RTC on RADIATION PROTECTION OF PATIENTS FOR RADIOGRAPHERS


- Slides: 70

RTC on RADIATION PROTECTION OF PATIENTS FOR RADIOGRAPHERS Accra, Ghana, July 2011 Optimization of protection in fluoroscopy and image-guided interventional procedures IAEA International Atomic Energy Agency
IAEA Fellows welcome!! IAEA 2

Fluoroscopy • Continuous imaging of moving structures or • • contrast agents The photographic plate replaced by fluorescent screen Screen part of an Image Intensifier system coupled to a television camera Now also have direct digital acquisition Radiologist can watch the images “live” on TVmonitor; images can be recorded IAEA 3
Interventional (fluoroscopy) radiology • This are high dose procedures, and are covered in the next lecture, however the imaging principles are just the same IAEA 4
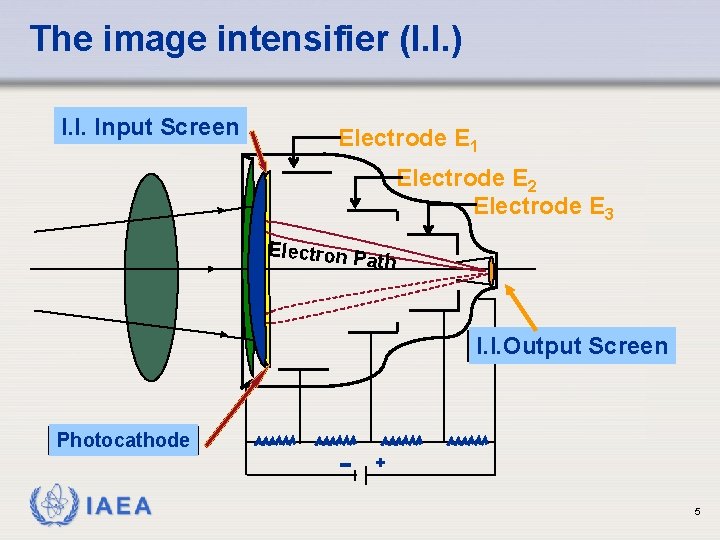
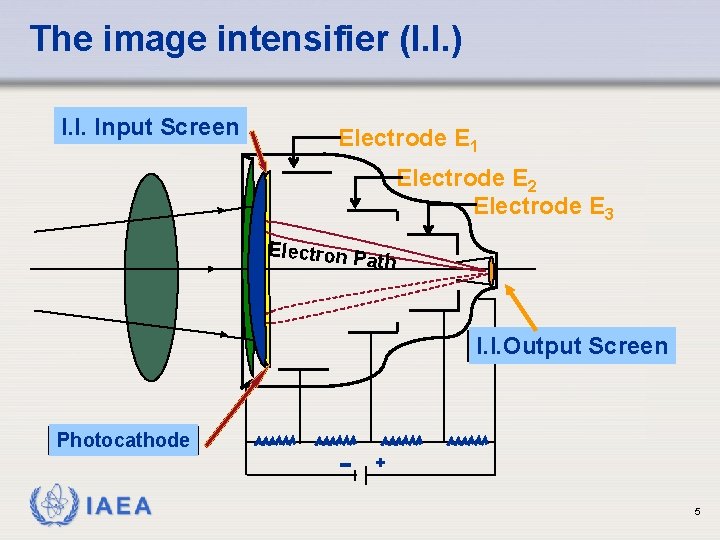
The image intensifier (I. I. ) I. I. Input Screen Electrode E 1 Electrode E 2 Electrode E 3 Electron P ath I. I. Output Screen Photocathode + IAEA 5
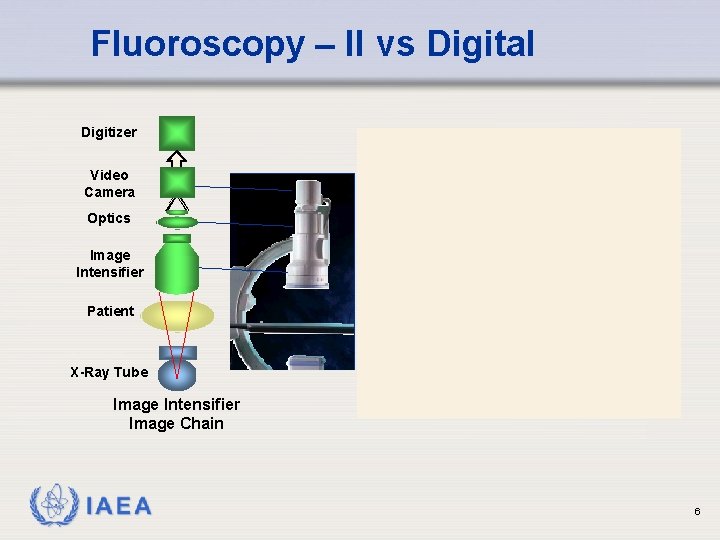
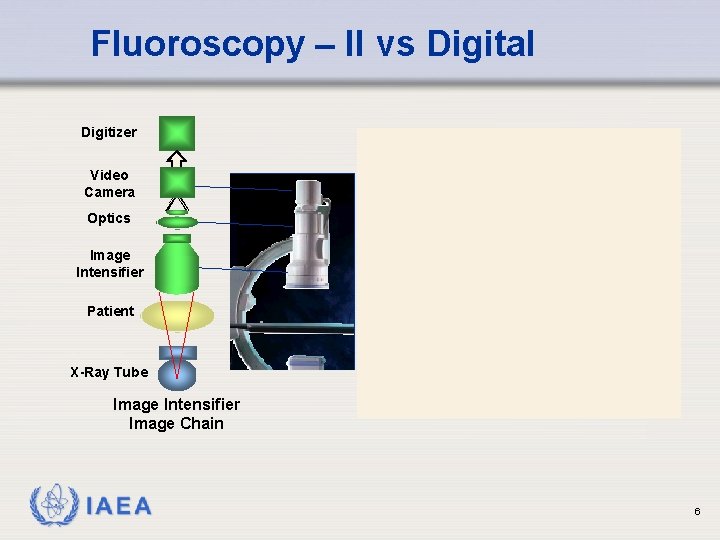
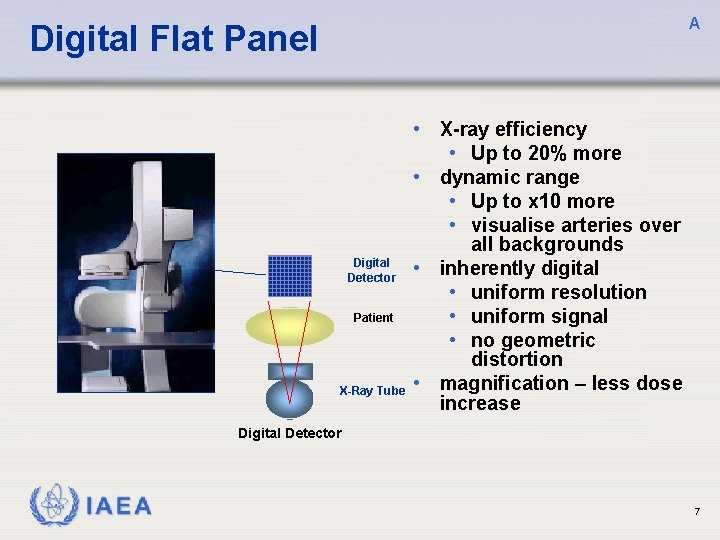
Fluoroscopy – II vs Digital Digitizer Video Camera Optics Image Intensifier Digital Detector Patient X-Ray Tube Image Intensifier Image Chain IAEA Digital Detector 6
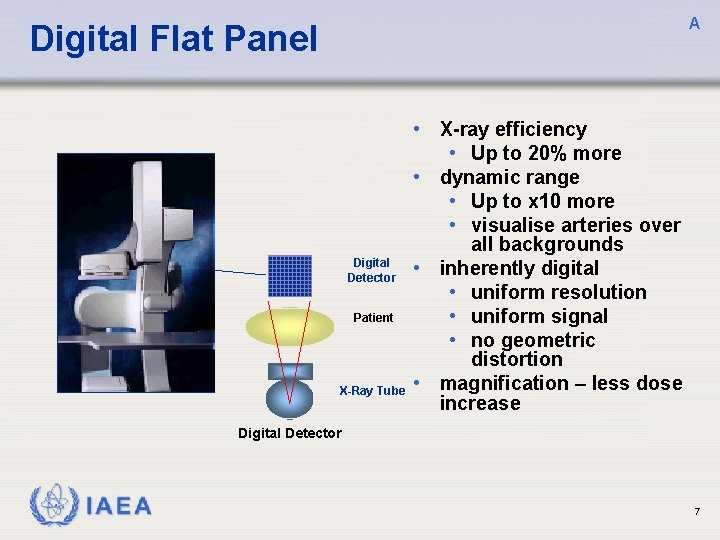
A Digital Flat Panel • X-ray efficiency • Up to 20% more • dynamic range • Up to x 10 more • visualise arteries over Digital Detector Patient X-Ray Tube all backgrounds • inherently digital • uniform resolution • uniform signal • no geometric distortion • magnification – less dose increase Digital Detector IAEA 7
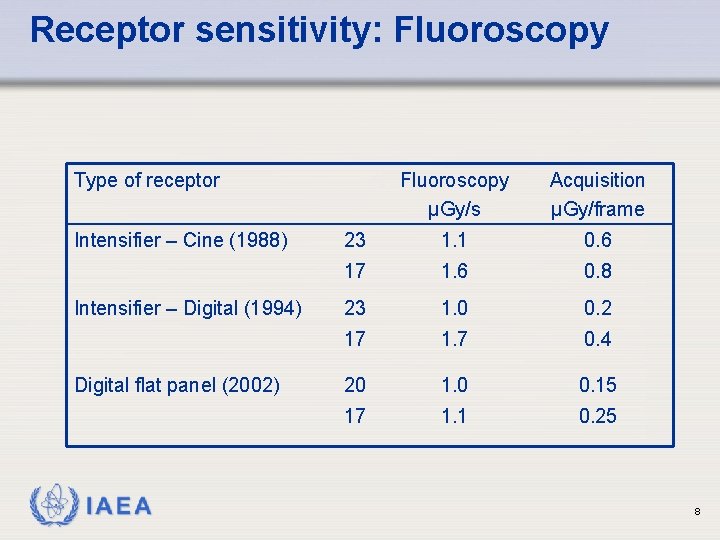
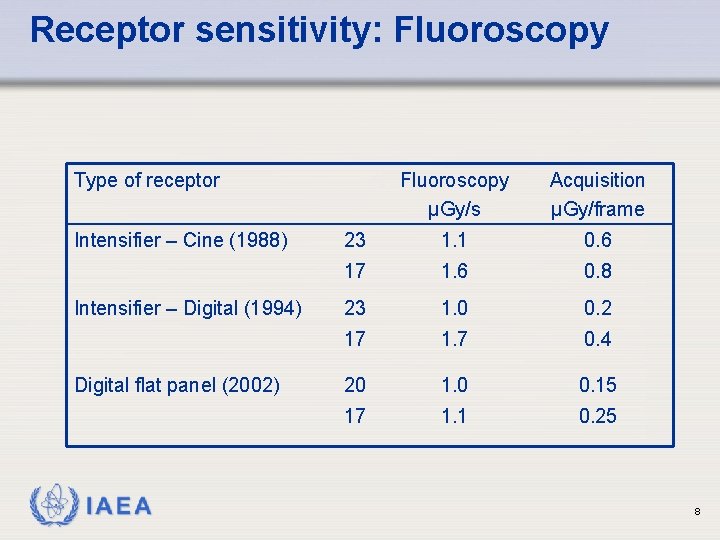
Receptor sensitivity: Fluoroscopy Type of receptor Intensifier – Cine (1988) Intensifier – Digital (1994) Digital flat panel (2002) IAEA Fluoroscopy µGy/s Acquisition µGy/frame 23 1. 1 0. 6 17 1. 6 0. 8 23 1. 0 0. 2 17 1. 7 0. 4 20 1. 0 0. 15 17 1. 1 0. 25 8
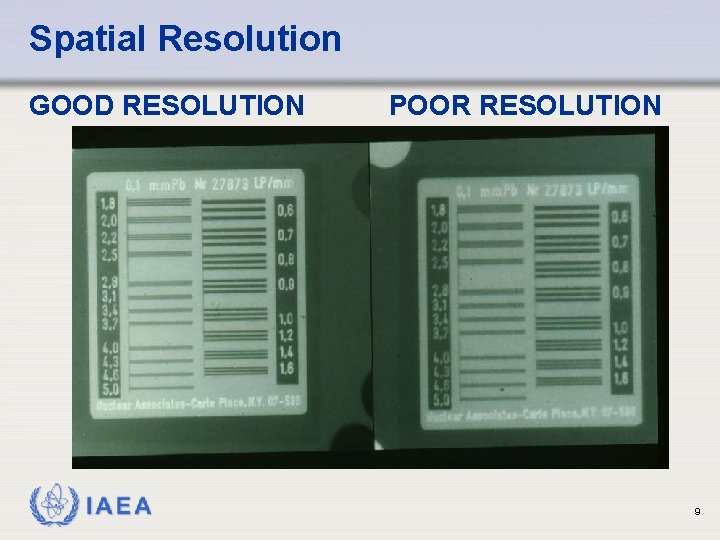
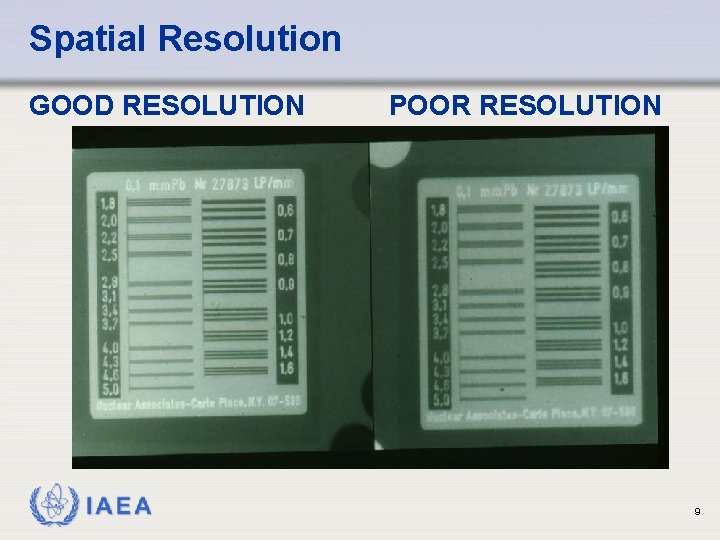
Spatial Resolution GOOD RESOLUTION IAEA POOR RESOLUTION 9
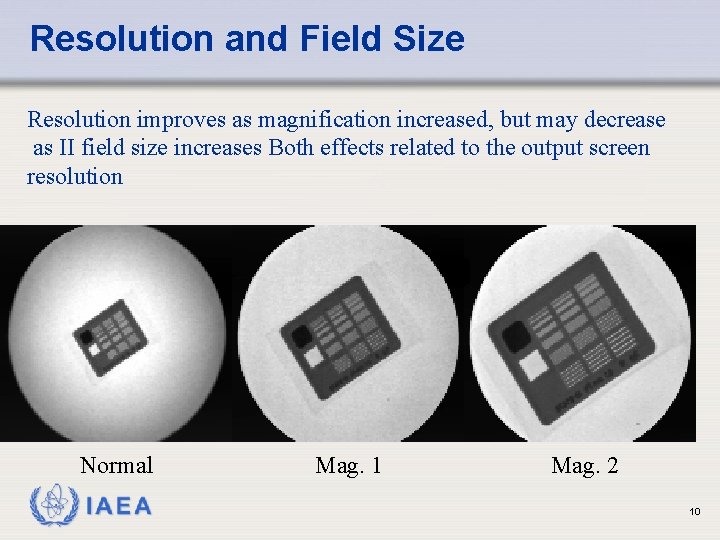
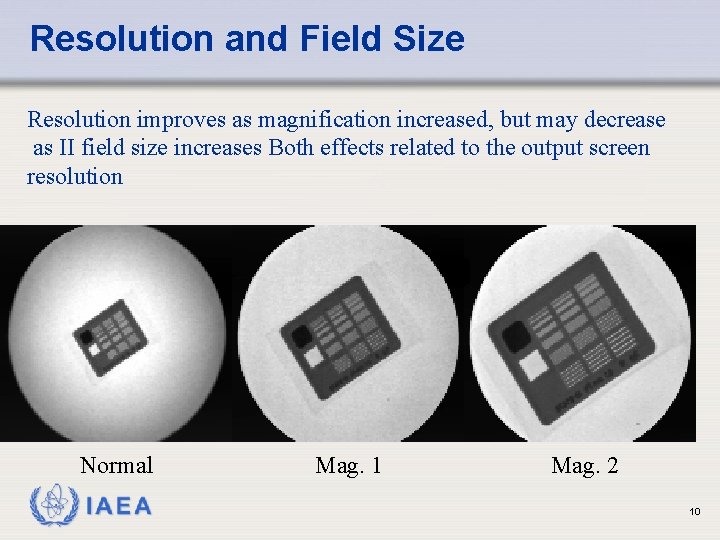
Resolution and Field Size Resolution improves as magnification increased, but may decrease as II field size increases Both effects related to the output screen resolution Normal IAEA Mag. 1 Mag. 2 10
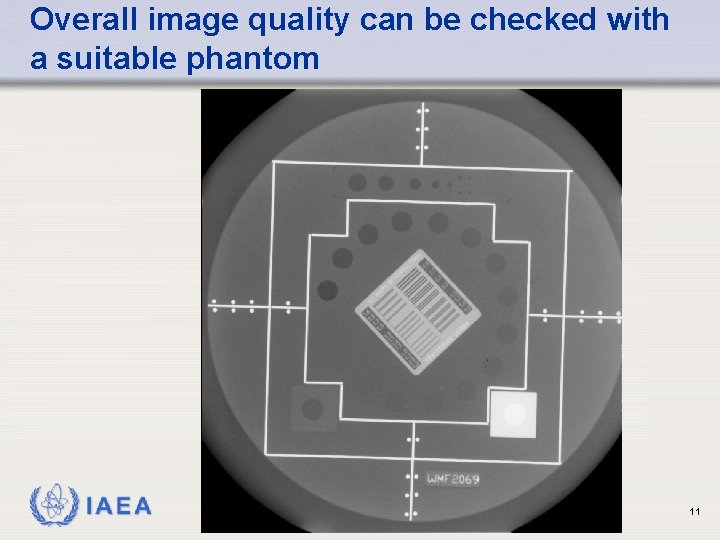
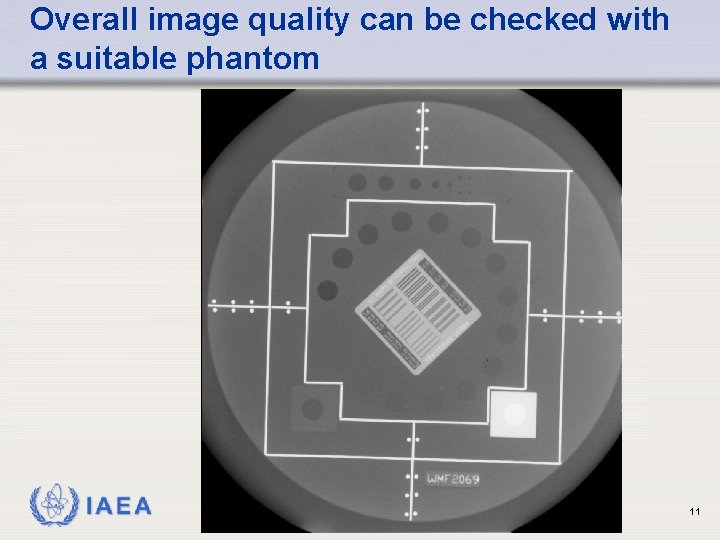
Overall image quality can be checked with a suitable phantom IAEA 11
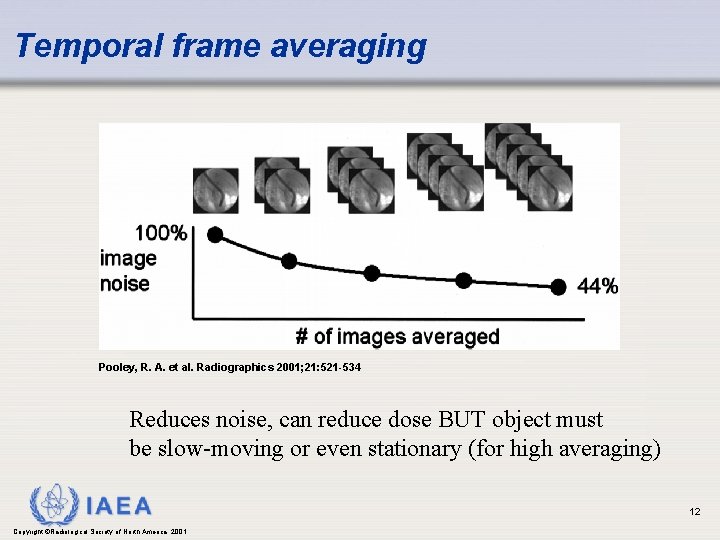
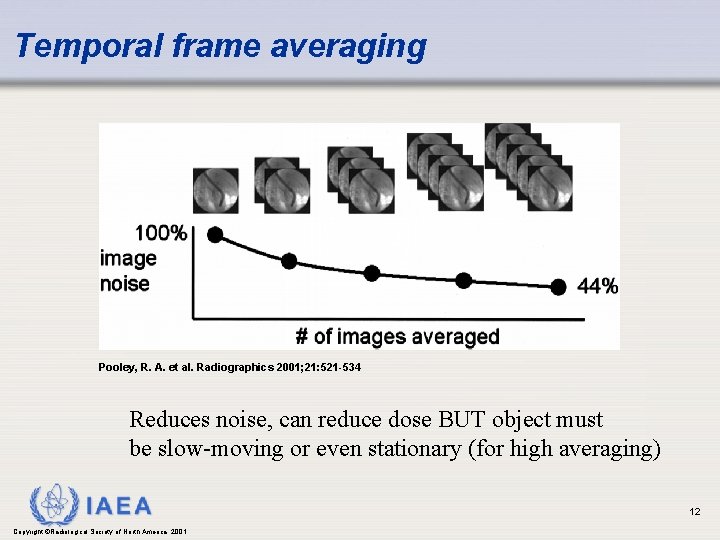
Temporal frame averaging Pooley, R. A. et al. Radiographics 2001; 21: 521 -534 Reduces noise, can reduce dose BUT object must be slow-moving or even stationary (for high averaging) IAEA Copyright ©Radiological Society of North America, 2001 12
