Human Resources Administration Medical Assistance Program MAP Office
- Slides: 26
Human Resources Administration Medical Assistance Program (MAP) Office of Eligibility Information Services Presentation for the Center for Medicare Medicaid Services(CMS) National Training Program August 6, 2018 KAREN LANE ………………. EXECUTIVE DEPUTY COMMISSIONER MAP MARIA TERESA ARCE ……………………. ……. . …CHIEF EXTERNAL AFFAIRS OFFICER MARIA ORTIZ-QUEZADA…………………DIRECTOR OF ELIGIBILITY INFORMATION SERVICES Copyright 2018 The City of New York, Department of Social Services for permission to reproduce all or part of this material contact the New York City Human Resources Administration
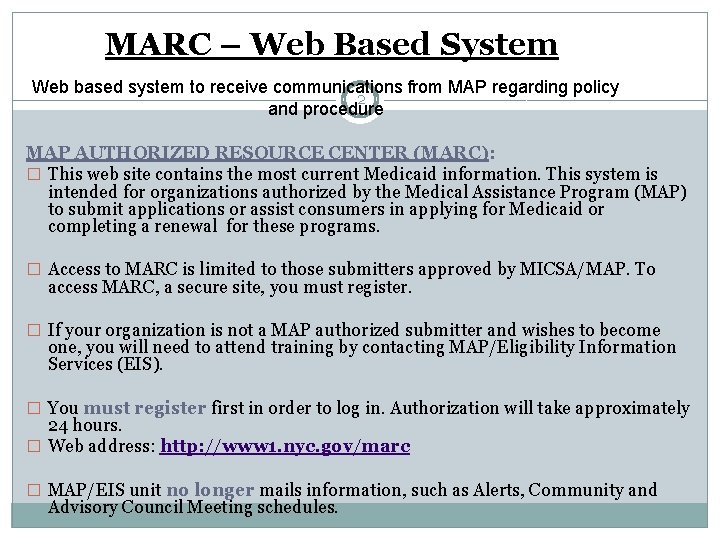
MARC – Web Based System Web based system to receive communications from MAP regarding policy 2 and procedure MAP AUTHORIZED RESOURCE CENTER (MARC): � This web site contains the most current Medicaid information. This system is intended for organizations authorized by the Medical Assistance Program (MAP) to submit applications or assist consumers in applying for Medicaid or completing a renewal for these programs. � Access to MARC is limited to those submitters approved by MICSA/MAP. To access MARC, a secure site, you must register. � If your organization is not a MAP authorized submitter and wishes to become one, you will need to attend training by contacting MAP/Eligibility Information Services (EIS). � You must register first in order to log in. Authorization will take approximately 24 hours. � Web address: http: //www 1. nyc. gov/marc � MAP/EIS unit no longer mails information, such as Alerts, Community and Advisory Council Meeting schedules.
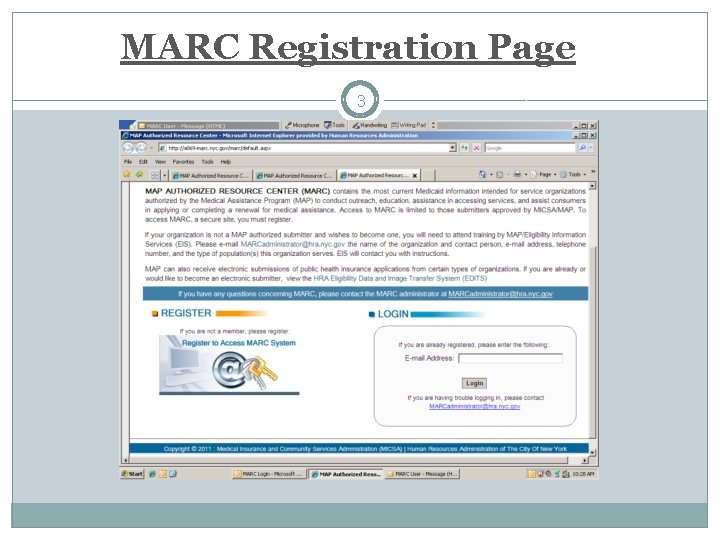
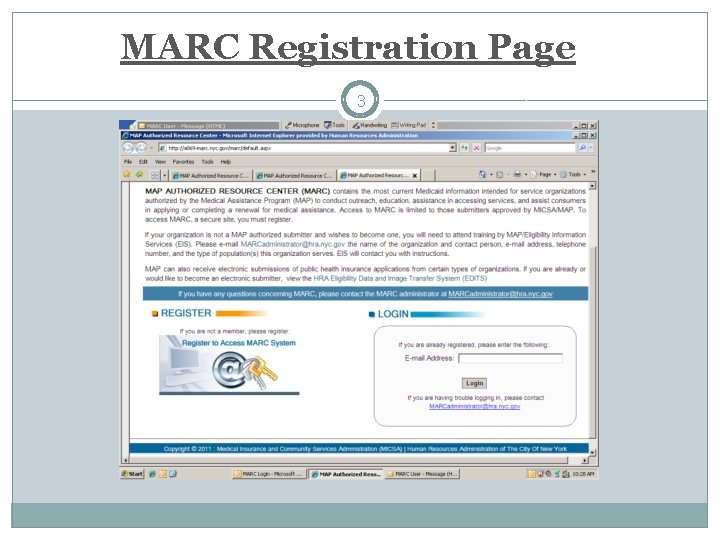
MARC Registration Page 3
