THE GERIATRIC GIANTS MEDICINE 400 Jane Courtney Hollywood






























- Slides: 77
THE GERIATRIC GIANTS MEDICINE 400 Jane Courtney Hollywood Private Hospital 30 th June 2008

Immobility Instability Incontinence Impaired intellect/memory

Impaired vision Impaired hearing Delirium Poly-pharmacy Care provision
Assessment Multi-disciplinary Functional - adl’s - iadl’s Problem oriented
FALLS
INCIDENCE – 30% community dwellers >65 years – 50% long term care – 60% fall in last year
CONSEQUENCES • 10 – 15% fracture • Decrease in functional status • 2% injurious falls result in death

COSTS • 8% ED presentations >70 years • 33% of these admitted • Median stay 8 days
RISKS • Rarely single cause
Falls usually occur when a threat to the normal homeostatic mechanisms that maintain postural stability is superimposed on age-related declines in balance, ambulation and cardiovascular function. Threat • Acute illness • Environmental stress • Unsafe walking surface

RISK FACTORS • • • Age Female Past fall Cognitive impairment Lower limb weakness Balance disturbance
RISK FACTORS • • • Psychotropic meds Arthritis Past CVA Orthostatic hypotension Dizziness

AGE RELATED FUNCTIONAL DECLINE • Visual • Proprioceptive • Vestibular

ENVIRONMENT • • • FOOTWEAR HOME MODIFICATIONS BEHAVIOUR SAFETY DEVICES SOCIAL INTEGRATION

DISEASE RELATED FUNTIONAL DECLINE
neurological • • CVA Parkinsons Cerebellar Neuropathy Dementia Delerium Epilepsy

cardiovascular • • Arrythmia Orthostatic hypotension Anatomical Vasomotor instability

GIT • Bleeding • D&V • Defecation syncope
metabolic • • Hypothyroid Hypoglycemia Hypokalemia hyponatremia
UGS • Micturition syncope • Nocturia • Incontinence

musculoskeletal • Arthritis • Myopathy • Deconditioning
Psychiatric • Anxiety • Depression

medications • • • Antihypertensives and cardiac Antidepressants Antipsychotics Benzodiazepines Levadopa Narcotics

toxins • Alcohol
MECHANISM • • • SYNCOPE /HYPOTENSION SEIZURE DIZZINESS / BALANCE GAIT DISTURBANCE PAIN / WEAKNESS MECHANICAL FALL
FUNCTIONAL IMPAIRMENT • • BP regulation Central processing Gait Neuromotor function Postural control Proprioception Vestibular vision
EVALUATION • • • History esp of fall Examination esp BP, balance, vision, gait Get up and go Divided attention Tests
PREVENTION • • Strength and balance Education Medications Environmental mods

PREVENT COMPLICATIONS
DEMENTIA
J-0 Causes of Cognitive Impairment

1 Delirium • Sepsis • Hypoxia • Biochemical disturbances Calcium, sodium, glucose, urea, hepatic
DEFINITION • An acute organic mental syndrome characterized by: • • • Global cognitive impairment Reduced consciousness Disturbed attention Psychomotor activity Sleep-wake cycle disturbance
2 Neurological disease • Brain tumour • Stroke • Subdural
3 Psychiatric Disease • Depression • Anxiety • Alcohol or other substance abuse
4 Medications
5 “Classics” • Thyroid • B 12 • Folate
6 Benign Forgetfulness

