Antihypertensive Drugs Dr Sasan Zaeri Pharm D Ph






- Slides: 33
Antihypertensive Drugs Dr. Sasan Zaeri Pharm. D, Ph. D (Department of Pharmacology)
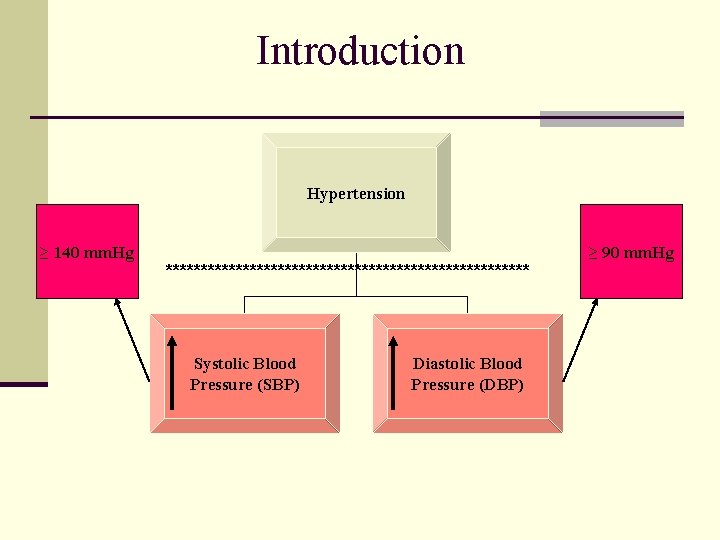
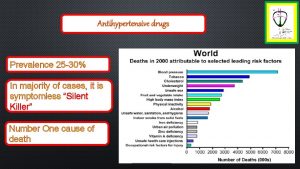
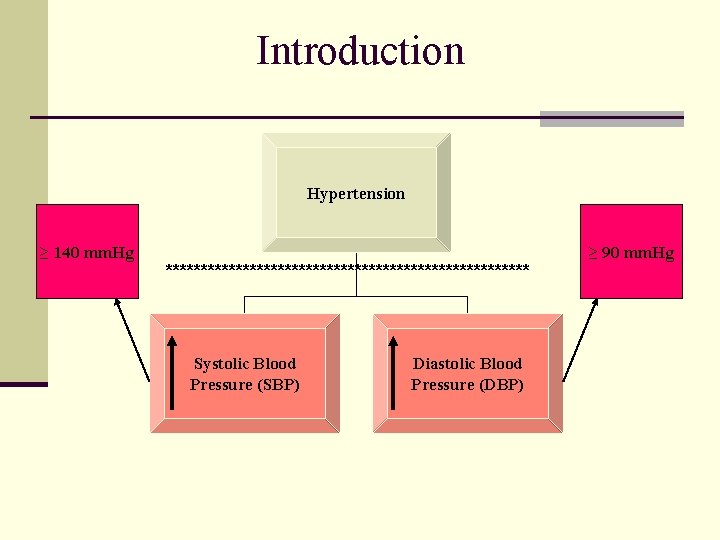
Introduction Hypertension ≥ 140 mm. Hg ************************** Systolic Blood Pressure (SBP) Diastolic Blood Pressure (DBP) ≥ 90 mm. Hg

Types of Hypertension Essential Secondary A disorder of unknown origin affecting the Blood Pressure regulating mechanisms Secondary to other disease processes ************************** Environmental Factors Stress Na+ Intake Obesity Smoking

Treatment – Why? n To prevent target organ damage: n Eye (retinopathy) n Brain (stroke) n Kidney (chronic renal disease) n Heart (coronary artery disease, CHF) n Peripheral arteries (atherosclerosis) n Even asymptomatic hypertension needs to be treated
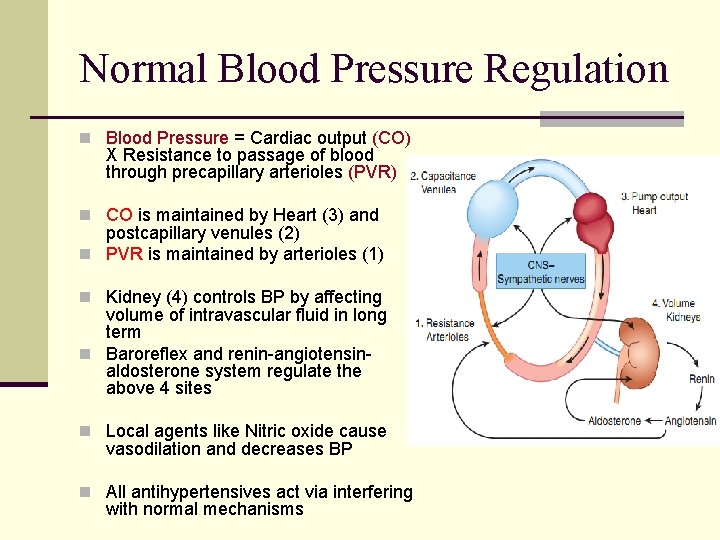
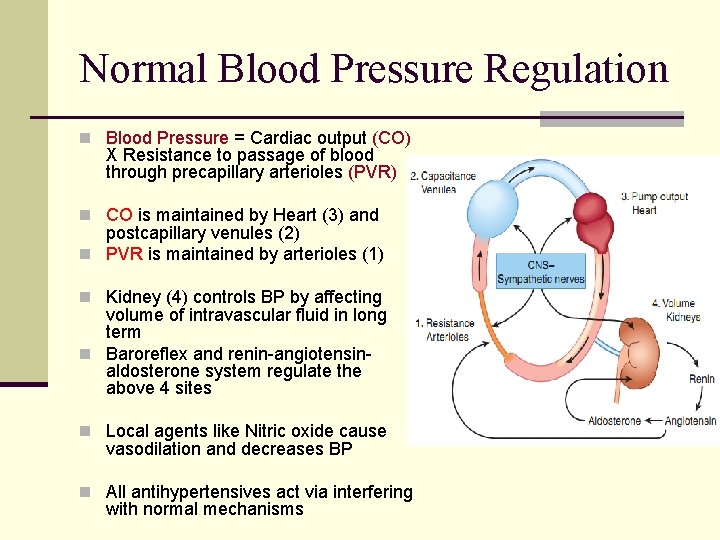
Normal Blood Pressure Regulation n Blood Pressure = Cardiac output (CO) X Resistance to passage of blood through precapillary arterioles (PVR) n CO is maintained by Heart (3) and postcapillary venules (2) n PVR is maintained by arterioles (1) n Kidney (4) controls BP by affecting volume of intravascular fluid in long term n Baroreflex and renin-angiotensin- aldosterone system regulate the above 4 sites n Local agents like Nitric oxide cause vasodilation and decreases BP n All antihypertensives act via interfering with normal mechanisms
