Surgical Site Infections Ignaz Semmelweis 1847 Realized that












- Slides: 56

Surgical Site Infections
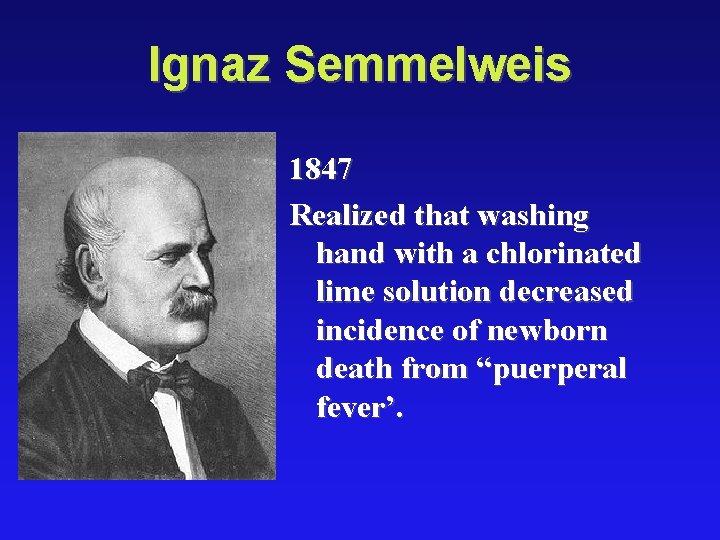
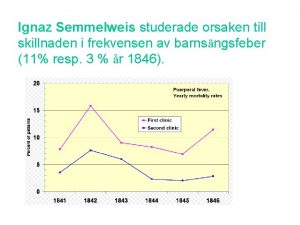
Ignaz Semmelweis 1847 Realized that washing hand with a chlorinated lime solution decreased incidence of newborn death from “puerperal fever’.
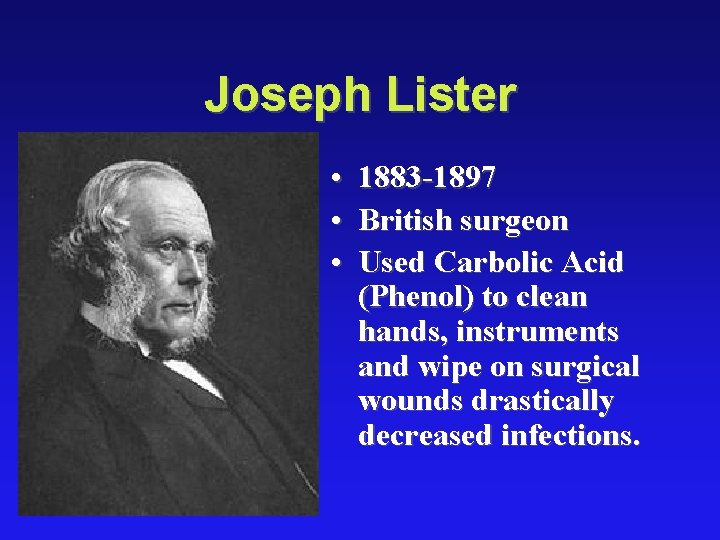
Joseph Lister • • • 1883 -1897 British surgeon Used Carbolic Acid (Phenol) to clean hands, instruments and wipe on surgical wounds drastically decreased infections.
Outline : • • Important Terms Antiseptics Surgical wounds Post-operative Infections – Surgical Site Infection – Hospital Acquired Infections • Antibiotic Prophylaxis
Definition : • Colonization – Bacteria present in a wound with no signs or symptoms of systemic inflammation – Usually less than 105 CFU/m. L
• Contamination – Transient exposure of a wound to bacteria – Varying concentrations of bacteria possible – Time of exposure suggested to be < 6 hours
• DECONTAMINATION: is the process of removing or neutralizing infectious or injurious m. o. from inanimate objects • CLEANING: physically removes ALL visible blood, body fluid, or other foreign material as dust or soil from skin or intimate objects.
• ASEPSIS/ASEPTIC TECH. : is the practices performed just before or during clinical or surgical procedure to reduce the risk of infection that produce a state of asepsis. • ANTISEPSIS: is the prevention of infection by killing or inhibiting the growth of m. o. on skin or body tissues.
• DISINFECTION: is the elimination of most (but not all) disease causing m. o. from inanimate objects. • High level disinfection –by boiling or chemicals- eliminate ALL m. o. except some bacterial endospores.
