Urinary Incontinence Evaluation and Nonsurgical Treatment WVU WOMENS
- Slides: 59
Urinary Incontinence: Evaluation and Nonsurgical Treatment WVU WOMENS HEALTH CURRICULUM Stanley Zaslau, MD, MBA, FACS Program Director & Associate Professor Division of Urology West Virginia University
Introduction and Terminology • Urinary incontinence: involuntary urine loss • 2 causes: urethral and extraurethral
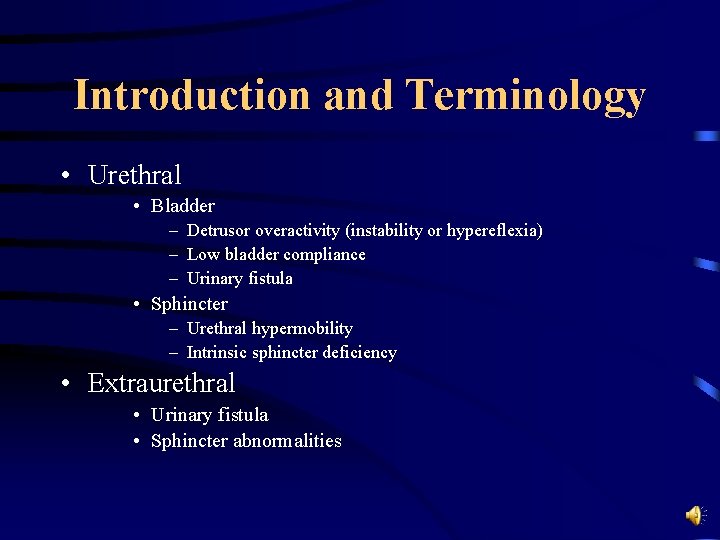
Introduction and Terminology • Urethral • Bladder – Detrusor overactivity (instability or hypereflexia) – Low bladder compliance – Urinary fistula • Sphincter – Urethral hypermobility – Intrinsic sphincter deficiency • Extraurethral • Urinary fistula • Sphincter abnormalities
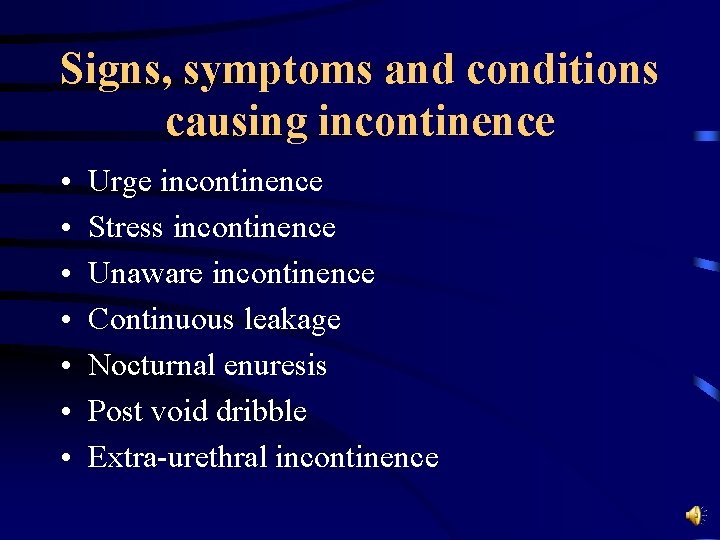
Signs, symptoms and conditions causing incontinence • • Urge incontinence Stress incontinence Unaware incontinence Continuous leakage Nocturnal enuresis Post void dribble Extra-urethral incontinence
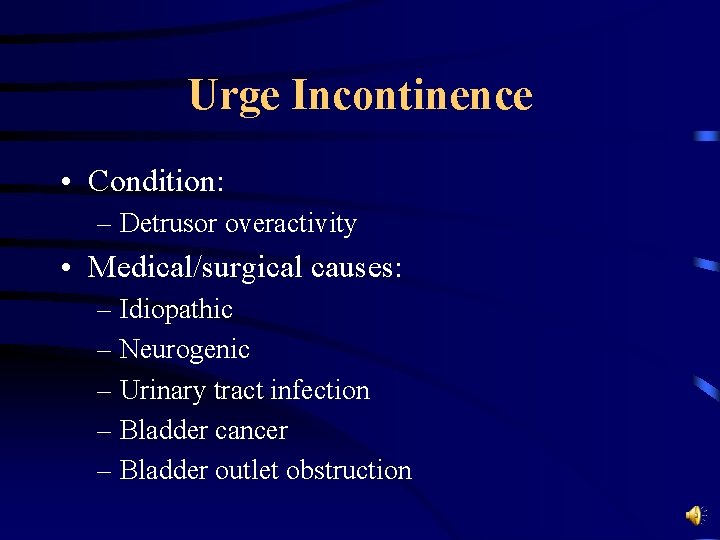
Urge Incontinence • Condition: – Detrusor overactivity • Medical/surgical causes: – Idiopathic – Neurogenic – Urinary tract infection – Bladder cancer – Bladder outlet obstruction
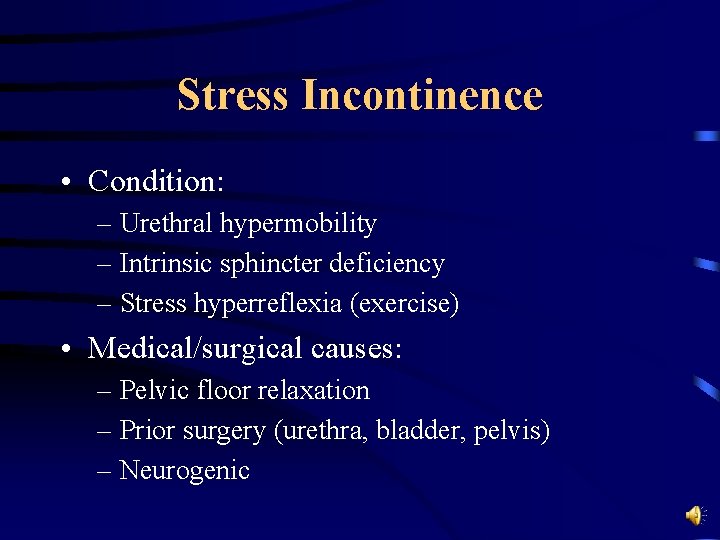
Stress Incontinence • Condition: – Urethral hypermobility – Intrinsic sphincter deficiency – Stress hyperreflexia (exercise) • Medical/surgical causes: – Pelvic floor relaxation – Prior surgery (urethra, bladder, pelvis) – Neurogenic
