disabled 1986: COBRA enacted to provide coverage for up to 18 months for employees who lose their jobs 1960: Federal Employees Health Benefit Plan (FEHBP) initiated to provide health insurance coverage to federal workers 1965: Medicare and Medicaid programs are signed into law by Lyndon Johnson 1973: Nixon signs the Health Maintenance Organization Act, setting aside $375 million to finance demonstration projects 1986: Emergency Medical Treatment and Active Labor Act (EMTALA) is enacted requiring hospitals participating in Medicare to treat all ER patients regardless of ability to pay 1960: Kerr-Mills Act passes, using federal funds to support state programs providing medical care to the poor and elderly; a precursor to the Medicaid program 1962: Kennedy’s plan stalls in Congress with the help of powerful lobbying by the medical industry 1976: Jimmy Carter is elected president and calls for a “comprehensive national health insurance system with universal and mandatory coverage 1983: DRGs are introduced as a prospective payment system for hospitals DRAFT – Private and Confidential
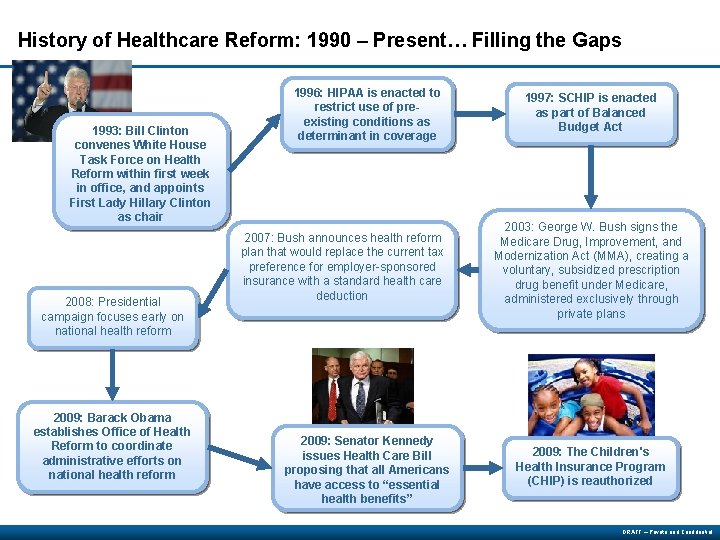
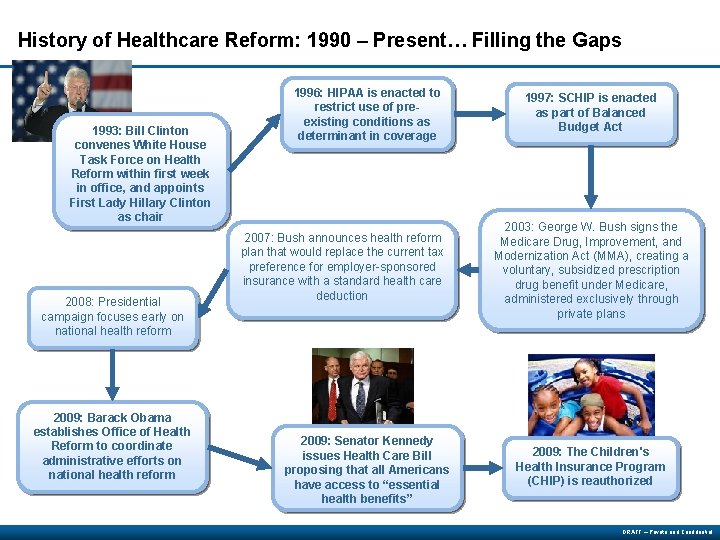
History of Healthcare Reform: 1990 – Present… Filling the Gaps 1993: Bill Clinton convenes White House Task Force on Health Reform within first week in office, and appoints First Lady Hillary Clinton as chair 2008: Presidential campaign focuses early on national health reform 2009: Barack Obama establishes Office of Health Reform to coordinate administrative efforts on national health reform 1996: HIPAA is enacted to restrict use of preexisting conditions as determinant in coverage 2007: Bush announces health reform plan that would replace the current tax preference for employer-sponsored insurance with a standard health care deduction 2009: Senator Kennedy issues Health Care Bill proposing that all Americans have access to “essential health benefits” 1997: SCHIP is enacted as part of Balanced Budget Act 2003: George W. Bush signs the Medicare Drug, Improvement, and Modernization Act (MMA), creating a voluntary, subsidized prescription drug benefit under Medicare, administered exclusively through private plans 2009: The Children's Health Insurance Program (CHIP) is reauthorized DRAFT – Private and Confidential
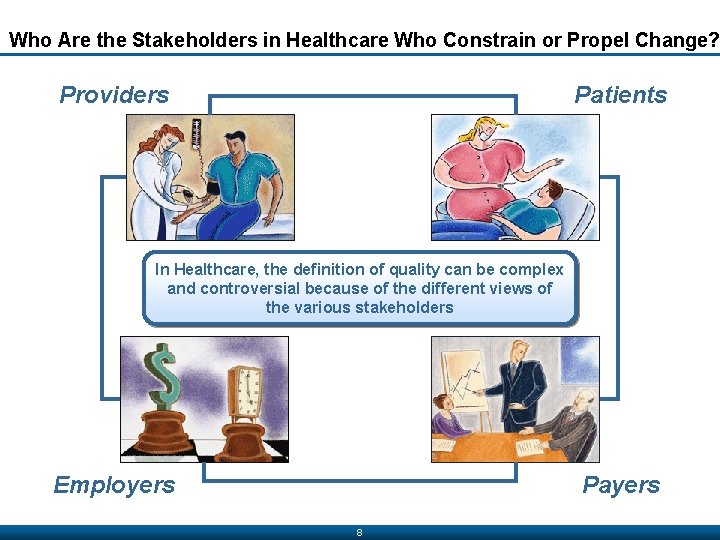
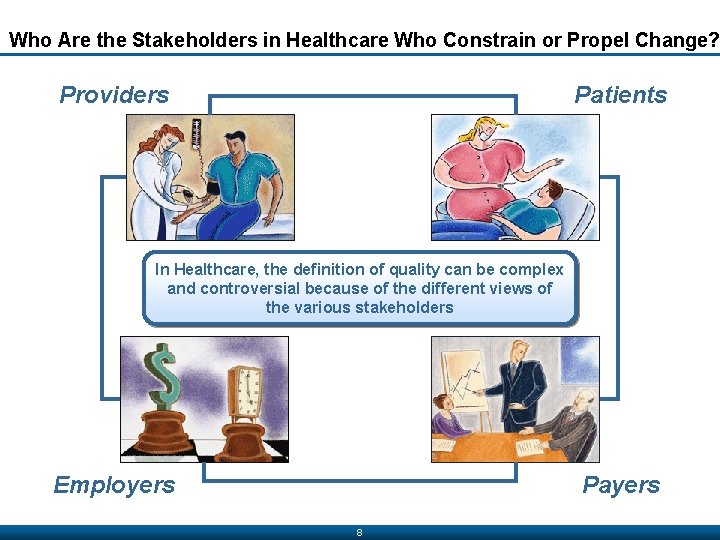