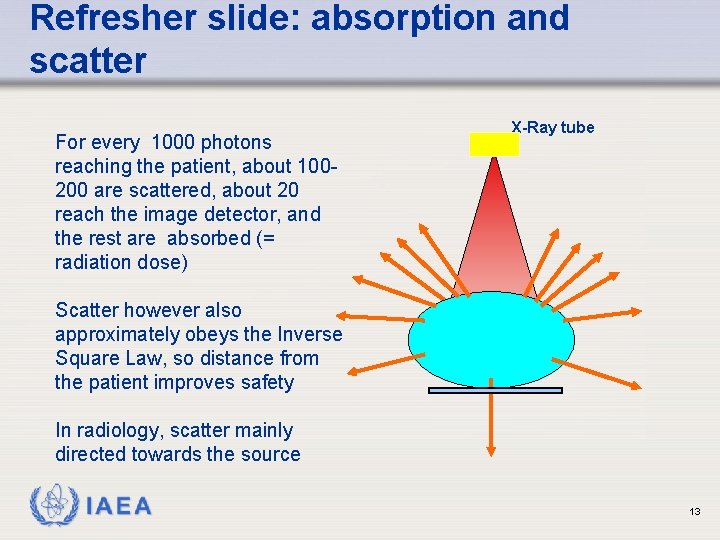
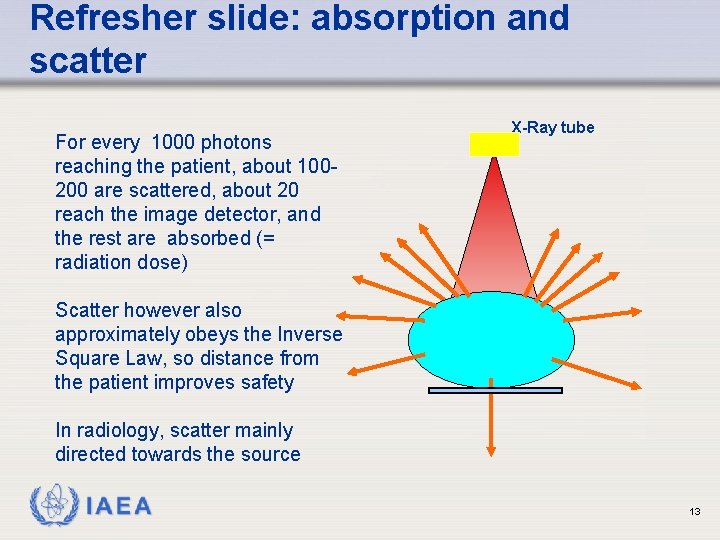
Refresher slide: absorption and scatter For every 1000 photons reaching the patient, about 100200 are scattered, about 20 reach the image detector, and the rest are absorbed (= radiation dose) X-Ray tube Scatter however also approximately obeys the Inverse Square Law, so distance from the patient improves safety In radiology, scatter mainly directed towards the source IAEA 13
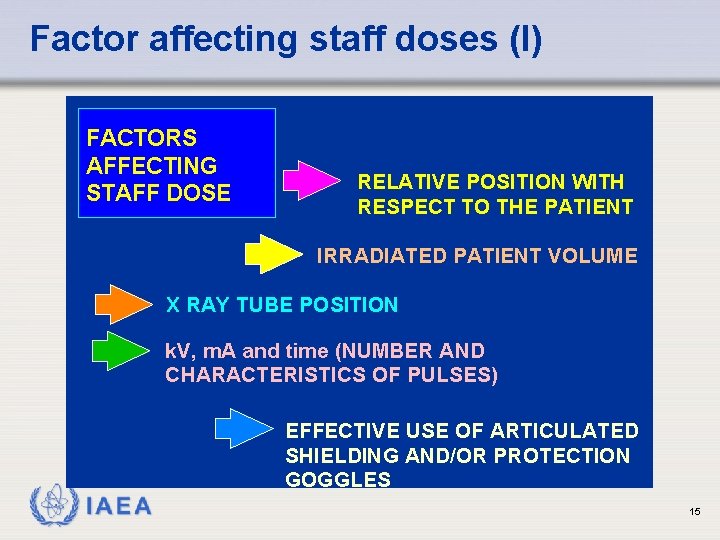
Factors affecting staff doses (I) • The main source of radiation for the staff in a fluoroscopy room is the patient (scattered radiation). • The scattered radiation is not uniform around the patient. • The level of dose rate around the patient is a complex function of a great number of factors. IAEA 14
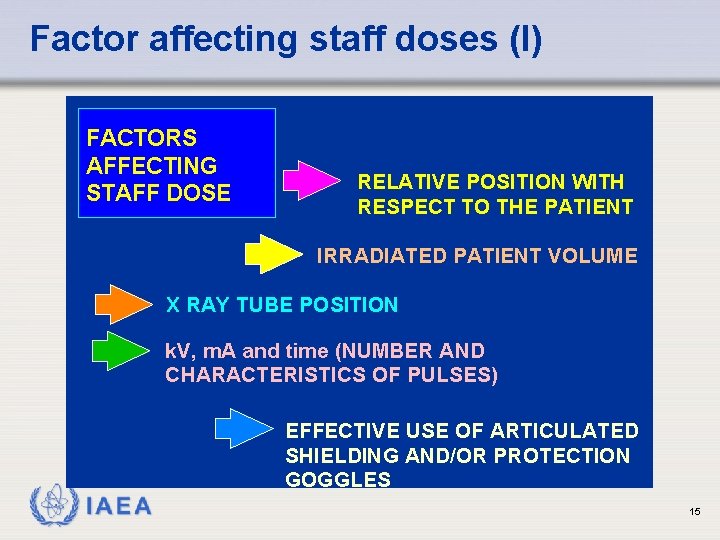
Factor affecting staff doses (I) FACTORS AFFECTING STAFF DOSE RELATIVE POSITION WITH RESPECT TO THE PATIENT IRRADIATED PATIENT VOLUME X RAY TUBE POSITION k. V, m. A and time (NUMBER AND CHARACTERISTICS OF PULSES) EFFECTIVE USE OF ARTICULATED SHIELDING AND/OR PROTECTION GOGGLES IAEA 15
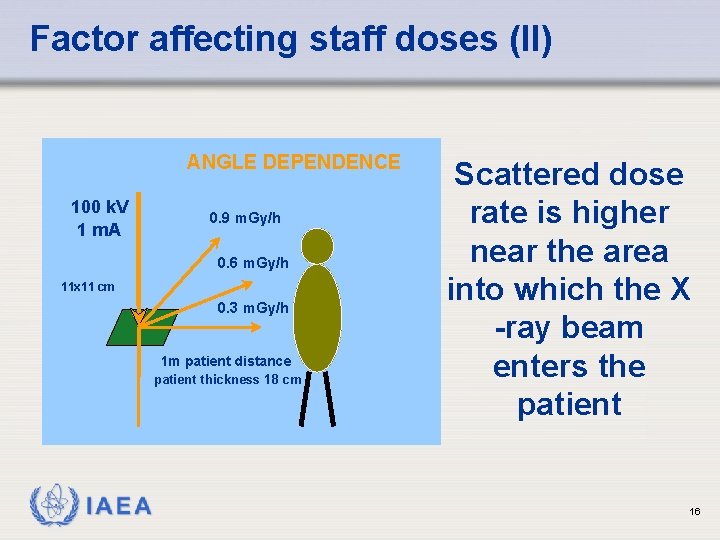
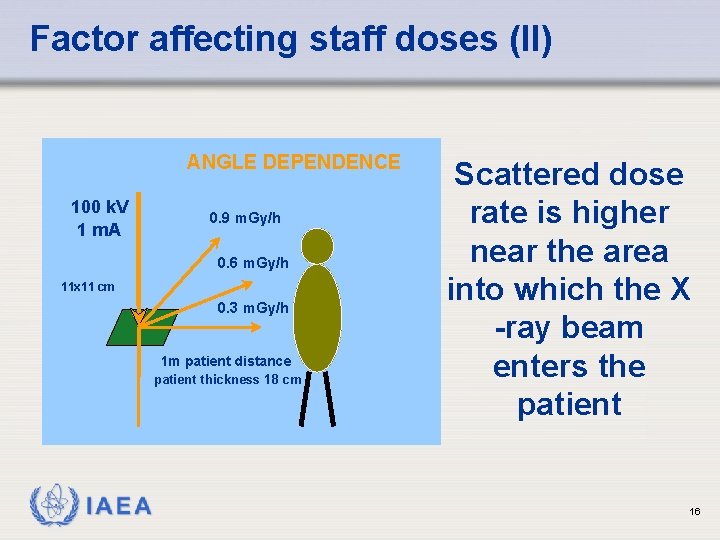
Factor affecting staff doses (II) ANGLE DEPENDENCE 100 k. V 1 m. A 0. 9 m. Gy/h 0. 6 m. Gy/h 11 x 11 cm 0. 3 m. Gy/h 1 m patient distance patient thickness 18 cm IAEA Scattered dose rate is higher near the area into which the X -ray beam enters the patient 16
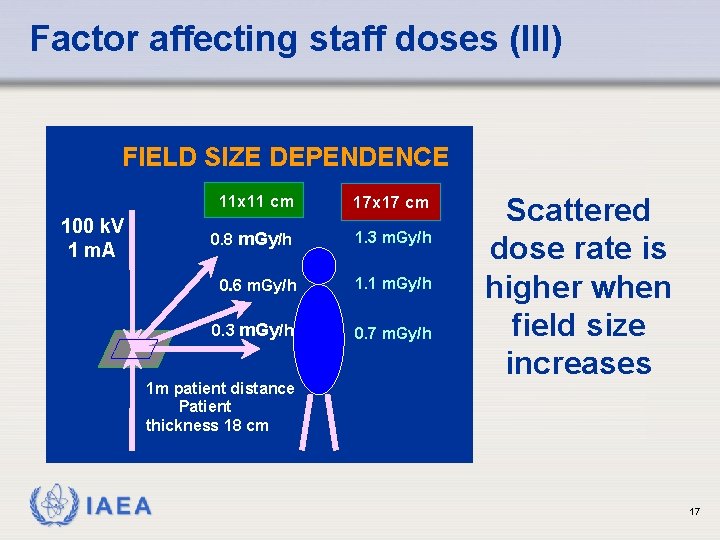
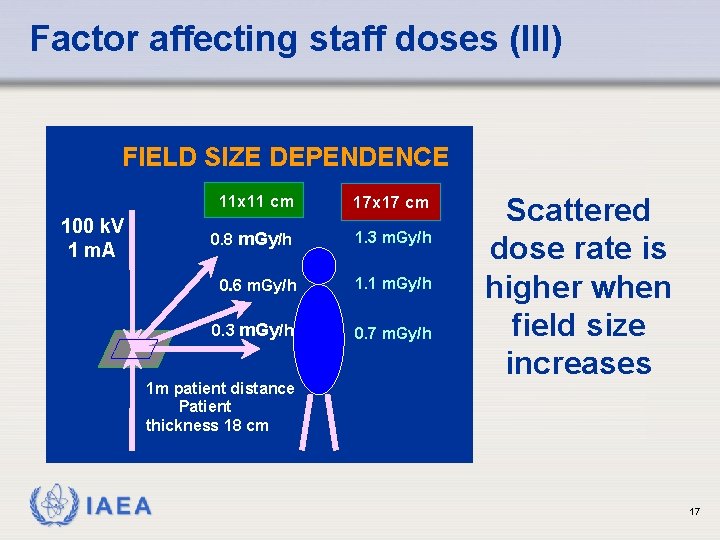
Factor affecting staff doses (III) FIELD SIZE DEPENDENCE 100 k. V 1 m. A 11 x 11 cm 17 x 17 cm 0. 8 m. Gy/h 1. 3 m. Gy/h 0. 6 m. Gy/h 1. 1 m. Gy/h 0. 3 m. Gy/h 0. 7 m. Gy/h 1 m patient distance Patient thickness 18 cm IAEA Scattered dose rate is higher when field size increases 17
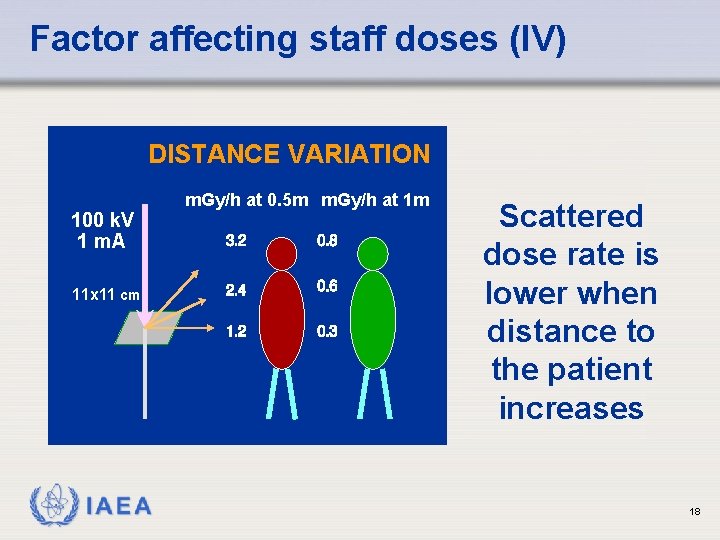
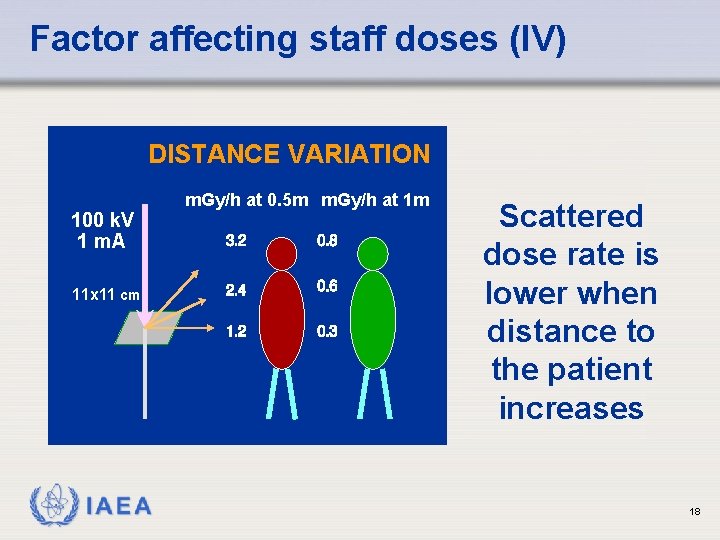
Factor affecting staff doses (IV) DISTANCE VARIATION 100 k. V 1 m. A 11 x 11 cm IAEA m. Gy/h at 0. 5 m m. Gy/h at 1 m Scattered dose rate is lower when distance to the patient increases 18
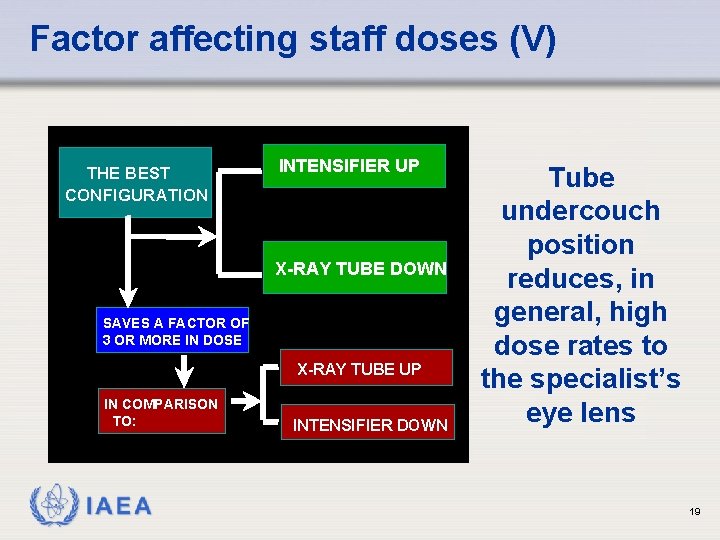
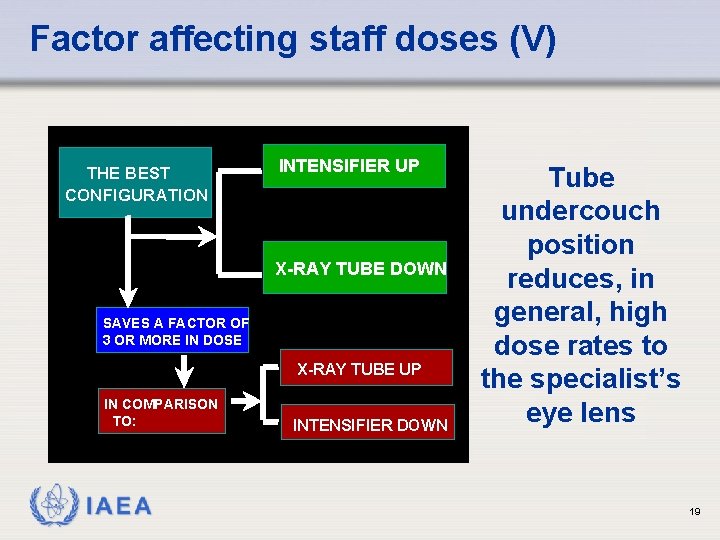
Factor affecting staff doses (V) THE BEST CONFIGURATION INTENSIFIER UP X-RAY TUBE DOWN SAVES A FACTOR OF 3 OR MORE IN DOSE X-RAY TUBE UP IN COMPARISON TO: IAEA INTENSIFIER DOWN Tube undercouch position reduces, in general, high dose rates to the specialist’s eye lens 19
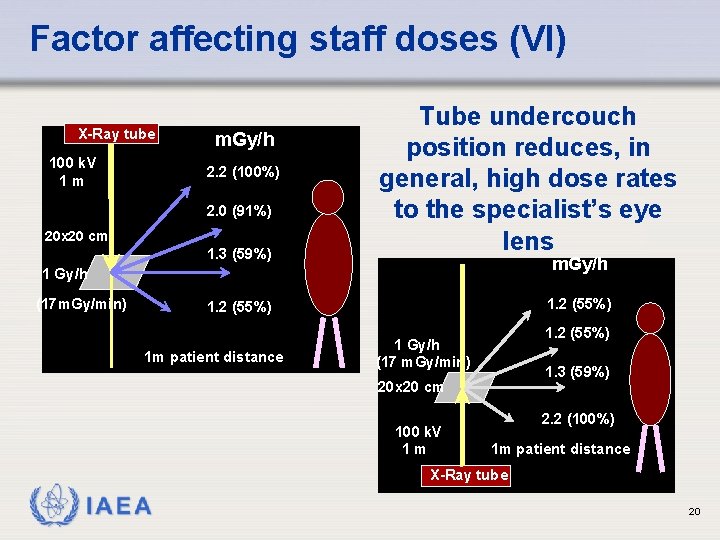
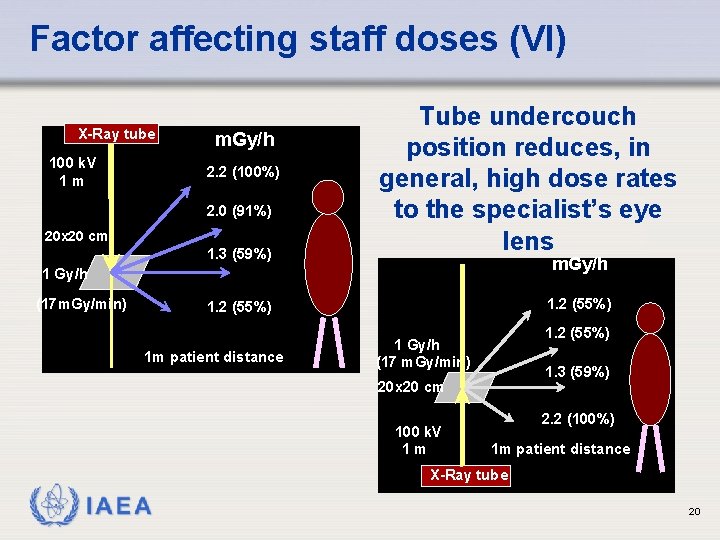