ACA - Exchanges 4 � As of January 1, 2014 the Medical Assistance Program only accepts certain applications from providers and entities that either submit Medicaid applications centrally or assist consumers in applying. � One goal of the ACA was to make it easier to obtain health insurance. The ACA created Health Exchanges where individuals and small businesses can obtain health insurance coverage. Individuals can apply on-line, by phone, by mail, or in person. � New York State has created its own Health Exchange known as New York State of Health. For those that can not enroll online, the number to call to apply for health insurance is: (855) 355 -5777
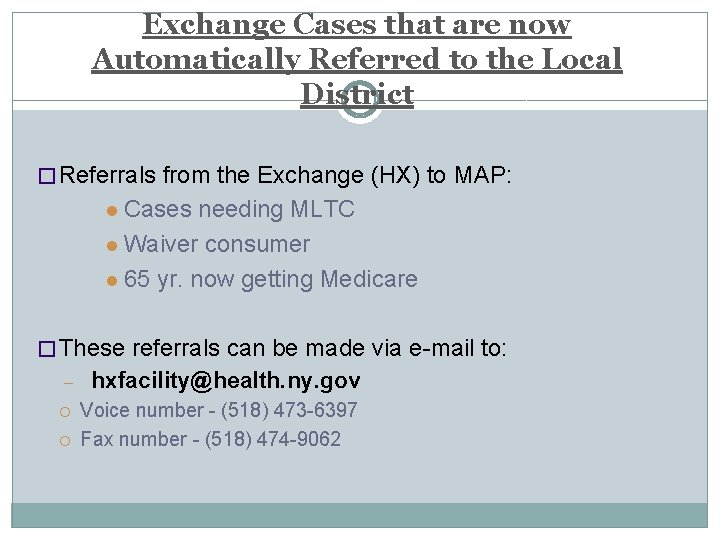
Exchange Cases that are now Automatically Referred to the Local District � Referrals from the Exchange (HX) to MAP: l Cases needing MLTC l Waiver consumer l 65 yr. now getting Medicare � These referrals can be made via e-mail to: – hxfacility@health. ny. gov Voice number - (518) 473 -6397 Fax number - (518) 474 -9062
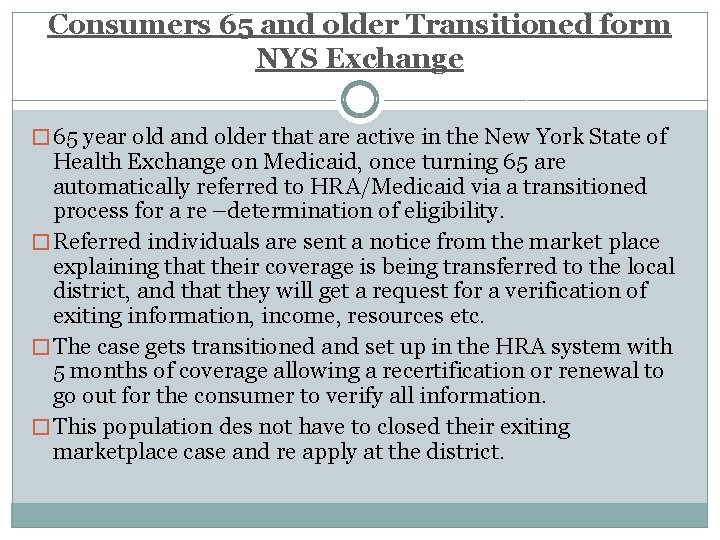
Consumers 65 and older Transitioned form NYS Exchange � 65 year old and older that are active in the New York State of Health Exchange on Medicaid, once turning 65 are automatically referred to HRA/Medicaid via a transitioned process for a re –determination of eligibility. � Referred individuals are sent a notice from the market place explaining that their coverage is being transferred to the local district, and that they will get a request for a verification of exiting information, income, resources etc. � The case gets transitioned and set up in the HRA system with 5 months of coverage allowing a recertification or renewal to go out for the consumer to verify all information. � This population des not have to closed their exiting marketplace case and re apply at the district.