• STERILIZATION: is the process that remove ALL m. o. including bacterial endospores form inanimate objects
antiseptics • Antiseptics: � Kill m. o. on skin � Not strong enough to use on instruments � For surgical scrubs; preparations of pt. skin or mm before clinical procedures � DO NOT use for processing or storage of instruments • Disinfectants: � Kill m. o. on surfaces (counters; exam tables; floors…etc. ) � DO NOT use on skin , may irritate skin § Acceptable antiseptics: As ( Alcohol; Chlorhexidine; Iodine preparations; Iodophor; Triclosan)
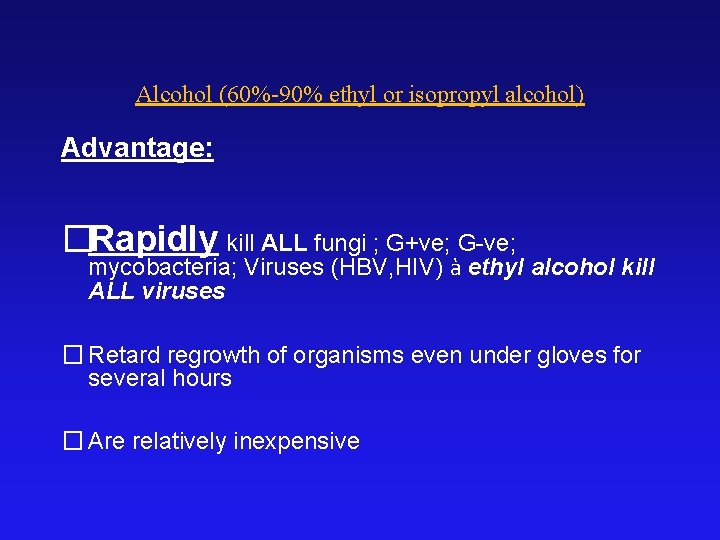
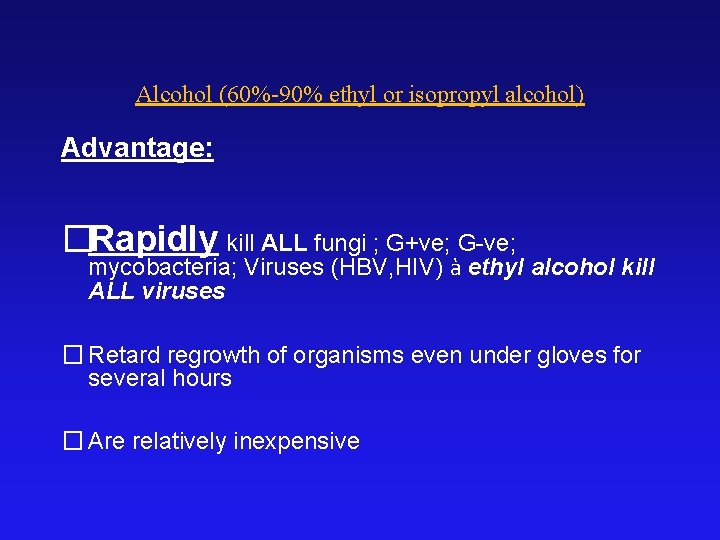
Alcohol (60%-90% ethyl or isopropyl alcohol) Advantage: �Rapidly kill ALL fungi ; G+ve; G-ve; mycobacteria; Viruses (HBV, HIV) à ethyl alcohol kill ALL viruses � Retard regrowth of organisms even under gloves for several hours � Are relatively inexpensive
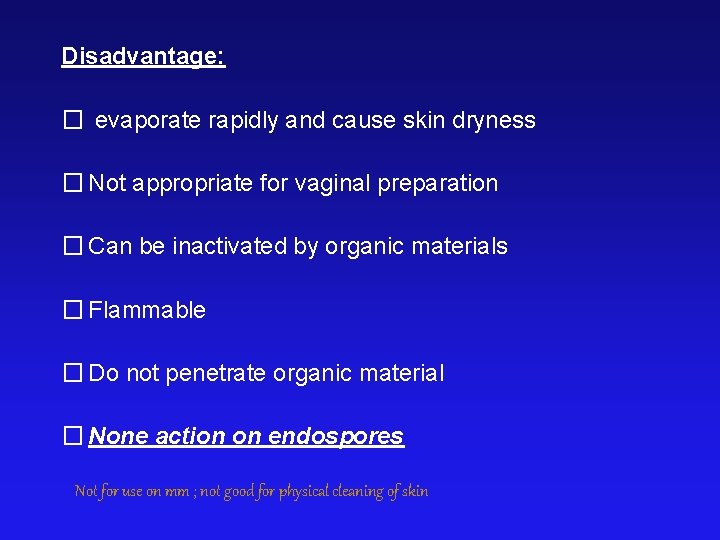
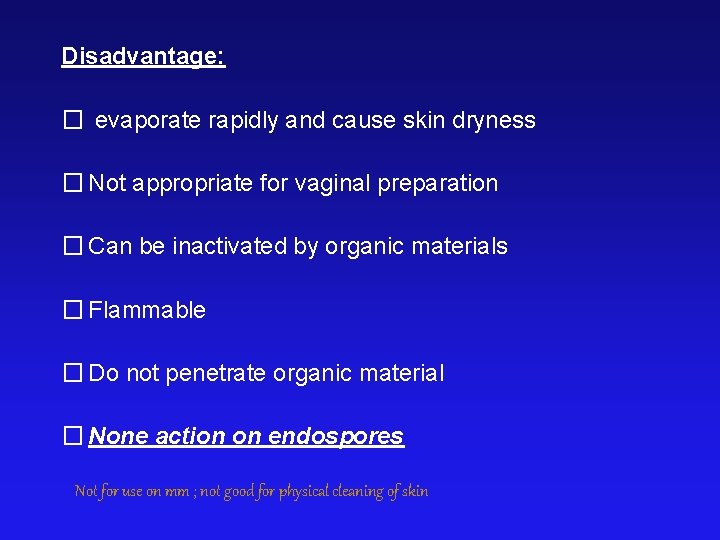
Disadvantage: � evaporate rapidly and cause skin dryness � Not appropriate for vaginal preparation � Can be inactivated by organic materials � Flammable � Do not penetrate organic material � None action on endospores Not for use on mm ; not good for physical cleaning of skin
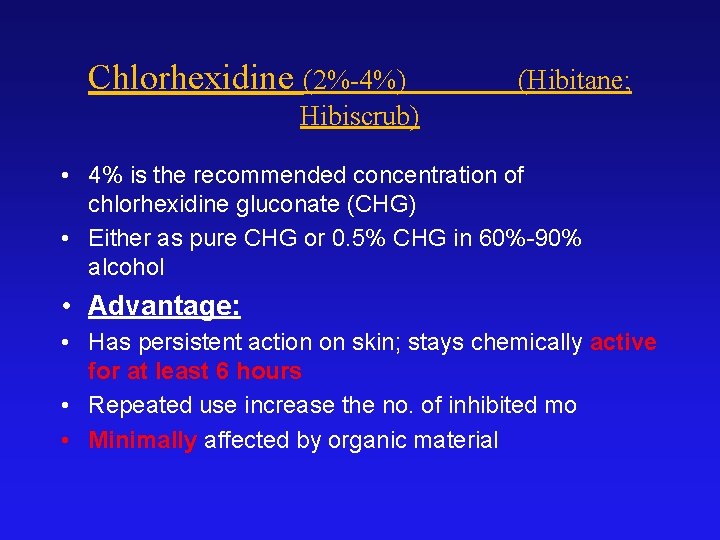
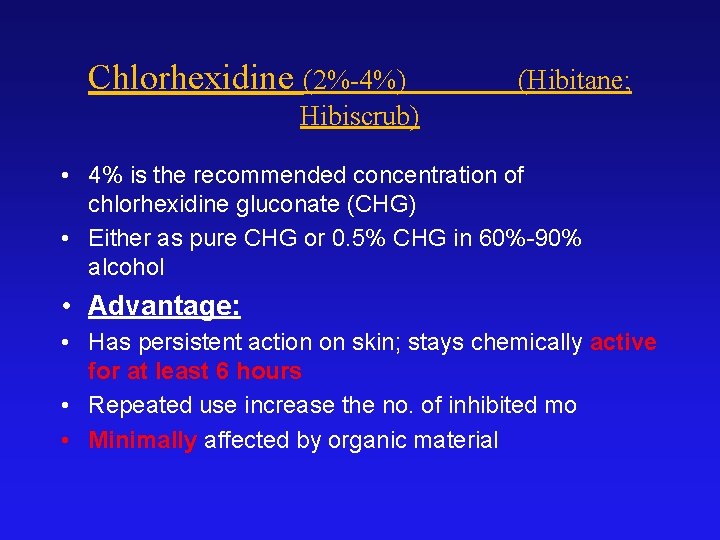
Chlorhexidine (2%-4%) (Hibitane; Hibiscrub) • 4% is the recommended concentration of chlorhexidine gluconate (CHG) • Either as pure CHG or 0. 5% CHG in 60%-90% alcohol • Advantage: • Has persistent action on skin; stays chemically active for at least 6 hours • Repeated use increase the no. of inhibited mo • Minimally affected by organic material
