Urinary Incontinence and Retention SelfStudy Urinary Incontinence Involuntary
- Slides: 15
Urinary Incontinence and Retention: Self-Study
Urinary Incontinence • Involuntary leakage of urine • Not a natural consequence of aging
Diagnostic Studies • H&P • Bladder Log or voiding record • Onset, factors that provoke leakage • Pelvic exam (skin for rashes or erosion) • Urinalysis • PVR (postvoid residual; can be done with catheter or ultrasound after voiding)
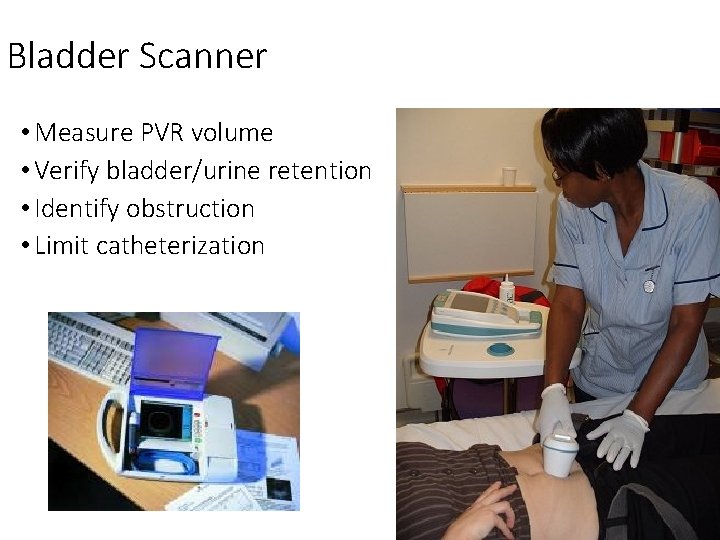
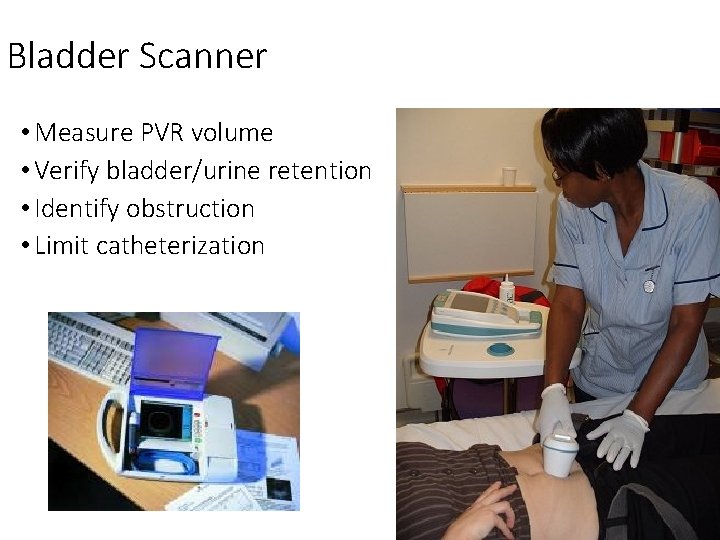
Bladder Scanner • Measure PVR volume • Verify bladder/urine retention • Identify obstruction • Limit catheterization
Interprofessional Care • Depends on the type • Stress incontinence: sudden increase in intraabdominal pressure • Urge incontinence occurs randomly when involuntary urination is preceded by urinary urgency • Overflow incontinence: pressure of urine in overfull bladder overcomes sphincter control • Reflex incontinence: no warning or stress precedes involuntary urination • Incontinence after trauma or surgery • Functional incontinence: from cognitive, functional, or environmental factors • Less invasive treatment first
General Interventions • Pelvic floor muscle training • Weight loss if needed • Bladder retraining • Decrease irritants: coffee, tea, cola drinks, chocolate, alcohol, artificial sweeteners and cigarettes • Catheterization • Modify environment to facilitate regular, easy access to bathroom
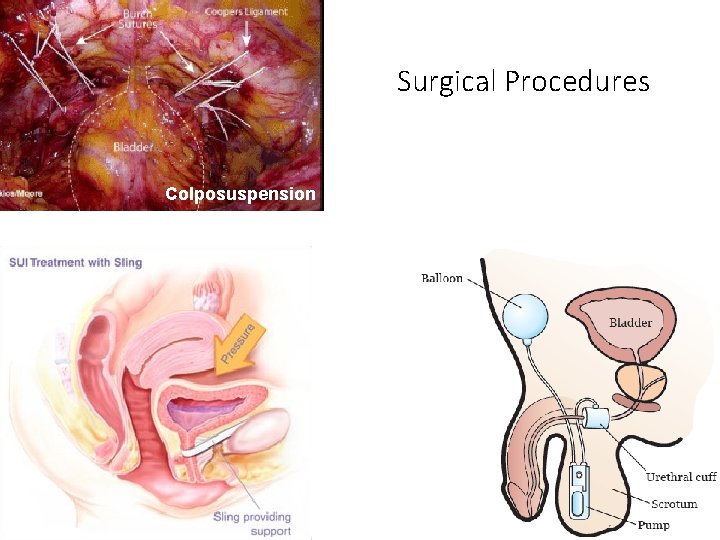
Surgical Therapy for Urinary Incontinence • Surgical technique depends on the type of incontinence • Repositioning/stabilization of the urethra • Retropubic colposuspension and pubovaginal sling • Suburethral sling (can use cadaver or person’s own fascia or synthetic material) • Complications: vascular and bowel injury, mesh or sling erosion, infection, bladder perforation, urinary retention or urgency • Bulking agent injected underneath mucosa of the urethra to correct stress incontinence (avoids the risk of open surgery, reinjection typically required after several years) • Artificial sphincter: silicone inflatable ring • pt has to inflate and deflate
