Risk Management Patient Safety Dr Hamid Ravaghi What
















![“the very first requirement in a hospital [is] that it should do the sick “the very first requirement in a hospital [is] that it should do the sick](https://slidetodoc.com/presentation_image_h/f9c8032ce318bae04b9e99492c5a4deb/image-70.jpg)




























- Slides: 147

Risk Management: Patient Safety Dr Hamid Ravaghi
What is Risk Management? Whose responsibility is it in your institution?


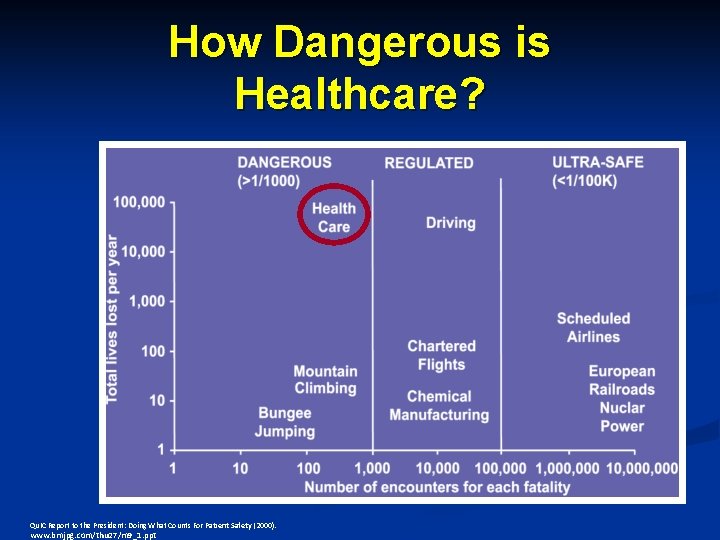
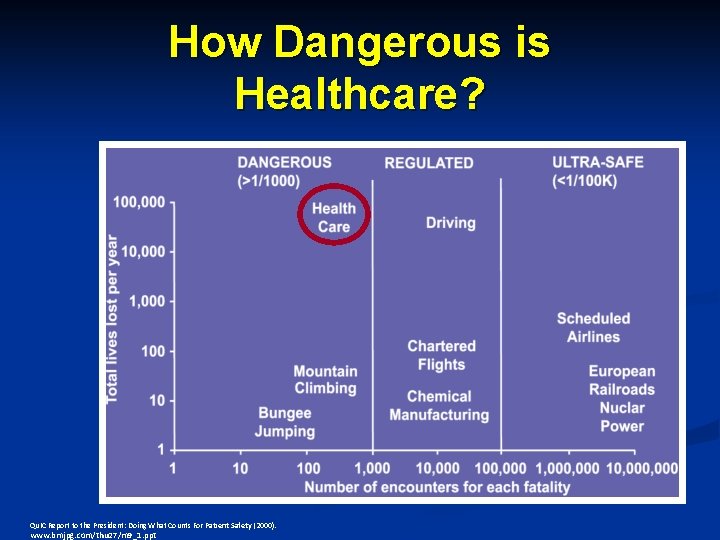
How Dangerous is Healthcare? Qu. IC Report to the President: Doing What Counts For Patient Safety (2000). www. bmjpg. com/thu 27/m 9_1. ppt Error problem
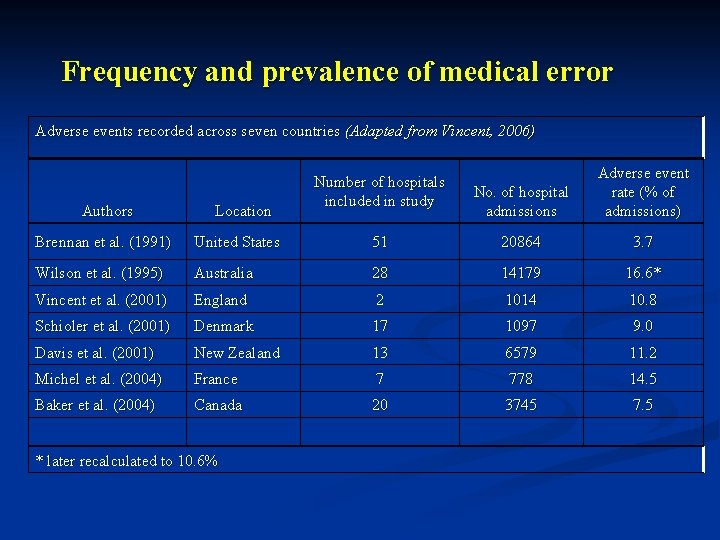
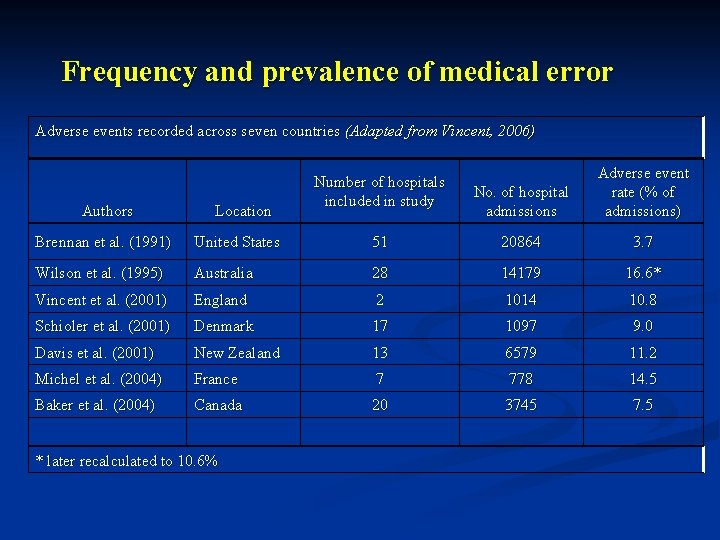
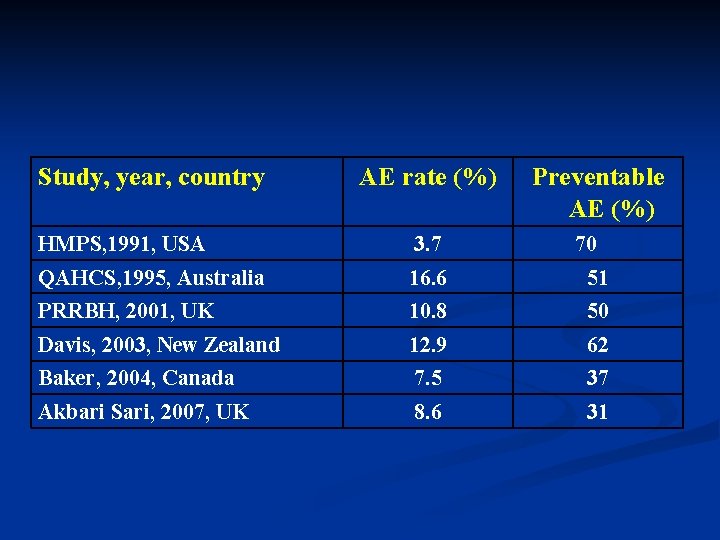
Frequency and prevalence of medical error Adverse events recorded across seven countries (Adapted from Vincent, 2006) Authors Location Number of hospitals included in study No. of hospital admissions Adverse event rate (% of admissions) Brennan et al. (1991) United States 51 20864 3. 7 Wilson et al. (1995) Australia 28 14179 16. 6* Vincent et al. (2001) England 2 1014 10. 8 Schioler et al. (2001) Denmark 17 1097 9. 0 Davis et al. (2001) New Zealand 13 6579 11. 2 Michel et al. (2004) France 7 778 14. 5 Baker et al. (2004) Canada 20 3745 7. 5 * later recalculated to 10. 6%
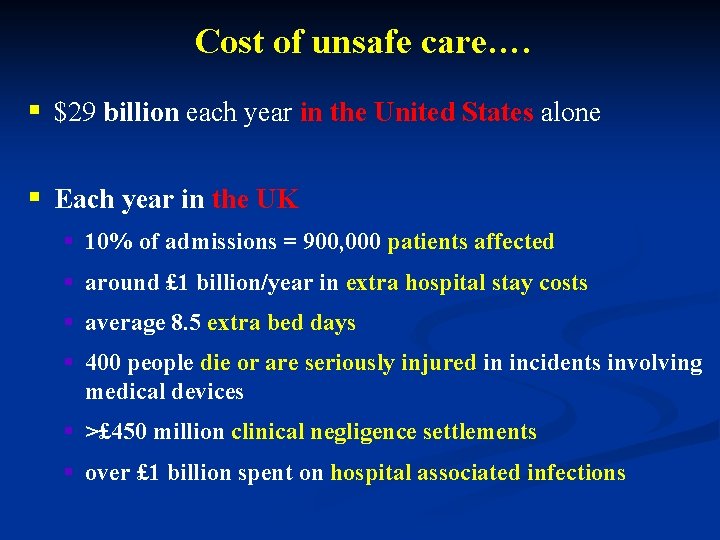
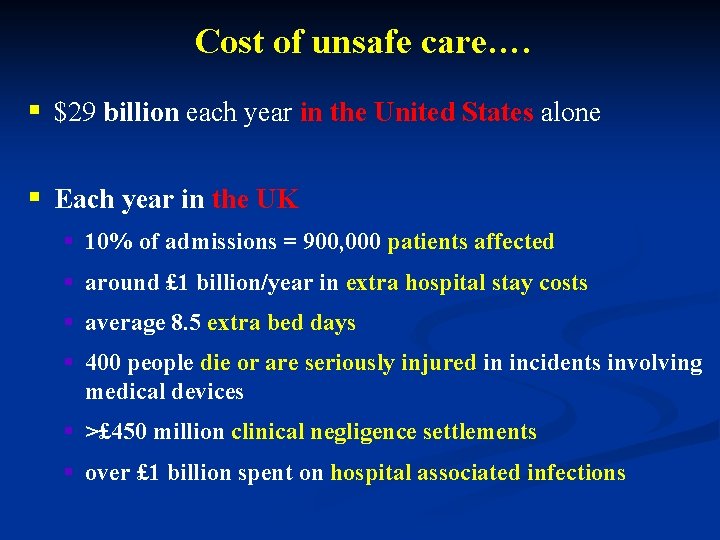
Cost of unsafe care…. § $29 billion each year in the United States alone § Each year in the UK § 10% of admissions = 900, 000 patients affected § around £ 1 billion/year in extra hospital stay costs § average 8. 5 extra bed days § 400 people die or are seriously injured in incidents involving medical devices § >£ 450 million clinical negligence settlements § over £ 1 billion spent on hospital associated infections
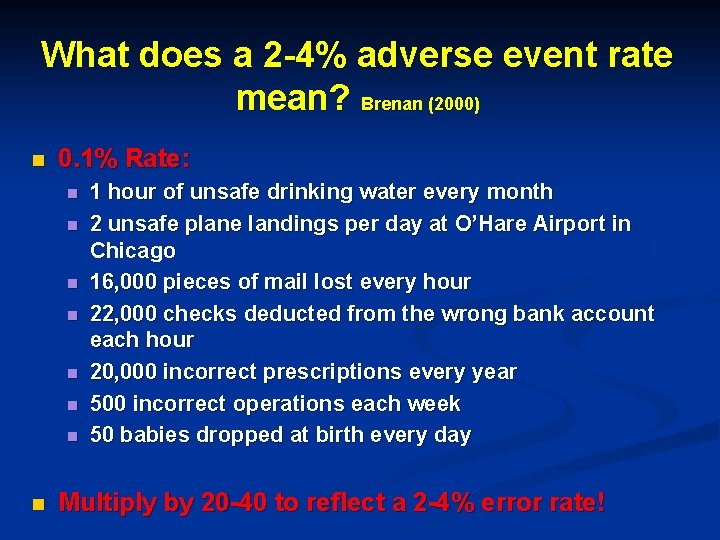
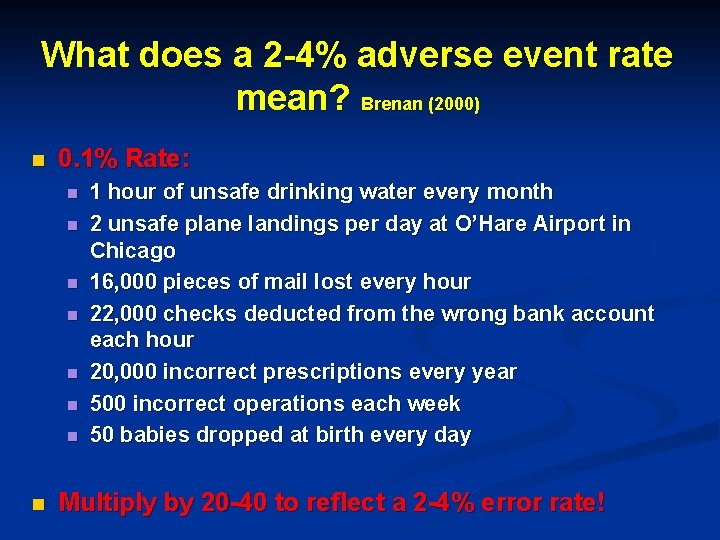
What does a 2 -4% adverse event rate mean? Brenan (2000) n 0. 1% Rate: n n n n 1 hour of unsafe drinking water every month 2 unsafe plane landings per day at O’Hare Airport in Chicago 16, 000 pieces of mail lost every hour 22, 000 checks deducted from the wrong bank account each hour 20, 000 incorrect prescriptions every year 500 incorrect operations each week 50 babies dropped at birth every day Multiply by 20 -40 to reflect a 2 -4% error rate!
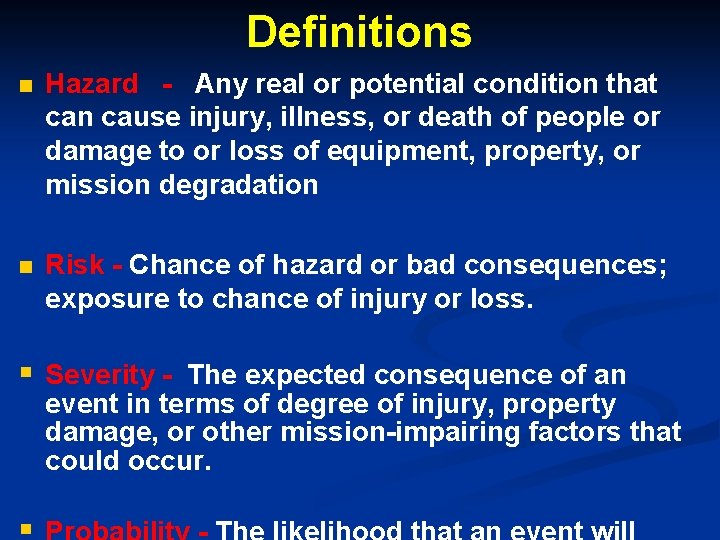
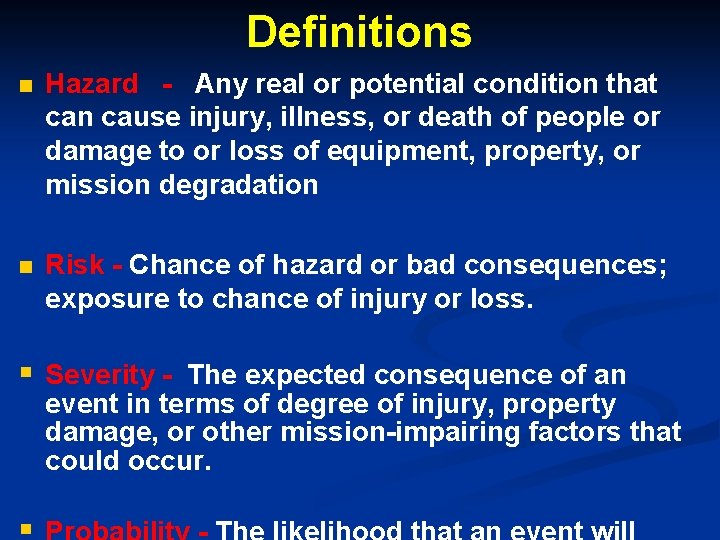
Definitions n Hazard - Any real or potential condition that can cause injury, illness, or death of people or damage to or loss of equipment, property, or mission degradation n Risk - Chance of hazard or bad consequences; exposure to chance of injury or loss. § Severity - The expected consequence of an event in terms of degree of injury, property damage, or other mission-impairing factors that could occur.


Oops no ramp….




