Kentucky Department for Medicaid Services Magellan Medicaid Administration

- Slides: 32
Kentucky Department for Medicaid Services & Magellan Medicaid Administration
Website Changes https: //kentucky. magellanmedicaid. com
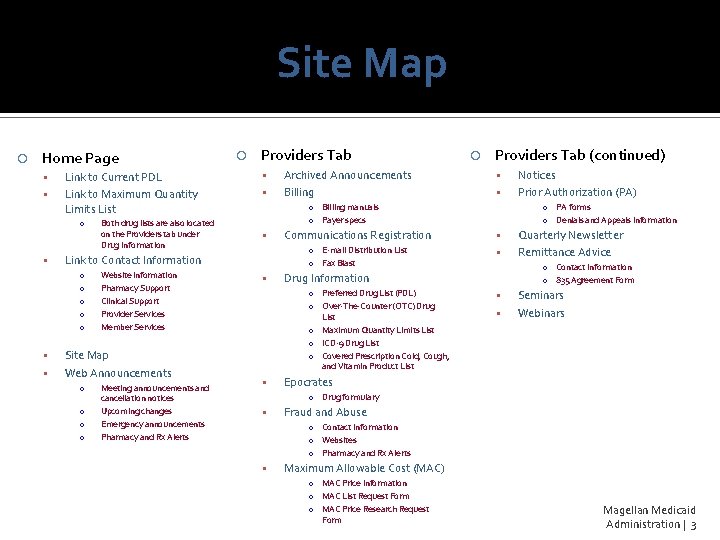
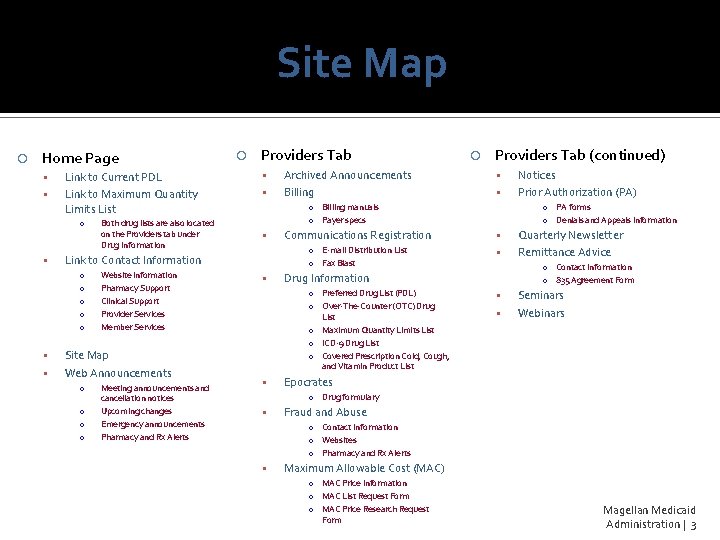
Site Map Home Page Link to Current PDL Link to Maximum Quantity Limits List o Providers Tab Website information Pharmacy Support Clinical Support Provider Services Member Services Site Map Web Announcements o o Meeting announcements and cancellation notices Upcoming changes Emergency announcements Pharmacy and Rx Alerts Archived Announcements Billing Providers Tab (continued) o Billing manuals o Payer specs Link to Contact Information o o o Both drug lists are also located on the Providers tab under Drug Information o E-mail Distribution List o Fax Blast Quarterly Newsletter Remittance Advice o Contact Information o 835 Agreement Form Drug Information List o Maximum Quantity Limits List o ICD-9 Drug List o Covered Prescription Cold, Cough, and Vitamin Product List o PA forms o Denials and Appeals Information Communications Registration o Preferred Drug List (PDL) o Over-The-Counter (OTC) Drug Notices Prior Authorization (PA) Seminars Webinars Epocrates o Drug formulary Fraud and Abuse o Contact Information o Websites o Pharmacy and Rx Alerts Maximum Allowable Cost (MAC) o MAC Price Information o MAC List Request Form o MAC Price Research Request Form Magellan Medicaid Administration | 3
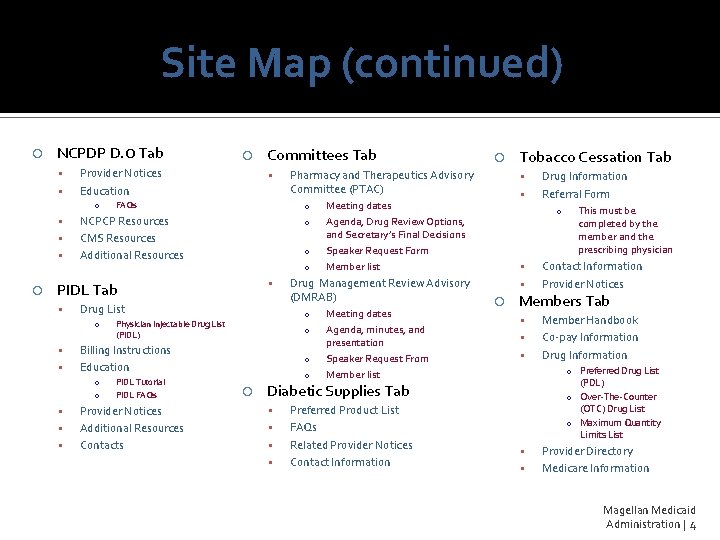
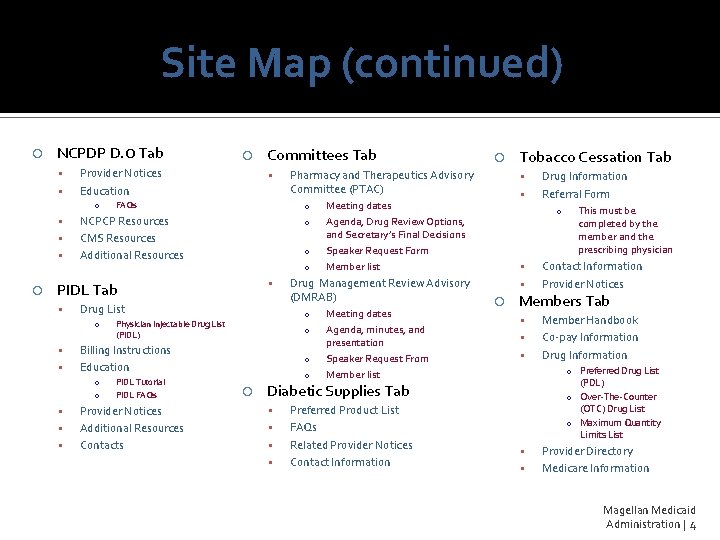