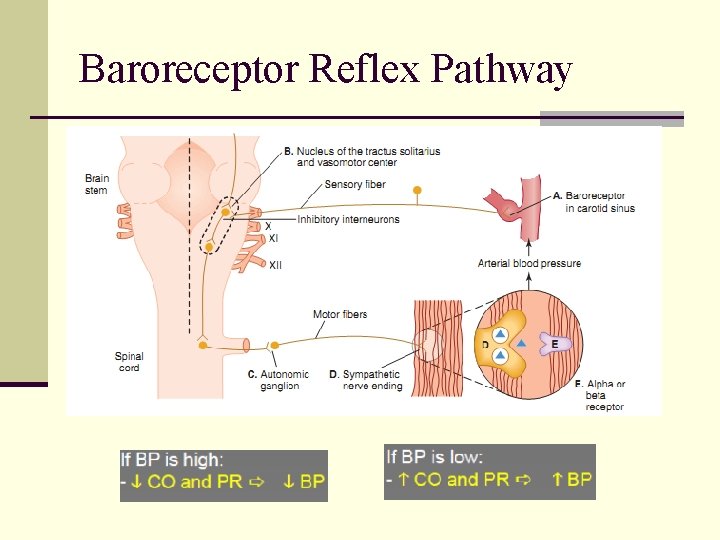
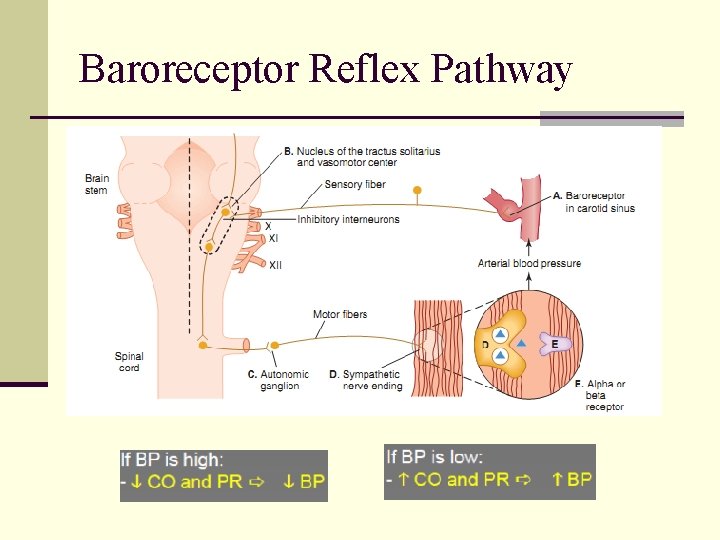
Baroreceptor Reflex Pathway
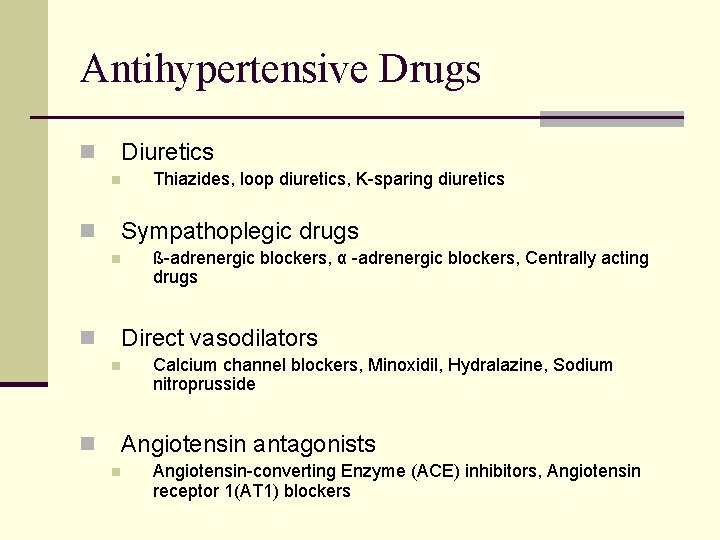
Antihypertensive Drugs Diuretics n n Thiazides, loop diuretics, K-sparing diuretics Sympathoplegic drugs n n ß-adrenergic blockers, α -adrenergic blockers, Centrally acting drugs Direct vasodilators n n Calcium channel blockers, Minoxidil, Hydralazine, Sodium nitroprusside Angiotensin antagonists n n Angiotensin-converting Enzyme (ACE) inhibitors, Angiotensin receptor 1(AT 1) blockers
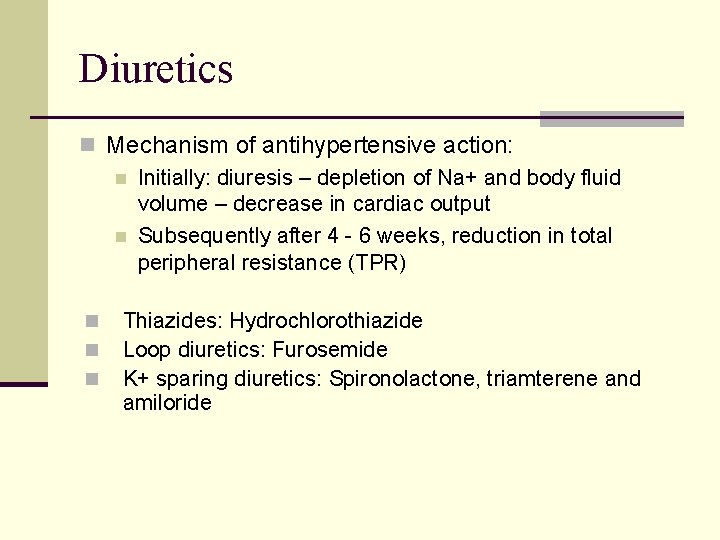
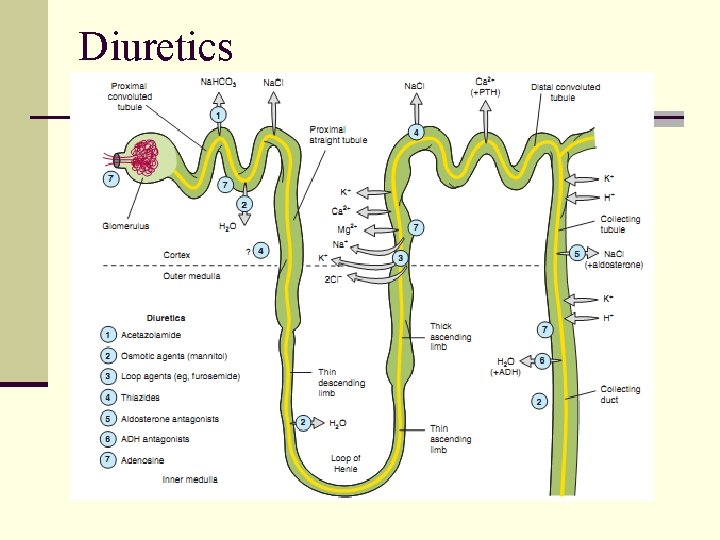
Diuretics n Mechanism of antihypertensive action: n Initially: diuresis – depletion of Na+ and body fluid volume – decrease in cardiac output n Subsequently after 4 - 6 weeks, reduction in total peripheral resistance (TPR) n n n Thiazides: Hydrochlorothiazide Loop diuretics: Furosemide K+ sparing diuretics: Spironolactone, triamterene and amiloride
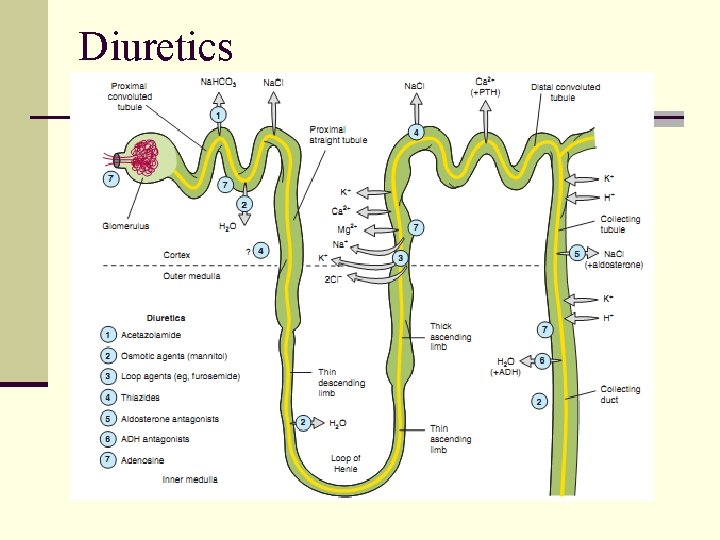
Diuretics
Diuretics n Thiazide diuretic is the first-choice drug in mild hypertension n Thiazide diuretic can be used with a potassium sparing diuretic n Example: Triamterene-H n Loop diuretics are used only in complicated cases n CRF, CHF marked fluid retention cases
