1 ARTHROGRAMS RT 255 Radiography of a joint






























- Slides: 103
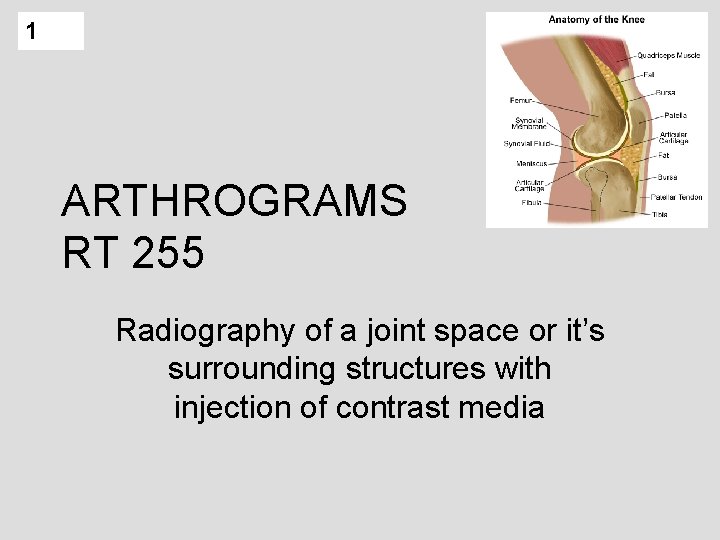
1 ARTHROGRAMS RT 255 Radiography of a joint space or it’s surrounding structures with injection of contrast media
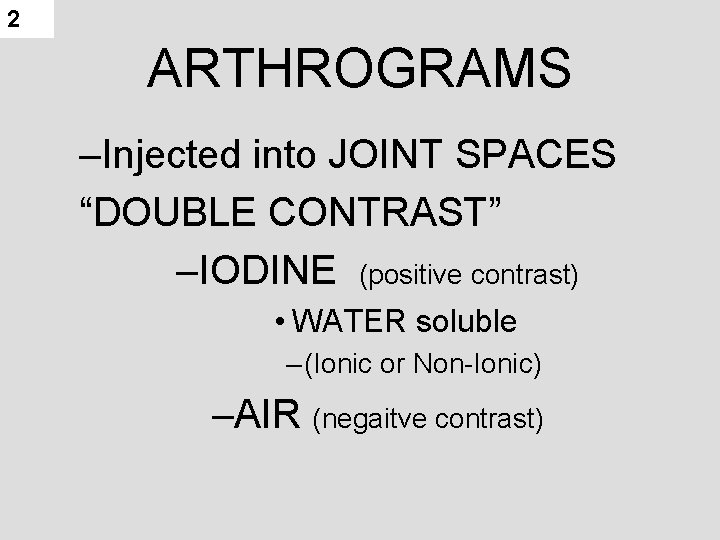
2 ARTHROGRAMS –Injected into JOINT SPACES “DOUBLE CONTRAST” –IODINE (positive contrast) • WATER soluble – (Ionic or Non-Ionic) –AIR (negaitve contrast)
3 Arthrography is concerned with synovial joints MOSTLY REPLACED BY MRI – non invasive, good detail of soft tissue structures CONTRAINDICATIONS TO MRI: • CLAUSTROPHOBIC • PT SIZE • Foreign Body (metal) • COST / INSURANCE REIMBURSEMENT
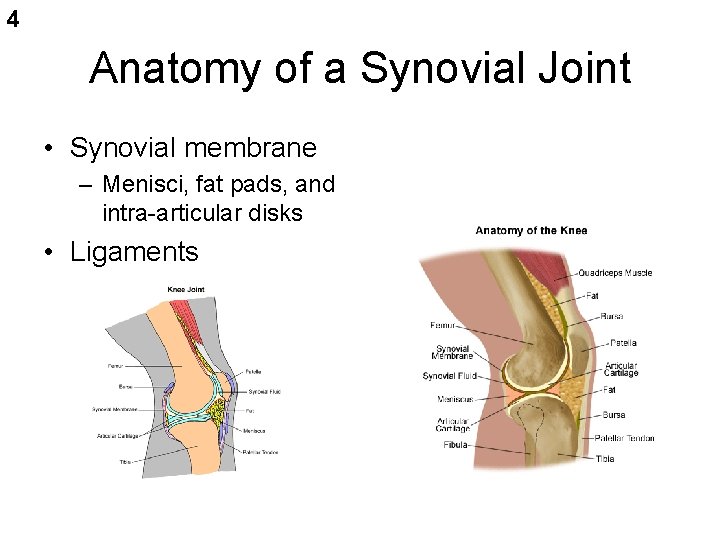
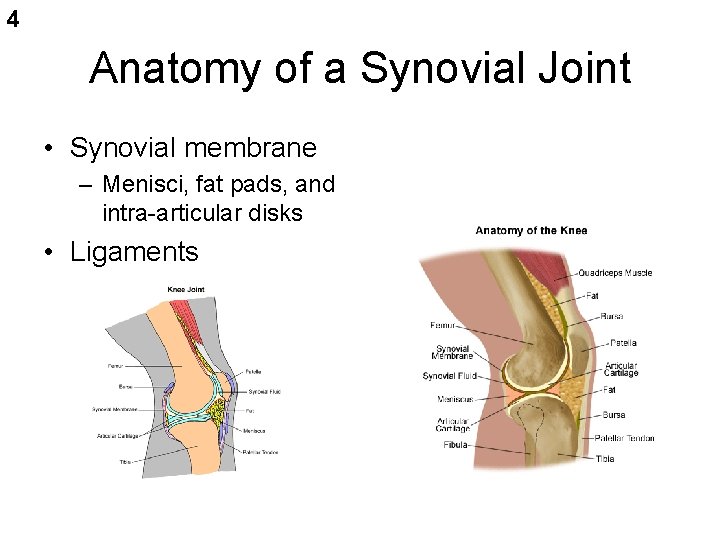
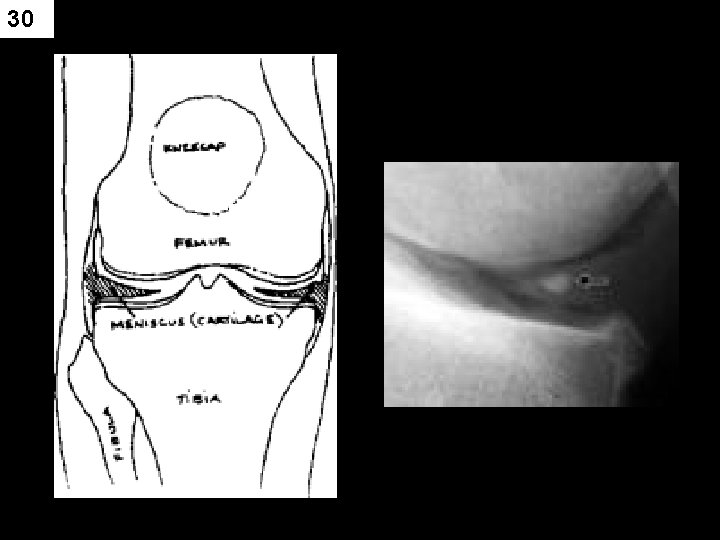
4 Anatomy of a Synovial Joint • Synovial membrane – Menisci, fat pads, and intra-articular disks • Ligaments
5 INDICATIONS FOR EXAM • This procedure is used to obtain diagnostic information regarding the joints and surrounding soft tissues or cartilage. • ligament, meniscus (cartilage), bursa Usually done for the knee • shoulder, hip, wrist, TMJ
6 Indications and Contraindications for Arthrography • Indications: – – – – Suspected injury of meniscus (tears) Suspected capsular damage Rupture of articular ligaments Cartilaginous defects Arthritic deformities (specifically TMJ) Congenital luxation ( dislocation) of hip Extent of damage from trauma • Contraindications: – Hypersensitivity to iodine
7 Clinical Symptoms • Pain • Swelling • Limited range of motion • Recurrent instability (such as ankle)
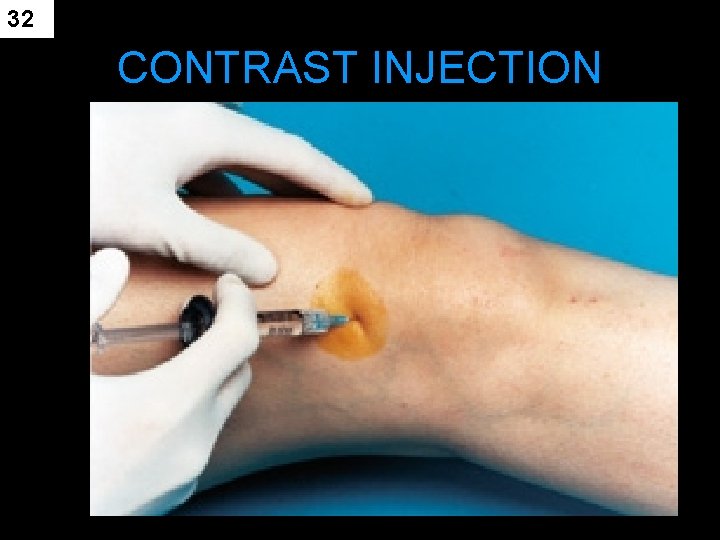
8 Contrast media • Contrast INJECTED into joint space – capsular space – bursa (30 – 100 ml may be needed) • CONTRAST – water based only – iodinated (ionic or nonionic) • Negative , positive or both (Double Contrast) • Negative – room air, CO 2 • Possible hazard of air is an air embolism • Water-soluble contrast agents – easily absorbed
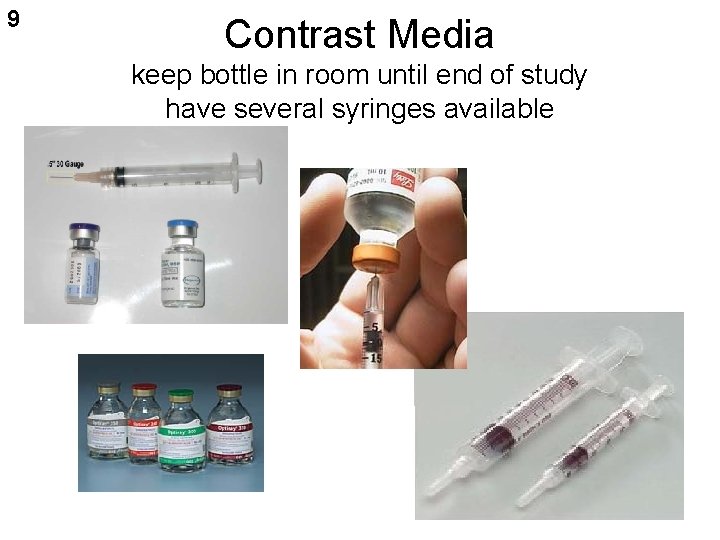
9 Contrast Media keep bottle in room until end of study have several syringes available
10 PROCEDURE – PREP • Patient Prep – (none prior to exam) – Pt comfort (gown, empty bladder) • get history • check allergies • SKIN PREP – may need to shave area of injection • betadine scrub – circular motions
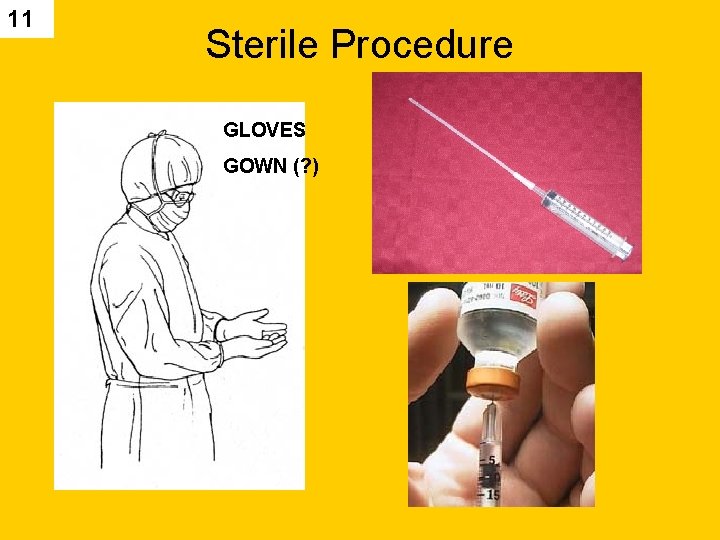
11 Sterile Procedure GLOVES GOWN (? )
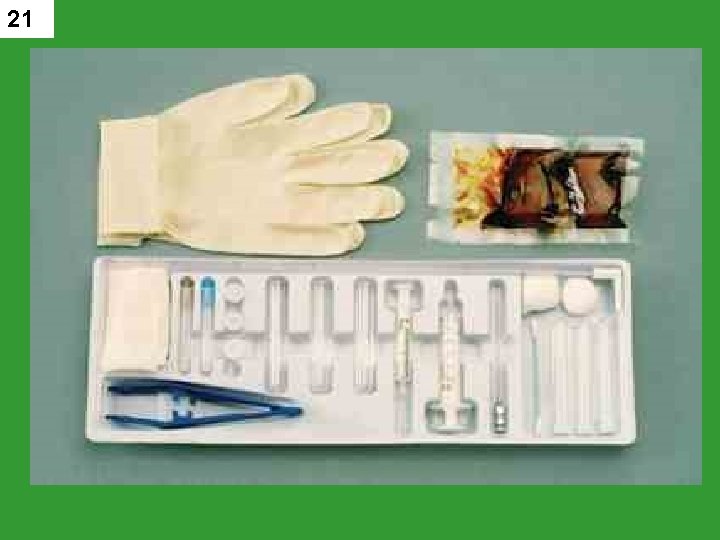
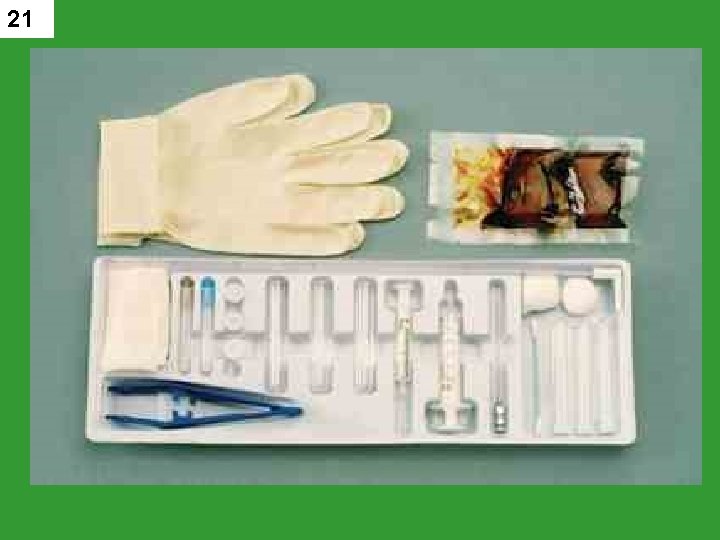
12 Sterile tray “arthrogram tray” Aseptic technique for skin cleansing – (betadine – check for allergy) • Local anesthetic • (usually on tray, put may have to draw up – sterile procedure) • do not contaminate tray