Factor affecting staff doses (VI) X-Ray tube 100 k. V 1 m m. Gy/h 2. 2 (100%) 2. 0 (91%) 20 x 20 cm 1. 3 (59%) Tube undercouch position reduces, in general, high dose rates to the specialist’s eye lens m. Gy/h 1 Gy/h (17 m. Gy/min) 1. 2 (55%) 1 m patient distance 1. 2 (55%) 1 Gy/h (17 m. Gy/min) 1. 3 (59%) 20 x 20 cm 100 k. V 1 m 2. 2 (100%) 1 m patient distance X-Ray tube IAEA 20
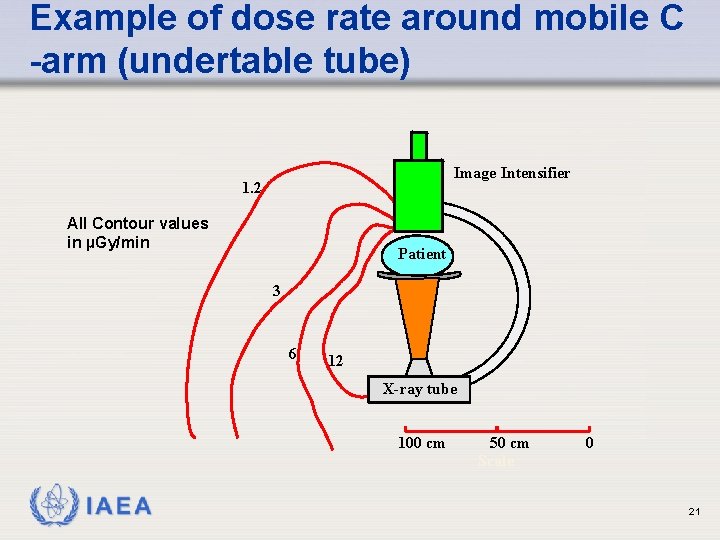
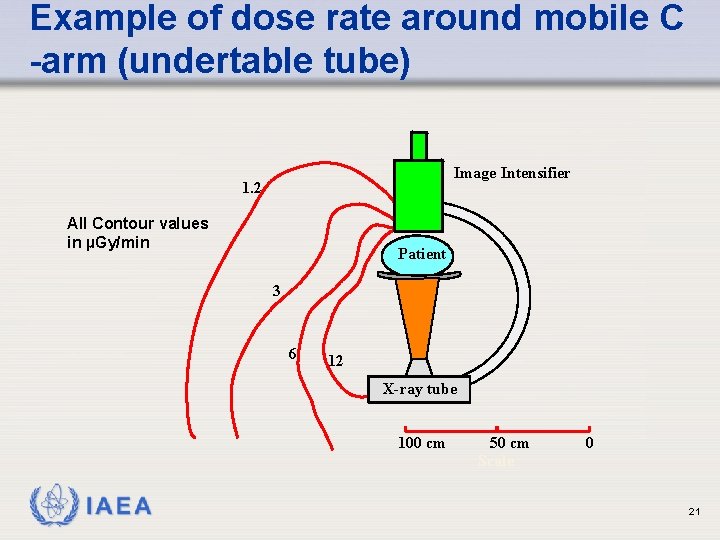
Example of dose rate around mobile C -arm (undertable tube) Image Intensifier 1. 2 All Contour values in µGy/min Patient 3 6 12 X-ray tube 100 cm IAEA 50 cm Scale 0 21
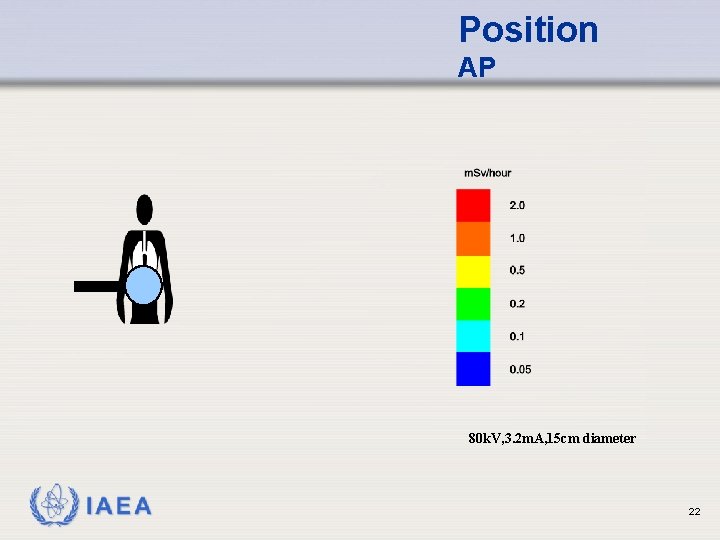
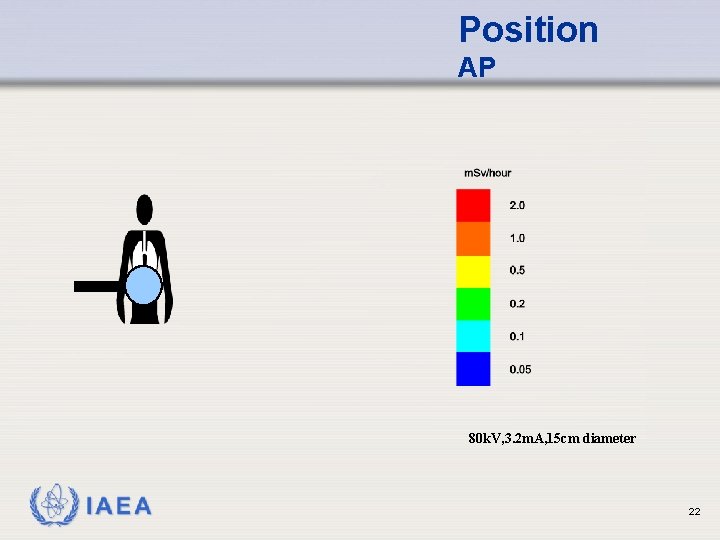
Position AP 80 k. V, 3. 2 m. A, 15 cm diameter IAEA 22
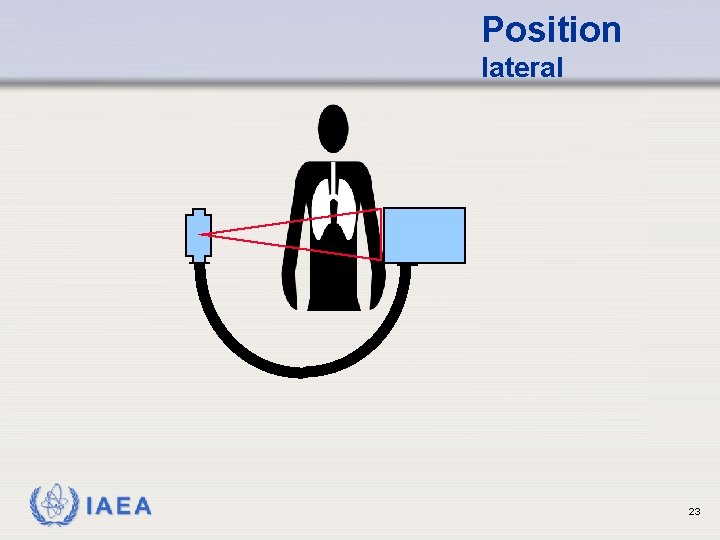
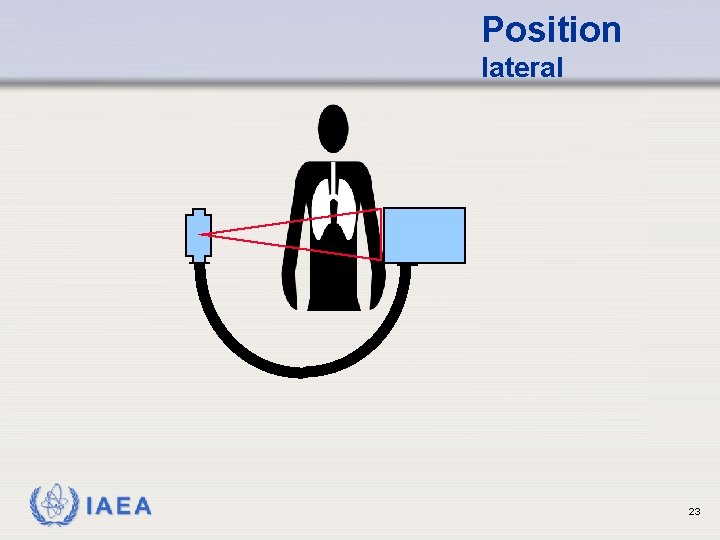
Position lateral IAEA 23
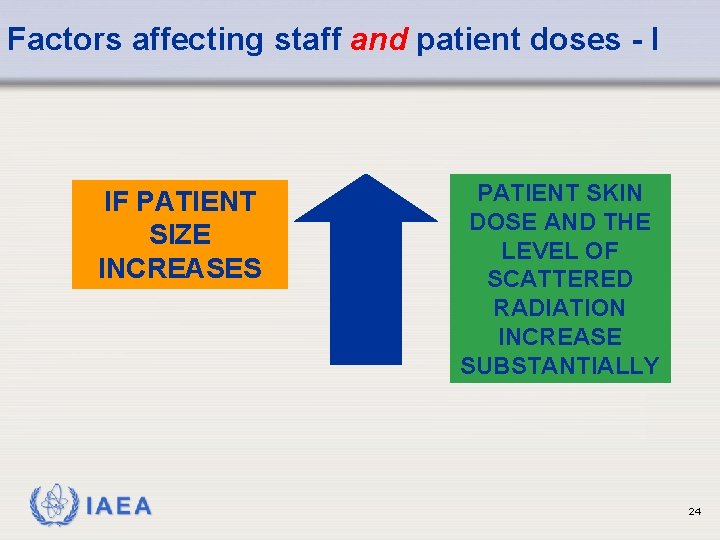
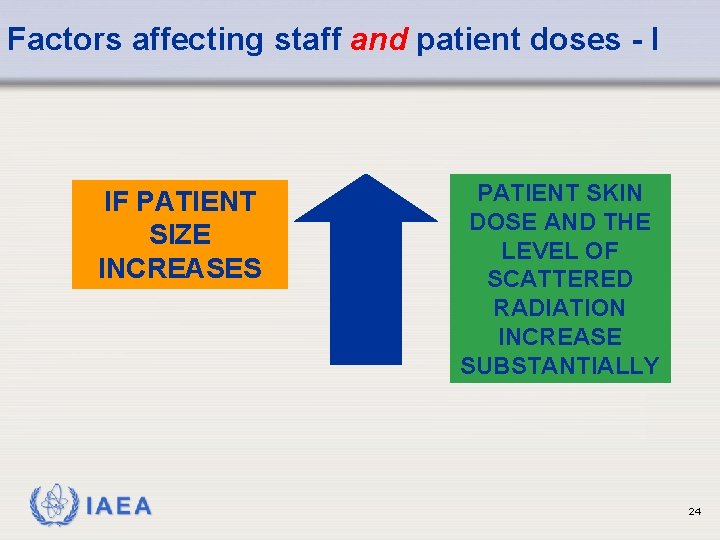
Factors affecting staff and patient doses - I IF PATIENT SIZE INCREASES IAEA PATIENT SKIN DOSE AND THE LEVEL OF SCATTERED RADIATION INCREASE SUBSTANTIALLY 24
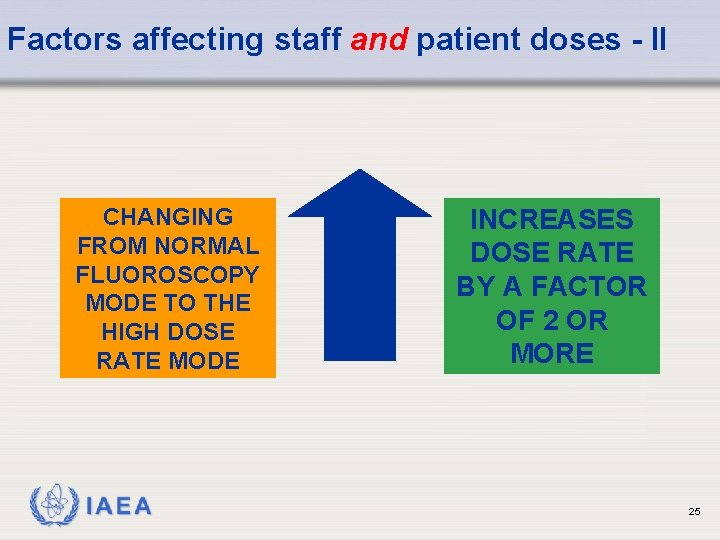
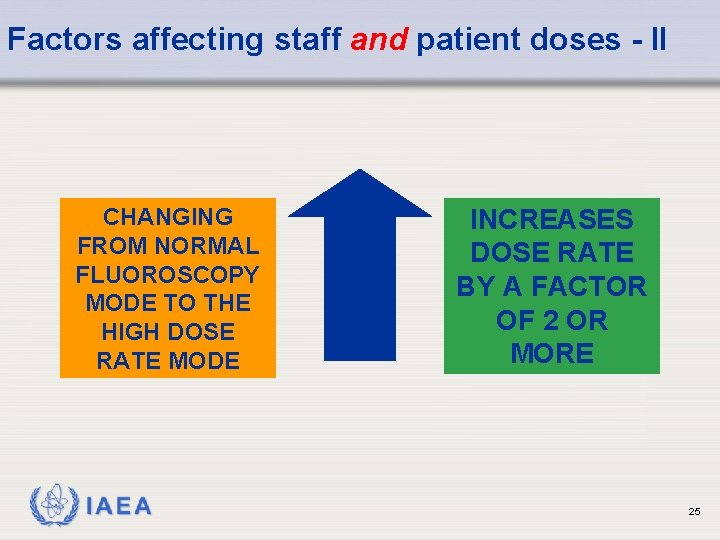
Factors affecting staff and patient doses - II CHANGING FROM NORMAL FLUOROSCOPY MODE TO THE HIGH DOSE RATE MODE IAEA INCREASES DOSE RATE BY A FACTOR OF 2 OR MORE 25
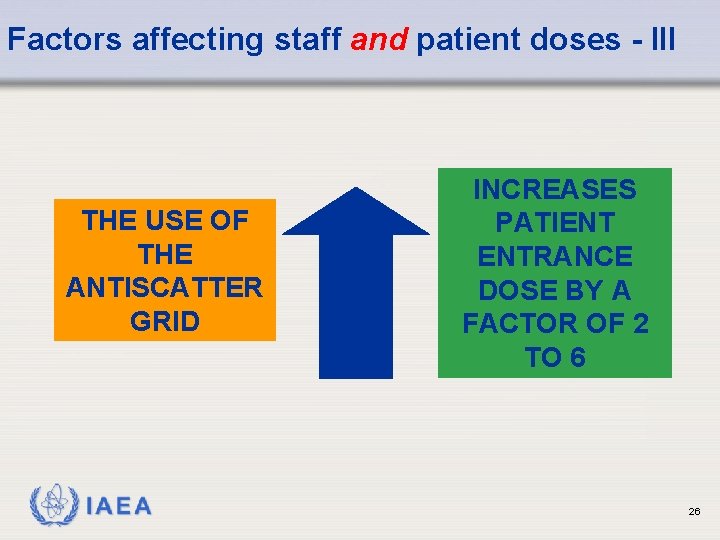
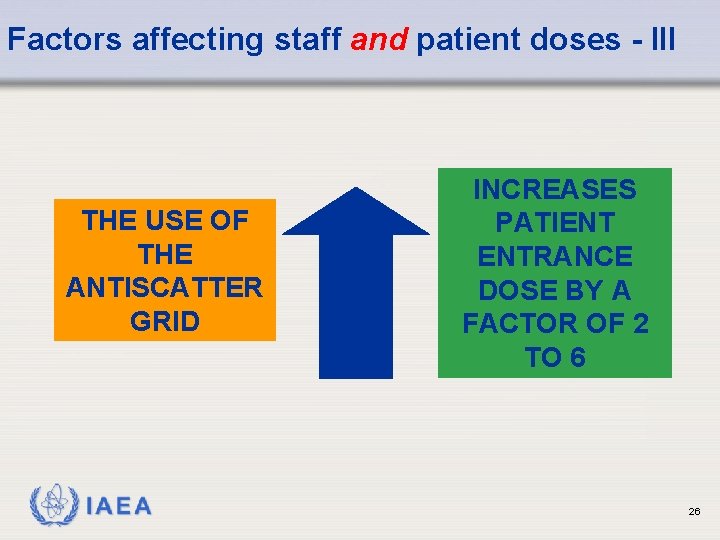
Factors affecting staff and patient doses - III THE USE OF THE ANTISCATTER GRID IAEA INCREASES PATIENT ENTRANCE DOSE BY A FACTOR OF 2 TO 6 26
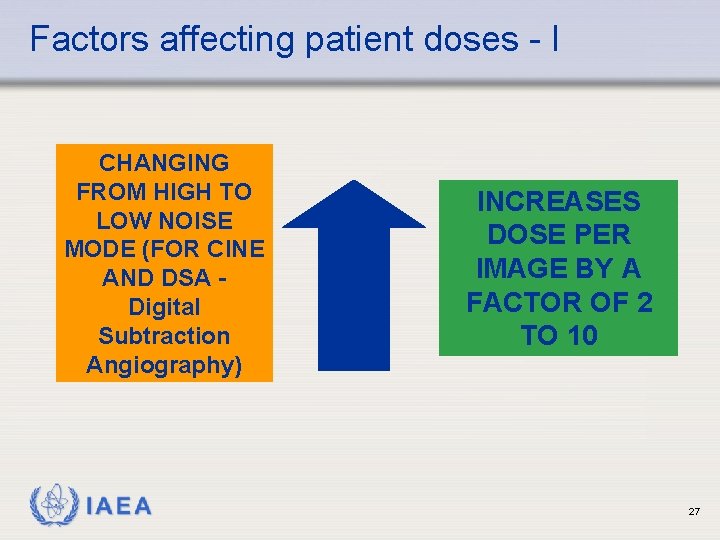
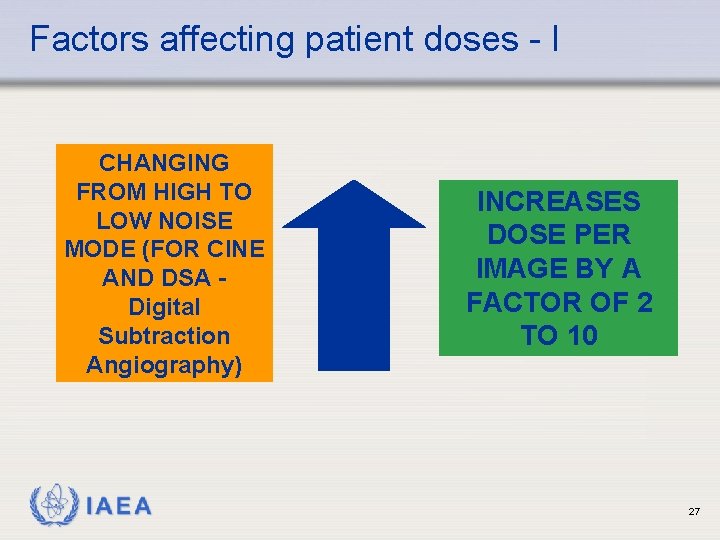
Factors affecting patient doses - I CHANGING FROM HIGH TO LOW NOISE MODE (FOR CINE AND DSA Digital Subtraction Angiography) IAEA INCREASES DOSE PER IMAGE BY A FACTOR OF 2 TO 10 27
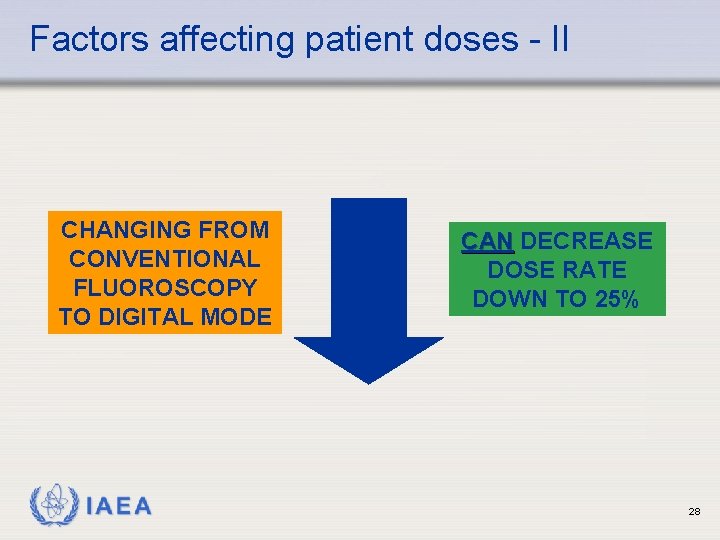
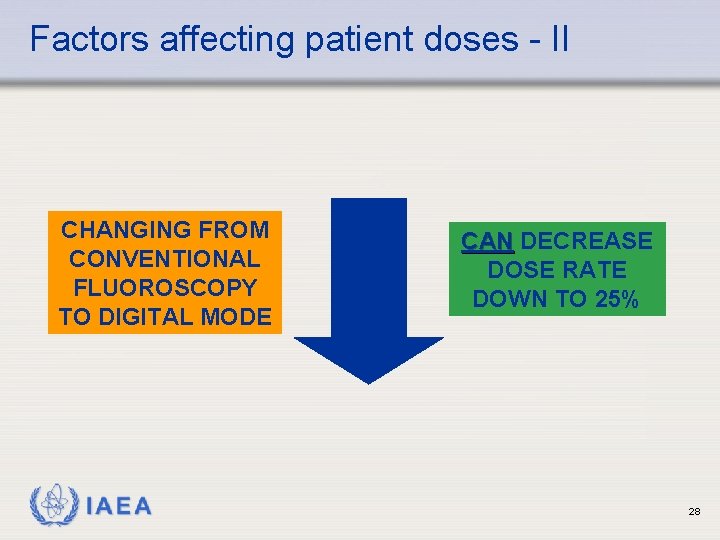
Factors affecting patient doses - II CHANGING FROM CONVENTIONAL FLUOROSCOPY TO DIGITAL MODE IAEA CAN DECREASE DOSE RATE DOWN TO 25% 28
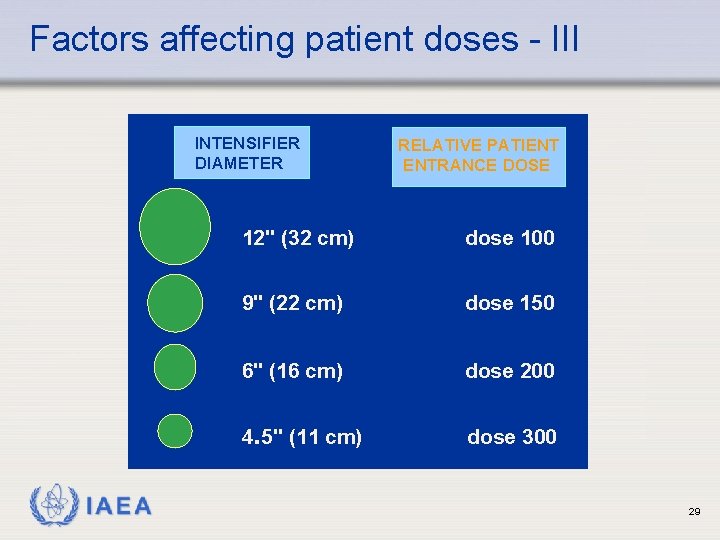
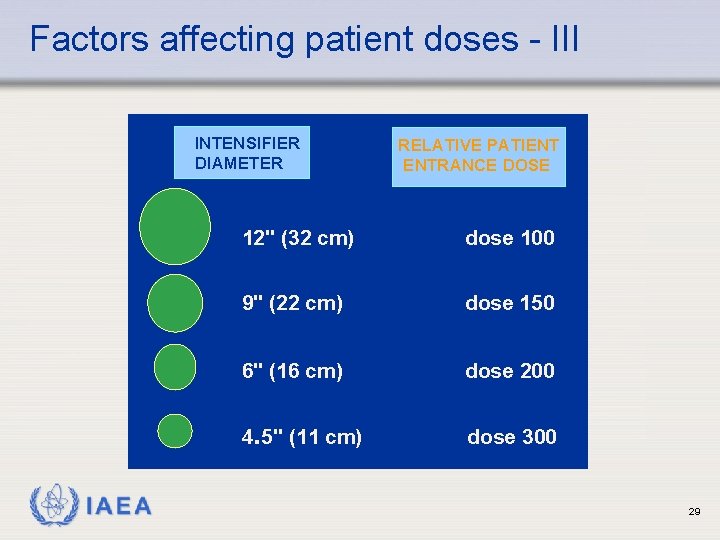
Factors affecting patient doses - III INTENSIFIER DIAMETER IAEA RELATIVE PATIENT ENTRANCE DOSE 12" (32 cm) dose 100 9" (22 cm) dose 150 6" (16 cm) dose 200 4. 5" (11 cm) dose 300 29
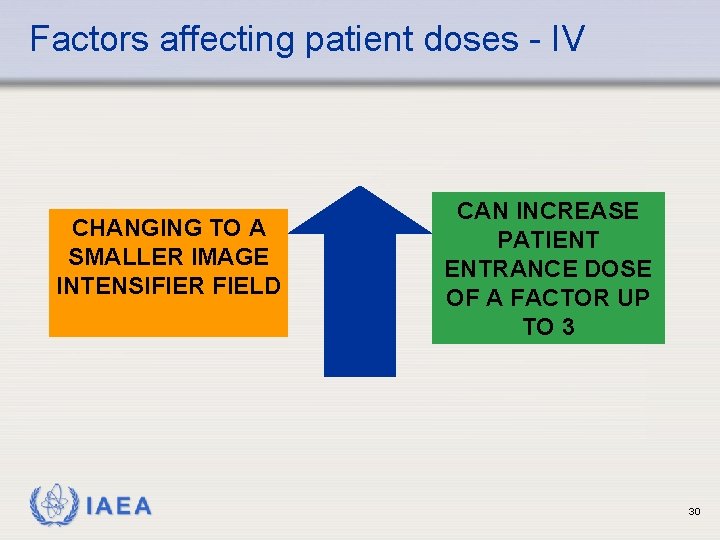
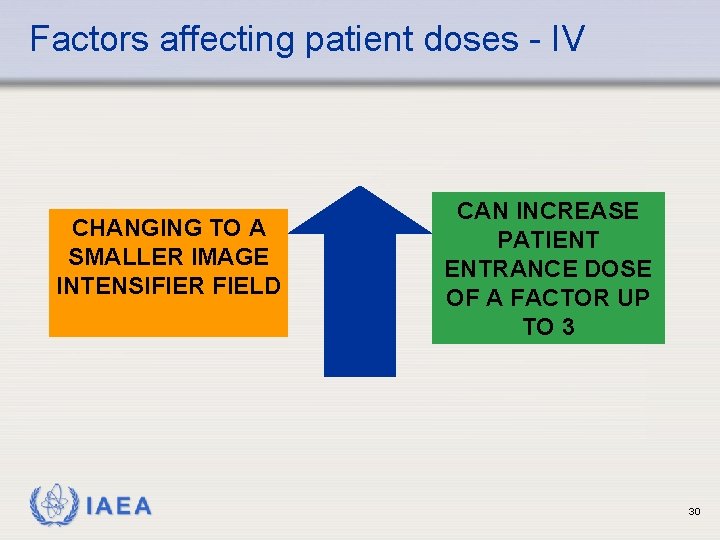
Factors affecting patient doses - IV CHANGING TO A SMALLER IMAGE INTENSIFIER FIELD IAEA CAN INCREASE PATIENT ENTRANCE DOSE OF A FACTOR UP TO 3 30
Example of entrance dose rate in fluoroscopy LOW DOSE MODE 10 m. Gy/min MEDIUM DOSE MODE 20 m. Gy/min HIGH DOSE MODE 40 m. Gy/min BE AWARE OF YOUR OWN UNIT’S DOSES! (if digital, these will probably be displayed in real time) IAEA 31
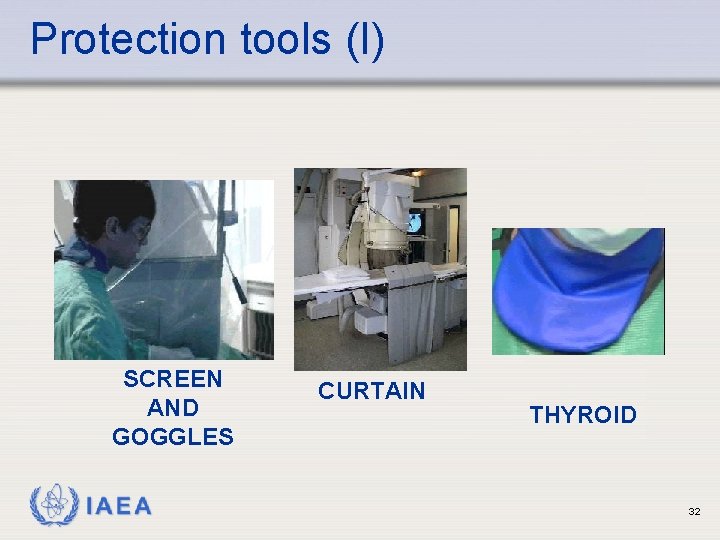
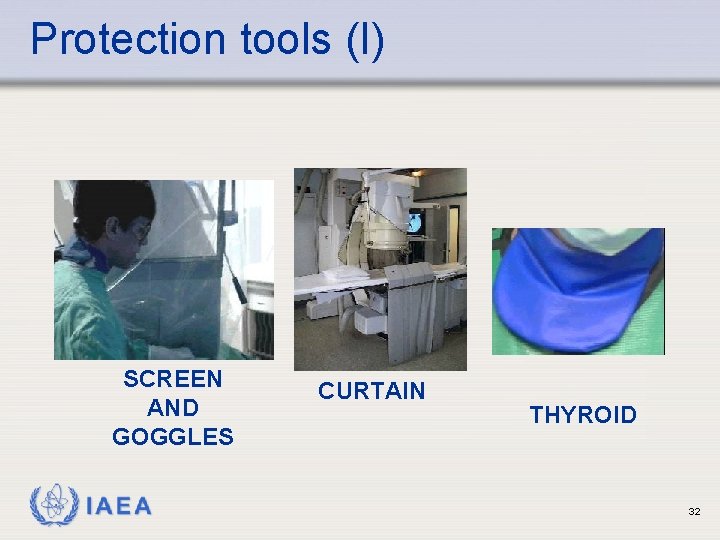
Protection tools (I) SCREEN AND GOGGLES IAEA CURTAIN THYROID 32
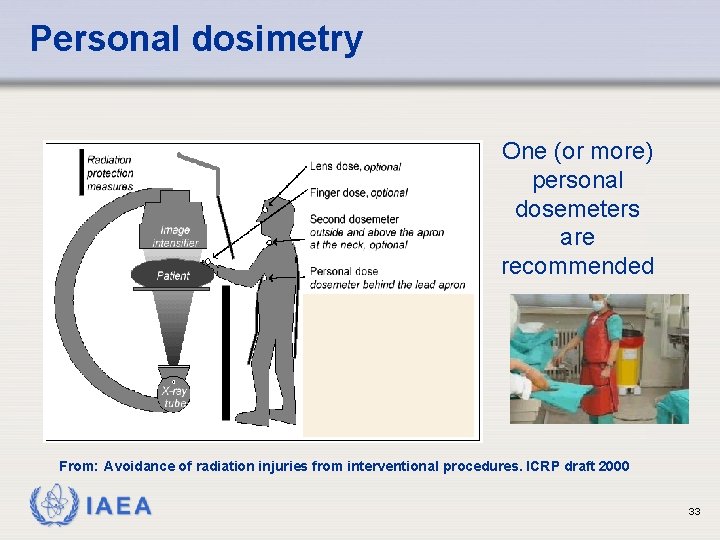
