New York State Medicaid FeeforService FFS Pharmacy Prior



- Slides: 30
New York State Medicaid Fee-for-Service (FFS) Pharmacy Prior Authorization Programs Presented by: Magellan Medicaid Administration, Inc. & New York State Department of Health (DOH) Revised March 2014
Overview § What are the Medicaid FFS Pharmacy Prior Authorization (PA) Programs? § How do I obtain Prior Authorization? § Where can I go for more information? 2
Who is Subject to the FFS Pharmacy PA Programs? § Enrollees of the following program receive pharmacy services through NYS Medicaid Pharmacy Benefit Programs § Medicaid Fee-For-Service § Approximately 1. 5 million people § Will continue to present their Medicaid card at the pharmacy § Will continue to receive their pharmacy benefits from Medicaid until such time that they are moved into managed or care management 3
Preferred Drug Program (PDP) Implemented June 28, 2006 4

Preferred Drug Program (PDP) § Clinically driven & evidence-based § Maintains access to all drugs § Competitive pricing through supplemental rebates § Savings offset high drug costs 5
Preferred Drug List (PDL) § Categorized by therapeutic drug class § Preferred and non-preferred drugs § Footnotes provide useful information § Developed by the Drug Utilization Review (DUR) Board 6
DUR Board Meetings § Committee Members § Practicing physicians, nurse practitioners, pharmacists and patient advocates § Make recommendations on preferred status within PDP drugs classes § Review of existing therapeutic classes § Newly FDA-approved drugs § Addition of new therapeutic classes § Review and develop clinical criteria for PDP and the Clinical Drug Review Program (CDRP) 7
DUR Board Meetings § Public session announced on DOH website § Clinical Evidence & Discussion § § § Healthcare professionals Drug Effectiveness Review Project (Oregon Health & Sciences University) Pharmaceutical manufacturers and other interested parties § Executive Session § Financial information is considered only after the clinical discussion is completed § Committee formulates recommendations § Commissioner of Health makes the final determination 8

