URINARY ELIMINATION Catheters TO PEE OR NOT TO

- Slides: 53
URINARY ELIMINATION & Catheters TO PEE OR NOT TO PEE, WHAT IS THE COLOR? Jennifer Bettag RN, BSN
Objectives – Demonstrate correct technique for inserting indwelling and straight catheters – Recognizes signs and symptoms of infection related to urinary catheters – Demonstrate aseptic routine care of a patient with an indwelling catheter – Demonstrate correct technique for removing an indwelling catheter. – Demonstrate correct procedure for application of condom catheter – Document and report to RN care related to urinary drainage
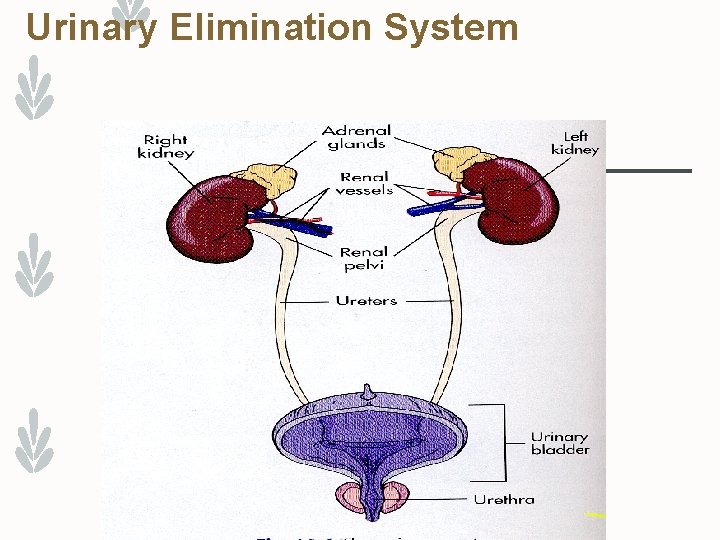
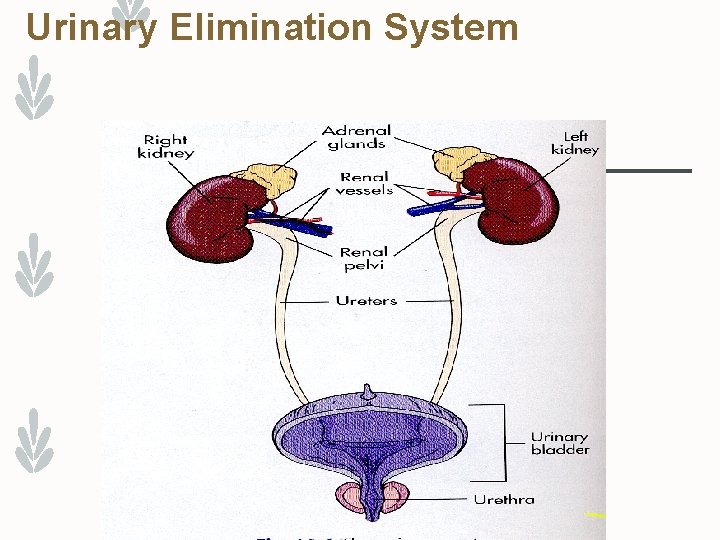
Urinary Elimination System
Anatomy Kidney - Urine production Ureters - Tubes which connect the kidneys to the bladder. Bladder - Reservoir for urine until the urge to void takes place. Urethra - Tube from the bladder to the outside of the body in normal anatomy. Male = 20 cm long Female = 4 cm long
Anatomy Facts – A continuous layer of mucous membrane lines the kidney pelvis, ureters, urethra & bladder – Because there is no break in this lining, bacteria introduced into this normally sterile environment can quickly spread throughout the entire system – When the bladder is empty it falls into folds which provide pockets where bacteria can multiply – Because this membrane layer is highly vascular, bacteria can easily enter the blood stream & cause septicemia
Normal Urination – The healthy adult excretes about 1500 milliliters (ml) (3 pints) of urine a day. – Factors affecting urine production include: – Age – Disease – The amount and kinds of fluid ingested – Dietary salt – Body temperature – Perspiration – Drugs – Urination, micturition, and voiding mean the process of emptying urine from the bladder. – Certain factors affect frequency, including: – The amount of fluid intake – Personal habits – People usually void at bedtime, after getting up, and before meals. – Some people void. every 2 to 3 hours.
What is your color?
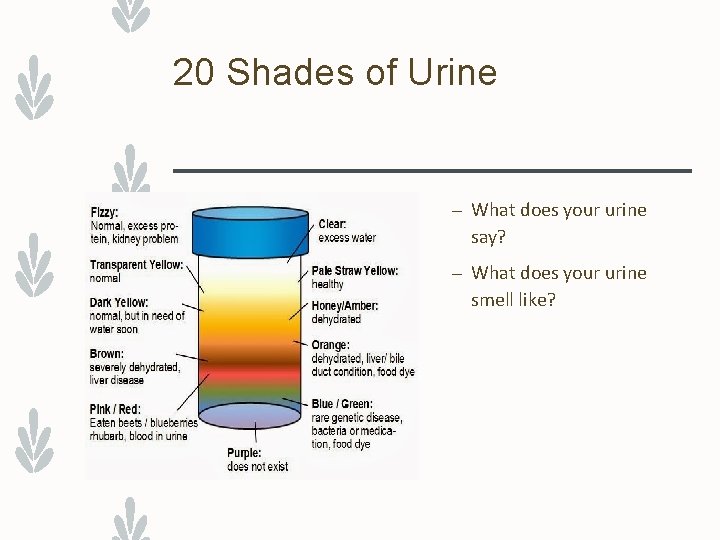
Urine observations – Normal urine: – Is pale yellow, straw colored, or amber – Is clear with no particles – Has a faint odor – Observe urine for color, clarity, odor, amount, and particles. – Some foods affect urine color and odor. – Certain drugs change urine color. – Report the following to the nurse: – Any urine that looks or smells abnormal – Complaints of urgency, burning on urination, or painful or difficult urination.