Site Map (continued) NCPDP D. 0 Tab Provider Notices Education o FAQs NCPCP Resources CMS Resources Additional Resources o o o Drug List o Billing Instructions Education o o o PIDL Tutorial PIDL FAQs Provider Notices Additional Resources Contacts o o Meeting dates Agenda, minutes, and presentation Speaker Request From Member list Tobacco Cessation Tab Meeting dates Agenda, Drug Review Options, and Secretary’s Final Decisions Speaker Request Form Member list Drug Management Review Advisory (DMRAB) o Physician Injectable Drug List (PIDL) Pharmacy and Therapeutics Advisory Committee (PTAC) o PIDL Tab Committees Tab o Preferred Product List FAQs Related Provider Notices Contact Information This must be completed by the member and the prescribing physician Contact Information Provider Notices Members Tab Member Handbook Co-pay Information Drug Information o Preferred Drug List (PDL) o Over-The-Counter (OTC) Drug List o Maximum Quantity Limits List Diabetic Supplies Tab Drug Information Referral Form Provider Directory Medicare Information Magellan Medicaid Administration | 4
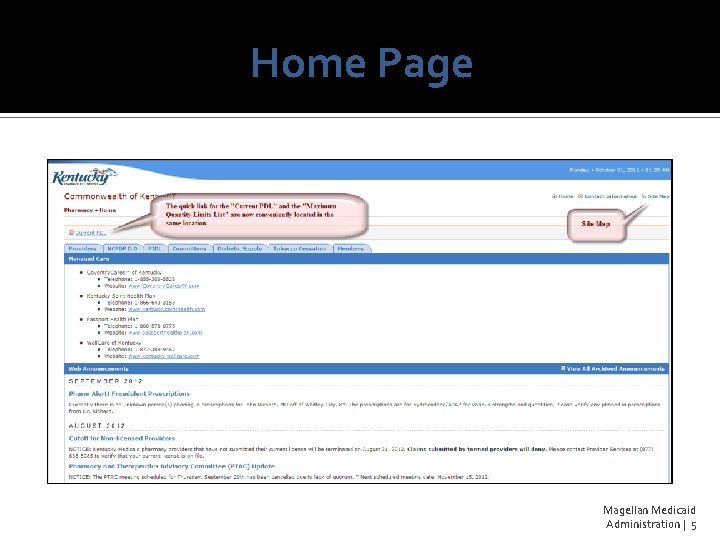
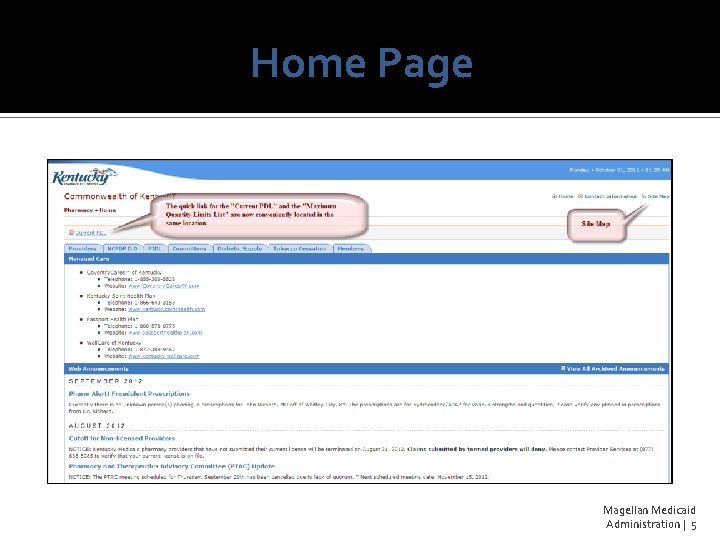
Home Page Magellan Medicaid Administration | 5
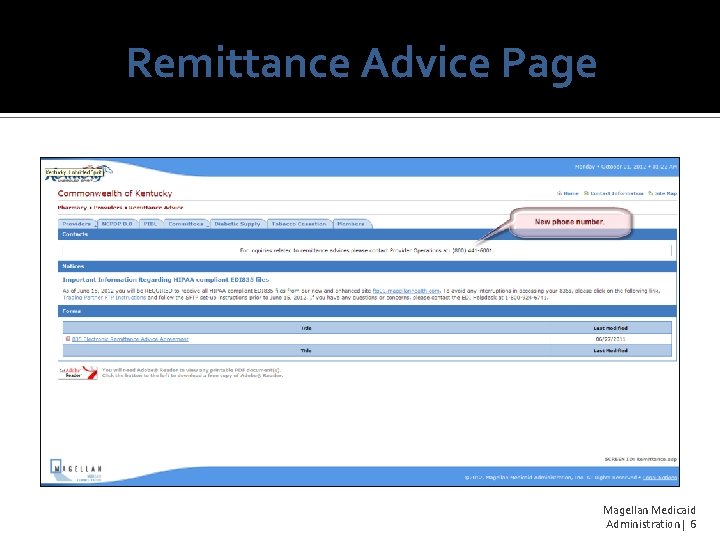
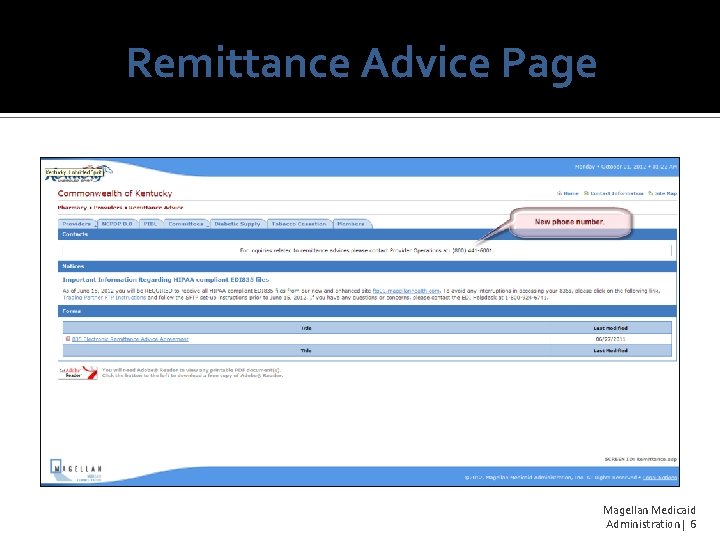
Remittance Advice Page Magellan Medicaid Administration | 6
Drug List Changes Magellan Medicaid Administration | 7
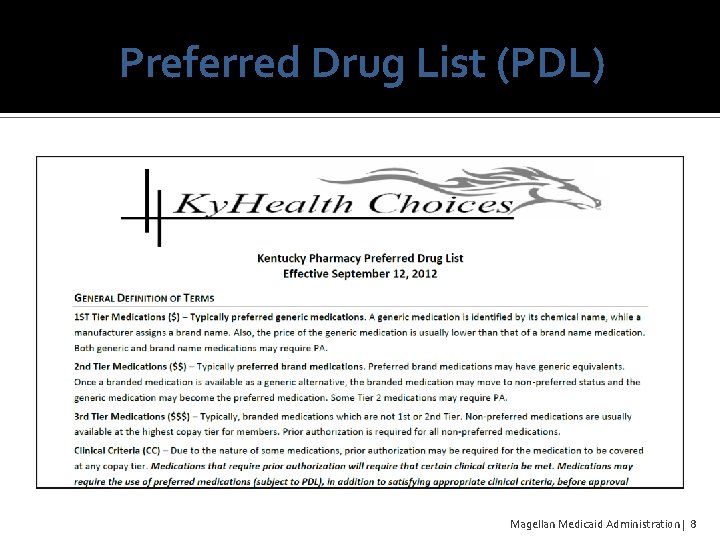
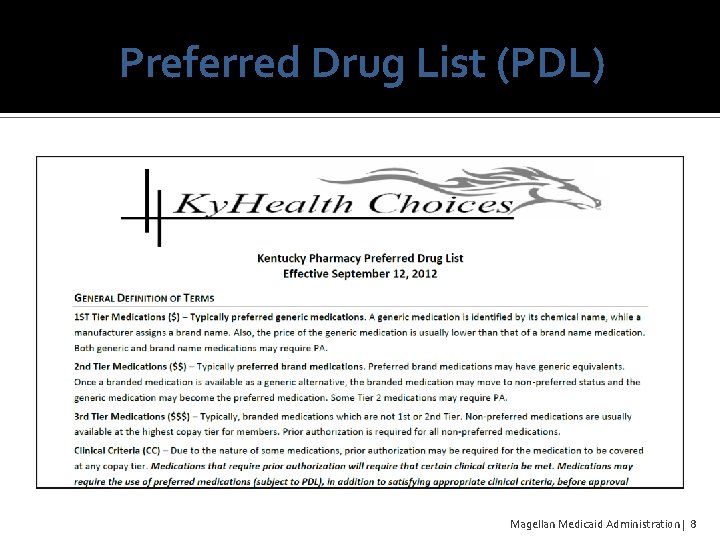
Preferred Drug List (PDL) Magellan Medicaid Administration | 8
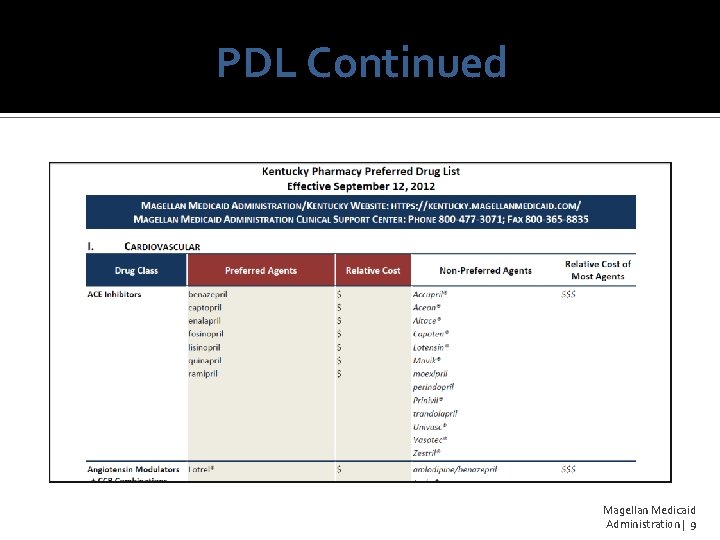
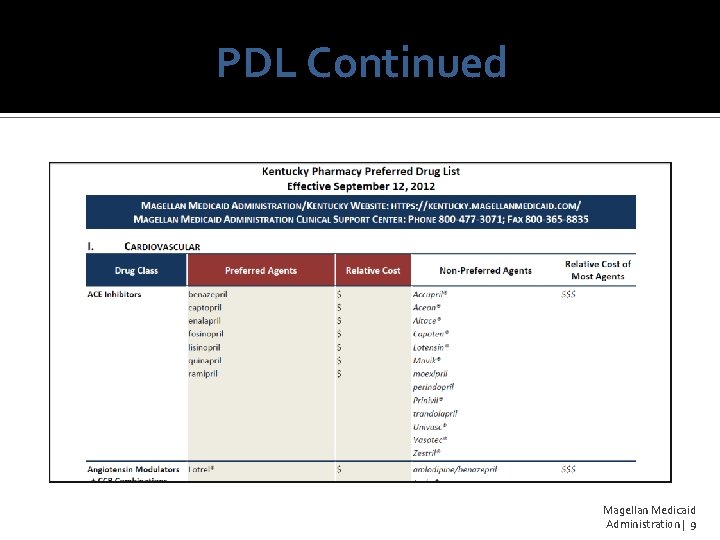
PDL Continued Magellan Medicaid Administration | 9
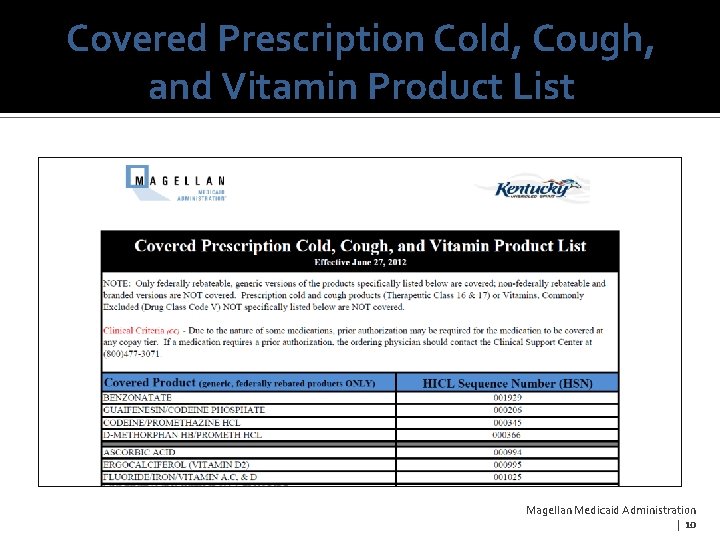
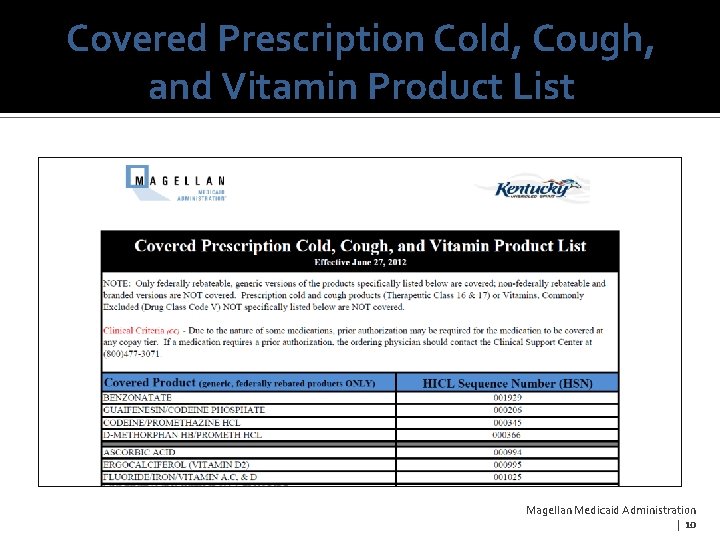
Covered Prescription Cold, Cough, and Vitamin Product List Magellan Medicaid Administration | 10
Billing Changes Magellan Medicaid Administration | 11
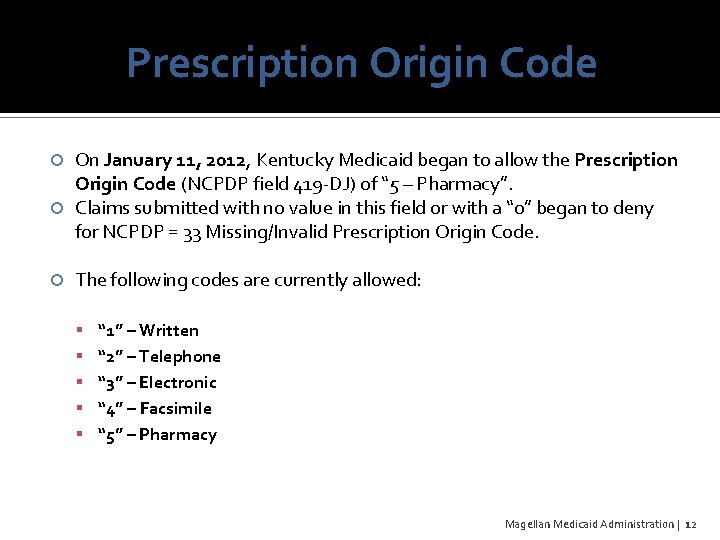
