Diagnostic tests of urinary incontinence EVALUATION The initial



- Slides: 51
Diagnostic tests of urinary incontinence
EVALUATION • The initial evaluation of urinary incontinence includes • characterizing and classifying the type of incontinence • identifying reversible or serious underlying conditions, that may manifest as urinary incontinence • The initial evaluation includes a thorough • history • physical examination, and urinalysis
• IMPACT ON HEALTH • ●Quality of life – Urinary incontinence is associated with depression and anxiety, work impairment, and social isolation • ●Sexual dysfunction – Incontinence during sexual activity (coital incontinence) • , ●Morbidity –perineal infections from moisture and irritation (eg, candida or cellulitis) and falls and fractures. • ●Increased caregiver burden – Incontinence in older persons is associated with increased caregiver
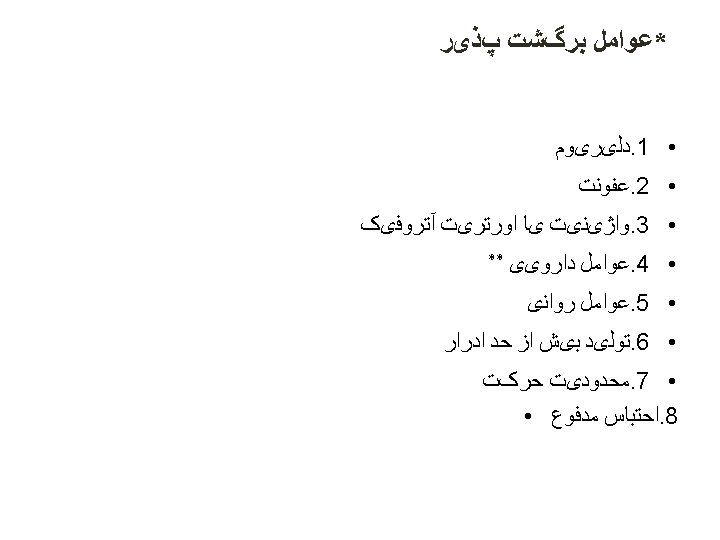
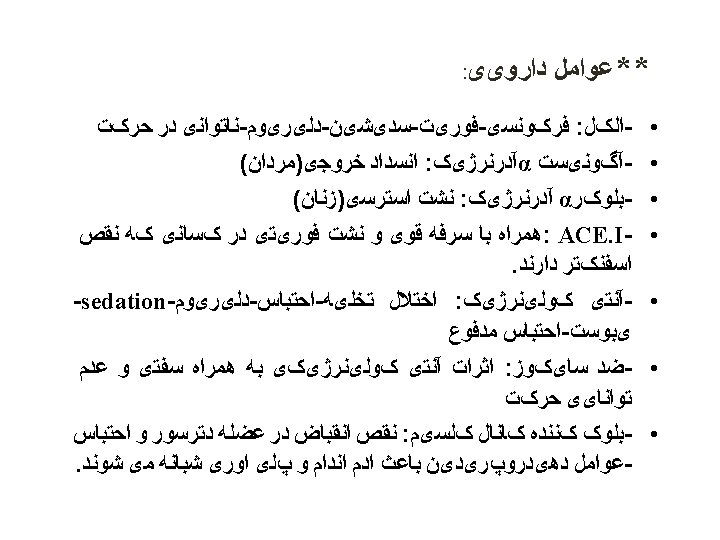
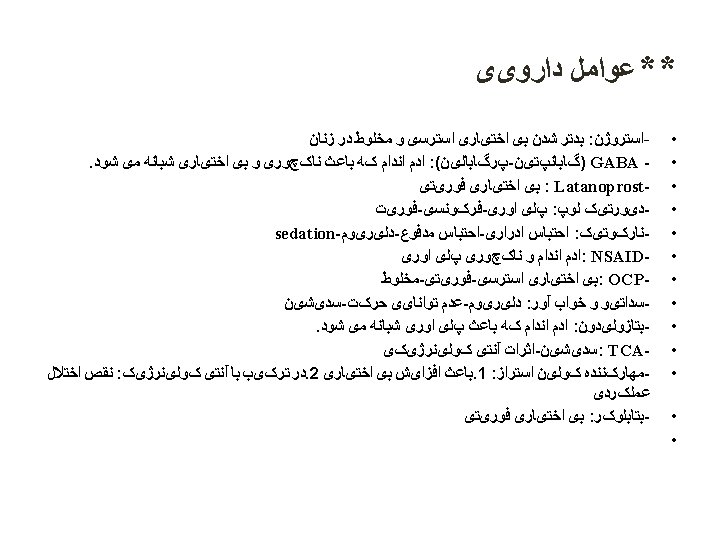
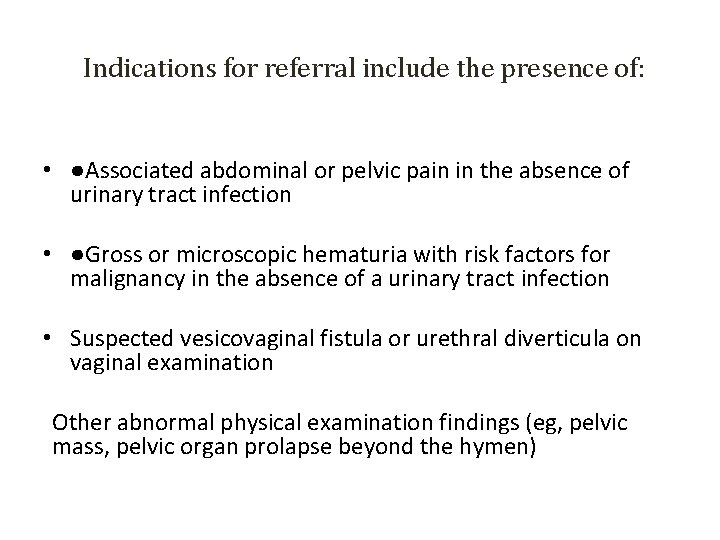
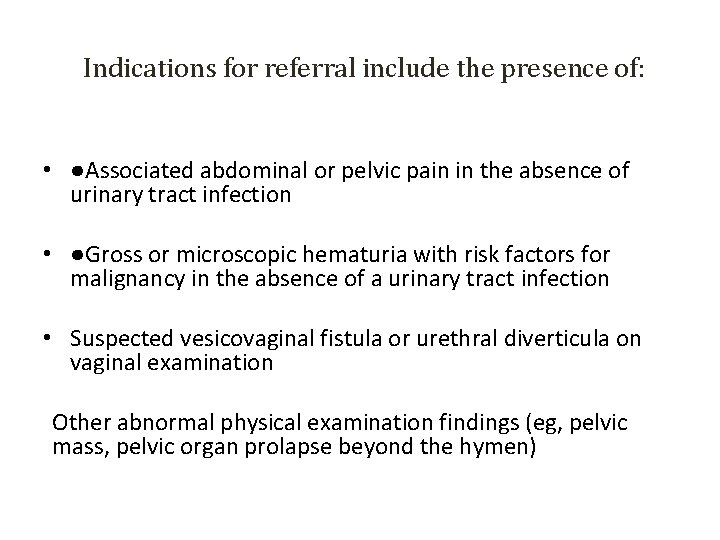
Indications for referral include the presence of: • ●Associated abdominal or pelvic pain in the absence of urinary tract infection • ●Gross or microscopic hematuria with risk factors for malignancy in the absence of a urinary tract infection • Suspected vesicovaginal fistula or urethral diverticula on vaginal examination Other abnormal physical examination findings (eg, pelvic mass, pelvic organ prolapse beyond the hymen)