13 Aseptic Technique betadine scrub

14
15 ARTHROGRAM TRAY
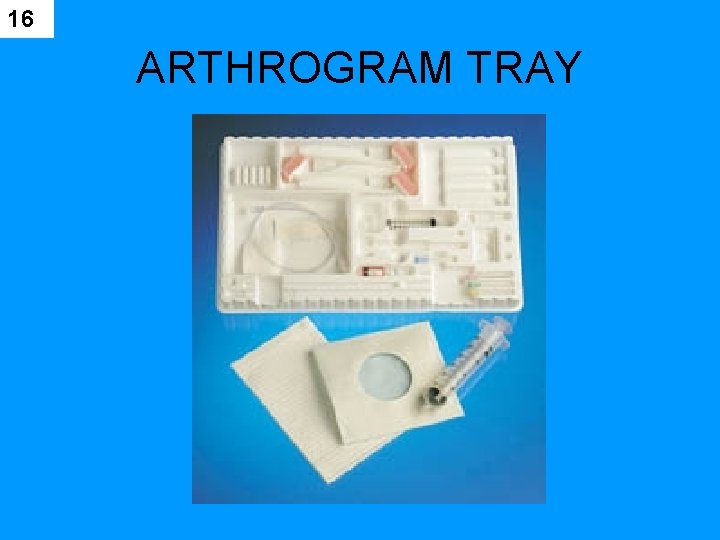
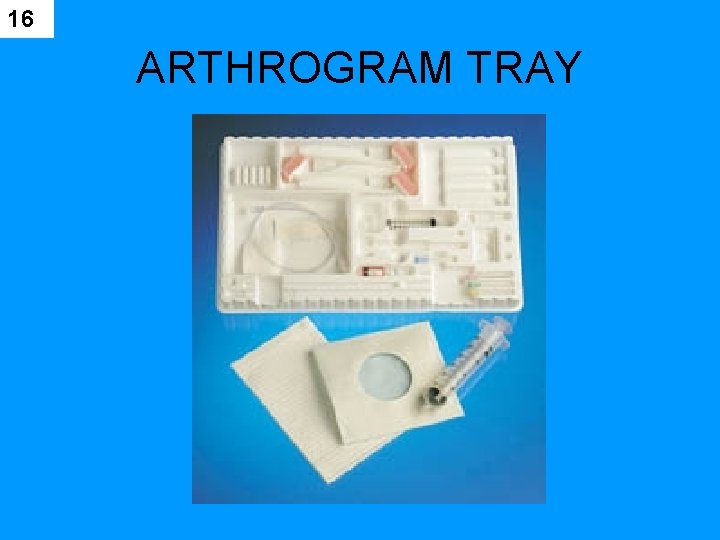
16 ARTHROGRAM TRAY
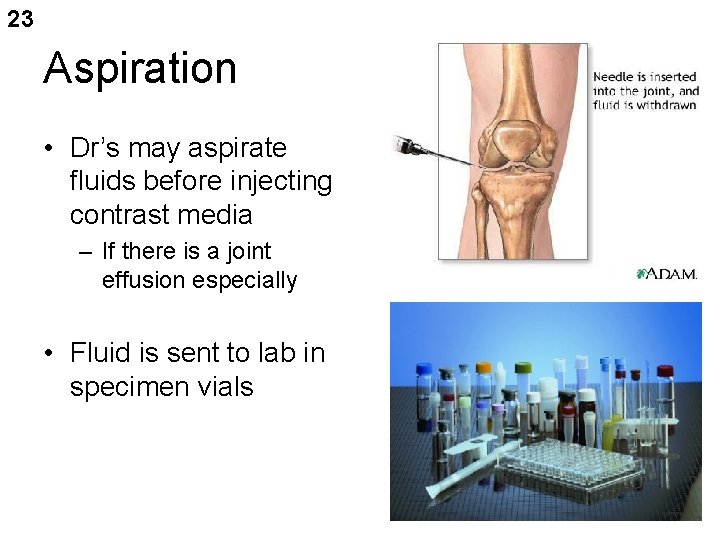
17 SUPPLIES Needles used – • length and gauge depends on part being examined • DR may aspirate joint prior to injection of contrast media • (have large syringes available) • Sterile gauze, towels, ace bandages
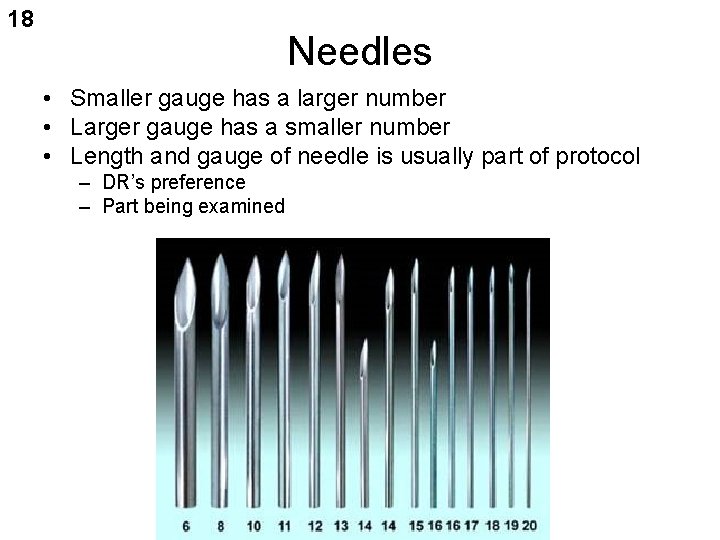
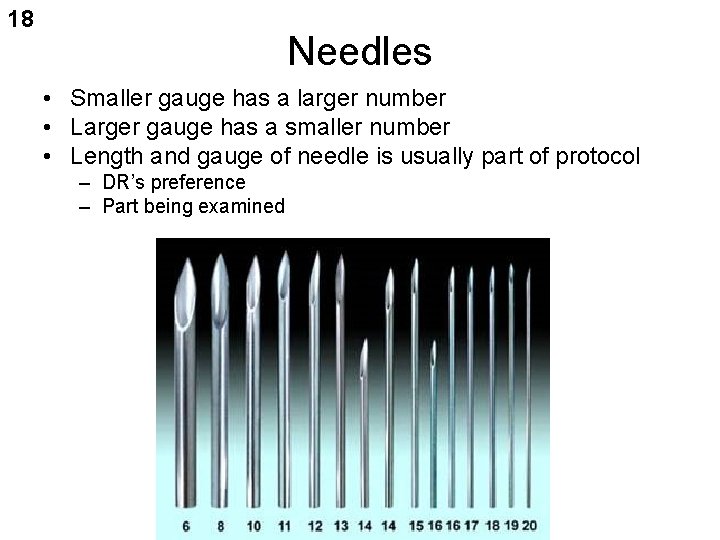
18 Needles • Smaller gauge has a larger number • Larger gauge has a smaller number • Length and gauge of needle is usually part of protocol – DR’s preference – Part being examined

19

20 Supplies Needed
21
22
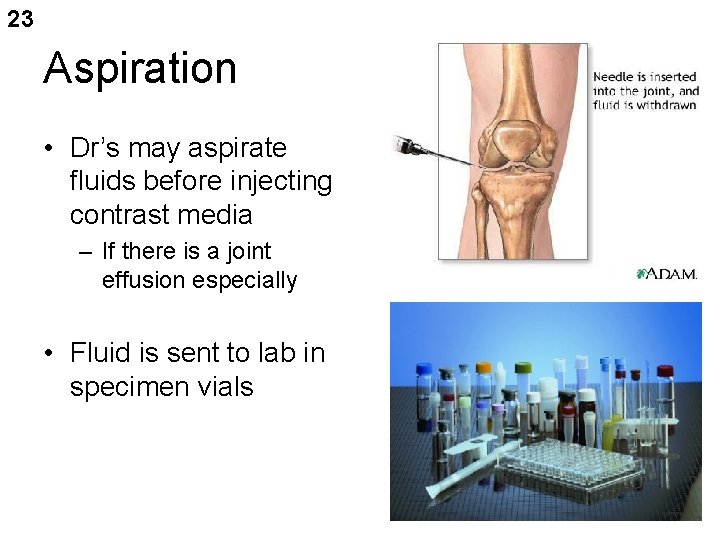
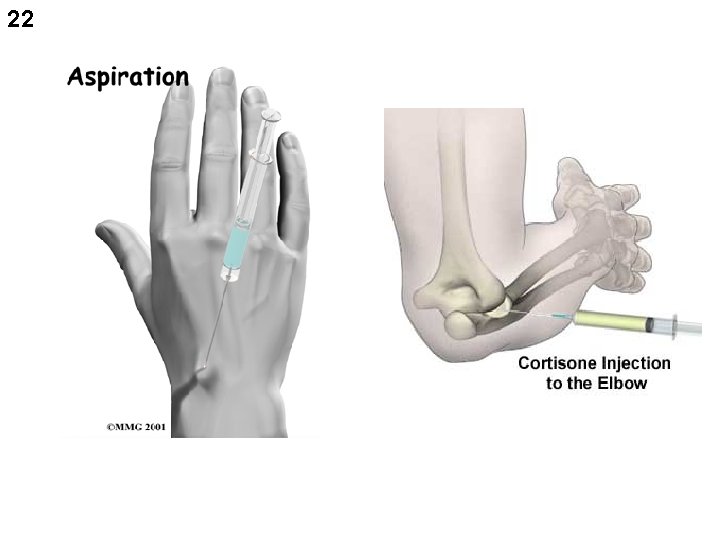
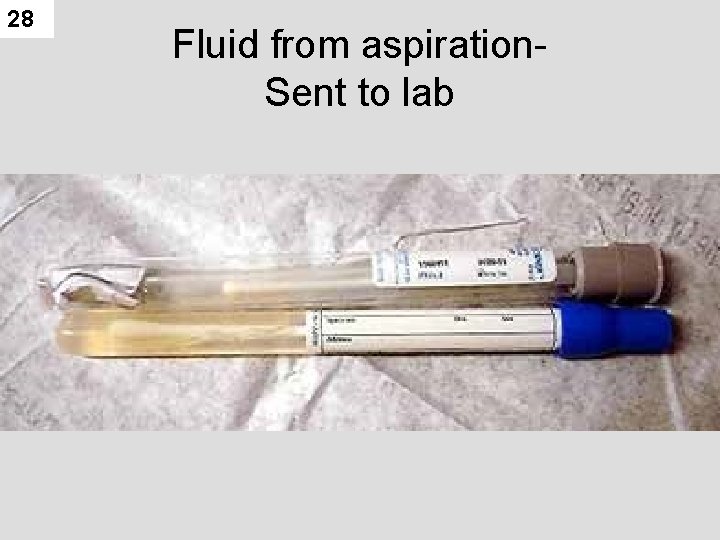
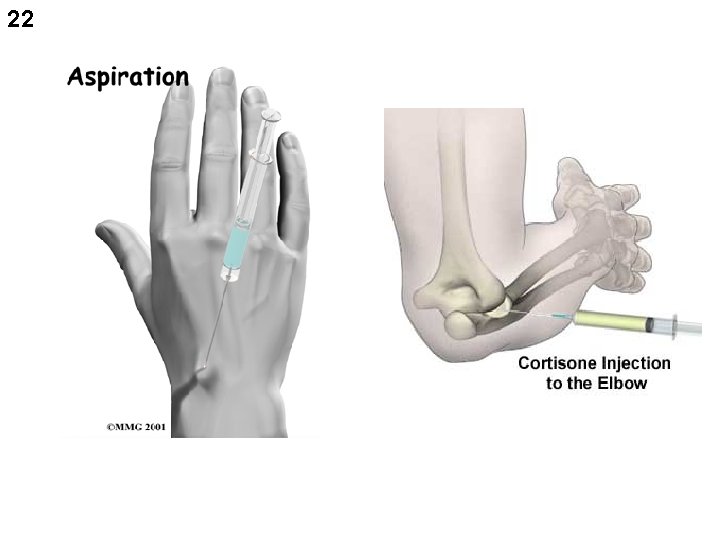
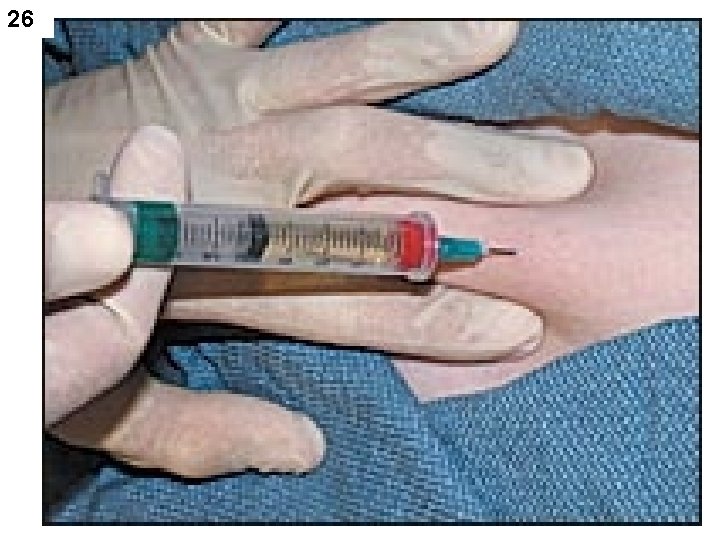
23 Aspiration • Dr’s may aspirate fluids before injecting contrast media – If there is a joint effusion especially • Fluid is sent to lab in specimen vials

24

25
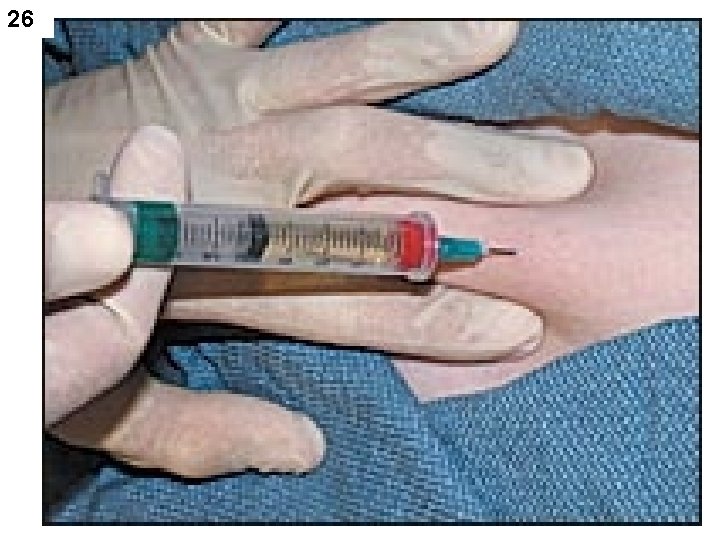
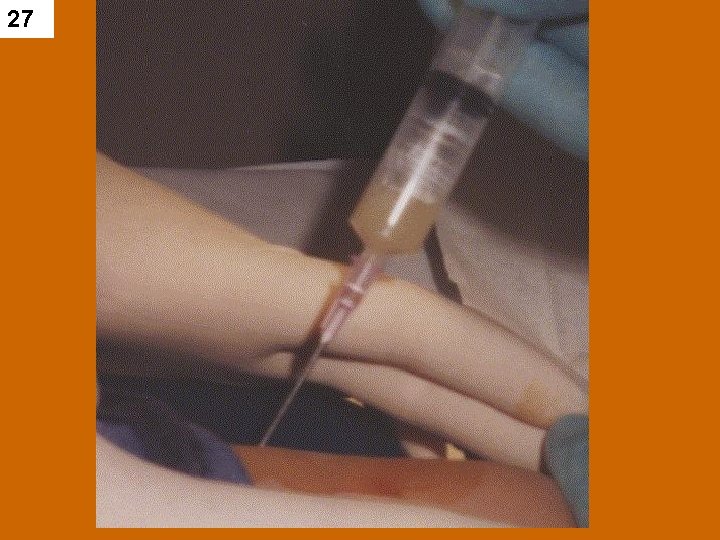
26
27
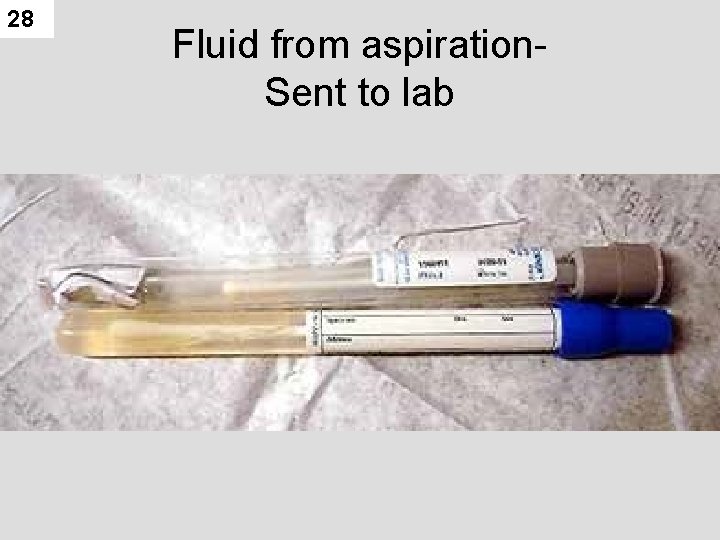
28 Fluid from aspiration. Sent to lab
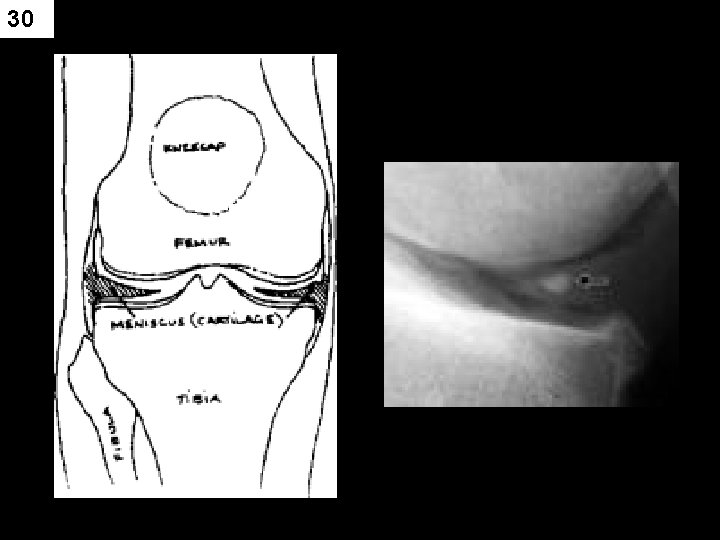
29 KNEE ARTHOGRAM Most common problem : • Pain and Swelling, – Limited ROM (range of motion) • athletic injuries • Knee support to stress knee • Contrast Injected – then part is stressed or moved to work contrast into joint spaces –
30
31 RADIOGRAPHY • SCOUT FILMS • AP • LATERAL • Other • (CHECK WITH Radiologist)
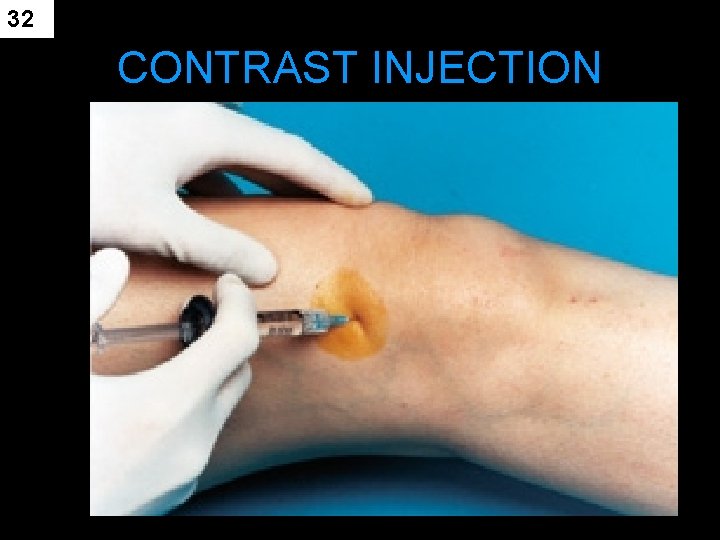
32 CONTRAST INJECTION

