JOINTS Joints Joints or articulations sites where two


- Slides: 145
JOINTS
Joints • Joints or articulations: sites where two or more bones meet – Gives our skeleton mobility and holds it together – Weakest parts of the skeleton: • Yet, their structure resists various forces, such as crushing or tearing, that threaten to force them out of alignment
Structural Classification • Focuses on the material binding the bones together and whether or not a joint cavity is present – In fibrous joints the bones are joined together by fibrous tissue and lack a joint cavity – In cartilaginous joints the bones are joined together by cartilage and they lack a joint cavity – In synovial joints, the articulating bones are separated by a fluid-containing joint cavity
Functional Classification • Is based on the amount of movement allowed at the joint: – Synarthroses are immovable joints – Amphiarthroses are slightly movable joints – Diarthroses are freely movable joints
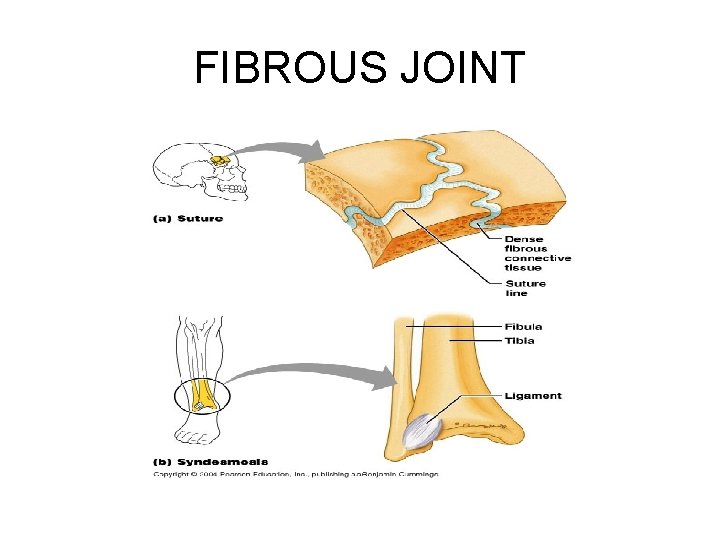
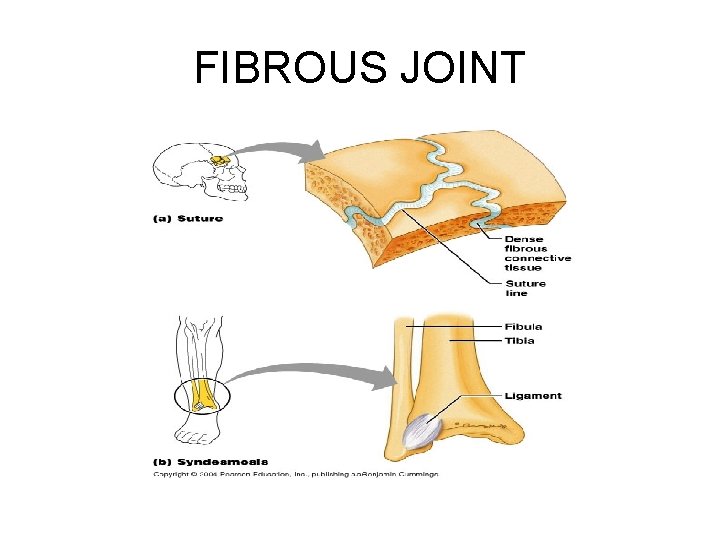
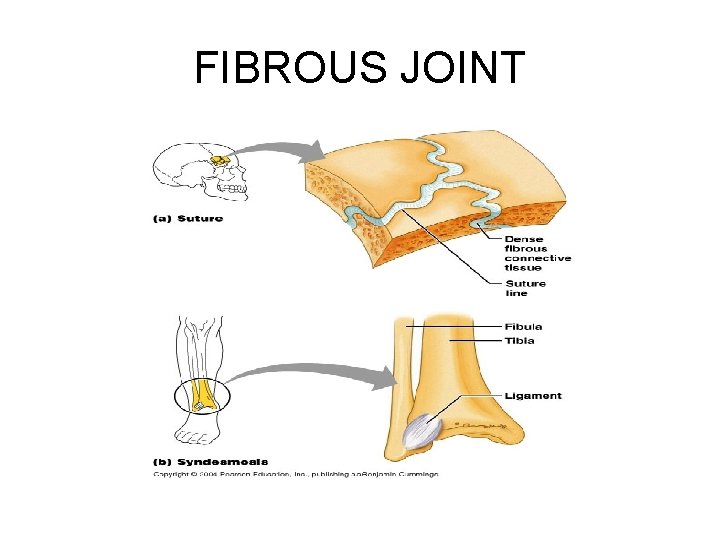
Fibrous Joints • Bones joined by fibrous tissue • No joint cavity • Amount of movement allowed depends on the length of the connective tissue fibers uniting the bones – A few are slightly movable, most are immovable • Three types: – Sutures – Syndesmoses – Gomphoses
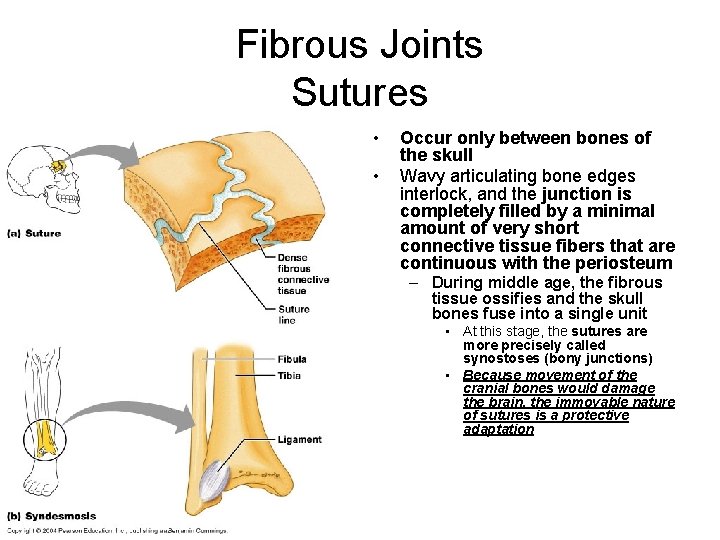
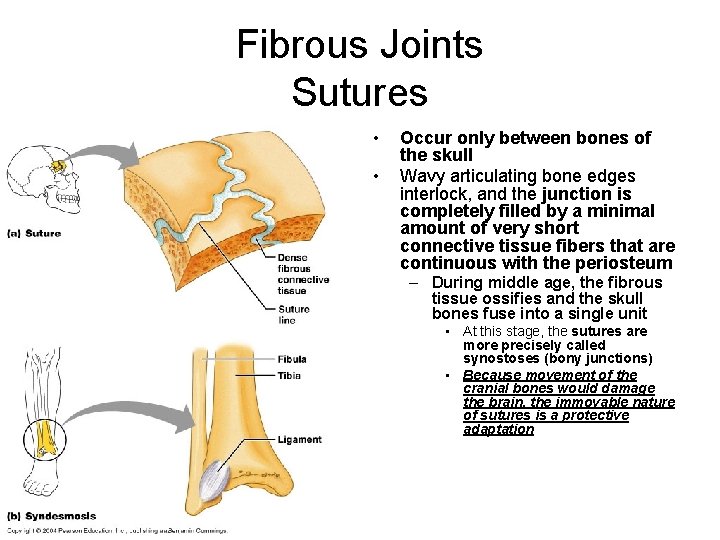
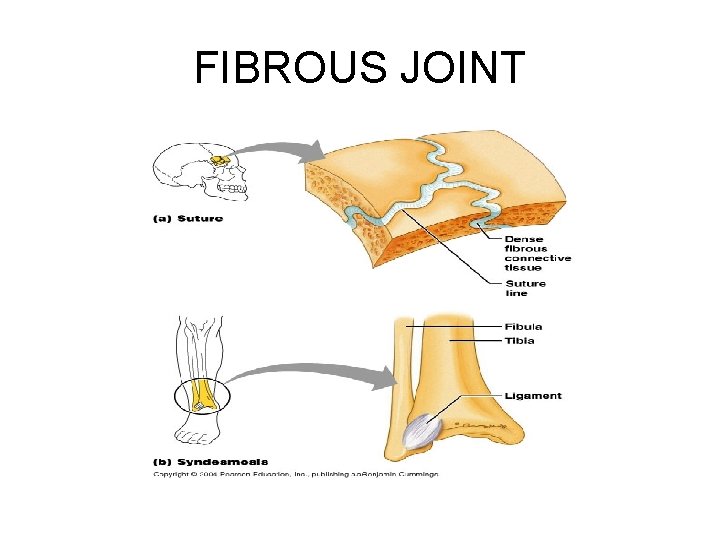
Fibrous Joints Sutures • • Occur only between bones of the skull Wavy articulating bone edges interlock, and the junction is completely filled by a minimal amount of very short connective tissue fibers that are continuous with the periosteum – During middle age, the fibrous tissue ossifies and the skull bones fuse into a single unit • At this stage, the sutures are more precisely called synostoses (bony junctions) • Because movement of the cranial bones would damage the brain, the immovable nature of sutures is a protective adaptation
FIBROUS JOINT
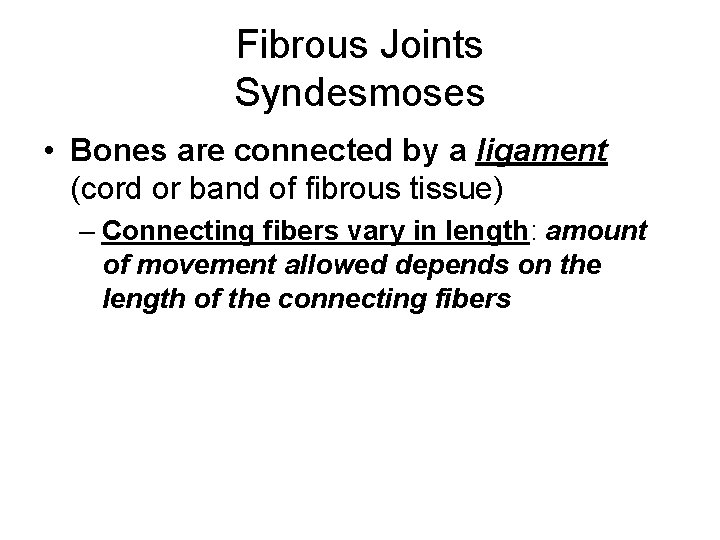
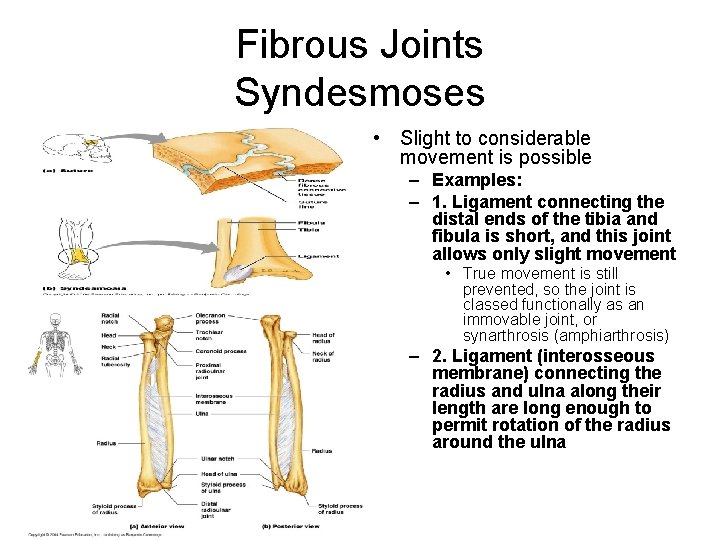
Fibrous Joints Syndesmoses • Bones are connected by a ligament (cord or band of fibrous tissue) – Connecting fibers vary in length: amount of movement allowed depends on the length of the connecting fibers
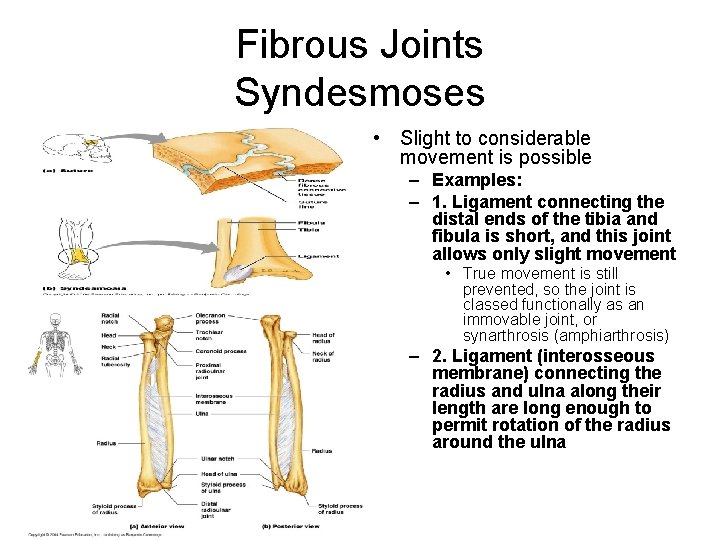
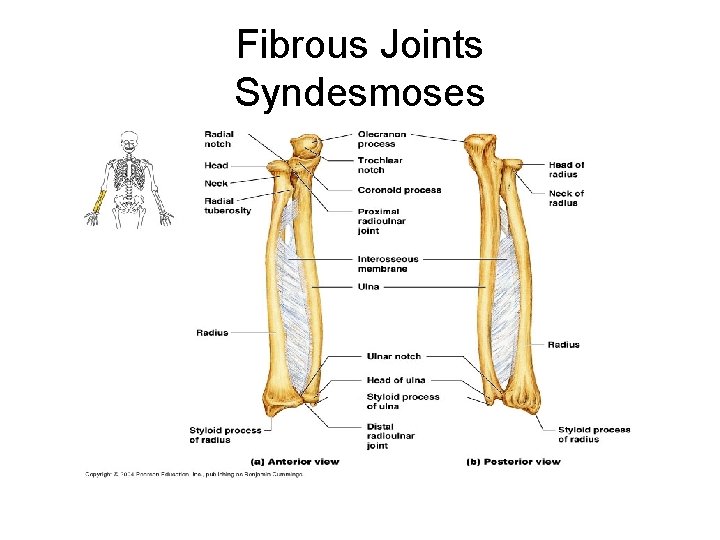
Fibrous Joints Syndesmoses • Slight to considerable movement is possible – Examples: – 1. Ligament connecting the distal ends of the tibia and fibula is short, and this joint allows only slight movement • True movement is still prevented, so the joint is classed functionally as an immovable joint, or synarthrosis (amphiarthrosis) – 2. Ligament (interosseous membrane) connecting the radius and ulna along their length are long enough to permit rotation of the radius around the ulna
FIBROUS JOINT
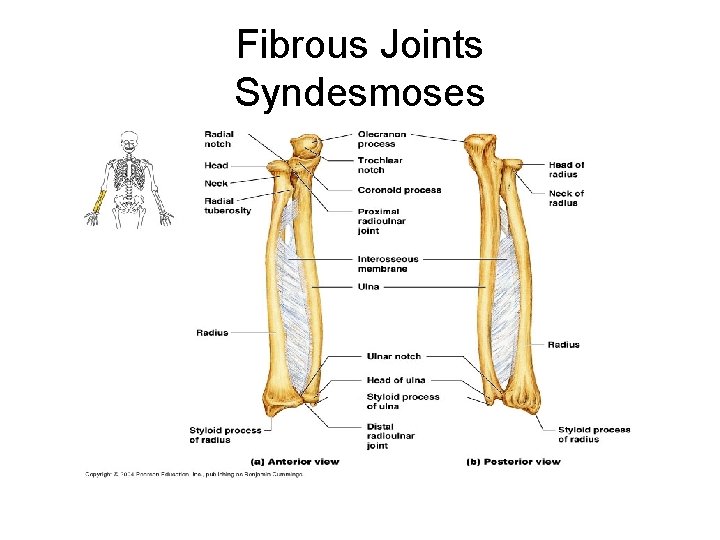
Fibrous Joints Syndesmoses
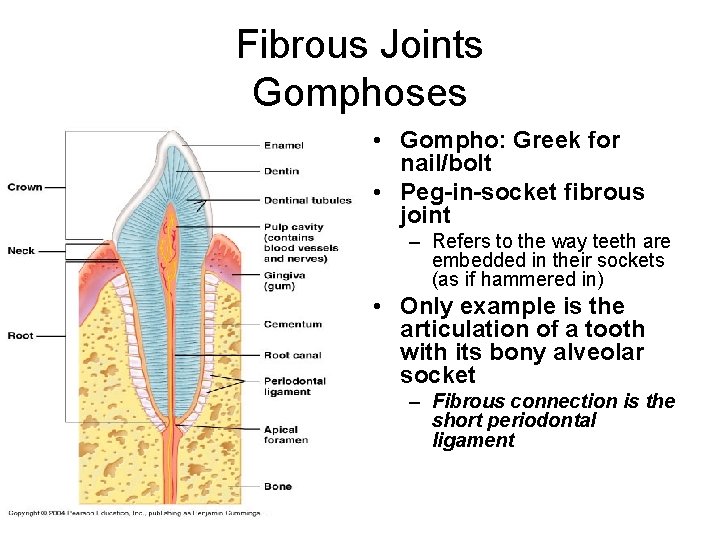
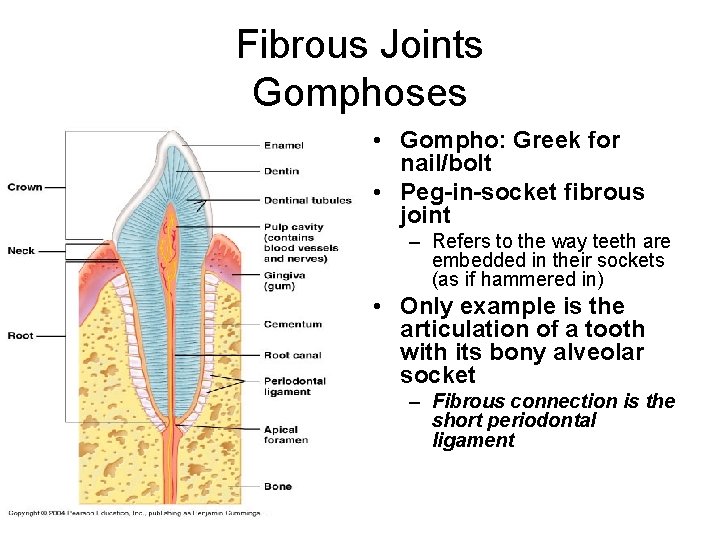
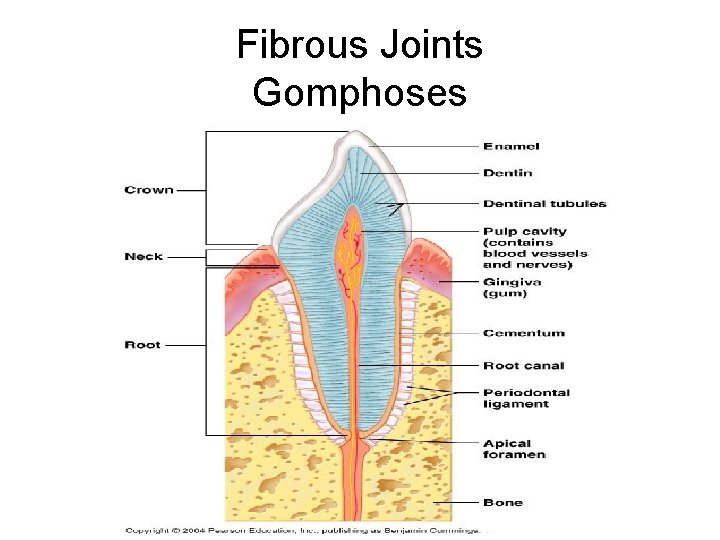
Fibrous Joints Gomphoses • Gompho: Greek for nail/bolt • Peg-in-socket fibrous joint – Refers to the way teeth are embedded in their sockets (as if hammered in) • Only example is the articulation of a tooth with its bony alveolar socket – Fibrous connection is the short periodontal ligament
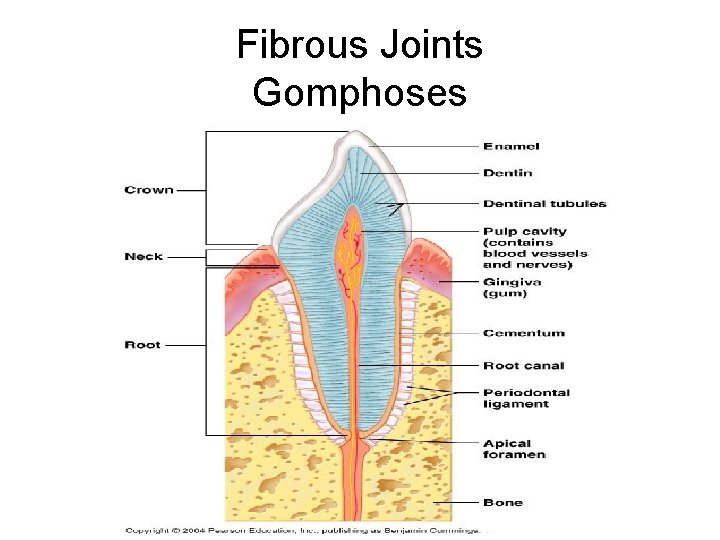
Fibrous Joints Gomphoses
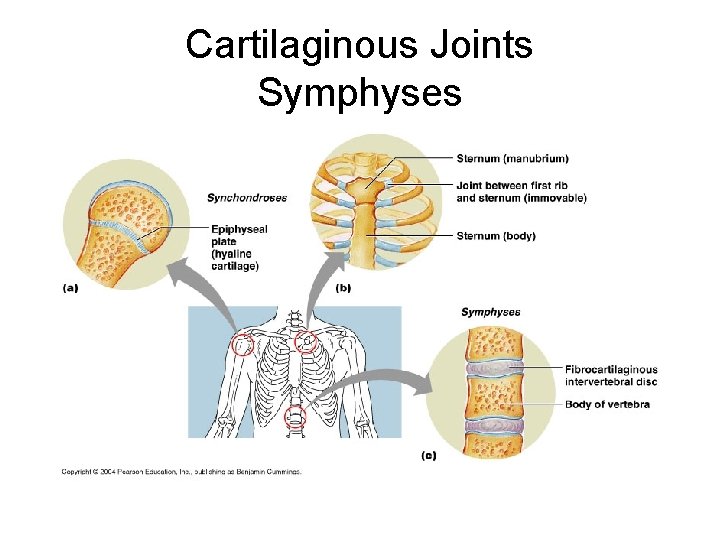
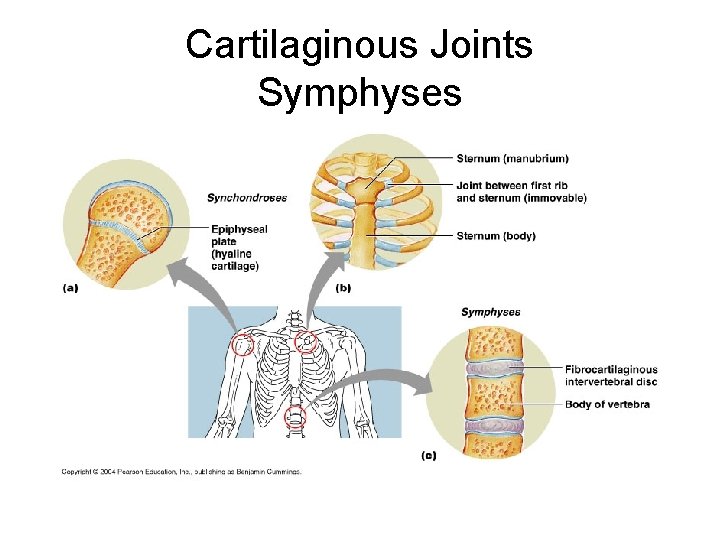
Cartilaginous Joints • Articulating joints are united by cartilage • Lack joint cavity • Two types: – Synchondroses – Symphyses
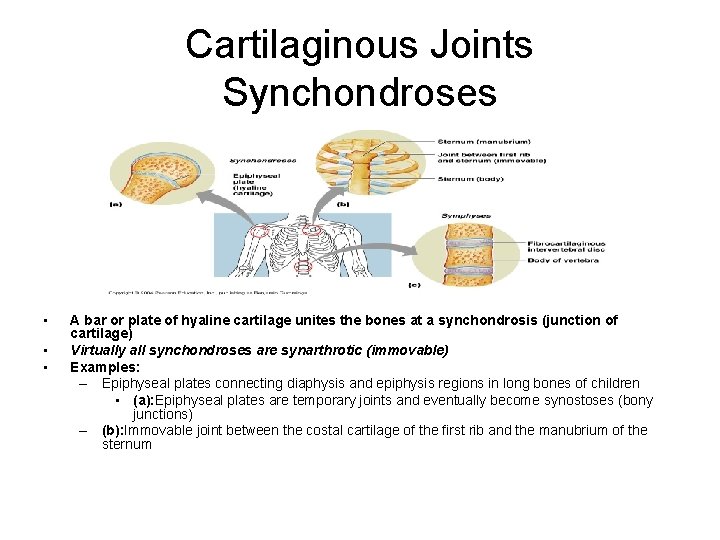
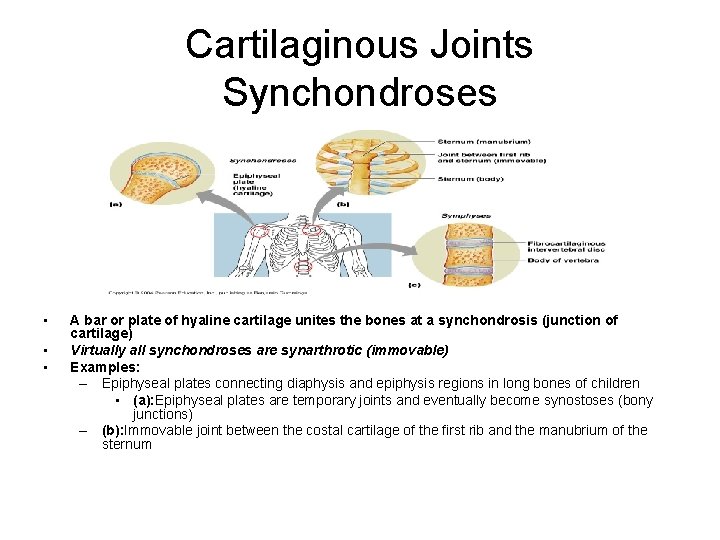
Cartilaginous Joints Synchondroses • • • A bar or plate of hyaline cartilage unites the bones at a synchondrosis (junction of cartilage) Virtually all synchondroses are synarthrotic (immovable) Examples: – Epiphyseal plates connecting diaphysis and epiphysis regions in long bones of children • (a): Epiphyseal plates are temporary joints and eventually become synostoses (bony junctions) – (b): Immovable joint between the costal cartilage of the first rib and the manubrium of the sternum
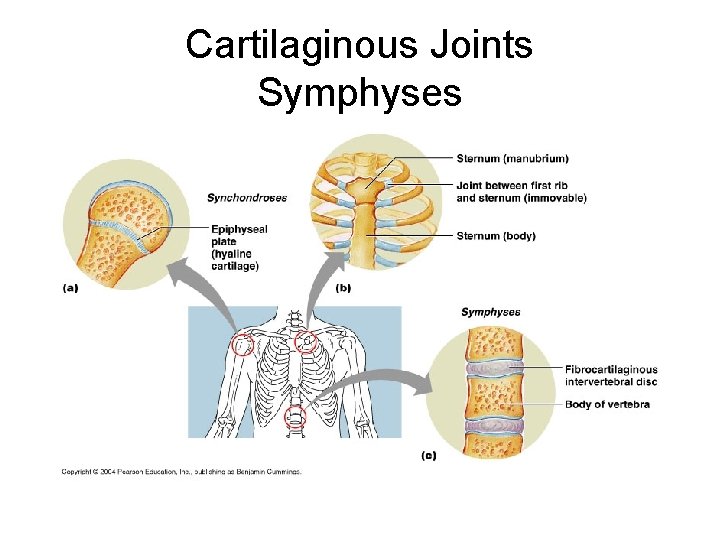
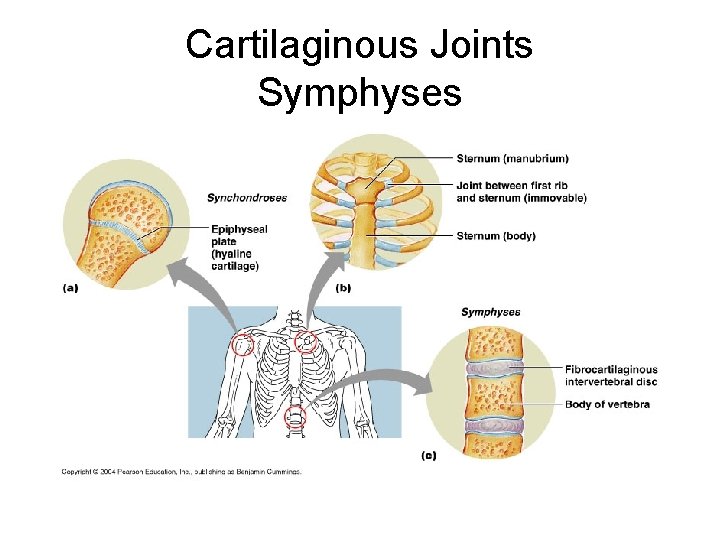
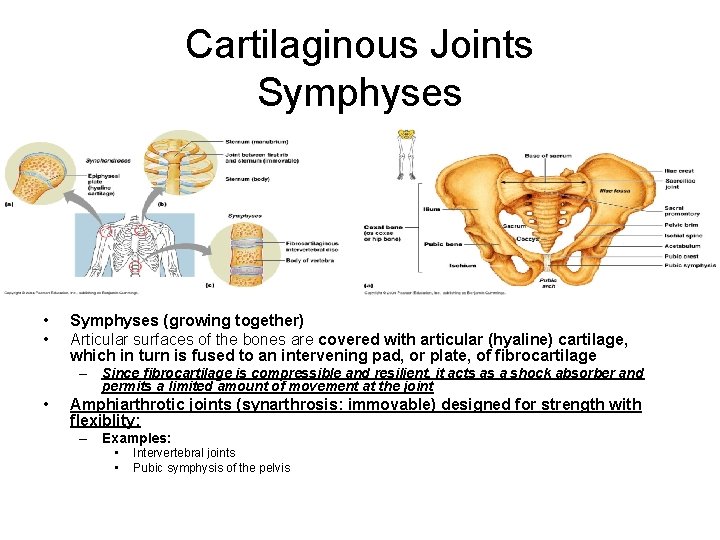
Cartilaginous Joints Symphyses
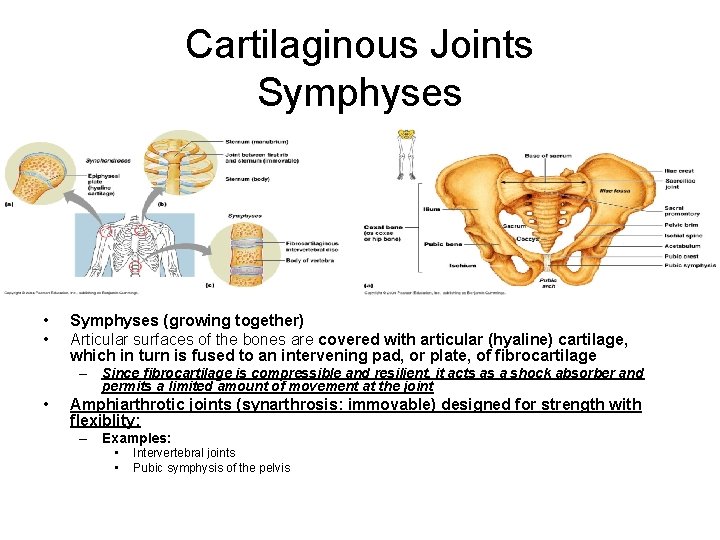
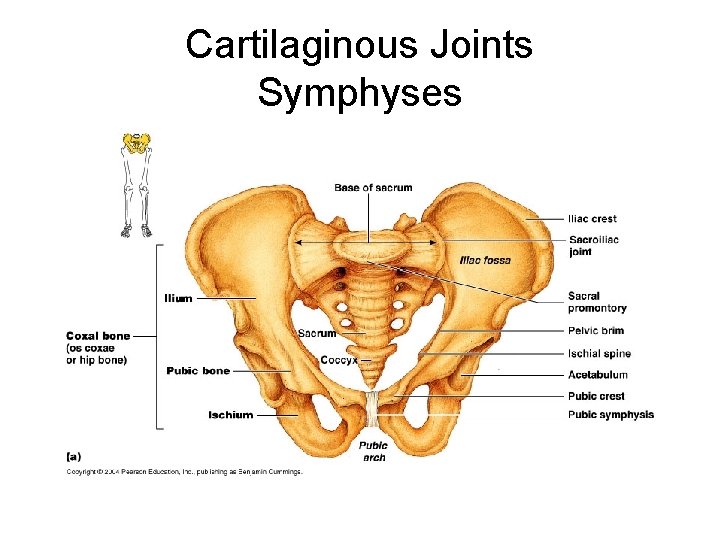
Cartilaginous Joints Symphyses • • Symphyses (growing together) Articular surfaces of the bones are covered with articular (hyaline) cartilage, which in turn is fused to an intervening pad, or plate, of fibrocartilage – Since fibrocartilage is compressible and resilient, it acts as a shock absorber and permits a limited amount of movement at the joint • Amphiarthrotic joints (synarthrosis: immovable) designed for strength with flexiblity: – Examples: • • Intervertebral joints Pubic symphysis of the pelvis
Cartilaginous Joints Symphyses
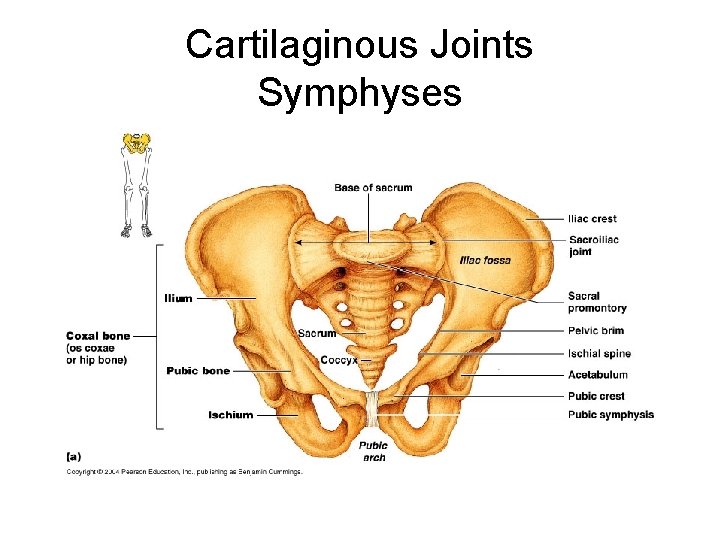
Cartilaginous Joints Symphyses
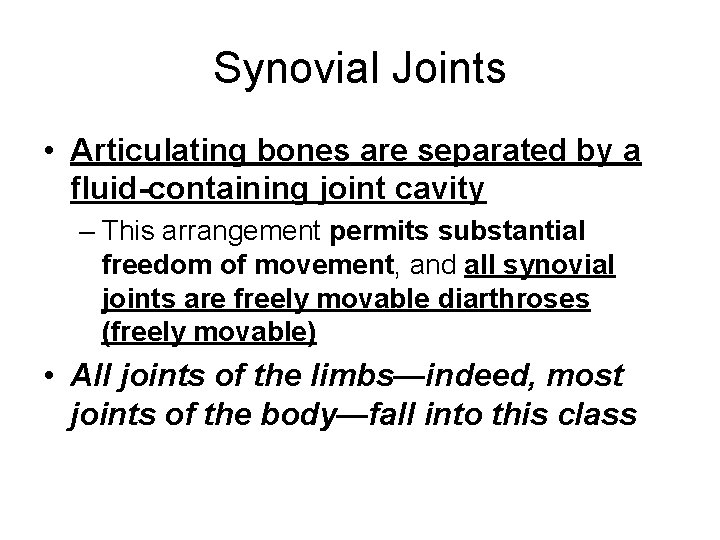
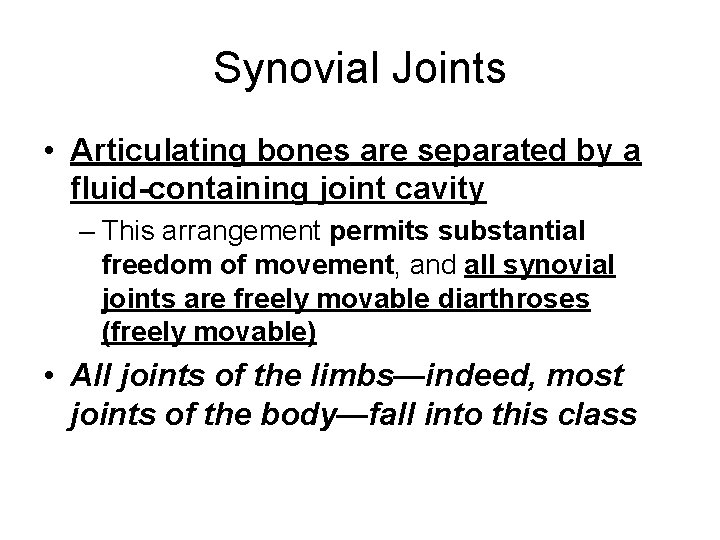
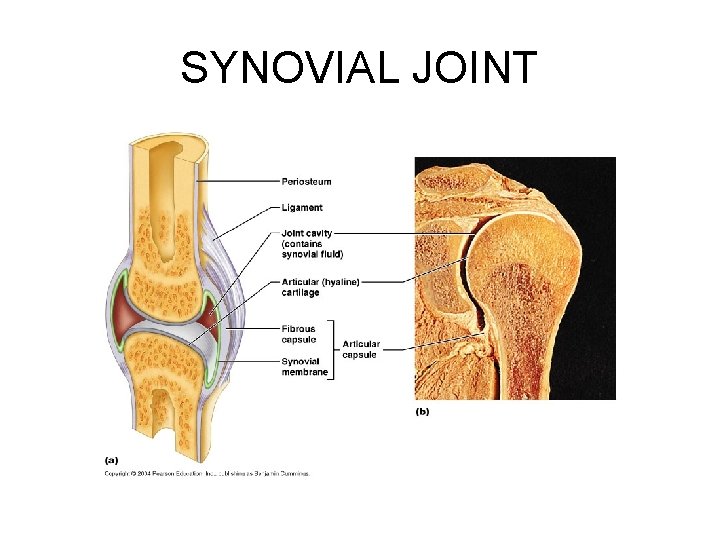
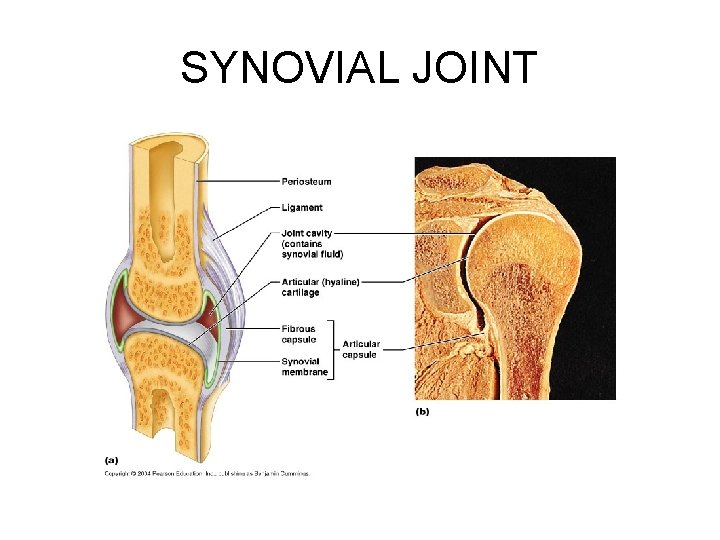