Thiazide diuretics n Adverse Effects (mostly seen in higher doses): n Hypokalaemia n Hyperglycemia: precipitation of diabetes n Hyperlipidemia: rise in total LDL level – risk of stroke n Hyperurecaemia: inhibition of uric acid excretion n Hypercalcemia n Thiazide diuretics reduce mortality and morbidity in patients with BP
Beta-adrenergic blockers n Mechanism of action: n n Reduction in CO Decrease in renin release from kidney (beta-1 mediated) n Non-selective: Propranolol (others: nadolol, timolol, pindolol, labetolol) n Cardioselective: Metoprolol (others: atenolol, esmolol, betaxolol) n Advantages: n Prevention of sudden cardiac death in post MI patients n Prevention of CHF progression
Beta-adrenergic blockers n Advantages of cardio-selective over non-selective: n In asthma n In diabetes mellitus n In peripheral vascular disease n Current status in treatment of BP: n First line along with diuretics and ACEIs n Preferred in angina pectoris n Preferred in Post MI patients – useful in preventing progression to CHF and mortality

Αlpha-adrenergic blockers n Mechanism of action: n Vasodilatation by blocking of alpha adrenergic receptors in smooth muscles: Reduction in PVR, reduction in CO by reduction in venomotor tone n Specific alpha-1 blockers: prazosin, terazosin and doxazosine n Non selective alpha blockers (phenoxybenzamine, phentolamine) are not used in chronic essential hypertension n Only used in pheochromocytoma