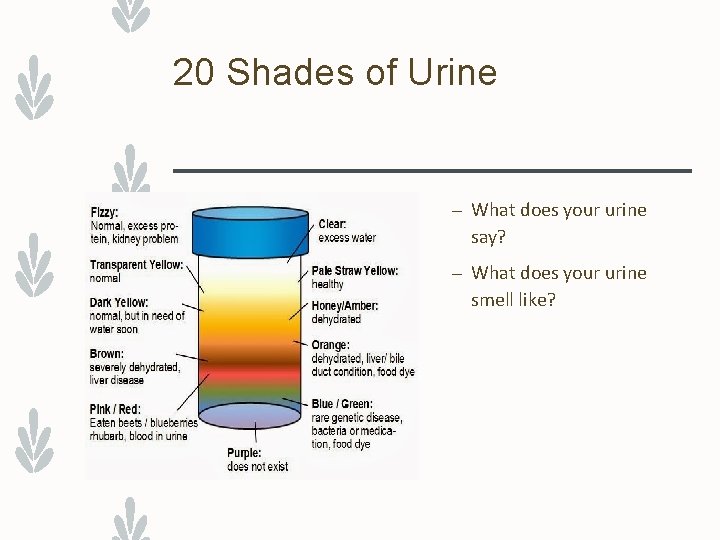
20 Shades of Urine – What does your urine say? – What does your urine smell like?
Urinary Incontinence – Urinary incontinence is the involuntary loss of urine from the bladder. – It may be temporary or permanent. – Basic types of incontinence (review page 382) – Stress – Urge – Overflow – Functional – Reflex – Mixed
Effects of incontinence: – Incontinence is embarrassing. – Skin irritation, infection, and skin breakdown can occur. – Falling is a risk. – The person’s pride, dignity, and self-esteem are affected. – Loss of independence, social isolation, and depression are common. .
Effects of Incontinence – Incontinence is linked to abuse, mistreatment, and neglect. – Caring for persons with incontinence is stressful. – Remember, incontinence is beyond the person’s control. – Be patient. – If you become short-tempered and impatient, talk to the nurse at once. – The person has the right to be free from abuse, mistreatment, and neglect. .
Persons with Dementia – may void in the wrong places. – Some persons remove incontinence products and throw them on the floor or in the toilet. – Some resist staff efforts to keep them clean and dry. – Check with the nurse and the care plan for measures to help the person. .
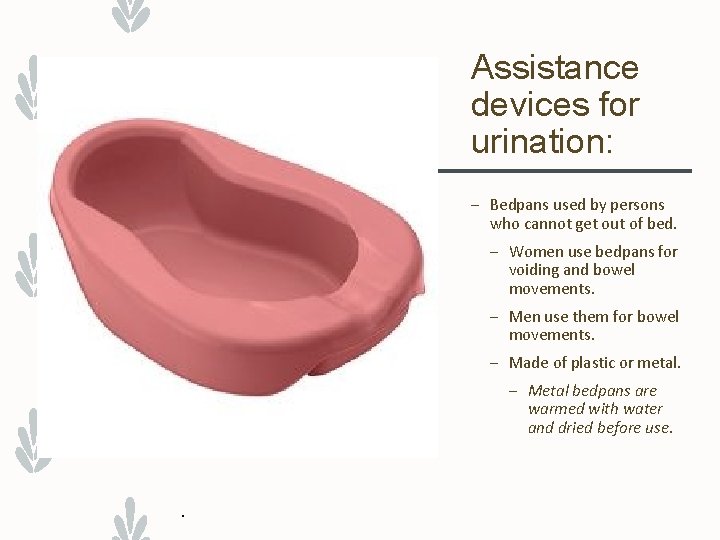
Assistance devices for urination: – Bedpans used by persons who cannot get out of bed. – Women use bedpans for voiding and bowel movements. – Men use them for bowel movements. – Made of plastic or metal. – Metal bedpans are warmed with water and dried before use. .
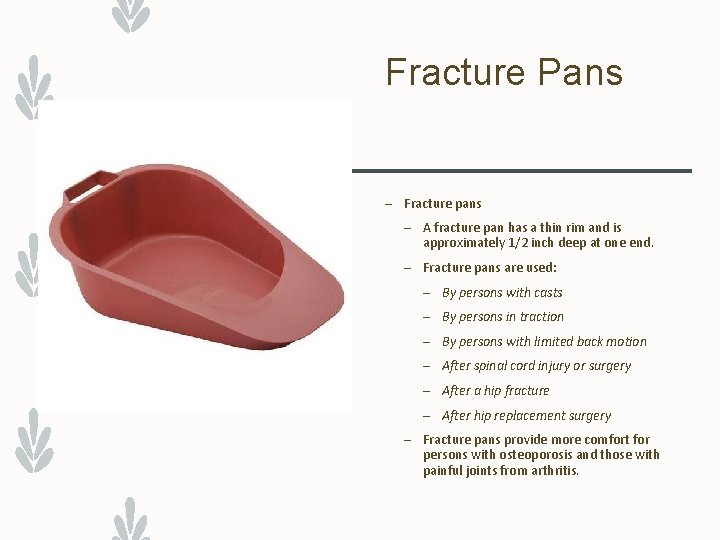
Fracture Pans – Fracture pans – A fracture pan has a thin rim and is approximately 1/2 inch deep at one end. – Fracture pans are used: – By persons with casts – By persons in traction – By persons with limited back motion – After spinal cord injury or surgery – After a hip fracture – After hip replacement surgery – Fracture pans provide more comfort for persons with osteoporosis and those with painful joints from arthritis.
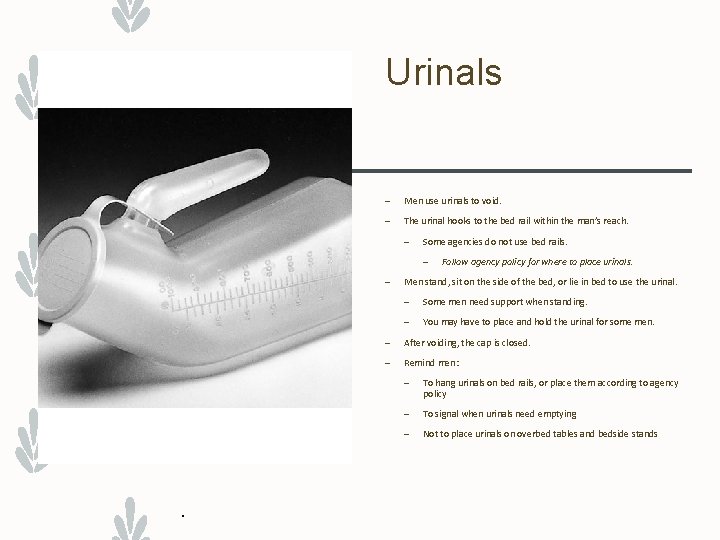
Urinals – Men use urinals to void. – The urinal hooks to the bed rail within the man’s reach. – Some agencies do not use bed rails. – – . Follow agency policy for where to place urinals. Men stand, sit on the side of the bed, or lie in bed to use the urinal. – Some men need support when standing. – You may have to place and hold the urinal for some men. – After voiding, the cap is closed. – Remind men: – To hang urinals on bed rails, or place them according to agency policy – To signal when urinals need emptying – Not to place urinals on overbed tables and bedside stands

Commodes – A commode is a chair or wheelchair with an opening for a bedpan or container. – Persons unable to walk to the bathroom often use commodes. – Commodes allow a normal position for elimination. – Some commodes are wheeled into bathrooms and placed over toilets. – The container is removed if the commode is used with the toilet. – Wheels are locked after the commode is positioned over the toilet. – Review ~ Helping the Person to the Commode p 381 .
