Department of Medical Assistance Services Medicaid 101 www



- Slides: 169
Department of Medical Assistance Services Medicaid 101 www. dmas. virginia. gov
This presentation is to facilitate training of the subject matter in Virginia Medicaid Hospital Manual. This training contains only highlights of the manual and is not meant to substitute for or take the place of the manual. Providers are responsible for reviewing and adhering to all Medicaid manual requirements. 22
Agenda 1. DMAS Website 2. Excluded Individuals/Entities 3. Medicaid Eligibility Verification Options 4. Medicaid Programs and Benefit Packages 5. UB-04 Billing Guidelines 3
DMAS Website www. dmas. virginia. gov • Current, most up-to-date information on Virginia Medicaid programs • Provider memos available for review • Access to Medicaid manuals • 50 Common Error Reason Codes with Resolutions • Numeric Insurance Code List • Primary Carrier Coverage Code List 4
DMAS Website www. dmas. virginia. gov • Financial Reason Code Description List • Hospital DRG Rates • Medicaid Forms • 2010 Medicaid/FAMIS-PLUS Handbook 5

6
Excluded Individual/Entities • No payment can be made for any items or services ordered or prescribed by an excluded physician when the furnishing party either knew or should have known of the exclusion • Medicaid providers may be subject overpayment liability and civil monetary penalties when they do not abide by this Federal Regulation 7
Excluded Individual/Entities • This ban includes payment for administrative and management services not directly related to patient care • Providers are required to identify excluded individuals and entities • This ensures that DMAS is not paying any excluded individuals or entities for services rendered 8
How to Ensure Program Integrity • Screen all employees and contractors to determine whether they have been excluded • Search HS-OIG List of Excluded Individuals/Entities (LEIE) website monthly • Immediately report to DMAS any exclusion information discovered 9
Reporting • Discoveries are to be sent in writing to the address below and should include the: – individual or business name – provider identification number • State action, if any, has been taken DMAS Attn: Program Integrity/Exclusions 600 E. Broad St. Ste 1300 Richmond, VA 23219 10
Accessing the LEIE • HHS-OIG maintains the LEIE • Provides information about parties excluded from participation in Medicare, Medicaid and all other Federal healthcare programs • The online database is located at http: //www. oig. hhs. gov/fraud/exclusions. asp 11
As A Participating Provider You Must • • Determine the patient’s identity. Verify the patient’s age. Verify the patient’s eligibility. Accept, as payment in full, the amount paid by Virginia Medicaid. • Bill any and all other third-party carriers. 12
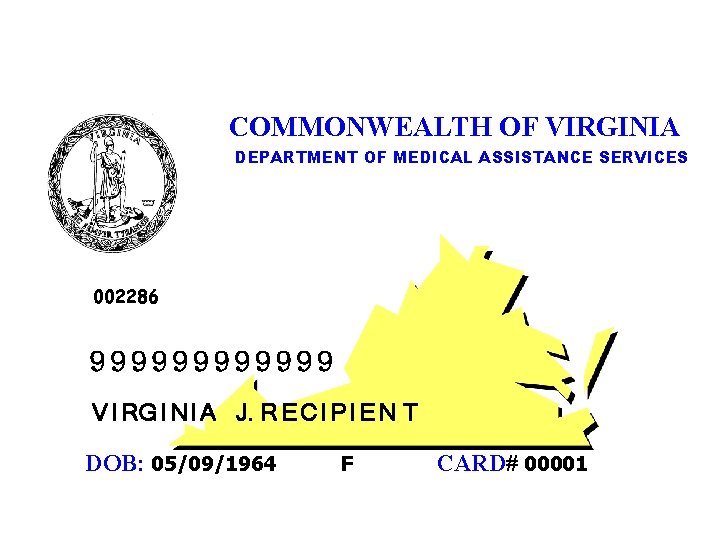
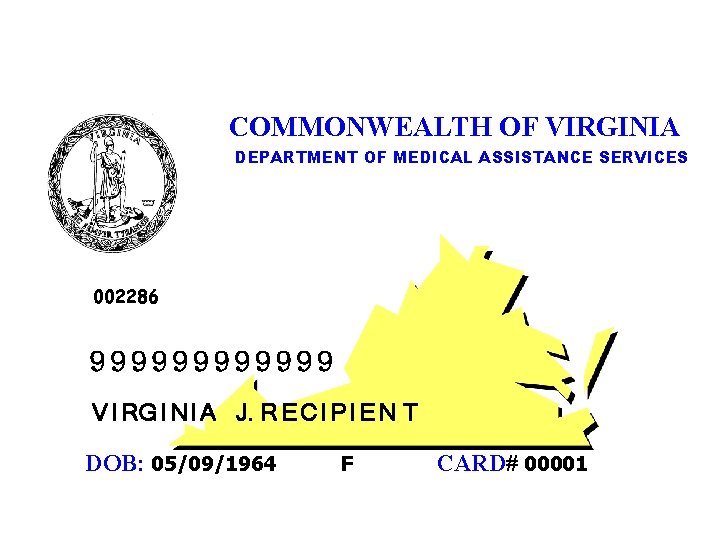
COMMONWEALTH OF VIRGINIA DEPARTMENT OF MEDICAL ASSISTANCE SERVICES 002286 999999 V I RG I N I A J. R E C I P I E N T DOB: 05/09/1964 F CARD# 00001 13
Medicaid Verification Options • Medi. Call • Medicaid Web Portal 14
Medi. Call/Medicaid Web Portal Information Available • Medicaid member eligibility/benefit verification • Service limit information • Claim status • Service authorization • Provider check log • Primary Payer Information • Medallion Participation • Managed Care Organization Assignment 15
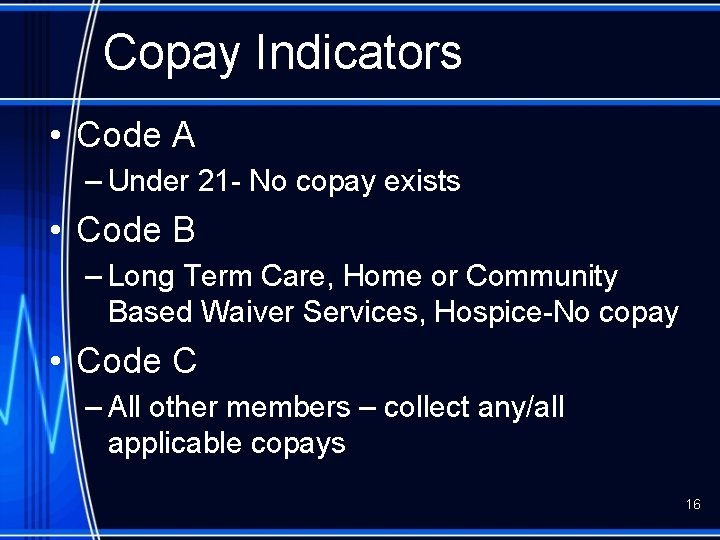
Copay Indicators • Code A – Under 21 - No copay exists • Code B – Long Term Care, Home or Community Based Waiver Services, Hospice-No copay • Code C – All other members – collect any/all applicable copays 16
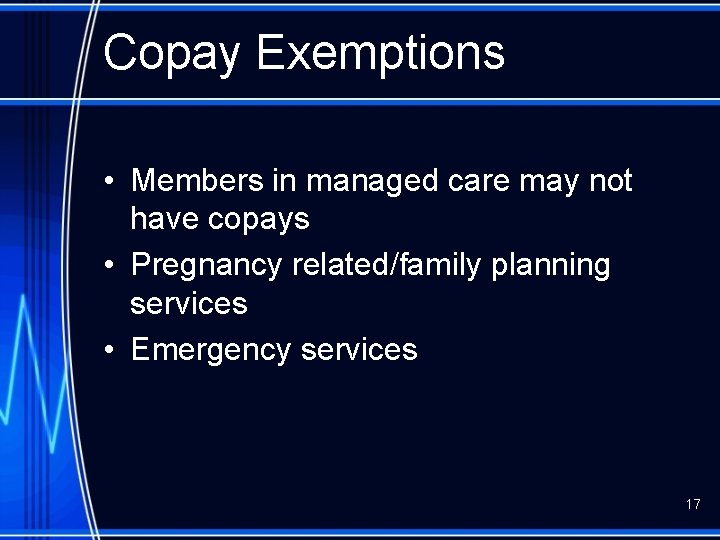
Copay Exemptions • Members in managed care may not have copays • Pregnancy related/family planning services • Emergency services 17
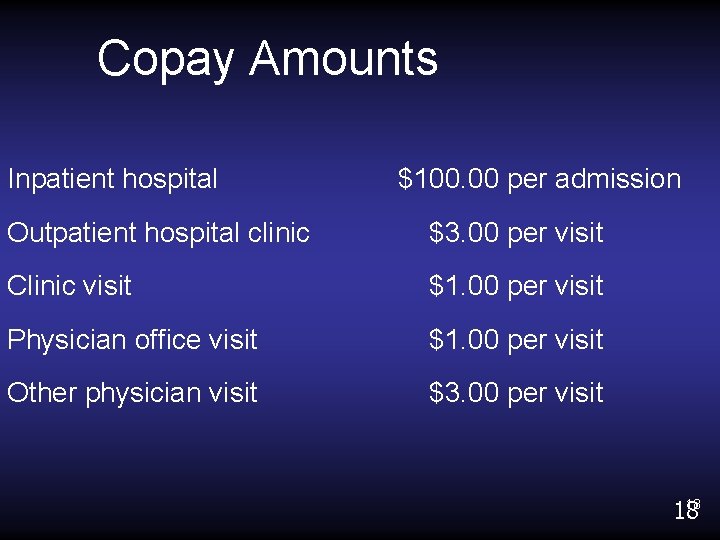
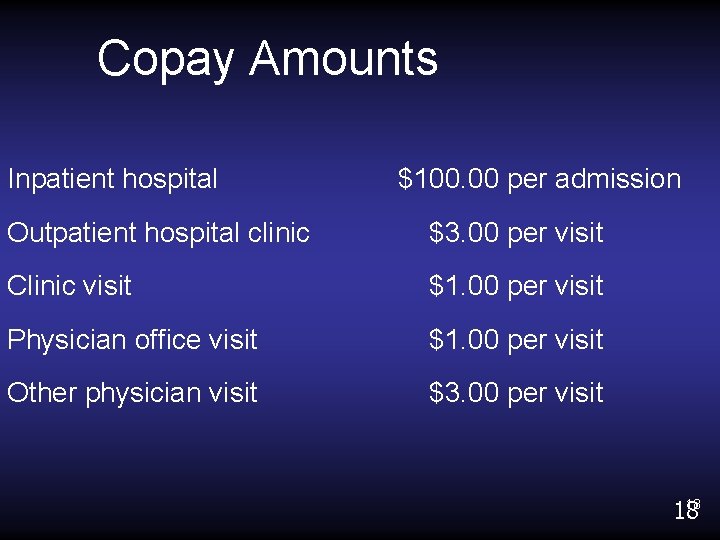
Copay Amounts Inpatient hospital $100. 00 per admission Outpatient hospital clinic $3. 00 per visit Clinic visit $1. 00 per visit Physician office visit $1. 00 per visit Other physician visit $3. 00 per visit 18 18
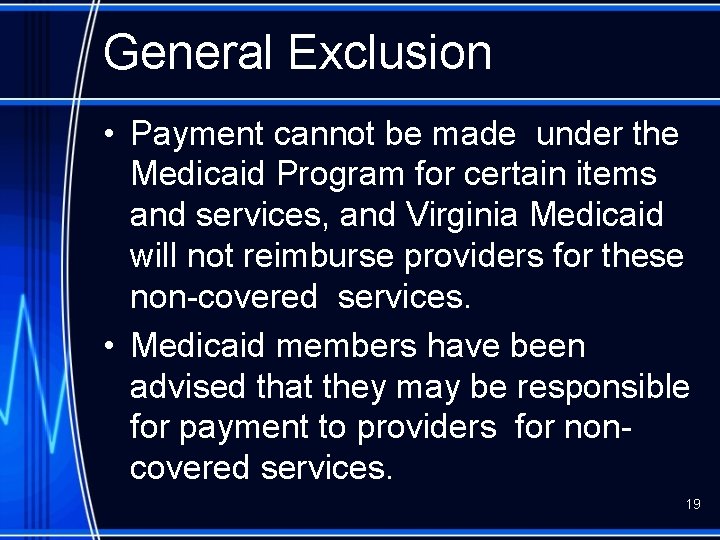
General Exclusion • Payment cannot be made under the Medicaid Program for certain items and services, and Virginia Medicaid will not reimburse providers for these non-covered services. • Medicaid members have been advised that they may be responsible for payment to providers for noncovered services. 19
General Exclusion - Directive • Prior to the provision of service, the provider must advise the Medicaid member that he or she may be billed for a non-covered service. • A directive signed by the patient, meets Virginia Medicaid’s requirement of patient notification of financial responsibility for noncovered services. 20

Medi. Call • • 800 -884 -9730 800 -772 -9996 804 -965 -9732 804 -965 -9733 21
Medicaid Web Portal • Web-based eligibility verification option – Free of Charge. – Information received in “real time”. – Secure – Fully HIPAA compliant 22
Changes • A new enhanced web portal will allow providers to transact all Medicaid business via one central location. • The web portal will provide access to: – Member Eligibility Status – Payment History – Remittance Advices – Service Authorization 23
Registration Process • First Time Users – Go to www. virginiamedicaid. dmas. virginia. gov – Establish an user ID and password – By registering you are acknowledging yourself as a staff member with administrative rights for the organization • Established Users- Delegated Administrators – will receive a letter containing their NPI and instructions on accessing the Web Portal – must access the Web Portal and change their temporary password no later than June 27, 2010 – will be able to add new users beginning June 28, 24 2010. 24
ACS Web Registration Support Call Center • Questions regarding new user registration, existing user access letter, or temporary password – 1 -866 -352 -0496 – Available after June 8, 2010 – 8 am – 5 pm Monday thru Friday – No holidays 25
Key Dates and Times • May 26 th – New registration to FHS/UAC discontinued • Through June 27 th – Current FHS/UAC users can continue to request password resets, routine maintenance, or access information as normal • June 27 th – Access to ARS via FHS/UAC will be discontinued 26
Key Dates and Times • June 28 th – new registration and users can be added via the new Virginia Medicaid Web Portal – access to eligibility and claims information will be available in the new Virginia Medicaid Web Portal at 7: 01 am www. virgniniamedicaid. dmas. virginia. gov 27

Provider Call Center Claims, covered services, billing inquiries: 800 -552 -8627 804 -786 -6273 8: 30 am – 4: 30 pm (Monday-Friday) 11: 00 am – 4: 30 pm (Wednesday) 28
Provider Enrollment NPI enrollment, EFT sign-up, update facility contact and email, change of address or phone number: Provider Enrollment Unit P. O. Box 26803 Richmond, VA 23261 888 -829 -5373 804 -270 -5105 804 -270 -7027 - Fax 29
Medicaid Programs/ Benefit Packages
Medicaid Programs Medicaid Feefor-Service • No Primary Care Physician (PCP) • No mandatory referral from the PCP. Medallion • Primary Care Physician who directs all care. • PCP referral required for all non-emergency services. 31
Medicaid Programs • FAMIS – Medicaid program for children under age 19 – First 30 days coverage provided under the FAMIS fee-for-service program – Mandatory Managed Care Organization assignment (where available) after the initial 30 days of 32 coverage
Medicaid Programs • FAMIS MOMS – For pregnant women with incomes above the Medicaid income guidelines – Managed Care Organization assignment rules same as FAMIS – Apply thru local Department of Social Services or Central Processing Unit – Baby is not covered until application submitted and approved 33
Medallion II MCO ID Cards • Issued by the Managed Care Organizations • Medicaid member will have both MCO and Medicaid cards • Eligibility verification is a REQUIREMENT • Each verification option will give the MCO enrollment information if applicable 34
Medallion II MCO ID Cards • The Anthem card for Medicaid members indicates Anthem Health Keepers Plus (PLUS identifies the Medicaid plan). • The Optima Card for Medicaid members indicates Optima Family Care (FAMILY CARE identifies the Medicaid plan). • Virginia Premier - anyone presenting a VA Premier Card is a Medicaid client. 35
Medallion II MCO ID Cards • Care. Net identifies the Southern Health Services card for Medicaid members. • AMERIGROUP of Virginia is for Medicaid members. 36
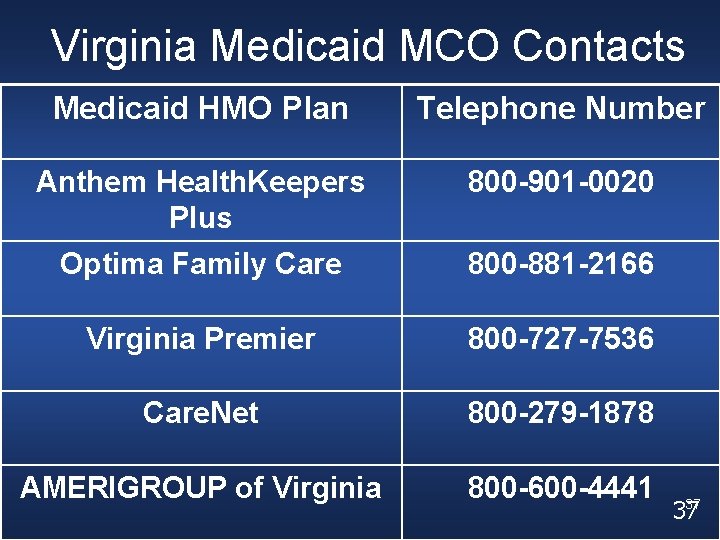
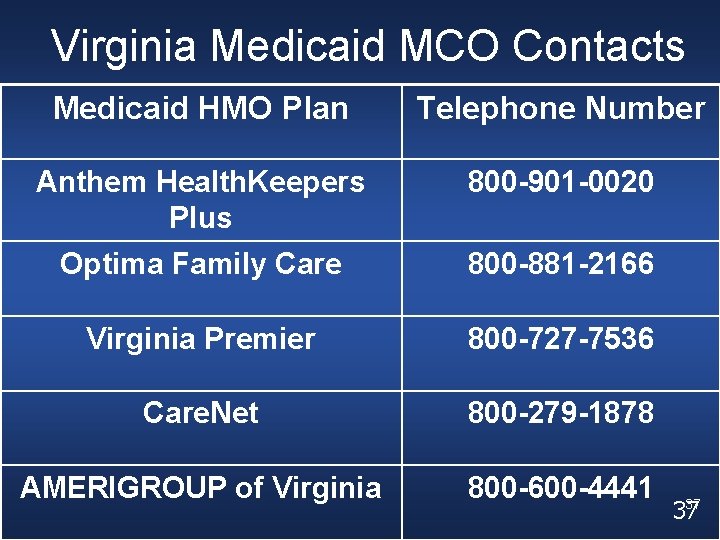
Virginia Medicaid MCO Contacts Medicaid HMO Plan Telephone Number Anthem Health. Keepers Plus 800 -901 -0020 Optima Family Care 800 -881 -2166 Virginia Premier 800 -727 -7536 Care. Net 800 -279 -1878 AMERIGROUP of Virginia 800 -600 -4441 37 37
Member Choice - MCO Selection (Areas Where MCO is Available) • Member will be enrolled in Medicaid fee-forservice plan for the first 30 days. • Member will then have 90 days to select an MCO plan. • During the 90 day period, a member can select a new MCO for the upcoming month as long as the request is received by the 15 th of the current month. • At the end of the 90 day period, the member will be enrolled in the chosen MCO until the next open enrollment period. 38
Managed Care Helpline 1 -800 -643 -2273 TDD# 1 -800 -817 -6608 Monday – Friday 8: 30 a. m. – 6: 00 p. m. (Translation Services Available) 39
Client Medical Management- CMM • Mandatory Primary Care Physician (PCP) and Pharmacist who directs all care • Responsibilities: – coordinating routine medical care – making referrals to specialists as necessary – arrange 24 hour coverage when not available – explain to members all procedures to follow when office is closed or there is an urgent or emergency situation 40
Client Medical Management - CMM • Services received by a CMM member not provided by the PCP will be reimbursed only: – in a medical emergency/delay in treatment may cause death, lasting injury or harm – on written referral from PCP using the Practitioner Referral Form (DMAS-70), includes covering physicians – covered services excluded from CMM program requirements • If not a medical emergency or no referral form is attached, hospital emergency room CMM claims will be denied, not paid at a reduced rate • CMM patient can be billed for these non 41 41 emergency services
Aliens • Section 1903 v of the Social Security Act requires Medicaid to cover emergency services for specified aliens when the services are provided in an emergency room or inpatient hospital setting. • Hospital outpatient follow-up visits or physician office visits are not included in the covered services. 42
Aliens • Emergency medical treatment only • Eligibility requests should be sent to the local DSS • Emergency Medical Certification form required for claim submission 43
Aliens Covered services must meet emergency treatment criteria and are limited to : • Emergency room care • Physician services • Inpatient hospitalization not to exceed limits established for other Medicaid recipients • Ambulance service to the emergency room • Inpatient and outpatient pharmacy services 44 related to the emergency treatment
Early Periodic Screening Diagnosis and Treatment - EPSDT • The EPSDT Program is Medicaid’s comprehensive and preventative child health program for individuals under the age of 21. • Federal law requires a broad range of outreach, coordination, and health services under EPSDT distinct from general state Medicaid requirements. • The goal of EPSDT is to identify and treat health problems as early as possible. • EPSDT provides examination and treatment at 45 no cost to the individual.
Early Periodic Screening Diagnosis and Treatment - EPSDT • For individuals under age 21, EPSDT must include the services listed below • Screening services, which encompass all of the following services: – Comprehensive health and developmental history – Comprehensive unclothed physical exam – Appropriate immunizations according to age and health history – Laboratory tests (including blood lead screening) 46 – Health education
Qualified Medicare Beneficiaries. QMB • Eligible only for Medicaid payment of Medicare premiums, deductibles, coinsurance and Medicare Advantage Plan copays. • Medicaid will consider the Medicare deductibles, coinsurance and copays for benefits. • If Medicare does not cover the service, the service cannot be billed to Medicaid. 47
Qualified Medicare Beneficiaries. QMB Extended • This group is eligible for Medicaid coverage of premiums, deductibles, coinsurance and Medicare Advantage Plans copays, plus all other Medicaidcovered services. • Medicaid will consider the Medicare deductibles, coinsurance and copays for benefits. • Members are also eligible for all Medicaid covered services. 48
Medicare Advantage Plans • VA Medicaid handles and processes Medicare Advantage Plans the same way as traditional Medicare. • DMAS does not process the Medicare Advantage Plans as Third Party Liability (TPL) • Advantage Plan deductible, copay or coinsurance amounts submitted, will be considered by VA Medicaid for payment 49 •
Special Low-Income Beneficiaries- SLMB • This group is only eligible for Medicaid coverage of the Medicare Part B premium only. • The member will have a Medicaid number, but will not received a Medicaid card. • Medicaid will not cover any medical services for this member. 50
Plan First • Medicaid fee-for-service family planning waiver program • Men and women ages 19 years and older may be eligible • Participant income must be less than or equal to 133% of federal poverty level • Must meet citizenship and identity requirements 51
Plan First • Plan First includes coverage of those services necessary to prevent or delay a pregnancy • Family planning does not include counseling about, recommendations for or performance of abortions, hysterectomies or procedures performed for medical reasons such as the removal of intrauterine devices due 52 to infections.
Plan First • Not eligible for the waiver: – Individuals who have major medical insurance – Individuals who are eligible for full Medicaid benefits coverage – Individuals who have had a sterilization procedure 53
Plan First- Covered Services • Plan First covers routine and periodic family planning office visits and related services. • Medicaid will only reimburse approved procedure codes and the code must be accompanied with a V 25 category (family planning) as a primary diagnosis on the claim. • Please review the Plan First manual, 54 Chapter IV for codes.
Spend Down • Medicaid applicants whose income is over the Medicaid limit, the applicant may become eligible for a limited period of Medicaid coverage if all other eligibility factors are met. • This process is called a “spend-down”. • The applicant’s medical expenses must equal or exceed the difference between his or her income and the Medicaid income limit. 55
Spend Down • If the allowable expenses of the applicant equal this spend-down amount before the end of a budget period (six months for noninstitutionalized individuals or a one month period for institutionalized individuals), the applicant may receive a limited period of Medicaid coverage which will stop at the end of the budget period. • Eligibility must be re-determined in order to establish eligibility in subsequent budget 56 periods.
Medicaid Waiver • There are key requirements with which a state’s Medicaid program must comply. • These basic requirements govern Medicaid programs nationwide. – State must make services available to individuals on a comparable basis. – State must guarantee members freedom of choice in selecting service providers when obtaining Medicaid services. – State must make Medicaid services available statewide and provide that individuals have ready access to them. 57
Medicaid Waiver • In some cases the states may request waivers of some of these requirements. • Medicaid home and community-based service waiver programs operate under these rules. • The waiver allows Medicaid to pay for additional services not covered by traditional Medicaid. • The state has the ability to decide who gets funded for what service (criteria for eligibility 58 and coverage).
VA Medicaid Waivers • Alzheimer’s Assisted Living Waiver • Assisted Technology and Environmental Modifications • Elderly or Disabled With Consumer Direction • HIV/AIDS • Individual and Family Developmental Supports (IFDDS) • Intellectual Disabilities/Mental Retardation (ID/MR) • Technology Assisted (Tech) 59
Temporary Detention Order • The General Assembly directed DMAS to process all requests for payment of services rendered as a request of Civil/Criminal Mental Temporary Detention Orders (TDO) effective July 1, 1995. • Any magistrate may, within the specified guidelines, issue a temporary detention. • A law enforcement officer executes Temporary Detention Orders. • Employee of the community services board or its designee shall determine the facility of 60 temporary detention for all individuals.