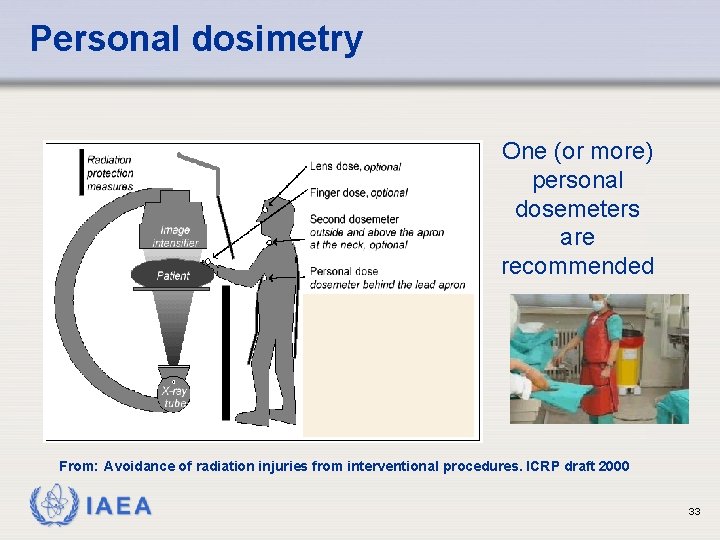
Personal dosimetry One (or more) personal dosemeters are recommended From: Avoidance of radiation injuries from interventional procedures. ICRP draft 2000 IAEA 33
To control dose to the staff in fluoroscopy ß Personnel must know how to position themselves and the machines for minimum dose. ß If the beam is horizontal, or near horizontal, the operator should stand on the image intensifier side [to reduce dose]. ß If the beam is vertical, or near vertical, keep the tube under the patient. IAEA 34
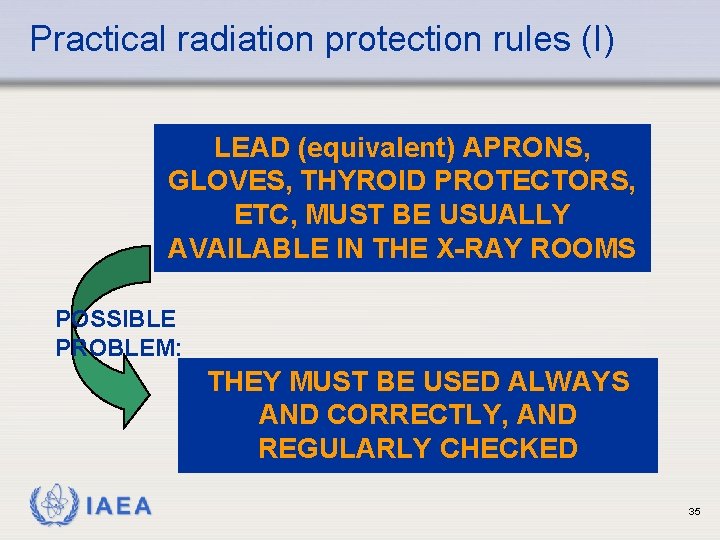
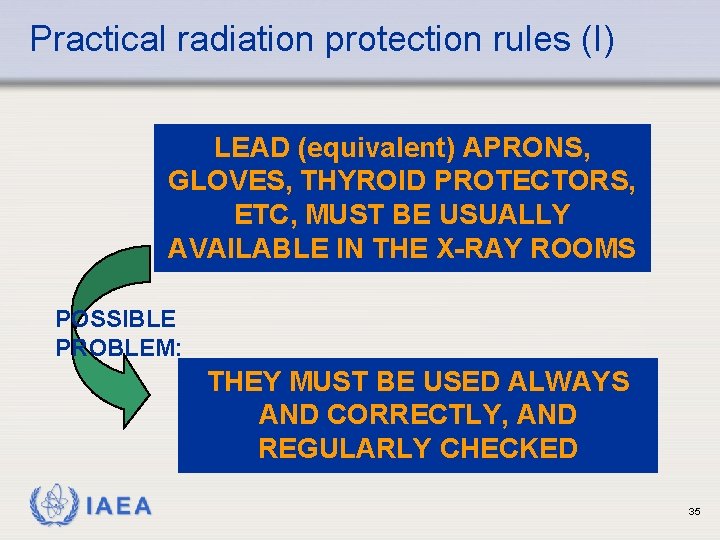
Practical radiation protection rules (I) LEAD (equivalent) APRONS, GLOVES, THYROID PROTECTORS, ETC, MUST BE USUALLY AVAILABLE IN THE X-RAY ROOMS POSSIBLE PROBLEM: THEY MUST BE USED ALWAYS AND CORRECTLY, AND REGULARLY CHECKED IAEA 35
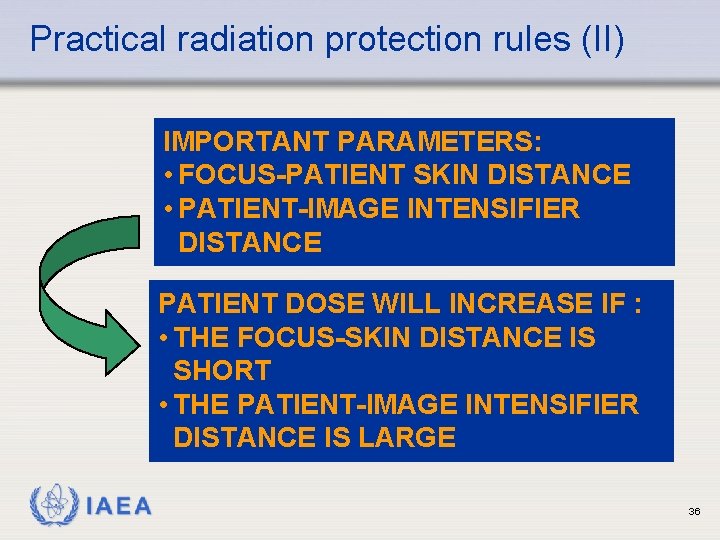
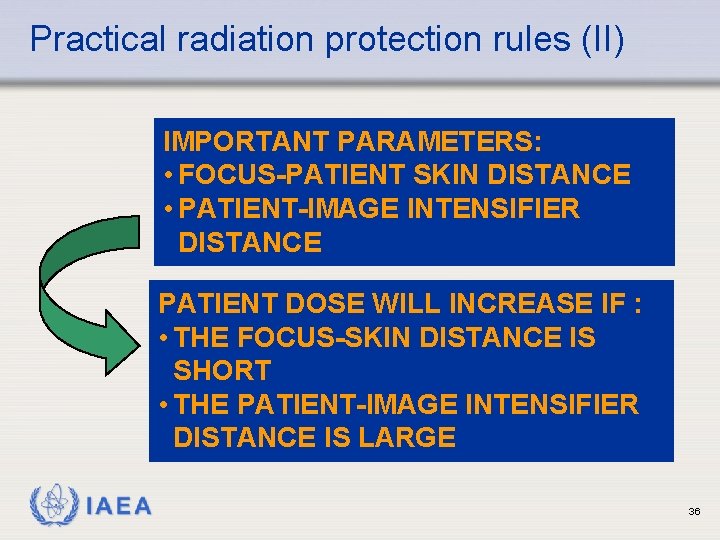
Practical radiation protection rules (II) IMPORTANT PARAMETERS: • FOCUS-PATIENT SKIN DISTANCE • PATIENT-IMAGE INTENSIFIER DISTANCE PATIENT DOSE WILL INCREASE IF : • THE FOCUS-SKIN DISTANCE IS SHORT • THE PATIENT-IMAGE INTENSIFIER DISTANCE IS LARGE IAEA 36
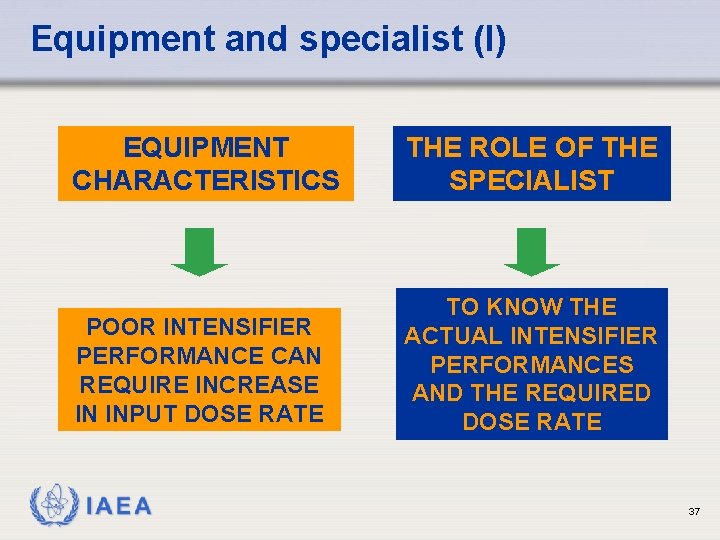
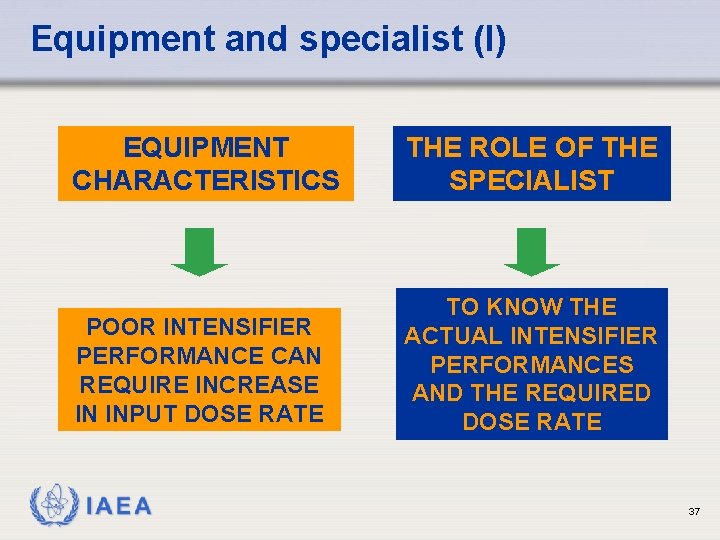
Equipment and specialist (I) EQUIPMENT CHARACTERISTICS THE ROLE OF THE SPECIALIST POOR INTENSIFIER PERFORMANCE CAN REQUIRE INCREASE IN INPUT DOSE RATE TO KNOW THE ACTUAL INTENSIFIER PERFORMANCES AND THE REQUIRED DOSE RATE IAEA 37
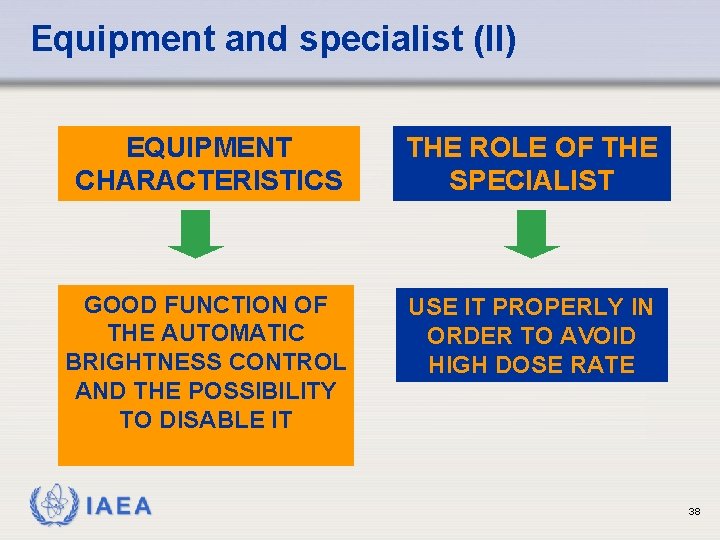
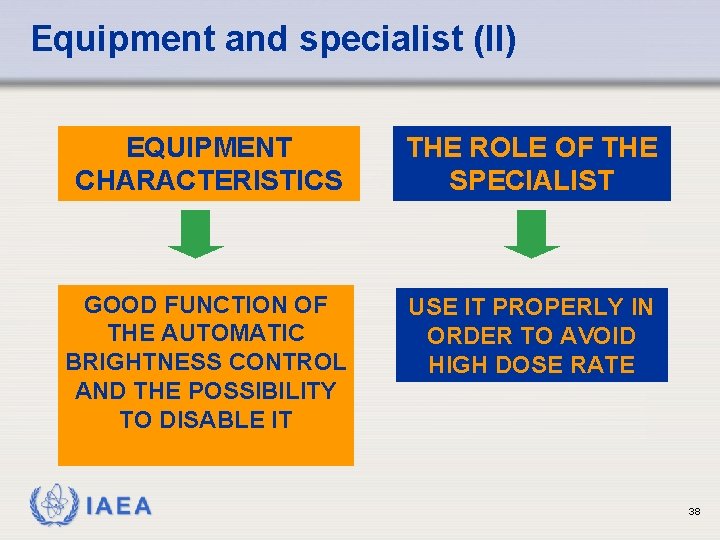
Equipment and specialist (II) EQUIPMENT CHARACTERISTICS THE ROLE OF THE SPECIALIST GOOD FUNCTION OF THE AUTOMATIC BRIGHTNESS CONTROL AND THE POSSIBILITY TO DISABLE IT USE IT PROPERLY IN ORDER TO AVOID HIGH DOSE RATE IAEA 38
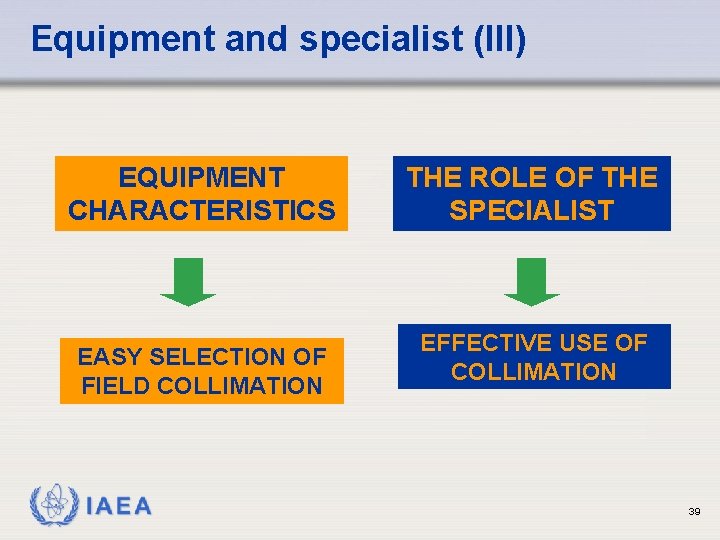
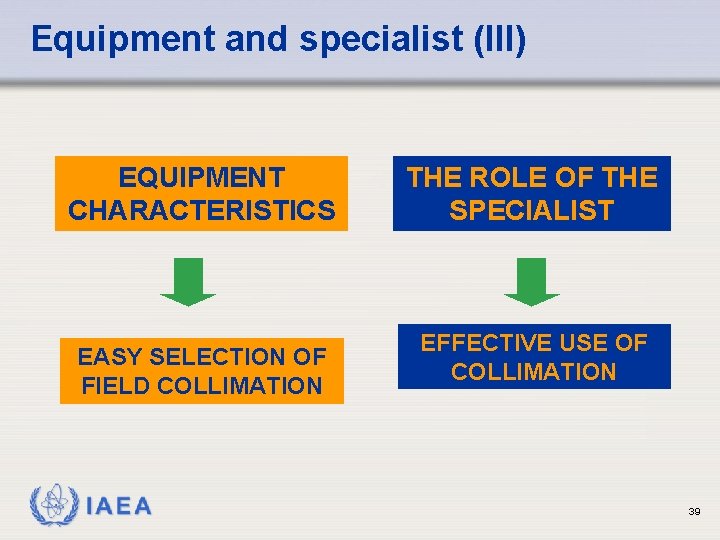
Equipment and specialist (III) EQUIPMENT CHARACTERISTICS EASY SELECTION OF FIELD COLLIMATION IAEA THE ROLE OF THE SPECIALIST EFFECTIVE USE OF COLLIMATION 39
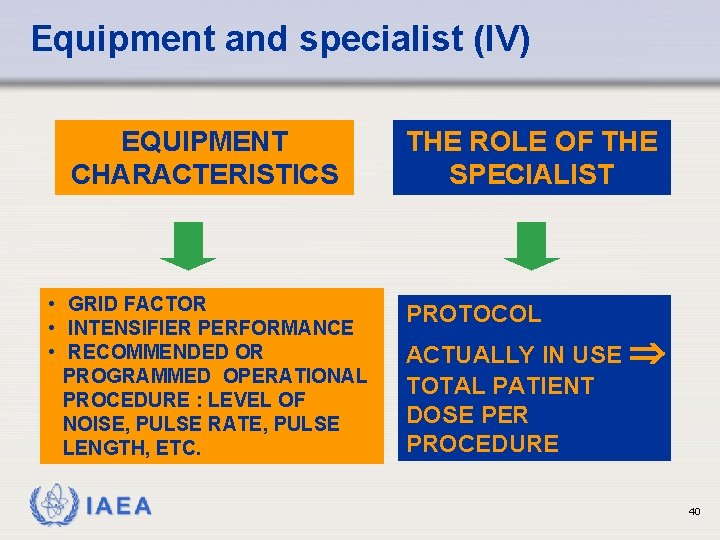
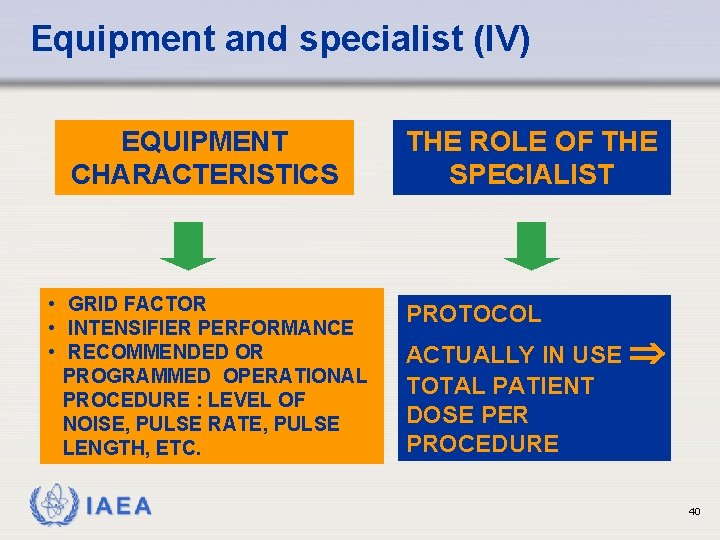
Equipment and specialist (IV) EQUIPMENT CHARACTERISTICS • GRID FACTOR • INTENSIFIER PERFORMANCE • RECOMMENDED OR PROGRAMMED OPERATIONAL PROCEDURE : LEVEL OF NOISE, PULSE RATE, PULSE LENGTH, ETC. IAEA THE ROLE OF THE SPECIALIST PROTOCOL ACTUALLY IN USE TOTAL PATIENT DOSE PER PROCEDURE 40
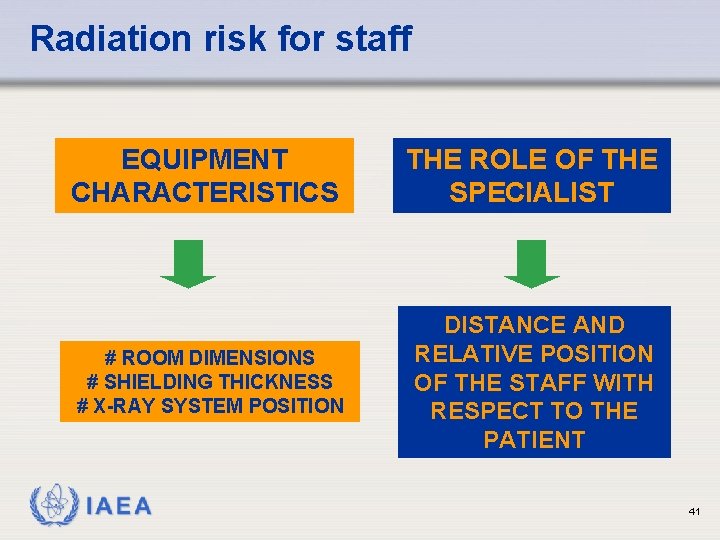
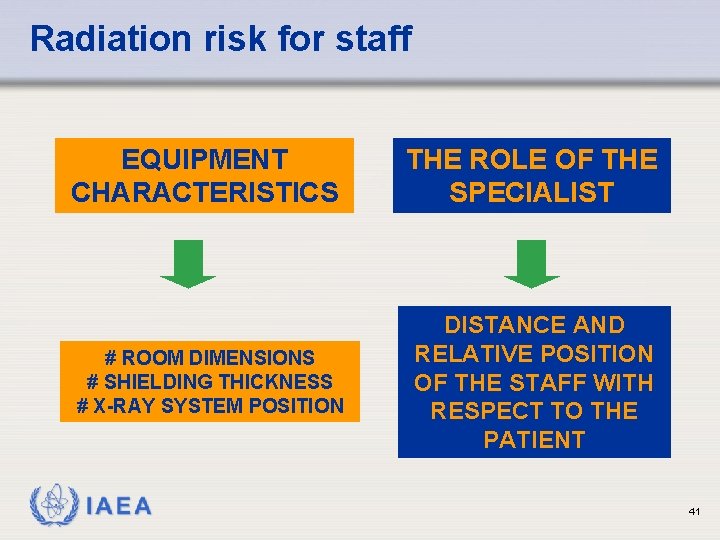
Radiation risk for staff EQUIPMENT CHARACTERISTICS THE ROLE OF THE SPECIALIST # ROOM DIMENSIONS # SHIELDING THICKNESS # X-RAY SYSTEM POSITION DISTANCE AND RELATIVE POSITION OF THE STAFF WITH RESPECT TO THE PATIENT IAEA 41
Particular Issues for Interventional Radiology IAEA International Atomic Energy Agency