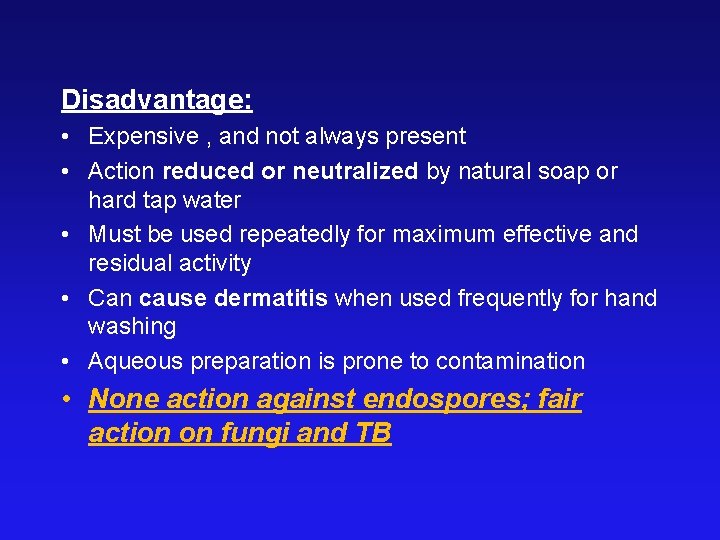
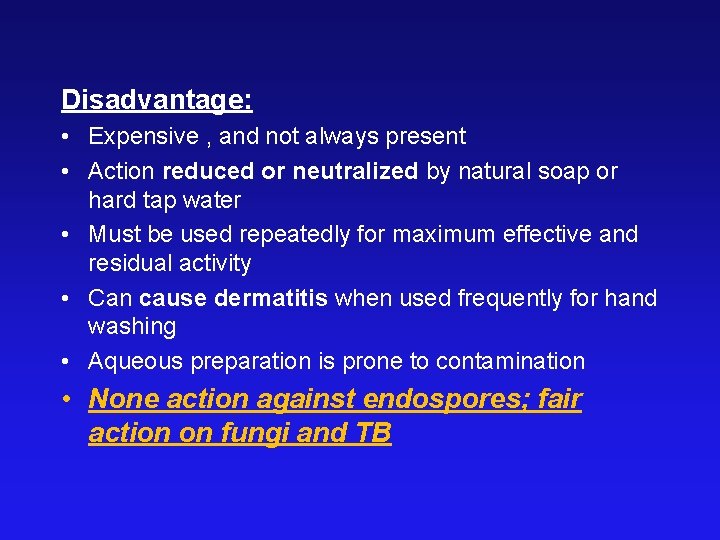
Disadvantage: • Expensive , and not always present • Action reduced or neutralized by natural soap or hard tap water • Must be used repeatedly for maximum effective and residual activity • Can cause dermatitis when used frequently for hand washing • Aqueous preparation is prone to contamination • None action against endospores; fair action on fungi and TB
Iodine and iodophor solutions v 2 types: � 1 -3% aqueous solution à Lugol � 70% alcoholic tincture • Iodophor are solutions of iodine mixed with carrier that release small amount of iodine • The most common iodophor is Betadine • Iodophor require up to 2 min. of contact time to release free iodine
Advantage: • Inexpensive; effective and commonly available • Iodophor are non-irritating to skin and mm making them ideal for vaginal preparation before IUD insertion • Does not stain skin at 1: 2500 concentration
Disadvantage: • Little residual effect (30 -60 minutes) • Inactivated by organic materials • Iodine à skin irritation ( need alcohol for removing it). • May cause hypothyroidisms in neonates due to skin absorption Iodine not iodophor is the only antiseptic effective against endospores
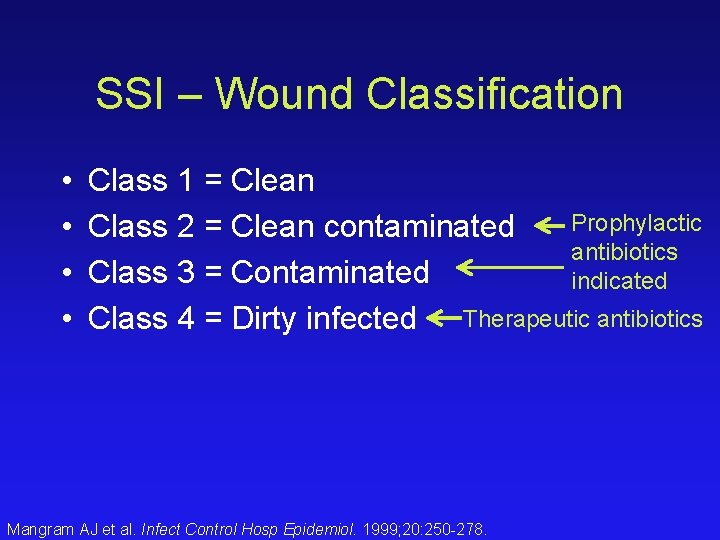
Surgical Wound Classification • • Clean contaminated Contaminated Dirty
Class I Wound (Clean) • Atraumatic wound without inflammation • Do not enter GI, GU, biliary, or respiratory tract • 1. 5% infection rate
Class II Wound (Clean-Contaminated) • Respiratory, GI, GU, or biliary tract entered under controlled conditions • 5% infection rate expected
Class III Wounds (Contaminated) • Traumatic wounds • Breaks in sterile technique • Gross spillage from GI tract • Acute, nonpurulent inflammation • 10% anticipated infection rate