Temporary Detention Order • The duration of the temporary detention shall not exceed 48 hours prior to a hearing. • If the forty-eight hour period herein specified terminated on a Saturday or Sunday, or a legal holiday, such person shall be detained until the next day which is not a Saturday, Sunday or legal holiday, but in no event may be detained longer than 96 hours. 61
Temporary Detention Order • Hospitals and physicians must submit claims to DMAS as the result of issuance by a court. • DMAS will accept only the original claim forms. • All TDO submissions must have the TDO form attached to the claim with the pre-printed case identification number. • Failure to provide the TDO form will result in claims being returned to the provider for incomplete information. • The Execution section on the TDO form must be signed by the law enforcement officer and dated to 62 be valid. 62
Temporary Detention Order • Processing of TDO claims includes both Medicaid-eligible and non-Medicaid eligible patients. • TDO is the payer of last resort and attempts must always be made to first bill the primary carrier , including Medicaid, prior to billing TDO. • Each claim will be researched for coverage by another resource. • If the patient has other resources, the claim will be returned to the provider. • The returned claim will have a letter attached, advising the provider to bill primary payer. 63
Fiscal Agent Transition Updates and Changes
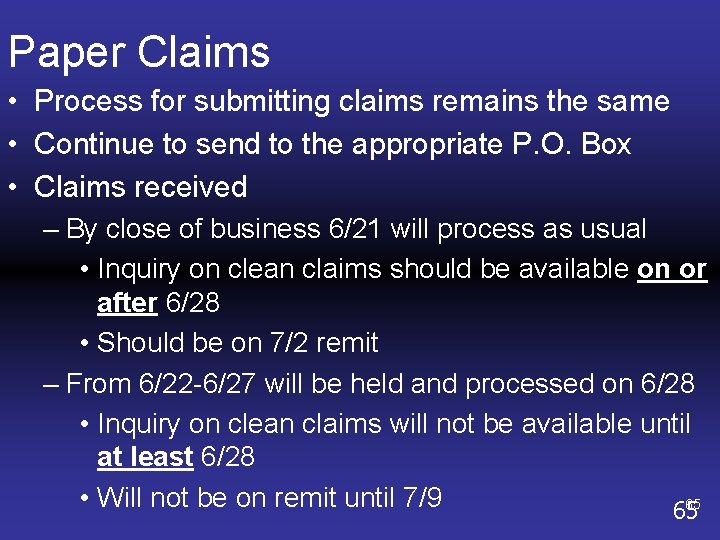
Paper Claims • Process for submitting claims remains the same • Continue to send to the appropriate P. O. Box • Claims received – By close of business 6/21 will process as usual • Inquiry on clean claims should be available on or after 6/28 • Should be on 7/2 remit – From 6/22 -6/27 will be held and processed on 6/28 • Inquiry on clean claims will not be available until at least 6/28 • Will not be on remit until 7/9 65 65
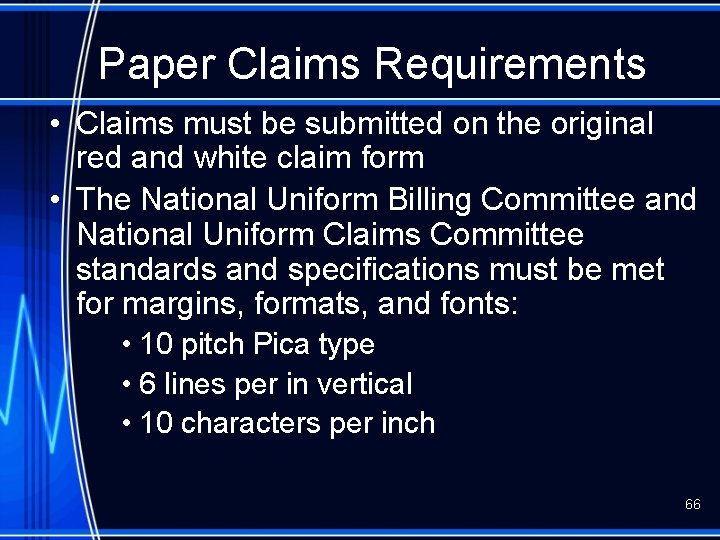
Paper Claims Requirements • Claims must be submitted on the original red and white claim form • The National Uniform Billing Committee and National Uniform Claims Committee standards and specifications must be met for margins, formats, and fonts: • 10 pitch Pica type • 6 lines per in vertical • 10 characters per inch 66
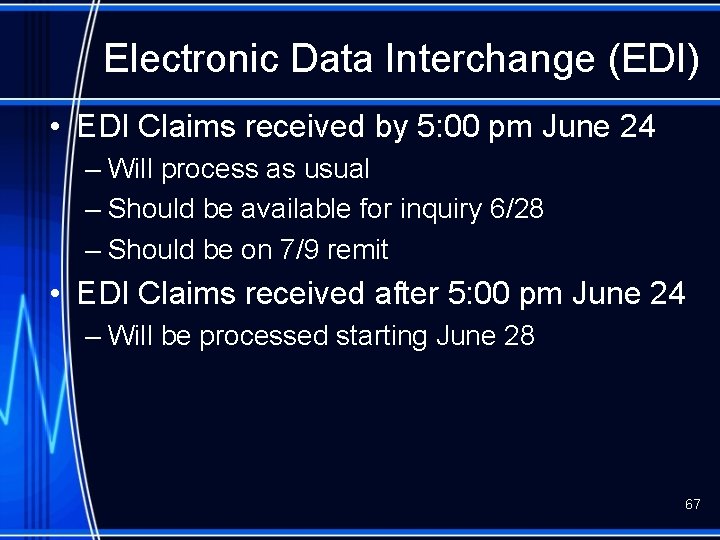
Electronic Data Interchange (EDI) • EDI Claims received by 5: 00 pm June 24 – Will process as usual – Should be available for inquiry 6/28 – Should be on 7/9 remit • EDI Claims received after 5: 00 pm June 24 – Will be processed starting June 28 67
Electronic Data Interchange (EDI) • Requirements – You or your designee must have established and been given a • New user ID • New password • New File Transfer Protocol (FTP) 68
Trader Partner Testing • Communications validation testing is being conducted – Clearinghouses – Service centers – Software vendors • Letter sent to all trading partners containing information regarding testing of EDI batch processing 69
Trader Partner Testing • If you or your designee has not received this letter – email Virginia. EDISupport@acs-inc. com – four position submitter ID – contact information 70
Hospital Billing Guidelines 71
MAIL CMS-1450 FORMS TO: DEPARTMENT OF MEDICAL ASSISTANCE SERVICES Facility P. O. Box 27443 Richmond, Virginia 23261 -7443 72
TIMELY FILING • ALL CLAIMS MUST BE SUBMITTED AND PROCESSED WITHIN ONE YEAR FROM THE DATE OF SERVICE • EXCEPTIONS – Retroactive/Delayed Eligibility – Denied Claims • NO EXCEPTIONS – Accidents – Other Primary Insurance 73
TIMELY FILING • Submit claims with documentation attached (to the back of claim) explaining the reason for delayed submission 74
CMS-1450 CLAIM FORM: Use ONLY the ORIGINAL RED & WHITE Invoice Photocopies are not Acceptable Computer generated claims must match NUBC 75 uniform standards 75
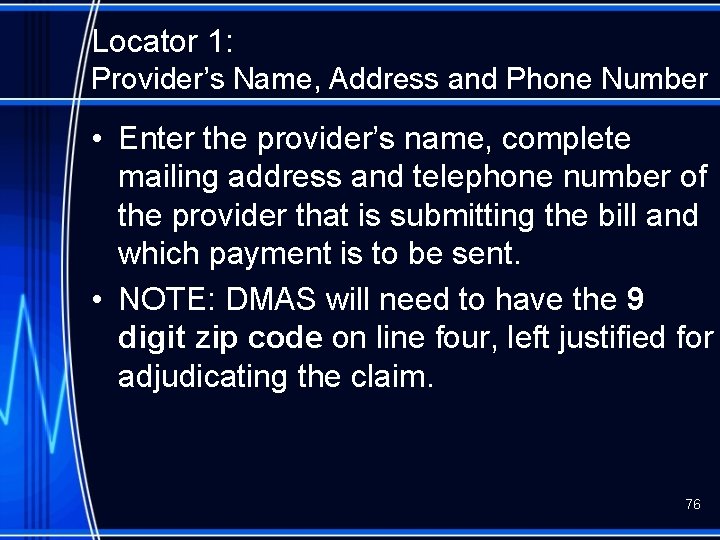
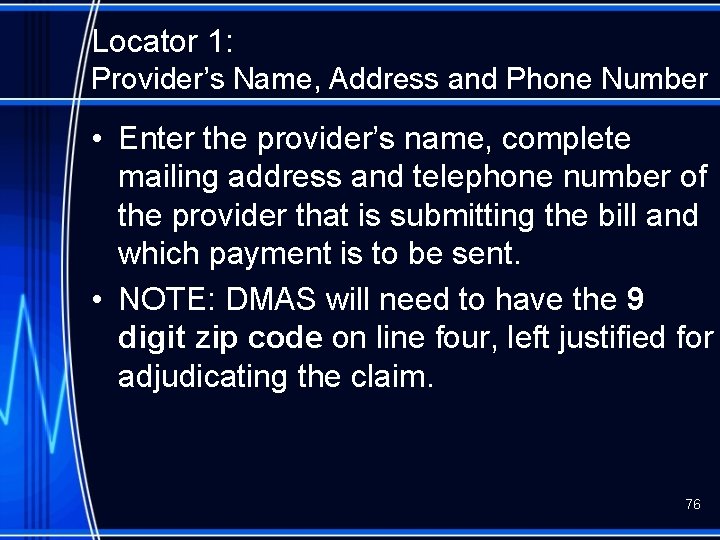
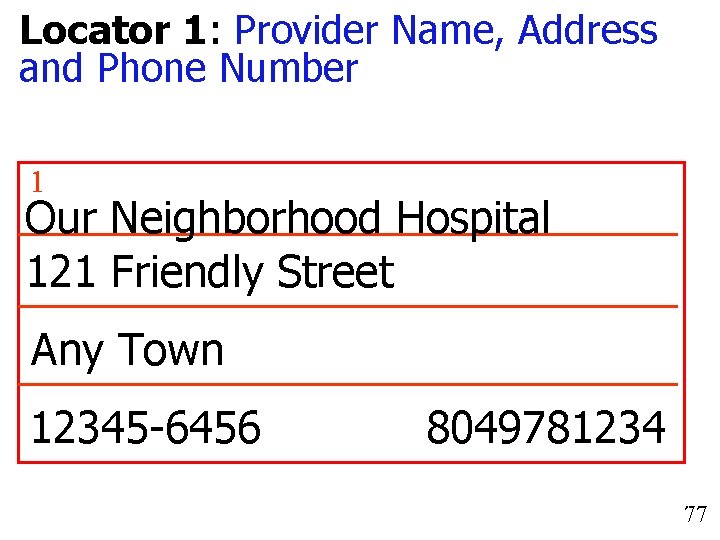
Locator 1: Provider’s Name, Address and Phone Number • Enter the provider’s name, complete mailing address and telephone number of the provider that is submitting the bill and which payment is to be sent. • NOTE: DMAS will need to have the 9 digit zip code on line four, left justified for adjudicating the claim. 76
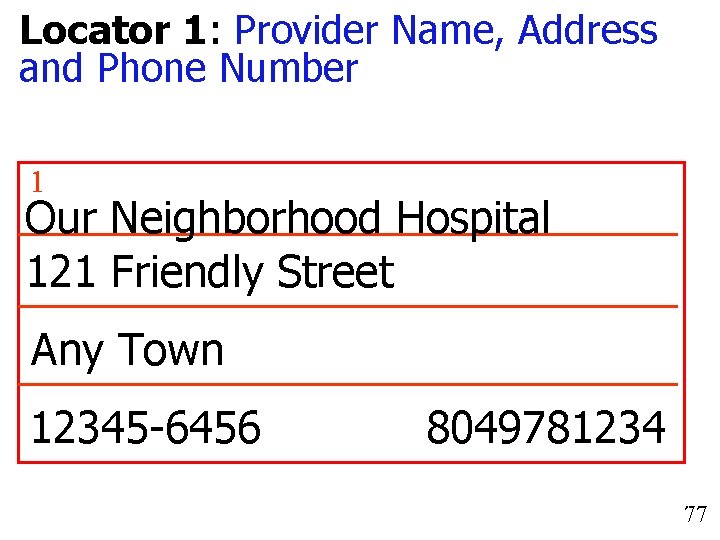
Locator 1: Provider Name, Address and Phone Number 1 Our Neighborhood Hospital 121 Friendly Street Any Town 12345 -6456 VA 8049781234 77 77
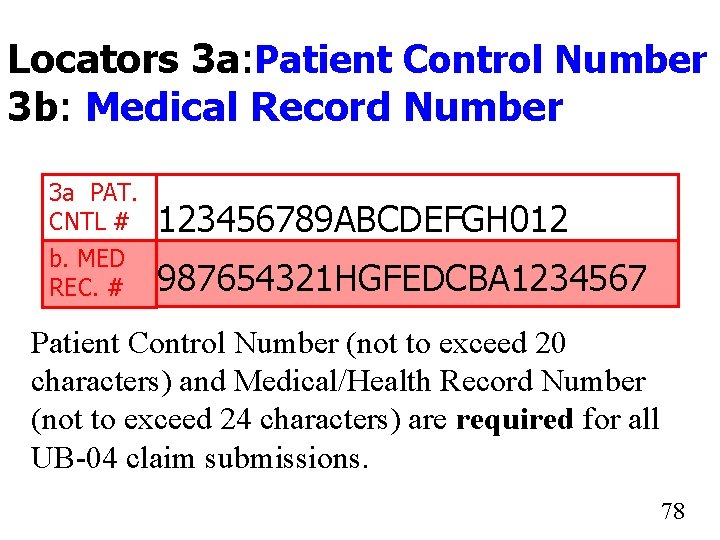
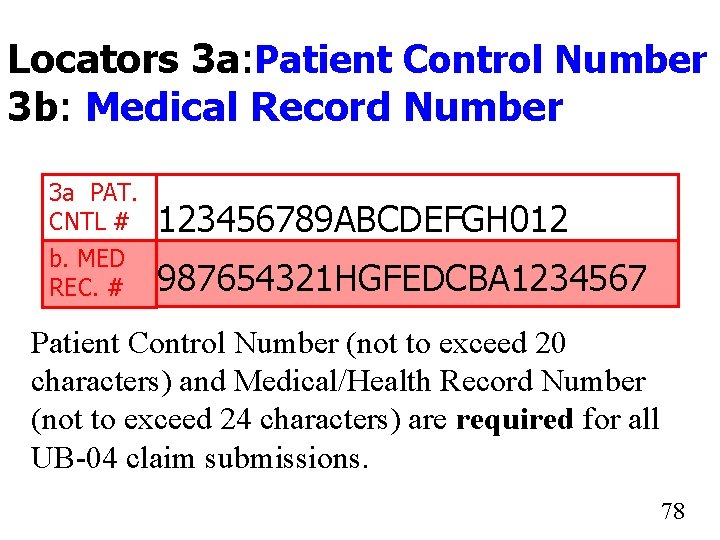
Locators 3 a: Patient Control Number 3 b: Medical Record Number 3 a PAT. CNTL # 123456789 ABCDEFGH 012 b. MED REC. # 987654321 HGFEDCBA 1234567 Patient Control Number (not to exceed 20 characters) and Medical/Health Record Number (not to exceed 24 characters) are required for all UB-04 claim submissions. 7878
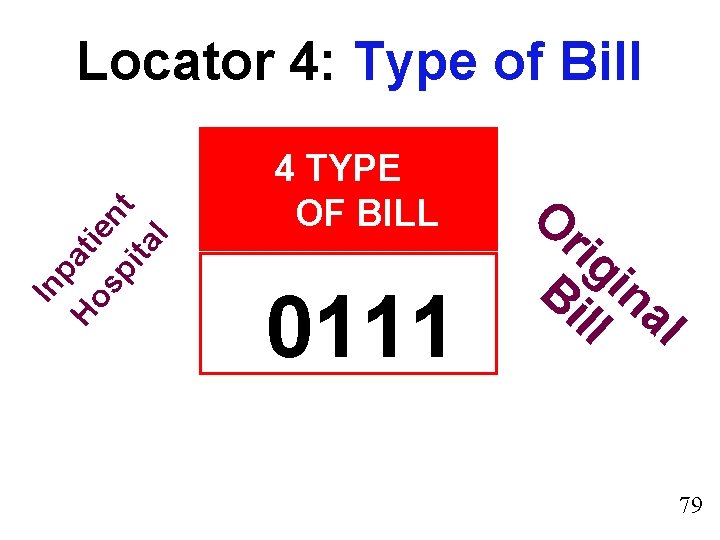
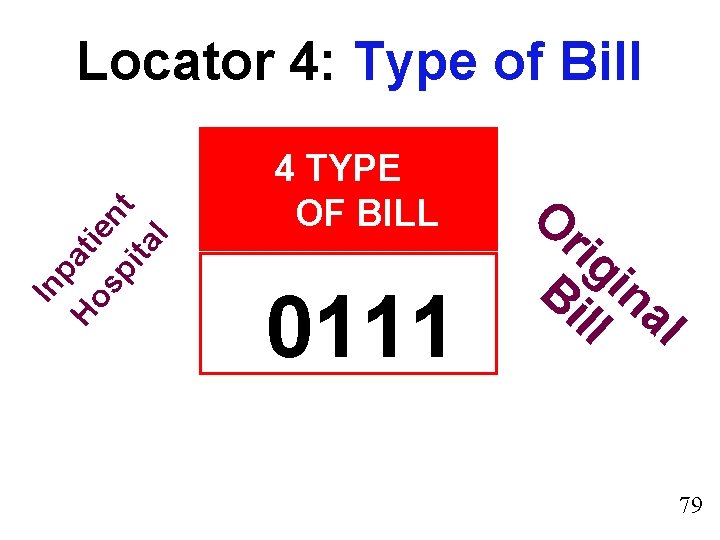
In pa Ho ti sp ent ita l Locator 4: Type of Bill 4 TYPE OF BILL 0111 O rig Bi in ll al 79 79
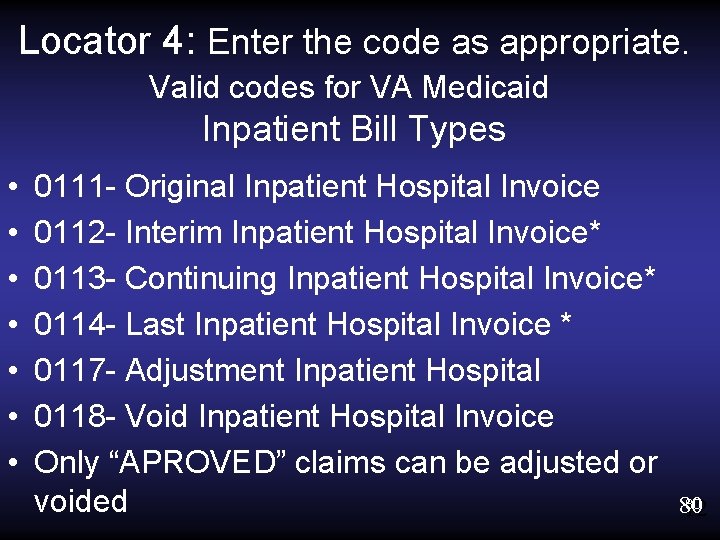
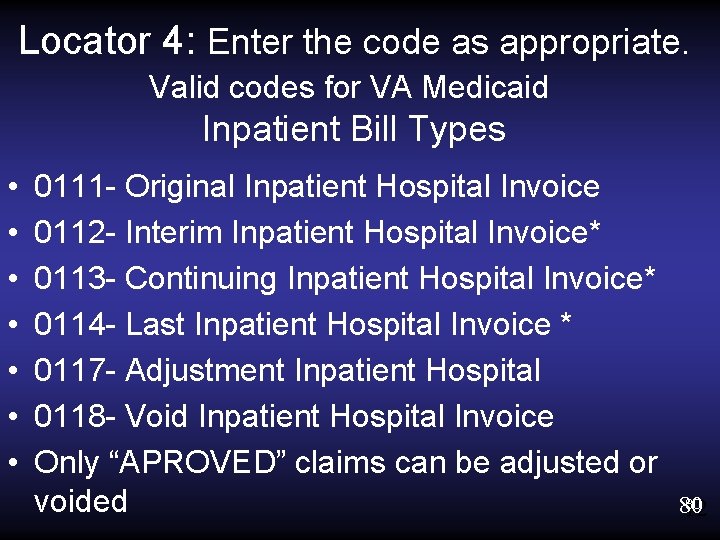
