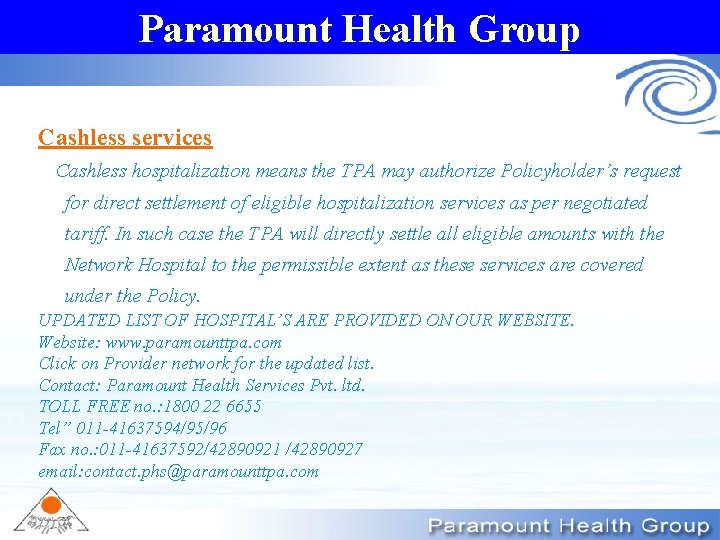
Paramount Health Group Paramount Health Group Cashless services


- Slides: 9
Paramount Health Group
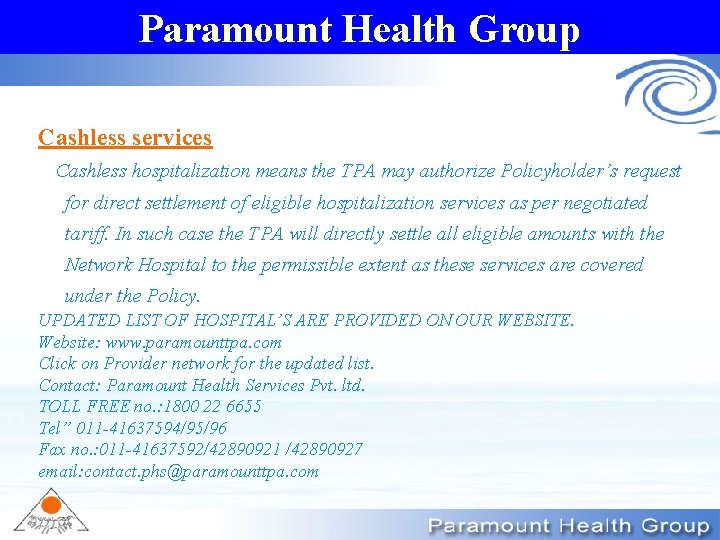
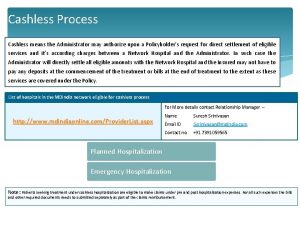
Paramount Health Group Cashless services Cashless hospitalization means the TPA may authorize Policyholder’s request for direct settlement of eligible hospitalization services as per negotiated tariff. In such case the TPA will directly settle all eligible amounts with the Network Hospital to the permissible extent as these services are covered under the Policy. UPDATED LIST OF HOSPITAL’S ARE PROVIDED ON OUR WEBSITE. Website: www. paramounttpa. com Click on Provider network for the updated list. Contact: Paramount Health Services Pvt. ltd. TOLL FREE no. : 1800 22 6655 Tel” 011 -41637594/95/96 Fax no. : 011 -41637592/42890921 /42890927 email: contact. phs@paramounttpa. com