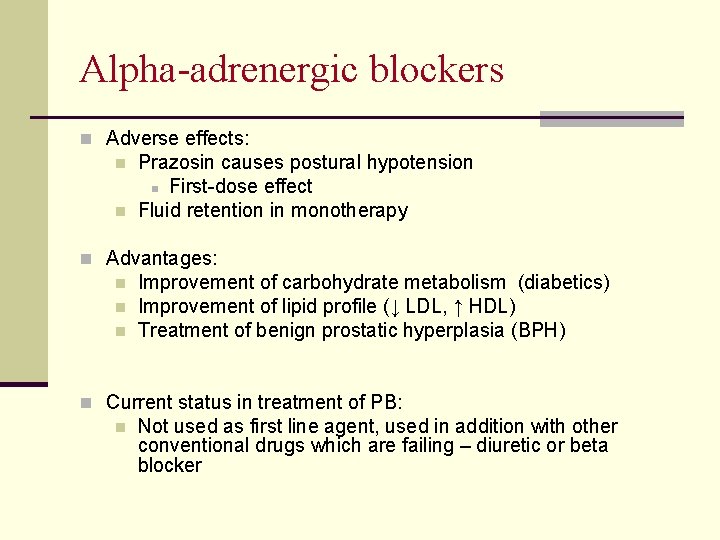
Αlpha-adrenergic blockers n Adverse effects: n n Prazosin causes postural hypotension n First-dose effect Fluid retention in monotherapy n Advantages: n n n Improvement of carbohydrate metabolism (diabetics) Improvement of lipid profile (↓ LDL, ↑ HDL) Treatment of benign prostatic hyperplasia (BPH) n Current status in treatment of PB: n Not used as first line agent, used in addition with other conventional drugs which are failing – diuretic or beta blocker
Centrally-Acting Drugs n Mechanism of action: n Inhibition of adrenergic discharge in brain by agonizing alpha -2 receptors: fall in PVR and CO n Methyldopa n Various adverse effects – cognitive impairement, postural hypotension, hemolytic anemia n Not used therapeutically now except in Hypertension during pregnancy n Clonidine n Not frequently used now because of tolerance and withdrawal hypertension
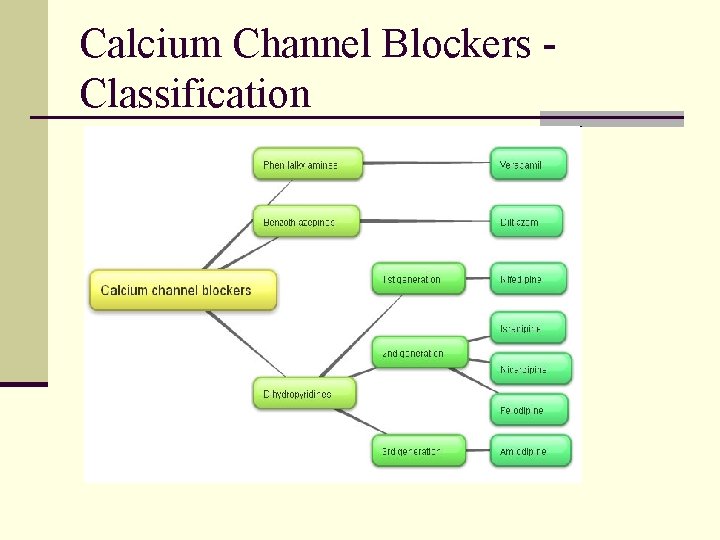
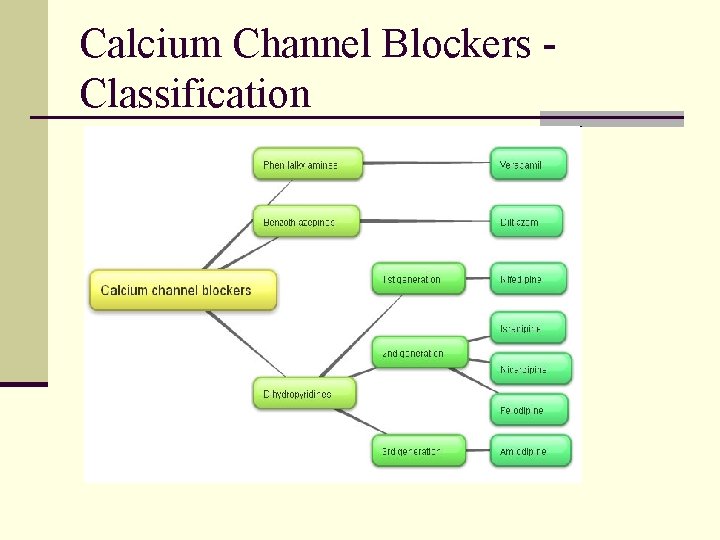
Calcium Channel Blockers Classification
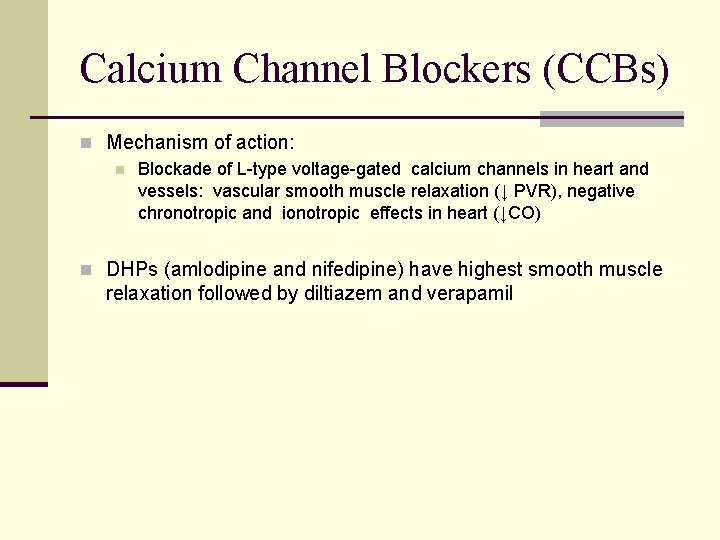
Calcium Channel Blockers (CCBs) n Mechanism of action: n Blockade of L-type voltage-gated calcium channels in heart and vessels: vascular smooth muscle relaxation (↓ PVR), negative chronotropic and ionotropic effects in heart (↓CO) n DHPs (amlodipine and nifedipine) have highest smooth muscle relaxation followed by diltiazem and verapamil