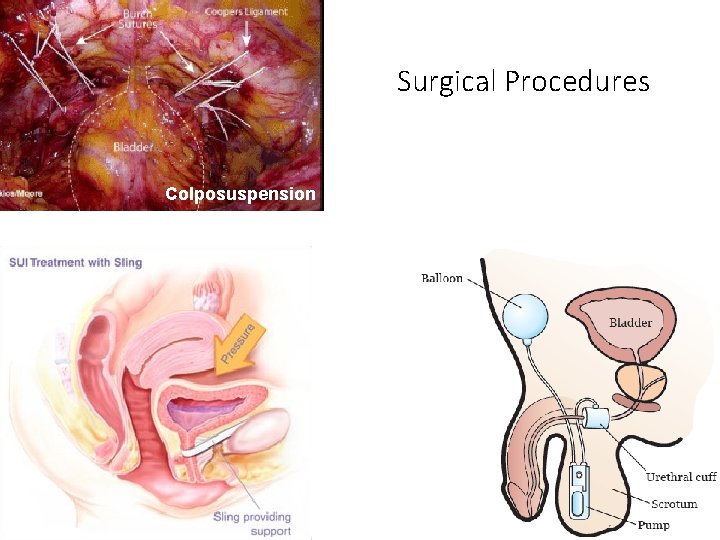
Surgical Procedures Colposuspension
Just FYI, because I bet some of you will want to know… Artificial Urinary Sphincter: How it works To void, the patient must open the artificial sphincter. The patient manually squeezes the control pump that is located in the scrotum or the labia. When the control pump is squeezed, the fluid in the control pump is sent up to the balloon reservoir. The control pump then automatically re-expands; as it re-expands, it pulls the fluid out from the cuff, which causes the sphincter cuff to deflate. The patient repeats this maneuver 3 -4 times until the pump remains flat, which indicates that the cuff is completely empty. At this point, the urine flows freely from the bladder. Urination continues until the bladder is empty. After 3 -5 minutes, the fluid from the balloon reservoir automatically flows through a delayed-fill resistor within the pump and down back to the cuff. When the cuff re-inflates, the urethra becomes effectively closed and the patient becomes dry. (from Medscape)
Interventions for Urinary Incontinence • Containment devices to manage existing leakage • Plan to reduce or resolve factors leading to urinary incontinence Management options (Table 45. 17) • Review this table completely, focusing on lifestyle modifications, scheduled voiding regimens, and pelvic floor rehabilitation
Urinary Retention • Inability to empty the bladder when a person voids OR the accumulation of urine in the bladder because of an inability to void • Acute urinary retention: total inability to pass urine via micturation – medical emergency • Chronic urinary retention: incomplete bladder emptying despite urination • PVR varies widely (normal PVR is 50 -75 m. L) • Over 100 m. L = repeat to verify • Over 200 m. L in older adult on 2 separate occasions = further evaluation (smaller PVR with recurrent UTIs = evaluate)
Urinary Retention • Diagnostic studies same as for urinary incontinence (slide 64) • Interprofessional Care • Behavioral therapies listed for urinary incontinence • Scheduled toileting (q 3 -4 hr)/double voiding (void, wait 3 -4 minutes on toilet, void again) good for chronic retention • Catheterization may be required • Intermittent best • Surgery • Used to treat obstruction(tumor, stricture, pelvic organ prolapse) • In general, minimal role in retention
