Urinary elimination Dr Dergham M Hameed Urinary System







- Slides: 33
Urinary elimination Dr. Dergham M. Hameed
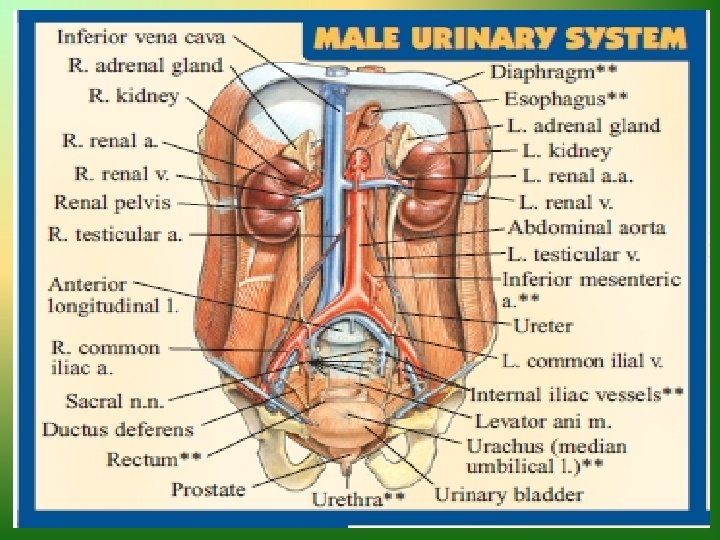
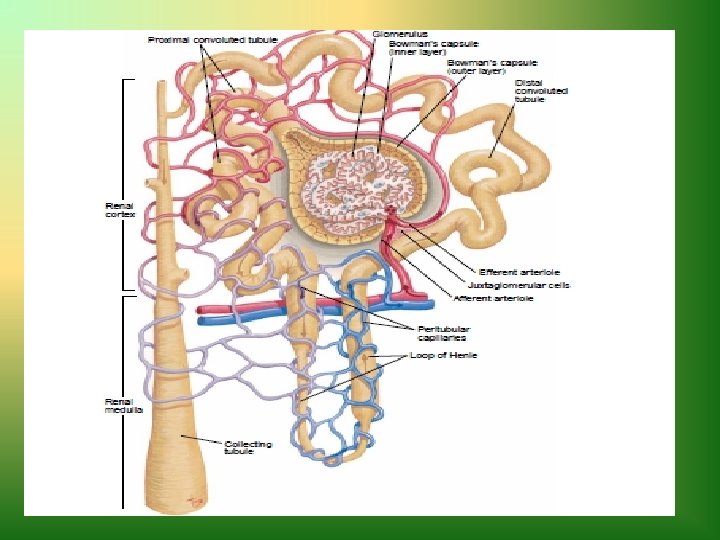
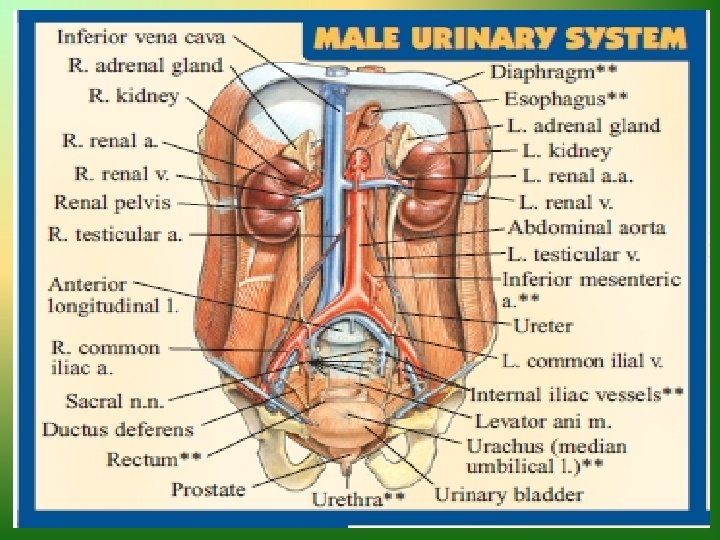
Urinary System • Kidneys and ureters • Bladder • Urethra
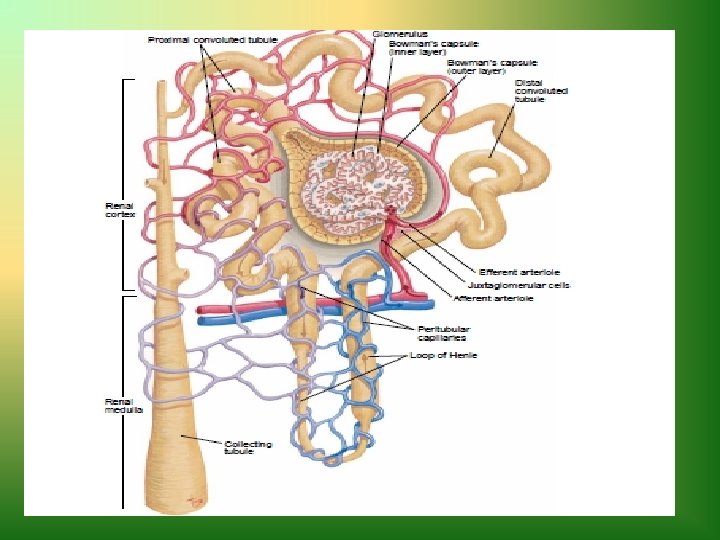
Kidneys and Ureters • Maintain composition and volume of body fluids • Filter and excrete blood constituents not needed, retain those that are needed • Excrete waste product (urine) • Nephrons remove the end products of metabolism and regulate fluid balance • Urine from the nephrons empties into the kidneys