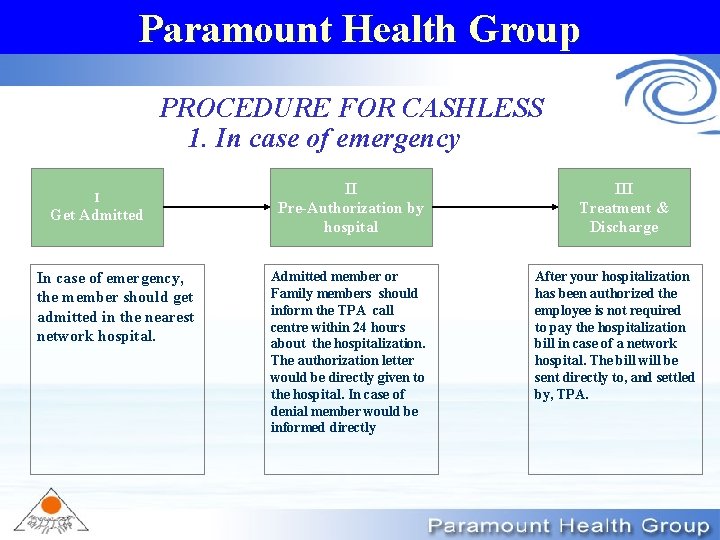
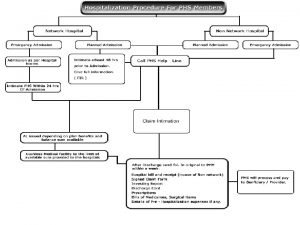
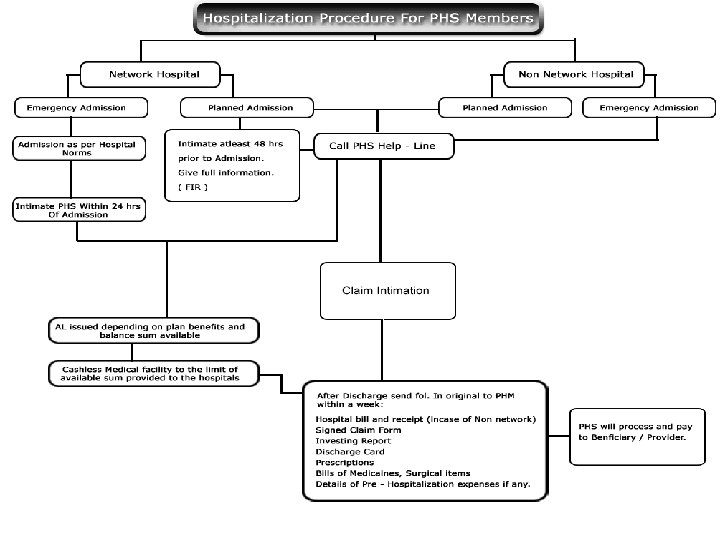
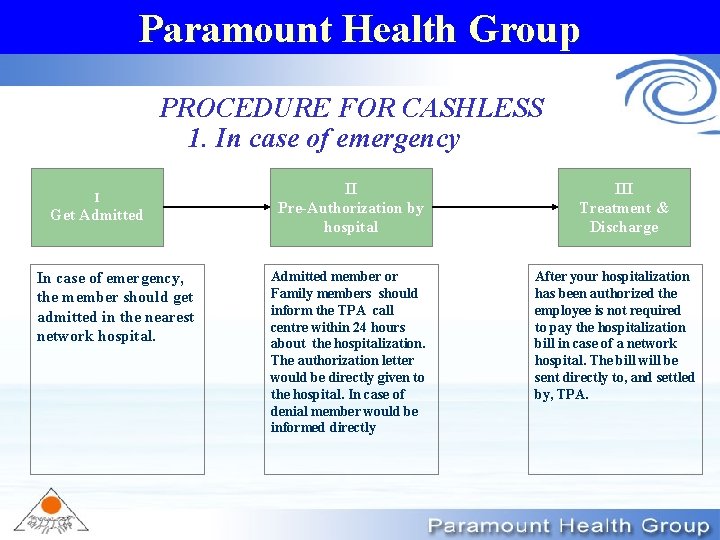
Paramount Health Group PROCEDURE FOR CASHLESS 1. In case of emergency I Get Admitted In case of emergency, the member should get admitted in the nearest network hospital. II Pre-Authorization by hospital Admitted member or Family members should inform the TPA call centre within 24 hours about the hospitalization. The authorization letter would be directly given to the hospital. In case of denial member would be informed directly III Treatment & Discharge After your hospitalization has been authorized the employee is not required to pay the hospitalization bill in case of a network hospital. The bill will be sent directly to, and settled by, TPA.