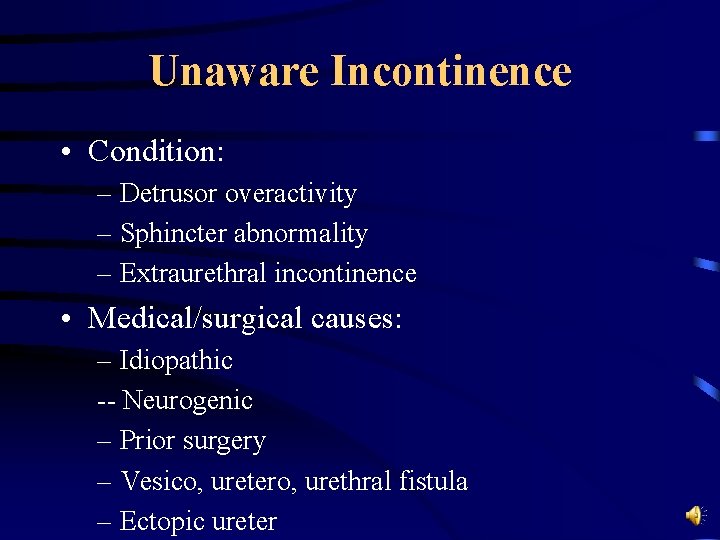
Unaware Incontinence • Condition: – Detrusor overactivity – Sphincter abnormality – Extraurethral incontinence • Medical/surgical causes: – Idiopathic -- Neurogenic – Prior surgery – Vesico, uretero, urethral fistula – Ectopic ureter
Continuous Leakage • Condition: – Sphincter abnormality – Impaired detrusor contractility – Extraurethral incontinence • Medical/surgical causes: – Neurogenic – Prior urethral, bladder or pelvic surgery – Ectopic ureter or urinary/vaginal fistula
Nocturnal Enuresis • Condition: – Sphincter abnormality – Detrusor overactivity • Medical/surgical cause: – Idiopathic – Neurogenic – Outlet obstruction
Post-Void Dribble • Condition: – Post-sphincteric collection of urine • Medical/surgical causes: – Idiopathic – Urethral diverticulum
Extra-Urethral Incontinence • Condition: – Vesico, uretero or urethrovaginal fistula – Ectopic ureter • Medical/surgical cause: – Trauma -- Surgical – Obstetrical – Congenital – Other
Diagnostic Evaluation • • History of present illness Past medical history Physical examination Laboratory urodynamic evaluation
History of Present Illness • Patient’s symptoms – Frequency, urgency, dysuria, incontinence-type – Incontinence with stress vs. urge – Difficulty with initiating stream? • Symptom severity – Wears pads? -- do they become saturated? – How often change pads?