Catheterization - Reasons Ø Collect a sterile specimen Ø Check residual urine Ø Inability to void related to post-op complications Ø Before, during or after surgery to empty bladder Ø Temporary/Permanent Incontinence: a. Total- continuous loss of urine from bladder b. Stress- leakage of small amounts of urine with physical stress i. e. coughing or sneezing
Catheterization - Reasons Ø Urge - Involuntary passage of urine after feeling strong need to void. Unable to stop urinating and can’t get to bathroom on time. Seen in the elderly, with UTIs and tumors. Ø Functional - Involuntary, unpredictable passage of urine related to no call light or immobility, etc.
Alternative to Catheterization – Bladder Scan – Estimates residual urine – Increased use over straight catheterization – 90% accuracy – Decreases risk of infection and discomfort to patient
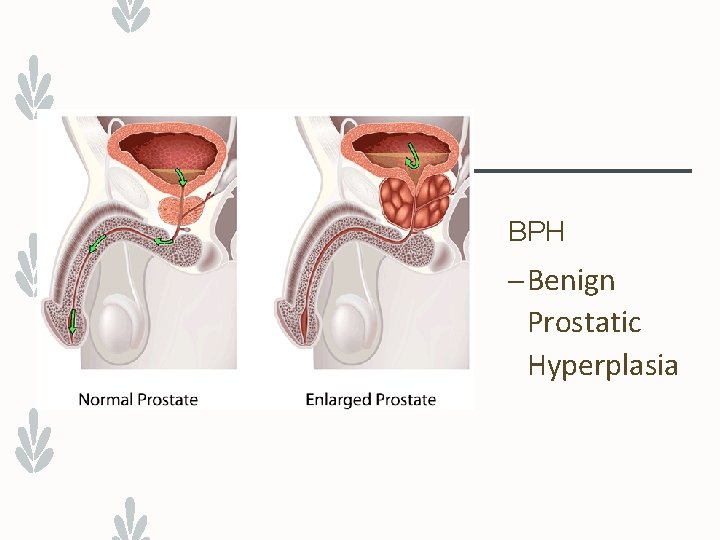
PRIOR to Catheterization Know and Confirm – Doctor’s order – Last void – Patient’s level of consciousness and understanding – Mobility, physical limitations, ability to cooperate – Sex, age, catheter size – Kids 6 -10 – Female 14 -16 – Male 16 -18) – Allergies to antiseptics, tape, rubber, latex – Adverse conditions – Impaired passage such as enlarge prostate
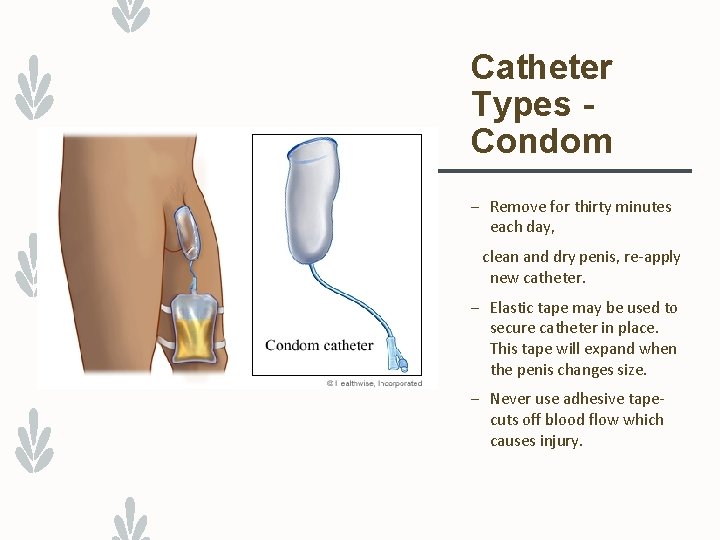
Catheter Types - Condom Catheter (External, Texas, Urinary Sheath) Incontinent men Soft rubber, latex, silicone Slides over Penis Tubing connects to tip of condom and flows into collection bag.
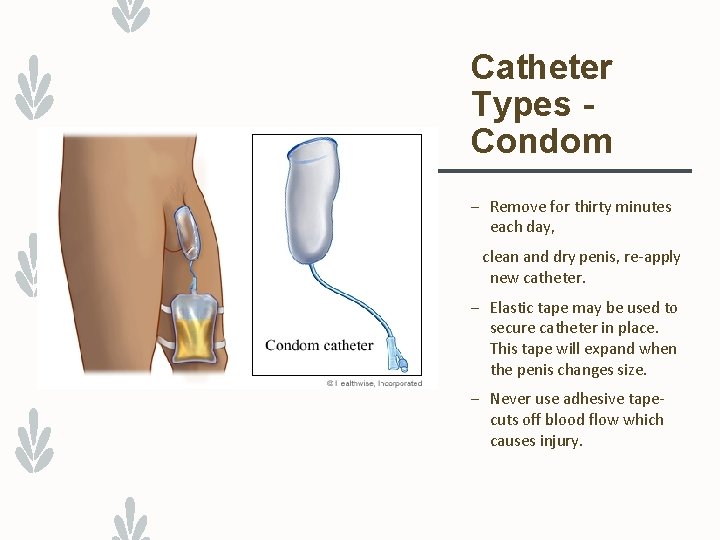
Catheter Types Condom – Remove for thirty minutes each day, clean and dry penis, re-apply new catheter. – Elastic tape may be used to secure catheter in place. This tape will expand when the penis changes size. – Never use adhesive tapecuts off blood flow which causes injury.
