Urinary System Disorders Incontinence and Retention Loss of
- Slides: 23
Urinary System Disorders
Incontinence and Retention • Loss of voluntary control of bladder • Stress incontinence – Increase in intra-abdominal pressure • Forces urine through sphincter – Laughing – Coughing – Females weakened • Spinal cord injuries, brain damage • Inability to empty bladder • May accomp overflow incontinence • Spinal cord injury • Inability to control managed by pads, briefs • Catheter – Tube inserted in urethra – Drains urine from bladder to collecting bag – Common source of UTI
Diagnostic Tests—Urinalysis • Constituents, characteristics of urine vary w/ dietary intake, drugs, care of specimen • Normally clear, straw-colored; p. H 4. 5 -8. 0 • Appearance – Cloudy • Presence of lg amts protein, blood cells, bacteria, pus – Dark color • Hematuria (blood), excessive bilirubin, high concentration of urine – Unpleasant, unusual odor • infection
Diagnostic Tests—Urinalysis • Abnormal constituents (high in numbers) – Blood (hematuria) • Small, microscopic amts – Infection, inflammation, tumors of UT • Lg # RBC – Increased glomerular permeability or hemorrhage in tract – Protein (Proteinuria) • Leakage of albumin into filtrate – Inflammation, increased glomerular permeability – Bacteria (Bacteriuria) and Pus (Pyuria) • Indicates UTI – Urinary casts • Microscopic mold of tubules – Consists of one or more cells, bacteria, protein • Inflammation of tubules – Specific gravity • Ability of tubules to concentrate urine • Low is related to renal failure
Diagnostic Tests—Blood Tests • High serum urea and creatinine – Indicate failure to excrete N wastes • Due to low GFR • Metabolic acidosis – Indicates low GFR, failure of tubules to control acid/base balance • Anemia – Indicates low erythropoietin secretion and/or bone marrow depression • Due to accumulating wastes • Electrolytes • Antibody level – Antistreptolysin O (ASO) or antistreptokinase (ASK) • Renin levels – Indicate cause of hypertension