Principle of Interventional Radiology • Interventional radiology (fluoroscopically-guided) techniques are being used by an increasing number of clinicians not adequately trained in radiation safety or radiobiology • Patients are suffering radiation-induced skin injuries due to unnecessarily high radiation doses. • Younger patients may face an increased risk of future cancer IAEA 43
Principle of Interventional Radiology • Many interventionists are not aware of the potential for injury from procedures, their occurrence or the simple methods for decreasing their incidence utilising dose control strategies. • Many patients are not being counselled on the radiation risks, nor followed up for the onset of injury, when radiation doses from difficult procedures may lead to injury. IAEA 44
Principle of Interventional Radiology • Interventionalists who are not “dose aware” may have their practice limited or suffer injury, and are exposing their staff to high doses. • Occupational doses can be reduced by reducing unnecessary patient dose, the correct use and procurement of equipment (including the use of shielding devices). IAEA 45
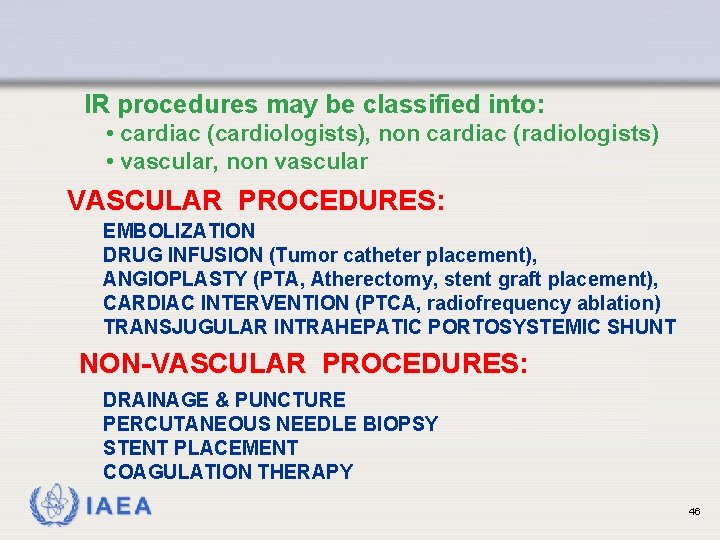
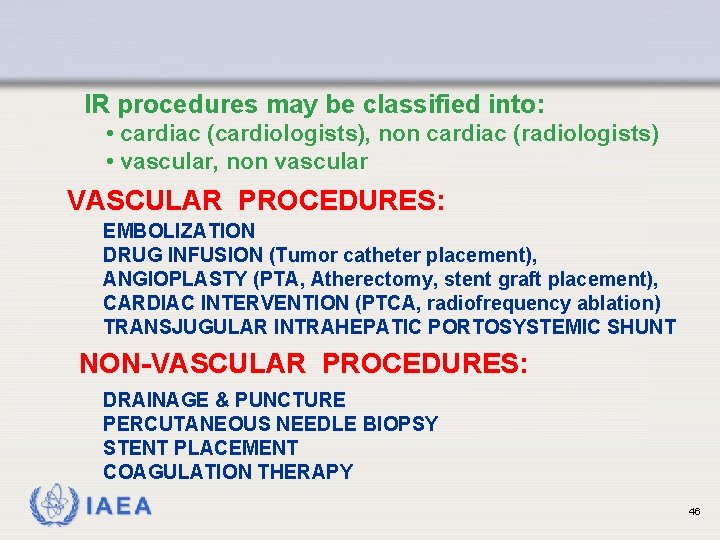
IR procedures may be classified into: • cardiac (cardiologists), non cardiac (radiologists) • vascular, non vascular VASCULAR PROCEDURES: EMBOLIZATION DRUG INFUSION (Tumor catheter placement), ANGIOPLASTY (PTA, Atherectomy, stent graft placement), CARDIAC INTERVENTION (PTCA, radiofrequency ablation) TRANSJUGULAR INTRAHEPATIC PORTOSYSTEMIC SHUNT NON-VASCULAR PROCEDURES: DRAINAGE & PUNCTURE PERCUTANEOUS NEEDLE BIOPSY STENT PLACEMENT COAGULATION THERAPY IAEA 46
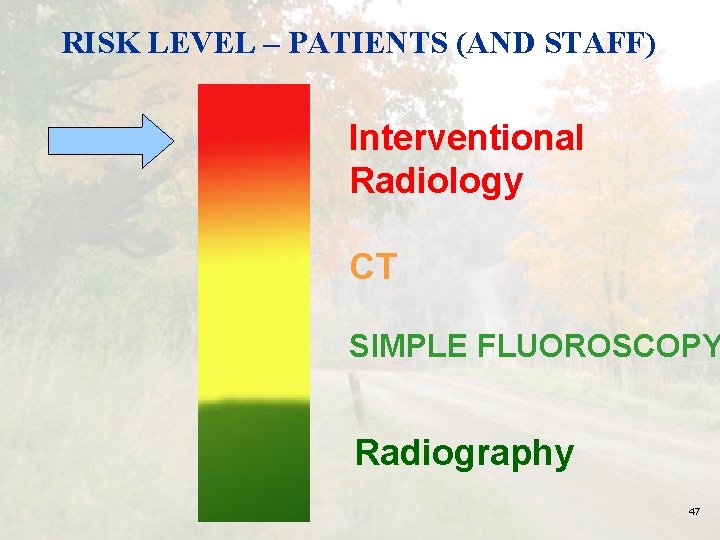
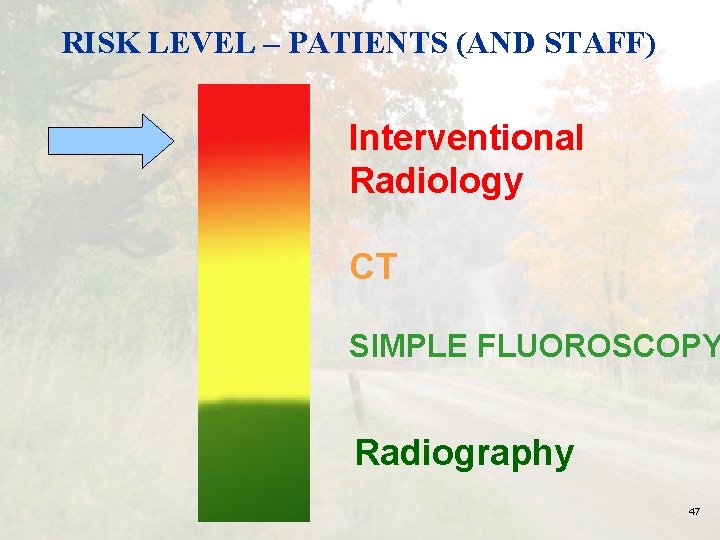
RISK LEVEL – PATIENTS (AND STAFF) Interventional Radiology CT SIMPLE FLUOROSCOPY Radiography IAEA 47
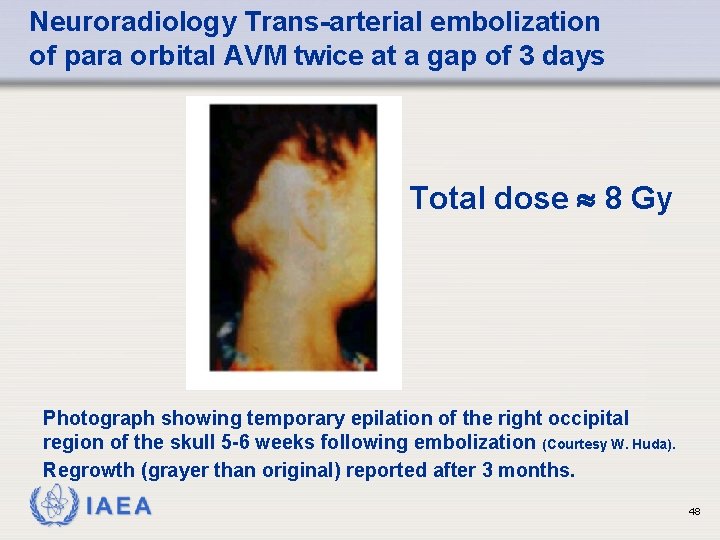
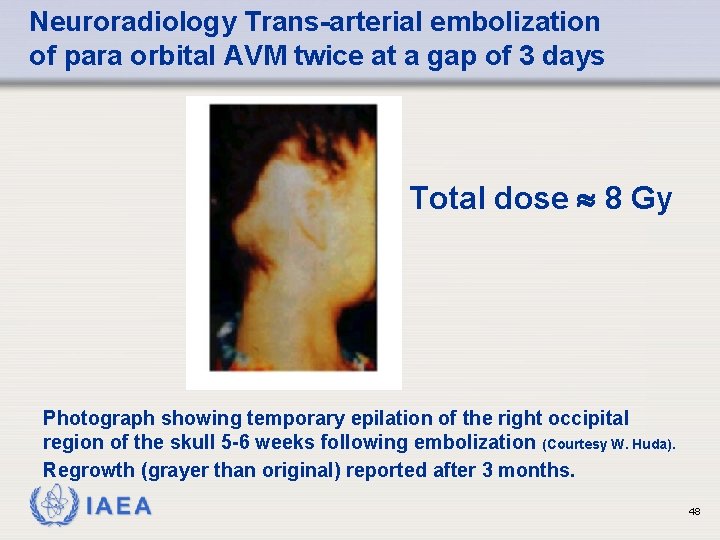
Neuroradiology Trans-arterial embolization of para orbital AVM twice at a gap of 3 days Total dose 8 Gy Photograph showing temporary epilation of the right occipital region of the skull 5 -6 weeks following embolization (Courtesy W. Huda). Regrowth (grayer than original) reported after 3 months. IAEA 48
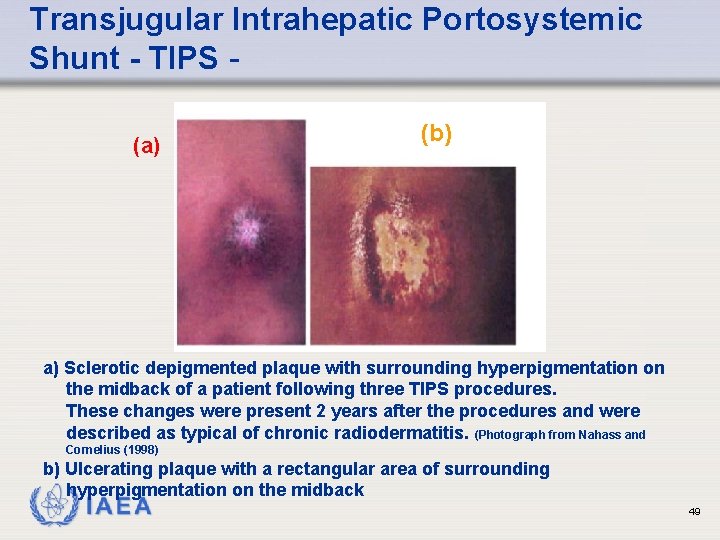
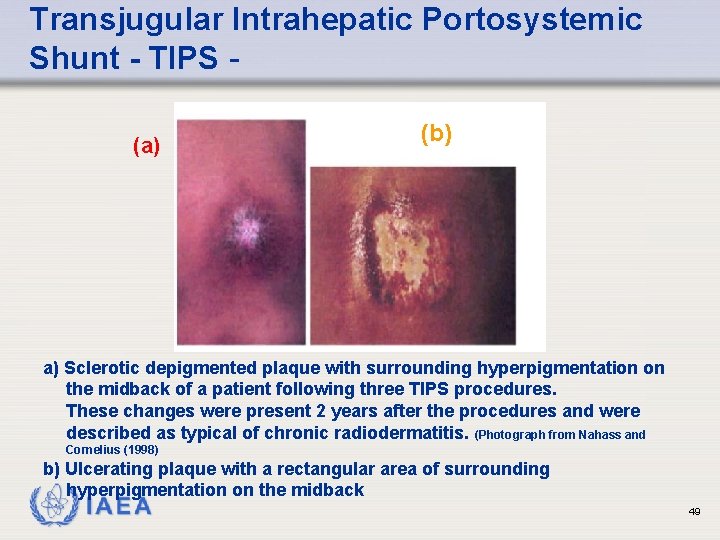
Transjugular Intrahepatic Portosystemic Shunt - TIPS (a) (b) a) Sclerotic depigmented plaque with surrounding hyperpigmentation on the midback of a patient following three TIPS procedures. These changes were present 2 years after the procedures and were described as typical of chronic radiodermatitis. (Photograph from Nahass and Cornelius (1998) b) Ulcerating plaque with a rectangular area of surrounding hyperpigmentation on the midback IAEA 49
Many of these injuries are avoidable – ALL of the serious ones are! IAEA 50