33
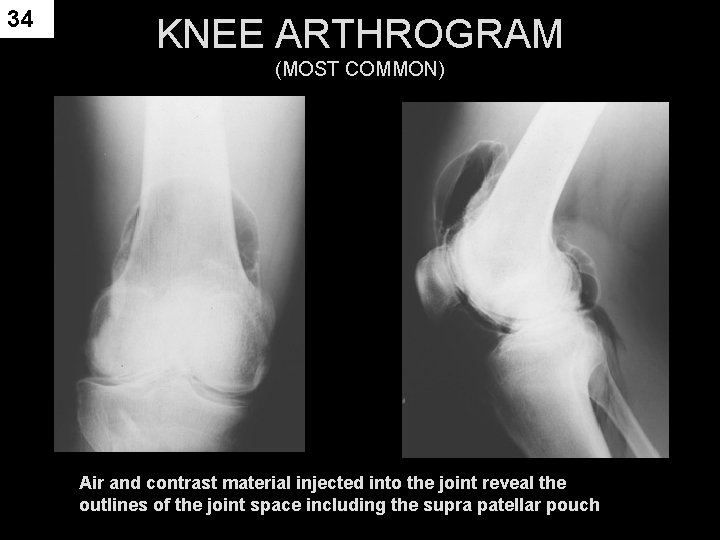
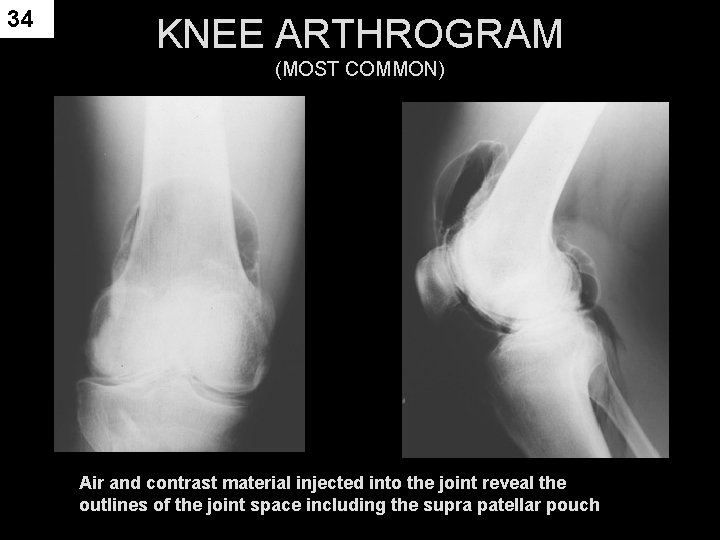
34 KNEE ARTHROGRAM (MOST COMMON) Air and contrast material injected into the joint reveal the outlines of the joint space including the supra patellar pouch
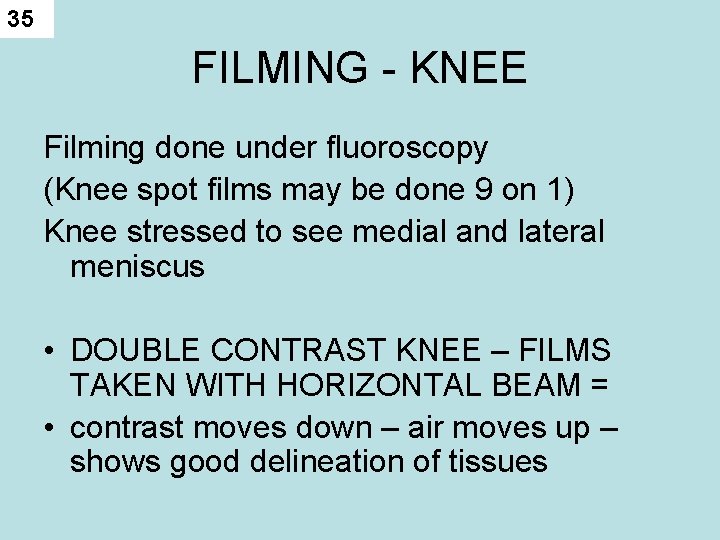
35 FILMING - KNEE Filming done under fluoroscopy (Knee spot films may be done 9 on 1) Knee stressed to see medial and lateral meniscus • DOUBLE CONTRAST KNEE – FILMS TAKEN WITH HORIZONTAL BEAM = • contrast moves down – air moves up – shows good delineation of tissues

36 For Cruciate ligaments patient may sit on end of table • Then a cross table lateral with knee flexed 90 degrees – taken
37
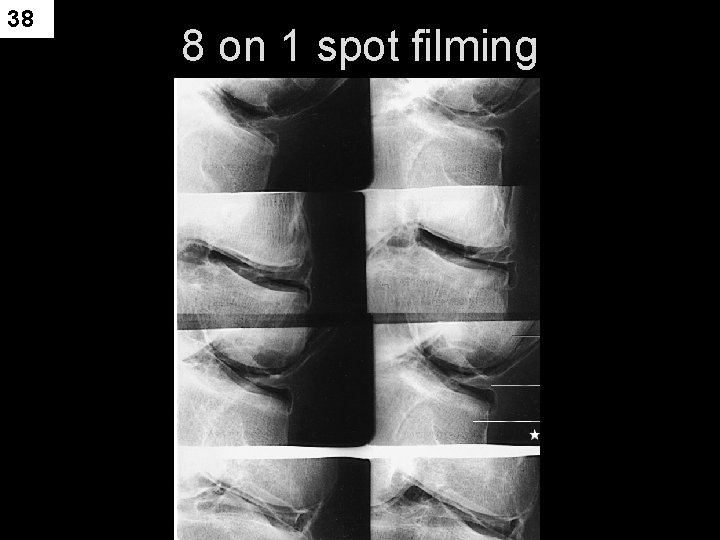
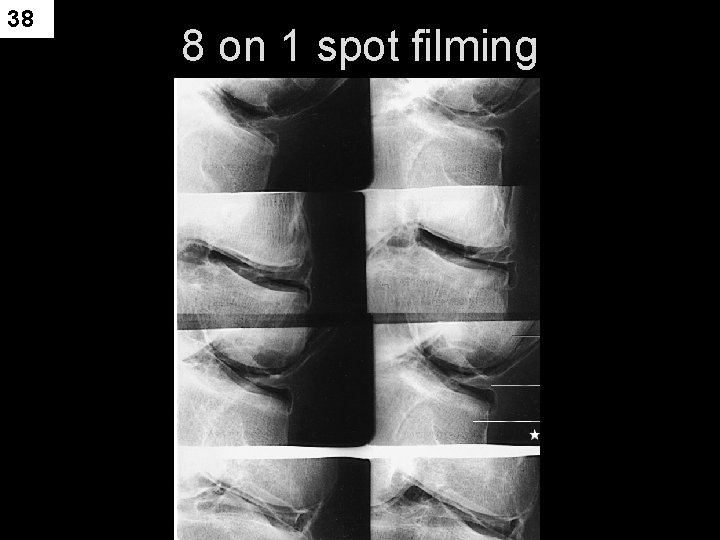
38 8 on 1 spot filming
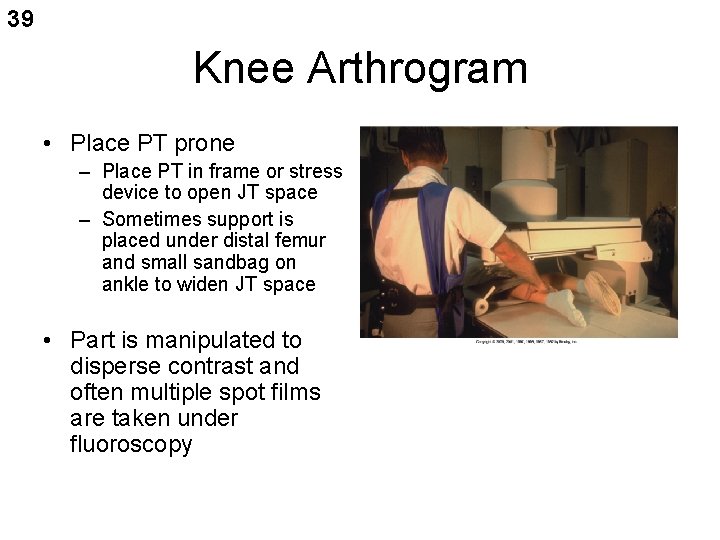
39 Knee Arthrogram • Place PT prone – Place PT in frame or stress device to open JT space – Sometimes support is placed under distal femur and small sandbag on ankle to widen JT space • Part is manipulated to disperse contrast and often multiple spot films are taken under fluoroscopy

40 Knee stressed to see medial and lateral meniscus
41 Knee Arthrogram • Overheads are done – AP, lateral, 20 degree right and left oblique – Sometimes Interconyloid fossa projections are required • Single contrast study for a torn meniscus may fail to demonstrate the tear • Usually single contrast studies are used to demonstrate loose particles of the JT • Post procedure – PT may feel tightness – This should go away in 1 -2 days – Can be treated with analgesics
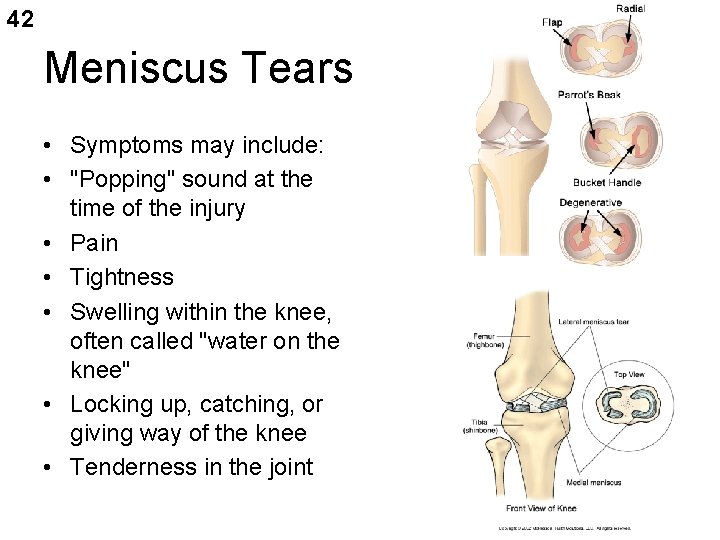
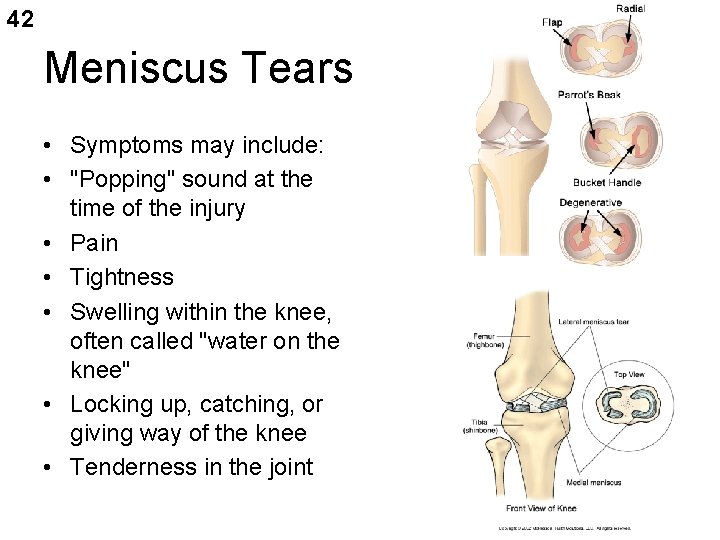
42 Meniscus Tears • Symptoms may include: • "Popping" sound at the time of the injury • Pain • Tightness • Swelling within the knee, often called "water on the knee" • Locking up, catching, or giving way of the knee • Tenderness in the joint