7 Dementia
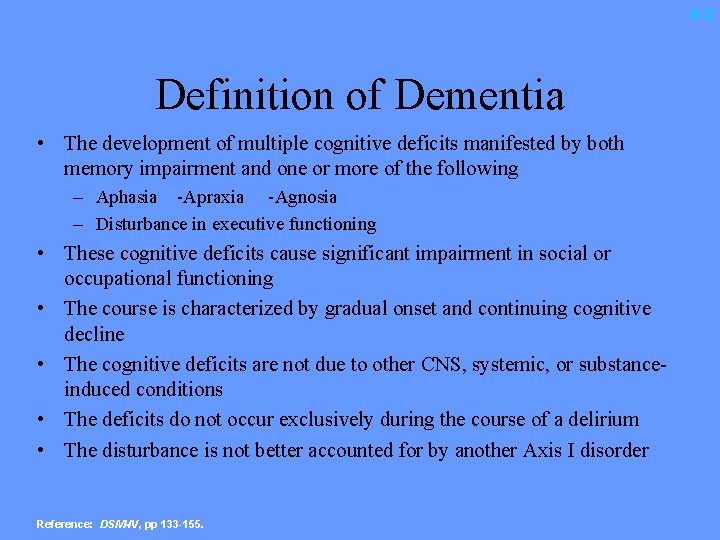
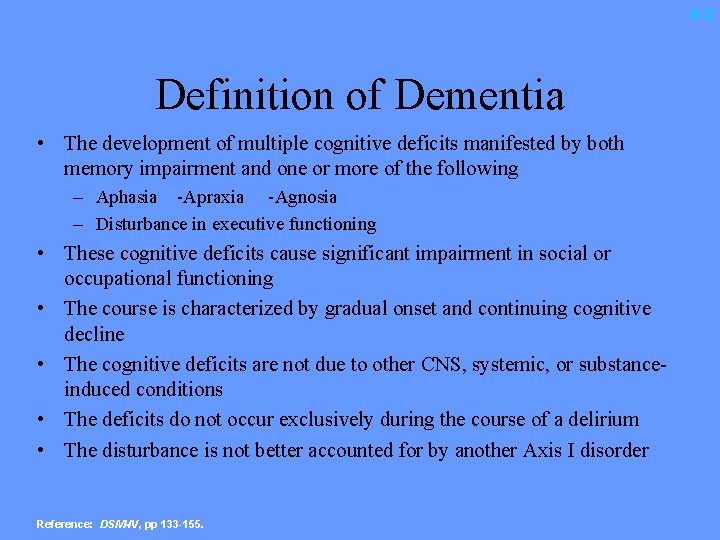
A-2 Definition of Dementia • The development of multiple cognitive deficits manifested by both memory impairment and one or more of the following – Aphasia -Apraxia -Agnosia – Disturbance in executive functioning • These cognitive deficits cause significant impairment in social or occupational functioning • The course is characterized by gradual onset and continuing cognitive decline • The cognitive deficits are not due to other CNS, systemic, or substanceinduced conditions • The deficits do not occur exclusively during the course of a delirium • The disturbance is not better accounted for by another Axis I disorder Reference: DSM-IV, pp 133 -155.