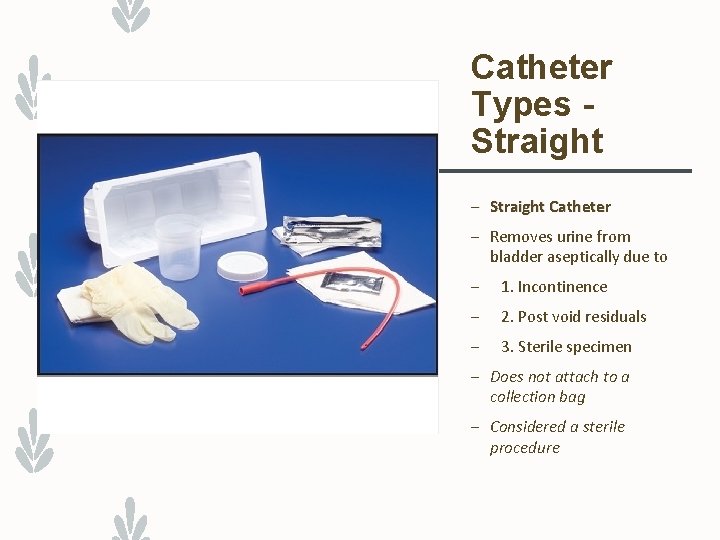
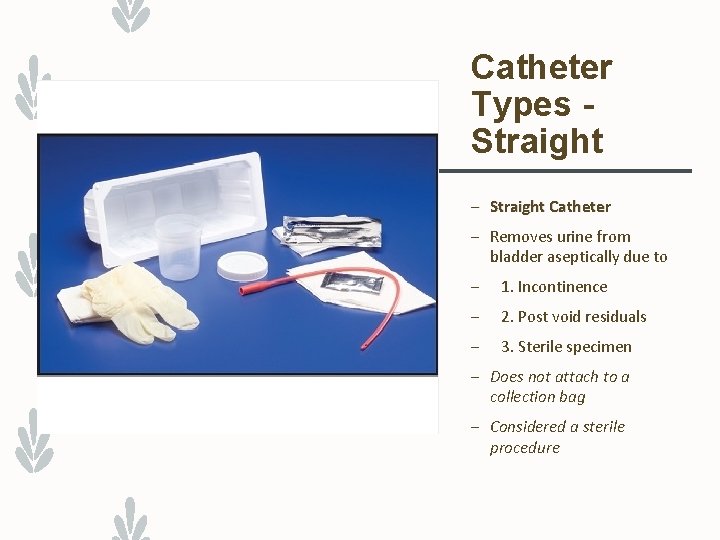
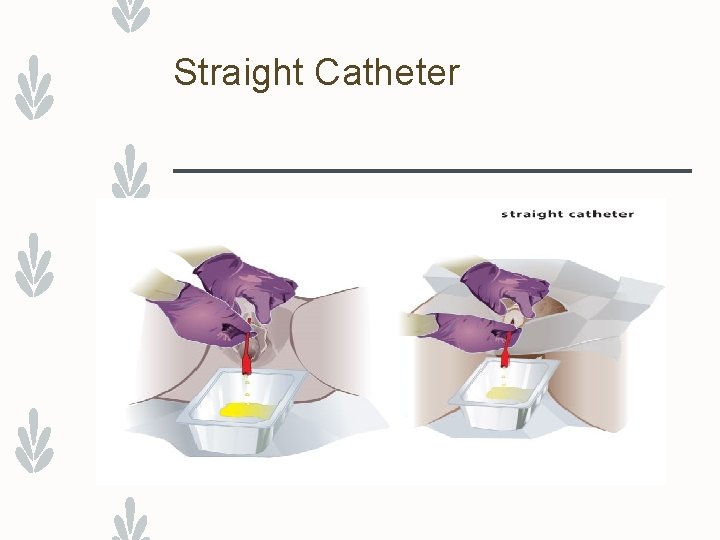
Catheter Types Straight – Straight Catheter – Removes urine from bladder aseptically due to – 1. Incontinence – 2. Post void residuals – 3. Sterile specimen – Does not attach to a collection bag – Considered a sterile procedure
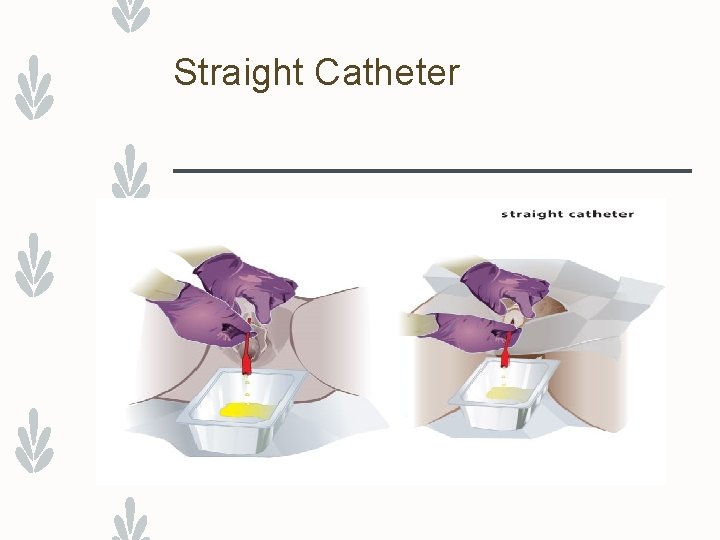
Straight Catheter
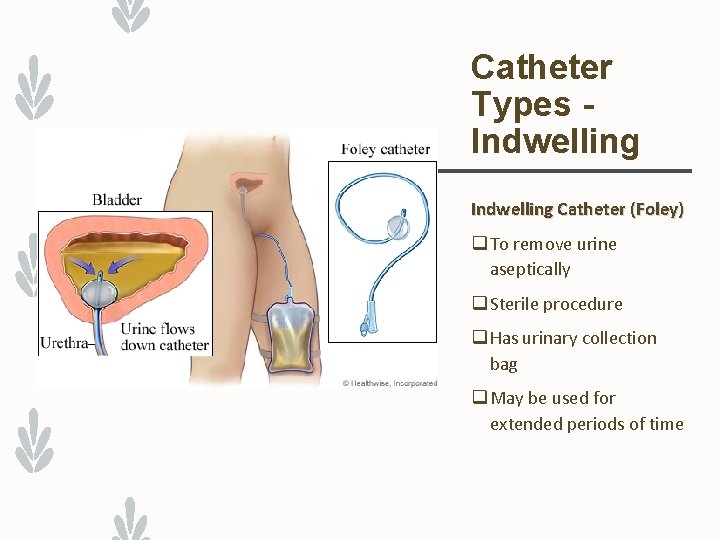
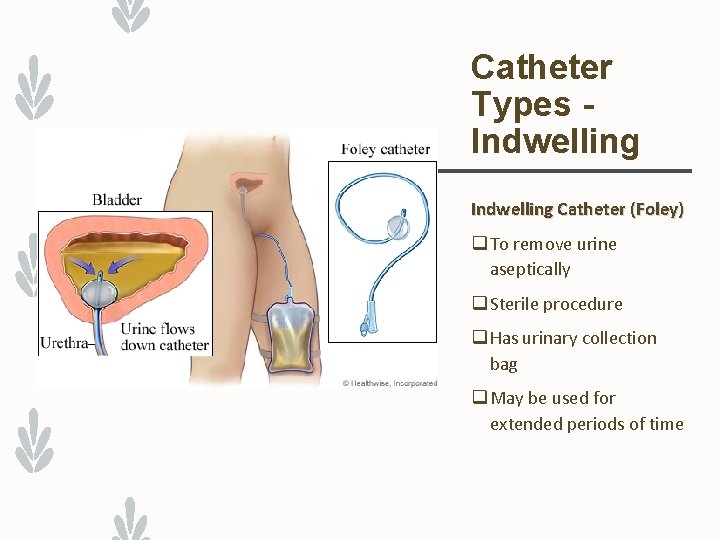