43 Knee Arthrogram double contrast study • smaller amounts of contrast can be used – Decreases discomfort to PT – Provides are more accurate study – Demonstrates menisci the best – Positive contrast coats menisci – Air rises
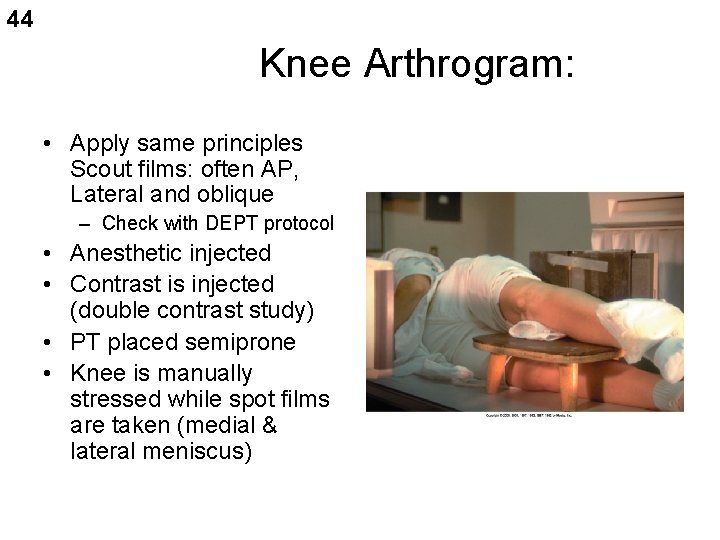
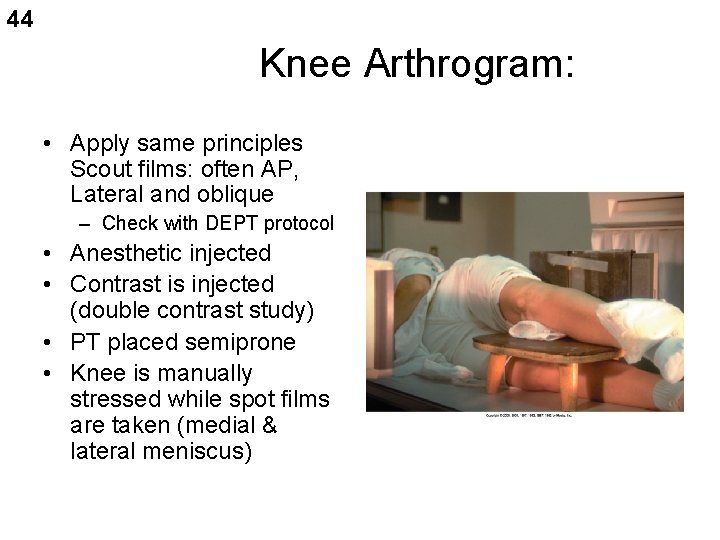
44 Knee Arthrogram: • Apply same principles Scout films: often AP, Lateral and oblique – Check with DEPT protocol • Anesthetic injected • Contrast is injected (double contrast study) • PT placed semiprone • Knee is manually stressed while spot films are taken (medial & lateral meniscus)
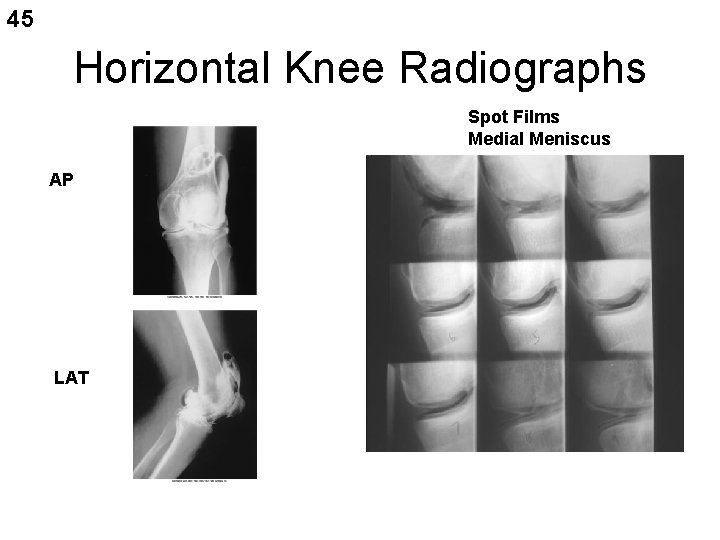
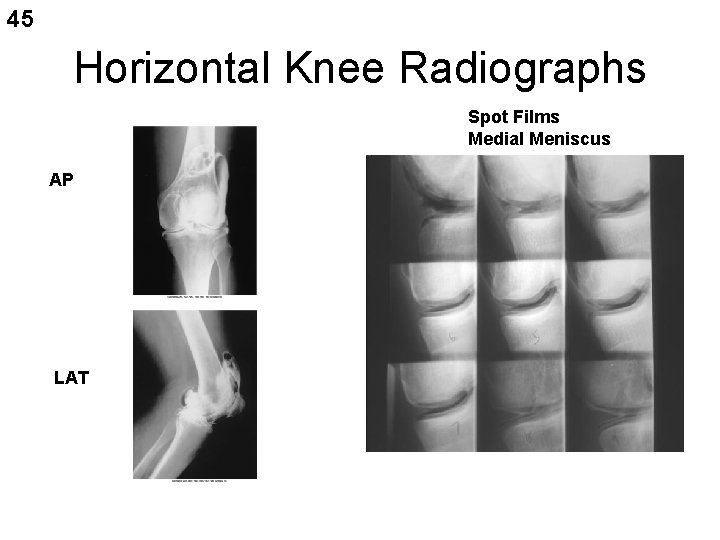
45 Horizontal Knee Radiographs Spot Films Medial Meniscus AP LAT
46 For Cruciate Ligaments • Double Contrast study • PT’ s sits with knee flexed 90 degrees over the side of the table • Firm pillow placed under knee so that forward pressure can be applied • PT holds IR with grid • Closely collimate • Tightly overexposed lateral projection is made
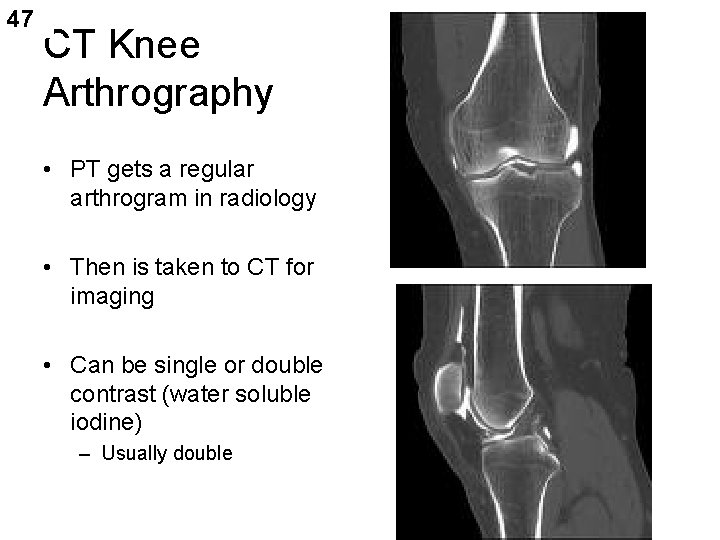
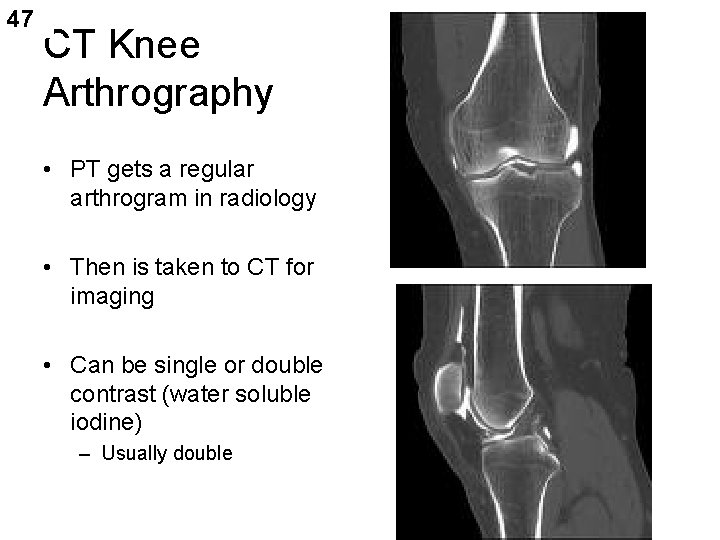
47 CT Knee Arthrography • PT gets a regular arthrogram in radiology • Then is taken to CT for imaging • Can be single or double contrast (water soluble iodine) – Usually double
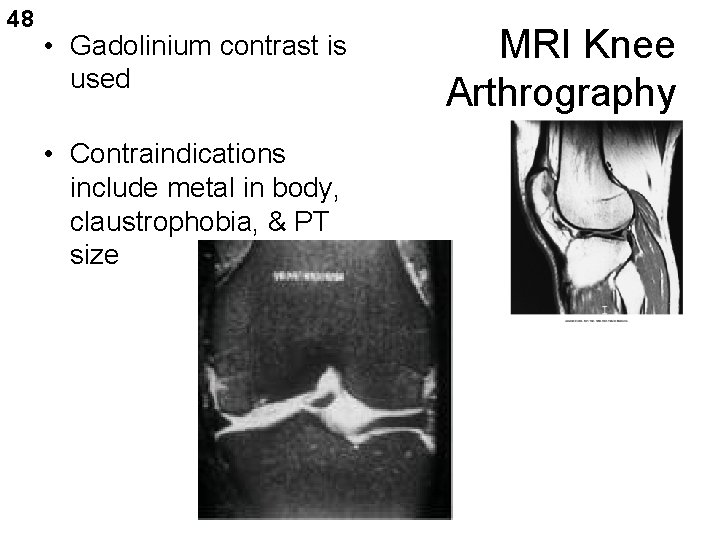
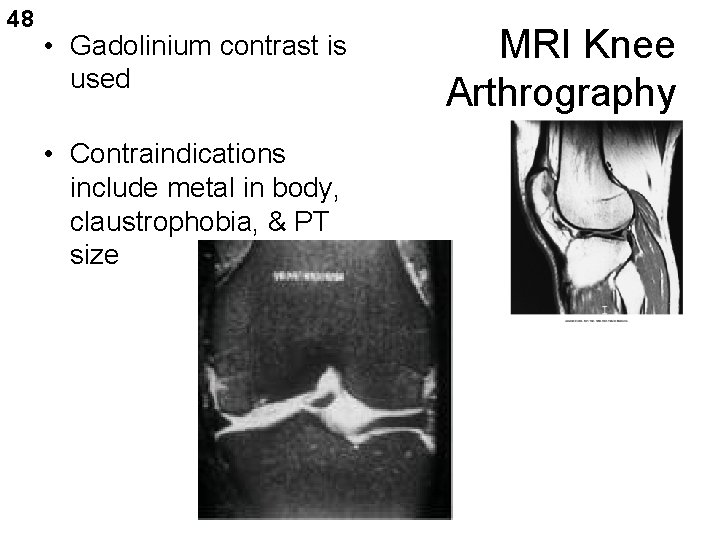
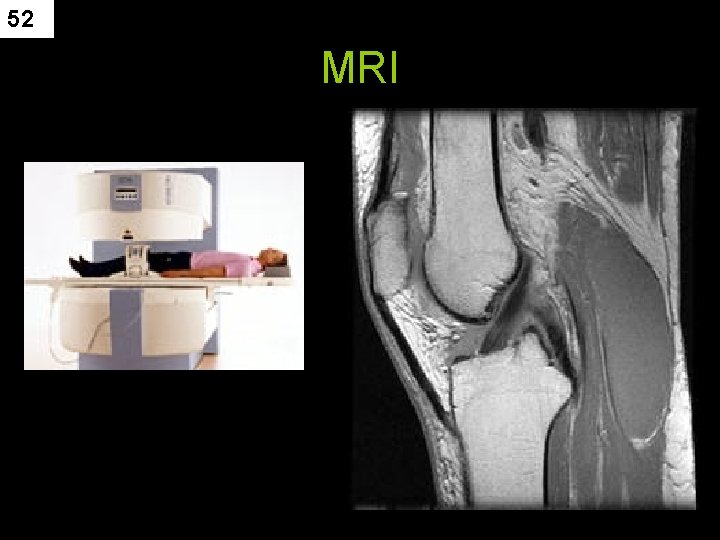
48 • Gadolinium contrast is used • Contraindications include metal in body, claustrophobia, & PT size MRI Knee Arthrography
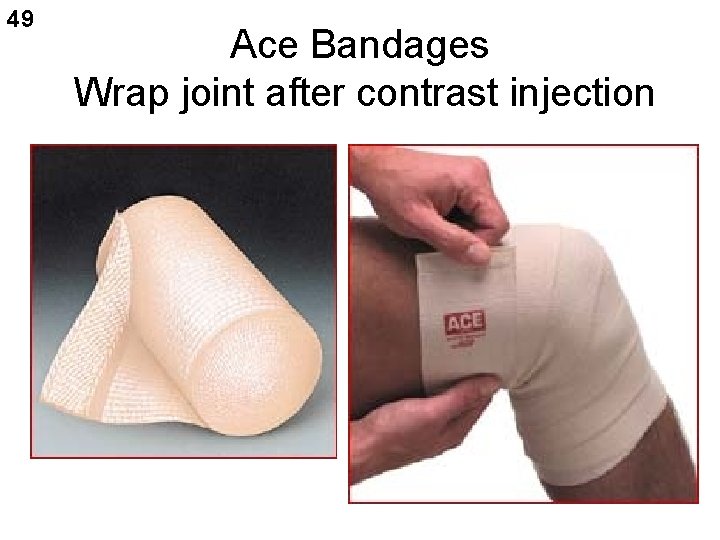
49 Ace Bandages Wrap joint after contrast injection
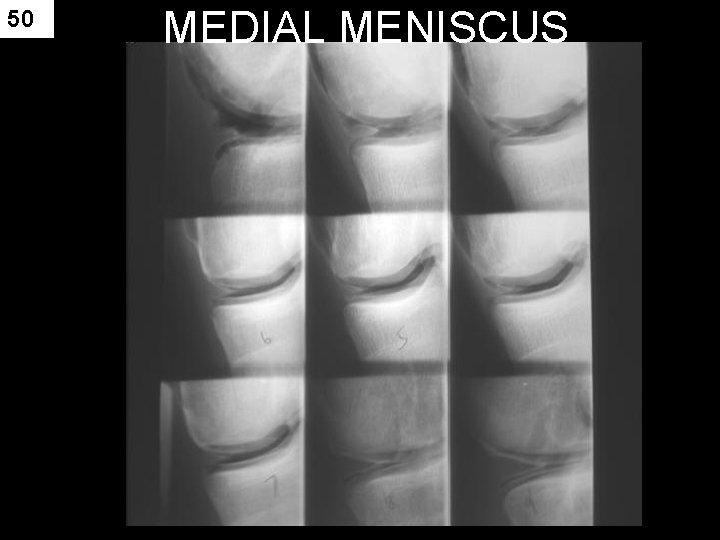
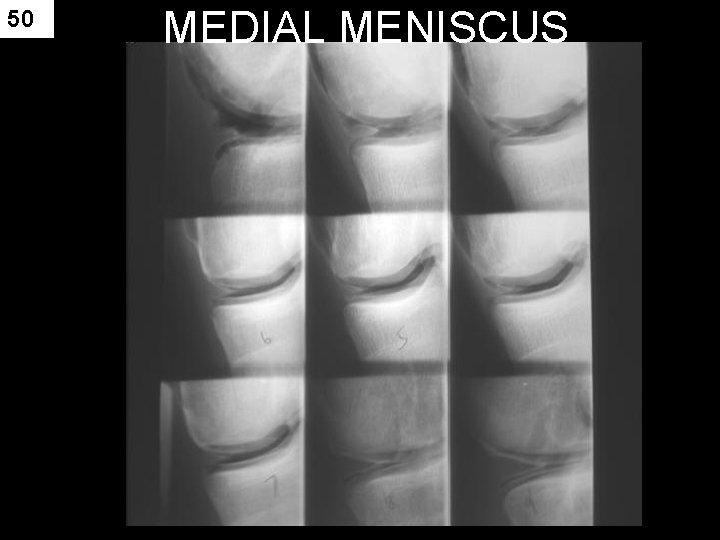
50 MEDIAL MENISCUS