Need for Management of Risk n To enhance patient safety n Increasing patient, professional and staff expectations n Competitive pressures in a managed market n Continuing pressure on internal costs n Higher service performance demands from government
Need for Management of Risk (cont) n Rising levels of complaints, claims and litigation n Patient satisfaction surveys showing weaknesses and negative perceptions n Clinical research indicating areas for improvement
Four Ways to Manage Risk n Avoiding the risk n Minimizing or reducing the negative effect of the risk n Transferring the risk n Accepting some or all of the consequences of the risk
Who uses Risk Management? Are widely used in public and the private sectors • Finance and Investment • Insurance • Health Care • Public Institutions • Governments
Risk management in health care Definition: Clinical and administrative activities undertaken to identify, evaluate, and reduce the risk of injury to patients, staff, and visitors and the risk of loss to the organization itself (Joint commission, 2007)
Risk management in health care Risk Management is the: identification, investigation, analysis, and evaluation of risks AND the selection of the most advantageous method of : correcting, reducing, or eliminating identifiable risks
Why is risk management an effective strategy to reduce harm? n Positive evidence from other high risk industries High Reliability Organizations (HROs) n Effective strategies focusing on Human Factors Engineering (HFE) approach
Risk management approaches n “Reactive” and “Proactive” approaches n learning from things that has gone wrong (Reactive) n preventing potential risks from impacting in the service that the health organization provides (Proactive)
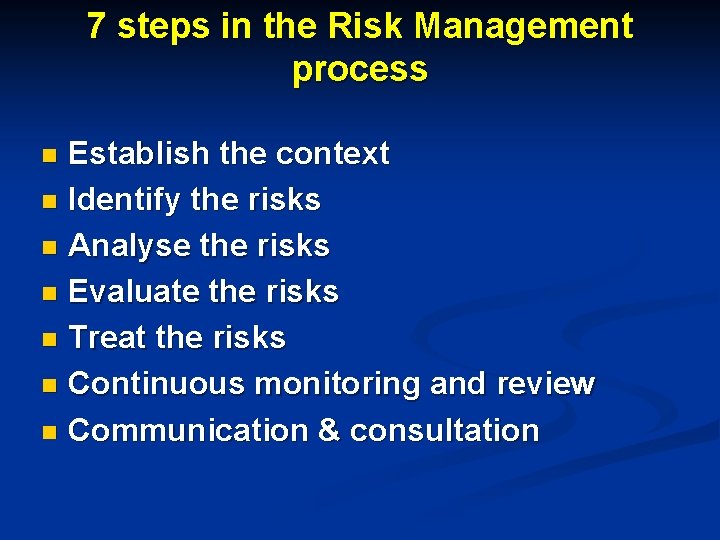
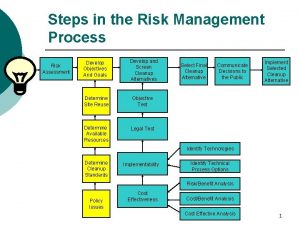
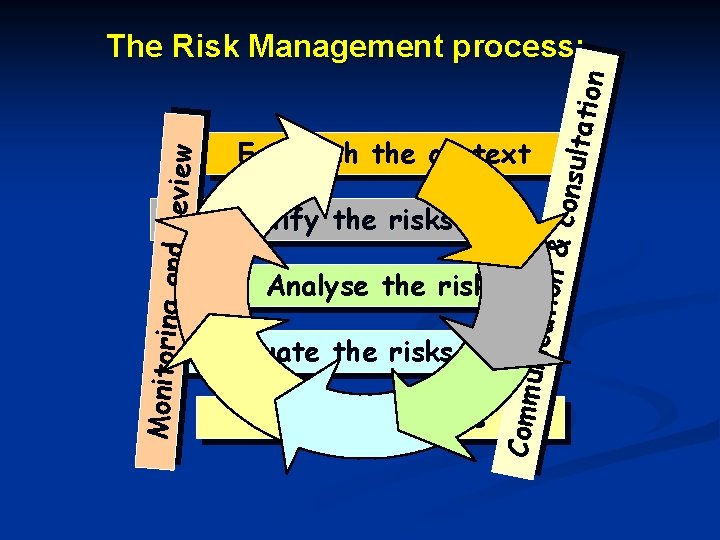
7 steps in the Risk Management process Establish the context n Identify the risks n Analyse the risks n Evaluate the risks n Treat the risks n Continuous monitoring and review n Communication & consultation n
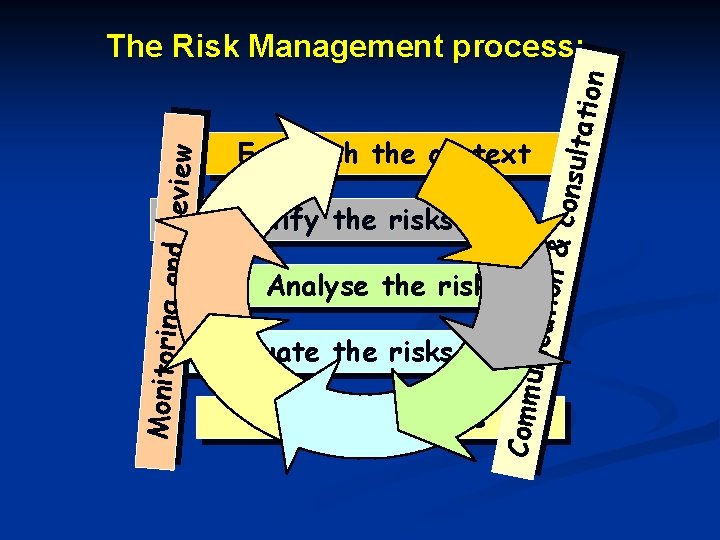
ion & consu ltatio n Establish the context Identify the risks Evaluate the risks Treat the risks unicat Analyse the risks Comm Monitoring a nd review The Risk Management process:
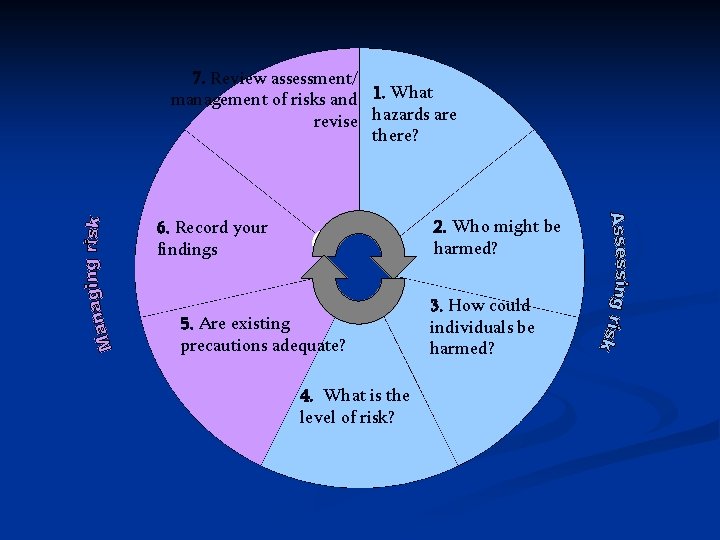
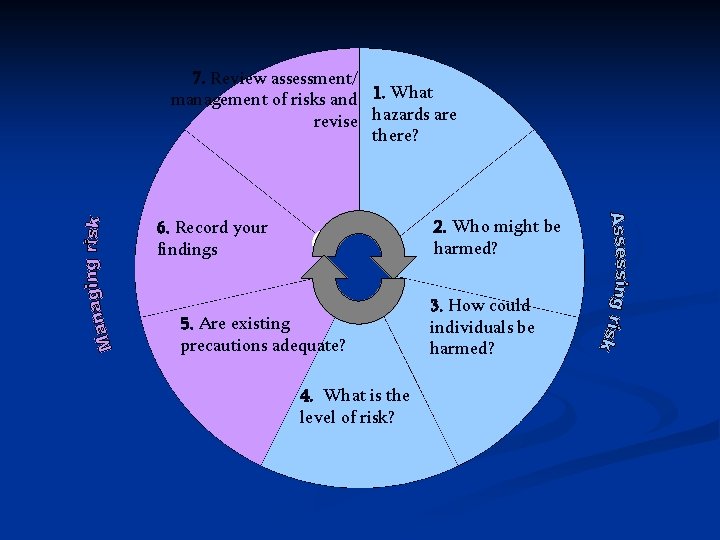
7. Review assessment/ management of risks and 1. What revise hazards are there? 2. Who might be harmed? 6. Record your findings 5. Are existing precautions adequate? 4. What is the level of risk? 3. How could individuals be harmed?
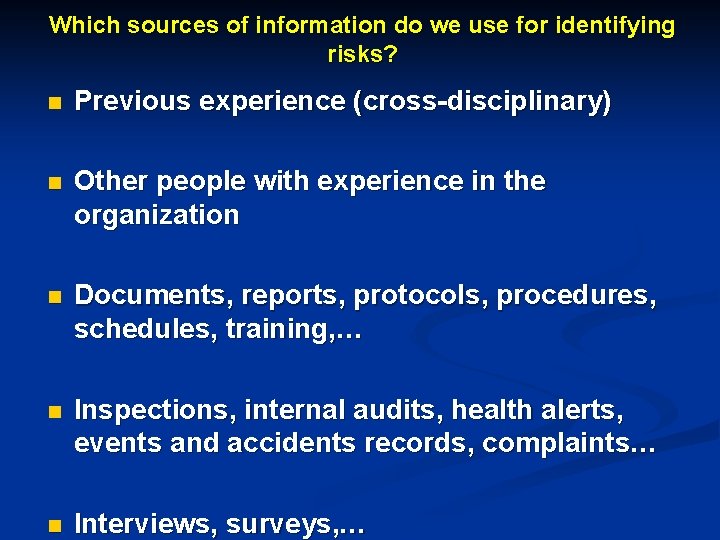
Which sources of information do we use for identifying risks? n Previous experience (cross-disciplinary) n Other people with experience in the organization n Documents, reports, protocols, procedures, schedules, training, … n Inspections, internal audits, health alerts, events and accidents records, complaints… n Interviews, surveys, …


The identified risks will be the root material (“ingredients”) with which we will prepare the rest of the risk management plan (the “meal” ready to eat)
n we cannot be covered for 100% of the risks n which risks are we going to prevent or minimize? n what risk level can we afford?
Evaluate the Risks § Description or quantification exactly what the ‘Likelihood’ and ‘Consequence’ terms means § Ensuring a consistent approach in future risk assessment and review and monitoring
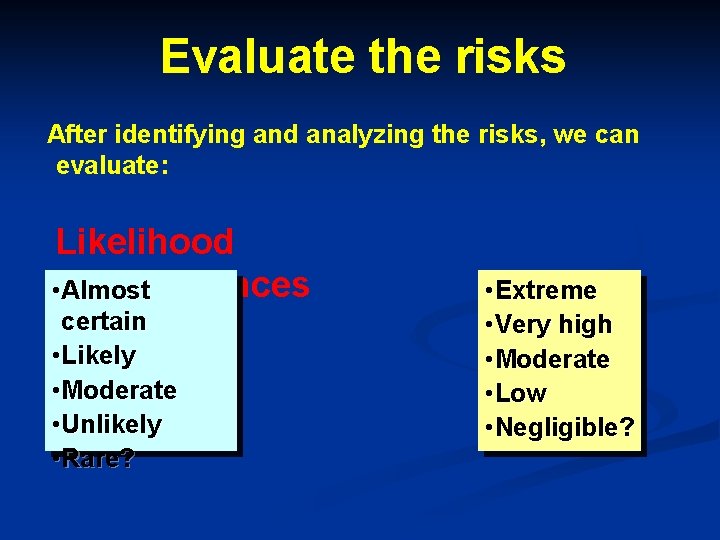
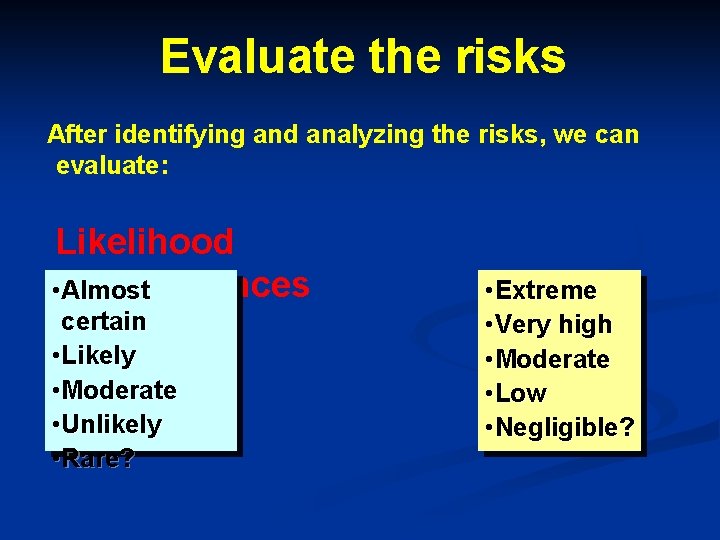
Evaluate the risks After identifying and analyzing the risks, we can evaluate: Likelihood • Consequences Almost certain • Likely • Moderate • Unlikely • Rare? • Extreme • Very high • Moderate • Low • Negligible?
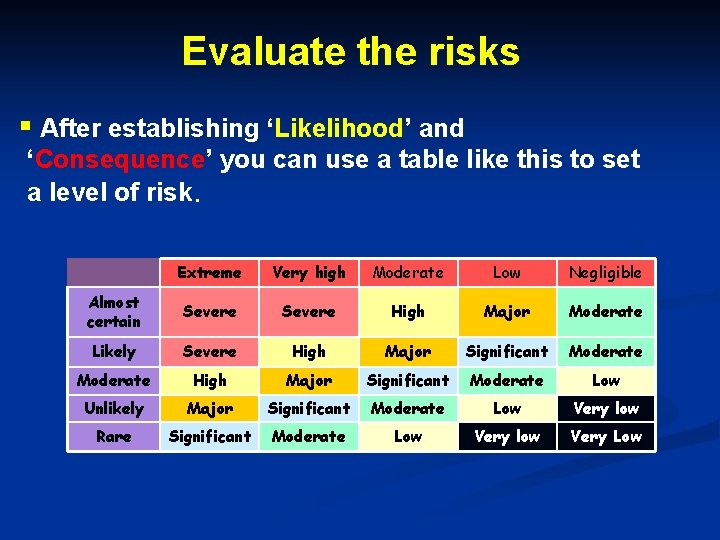
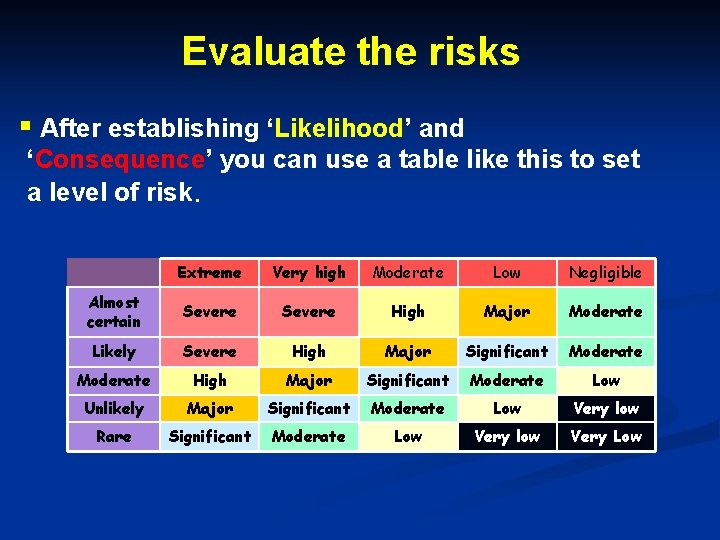
Evaluate the risks § After establishing ‘Likelihood’ and ‘Consequence’ you can use a table like this to set a level of risk. Extreme Very high Moderate Low Negligible Almost certain Severe High Major Moderate Likely Severe High Major Significant Moderate Low Unlikely Major Significant Moderate Low Very low Rare Significant Moderate Low Very low Very Low
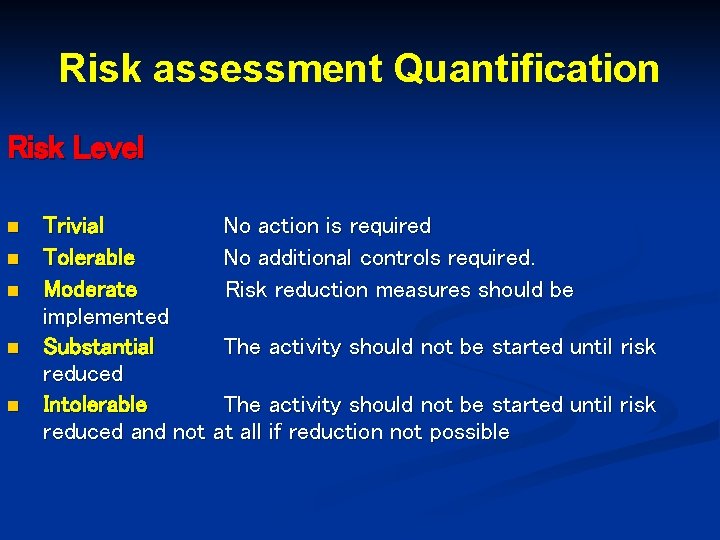
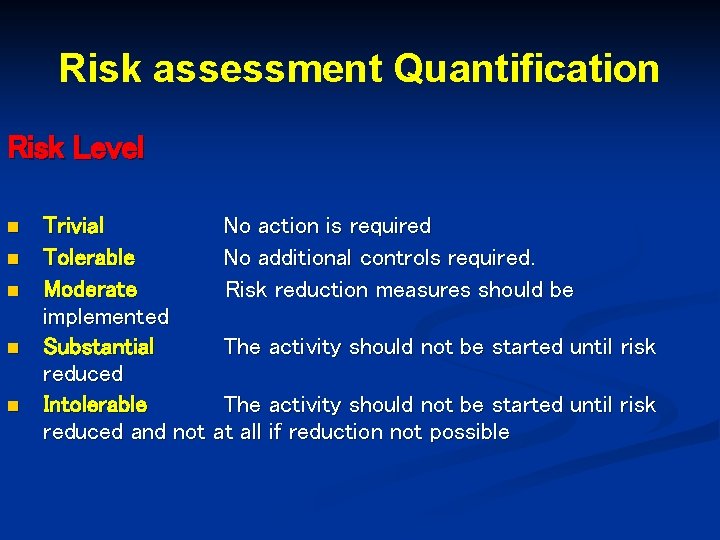
Risk assessment Quantification Risk Level n n n Trivial No action is required Tolerable No additional controls required. Moderate Risk reduction measures should be implemented Substantial The activity should not be started until risk reduced Intolerable The activity should not be started until risk reduced and not at all if reduction not possible