Indications for referral include the presence of New neurologic symptoms in addition to incontinence ●Uncertainty in diagnosis ●History of pelvic reconstructive surgery pelvic irradiation ●Persistently elevated PVR after treatment of possible causes (eg, medications, stool impaction) • ●Suspected overflow incontinence, particularly in the setting of underlying conditions (eg, neurologic conditions, diabetes • • •
Bladder stress test • Visualization of urine loss from the urethra simultaneous with a cough is diagnostic of Stress urinary incontinence • The bladder stress test can be performed in the supine position during the physical examination. • however , if urine leakage is not observed , the test needs to be performed with a full bladder, in standing position and a single vigorous cough. • A pad is held underneath the perineum and the clinician observes directly whethere is leakage from the urethra.
Bladder stress test. • Delayed leakage suggests detrusor overactivity , especially if there is a large flow of leakage • that is difficult for the patient to stop.
Bladder stress test • A positive bladder stress test does not require treatment unless the patient reports ; significant bother related to the incontinence. • A negative test is less useful because a false negative may result from a small urine volume in the bladder or from patient inhibition. • fill the bladder until the patient feels bladder fullness or is holding at least 300 cc of fluid and then repeat the test. • If the standing cough stress test result remain negative despite patient symptoms of SUI , then multichannel urodynamic testing is recommended.
Measuring Urethral Mobility • Urethral hypermobility (bladder neck hypermobility) is present in most women who have primary SUI. • Urethral mobility in continent women is related to age, parity, and support defects of the anterior vaginal wall.