Who Are the Stakeholders in Healthcare Who Constrain or Propel Change? Providers Patients In Healthcare, the definition of quality can be complex and controversial because of the different views of the various stakeholders Employers Payers 8
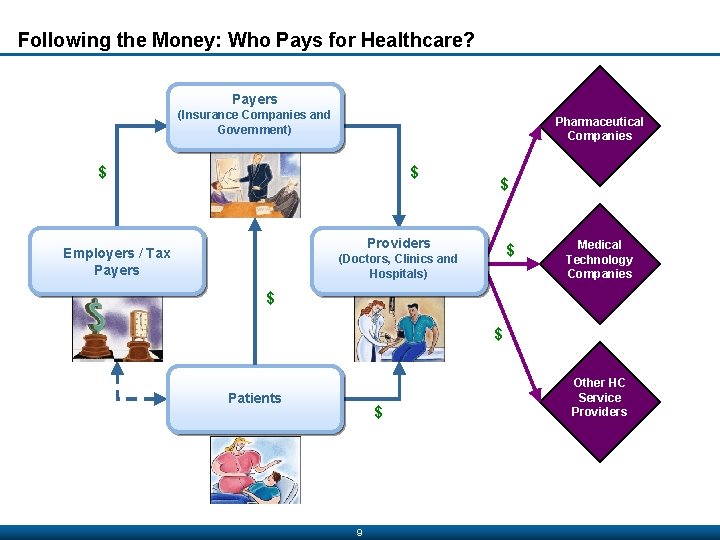
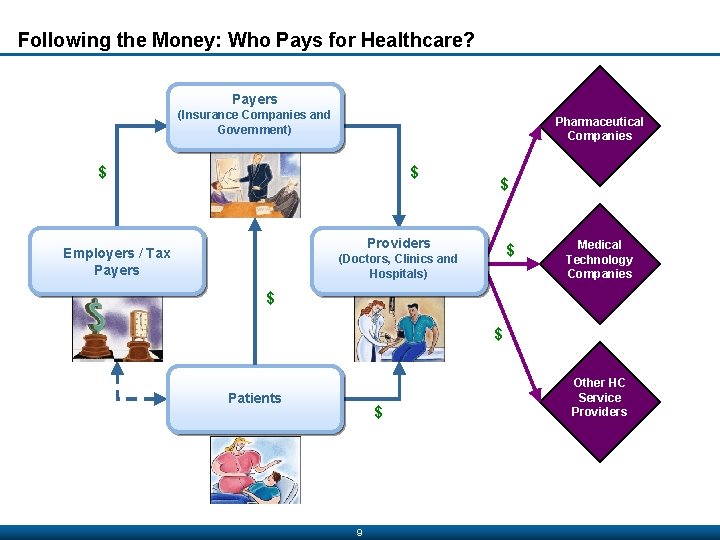
Following the Money: Who Pays for Healthcare? Payers (Insurance Companies and Government) Pharmaceutical Companies $ $ $ Providers Employers / Tax Payers $ (Doctors, Clinics and Hospitals) Medical Technology Companies $ $ Patients $ 9 Other HC Service Providers
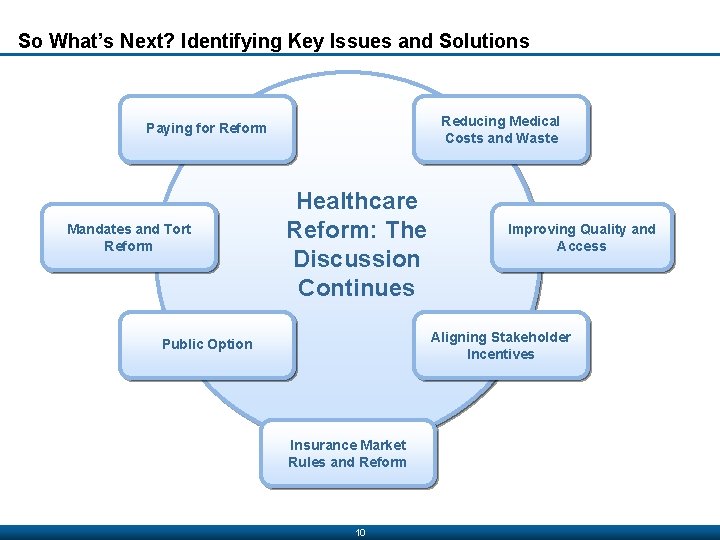
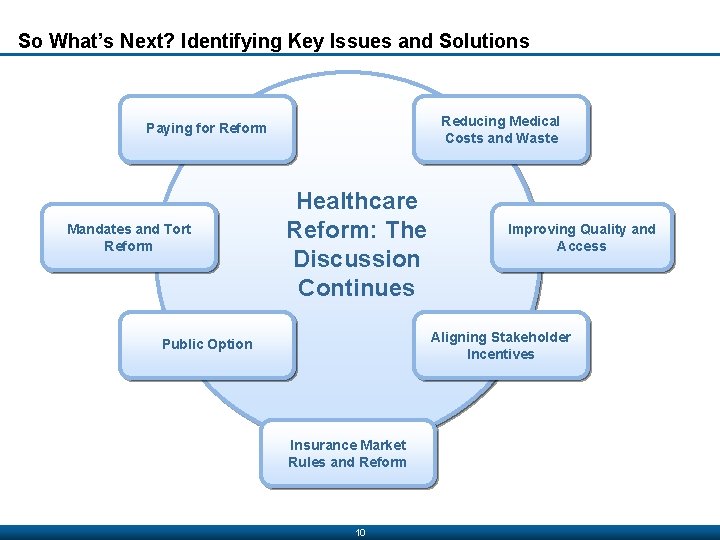
So What’s Next? Identifying Key Issues and Solutions Reducing Medical Costs and Waste Paying for Reform Mandates and Tort Reform Healthcare Reform: The Discussion Continues Improving Quality and Access Aligning Stakeholder Incentives Public Option Insurance Market Rules and Reform 10
Major Issues and Concerns Facing the Health Sector 4 Improving quality – medical errors; substance abuse, mental health, asthma, diabetics receive ineffective care 4 Improving access and coverage - 50. 7 million American lacked insurance coverage in 2009 and millions more had inadequate coverage. 4 Slowing the growth of health care costs – health care costs are growing much more rapidly than the rest of the economy. 4 Encouraging healthy behavior – health behavior can help people avoid diseases and injury or prevent disease or disability from worsening. 4 Improving the coordination, transparency, and accountability of local system of care – problems of quality, cost, and access are largely attributable to the fragmentation and lack of coordination with the system. 4 Health disparities – inequalities in health status among various income groups, social classes, and ethnic groups 4 https: //www. youtube. com/watch? v=5 Lul 6 KNIw_8 11
Defining Characteristics of the U. S. Health Care System 4 The first defining characteristic of the health care system is the line between activities directed at keeping people healthy and those directed at restoring health once a disease or injury occurs. 4 Additional defining features of the U. S. health care system: • The importance of institutions in delivering care • The roles of professionals in running the system • Medical technology, electronic communication, and new drugs that fuel change in health care delivery • Tension between “the free market” and “government control. ” • The dysfunctional financing and payment system –How we pay health care providers does not provide adequate incentives to emphasize quality, value, and efficiency 12