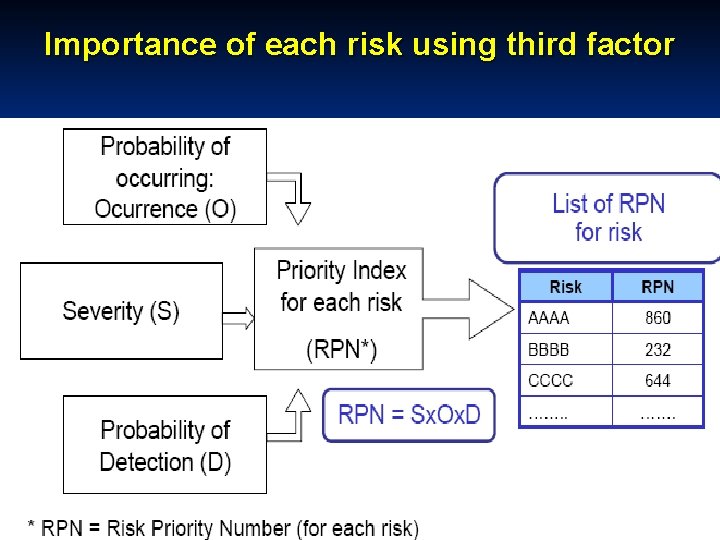
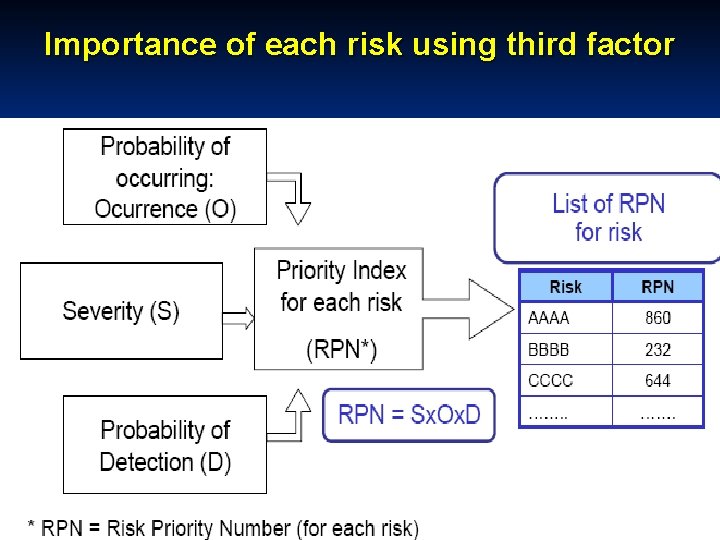
Importance of each risk using third factor
7 steps in the Risk Management process Establish the context n Identify the risks n Analyse the risks n Evaluate the risks n Treat the risks n Continuous monitoring and review n Communication & consultation n
Reactive approach: Root Cause Analysis
Risk management approaches n “Reactive” and “Proactive” approaches n learning from things that has gone wrong (Reactive) n preventing potential risks from impacting in the service that the health organization provides (Proactive)

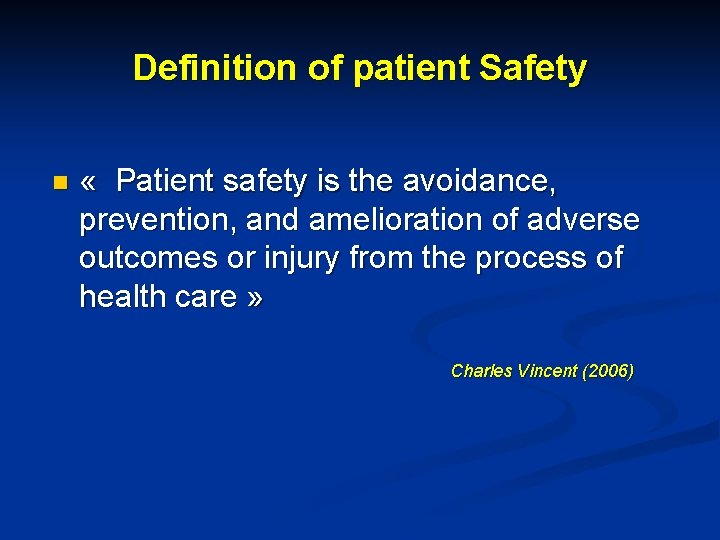
Adverse and Sentinel Events Adverse evens: “Unintended injury to patients resulting from a medical intervention, which includes any action by healthcare workers, including clerical and maintenance staff. ” n Institute of Medicine Sentinel event: “An unexpected occurrence involving death or serious physical or psychological injury or risk thereof. ” Joint n
Sentinel events n Procedures involving wrong patient or body part n Retained instruments after surgery n Intravascular gas embolism causing death n Blood transfusion reaction from ABO incompatibility
Sentinel events n Maternal death from labour or delivery n A baby discharged to the wrong family n Suicide of a patient in an in-patient unit n Medication error leading to the death of patient
Why do root causes exist? n Adverse and sentinel events are symptoms of a pathology in the organization n A disease in an organization cause collapse of multiple work systems n Must look at ACTIONS and CONDITIONS
Causes n We should know: n The proximate causes (or superficial, obvious, or immediate causes) n The root or underlying causes (the causes that led to proximate causes) n The interrelationship of causes
What is a root cause? n A root cause is the most basic causal factor, or factors, which if corrected or removed will prevent the recurrence of a situation, such as an error in performing a procedure