Past Medical History • Neurologic conditions: – Multiple sclerosis – Spinal cord injury – Parkinson’s disease • Surgical history – Prostate, vaginal surgery, prior repair for SUI? – APR, radical hysterectomy
Past Medical History • Radiation therapy? • Medications – Sympathomimetics – Tricyclic antidepressants – Parasympatheticomimetics
Physical Examination • Why? – Demonstrate incontinence – Detect prolapse and other pelvic conditions • interstitial cystitis – Detect prostate conditions in men – Detect neurologic abnormalities
Physical Examination • Key points – Observe gait – Examine abdomen/flanks for masses – Rectal examination (sphincter tone) – Perineal sensation – Bulbocavernosal reflex • absence in 30% of normal women
Physical Examination • Women: – Vaginal examination with empty and full bladder – Assess urethral hypermobility (Q tip test) – Assess prolapse (cystocele, rectocele or enterocele) • “transverse groove” separates enterocele from rectocele – Assess vaginal mucosa – Assess incontinence (lithotomy vs. standing)
Urodynamic Evaluation • Why? – Determine etiology of incontinence – Evaluate detrusor function – Determine degree of pelvic floor prolapse
Urodynamic Evaluation • Why? – Indentify risk factors for upper tract deterioration • • detrusor external sphincter dyssynergia low compliance bladder outlet obstruction vesicoureteral reflux
Urodynamic Evaluation • When? – When simpler tests are inconclusive – When patient complains of incontinence and it can’t be demonstrated clinically – History of prior incontinence surgery – History of APR or radical hysterectomy – History of known neurologic disorder
Urodynamic Evaluation • Questions to ask before you start? – What symptoms do you want to reproduce? – What is the functional bladder capacity? – Does the patient empty their bladder? – Is urinary incontinence a complaint? – Is there a neurologic lesion that can cause DESD, hyperreflexia or areflexia?
Cystometry • Graphic representation of intravesical pressure as a function of bladder volume • Detrusor activity: – overactive – underactive – normal activity
Nonsurgical Treatment: Overview • Nonsurgical treatment of lower urinary tract dysfunction – Behavioral interventions (Bladder training, habit training, timed voiding, prompted voiding) – Biofeedback therapy – Pelvic floor rehabilitation – Principles of pharmacologic therapy