Prescription Origin Code On January 11, 2012, Kentucky Medicaid began to allow the Prescription Origin Code (NCPDP field 419 -DJ) of “ 5 – Pharmacy”. Claims submitted with no value in this field or with a “ 0” began to deny for NCPDP = 33 Missing/Invalid Prescription Origin Code. The following codes are currently allowed: “ 1” – Written “ 2” – Telephone “ 3” – Electronic “ 4” – Facsimile “ 5” – Pharmacy Magellan Medicaid Administration | 12
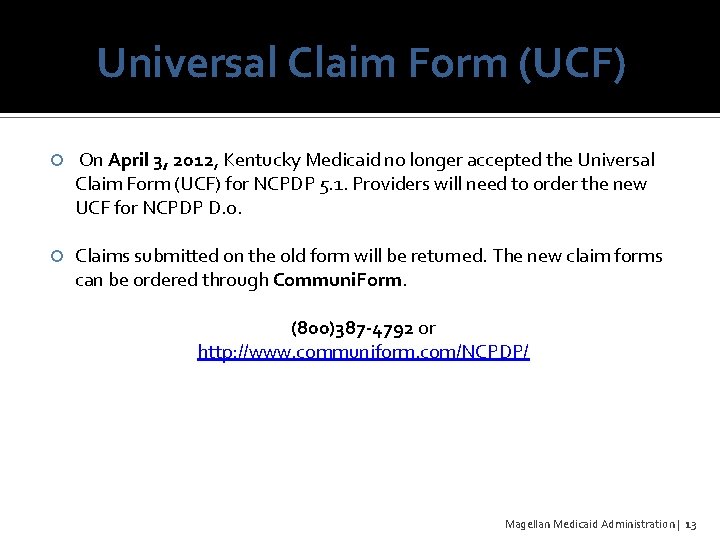
Universal Claim Form (UCF) On April 3, 2012, Kentucky Medicaid no longer accepted the Universal Claim Form (UCF) for NCPDP 5. 1. Providers will need to order the new UCF for NCPDP D. 0. Claims submitted on the old form will be returned. The new claim forms can be ordered through Communi. Form. (800)387 -4792 or http: //www. communiform. com/NCPDP/ Magellan Medicaid Administration | 13
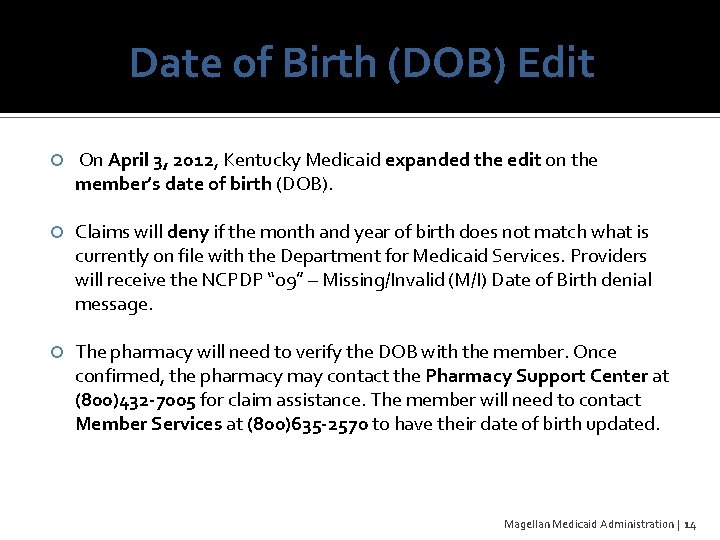
Date of Birth (DOB) Edit On April 3, 2012, Kentucky Medicaid expanded the edit on the member’s date of birth (DOB). Claims will deny if the month and year of birth does not match what is currently on file with the Department for Medicaid Services. Providers will receive the NCPDP “ 09” – Missing/Invalid (M/I) Date of Birth denial message. The pharmacy will need to verify the DOB with the member. Once confirmed, the pharmacy may contact the Pharmacy Support Center at (800)432 -7005 for claim assistance. The member will need to contact Member Services at (800)635 -2570 to have their date of birth updated. Magellan Medicaid Administration | 14
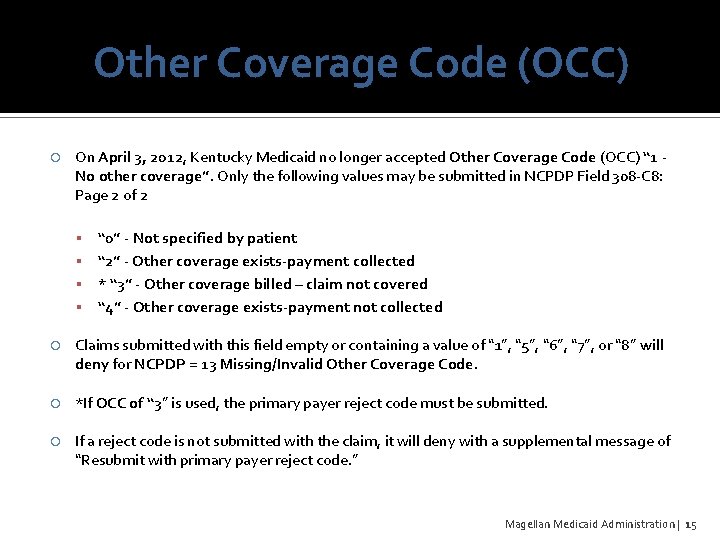
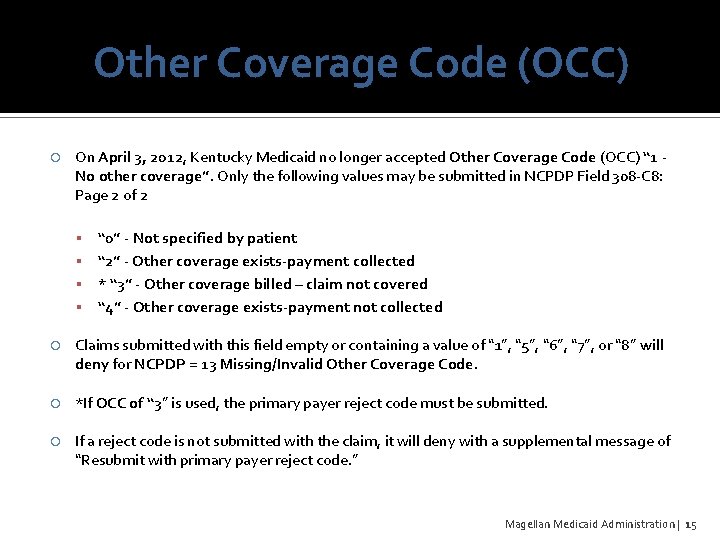
Other Coverage Code (OCC) On April 3, 2012, Kentucky Medicaid no longer accepted Other Coverage Code (OCC) “ 1 No other coverage”. Only the following values may be submitted in NCPDP Field 308 -C 8: Page 2 of 2 “ 0” - Not specified by patient “ 2” - Other coverage exists-payment collected * “ 3” - Other coverage billed – claim not covered “ 4” - Other coverage exists-payment not collected Claims submitted with this field empty or containing a value of “ 1”, “ 5”, “ 6”, “ 7”, or “ 8” will deny for NCPDP = 13 Missing/Invalid Other Coverage Code. *If OCC of “ 3” is used, the primary payer reject code must be submitted. If a reject code is not submitted with the claim, it will deny with a supplemental message of “Resubmit with primary payer reject code. ” Magellan Medicaid Administration | 15
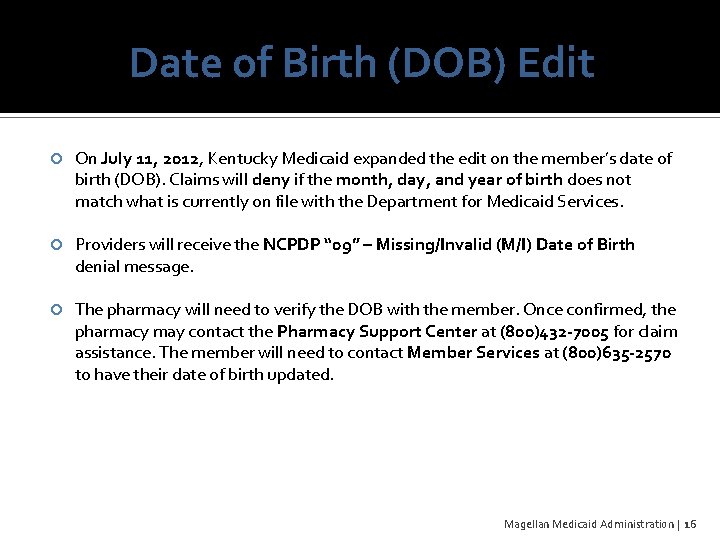
Date of Birth (DOB) Edit On July 11, 2012, Kentucky Medicaid expanded the edit on the member’s date of birth (DOB). Claims will deny if the month, day, and year of birth does not match what is currently on file with the Department for Medicaid Services. Providers will receive the NCPDP “ 09” – Missing/Invalid (M/I) Date of Birth denial message. The pharmacy will need to verify the DOB with the member. Once confirmed, the pharmacy may contact the Pharmacy Support Center at (800)432 -7005 for claim assistance. The member will need to contact Member Services at (800)635 -2570 to have their date of birth updated. Magellan Medicaid Administration | 16
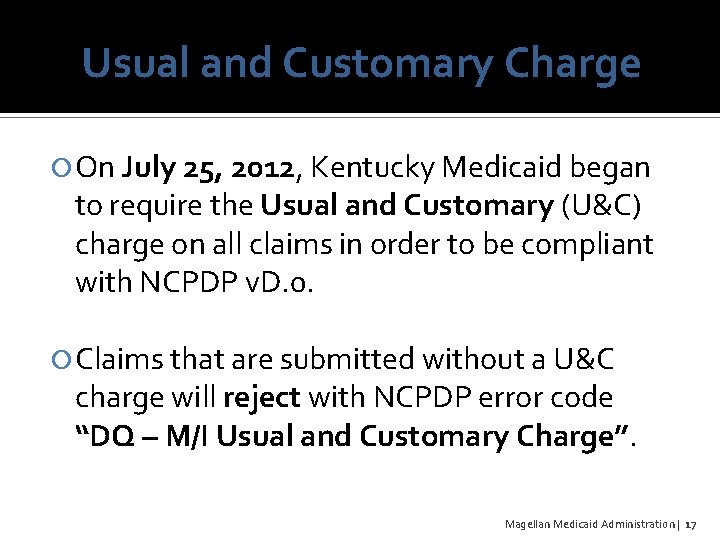
Usual and Customary Charge On July 25, 2012, Kentucky Medicaid began to require the Usual and Customary (U&C) charge on all claims in order to be compliant with NCPDP v. D. 0. Claims that are submitted without a U&C charge will reject with NCPDP error code “DQ – M/I Usual and Customary Charge”. Magellan Medicaid Administration | 17

Policy Changes Magellan Medicaid Administration | 18
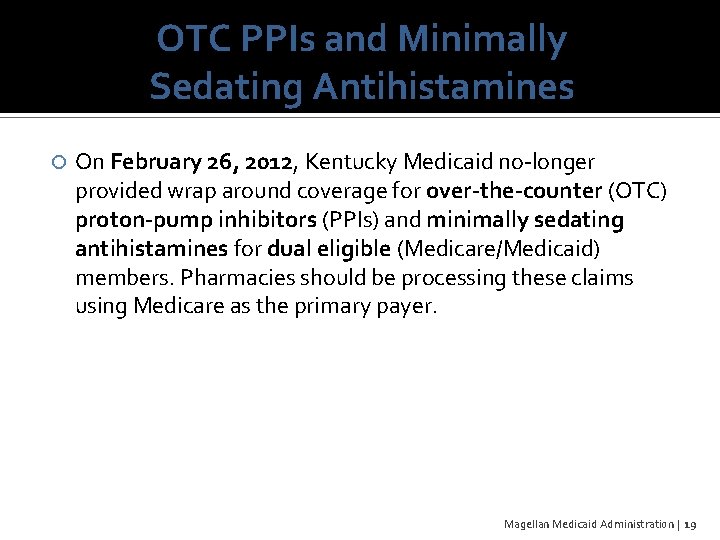