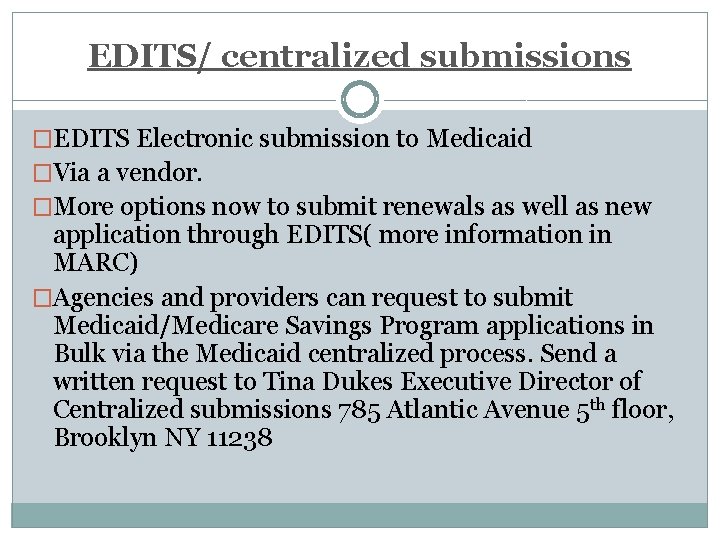
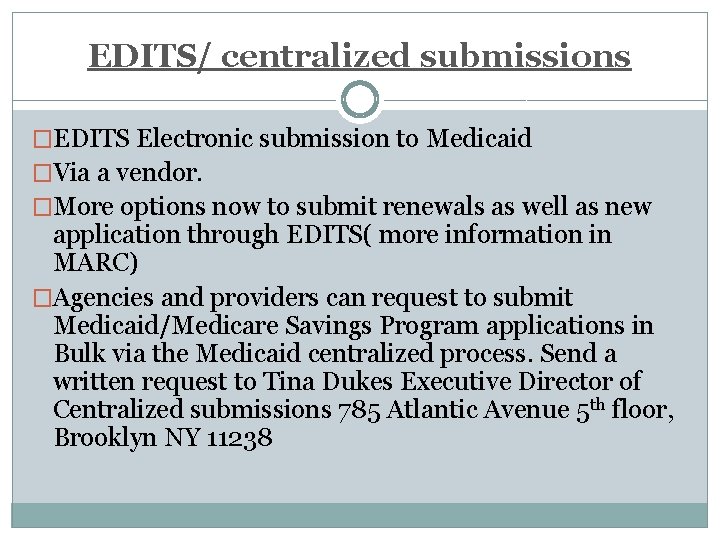
EDITS/ centralized submissions �EDITS Electronic submission to Medicaid �Via a vendor. �More options now to submit renewals as well as new application through EDITS( more information in MARC) �Agencies and providers can request to submit Medicaid/Medicare Savings Program applications in Bulk via the Medicaid centralized process. Send a written request to Tina Dukes Executive Director of Centralized submissions 785 Atlantic Avenue 5 th floor, Brooklyn NY 11238
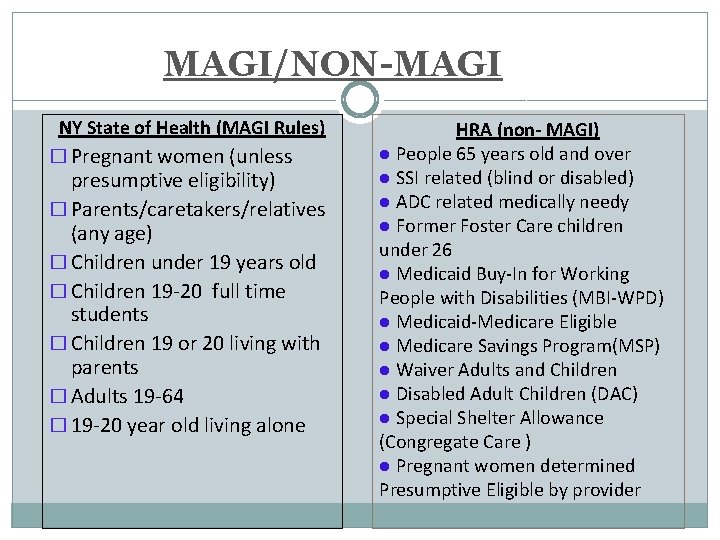
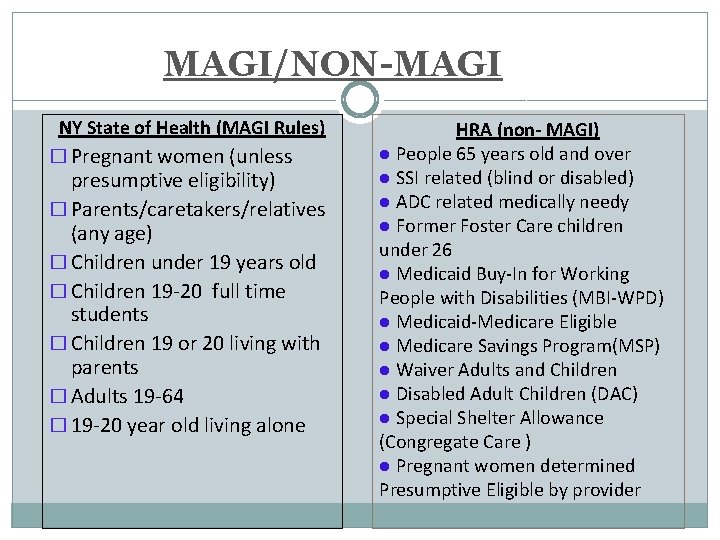
MAGI/NON-MAGI NY State of Health (MAGI Rules) � Pregnant women (unless presumptive eligibility) � Parents/caretakers/relatives (any age) � Children under 19 years old � Children 19 -20 full time students � Children 19 or 20 living with parents � Adults 19 -64 � 19 -20 year old living alone HRA (non- MAGI) l People 65 years old and over l SSI related (blind or disabled) l ADC related medically needy l Former Foster Care children under 26 l Medicaid Buy-In for Working People with Disabilities (MBI-WPD) l Medicaid-Medicare Eligible l Medicare Savings Program(MSP) l Waiver Adults and Children l Disabled Adult Children (DAC) l Special Shelter Allowance (Congregate Care ) l Pregnant women determined Presumptive Eligible by provider
Overview 9 What is Medicaid? Medicaid is a means tested government assistance program which pays for a comprehensive range of health related services for persons with low income and resources.
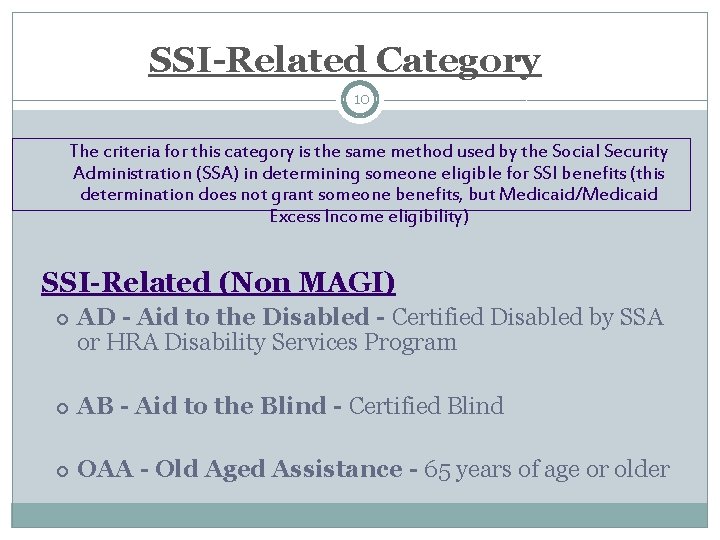
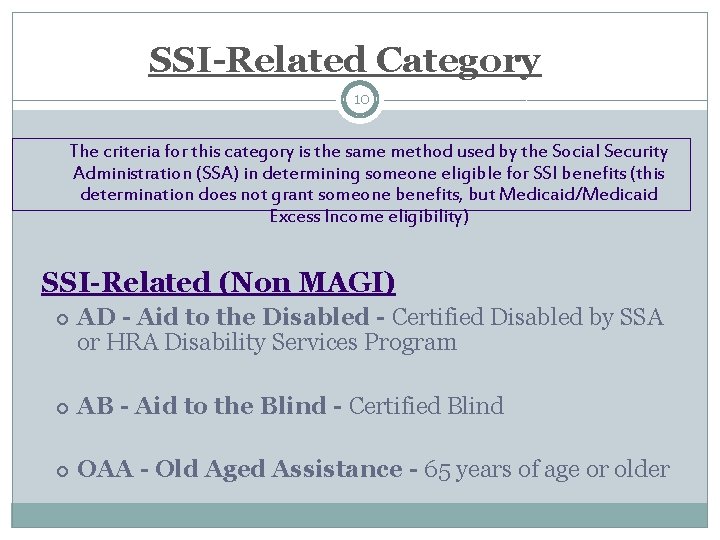
SSI-Related Category 10 The criteria for this category is the same method used by the Social Security Administration (SSA) in determining someone eligible for SSI benefits (this determination does not grant someone benefits, but Medicaid/Medicaid Excess Income eligibility) SSI-Related (Non MAGI) AD - Aid to the Disabled - Certified Disabled by SSA or HRA Disability Services Program AB - Aid to the Blind - Certified Blind OAA - Old Aged Assistance - 65 years of age or older