Behavioral Interventions for Urinary Incontinence • • Bladder training Habit training Timed voiding Prompted voiding
Bladder Training • Three primary components – Education • physiology & pathophysiology of incontinence – Scheduled voiding • gradual increase in time between voids • distraction/relaxation techniques – Positive reinforcement • praise: if increase time between voids
Bladder retraining • Systematic delay in voiding through use of urge suppression • Patient must be able to identify urge, understand how to inhibit the urge and be motivated to do so! • Care can be independent or dependent on caregivers
Bladder retraining • Urge is suppressed using a pelvic muscle exercise (Kegel) • Time between voids is gradually increased in 15 minute increments, up to goal time of two to three hours between voids
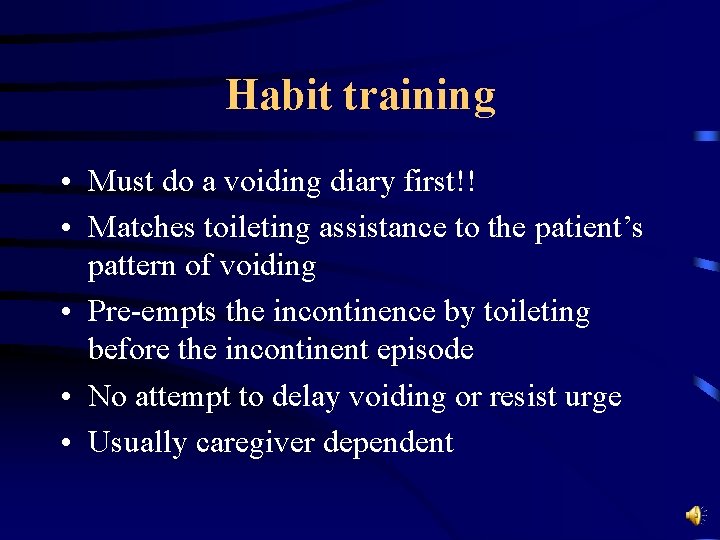
Habit training • Must do a voiding diary first!! • Matches toileting assistance to the patient’s pattern of voiding • Pre-empts the incontinence by toileting before the incontinent episode • No attempt to delay voiding or resist urge • Usually caregiver dependent
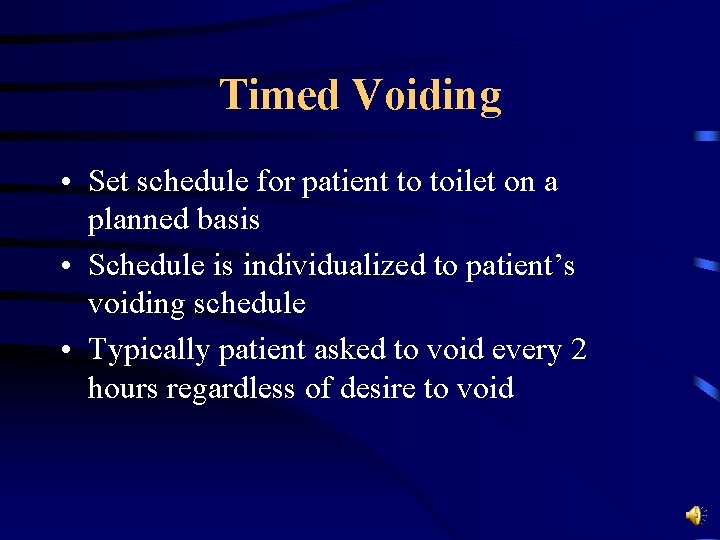
Timed Voiding • Set schedule for patient to toilet on a planned basis • Schedule is individualized to patient’s voiding schedule • Typically patient asked to void every 2 hours regardless of desire to void
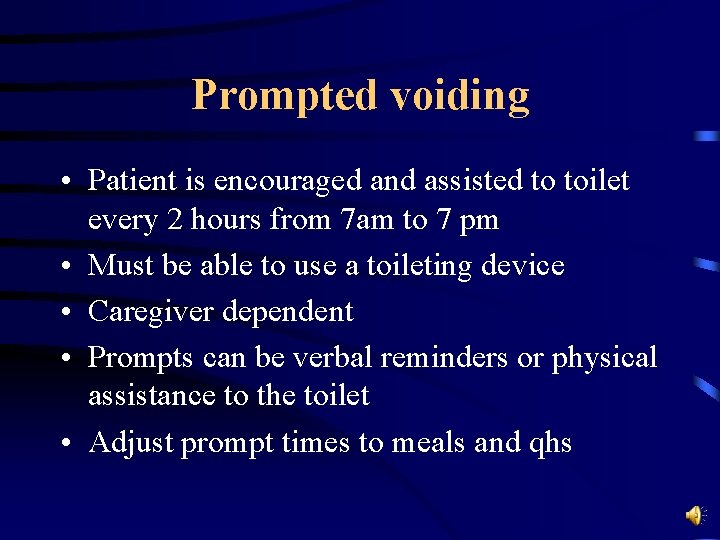
Prompted voiding • Patient is encouraged and assisted to toilet every 2 hours from 7 am to 7 pm • Must be able to use a toileting device • Caregiver dependent • Prompts can be verbal reminders or physical assistance to the toilet • Adjust prompt times to meals and qhs
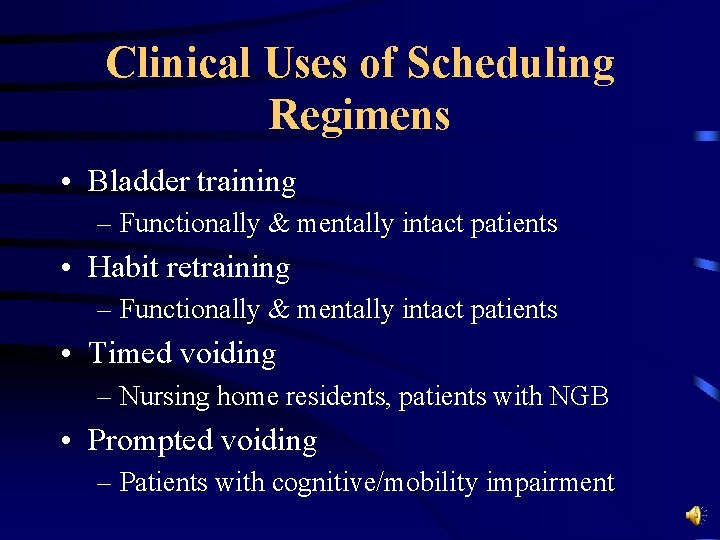
Clinical Uses of Scheduling Regimens • Bladder training – Functionally & mentally intact patients • Habit retraining – Functionally & mentally intact patients • Timed voiding – Nursing home residents, patients with NGB • Prompted voiding – Patients with cognitive/mobility impairment
Conclusions about Behavioral Therapy • • • Can treat urinary incontinence (UI> SUI) Can treat sensory urgency Inexpensive Has no side effects Can be done in inpatient or outpatient setting No special equipment required