OTC PPIs and Minimally Sedating Antihistamines On February 26, 2012, Kentucky Medicaid no-longer provided wrap around coverage for over-the-counter (OTC) proton-pump inhibitors (PPIs) and minimally sedating antihistamines for dual eligible (Medicare/Medicaid) members. Pharmacies should be processing these claims using Medicare as the primary payer. Magellan Medicaid Administration | 19
Prior Authorization (PA) On April 3, 2012, Kentucky Medicaid made the following change to reimbursement on medications that require prior authorization: “Reimbursement shall be denied if prior authorization is required by the department and the request for prior authorization has not been submitted prior to dispensing the drug. ” Magellan Medicaid Administration | 20
Website Reminders Magellan Medicaid Administration | 21
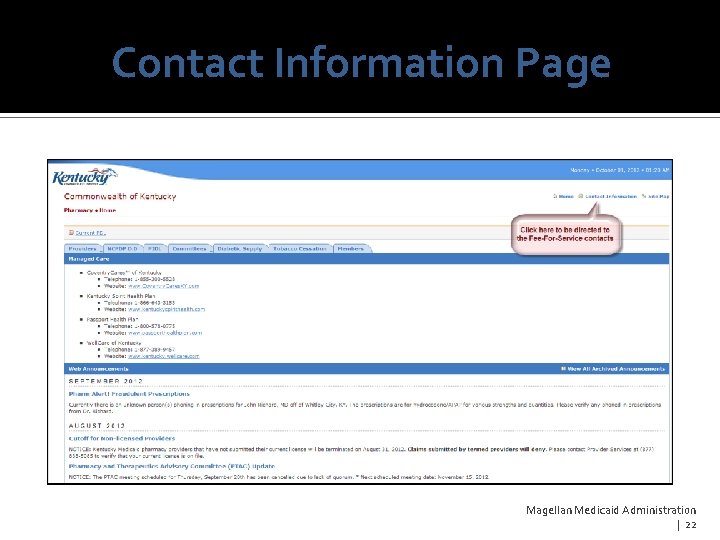
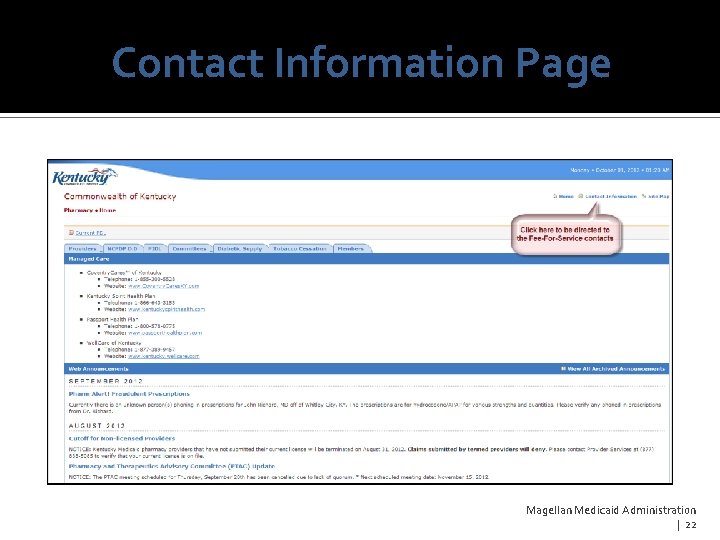
Contact Information Page Magellan Medicaid Administration | 22
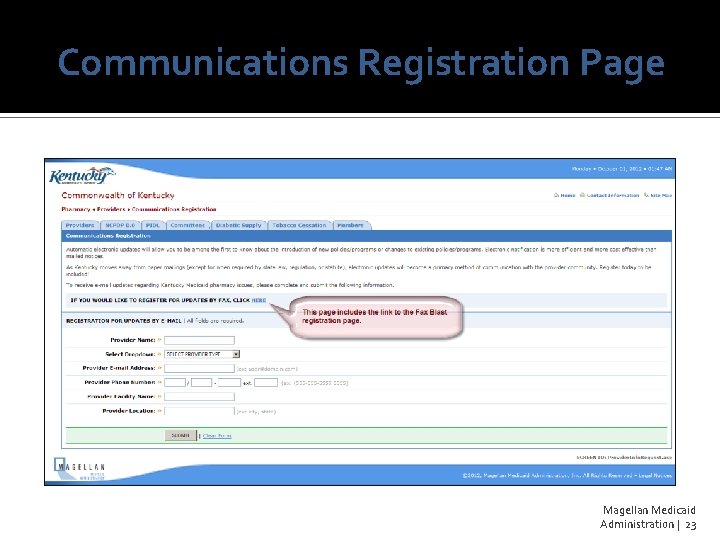
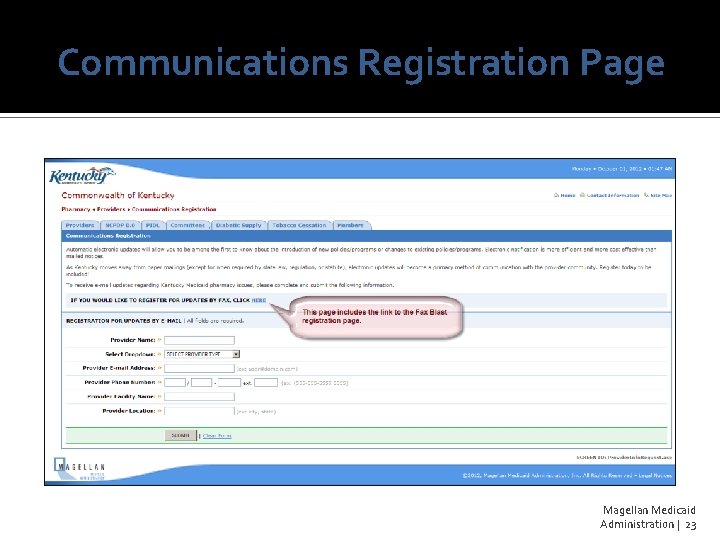
Communications Registration Page Magellan Medicaid Administration | 23
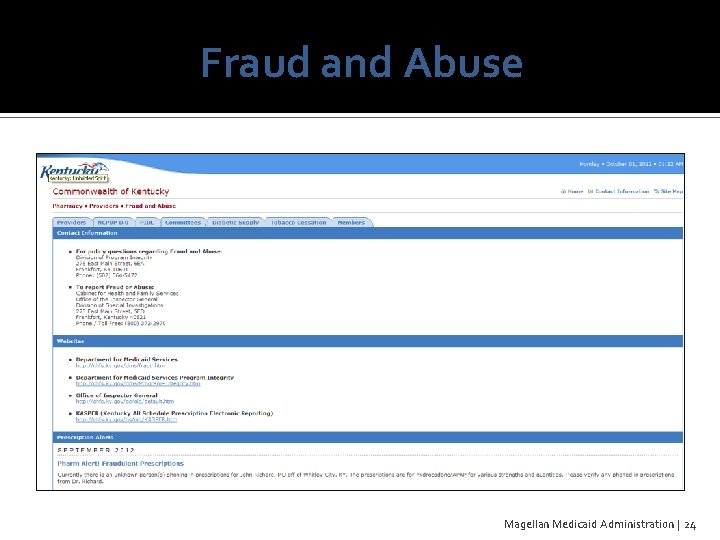
Fraud and Abuse Magellan Medicaid Administration | 24
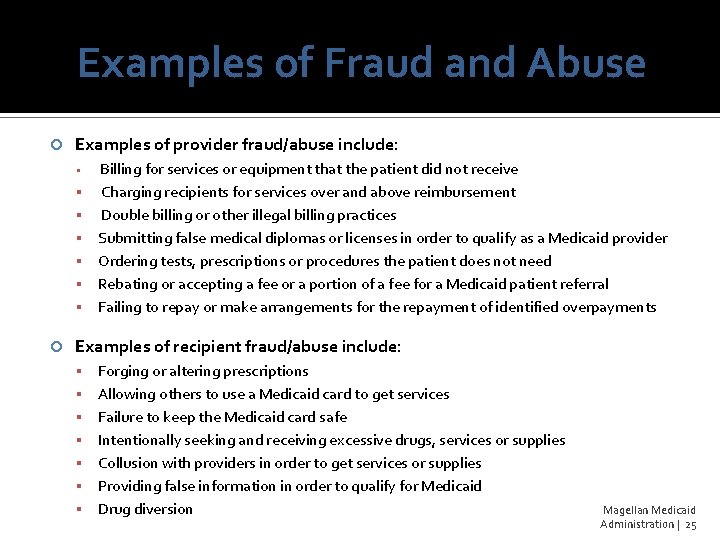
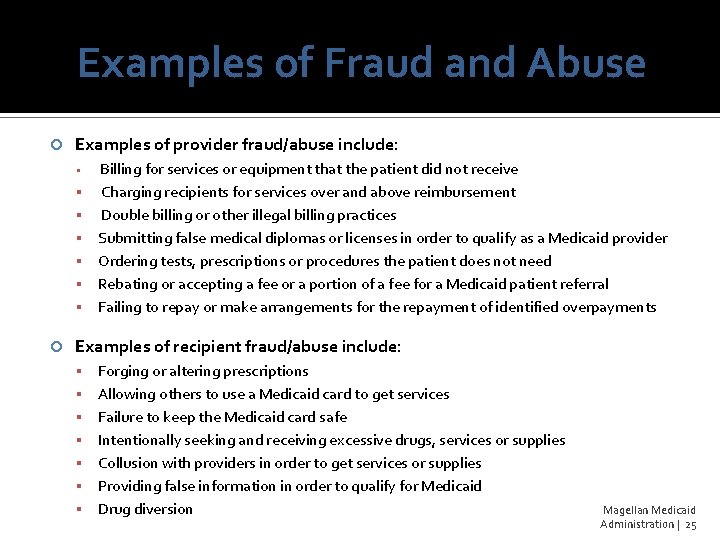
Examples of Fraud and Abuse Examples of provider fraud/abuse include: Billing for services or equipment that the patient did not receive Charging recipients for services over and above reimbursement Double billing or other illegal billing practices Submitting false medical diplomas or licenses in order to qualify as a Medicaid provider Ordering tests, prescriptions or procedures the patient does not need Rebating or accepting a fee or a portion of a fee for a Medicaid patient referral Failing to repay or make arrangements for the repayment of identified overpayments Examples of recipient fraud/abuse include: Forging or altering prescriptions Allowing others to use a Medicaid card