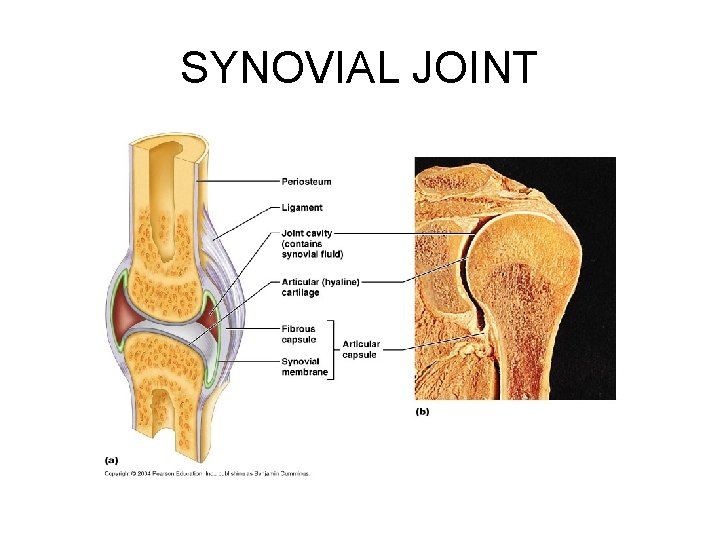
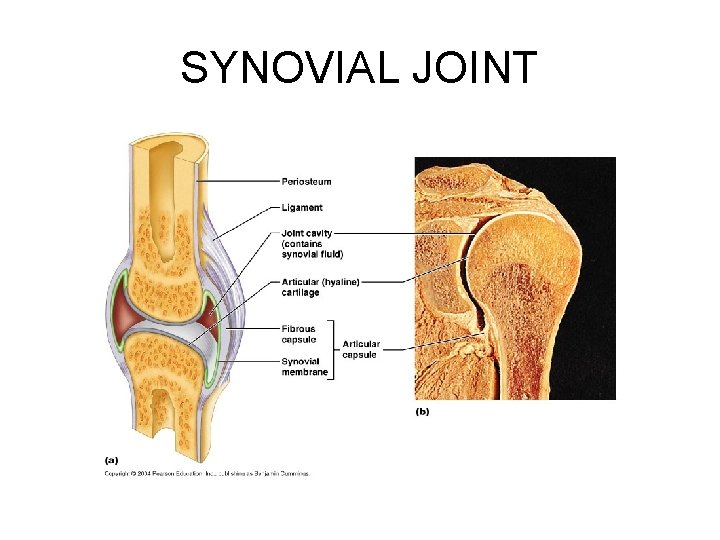
Synovial Joints • Articulating bones are separated by a fluid-containing joint cavity – This arrangement permits substantial freedom of movement, and all synovial joints are freely movable diarthroses (freely movable) • All joints of the limbs—indeed, most joints of the body—fall into this class
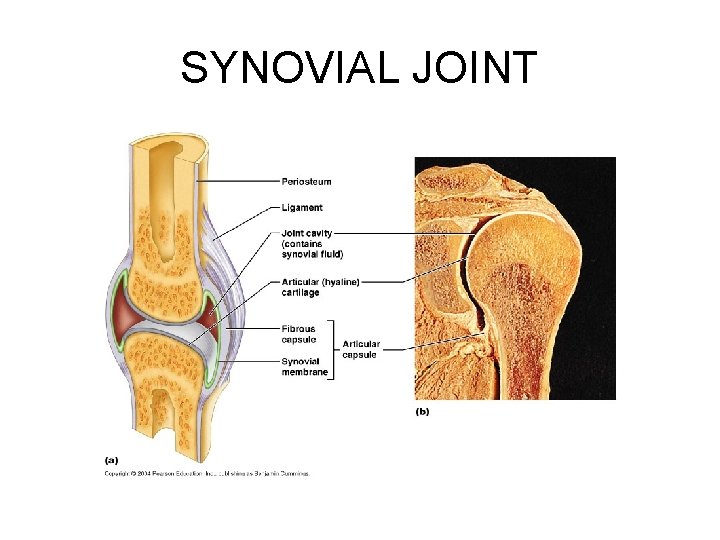
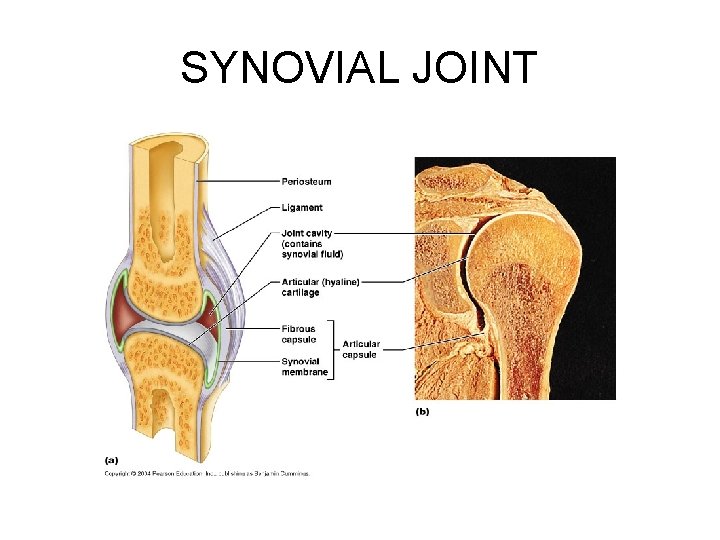
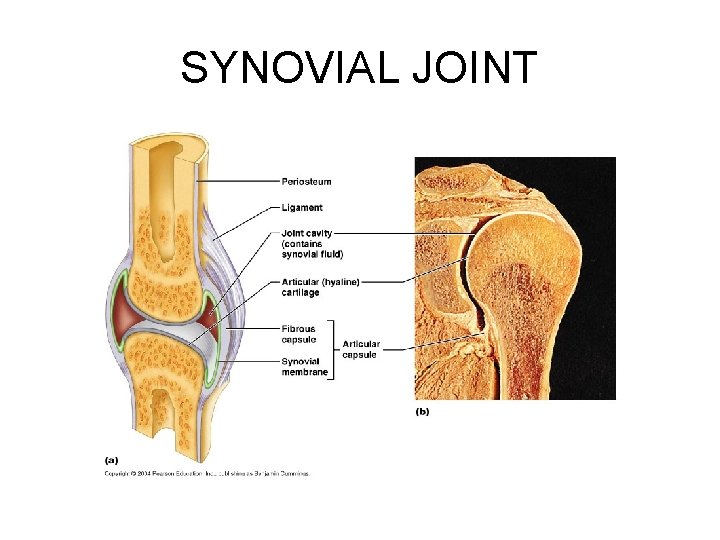
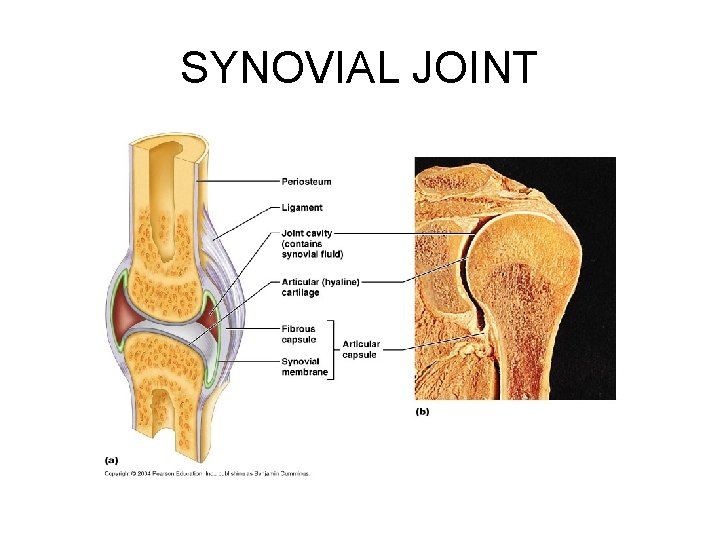
SYNOVIAL JOINT
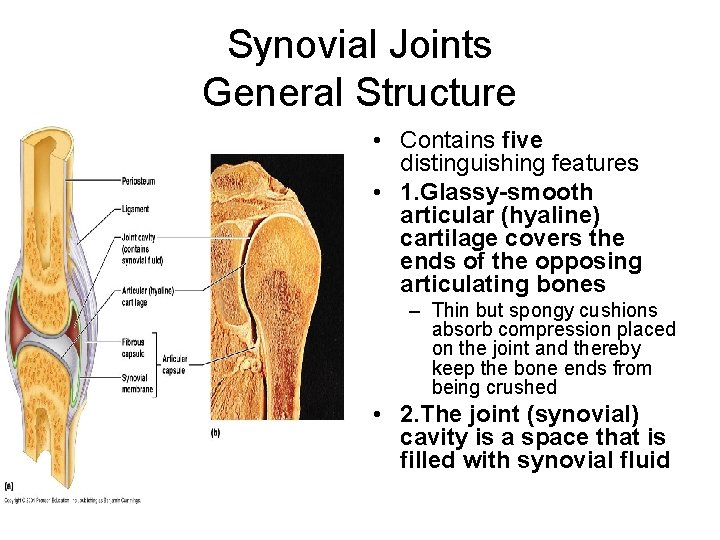
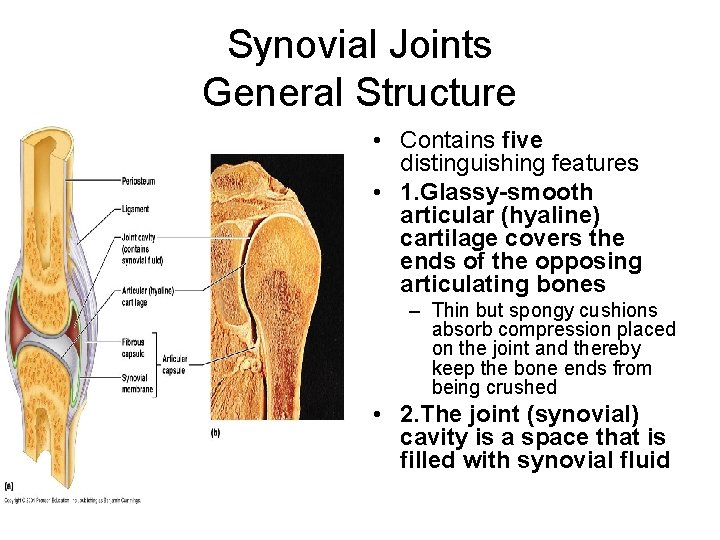
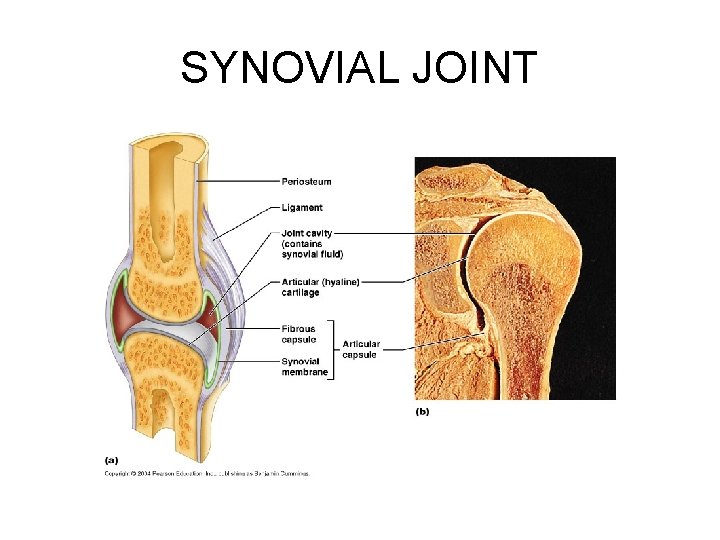
Synovial Joints General Structure • Contains five distinguishing features • 1. Glassy-smooth articular (hyaline) cartilage covers the ends of the opposing articulating bones – Thin but spongy cushions absorb compression placed on the joint and thereby keep the bone ends from being crushed • 2. The joint (synovial) cavity is a space that is filled with synovial fluid
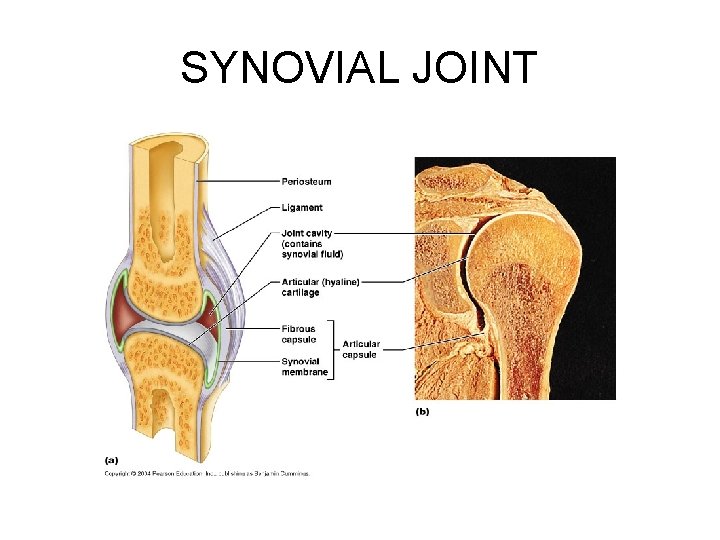
SYNOVIAL JOINT
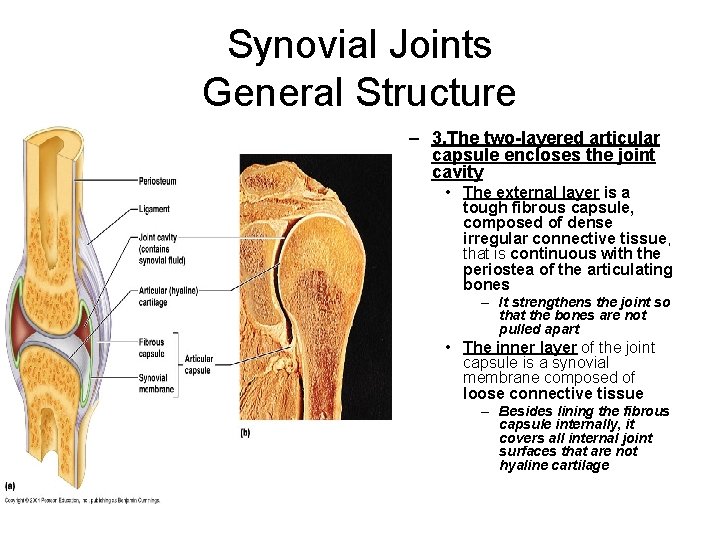
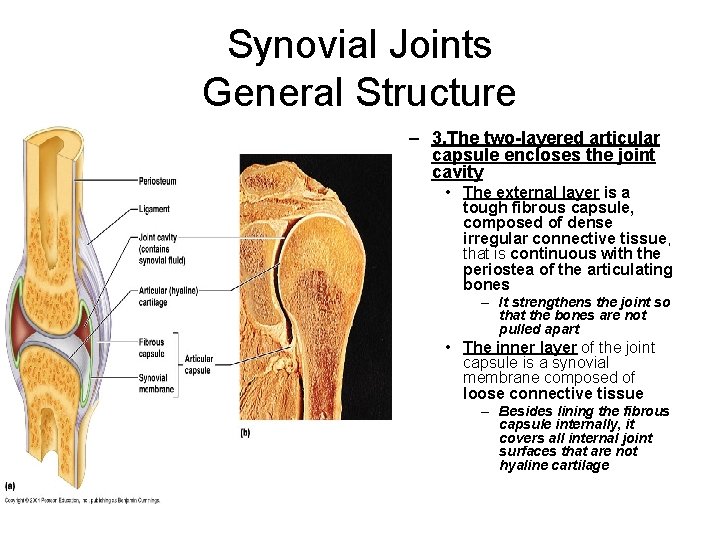
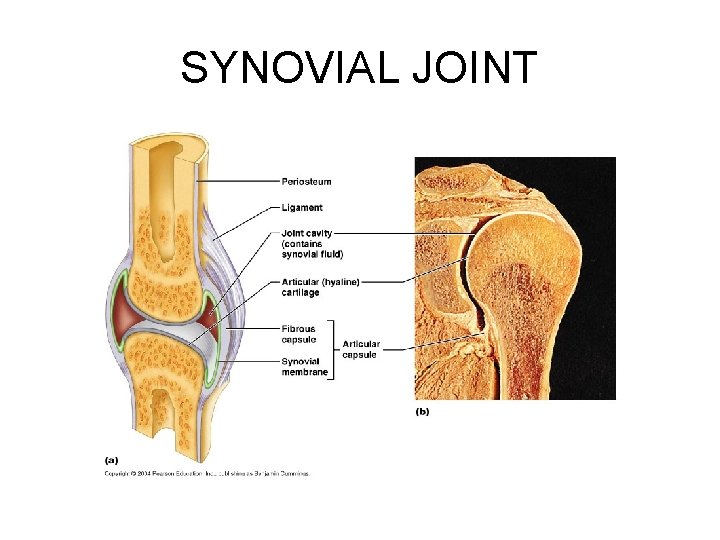
Synovial Joints General Structure – 3. The two-layered articular capsule encloses the joint cavity • The external layer is a tough fibrous capsule, composed of dense irregular connective tissue, that is continuous with the periostea of the articulating bones – It strengthens the joint so that the bones are not pulled apart • The inner layer of the joint capsule is a synovial membrane composed of loose connective tissue – Besides lining the fibrous capsule internally, it covers all internal joint surfaces that are not hyaline cartilage
SYNOVIAL JOINT
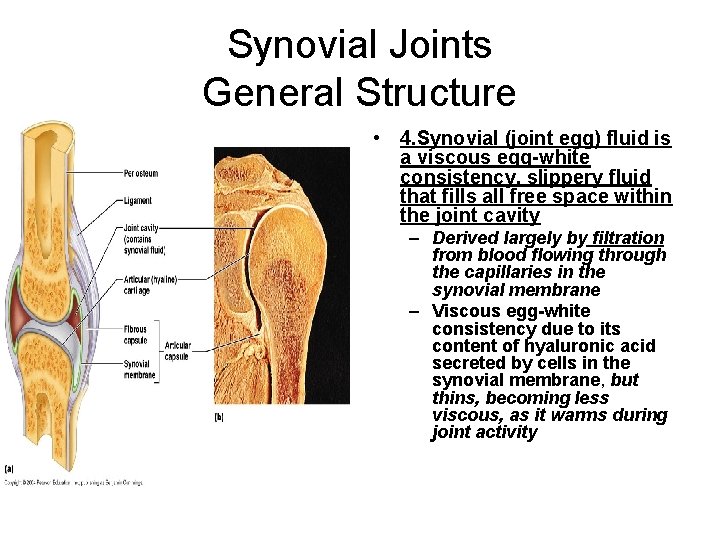
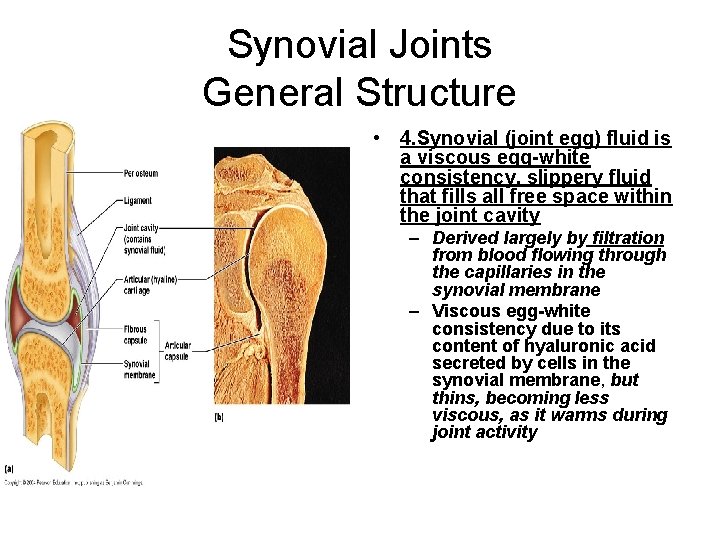
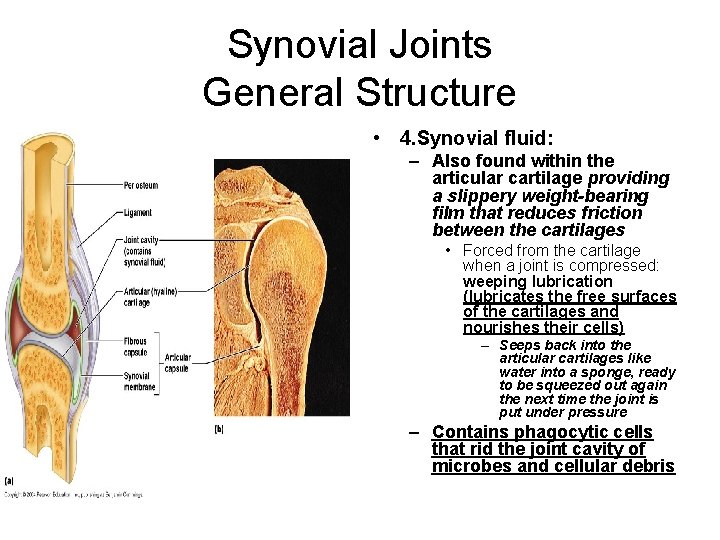
Synovial Joints General Structure • 4. Synovial (joint egg) fluid is a viscous egg-white consistency, slippery fluid that fills all free space within the joint cavity – Derived largely by filtration from blood flowing through the capillaries in the synovial membrane – Viscous egg-white consistency due to its content of hyaluronic acid secreted by cells in the synovial membrane, but thins, becoming less viscous, as it warms during joint activity
SYNOVIAL JOINT
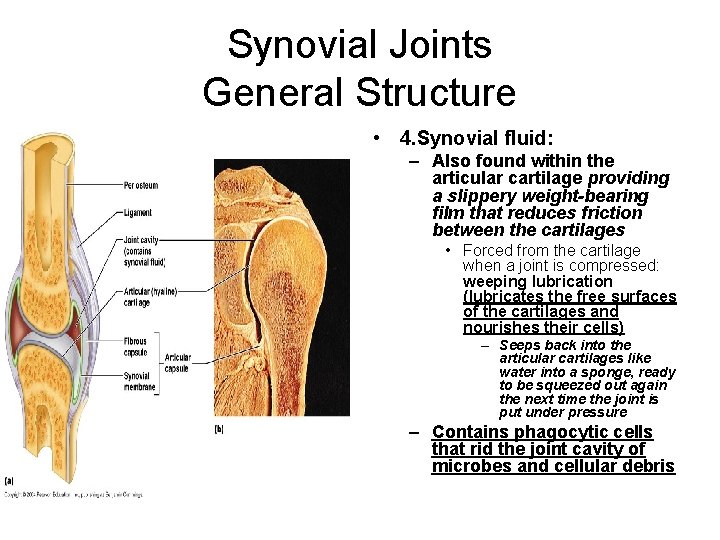
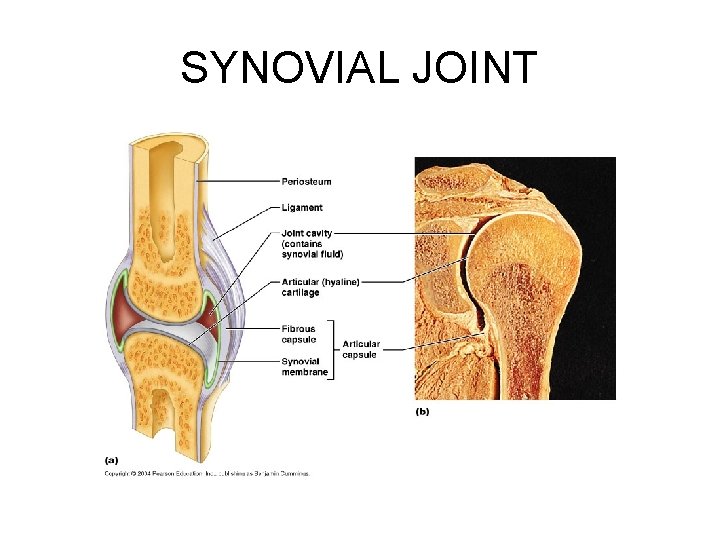
Synovial Joints General Structure • 4. Synovial fluid: – Also found within the articular cartilage providing a slippery weight-bearing film that reduces friction between the cartilages • Forced from the cartilage when a joint is compressed: weeping lubrication (lubricates the free surfaces of the cartilages and nourishes their cells) – Seeps back into the articular cartilages like water into a sponge, ready to be squeezed out again the next time the joint is put under pressure – Contains phagocytic cells that rid the joint cavity of microbes and cellular debris
SYNOVIAL JOINT
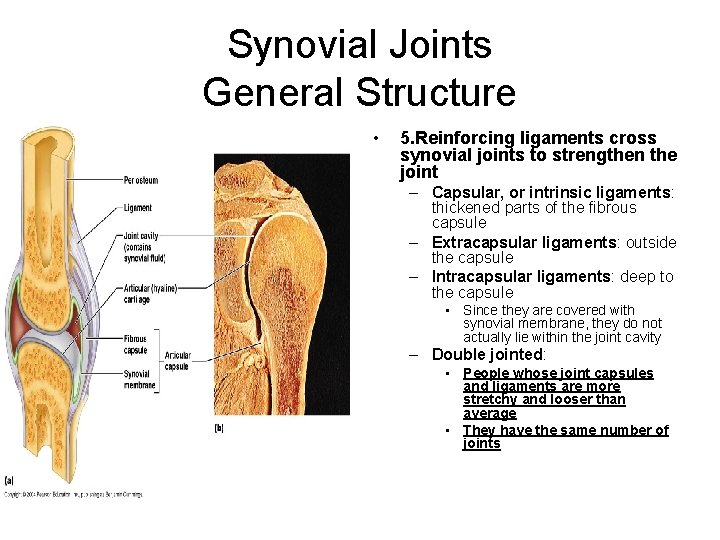
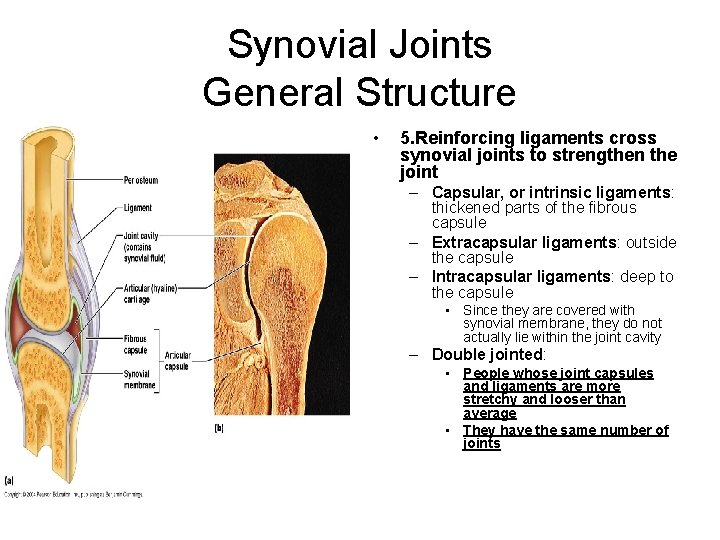
Synovial Joints General Structure • 5. Reinforcing ligaments cross synovial joints to strengthen the joint – Capsular, or intrinsic ligaments: thickened parts of the fibrous capsule – Extracapsular ligaments: outside the capsule – Intracapsular ligaments: deep to the capsule • Since they are covered with synovial membrane, they do not actually lie within the joint cavity – Double jointed: • People whose joint capsules and ligaments are more stretchy and looser than average • They have the same number of joints
SYNOVIAL JOINT
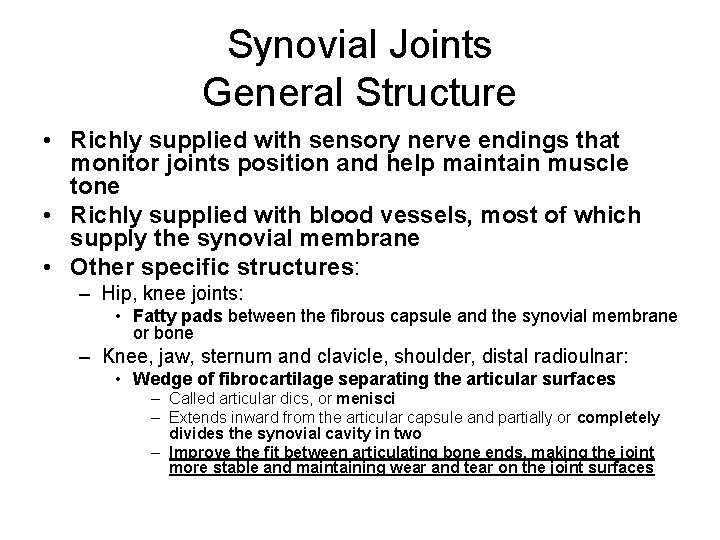
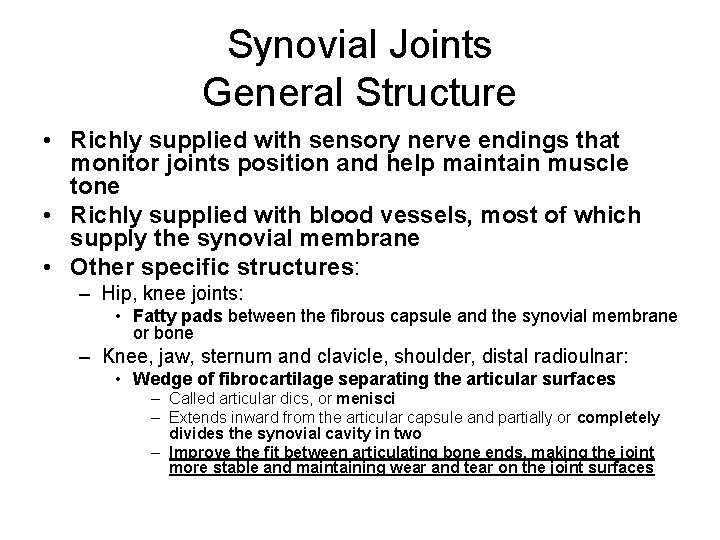
Synovial Joints General Structure • Richly supplied with sensory nerve endings that monitor joints position and help maintain muscle tone • Richly supplied with blood vessels, most of which supply the synovial membrane • Other specific structures: – Hip, knee joints: • Fatty pads between the fibrous capsule and the synovial membrane or bone – Knee, jaw, sternum and clavicle, shoulder, distal radioulnar: • Wedge of fibrocartilage separating the articular surfaces – Called articular dics, or menisci – Extends inward from the articular capsule and partially or completely divides the synovial cavity in two – Improve the fit between articulating bone ends, making the joint more stable and maintaining wear and tear on the joint surfaces
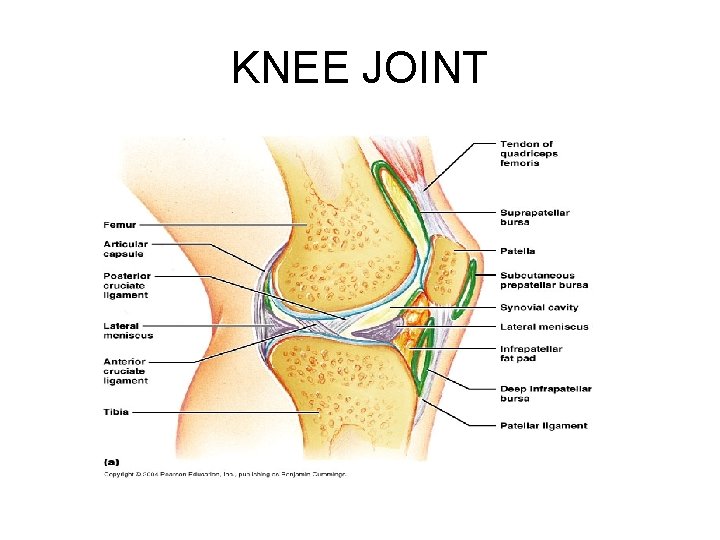
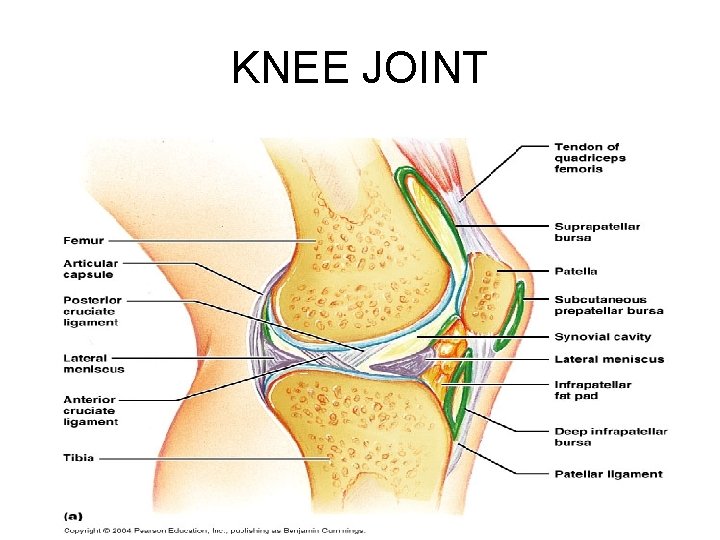
KNEE JOINT
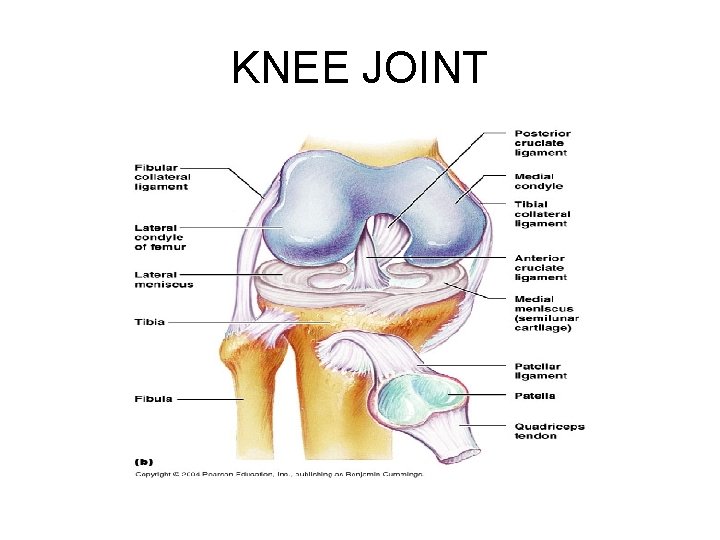
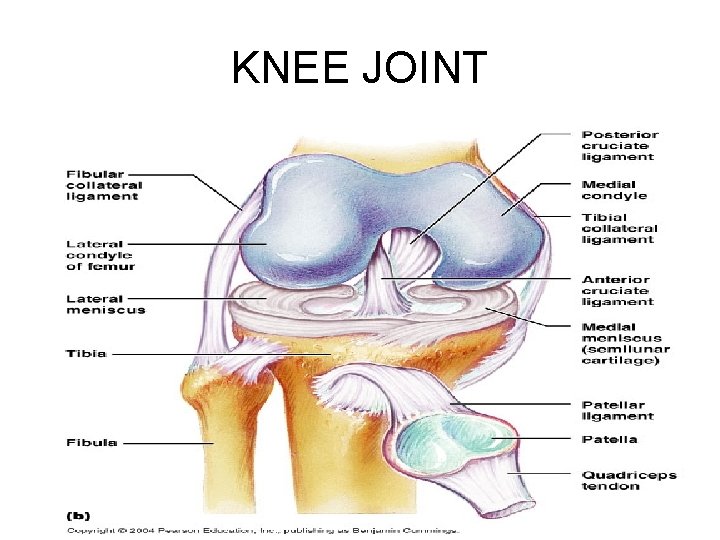
KNEE JOINT
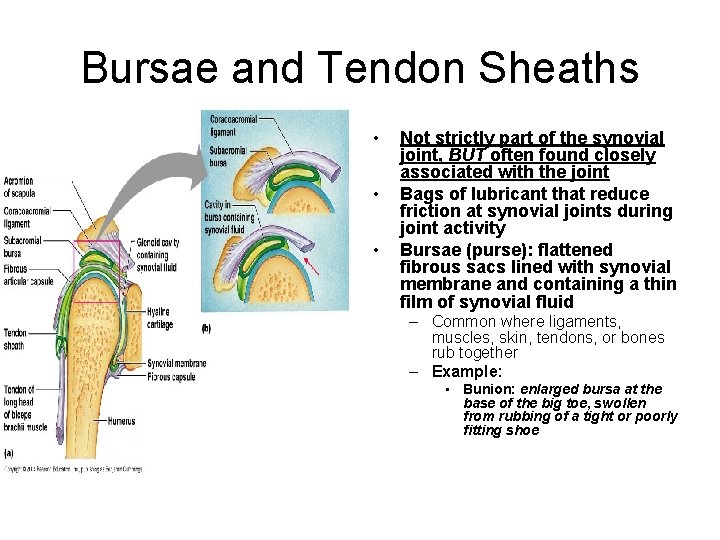
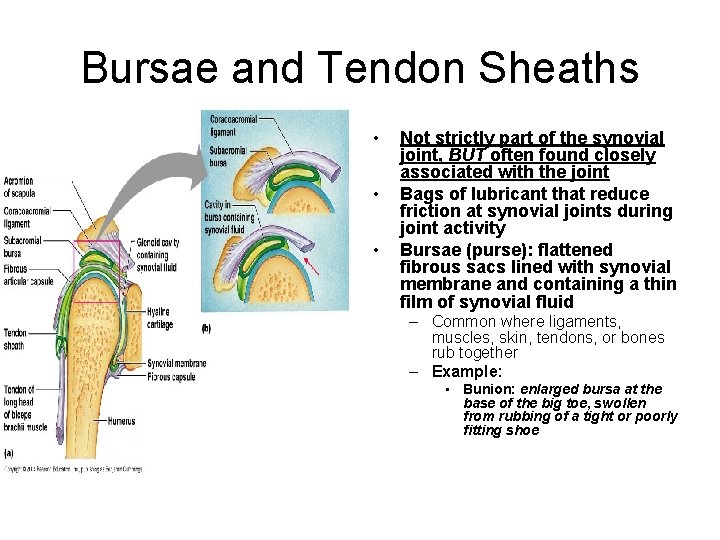
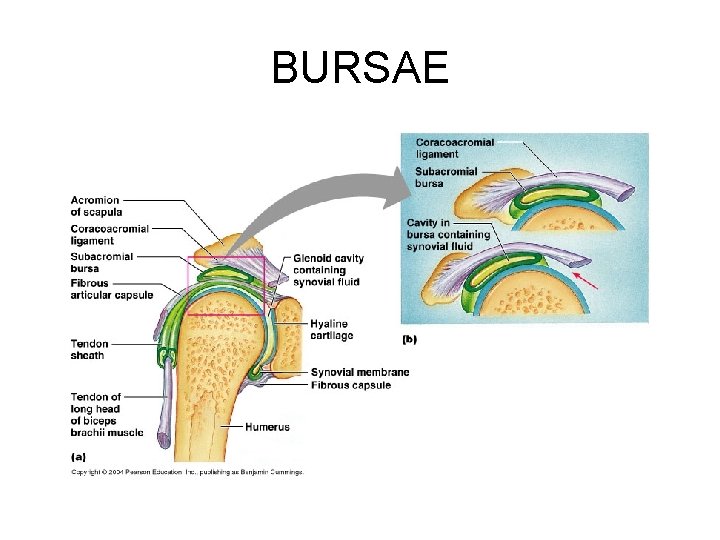
Bursae and Tendon Sheaths • • • Not strictly part of the synovial joint, BUT often found closely associated with the joint Bags of lubricant that reduce friction at synovial joints during joint activity Bursae (purse): flattened fibrous sacs lined with synovial membrane and containing a thin film of synovial fluid – Common where ligaments, muscles, skin, tendons, or bones rub together – Example: • Bunion: enlarged bursa at the base of the big toe, swollen from rubbing of a tight or poorly fitting shoe
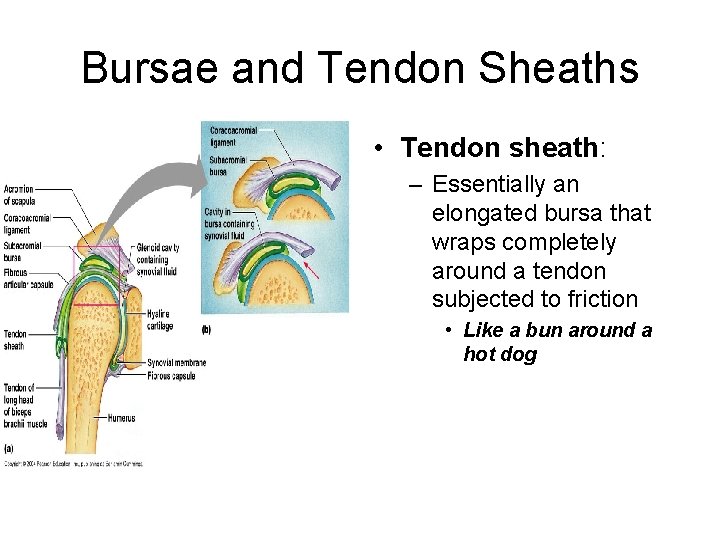
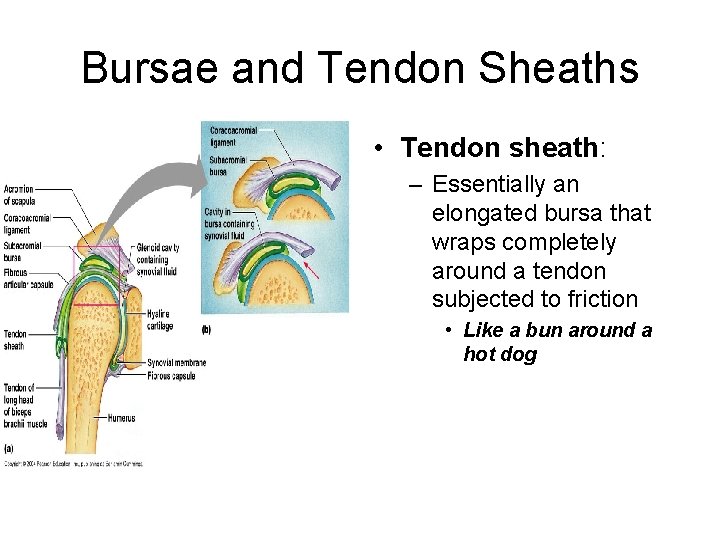
Bursae and Tendon Sheaths • Tendon sheath: – Essentially an elongated bursa that wraps completely around a tendon subjected to friction • Like a bun around a hot dog
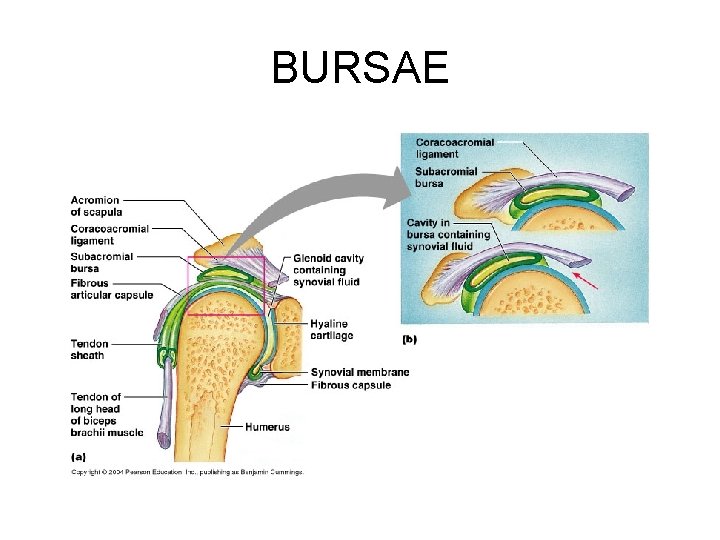
BURSAE
Factors Influencing the Stability of Synovial Joints • Because joints are constantly stretched and compressed, they must be stabilized so that they do not dislocate (come out of alignment) • Stability of a synovial joint depends chiefly on three factors: – 1. The shapes of the articular surfaces of bones found at a synovial joint : • Determines the movements that occur at the joint • Play a minimal role in stabilizing the joint – Example: ball and deep socket of the hip joint provides the best example of a joint made extremely stable by the shape of its articular surfaces
Factors Influencing the Stability of Synovial Joints • 2. Number and positioning of ligaments: – Ligament: band of regular fibrous tissue that connects bones – Capsules and ligaments of synovial joints unite the bones and prevent excessive or undesirable motion • As a rule: the more ligaments a joint has, the stronger it is – When other stabilizing factors are inadequate, undue tension is placed on the ligaments and they stretch • Stretched ligaments stay stretched (like taffy) • A ligament can stretch only about 6% of its length before it snaps – When ligaments are the major means of bracing a joint, the joint is not very stable
Factors Influencing the Stability of Synovial Joints • 3. Muscle tone: low levels of contractile activity in relaxed muscles – Keeps the muscles healthy and ready to react to stimulation – For most joints, the muscle tendons that cross the joint are the most important stabilizing factor • Tendon: cord of dense fibrous tissue attaching muscle to bone – Kept taut at all times by the tone of their muscles – Extremely important in reinforcing the shoulder and knee joints and the arches of the foot
Movements Allowed by Synovial Joints • Every skeletal muscle of the body is attached to bone or other connective tissue structures at no fewer than two points – The muscle’s origin is attached to the immovable (or less movable) bone – The other end, the insertion, is attached to the movable bone • Body movement occurs when muscles contract across joints and their insertion moves toward their origin • Movements can be described in directional terms relative to the lines, or axes, around which the body part moves and the planes of space along which movement occurs, that is, along the transverse, frontal, or sagittal plane
Movements Allowed by Synovial Joints • Range of motion: – Nonaxial: slipping movements only • No axis around which movement can occur – Uniaxial: • Movement in one plane – Biaxial: • Movement in two planes – Multiaxial: • Movement in or around all three planes of space and axes
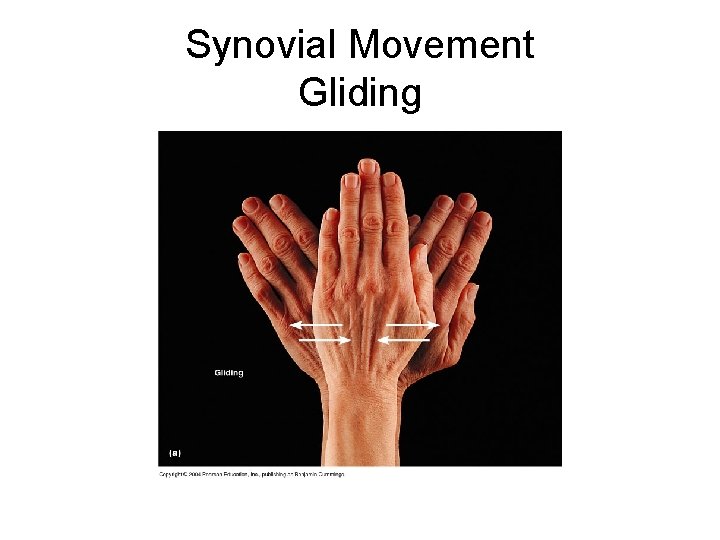
Movements Allowed by Synovial Joints • Three general types of movement: – 1. Gliding – 2. Angular – 3. Rotation
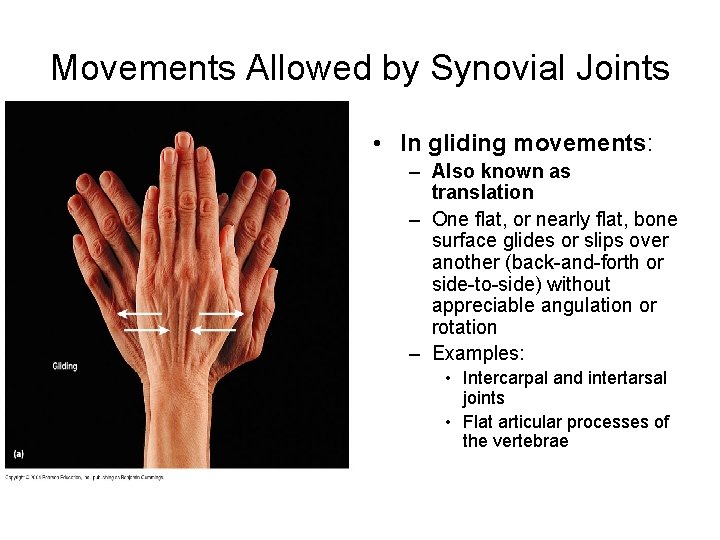
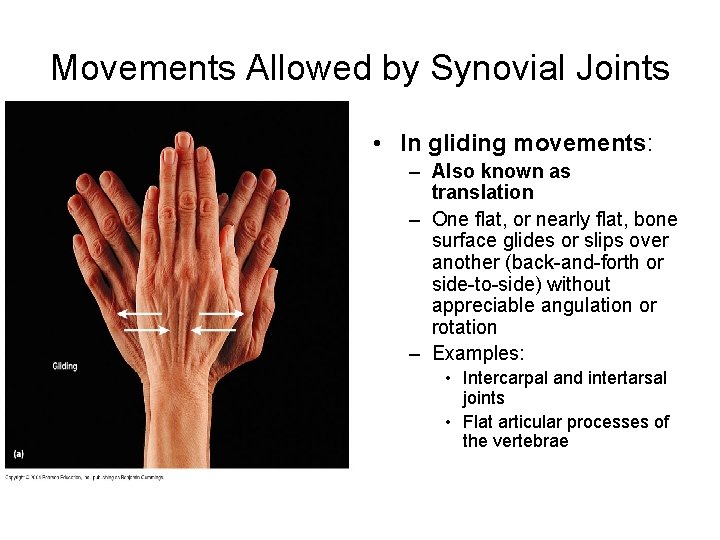
Movements Allowed by Synovial Joints • In gliding movements: – Also known as translation – One flat, or nearly flat, bone surface glides or slips over another (back-and-forth or side-to-side) without appreciable angulation or rotation – Examples: • Intercarpal and intertarsal joints • Flat articular processes of the vertebrae
Synovial Movement Gliding
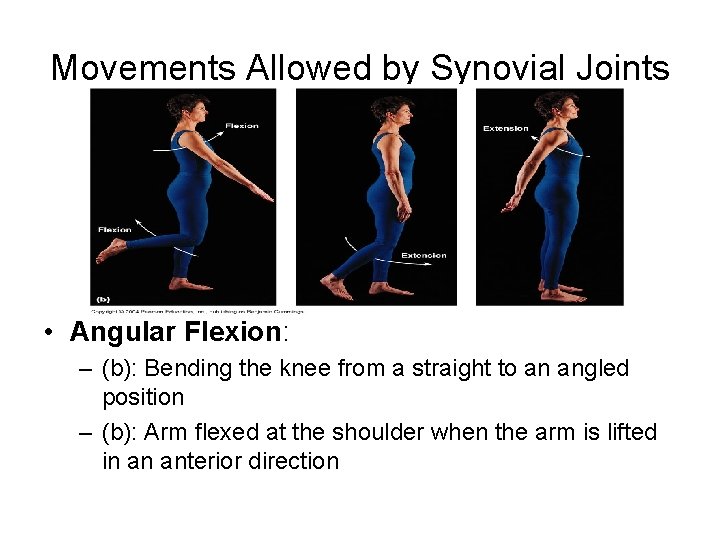
Movements Allowed by Synovial Joints • Angular movements: – Increase or decrease the angle between two bones – May occur in any plane of the body and include: • • • Flexion Extension Hyperextension Abduction Adduction Circumduction
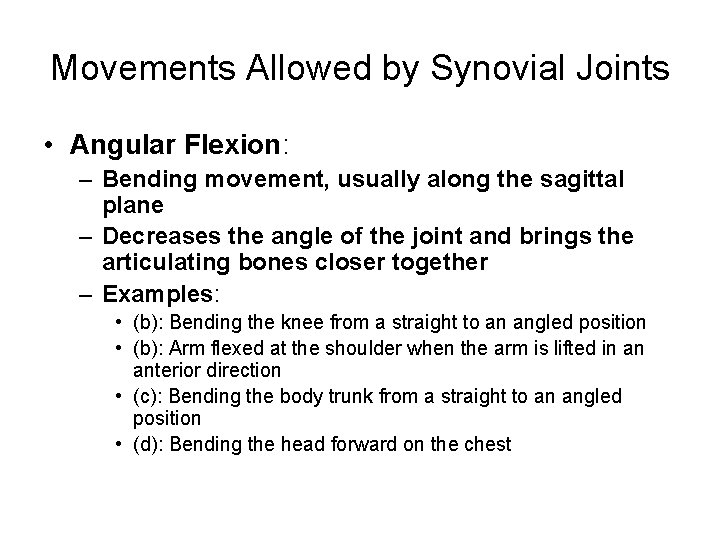
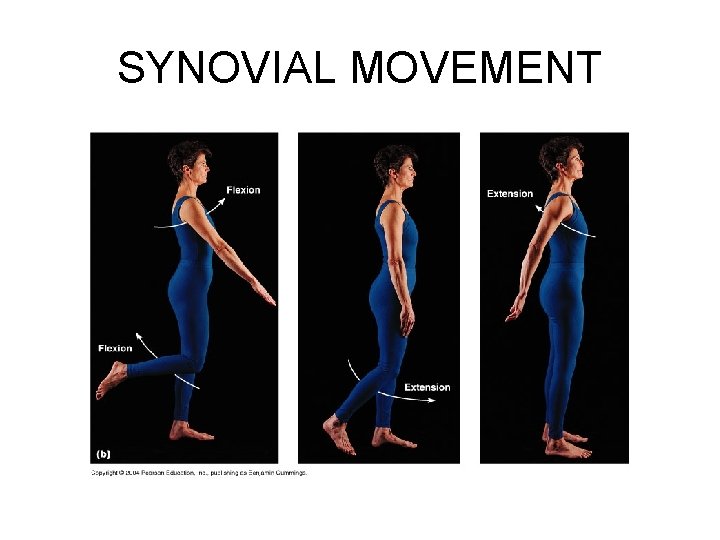
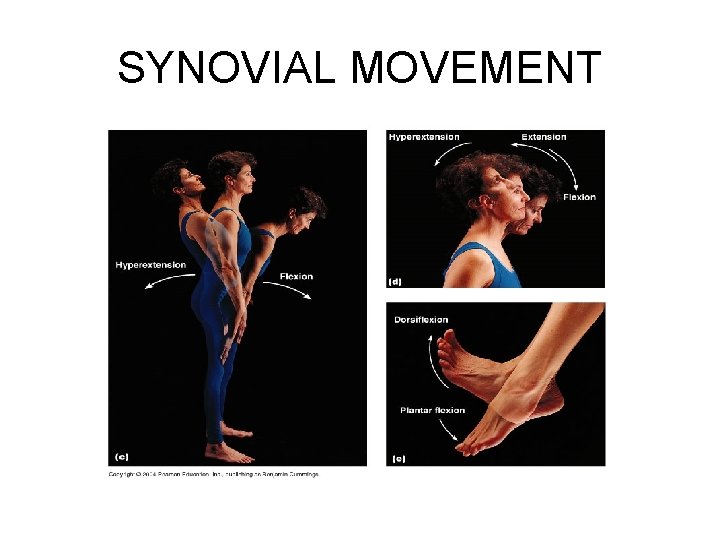
Movements Allowed by Synovial Joints • Angular Flexion: – Bending movement, usually along the sagittal plane – Decreases the angle of the joint and brings the articulating bones closer together – Examples: • (b): Bending the knee from a straight to an angled position • (b): Arm flexed at the shoulder when the arm is lifted in an anterior direction • (c): Bending the body trunk from a straight to an angled position • (d): Bending the head forward on the chest
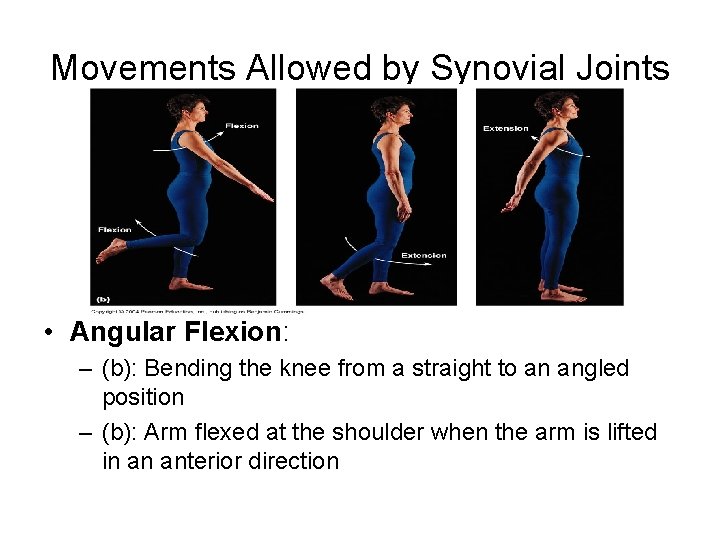
Movements Allowed by Synovial Joints • Angular Flexion: – (b): Bending the knee from a straight to an angled position – (b): Arm flexed at the shoulder when the arm is lifted in an anterior direction
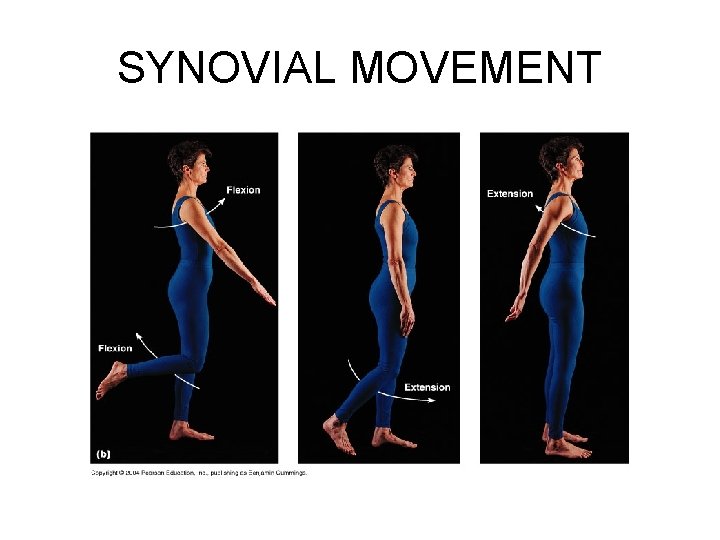
SYNOVIAL MOVEMENT
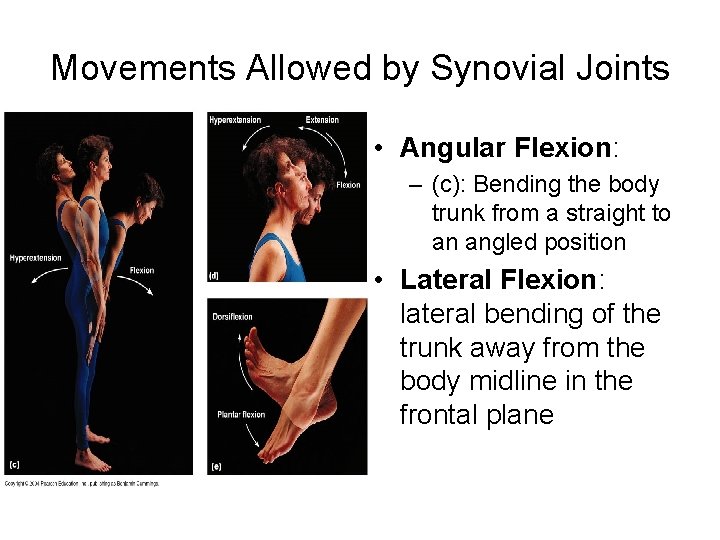
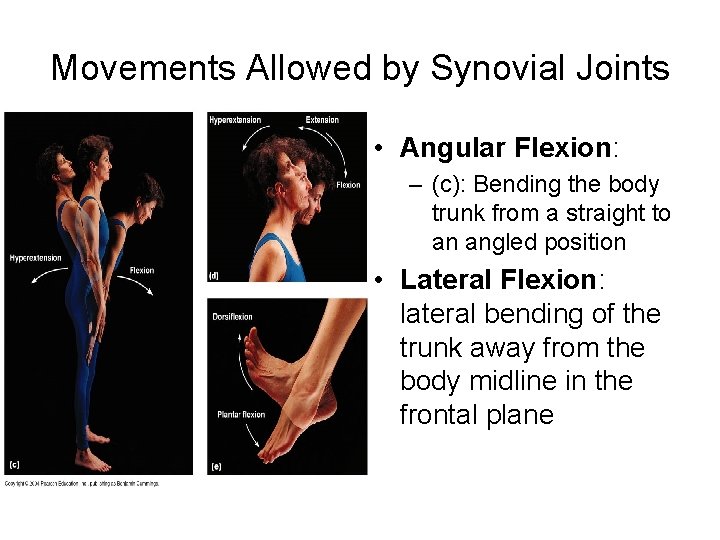
Movements Allowed by Synovial Joints • Angular Flexion: – (c): Bending the body trunk from a straight to an angled position • Lateral Flexion: lateral bending of the trunk away from the body midline in the frontal plane
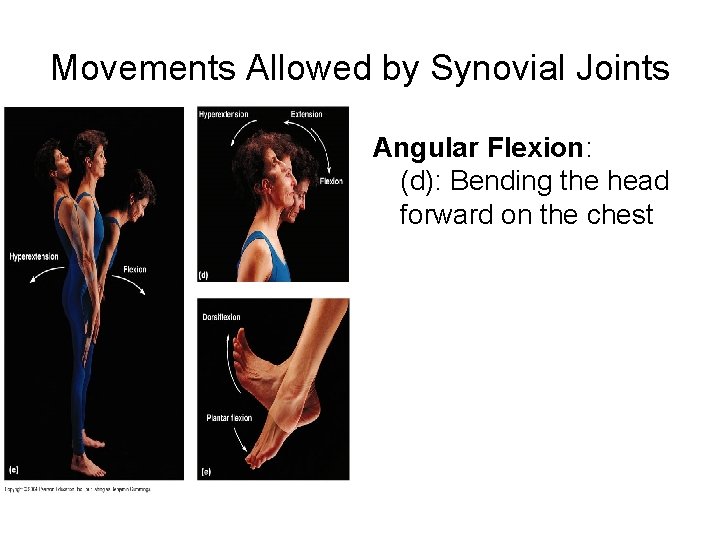
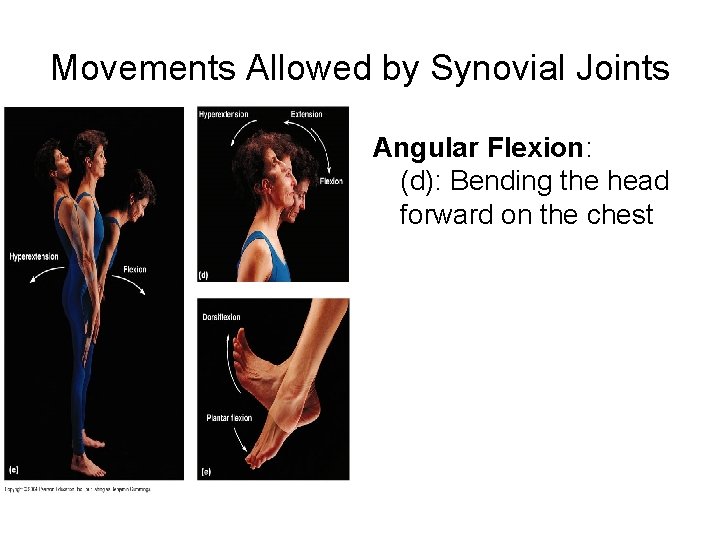
Movements Allowed by Synovial Joints Angular Flexion: (d): Bending the head forward on the chest
SYNOVIAL MOVEMENT
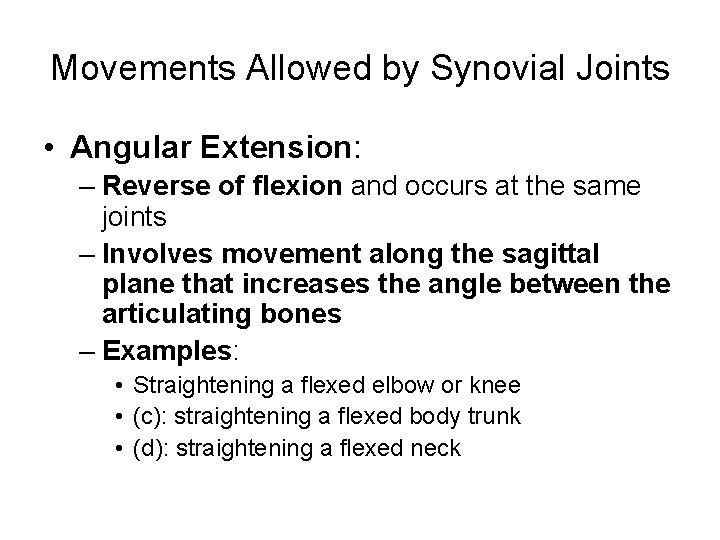
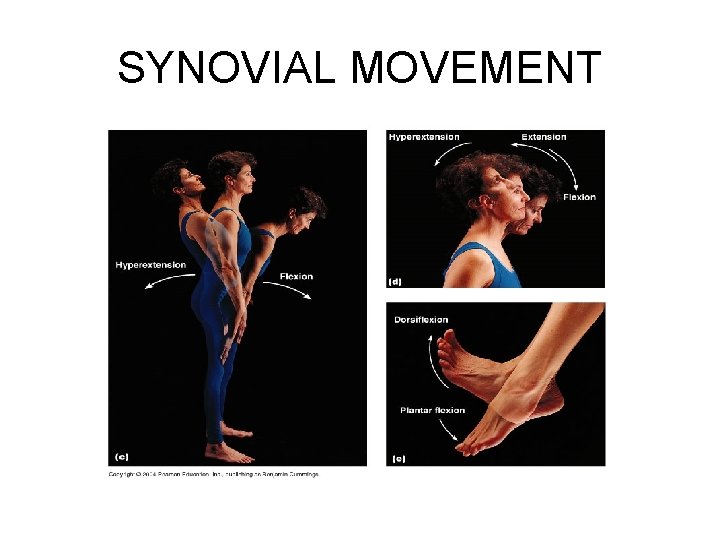
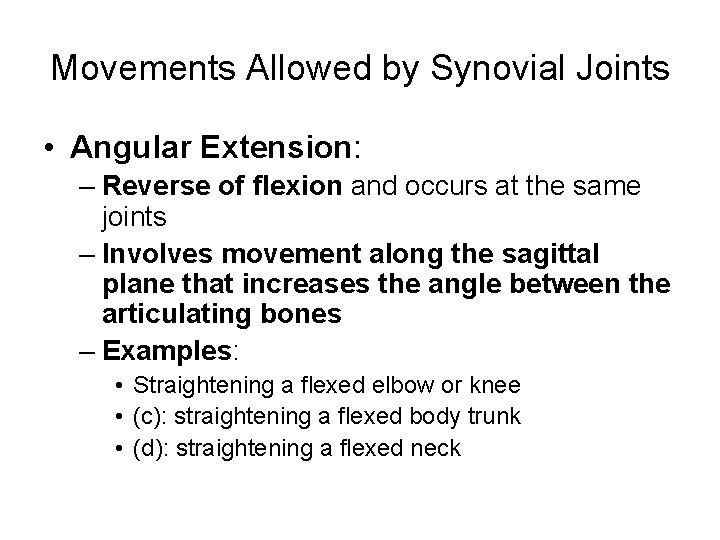
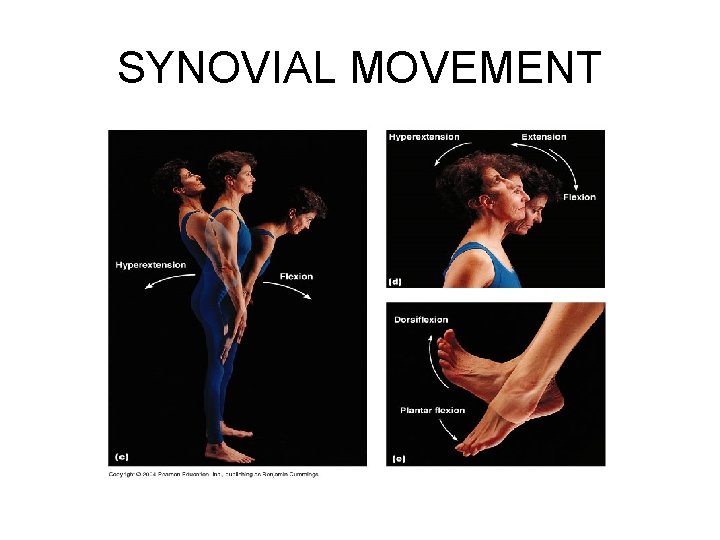
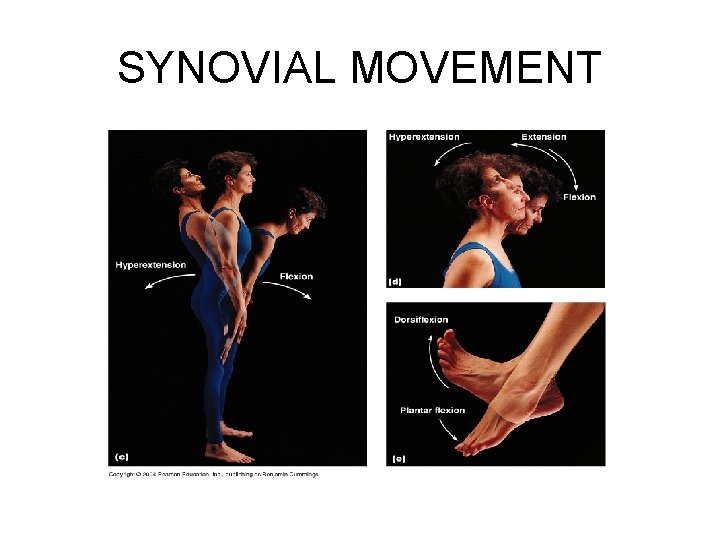
Movements Allowed by Synovial Joints • Angular Extension: – Reverse of flexion and occurs at the same joints – Involves movement along the sagittal plane that increases the angle between the articulating bones – Examples: • Straightening a flexed elbow or knee • (c): straightening a flexed body trunk • (d): straightening a flexed neck
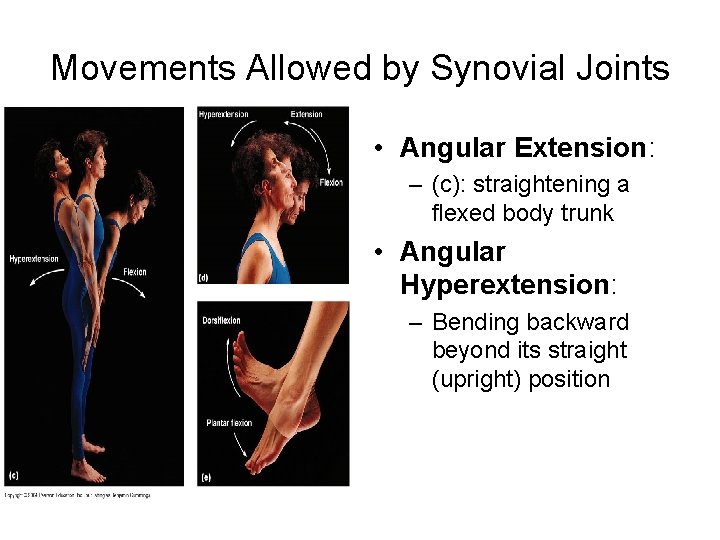
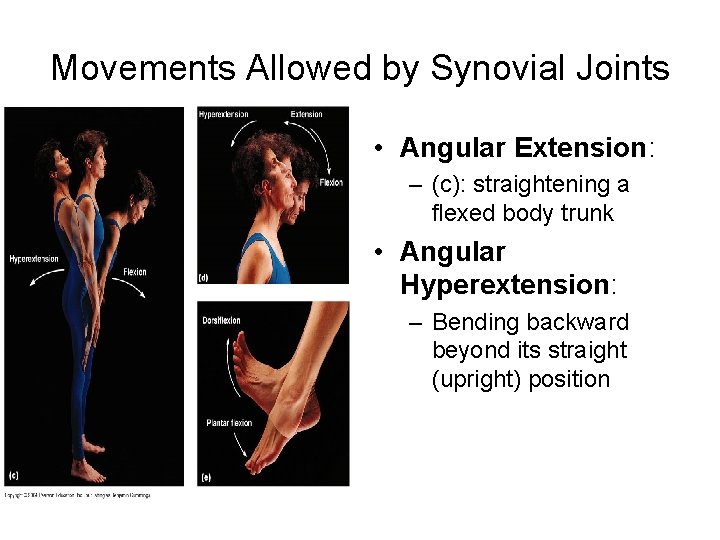
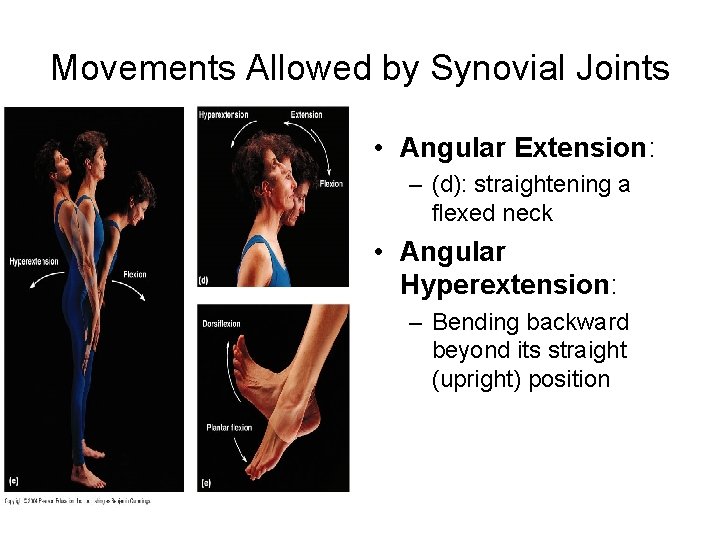
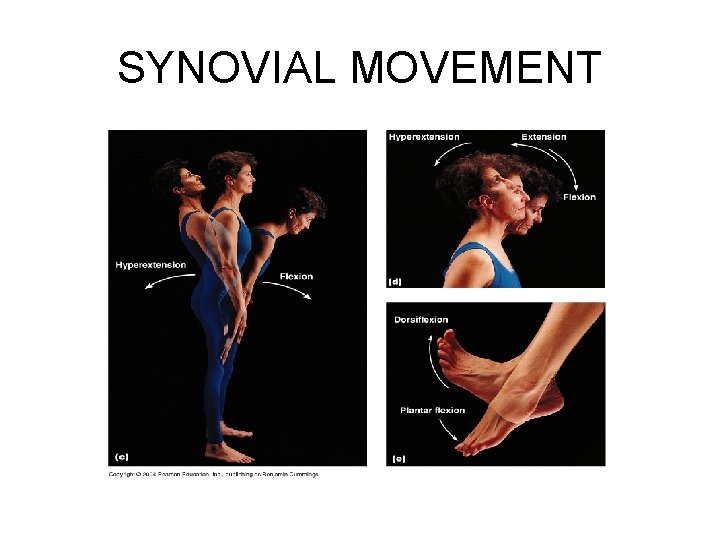
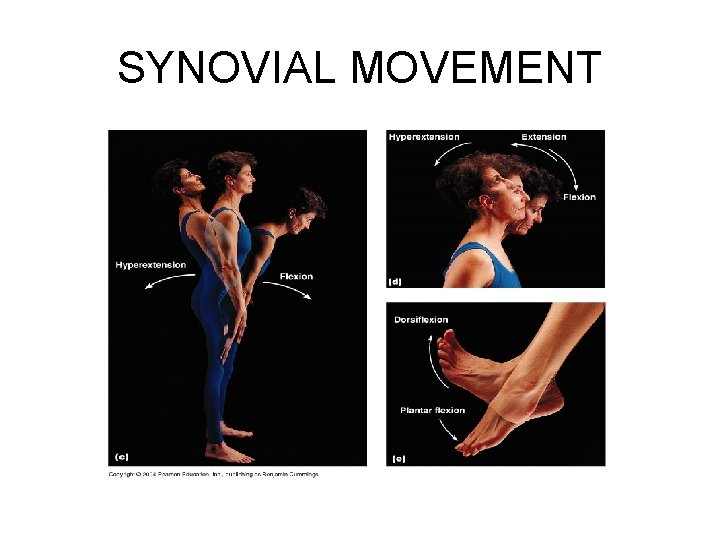
Movements Allowed by Synovial Joints • Angular Extension: – (c): straightening a flexed body trunk • Angular Hyperextension: – Bending backward beyond its straight (upright) position
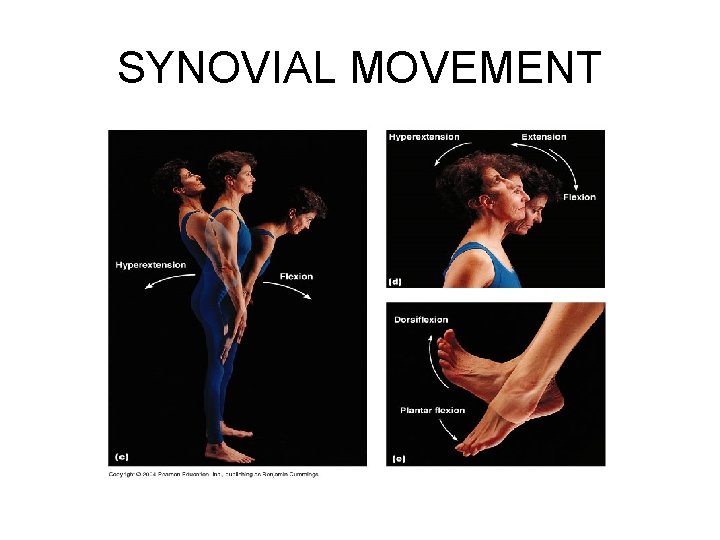
SYNOVIAL MOVEMENT
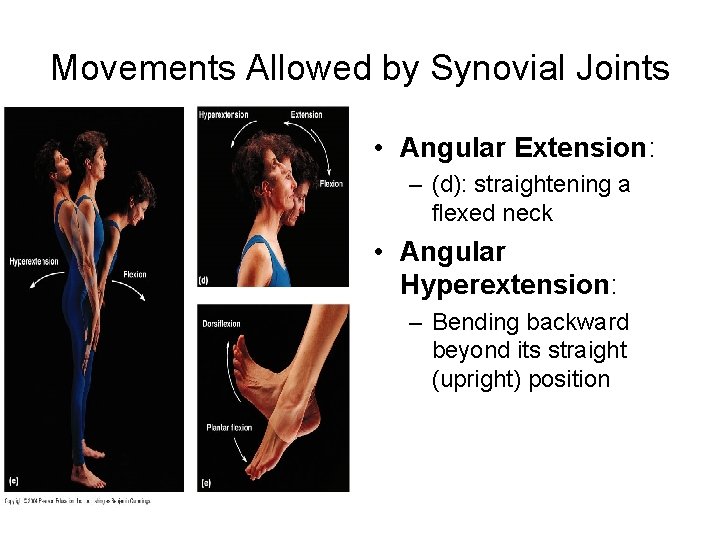
Movements Allowed by Synovial Joints • Angular Extension: – (d): straightening a flexed neck • Angular Hyperextension: – Bending backward beyond its straight (upright) position
SYNOVIAL MOVEMENT
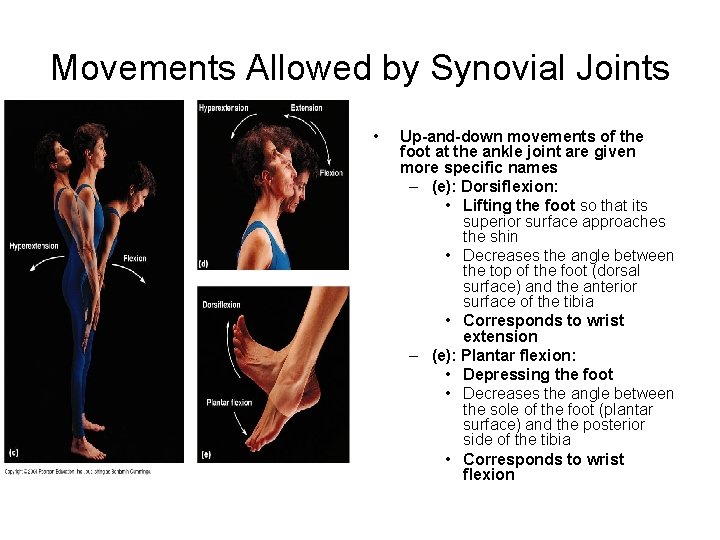
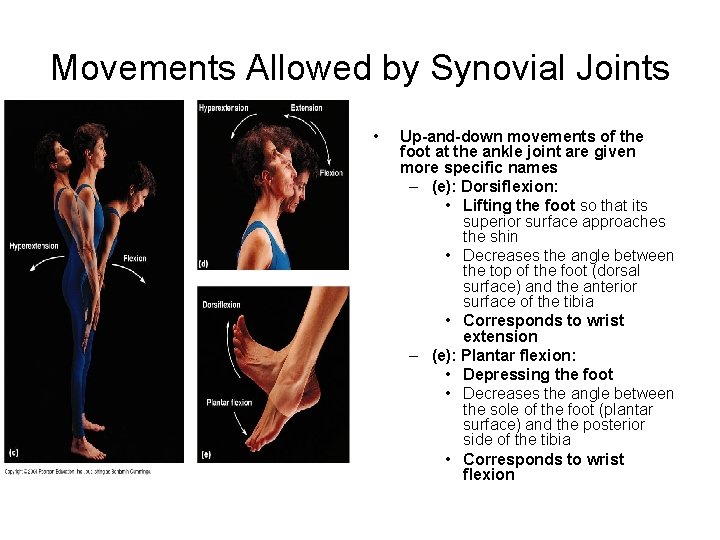
Movements Allowed by Synovial Joints • Up-and-down movements of the foot at the ankle joint are given more specific names – (e): Dorsiflexion: • Lifting the foot so that its superior surface approaches the shin • Decreases the angle between the top of the foot (dorsal surface) and the anterior surface of the tibia • Corresponds to wrist extension – (e): Plantar flexion: • Depressing the foot • Decreases the angle between the sole of the foot (plantar surface) and the posterior side of the tibia • Corresponds to wrist flexion
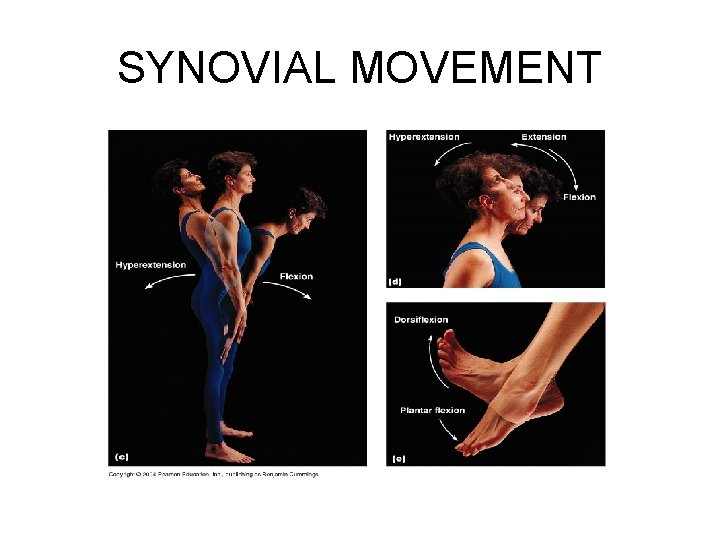
SYNOVIAL MOVEMENT
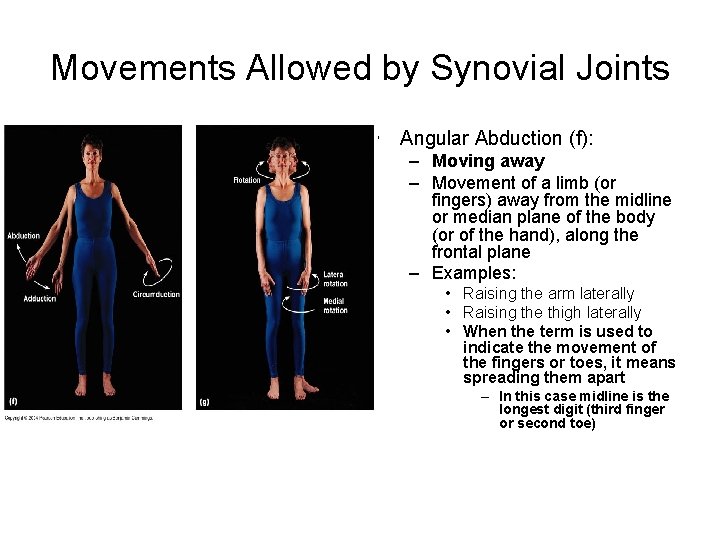
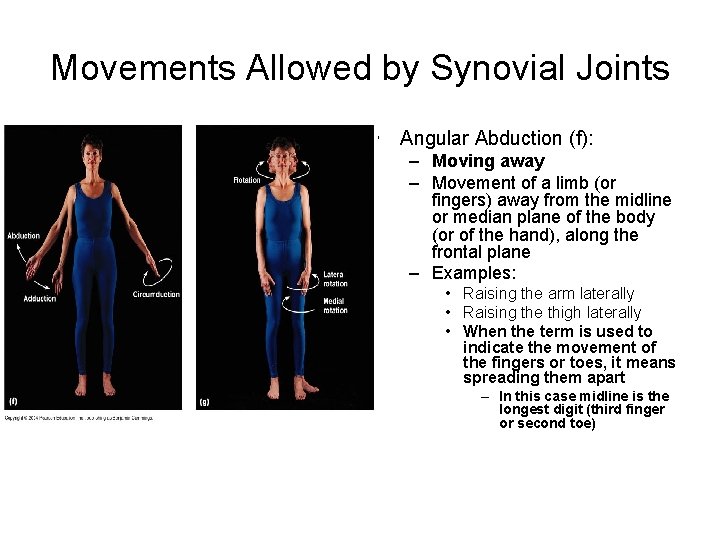
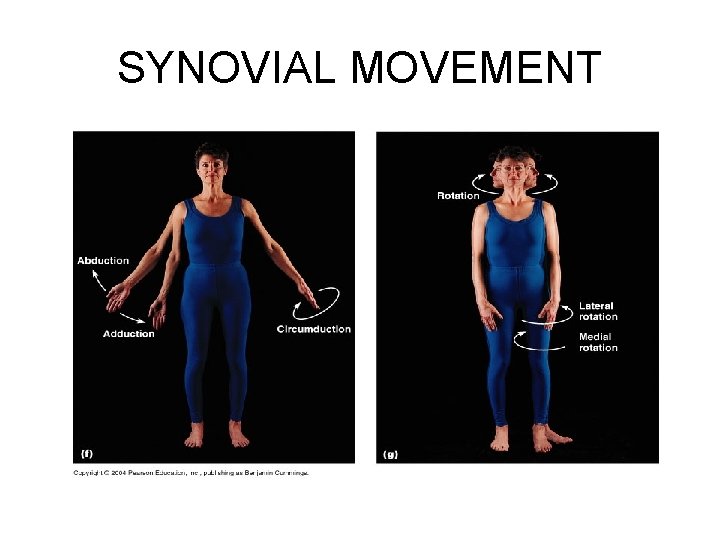
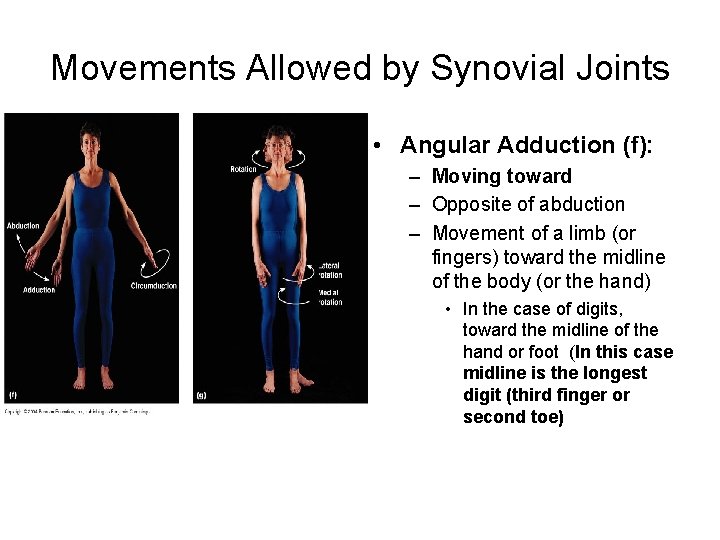
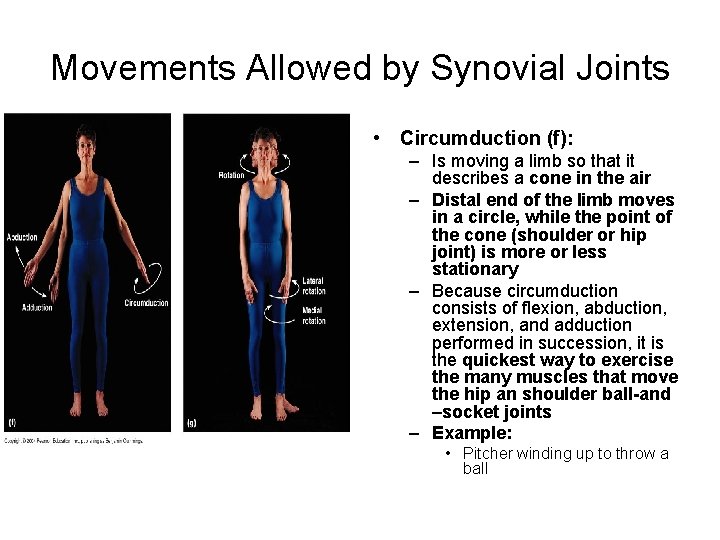
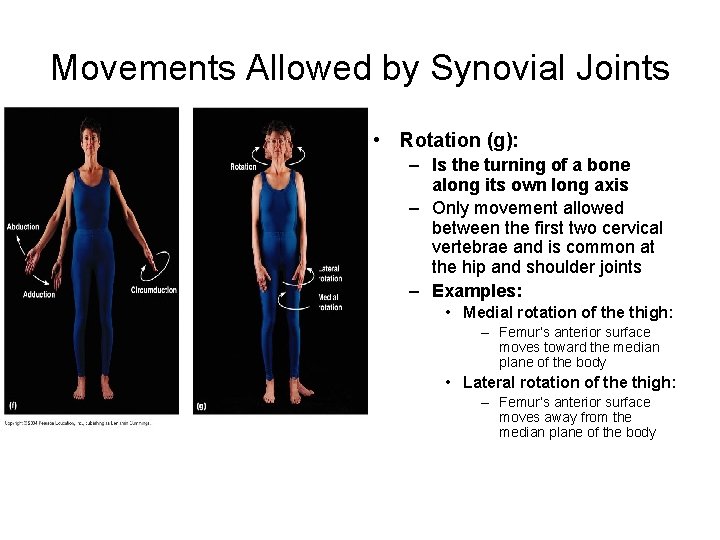
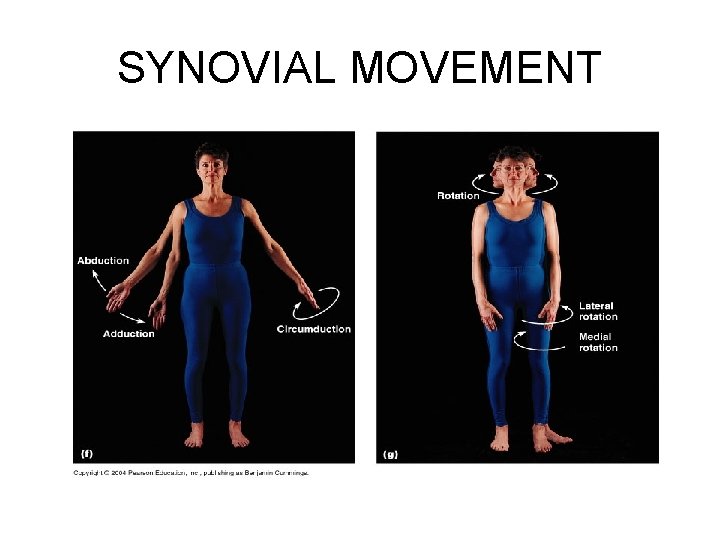
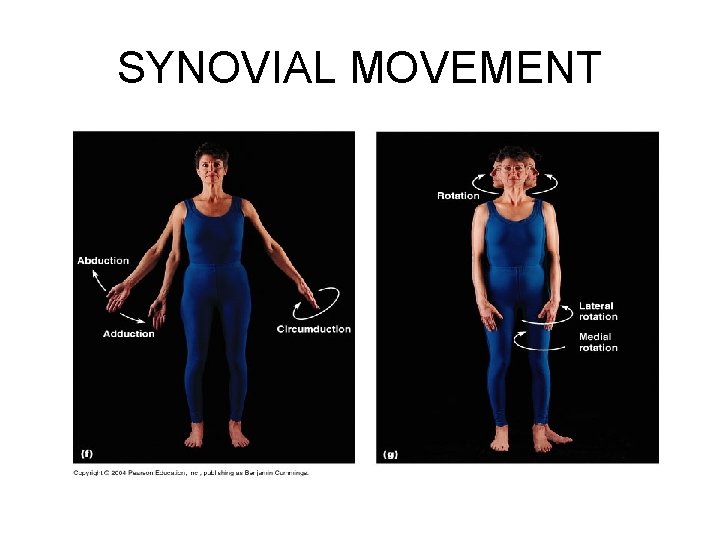
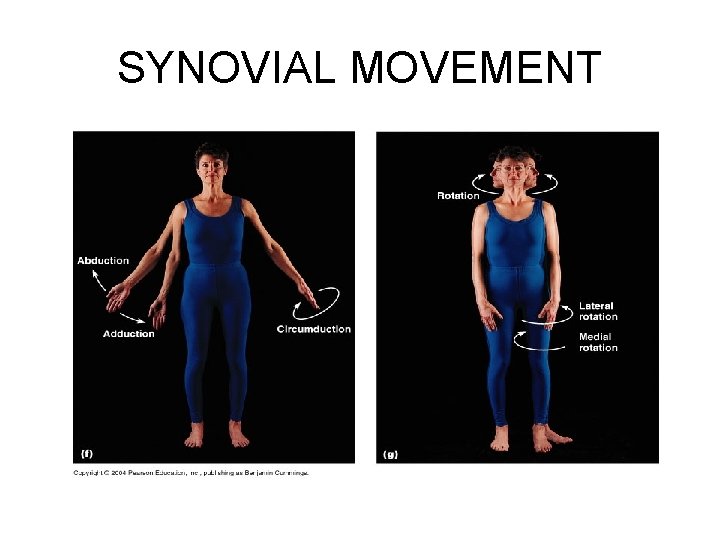
Movements Allowed by Synovial Joints • Angular Abduction (f): – Moving away – Movement of a limb (or fingers) away from the midline or median plane of the body (or of the hand), along the frontal plane – Examples: • Raising the arm laterally • Raising the thigh laterally • When the term is used to indicate the movement of the fingers or toes, it means spreading them apart – In this case midline is the longest digit (third finger or second toe)
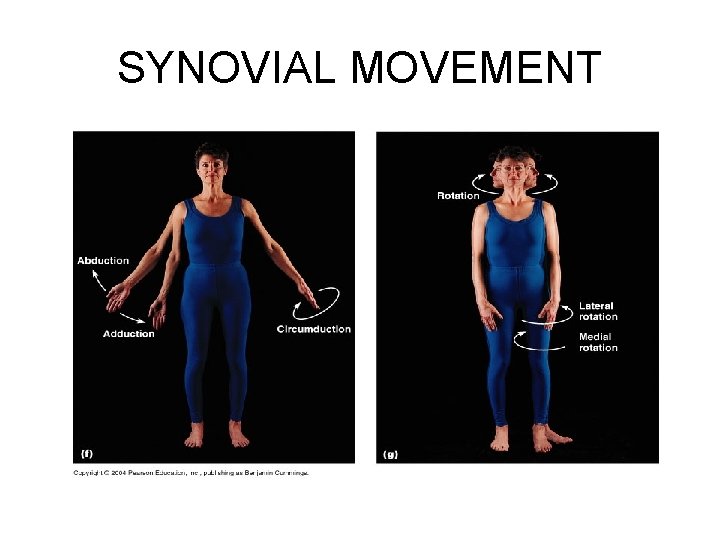
SYNOVIAL MOVEMENT
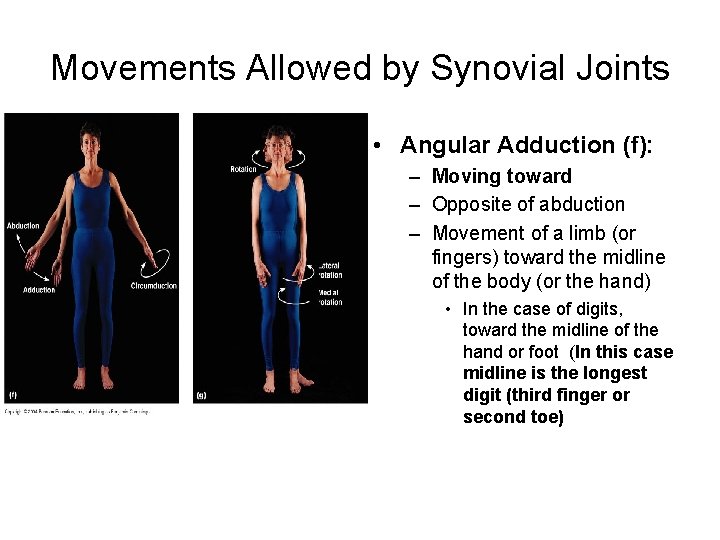
Movements Allowed by Synovial Joints • Angular Adduction (f): – Moving toward – Opposite of abduction – Movement of a limb (or fingers) toward the midline of the body (or the hand) • In the case of digits, toward the midline of the hand or foot (In this case midline is the longest digit (third finger or second toe)
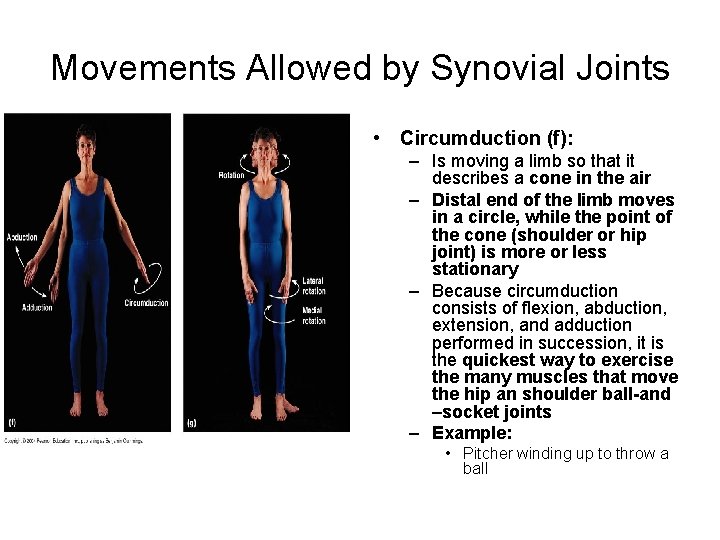
Movements Allowed by Synovial Joints • Circumduction (f): – Is moving a limb so that it describes a cone in the air – Distal end of the limb moves in a circle, while the point of the cone (shoulder or hip joint) is more or less stationary – Because circumduction consists of flexion, abduction, extension, and adduction performed in succession, it is the quickest way to exercise the many muscles that move the hip an shoulder ball-and –socket joints – Example: • Pitcher winding up to throw a ball
SYNOVIAL MOVEMENT
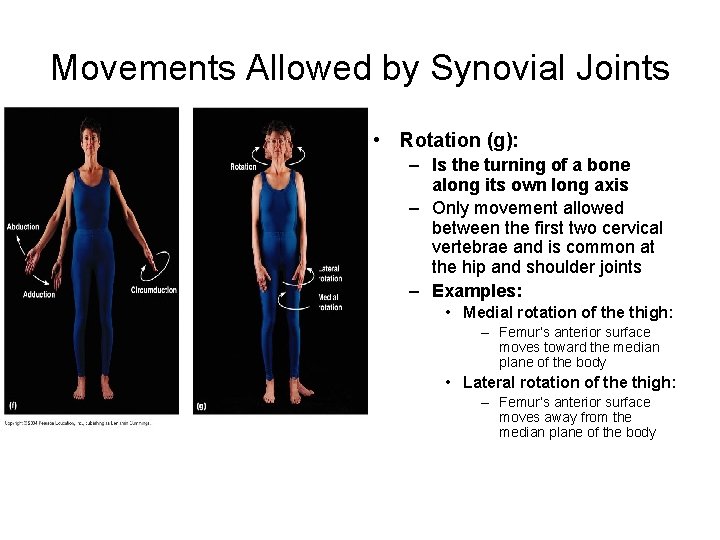
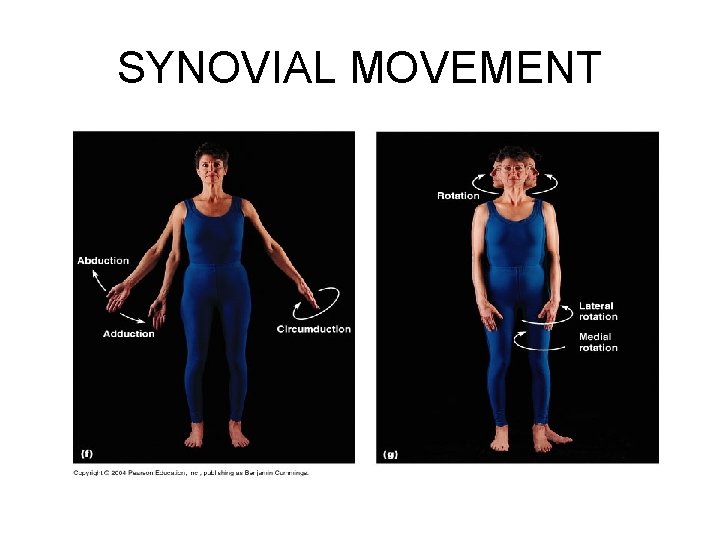
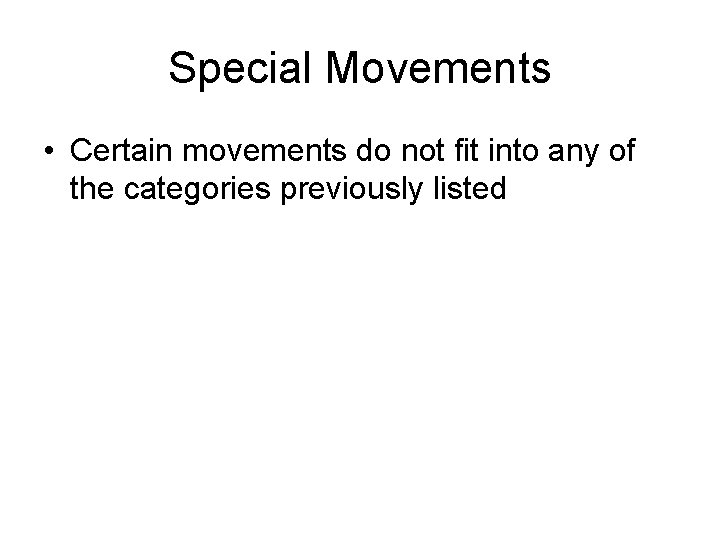
Movements Allowed by Synovial Joints • Rotation (g): – Is the turning of a bone along its own long axis – Only movement allowed between the first two cervical vertebrae and is common at the hip and shoulder joints – Examples: • Medial rotation of the thigh: – Femur’s anterior surface moves toward the median plane of the body • Lateral rotation of the thigh: – Femur’s anterior surface moves away from the median plane of the body
SYNOVIAL MOVEMENT
Special Movements • Certain movements do not fit into any of the categories previously listed
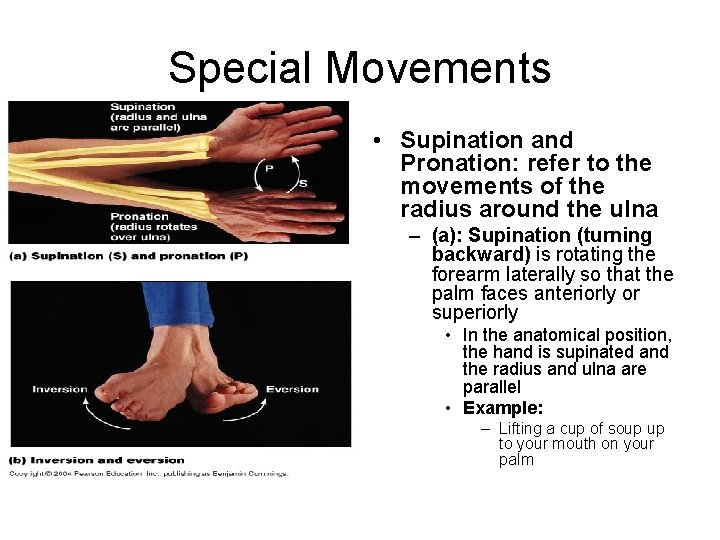
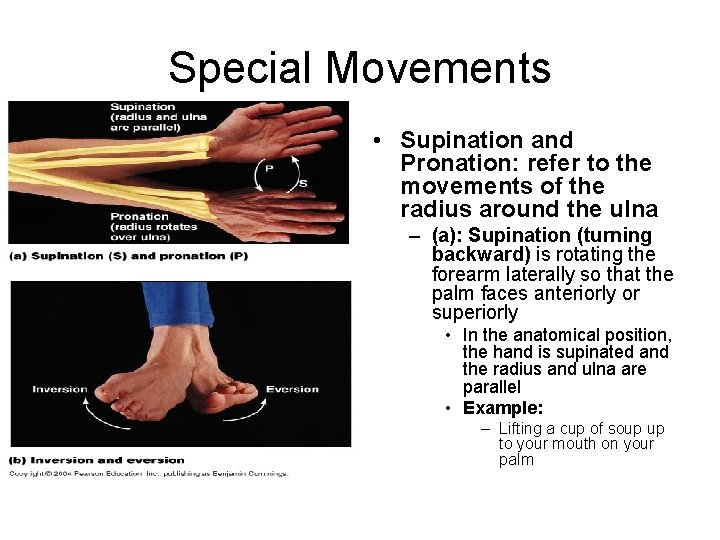
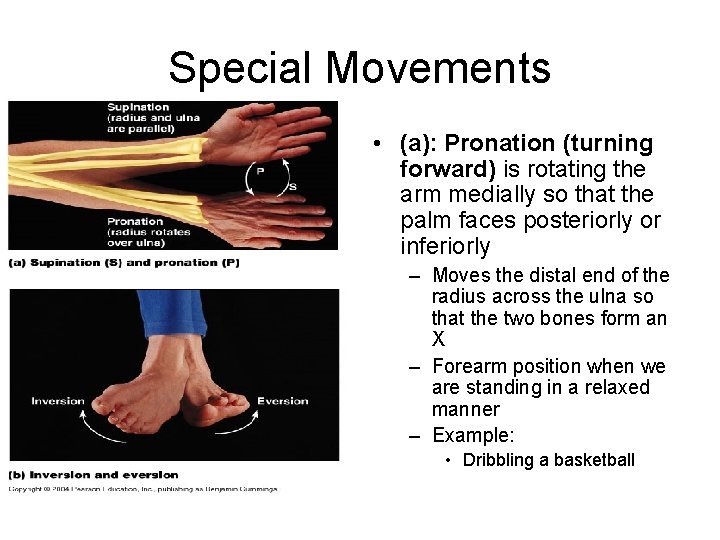
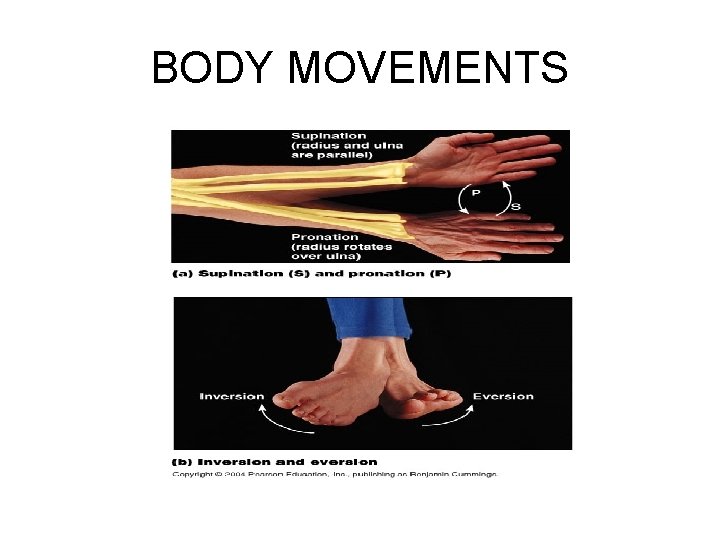
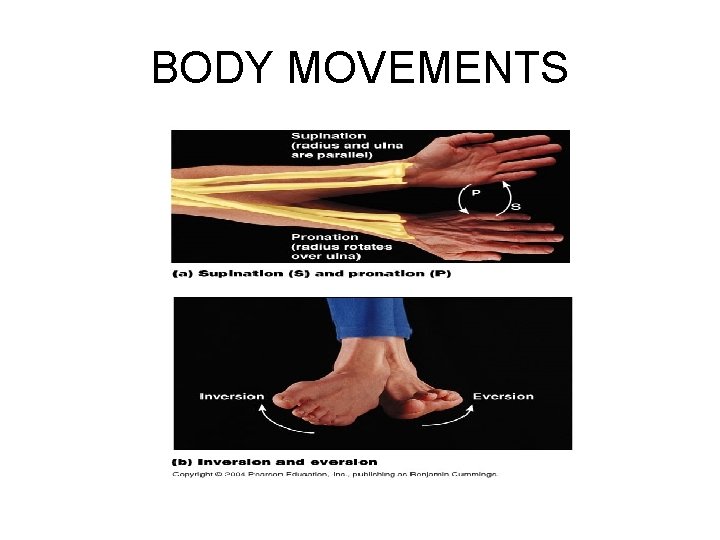
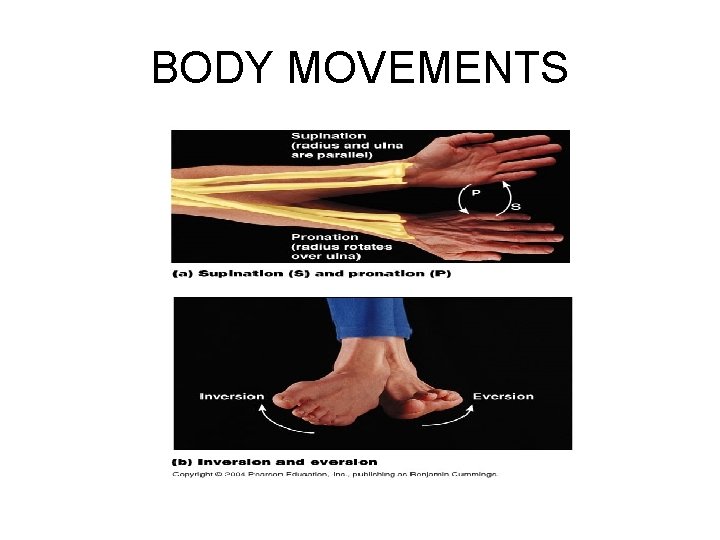
Special Movements • Supination and Pronation: refer to the movements of the radius around the ulna – (a): Supination (turning backward) is rotating the forearm laterally so that the palm faces anteriorly or superiorly • In the anatomical position, the hand is supinated and the radius and ulna are parallel • Example: – Lifting a cup of soup up to your mouth on your palm
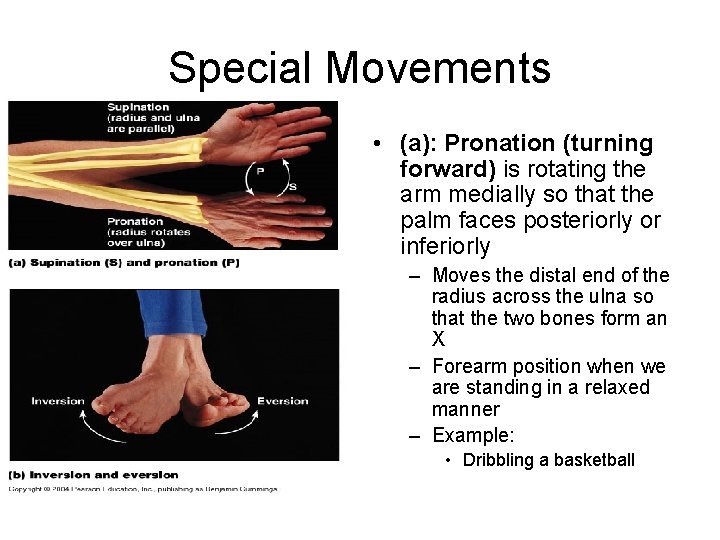
Special Movements • (a): Pronation (turning forward) is rotating the arm medially so that the palm faces posteriorly or inferiorly – Moves the distal end of the radius across the ulna so that the two bones form an X – Forearm position when we are standing in a relaxed manner – Example: • Dribbling a basketball
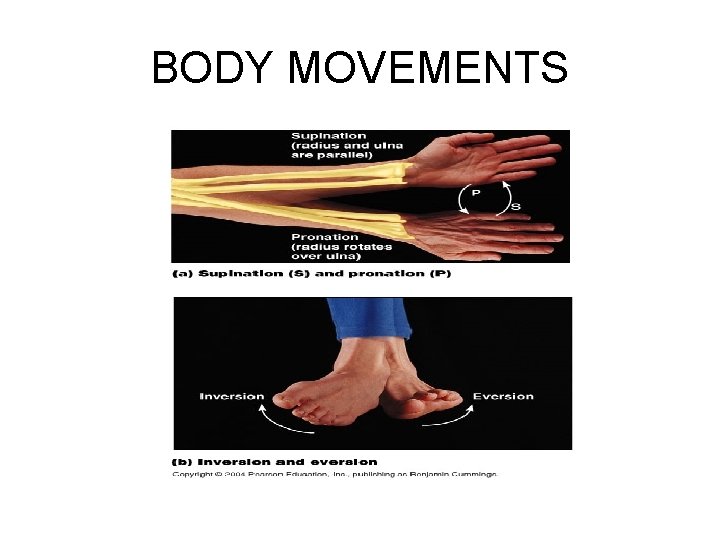
BODY MOVEMENTS
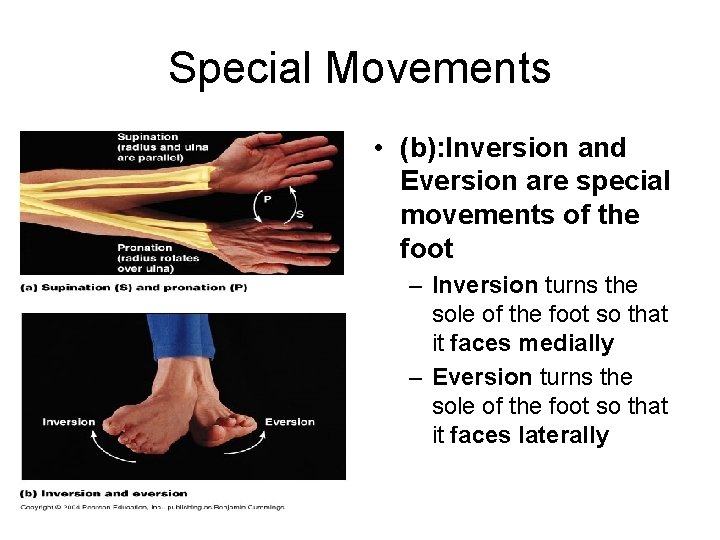
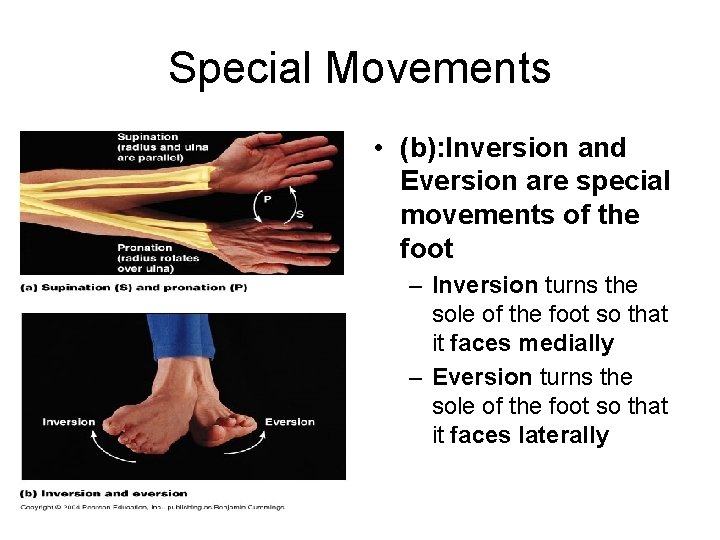
Special Movements • (b): Inversion and Eversion are special movements of the foot – Inversion turns the sole of the foot so that it faces medially – Eversion turns the sole of the foot so that it faces laterally
BODY MOVEMENTS
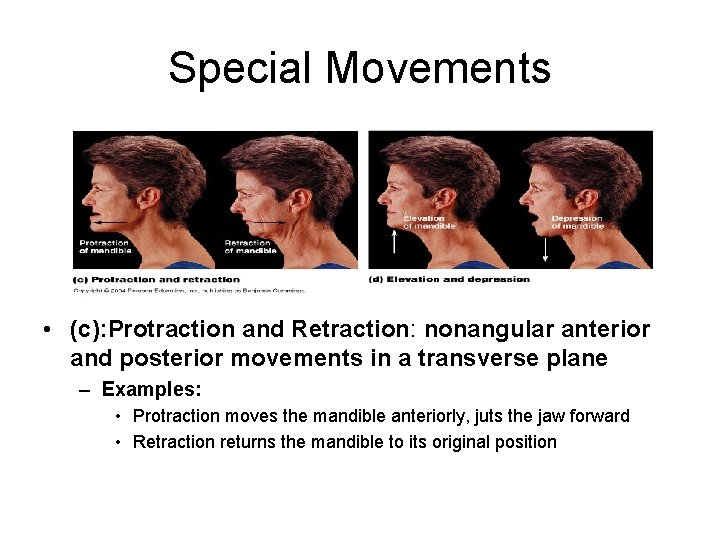
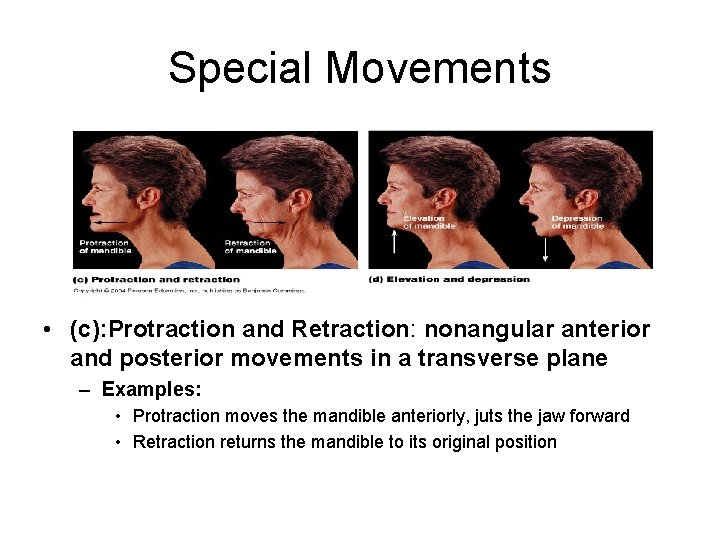
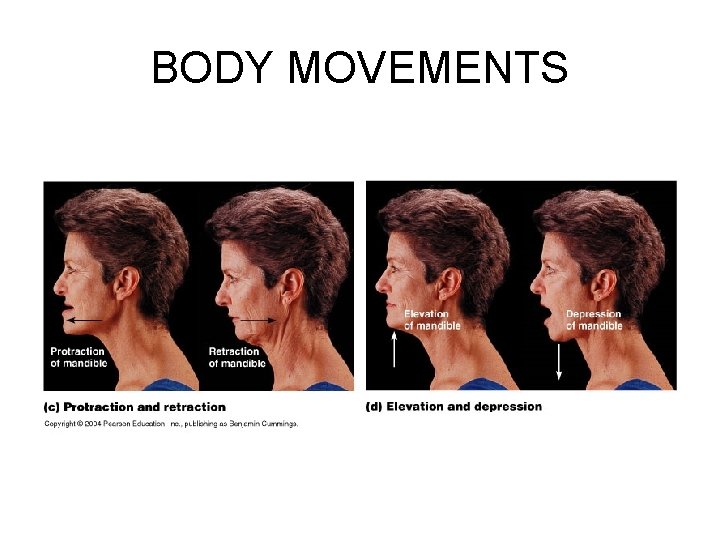
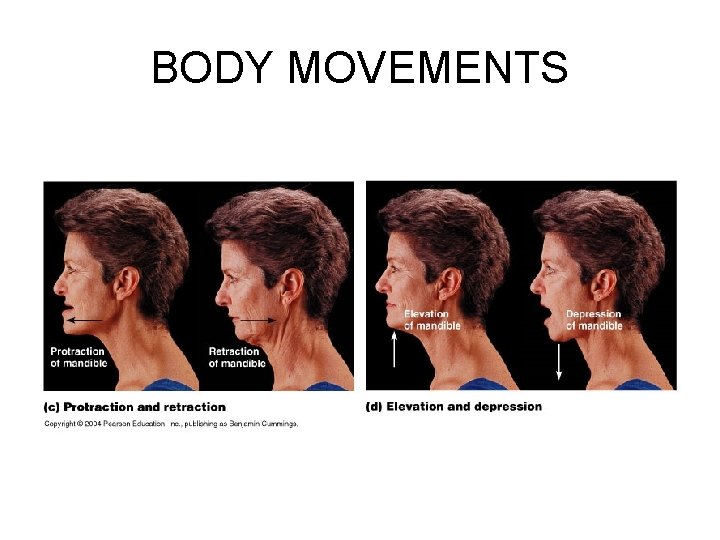
Special Movements • (c): Protraction and Retraction: nonangular anterior and posterior movements in a transverse plane – Examples: • Protraction moves the mandible anteriorly, juts the jaw forward • Retraction returns the mandible to its original position
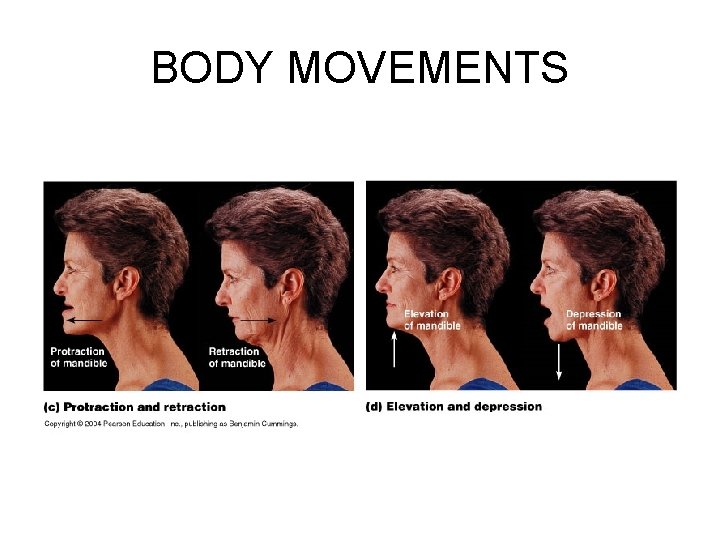
BODY MOVEMENTS
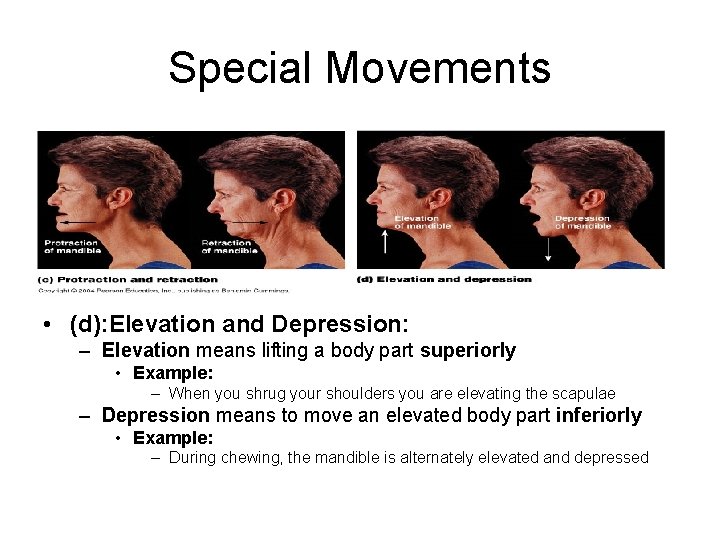
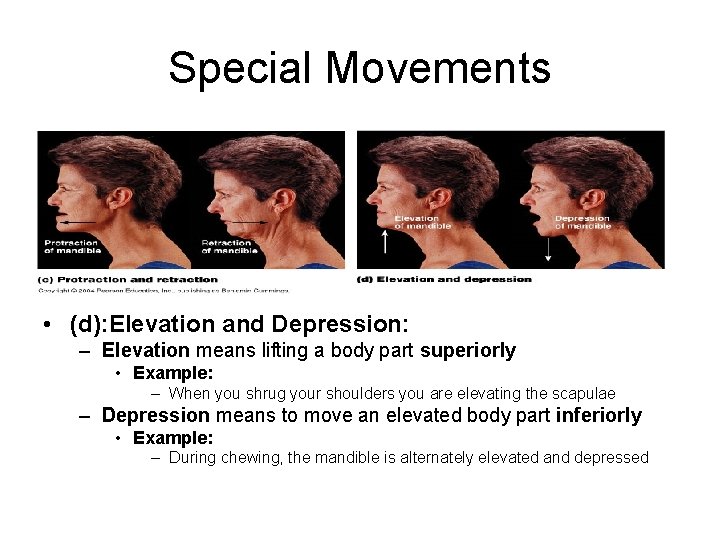
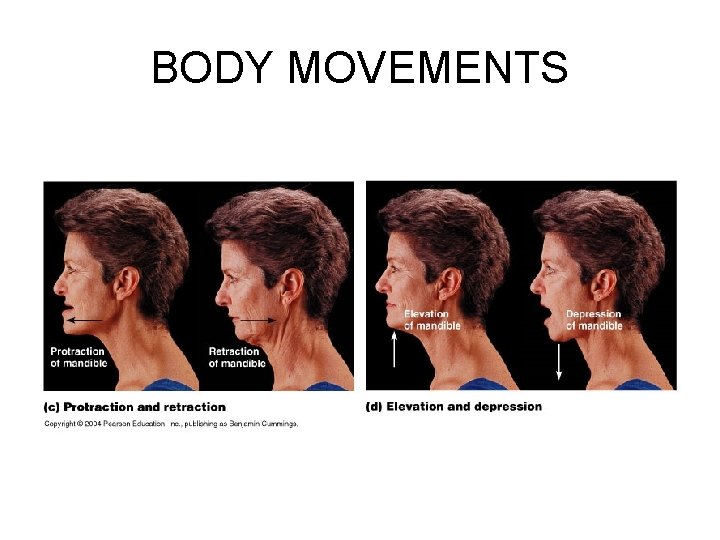
Special Movements • (d): Elevation and Depression: – Elevation means lifting a body part superiorly • Example: – When you shrug your shoulders you are elevating the scapulae – Depression means to move an elevated body part inferiorly • Example: – During chewing, the mandible is alternately elevated and depressed
BODY MOVEMENTS
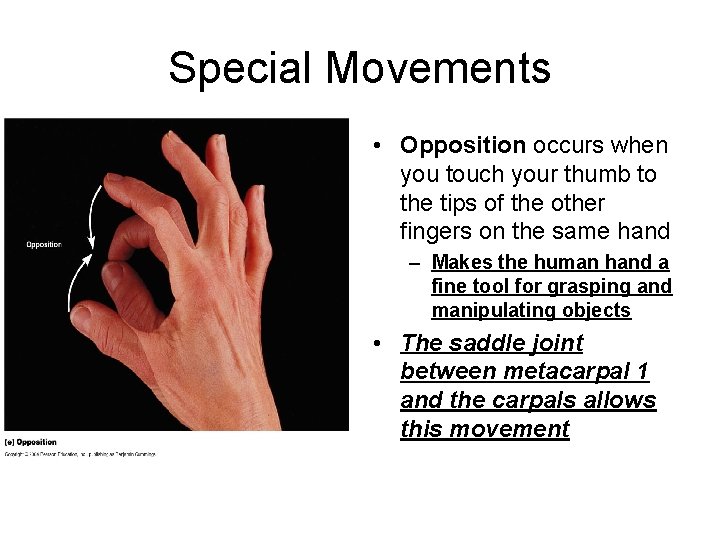
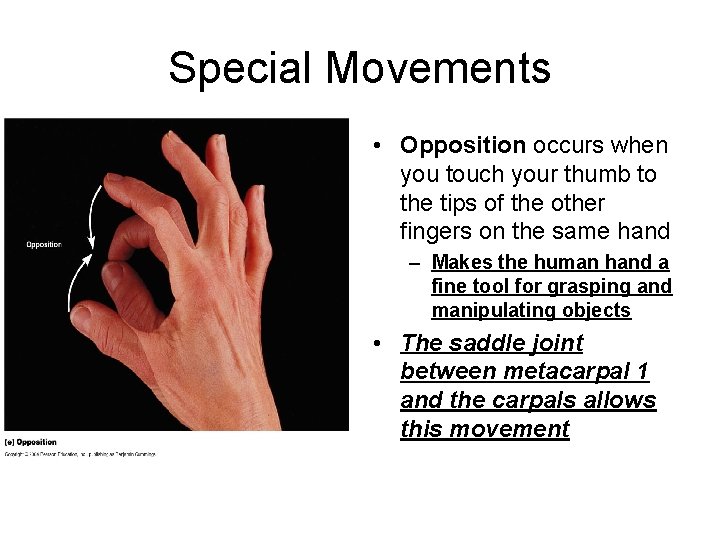
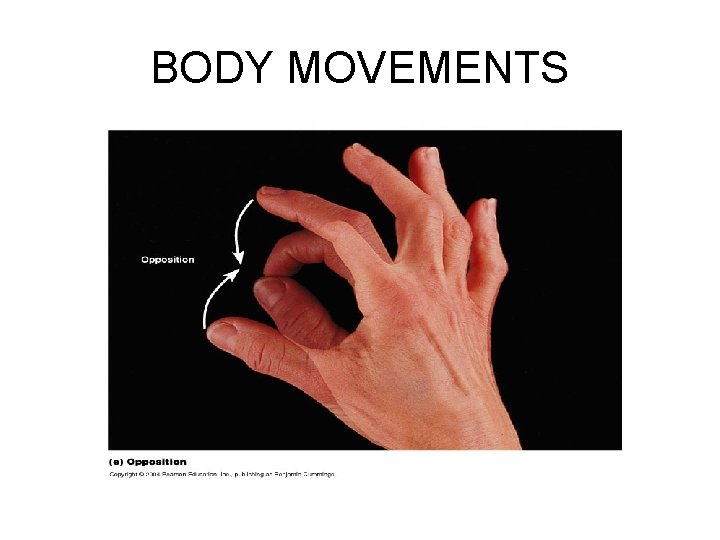
Special Movements • Opposition occurs when you touch your thumb to the tips of the other fingers on the same hand – Makes the human hand a fine tool for grasping and manipulating objects • The saddle joint between metacarpal 1 and the carpals allows this movement
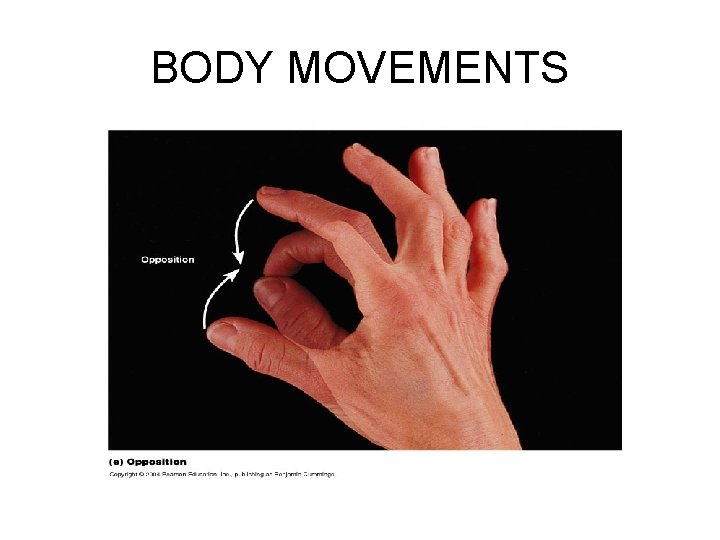
BODY MOVEMENTS
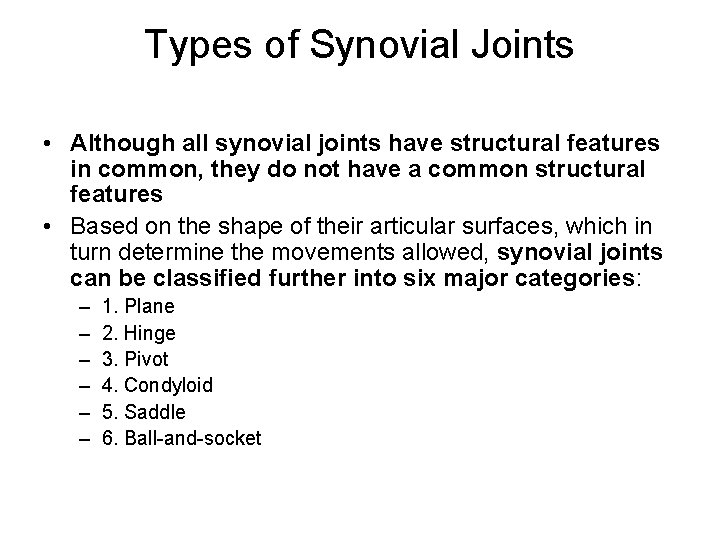
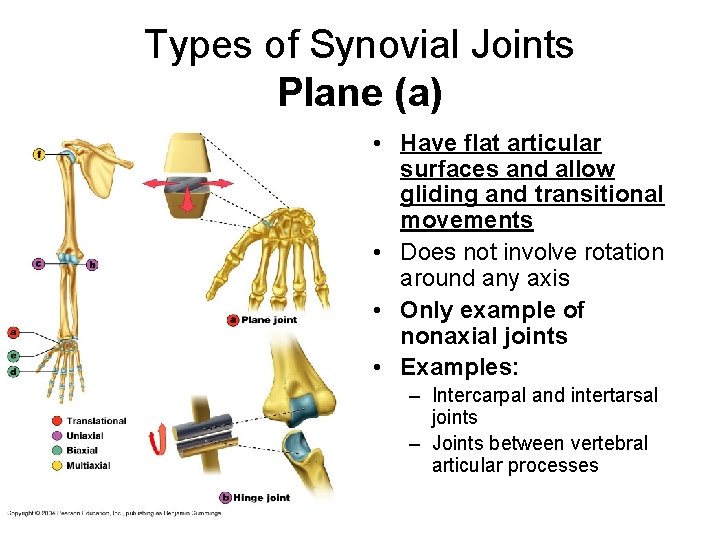
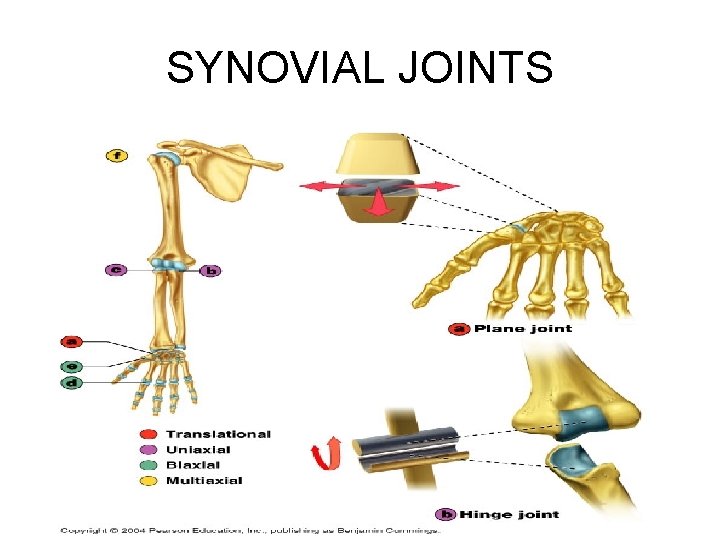
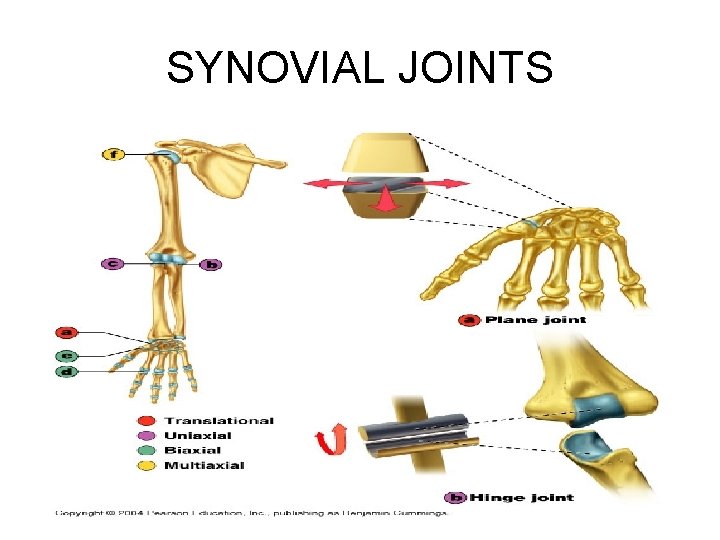
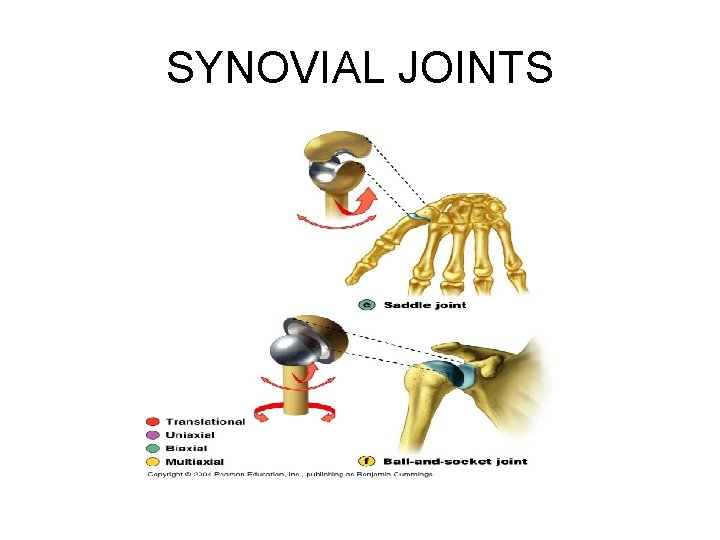
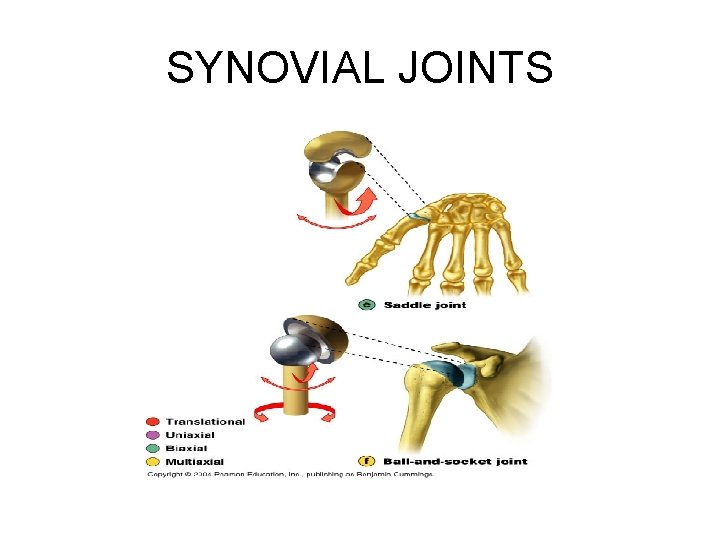
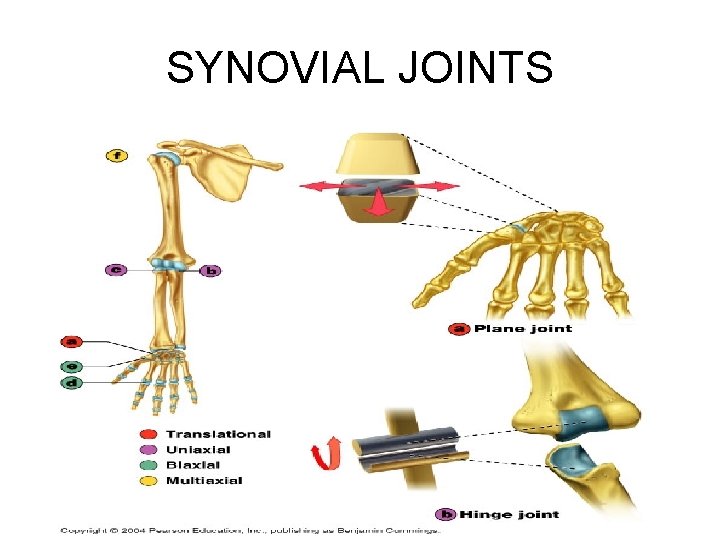
Types of Synovial Joints • Although all synovial joints have structural features in common, they do not have a common structural features • Based on the shape of their articular surfaces, which in turn determine the movements allowed, synovial joints can be classified further into six major categories: – – – 1. Plane 2. Hinge 3. Pivot 4. Condyloid 5. Saddle 6. Ball-and-socket
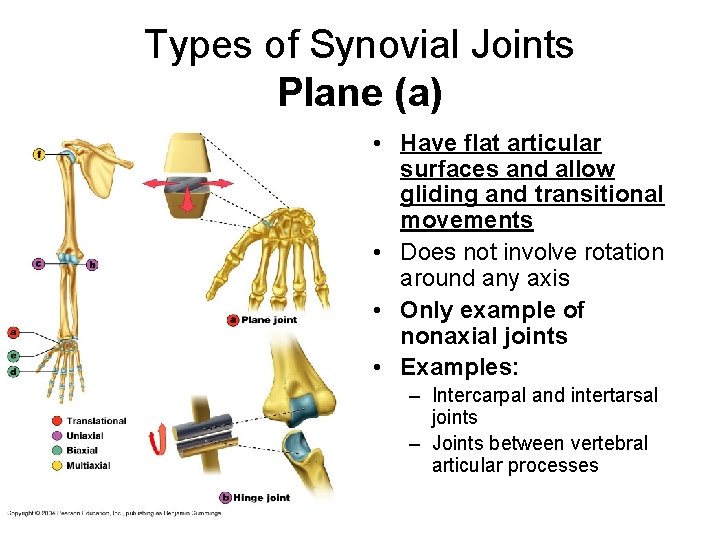
Types of Synovial Joints Plane (a) • Have flat articular surfaces and allow gliding and transitional movements • Does not involve rotation around any axis • Only example of nonaxial joints • Examples: – Intercarpal and intertarsal joints – Joints between vertebral articular processes
SYNOVIAL JOINTS
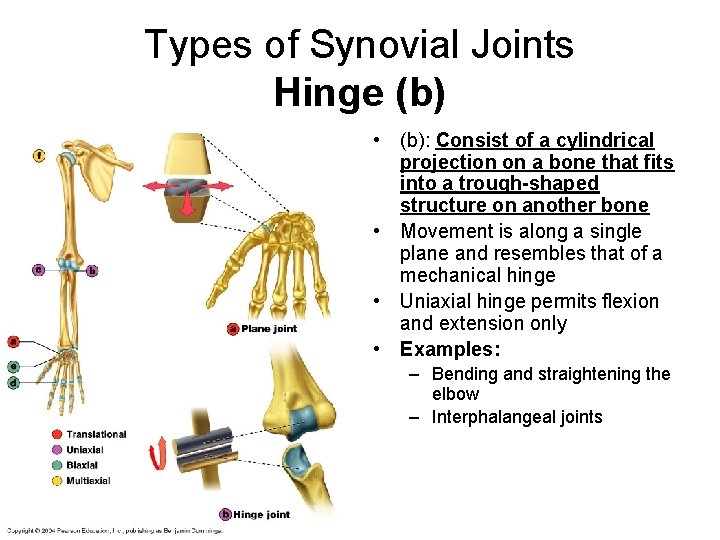
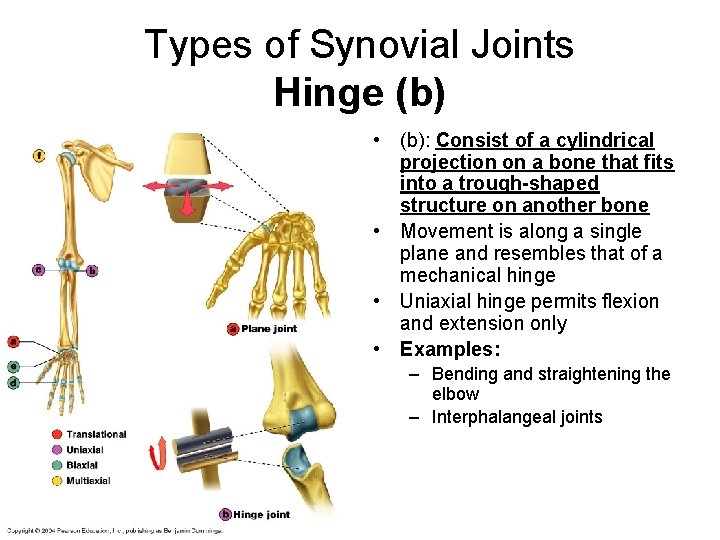
Types of Synovial Joints Hinge (b) • (b): Consist of a cylindrical projection on a bone that fits into a trough-shaped structure on another bone • Movement is along a single plane and resembles that of a mechanical hinge • Uniaxial hinge permits flexion and extension only • Examples: – Bending and straightening the elbow – Interphalangeal joints
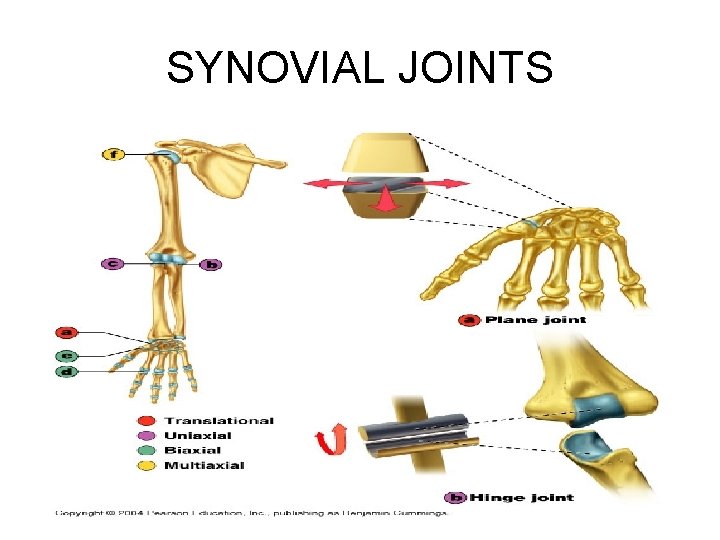
SYNOVIAL JOINTS
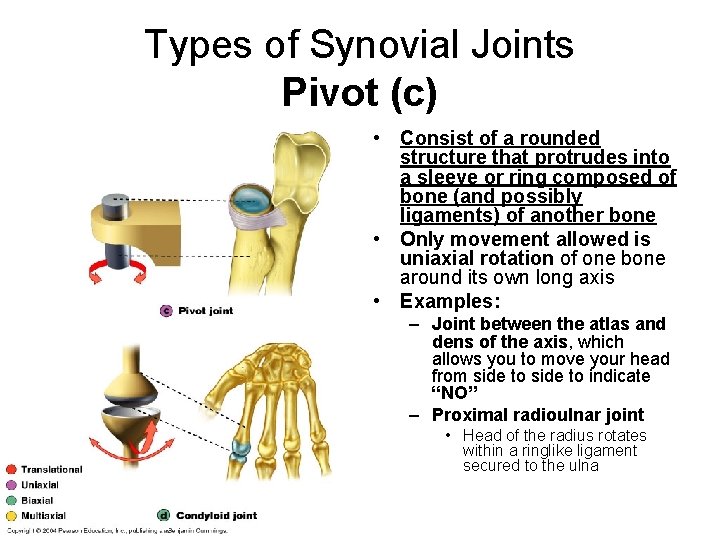
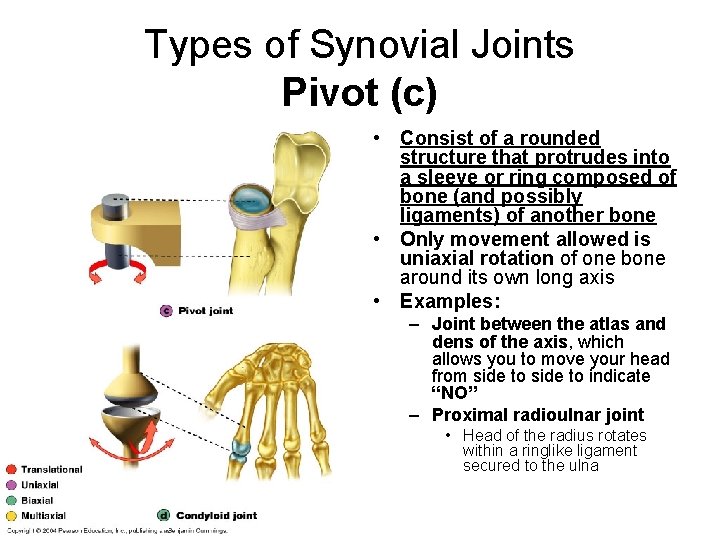
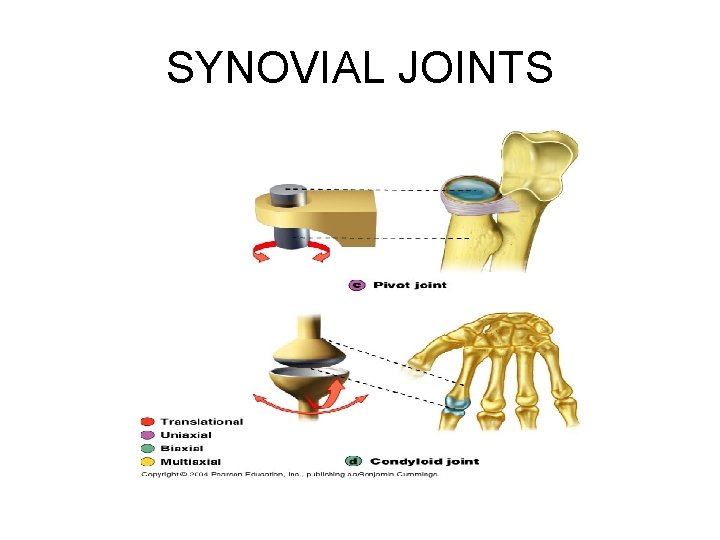
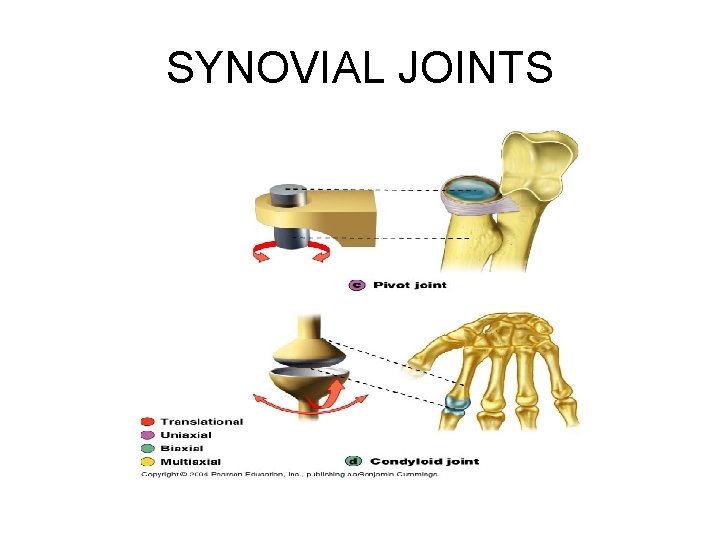
Types of Synovial Joints Pivot (c) • Consist of a rounded structure that protrudes into a sleeve or ring composed of bone (and possibly ligaments) of another bone • Only movement allowed is uniaxial rotation of one bone around its own long axis • Examples: – Joint between the atlas and dens of the axis, which allows you to move your head from side to indicate “NO” – Proximal radioulnar joint • Head of the radius rotates within a ringlike ligament secured to the ulna
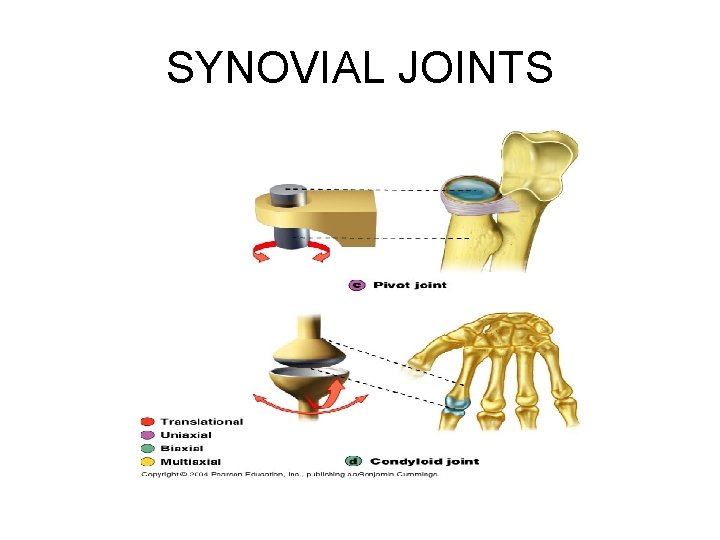
SYNOVIAL JOINTS
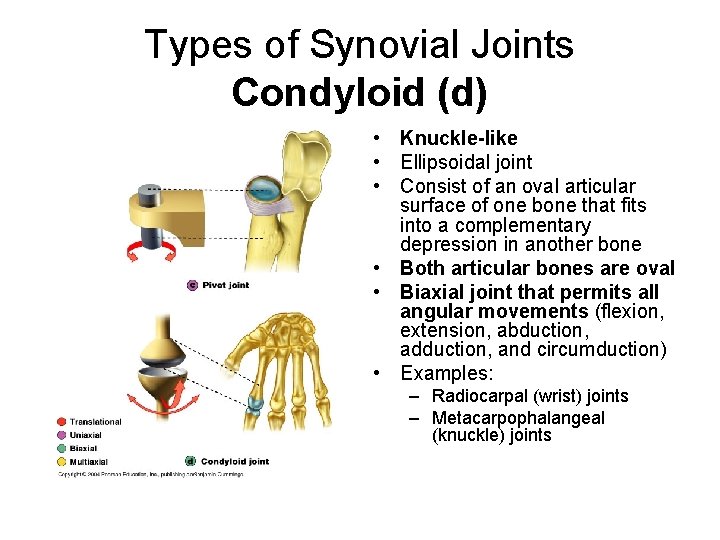
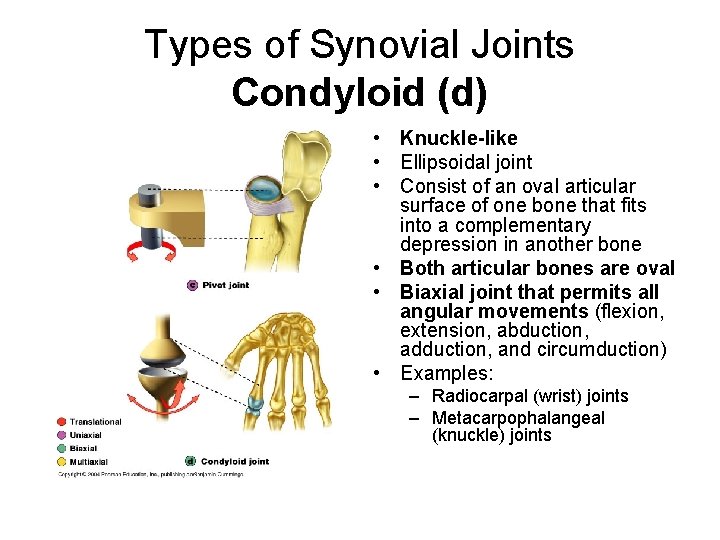
Types of Synovial Joints Condyloid (d) • Knuckle-like • Ellipsoidal joint • Consist of an oval articular surface of one bone that fits into a complementary depression in another bone • Both articular bones are oval • Biaxial joint that permits all angular movements (flexion, extension, abduction, adduction, and circumduction) • Examples: – Radiocarpal (wrist) joints – Metacarpophalangeal (knuckle) joints
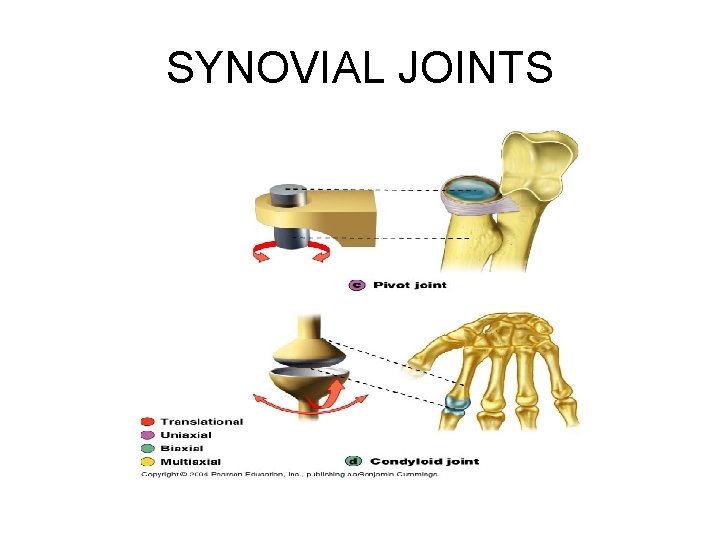
SYNOVIAL JOINTS
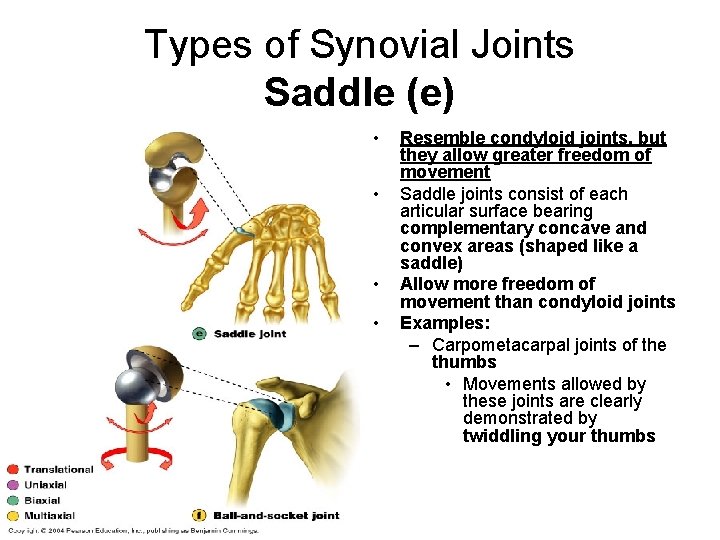
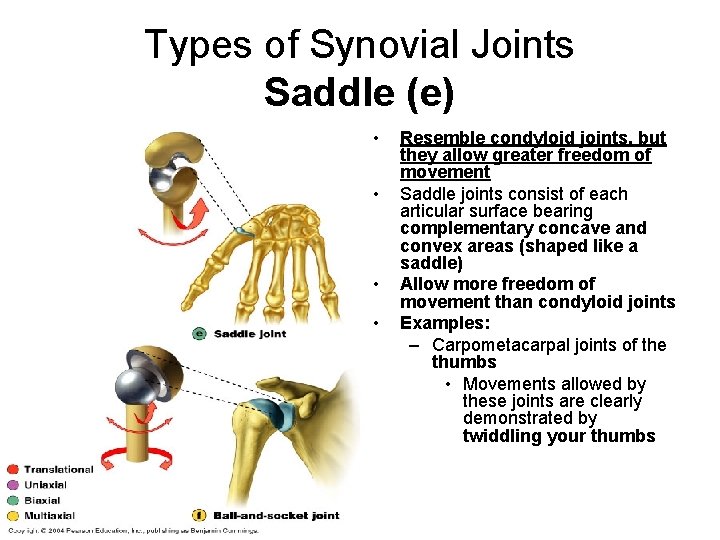
Types of Synovial Joints Saddle (e) • • Resemble condyloid joints, but they allow greater freedom of movement Saddle joints consist of each articular surface bearing complementary concave and convex areas (shaped like a saddle) Allow more freedom of movement than condyloid joints Examples: – Carpometacarpal joints of the thumbs • Movements allowed by these joints are clearly demonstrated by twiddling your thumbs
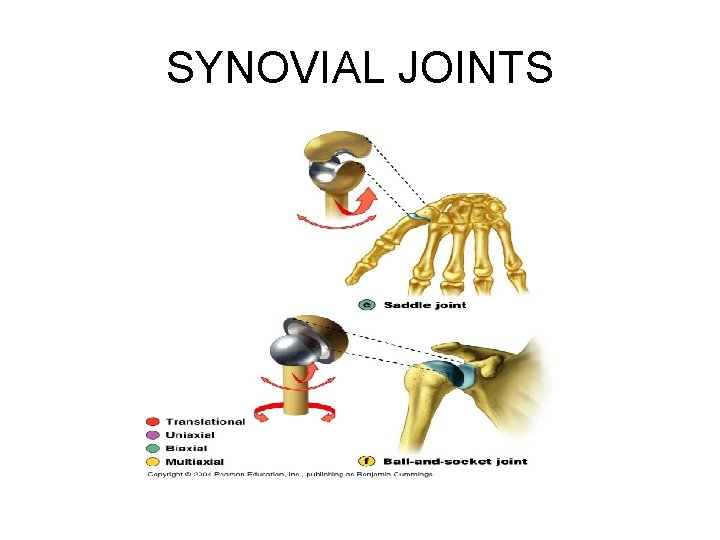
SYNOVIAL JOINTS
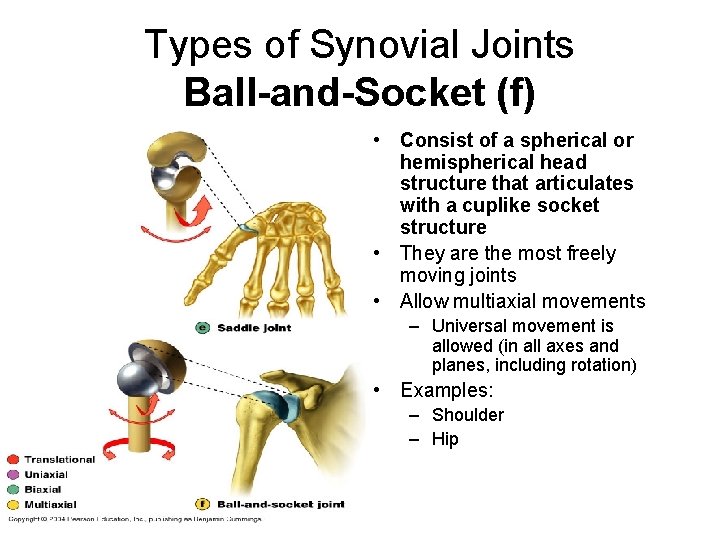
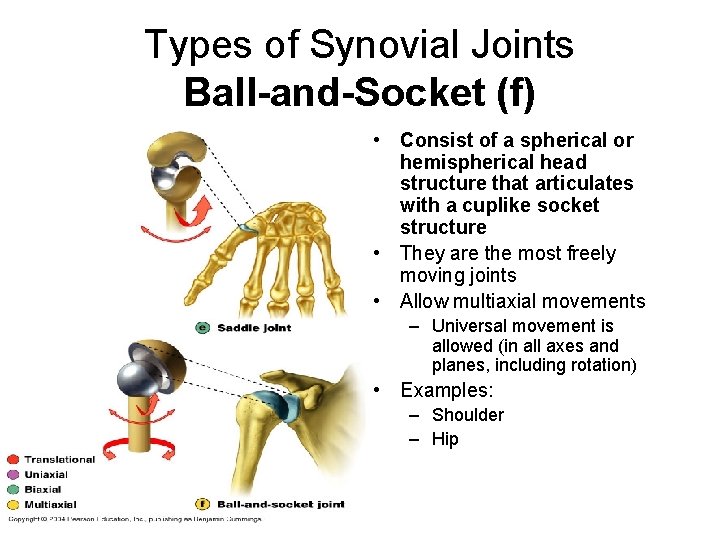
Types of Synovial Joints Ball-and-Socket (f) • Consist of a spherical or hemispherical head structure that articulates with a cuplike socket structure • They are the most freely moving joints • Allow multiaxial movements – Universal movement is allowed (in all axes and planes, including rotation) • Examples: – Shoulder – Hip
SYNOVIAL JOINTS
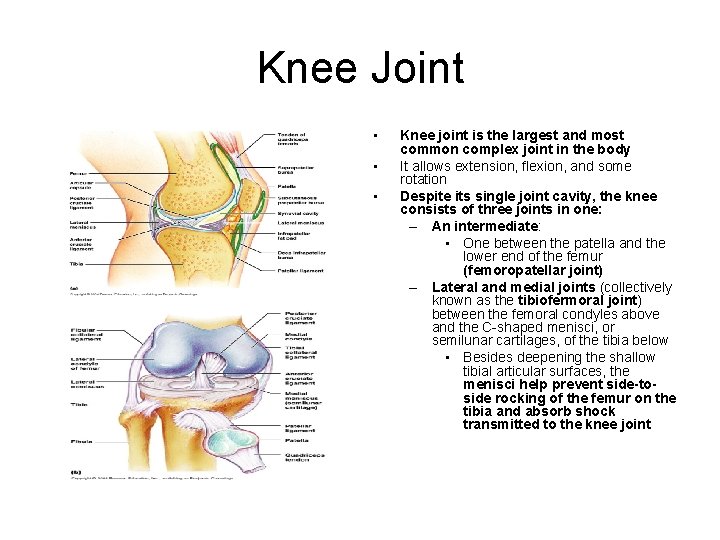
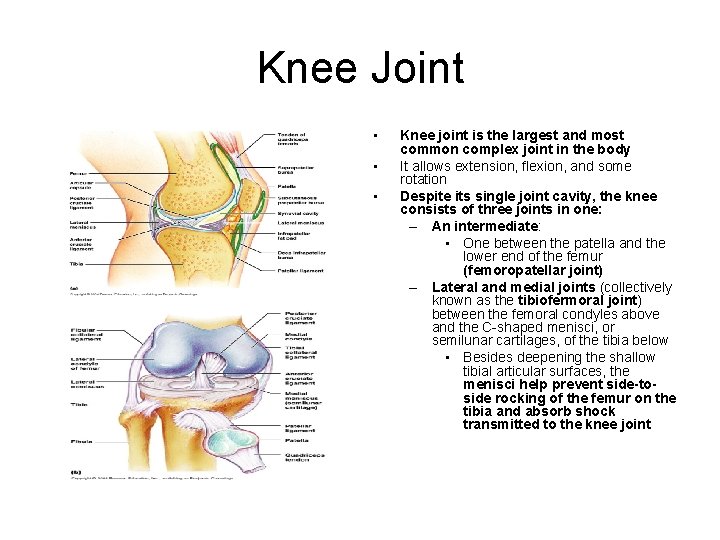
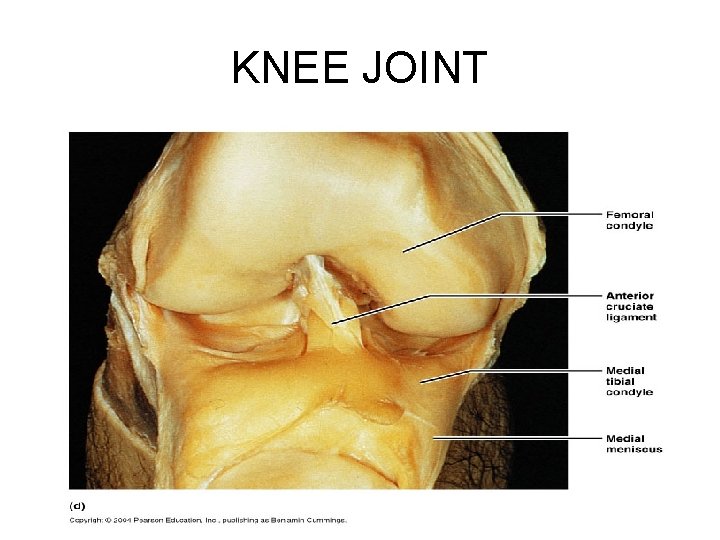
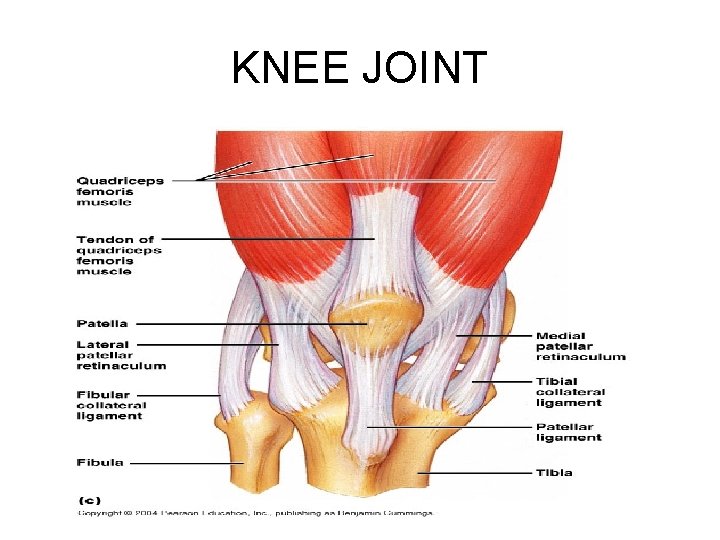
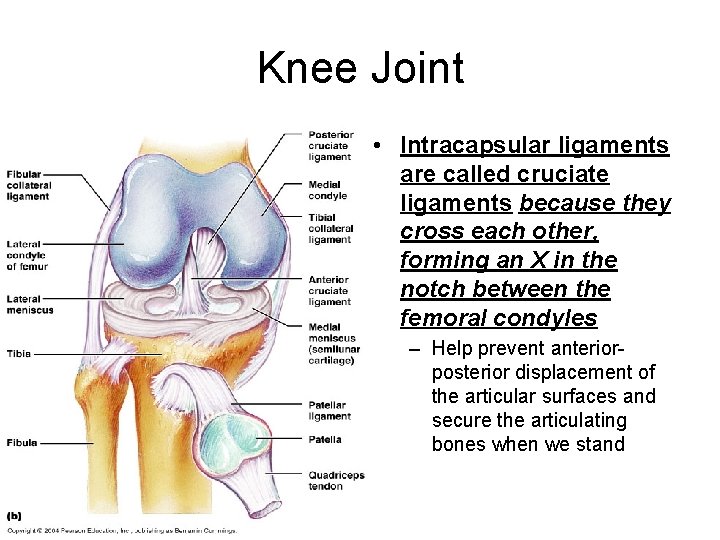
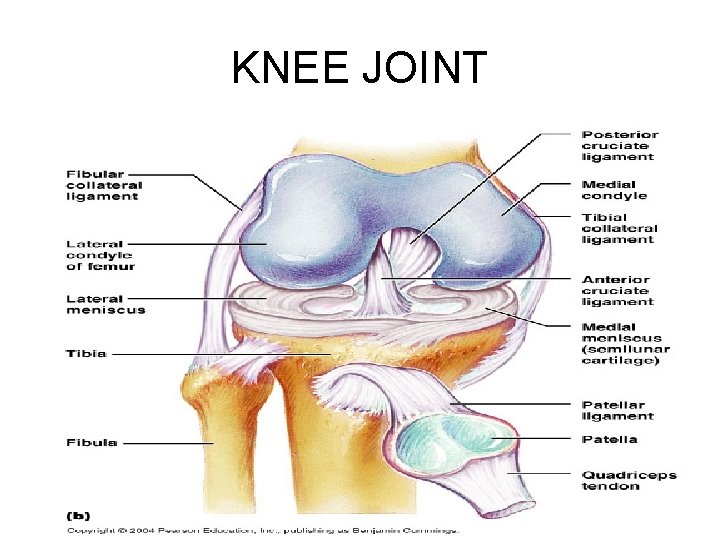
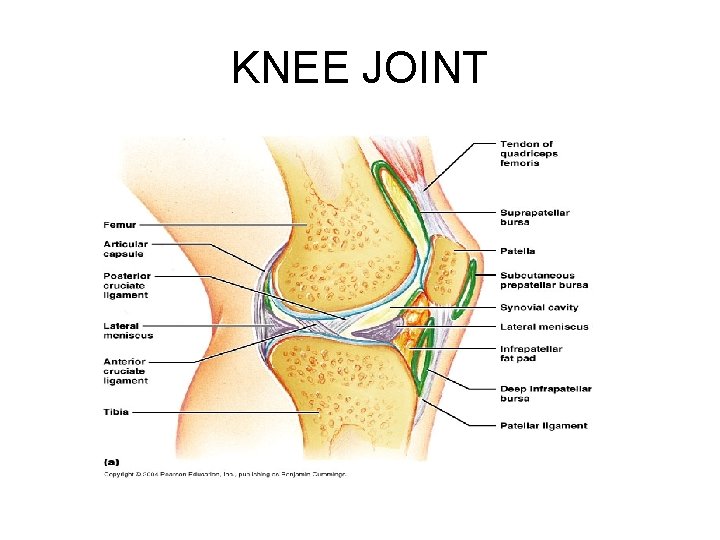
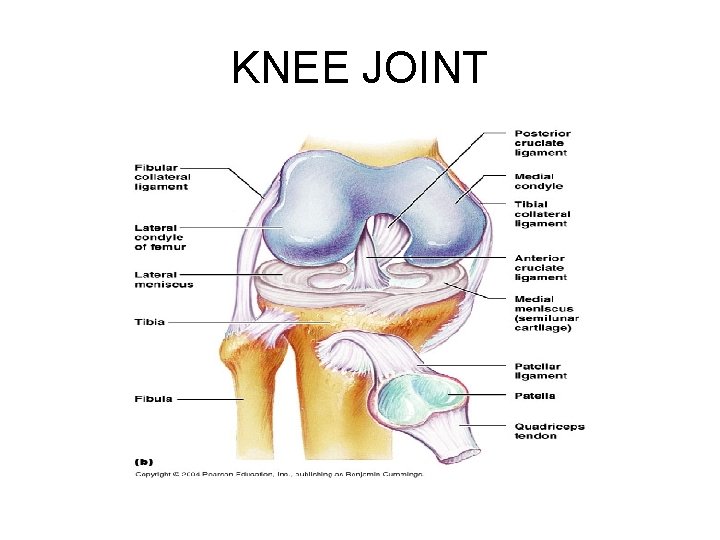
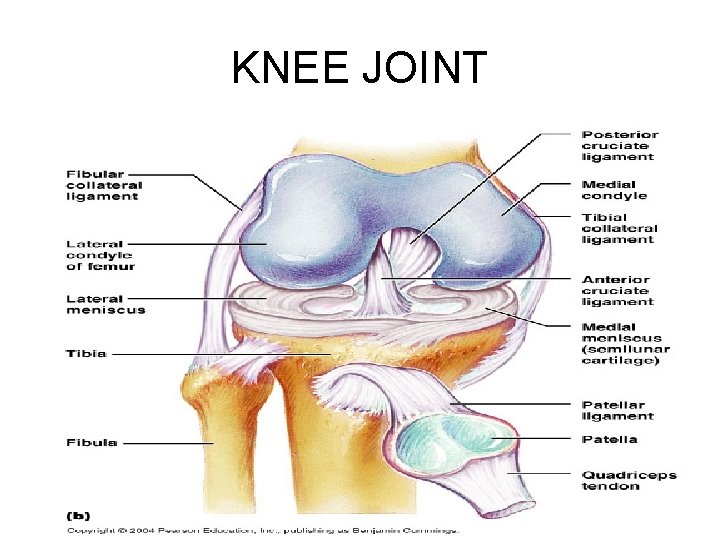
Knee Joint • • • Knee joint is the largest and most common complex joint in the body It allows extension, flexion, and some rotation Despite its single joint cavity, the knee consists of three joints in one: – An intermediate: • One between the patella and the lower end of the femur (femoropatellar joint) – Lateral and medial joints (collectively known as the tibiofermoral joint) between the femoral condyles above and the C-shaped menisci, or semilunar cartilages, of the tibia below • Besides deepening the shallow tibial articular surfaces, the menisci help prevent side-toside rocking of the femur on the tibia and absorb shock transmitted to the knee joint
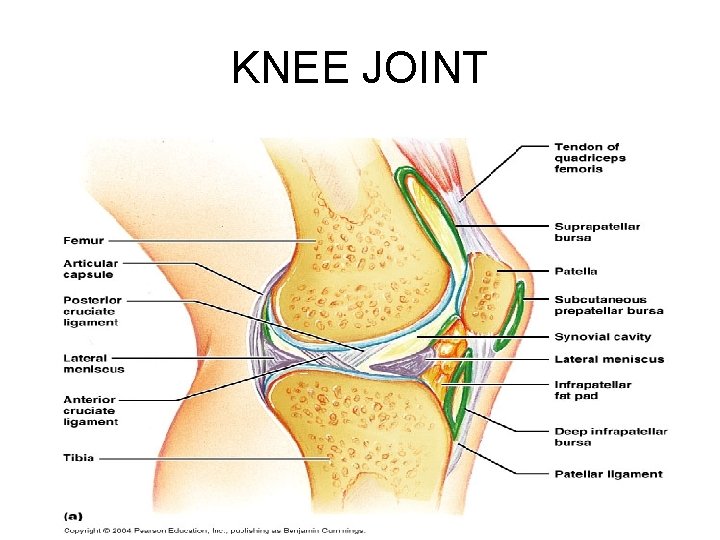
KNEE JOINT
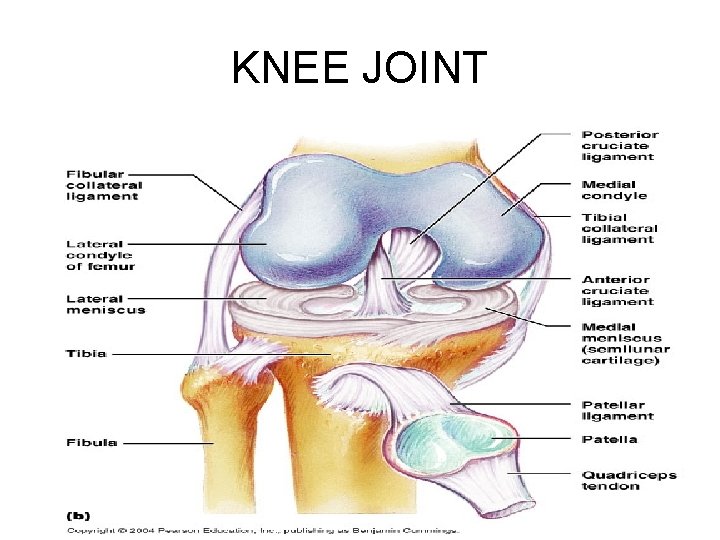
KNEE JOINT
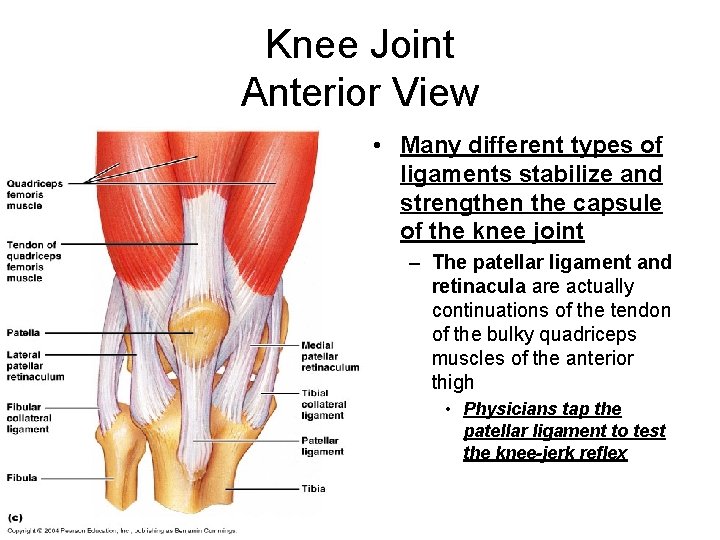
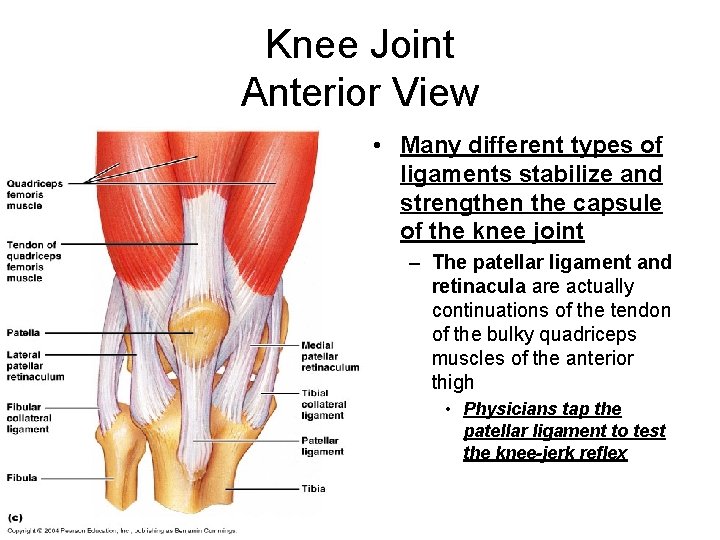
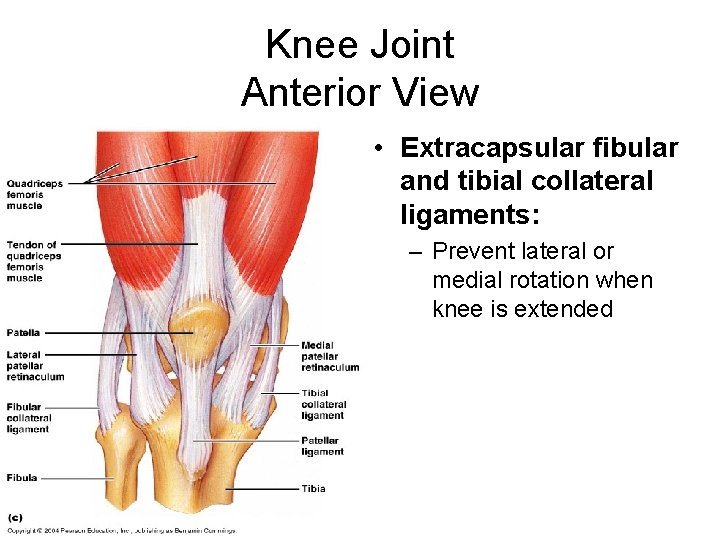
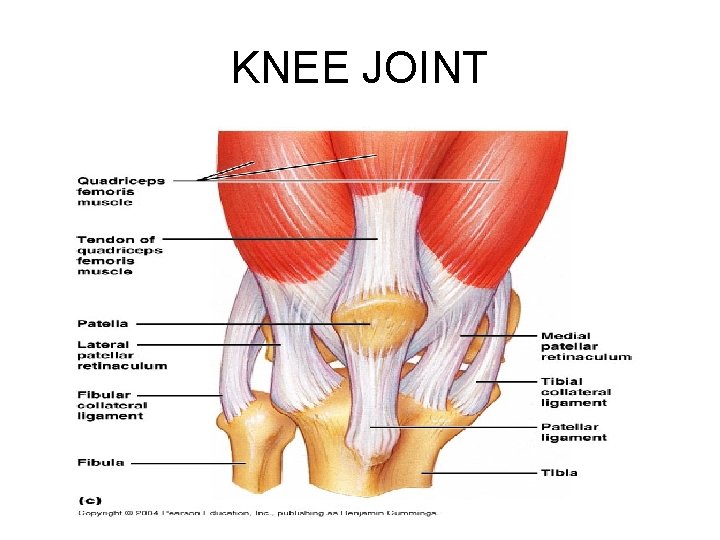
Knee Joint Anterior View • Many different types of ligaments stabilize and strengthen the capsule of the knee joint – The patellar ligament and retinacula are actually continuations of the tendon of the bulky quadriceps muscles of the anterior thigh • Physicians tap the patellar ligament to test the knee-jerk reflex
KNEE JOINT
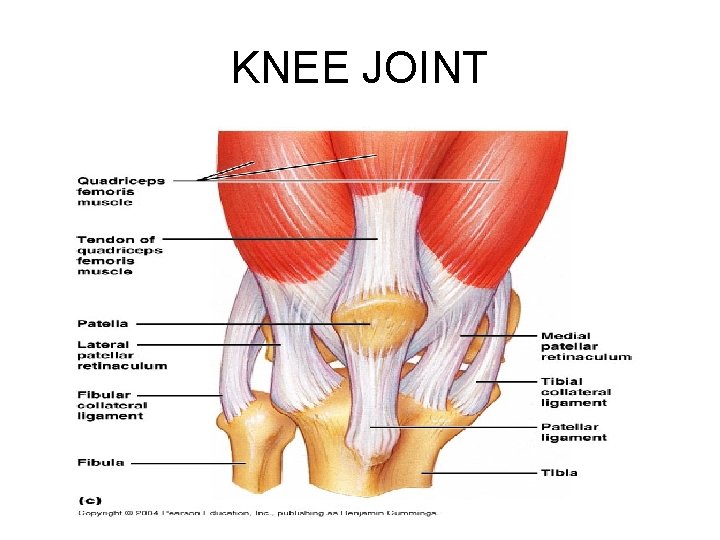
KNEE JOINT
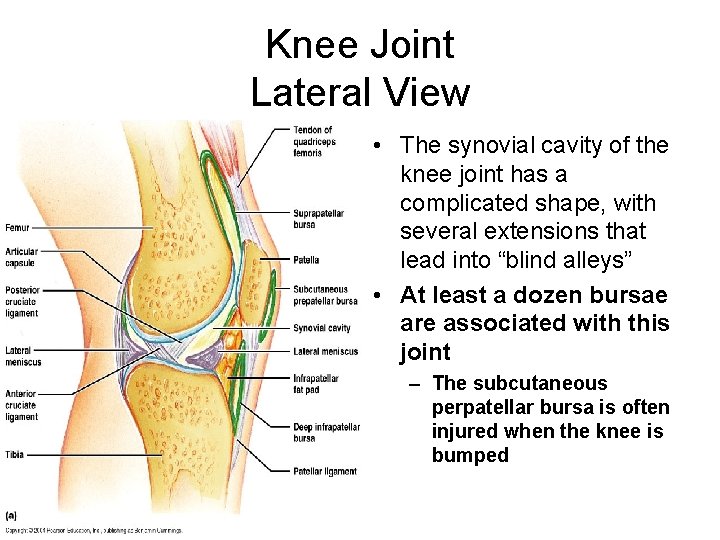
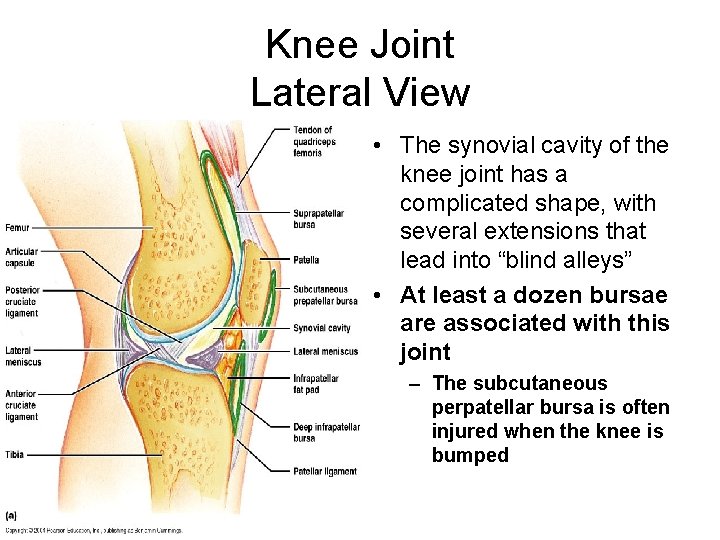
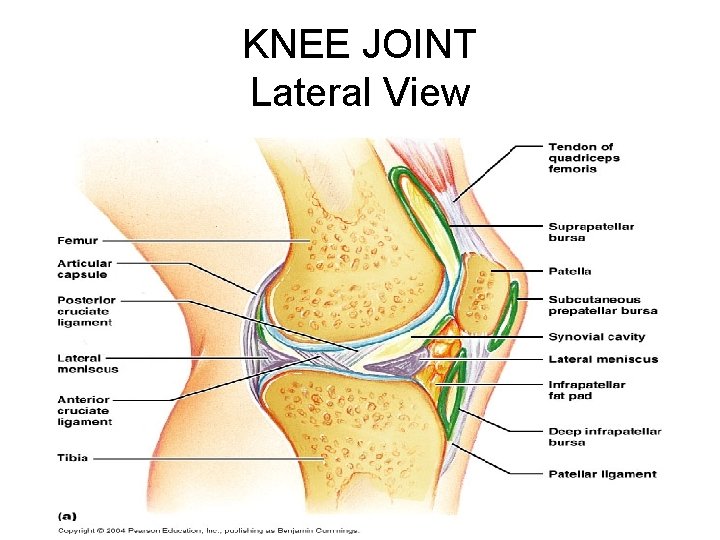
Knee Joint Lateral View • The synovial cavity of the knee joint has a complicated shape, with several extensions that lead into “blind alleys” • At least a dozen bursae are associated with this joint – The subcutaneous perpatellar bursa is often injured when the knee is bumped
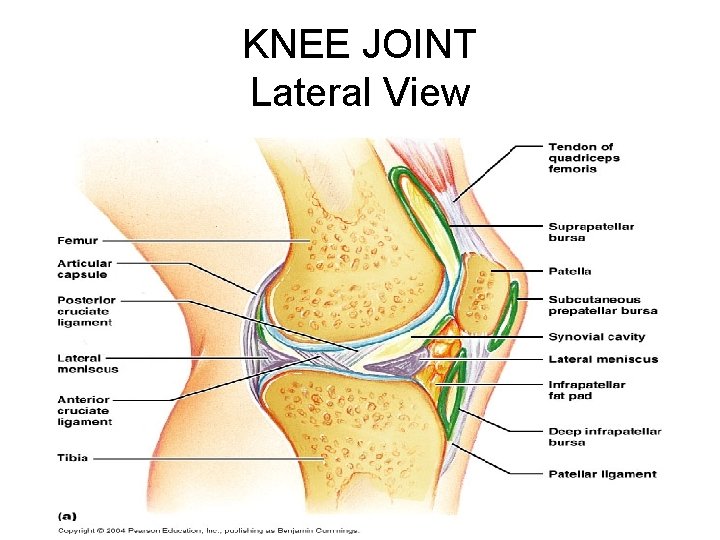
KNEE JOINT Lateral View
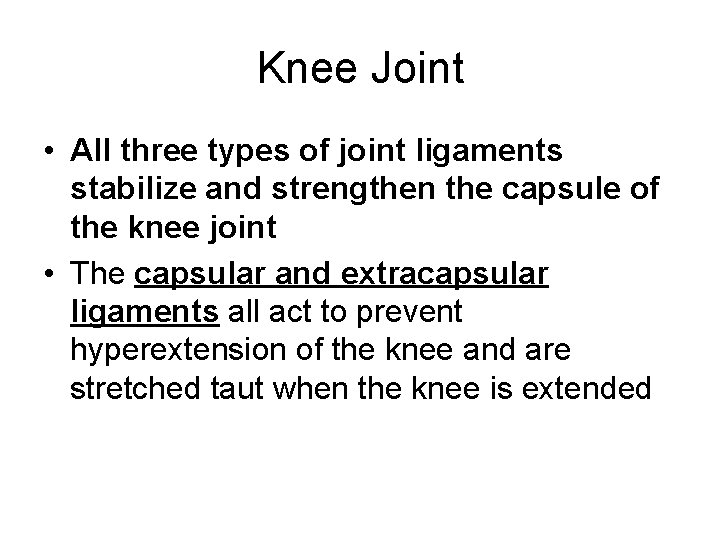
Knee Joint • All three types of joint ligaments stabilize and strengthen the capsule of the knee joint • The capsular and extracapsular ligaments all act to prevent hyperextension of the knee and are stretched taut when the knee is extended
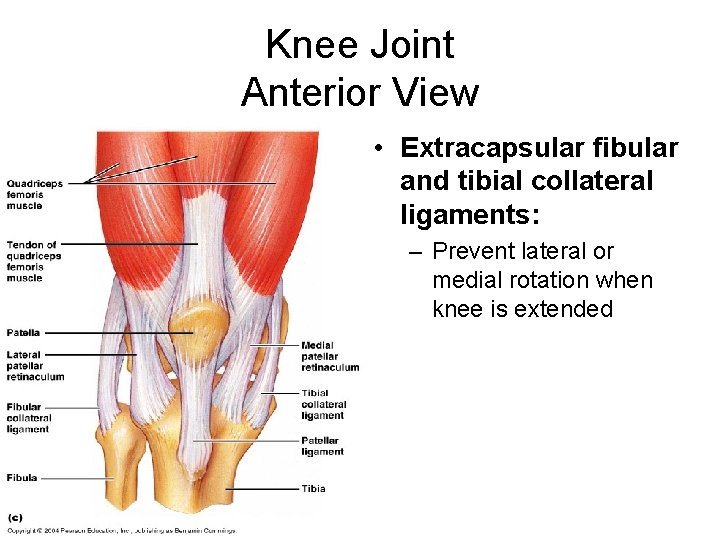
Knee Joint Anterior View • Extracapsular fibular and tibial collateral ligaments: – Prevent lateral or medial rotation when knee is extended
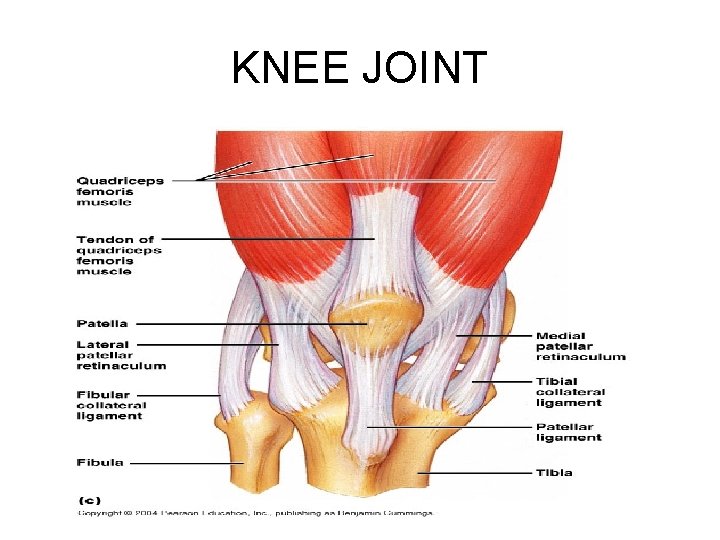
KNEE JOINT
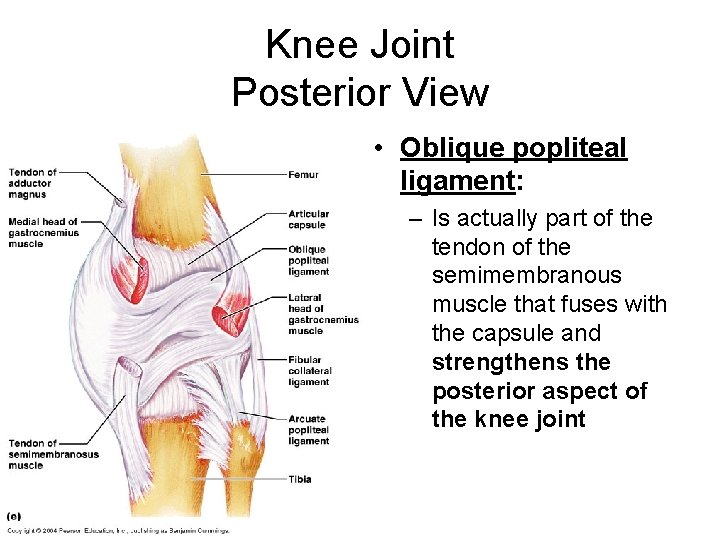
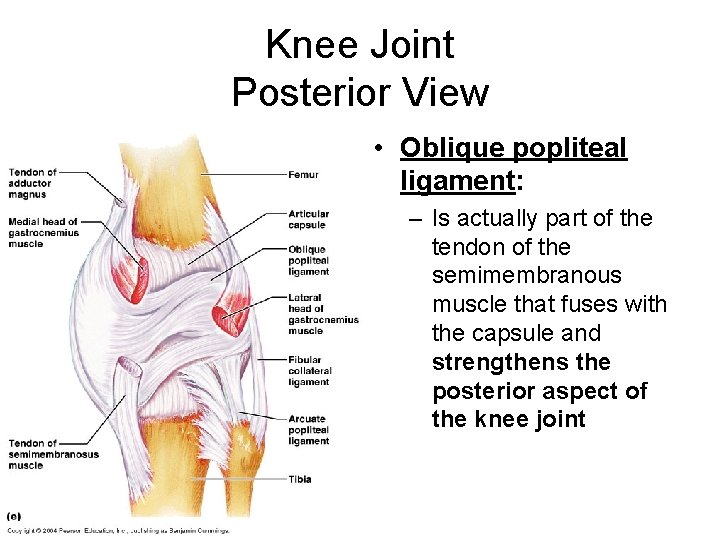
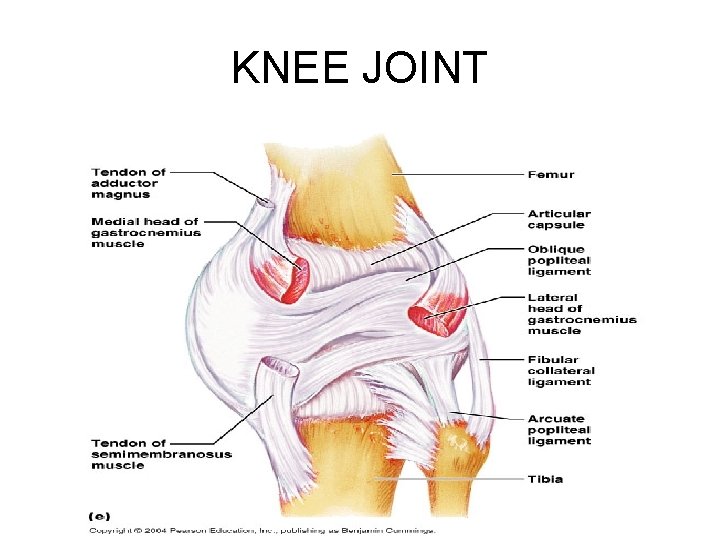
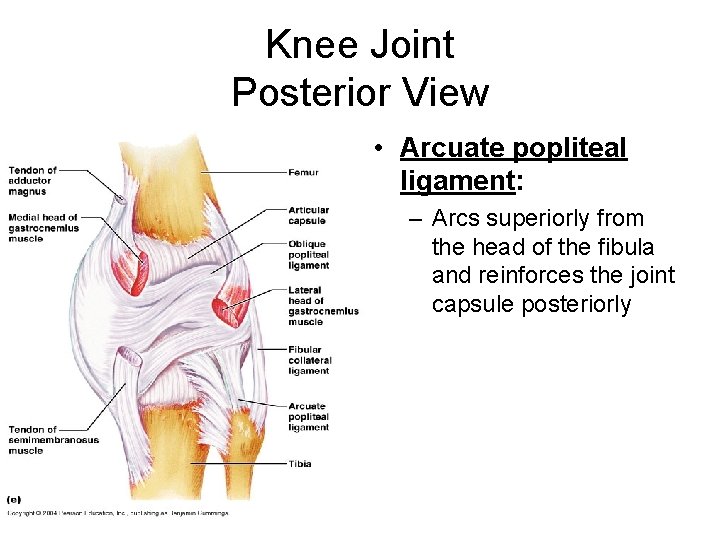
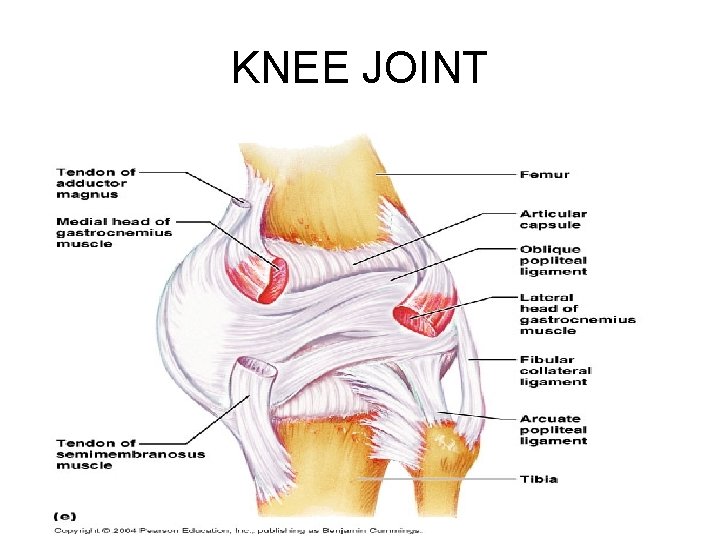
Knee Joint Posterior View • Oblique popliteal ligament: – Is actually part of the tendon of the semimembranous muscle that fuses with the capsule and strengthens the posterior aspect of the knee joint
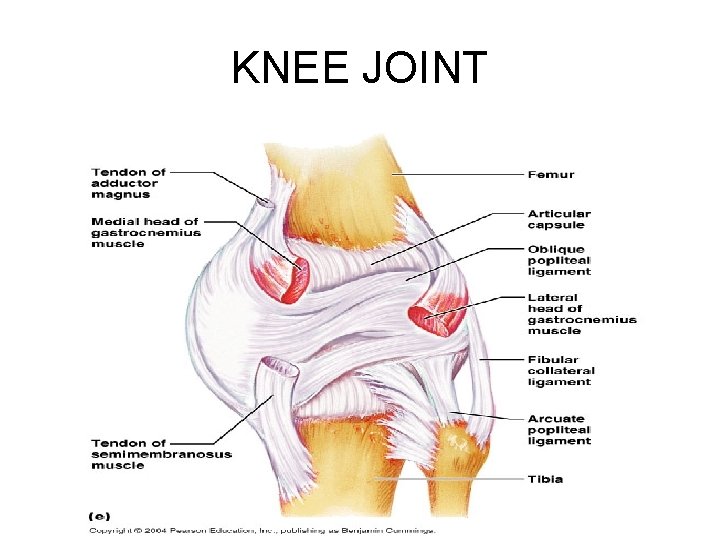
KNEE JOINT
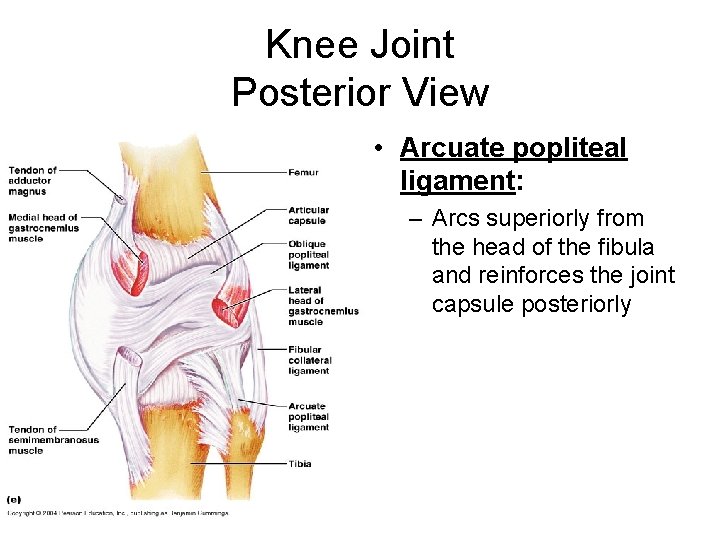
Knee Joint Posterior View • Arcuate popliteal ligament: – Arcs superiorly from the head of the fibula and reinforces the joint capsule posteriorly
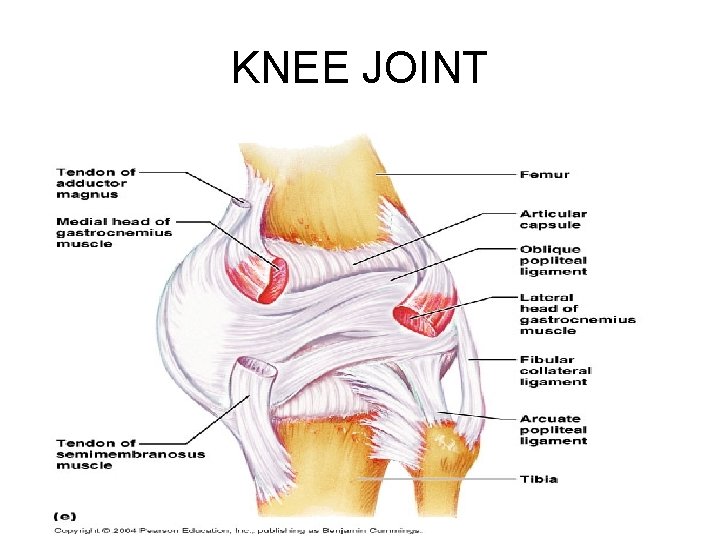
KNEE JOINT
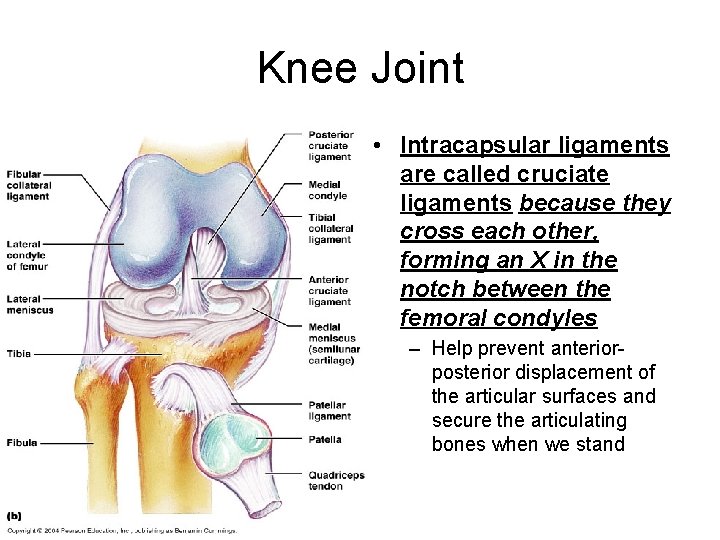
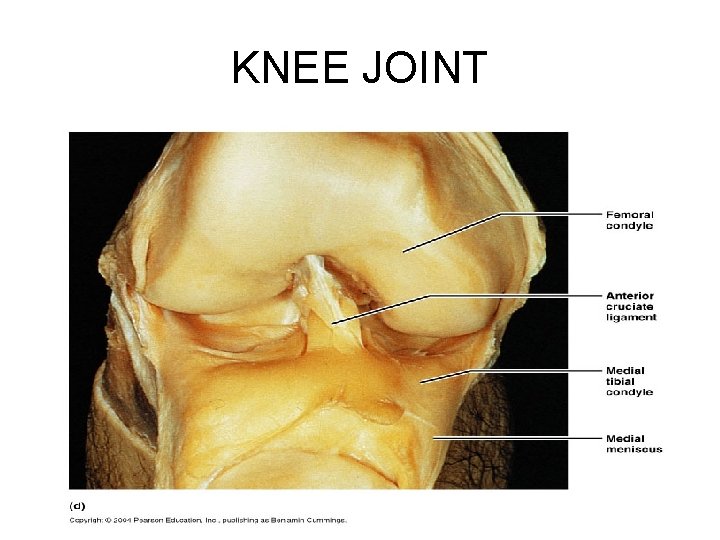
Knee Joint • Intracapsular ligaments are called cruciate ligaments because they cross each other, forming an X in the notch between the femoral condyles – Help prevent anteriorposterior displacement of the articular surfaces and secure the articulating bones when we stand
KNEE JOINT
HOMEOSTATIC IMBALANCE • Of all body joints, the knees are most susceptible to sports injuries because of their high reliance on nonarticular factors for stability and the fact that they carry the body’s weight • The knee can absorb a vertical force equal to nearly seven times body weight – However, it is very vulnerable to horizontal blows, such as those that occur during blocking and tackling in football
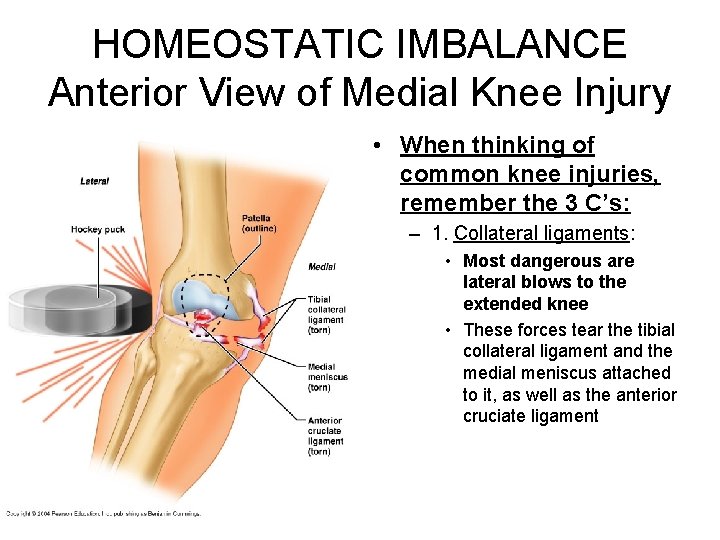
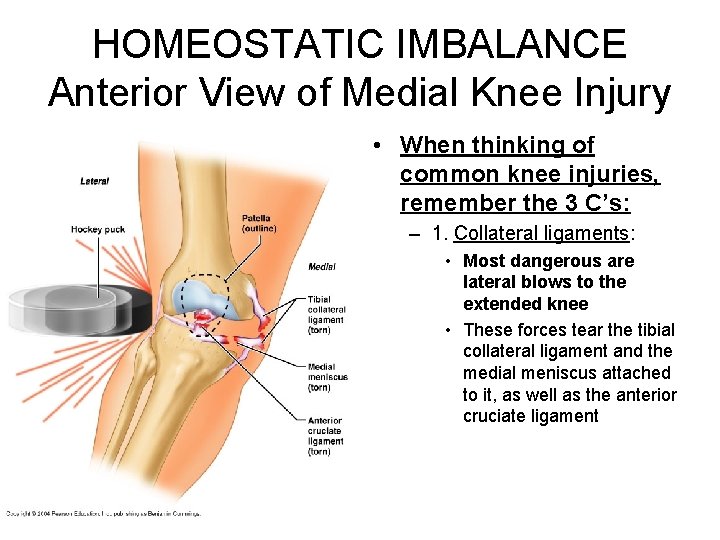
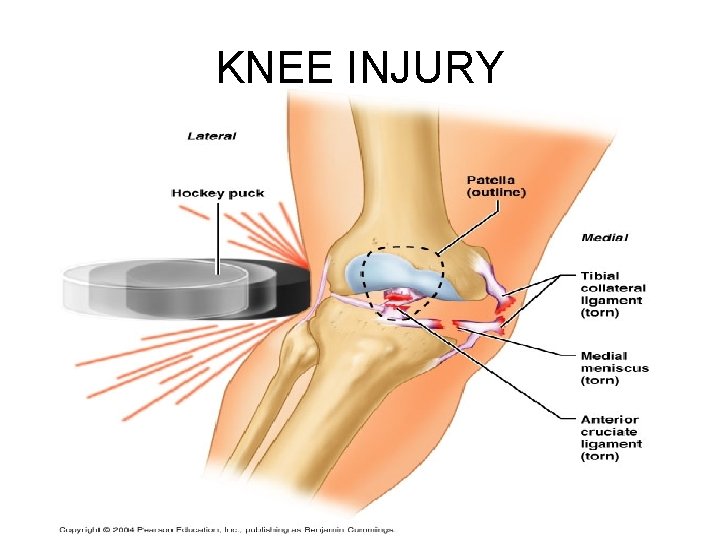
HOMEOSTATIC IMBALANCE Anterior View of Medial Knee Injury • When thinking of common knee injuries, remember the 3 C’s: – 1. Collateral ligaments: • Most dangerous are lateral blows to the extended knee • These forces tear the tibial collateral ligament and the medial meniscus attached to it, as well as the anterior cruciate ligament
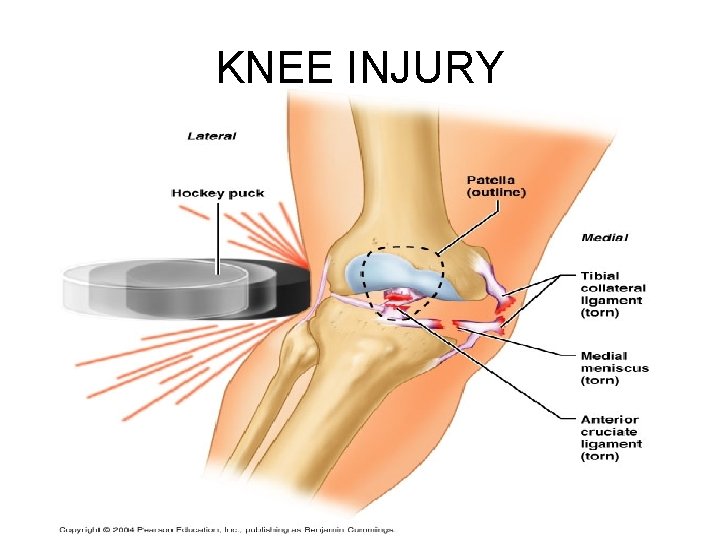
KNEE INJURY
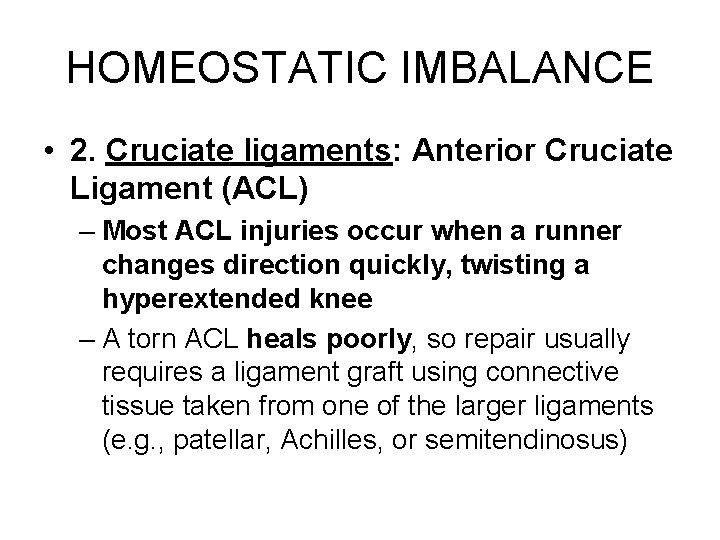
HOMEOSTATIC IMBALANCE • 2. Cruciate ligaments: Anterior Cruciate Ligament (ACL) – Most ACL injuries occur when a runner changes direction quickly, twisting a hyperextended knee – A torn ACL heals poorly, so repair usually requires a ligament graft using connective tissue taken from one of the larger ligaments (e. g. , patellar, Achilles, or semitendinosus)
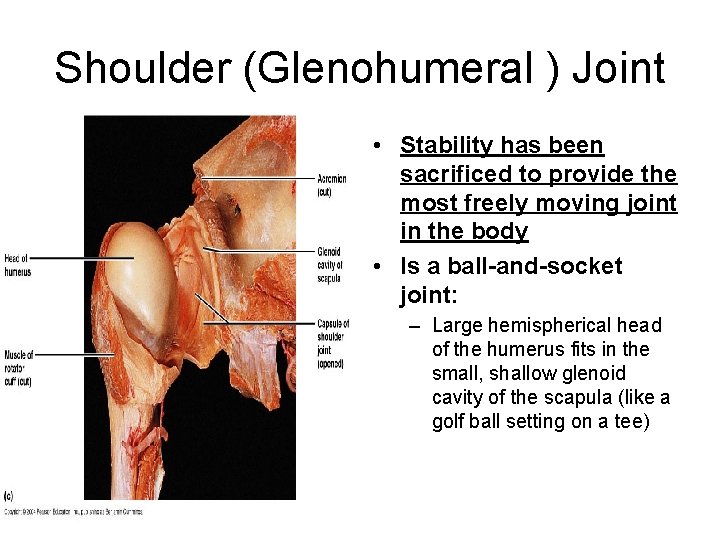
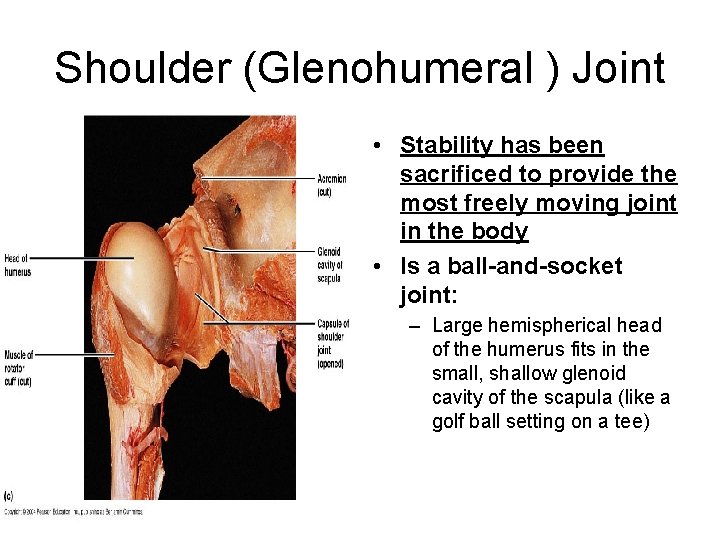
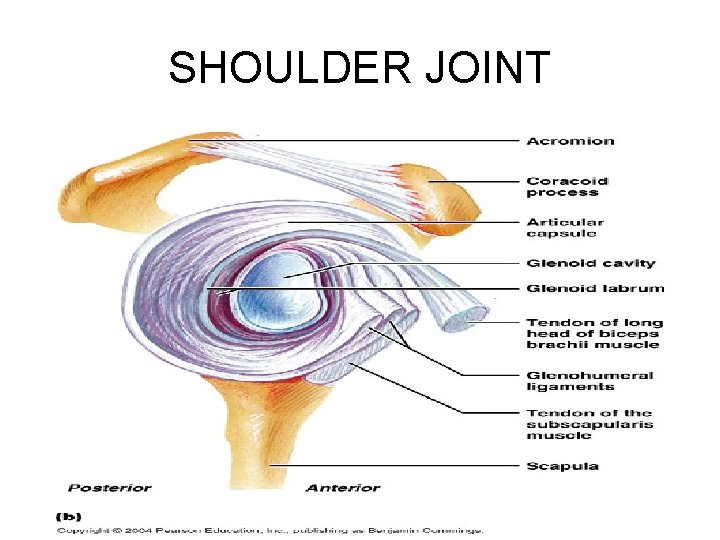
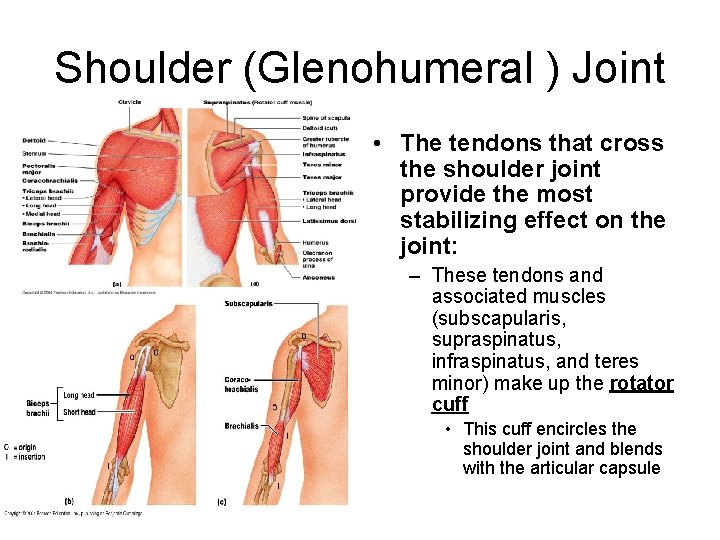
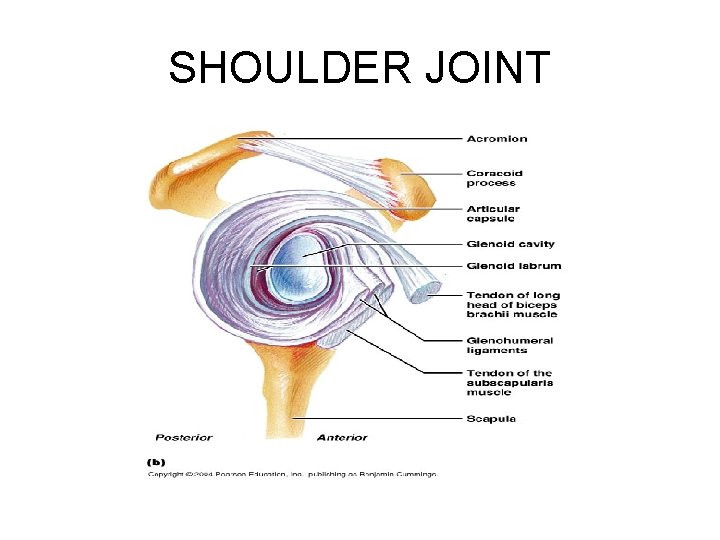
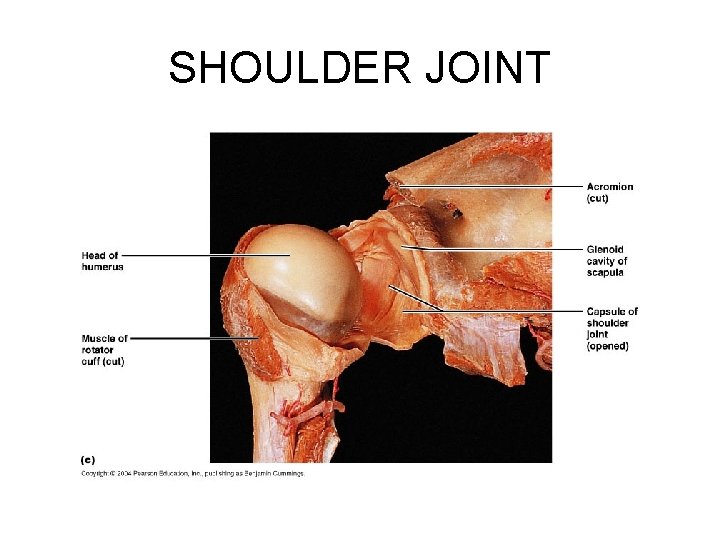
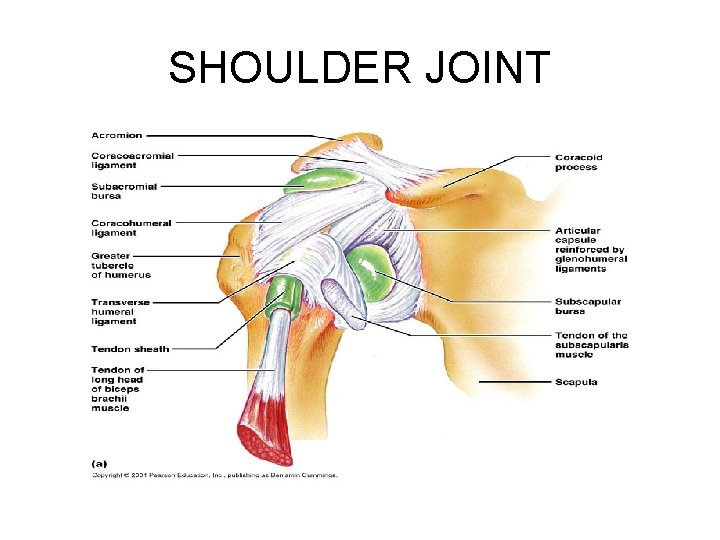
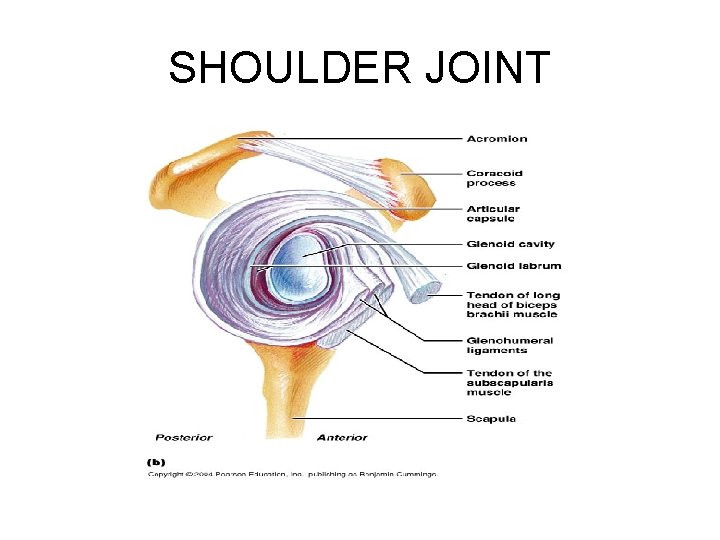
Shoulder (Glenohumeral ) Joint • Stability has been sacrificed to provide the most freely moving joint in the body • Is a ball-and-socket joint: – Large hemispherical head of the humerus fits in the small, shallow glenoid cavity of the scapula (like a golf ball setting on a tee)
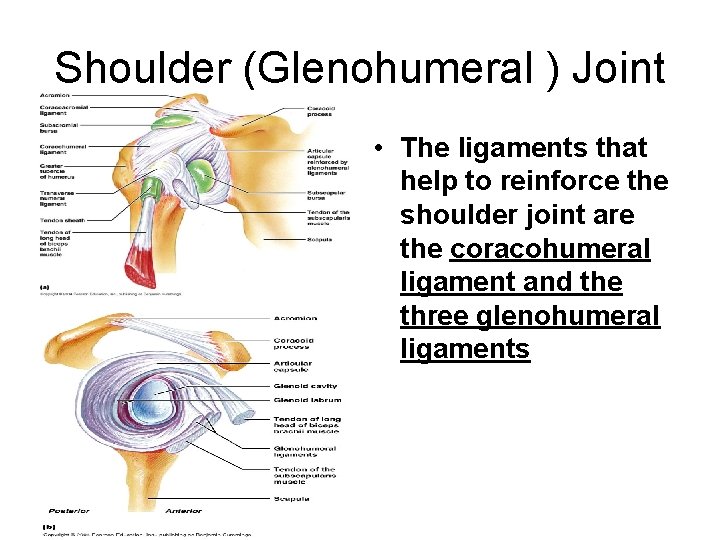
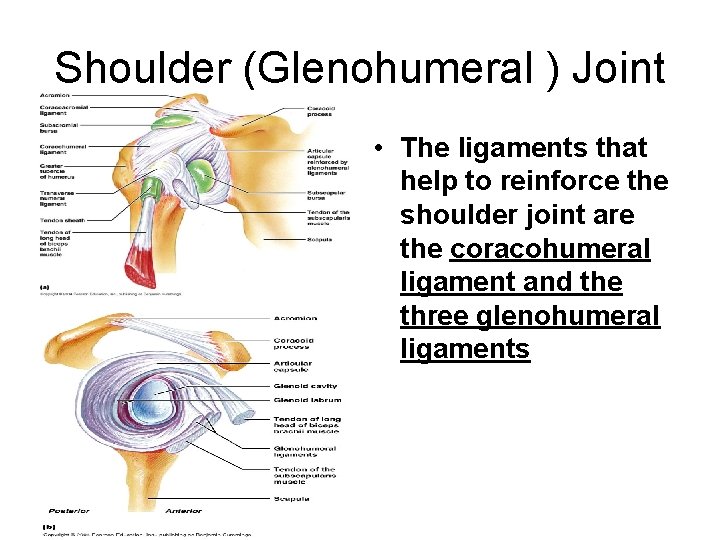
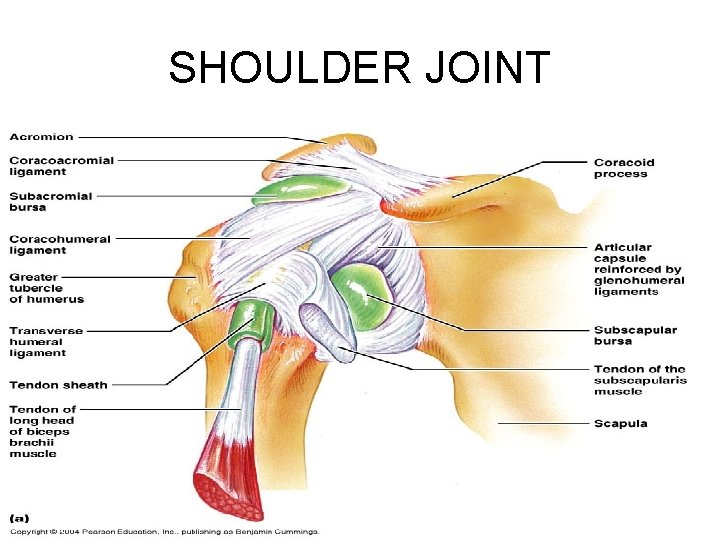
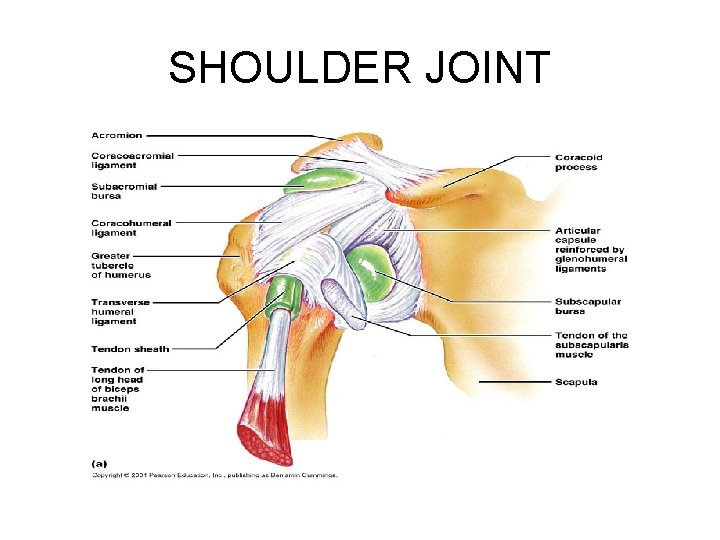
Shoulder (Glenohumeral ) Joint • The ligaments that help to reinforce the shoulder joint are the coracohumeral ligament and the three glenohumeral ligaments
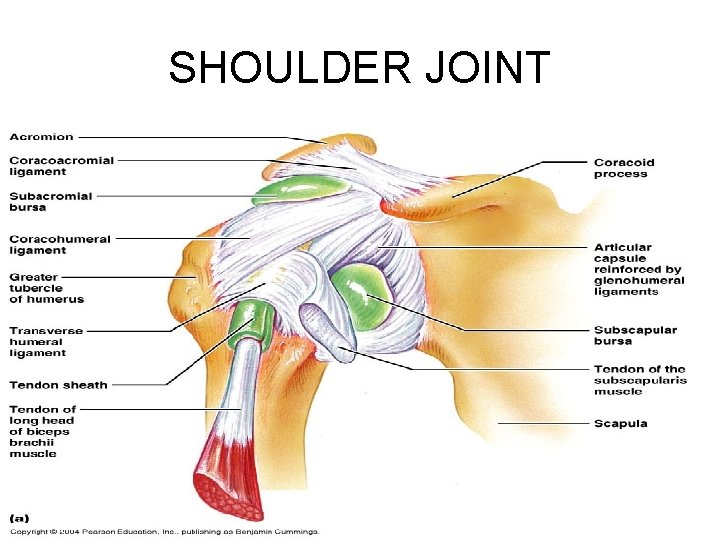
SHOULDER JOINT
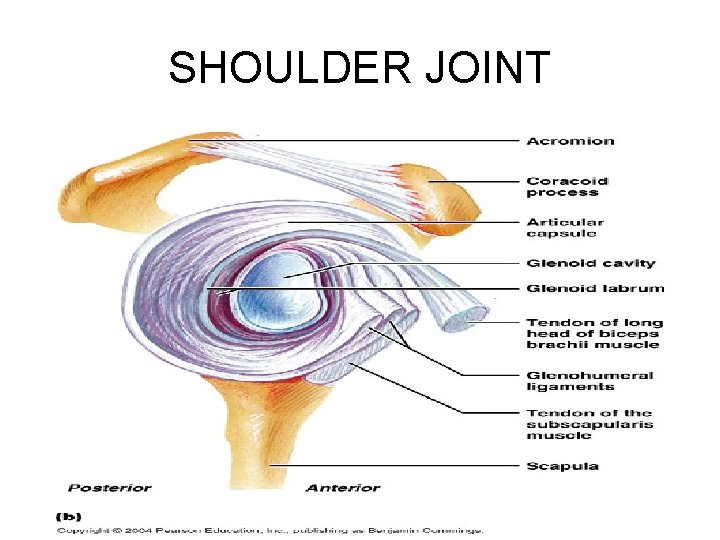
SHOULDER JOINT
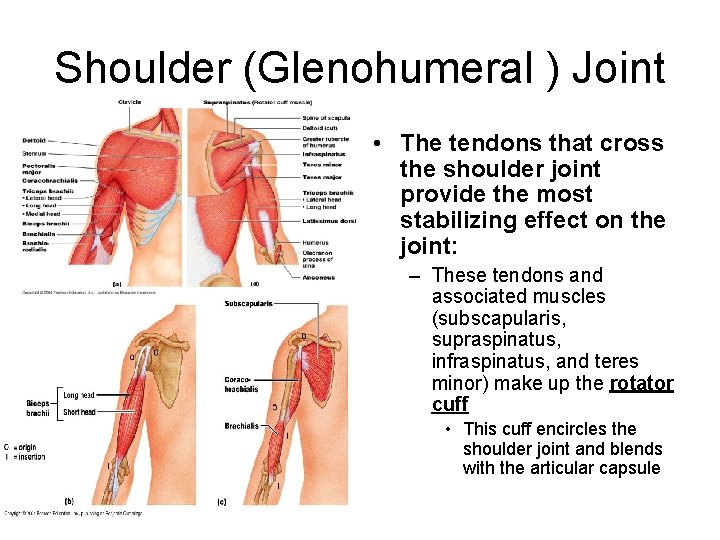
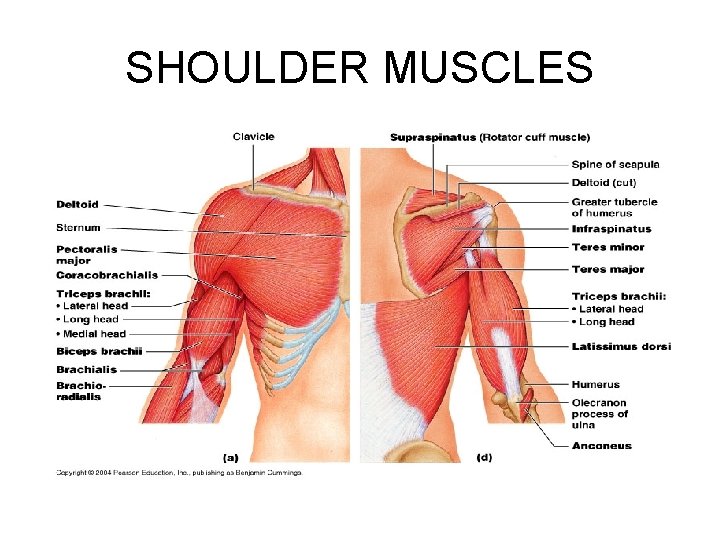
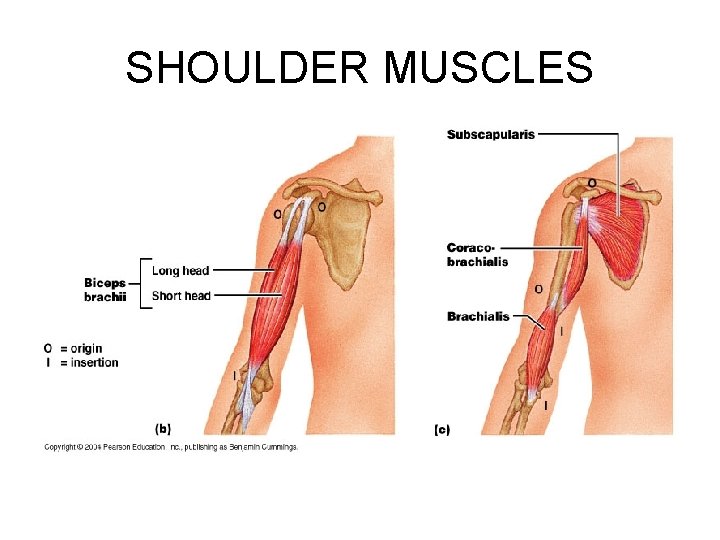
Shoulder (Glenohumeral ) Joint • The tendons that cross the shoulder joint provide the most stabilizing effect on the joint: – These tendons and associated muscles (subscapularis, supraspinatus, infraspinatus, and teres minor) make up the rotator cuff • This cuff encircles the shoulder joint and blends with the articular capsule
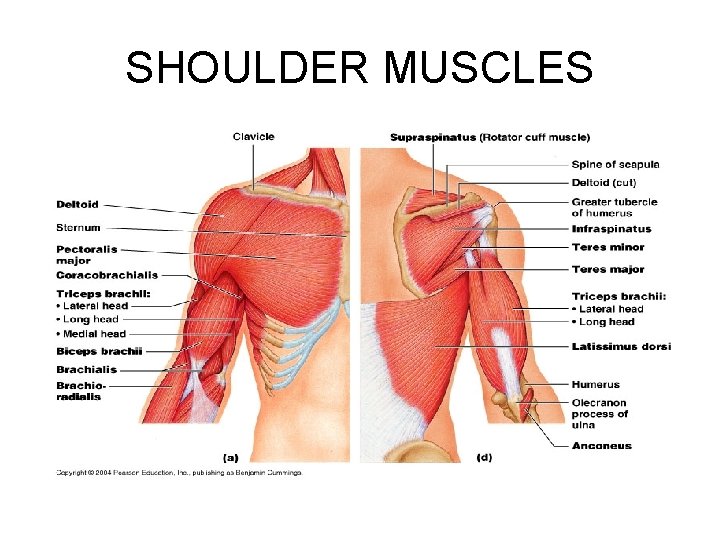
SHOULDER MUSCLES
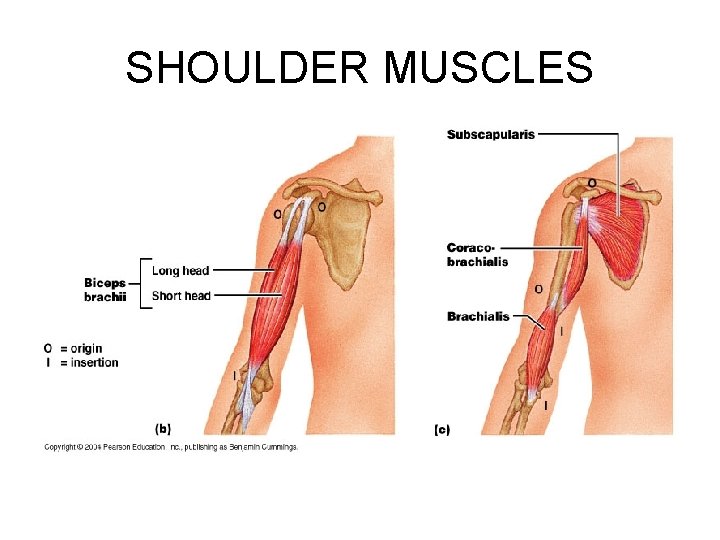
SHOULDER MUSCLES
SHOULDER JOINT
SHOULDER JOINT
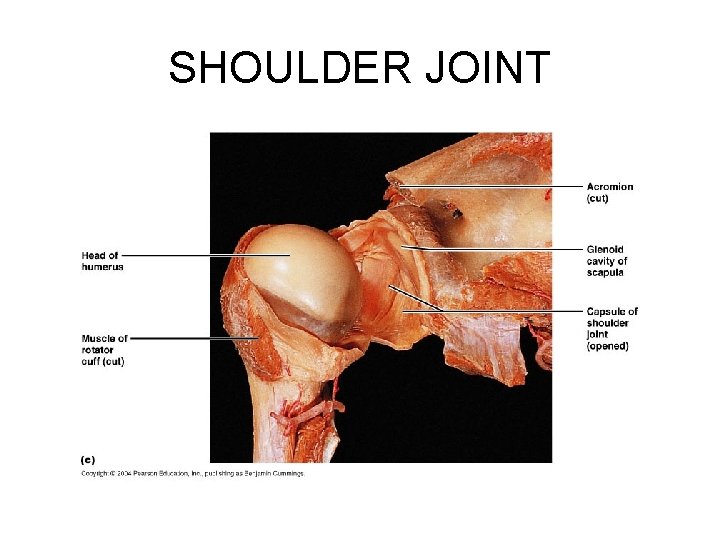
SHOULDER JOINT
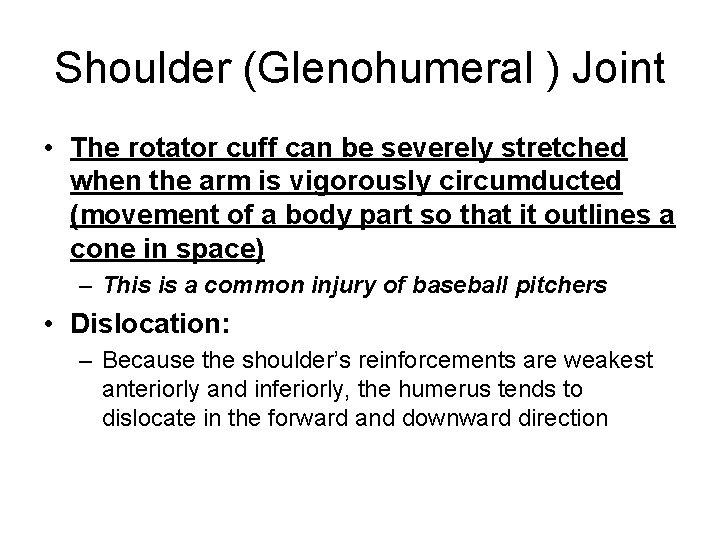
Shoulder (Glenohumeral ) Joint • The rotator cuff can be severely stretched when the arm is vigorously circumducted (movement of a body part so that it outlines a cone in space) – This is a common injury of baseball pitchers • Dislocation: – Because the shoulder’s reinforcements are weakest anteriorly and inferiorly, the humerus tends to dislocate in the forward and downward direction
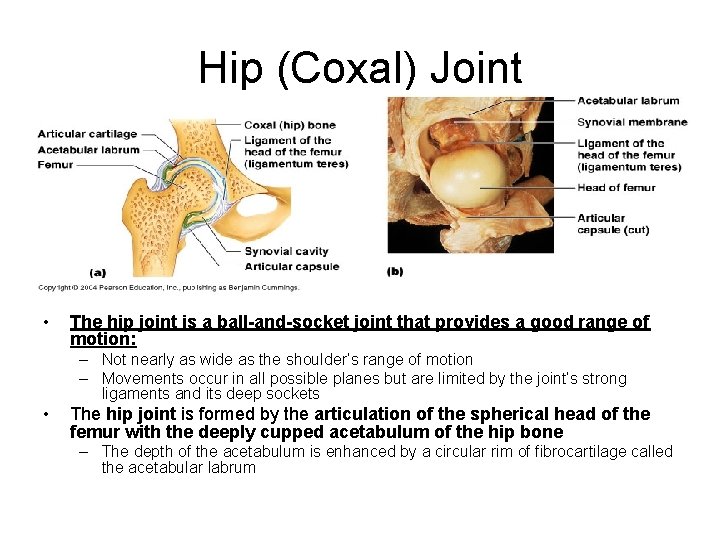
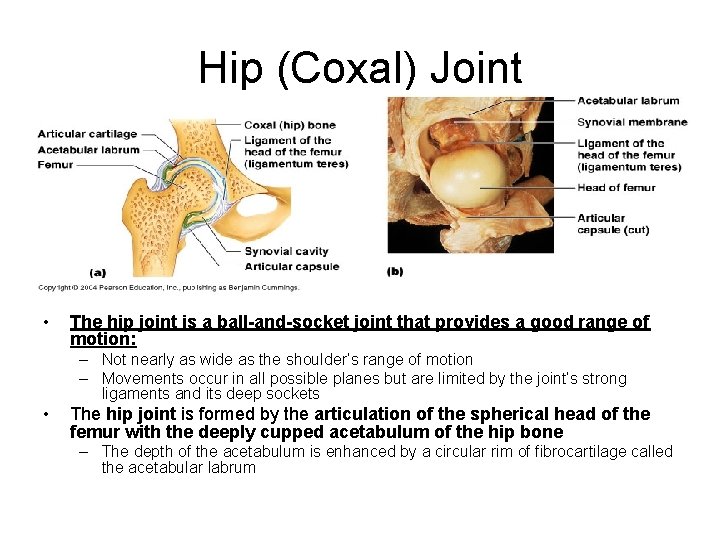
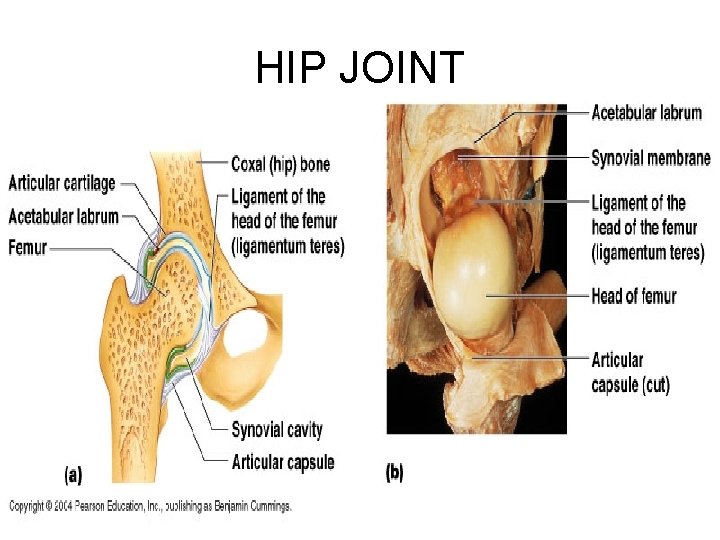
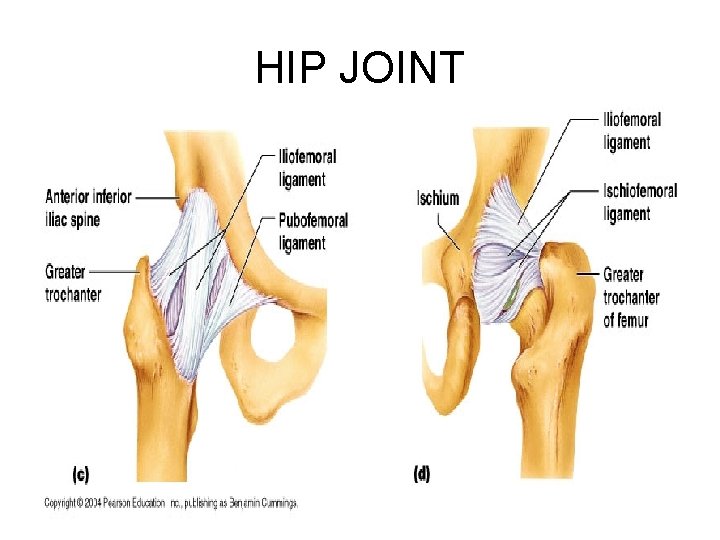
Hip (Coxal) Joint • The hip joint is a ball-and-socket joint that provides a good range of motion: – Not nearly as wide as the shoulder’s range of motion – Movements occur in all possible planes but are limited by the joint’s strong ligaments and its deep sockets • The hip joint is formed by the articulation of the spherical head of the femur with the deeply cupped acetabulum of the hip bone – The depth of the acetabulum is enhanced by a circular rim of fibrocartilage called the acetabular labrum
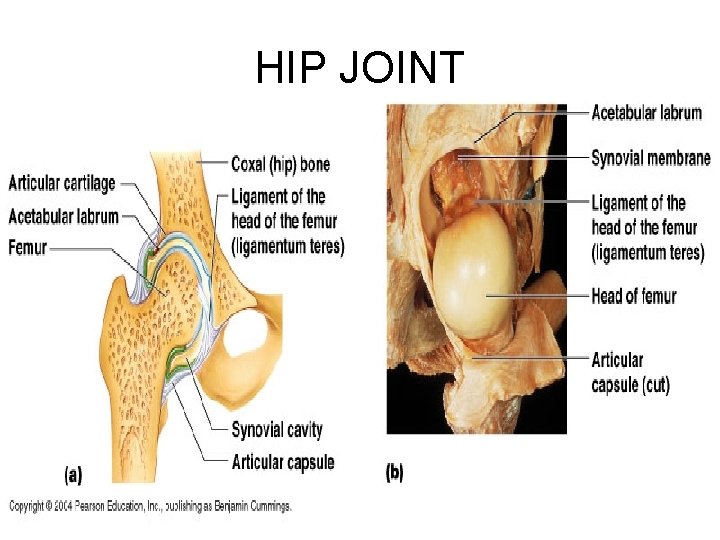
HIP JOINT
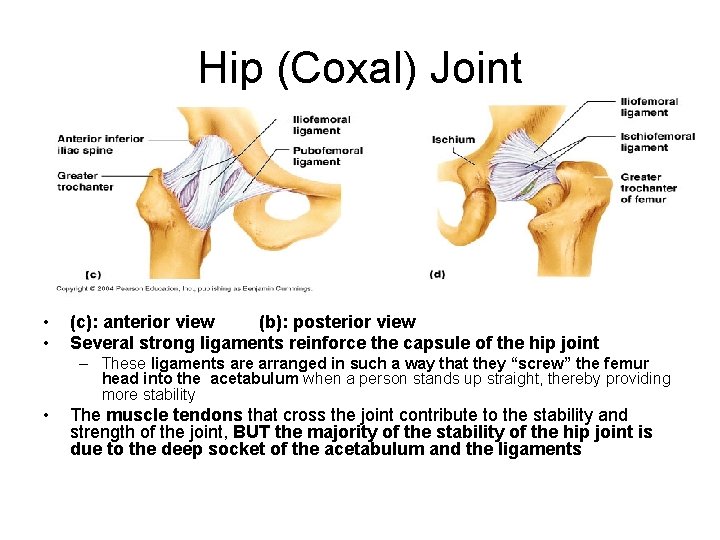
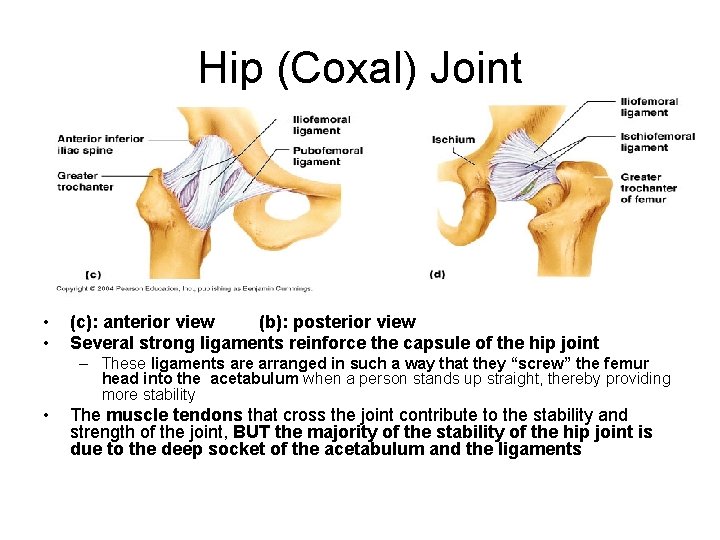
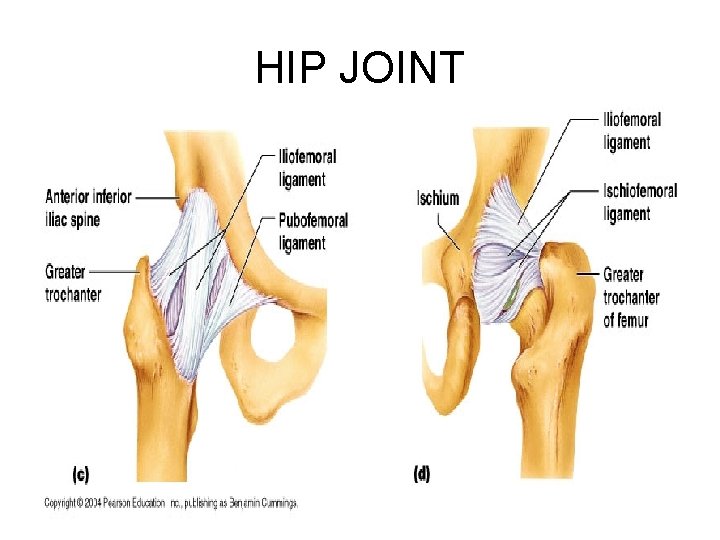
Hip (Coxal) Joint • • (c): anterior view (b): posterior view Several strong ligaments reinforce the capsule of the hip joint – These ligaments are arranged in such a way that they “screw” the femur head into the acetabulum when a person stands up straight, thereby providing more stability • The muscle tendons that cross the joint contribute to the stability and strength of the joint, BUT the majority of the stability of the hip joint is due to the deep socket of the acetabulum and the ligaments
HIP JOINT
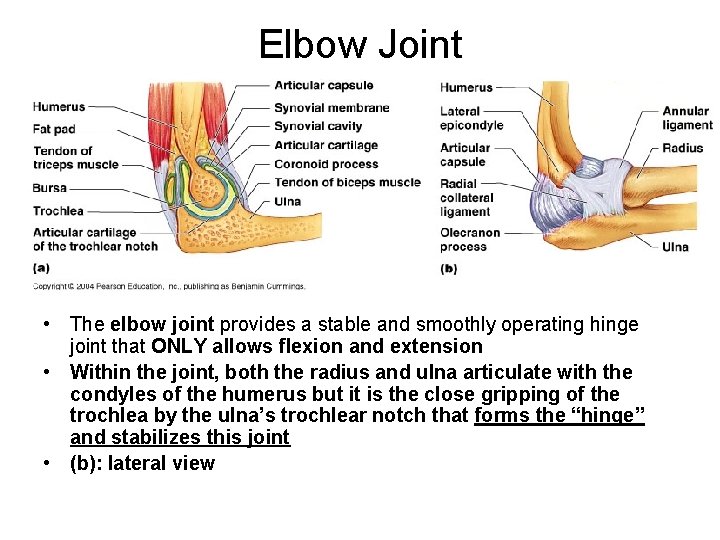
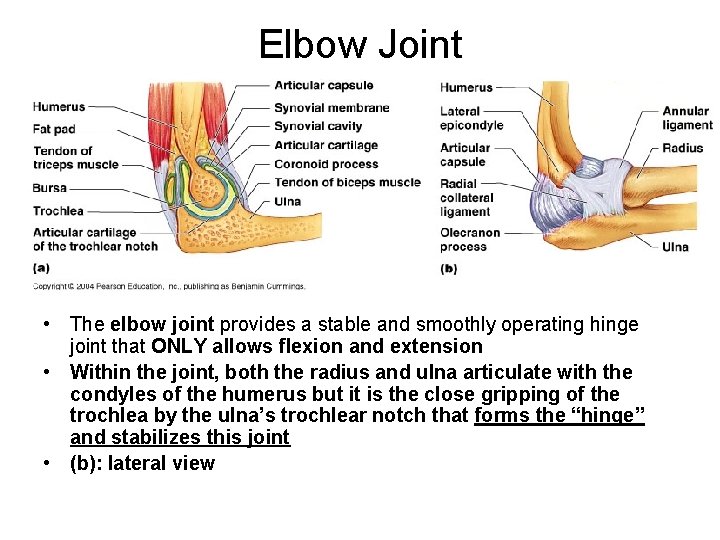
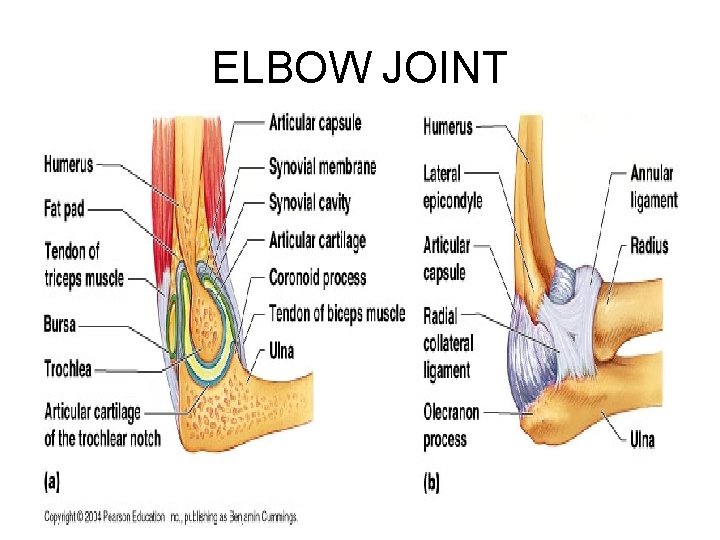
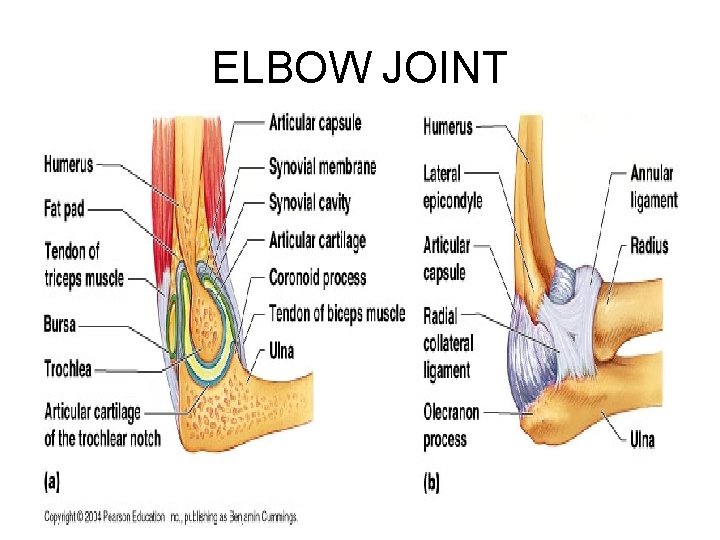
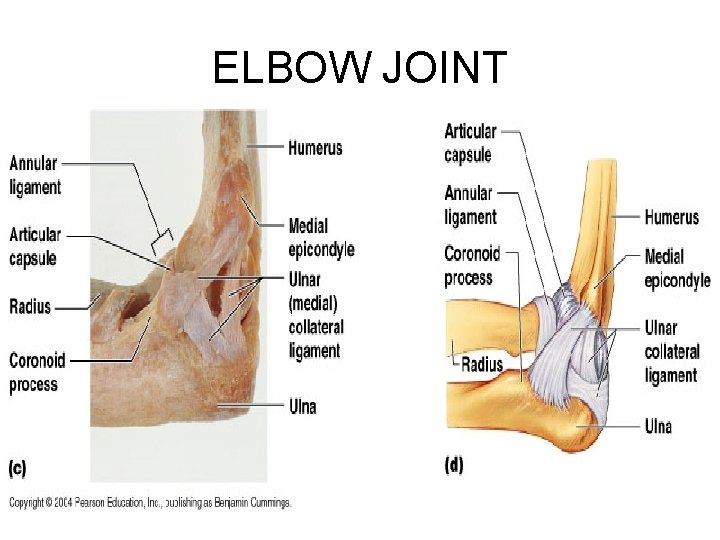
Elbow Joint • The elbow joint provides a stable and smoothly operating hinge joint that ONLY allows flexion and extension • Within the joint, both the radius and ulna articulate with the condyles of the humerus but it is the close gripping of the trochlea by the ulna’s trochlear notch that forms the “hinge” and stabilizes this joint • (b): lateral view
ELBOW JOINT
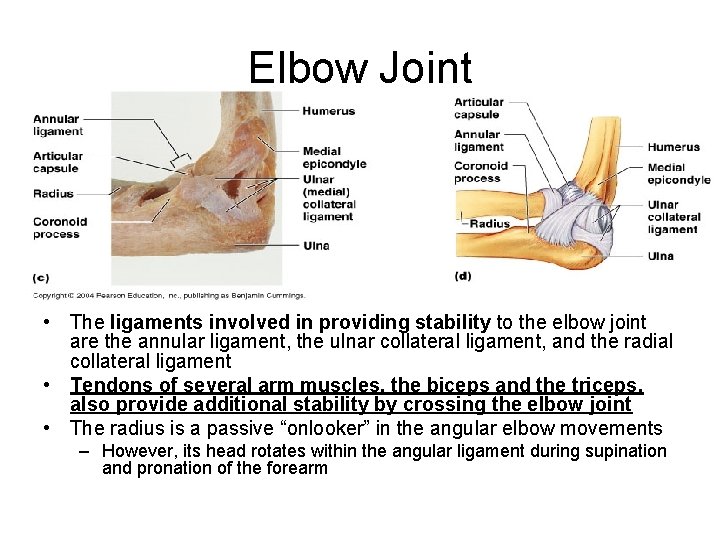
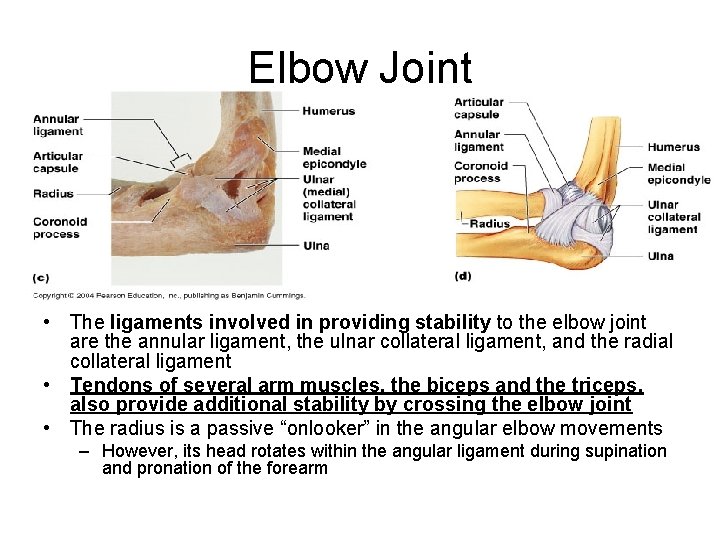
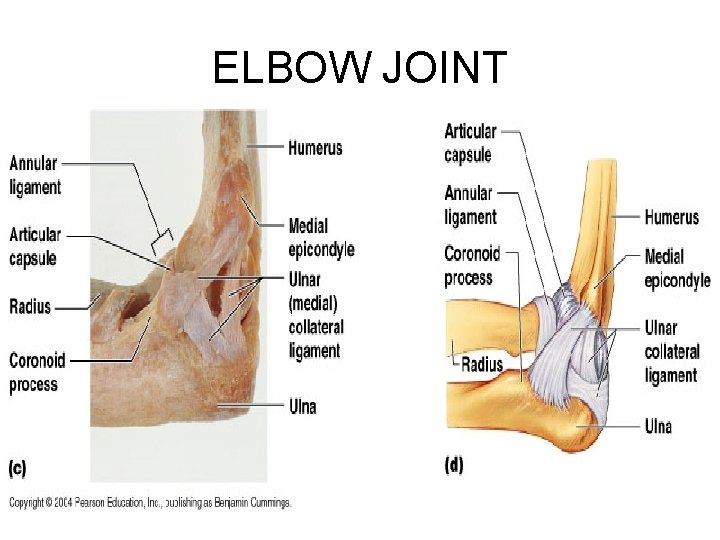
Elbow Joint • The ligaments involved in providing stability to the elbow joint are the annular ligament, the ulnar collateral ligament, and the radial collateral ligament • Tendons of several arm muscles, the biceps and the triceps, also provide additional stability by crossing the elbow joint • The radius is a passive “onlooker” in the angular elbow movements – However, its head rotates within the angular ligament during supination and pronation of the forearm
ELBOW JOINT
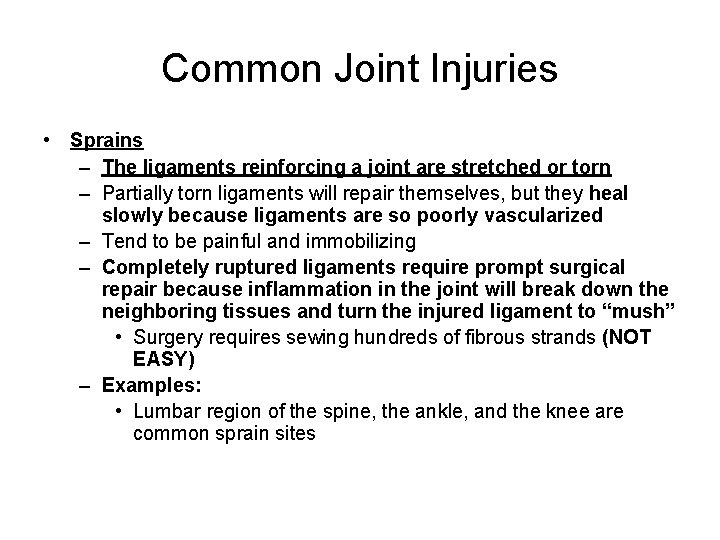
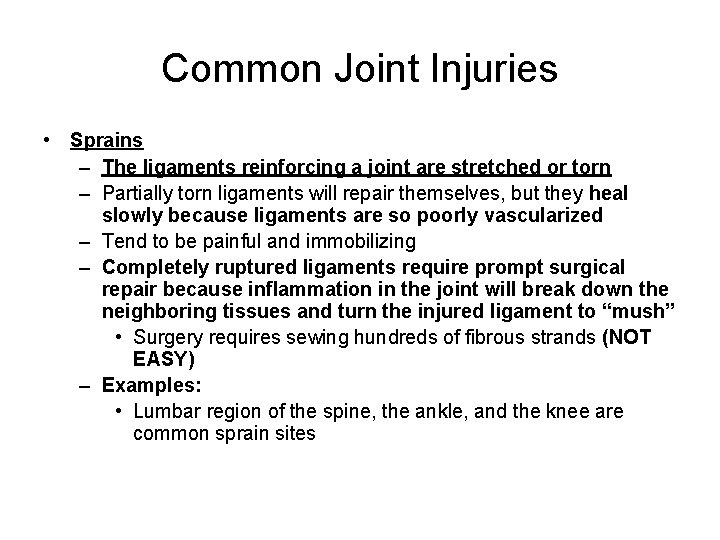
Common Joint Injuries • Sprains – The ligaments reinforcing a joint are stretched or torn – Partially torn ligaments will repair themselves, but they heal slowly because ligaments are so poorly vascularized – Tend to be painful and immobilizing – Completely ruptured ligaments require prompt surgical repair because inflammation in the joint will break down the neighboring tissues and turn the injured ligament to “mush” • Surgery requires sewing hundreds of fibrous strands (NOT EASY) – Examples: • Lumbar region of the spine, the ankle, and the knee are common sprain sites
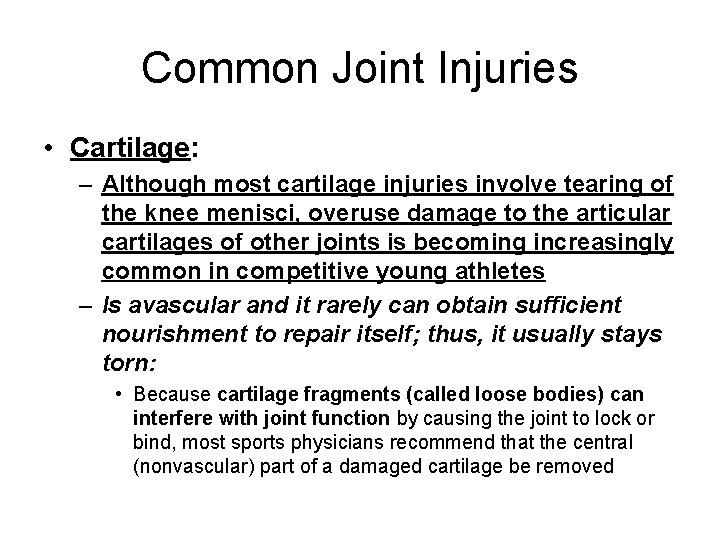
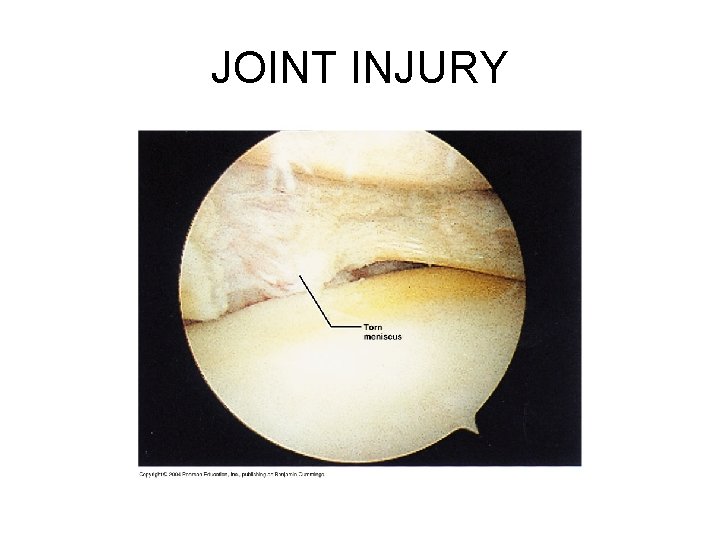
Common Joint Injuries • Cartilage: – Although most cartilage injuries involve tearing of the knee menisci, overuse damage to the articular cartilages of other joints is becoming increasingly common in competitive young athletes – Is avascular and it rarely can obtain sufficient nourishment to repair itself; thus, it usually stays torn: • Because cartilage fragments (called loose bodies) can interfere with joint function by causing the joint to lock or bind, most sports physicians recommend that the central (nonvascular) part of a damaged cartilage be removed

Common Joint Injuries • Cartilage: – Arthroscopic surgery: • A small instrument bearing a tiny lens and fiber-optic light source, enables the surgeon to view the joint interior – Repair ligament – Remove cartilage fragments – Removal of part of a meniscus » Removal of part of a meniscus does not severely impair joint mobility, but the joint is definitely less stable • Minimizes tissue damage and scarring
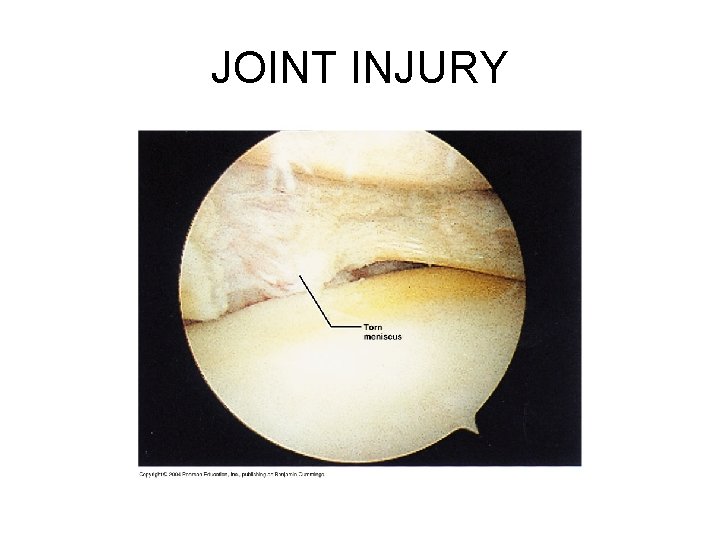
JOINT INJURY

Common Joint Injuries • Dislocation: luxation – Occurs when bones are forced out of alignment • Usually accompanied by sprains, inflammation, and joint immobilization – Like fractures, dislocations must be reduced (bone ends must be returned to their proper positions) – Examples: • • Jaw Shoulder Fingers Thumb – Subluxation: partial dislocation of a joint
Inflammatory and Degenerative Conditions • Bursitis: – Inflammation of the bursa • Is usually caused by a blow or friction – Severe cases are treated by injecting antiinflammatory drugs into the bursa – If excessive fluid accumulates, removing some fluid by needle aspiration may relieve the pressure – Examples: • Falling on one’s knee may result in a painful bursitis of the prepatellar bursa (housemaid’s knee / water on the knee) • Prolonged leaning on one’s elbow may damage the bursa close to the olecranon process (student’s elbow / olecranon bursitis)
Inflammatory and Degenerative Conditions • Tendonitis: – Is inflammation of the tendon sheaths, and is usually caused by overuse – Symptoms: pain and swelling – Treatment: rest, ice, anti-inflammatory drugs
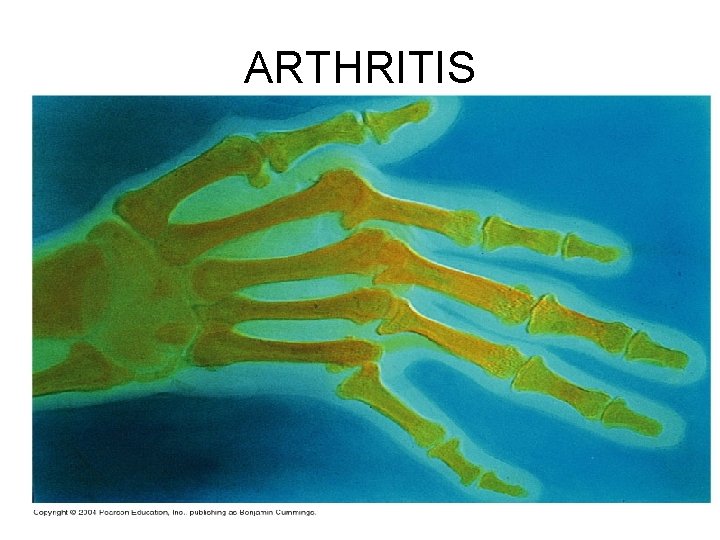
Inflammatory and Degenerative Conditions • Arthritis: – Describes many inflammatory or degenerative diseases (over 100) that damage the joints – Resulting in pain, stiffness, and swelling of the joint – Acute forms: • Usually result from bacterial invasion and are treated with antibiotics • Synovial membrane thickens and fluid production decreases, causing increased friction and pain – Chronic (long-term) forms: osteoarthritis, rheumatoid arthritis, and gouty arthritis
Inflammatory and Degenerative Conditions • Osteoarthritis (OA): – Most common chronic arthritis – Often called “wear-and-tear” arthritis – Probably related to aging • But a genetic basis – Slow and irreversible – It is the result of breakdown of articular cartilage (by enzymes: but in healthy people replaced) and subsequent thickening of bone tissue, which may restrict joint movement • Cartilage softened, roughened, pitted, and eroded – Treatment: • Aspirin, acetaminophen, magnetic therapy (assumed to stimulate the growth and repair of articular cartilage), glucosamine (nutritional supplement: decrease pain and inflammation, preserve articular cartilage) – Examples: cervical and lumbar spines, fingers, knuckles, knees, hips
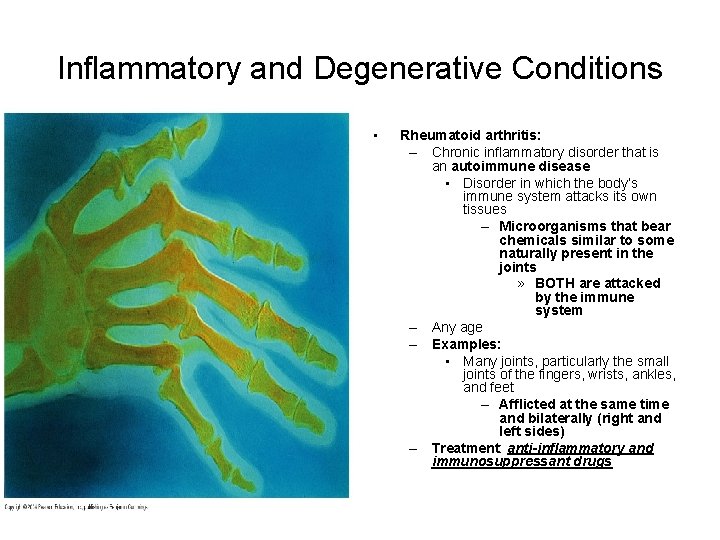
Inflammatory and Degenerative Conditions • Rheumatoid arthritis: – Chronic inflammatory disorder that is an autoimmune disease • Disorder in which the body’s immune system attacks its own tissues – Microorganisms that bear chemicals similar to some naturally present in the joints » BOTH are attacked by the immune system – Any age – Examples: • Many joints, particularly the small joints of the fingers, wrists, ankles, and feet – Afflicted at the same time and bilaterally (right and left sides) – Treatment: anti-inflammatory and immunosuppressant drugs
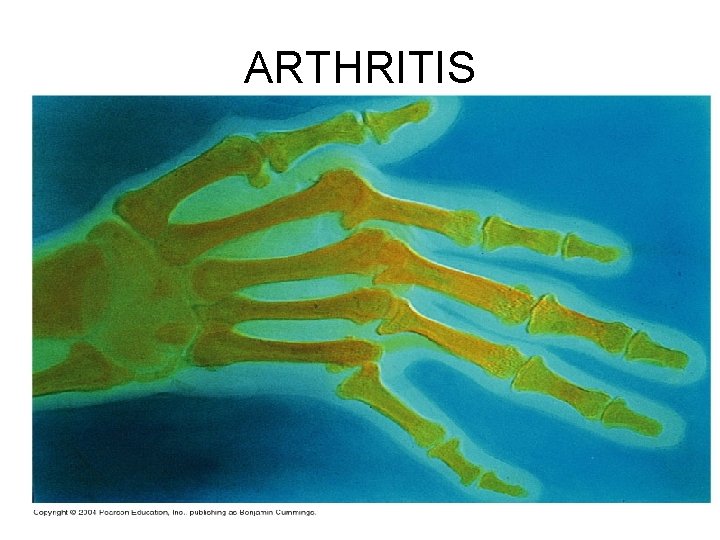
ARTHRITIS
Inflammatory and Degenerative Conditions • Gouty Arthritis: gout – Uric acid, a normal waste product of nucleic acid metabolism, is ordinarily excreted in urine without any problems – However, when blood levels of uric acid rise excessively (due to its excessive production or slow excretion), it may be deposited as needle-shaped urate crystals in the soft tissues of joints • Inflammatory response follows – Genetic factors are definitely implicated – Untreated: • Articular bone ends fuse and immobilizes the joints – Treatment: • Anti-inflammatory drugs • Avoid alcohol: promotes uric acid overproduction • Avoid foods high in purine-containing nucleic acids (liver, kidneys, sardines)
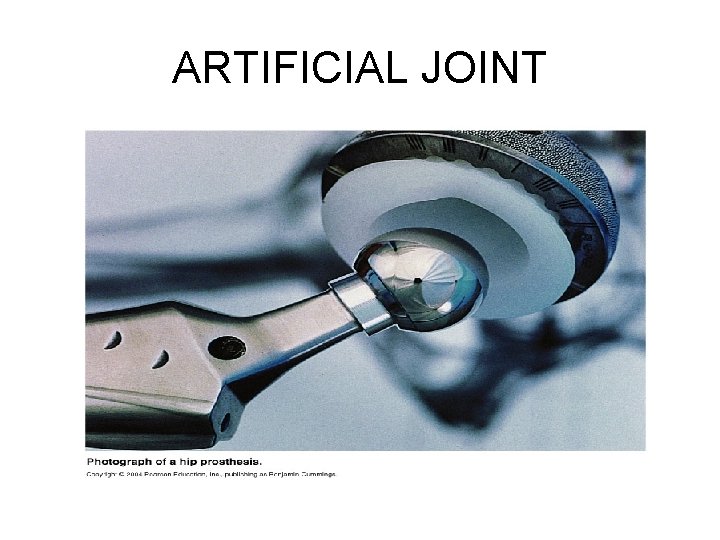
ARTIFICIAL JOINT
DEVELOPMENTAL ASPECTS OF JOINTS • Joints develop at the same time as bones, resembling adult form by eight weeks gestation • At late middle age and beyond, ligaments and tendons shorten and weaken, intervertebral discs become more likely to herniate, and there is onset of osteoarthritis