Why do they occur? No training in radiation protection for those performing these studies, like: • Cardiologist • Urologist • Gastro-enterologist • Orthopedic Surgeon • Vascular Surgeon • Traumatologist • Pediatrician • Anesthesiologist IAEA 51
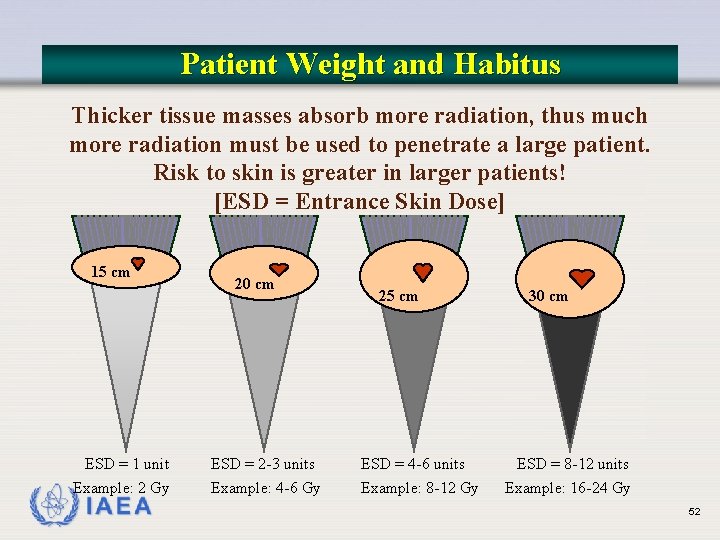
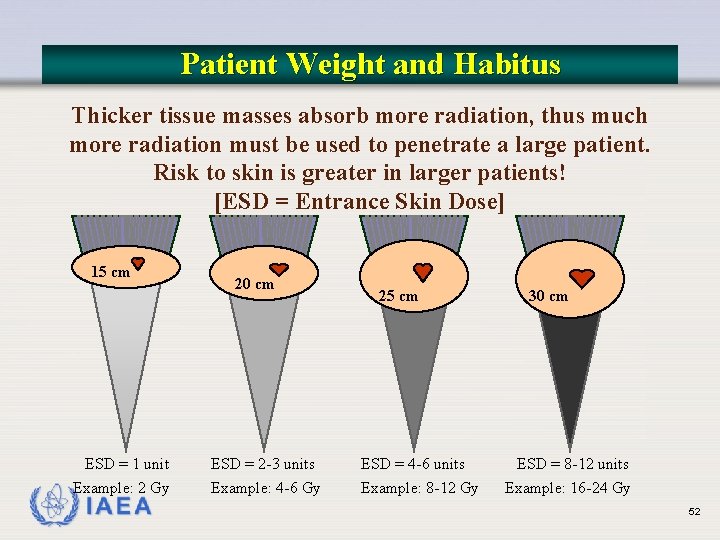
Patient Weight and Habitus Thicker tissue masses absorb more radiation, thus much more radiation must be used to penetrate a large patient. Risk to skin is greater in larger patients! [ESD = Entrance Skin Dose] 15 cm ESD = 1 unit Example: 2 Gy IAEA 20 cm ESD = 2 -3 units Example: 4 -6 Gy 25 cm ESD = 4 -6 units Example: 8 -12 Gy 30 cm ESD = 8 -12 units Example: 16 -24 Gy 52
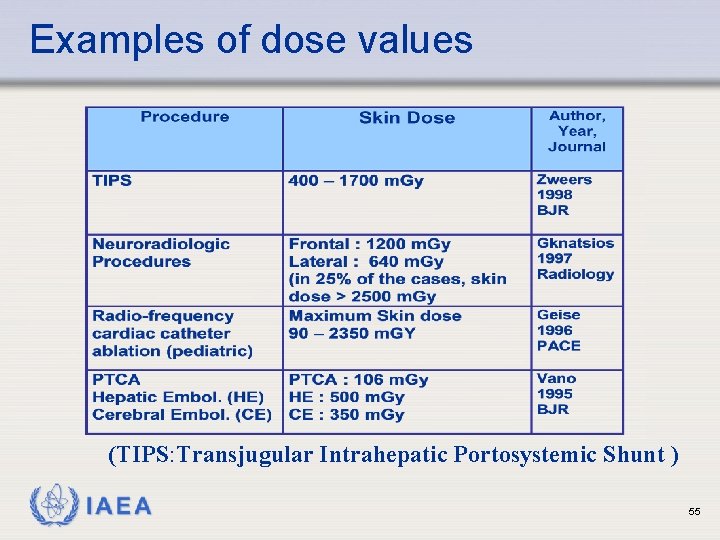
Topic 5: Examples of dose values IAEA International Atomic Energy Agency
Examples of dose values IAEA 54
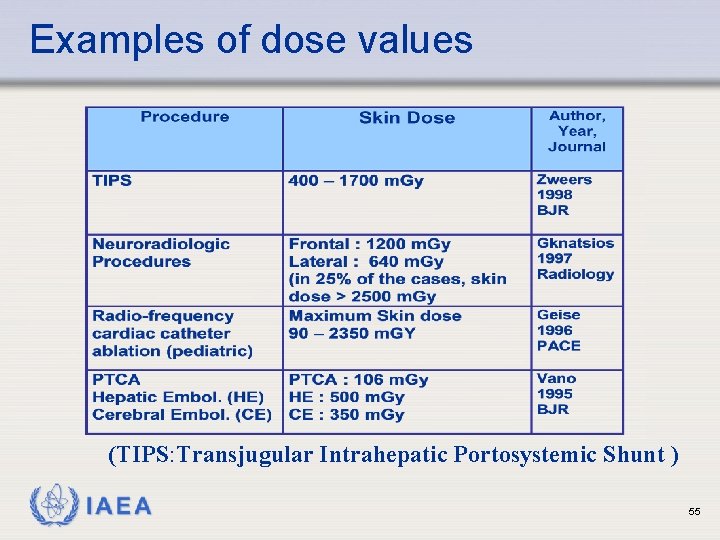
Examples of dose values (TIPS: Transjugular Intrahepatic Portosystemic Shunt ) IAEA 55
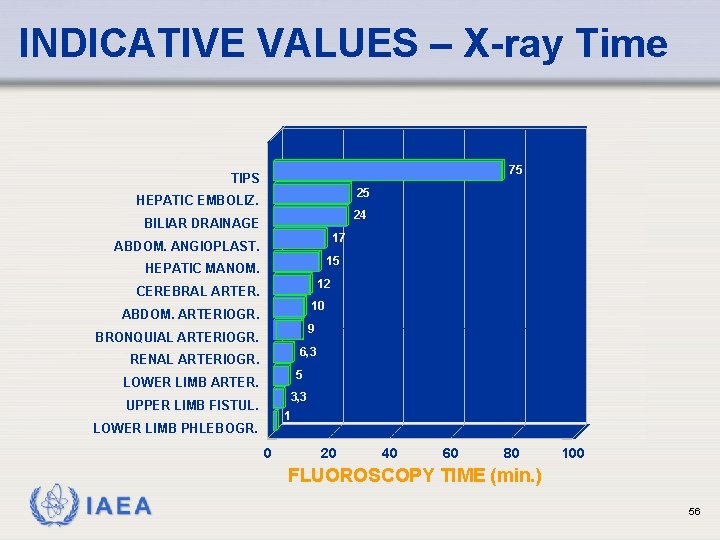
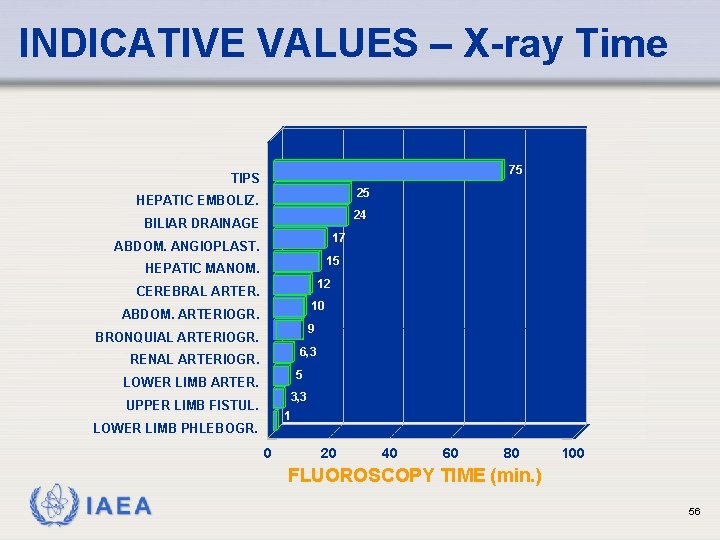
INDICATIVE VALUES – X-ray Time 75 TIPS 25 HEPATIC EMBOLIZ. 24 BILIAR DRAINAGE 17 ABDOM. ANGIOPLAST. 15 HEPATIC MANOM. 12 CEREBRAL ARTER. 10 ABDOM. ARTERIOGR. 9 BRONQUIAL ARTERIOGR. 6, 3 RENAL ARTERIOGR. 5 LOWER LIMB ARTER. 3, 3 UPPER LIMB FISTUL. 1 LOWER LIMB PHLEBOGR. 0 20 40 60 80 100 FLUOROSCOPY TIME (min. ) IAEA 56
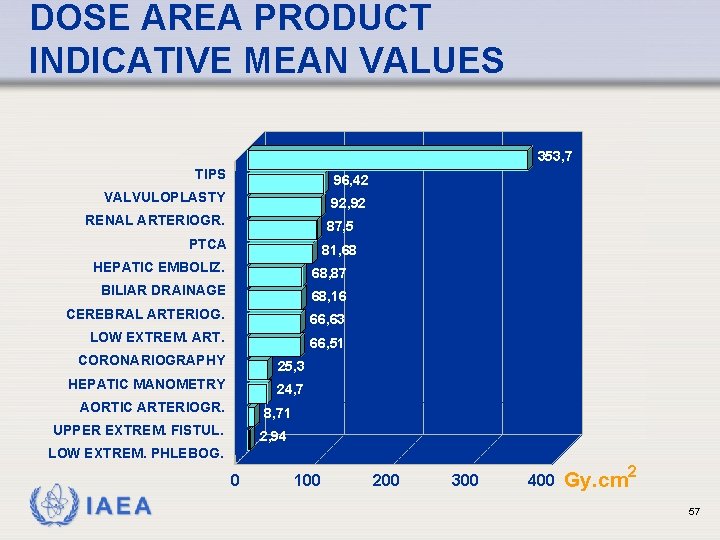
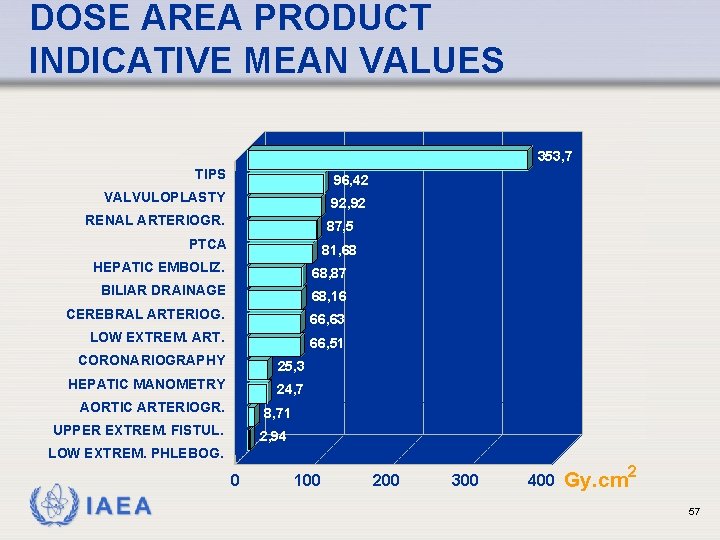
DOSE AREA PRODUCT INDICATIVE MEAN VALUES 353, 7 TIPS 96, 42 VALVULOPLASTY 92, 92 RENAL ARTERIOGR. 87, 5 PTCA 81, 68 HEPATIC EMBOLIZ. 68, 87 BILIAR DRAINAGE 68, 16 CEREBRAL ARTERIOG. 66, 63 LOW EXTREM. ART. 66, 51 CORONARIOGRAPHY 25, 3 HEPATIC MANOMETRY 24, 7 AORTIC ARTERIOGR. 8, 71 UPPER EXTREM. FISTUL. 2, 94 LOW EXTREM. PHLEBOG. 0 IAEA 100 200 300 400 Gy. cm 2 57
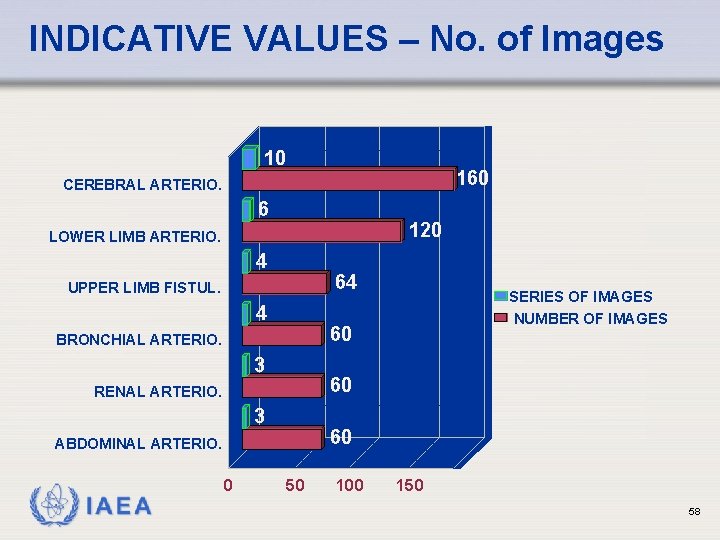
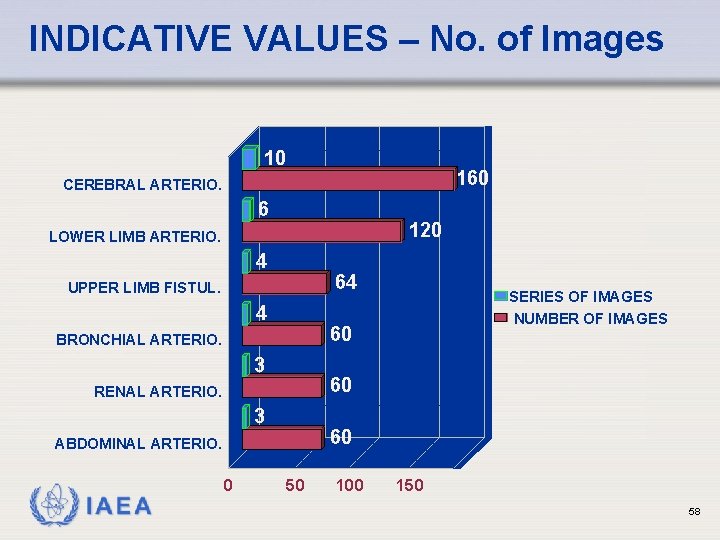
INDICATIVE VALUES – No. of Images 10 160 CEREBRAL ARTERIO. 6 120 LOWER LIMB ARTERIO. 4 64 UPPER LIMB FISTUL. 4 60 BRONCHIAL ARTERIO. 3 60 RENAL ARTERIO. 3 60 ABDOMINAL ARTERIO. IAEA 0 SERIES OF IMAGES NUMBER OF IMAGES 50 100 150 58
CINE ACQUISITION DOSES Patient entrance doses for cine can require between 70 and 130 µGy/frame Ø 1 minute of cine at 25 fr/s would lead to 150 m. Gy, almost equivalent to: Ø 15 abdomen X Rays or to 400 chest X Rays IAEA 59
Influence of patient thickness and operation modes in scatter dose rate IAEA 60
Influence of operation modes: from low fluoroscopy to cine, scatter dose rate could increase in a factor of 10 (from 2 to 20 m. Sv/h for normal size) IAEA 61
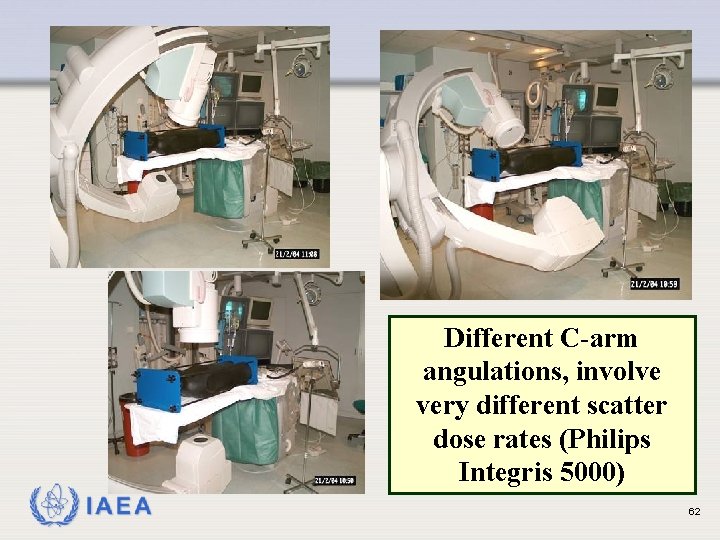
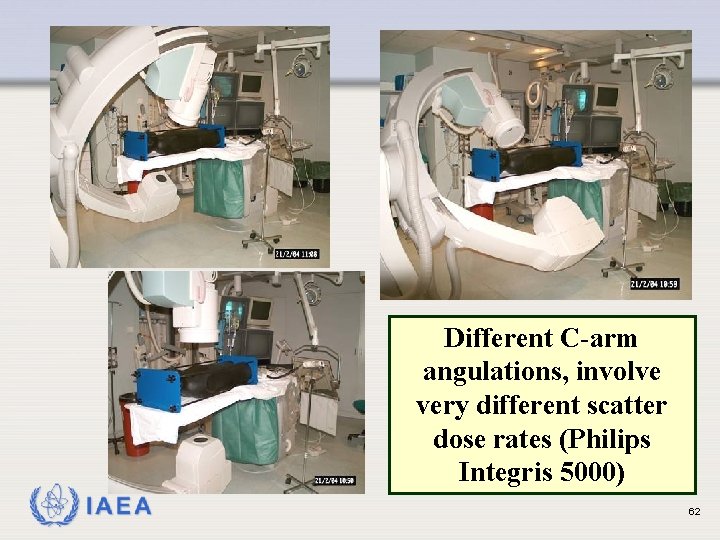
Different C-arm angulations, involve very different scatter dose rates (Philips Integris 5000) IAEA 62