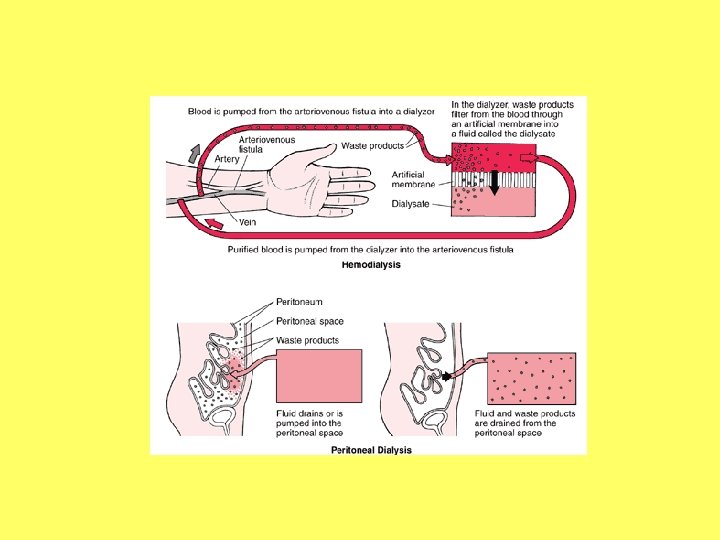
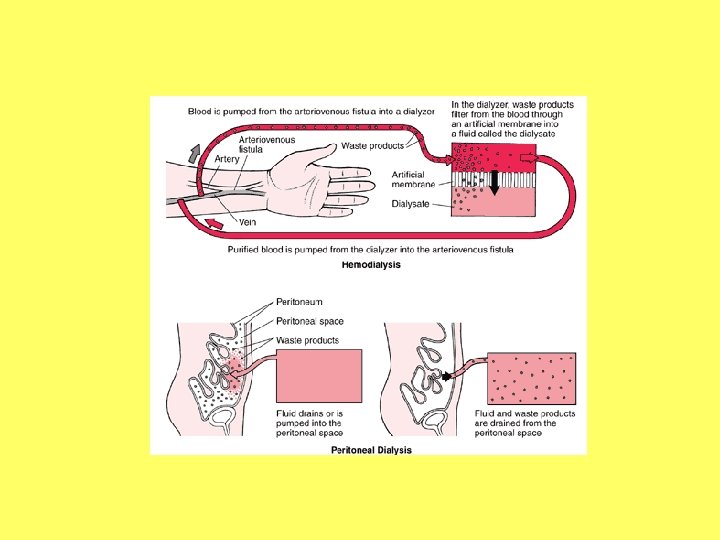
Dialysis • Provides “artificial kidney” – Sustains life after kidney fails • Acute renal failure or end-stage renal failure (those waiting for a transplant) • 2 forms – Hemodialysis – Peritoneal dialysis
Disorders of the Urinary System: Urinary Tract Infections (UTI) • Very common • Urine is excellent medium for microorganismal growth – Escherichia coli • Most are ascending – Perineal cavity mucosa bladder ureters kidneys
UTI—Etiology • Females more anatomically vulnerable – Short urethra – Proximity to anus – Frequent irritation to tissues • Tampons, bubble bath, sexual activity • Older males with prostatic hypertrophy and retention of urine prone to UTI
UTI: Cystitis—Signs and Symptoms • Pain in lower abdomen • Dysuria, frequency, urgency – Inflammation of bladder wall irritated by urine • Systemic signs of infection • Cloudy urine with unusual odor • Urinalysis indicates bacteria (+100, 000/m. L), pyuria, microscopic hematuria
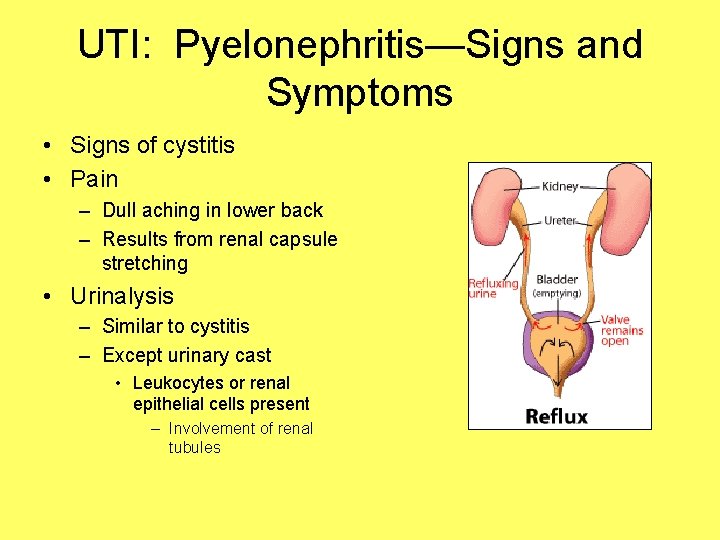
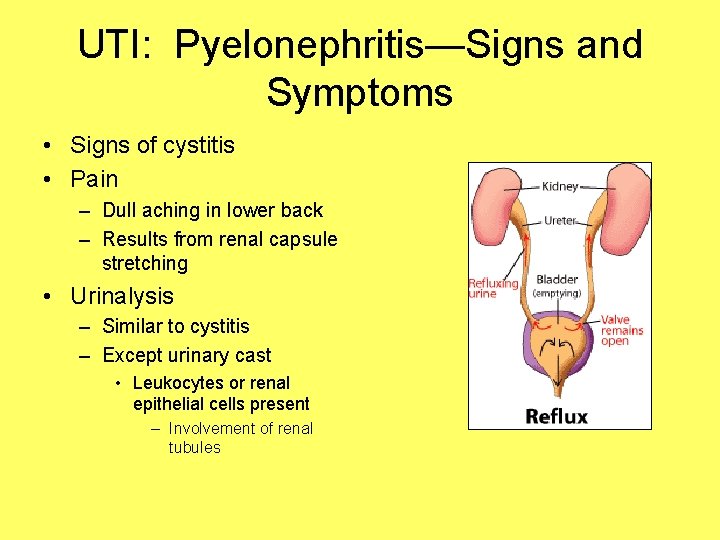
UTI: Pyelonephritis—Signs and Symptoms • Signs of cystitis • Pain – Dull aching in lower back – Results from renal capsule stretching • Urinalysis – Similar to cystitis – Except urinary cast • Leukocytes or renal epithelial cells present – Involvement of renal tubules
UTI—Treatment • Antibiotics (Bactrim) • Increase fluid intake – Especially cranberry juice • Tannin decreases ability of E. coli to adhere to bladder mucosa • Infection reoccurs unless predisposing factors removed
Disorders of the Urinary System: Inflammatory Disorders • Glomerulonephritis – Many forms • Acute Poststreptococcal Glomerulonephritis (APSGN) – Follows streptococcal infection » Originates as upper resp infection, middle ear infection, strep throat – Primarily affects kids 3 -7 (especially boys) – develops 2 weeks after previous infection