11 Medicaid Eligibility Criteria � Residency � Identity � Citizenship/Immigration Status � Income � Resources
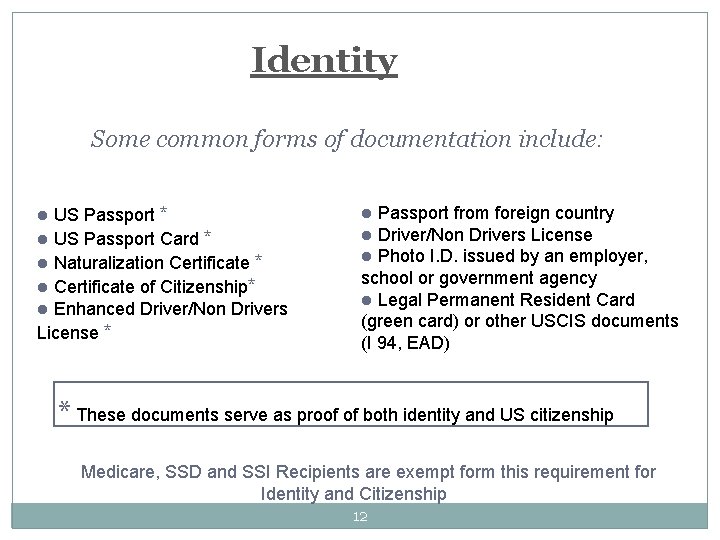
Identity Some common forms of documentation include: l US Passport * l US Passport Card * * l Certificate of Citizenship* l Naturalization Certificate l Enhanced Driver/Non Drivers License * l Passport from foreign country l Driver/Non Drivers License l Photo I. D. issued by an employer, school or government agency l Legal Permanent Resident Card (green card) or other USCIS documents (I 94, EAD) * These documents serve as proof of both identity and US citizenship Medicare, SSD and SSI Recipients are exempt form this requirement for Identity and Citizenship 12
Verification of Identity & 13 Citizenship � As of October 1, 2010, and as part of the Children’s Health Insurance Program Reauthorization Act (CHIPRA) of 2009, individuals who declare to be United States Citizens and provide a valid Social Security Number (SSN), no longer have to provide proof of citizenship and identity as a condition of initial eligibility when submitting applications for Medicaid. � For these individuals, verification of citizenship and identity is be done through an electronic data file match with the Social Security Administration (SSA).
The Application Process Elimination of the Face to Face Interview 14 � Applications for NYS of Health Exchange are not submitted to local district (not manually). � For those applicants who wish to apply by mail and are appropriate to apply at HRA/MAP, the mailing address is: Initial Eligibility Unit HRA/Medical Assistance Program PO Box 24390 Brooklyn, NY 11202 -9814 � For mailed applications, the application date is the date that a signed application is received by the local district. Please note that entities will not receive notification on applications mailed directly by the consumer. � For applications that do not have all required documentation, a deferral notice will be sent to the consumer, which will list any missing documentation. The applicant will have 14 days to return all requested material in the business return envelope provided.