51
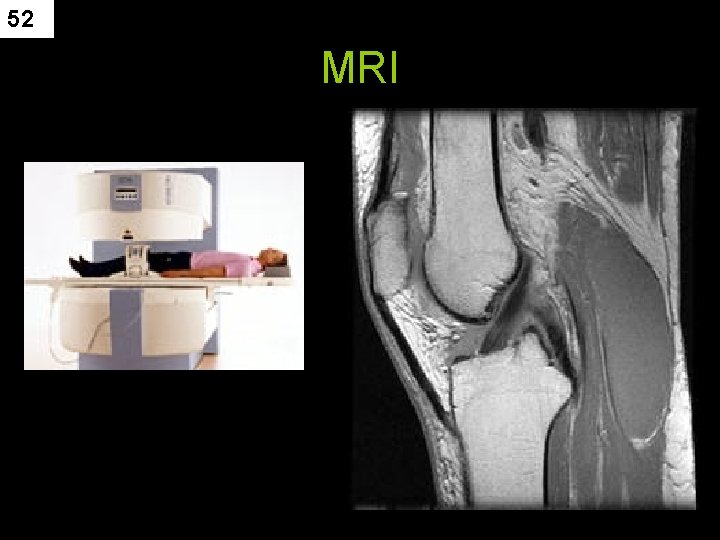
52 MRI
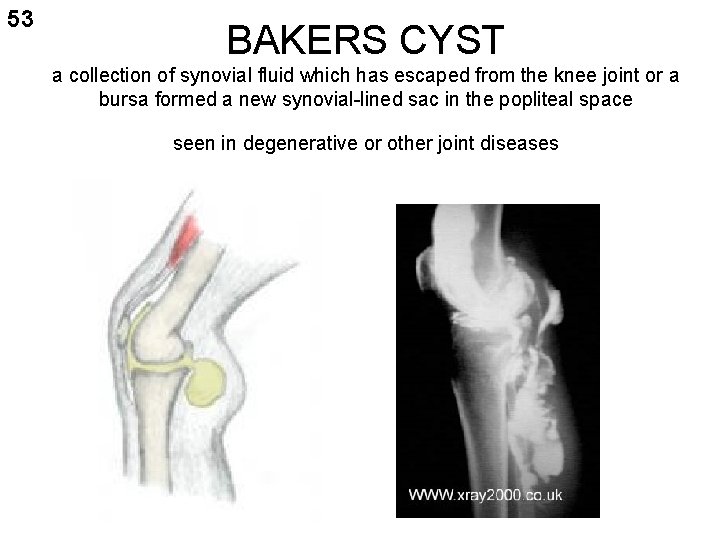
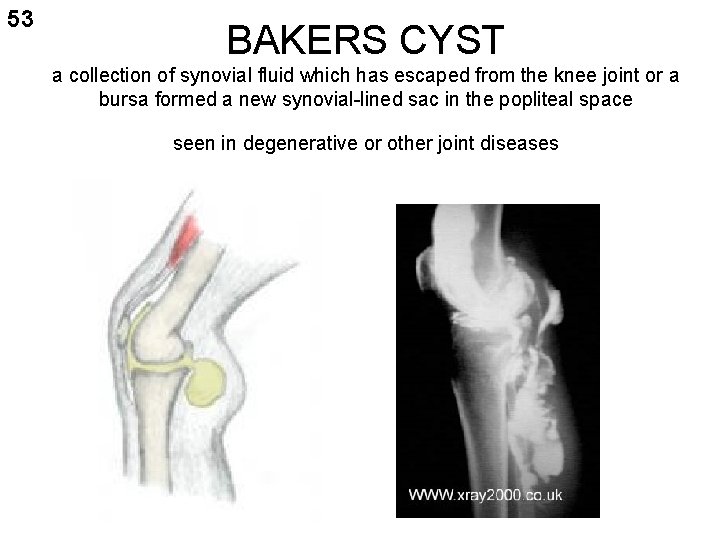
53 BAKERS CYST a collection of synovial fluid which has escaped from the knee joint or a bursa formed a new synovial-lined sac in the popliteal space seen in degenerative or other joint diseases

54
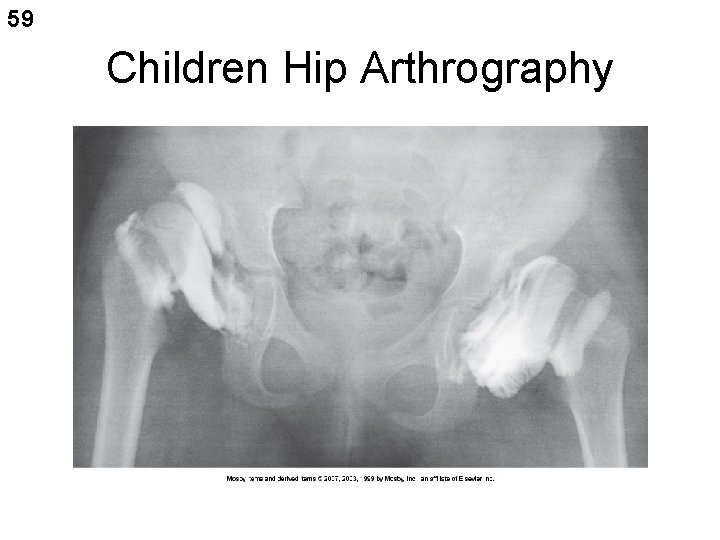
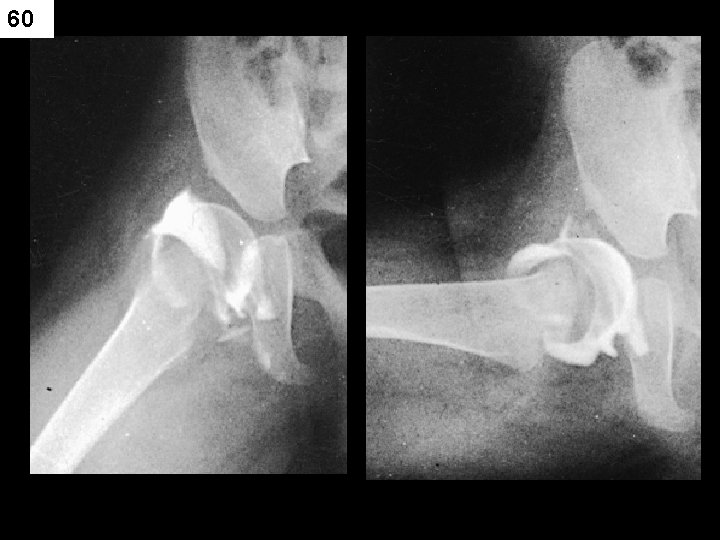
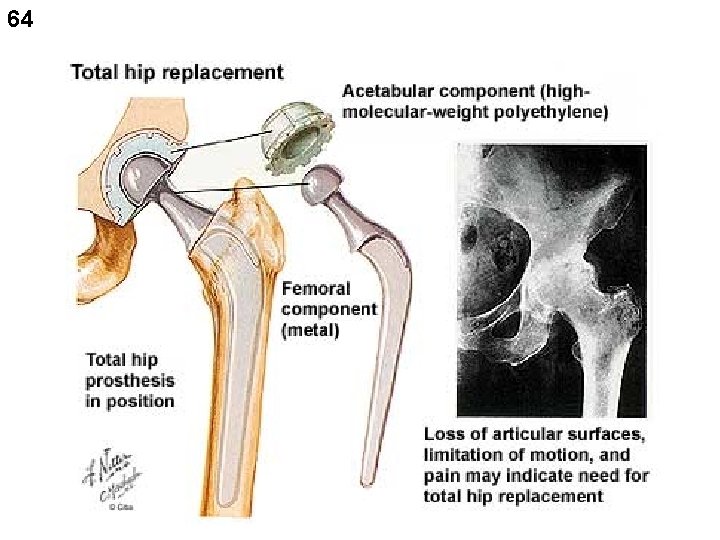
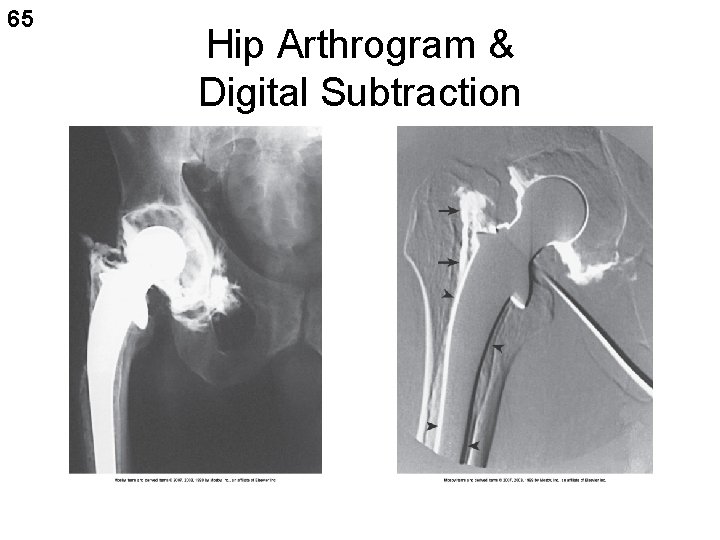
55 HIP ARTHROGRAM • Children - to check for congenital hip dislocation – before and after treatment • Adults – to check position of hip prosthesis - subtraction gives better images • Note: cement in the joint and contrast have the same density – see pg 567 Merrill’s

56
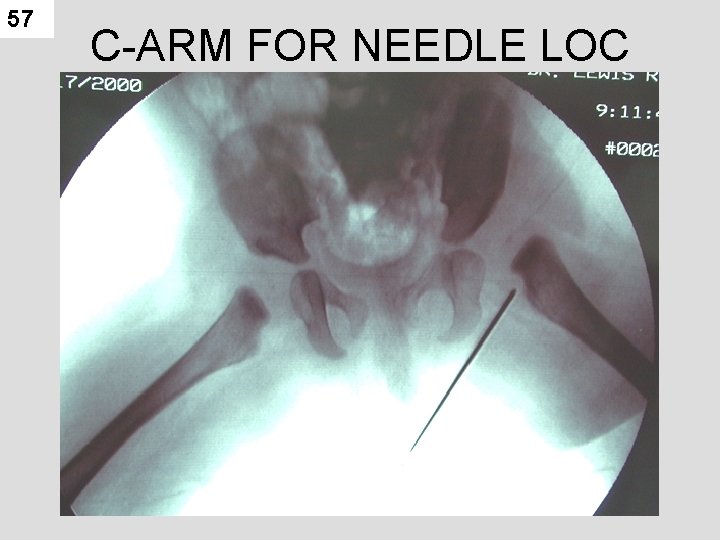
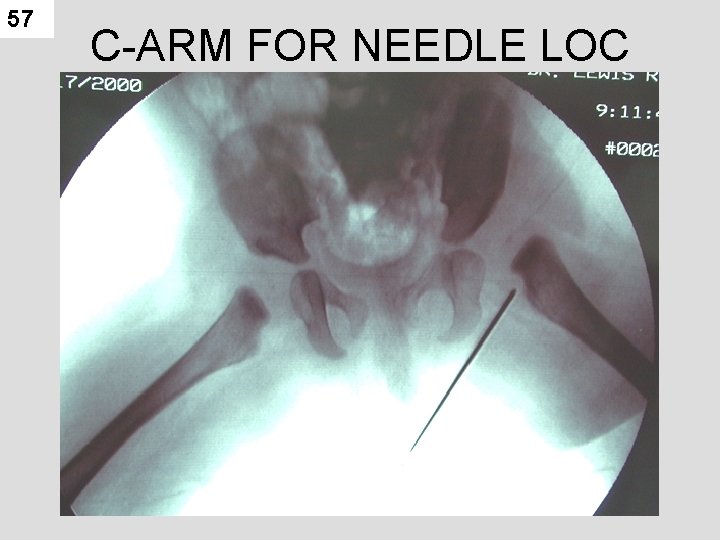
57 C-ARM FOR NEEDLE LOC
58 Hip Arthrogram • Common puncture site – ¾ “ distal to the inguinal crease – ¾” lateral to the palpated femoral pulse • Spinal needle is used due to how deep the hip joint is into the body.
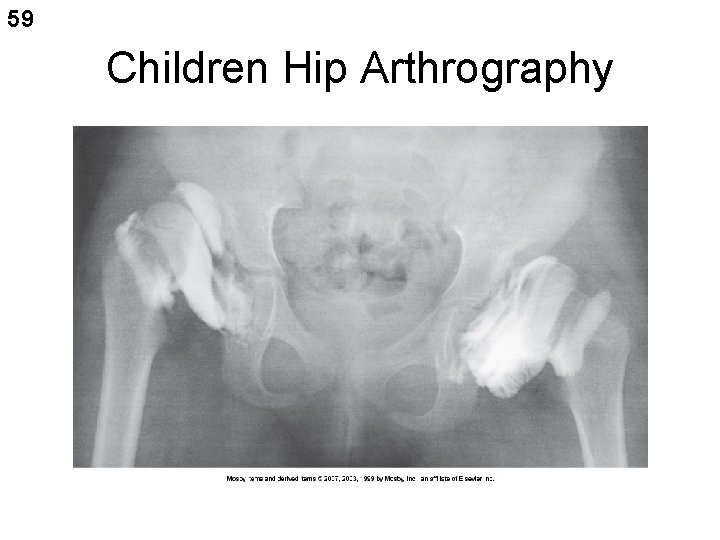
59 Children Hip Arthrography
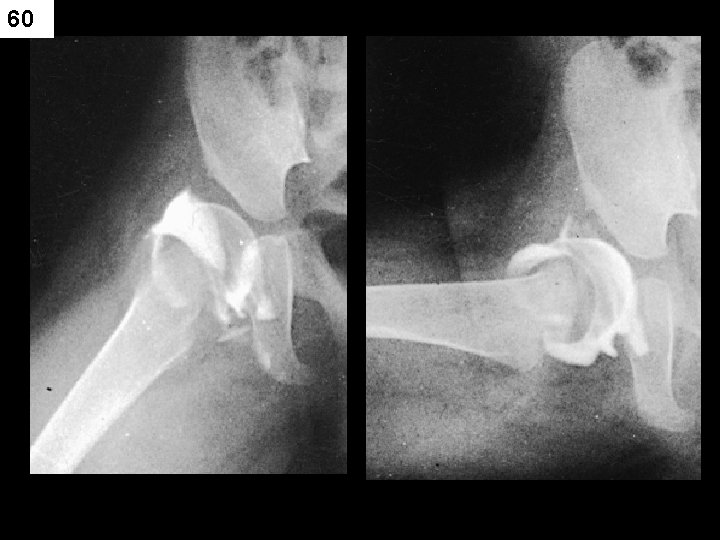
60

61
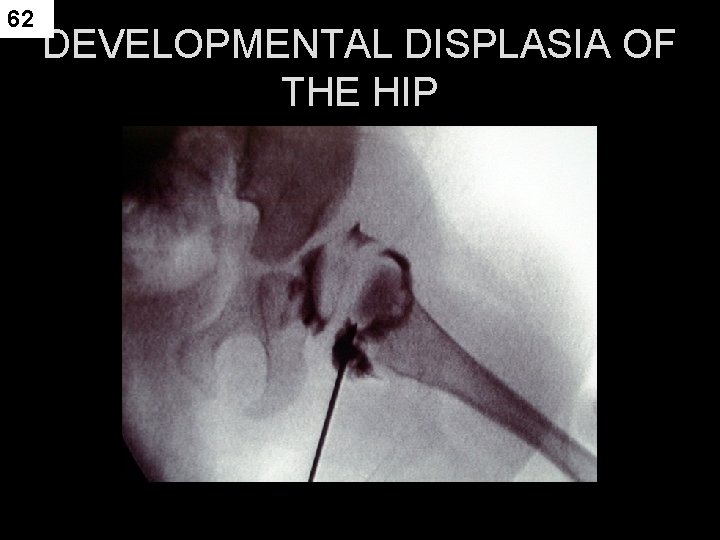
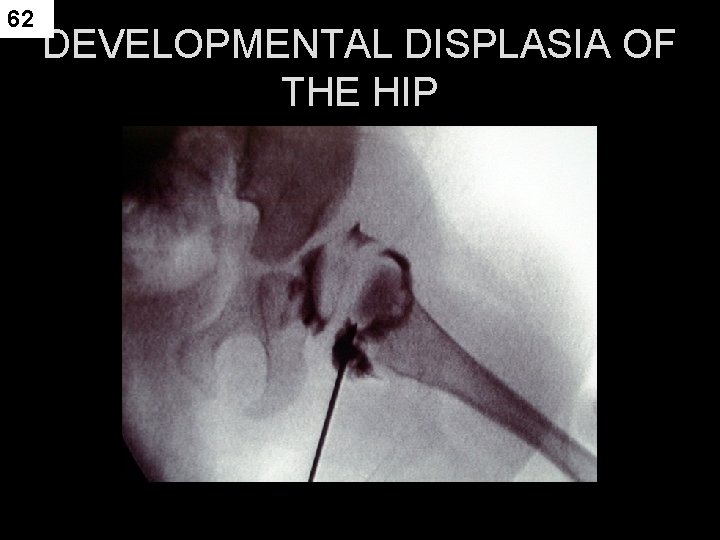
62 DEVELOPMENTAL DISPLASIA OF THE HIP