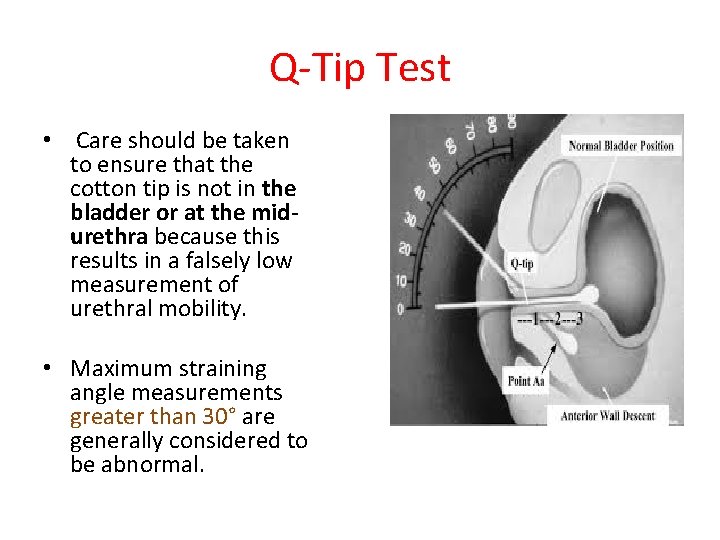
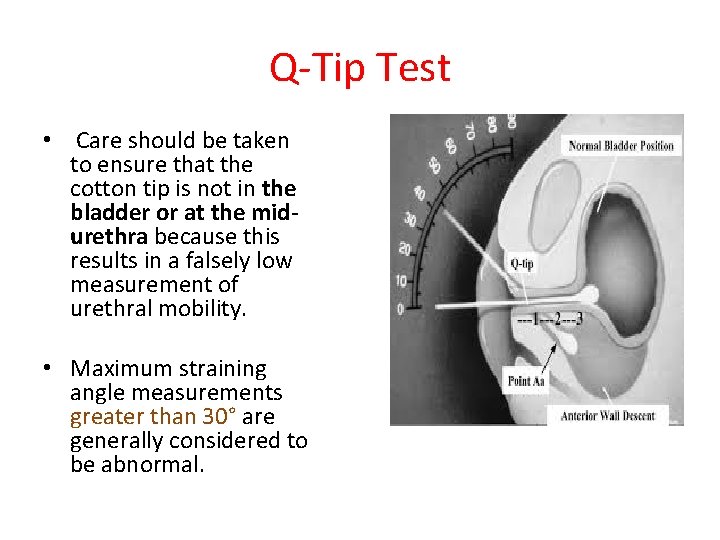
Q-Tip Test • Care should be taken to ensure that the cotton tip is not in the bladder or at the midurethra because this results in a falsely low measurement of urethral mobility. • Maximum straining angle measurements greater than 30° are generally considered to be abnormal.

Q-Tip Test • Women with urodynamic stress incontinence have higher maximum straining Q-tip angles , although there wide overlap in measurements between the continent and incontinent women. • In general, arbitrary cutoff values around 30° are too low to define “normal” urethral mobility for parous women.
Q-Tip Test • Urethral hypermobility is common in asymptomatic women and many women with a positive Q-tip test result do not have stress incontinence. • the presence or absence of hypermobility does not appear to change management of urinary incontinence and this test is no considered useful in helping to diagnosis or treatment of urinary incontinence.
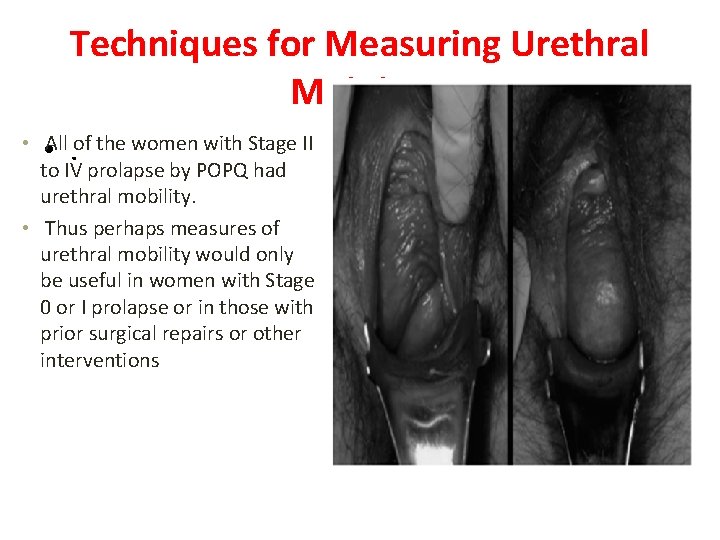