Medicare as a Condition of Medicaid Eligibility 15 �It is a requirement for certain Medicaid applicant/recipients who appear to be eligible for Medicare to apply for the benefit as a condition of Medicaid eligibility. �This includes recipients receiving Medicaid-only and those on a Cash Assistance case.
Medicare as a Condition of Medicaid Eligibility (con’t) � Who must apply for Medicare: Fully eligible A/R at or below the applicable income level with income at or below 120% of FPL who are age 64 and 9 months � There are certain populations that are excluded from this requirement : Individuals not fully eligible for Medicaid Those with income over 120% of the FPL Most immigrants and non citizens are excluded: Only lawful permanent residents in the US for five years or more must apply for Medicare as a condition of Medicaid eligibility (5 year ban)
Managed Long Term Care & Conflict Free Evaluation Enrollment Center � Consumers who are dual eligible needing personal care prior to MLTC assessment for services; must have an evaluation assessment done by the Conflict Free Evaluation Enrollment Center. The dedicated MLTC number at Medicaid choice is (888) 401 -6582 � After the Conflict Free Evaluation has taken place the desired MLTC plan evaluates the consumer for services hours. Medicaid recipient seeking MLTC enrollment should call the CFEEC at (855) 222 -8350 � Consumers that have excess income and do not submit medical bills the case will be authorized as 06 coverage - H 76. � This allows Maximus to prospectively enroll into a MLTC plan.
Excess Income Program 18 �The Excess Income Program is for individuals who meet all the eligibility criteria for Medicaid except income and are part of a federally participating category. �The amount by which consumers exceed the Medicaid level is defined as the “excess income”, “surplus” or “spend-down”. �These individuals are allowed to “spend-down” to the Medicaid level for their household size using theirs &/or household members’ medical bills or by directly paying the amount of the surplus to HRA.