Catheter Types Indwelling Catheter (Foley) q To remove urine aseptically q Sterile procedure q Has urinary collection bag q May be used for extended periods of time
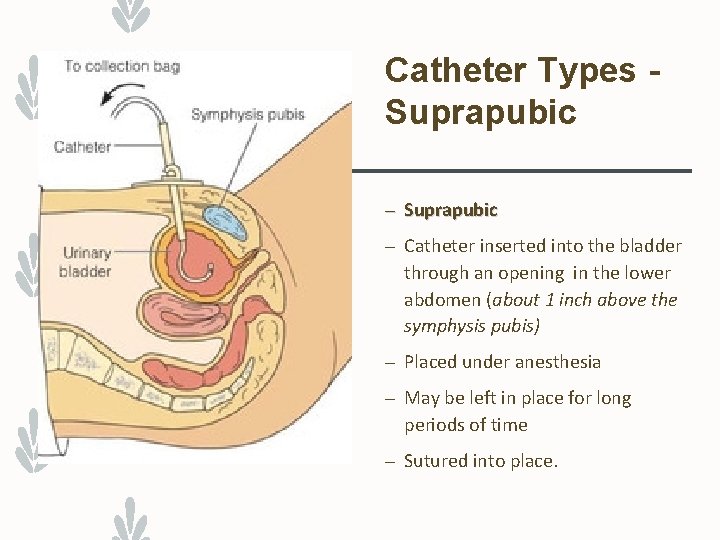
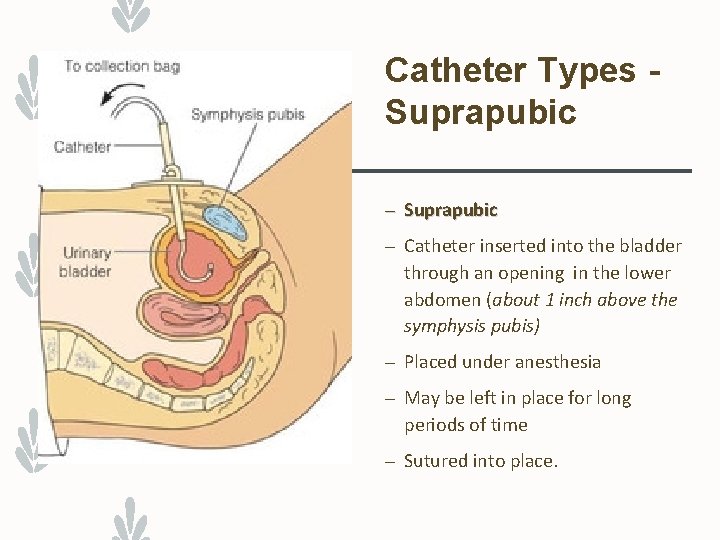
Catheter Types Suprapubic – Catheter inserted into the bladder through an opening in the lower abdomen (about 1 inch above the symphysis pubis) – Placed under anesthesia – May be left in place for long periods of time – Sutured into place.
Subrapubic Catheter Reasons for infections? ? ?