Techniques for Measuring Urethral Mobility • Some clinicians assess for urethral hypermobility solely by assessing the severity of point Aa prolapse. • Studies have demonstrated that almost all (>90 %) women with advanced point Aa prolapse will have a positive cotton swab test.
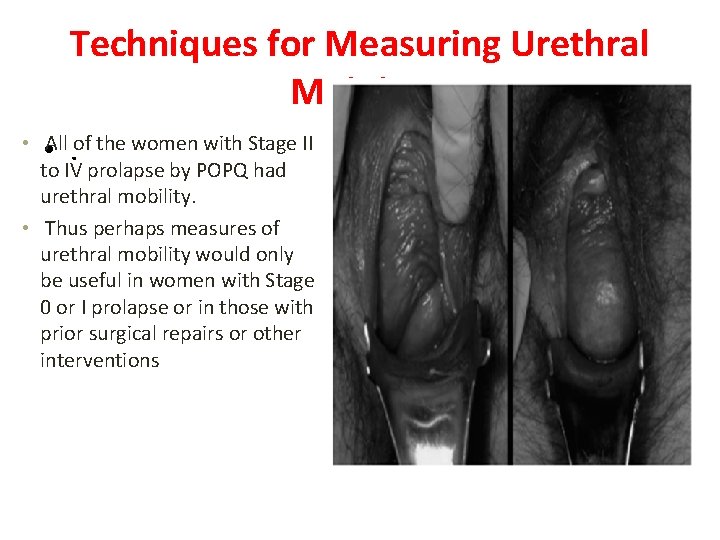
Techniques for Measuring Urethral Mobility • All of the women with Stage II • . to IV prolapse by POPQ had urethral mobility. • Thus perhaps measures of urethral mobility would only be useful in women with Stage 0 or I prolapse or in those with prior surgical repairs or other interventions
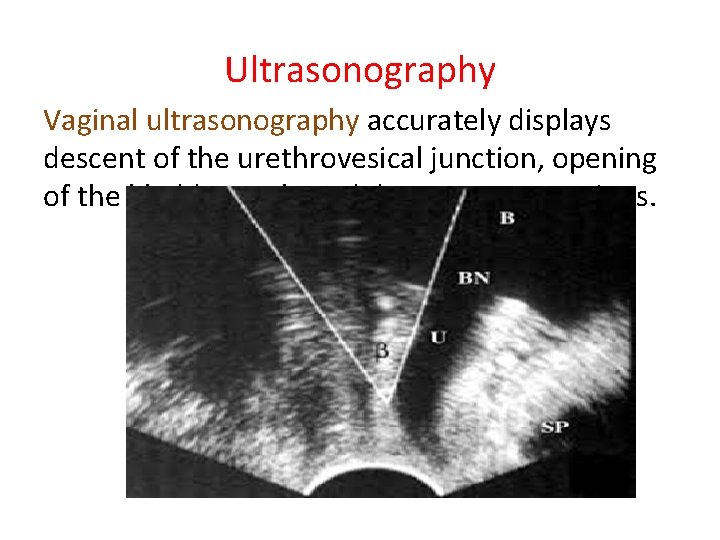
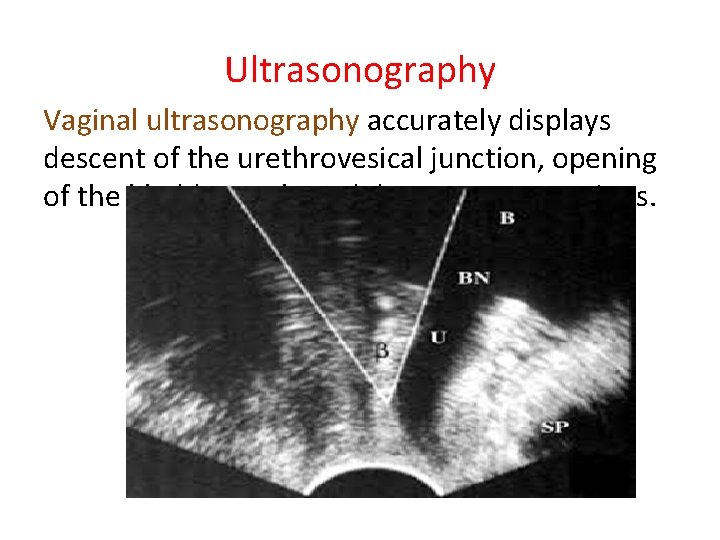
Ultrasonography Vaginal ultrasonography accurately displays descent of the urethrovesical junction, opening of the bladder neck, and detrusor contractions.

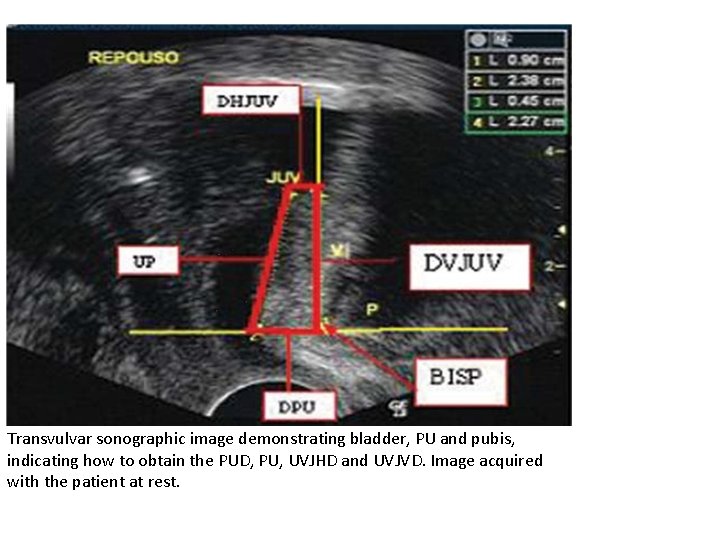
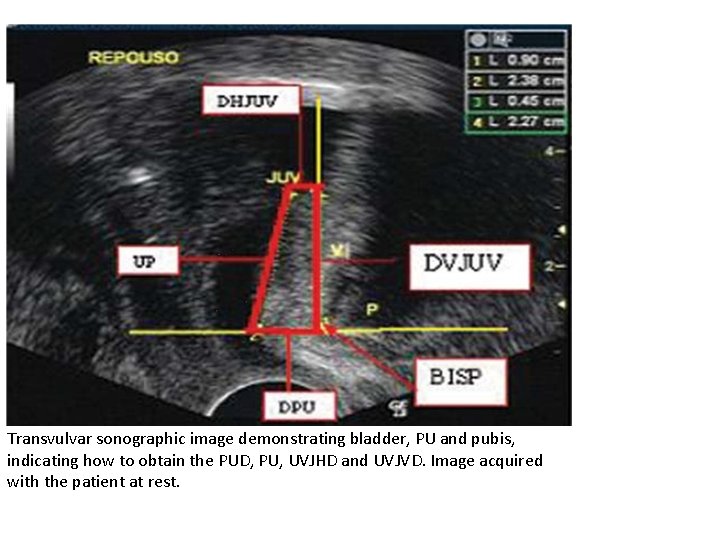
Transvulvar sonographic image demonstrating bladder, PU and pubis, indicating how to obtain the PUD, PU, UVJHD and UVJVD. Image acquired with the patient at rest.