http: //www. thinkreliability. com/Root-Cause-Analysis-CMBasics. aspx
Root cause analysis (RCA) n An investigative technique that allows organizations to identify retrospectively the reasons (basic or casual factors) why certain outcomes occurred n Can also be used in a “near miss” event
Objectives of Root Cause Analysis To find out n What happened n Why did it happen n What can be done to prevent future occurrence n Focus on process and systems rather than individual performance
Root causes analysis (RCA) n RCA is part of a Safety and Quality process n Is a questioning process n It supports the organization to learn and develop
RCA Techniques 5 Whys n Safeguard analysis n Change analysis n Causal factor tree analysis n Failure mode and effects analysis n Ishikawa diagram (the fishbone diagram or cause and effect diagram) n Fault tree analysis n
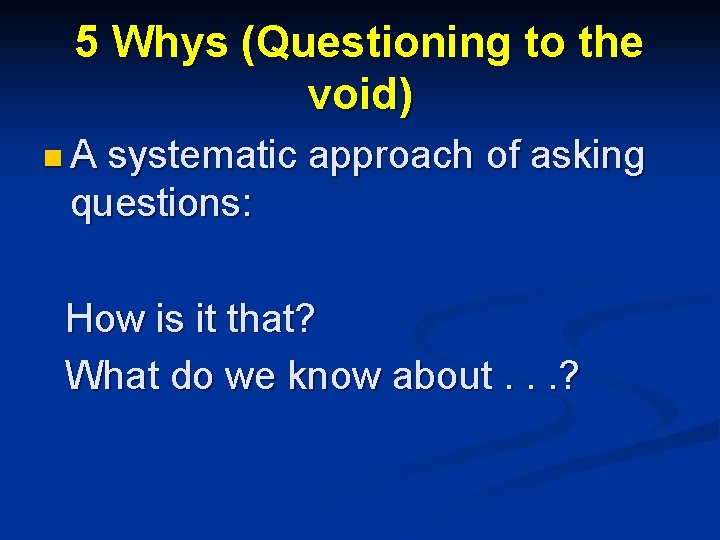
5 Whys (Questioning to the void) n A systematic approach of asking questions: How is it that? What do we know about. . . ?
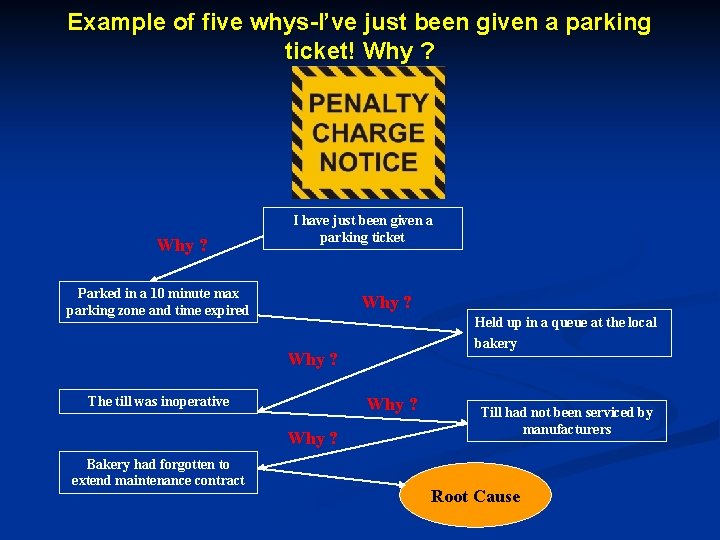
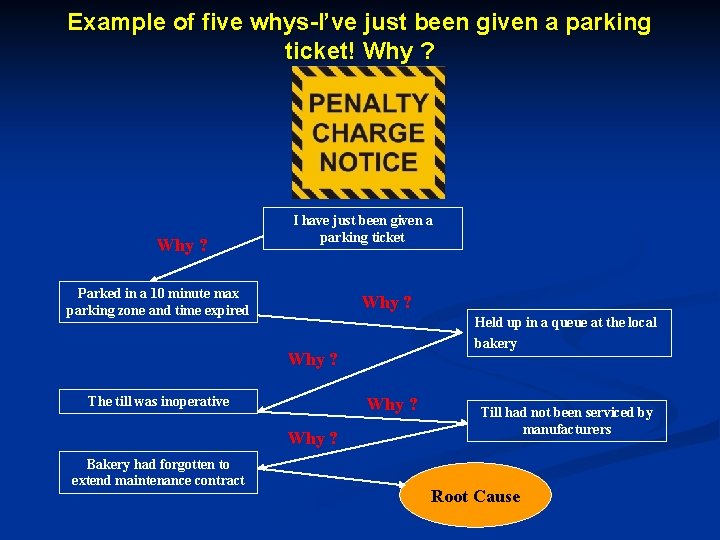
Example of five whys-I’ve just been given a parking ticket! Why ? I have just been given a parking ticket Parked in a 10 minute max parking zone and time expired Why ? Held up in a queue at the local bakery Why ? The till was inoperative Why ? Bakery had forgotten to extend maintenance contract Till had not been serviced by manufacturers Root Cause
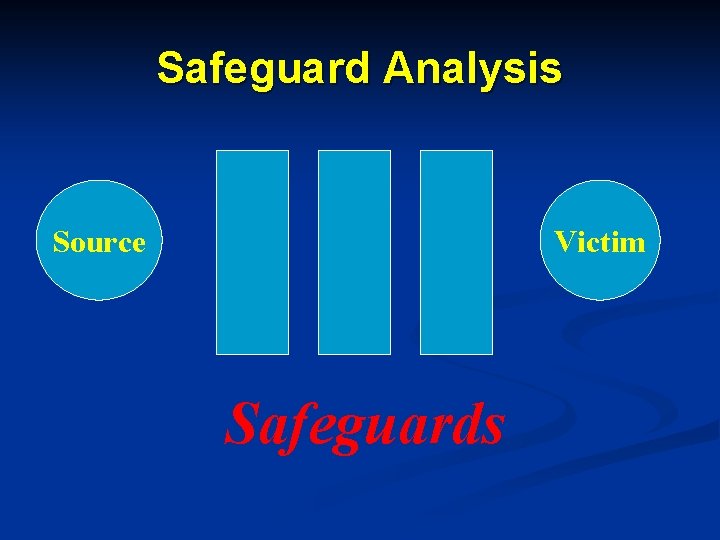
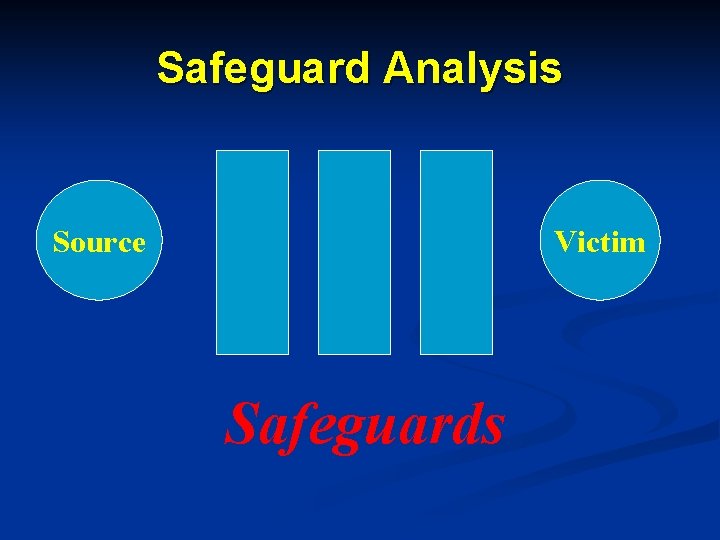
Safeguard Analysis Source Victim Safeguards
Steps in Safeguard Analysis n Identify potential or actual source of an event and identify the actual or potential victim n Identify safeguards currently in place and determine effectiveness n Develop plan to strengthen weak safeguards
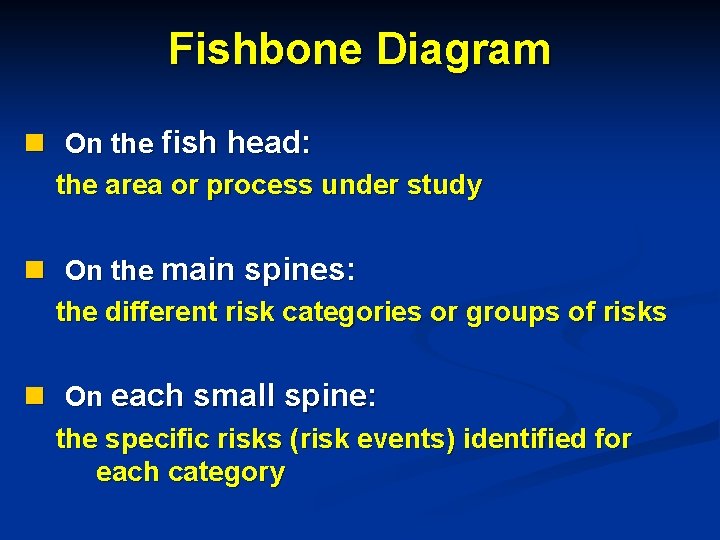
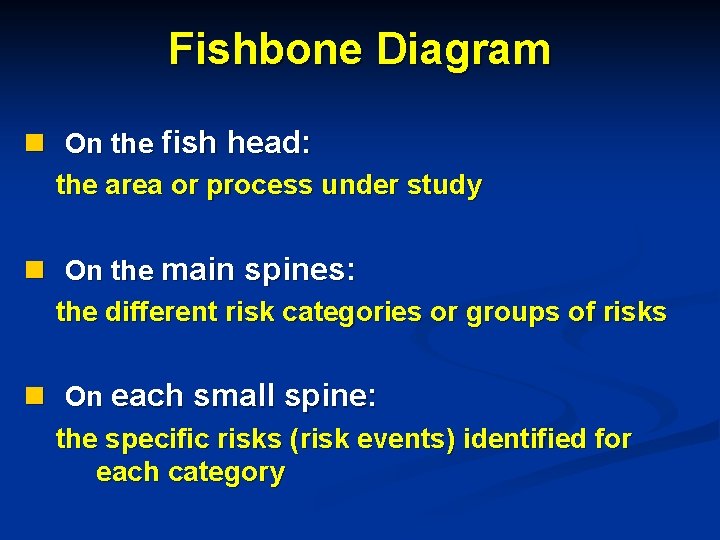
Fishbone Diagram n On the fish head: the area or process under study n On the main spines: the different risk categories or groups of risks n On each small spine: the specific risks (risk events) identified for each category
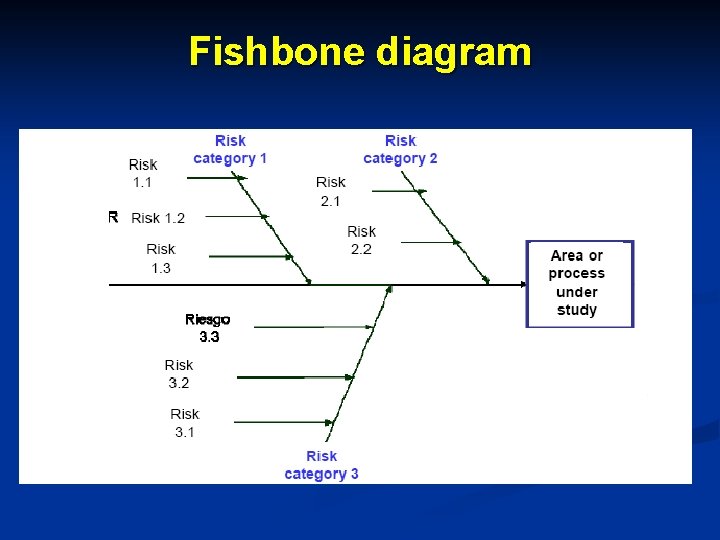
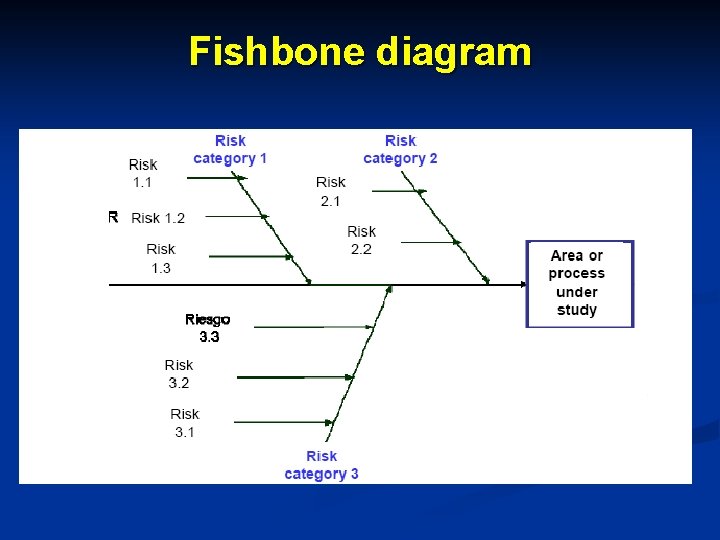
Fishbone diagram
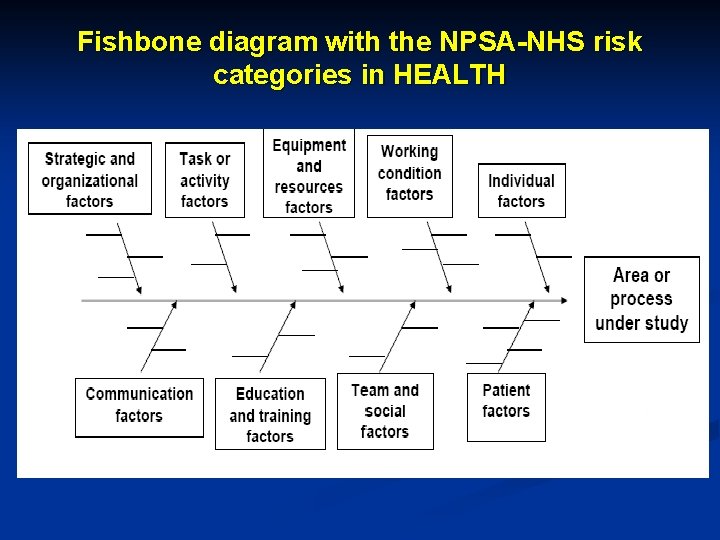
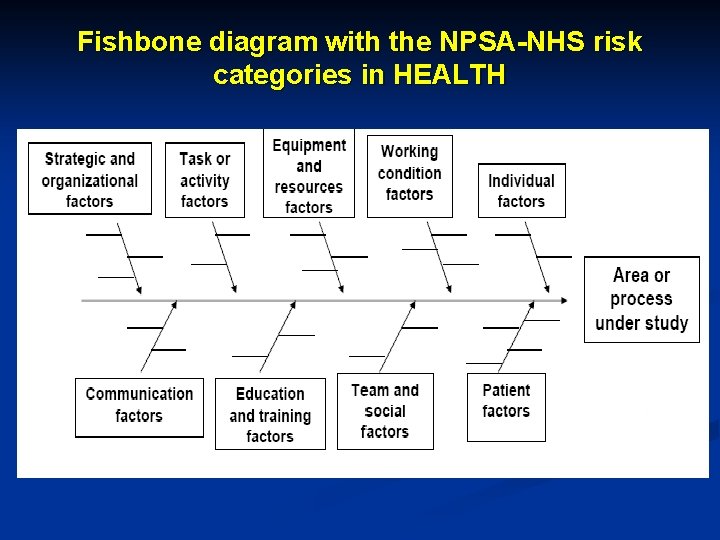
Fishbone diagram with the NPSA-NHS risk categories in HEALTH
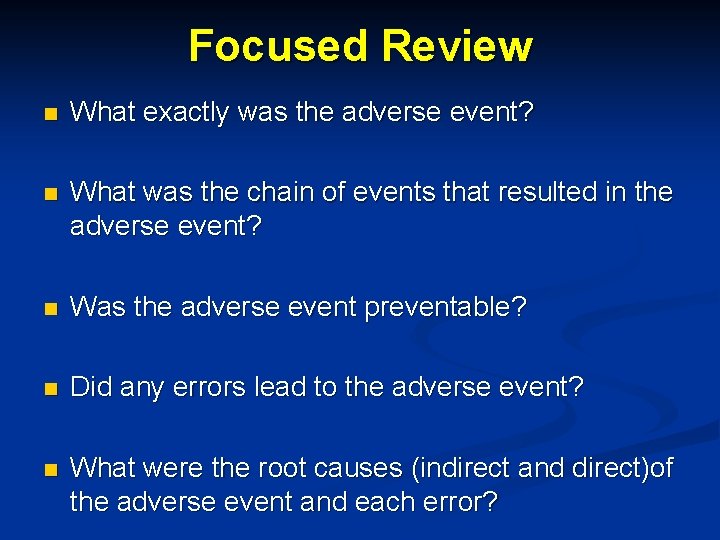
Focused Review n What exactly was the adverse event? n What was the chain of events that resulted in the adverse event? n Was the adverse event preventable? n Did any errors lead to the adverse event? n What were the root causes (indirect and direct)of the adverse event and each error?
Focused Review n Did any errors or root causes involve an inadequate system or a system failure? n Do we need to redesign the system? n Were any actions taken by staff in responding to the adverse event particularly helpful? n Should any personnel actions be initiated? n Any lessons that need to be learned?
Root causes analysis process Organize a team n Gather information n Define the event n Determine proximate causes n Identify root causes n Identify risk reduction strategies n Implement strategies n Evaluate effectiveness of actions taken n
Problems with root cause taxonomies n Most root causes are identified as being related to a weakness in the management system n Most root cause categories do not dig deep enough
Obstacles (1) n Punitive culture n Emotional impact of the event on personnel n Insufficient information about the event n Lack of personnel time to participate in RCA n Lack of resources to implement improvement strategies
Obstacles (2) n Lack of support from leadership n Lack of political support in relation with patient safety and quality n Arrogance n Lack of understanding, knowledge n Sense of entitlement among the staff
To err is Human To cover up is unforgivable To fail to learn is inexcusable

Patient Safety: Seven Steps Model
![the very first requirement in a hospital is that it should do the sick “the very first requirement in a hospital [is] that it should do the sick](https://slidetodoc.com/presentation_image_h/f9c8032ce318bae04b9e99492c5a4deb/image-70.jpg)
“the very first requirement in a hospital [is] that it should do the sick no harm” Notes on hospitals (Folrence Nightingale, 1863)
Safety is like peeling an onion; the more you look, the more you find, the more you cry! (Haig, 2004)

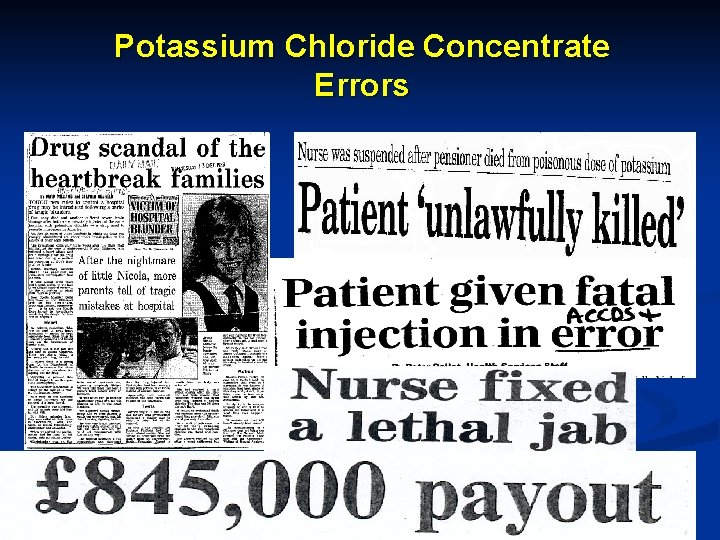
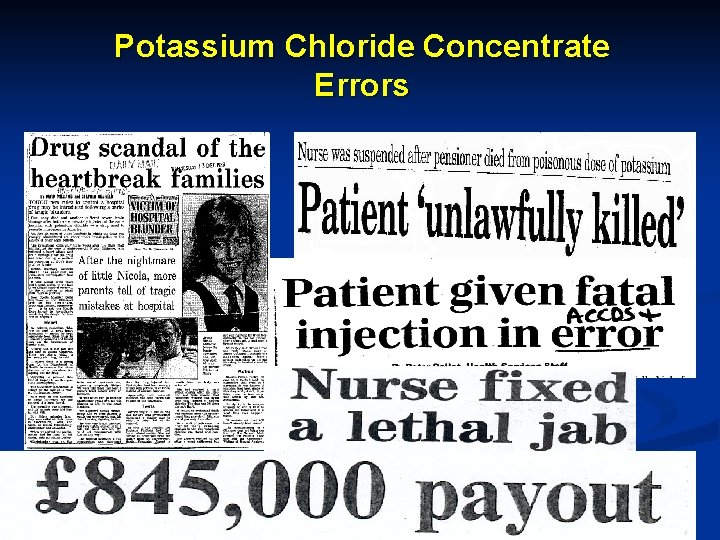
Potassium Chloride Concentrate Errors
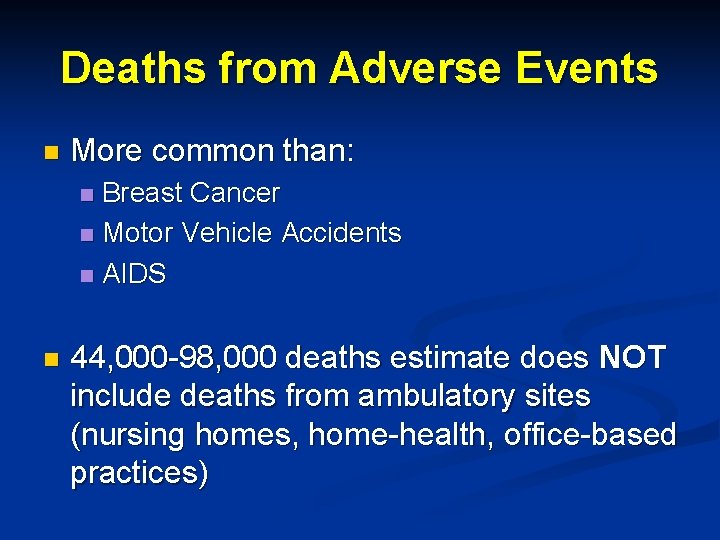
Deaths from Adverse Events n More common than: Breast Cancer n Motor Vehicle Accidents n AIDS n n 44, 000 -98, 000 deaths estimate does NOT include deaths from ambulatory sites (nursing homes, home-health, office-based practices)
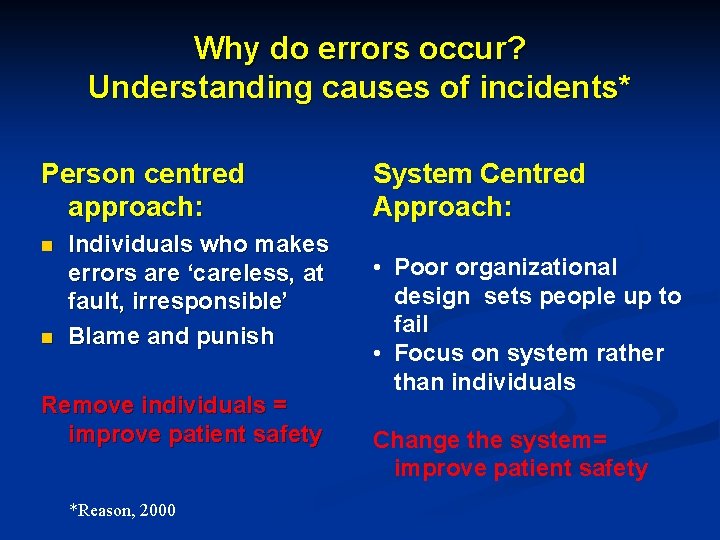
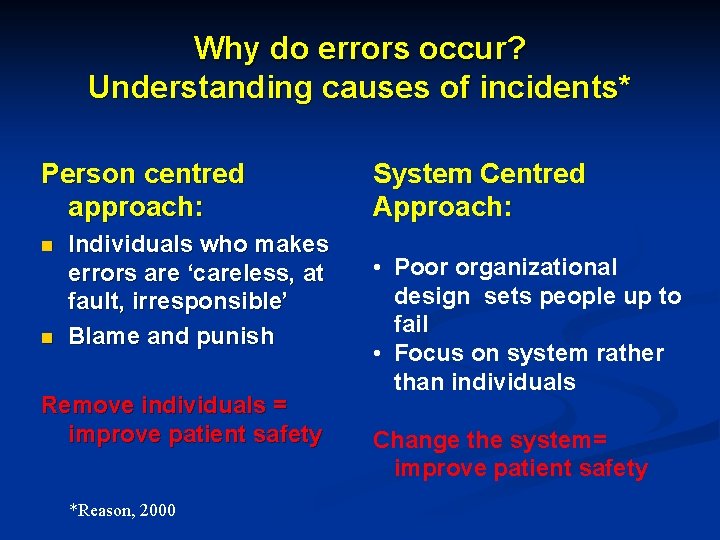
Why do errors occur? Understanding causes of incidents* Person centred approach: n n Individuals who makes errors are ‘careless, at fault, irresponsible’ Blame and punish Remove individuals = improve patient safety *Reason, 2000 System Centred Approach: • Poor organizational design sets people up to fail • Focus on system rather than individuals Change the system= improve patient safety
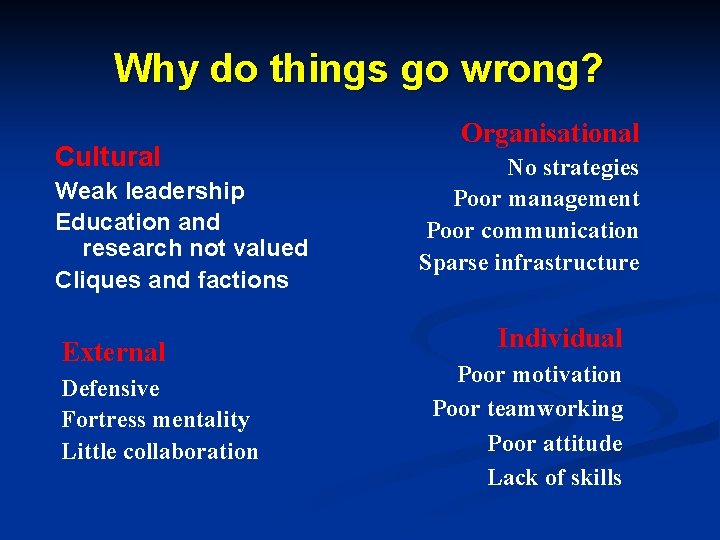
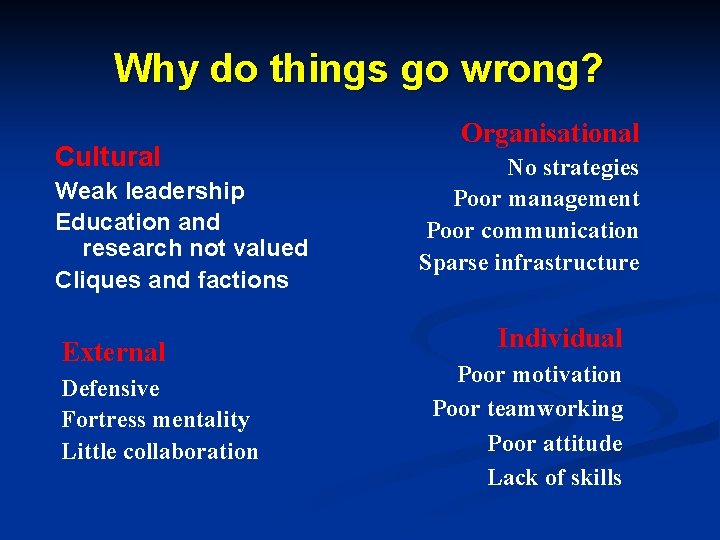
Why do things go wrong? Cultural Weak leadership Education and research not valued Cliques and factions External Defensive Fortress mentality Little collaboration Organisational No strategies Poor management Poor communication Sparse infrastructure Individual Poor motivation Poor teamworking Poor attitude Lack of skills
n Aoccdrnig to a rscheearch at Cmabrigde Uinervtisy, it deosn't mttaer in waht oredr the ltteers in a wrod are, the olny iprmoetnt tihng is taht the frist and lsat ltteer be at the rghit pclae. The rset can be a total mses and you can sitll raed it wouthit porbelm. Tihs is bcuseae the huamn mnid deos not raed ervey lteter by istlef, but the wrod as a wlohe
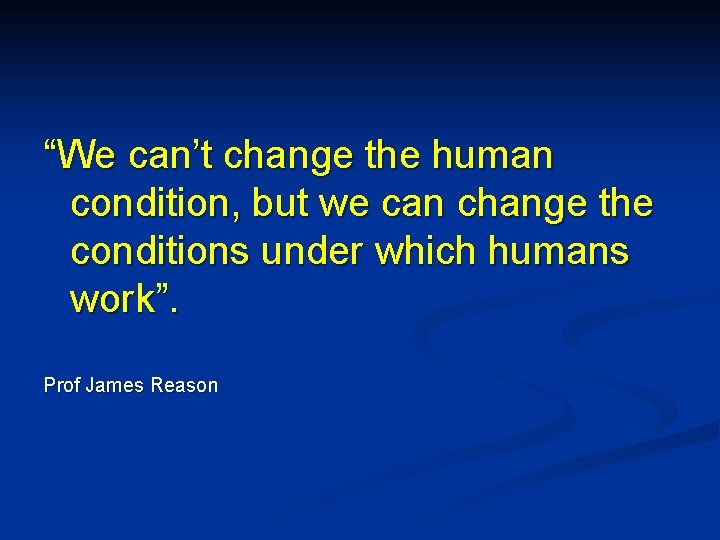
“We can’t change the human condition, but we can change the conditions under which humans work”. Prof James Reason