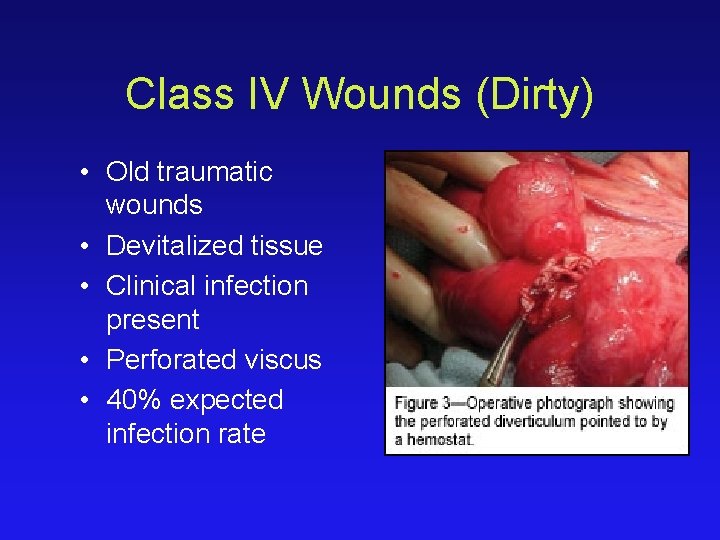
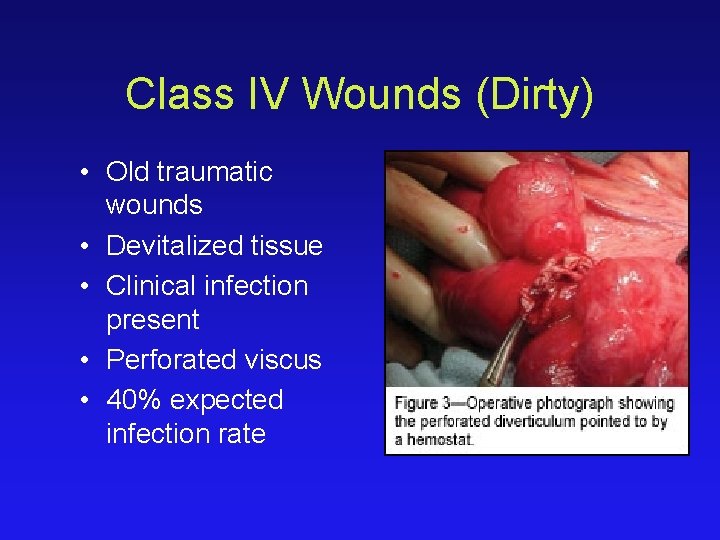
Class IV Wounds (Dirty) • Old traumatic wounds • Devitalized tissue • Clinical infection present • Perforated viscus • 40% expected infection rate
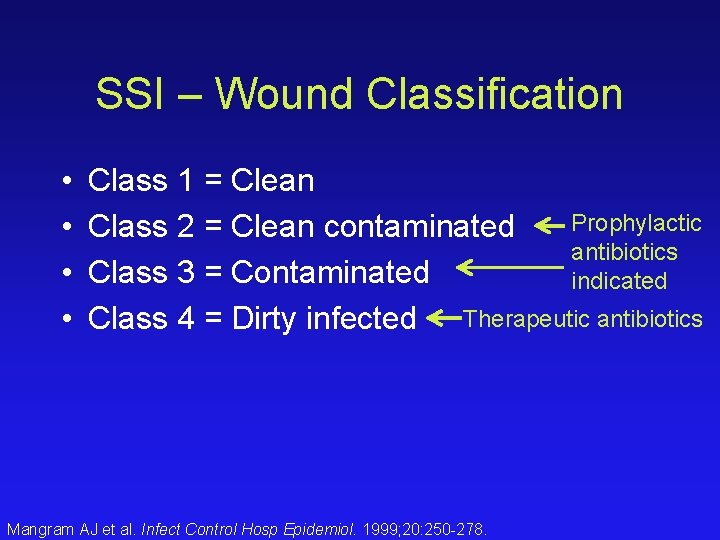
SSI – Wound Classification • • Class 1 = Clean Prophylactic Class 2 = Clean contaminated antibiotics Class 3 = Contaminated indicated Class 4 = Dirty infected Therapeutic antibiotics Mangram AJ et al. Infect Control Hosp Epidemiol. 1999; 20: 250 -278.
Infection is defined by: 1. Microorganisms in host tissue or the bloodstream 2. Inflammatory response to their presence.
Inflammatory Response Localized: – Rubor, Calor, Dolor, Tumor, and functio laesa (loss of function) Systemic: – Systemic Inflammatory Response Syndrome (SIRS)
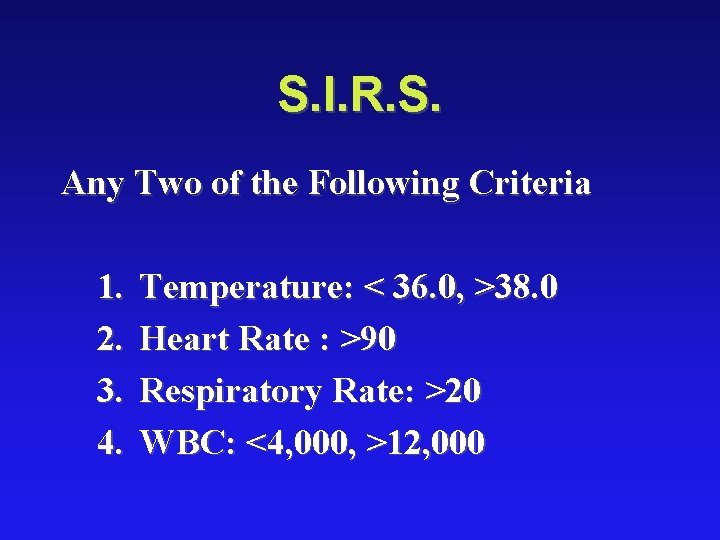
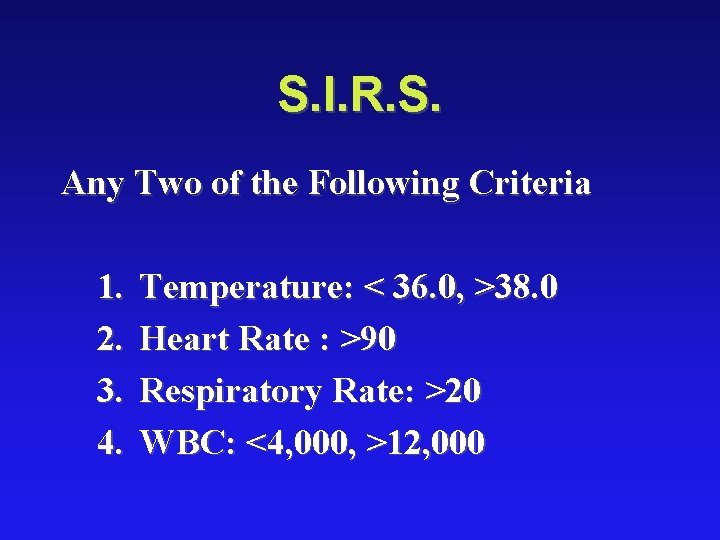
S. I. R. S. Any Two of the Following Criteria 1. 2. 3. 4. Temperature: < 36. 0, >38. 0 Heart Rate : >90 Respiratory Rate: >20 WBC: <4, 000, >12, 000
Sepsis Definition: SIRS plus evidence of local or systemic infection. Septic Shock Definition: Sepsis plus end organ hypoprofusion. Mortality of up to 40%

Soft Tissue Infections: 1. 2. 3. Cellulitis Abscess Necrotizing Infections

Cellulitis

Cellulitis Definition: Diffuse infection with severe inflammation of dermal and subcutaneous layers of the skin Diagnosis: Pain, Warmth, Hyperesthesia Treatment: Antibiotics. Common Pathogens: Skin Flora (Streptococcus/Staphylococcus)

Abscess
Abscess Definition: Infectious accumulation of purulent material (Neutrophils) in a closed cavity Diagnosis: Fluctuant: Moveable and compressible Treatment: Drainage