Biofeedback • Originated in laboratory research 25 years ago • Applied to urinary bladder • ? Mechanism of action: reflex inhibition? • Programs: voluntary contraction of pelvic muscles (pubococcygeous & levator) • Goal: modify visceral control (bladder)
Biofeedback • Relates to anatomy of pelvic muscles – identify pubococcygeous muscle – identify muscles of external and urethral sphincter • all muscles innervated by S 2 via pudendal nerve – voluntary contraction of EUS can interrupt incontinence during an episode of urgency and relax detrusor
Biofeedback • • • Bladder Filling Signal Source Equipment Patient Selection Results
Results for Biofeedback • Conclusions – Effective to reduce episodes of urge incontinence – Less is known about: • Frequency: hallmark of bladder training • Urgency: difficult to measure • Nocturia: multi-factorial condition Borgio, JAGS 2000
Electrostimulation • Transvaginal or transanal • Effects: – cause passive contraction of pelvic floor musculature • Potential uses: – “Re-educate” weak muscles to contract – Relieve symptoms of urge incontinence/pelvic pain
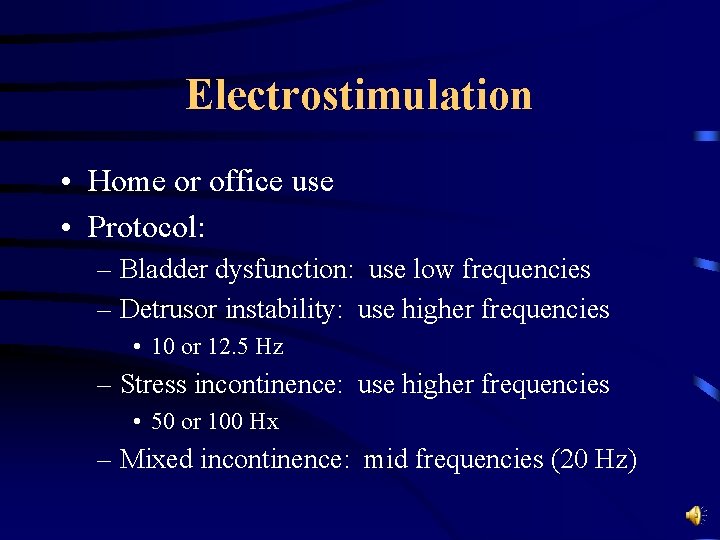
Electrostimulation • Home or office use • Protocol: – Bladder dysfunction: use low frequencies – Detrusor instability: use higher frequencies • 10 or 12. 5 Hz – Stress incontinence: use higher frequencies • 50 or 100 Hx – Mixed incontinence: mid frequencies (20 Hz)
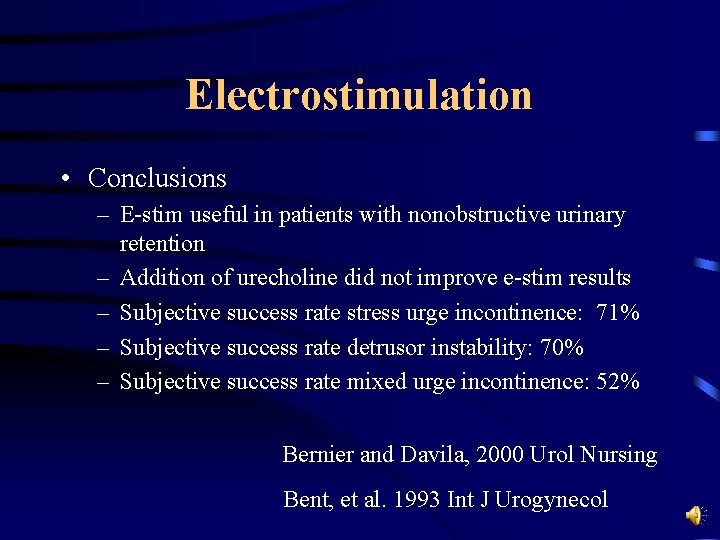
Electrostimulation • Conclusions – E-stim useful in patients with nonobstructive urinary retention – Addition of urecholine did not improve e-stim results – Subjective success rate stress urge incontinence: 71% – Subjective success rate detrusor instability: 70% – Subjective success rate mixed urge incontinence: 52% Bernier and Davila, 2000 Urol Nursing Bent, et al. 1993 Int J Urogynecol
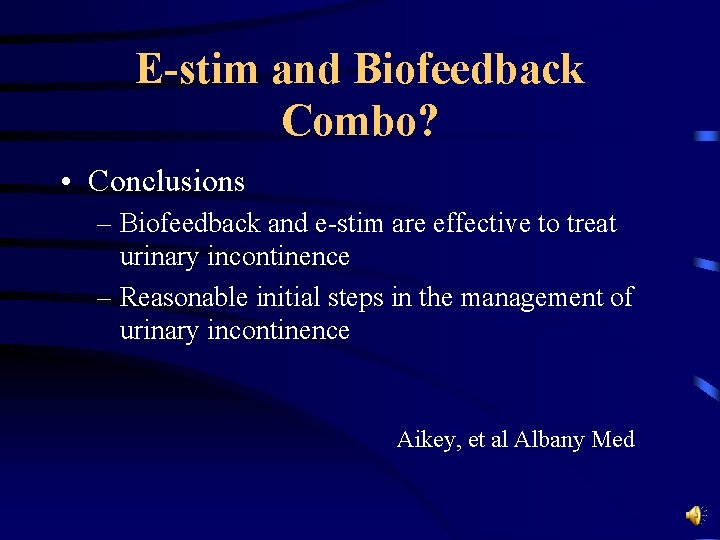
E-stim and Biofeedback Combo? • Conclusions – Biofeedback and e-stim are effective to treat urinary incontinence – Reasonable initial steps in the management of urinary incontinence Aikey, et al Albany Med
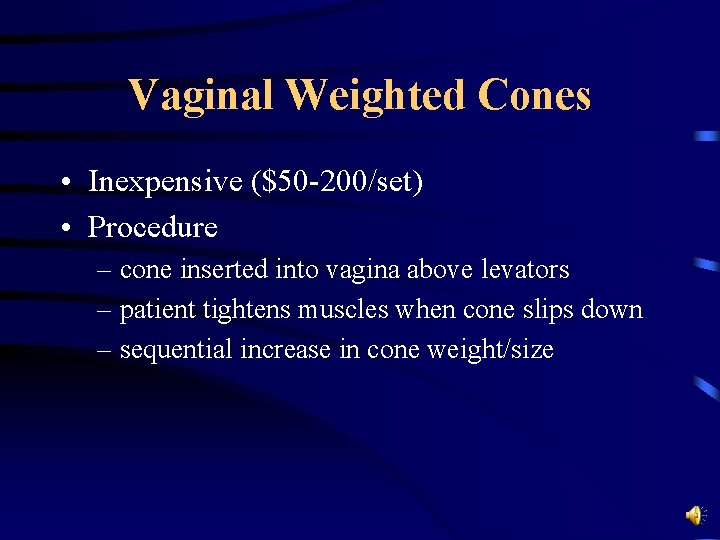
Vaginal Weighted Cones • Inexpensive ($50 -200/set) • Procedure – cone inserted into vagina above levators – patient tightens muscles when cone slips down – sequential increase in cone weight/size
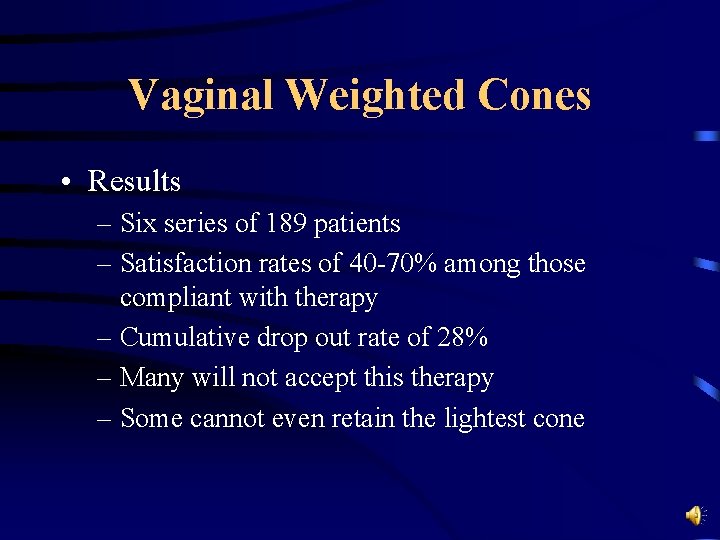