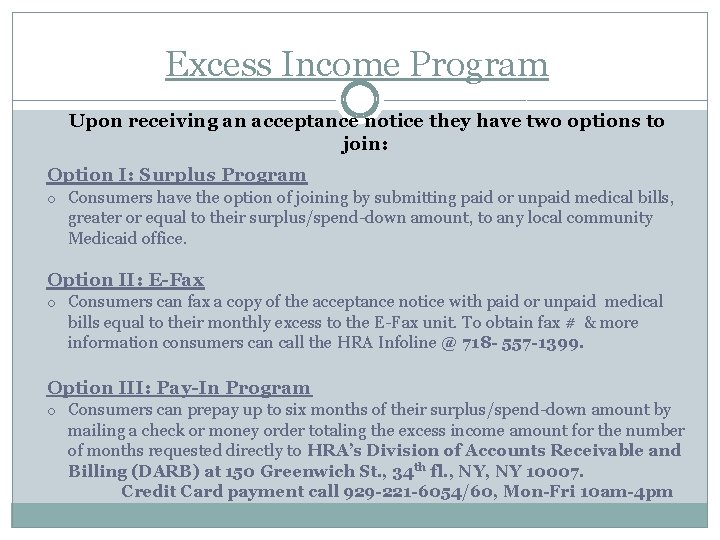
Excess Income Program Upon receiving an acceptance notice they have two options to join: Option I: Surplus Program Consumers have the option of joining by submitting paid or unpaid medical bills, greater or equal to their surplus/spend-down amount, to any local community Medicaid office. Option II: E-Fax Consumers can fax a copy of the acceptance notice with paid or unpaid medical bills equal to their monthly excess to the E-Fax unit. To obtain fax # & more information consumers can call the HRA Infoline @ 718 - 557 -1399. Option III: Pay-In Program Consumers can prepay up to six months of their surplus/spend-down amount by mailing a check or money order totaling the excess income amount for the number of months requested directly to HRA’s Division of Accounts Receivable and Billing (DARB) at 150 Greenwich St. , 34 th fl. , NY 10007. Credit Card payment call 929 -221 -6054/60, Mon-Fri 10 am-4 pm
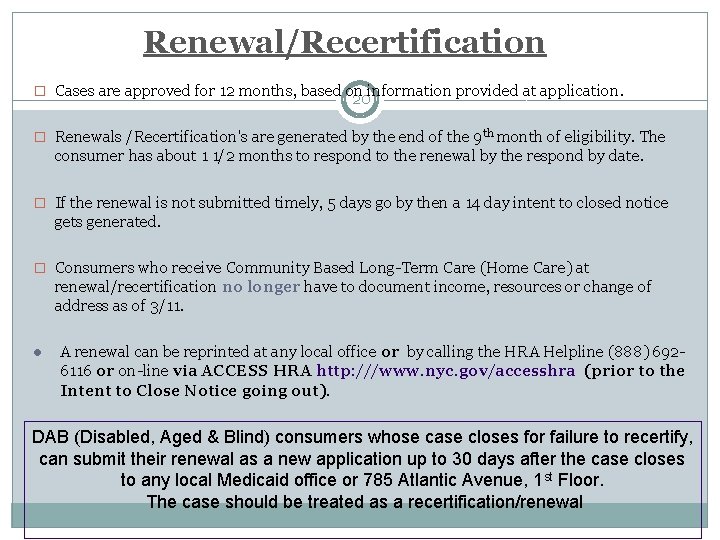
Renewal/Recertification � Cases are approved for 12 months, based on information provided at application. 20 � Renewals /Recertification's are generated by the end of the 9 th month of eligibility. The consumer has about 1 1/2 months to respond to the renewal by the respond by date. � If the renewal is not submitted timely, 5 days go by then a 14 day intent to closed notice gets generated. � Consumers who receive Community Based Long-Term Care (Home Care) at renewal/recertification no longer have to document income, resources or change of address as of 3/11. l A renewal can be reprinted at any local office or by calling the HRA Helpline (888) 6926116 or on-line via ACCESS HRA http: ///www. nyc. gov/accesshra (prior to the Intent to