Necrotizing Soft Tissue Infection
Necrotizing Soft Tissue Infection Definition: Deep infection of skin and soft tissue that may spread rapidly along facial planes. Diagnosis: Purely Clinical, dishwater discharge, gray tissue, pain out of proportion to examination, bulla, and dark, golden discoloration. Treatment: True Surgical Emergency, Antibiotics
Necrotizing Soft Tissue Infection • Common Pathogens – Clostridium – Group A streptococcus – Polymicrobial

Post-Operative Infections • Fever After Surgery • The “Five W’s” – Wind: Atelectisis – Water: UTI – Walking: DVT – Wonder Drug: Medication Induced – Wound: Surgical Site Infection
Surgical Site Infection(SSI) : • Infection at or near the site of surgery that occurs within 30 days of surgery if there is no implant (hardware, artificial graft, mesh, etc) OR occurs within 3 months of the surgery with an implant in place From CDC’s NNIS

Why Prevent SSIs? • Approximately 500, 000 surgical site infections (SSI) occur annually in the United States • Patients that develop SSI have twice the mortality and are: – 60% more likely to spend time in ICU – 5 times more likely to be readmitted
Surgical Site Infections • 3 rd most common hospital infection • Incisional – Superficial – Deep • Organ Space – Generalized (peritonitis) – Abscess
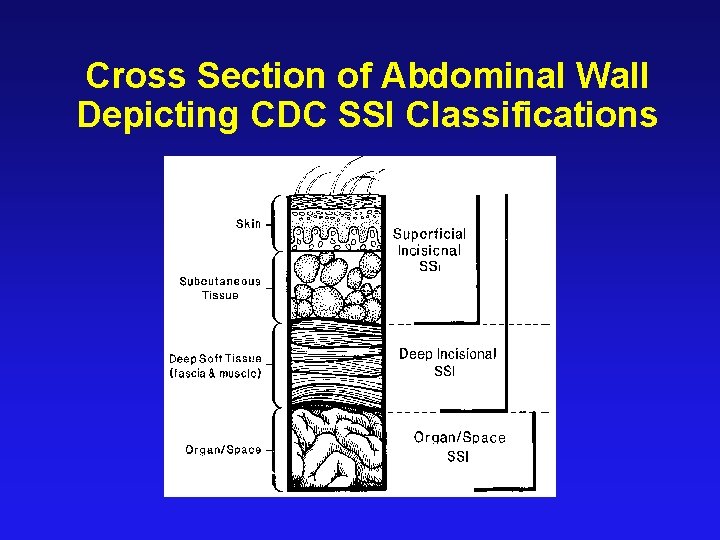
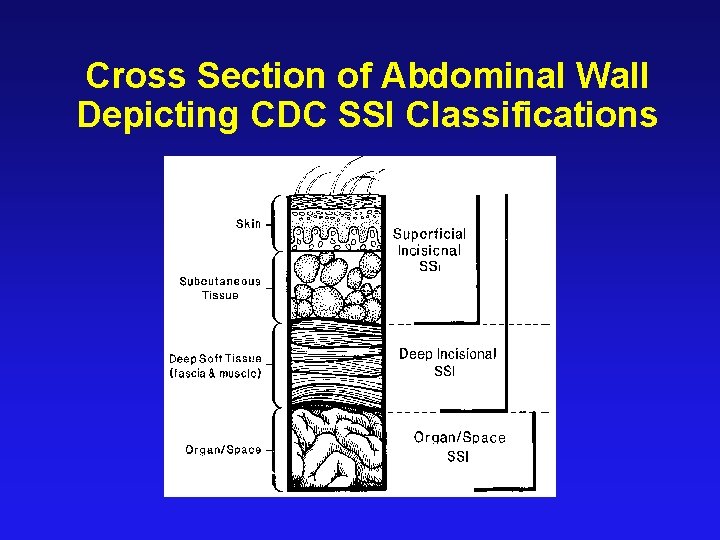
Cross Section of Abdominal Wall Depicting CDC SSI Classifications
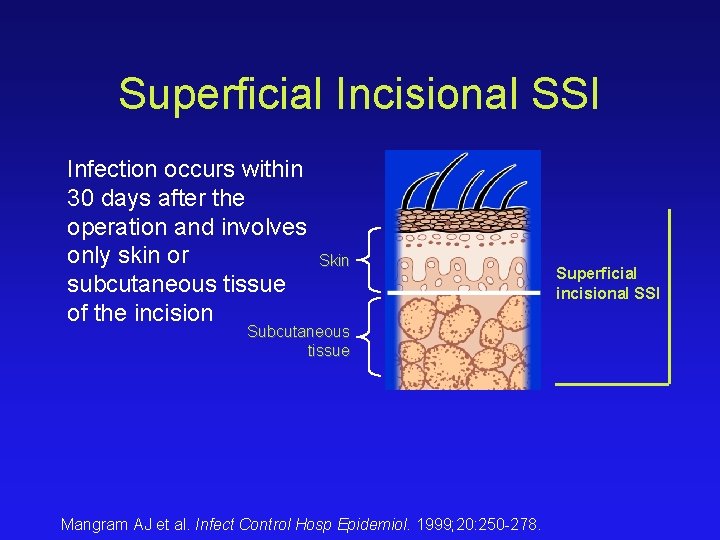
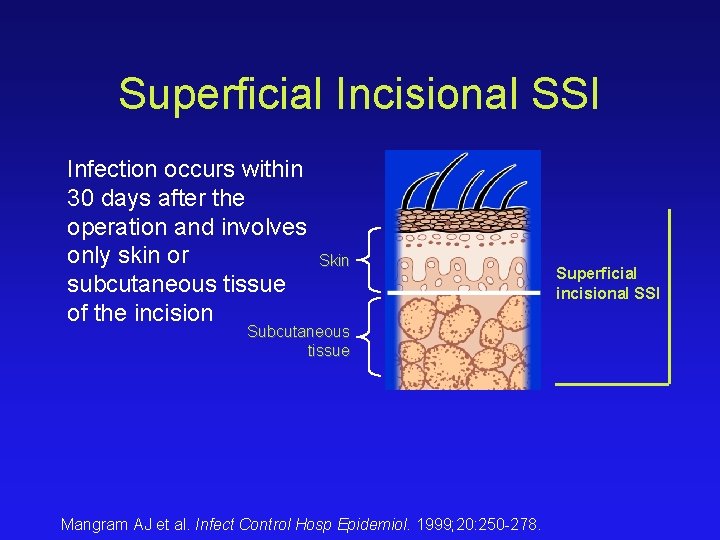
Superficial Incisional SSI Infection occurs within 30 days after the operation and involves only skin or Skin subcutaneous tissue of the incision Subcutaneous tissue Mangram AJ et al. Infect Control Hosp Epidemiol. 1999; 20: 250 -278. Superficial incisional SSI