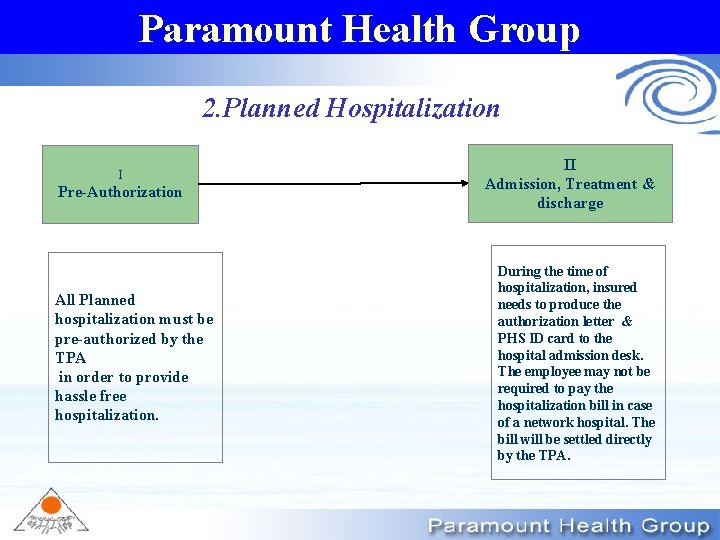
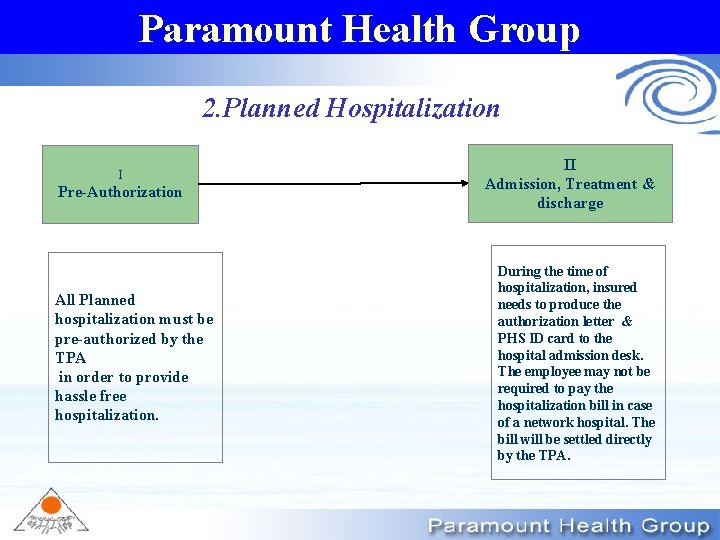
Paramount Health Group 2. Planned Hospitalization I Pre-Authorization All Planned hospitalization must be pre-authorized by the TPA in order to provide hassle free hospitalization. II Admission, Treatment & discharge During the time of hospitalization, insured needs to produce the authorization letter & PHS ID card to the hospital admission desk. The employee may not be required to pay the hospitalization bill in case of a network hospital. The bill will be settled directly by the TPA.

Paramount Health Group Pre- Authorization Member intimates TPA of the planned hospitalization in a admission request form 48 hours prior to hospitalization Pre – Authorization Form At web: www. paramounttpa. com Claim Registered by TPA on same day Yes TPA intimates the hospital/ Insured within 3 hours & issues authorization letter within for planned hospitalization to the hospital. No Follow non cashless process Pre-Authorization Completed
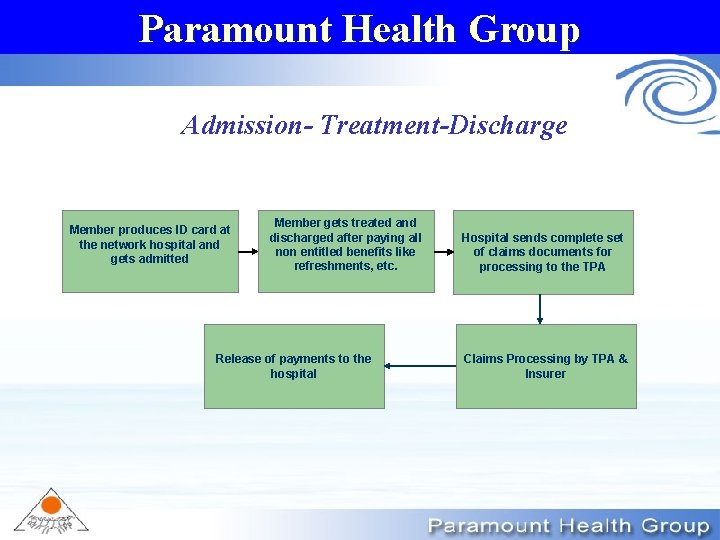
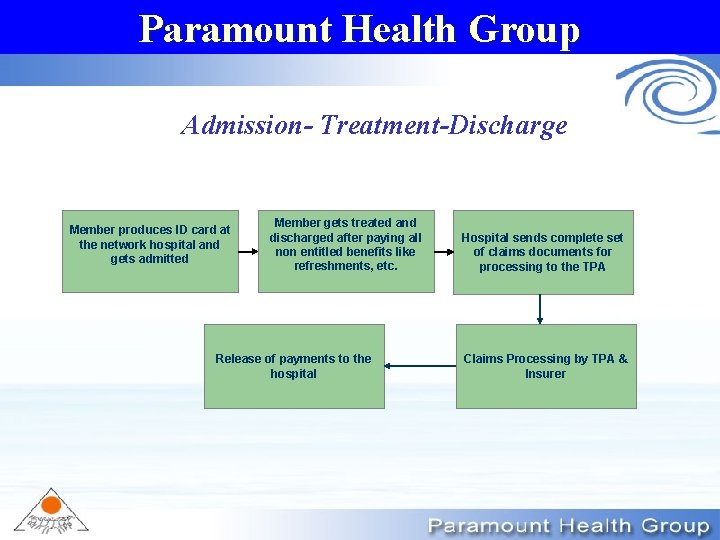