Close Notice going out). DAB (Disabled, Aged & Blind) consumers whose case closes for failure to recertify, can submit their renewal as a new application up to 30 days after the case closes to any local Medicaid office or 785 Atlantic Avenue, 1 st Floor. The case should be treated as a recertification/renewal
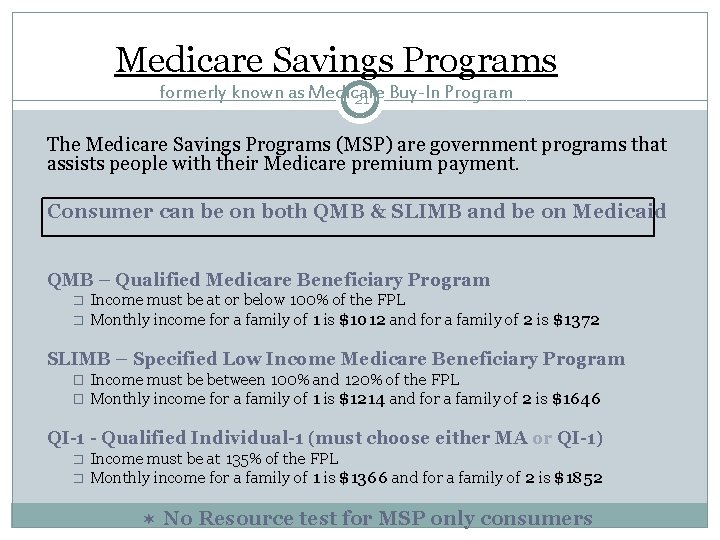
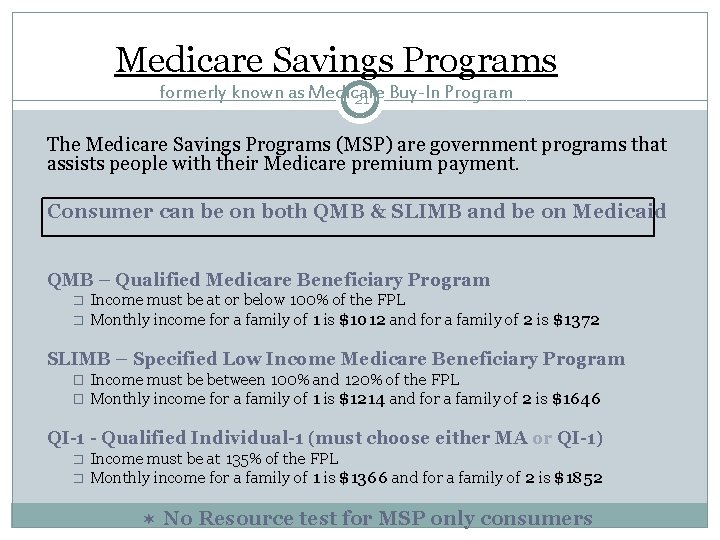
Medicare Savings Programs formerly known as Medicare 21 Buy-In Program The Medicare Savings Programs (MSP) are government programs that assists people with their Medicare premium payment. Consumer can be on both QMB & SLIMB and be on Medicaid QMB – Qualified Medicare Beneficiary Program � � Income must be at or below 100% of the FPL Monthly income for a family of 1 is $1012 and for a family of 2 is $1372 SLIMB – Specified Low Income Medicare Beneficiary Program � � Income must be between 100% and 120% of the FPL Monthly income for a family of 1 is $1214 and for a family of 2 is $1646 QI-1 - Qualified Individual-1 (must choose either MA or QI-1) � � Income must be at 135% of the FPL Monthly income for a family of 1 is $1366 and for a family of 2 is $1852 ¬ No Resource test for MSP only consumers
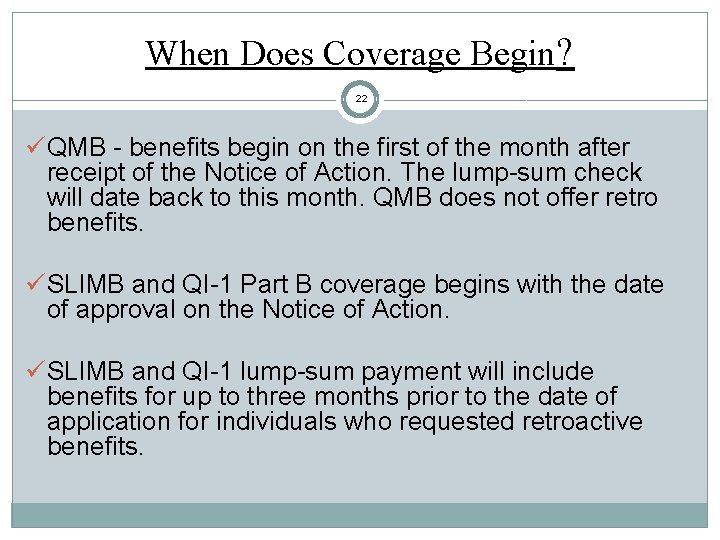
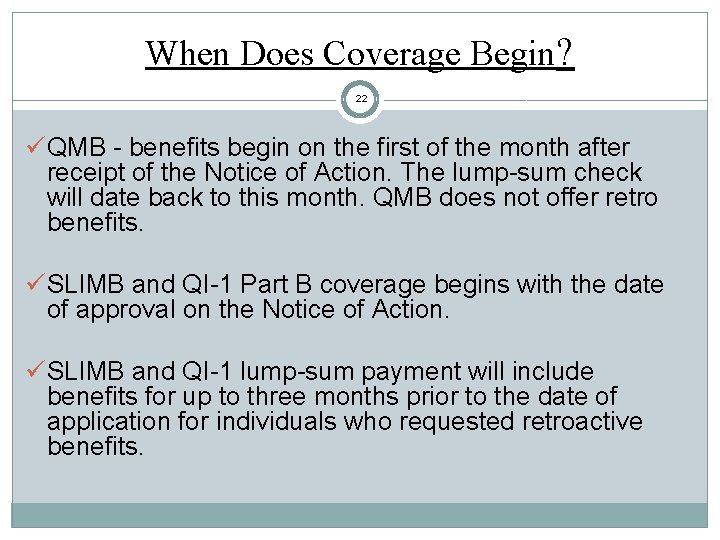
When Does Coverage Begin? 22 ü QMB - benefits begin on the first of the month after receipt of the Notice of Action. The lump-sum check will date back to this month. QMB does not offer retro benefits. ü SLIMB and QI-1 Part B coverage begins with the date of approval on the Notice of Action. ü SLIMB and QI-1 lump-sum payment will include benefits for up to three months prior to the date of application for individuals who requested retroactive benefits.