DUR Programs § Programs to help ensure that prescriptions for outpatient drugs are appropriate, medically necessary, and not likely to result in adverse medical consequences: § Step Therapy Program § Frequency/Quantity/Duration (F/Q/D) Program § Dose Optimization Program § DUR edits can be reviewed on the PDL: § https: //newyork. fhsc. com/downloads/providers/NYRx_PDP_PDL. pdf 9
DUR Programs § System editing will be performed at the point-of-sale to allow claims to pay without prior authorization when clinical criteria and F/Q/D limits are met § An automated approval will be issued if all rules associated with the requested product are satisfied; which will result in a paid claim § A failed clinical rule will result in a failed claim § A rejection message will be provided at the point-of-sale instructing pharmacy providers to notify the prescriber to change the prescription if appropriate or to obtain prior authorization § Prescribers must obtain prior authorization through the clinical call center for claims that do not meet clinical criteria 10
Brand When Less than Generic Program § Promotes the use of multi-source brand name drugs when the cost of the brand name drug is less expensive than the generic § Do not require “DAW” or “Brand Medically Necessary” on the prescription § Please visit the following website for recent news and a listing of drugs subject to the program: § https: //newyork. fhsc. com/providers/bltgp_about. asp 11
Clinical Drug Review Program (CDRP) Implemented October 18, 2006 12
Intent of CDRP § To ensure that certain drugs are utilized in a medically appropriate manner § To protect the long-term efficacy of certain drugs and the public’s health § To prevent overuse, abuse and illegal utilization of certain drugs 13
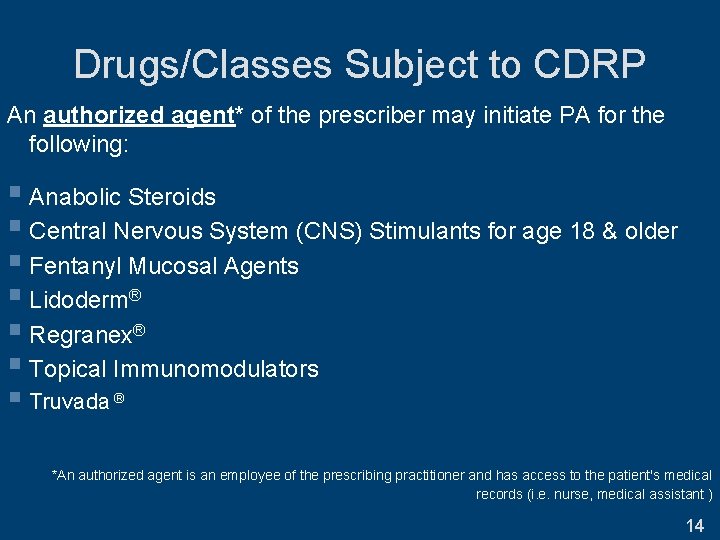
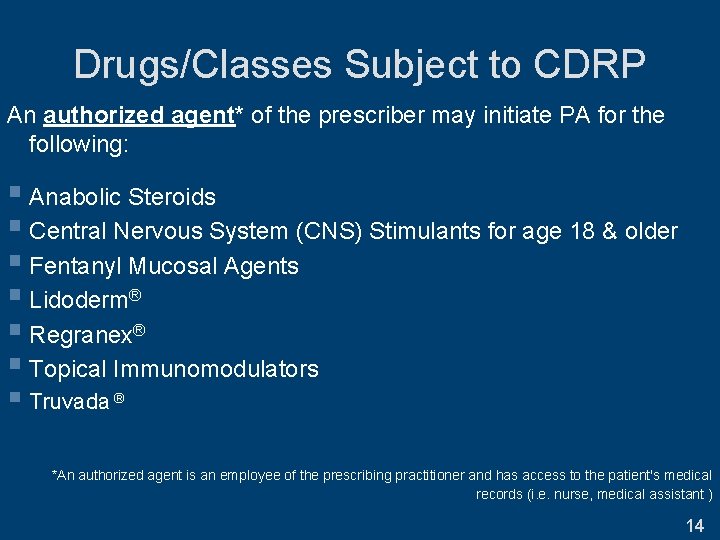