THE SCATTERED DOSE RATE AT 1 METRE FROM THE PATIENT CAN BE HIGHER THAN 1 m. Gy/min FOR SOME ARC POSITIONS WITH DIGITAL FLUOROSCOPY MODE, DOSE RATE COULD BE REDUCED (25%) WITH RESPECT TO CONVENTIONAL MODE IAEA 63
Practical Actions in controlling dose Keep beam-on time to an absolute minimum --The Golden Rule for control of dose to patient and staff Remember that dose rates will be greater and dose will accumulate faster in thicker patients. Keep the X Ray tube at maximal distance from the patient. Keep the image intensifier as close to the patient as possible. IAEA 64
ì Don’t over-use geometric magnification. ì Remove the grid during procedures on small patients or when the image intensifier cannot be placed close to the patient. ì Always collimate closely to the area of interest. IAEA 65
ì When the procedure is unexpectedly prolonged, consider options for positioning the patient or altering the X Ray field or other means to alter beam angulation so that the same area of skin is not continuously in the direct X Ray field. • Dose rate varies continuously during the procedure IAEA 66
ì Fluoroscopy time is only a very rough indicator of whether radiation injuries may occur. ì Patient size and procedural aspects such as location(s) of the beam, beam angle, normal or high dose rates, distance of the tube from the patient and number of acquisitions can cause the maximum patient skin doses to be tenfold different for a specific total fluoroscopy time. IAEA 67
Minimize Exposure Time • Everything you do to minimize exposure time reduces radiation dose!! • Minimize fluoro and cine times • Whenever possible, step out of room • Step behind barrier (or another person) during fluoro or cine • Use pulsed fluoroscopy– minimizes time X ray tube is producing X rays IAEA 68
Angiography - Patient Protection Patients should be counseled on radiation risks if the procedure carries a significant risk of such injury. Records of exposure should be kept if the estimated maximum cumulative dose to skin is 3 Gy or above. All patients with estimated skin doses of 3 Gy or above should be followed up 10 to 14 days after exposure. The patient’s personal physician should be informed of the possibility of radiation effects. If the dose is sufficient to cause observable effects, the patient should be counseled after the procedure. A system to identify repeated procedures should be set up. IAEA 69
IAEA 70
 Rtc protective film
Rtc protective film Jennie reeves radiographers agency ltd
Jennie reeves radiographers agency ltd Fowler's position angle
Fowler's position angle Cardinal principles of radiation protection
Cardinal principles of radiation protection National radiation protection authority namibia
National radiation protection authority namibia Radiation protection officer qualifications