Defining Characteristics of the U. S. Health Care System 4 No central governing agency and little integration and coordination 4 Technology-driven deliver system focusing on acute care 4 High in cost, unequal in access, and average in outcome 4 Delivery of health care under imperfect market conditions 4 Government as subsidiary to the private sector 4 Fusion of market justice and social justice 4 Multiple players and balance of power 4 Quest for integration and accountability 4 Access to health care services selectively based on insurance coverage 4 Legal risks influence practice behaviors 13
Defining Characteristics of the U. S. Health Care System 4 No central governing agency and little integration and coordination • U. S. is not centrally controlled –Financed both publicly and privately; variety of of payment, insurance, and delivery mechanisms –Private payers account for 54%; Gov’t 46% • Centrally controlled healthcare systems are less complex; less costly 14
Defining Characteristics of the U. S. Health Care System 4 Technology-driven deliver system focusing on acute care • U. S. research and innovation in new technology creates a demand for new services • The latest innovations are believed to provide the best care • Many physicians want to try the latest innovations • Technology causes competition between hospitals • Legal risks for providers play a role in the reluctance to deny new technology. 15
Defining Characteristics of the U. S. Health Care System 4 High in cost, unequal in access, and average in outcome • U. S. spends more money than any other country on healthcare • Many residents still do not have access to care • Access is restricted to: –Having health insurance –Those covered under government programs –Those who can afford to buy insurance –Those able to pay privately –Those who can obtain services through safety net providers 16
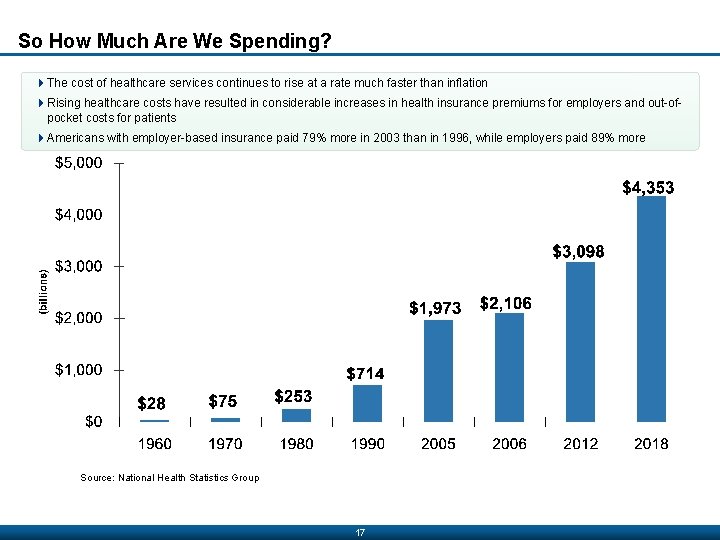
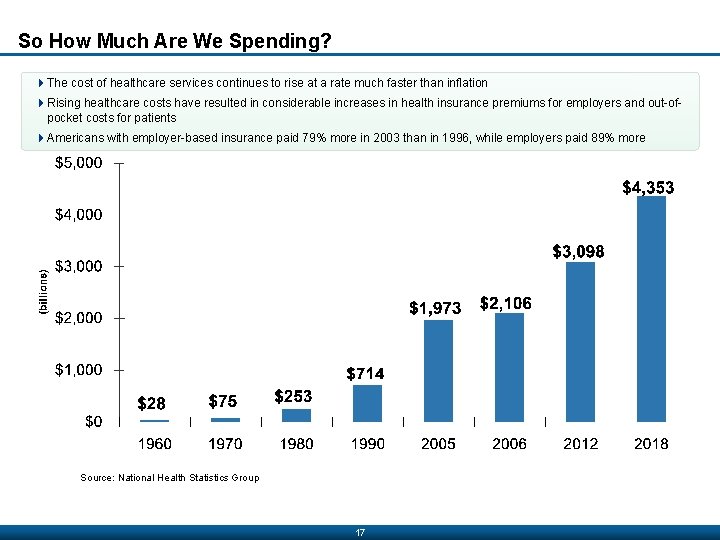