Drugs/Classes Subject to CDRP An authorized agent* of the prescriber may initiate PA for the following: § Anabolic Steroids § Central Nervous System (CNS) Stimulants for age 18 & older § Fentanyl Mucosal Agents § Lidoderm® § Regranex® § Topical Immunomodulators § Truvada ® *An authorized agent is an employee of the prescribing practitioner and has access to the patient's medical records (i. e. nurse, medical assistant ) 14
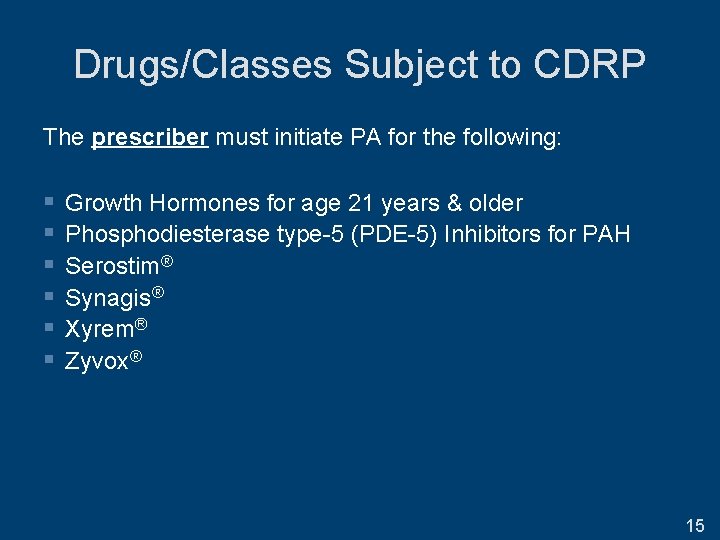
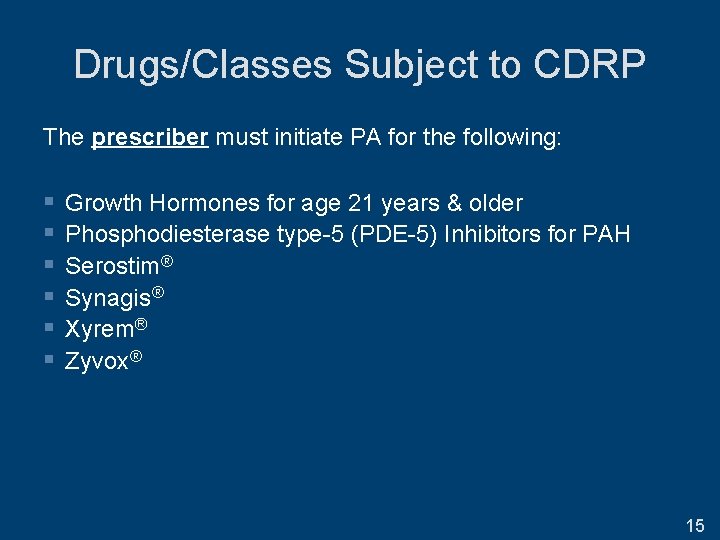
Drugs/Classes Subject to CDRP The prescriber must initiate PA for the following: § § § Growth Hormones for age 21 years & older Phosphodiesterase type-5 (PDE-5) Inhibitors for PAH Serostim® Synagis® Xyrem® Zyvox® 15
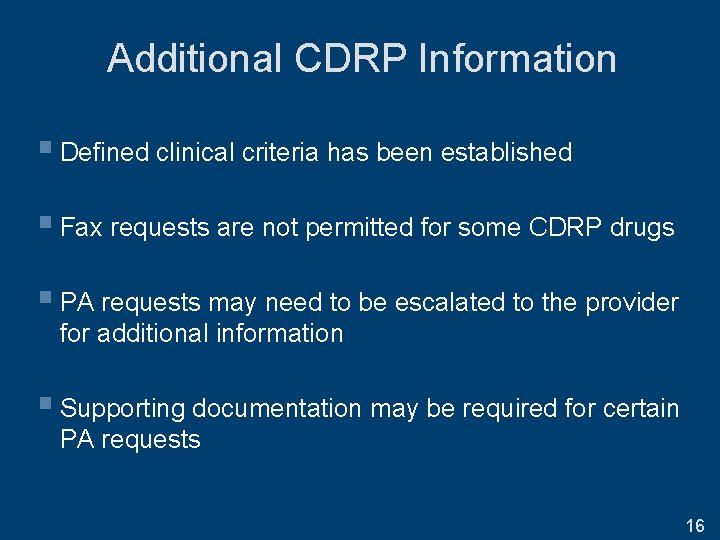
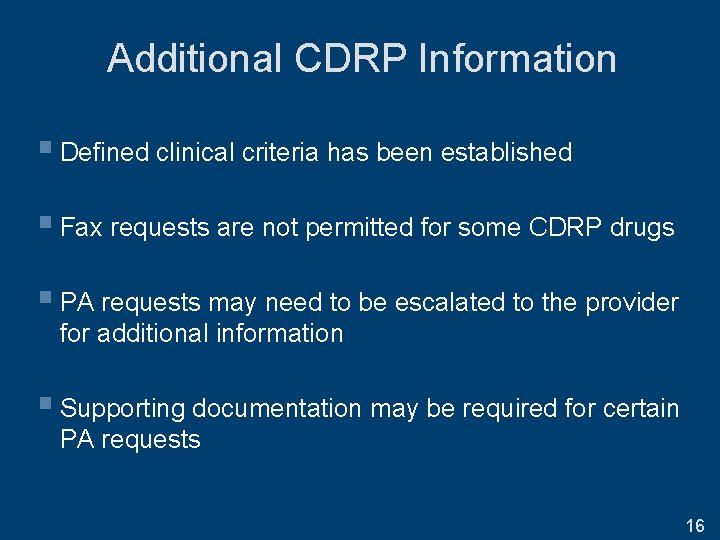
Additional CDRP Information § Defined clinical criteria has been established § Fax requests are not permitted for some CDRP drugs § PA requests may need to be escalated to the provider for additional information § Supporting documentation may be required for certain PA requests 16
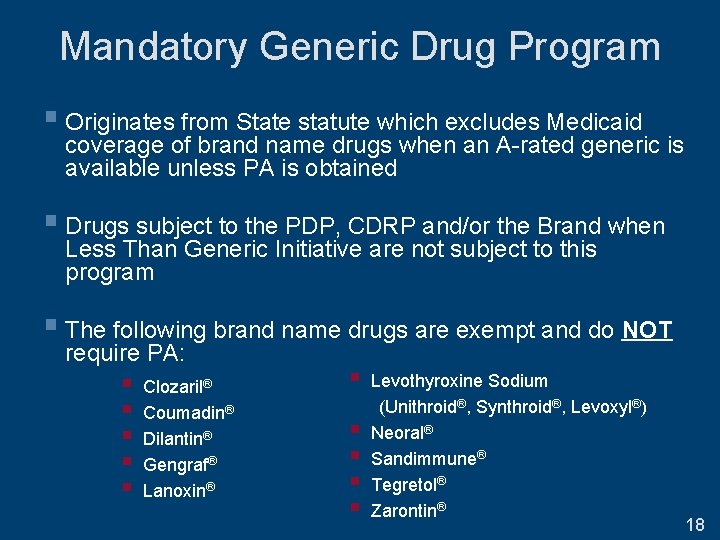
Mandatory Generic Drug Program (MGDP) Implemented November 17, 2002 17
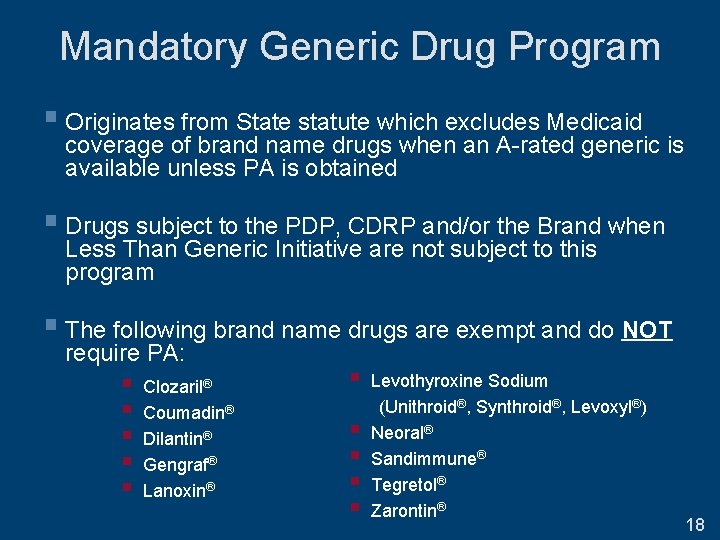
Mandatory Generic Drug Program § Originates from State statute which excludes Medicaid coverage of brand name drugs when an A-rated generic is available unless PA is obtained § Drugs subject to the PDP, CDRP and/or the Brand when Less Than Generic Initiative are not subject to this program § The following brand name drugs are exempt and do NOT require PA: § § § Clozaril® Coumadin® Dilantin® Gengraf® Lanoxin® § § § Levothyroxine Sodium (Unithroid®, Synthroid®, Levoxyl®) Neoral® Sandimmune® Tegretol® Zarontin® 18
Preferred Diabetic Supply Program (PDSP) Implemented October 1, 2009 19