to get services Failure to keep the Medicaid card safe Intentionally seeking and receiving excessive drugs, services or supplies Collusion with providers in order to get services or supplies Providing false information in order to qualify for Medicaid Drug diversion Magellan Medicaid Administration | 25
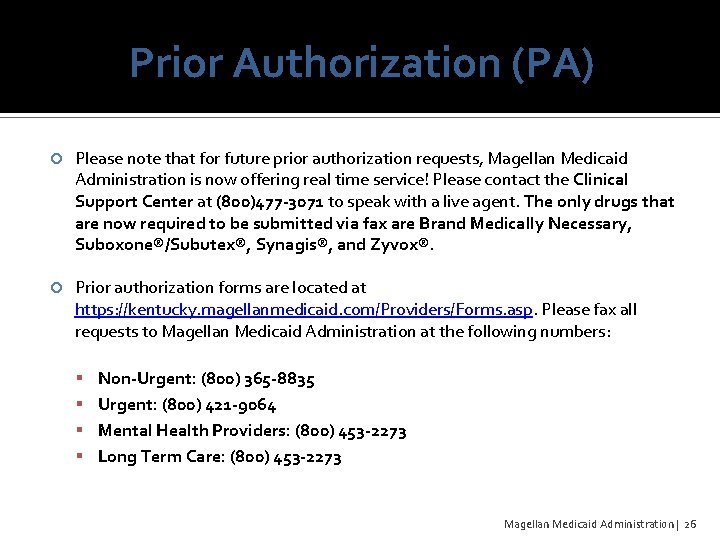
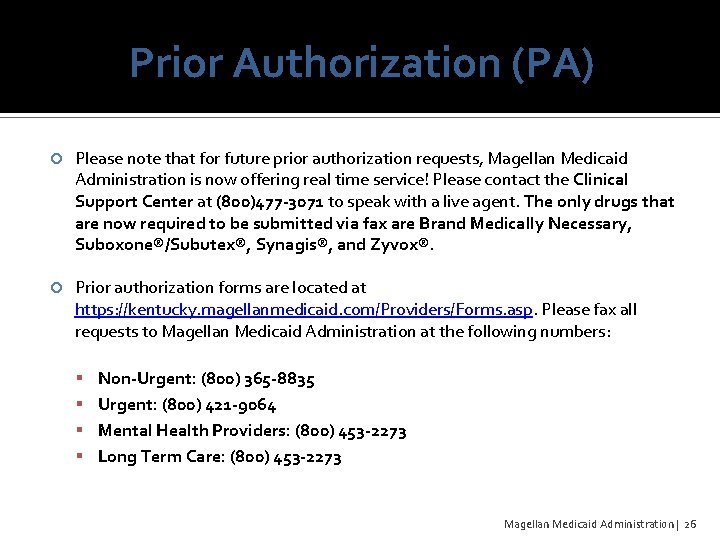
Prior Authorization (PA) Please note that for future prior authorization requests, Magellan Medicaid Administration is now offering real time service! Please contact the Clinical Support Center at (800)477 -3071 to speak with a live agent. The only drugs that are now required to be submitted via fax are Brand Medically Necessary, Suboxone®/Subutex®, Synagis®, and Zyvox®. Prior authorization forms are located at https: //kentucky. magellanmedicaid. com/Providers/Forms. asp. Please fax all requests to Magellan Medicaid Administration at the following numbers: Non-Urgent: (800) 365 -8835 Urgent: (800) 421 -9064 Mental Health Providers: (800) 453 -2273 Long Term Care: (800) 453 -2273 Magellan Medicaid Administration | 26
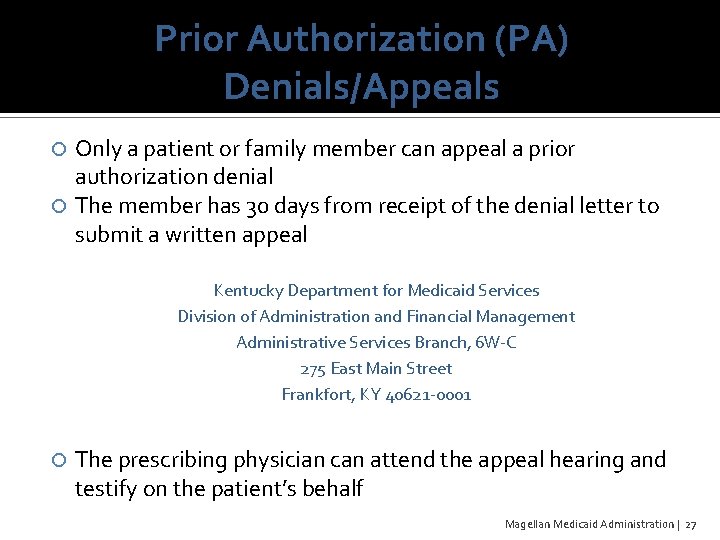
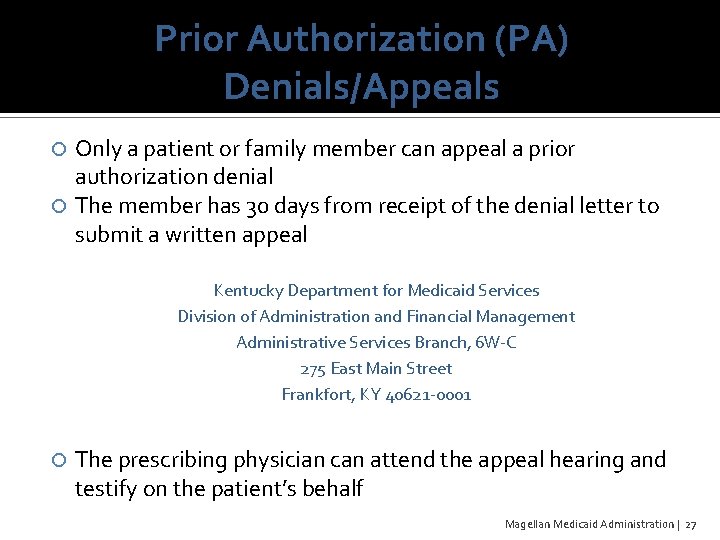
Prior Authorization (PA) Denials/Appeals Only a patient or family member can appeal a prior authorization denial The member has 30 days from receipt of the denial letter to submit a written appeal Kentucky Department for Medicaid Services Division of Administration and Financial Management Administrative Services Branch, 6 W-C 275 East Main Street Frankfort, KY 40621 -0001 The prescribing physician can attend the appeal hearing and testify on the patient’s behalf Magellan Medicaid Administration | 27
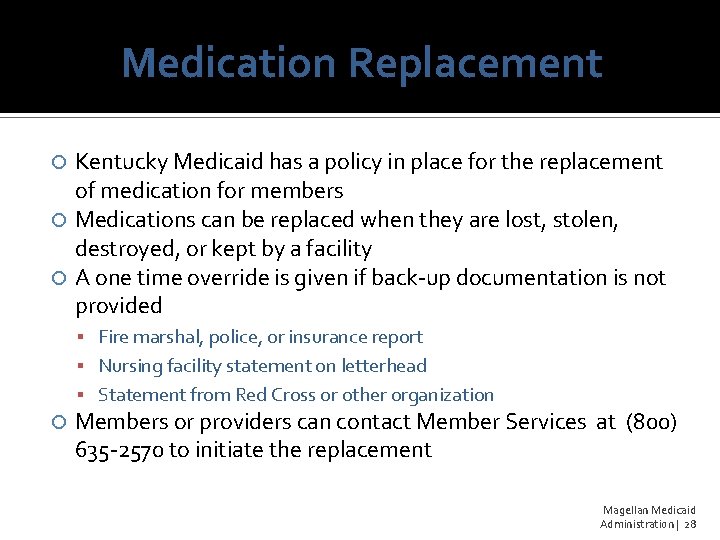