Glomerulonephritis—Signs and Symptoms • Back pain – Stretching renal capsule • Dark, cloudy urine • Oliguria • Facial edema, then generalized – Low osmotic pressure of blood – Salt, water retention • Generalized signs of inflammation • Increased bp
Glomerulonephritis—Diagnostic Tests • Blood tests – High serum urea and creatinine and decreasing GFR – Streptococcal antibodies, ASO, ASK – Metabolic acidosis • Low serum bicarbonate, low p. H • Urinalysis – Confirms presence of proteinuria, erythrocyte casts
Glomerulonephritis—Treatment • • Sodium restriction Glucocorticoids Antibiotics Recovery w/ minimal damage – Imp to prevent further exposure to streptococcal infection and recurrent inflam – Adults more difficult • Acute renal failure in 2% • Chronic glomerulonephritis in 10% – Gradually destroys kidneys • Postrecovery testing should be done
Urinary Tract Obstructions: Urolithiasis • Also called: – Calculi – Kidney stones • Frequently reoccur if not treated
Calculi—Pathophysiology • Can develop anywhere in UT; lg or small • Once any solid material or debris forms • Tend to form when: – excessive amts of relatively insoluble salts are in filtrate – Insufficient fluid intake creates highly concentrated filtrate • 75% composed of calcium salts – Remainder: uric acid, struvite, oxalate • Usually cause manifestations only when obstruct flow of urine – Infection if stasis of urine
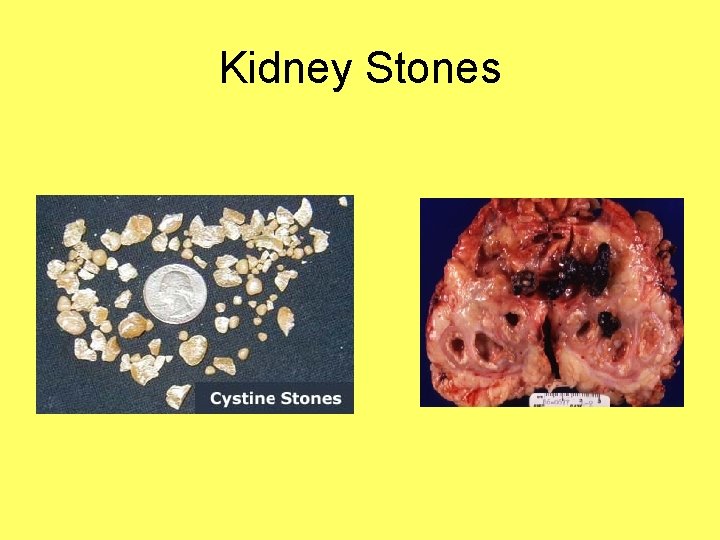
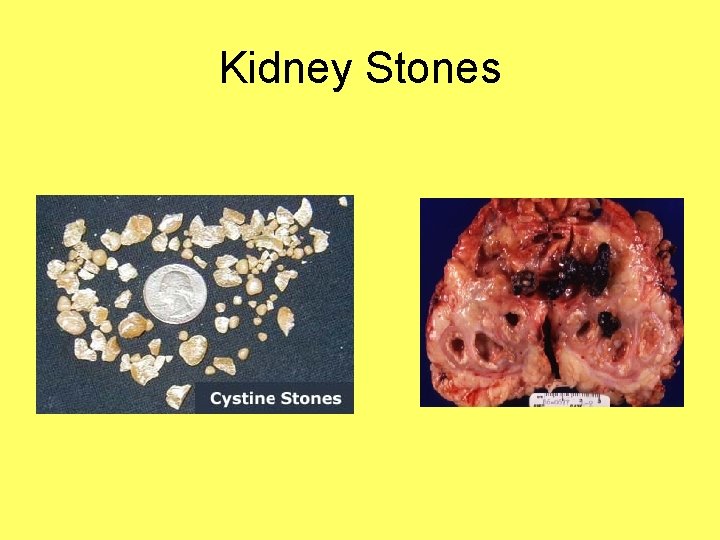
Kidney Stones
Calculi—Signs and Symptoms • Stones in kidney/bladder frequently asymptomatic • Obstruction of ureter causes attack – “renal colic” • Consists of intense spasms in back and groin • Pain caused by vigorous contractions of ureter – Effort to pass the stone
Calculi—Treatment • Small stones eventually passed out • Larger stones – Extracorporeal shock-wave lithotripsy (ESWL) • Decreases need for invasive surgery – Some drugs can partially dissolve • Need to prevent recurrences