Preferred Diabetic Supply Program § Preferred blood glucose monitors and corresponding test strips are available without prior approval or dispensing validation system (DVS) authorization § “Talking” and disposable blood glucose monitors are NOT included in the PDSP and will continue to be covered by Medicaid through the existing prior approval process § Preferred Supply List (PSL) is available online 20
How Do I Obtain Prior Authorization? 21
PDP, MGDP & CDRP PA Process § Dial (877) 309 -9493 and select option #1, then option #1 § Use the telephone key pad to enter: § Prescriber NPI § Prescriber Phone Number § Certified Pharmacy Technician will assist in completing PA § Faxing of PA requests to (800) 268 -2990 is available for PDP and some CDRP drugs § PAs can be obtained 24 hours a day, 7 days a week 22
DUR Program & PDSP PA Process § Drug Utilization Review Program § Dial (877) 309 -9493 and follow appropriate prompts § Preferred Diabetic Supply Programs § Dial (800) 342 -3005 to reach NYS DOH 23
Where Can I Go for More Information? 24
Program Updates Will be Communicated Through: § Email Notifications § Program Updates § Medicaid Update Article § Mailings § May be sent to prescribers most affected by program updates to minimize practice impact § Website Updates 25

https: //newyork. fhsc. com § PDL § PSL § Prior authorization fax form and worksheets § Clinical criteria § Material for enrollees 26
www. nyhealth. gov § Medicaid Update monthly publication § NYS health insurance & pharmacy programs § DUR Board § http: //www. nyhealth. gov/health_care/medicaid/program/dur/ 27
www. emedny. org § Formulary finder file § Provider enrollment forms & manuals § Patient eligibility verification instructions § Billing information § Fraud alerts 28
Important Numbers § Clinical Call Center: (877) 309 -9493 § Clinical Call Center Fax: (800) 268 -2990 § Diabetic Supply Prior Approval line: (800) 342 -3005 § Pharmacy Policy: (518) 486 -3209 § Enteral formula PA line: (866) 211 -1736 § Billing: (800) 343 -9000 29
New York State Medicaid Prior Authorization Programs Questions and Discussion 30
 New york state medicaid prior authorization