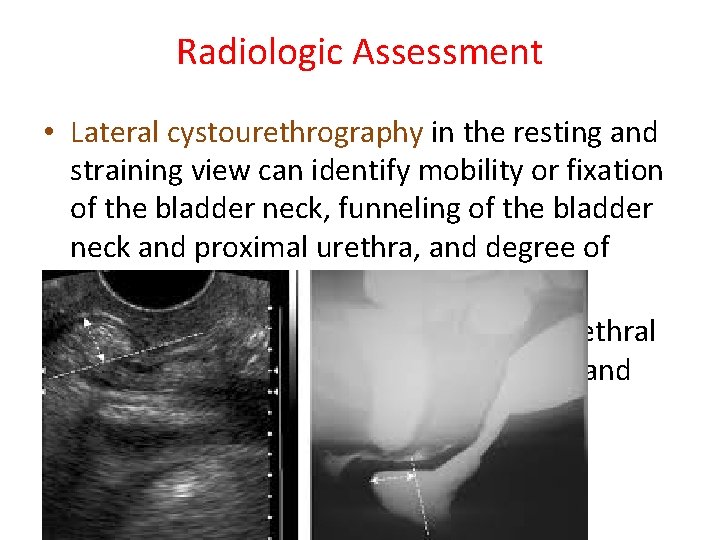
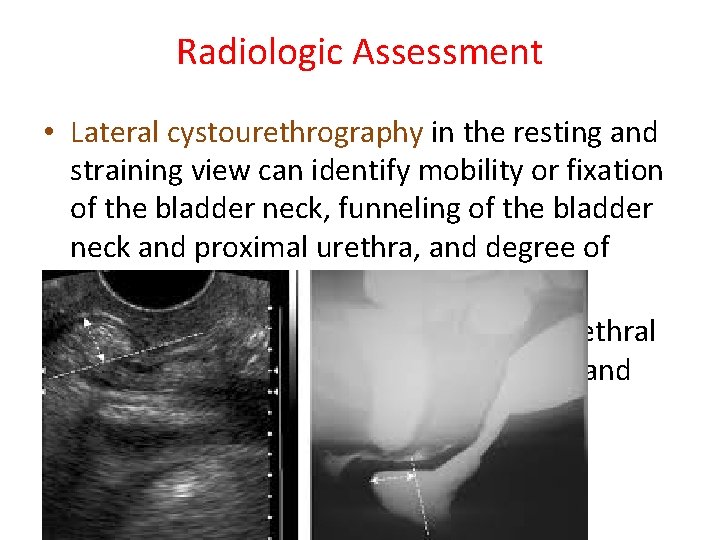
Radiologic Assessment • Lateral cystourethrography in the resting and straining view can identify mobility or fixation of the bladder neck, funneling of the bladder neck and proximal urethra, and degree of cystocele. • The voiding component can identify urethral diverticulum, fistula, mass, obstruction and vesicoureteral reflux.
Intrinsic sphincteric deficiency (ISD) • results from a loss of urethral tone that normally keeps the urethra closed. • This can occur in the presence or absence of urethral hypermobility and typically results in severe urinary leakage even with minimal increases in abdominal pressure. • ISD results from neuromuscular damage and can be seen in women who have had multiple pelvic or incontinence surgeries. • It is challenging to treat women with ISD, and they have worse surgical outcomes
Perineal Pad Tests • Test one hour is started without the patient voiding and with drinking approximately 500 m. L of fluid. • A period of walking, coughing, exercise, and hand -washing is done. • At the end of the 1 -h test, the collecting device is removed and weighed. • A pad wright gain of 1 gr or more is considered positive for a 1 hour test and a pad weight gain greater than 4 gr is positive for a 24 hour test.
Perineal Pad Tests • It has low sensitivity • poor correlation between pad test and videographic assessment of incontinence severity. • limited acceptance of pad tests as a routine part of the evaluation of incontinence.
Postvoid residual volume • (PVR) to exclude • overflow incontinence or voiding dysfunction. assessed by either direct catheterization or ultrasonography. • ultrasonography measurements of PVR have a standard error of 15% to 20%.
Postvoid residual volume • To measure the PVR, the patient is asked to start with a full bladder and void as she normally would (without additional effort to fully empty the bladder). perform this test within 10 minutes of a void • to avoid an artificially elevated result because of diuresis. • women should be able to void at least 80% of the total bladder volume
Postvoid residual volume • a PVR <50 m. L is considered adequate emptying • PVR >200 m. L is considered inadequate and suggestive of either detrusor weakness or bladder outlet obstruction. • The range of normal values for PVR remains controversial • . Because many women are unable to void well during an anxiety ridden first visit • it is helpful to recheck the PVR volume at a future visit before embarking on further diagnostic tests.