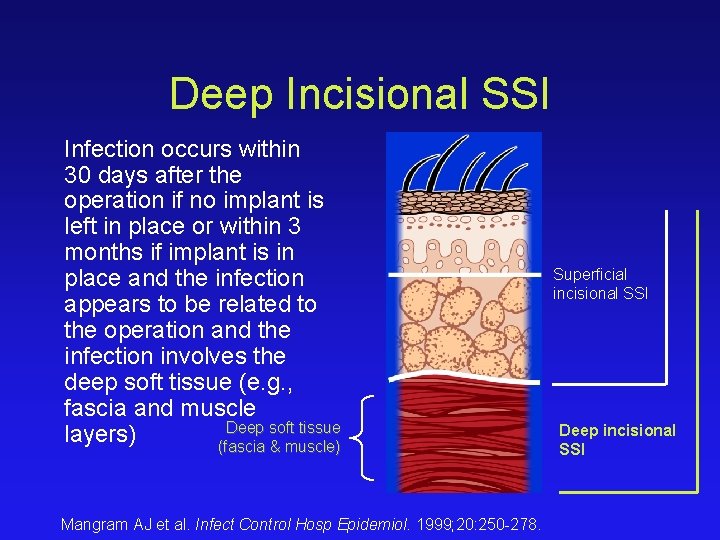
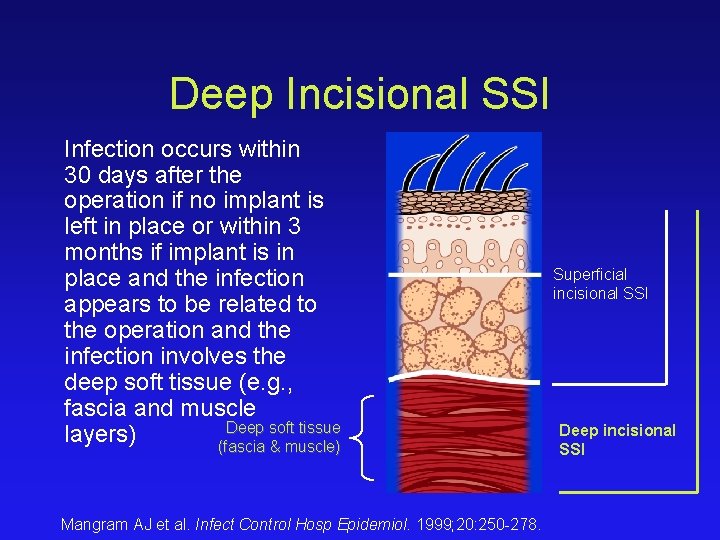
Deep Incisional SSI Infection occurs within 30 days after the operation if no implant is left in place or within 3 months if implant is in place and the infection appears to be related to the operation and the infection involves the deep soft tissue (e. g. , fascia and muscle Deep soft tissue layers) (fascia & muscle) Mangram AJ et al. Infect Control Hosp Epidemiol. 1999; 20: 250 -278. Superficial incisional SSI Deep incisional SSI
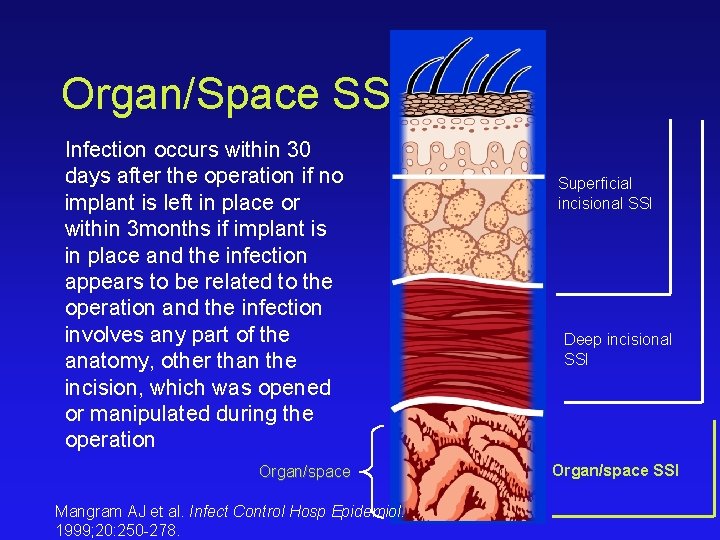
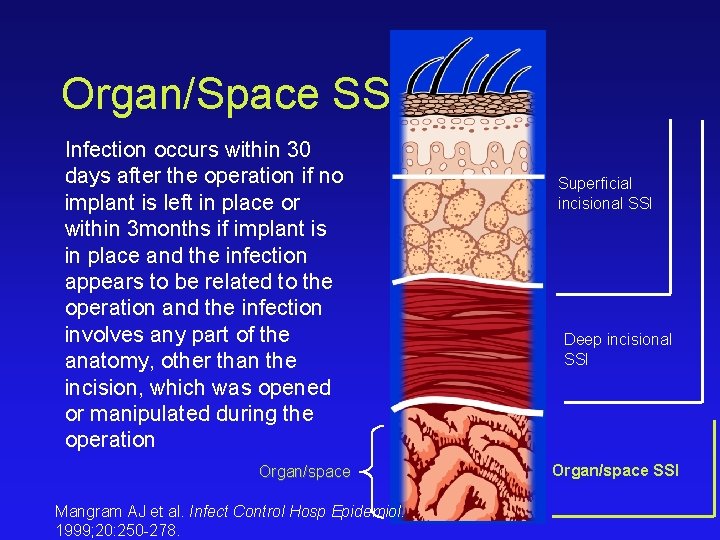
Organ/Space SSI Infection occurs within 30 days after the operation if no implant is left in place or within 3 months if implant is in place and the infection appears to be related to the operation and the infection involves any part of the anatomy, other than the incision, which was opened or manipulated during the operation Organ/space Mangram AJ et al. Infect Control Hosp Epidemiol. 1999; 20: 250 -278. Superficial incisional SSI Deep incisional SSI Organ/space SSI


Risk factors • endogenous contamination (for example, procedures that involve parts of the body with a high concentration of normal flora such as the bowel) • exogenous contamination (for example, prolonged operations that increase the length of time that tissues are exposed)
• diminish the general immune response (for example, diabetes, malnutrition, or immunosuppressive therapy with radiotherapy, chemotherapy or steroids) or local immune response (for example, foreign bodies, damaged tissue or formation of a haematoma).