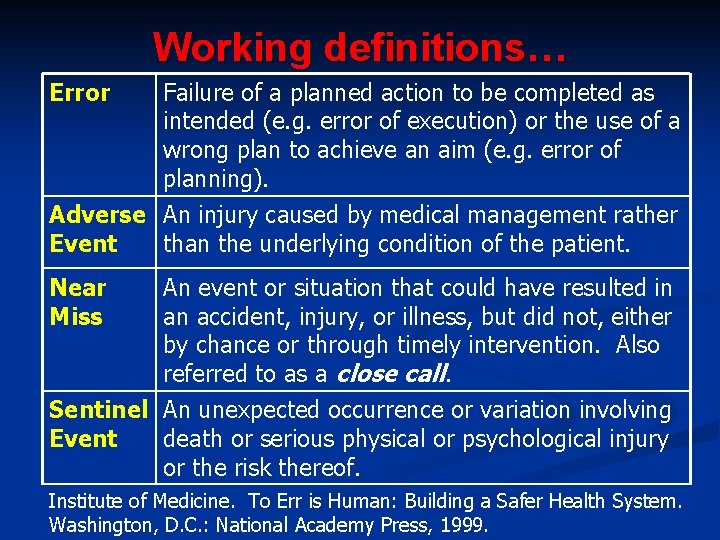
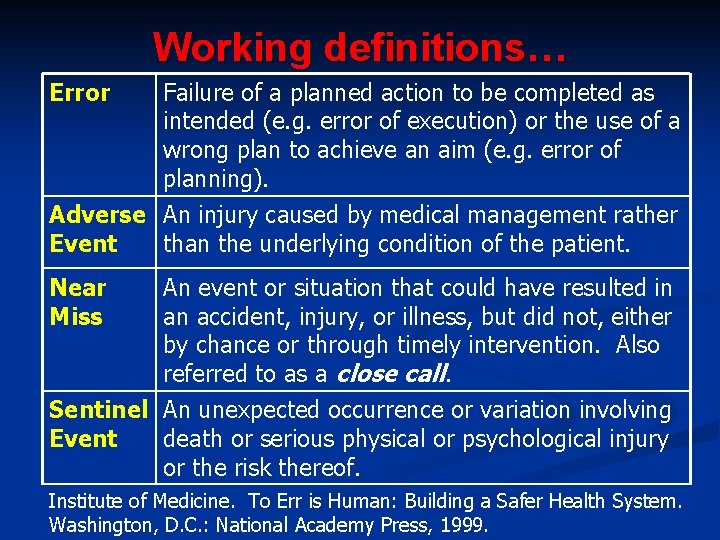
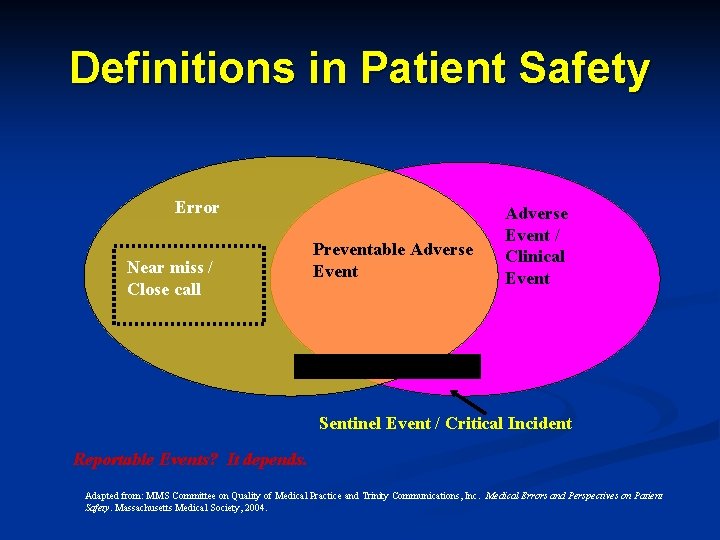
Working definitions… Error Failure of a planned action to be completed as intended (e. g. error of execution) or the use of a wrong plan to achieve an aim (e. g. error of planning). Adverse An injury caused by medical management rather Event than the underlying condition of the patient. Near Miss An event or situation that could have resulted in an accident, injury, or illness, but did not, either by chance or through timely intervention. Also referred to as a close call. Sentinel An unexpected occurrence or variation involving Event death or serious physical or psychological injury or the risk thereof. Institute of Medicine. To Err is Human: Building a Safer Health System. Washington, D. C. : National Academy Press, 1999.
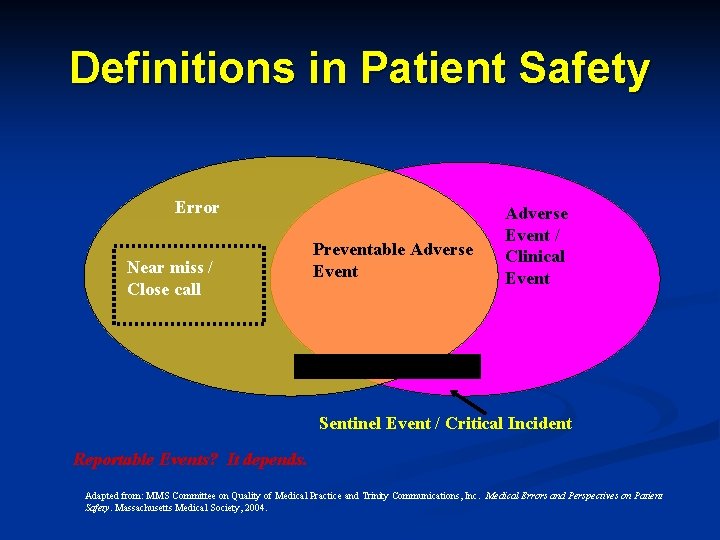
Definitions in Patient Safety Error Near miss / Close call Preventable Adverse Event / Clinical Event Sentinel Event / Critical Incident Reportable Events? It depends. Adapted from: MMS Committee on Quality of Medical Practice and Trinity Communications, Inc. Medical Errors and Perspectives on Patient Safety. Massachusetts Medical Society, 2004.
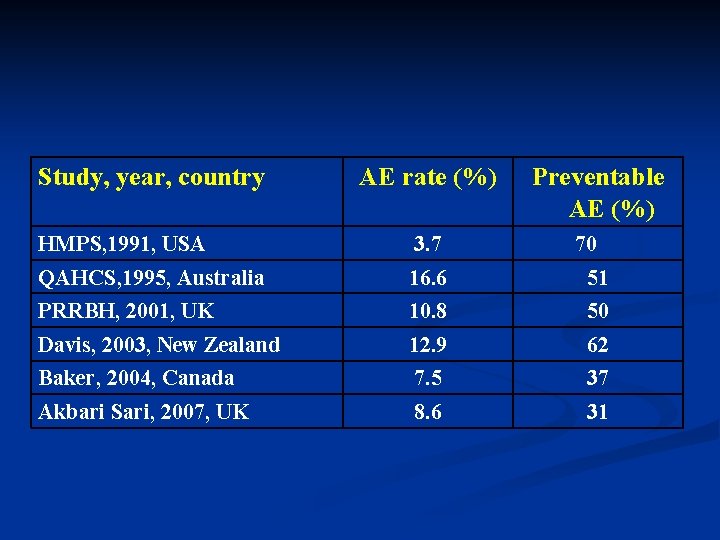
Study, year, country AE rate (%) Preventable AE (%) HMPS, 1991, USA 3. 7 70 QAHCS, 1995, Australia 16. 6 51 PRRBH, 2001, UK 10. 8 50 Davis, 2003, New Zealand 12. 9 62 Baker, 2004, Canada 7. 5 37 Akbari Sari, 2007, UK 8. 6 31