Radiation protection officer qualifications Barium sulphate board for radiation protection
Barium sulphate board for radiation protection Rtč test
Rtč test Red de conmutacion
Red de conmutacion Rajeev chawla ias
Rajeev chawla ias Rtc flex ride
Rtc flex ride Pyki rtc
Pyki rtc Getusermedia
Getusermedia Wen rtc
Wen rtc Contact center webrtc
Contact center webrtc Rtc code review tool
Rtc code review tool Rtc key club
Rtc key club Autokratiskt ledarskap
Autokratiskt ledarskap Humanitr
Humanitr Datorkunskap för nybörjare
Datorkunskap för nybörjare Rita perspektiv
Rita perspektiv Toppslätskivling dos
Toppslätskivling dos Returpilarna
Returpilarna Redogör för vad psykologi är
Redogör för vad psykologi är Ramsa geometriska former
Ramsa geometriska former Claes martinsson
Claes martinsson Lyrik texte
Lyrik texte Etik och ledarskap etisk kod för chefer
Etik och ledarskap etisk kod för chefer Offentlig förvaltning
Offentlig förvaltning Antikt plagg i rom
Antikt plagg i rom Tidböcker
Tidböcker Fspos
Fspos Vilken grundregel finns det för tronföljden i sverige?
Vilken grundregel finns det för tronföljden i sverige? Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Jätte råtta
Jätte råtta Tillitsbaserad ledning
Tillitsbaserad ledning Vem räknas som jude
Vem räknas som jude Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Romarriket tidslinje
Romarriket tidslinje Boverket ka
Boverket ka Informationskartläggning
Informationskartläggning Handledning reflektionsmodellen
Handledning reflektionsmodellen Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? Matematisk modellering eksempel
Matematisk modellering eksempel Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Shivaiter
Shivaiter Cks
Cks Inköpsprocessen steg för steg
Inköpsprocessen steg för steg Expektans eller exspektans
Expektans eller exspektans Lyckans minut erik lindorm analys
Lyckans minut erik lindorm analys Strategi för svensk viltförvaltning
Strategi för svensk viltförvaltning A gastrica
A gastrica Novell typiska drag
Novell typiska drag Stickprovsvarians
Stickprovsvarians Tack för att ni har lyssnat
Tack för att ni har lyssnat Läkarutlåtande för livränta
Läkarutlåtande för livränta Treserva lathund
Treserva lathund Att skriva en debattartikel
Att skriva en debattartikel Påbyggnader för flakfordon
Påbyggnader för flakfordon Tack för att ni lyssnade
Tack för att ni lyssnade En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Egg för emanuel
Egg för emanuel Atmosfr
Atmosfr Lågenergihus nyproduktion
Lågenergihus nyproduktion Rutin för avvikelsehantering
Rutin för avvikelsehantering Var finns arvsanlagen
Var finns arvsanlagen Presentera för publik crossboss
Presentera för publik crossboss Rbk mätning
Rbk mätning Myndigheten för delaktighet
Myndigheten för delaktighet Var 1721 för stormaktssverige
Var 1721 för stormaktssverige Densitet vatten
Densitet vatten