CRITERIA FOR DIAGNOSIS • MEMORY IMPAIRMENT • OTHER COGNITIVE IMPAIRMENT – Language, motor skills, perception • • ADL IMPAIRMENT INSIDIOUS ONSET DETERIORATING NO OTHER CAUSE – Systemic, neurological, psychiatric
CRITERIA FOR DIAGNOSIS • PATHOLOGY- autopsy or brain biopsy
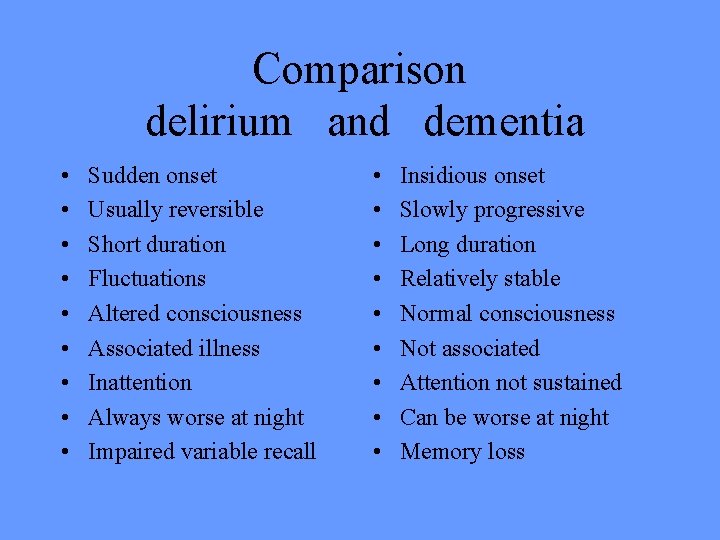
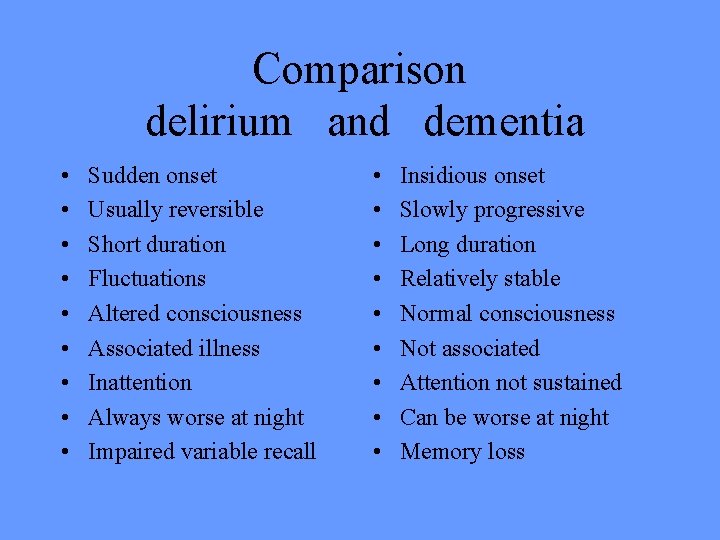
Comparison delirium and dementia • • • Sudden onset Usually reversible Short duration Fluctuations Altered consciousness Associated illness Inattention Always worse at night Impaired variable recall • • • Insidious onset Slowly progressive Long duration Relatively stable Normal consciousness Not associated Attention not sustained Can be worse at night Memory loss
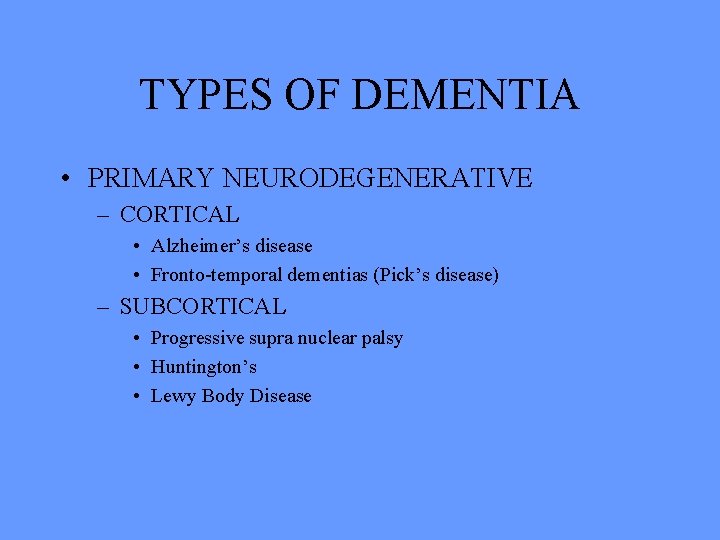
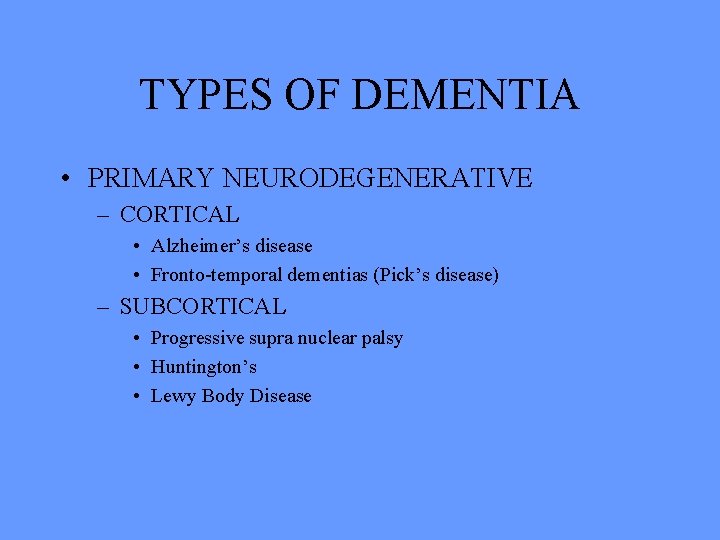
TYPES OF DEMENTIA • PRIMARY NEURODEGENERATIVE – CORTICAL • Alzheimer’s disease • Fronto-temporal dementias (Pick’s disease) – SUBCORTICAL • Progressive supra nuclear palsy • Huntington’s • Lewy Body Disease
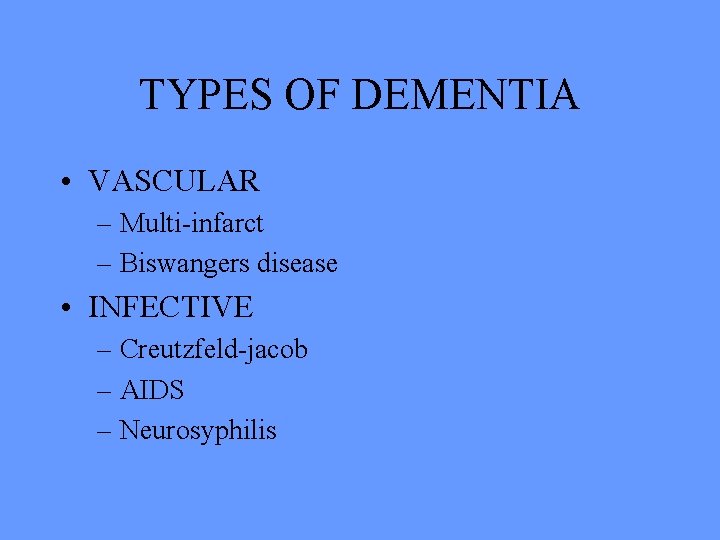
TYPES OF DEMENTIA • VASCULAR – Multi-infarct – Biswangers disease • INFECTIVE – Creutzfeld-jacob – AIDS – Neurosyphilis
TYPES OF DEMENTIA • TRAUMA – Sub dural – Dementia pugulistica – radiotherapy • NORMAL PRESSURE HYDROCEPHALUS
TYPES OF DEMENTIA • ASSOCIATED WITH OTHER DISEASES – Parkinson’s – Wilson’s – Multiple sclerosis – Tumours – Vasculitis