So How Much Are We Spending? 4 The cost of healthcare services continues to rise at a rate much faster than inflation 4 Rising healthcare costs have resulted in considerable increases in health insurance premiums for employers and out-ofpocket costs for patients 4 Americans with employer-based insurance paid 79% more in 2003 than in 1996, while employers paid 89% more Source: National Health Statistics Group 17
Defining Characteristics of the U. S. Health Care System 4 Delivery of health care under imperfect market conditions • In U. S. healthcare is only partially govern by free markets; hence the quasi market or imperfect market • Payors set the price of healthcare, not the patient • There is restrain competition among providers on the basis of price and quality. • Patients are not always aware of choices involving technology, pharmaceuticals, diagnostic methods • Current pricing methods for healthcare make it difficult to gauge expense 18
Defining Characteristics of the U. S. Health Care System 4 Government as subsidiary to the private sector • In the U. S. , the private sector plays the dominant role; the government the lesser role –American wants less government intervention 19
Defining Characteristics of the U. S. Health Care System 4 Legal risks influence practice behaviors 4 Americans are quick to engage in lawsuits 4 Patients are persuaded easily to go to court if harm is perceived to have incurred 4 Provider engage in defensive medicine that can lead to higher cost 20
Defining Characteristics of the U. S. Health Care System 4 No central governing agency and little integration and coordination 4 Technology-driven deliver system focusing on acute care 4 High in cost, unequal in access, and average in outcome 4 Delivery of health care under imperfect market conditions 4 Government as subsidiary to the private sector 4 Fusion of market justice and social justice 4 Multiple players and balance of power 4 Quest for integration and accountability 4 Access to health care services selectively based on insurance coverage 4 Legal risks influence practice behaviors 21
Defining Characteristics of the U. S. Health Care System 4 No central governing agency and little integration and coordination 4 Technology-driven deliver system focusing on acute care 4 High in cost, unequal in access, and average in outcome 4 Delivery of health care under imperfect market conditions 4 Government as subsidiary to the private sector 4 Fusion of market justice and social justice 4 Multiple players and balance of power 4 Quest for integration and accountability 4 Access to health care services selectively based on insurance coverage 4 Legal risks influence practice behaviors 22