Locator 4: Enter the code as appropriate. Valid codes for VA Medicaid Inpatient Bill Types • • 0111 - Original Inpatient Hospital Invoice 0112 - Interim Inpatient Hospital Invoice* 0113 - Continuing Inpatient Hospital Invoice* 0114 - Last Inpatient Hospital Invoice * 0117 - Adjustment Inpatient Hospital 0118 - Void Inpatient Hospital Invoice Only “APROVED” claims can be adjusted or voided 80 80 12
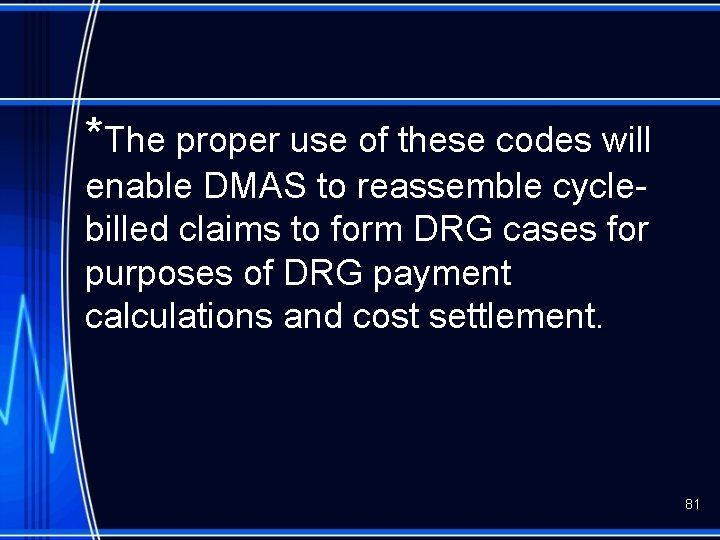
*The proper use of these codes will enable DMAS to reassemble cyclebilled claims to form DRG cases for purposes of DRG payment calculations and cost settlement. 81
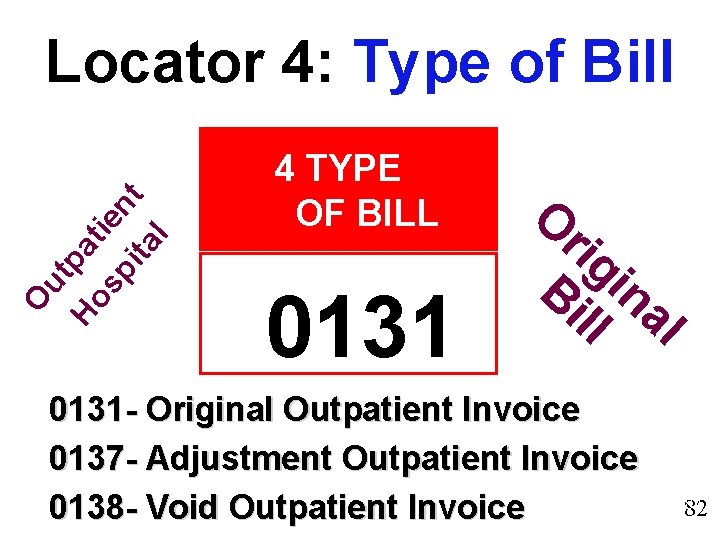
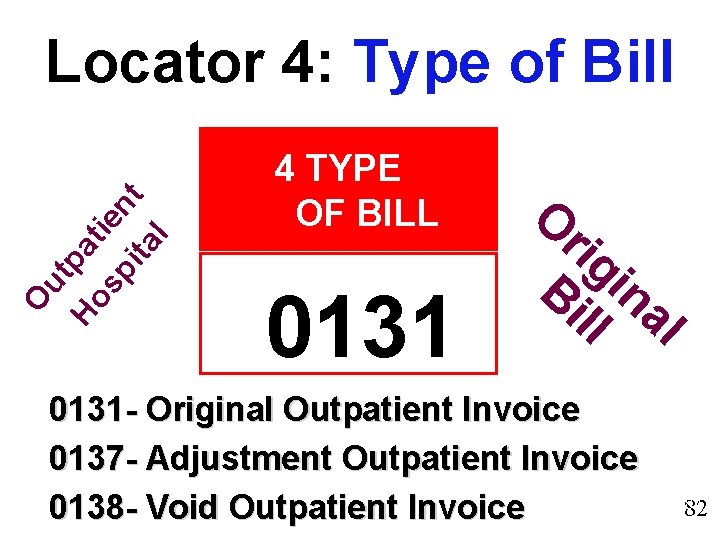
O ut Ho pat sp ien ita t l Locator 4: Type of Bill 4 TYPE OF BILL 0131 O rig Bi in ll al 0131 - Original Outpatient Invoice 0137 - Adjustment Outpatient Invoice 0138 - Void Outpatient Invoice 82 82
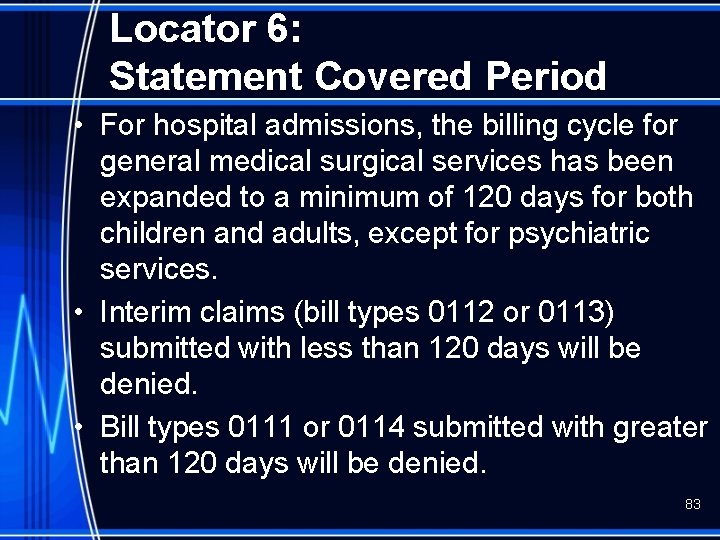
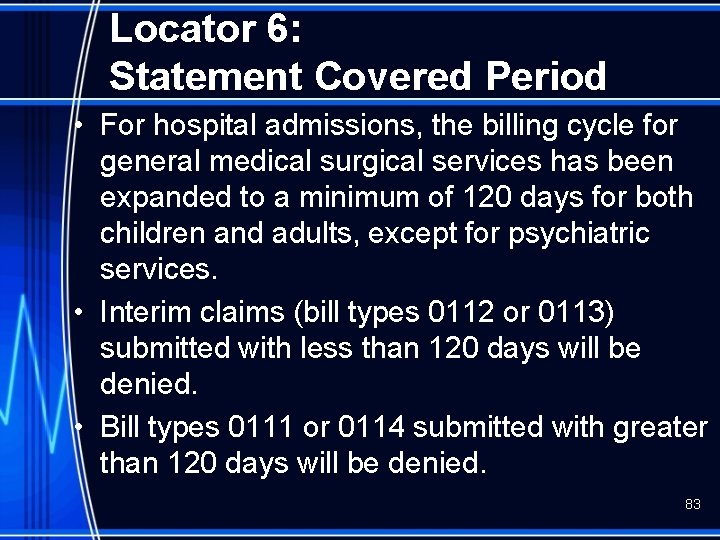
Locator 6: Statement Covered Period • For hospital admissions, the billing cycle for general medical surgical services has been expanded to a minimum of 120 days for both children and adults, except for psychiatric services. • Interim claims (bill types 0112 or 0113) submitted with less than 120 days will be denied. • Bill types 0111 or 0114 submitted with greater than 120 days will be denied. 83
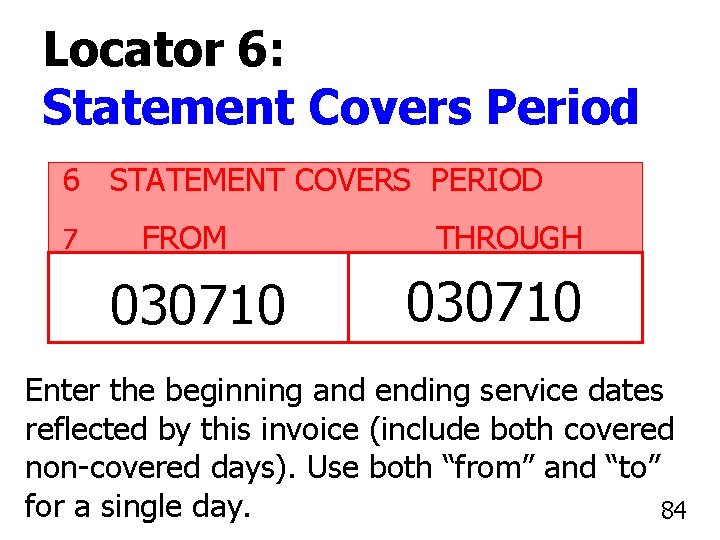
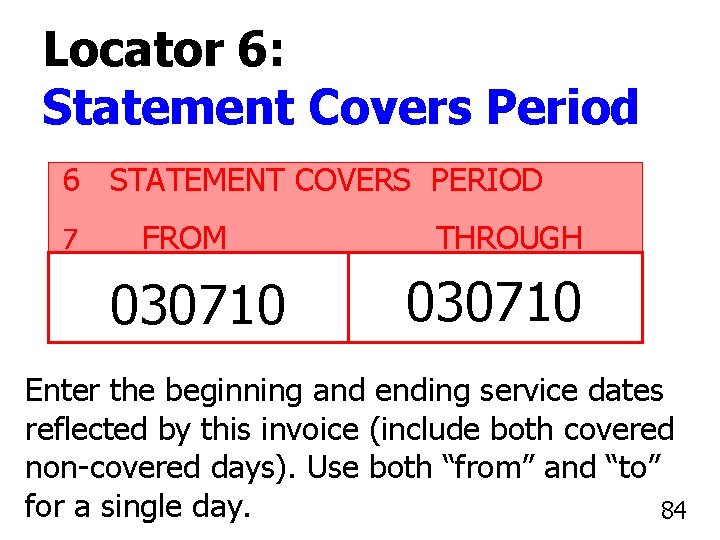
Locator 6: Statement Covers Period 6 STATEMENT COVERS PERIOD 7 FROM 030710 THROUGH 030710 Enter the beginning and ending service dates reflected by this invoice (include both covered non-covered days). Use both “from” and “to” for a single day. 8484
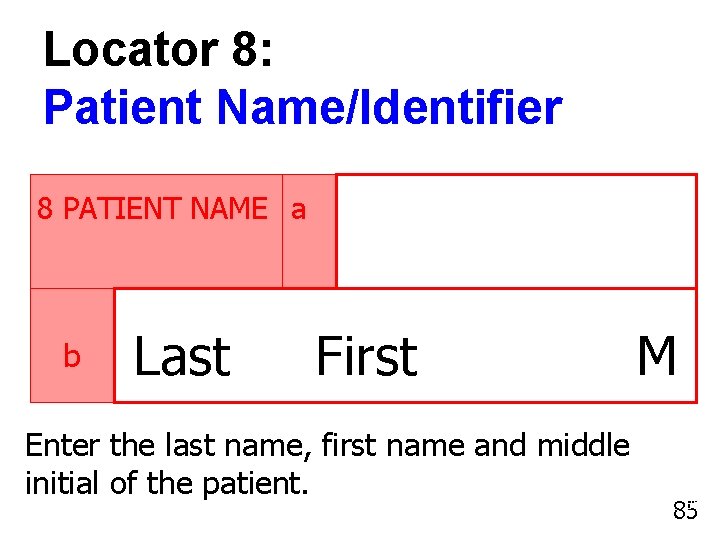
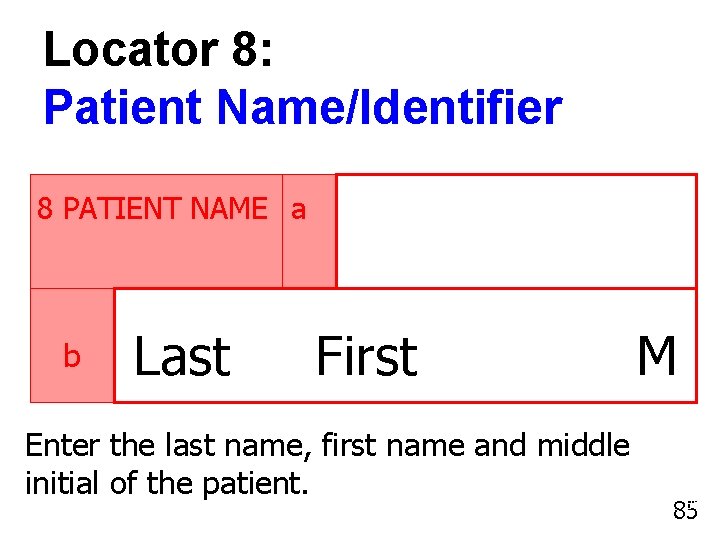
Locator 8: Patient Name/Identifier 8 PATIENT NAME a b Last First Enter the last name, first name and middle initial of the patient. M 85 85
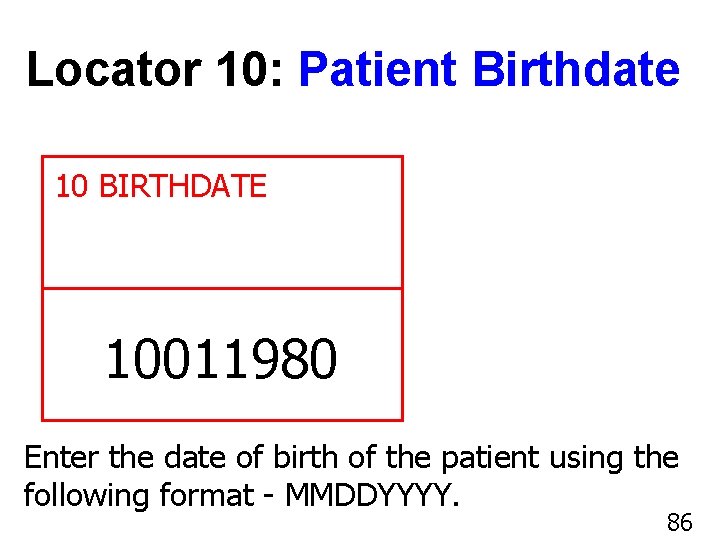
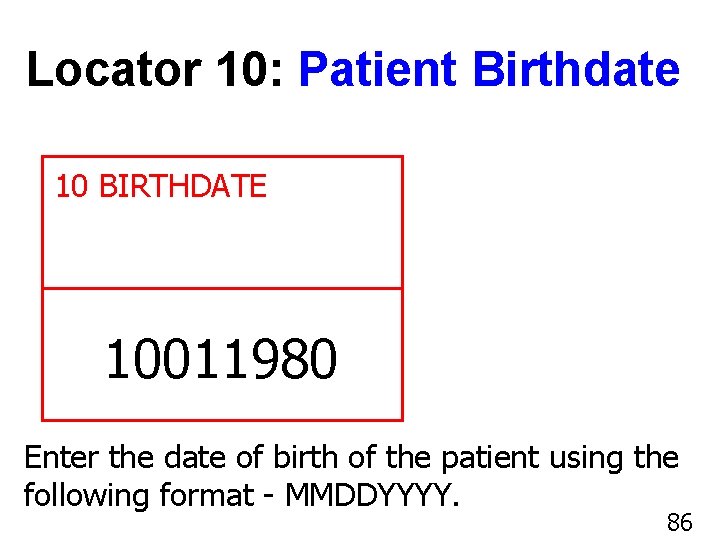
Locator 10: Patient Birthdate 10 BIRTHDATE 10011980 Enter the date of birth of the patient using the following format - MMDDYYYY. 86 86
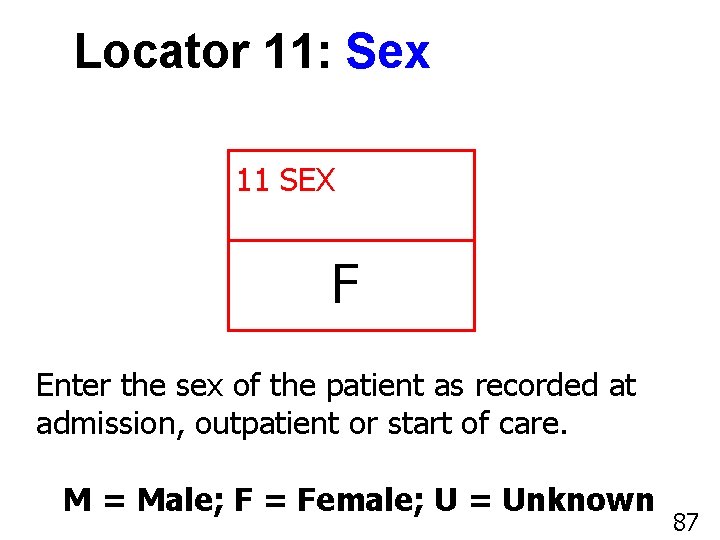
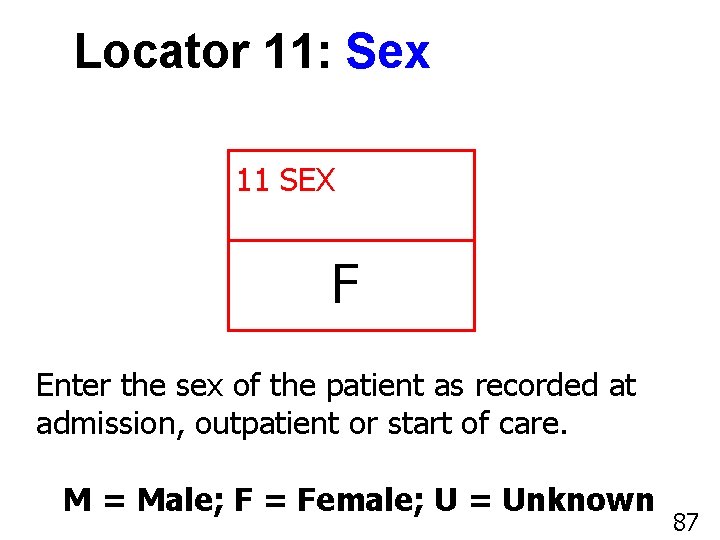
Locator 11: Sex 11 SEX F Enter the sex of the patient as recorded at admission, outpatient or start of care. M = Male; F = Female; U = Unknown 87 87
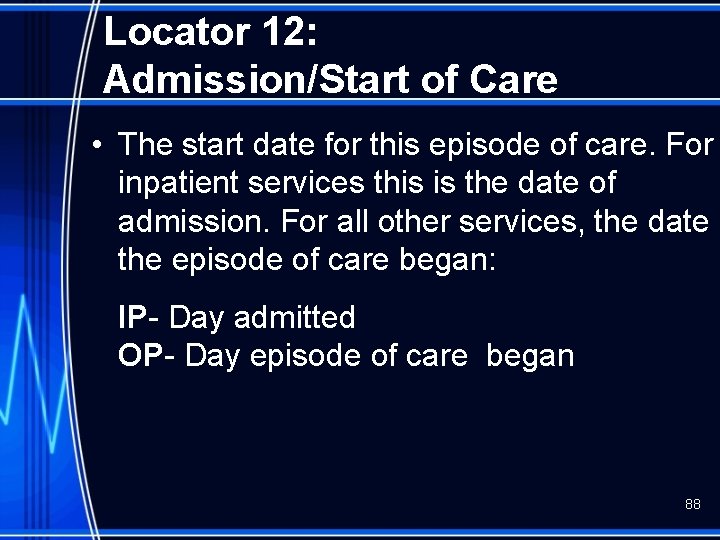
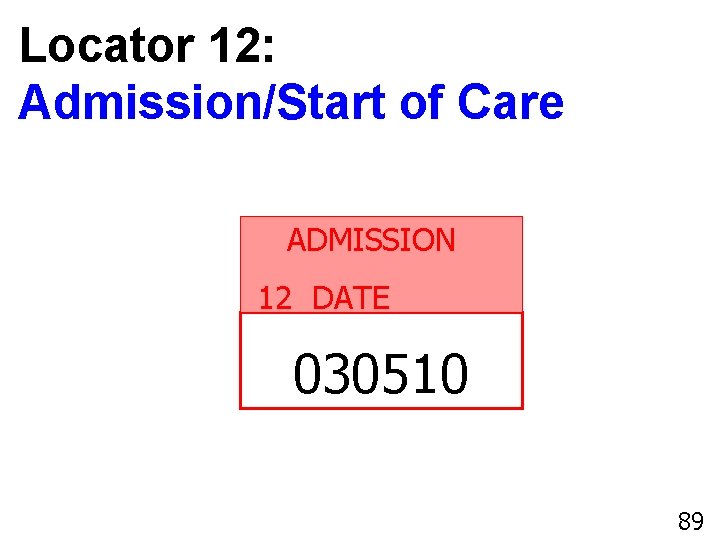
Locator 12: Admission/Start of Care • The start date for this episode of care. For inpatient services this is the date of admission. For all other services, the date the episode of care began: IP- Day admitted OP- Day episode of care began 88
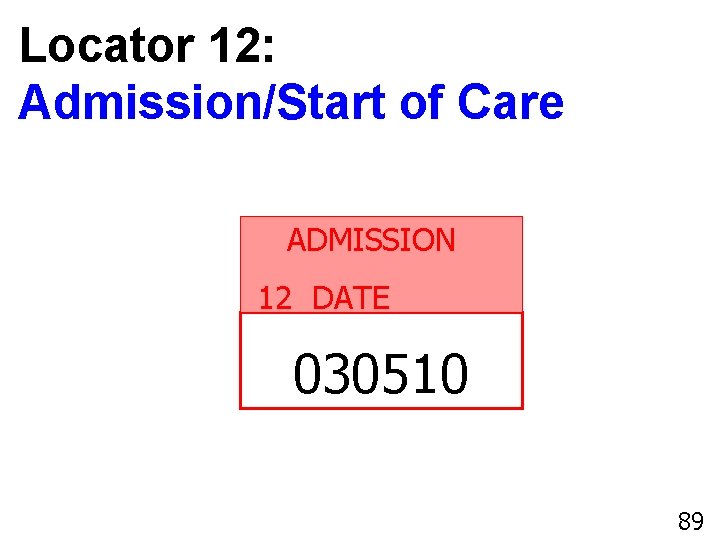
Locator 12: Admission/Start of Care ADMISSION 12 DATE 030510 89 89
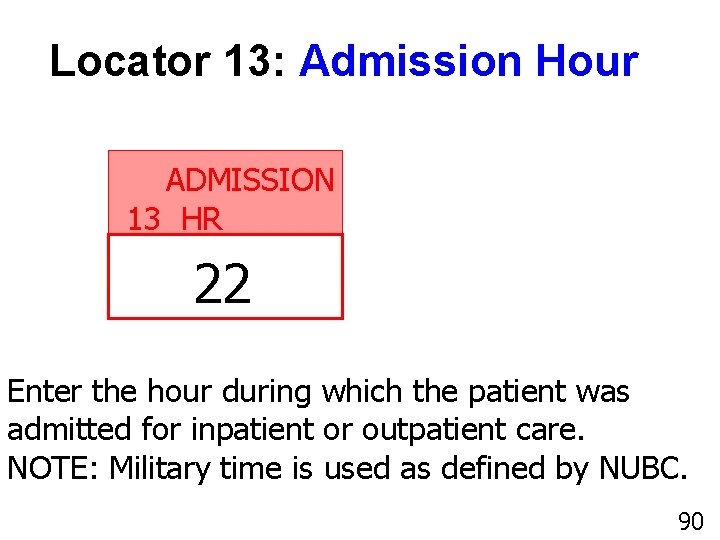
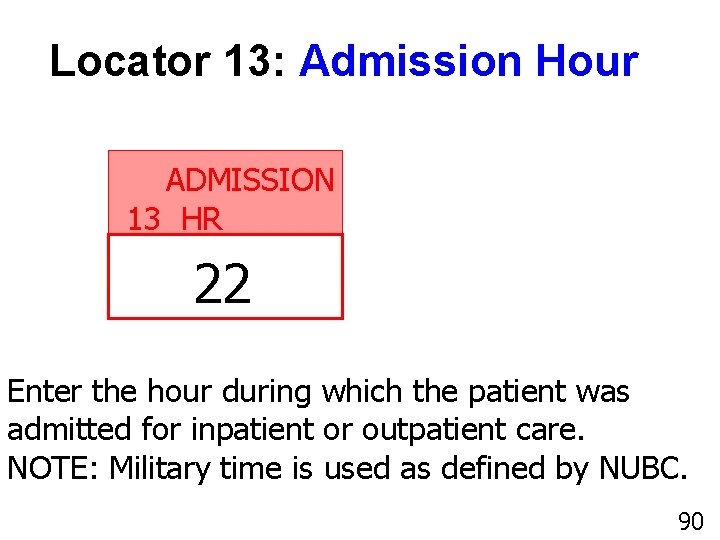
Locator 13: Admission Hour ADMISSION 13 HR 22 Enter the hour during which the patient was admitted for inpatient or outpatient care. NOTE: Military time is used as defined by NUBC. 90 90
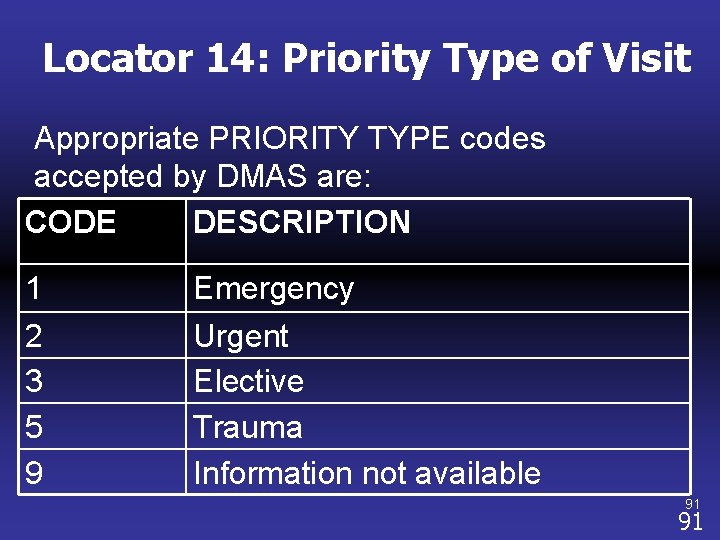
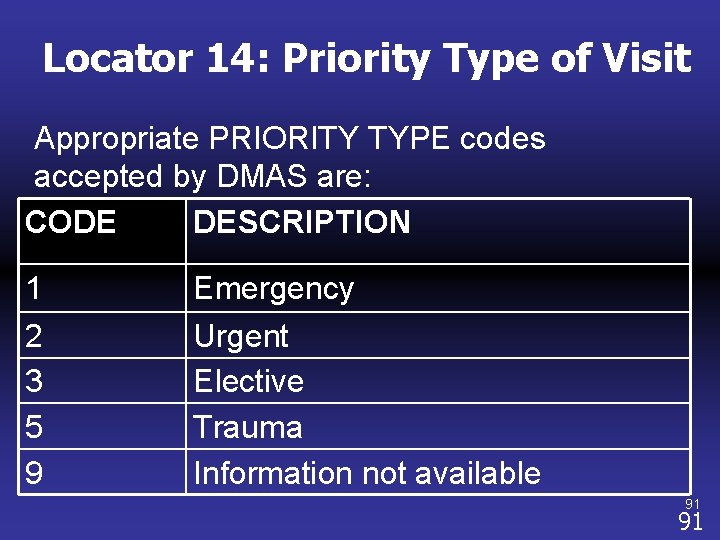
Locator 14: Priority Type of Visit Appropriate PRIORITY TYPE codes accepted by DMAS are: CODE DESCRIPTION 1 2 3 5 9 Emergency Urgent Elective Trauma Information not available 91 91
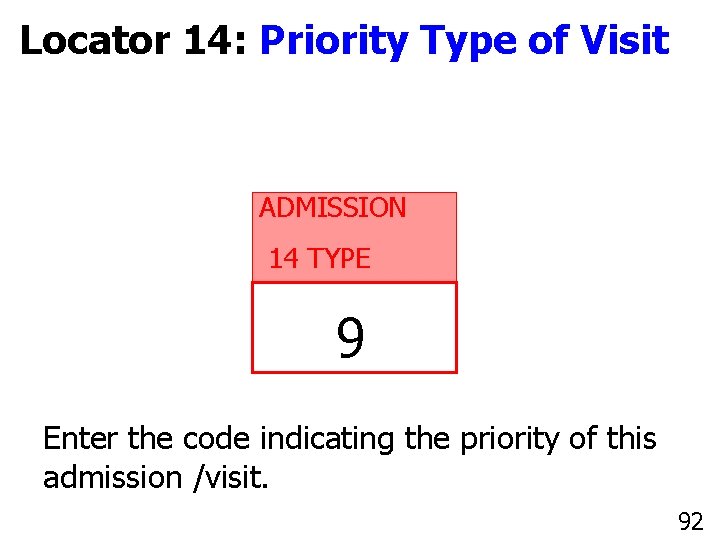
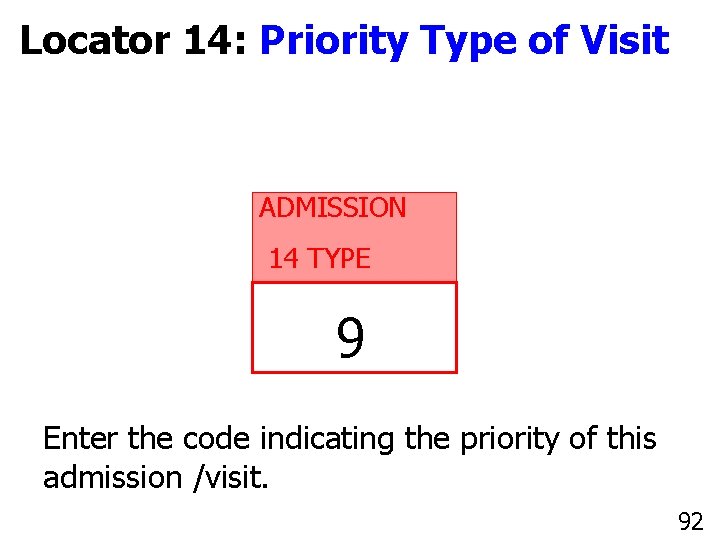
Locator 14: Priority Type of Visit ADMISSION 14 TYPE 9 Enter the code indicating the priority of this admission /visit. 92 92
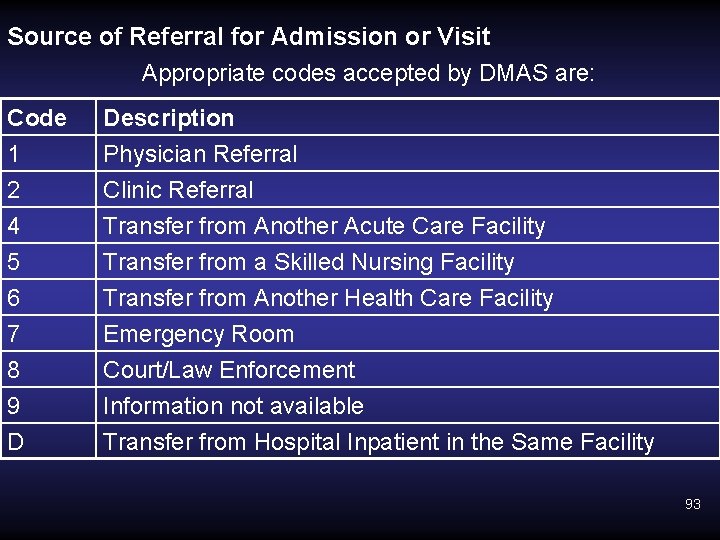
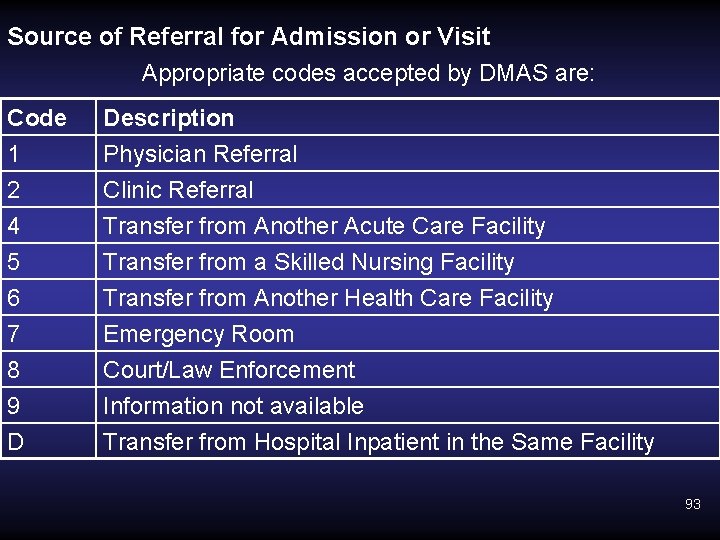
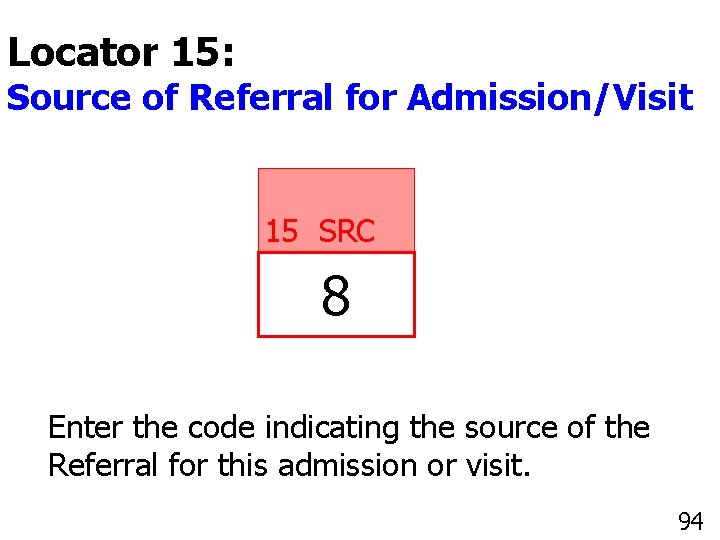
Source of Referral for Admission or Visit Appropriate codes accepted by DMAS are: Code 1 2 4 Description Physician Referral Clinic Referral Transfer from Another Acute Care Facility 5 6 7 8 9 D Transfer from a Skilled Nursing Facility Transfer from Another Health Care Facility Emergency Room Court/Law Enforcement Information not available Transfer from Hospital Inpatient in the Same Facility 93
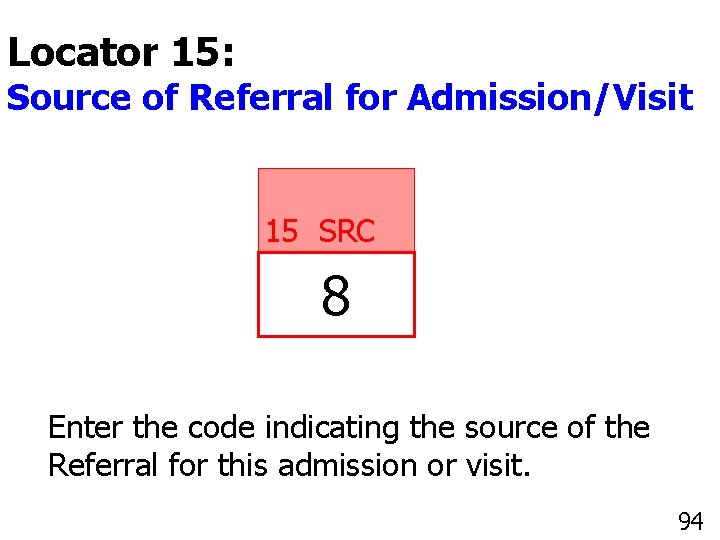
Locator 15: Source of Referral for Admission/Visit 15 SRC 8 Enter the code indicating the source of the Referral for this admission or visit. 94 94
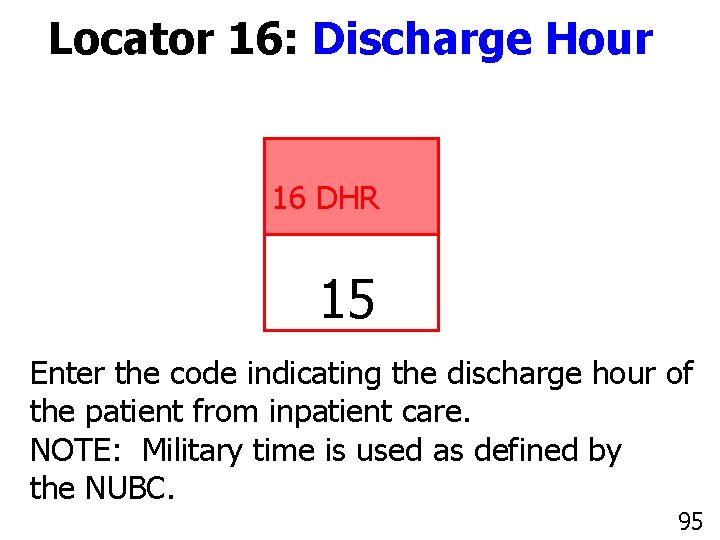
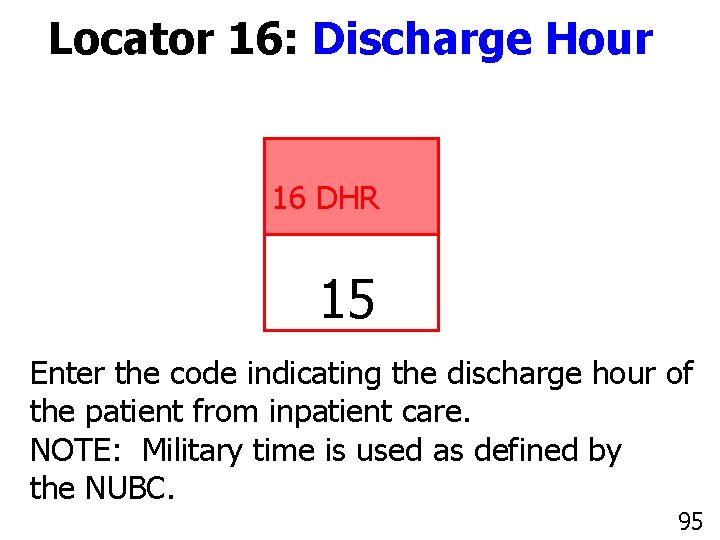
Locator 16: Discharge Hour 16 DHR 15 Enter the code indicating the discharge hour of the patient from inpatient care. NOTE: Military time is used as defined by the NUBC. 95 95
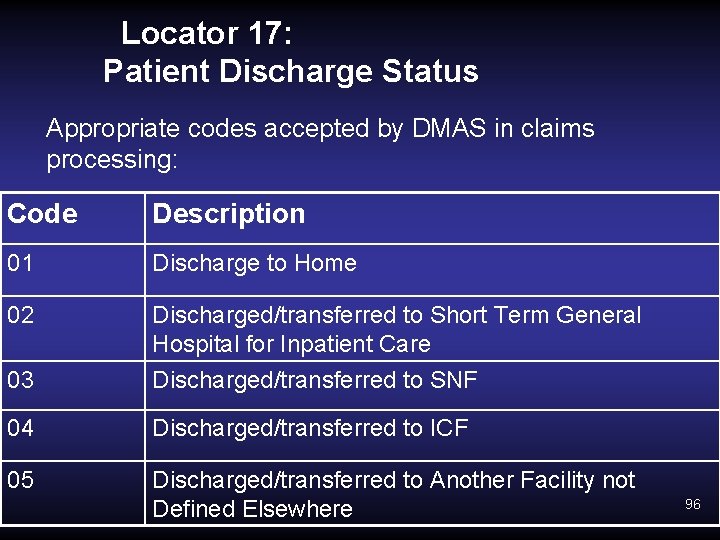
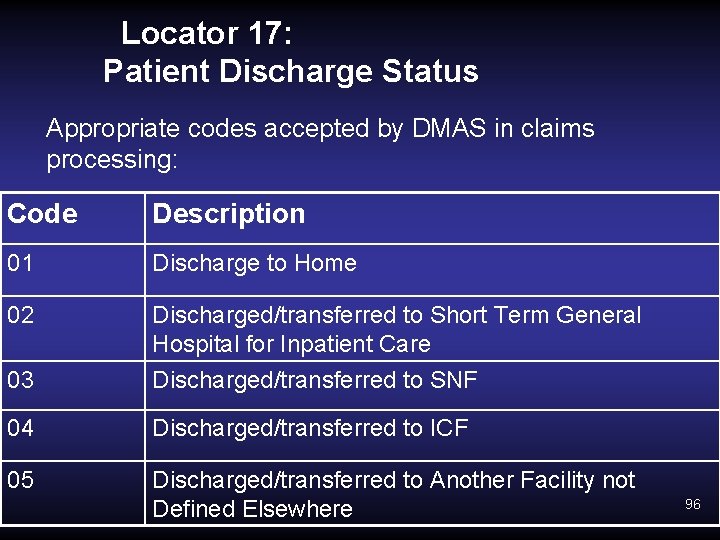
Locator 17: Patient Discharge Status Appropriate codes accepted by DMAS in claims processing: Code Description 01 Discharge to Home 02 Discharged/transferred to Short Term General Hospital for Inpatient Care 03 Discharged/transferred to SNF 04 Discharged/transferred to ICF 05 Discharged/transferred to Another Facility not Defined Elsewhere 96
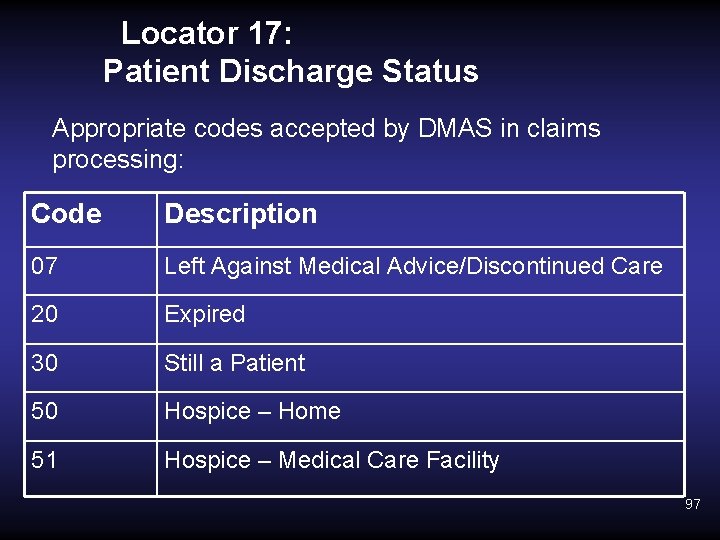
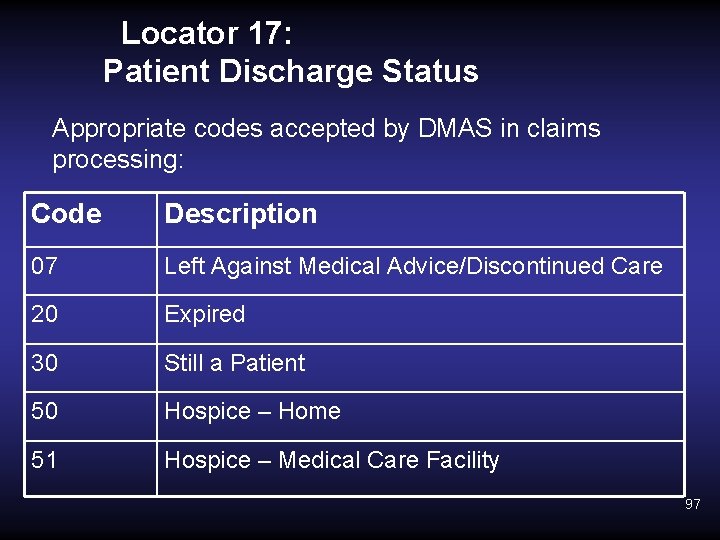
Locator 17: Patient Discharge Status Appropriate codes accepted by DMAS in claims processing: Code Description 07 Left Against Medical Advice/Discontinued Care 20 Expired 30 Still a Patient 50 Hospice – Home 51 Hospice – Medical Care Facility 97