Indications for obtaining a PVR specific neurologic disease diabetes mellitus with peripheral neuropathy recurrent UTI bladder outlet obstruction severe constipation significant POP new onset or recurrent incontinence after surgery for incontinence • medications that suppress detrusor contractility or increase sphincter tone • •
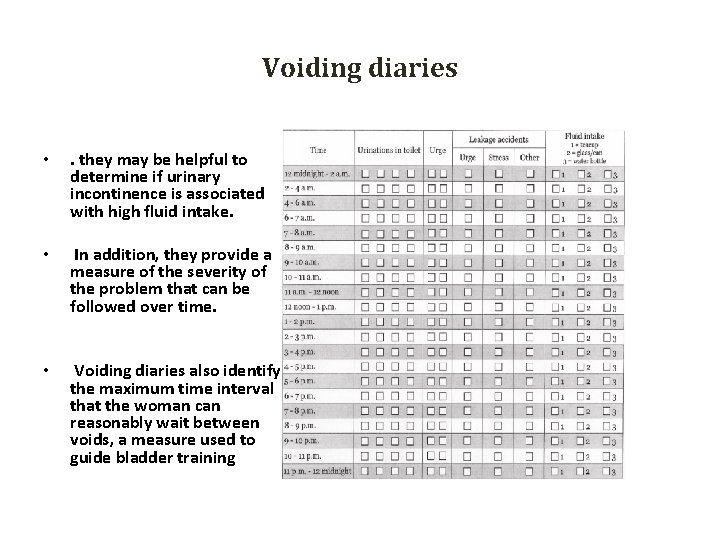
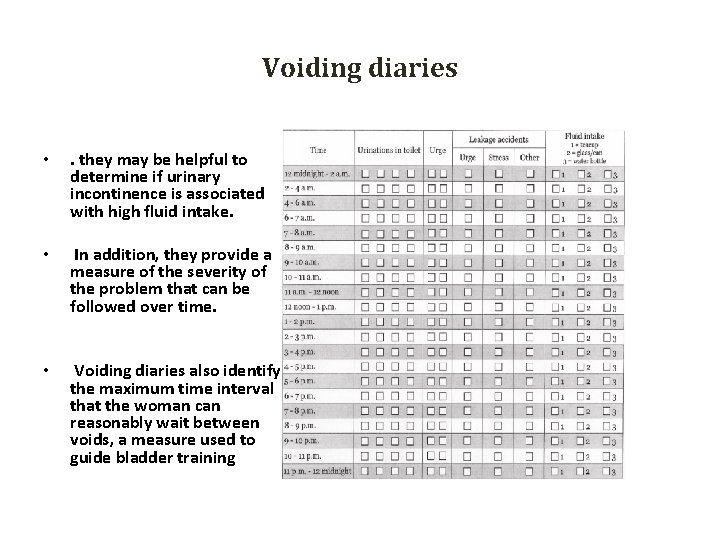
Voiding diaries • . they may be helpful to determine if urinary incontinence is associated with high fluid intake. • In addition, they provide a measure of the severity of the problem that can be followed over time. • Voiding diaries also identify the maximum time interval that the woman can reasonably wait between voids, a measure used to guide bladder training
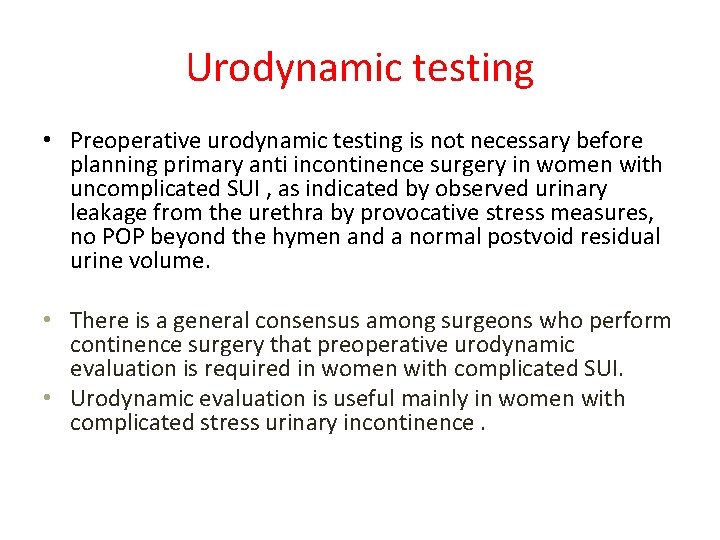
Urodynamic testing • UDS is indicated when the information and diagnosis provided will guide patient treatment. • when invasive therapy is planned. • symptoms are not consistent with physical examination findings or in women with complicated incontinence scenarios.
Urodynamic testing • Urodynamic evaluation is not necessary for many women with uncomplicated stress urinary incontinence (pure SUI). • Urodynamic evaluation is not required to confirm the diagnosis of SUI in women with typical SUI symptoms and physical examination findings (positive stress urinary test).