New york state medicaid prior authorization Kepro prior authorization form
Kepro prior authorization form Ffs fiche individuelle
Ffs fiche individuelle Ffs paducah
Ffs paducah Ffs file system
Ffs file system Ffs file system
Ffs file system Jonathan slides distributors
Jonathan slides distributors New york state nurse practitioner association
New york state nurse practitioner association Nys student aid payment application
Nys student aid payment application New york state teacher certification examinations
New york state teacher certification examinations New york state science standards
New york state science standards Math state test 2018 answer key
Math state test 2018 answer key Nys mesonet now
Nys mesonet now Ny state vegetable
Ny state vegetable Nys environmental facilities corporation
Nys environmental facilities corporation New york state professional firefighters association
New york state professional firefighters association What is nysiis
What is nysiis New york state association of transportation engineers
New york state association of transportation engineers Nysid catalog
Nysid catalog Department of criminal justice services ny
Department of criminal justice services ny Nysrc
Nysrc Latham traffic circle
Latham traffic circle New york tax practitioner hotline
New york tax practitioner hotline New york state nurse practitioner scope of practice
New york state nurse practitioner scope of practice New york state fish
New york state fish New york state nickname
New york state nickname New york state amateur hockey association
New york state amateur hockey association New york state county highway superintendents association
New york state county highway superintendents association New york, new jersey, pennsylvania, and delaware
New york, new jersey, pennsylvania, and delaware Marquee cinemas - orchard 10
Marquee cinemas - orchard 10 Strengths and weaknesses of the articles of confederation
Strengths and weaknesses of the articles of confederation