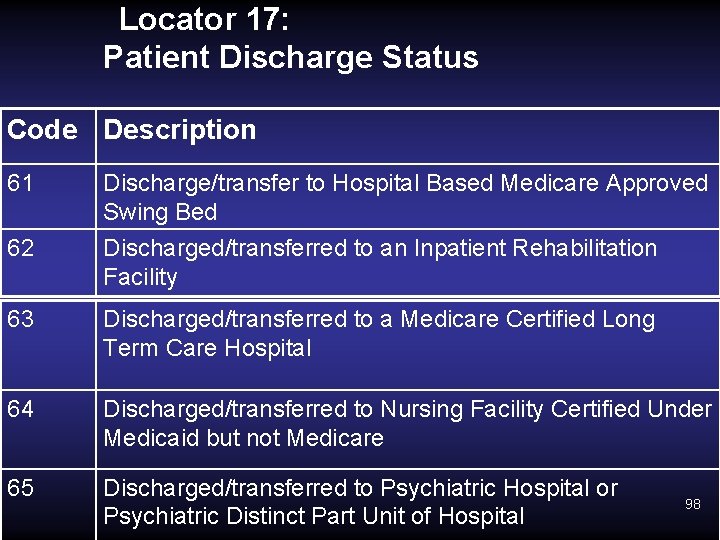
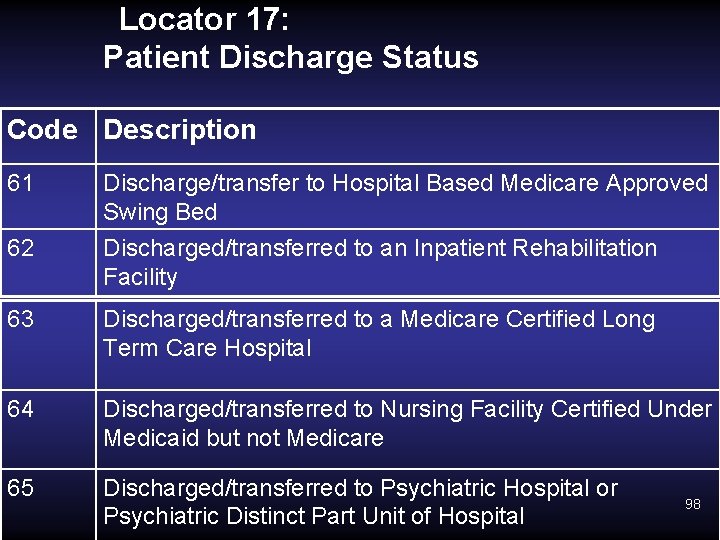
Locator 17: Patient Discharge Status Code Description 61 62 Discharge/transfer to Hospital Based Medicare Approved Swing Bed Discharged/transferred to an Inpatient Rehabilitation Facility 63 Discharged/transferred to a Medicare Certified Long Term Care Hospital 64 Discharged/transferred to Nursing Facility Certified Under Medicaid but not Medicare 65 Discharged/transferred to Psychiatric Hospital or Psychiatric Distinct Part Unit of Hospital 98
Locator 17: Patient Status Correct reporting of patient status code will facilitate quick and accurate determination of DRG reimbursement. In particular, accurate reporting of the values 01, 02, 05, and 30 will be very important in DRG methodology. 99
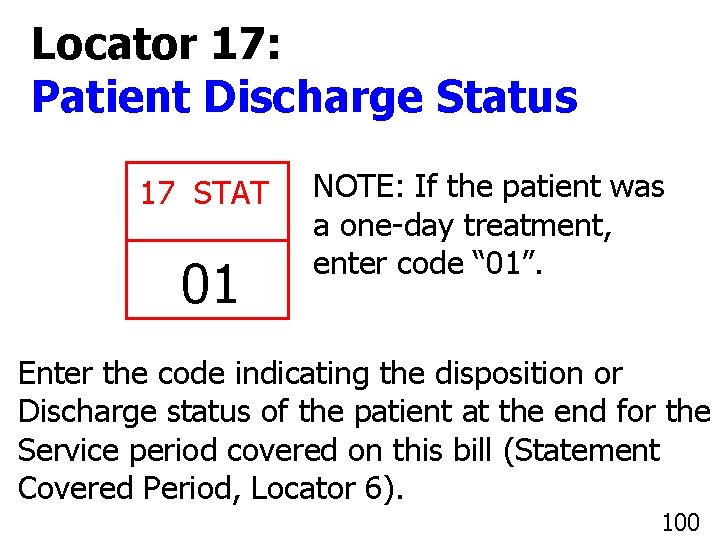
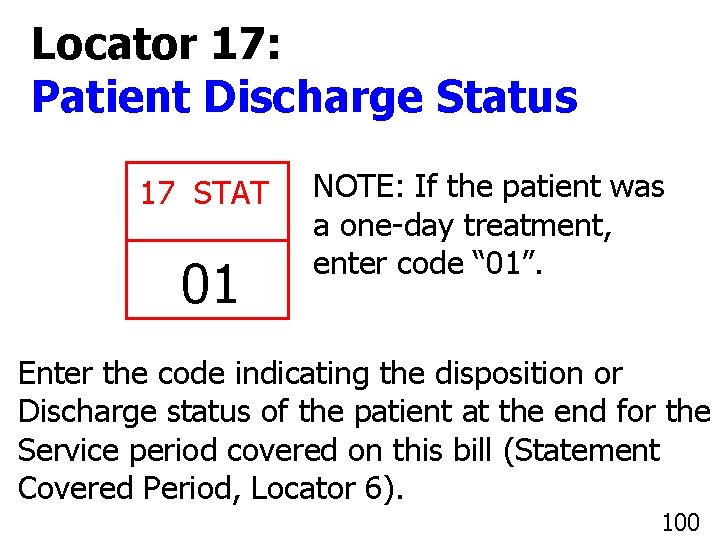
Locator 17: Patient Discharge Status 17 STAT 01 NOTE: If the patient was a one-day treatment, enter code “ 01”. Enter the code indicating the disposition or Discharge status of the patient at the end for the Service period covered on this bill (Statement Covered Period, Locator 6). 100
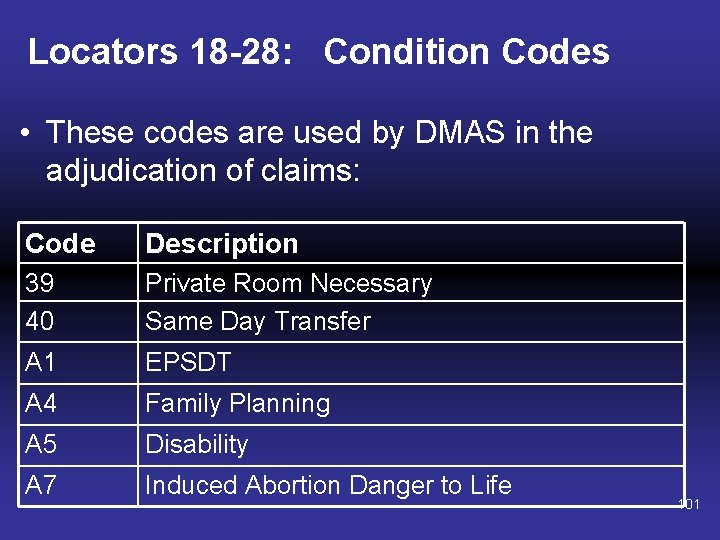
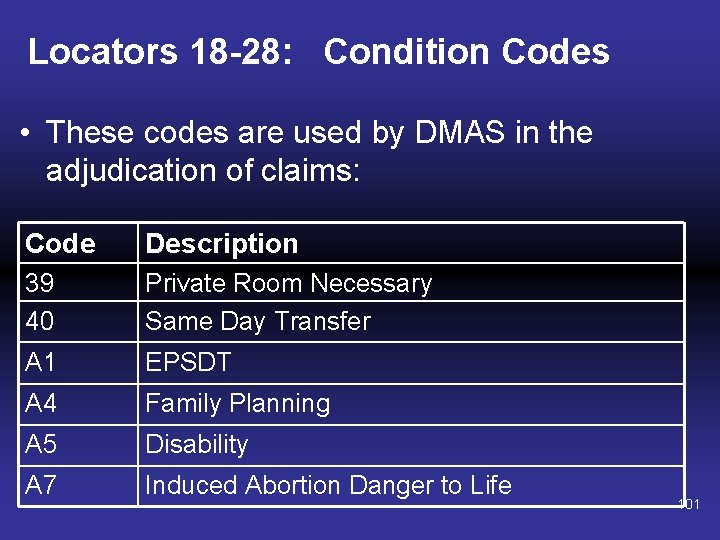
Locators 18 -28: Condition Codes • These codes are used by DMAS in the adjudication of claims: Code Description 39 40 Private Room Necessary Same Day Transfer A 1 EPSDT A 4 Family Planning A 5 Disability A 7 Induced Abortion Danger to Life 101
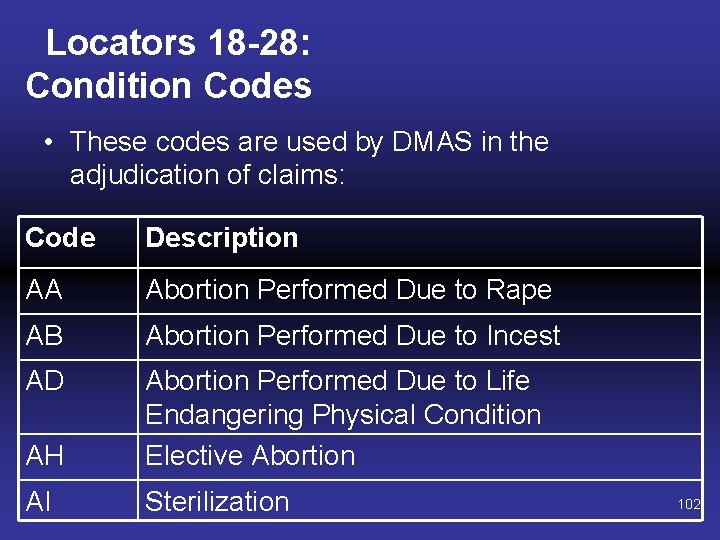
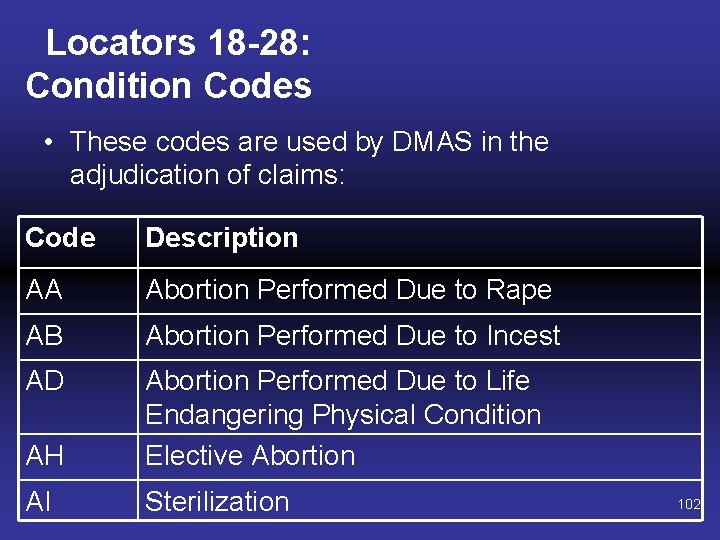
Locators 18 -28: Condition Codes • These codes are used by DMAS in the adjudication of claims: Code Description AA Abortion Performed Due to Rape AB Abortion Performed Due to Incest AD AH Abortion Performed Due to Life Endangering Physical Condition Elective Abortion AI Sterilization 102
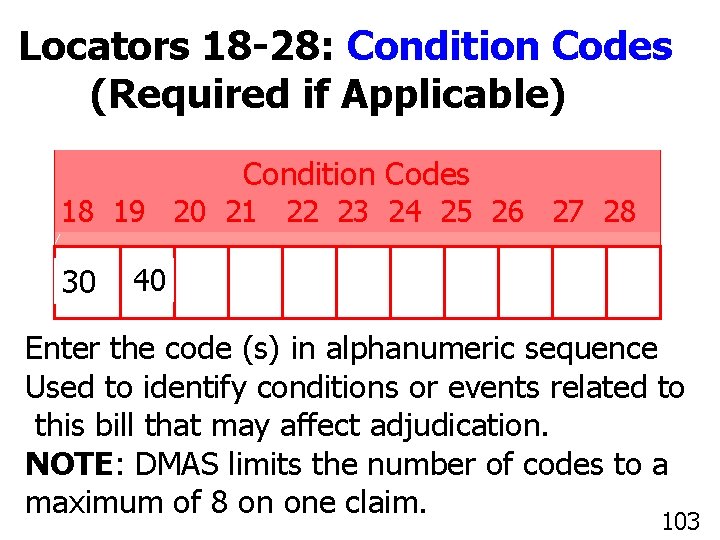
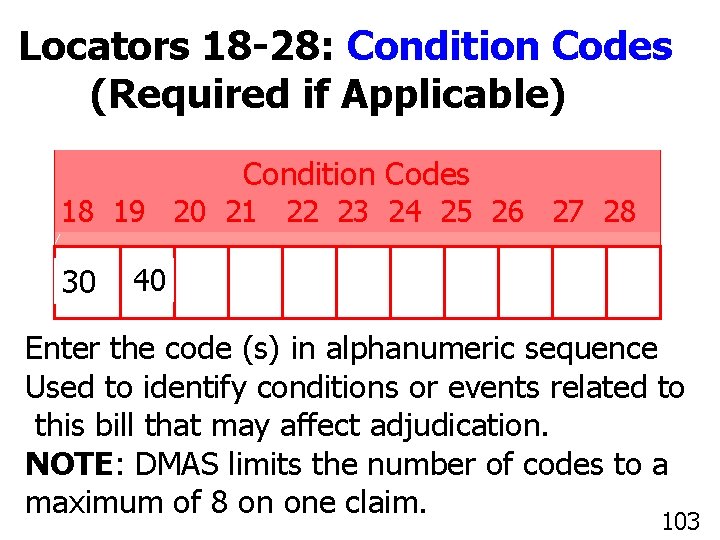
Locators 18 -28: Condition Codes (Required if Applicable) Condition Codes 18 19 20 21 22 23 24 25 26 27 28 30 40 Enter the code (s) in alphanumeric sequence Used to identify conditions or events related to this bill that may affect adjudication. NOTE: DMAS limits the number of codes to a 103 maximum of 8 on one claim. 103
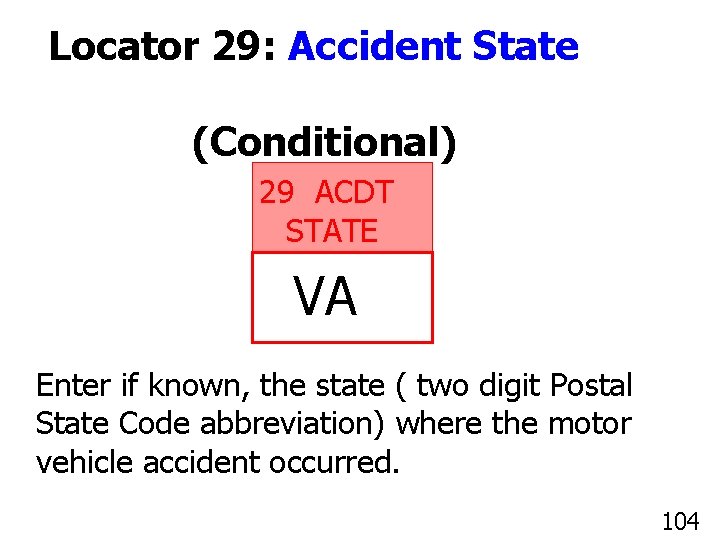
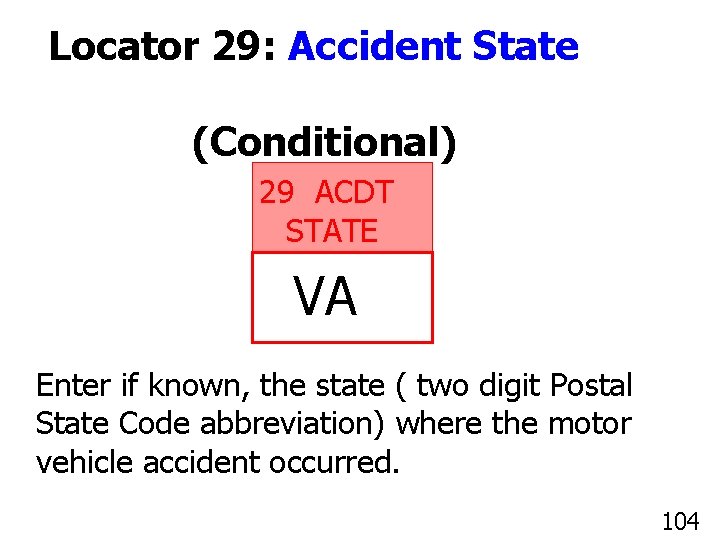
Locator 29: Accident State (Conditional) 29 ACDT STATE VA Enter if known, the state ( two digit Postal State Code abbreviation) where the motor vehicle accident occurred. 104
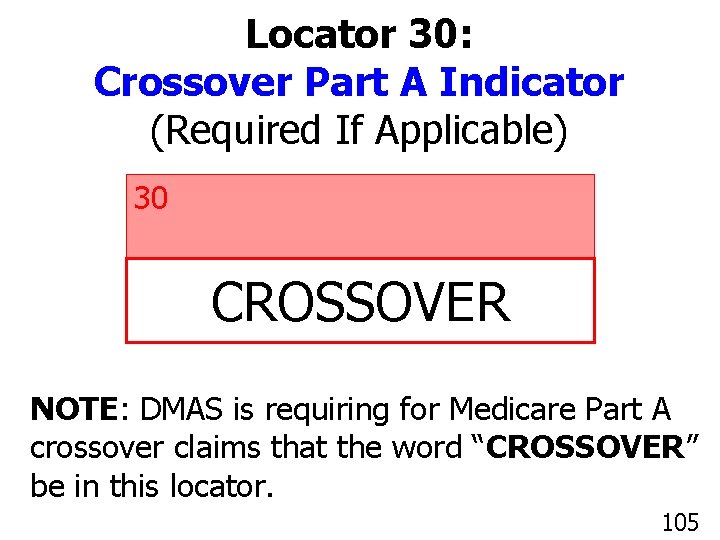
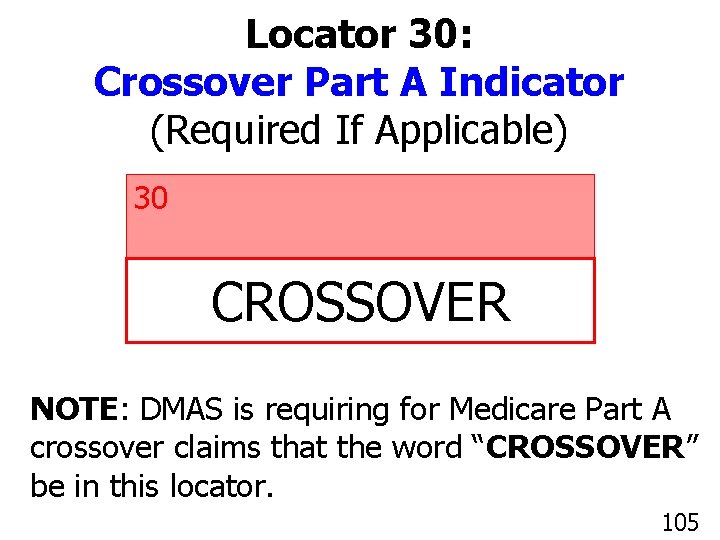
Locator 30: Crossover Part A Indicator (Required If Applicable) 30 CROSSOVER NOTE: DMAS is requiring for Medicare Part A crossover claims that the word “CROSSOVER” be in this locator. 105
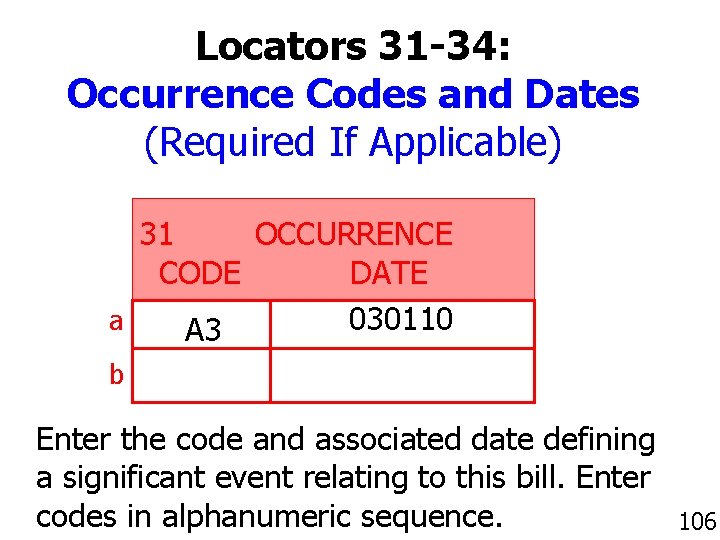
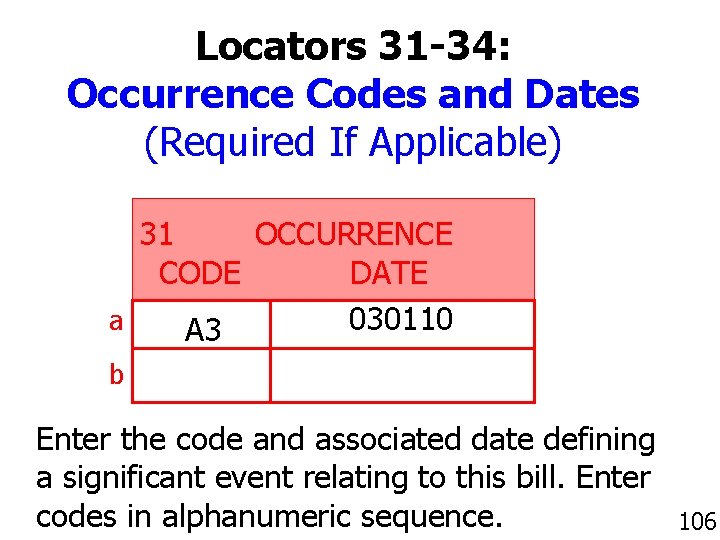
Locators 31 -34: Occurrence Codes and Dates (Required If Applicable) 31 OCCURRENCE CODE DATE a 030110 A 3 b Enter the code and associated date defining a significant event relating to this bill. Enter codes in alphanumeric sequence. 106
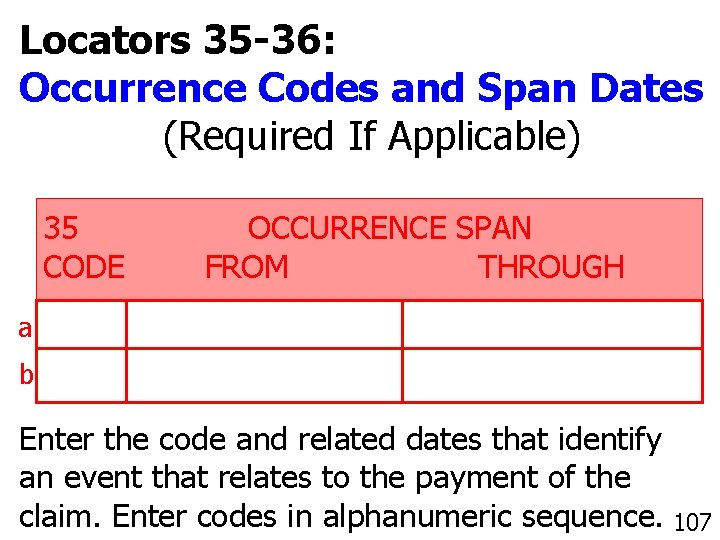
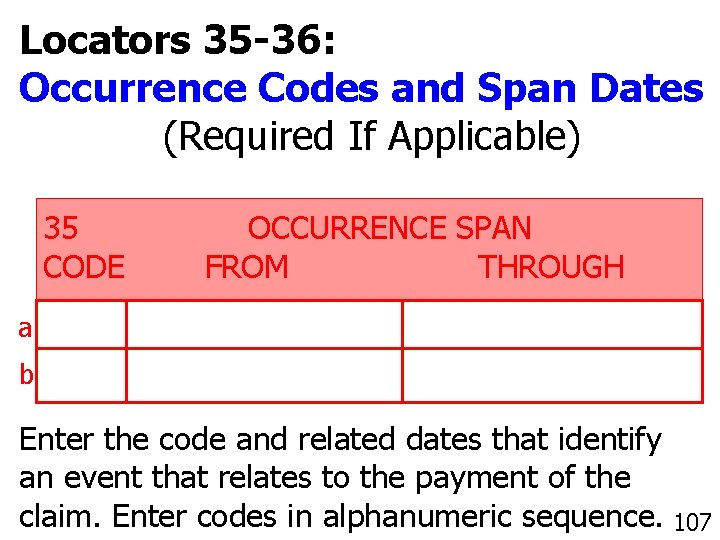
Locators 35 -36: Occurrence Codes and Span Dates (Required If Applicable) 35 CODE OCCURRENCE SPAN FROM THROUGH a b Enter the code and related dates that identify an event that relates to the payment of the 107 claim. Enter codes in alphanumeric sequence. 107
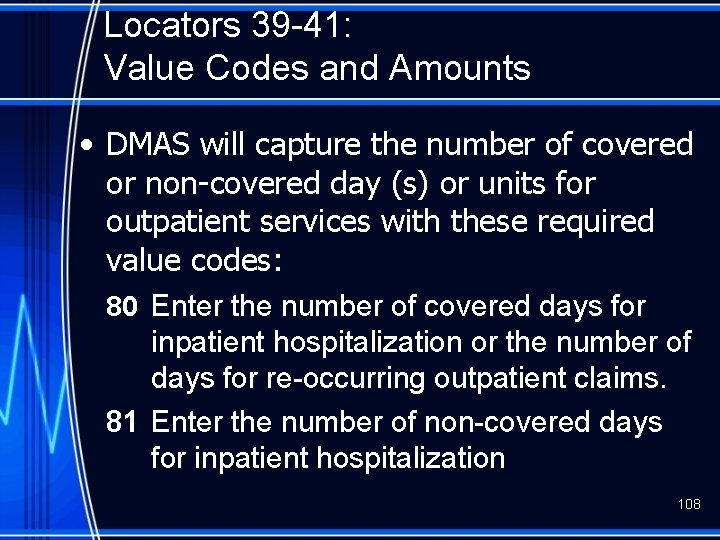
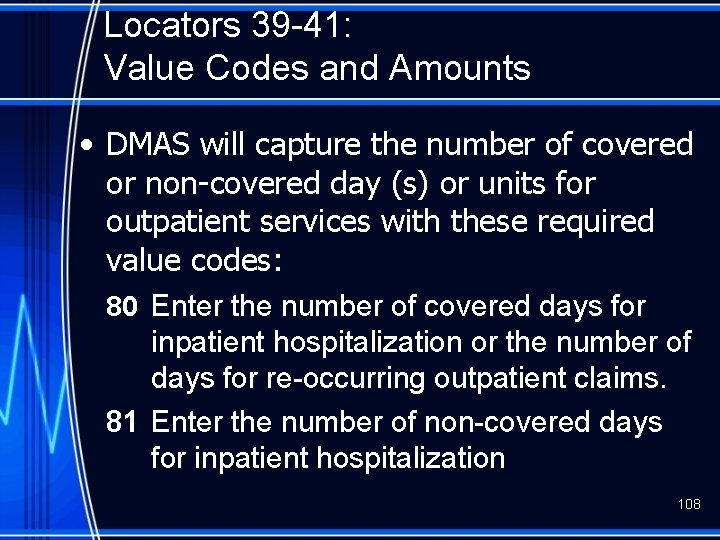
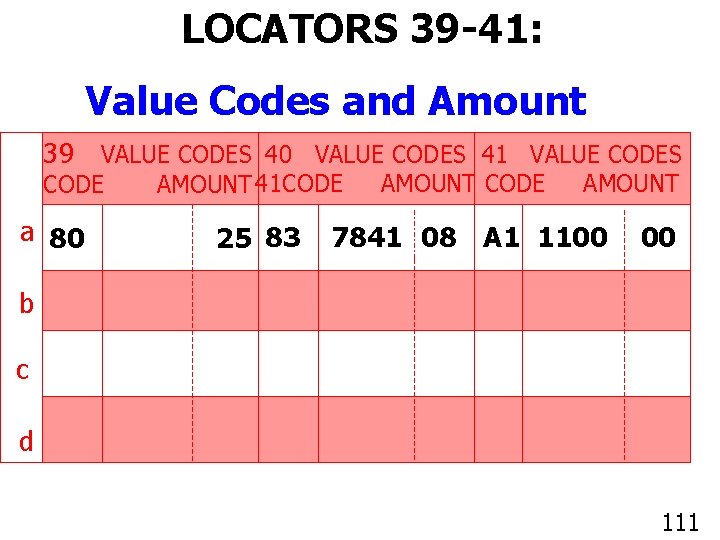
Locators 39 -41: Value Codes and Amounts • DMAS will capture the number of covered or non-covered day (s) or units for outpatient services with these required value codes: 80 Enter the number of covered days for inpatient hospitalization or the number of days for re-occurring outpatient claims. 81 Enter the number of non-covered days for inpatient hospitalization 108
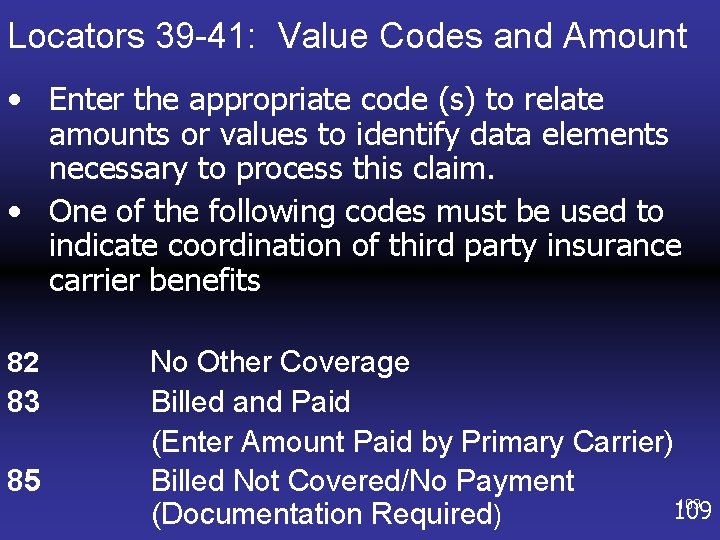
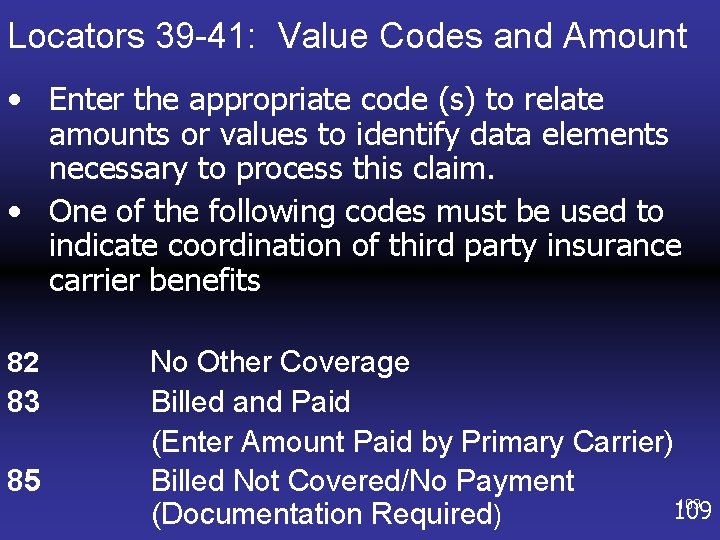
Locators 39 -41: Value Codes and Amount • Enter the appropriate code (s) to relate amounts or values to identify data elements necessary to process this claim. • One of the following codes must be used to indicate coordination of third party insurance carrier benefits 82 83 85 No Other Coverage Billed and Paid (Enter Amount Paid by Primary Carrier) Billed Not Covered/No Payment 109 (Documentation Required)
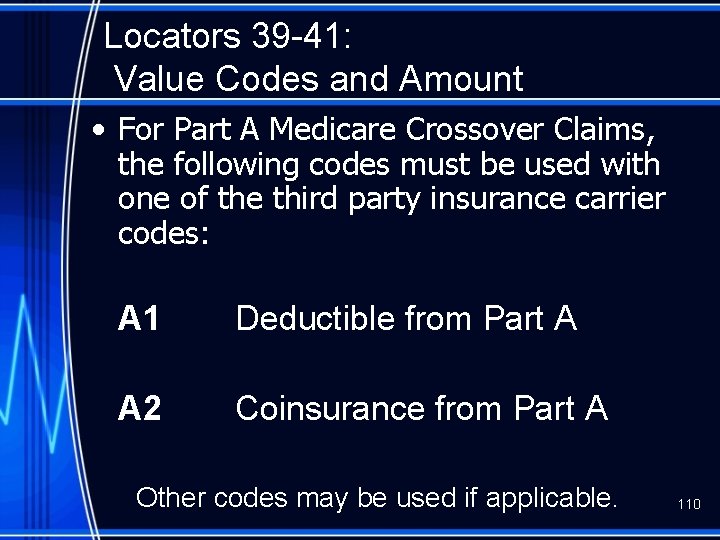
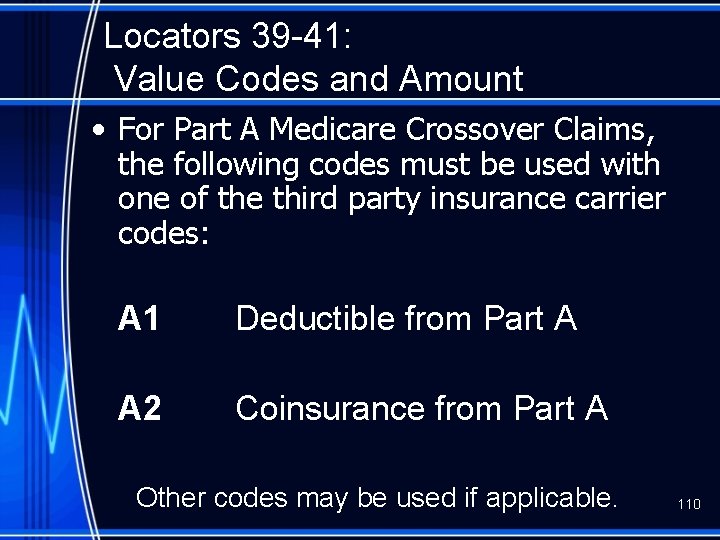
Locators 39 -41: Value Codes and Amount • For Part A Medicare Crossover Claims, the following codes must be used with one of the third party insurance carrier codes: A 1 Deductible from Part A A 2 Coinsurance from Part A Other codes may be used if applicable. 110
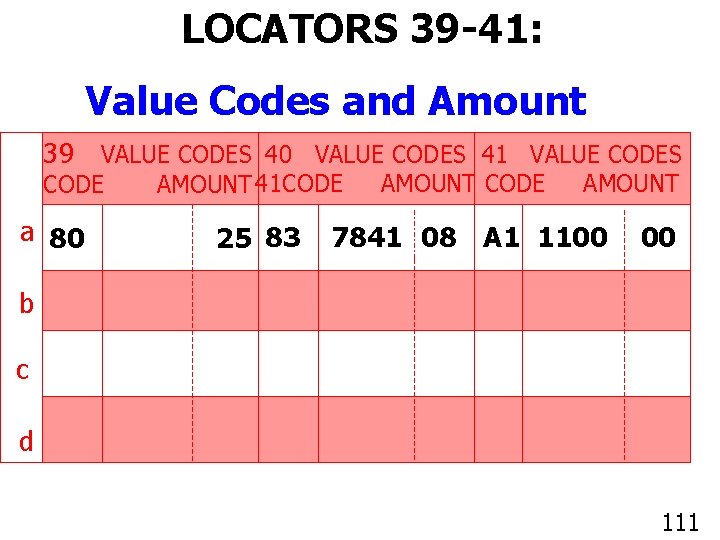
LOCATORS 39 -41: Value Codes and Amount 39 VALUE CODES 40 VALUE CODES 41 VALUE CODES CODE a 80 AMOUNT 41 CODE 25 83 AMOUNT CODE AMOUNT 7841 08 A 1 1100 00 b c d 111
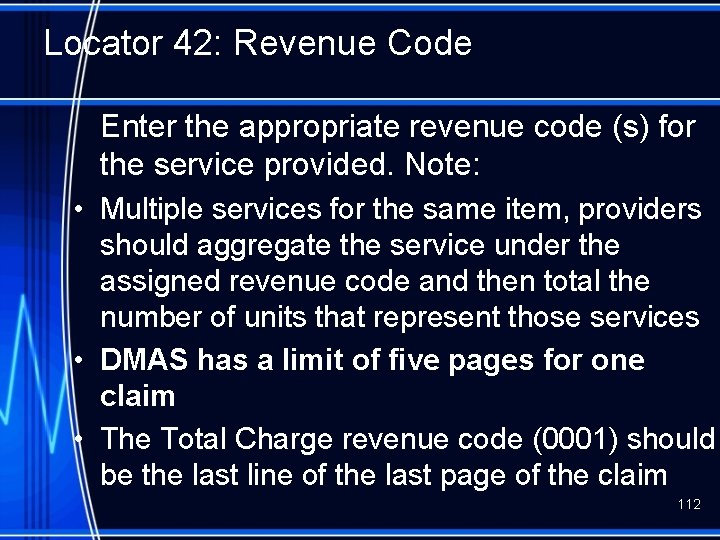
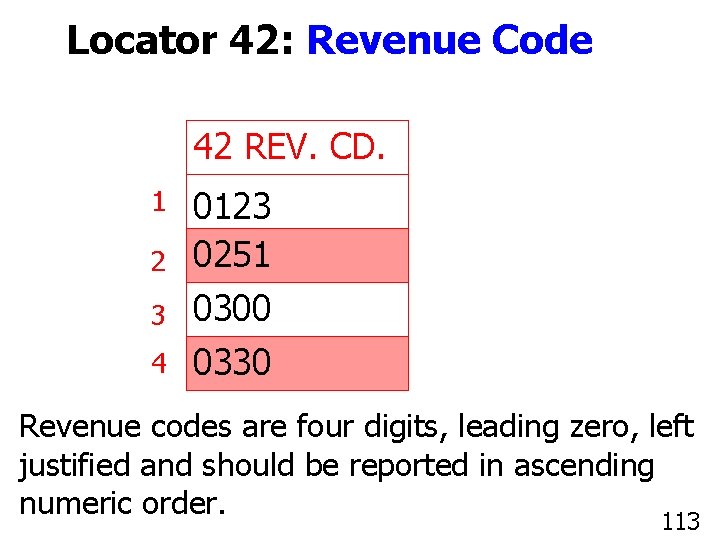