Calcium Channel Blockers n Advantages: n Can be given to patients with n n Asthma with BP Angina with/without BP Peripheral vascular disease Prophylaxis of migraine n Immediate acting Nifedipine is not encouraged anymore n Not first line of antihypertensive unless indicated
Vasodilators - Hydralazine n Mechanism of action: Hydralazine molecules combine with receptors in the endothelium of arterioles and causes Nitric oxide release – relaxation of vascular smooth muscle – fall in PVR n Adverse effects: n Reflex tachycardia n Salt and water retention n Drug-induced lupus erythematosus n n Uses: n n Moderate hypertension when 1 st line fails – with betablockers and diuretics Hypertension in pregnancy
Vasodilators-Sodium Nitroprusside n Mechanism of action: n Rapidly produces nitric oxide to relax both resistance and capacitance vessels (↓PVR and CO) n Uses: Hypertensive Emergencies n (slow infusion)
Vasodilators – Minoxidil n Mechanism of action: n Hyperpolarization of smooth muscles by opening potassium channels and thereby relaxation of vascular smooth muscles n mainly 2 major uses – antihypertensive and alopecia n Rarely indicated in hypertension n Only in life threatening chronic hypertensions e. g. in chronic renal failure n More often in alopecia to promote hair growth

Angiotensin Converting Enzyme (ACE) Inhibitors What is Renin – Angiotensin System (RAS)?