A-1 Alzheimer’s Disease Diagnosis • Acquired decline in cognitive function of an insidious and progressive nature – Loss of memory – Impairment of at least one of; • • • Language Perception Praxis Problem solving, planning, organization Judgement, insight or abstract thought – Decline in ability to perform activities of daily living

A-7 A B • (A) Immunocytochemical staining of NFTs in the isocortex of human AD brain with the anti-tau antibody AT 8 • (B) Immunocytochemical staining of senile plaques in the isocortex of human AD brain with the anti-amyloid antibody 4 G 8

A-9 • Role Cholinergic Hypothesis – Acetylcholine (ACh) is an important neurotransmitter in areas of the brain involved in memory formation (eg. hippocampus, cerebral cortex, and amygdala) • Impact – Loss of ACh occurs early in AD and correlates with the impairment of memory • Treatment approach – Enhancement or restoration of cholinergic function may significantly reduce the severity of cognitive loss Reference: Mayeux R, et al. N Engl J Med. 1999; 341: 1670 -1679.
TREATMENT
Overall Management • • • Is it Alzheimers? OR what? Are there any reversible components? Any specific treatments? Educate and support carer/family. Treat symptoms as they arise. Treat intercurrent problems.
Medications • Can cause cognitive impairment • Can treat memory loss (Alzheimer’s, DLB) • Can treat symptoms • Can prevent (vascular)
Cause Cognitive Impairment • • • Sedatives Antidepressants Analgesics “SIADH” Antiepileptics Specials – Digoxin, cimetidine, lithium.