Locator 42: Revenue Code Enter the appropriate revenue code (s) for the service provided. Note: • Multiple services for the same item, providers should aggregate the service under the assigned revenue code and then total the number of units that represent those services • DMAS has a limit of five pages for one claim • The Total Charge revenue code (0001) should be the last line of the last page of the claim 112
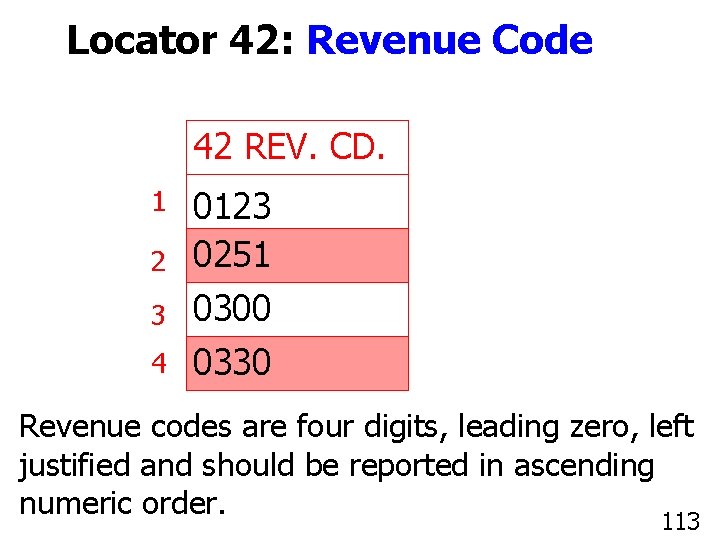
Locator 42: Revenue Code 42 REV. CD. 1 2 3 4 0123 0251 0300 0330 Revenue codes are four digits, leading zero, left justified and should be reported in ascending 113 numeric order. 113
Outpatient Hospital Setting Billing Requirements for NDC • CMS requirements related to the Deficit Reduction Act (DRA) of 2005, mandate DMAS to require hospital providers who bill drug products administered in an outpatient hospital setting to include the National Drug Code (NDC) information of the drug dispensed on all claim submissions. 114
Outpatient Hospital Setting NDC Billing Requirements • The NDC information will be required on all electronic (ASC X 12 N: 837 I) and paper (Universal Billing “UB”) claim submissions. • This requirement also applies to Medicare Crossover claim submissions. • Outpatient hospital claims submitted without a valid NDC will have the revenue code line reduced to a non-covered service line. 115
Outpatient Hospital Setting NDC Billing Requirements • Providers billing for compound medication with more than one NDC included in the medication dispensed, each applicable NDC must be submitted on a separate claim line to include both prescription and over-the-counter ingredients. • Each claim line submitted with pharmacy revenue codes 0250 -0259 and 0630 -0639 will require the NDC information. 116
Outpatient Hospital Setting NDC Billing Requirements • Effective 07/01/08, a valid NDC will be required for all drug products administered in an outpatient hospital setting. • By definition, a valid NDC is a formatted number using the 5 -4 -2 format, i. e. , 5 -digits, followed by 4 -digits, followed by 2 -digits: – 99999888877 • Each NDC must be an 11 -digit code unique to the manufacturer of the specific product administered to the patient. 117
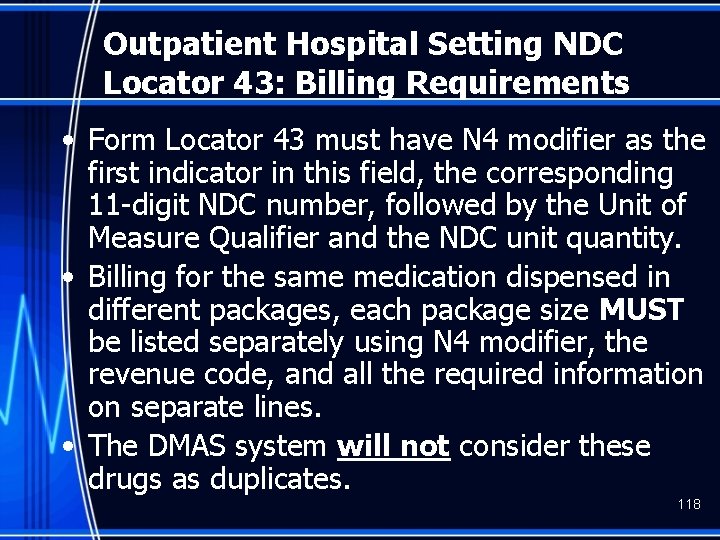
Outpatient Hospital Setting NDC Locator 43: Billing Requirements • Form Locator 43 must have N 4 modifier as the first indicator in this field, the corresponding 11 -digit NDC number, followed by the Unit of Measure Qualifier and the NDC unit quantity. • Billing for the same medication dispensed in different packages, each package size MUST be listed separately using N 4 modifier, the revenue code, and all the required information on separate lines. • The DMAS system will not consider these drugs as duplicates. 118
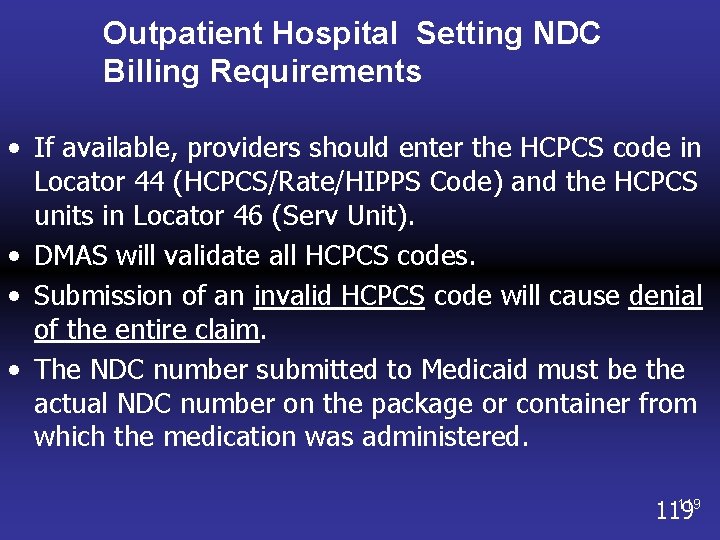
Outpatient Hospital Setting NDC Billing Requirements • If available, providers should enter the HCPCS code in Locator 44 (HCPCS/Rate/HIPPS Code) and the HCPCS units in Locator 46 (Serv Unit). • DMAS will validate all HCPCS codes. • Submission of an invalid HCPCS code will cause denial of the entire claim. • The NDC number submitted to Medicaid must be the actual NDC number on the package or container from which the medication was administered. 119
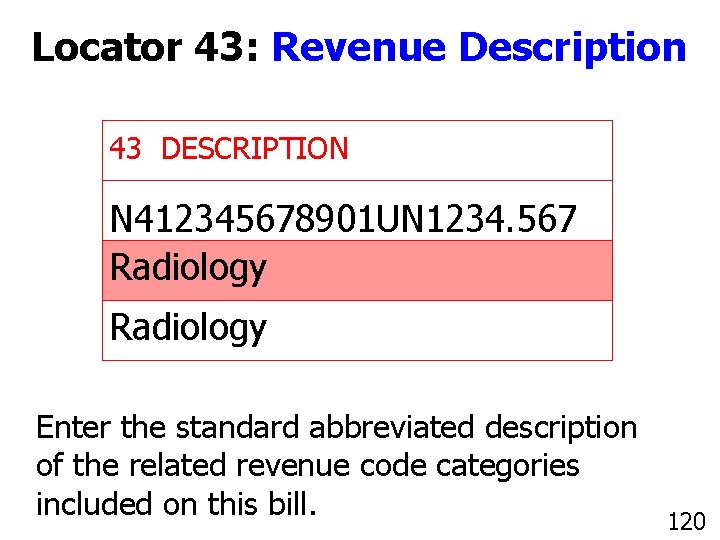
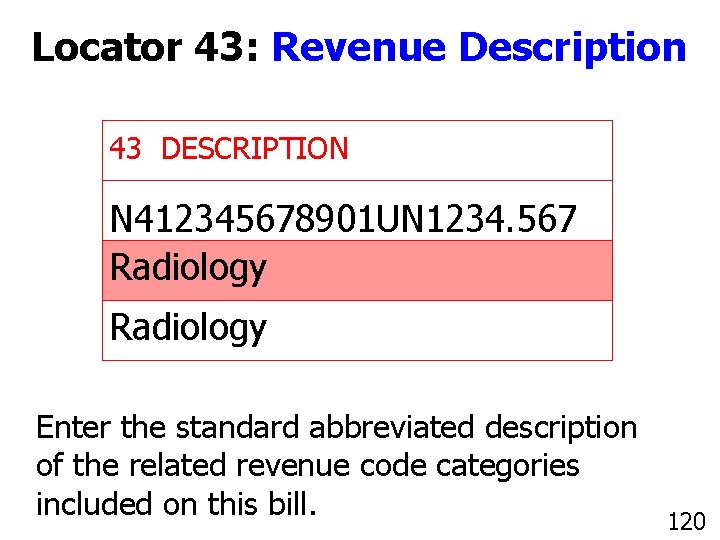
Locator 43: Revenue Description 43 DESCRIPTION N 412345678901 UN 1234. 567 Radiology Enter the standard abbreviated description of the related revenue code categories included on this bill. 120
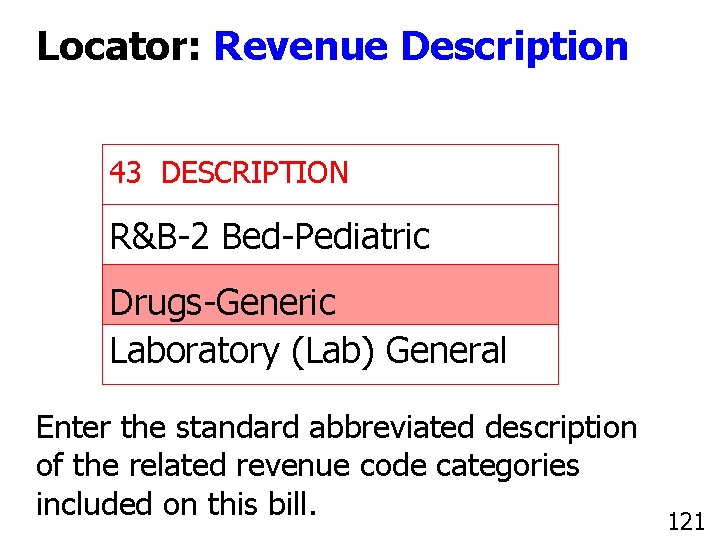
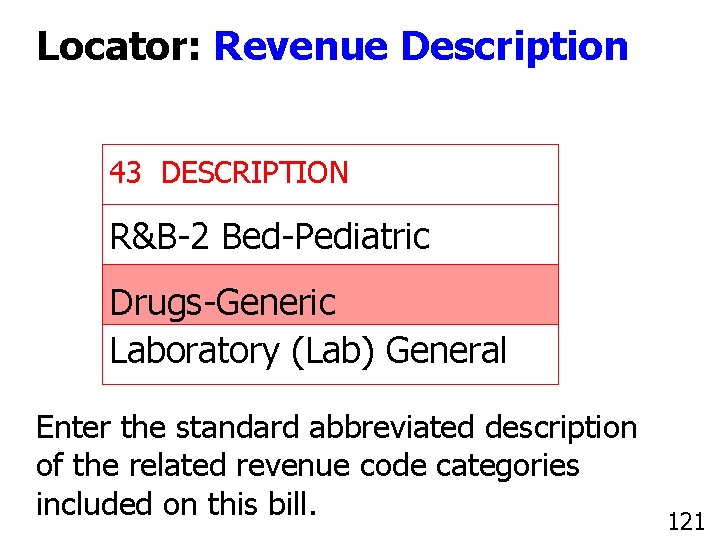
Locator: Revenue Description 43 DESCRIPTION R&B-2 Bed-Pediatric Drugs-Generic Laboratory (Lab) General Enter the standard abbreviated description of the related revenue code categories included on this bill. 121
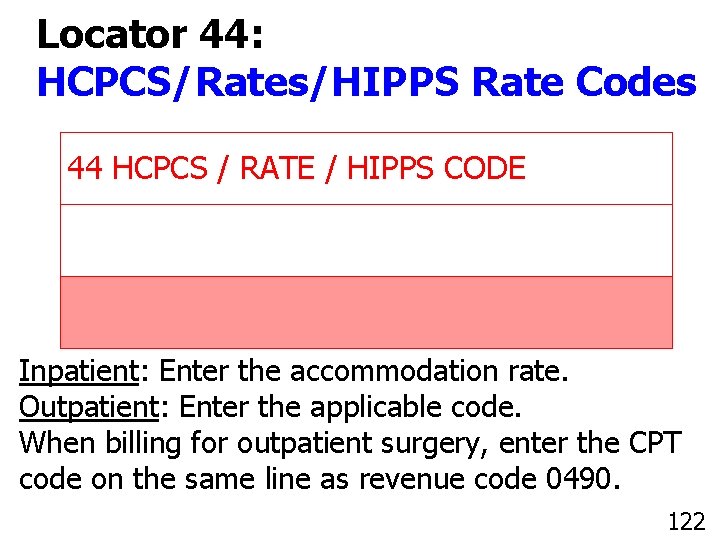
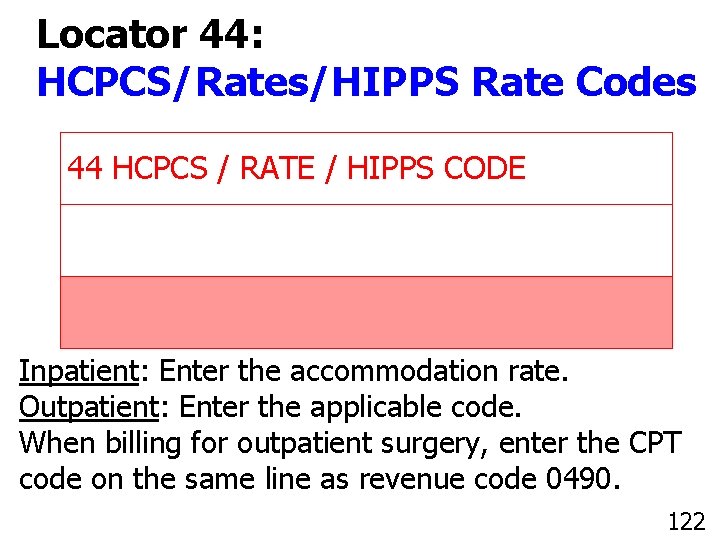
Locator 44: HCPCS/Rates/HIPPS Rate Codes 44 HCPCS / RATE / HIPPS CODE Inpatient: Enter the accommodation rate. Outpatient: Enter the applicable code. When billing for outpatient surgery, enter the CPT code on the same line as revenue code 0490. 122 112 122
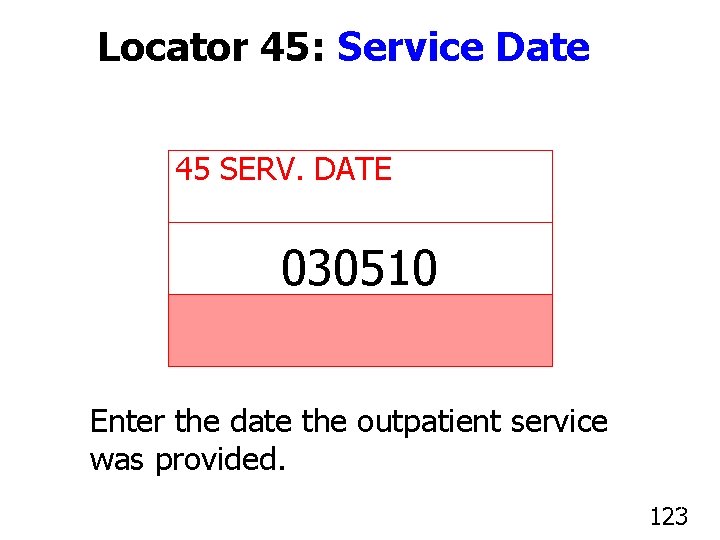
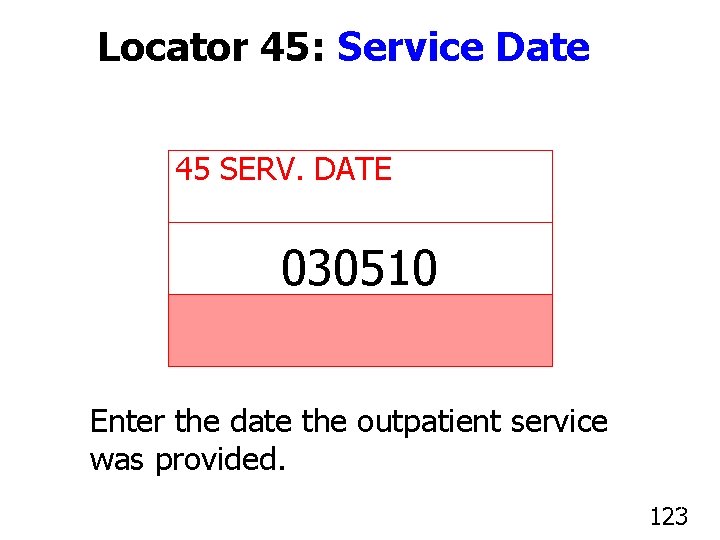
Locator 45: Service Date 45 SERV. DATE 030510 Enter the date the outpatient service was provided. 123
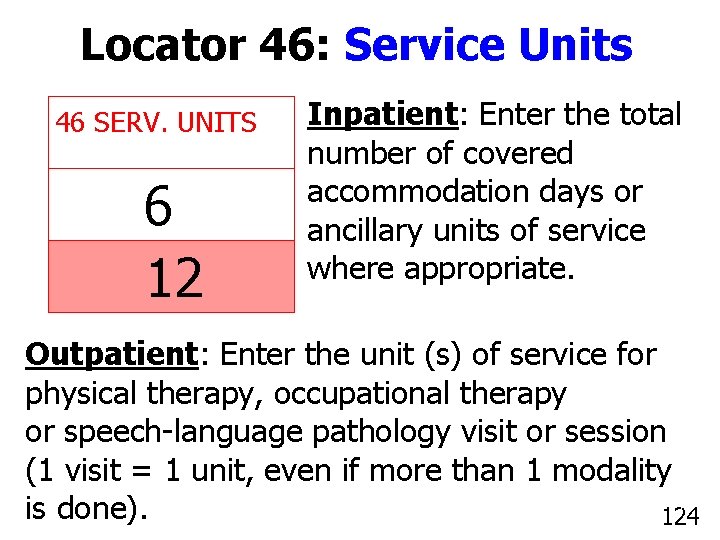
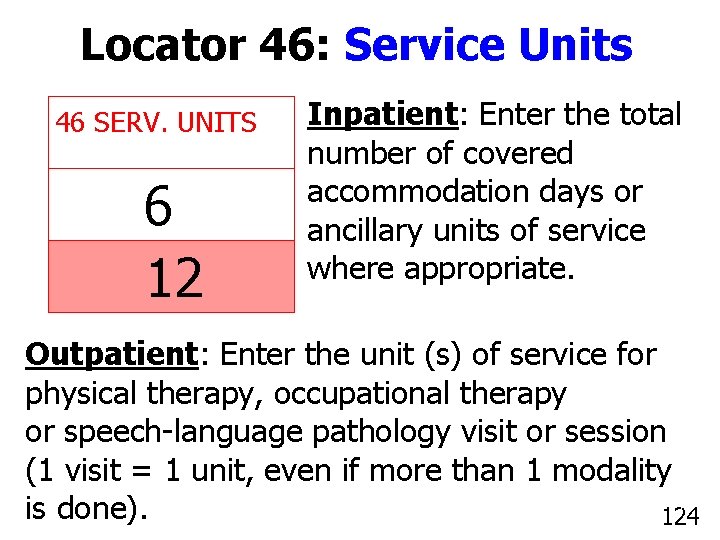
Locator 46: Service Units 46 SERV. UNITS 6 12 Inpatient: Enter the total number of covered accommodation days or ancillary units of service where appropriate. Outpatient: Enter the unit (s) of service for physical therapy, occupational therapy or speech-language pathology visit or session (1 visit = 1 unit, even if more than 1 modality 124 is done). 124
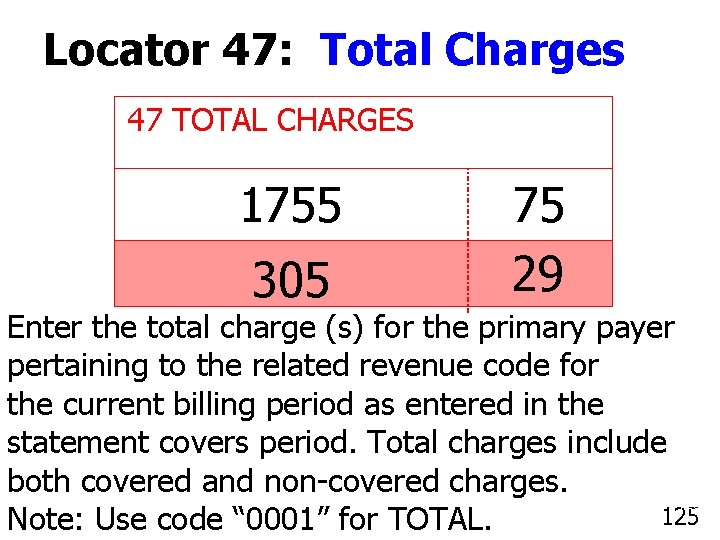
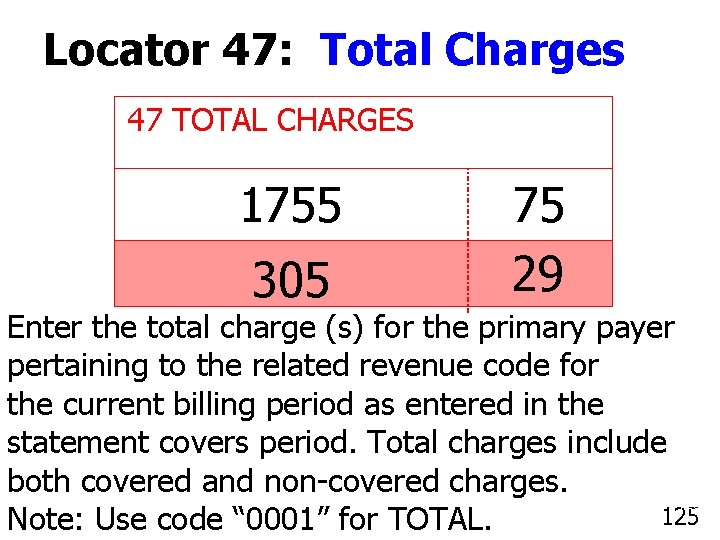
Locator 47: Total Charges 47 TOTAL CHARGES 1755 305 75 29 Enter the total charge (s) for the primary payer pertaining to the related revenue code for the current billing period as entered in the statement covers period. Total charges include both covered and non-covered charges. 125 Note: Use code “ 0001” for TOTAL.