63
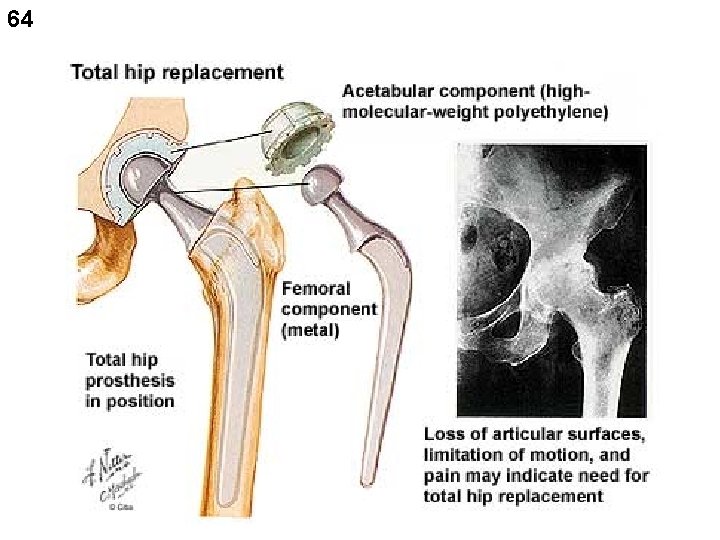
64
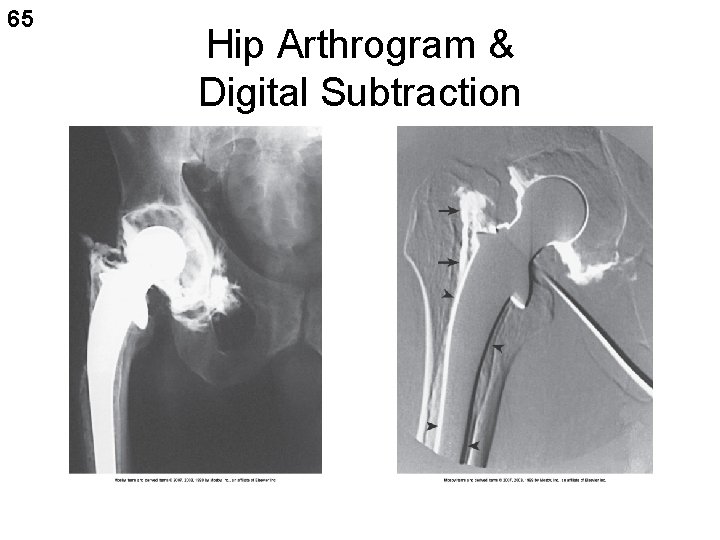
65 Hip Arthrogram & Digital Subtraction

66

67

68

69

70
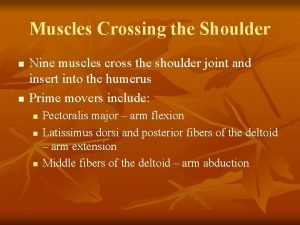
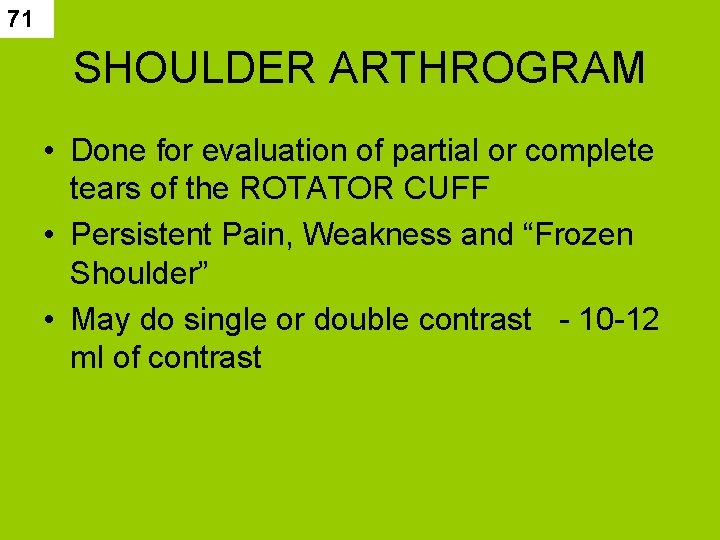
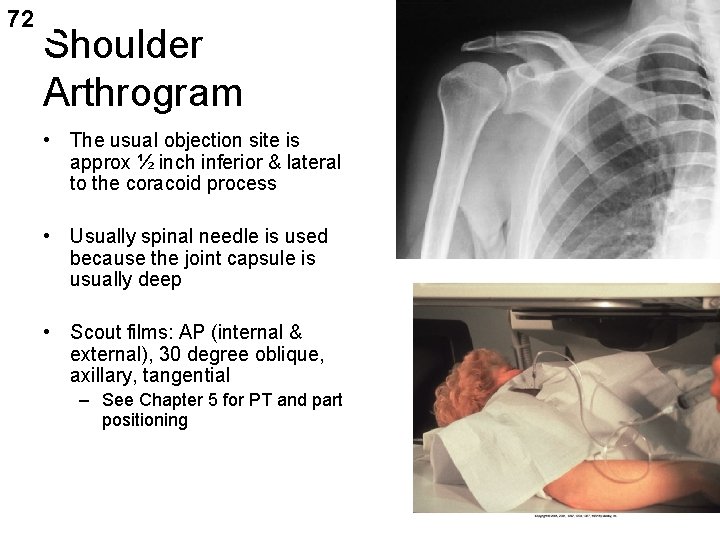
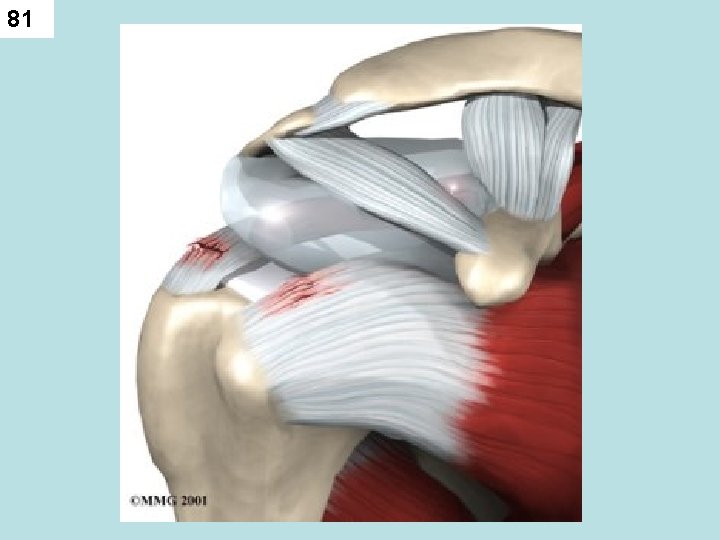
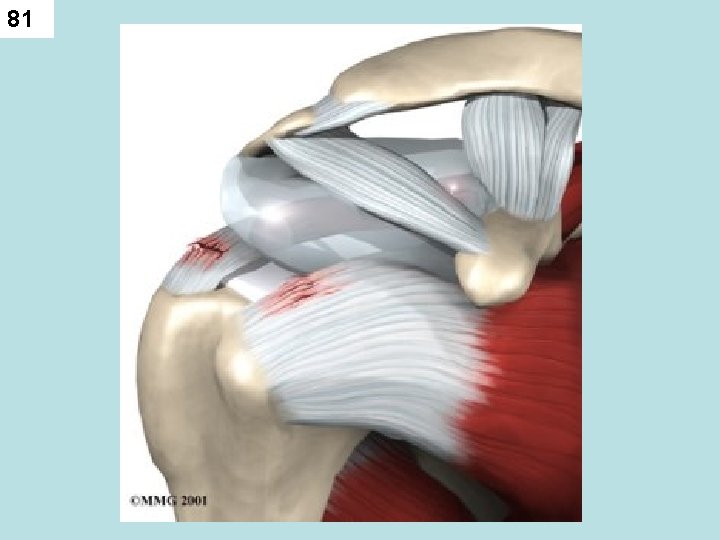
71 SHOULDER ARTHROGRAM • Done for evaluation of partial or complete tears of the ROTATOR CUFF • Persistent Pain, Weakness and “Frozen Shoulder” • May do single or double contrast - 10 -12 ml of contrast
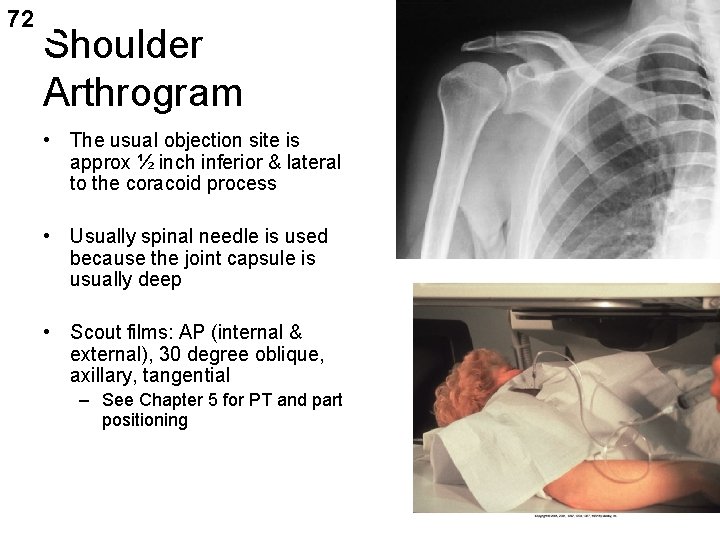
72 Shoulder Arthrogram • The usual objection site is approx ½ inch inferior & lateral to the coracoid process • Usually spinal needle is used because the joint capsule is usually deep • Scout films: AP (internal & external), 30 degree oblique, axillary, tangential – See Chapter 5 for PT and part positioning AP scout
73 SCOUT FILMS • AP – – INTERNAL & EXTERNAL ROTATION • GRASHEY (OBL FOR FOSSA) • AXILLARY (THUMB UP) FOR GROOVE • TRANSTHORACIC or Y -VIEW
74 Shoulder Arthrogram • Indications: – Partial or complete tears of rotator cuff – Tears of glenoid labrum – Persistent pain or weakness – Frozen shoulder • Single or double contrast can be used – Single 10 -12 ml – Double 3 -4 positive contrast and 10 -12 of air
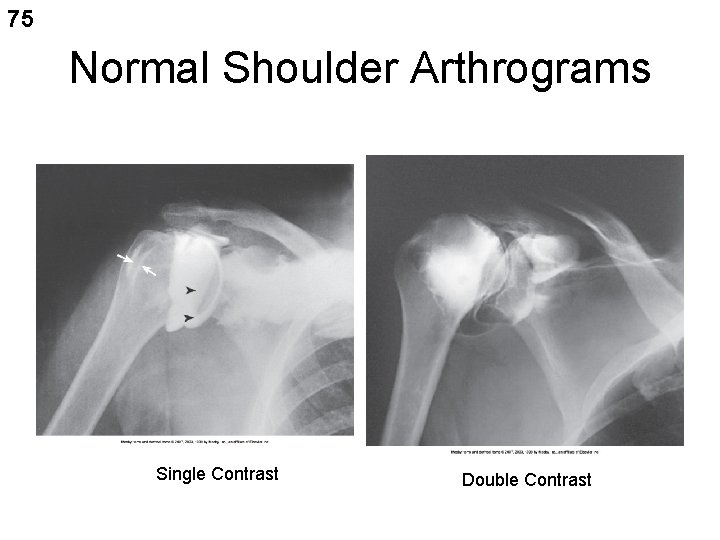
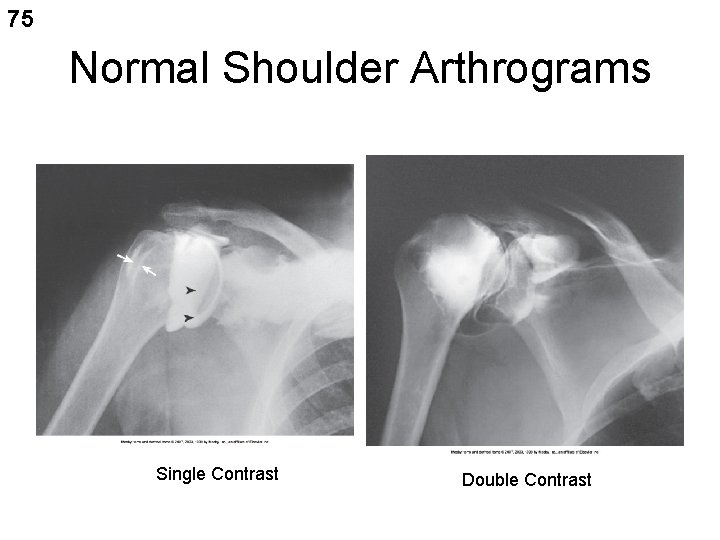
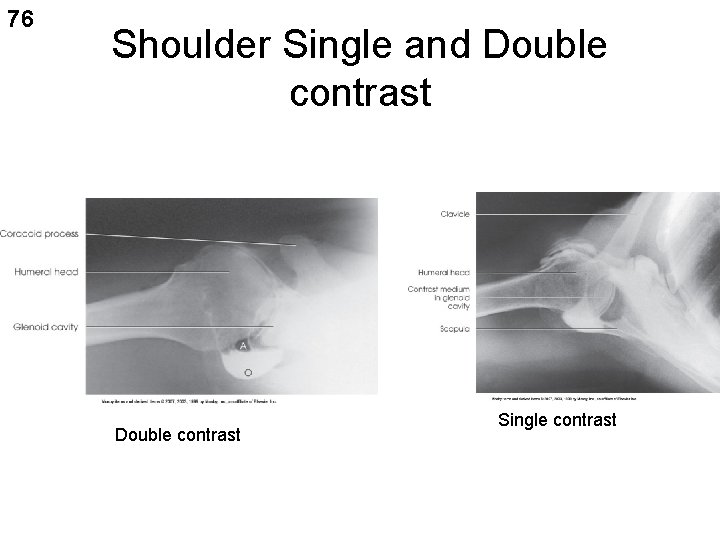
75 Normal Shoulder Arthrograms Single Contrast Double Contrast
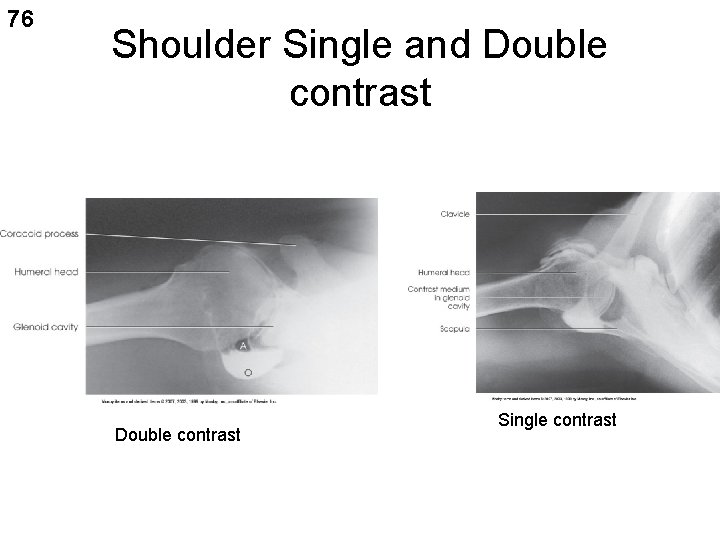
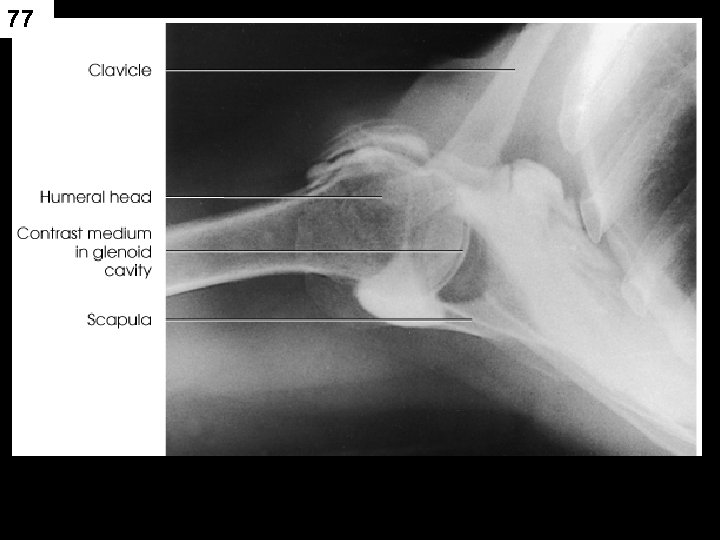
76 Shoulder Single and Double contrast Single contrast
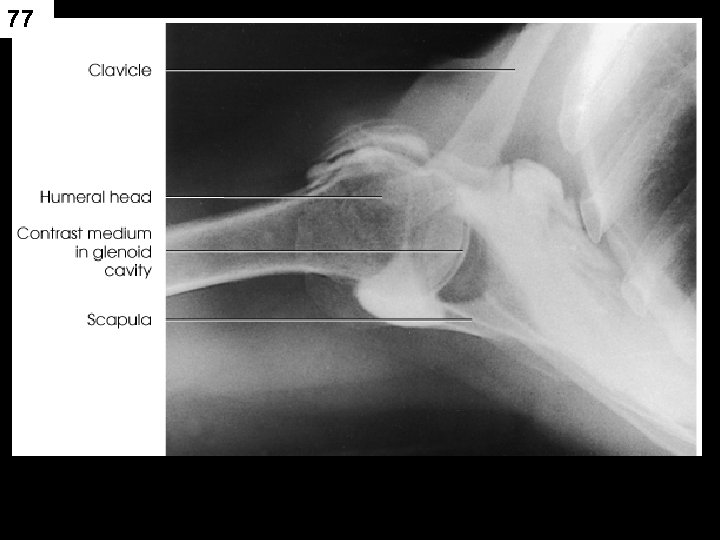
77
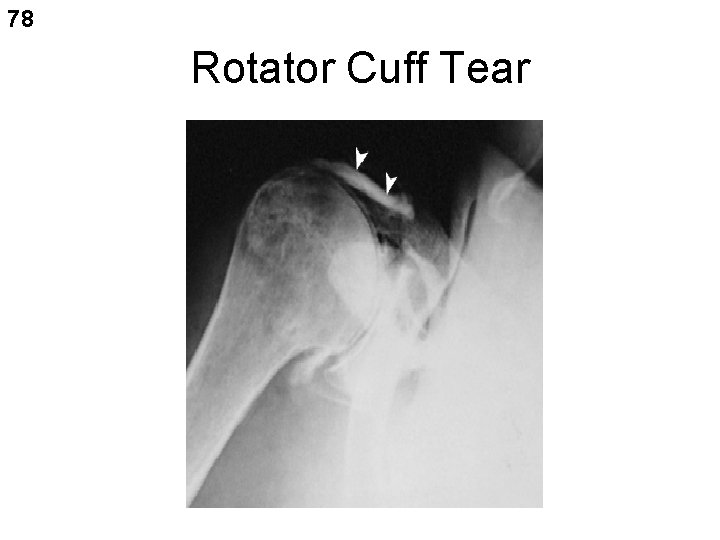
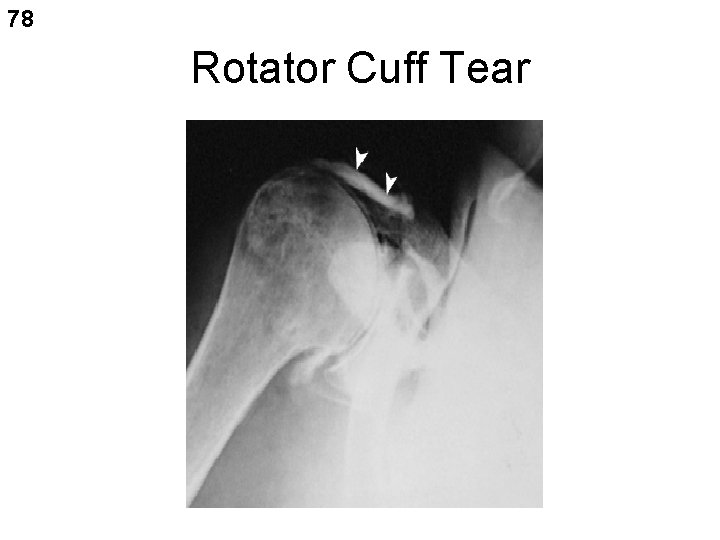
78 Rotator Cuff Tear
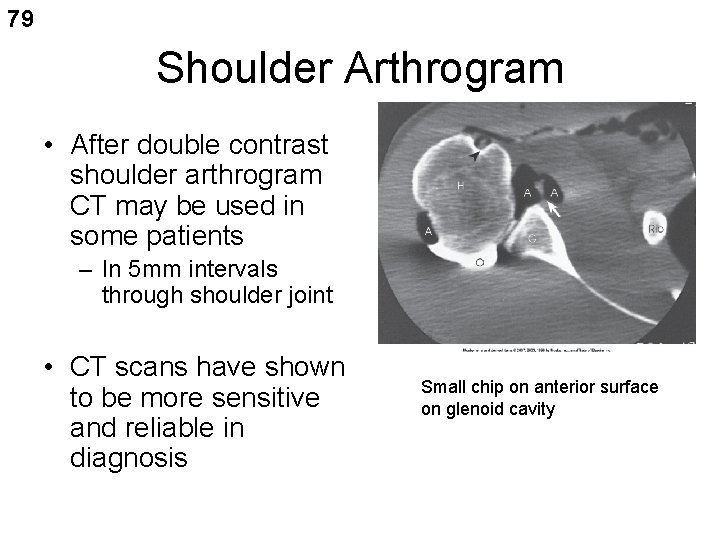
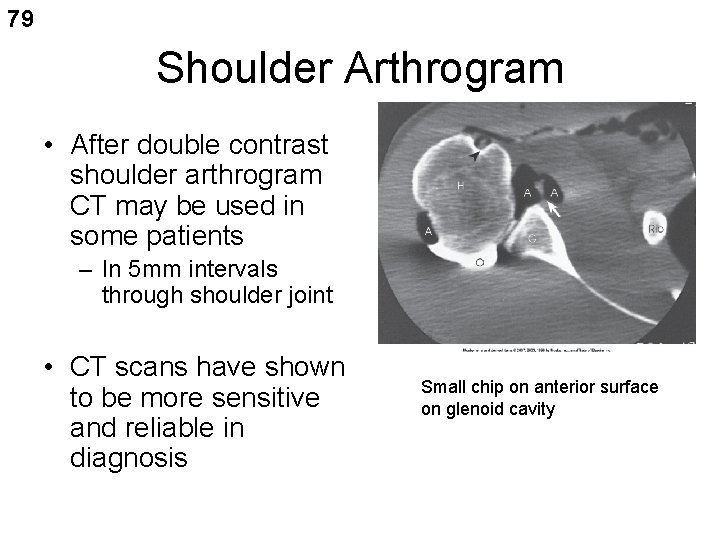
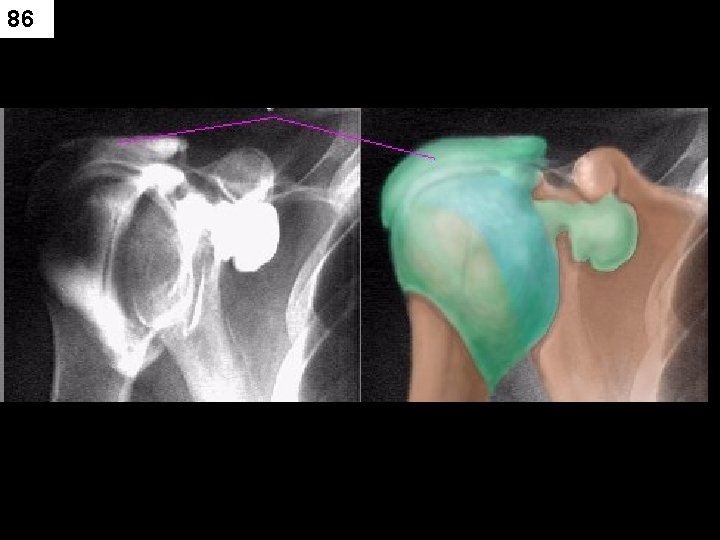
79 Shoulder Arthrogram • After double contrast shoulder arthrogram CT may be used in some patients – In 5 mm intervals through shoulder joint • CT scans have shown to be more sensitive and reliable in diagnosis Small chip on anterior surface on glenoid cavity