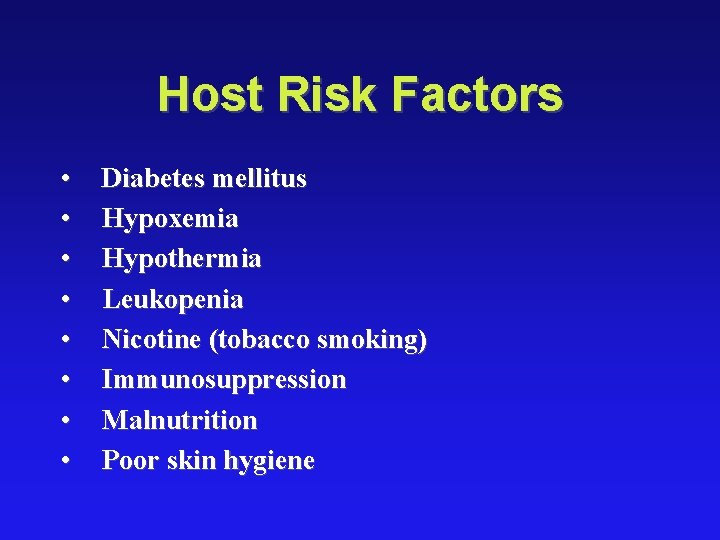
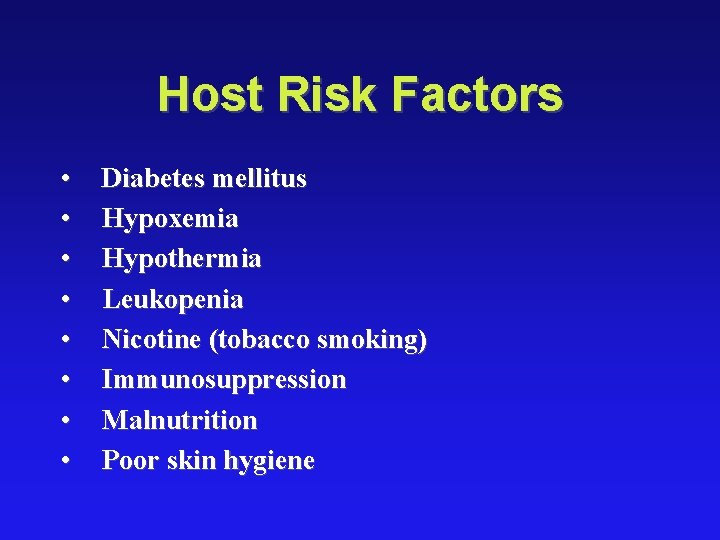
Host Risk Factors • • Diabetes mellitus Hypoxemia Hypothermia Leukopenia Nicotine (tobacco smoking) Immunosuppression Malnutrition Poor skin hygiene
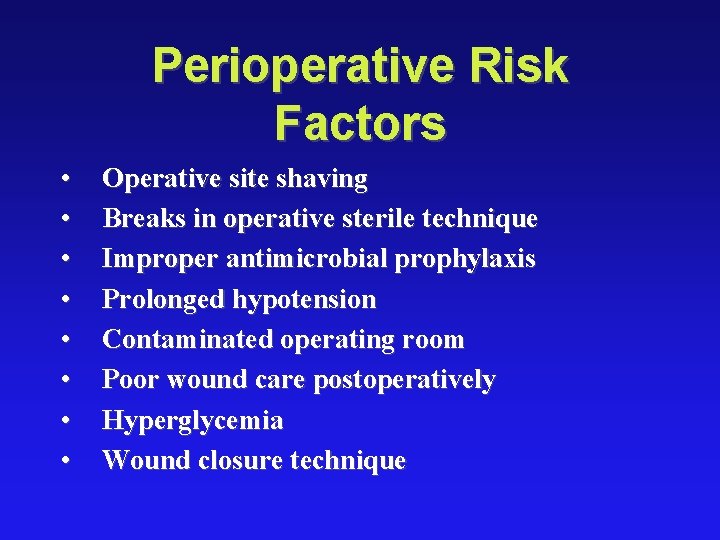
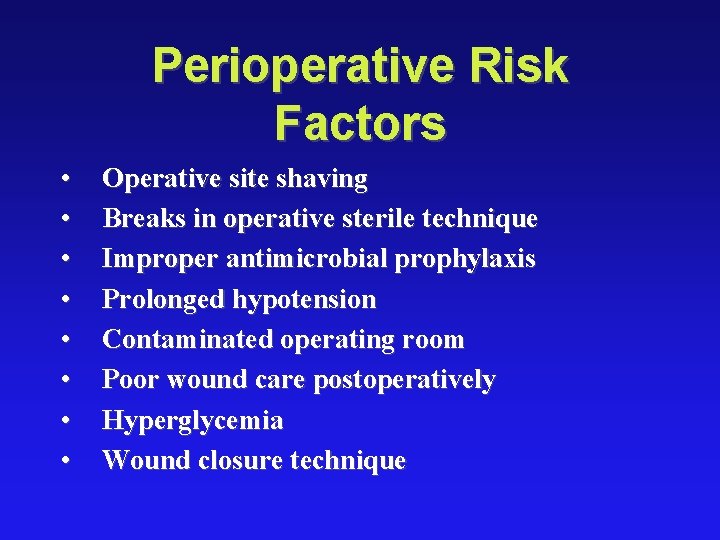
Perioperative Risk Factors • • Operative site shaving Breaks in operative sterile technique Improper antimicrobial prophylaxis Prolonged hypotension Contaminated operating room Poor wound care postoperatively Hyperglycemia Wound closure technique
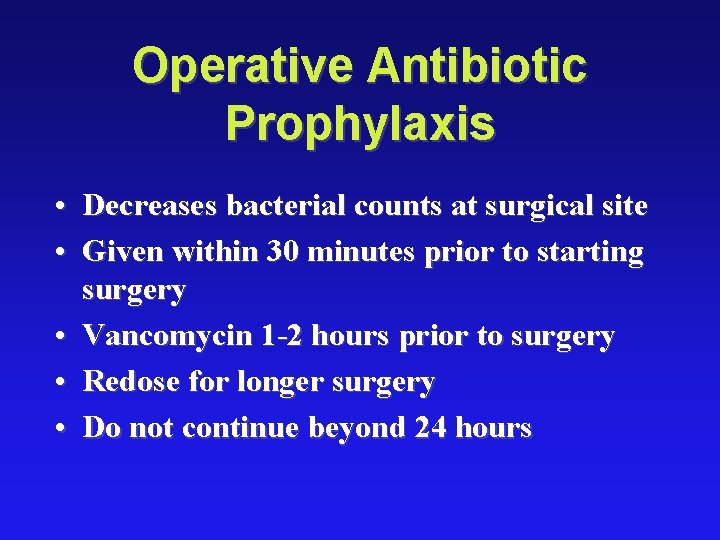
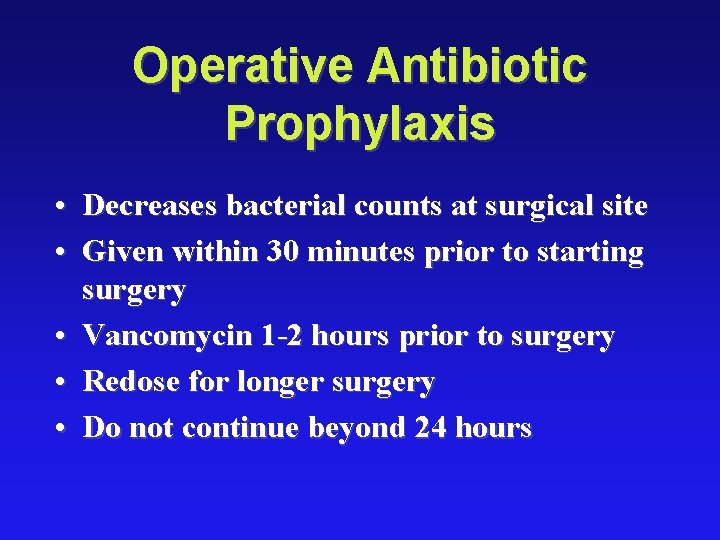
Operative Antibiotic Prophylaxis • Decreases bacterial counts at surgical site • Given within 30 minutes prior to starting surgery • Vancomycin 1 -2 hours prior to surgery • Redose for longer surgery • Do not continue beyond 24 hours
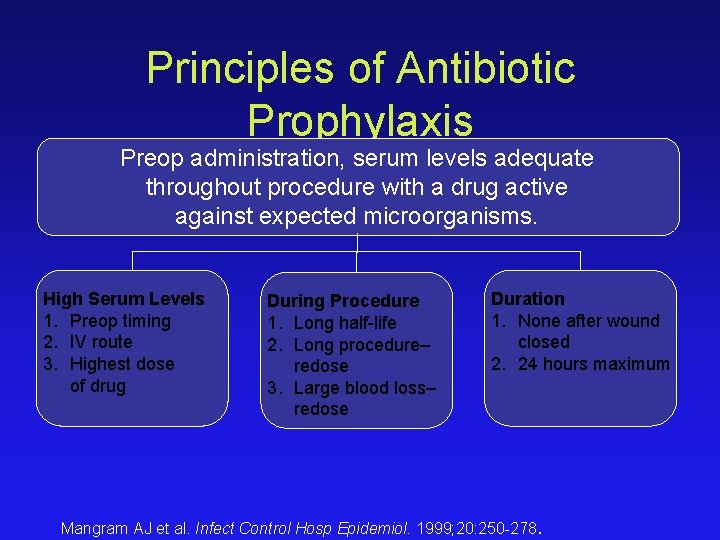
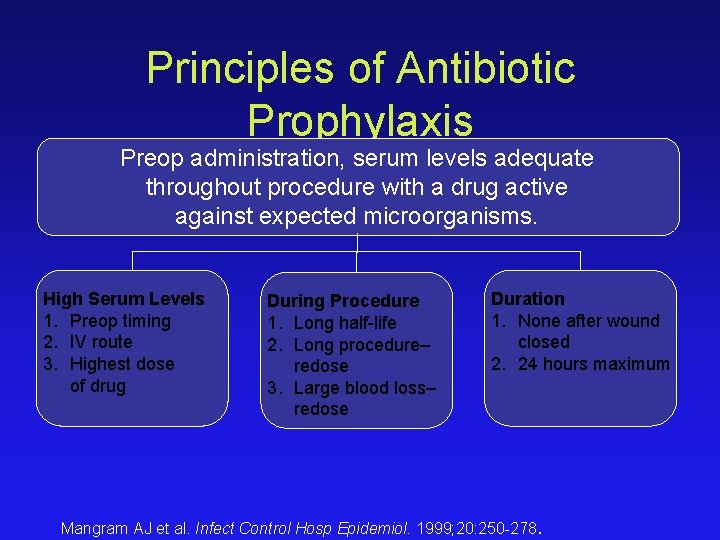
Principles of Antibiotic Prophylaxis Preop administration, serum levels adequate throughout procedure with a drug active against expected microorganisms. High Serum Levels 1. Preop timing 2. IV route 3. Highest dose of drug During Procedure 1. Long half-life 2. Long procedure– redose 3. Large blood loss– redose Duration 1. None after wound closed 2. 24 hours maximum Mangram AJ et al. Infect Control Hosp Epidemiol. 1999; 20: 250 -278.

Treatment • Incisional: open surgical wound, antibiotics for cellulitis or sepsis • Deep/Organ space: Source control, antibiotics for sepsis
Use/Choice of Antibiotics • Use only when indicated • Start with broad spectrum antibiotics designed to cover likely pathogens • Take cultures when possible • Deescalate spectrum once pathogen is know • Have a plan for duration

Thank You
 Ignaz felbiger
Ignaz felbiger Weilaner
Weilaner Thomas edison was born in 1847
Thomas edison was born in 1847 Ameerika leidur 1847-1931
Ameerika leidur 1847-1931 Liverpool 1847
Liverpool 1847 Kauna unahang batas sa daigdig
Kauna unahang batas sa daigdig Ngoại tâm thu thất chùm đôi
Ngoại tâm thu thất chùm đôi Premature atrial contraction
Premature atrial contraction Thể thơ truyền thống
Thể thơ truyền thống Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Walmart thất bại ở nhật
Walmart thất bại ở nhật Tìm độ lớn thật của tam giác abc