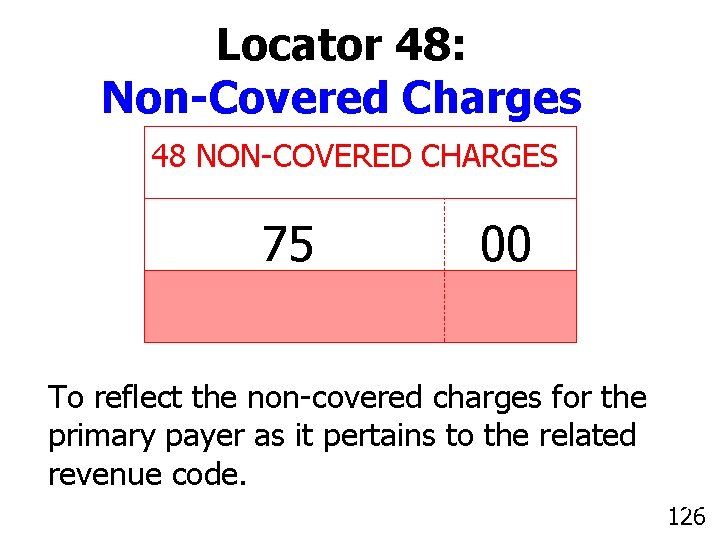
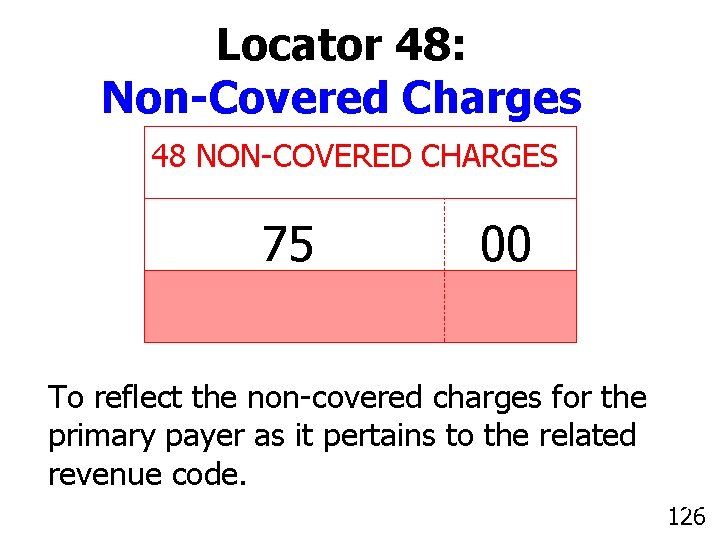
Locator 48: Non-Covered Charges 48 NON-COVERED CHARGES 75 00 To reflect the non-covered charges for the primary payer as it pertains to the related revenue code. 126
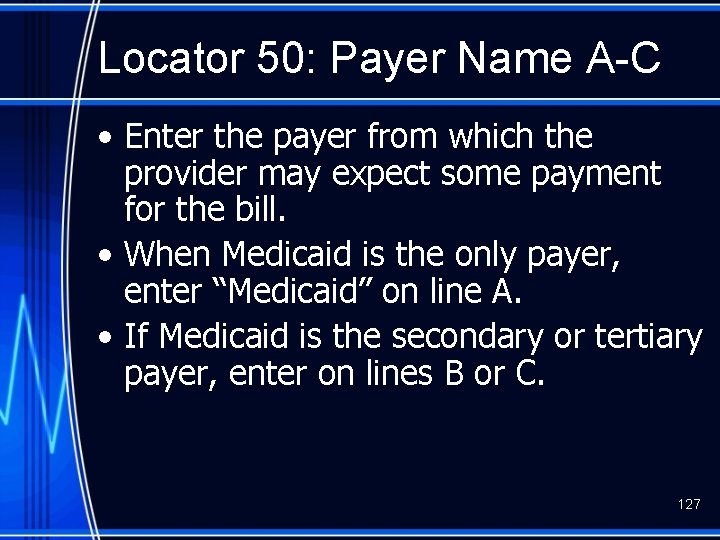
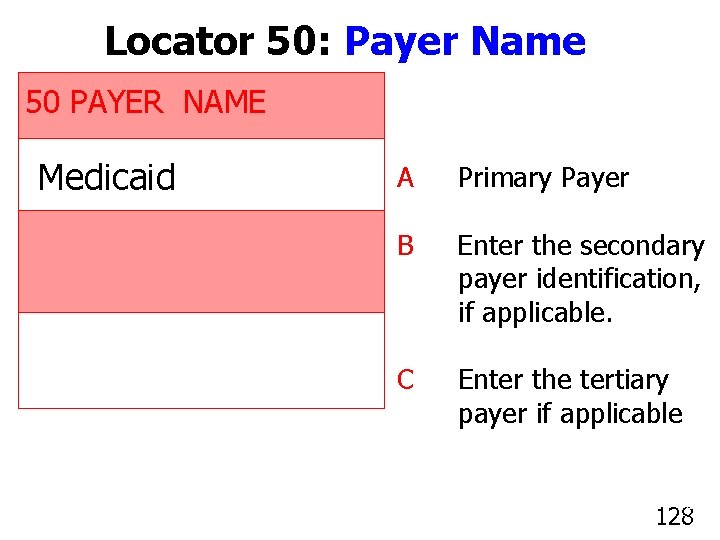
Locator 50: Payer Name A-C • Enter the payer from which the provider may expect some payment for the bill. • When Medicaid is the only payer, enter “Medicaid” on line A. • If Medicaid is the secondary or tertiary payer, enter on lines B or C. 127
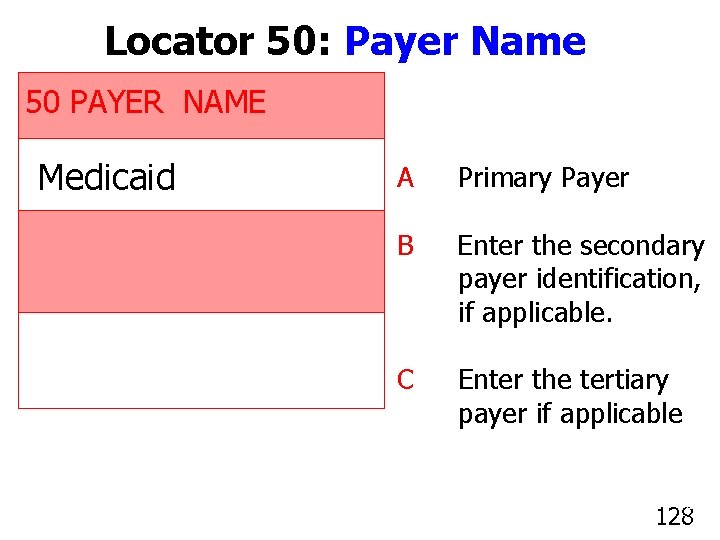
Locator 50: Payer Name 50 PAYER NAME Medicaid A Primary Payer B Enter the secondary payer identification, if applicable. C Enter the tertiary payer if applicable. 128
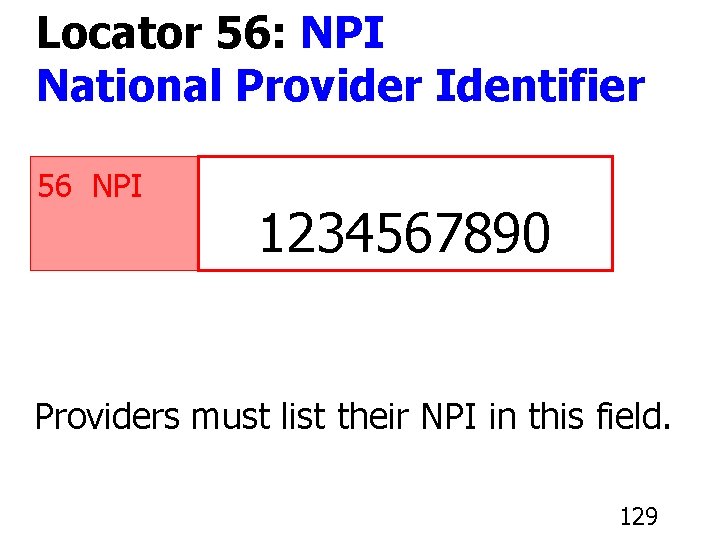
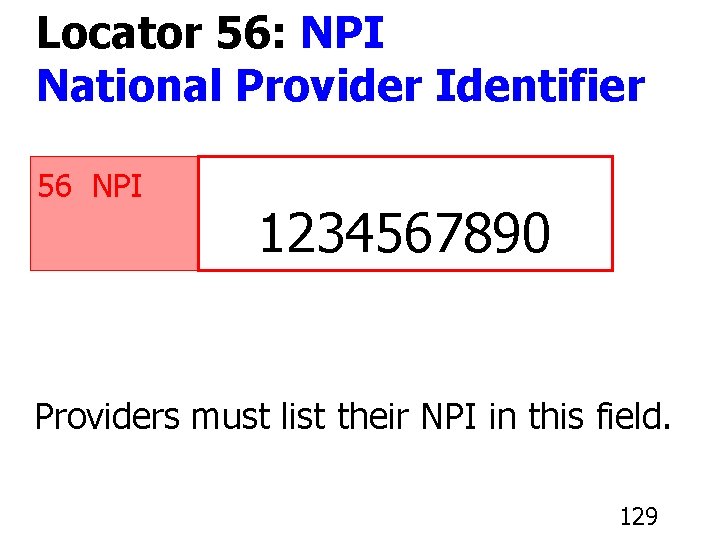
Locator 56: NPI National Provider Identifier 56 NPI 1234567890 Providers must list their NPI in this field. 129
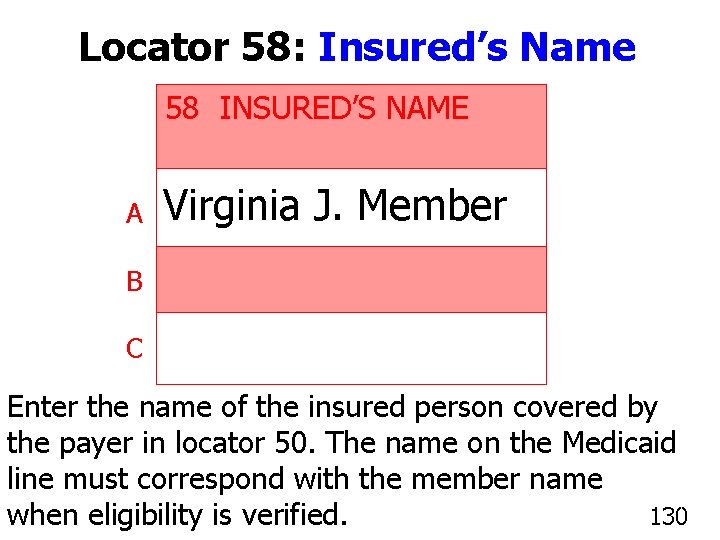
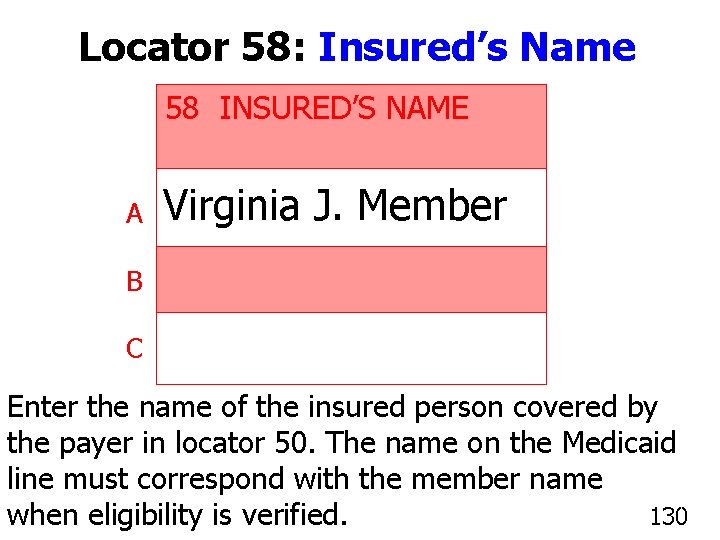
Locator 58: Insured’s Name 58 INSURED’S NAME A Virginia J. Member B C Enter the name of the insured person covered by the payer in locator 50. The name on the Medicaid line must correspond with the member name 130 when eligibility is verified. 130
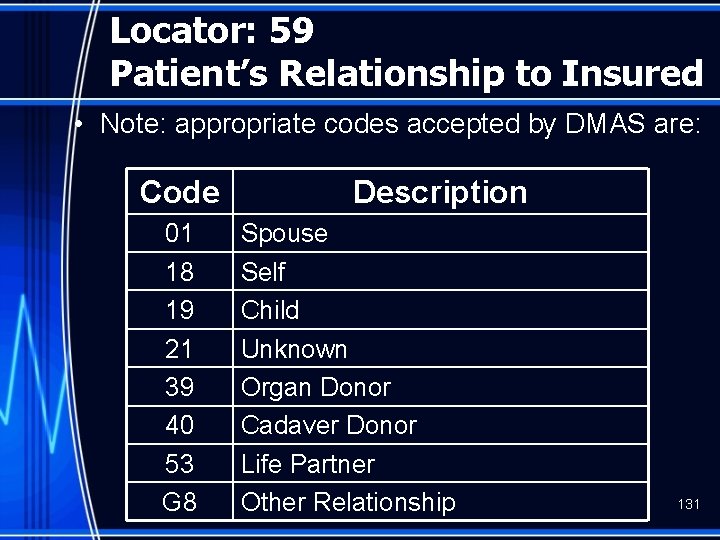
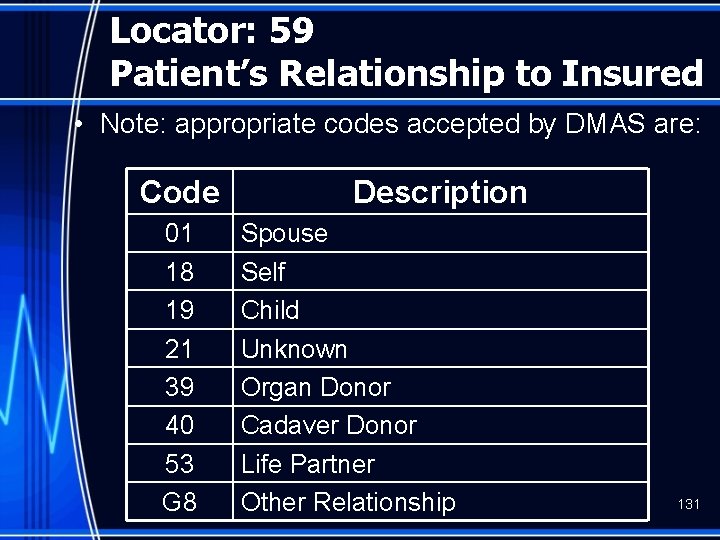
Locator: 59 Patient’s Relationship to Insured • Note: appropriate codes accepted by DMAS are: Code 01 18 19 21 39 40 53 G 8 Description Spouse Self Child Unknown Organ Donor Cadaver Donor Life Partner Other Relationship 131
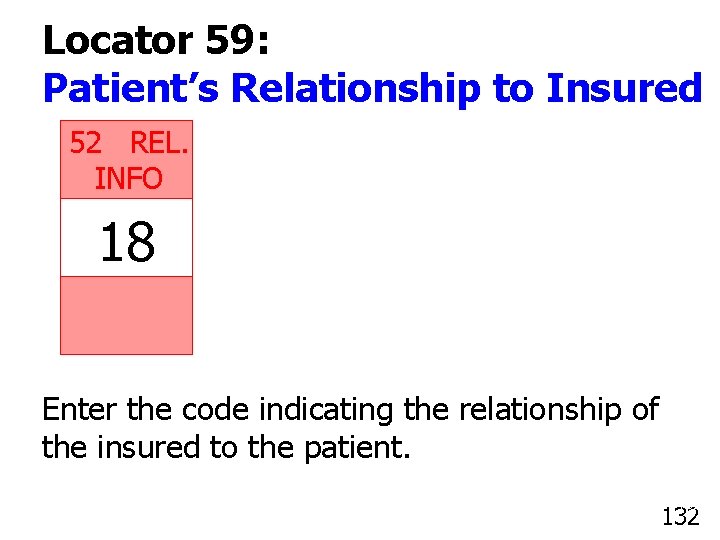
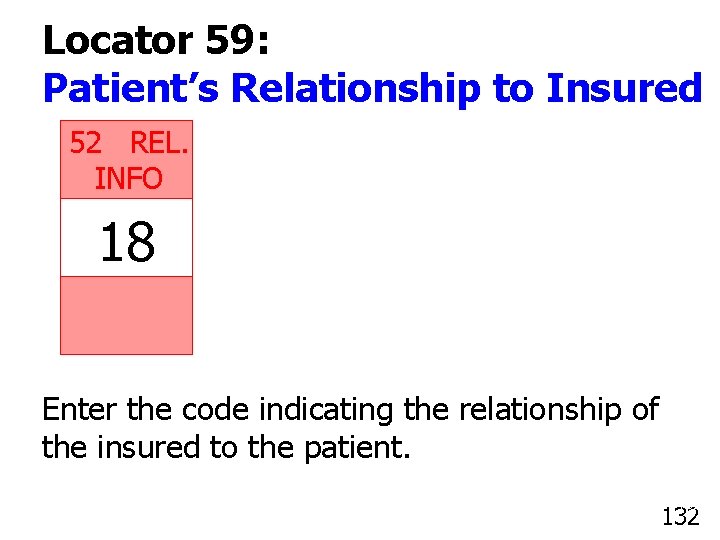
Locator 59: Patient’s Relationship to Insured 52 REL. INFO 18 Enter the code indicating the relationship of the insured to the patient. 132
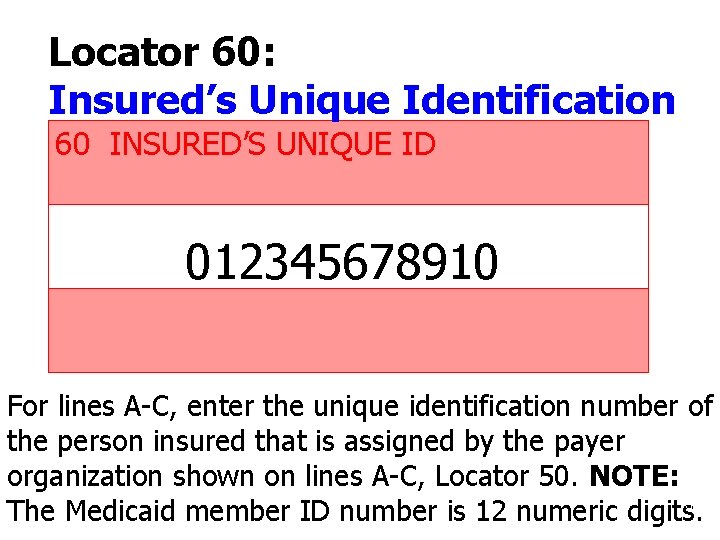
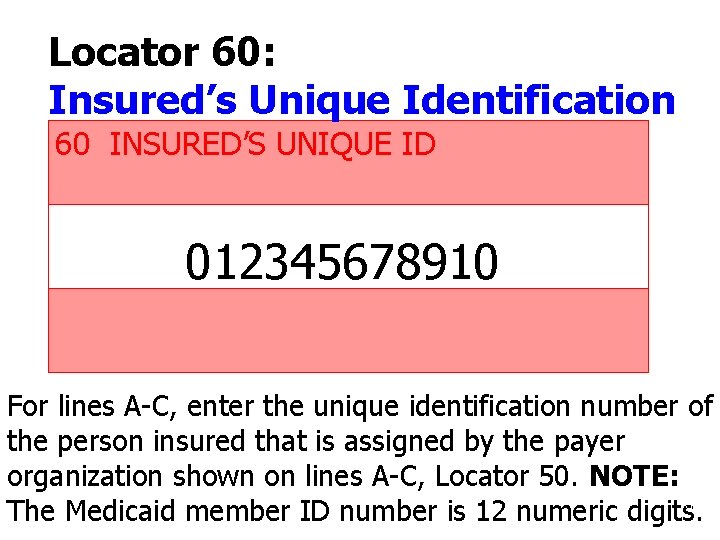
Locator 60: Insured’s Unique Identification 60 INSURED’S UNIQUE ID 012345678910 For lines A-C, enter the unique identification number of the person insured that is assigned by the payer organization shown on lines A-C, Locator 50. NOTE: 133 The Medicaid member ID number is 12 numeric digits.