80
81
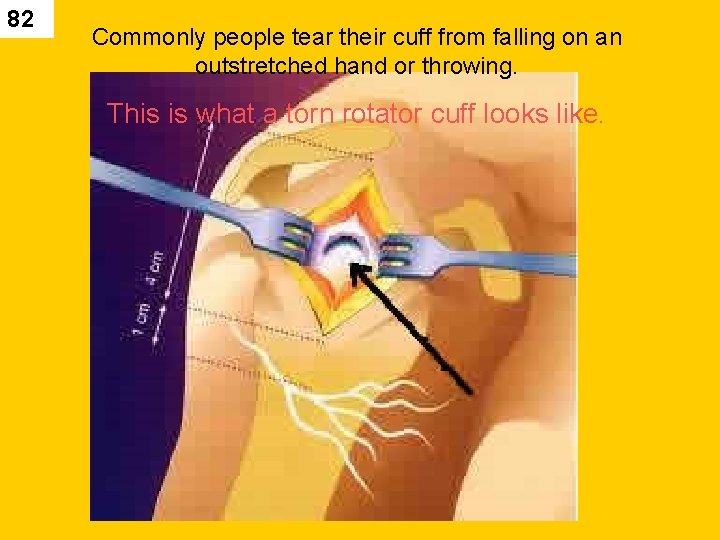
82 Commonly people tear their cuff from falling on an outstretched hand or throwing. This is what a torn rotator cuff looks like.
83

84

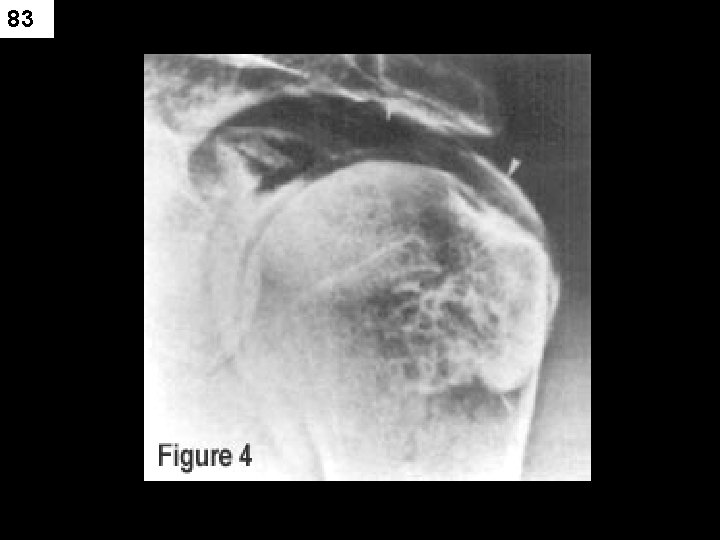
85 Single-contrast arthrogram showing rotator cuff tear (arrow).
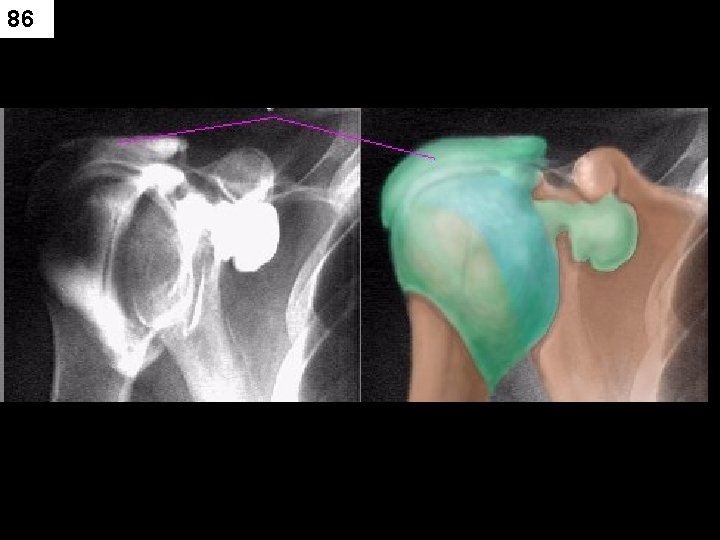
86

87
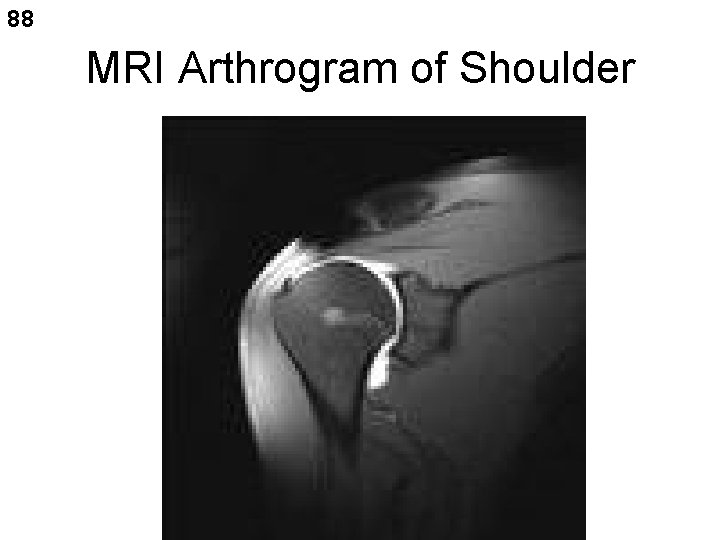
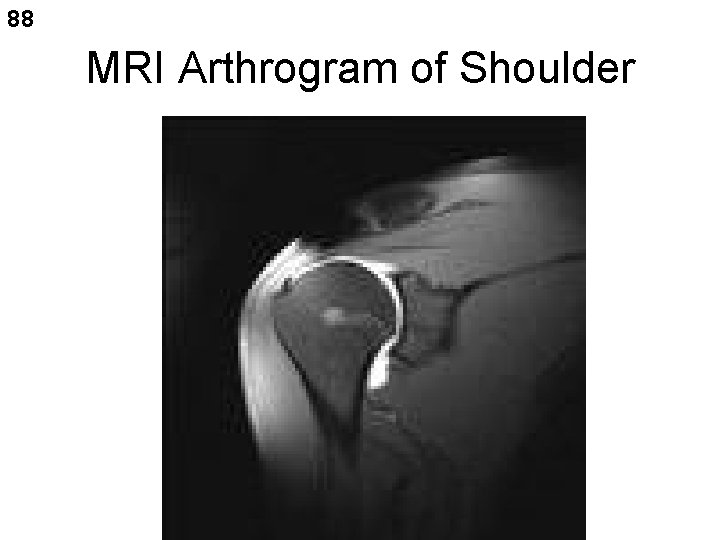
88 MRI Arthrogram of Shoulder