Vaginal Weighted Cones • Results – Six series of 189 patients – Satisfaction rates of 40 -70% among those compliant with therapy – Cumulative drop out rate of 28% – Many will not accept this therapy – Some cannot even retain the lightest cone
Summary of Techniques • Review of 22 trials: – Pelvic floor muscle exercises treat SUI – Biofeedback + PFM no better than PFM alone – No difference between e-stim and otherapies – Weak evidence to suggest bladder retaining is no more effective than drug therapy
Medical Therapy • Medications for Stress Incontinence – Alpha adrenergics – Estrogens • Medications for Urge Incontinence – Tolterodine – Oxybutynin XL – Oxybutynin Transdermal
Medical Therapy- Alpha Agonists • Phenylpropanolamine(PPA) – best studied alpha agonist – taken off market -- hemorrhagic strokes in young women – 5/8 studies with PPA demonstrated improvement in SUI by 19 - 60% vs. placebo – However, pseudoephedrine is available with similar efficacy
Medical Therapy - Alpha Agonists • Estrogens – controversial – receptors in urethra, vagina --> tissue atrophy with menopause? – Metaanalysis of 8 trials “superior to control” – Contrary -- Grady, et al 2000 -- “worsening of incontinence vs. controls at 4 years) • problem -- in study only 26% had SUI
Medical Therapy – Overactive Bladder (OAB) • Oral oxybutynin – proven muscarinic activity of active agent – efficacy similar with XL form – benefit of XL for side effects – dosing magnitude higher • improved tolerability
Medical Therapy - OAB • Oral oxybutynin – compliance benefit with once daily dosing – steady state pharmacokinetics • modulated serum peaks • less variance below threshold levels – lower discontinuance rates
Medical Therapy - OAB • Tolterodine tartrate – active anti-muscarinic compound – binding selectivity for bladder – improved xerostomia – generally well tolerated – extended release formulation -- good for xerostomia – ER form works as well as IR form
Medical Therapy - OAB • Transdermal oxybutynin – altered metabolism of parent • avoidance of proximal gut CYP 450 – equal efficacy to IR formulation – substantially less systemic side effects – compliance benefit • twice weekly application
Medical Therapy - OAB • OPERA Trial (Diokno et al), Mayo Clin Proc – Tol ER vs. Oxy ER – 12 week double-blind study – 790 women enrolled – Primary outcomes • urge incontinence • total incontinence • urinary frequency