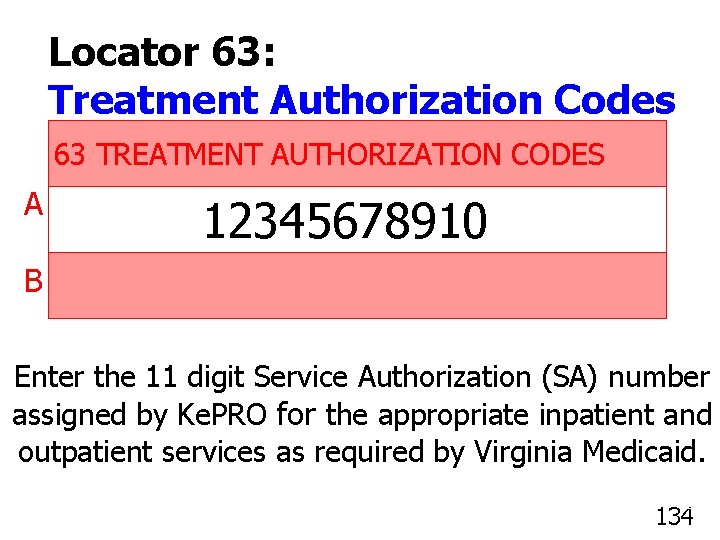
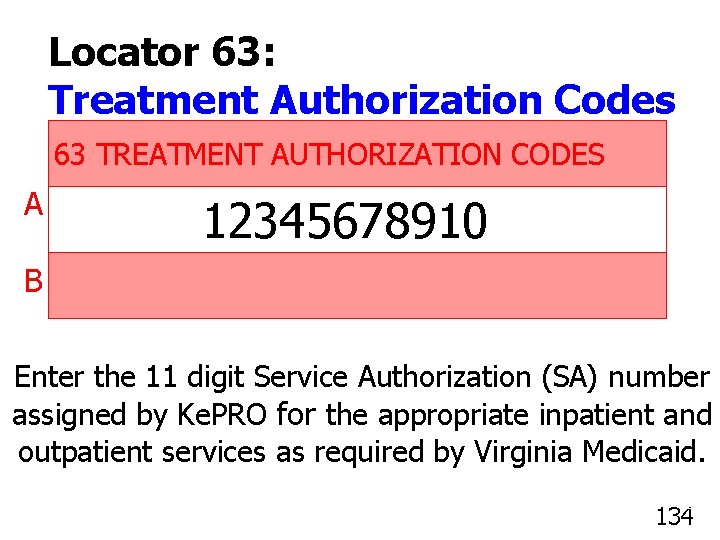
Locator 63: Treatment Authorization Codes 63 TREATMENT AUTHORIZATION CODES A 12345678910 B Enter the 11 digit Service Authorization (SA) number assigned by Ke. PRO for the appropriate inpatient and outpatient services as required by Virginia Medicaid. 134
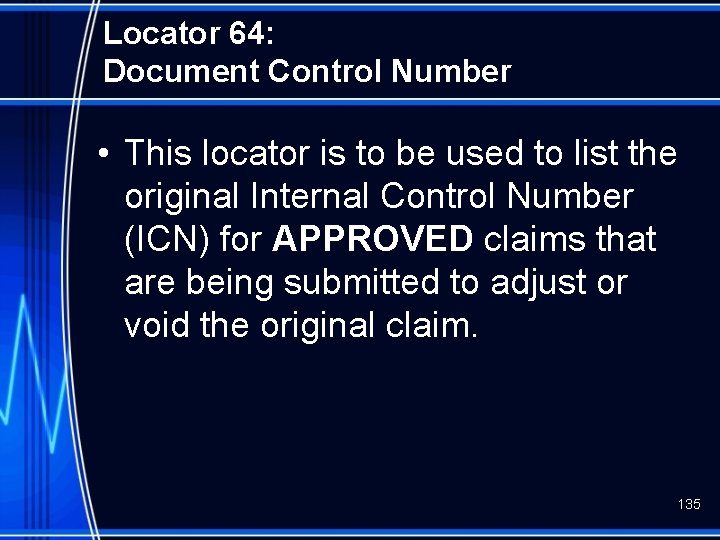
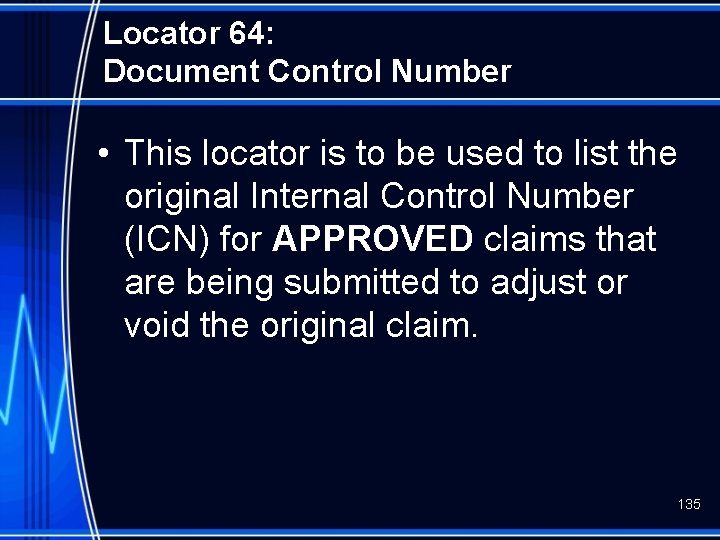
Locator 64: Document Control Number • This locator is to be used to list the original Internal Control Number (ICN) for APPROVED claims that are being submitted to adjust or void the original claim. 135
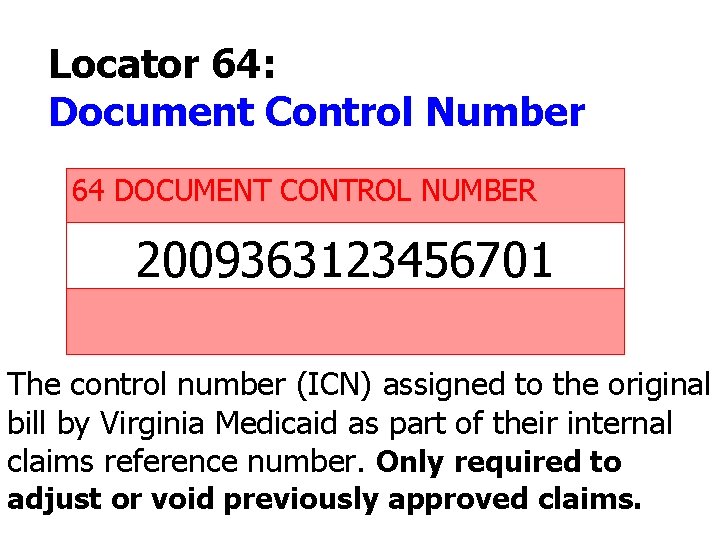
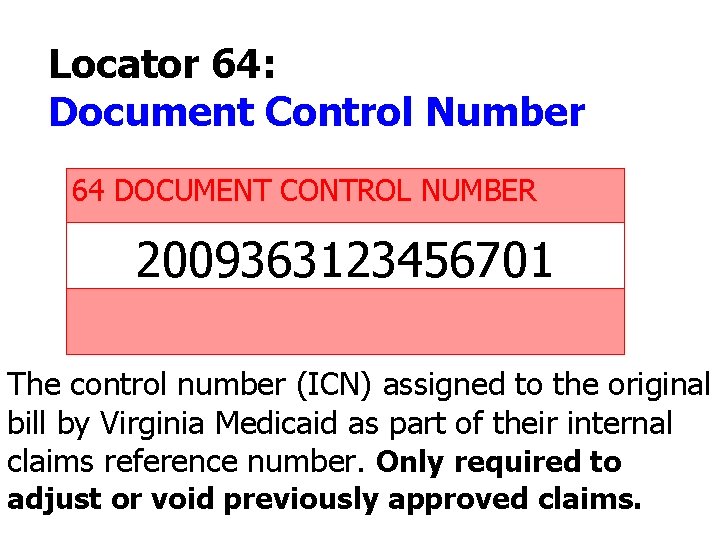
Locator 64: Document Control Number 64 DOCUMENT CONTROL NUMBER 2009363123456701 The control number (ICN) assigned to the original bill by Virginia Medicaid as part of their internal claims reference number. Only required to adjust or void previously approved claims. 91 136
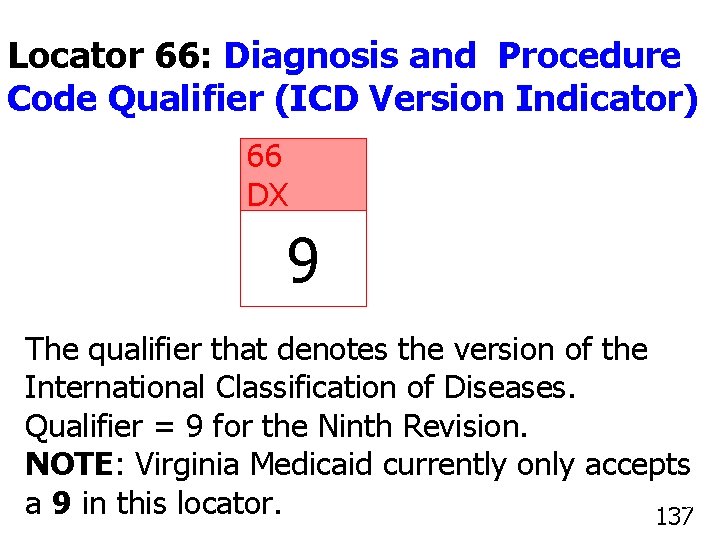
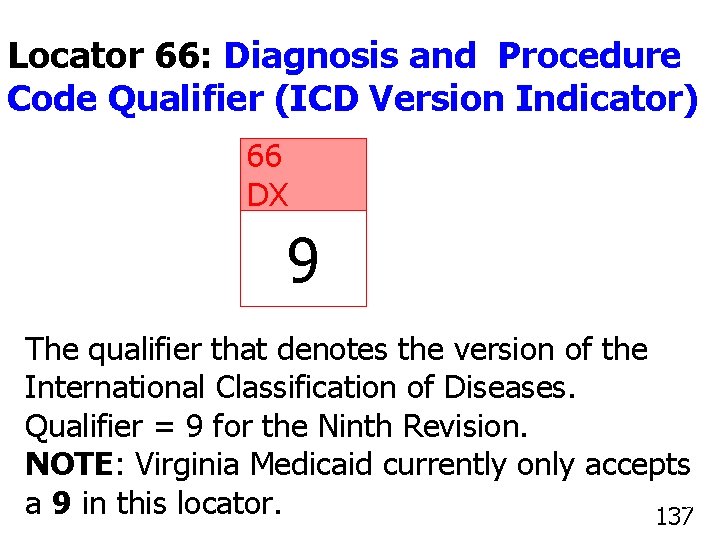
Locator 66: Diagnosis and Procedure Code Qualifier (ICD Version Indicator) 66 DX 9 The qualifier that denotes the version of the International Classification of Diseases. Qualifier = 9 for the Ninth Revision. NOTE: Virginia Medicaid currently only accepts 137 a 9 in this locator. 137
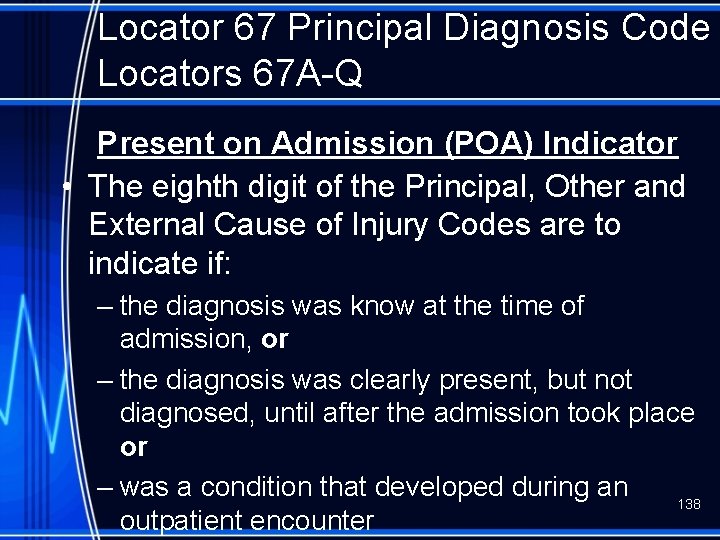
Locator 67 Principal Diagnosis Code Locators 67 A-Q Present on Admission (POA) Indicator • The eighth digit of the Principal, Other and External Cause of Injury Codes are to indicate if: – the diagnosis was know at the time of admission, or – the diagnosis was clearly present, but not diagnosed, until after the admission took place or – was a condition that developed during an 138 outpatient encounter
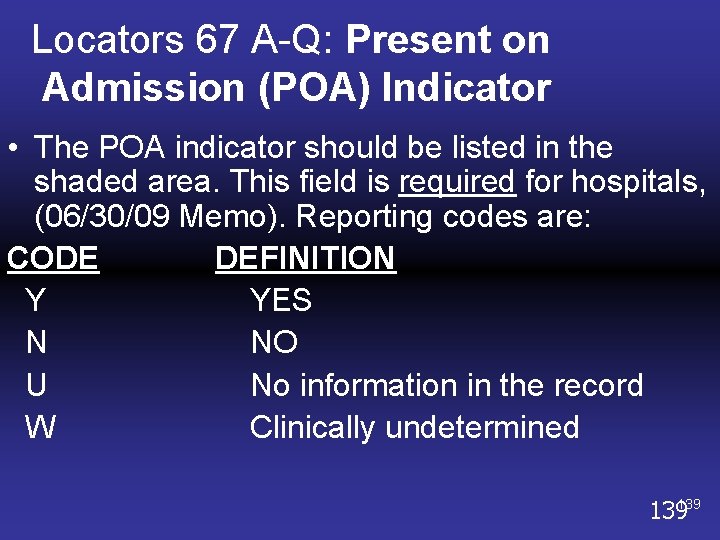
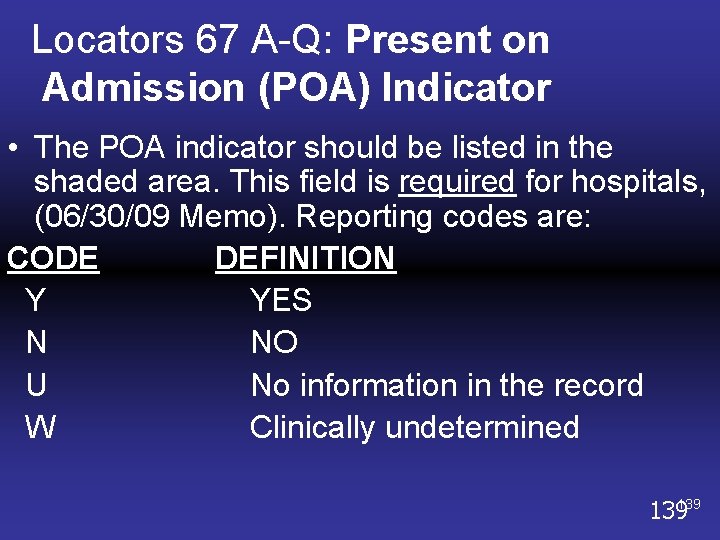
Locators 67 A-Q: Present on Admission (POA) Indicator • The POA indicator should be listed in the shaded area. This field is required for hospitals, (06/30/09 Memo). Reporting codes are: CODE DEFINITION Y YES N NO U No information in the record W Clinically undetermined 139139
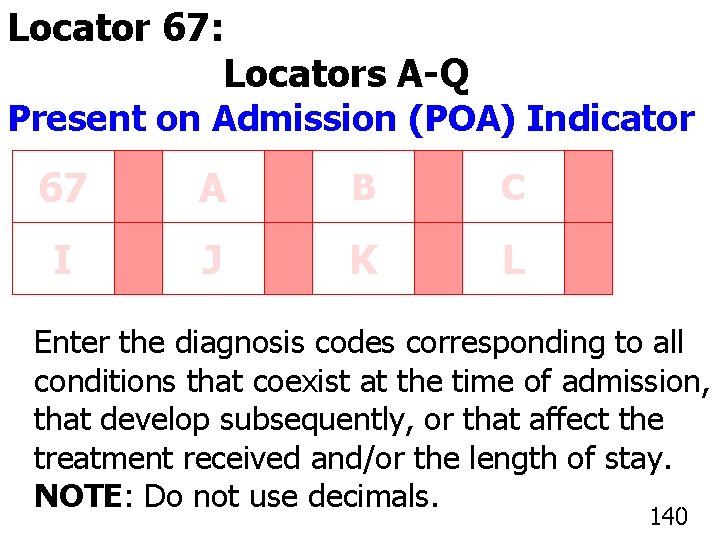
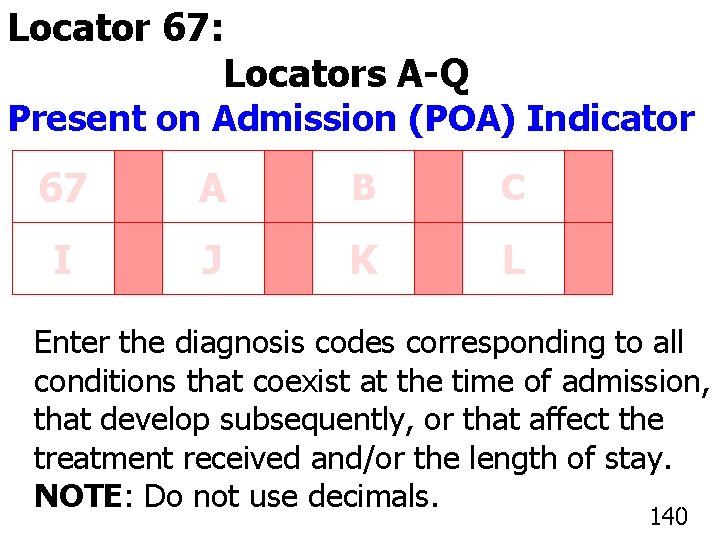
Locator 67: Principal Diagnosis Code Locators A-Q Present on Admission (POA) Indicator 67 A B C I J K L Enter the diagnosis codes corresponding to all conditions that coexist at the time of admission, that develop subsequently, or that affect the treatment received and/or the length of stay. NOTE: Do not use decimals. 140
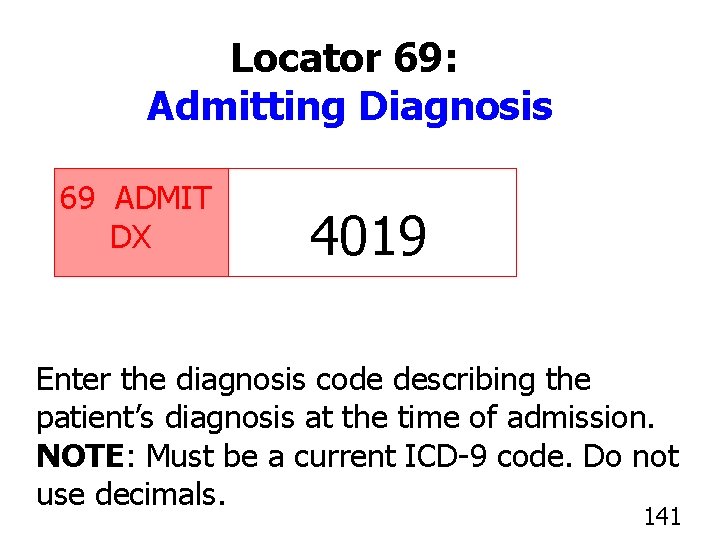
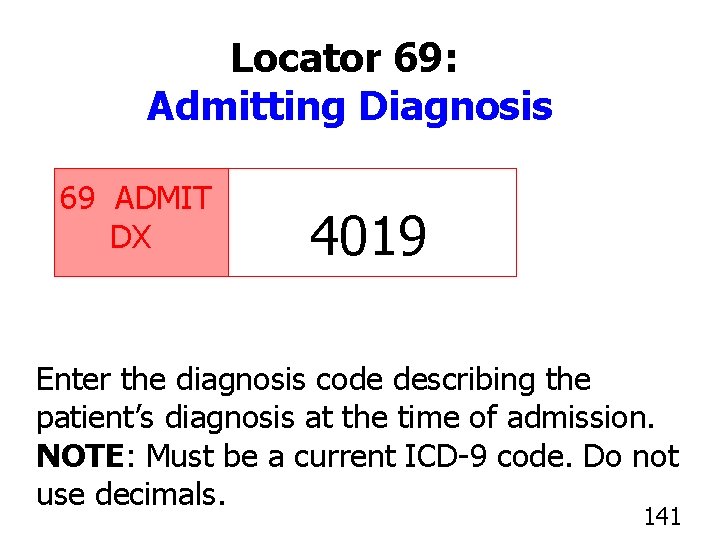
Locator 69: Admitting Diagnosis 69 ADMIT DX 4019 Enter the diagnosis code describing the patient’s diagnosis at the time of admission. NOTE: Must be a current ICD-9 code. Do not use decimals. 141
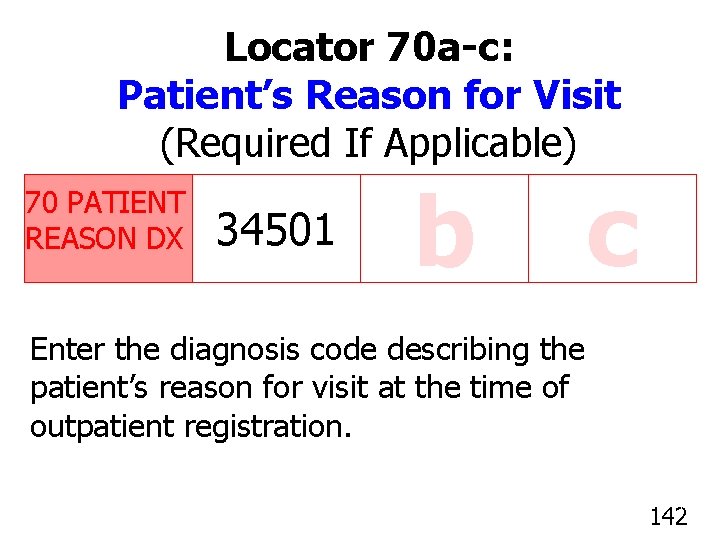
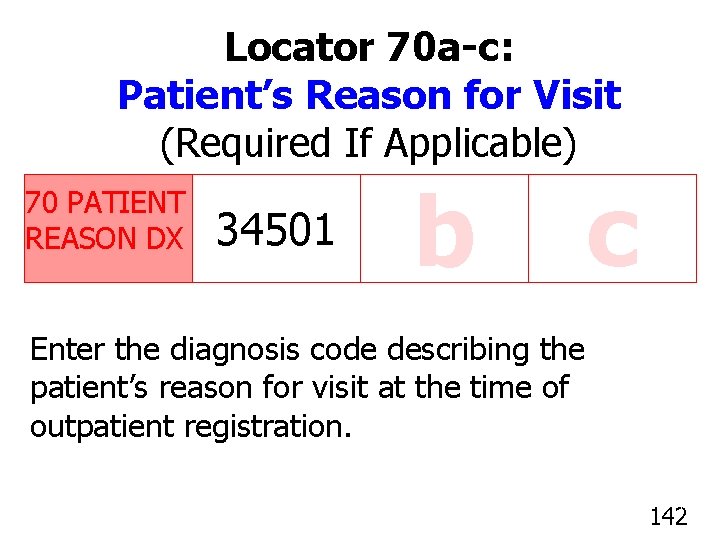
Locator 70 a-c: Patient’s Reason for Visit (Required If Applicable) 70 PATIENT REASON DX 34501 b c Enter the diagnosis code describing the patient’s reason for visit at the time of outpatient registration. 142
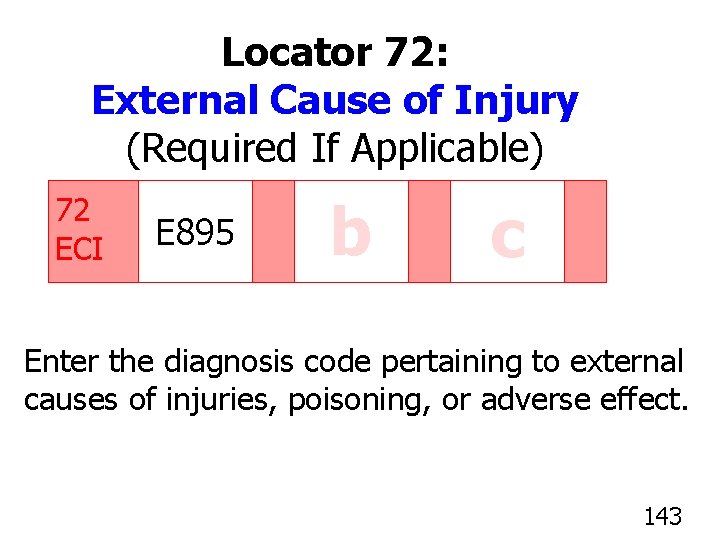
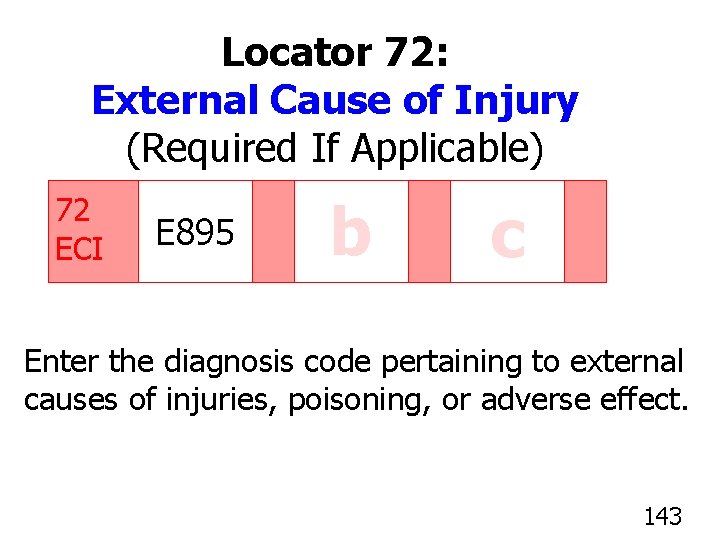
Locator 72: External Cause of Injury (Required If Applicable) 72 ECI E 895 b c Enter the diagnosis code pertaining to external causes of injuries, poisoning, or adverse effect. 143
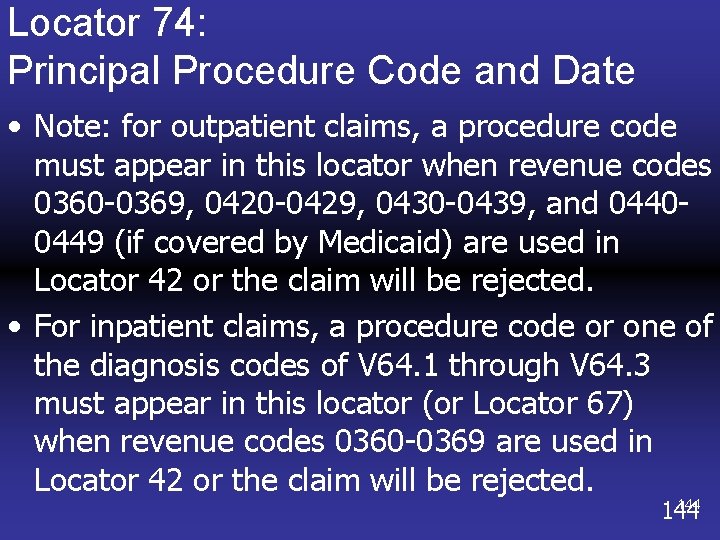
Locator 74: Principal Procedure Code and Date • Note: for outpatient claims, a procedure code must appear in this locator when revenue codes 0360 -0369, 0420 -0429, 0430 -0439, and 04400449 (if covered by Medicaid) are used in Locator 42 or the claim will be rejected. • For inpatient claims, a procedure code or one of the diagnosis codes of V 64. 1 through V 64. 3 must appear in this locator (or Locator 67) when revenue codes 0360 -0369 are used in Locator 42 or the claim will be rejected. 144
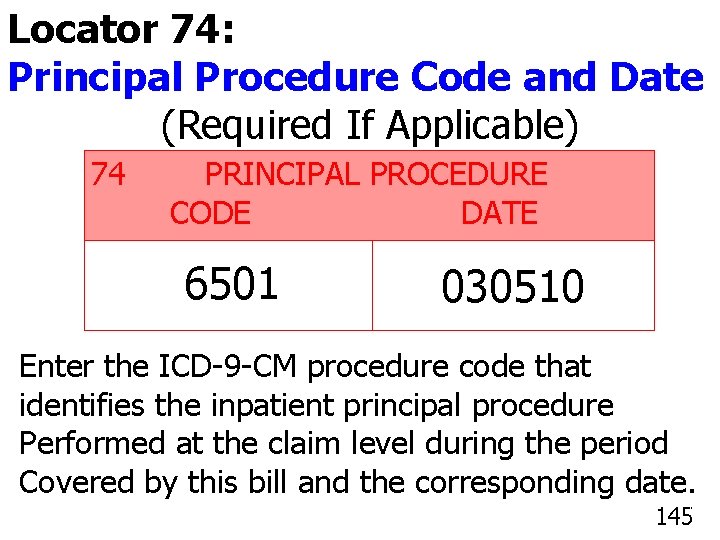
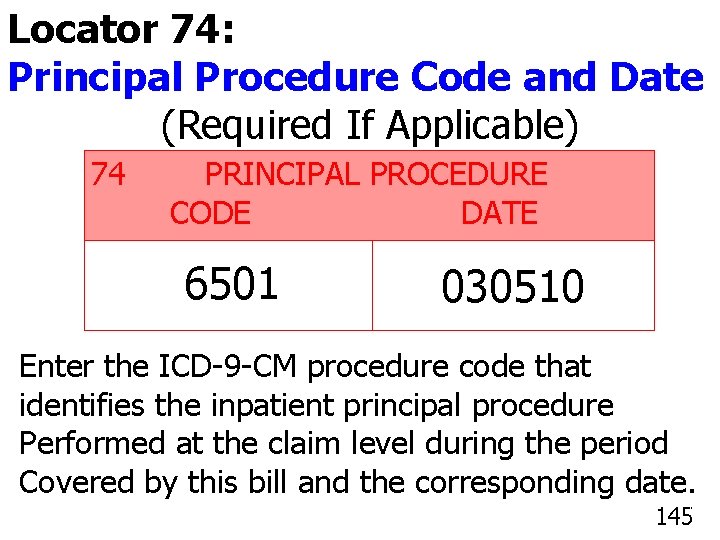
Locator 74: Principal Procedure Code and Date (Required If Applicable) 74 PRINCIPAL PROCEDURE CODE DATE 6501 030510 Enter the ICD-9 -CM procedure code that identifies the inpatient principal procedure Performed at the claim level during the period Covered by this bill and the corresponding date. 145
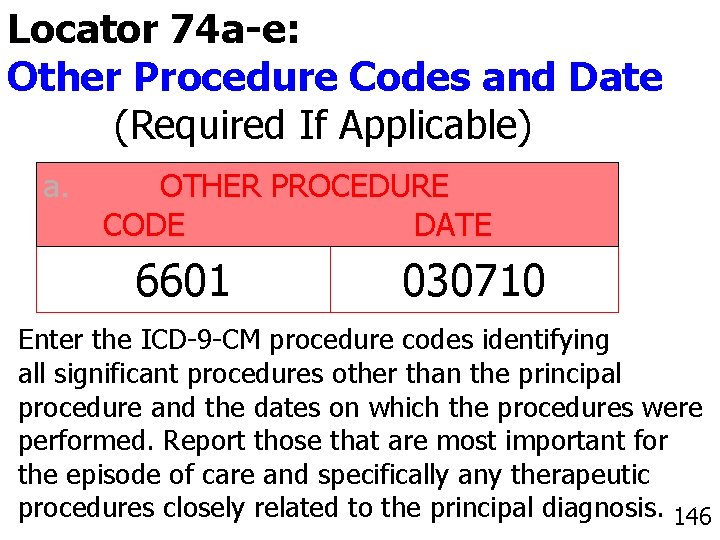
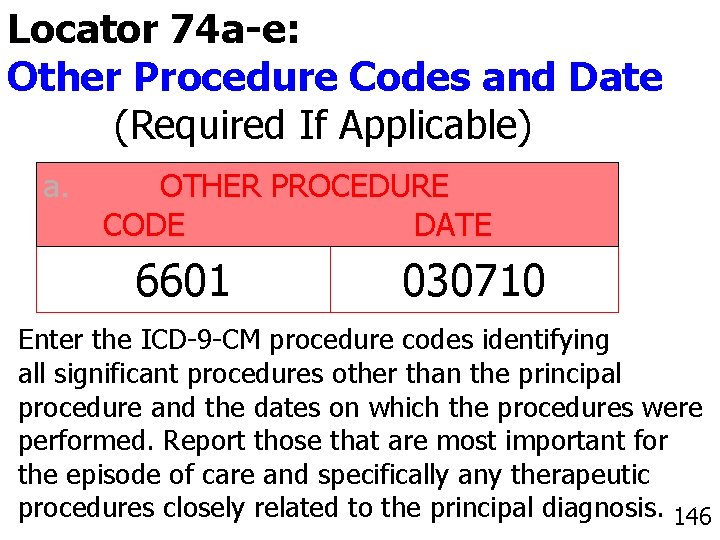
Locator 74 a-e: Other Procedure Codes and Date (Required If Applicable) a. OTHER PROCEDURE CODE DATE 6601 030710 Enter the ICD-9 -CM procedure codes identifying all significant procedures other than the principal procedure and the dates on which the procedures were performed. Report those that are most important for the episode of care and specifically any therapeutic 146 procedures closely related to the principal diagnosis. 146
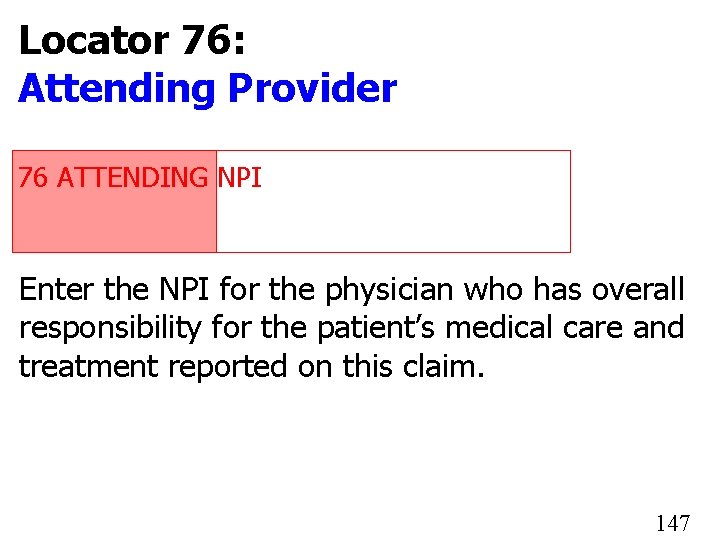
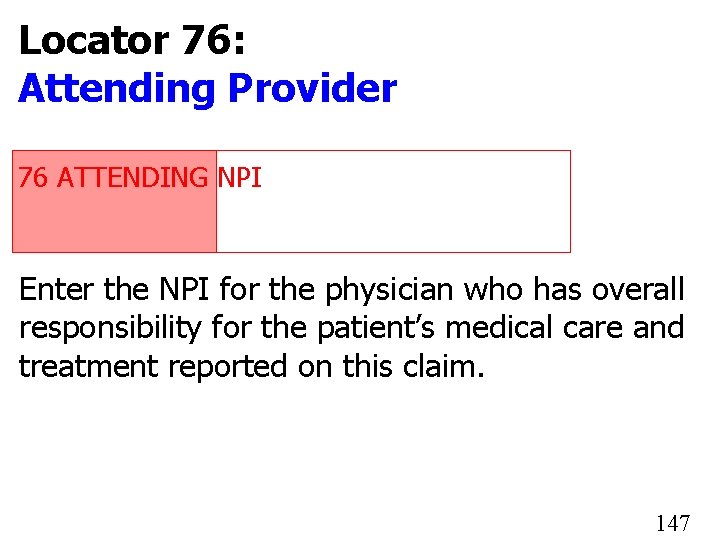
Locator 76: Attending Provider 76 ATTENDING NPI 1234567890 Enter the NPI for the physician who has overall responsibility for the patient’s medical care and treatment reported on this claim. 147
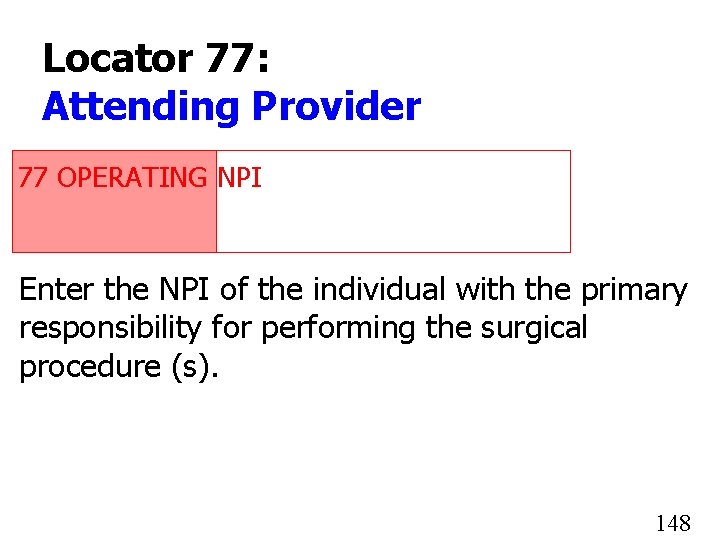
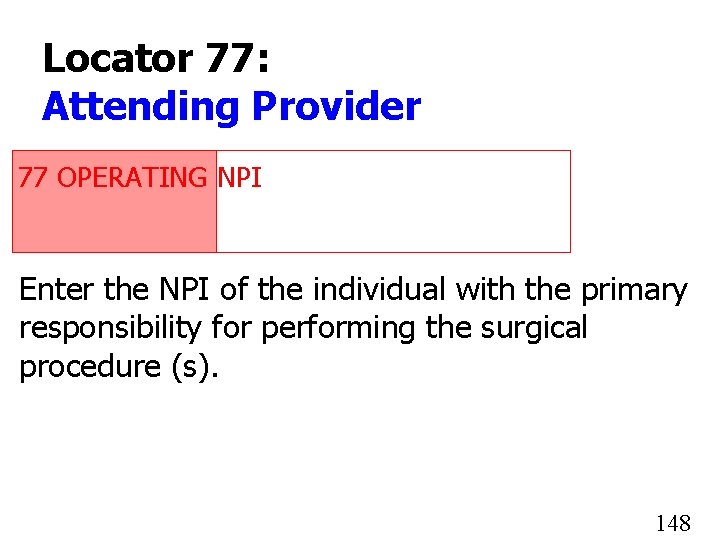
Locator 77: Attending Provider 77 OPERATING NPI 1234567890 Enter the NPI of the individual with the primary responsibility for performing the surgical procedure (s). 148
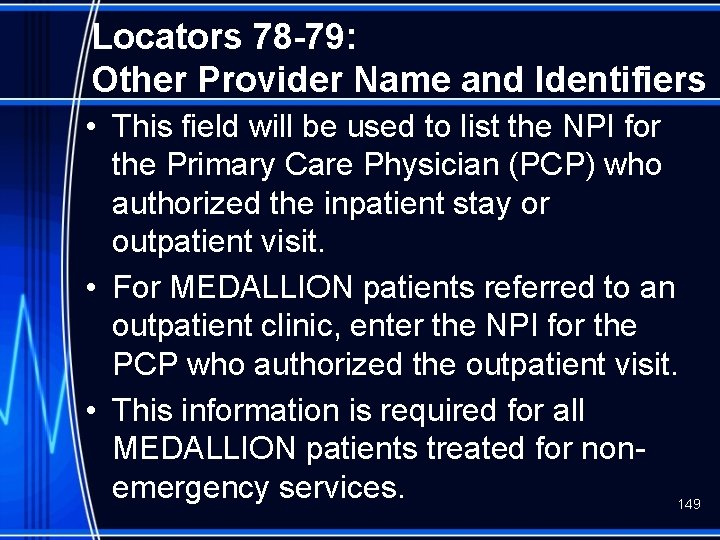
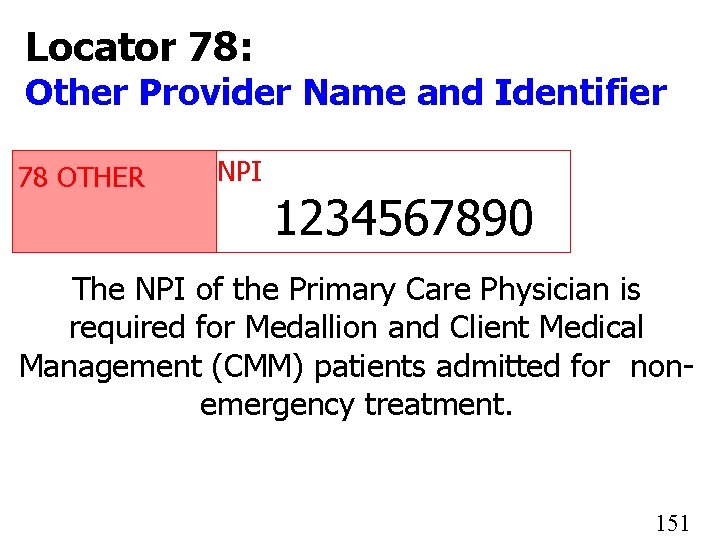
Locators 78 -79: Other Provider Name and Identifiers • This field will be used to list the NPI for the Primary Care Physician (PCP) who authorized the inpatient stay or outpatient visit. • For MEDALLION patients referred to an outpatient clinic, enter the NPI for the PCP who authorized the outpatient visit. • This information is required for all MEDALLION patients treated for nonemergency services. 149
Locators 78 -79: Other Provider Name and Identifiers • For Client Medical Management (CMM) patients referred to the emergency room by the PCP or admitted for non-emergency inpatient stay, enter the provider’s ID number and attach the Practitioner Referral Form (DMAS-70). 150
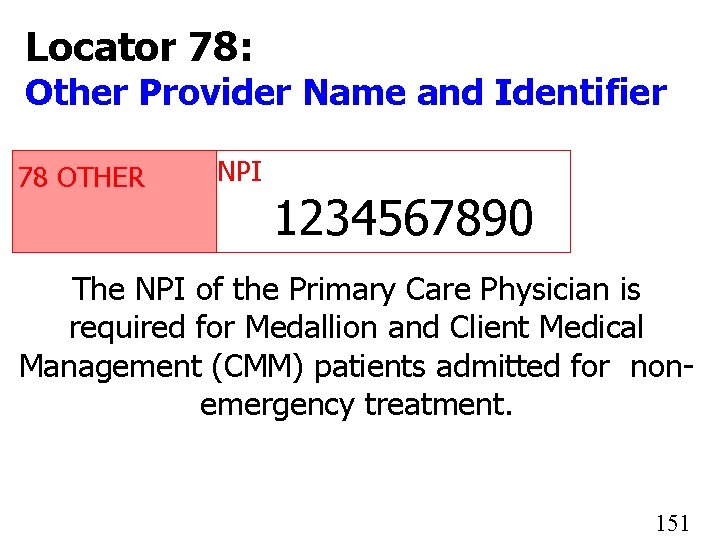
Locator 78: Other Provider Name and Identifier 78 OTHER NPI 1234567890 The NPI of the Primary Care Physician is required for Medallion and Client Medical Management (CMM) patients admitted for nonemergency treatment. 151
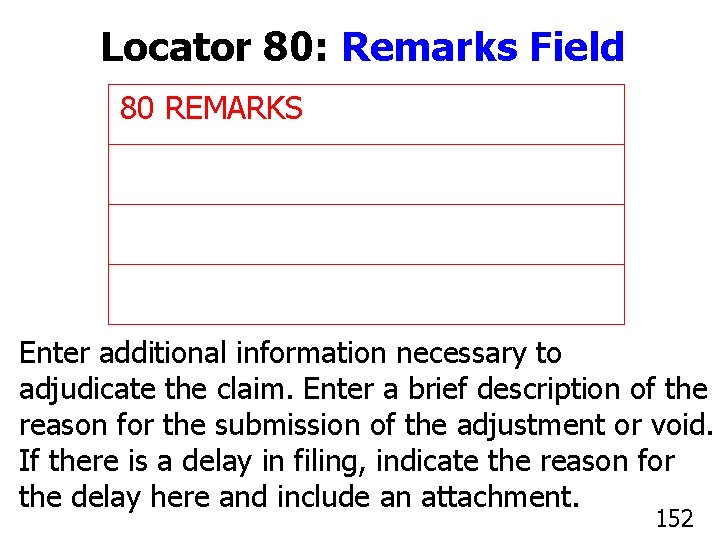
Locator 80: Remarks Field 80 REMARKS Enter additional information necessary to adjudicate the claim. Enter a brief description of the reason for the submission of the adjustment or void. If there is a delay in filing, indicate the reason for the delay here and include an attachment. 152
TAXONOMY Locator 81: Code-Code Field • DMAS will be using this field to capture a taxonomy code for claims that are submitted for one NPI with multiple business types or locations (e. g. , Rehabilitative or Psychiatric units within an acute care facility, Home Health Agency with multiple locations). 153
TAXONOMY Locator 81: Code-Code Field • The taxonomy code will be required for providers who do not have a separate NPI for each different service billed to VA Medicaid. • The taxonomy code will also be required for providers who have one NPI for multiple business locations. • Code B 3 is to be entered in the first small space and the provider taxonomy code is to be entered in the second large space. The 154 third space should be blank.