Tìm độ lớn thật của tam giác abc Con hãy đưa tay khi thấy người vấp ngã
Con hãy đưa tay khi thấy người vấp ngã Tôn thất thuyết là ai
Tôn thất thuyết là ai Gây tê cơ vuông thắt lưng
Gây tê cơ vuông thắt lưng Sau thất bại ở hồ điển triệt
Sau thất bại ở hồ điển triệt Surgical site infection bundle checklist
Surgical site infection bundle checklist Opportunistic infections
Opportunistic infections Methotrexate yeast infection
Methotrexate yeast infection Opportunistic infections
Opportunistic infections Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Johnson and johnson botnet infections
Johnson and johnson botnet infections Storch infections
Storch infections Storch infections
Storch infections Bone and joint infections
Bone and joint infections Infections opportunistes digestives
Infections opportunistes digestives Bacterial vaginosis
Bacterial vaginosis Postpartum infections
Postpartum infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Genital infections
Genital infections Amber blumling
Amber blumling Opsonization
Opsonization Acute gingival infections
Acute gingival infections Hot site cold site warm site disaster recovery
Hot site cold site warm site disaster recovery Realized niche
Realized niche Can a realized niche be larger than a fundamental niche
Can a realized niche be larger than a fundamental niche Fundamental vs realized niche
Fundamental vs realized niche Realized eschatology definition
Realized eschatology definition Second conditional
Second conditional Realized niche
Realized niche Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Doktori hivatal sote
Doktori hivatal sote Youtube.com
Youtube.com Casecenter semmelweis
Casecenter semmelweis Vesicle fusion
Vesicle fusion Agnes csaki semmelweis
Agnes csaki semmelweis Orthodontics semmelweis
Orthodontics semmelweis Semmelweis
Semmelweis Semmelweis egyetem konzerváló fogászati klinika budapest
Semmelweis egyetem konzerváló fogászati klinika budapest Cornea guttata
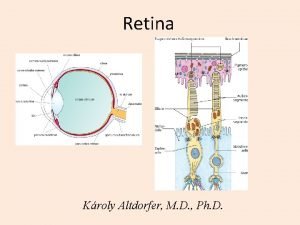
Cornea guttata Semmelweis egyetem doktori iskola
Semmelweis egyetem doktori iskola Semmelweis
Semmelweis Semmelweis
Semmelweis Erasmus plus semmelweis
Erasmus plus semmelweis Itc semmelweis
Itc semmelweis Semmelweis
Semmelweis Semmelweis arc
Semmelweis arc