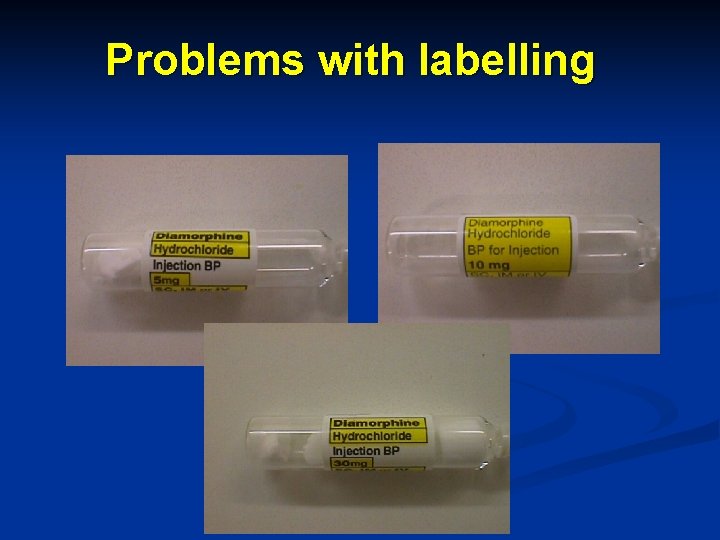
Problems with labelling
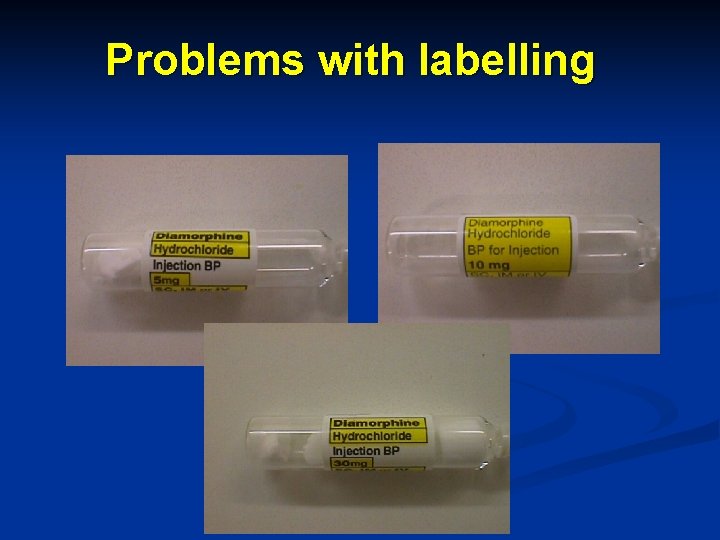
Problems with labelling
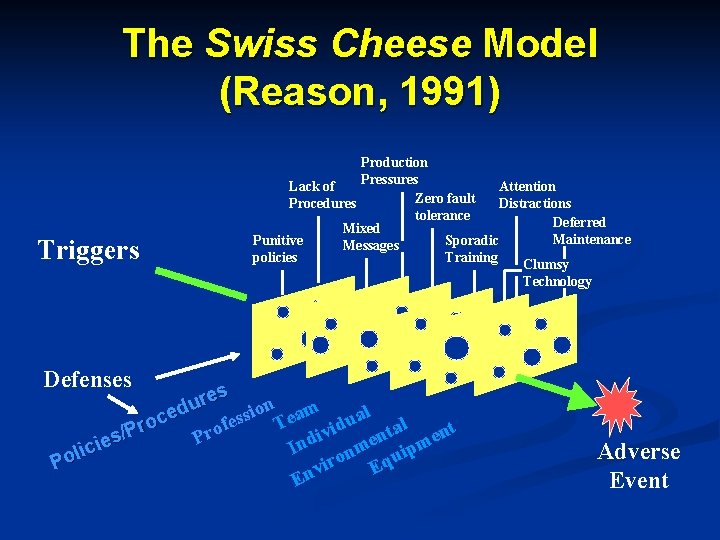
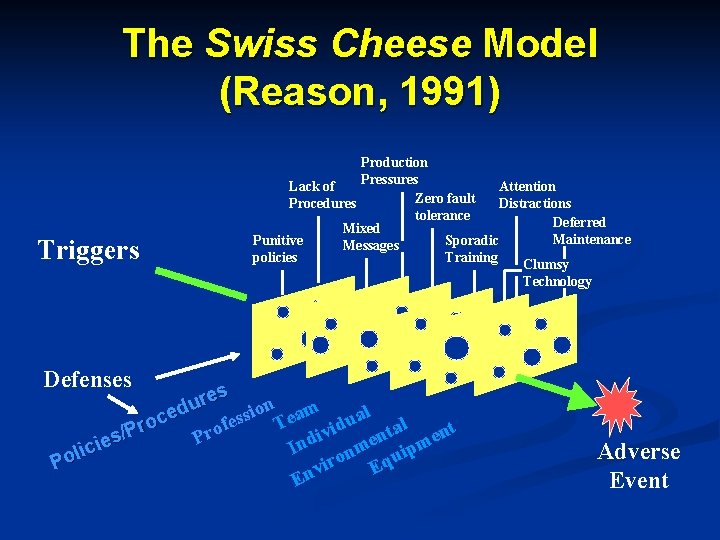
The Swiss Cheese Model (Reason, 1991) Triggers Production Pressures Lack of Attention Zero fault Procedures Distractions tolerance Deferred Mixed Maintenance Punitive Sporadic Messages policies Training Clumsy Technology Defenses es r u n am o d l i e s a c s e u e o l T f d r t a i o t P n v r / i n e s P d e m ie n m I c p i i l n u ro Eq Po i v En Adverse Event
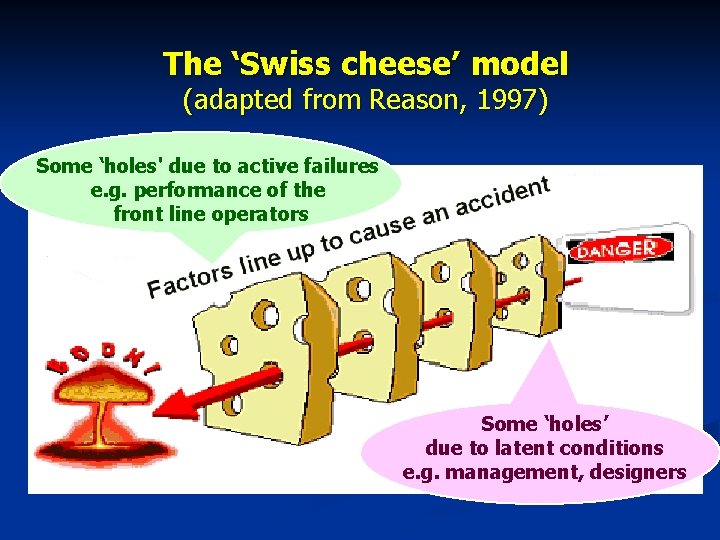
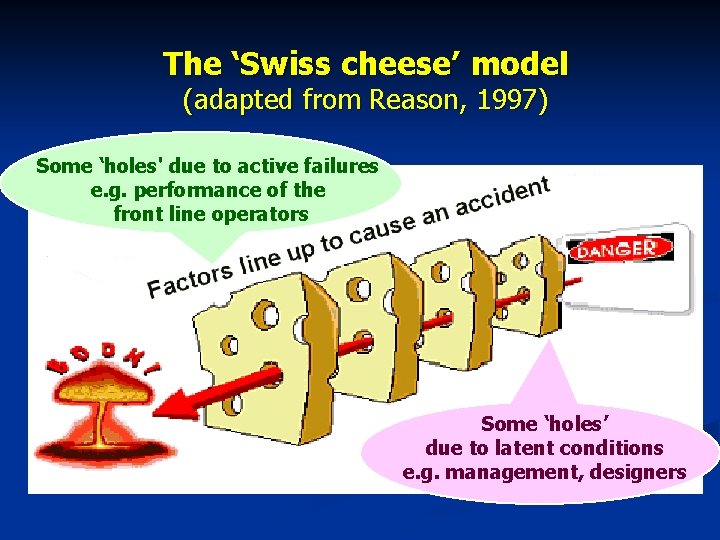
The ‘Swiss cheese’ model (adapted from Reason, 1997) Some ‘holes' due to active failures e. g. performance of the front line operators Some ‘holes’ due to latent conditions e. g. management, designers
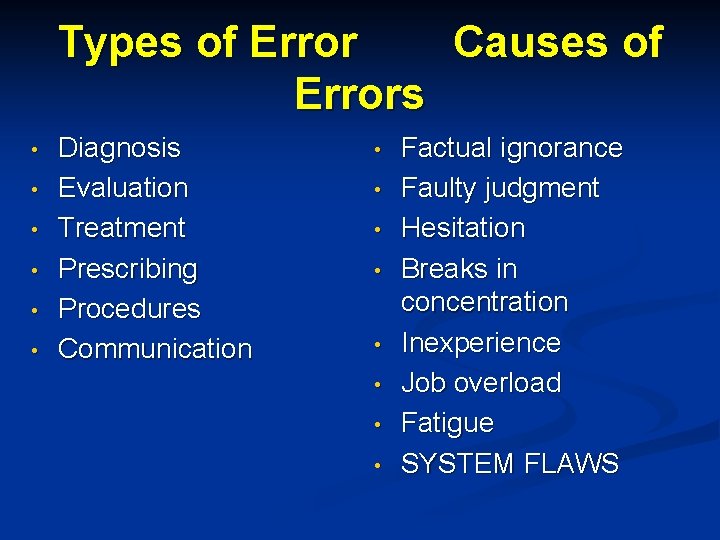
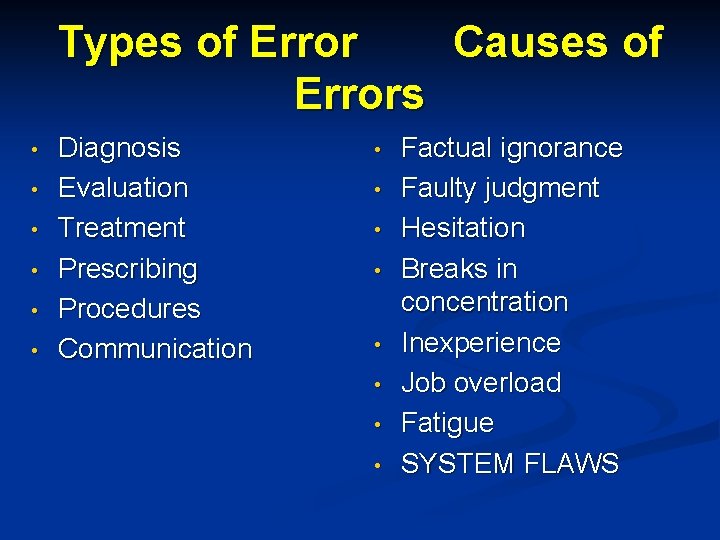
Types of Error Causes of Errors • • • Diagnosis Evaluation Treatment Prescribing Procedures Communication • • Factual ignorance Faulty judgment Hesitation Breaks in concentration Inexperience Job overload Fatigue SYSTEM FLAWS








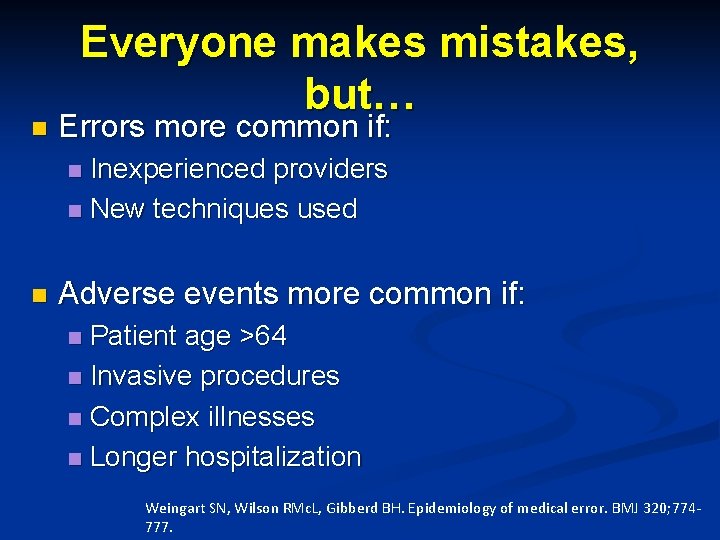
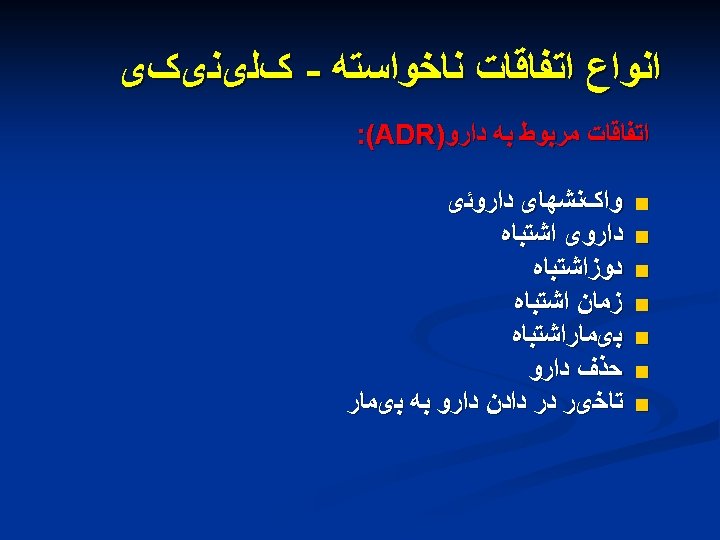
n Everyone makes mistakes, but… Errors more common if: Inexperienced providers n New techniques used n n Adverse events more common if: Patient age >64 n Invasive procedures n Complex illnesses n Longer hospitalization n Weingart SN, Wilson RMc. L, Gibberd BH. Epidemiology of medical error. BMJ 320; 774777.
Errors are inevitable …………. but most are preventable Often it is the best people who make the worst errors
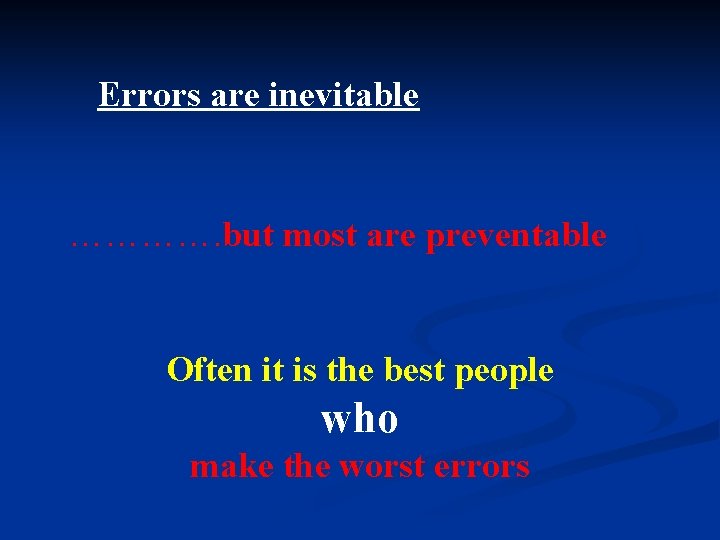
Definition of patient Safety n « Patient safety is the avoidance, prevention, and amelioration of adverse outcomes or injury from the process of health care » Charles Vincent (2006)
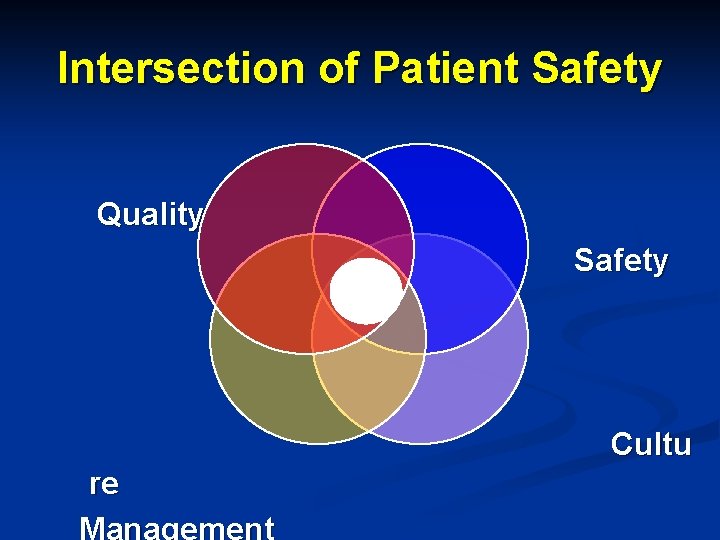
Intersection of Patient Safety Quality Safety Cultu re Management
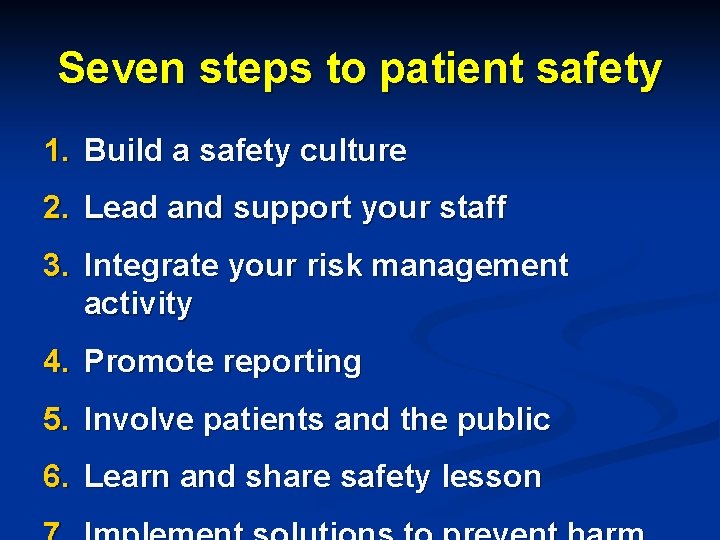
Seven steps to patient safety 1. Build a safety culture 2. Lead and support your staff 3. Integrate your risk management activity 4. Promote reporting 5. Involve patients and the public 6. Learn and share safety lesson
Patient Safety Culture n System of shared values (what is important) and beliefs (how things work) that interact with a company's people, organizational structures, and control systems to produce behavioral norms (the way we do (or do not) things around here). Webster’s Dictionary online
Organizational Culture n the sum total of an organization's ways of operating and working together. . . the shared values, beliefs and the written and unwritten policies and procedures that determine the ways in which the organization and its people behave and things that they do (and don’t do)
Organizational culture n an organizational culture may be generally described as a set of norms, beliefs, principles and ways of behaving that together give each organisation a distinctive character
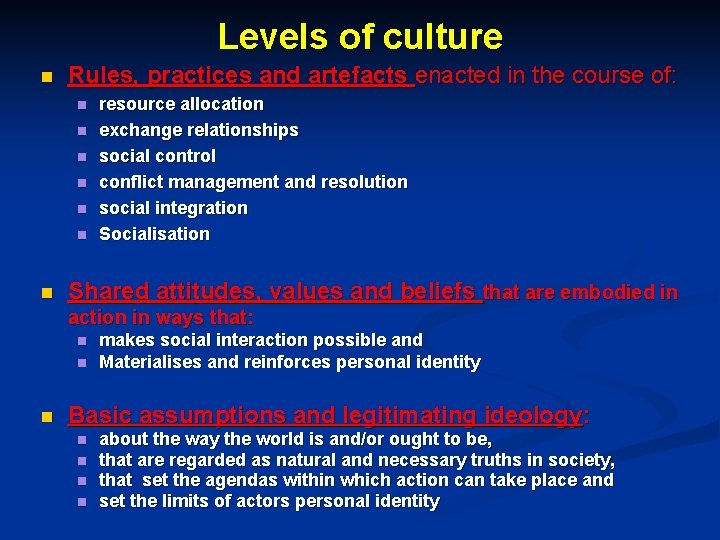
Levels of culture n Rules, practices and artefacts enacted in the course of: n n n n resource allocation exchange relationships social control conflict management and resolution social integration Socialisation Shared attitudes, values and beliefs that are embodied in action in ways that: n n n makes social interaction possible and Materialises and reinforces personal identity Basic assumptions and legitimating ideology: n n about the way the world is and/or ought to be, that are regarded as natural and necessary truths in society, that set the agendas within which action can take place and set the limits of actors personal identity
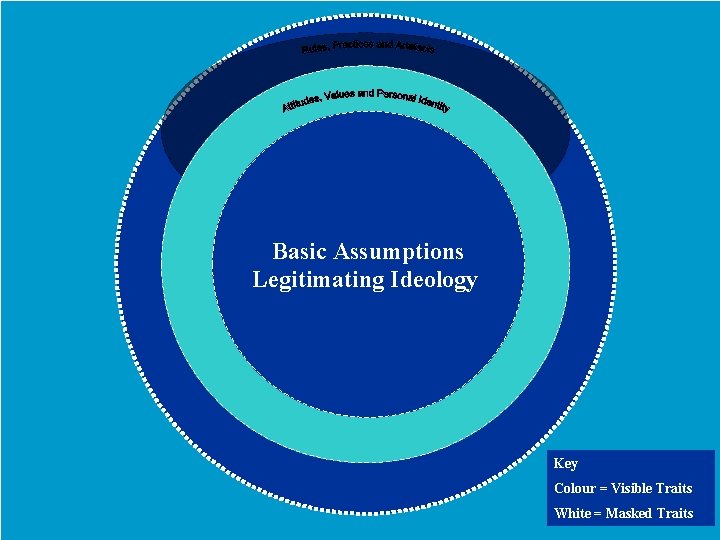
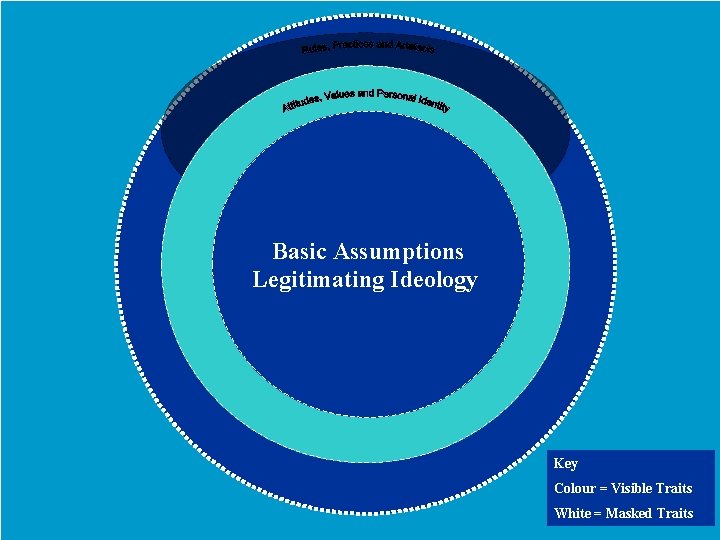
Basic Assumptions Legitimating Ideology Key Colour = Visible Traits White = Masked Traits