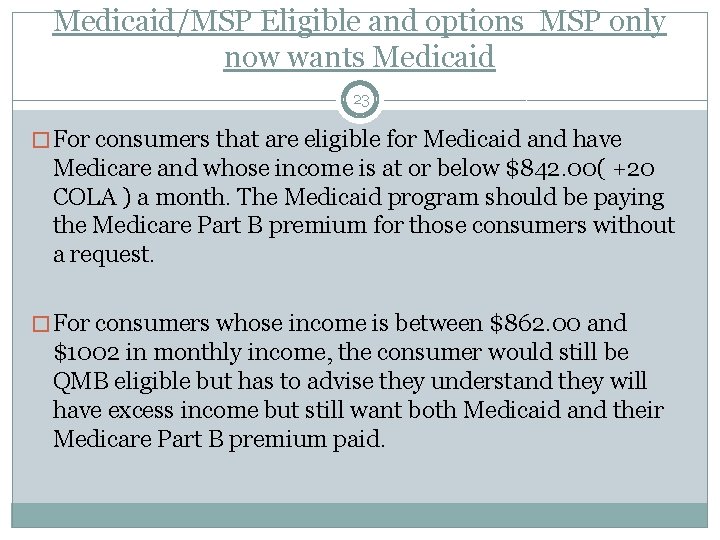
Medicaid/MSP Eligible and options MSP only now wants Medicaid 23 � For consumers that are eligible for Medicaid and have Medicare and whose income is at or below $842. 00( +20 COLA ) a month. The Medicaid program should be paying the Medicare Part B premium for those consumers without a request. � For consumers whose income is between $862. 00 and $1002 in monthly income, the consumer would still be QMB eligible but has to advise they understand they will have excess income but still want both Medicaid and their Medicare Part B premium paid.
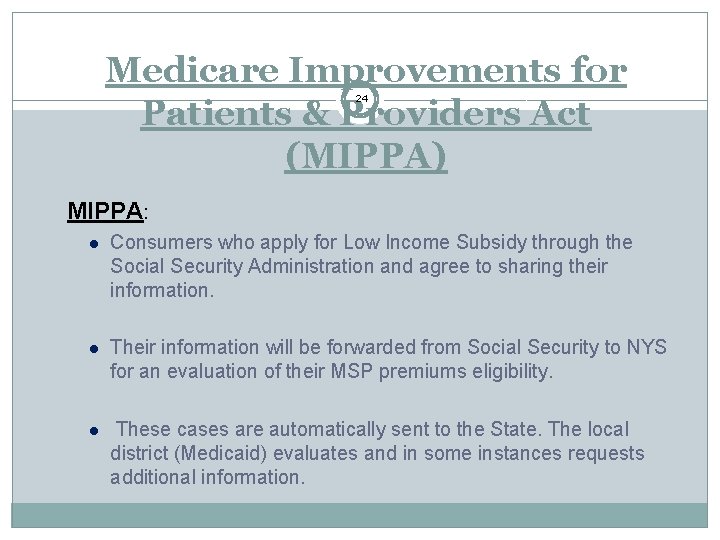
Medicare Improvements for Patients & Providers Act (MIPPA) 24 MIPPA: l Consumers who apply for Low Income Subsidy through the Social Security Administration and agree to sharing their information. l Their information will be forwarded from Social Security to NYS for an evaluation of their MSP premiums eligibility. l These cases are automatically sent to the State. The local district (Medicaid) evaluates and in some instances requests additional information.
Medicare Part D Plans 25 Dually eligible(Medicaid, Medicare) individuals must enroll in Part D, New York State pays for Part D benchmark Medicare Plan for dual eligibles. Dually eligible who refuse to enroll in Medicare Part D will not be eligible for Medicaid Individuals must enroll in a plan that offers the prescriptions they are using or that the prescription is in their formulary The consumer may also have prescriptions covered by Medicare Part B Questions can be answered by calling 1 -800 -Medicare
26 Low Income Subsidy & Medicare Part D �Once a Medicaid consumer obtains Medicare, the consumer is considered a dual eligible. �Dual eligible consumers are entitled to the Low Income Subsidy (LIS) and free Medicare Part D prescription program.