Defining Characteristics of the U. S. Health Care System 4 No central governing agency and little integration and coordination 4 Technology-driven deliver system focusing on acute care 4 High in cost, unequal in access, and average in outcome 4 Delivery of health care under imperfect market conditions 4 Government as subsidiary to the private sector 4 Fusion of market justice and social justice 4 Multiple players and balance of power 4 Quest for integration and accountability 4 Access to health care services selectively based on insurance coverage 4 Legal risks influence practice behaviors 23
Defining Characteristics of the U. S. Health Care System 4 No central governing agency and little integration and coordination 4 Technology-driven deliver system focusing on acute care 4 High in cost, unequal in access, and average in outcome 4 Delivery of health care under imperfect market conditions 4 Government as subsidiary to the private sector 4 Fusion of market justice and social justice 4 Multiple players and balance of power 4 Quest for integration and accountability 4 Access to health care services selectively based on insurance coverage 4 Legal risks influence practice behaviors 24
Group Discussion Topics DRAFT – Private and Confidential
 Levels of health care primary secondary tertiary
Levels of health care primary secondary tertiary Care value base health and social care
Care value base health and social care Health and social care component 3
Health and social care component 3 Service delivery objective
Service delivery objective Health care system definition
Health care system definition Introduction of health care delivery system
Introduction of health care delivery system Health care system definition
Health care system definition Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton Chúa sống lại
Chúa sống lại Các môn thể thao bắt đầu bằng tiếng bóng
Các môn thể thao bắt đầu bằng tiếng bóng Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính thế năng
Công thức tính thế năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Phép trừ bù
Phép trừ bù Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống