Geriatric Incontinence and Voiding Dysfunction Urinary incontinence is

- Slides: 69
Geriatric Incontinence and Voiding Dysfunction
�Urinary incontinence is a major problem for the elderly: �It afflicts 15% to 30% of older people living at home, �one third of those in acutecare settings, �and half of those in nursing homes �UI is twice as common in women as in men
Risk factors in women �Pregnancy and vaginal delivery are significant risk factors, but become less important with age. �Diabetes mellitus is a risk factor in most studies �pelvic organ prolapse (POP)
Risk factors in men �increasing age, lower urinary tract symptoms (LUTS), infections, functional and cognitive impairment, neurological disorders and prostatectomy.
�perineal rashes, pressure ulcers, UTI, urosepsis, falls, and fractures �embarrassment, stigmatization, isolation, depression, anxiety, sexual dysfunction,
�cost more than $26 billion to manage incontinence in America’s elderly in 1995
THE IMPACT OF AGE ON INCONTINENCE �However, it appears that although bladder capacity does not change with age, bladder sensation, contractility, and the ability to postpone voiding decline in both sexes, �while urethral length and maximum closure pressure, as well as striated muscle cells in the rhabdosphincter and urogenital diaphragm, probably decline withage in women
�Venous insufficiency, �renal disease, �heart failure, �or BPH
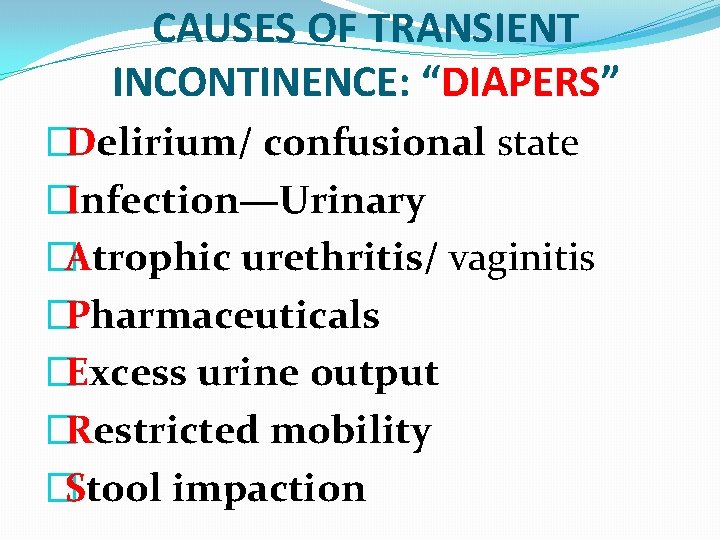
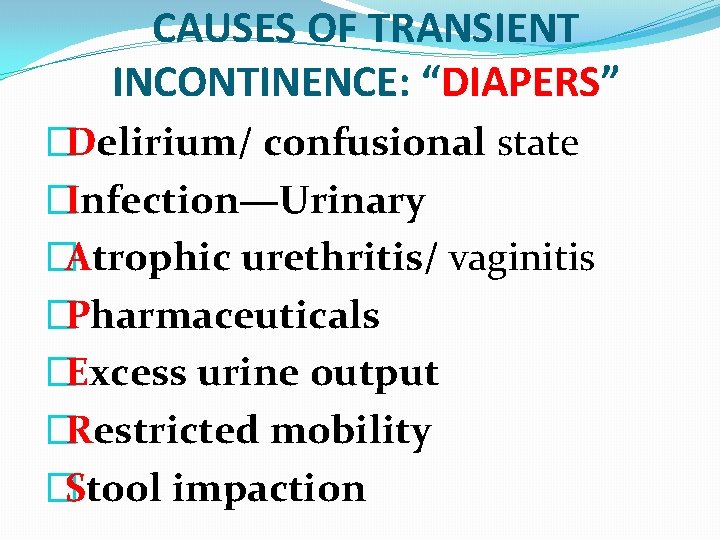
CAUSES OF TRANSIENT INCONTINENCE: “DIAPERS” �Delirium/ confusional state �Infection—Urinary �Atrophic urethritis/ vaginitis �Pharmaceuticals �Excess urine output �Restricted mobility �Stool impaction
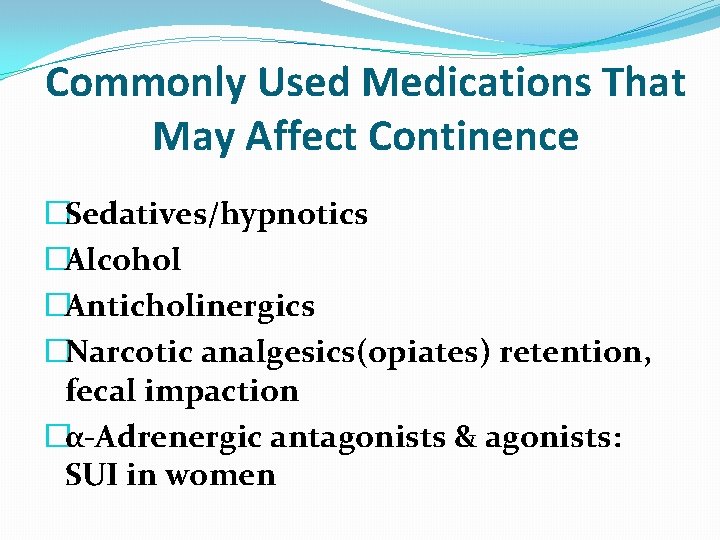
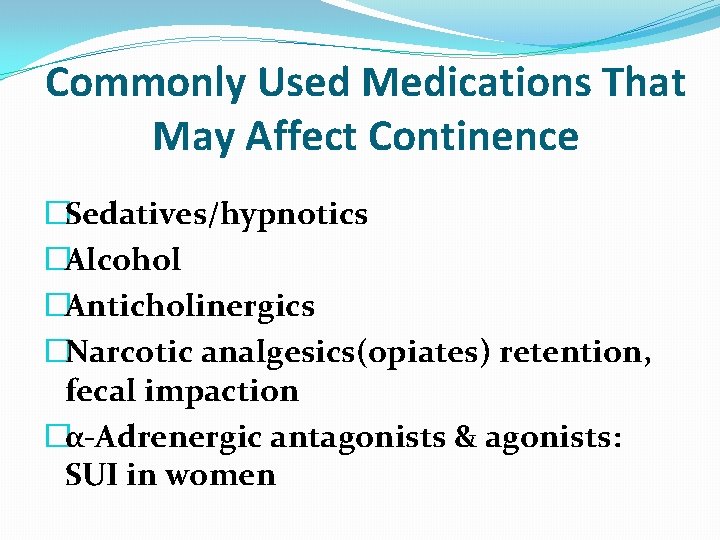
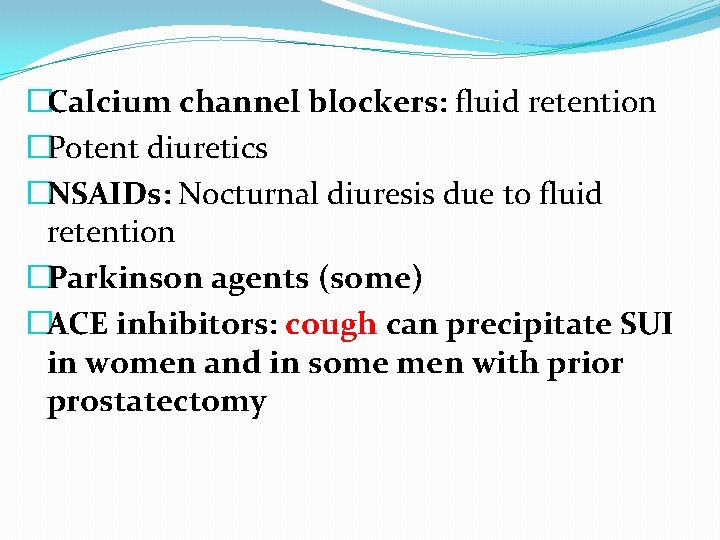
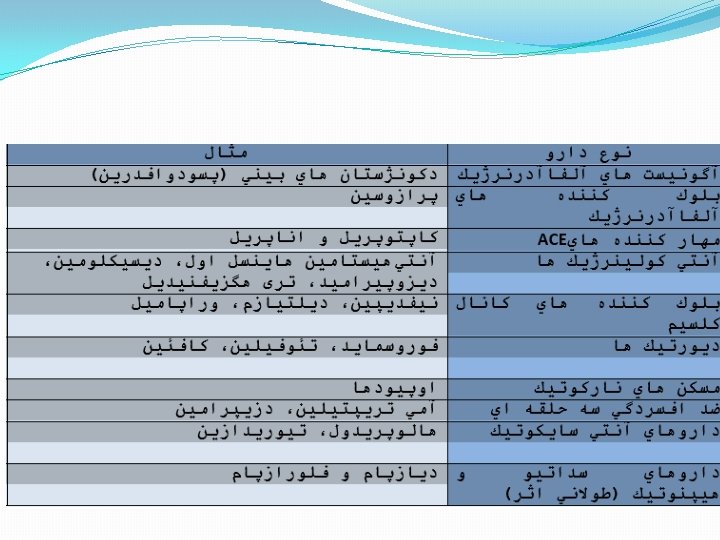
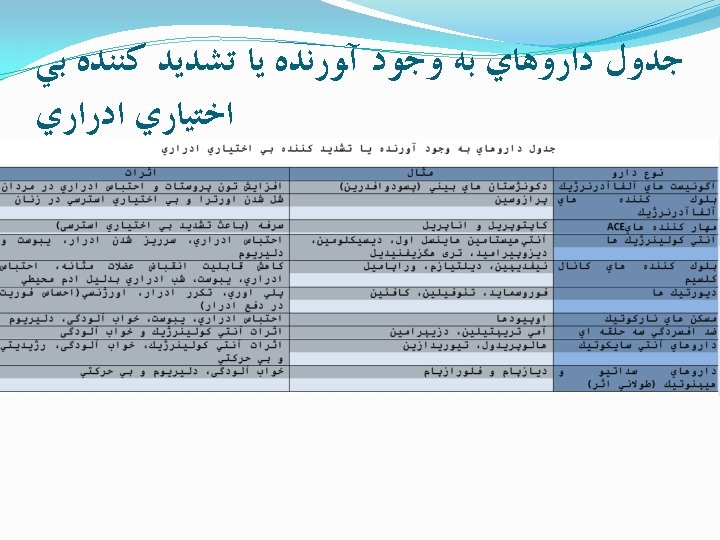
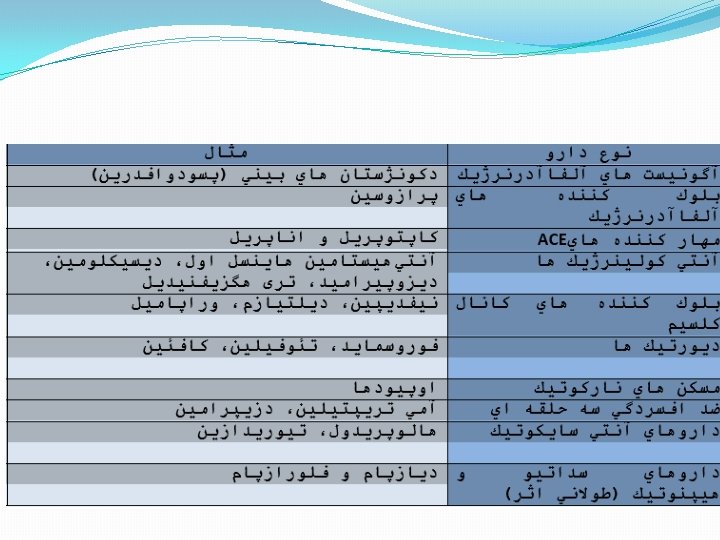
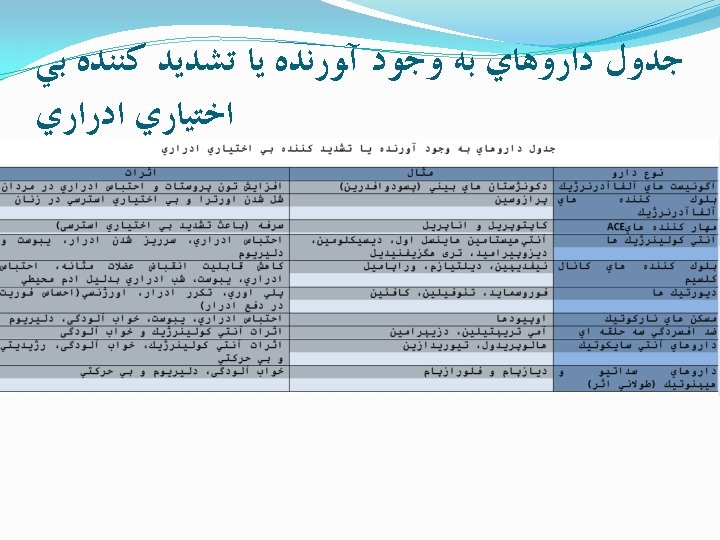
Commonly Used Medications That May Affect Continence �Sedatives/hypnotics �Alcohol �Anticholinergics �Narcotic analgesics(opiates) retention, fecal impaction �α-Adrenergic antagonists & agonists: SUI in women
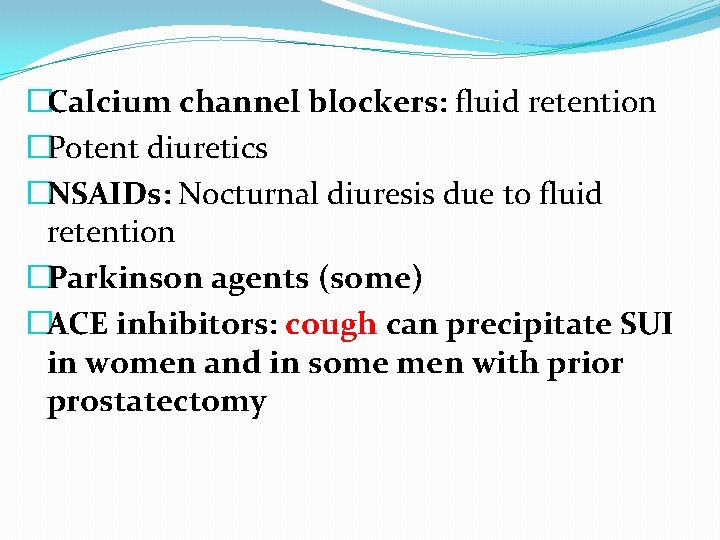
�Calcium channel blockers: fluid retention �Potent diuretics �NSAIDs: Nocturnal diuresis due to fluid retention �Parkinson agents (some) �ACE inhibitors: cough can precipitate SUI in women and in some men with prior prostatectomy
Excess urine output �excessive fluid intake; �Diuretics �metabolic abnormalities (e. g. , hyperglycemia and hypercalcemia); �fluid overload: CHF, peripheral venous insufficiency, hypo. ALB �drug-induced peripheral edema: NSAIDs, Ca channel blockers �amantadine (for Parkinson disease and influenza), �and β blockers.
Restricted mobility �arthritis, hip deformity, �postural or postprandial hypotension, �claudication, spinal stenosis, �heart failure, �poor eyesight, fear of falling, �stroke, foot problems, �drug induced disequilibrium or confusion, or being restrained in a bed or chair
stool impaction �urge or overflow incontinence and typically have associated fecal incontinence as well.
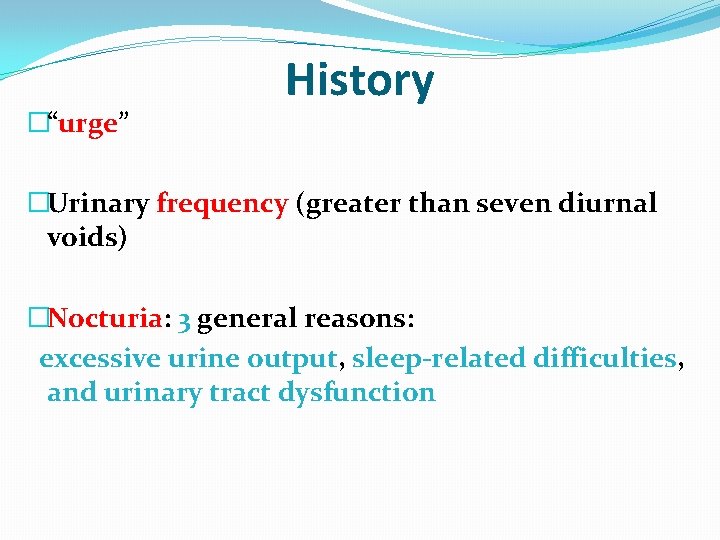
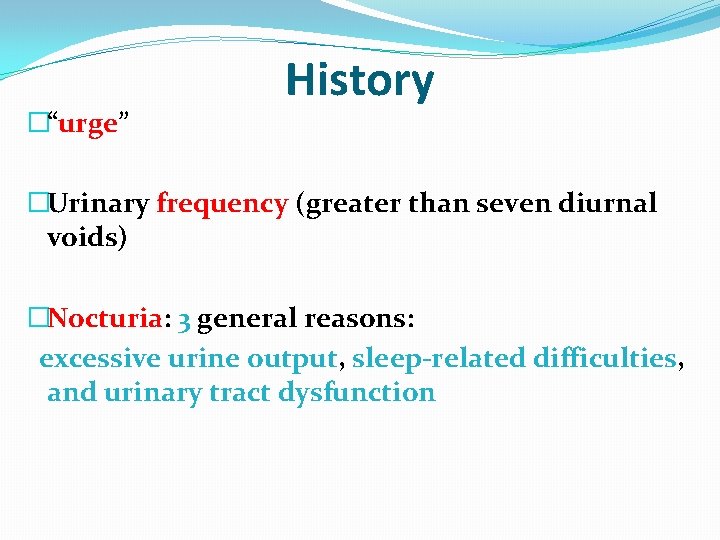
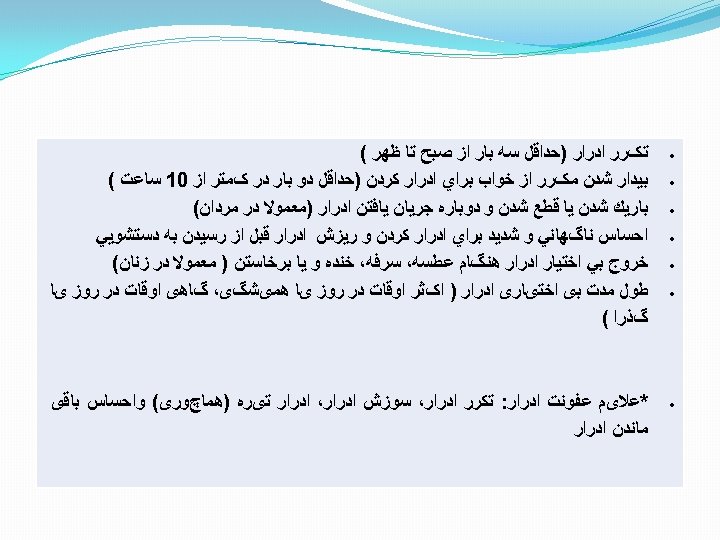
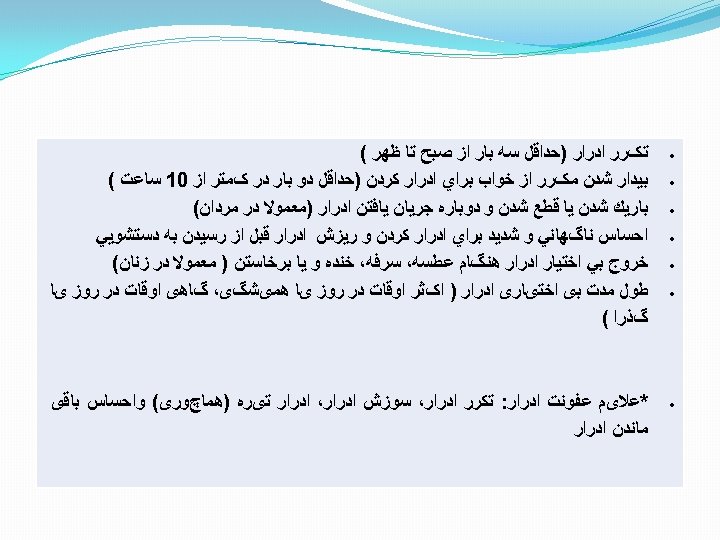
�“urge” History �Urinary frequency (greater than seven diurnal voids) �Nocturia: 3 general reasons: excessive urine output, sleep-related difficulties, and urinary tract dysfunction
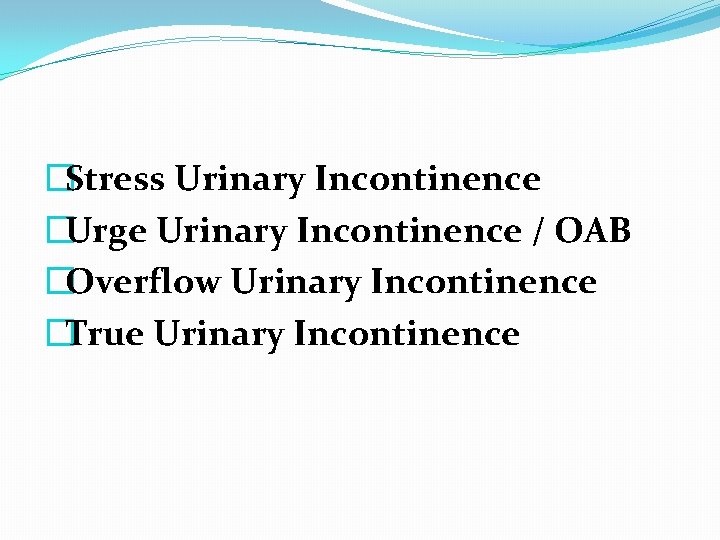
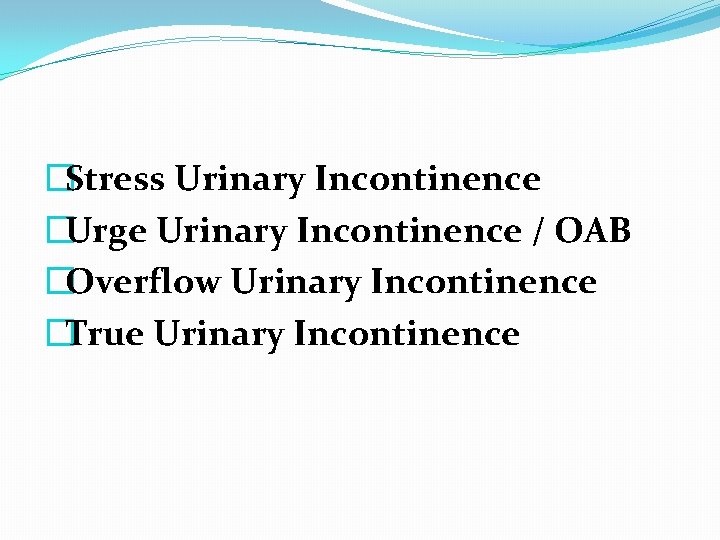
�Stress Urinary Incontinence �Urge Urinary Incontinence / OAB �Overflow Urinary Incontinence �True Urinary Incontinence
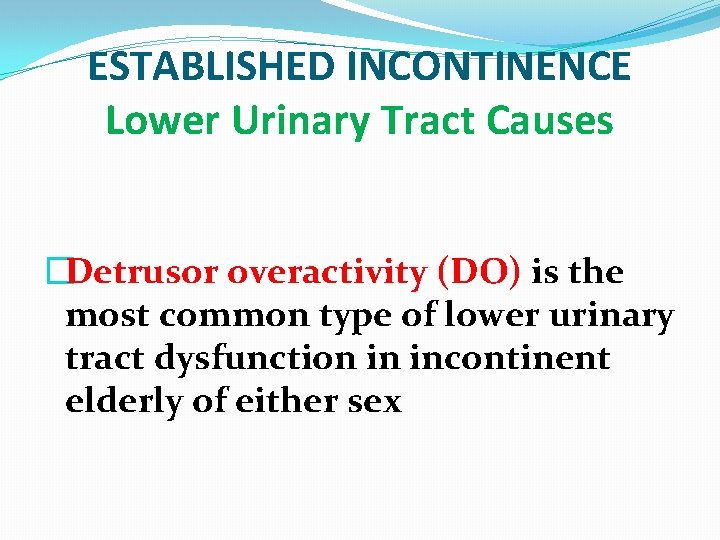
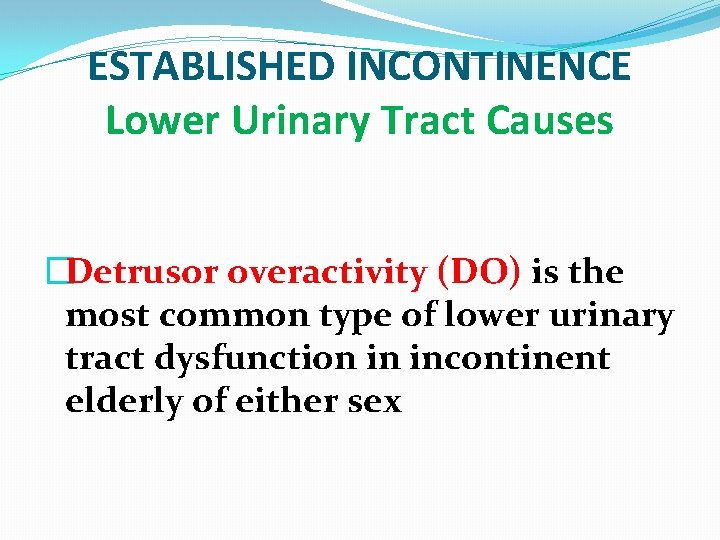
ESTABLISHED INCONTINENCE Lower Urinary Tract Causes �Detrusor overactivity (DO) is the most common type of lower urinary tract dysfunction in incontinent elderly of either sex
�one in which contractile function is preserved and one in which it is impaired: �The latter condition is termed detrusor hyperactivity with impaired contractility (DHIC) and is likely the most common form of DO in the elderly
�SUI is the second most common cause of incontinence in older women. �In men, SUI is usually due to sphincter damage following radical prostatectomy
�Incontinence in the setting of outlet obstruction is the second most common cause of incontinence �it generally presents as urge incontinence owing to the associated DO;
�Detrusor underactivity is usually idiopathic �When it causes incontinence, detrusor underactivity is associated with overflow incontinence
Causes Unrelated to the Lower Urinary Tract (“Functional” Incontinence) �attributed to deficits of cognition and mobility. �may still have obstruction or stress incontinence and benefit from targeted therapy
DIAGNOSTIC APPROACH Evaluation �The evaluation should identify transient and established causes of incontinence, �assess the patient’s environment and available support, �and detect uncommon but serious conditions that may underlie incontinence
Voiding Diary � 48 to 72 hours �the diary records the time of each void and incontinent episode �functional bladder capacity
Targeted Physical Examination �neurologic diseases �atrophic vaginitis �general medical illnesses
Stress Testing and PVR Measurement �The cough or strain �PVR
Laboratory Investigation �BUN, creatinine, U/A, U/C and PVR should be checked in all older patients. �Serum sodium, calcium, and glucose should be measured in patients with confusion
�The first step is to identify individuals with overflow inc (e. g. , PVR > 450 m. L) �Because obstruction and underactive detrusor cannot be differentiated clinically �The next step is to search for hydronephrosis in men whose PVR exceeds 200 m. L and to decompress those in whom it is found
Urodynamic Testing �When diagnostic uncertainty may affect therapy and when empiric therapy has failed and other approaches would be tried.
Thank you Dr. Peyman Salehi
Stepwise Approach to Treatment of Urinary Incontinence
Detrusor overactivity with normal contractility (DO): Urge �Bladder retraining or prompted voiding regimens pharmacologically and add intermittent or �indwelling catheterization
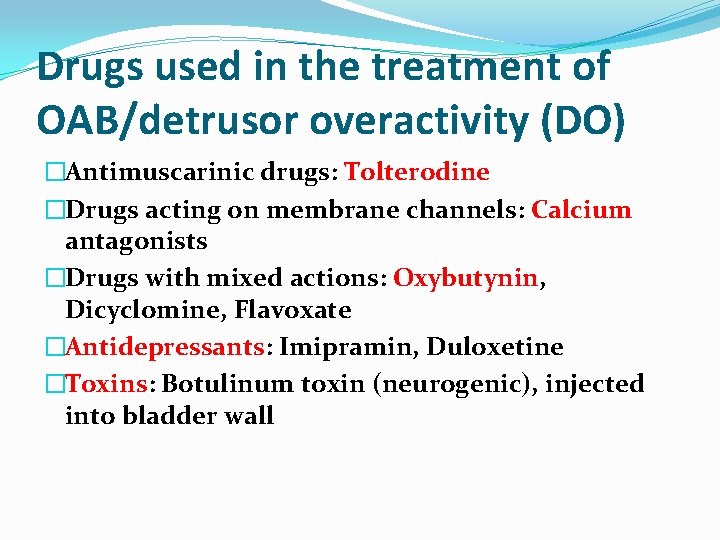
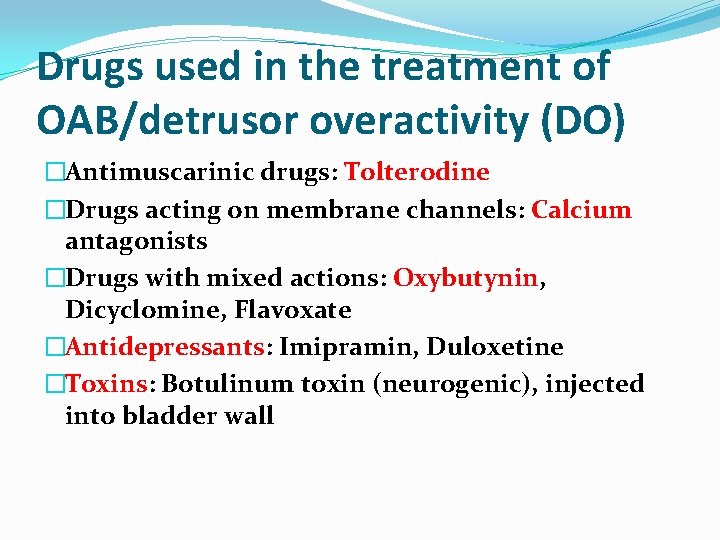
Drugs used in the treatment of OAB/detrusor overactivity (DO) �Antimuscarinic drugs: Tolterodine �Drugs acting on membrane channels: Calcium antagonists �Drugs with mixed actions: Oxybutynin, Dicyclomine, Flavoxate �Antidepressants: Imipramin, Duloxetine �Toxins: Botulinum toxin (neurogenic), injected into bladder wall
Detrusor hyperactivity with impaired contractility (DHIC): Urge �If bladder empties adequately, behavioral methods �If residual urine ≥ 150 m. L, augmented voiding techniques or intermittent catheterization
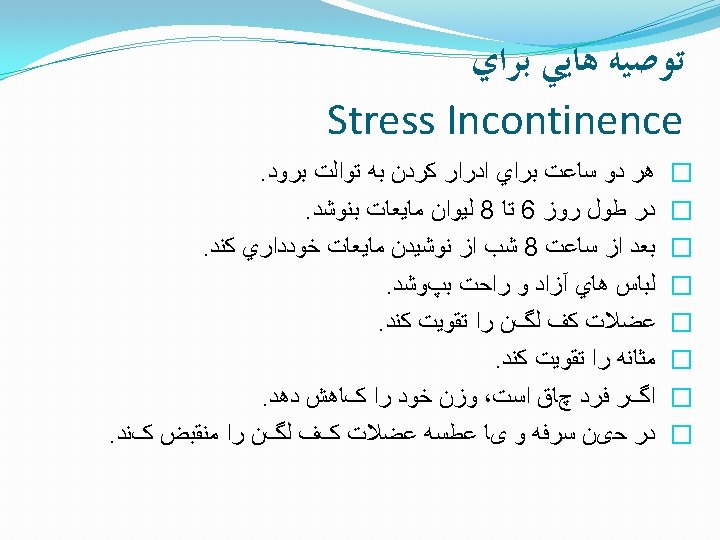
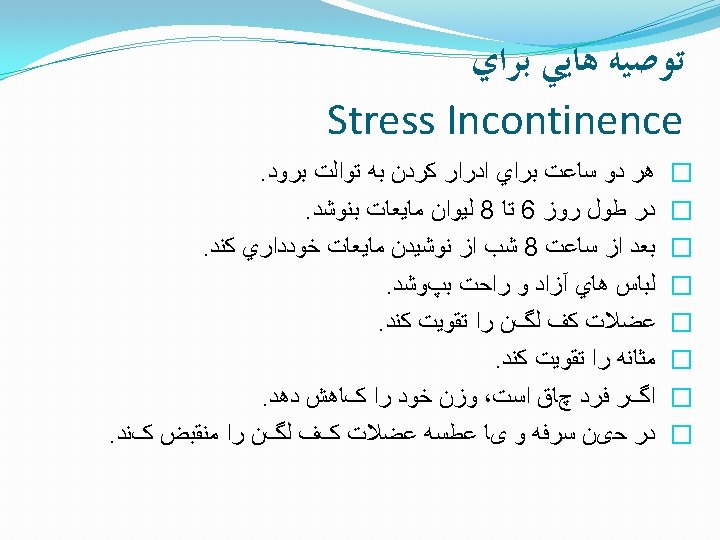
Stress incontinence: Stress � 1. Conservative methods (weight loss if obese; treatment of cough or atrophic vaginitis; physical maneuvers to prevent leakage [e. g. , tighten pelvic muscles before cough, cross legs]; occasionally, use of tampon or pessary is useful)
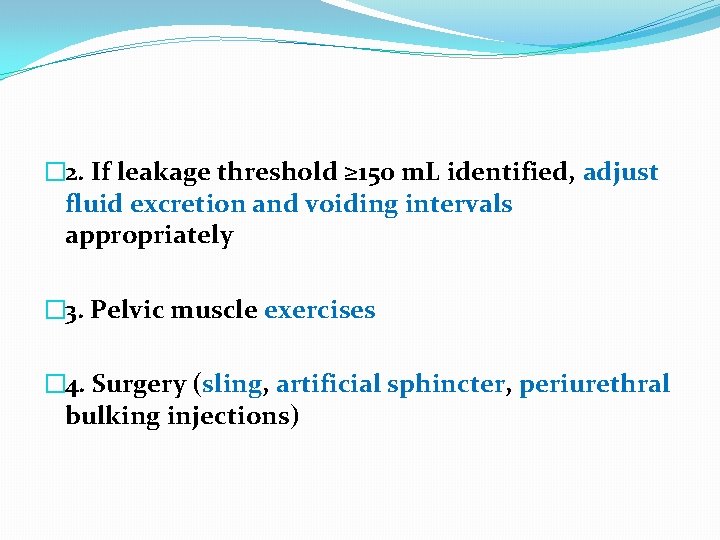
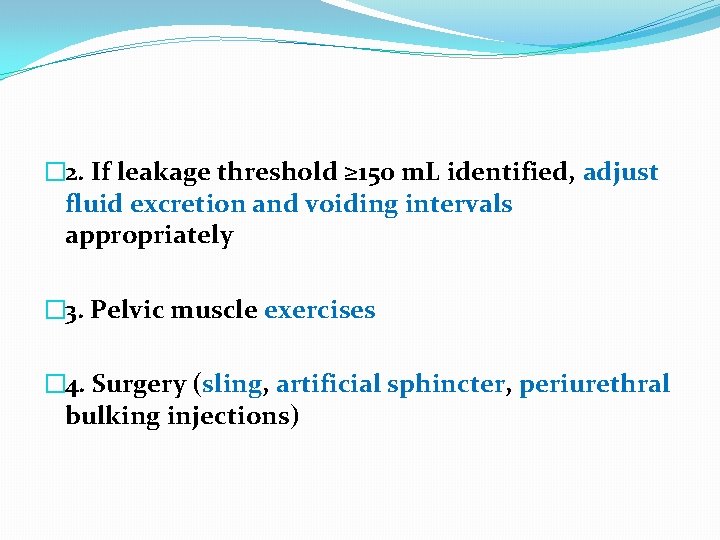
� 2. If leakage threshold ≥ 150 m. L identified, adjust fluid excretion and voiding intervals appropriately � 3. Pelvic muscle exercises � 4. Surgery (sling, artificial sphincter, periurethral bulking injections)
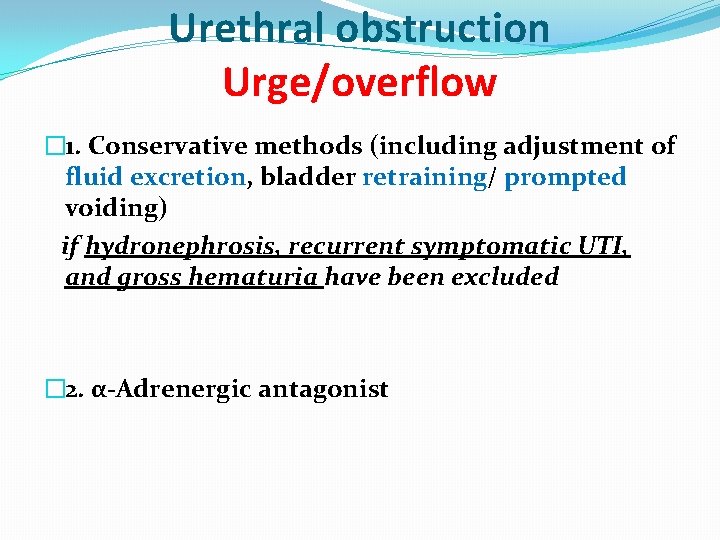
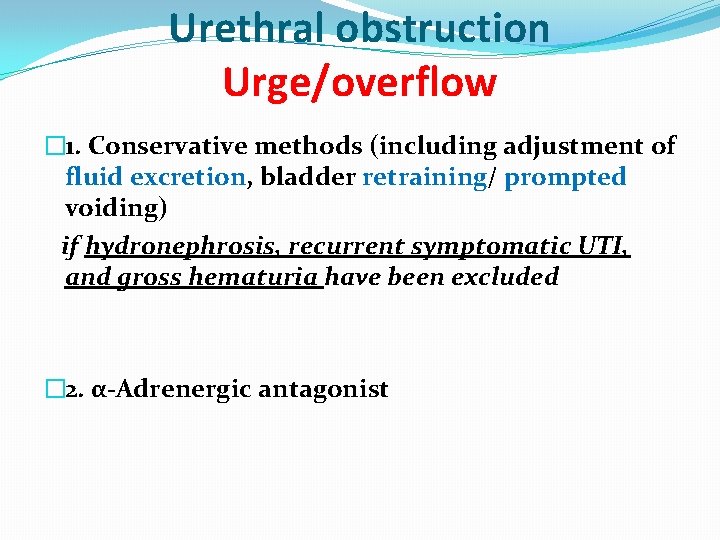
Urethral obstruction Urge/overflow � 1. Conservative methods (including adjustment of fluid excretion, bladder retraining/ prompted voiding) if hydronephrosis, recurrent symptomatic UTI, and gross hematuria have been excluded � 2. α-Adrenergic antagonist
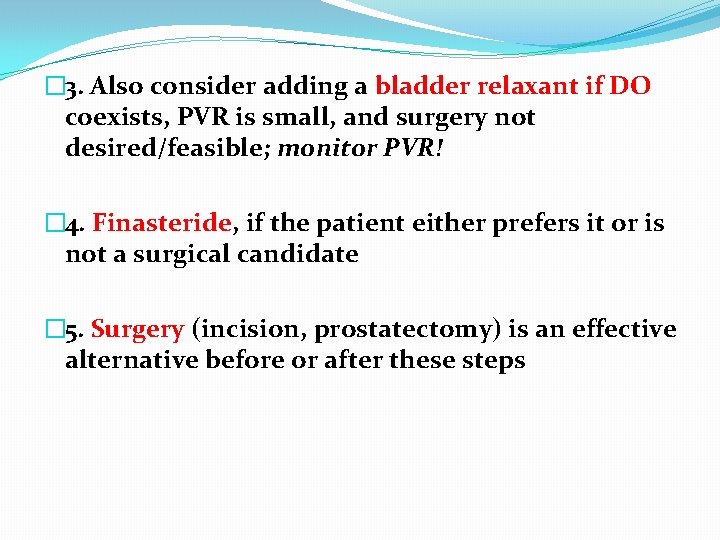
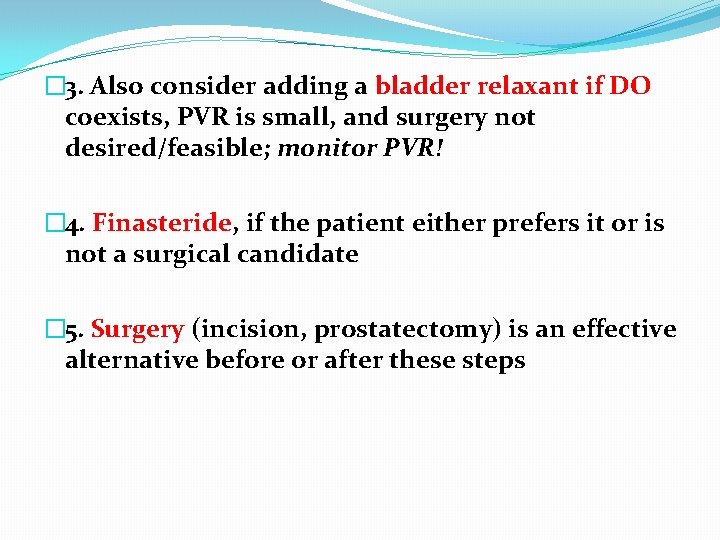
� 3. Also consider adding a bladder relaxant if DO coexists, PVR is small, and surgery not desired/feasible; monitor PVR! � 4. Finasteride, if the patient either prefers it or is not a surgical candidate � 5. Surgery (incision, prostatectomy) is an effective alternative before or after these steps
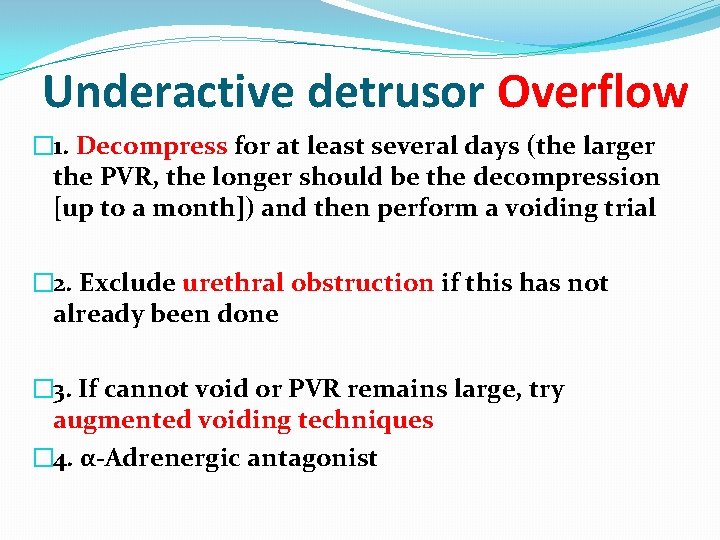
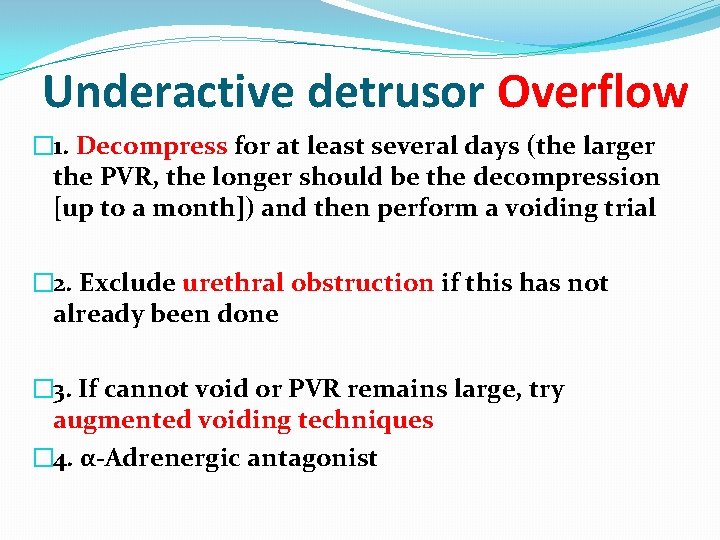
Underactive detrusor Overflow � 1. Decompress for at least several days (the larger the PVR, the longer should be the decompression [up to a month]) and then perform a voiding trial � 2. Exclude urethral obstruction if this has not already been done � 3. If cannot void or PVR remains large, try augmented voiding techniques � 4. α-Adrenergic antagonist
�For cognitively impaired patients, “prompted voiding” is used �Asked every 2 hours whether they need to void, patients are escorted to the toilet if the response is affirmative
�Thus oxybutynin and tolterodine should be considered first-line pharmacotherapy in this population �Regardless of which antimuscarinic is used, urinary retention may develop. �The PVR and urine output should be monitored, especially with DHIC, in which the detrusor is already weak.
�Other remedies for urge incontinence, including electrical stimulation and selective nerve blocks, are successful in selected situations
�there is little evidence that vasopressin is effective for geriatric incontinence �the high prevalence of contraindications to its use (e. g. , hyponatremia, renal insufficiency, heart failure), the risk of inducing serious hyponatremia with fluid retention, the potentially adverse impact on calcium and potassium excretion
Hormonal treatment of UI �Oestrogen �local administration may be the most beneficial route
Condom catheters �helpful for men, but they are associated with skin breakdown, bacteriuria, and decreased motivation to become dry
�Indwelling urethral catheters are not recommended for detrusor overactivity because they usually exacerbate it
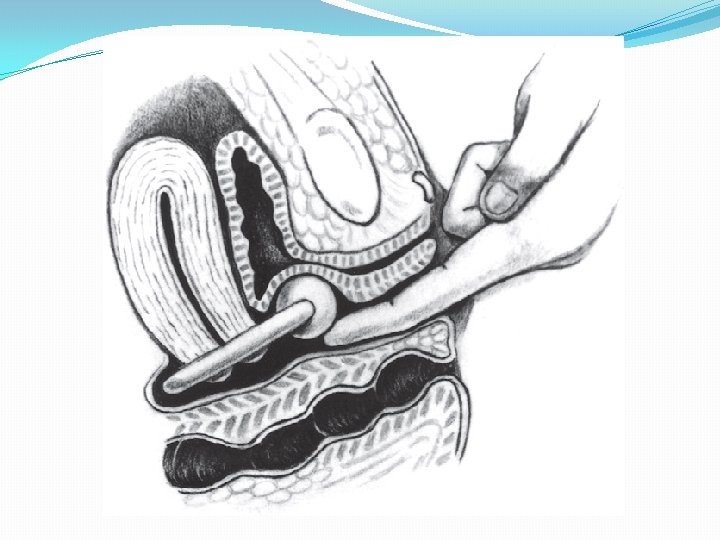
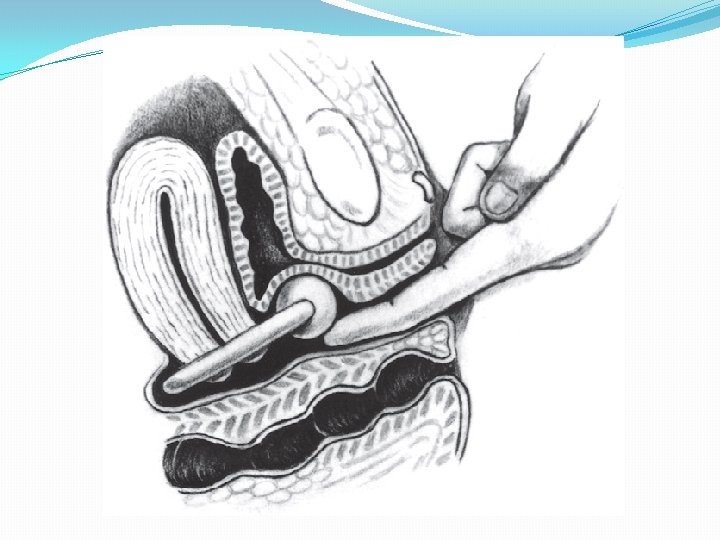
Stress Incontinence �weight loss �Caffeine intake reduction, �by postural maneuvers : Crossing the legs and bending forward during coughing �By therapy of precipitating conditions such as atrophic vaginitis or cough (e. g. , due to an ACE inhibitor), �and by insertion of a pessary
�Pelvic muscle exercises can decrease incontinence substantially in older women who are motivated
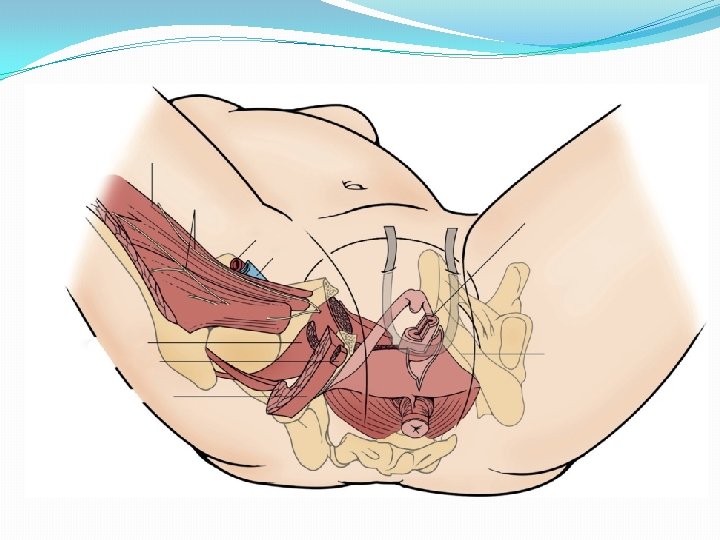
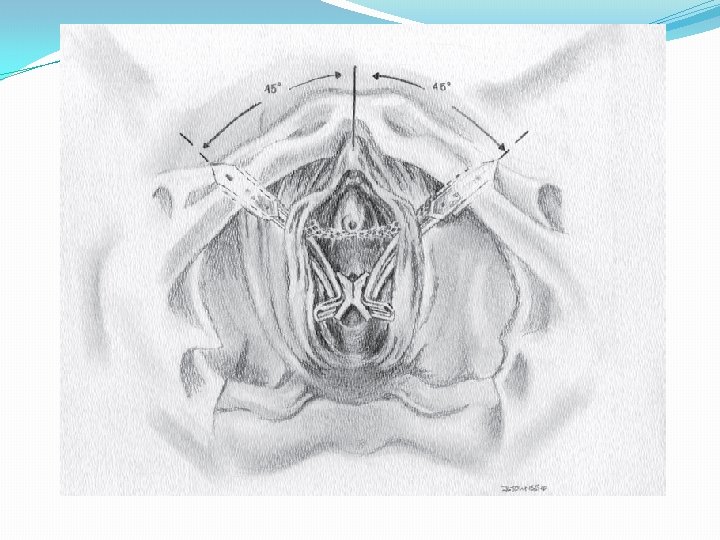
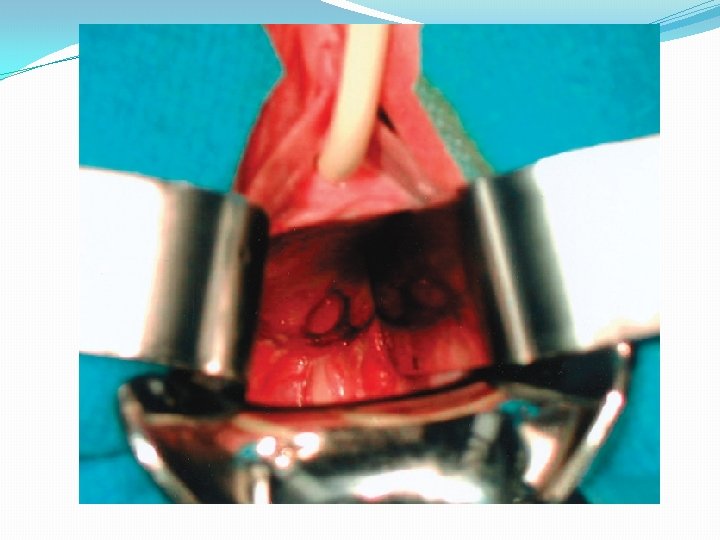
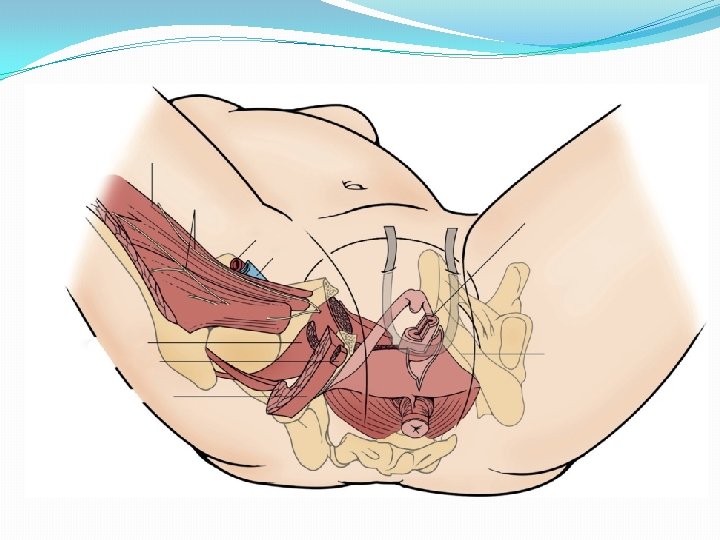
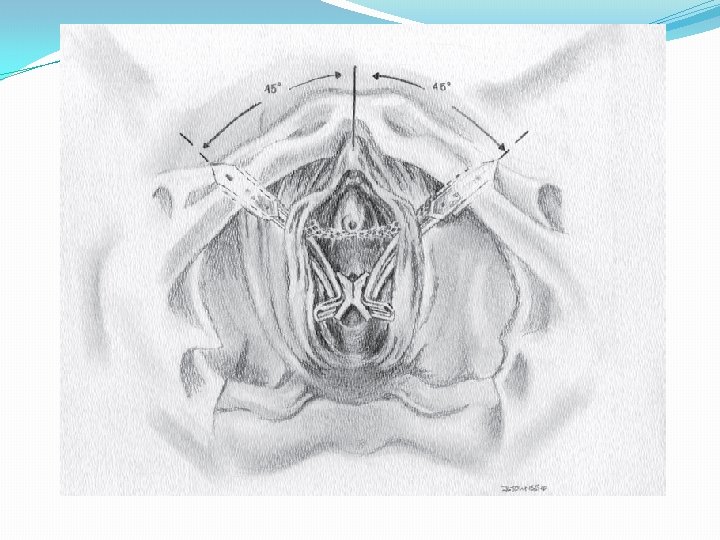
�Older women generally can tolerate a suburethral sling �but the ability to perform the midurethral procedures under regional, or even local, anesthesia on an outpatient basis makes them more feasible

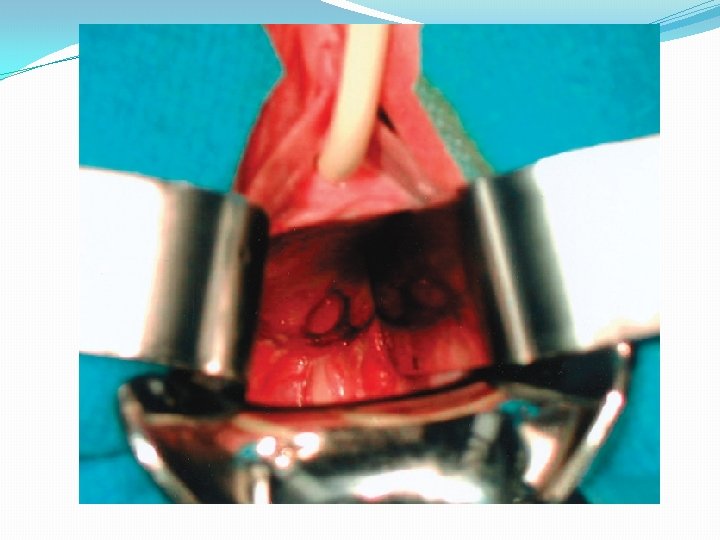
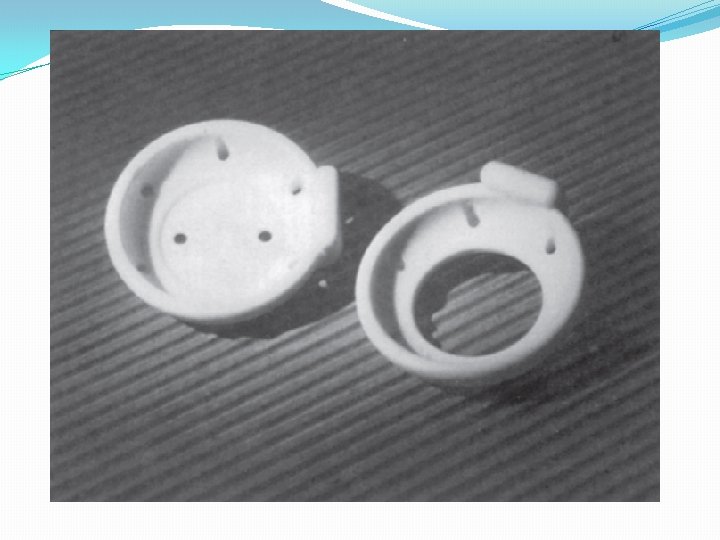
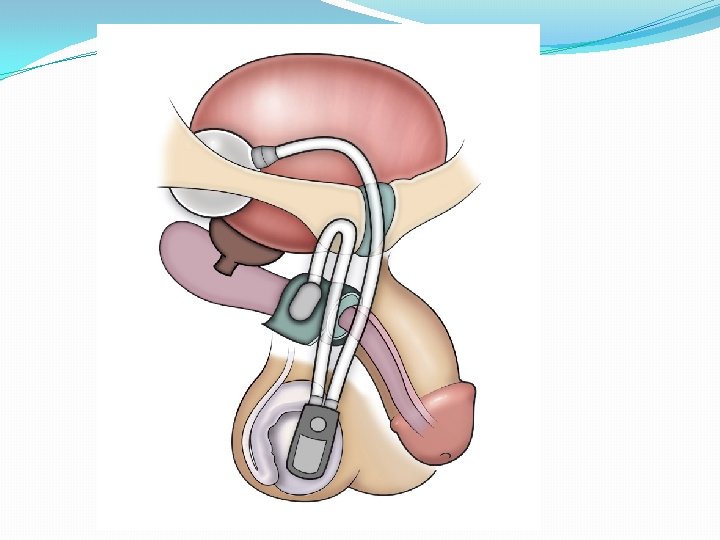
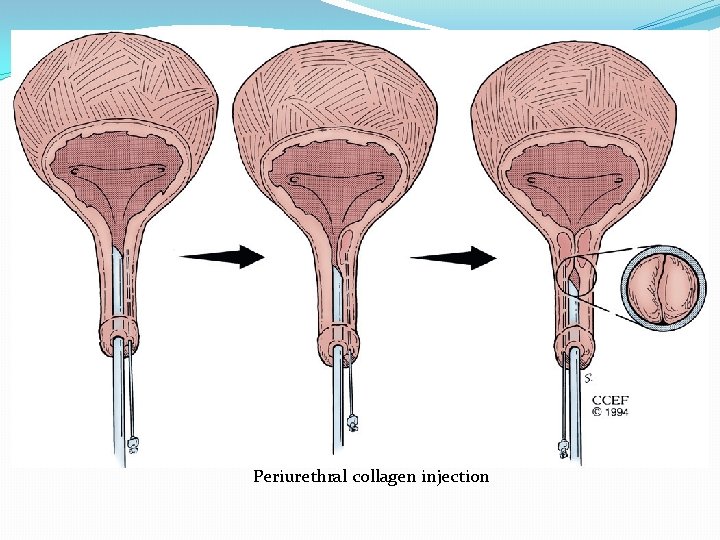
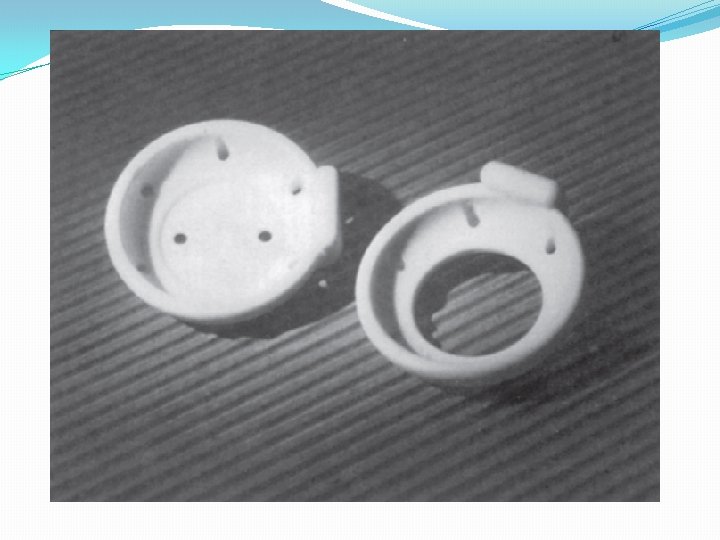
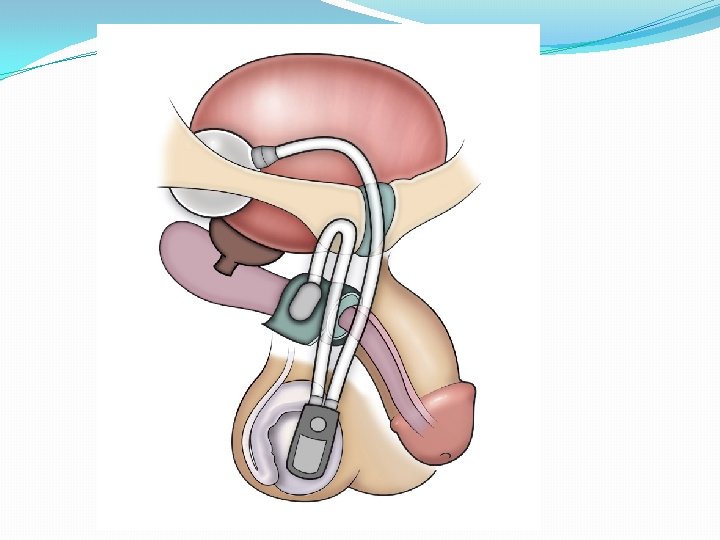
�Other treatments for sphincter incompetence include: �periurethral bulking injections and �insertion of an artificialsphincter
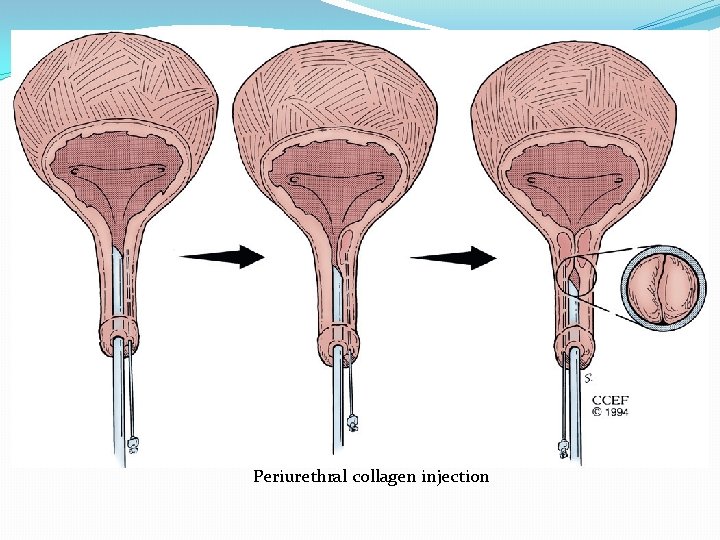
Periurethral collagen injection
Outlet Obstruction �α-adrenergic antagonists: tamsulosin and alfuzosin, are more selective �The 5α-reductase inhibitors (finasteride or dutasteride) have also proved effective as monotherapy
Underactive Detrusor �The first step is to use indwelling or intermittent catheterization: (at least 7 to 14 days) �For patients presenting with acute retention, an α blocker should be used as well.
�Bethanechol (40 to 200 mg/day in divided doses) is occasionally useful in a patient whose bladder contracts poorly because of treatment with anticholinergic agents that cannot be discontinued (e. g. , tricyclic antidepressant).
Principles of Indwelling Catheter Care �upper thigh or abdomen �Empty the bag every 8 hours. �Do not routinely irrigate the catheter �Surveillance cultures are unnecessary �to change it every 1 to 2 months