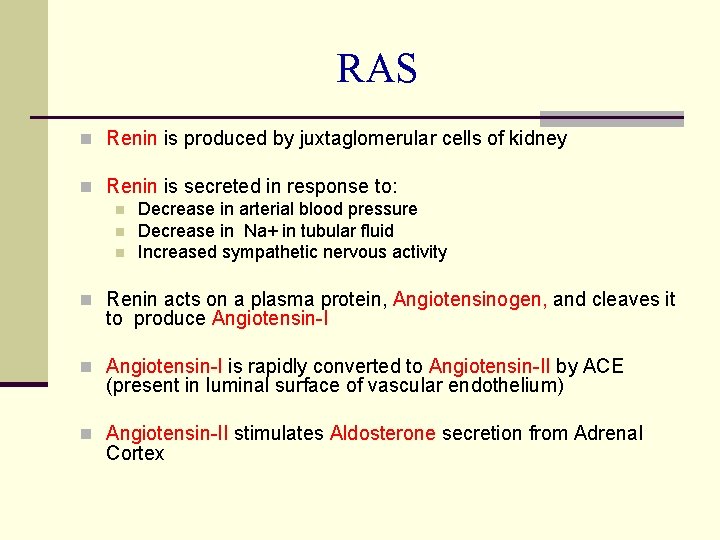
RAS n Renin is produced by juxtaglomerular cells of kidney n Renin is secreted in response to: n Decrease in arterial blood pressure n Decrease in Na+ in tubular fluid n Increased sympathetic nervous activity n Renin acts on a plasma protein, Angiotensinogen, and cleaves it to produce Angiotensin-I n Angiotensin-I is rapidly converted to Angiotensin-II by ACE (present in luminal surface of vascular endothelium) n Angiotensin-II stimulates Aldosterone secretion from Adrenal Cortex
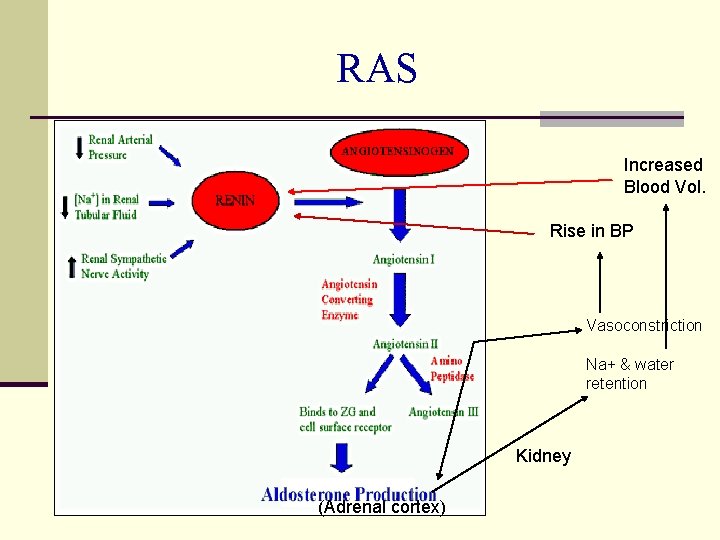
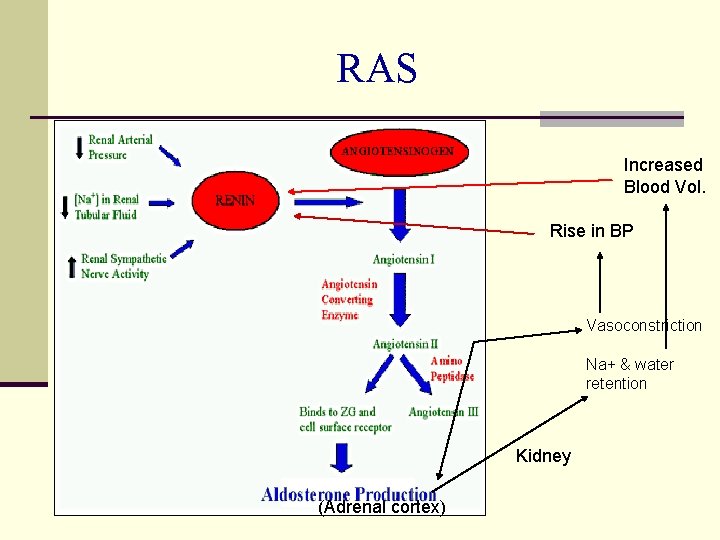
RAS Increased Blood Vol. Rise in BP Vasoconstriction Na+ & water retention Kidney (Adrenal cortex)
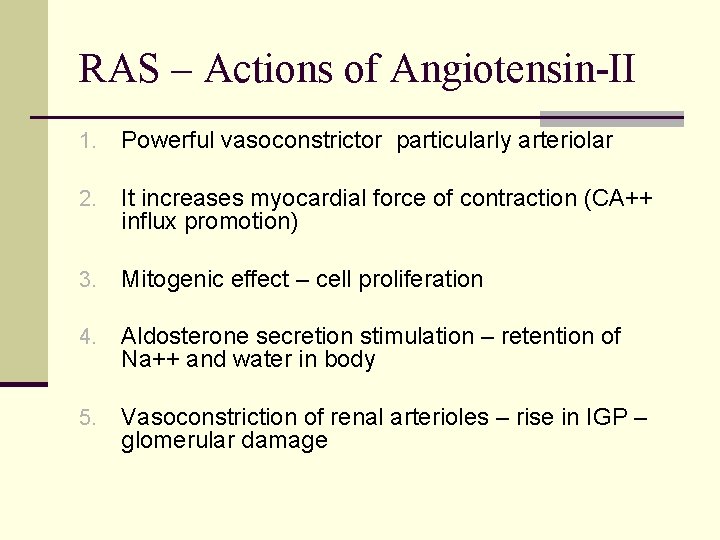