Treat Memory • • Cholinergics ? oestrogens Vitamin E Selegeline

Treat Symptoms • • • Treat family Non pharmacological Antipsychotics Benzodiazepines ANTIDEPRESSANTS
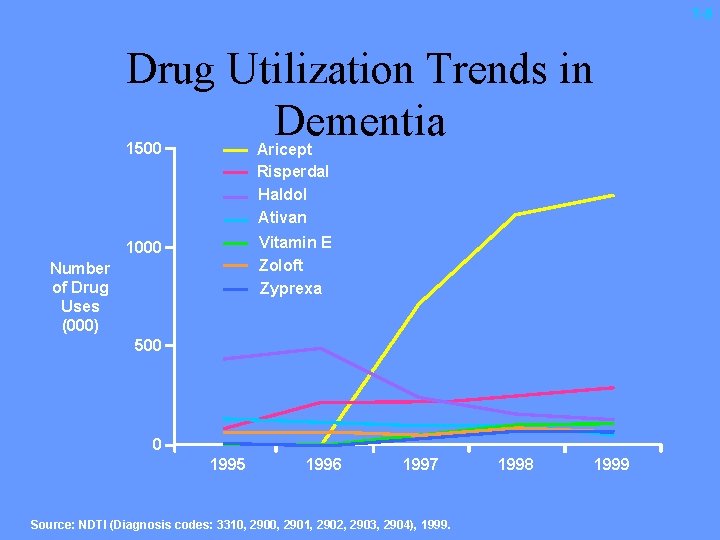
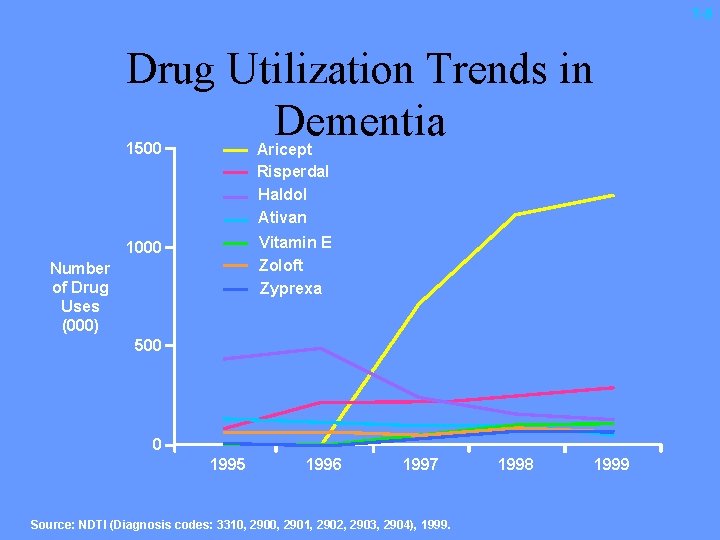
T-5 Drug Utilization Trends in Dementia 1500 Aricept Risperdal Haldol Ativan 1000 Vitamin E Zoloft Zyprexa Number of Drug Uses (000) 500 0 1995 1996 1997 Source: NDTI (Diagnosis codes: 3310, 2901, 2902, 2903, 2904), 1999. 1998 1999
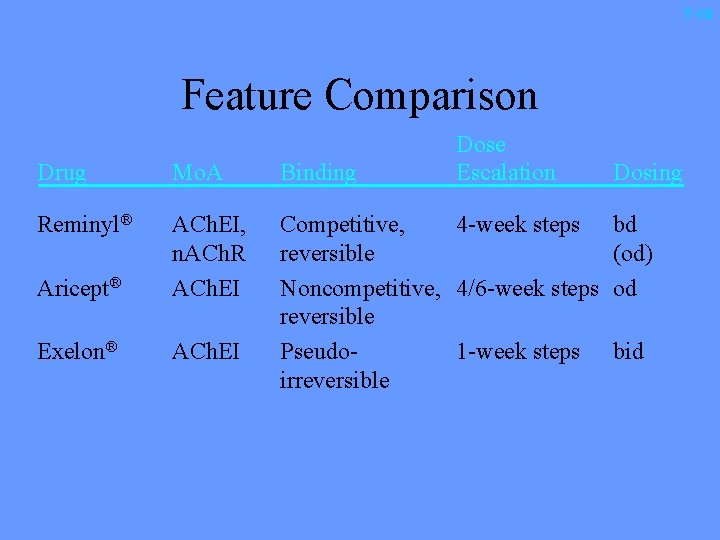
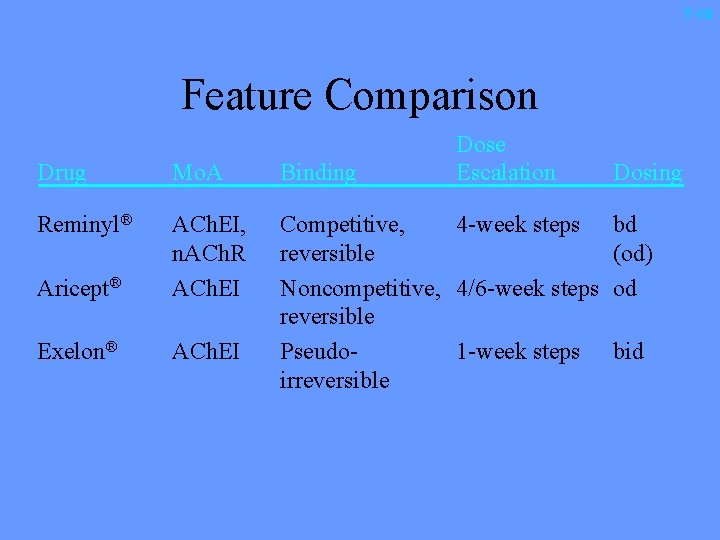
T-10 Feature Comparison Dose Escalation Drug Mo. A Binding Reminyl® Aricept® ACh. EI, n. ACh. R ACh. EI Exelon® ACh. EI Competitive, 4 -week steps reversible Noncompetitive, 4/6 -week steps reversible Pseudo 1 -week steps irreversible Dosing bd (od) od bid