Paramount Health Group Admission- Treatment-Discharge Member produces ID card at the network hospital and gets admitted Member gets treated and discharged after paying all non entitled benefits like refreshments, etc. Release of payments to the hospital Hospital sends complete set of claims documents for processing to the TPA Claims Processing by TPA & Insurer
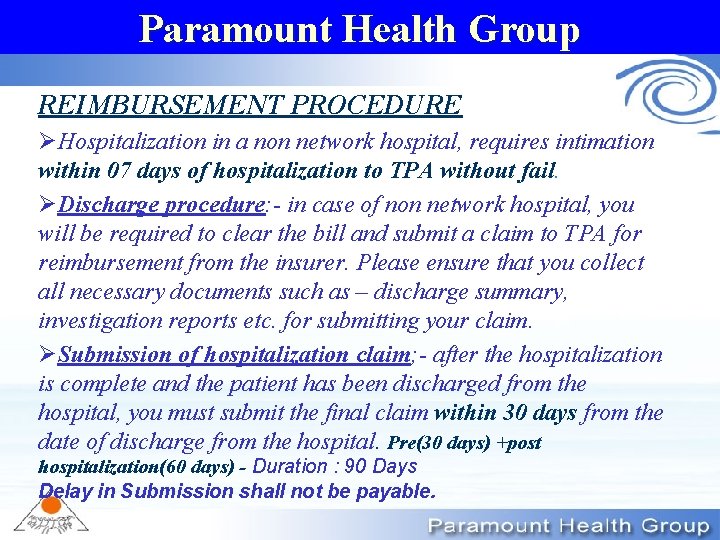
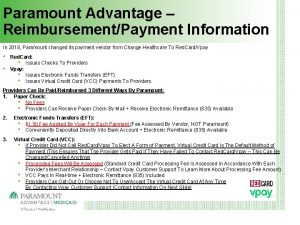
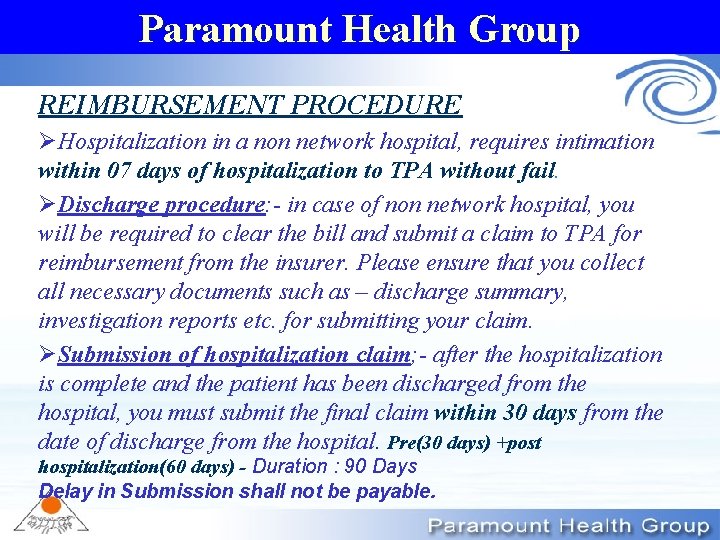
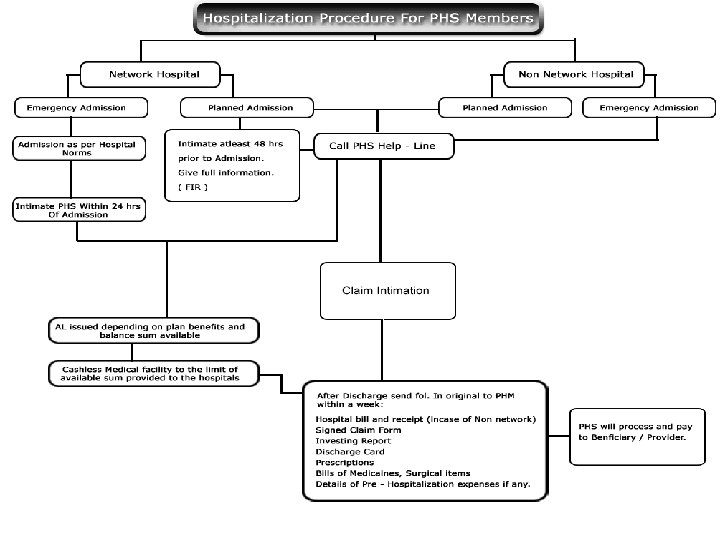
Paramount Health Group REIMBURSEMENT PROCEDURE ØHospitalization in a non network hospital, requires intimation within 07 days of hospitalization to TPA without fail. ØDischarge procedure: - in case of non network hospital, you will be required to clear the bill and submit a claim to TPA for reimbursement from the insurer. Please ensure that you collect all necessary documents such as – discharge summary, investigation reports etc. for submitting your claim. ØSubmission of hospitalization claim; - after the hospitalization is complete and the patient has been discharged from the hospital, you must submit the final claim within 30 days from the date of discharge from the hospital. Pre(30 days) +post hospitalization(60 days) - Duration : 90 Days Delay in Submission shall not be payable.