Nursing Care: Urinary Retention • Avoid intake of large volumes of fluid over a brief period • Smaller amounts throughout the day • Warm body temperature before voiding • Avoid excess alcohol • Drink a cup of coffee or caffeinated tea • Sit in a tub of warm water/take a warm shower • Behavioral therapies (scheduled toiling/double voiding) • Catheterization
Catheterization • Urethral catheterization • Look at indications for indwelling and intermittent catheterization on page 1061 (table 45 -20) • Types of catheters • Urethral catheters (most common; indwelling or intermittent q 3 -5 hr) • Ureteral catheters (already talked about) • Suprapubic catheters (Oldest method of urinary diversion; temporary with bladder/prostate/urethral surgery; can be long -term with some patients) • Nephrostomy tubes (Inserted directly into the pelvis of the kidney – temporary; used when ureter is completely obstructed)
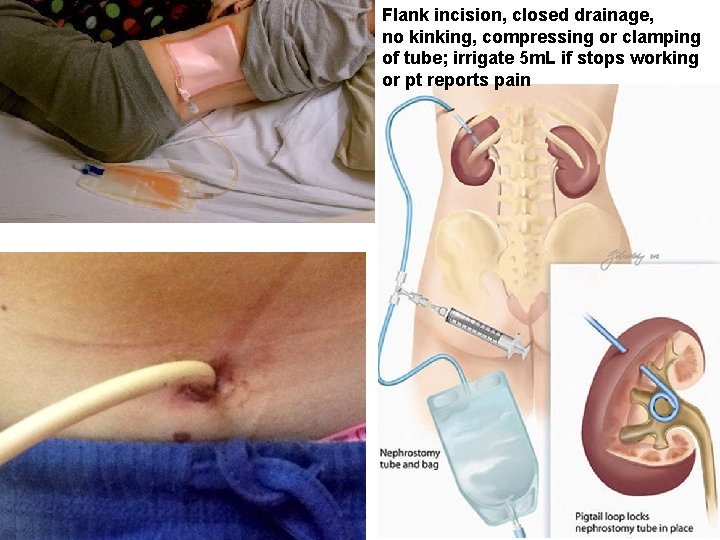
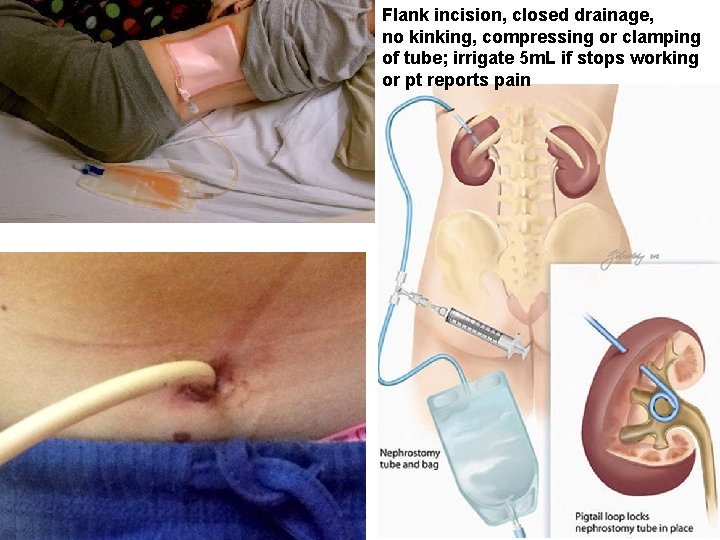
Flank incision, closed drainage, no kinking, compressing or clamping of tube; irrigate 5 m. L if stops working or pt reports pain
 Urinary retention
Urinary retention Purpose of catheterization
Purpose of catheterization Coital incontinence
Coital incontinence Acfi assessment
Acfi assessment Uui definition
Uui definition Sacral reflex
Sacral reflex Loop of henle function
Loop of henle function Motor unit
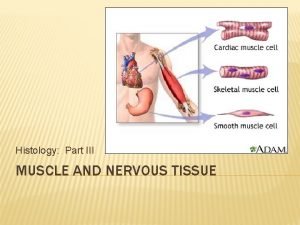
Motor unit Which type of muscle is non-striated and involuntary
Which type of muscle is non-striated and involuntary Voluntary group and involuntary group examples
Voluntary group and involuntary group examples Function of voluntary health organization
Function of voluntary health organization Military medical discharge pay chart
Military medical discharge pay chart Involuntary alienation
Involuntary alienation 4 quadrants of abdomen and organs
4 quadrants of abdomen and organs Voluntary vs involuntary
Voluntary vs involuntary Ascites examination
Ascites examination