M-4 Neuron and Acetylcholine ACh. E inhibitor Acetic acid Choline Presynaptic nerve terminal M receptor Postsynaptic nerve terminal N receptor ACh. E ACh AD REM 8 59
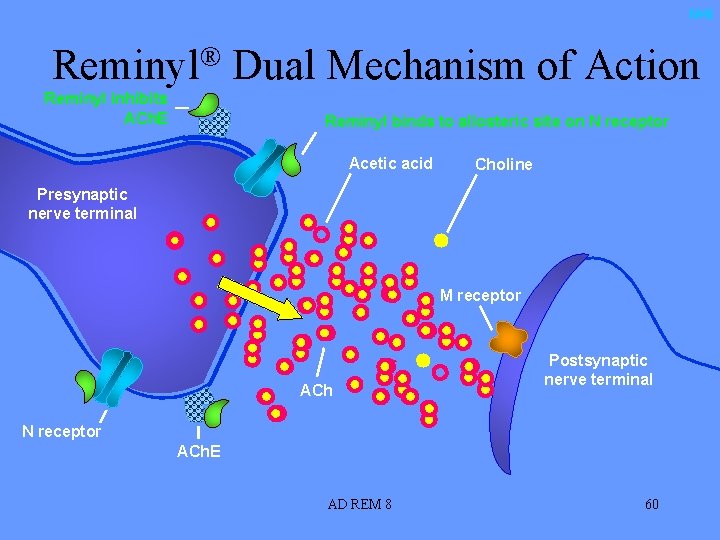
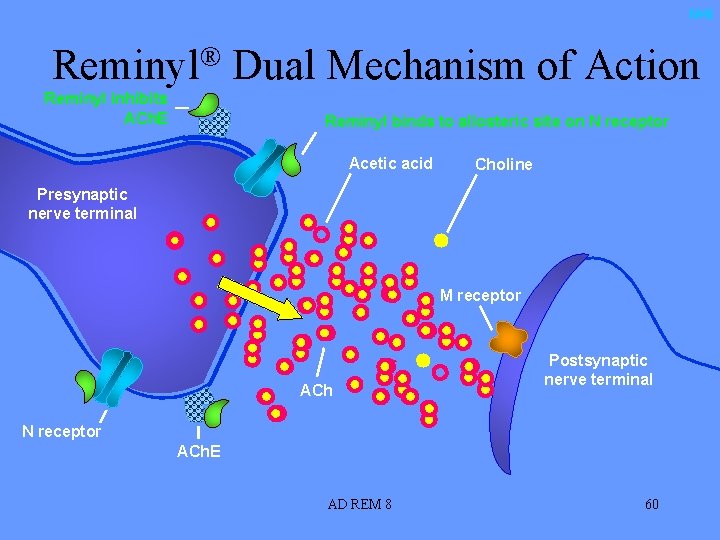
M-6 Reminyl® Dual Mechanism of Action Reminyl inhibits ACh. E Reminyl binds to allosteric site on N receptor Acetic acid Choline Presynaptic nerve terminal M receptor ACh Postsynaptic nerve terminal N receptor ACh. E AD REM 8 60
INCIDENCE • 15% - 30% community-dwelling • 30% hospitalized • 50% long-term care
Predisposes to • • • Rashes Pressure sores Urinary tract infections Falls Fractures Increased risk of institutional care

INCONTINENCE IS A SYMPTOM Incontinence is abnormal at any age. Prevalence increases with age. At no age does it affect the majority of individuals. Even with severe dementia not all people are incontinent NEW INCONTINENCE MUST BE INVESTIGATED

• Transient or established. • Urge, stress or overflow. • Clinical.