Approaches to the culture n Culture as an attribute , something an organization ‘has’ n Culture change agents: senior managers n What the organization ‘is’ (organization as culture) n Culture change agents: managers as well as other members of the organization
Sub-cultures n No unitary culture in health care organizations n Presence of a number of coexisting subcultures n Two approaches: n n n Subcultures relative to an organization’s overall cultural patterns (support, deny or simply coexist with the value of dominant culture) Subcultures relate to occupational, departmental, ward, specialty, clinical network, and other affiliations (e. g. enhancing cultures, orthogonal cultures and counter cultures) Both perspectives are likely to be found in an
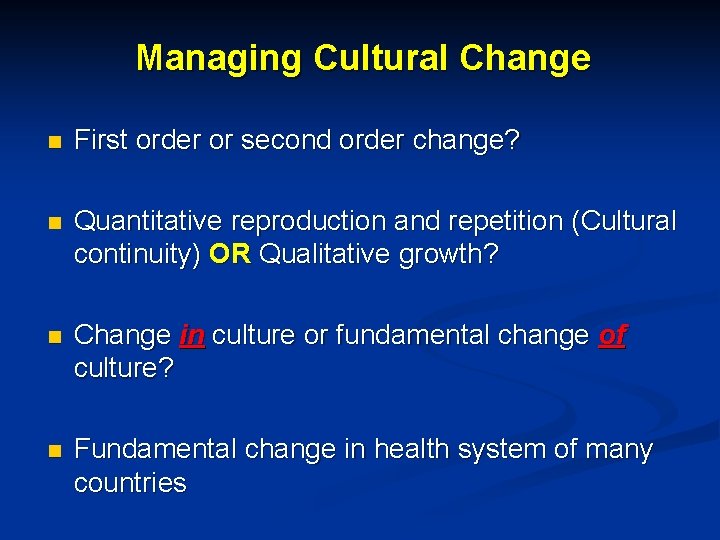
Managing Cultural Change n First order or second order change? n Quantitative reproduction and repetition (Cultural continuity) OR Qualitative growth? n Change in culture or fundamental change of culture? n Fundamental change in health system of many countries

Culture eats strategy for breakfast every morning

n Key sources of organizational inertia and resistance to cultural change Lack of ownership n Complexity n External influence n Lack of appropriate leadership n Cultural diversity n Dysfunctional consequences
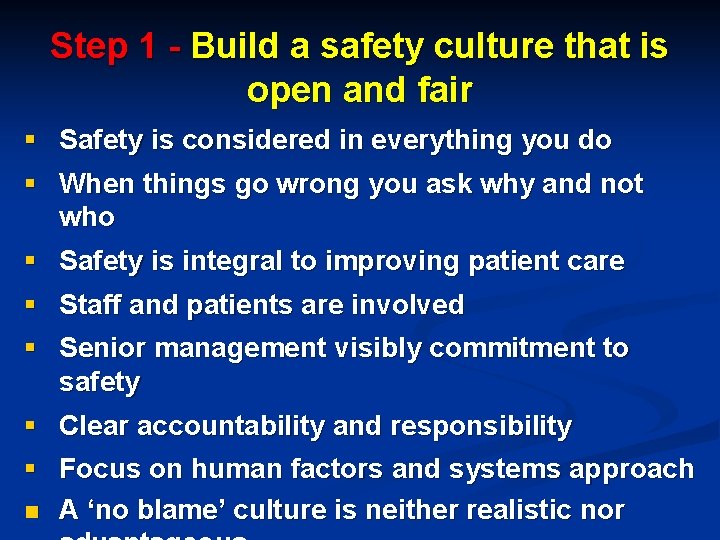
Step 1 - Build a safety culture that is open and fair § Safety is considered in everything you do § When things go wrong you ask why and not who § Safety is integral to improving patient care § Staff and patients are involved § Senior management visibly commitment to safety § Clear accountability and responsibility § Focus on human factors and systems approach n A ‘no blame’ culture is neither realistic nor
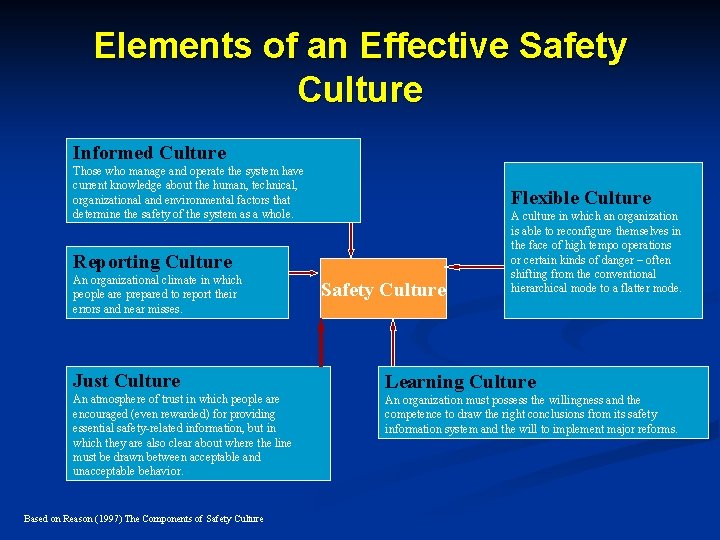
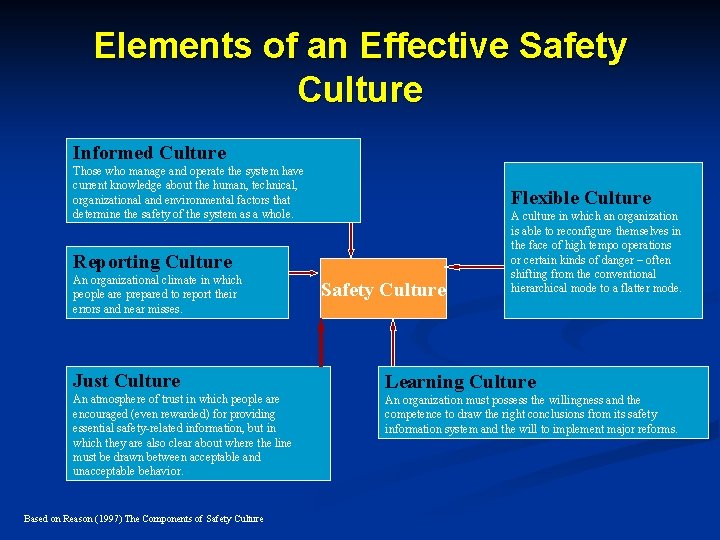
Elements of an Effective Safety Culture Informed Culture Those who manage and operate the system have current knowledge about the human, technical, organizational and environmental factors that determine the safety of the system as a whole. Flexible Culture Reporting Culture An organizational climate in which people are prepared to report their errors and near misses. Safety Culture A culture in which an organization is able to reconfigure themselves in the face of high tempo operations or certain kinds of danger – often shifting from the conventional hierarchical mode to a flatter mode. Just Culture Learning Culture An atmosphere of trust in which people are encouraged (even rewarded) for providing essential safety-related information, but in which they are also clear about where the line must be drawn between acceptable and unacceptable behavior. An organization must possess the willingness and the competence to draw the right conclusions from its safety information system and the will to implement major reforms. Based on Reason (1997) The Components of Safety Culture
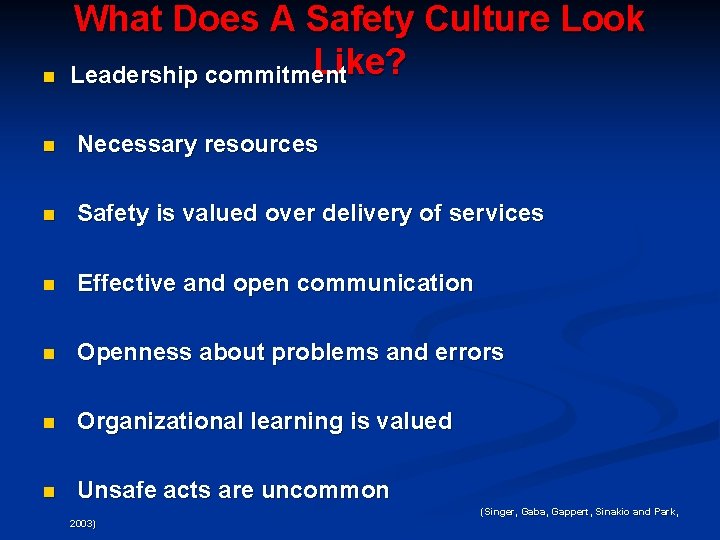
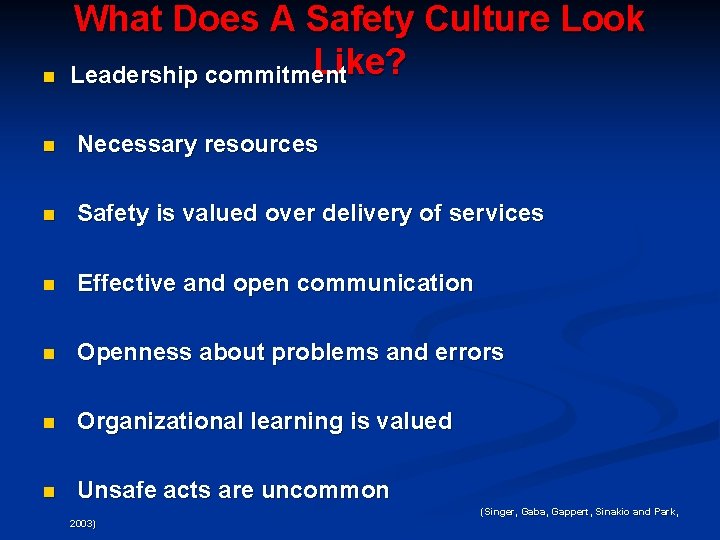
n What Does A Safety Culture Look Like? Leadership commitment n Necessary resources n Safety is valued over delivery of services n Effective and open communication n Openness about problems and errors n Organizational learning is valued n Unsafe acts are uncommon (Singer, Gaba, Gappert, Sinakio and Park, 2003)
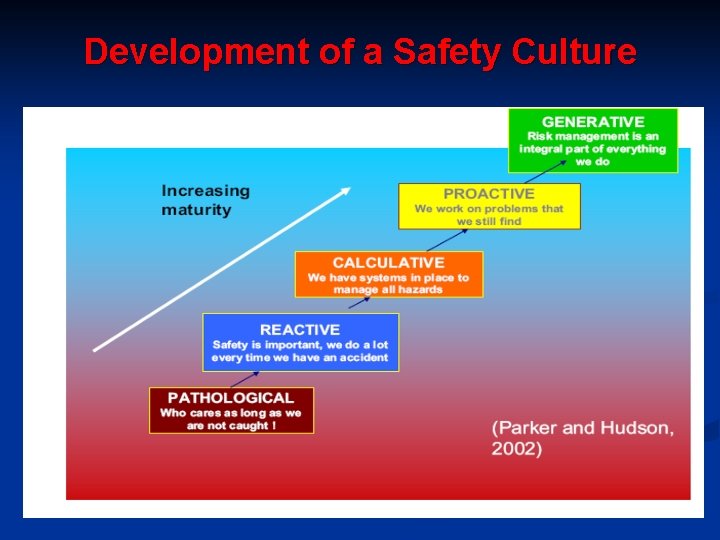
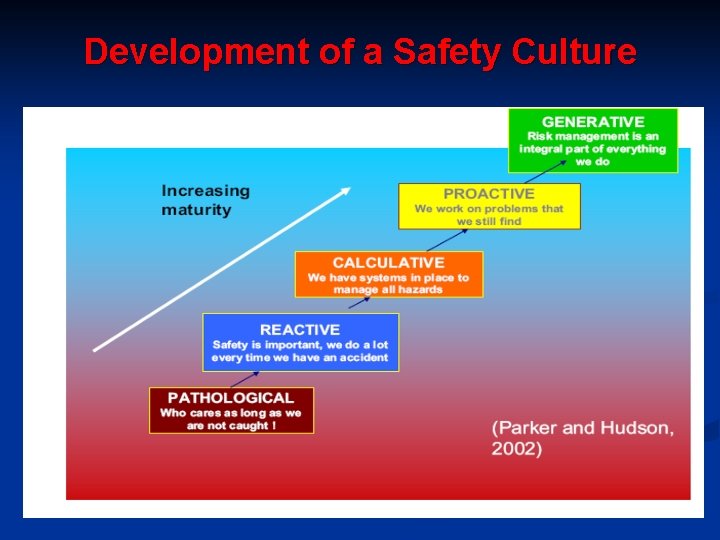
Development of a Safety Culture
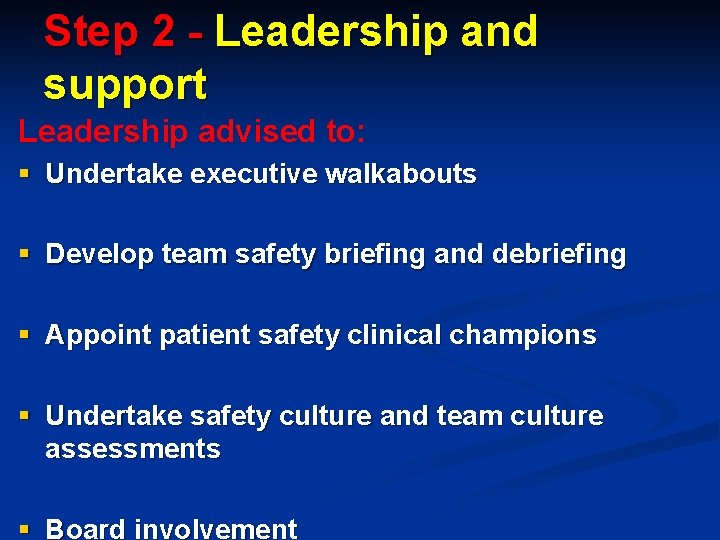
Step 2 - Leadership and support Leadership advised to: § Undertake executive walkabouts § Develop team safety briefing and debriefing § Appoint patient safety clinical champions § Undertake safety culture and team culture assessments § Board involvement
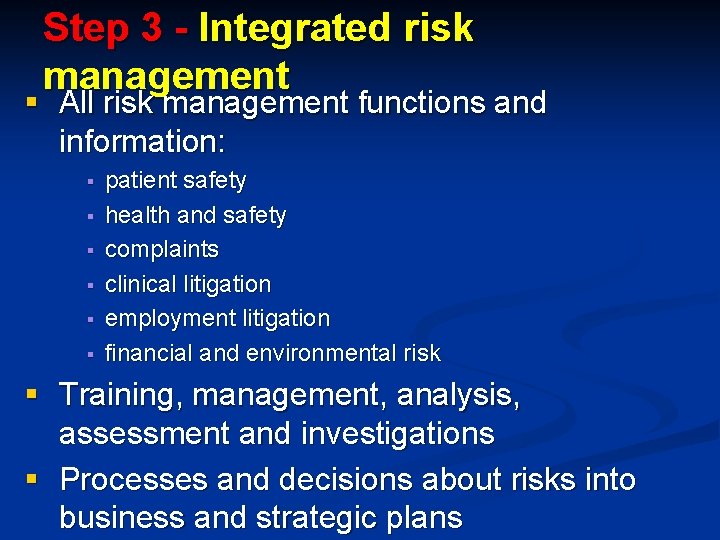
Step 3 - Integrated risk management § All risk management functions and information: § § § patient safety health and safety complaints clinical litigation employment litigation financial and environmental risk § Training, management, analysis, assessment and investigations § Processes and decisions about risks into business and strategic plans
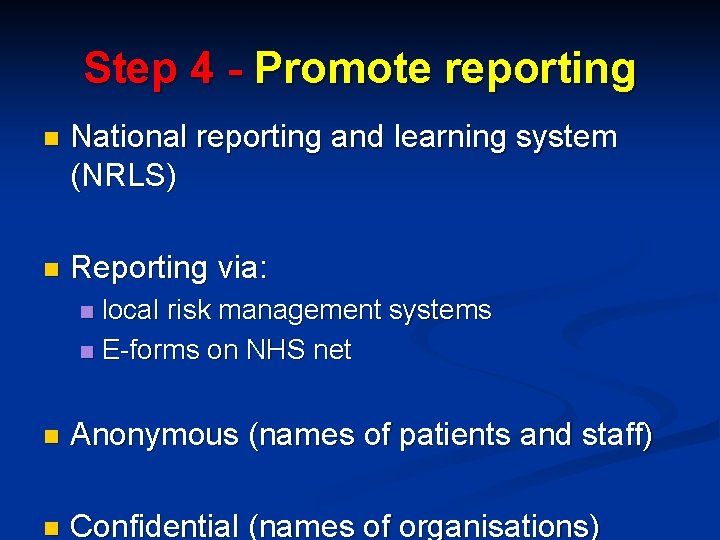
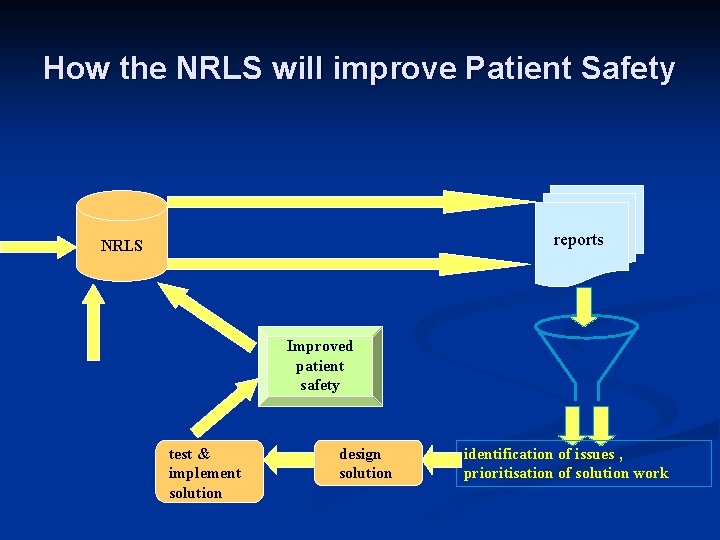
Step 4 - Promote reporting n National reporting and learning system (NRLS) n Reporting via: local risk management systems n E-forms on NHS net n n Anonymous (names of patients and staff) n Confidential (names of organisations)
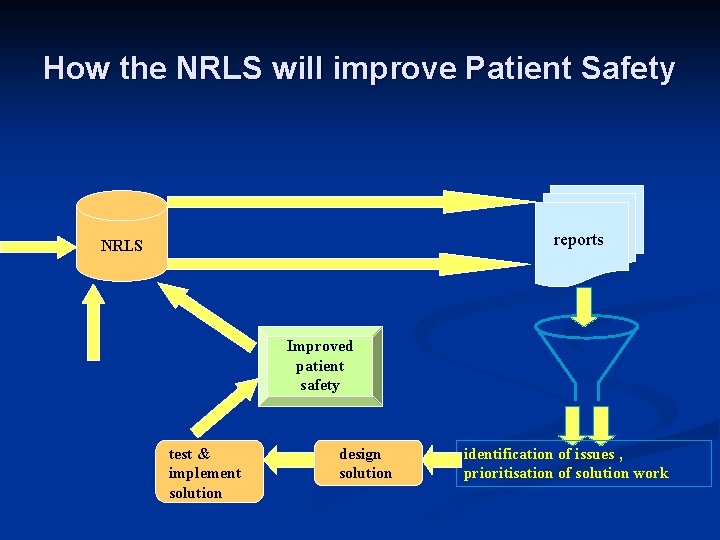
How the NRLS will improve Patient Safety standard reports dataset NRLS reports ad hoc reports other data sources monitor impact test & implement solution Improved patient safety design solution identification of issues , prioritisation of solution work
Step 5 - Involve and communicate with patients and the public n Initiatives: § § Being Open Ask about medicines leaflets SPEAK UP Involve in investigation
Step 6 - Learn and share safety lessons n NPSA Root Cause Analysis Programme n Over 6000 NHS staff trained in RCA methodology n E-learning toolkit n Guidance n Aggregated themed RCA n RCA data capture possibilities n Training for independent investigations
Learning organization and levels of learning n is an organization that posits learning as a core characteristic n Single-loop learning n Double-loop learning n Meta-learning
Step 7 - Solutions to Prevent Harm n Address root causes n Make designs of equipment, systems, processes, more intuitive n Make wrong actions more difficult n Make incorrect actions correct n Make it easier to discover error