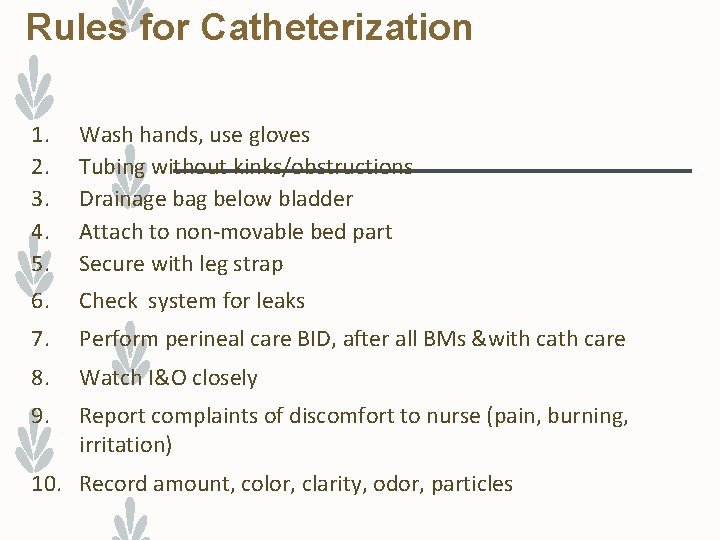
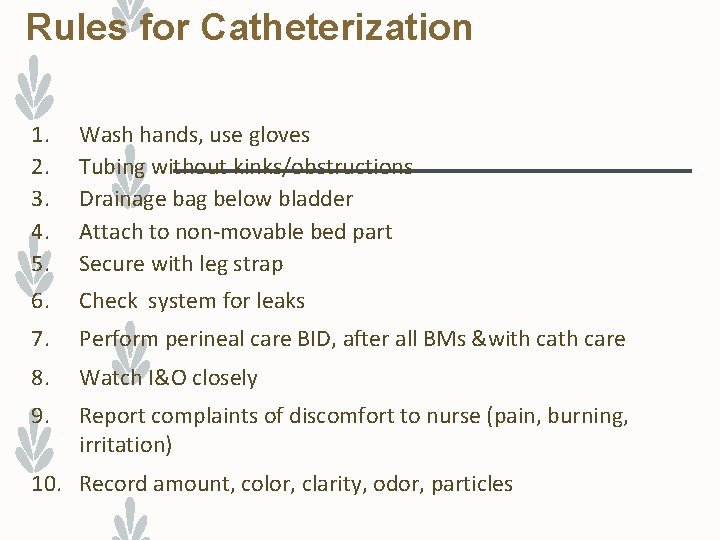
Rules for Catheterization 1. 2. 3. 4. 5. Wash hands, use gloves Tubing without kinks/obstructions Drainage bag below bladder Attach to non-movable bed part Secure with leg strap 6. Check system for leaks 7. Perform perineal care BID, after all BMs &with care 8. Watch I&O closely 9. Report complaints of discomfort to nurse (pain, burning, irritation) 10. Record amount, color, clarity, odor, particles
Insertion/Application - Condom Catheter – Clean gloves to remove old catheter – Wash and dry penis – Apply skin prep to penis shaft – Remove protective backing from condom exposing adhesive strip
Insertion/Application - Condom – Hold penis firmly. Roll condom onto penis leaving 1 inch space between penis and end of catheter. – Secure condom with elastic strip in spiral manner not completely on penis – Connect condom to drainage bag – Check penis for redness and excoriation
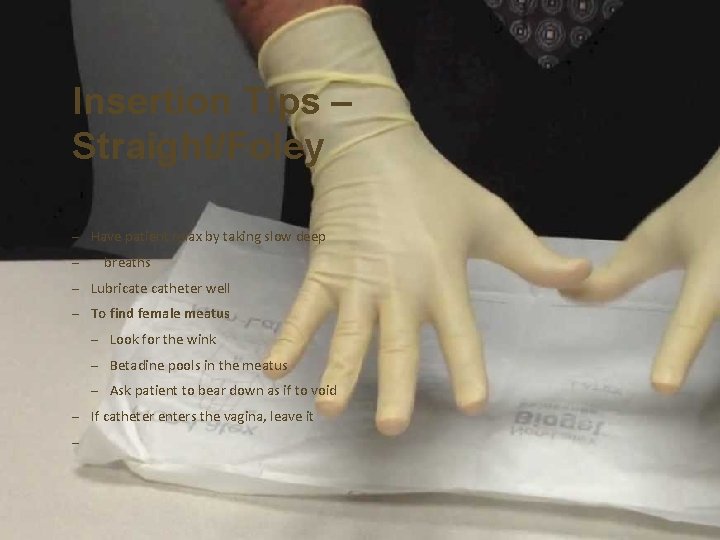
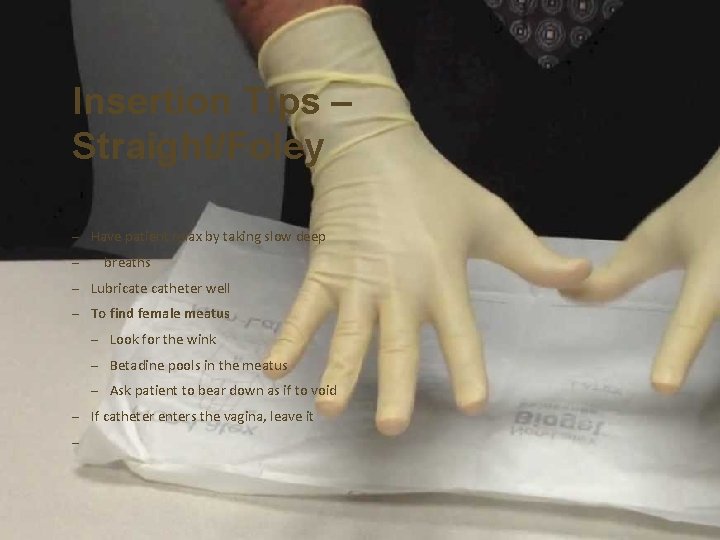
Insertion Tips – Straight/Foley – Have patient relax by taking slow deep – breaths – Lubricate catheter well – To find female meatus – Look for the wink – Betadine pools in the meatus – Ask patient to bear down as if to void – If catheter enters the vagina, leave it –
Catheter Insertion Video – https: //youtu. be/Yd. PMAGSs. J 20 – Please take notes as this will be a check off this year
Insertion of Indwelling Catheter – If indwelling catheter, GENTLY tug on catheter until resistance is met to insure placement in bladder – Do peri care and apply leg band to secure catheter to patient’s leg – Remove gloves and discard supplies properly
Other Considerations When performing straight cath q Know policy & procedure for maximum amount of urine allowed to be withdrawn. To place catheter in an uncircumcised man q Carefully pull back foreskin before cleansing