Medication Replacement Kentucky Medicaid has a policy in place for the replacement of medication for members Medications can be replaced when they are lost, stolen, destroyed, or kept by a facility A one time override is given if back-up documentation is not provided Fire marshal, police, or insurance report Nursing facility statement on letterhead Statement from Red Cross or other organization Members or providers can contact Member Services at (800) 635 -2570 to initiate the replacement Magellan Medicaid Administration | 28
Upcoming Changes Magellan Medicaid Administration | 29
340 B Program The 340 B Drug Pricing Program is administered by Health Resources and Services Administration’s (HRSA) Office of Pharmacy Affairs (OPA). The 340 B Program was designed to limit the cost of covered outpatient drugs to certain Federal grantees, including section 330 -funded health centers. The program should result in significant savings on the cost of pharmaceuticals. In the near future, Kentucky Medicaid will require providers to indicate if the claim is a 340 B claim. Additional information will be available in the upcoming months. Magellan Medicaid Administration | 30
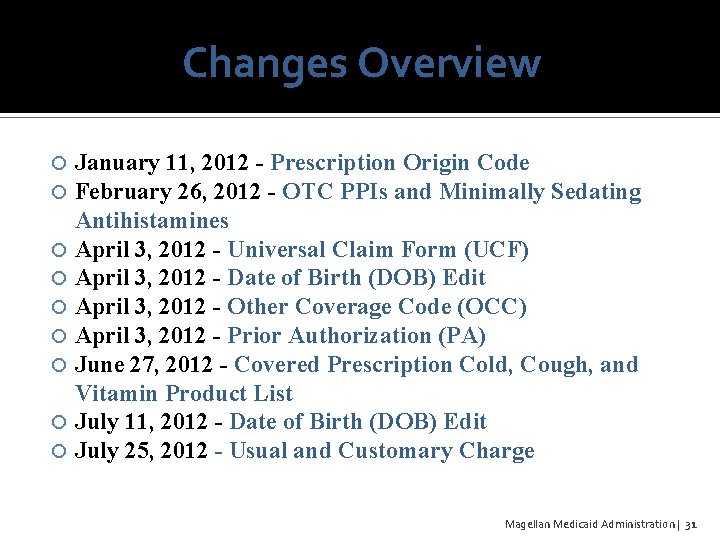
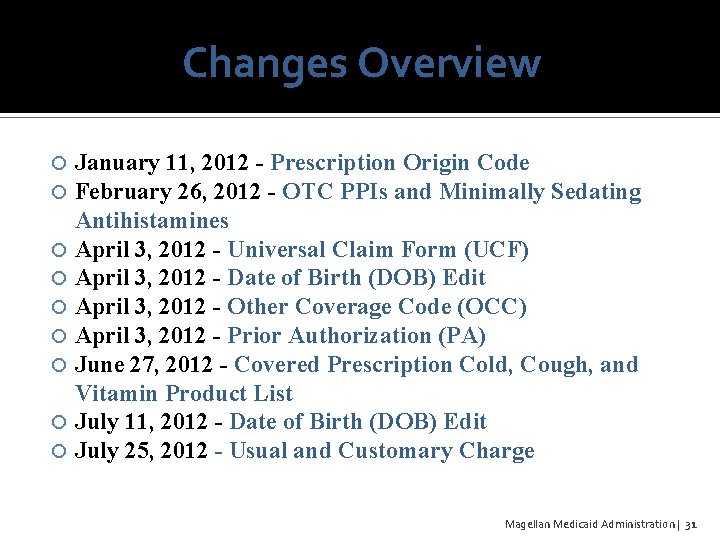
Changes Overview January 11, 2012 - Prescription Origin Code February 26, 2012 - OTC PPIs and Minimally Sedating Antihistamines April 3, 2012 - Universal Claim Form (UCF) April 3, 2012 - Date of Birth (DOB) Edit April 3, 2012 - Other Coverage Code (OCC) April 3, 2012 - Prior Authorization (PA) June 27, 2012 - Covered Prescription Cold, Cough, and Vitamin Product List July 11, 2012 - Date of Birth (DOB) Edit July 25, 2012 - Usual and Customary Charge Magellan Medicaid Administration | 31
Questions? Kasie Purvis, Provider Relations Manager klpurvis@magellanhealth. com (314) 387 -4792
 Magellan otc
Magellan otc Www.anthem.com/kymedicaid