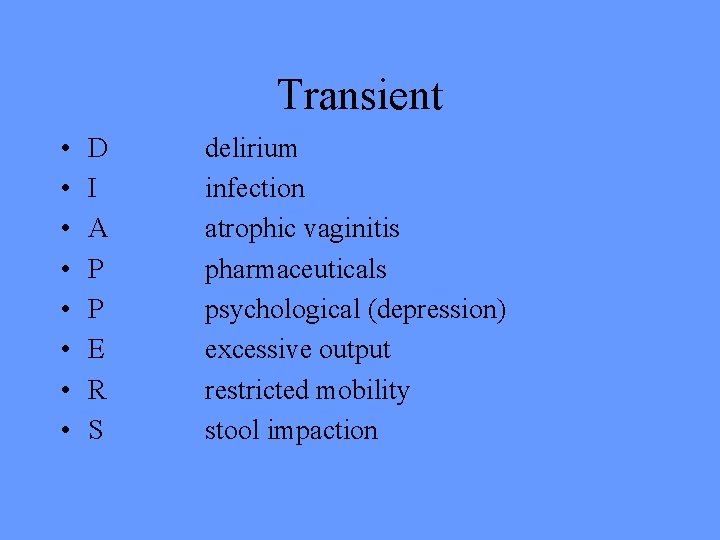
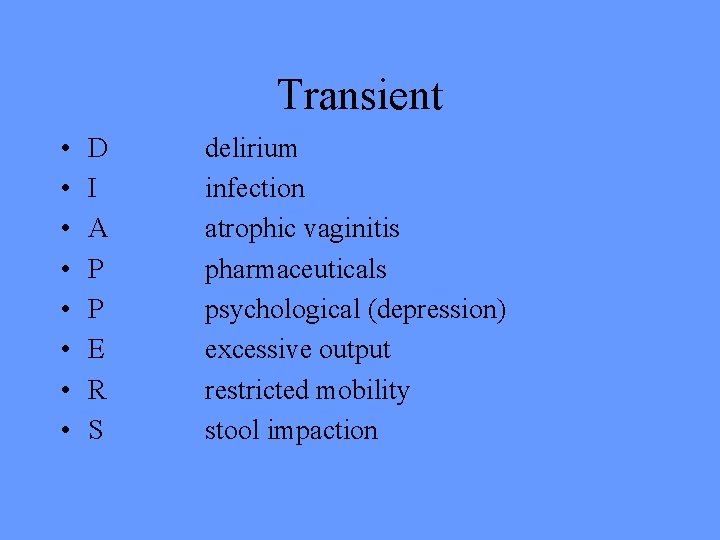
Transient • • D I A P P E R S delirium infection atrophic vaginitis pharmaceuticals psychological (depression) excessive output restricted mobility stool impaction

pharmaceuticals • • Anticholinergics Alpha agonists (men) Alpha antagonists (women) Calcium channel blockers ACE inhibitors (cough) Diruretics Sedatives (and alcohol)
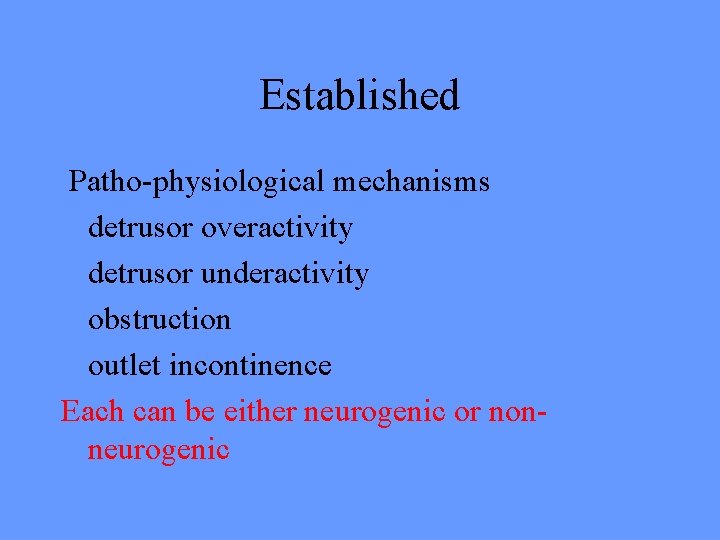
Established Patho-physiological mechanisms detrusor overactivity detrusor underactivity obstruction outlet incontinence Each can be either neurogenic or nonneurogenic