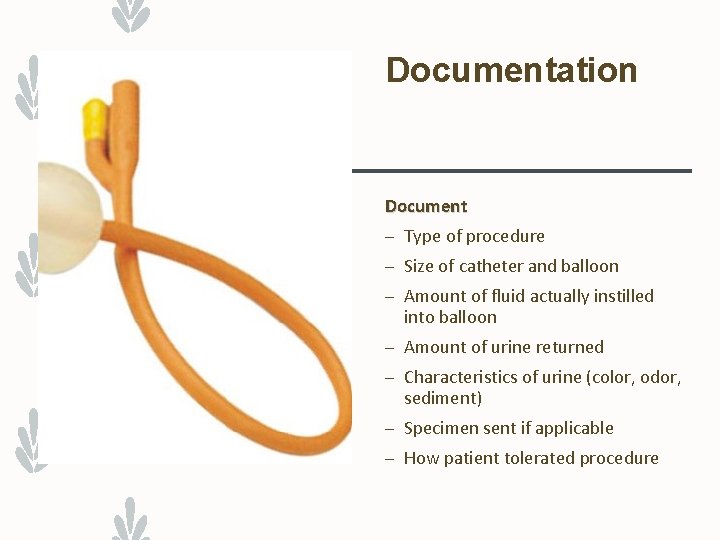
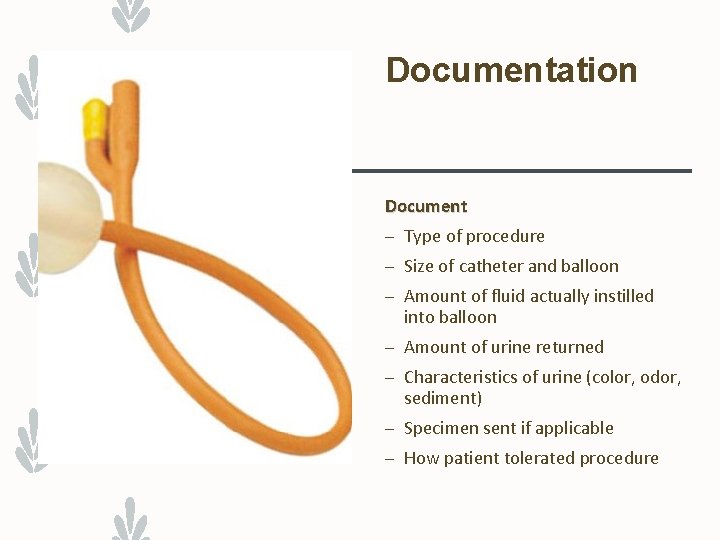
Documentation Document – Type of procedure – Size of catheter and balloon – Amount of fluid actually instilled into balloon – Amount of urine returned – Characteristics of urine (color, odor, sediment) – Specimen sent if applicable – How patient tolerated procedure
Problems During Insertion Catheter inserted into Vagina 1. Leave in place 2. Reposition fingers to re-visualize meatus 3. Use new catheter 4. Repeat procedure
Problems During Insertion Unable to insert into female 1. Ask patient or other team member to hold legs apart 2. Observe urethral opening (before cleansing) for movement when pressure is applied 3. Improve lighting 4. Repeat insertion procedure
Problems During Insertion Unable to insert catheter into male 1. Notify nurse 2. Repeat procedure but change the angle of the penis 3. Try an a coude catheter
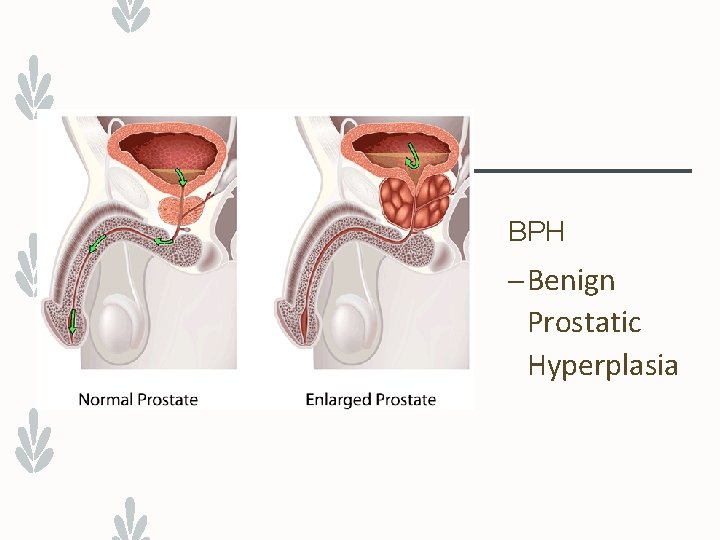
BPH – Benign Prostatic Hyperplasia
Problems During Insertion Catheter comes out with balloon inflated 1. Check with nurse 2. Check for urethral trauma (pain, bleeding) 3. Monitor urine output for bleeding 4. Obtain new catheter kit & reinsert with 10 ml balloon per nurse’s instruction
Care of Patient with a Catheter 1. Keep catheter bag below level of bladder 2. Attach drainage bag to bed frame (not side rails) 3. Secure tubing onto bed – urine should flow freely from catheter to bag (coil tubing on bed) 4. Empty catheter bag every 8 hours or prn 5. Provide catheter care & pericare as needed 6. Do not allow the drain on the bag to touch any surface 7. Keep drainage bag off the floor
Catheter Removal 1. Physician’s order 2. Gather supplies- 10 cc syringe, gloves, chux 3. Deflate balloon- note amount withdrawn 4. Avoid pubic hair 5. Pinch catheter; pull out on exhalation steadily & gently 6. Measure output 7. Discard catheter bag properly 8. Provide peri care 9. Monitor patient for output 10. If not voided in 4 -6 hours, notify nurse