Bladder • Smooth muscle sac • Serves as a reservoir for urine • Composed of three layers of muscle tissue called detrusor muscle • Sphincter guards opening between urinary bladder and urethra • Urethra conveys urine from bladder to exterior of body
Urethra • Conveys urine from the bladder to the exterior • Male urethra functions in excretory and reproductive system • No portion of female urethra is external to the body
Act of Micturition • Process of emptying the bladder – Detrusor muscle contracts, internal sphincter relaxes, urine enter posterior urethra – Muscles of perineum and external sphincter relax – Muscle of abdominal wall contracts slightly – Diaphragm lowers, micturition occurs
Factors Affecting Micturition • Developmental considerations • Food and fluid intake • Psychological variables • Activity and muscle tone • Pathologic conditions • Medication
Developmental Considerations • Children – Toilet training 18 to 24 months, enuresis • Effects of aging – Nocturia, increased frequency, urine retention and stasis, voluntary control affected by physical problems
Diseases Associated With Renal Problems • Congenital urinary tract abnormalities • Polycystic kidney disease • Urinary tract infection • Urinary calculi • Hypertension • Diabetes mellitus • Gout • Connective tissue disorders

Effects of Medications on Urine Production and Elimination • Diuretics — prevent reabsorption of water and certain electrolytes in tubules • Cholingeric medications — stimulate contraction of detrusor muscle, producing urination • Analgesics and tranquilizers — suppress CNS diminish effectiveness of neural reflex
Medications Affecting Color of Urine • Anticoagulants — red color • Diuretics — lighten urine to pale yellow • Pyridium — orange to orange-red urine • Elavil — green or blue-green • Levodopa — brown or black
Using the Nursing Process • Assessing data about voiding patterns, habits, past history of problems • Physical examination of urinary system, skin hydration, urine • Correlation of these findings with results of procedures and diagnostic tests
Assessing a Problem With Voiding • Explore its duration, severity, and precipitating factors. • Note patient’s perception of the problem. • Check adequacy of patient’s self-care behaviors.

Physical Assessment of Urinary Functioning • Kidneys — check for costovertebral tenderness • Urinary bladder — palpate and percuss the bladder or use bedside scanner • Urethral meatus — inspect for signs of infection, discharge, or odor • Skin — assess for color, texture, turgor, and excretion of wastes • Urine — assess for color, odor, clarity, and sediment


Measuring Urine Output • Ask patient to void into bedpan, urinal, or specimen container in bed or bathroom. • Pour urine into appropriate measuring device. • Place calibrated container on flat surface and read at eye level. • Note amount of urine voided and record on appropriate form. • Discard urine in toilet unless specimen is needed.

Urine Specimens • Routine urinalysis • Specimens from infants and children • Clean-catch or midstream specimens • Sterile specimens from indwelling catheter • 24 -hour urine specimen

Diagnoses • Urinary functioning as the problem – Incontinence, pattern alteration, urinary retention • Urinary functioning as the etiology – Anxiety, caregiver role strain, risk for infection
Planned Patient Goals • Urine output about equal to fluid intake • Maintain fluid and electrolyte balance • Empty bladder completely at regular intervals • Report ease of voiding • Maintain skin integrity
Promoting Normal Urination • Maintaining normal voiding habits • Promoting fluid intake • Strengthening muscle tone • Stimulating urination and resolving urinary retention
Maintaining Normal Voiding Habits • Schedule • Privacy • Position • Hygiene
Patients at Risk for UTIs • Sexually active women • Postmenopausal women • Individuals with indwelling urinary catheter • Individual with diabetes mellitus • Elderly people
Four Types of Urinary Incontinence • Stress — increase in intraabdominal pressure • Urge — urine lost during abrupt and strong desire to void • Mixed — symptoms of urge and stress incontinence present • Overflow — overdistention and overflow of bladder • Functional — caused by factors outside the urinary tract
Factors to Consider With Use of Absorbent Products • Functional disability of the patient • Type and severity of incontinence • Gender • Availability of caregivers • Failure with previous treatment programs • Patient preference
Reasons for Catheterization • Relieving urinary retention • Obtaining a sterile urine specimen • Measuring amount urine in bladder • Obtaining a urine specimen • Emptying bladder before during or after surgery • Monitoring of critically ill patients
Evaluating Effectiveness of Plan • Maintain fluid, electrolyte, and acid-base balance • Empty bladder completely at regular intervals with no discomfort • Provide care for urinary diversion and when to notify physician • Develop a plan to modify factors contributing to problem • Correct unhealthy urinary habits