Medical Therapy - OAB • OPERA – Similar effect between active arms • significant reduction for all outcomes – Statistical difference • urinary frequency (28% vs. 25%) • total continence (23% vs. 17%) – Adverse events • total dry mouth greater for OXY ER • discontinuation rates same
Medical Therapy - OAB • ACET, Sussman, et al 2002 – Open label direct comparison • OXY ER 5/10 • TOL ER 2/4 – 8 week analysis – 1289 patients – TOL ER 4 mg superior to all others (70% vs 60%) – Significantly less dry mouth with TOL ER – Discontinuation rates • 6% TOL ER vs. 13% OXY ER
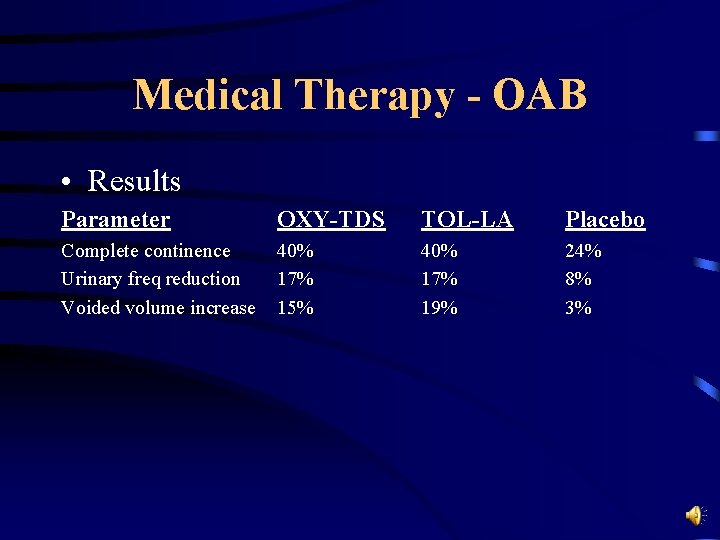
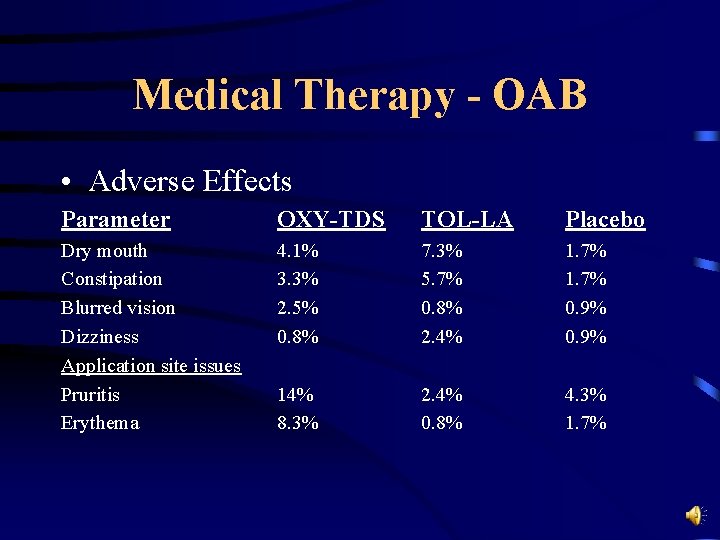
Medical Therapy - OAB • OXY-TDS vs. TOL-LA vs. Placebo • (Domchowski, et al Urol 2003) – compare efficacy and safety of OXY-TDS vs. TOL LA vs. placebo – Multi-center, double blind, randomized trial for 12 weeks & then 52 week open label – 361 patients randomized • OXY-TDS 3. 9 mg/d or TOL LA 4 mg/d
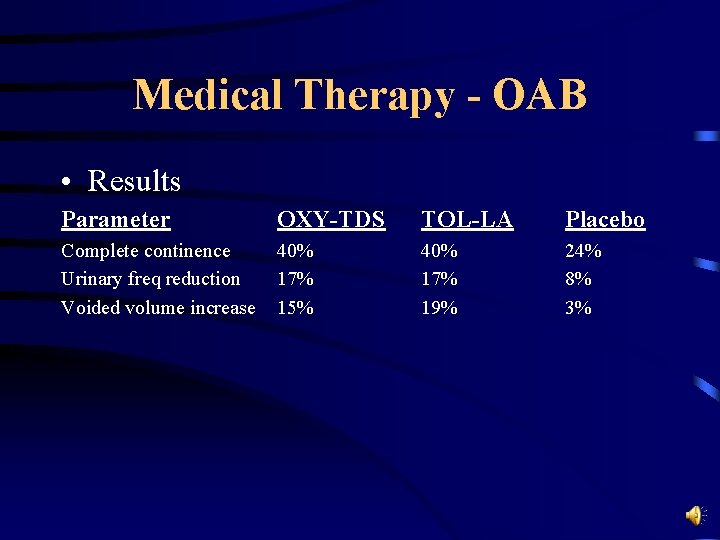
Medical Therapy - OAB • Results Parameter OXY-TDS TOL-LA Placebo Complete continence Urinary freq reduction Voided volume increase 40% 17% 15% 40% 17% 19% 24% 8% 3%
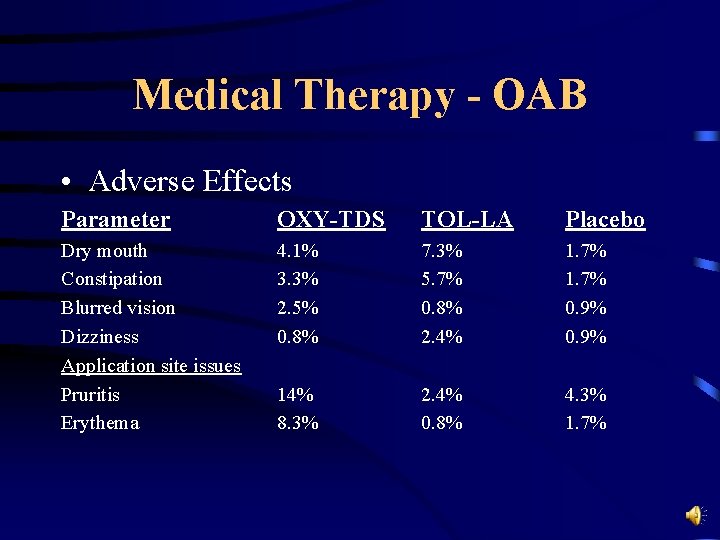
Medical Therapy - OAB • Adverse Effects Parameter OXY-TDS TOL-LA Placebo Dry mouth Constipation Blurred vision Dizziness Application site issues Pruritis Erythema 4. 1% 3. 3% 2. 5% 0. 8% 7. 3% 5. 7% 0. 8% 2. 4% 1. 7% 0. 9% 14% 8. 3% 2. 4% 0. 8% 4. 3% 1. 7%
Parting Thoughts • Improvement is attainable in the majority of patients – with combined behavioral therapies? • The ideal agent/non pharmacologic therapy is not yet available • Distinguishing criteria and outcomes – difficult to separate absolute results
References • • Aikey, et al, Albany Med. Bent et al. , Int J Urogynecol 1993. Bernier F and Davila GW, Urol Nurs 2000: 261 -4. Borgio KL, Locher JL, Goode PS. J Am Geriatr Soc 2000: 370 -4. Diokno AC et al, Mayo Clin Proc 2003 Jun; 78(6): 687 -95. Dmochowski RR, et al, Urology 2003 Aug; 62(2): 237 -42. Grady, et al, 2000. Sussman D, Garely A. Curr Med Res Opin. 2002; 18(4): 177 -84.
 Coital incontinence
Coital incontinence Acfi 12 questions
Acfi 12 questions Acupuncture for incontinence
Acupuncture for incontinence Sacral reflex
Sacral reflex Difference between mens and womens soccer
Difference between mens and womens soccer Womens ministry activities