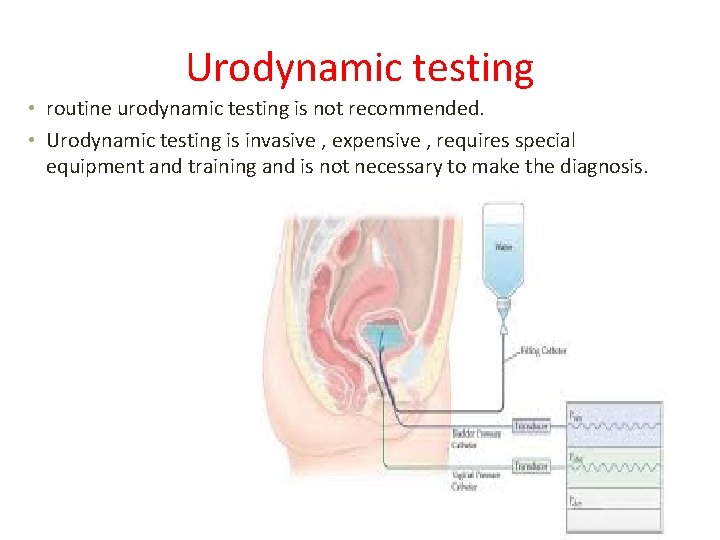
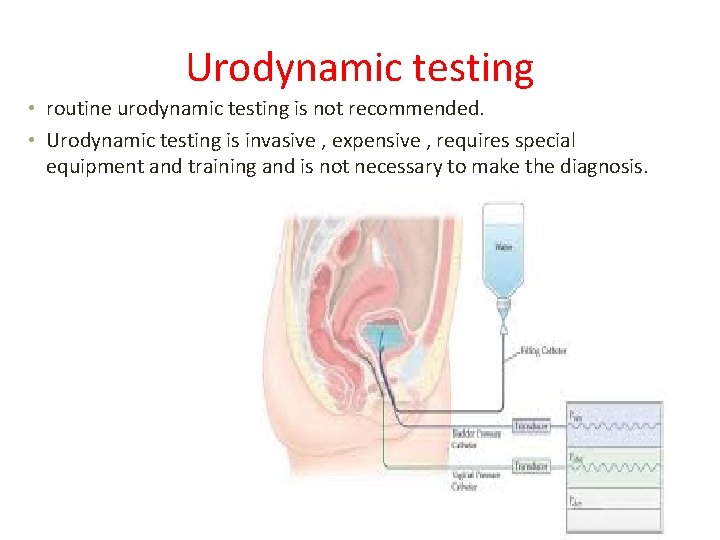
Urodynamic testing • routine urodynamic testing is not recommended. • Urodynamic testing is invasive , expensive , requires special equipment and training and is not necessary to make the diagnosis.
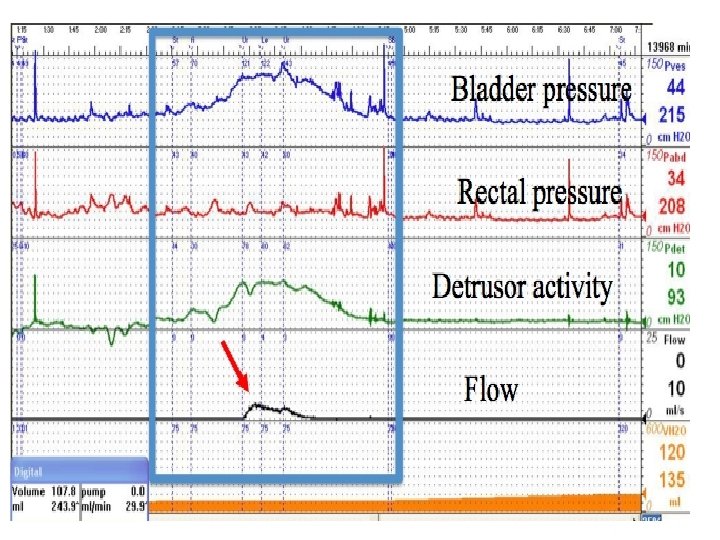
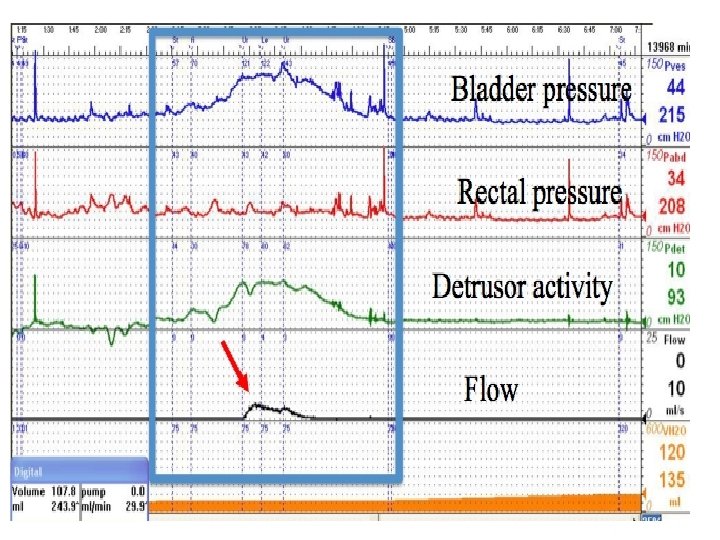
Some specific types of urodynamic testing are: ●Cystometry (or cystometrogram); evaluates bladder function by measuring pressure and volume of fluid in the bladder during filling, storage, and voiding. ●Uroflowmetry ; measures the rate of urine flow. ●upp; tests urethral function. ●Leak point pressure ; determines the bladder or abdominal pressure when leakage occurs due to increased abdominal pressure (Valsalva or cough) to assess urethral resistance.