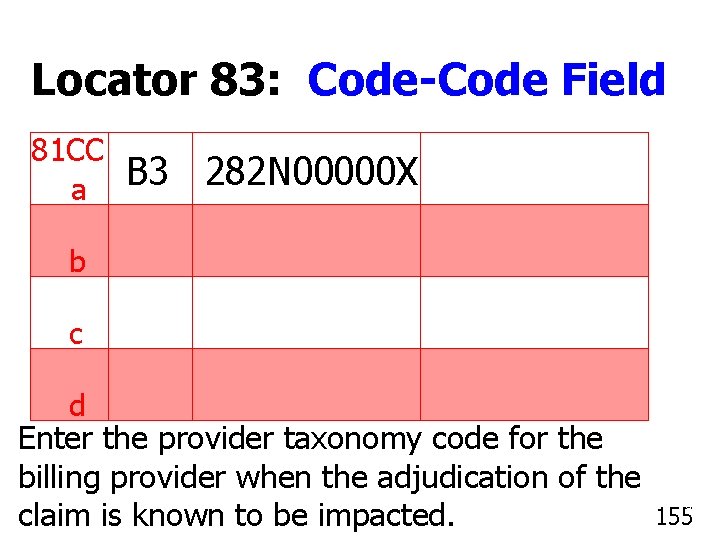
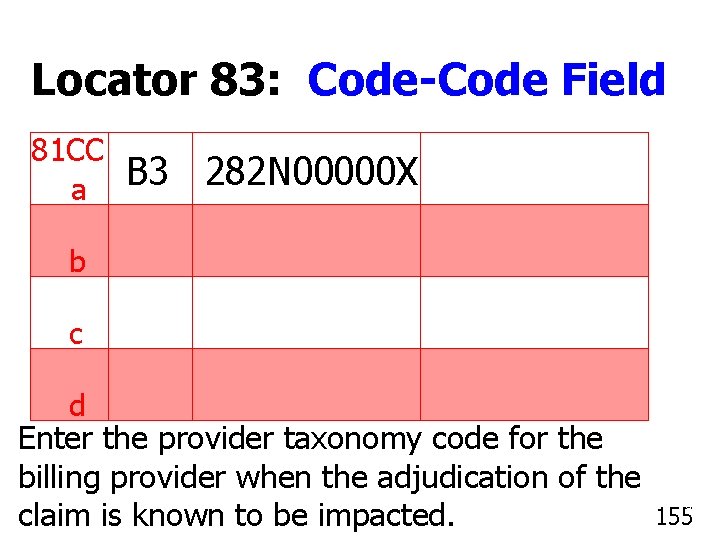
Locator 83: Code-Code Field 81 CC a B 3 282 N 00000 X b c d Enter the provider taxonomy code for the billing provider when the adjudication of the claim is known to be impacted. 155
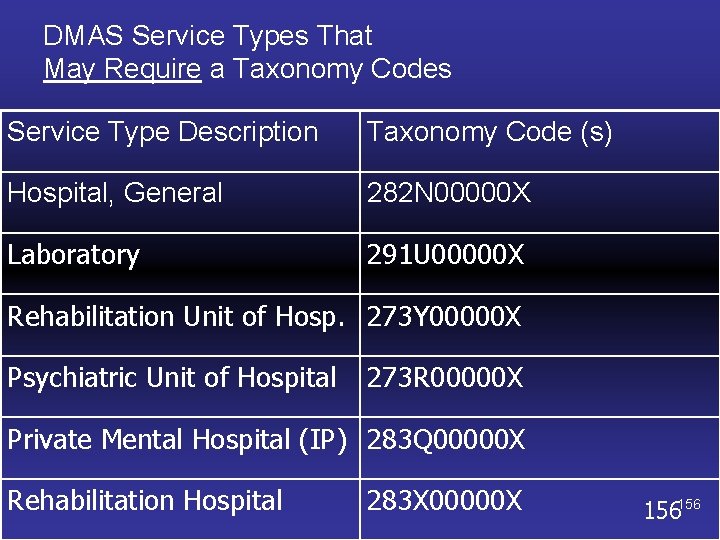
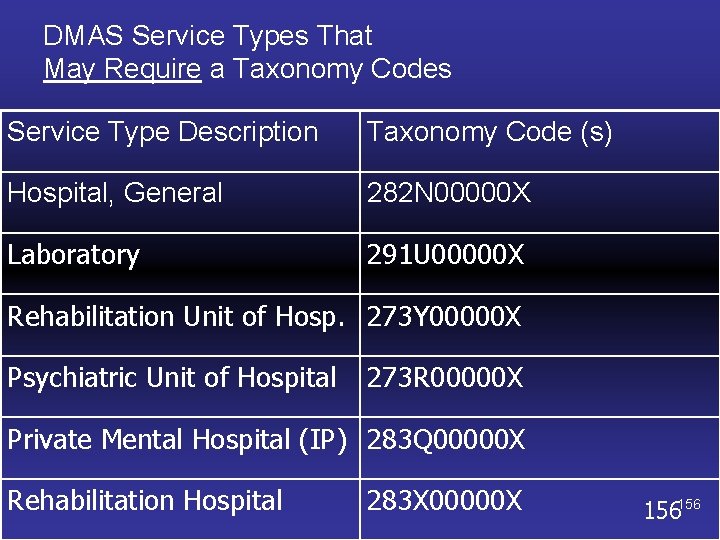
DMAS Service Types That May Require a Taxonomy Codes Service Type Description Taxonomy Code (s) Hospital, General 282 N 00000 X Laboratory 291 U 00000 X Rehabilitation Unit of Hosp. 273 Y 00000 X Psychiatric Unit of Hospital 273 R 00000 X Private Mental Hospital (IP) 283 Q 00000 X Rehabilitation Hospital 283 X 00000 X 156156
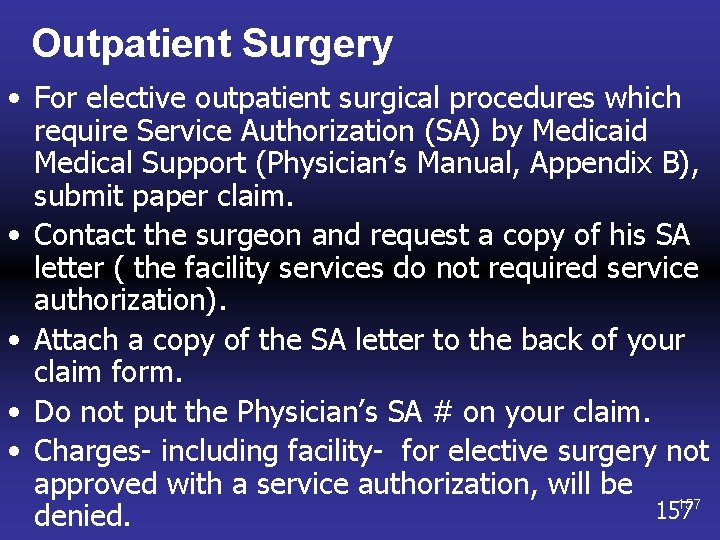
Outpatient Surgery • For elective outpatient surgical procedures which require Service Authorization (SA) by Medicaid Medical Support (Physician’s Manual, Appendix B), submit paper claim. • Contact the surgeon and request a copy of his SA letter ( the facility services do not required service authorization). • Attach a copy of the SA letter to the back of your claim form. • Do not put the Physician’s SA # on your claim. • Charges- including facility- for elective surgery not approved with a service authorization, will be 157 denied.
Medicare Primary Crossover Claims
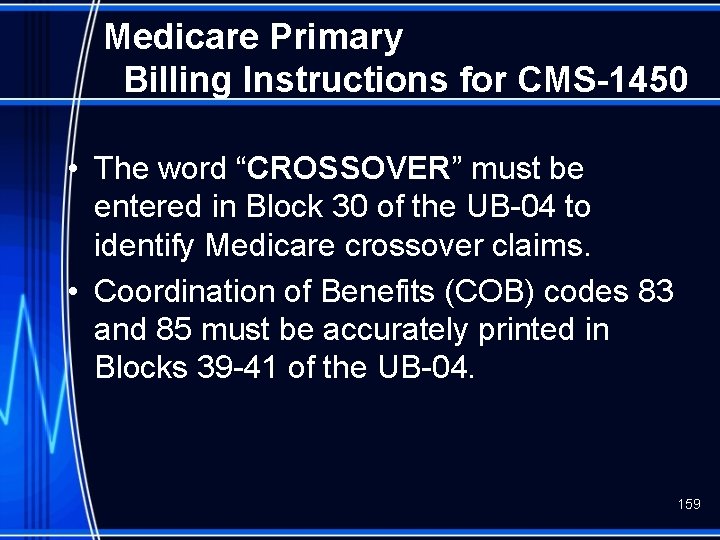
Medicare Primary Billing Instructions for CMS-1450 • The word “CROSSOVER” must be entered in Block 30 of the UB-04 to identify Medicare crossover claims. • Coordination of Benefits (COB) codes 83 and 85 must be accurately printed in Blocks 39 -41 of the UB-04. 159
Medicare Primary Billing Instructions for CMS-1450 • The first occurrence code 83 indicates that Medicare paid and there should always be a dollar value associated with this code. The A 1 indicates Medicare deductible and code A 2 indicates Medicare coinsurance 160
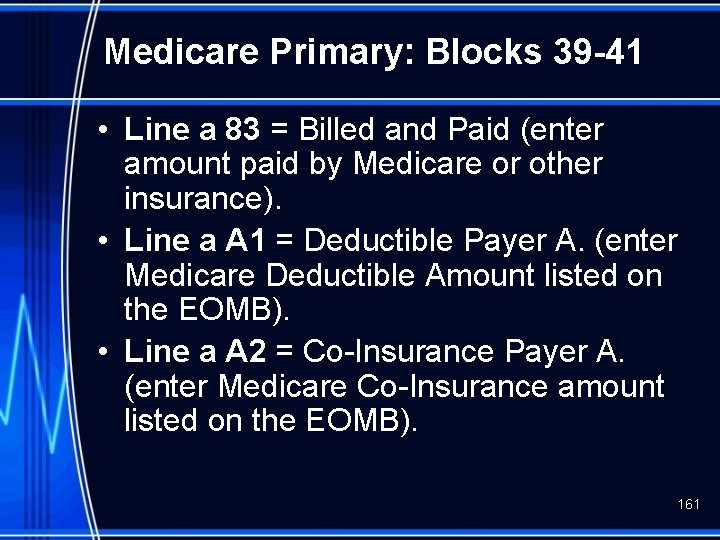
Medicare Primary: Blocks 39 -41 • Line a 83 = Billed and Paid (enter amount paid by Medicare or other insurance). • Line a A 1 = Deductible Payer A. (enter Medicare Deductible Amount listed on the EOMB). • Line a A 2 = Co-Insurance Payer A. (enter Medicare Co-Insurance amount listed on the EOMB). 161
Medicare Primary Billing Instructions for CMS-1450 • Note: Complete all information in Locators 39 a through 41 a first (payments by Medicare or payments by other insurance) before entering information in 39 b through 41 b locators etc. • COB code 85 is to be used when another insurance carrier is billed and there is no payment from that carrier. • For the deductibles and co-insurance due from any other carrier (s) (not Medicare) the code for reporting the amount paid is B 1 for the deductibles and B 2 for the coinsurance. 162
Medicare Exhaust Days • MEDICARE PRIMARY/Days Exhausted – Service authorization from Ke. PRO is required. – Proof of exhausted Medicare days must be submitted with service authorization request. 163
Medicare Exhaust Days • All days must be billed. • Initial stay less than 120 days, bill type 0111. • First 120 days bill type 0112 – next 120 days bill type 0113 – continue bill type 0113 for any additional 120 day periods. • Final bill type 0114. 164
Medicare Exhaust Days • Providers should list the amount Medicare paid on the 0112 bill type (less than 120 days list payment on 0111 bill type). • Medicare payment should be listed in Block 39 a and use COB code 83 (billed and paid). 165
Medicare Exhaust Days • DO NOT WRITE the word CROSSOVER in Block 30 (Medicare is exhausted and the days billed to Medicaid were not paid by Medicare) • Block 80 - providers MUST put write a statement MEDICARE DAYS EXHAUSTED and attach something showing Medicare exhausted (Medicare EOB). 166
Medicare Exhaust Days • If Medicaid has considered a crossover claim for deductible and coinsurance on days Medicare paid or any Part B charges– If the provider keeps all charges on the claim submitted for Medicare Exhaust days, all payments must be listed. – If the provider deletes Part B charges, do not list any Part B payment amounts. 167
Special Note • If the Medicaid member does not have Part A coverage, the COB code should be 82 (No Other Coverage). 168
Department of Medical Assistance Services THANK YOU www. dmas. virginia. gov
 Logisticare transportation texas
Logisticare transportation texas Kaiser permanente community benefit
Kaiser permanente community benefit Transitional medical assistance ohio
Transitional medical assistance ohio Darb medicaid
Darb medicaid Legal assistance services townsville
Legal assistance services townsville Bac pro service accueil assistance conseil
Bac pro service accueil assistance conseil Medical ethics 101
Medical ethics 101 Importance of medical records department
Importance of medical records department Medical education and drugs department
Medical education and drugs department Wells fargo merchant services
Wells fargo merchant services Iowa department of health and human services
Iowa department of health and human services Worcester inspectional services
Worcester inspectional services Washington state department of social and health services
Washington state department of social and health services Elements of a system of care
Elements of a system of care Florida department of agriculture and consumer services
Florida department of agriculture and consumer services Joshua deshaney mother
Joshua deshaney mother Caldwell county child protective services
Caldwell county child protective services Albany county department of social services
Albany county department of social services Seattle human services department
Seattle human services department Miami dade county internal services department
Miami dade county internal services department Icg grant illinois
Icg grant illinois Department of correctional services strategic plan
Department of correctional services strategic plan Virginia department of agriculture and consumer services
Virginia department of agriculture and consumer services California department of general services
California department of general services New york state division of criminal justice services
New york state division of criminal justice services Mussd
Mussd Department of health and senior services missouri
Department of health and senior services missouri Cacfp nebraska
Cacfp nebraska New hampshire department of administrative services
New hampshire department of administrative services Dms state of florida
Dms state of florida Milwaukee health and human services
Milwaukee health and human services Maine department of health and human services
Maine department of health and human services Delaware county department of human services
Delaware county department of human services Ptal california medical board
Ptal california medical board Gbmc medical records
Gbmc medical records Hepburn osteometric board
Hepburn osteometric board Torrance memorial tcu
Torrance memorial tcu Cartersville medical center medical records
Cartersville medical center medical records Wyoming acs web portal
Wyoming acs web portal Wyoming medicaid provider manual
Wyoming medicaid provider manual Wisconsin long term care partnership program
Wisconsin long term care partnership program Heather dane
Heather dane Unicare
Unicare Eapg medicaid
Eapg medicaid Mita medicaid
Mita medicaid Medicare vs medicaid washington state
Medicare vs medicaid washington state Louisiana ppm 49
Louisiana ppm 49 Medicaid eligibility florida
Medicaid eligibility florida Www.anthem.com/kymedicaid
Www.anthem.com/kymedicaid Acupuncturist medicaid
Acupuncturist medicaid Ohio medicaid insurance
Ohio medicaid insurance Medicaid transformation project
Medicaid transformation project Wyoming medicaid travel reimbursement
Wyoming medicaid travel reimbursement Medicaid integrity institute
Medicaid integrity institute Magellan medicaid administration
Magellan medicaid administration Medicaid claims data
Medicaid claims data Molina medicaid solutions west virginia
Molina medicaid solutions west virginia Iowa waiver comparison chart
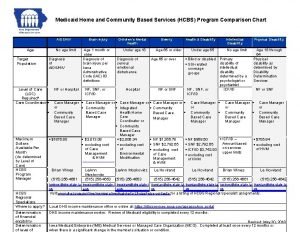
Iowa waiver comparison chart Medicaid wyoming
Medicaid wyoming Daniel timins
Daniel timins Logan ahs
Logan ahs Rowan county medicaid
Rowan county medicaid Alabama coordinated health network
Alabama coordinated health network Prism utah medicaid
Prism utah medicaid Texas health steps
Texas health steps Dc medicaid 719a form
Dc medicaid 719a form Logisticare suffolk county
Logisticare suffolk county Medicaid spending
Medicaid spending Enterprise management system
Enterprise management system Wyoming medicaid trust
Wyoming medicaid trust Nys office of medicaid inspector general
Nys office of medicaid inspector general Hbs medicaid
Hbs medicaid Pennsylvania evv
Pennsylvania evv Weathermen apush
Weathermen apush Kepro authorization forms
Kepro authorization forms Louisiana medicaid fraud control unit
Louisiana medicaid fraud control unit Medicaid transportation palm beach county
Medicaid transportation palm beach county Mmsea act of 2007
Mmsea act of 2007 Medicaid management information system (mmis)
Medicaid management information system (mmis) Arizona medicaid evv
Arizona medicaid evv Tricia roddy
Tricia roddy Wi estate recovery program
Wi estate recovery program Wnyhealthenet
Wnyhealthenet Paris project medicaid
Paris project medicaid Nylag medicaid
Nylag medicaid New york state medicaid prior authorization
New york state medicaid prior authorization National association of state medicaid directors
National association of state medicaid directors Eric seiber
Eric seiber Ny medicaid ehr incentive program
Ny medicaid ehr incentive program Community coverage w/cbltc
Community coverage w/cbltc Nhi medicaid
Nhi medicaid Indiana medicaid code sets
Indiana medicaid code sets Incidental medical services
Incidental medical services Medical social worker
Medical social worker Dr veronica mckinney
Dr veronica mckinney Florida association of medical staff services
Florida association of medical staff services Integrated services vs differentiated services
Integrated services vs differentiated services Wake county human services community services center
Wake county human services community services center Weatherization assistance program virginia
Weatherization assistance program virginia Employee assistance program washington
Employee assistance program washington Types of user support
Types of user support Writ of assistance
Writ of assistance Nc victim assistance network
Nc victim assistance network Social assistance definition
Social assistance definition Seminole county rental assistance
Seminole county rental assistance General assistance sf
General assistance sf Sagkeeng social assistance
Sagkeeng social assistance Riverside first time homebuyer program
Riverside first time homebuyer program Operational coordination is considered
Operational coordination is considered Nehemiah down payment assistance
Nehemiah down payment assistance Dr jennifer walden
Dr jennifer walden Ksas apply online
Ksas apply online Intervention assistance team
Intervention assistance team Immediate assistance
Immediate assistance Social assistance definition
Social assistance definition Discretionary assistance fund
Discretionary assistance fund Community lending pool
Community lending pool Employee assistance program townsville
Employee assistance program townsville Atap nevada
Atap nevada California fire assistance agreement
California fire assistance agreement Valeap
Valeap Usf eap
Usf eap Urban league energy assistance
Urban league energy assistance Careways employee wellness programme
Careways employee wellness programme American legion financial assistance
American legion financial assistance State of texas emergency assistance registry
State of texas emergency assistance registry Nsclsc
Nsclsc Industrial research assistance program
Industrial research assistance program Weatherization assistance program missouri
Weatherization assistance program missouri Leveraging educational assistance partnership
Leveraging educational assistance partnership Industrial research assistance program
Industrial research assistance program Hara rental assistance
Hara rental assistance Mflc fort gordon
Mflc fort gordon Export marketing and investment assistance
Export marketing and investment assistance Heat assistance iowa
Heat assistance iowa Assistance vitale de base
Assistance vitale de base Adfa income limits
Adfa income limits Special circumstances instructional assistance assessment
Special circumstances instructional assistance assessment Spartanburg housing authority
Spartanburg housing authority Osha compliance assistance
Osha compliance assistance Writing assistance inc
Writing assistance inc Nottingham private rented assistance scheme
Nottingham private rented assistance scheme Missouri state health insurance assistance program
Missouri state health insurance assistance program Newcap weatherization program
Newcap weatherization program Gap tuition assistance program
Gap tuition assistance program Travel assistance center
Travel assistance center Casualty notification officer training
Casualty notification officer training Aurora eap
Aurora eap Wv dhhr child care assistance
Wv dhhr child care assistance Definition of nursing by virginia henderson
Definition of nursing by virginia henderson Nde rule 51 technical assistance document
Nde rule 51 technical assistance document Writs of assistance
Writs of assistance Writs of assistance
Writs of assistance Saf student loan
Saf student loan What is seed capital assistance
What is seed capital assistance Active assistance rom
Active assistance rom Axa assistance panama canal area benefit plan
Axa assistance panama canal area benefit plan Insurance program administrators
Insurance program administrators Flood mitigation assistance program
Flood mitigation assistance program Poea legal assistance
Poea legal assistance Navigational assistance service
Navigational assistance service Apeda financial assistance scheme
Apeda financial assistance scheme Marketing development assistance
Marketing development assistance Council for mutual economic assistance
Council for mutual economic assistance Council for mutual economic assistance
Council for mutual economic assistance Practical assistance for expatriates
Practical assistance for expatriates Practical assistance for expatriates
Practical assistance for expatriates Humira abbvie patient assistance
Humira abbvie patient assistance Pekao eurokonto aktywne plus ubezpieczenie
Pekao eurokonto aktywne plus ubezpieczenie Sample technical assistance given to teachers
Sample technical assistance given to teachers