RAS – Actions of Angiotensin-II 1. Powerful vasoconstrictor particularly arteriolar 2. It increases myocardial force of contraction (CA++ influx promotion) 3. Mitogenic effect – cell proliferation 4. Aldosterone secretion stimulation – retention of Na++ and water in body 5. Vasoconstriction of renal arterioles – rise in IGP – glomerular damage
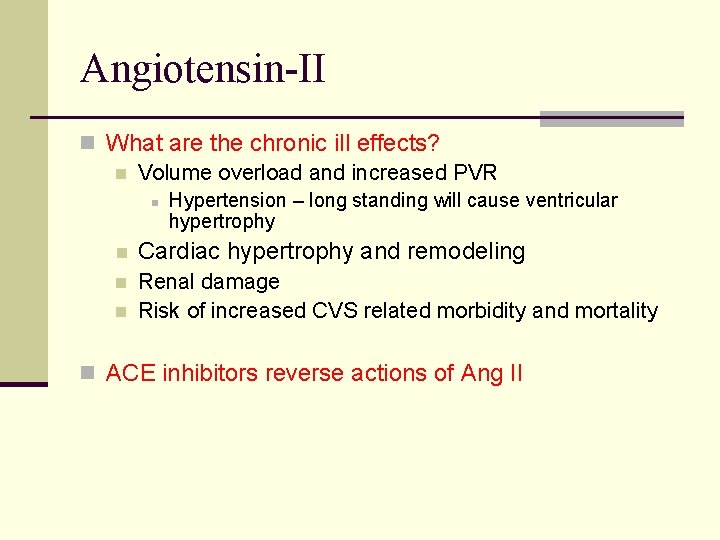
Angiotensin-II n What are the chronic ill effects? n Volume overload and increased PVR n Hypertension – long standing will cause ventricular hypertrophy n Cardiac hypertrophy and remodeling n Renal damage Risk of increased CVS related morbidity and mortality n n ACE inhibitors reverse actions of Ang II
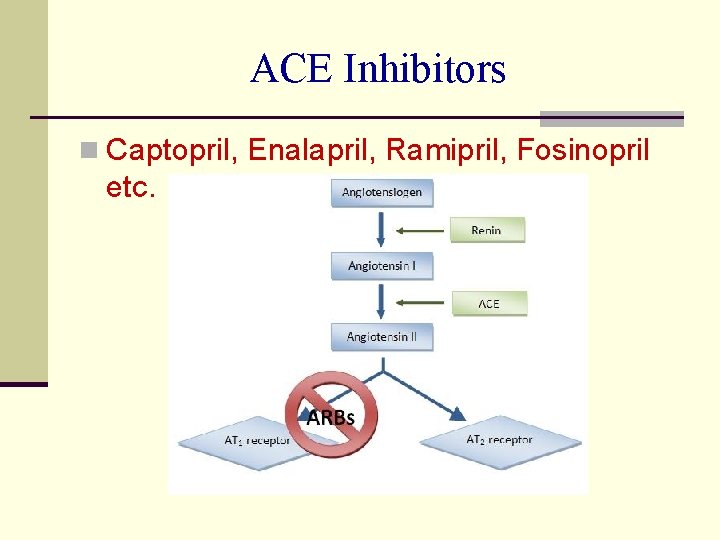
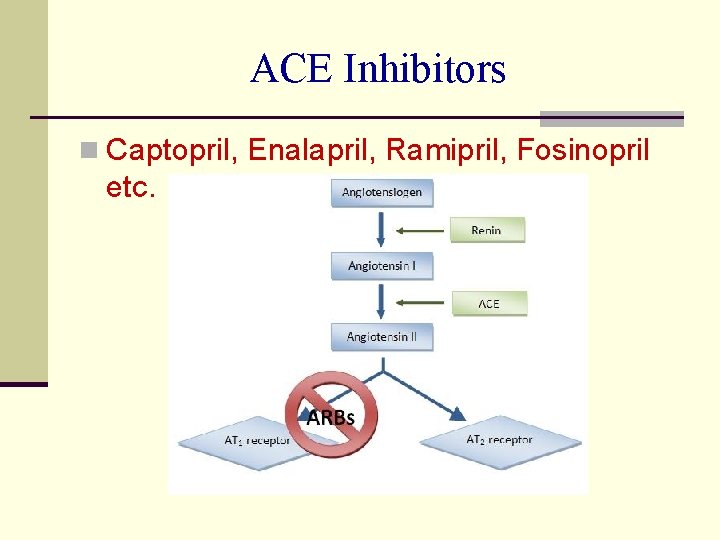
ACE Inhibitors n Captopril, Enalapril, Ramipril, Fosinopril etc.