Interpretation of Results: “ 3 C’s” and “ 2 S’s” Capacity Compliance Competence Sensations Stability
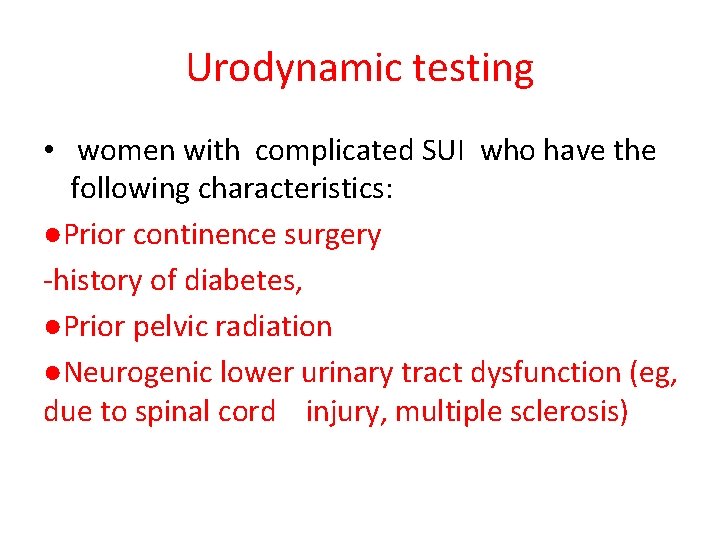
Urodynamic testing • Preoperative urodynamic testing is not necessary before planning primary anti incontinence surgery in women with uncomplicated SUI , as indicated by observed urinary leakage from the urethra by provocative stress measures, no POP beyond the hymen and a normal postvoid residual urine volume. • There is a general consensus among surgeons who perform continence surgery that preoperative urodynamic evaluation is required in women with complicated SUI. • Urodynamic evaluation is useful mainly in women with complicated stress urinary incontinence.
Urodynamic testing • women with complicated SUI who have the following characteristics: ●Prior continence surgery -history of diabetes, ●Prior pelvic radiation ●Neurogenic lower urinary tract dysfunction (eg, due to spinal cord injury, multiple sclerosis)
Suspicion of a non-stress etiology of urinary incontinence, ●suggested by the following components of the office evaluation: • Leakage of urine without exertion, particularly while standing • Nocturia (≥ 2 episodes per night) • Persistently elevated postvoid residual volume (PVR) (≥ 50 m. L) • Urinary stress test with leakage that is delayed, copious, and difficult to stop
Urodynamic testing • Women with these findings may have overflow incontinence, intrinsic sphincter deficiency, or other systemic or local causes of incontinence (eg, urethral diverticulum, issues with mobility). • Women with delayed leakage on the urinary stress test may have detrusor overactivity incontinence. • Urge incontinence seldom requires urodynamic testing except in cases where the patient does not respond to conservative management.
Urodynamic testing • Mixed urinary incontinence (coexistent stress and urgency incontinence) is common, and is not considered complicated SUI. • Urodynamic evaluation is useful mainly in women with mixed incontinence. • However, prior to surgery, women with urgepredominant mixed incontinence should undergo a trial of treatment with medical therapy for urge symptoms to assess whether this reduces the number of incontinence episodes.
Laboratory Tests • A urinalysis should be performed in all patients with catheterization or a clean midstream urine. • Examination of the urine by dipstick and microscopy is done to exclude infection, hematuria and metabolic abnormalities. • Hematuria cannot be diagnosed on the results of a dipstick test alone and confirmation by microscopic evaluation is mandatory. • Occasionally , a simple urinary tract infection causes the onset or exacerbation of urinary incontinence.
Laboratory Tests • Urine culture should be obtained when the dipstick test indicates infection. • Acute cystitis can present with multiple irritative symptoms, such as dysuria, frequency, urgency, incontinence, and voiding difficulty. In these cases, treatment of the infection usually eradicates the symptoms.
Laboratory Tests • Some women, particularly older ones, have asymptomatic bacteriuria that truly is asymptomatic, thus , if attempted treatment of a woman with bacteriuria but without classic urinary tract infection symptoms (such as dysuria, urgency, or frequency)does not improve incontinence, further antibacterial treatment is generally unnecessary.
Urine cytology • is not recommended in the routine evaluation of the incontinent • if there is pelvic pain, • persistent hematuria without infection • risk factors for bladder cancer • (eg, , current or past tobacco use, chemical exposures, previous bladder tumor).
Laboratory Tests • Routine testing of renal function is not recommended in urinary incontinence. • If there is a concern about urinary retention, we measure serum creatinine as part of the initial evaluation.
Radiographic imaging • In general, radiographic imaging is not necessary for the initial evaluation of urinary • Imaging with CT or MRI should be obtained, if there are findings on history or an abnormal neurologic examination that suggests disc herniation manifesting as urinary incontinence. • conditions (eg, Parkinson disease) presenting with new onset or worsening incontinence may also warrant diagnostic imaging.
• In general, cystoscopy is indicated for patients with persistent • irritative voiding symptoms, • hematuria, • postoperative incontinence, • voiding dysfunction • suspicion of a urethral diverticulum • fistula. Obvious causes of bladder overactivity, such as cystitis, stone disease, and tumor, can be easily diagnosed
THE END