Urinary Tract Obstructions: Tumors —Renal Cell Carcinoma • Primary, silent tumor • Arises from tubule epithelium • Asymptomatic in early stage – Often metastize to liver, lungs, bones, CNS at time of diagnosis • Common after 50 – More freq in males and smokers • Initial sign is painless hematuria • Other manifestations – Dull aching flank pain, palpable mass, anemia • Treatment is kidney removal – 5 yr survival rate 50%
 Chapter 47 urinary and reproductive disorders
Chapter 47 urinary and reproductive disorders Urinary retention
Urinary retention Nursing management of urinary retention ppt
Nursing management of urinary retention ppt Coital incontinence
Coital incontinence Acfi assessment
Acfi assessment Site:slidetodoc.com
Site:slidetodoc.com Bulbocavernosus reflex
Bulbocavernosus reflex Lymphatic system and urinary system
Lymphatic system and urinary system Difference between normal loss and abnormal loss
Difference between normal loss and abnormal loss Urinary system introduction
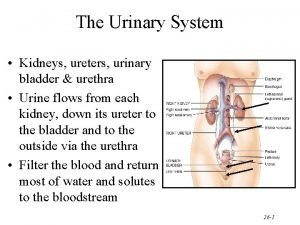
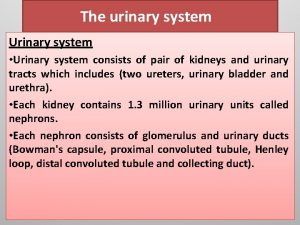
Urinary system introduction Figure 15-3 the urinary system
Figure 15-3 the urinary system Combining form for urinary bladder
Combining form for urinary bladder Whats gametes
Whats gametes Mammary papilla pig
Mammary papilla pig Chapter 30 the urinary system
Chapter 30 the urinary system Chapter 15 the urinary system figure 15-3
Chapter 15 the urinary system figure 15-3 Chapter 20 urinary/excretory system
Chapter 20 urinary/excretory system Urinary system model
Urinary system model Urinary system model
Urinary system model Alimentary canal
Alimentary canal Urinary system powerpoint
Urinary system powerpoint Urinary system also known as
Urinary system also known as Adh hormone function
Adh hormone function Urinary system histology
Urinary system histology