WHAT DO WE DO? HISTORY EXAMINATION INVESTIGATIONS.
TYPE FREQUENCY PATTERN MEDICAL MEDICATIONS FUNCTION

FULL PHYSICAL…. GUIDED PELVIC RECTAL NEUROLOGICAL STRESS
VOIDING CHART U&E, CALCIUM, GLUCOSE URINALYSIS+/- MSU RESIDUAL VOLUME ULTRASOUND URODYNAMICS CYSTOSCOPY
TREATMENT FIRST THE CAUSE IN TRANSIENT STRESS- PELVIC FLOOR EXERCISES - WEIGHT LOSS - OESTROGEN - SURGERY OBSTRUCTION - ALPHA ANTAGONIST - SURGERY
DO - ANTICHOLINERGIC DU - CATHETER PADS, BOTTLES, COMMODES
A LAST WORD ABOUT POLYPHARMACY THE GERIATRICIAN’S PEN v’s A BALANCING ACT
 Geriatric giants
Geriatric giants Geriatric gaints
Geriatric gaints Geriatric giants mnemonic
Geriatric giants mnemonic Geriatric syndrome 14i
Geriatric syndrome 14i 200+400+600+800
200+400+600+800 James neville mason
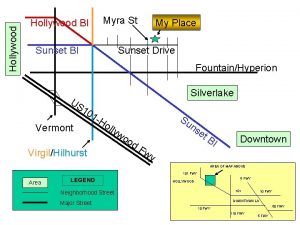
James neville mason Dream factory hollywood
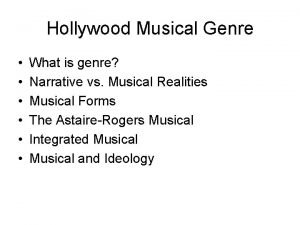
Dream factory hollywood Music genre hollywood
Music genre hollywood Etds universal studios hollywood
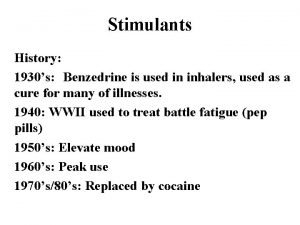
Etds universal studios hollywood Benzedrine inhaler hollywood
Benzedrine inhaler hollywood Hollywood renaissance films
Hollywood renaissance films Hollywood
Hollywood Hollywood africans
Hollywood africans Hollywood 1977
Hollywood 1977 Elements of classical hollywood cinema
Elements of classical hollywood cinema West hollywood rso
West hollywood rso Hollywood silver fox farm v emmett
Hollywood silver fox farm v emmett The hollywood studio system in the 1930s and 1940s
The hollywood studio system in the 1930s and 1940s Prensa rosa española
Prensa rosa española Hollywood vs history
Hollywood vs history Classical hollywood continuity editing
Classical hollywood continuity editing Film capital of the world
Film capital of the world Hollywood versus bollywood
Hollywood versus bollywood Capital of hollywood
Capital of hollywood Golden age of hollywood 1930s
Golden age of hollywood 1930s How was the hollywood ten affected by the accusations
How was the hollywood ten affected by the accusations Where is the hollywood sign
Where is the hollywood sign Inhalt des films
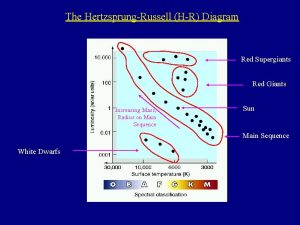
Inhalt des films Red giants and white dwarfs
Red giants and white dwarfs Geriatic giants
Geriatic giants On the hr diagram red supergiants like betelgeuse lie
On the hr diagram red supergiants like betelgeuse lie They might be giants periodic table
They might be giants periodic table Alalu mars
Alalu mars Standing on the shoulders of giants
Standing on the shoulders of giants What do the first four outer planets have in common
What do the first four outer planets have in common Giants by lydia pender
Giants by lydia pender Galileo: on the shoulders of giants
Galileo: on the shoulders of giants What is neptune made of
What is neptune made of Hundred handed giants greek mythology
Hundred handed giants greek mythology Hundred handed giants greek mythology
Hundred handed giants greek mythology Brokk hammer skin
Brokk hammer skin They might be giants math
They might be giants math They might be giants cells
They might be giants cells Courtney badger
Courtney badger Courtney clawson
Courtney clawson Courtney killion
Courtney killion Courtney douglass
Courtney douglass Becks depression inventory
Becks depression inventory Courtney marsh md
Courtney marsh md Courtney bohannon
Courtney bohannon Courtney bass mediator
Courtney bass mediator Colleen and clare
Colleen and clare Courtney given
Courtney given Courtney eccles
Courtney eccles Courtney zotaj
Courtney zotaj Courtney medeiros
Courtney medeiros Courtney sharpe
Courtney sharpe Courtney medeiros
Courtney medeiros Courtney barth
Courtney barth Oklahoma state college of osteopathic medicine
Oklahoma state college of osteopathic medicine Courtney courter
Courtney courter Courtney lisenbee
Courtney lisenbee Courtney beaton
Courtney beaton Sarc f
Sarc f Geriatric hat trick
Geriatric hat trick Geriatric giant
Geriatric giant Geriatric competency assessment
Geriatric competency assessment Chapter 10:4 confusion and disorientation in the elderly
Chapter 10:4 confusion and disorientation in the elderly Objectives of geriatric care
Objectives of geriatric care Community geriatric psychiatry
Community geriatric psychiatry What is geriatric syndromes
What is geriatric syndromes Gems assessment
Gems assessment Gems diamond geriatric
Gems diamond geriatric Va geriatric scholars program
Va geriatric scholars program Geriatric case presentation
Geriatric case presentation Frailty syndrome
Frailty syndrome Palmerston north geriatric
Palmerston north geriatric Centrum geriatric
Centrum geriatric