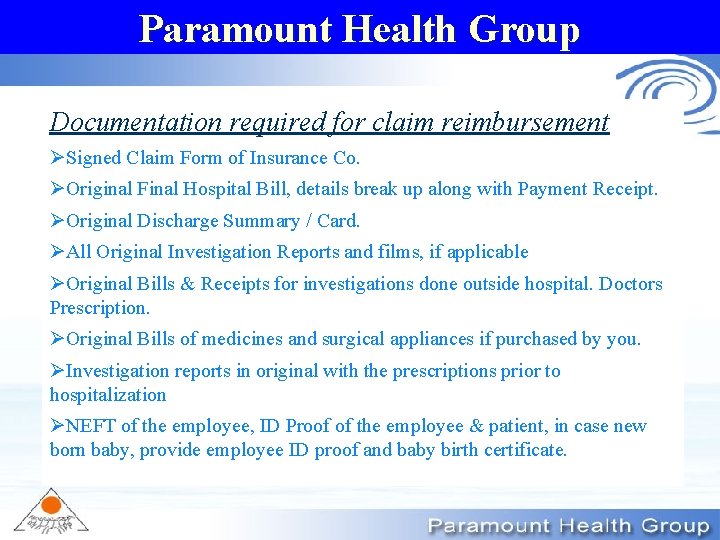
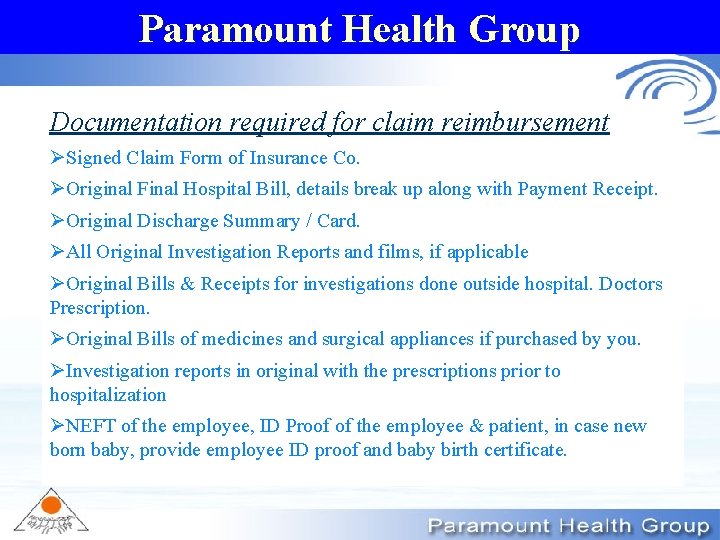
Paramount Health Group Documentation required for claim reimbursement ØSigned Claim Form of Insurance Co. ØOriginal Final Hospital Bill, details break up along with Payment Receipt. ØOriginal Discharge Summary / Card. ØAll Original Investigation Reports and films, if applicable ØOriginal Bills & Receipts for investigations done outside hospital. Doctors Prescription. ØOriginal Bills of medicines and surgical appliances if purchased by you. ØInvestigation reports in original with the prescriptions prior to hospitalization ØNEFT of the employee, ID Proof of the employee & patient, in case new born baby, provide employee ID proof and baby birth certificate.

Paramount Health Group Thank You