89

90
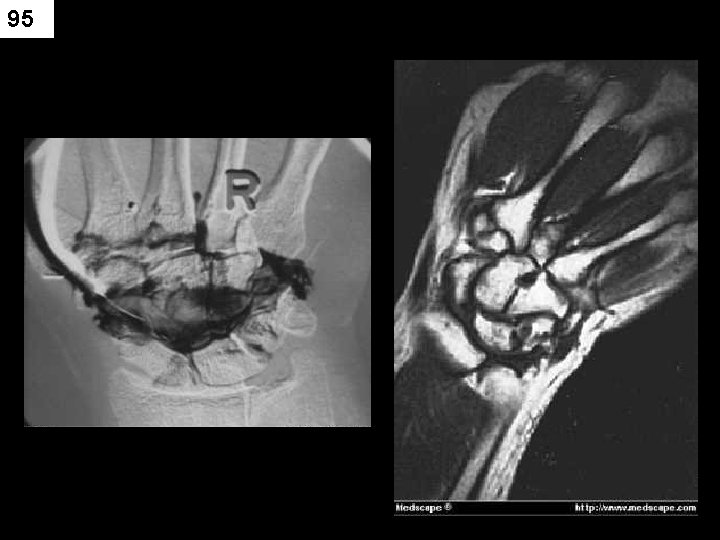
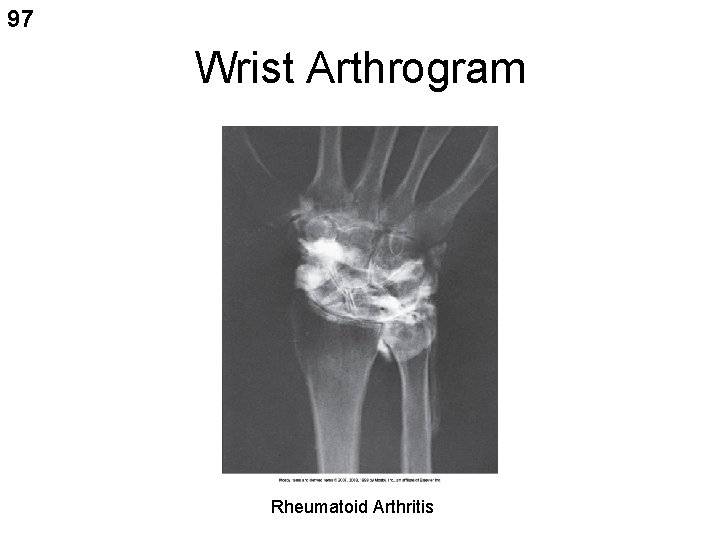
91 Wrist Arthrogram • Indications: trauma, persistent pain, limited ROM. • Contrast is injected through the dorsal wrist at the articulation of the radius, scaphoid and lunate – 1. 5 -4 ml water soluble iodinated contrast • After injection the wrist is carefully moved to spread contrast • Under fluoro or tape recording the wrist is rotated for exact area of leakage • AP, LAT and both obliques often taken (check DEPT protocols
92 WRIST ARTHROGRAM • Trauma, persistent pain, limited rom • Wrist gently manipulated after contrast media injection • 1. 5 – 4 ml of contrast injected

93

94
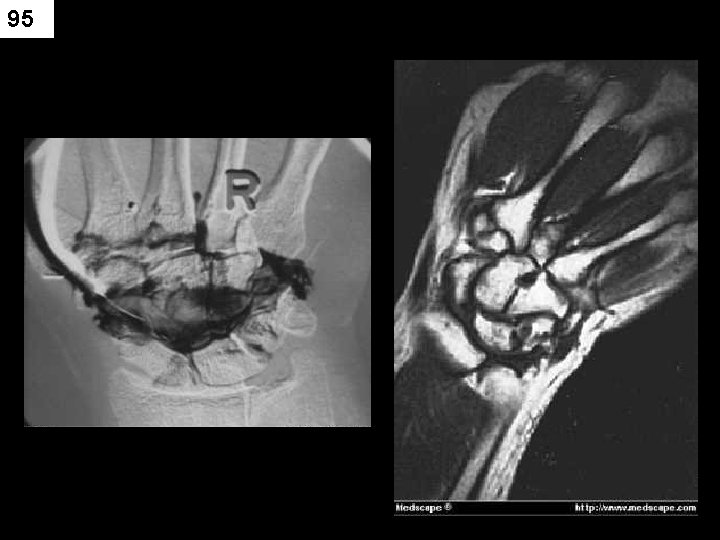
95

96 Wrist Arthrogram
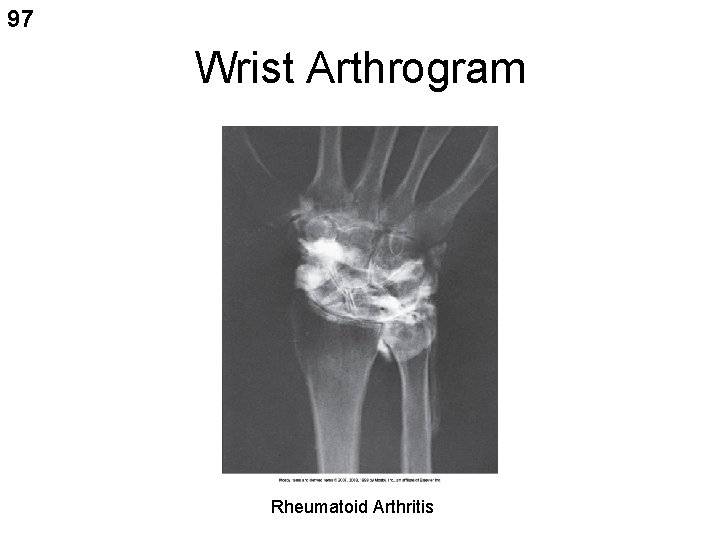
97 Wrist Arthrogram Rheumatoid Arthritis
98 OTHER JOINT SPACES • ANKLE • TMJ (USUALLY DONE IN CT)

99
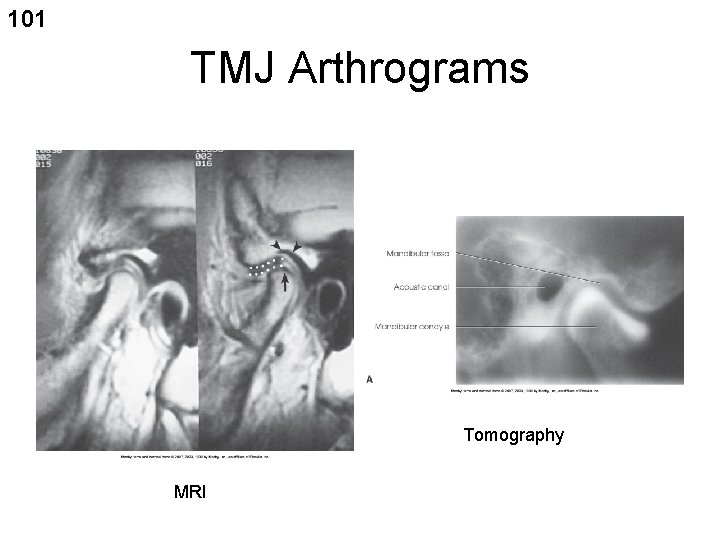
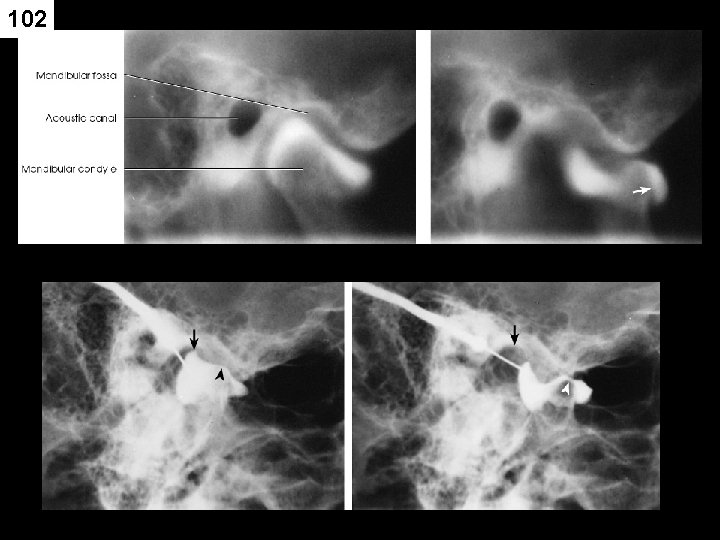
100 TMJ Arthrogram • CT and MRI have largely replaced TMJ arthrography because they are noninvasive • Useful in diagnosing – Abnormalities of the articular disk • Indications: pain, clicking sound, lock jaw when chewing sticky candy – Starburst – Taffy
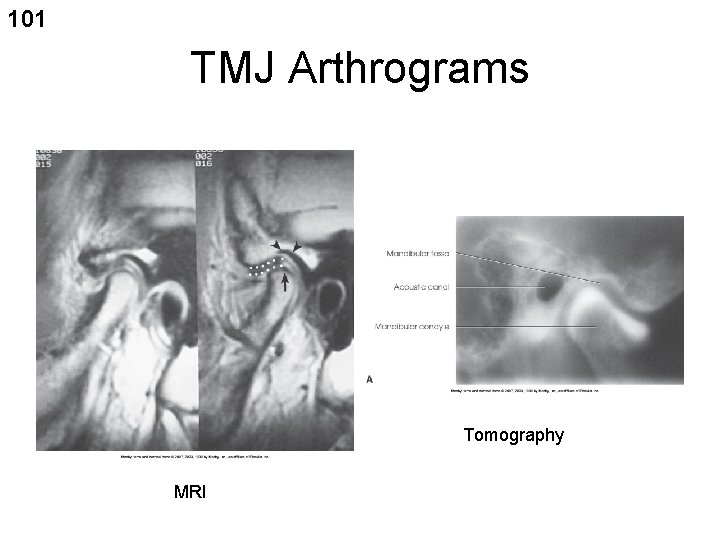
101 TMJ Arthrograms Tomography MRI
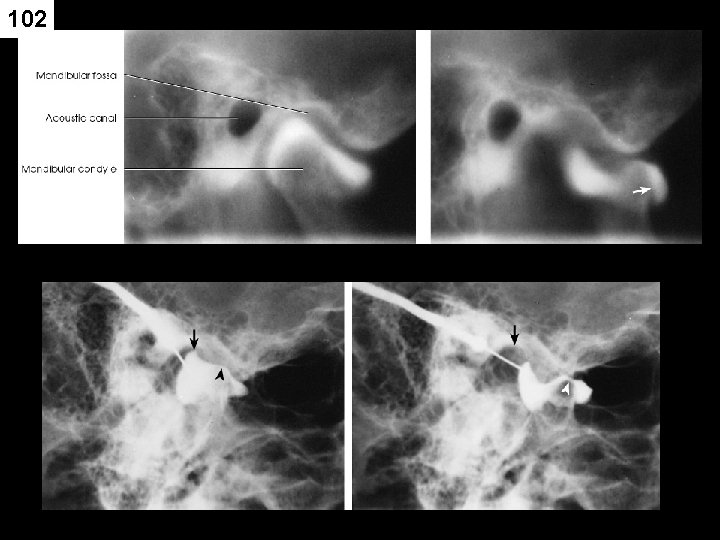
102
103
 255 255 255 255
255 255 255 255 Arthrography
Arthrography Grades of lamb
Grades of lamb Break joint vs spool joint
Break joint vs spool joint Superior costotransverse ligament
Superior costotransverse ligament Plane joint
Plane joint Temporary wood joints
Temporary wood joints Venture meaning in accounting
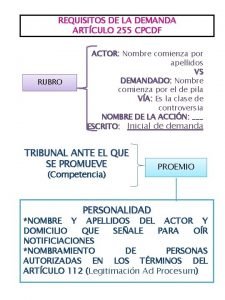
Venture meaning in accounting Requisitos de la demanda art 255
Requisitos de la demanda art 255 Hop255
Hop255 Mp 255
Mp 255 Ece 255
Ece 255 Sp 255
Sp 255 4096/255
4096/255 Alcatel deslizable
Alcatel deslizable Ak-sc 255
Ak-sc 255 Bakara süresi 255 ayet
Bakara süresi 255 ayet Char(0)
Char(0) 255-237
255-237 Welcome lodge 255
Welcome lodge 255 255 characters
255 characters Radiography
Radiography Cr cassette construction
Cr cassette construction Dark room radiographic darkroom layout
Dark room radiographic darkroom layout Focal trough in panoramic radiography
Focal trough in panoramic radiography Recumbent position
Recumbent position Occipito-frontal
Occipito-frontal Buccal object rule dental radiography
Buccal object rule dental radiography Gurney mott theory radiography
Gurney mott theory radiography Dental radiographic interpretation ppt
Dental radiographic interpretation ppt Enhancement using arithmetic/logic operations
Enhancement using arithmetic/logic operations Upper standard occlusal
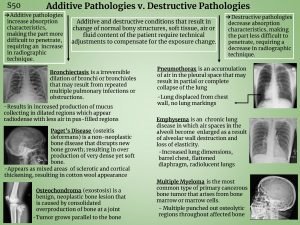
Upper standard occlusal Pneumothorax additive or destructive
Pneumothorax additive or destructive Radiography cordon off distance formula
Radiography cordon off distance formula Upside down grid error
Upside down grid error Industrial radiography training
Industrial radiography training Reverse towne projection
Reverse towne projection Soot and whitewash radiography
Soot and whitewash radiography Filmless radiography
Filmless radiography Iii image inhancement
Iii image inhancement Industrial radiography accidents
Industrial radiography accidents Optical density formula
Optical density formula Faulty
Faulty Limitations of radiography
Limitations of radiography What is computed radiography
What is computed radiography Industrial radiography accidents
Industrial radiography accidents Recorded detail in radiography
Recorded detail in radiography Radiography safety precautions
Radiography safety precautions Urethrorrhea is bleeding from the urethra. a. true b. false
Urethrorrhea is bleeding from the urethra. a. true b. false Rni radiography
Rni radiography Oscillating grid radiography
Oscillating grid radiography Latent image formation
Latent image formation Mask mode radiography
Mask mode radiography Jppso south east
Jppso south east Describe what a lap joint is in oxy fuel welding.
Describe what a lap joint is in oxy fuel welding. Ankle joint
Ankle joint Joint probability density function calculator
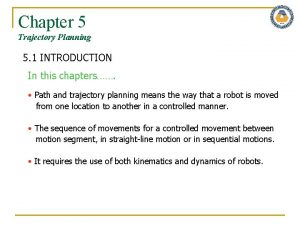
Joint probability density function calculator Joint space vs cartesian space
Joint space vs cartesian space Skewed t joint
Skewed t joint Joint monitoring program
Joint monitoring program Jesip jdm
Jesip jdm Joint inspection quick reference guide
Joint inspection quick reference guide Joint warfare analysis center
Joint warfare analysis center Joint innervation
Joint innervation Joint reasoning examples
Joint reasoning examples Materi akuntansi keuangan lanjutan 1 joint venture
Materi akuntansi keuangan lanjutan 1 joint venture Joint helicoflex
Joint helicoflex Dossier e32 joint de culasse
Dossier e32 joint de culasse What is a conditional relative frequency
What is a conditional relative frequency Vertebrocostal joint
Vertebrocostal joint Symphysis intervertebralis
Symphysis intervertebralis Erasmus mundus joint doctorates
Erasmus mundus joint doctorates Uncovertebral joint
Uncovertebral joint Graded oscillation techniques
Graded oscillation techniques Pearson
Pearson Amphiarthrosis examples
Amphiarthrosis examples What is condyloid joint
What is condyloid joint Internal rotasi hip
Internal rotasi hip Ginglymus joint
Ginglymus joint Conclusion of oral medication
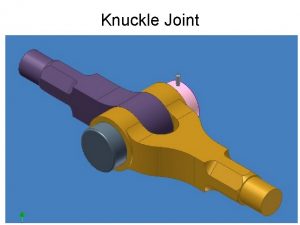
Conclusion of oral medication Single knuckle joint
Single knuckle joint Joint requirements office
Joint requirements office Katastar
Katastar Shoulder joint ppt
Shoulder joint ppt Radax joint
Radax joint Joint information system
Joint information system Tmh
Tmh Rekha shukla joint secretary
Rekha shukla joint secretary Industrial robot anatomy
Industrial robot anatomy Of the nine muscles that cross the shoulder joint
Of the nine muscles that cross the shoulder joint Pengaturan bersama adalah
Pengaturan bersama adalah Vitamin d joint health
Vitamin d joint health Joint geometry
Joint geometry Chain intermittent fillet weld symbol
Chain intermittent fillet weld symbol Unscented trajectory chapter 5
Unscented trajectory chapter 5 Condyloid joint
Condyloid joint Joint science and technology office
Joint science and technology office Joint characteristic function
Joint characteristic function Oregon joint use association
Oregon joint use association Joint strategic planning system
Joint strategic planning system Mobilization grades
Mobilization grades Joint set symbol
Joint set symbol Metacarpophalangeal joint
Metacarpophalangeal joint Elbow joint diagram
Elbow joint diagram