ACEIs – Antihypertensive action n RAS is overactive in 80% of hypertensive cases and contributes to the maintenance of vascular tone and volume overload n RAS inhibition by ACEIs causes Lower PVR and volume overload hence lower BP

ACEIs – Adverse effects n Cough – persistent cough in 20% cases induced by inhibition of bradykinin breakdown in lungs n Hyperkalemia (routine check of K+ level) n Acute renal failure (bilateral renal artery stenosis) n Angioedema: swelling of lips, mouth, nose etc. n Foetopathic: hypoplasia of organs, growth retardation etc n Contraindications: Pregnancy, bilateral renal artery stenosis, hypersensitivity and hyperkalaemia

Place of ACE inhibitors in HTN n Drug of choice in: n HTN with diabetes (nephroprotective) n HTN with chronic renal disease n HTN with CHF n HTN with MI n Minimal worsening of quality of life – general wellbeing, sleep and work performance etc.
ACE inhibitors – other uses n Congestive Heart Failure (CHF) n Myocardial Infarction (MI) n Diabetic Nephropathy
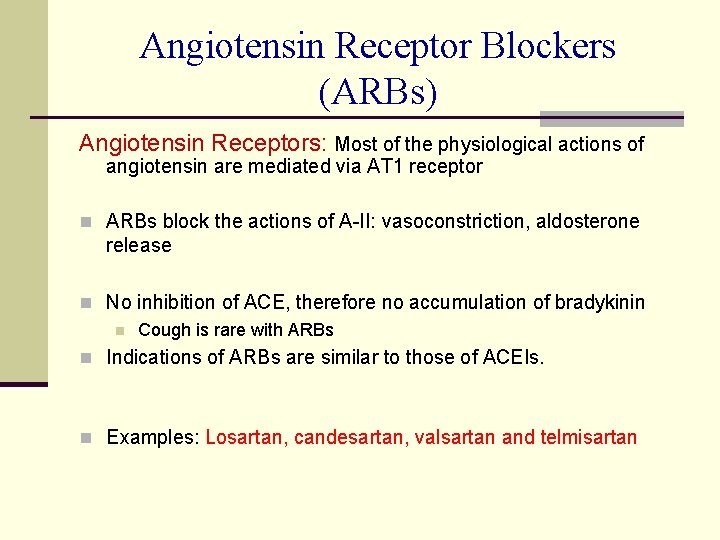
Angiotensin Receptor Blockers (ARBs) Angiotensin Receptors: Most of the physiological actions of angiotensin are mediated via AT 1 receptor n ARBs block the actions of A-II: vasoconstriction, aldosterone release n No inhibition of ACE, therefore no accumulation of bradykinin n Cough is rare with ARBs n Indications of ARBs are similar to those of ACEIs. n Examples: Losartan, candesartan, valsartan and telmisartan
 Adrenoceptor
Adrenoceptor Antihypertensive drugs
Antihypertensive drugs Heart hypertrophy
Heart hypertrophy Antihypertensive drugs classification
Antihypertensive drugs classification Classification of antihypertensive drugs with examples
Classification of antihypertensive drugs with examples Thracentesis
Thracentesis Centrally acting sympathoplegic drugs
Centrally acting sympathoplegic drugs Antihypertensive
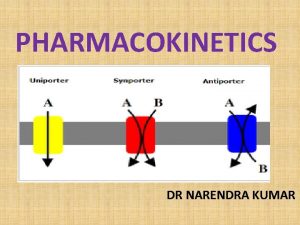
Antihypertensive What is the transport system of the body
What is the transport system of the body Pharm id
Pharm id Pharm406
Pharm406 Pharm gkb
Pharm gkb Pharm
Pharm Library.med.utah.edu/kw/pharm/hyper heart.html
Library.med.utah.edu/kw/pharm/hyper heart.html Ambio pharm
Ambio pharm Bc bio-pharm
Bc bio-pharm Secur pharm
Secur pharm Hpc exf
Hpc exf Outfield pharm
Outfield pharm Pharmlinks
Pharmlinks Noel pharm
Noel pharm Pharm
Pharm Pharm d means
Pharm d means Pharm degree
Pharm degree Hemostatika yang kerjanya mengendapkan protein darah adalah
Hemostatika yang kerjanya mengendapkan protein darah adalah Sympathomimetic drugs
Sympathomimetic drugs Parasympathomimetic drugs
Parasympathomimetic drugs Werkstuk drugs
Werkstuk drugs Advantage of alphabetical classification is
Advantage of alphabetical classification is Antidiuretic drugs
Antidiuretic drugs Difference between zero and first order kinetics
Difference between zero and first order kinetics What is ion trapping in pharmacology
What is ion trapping in pharmacology Drug that alters moods, thoughts, and sense perceptions
Drug that alters moods, thoughts, and sense perceptions Psychoactive drugs chart
Psychoactive drugs chart