Drainage system disconnected, what do you do? 1. Tell_________ 2. Do not_______ 3. Practice_______ 4. Wipe________ 5. Wipe________ 6. Do not_______ 7. Connect_______ 8. Discard_______ 9. Remove_______
Following Catheter Removal 1. Patient to void within 4 -6 hours 2. Urine amount 120 -240 ml (or per policy) 3. Observe bladder for distention 4. Monitor patient for any complaints of painful urination 5. Monitor patient for hematuria
Catheter Removal Documentation Document : – Size of catheter removed – Size and amount of fluid in balloon – Patient tolerance – Output in catheter bag – Description of urine – Peri care – Time of removal
Voiding Following Catheter Removal Hints to assist patient to void after catheter removal – Encourage oral fluids – Proper position to urinate – Sound of running water – Sitz bath
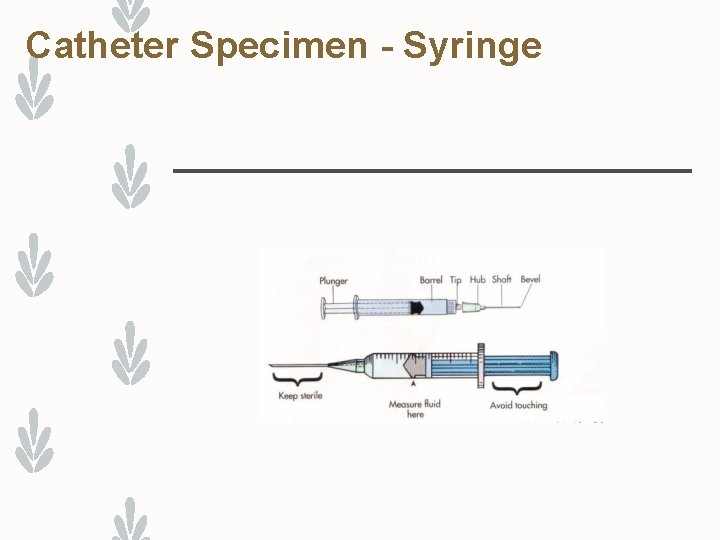
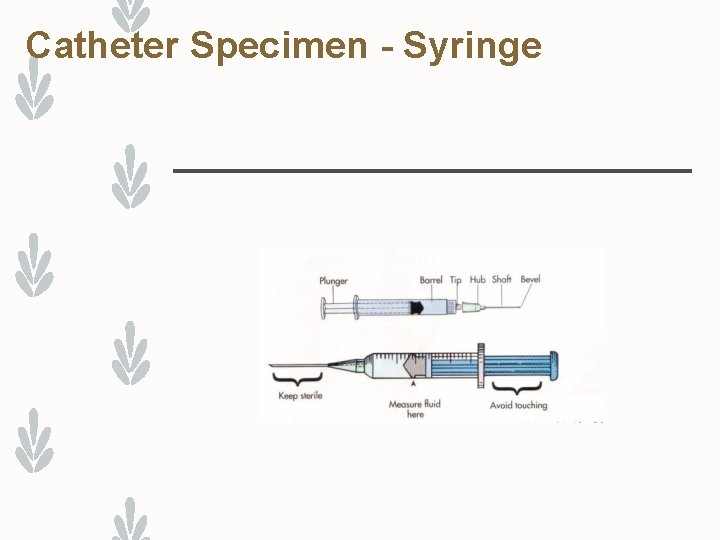
Catheter Specimen - Syringe
Urinary Diversions Definition Removal of bladder (cancer, bladder injuries) and making a new pathway for urine to exit the body. Two Categories 1. Continent 2. Noncontinent (incontinent)
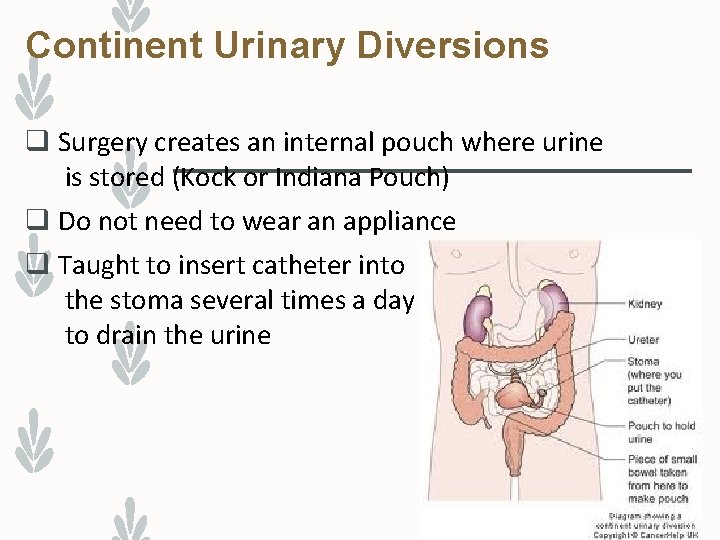
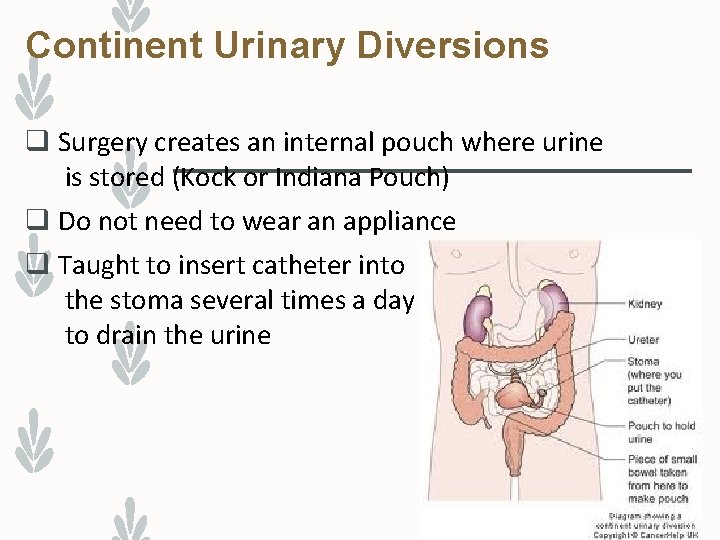
Continent Urinary Diversions q Surgery creates an internal pouch where urine is stored (Kock or Indiana Pouch) q Do not need to wear an appliance q Taught to insert catheter into the stoma several times a day to drain the urine
Noncontinent Urinary Diversions q Patient cannot control urine q Must wear an external urinary ostomy pouch Types of non-continent urinary diversions 1. Ureterostomy
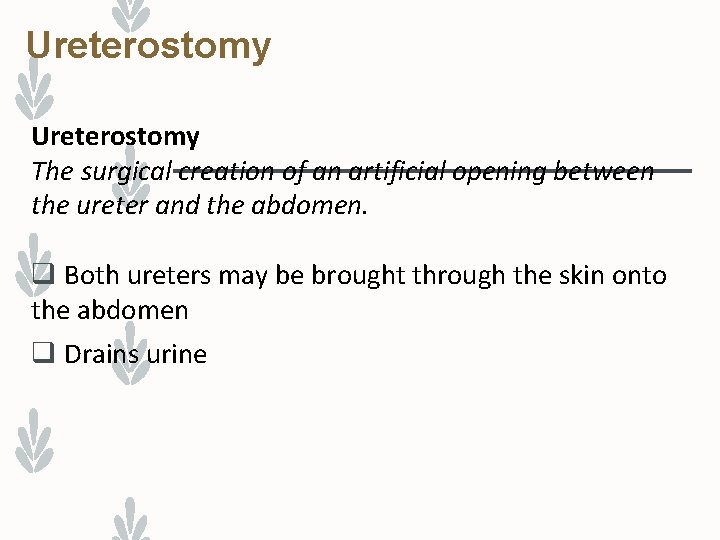
Ureterostomy The surgical creation of an artificial opening between the ureter and the abdomen. q Both ureters may be brought through the skin onto the abdomen q Drains urine
Measuring Urinary Output – https: //youtu. be/e 9 y 96 kmn. R 2 c