Www.anthem.com/kymedicaid Kentucky department of revenue
Kentucky department of revenue King county superior court ecr
King county superior court ecr Ms department of finance and administration
Ms department of finance and administration Cdpa tu
Cdpa tu Mississippi department of finance and administration
Mississippi department of finance and administration General administration department gujarat gr
General administration department gujarat gr Us department of transportation maritime administration
Us department of transportation maritime administration Indiana family and social services administration
Indiana family and social services administration Us general services administration per diem
Us general services administration per diem Romanian air traffic services administration
Romanian air traffic services administration Was magellan worth defending dbq
Was magellan worth defending dbq Ferdinand magellan god gold glory
Ferdinand magellan god gold glory Cans magellan
Cans magellan Ferdinand magellan background
Ferdinand magellan background Robert lasalle accomplishments
Robert lasalle accomplishments Limang ekspedisyon ni magellan
Limang ekspedisyon ni magellan Venus semimajor axis
Venus semimajor axis Magellan design software
Magellan design software Fernando magellan informatii
Fernando magellan informatii Jacques cartier sponsoring country
Jacques cartier sponsoring country Sonda magellan
Sonda magellan Fernanda magellan
Fernanda magellan Gellin like magellan
Gellin like magellan Aice marine science textbook answers
Aice marine science textbook answers Noanet fiber map
Noanet fiber map Magellan radar
Magellan radar Ma-gien-lăng
Ma-gien-lăng Magellan exchange
Magellan exchange Magellan imacs
Magellan imacs Ferdinand magellan characteristics
Ferdinand magellan characteristics Ateis magellan
Ateis magellan