Womens ministry activities Womens rights
Womens rights Late night womens hour
Late night womens hour Claire paine
Claire paine Womens right
Womens right Womens college kumbakonam
Womens college kumbakonam Womens college kumbakonam
Womens college kumbakonam Womens right
Womens right Womens shelter edmonton
Womens shelter edmonton Women's rights
Women's rights The female anatomy
The female anatomy Womens history month door
Womens history month door Womens community shelters
Womens community shelters Ballybeen womens centre
Ballybeen womens centre Harijah sivakumar
Harijah sivakumar Girls lacrosse helmets
Girls lacrosse helmets Bristol womens voice
Bristol womens voice Fundus of bladder
Fundus of bladder Lesson 14.2 male and female urinary structures
Lesson 14.2 male and female urinary structures Red and white blood cells difference
Red and white blood cells difference Chapter 47 urinary and reproductive disorders
Chapter 47 urinary and reproductive disorders Wvu risk management
Wvu risk management Vicki sealey wvu
Vicki sealey wvu Wvu degree works
Wvu degree works Wvu gef list
Wvu gef list Wvu citi training
Wvu citi training Wvu research corp jobs
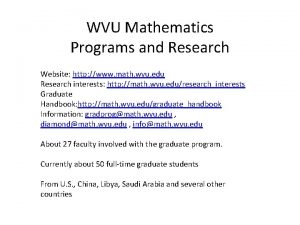
Wvu research corp jobs Math department wvu
Math department wvu Wvu student legal services
Wvu student legal services Accessibility services wvu
Accessibility services wvu Wvu mountaineer hub
Wvu mountaineer hub Cs101wvu
Cs101wvu Wvu department of surgery
Wvu department of surgery John quaranta wvu
John quaranta wvu Wvu oit
Wvu oit Wvu cafee
Wvu cafee Wvu emba
Wvu emba Symplicity wvu law
Symplicity wvu law Chris randall wvu
Chris randall wvu Degreeworks wvu
Degreeworks wvu Stat 211
Stat 211 Wvu oit
Wvu oit Wvu pe classes
Wvu pe classes Physiology of urine formation
Physiology of urine formation Superior surface of urinary bladder
Superior surface of urinary bladder Ureter blood supply
Ureter blood supply Figure 15-3 the urinary system
Figure 15-3 the urinary system Utericle
Utericle Combining form for urinary bladder
Combining form for urinary bladder Urinary system facts
Urinary system facts Fasthugs
Fasthugs Allantoic stalk fetal pig
Allantoic stalk fetal pig Chapter 30 the urinary system
Chapter 30 the urinary system Chapter 22 urinary elimination
Chapter 22 urinary elimination Kidney pyramid labeled
Kidney pyramid labeled