Design out the problem (design solution)

Improving Labelling and Packaging A partnership with UK manufacturers of Methotrexate to develop novel packaging designs

Some preventative strategies n Legislation, accreditation n Organization, structure, and culture n Education/training interventions n Reporting systems n Information analysis
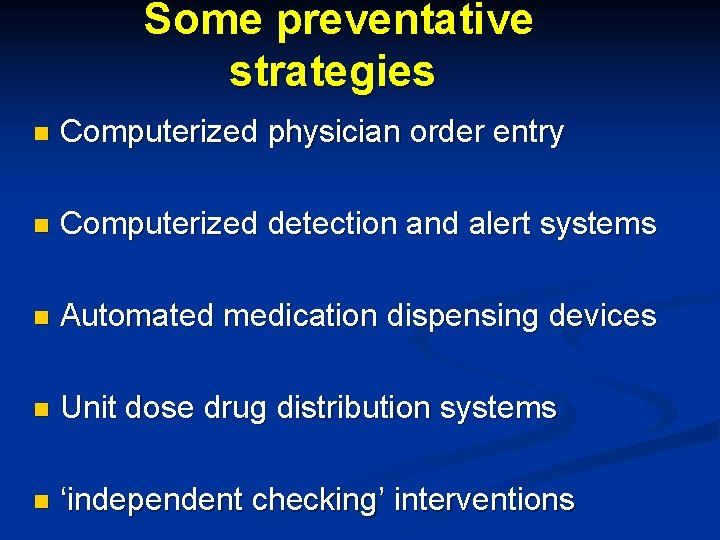
Some preventative strategies n Computerized physician order entry n Computerized detection and alert systems n Automated medication dispensing devices n Unit dose drug distribution systems n ‘independent checking’ interventions
When faced with adversity, use your initiative wisely…


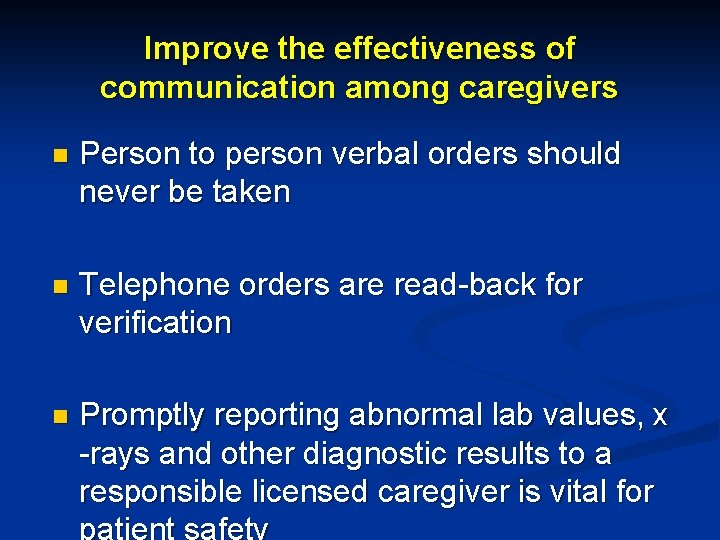
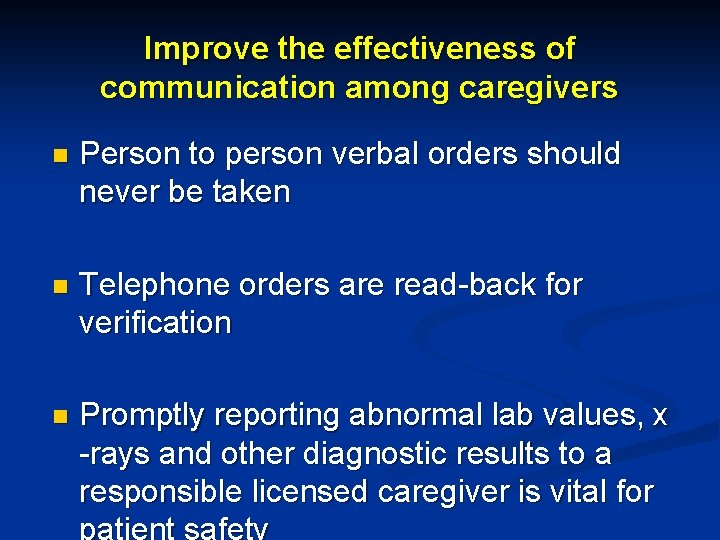
Improve the effectiveness of communication among caregivers n Person to person verbal orders should never be taken n Telephone orders are read-back for verification n Promptly reporting abnormal lab values, x -rays and other diagnostic results to a responsible licensed caregiver is vital for
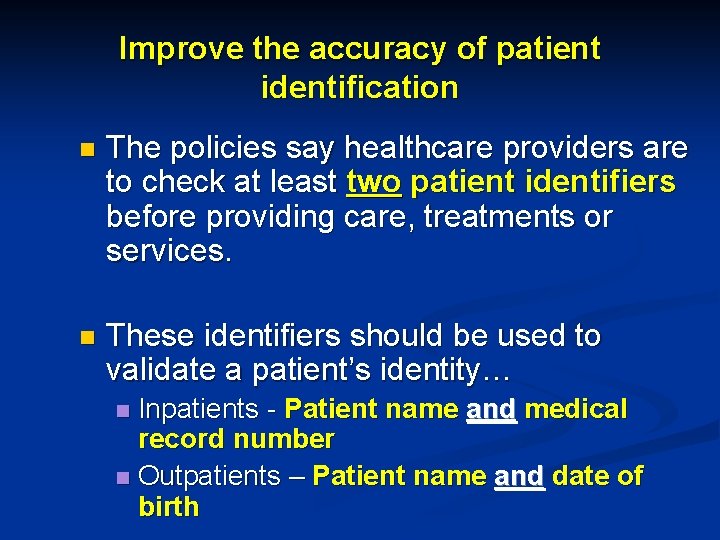
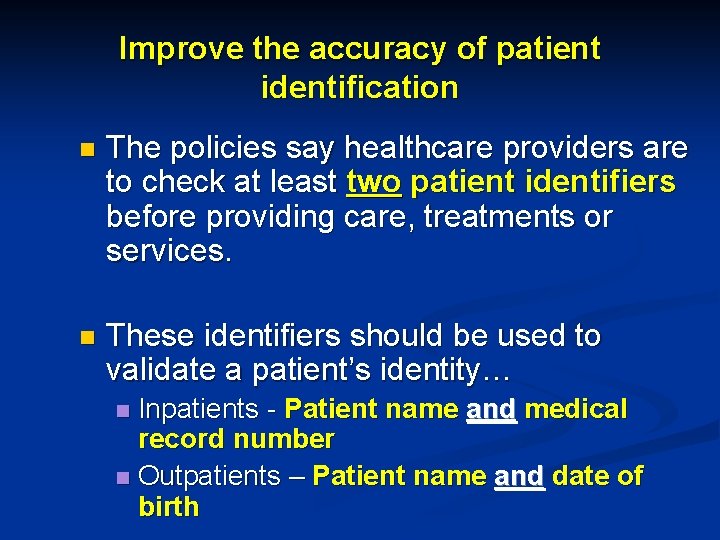
Improve the accuracy of patient identification n The policies say healthcare providers are to check at least two patient identifiers before providing care, treatments or services. n These identifiers should be used to validate a patient’s identity… Inpatients - Patient name and medical record number n Outpatients – Patient name and date of birth n

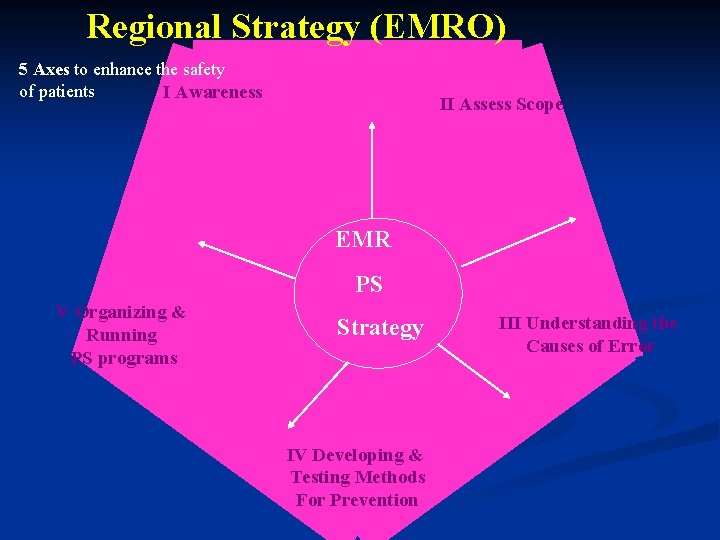
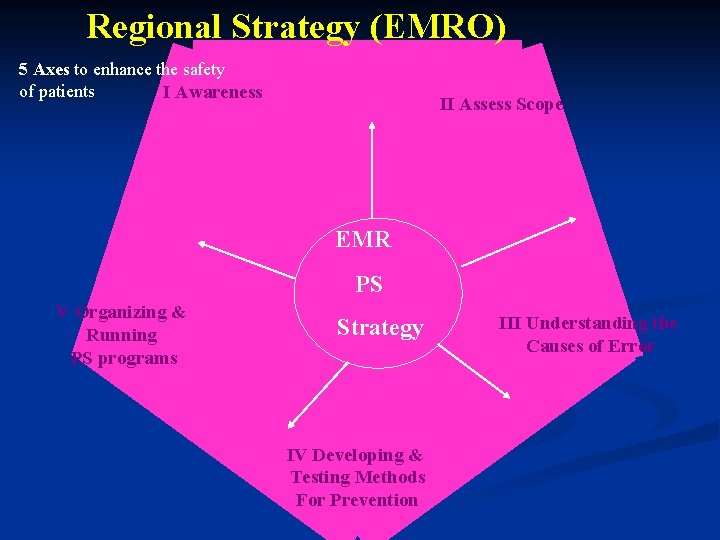
Regional Strategy (EMRO) 5 Axes to enhance the safety of patients I Awareness II Assess Scope EMR PS V Organizing & Running PS programs Strategy IV Developing & Testing Methods For Prevention 135 III Understanding the Causes of Error

Patient Safety Friendly Hospital Initiative (PSFHI) encouraging safe hospital practices in the Eastern Mediterranean region (EMR)

Global Patient Safety Challenges 1 st Global PS Challenge: Clean Care is Safer Care

1 st Global Patient Safety Challenge: Clean Care is Safer Care √ √ Launched Challenge Pilot site 138 Complementary site √ √ √ √
2 nd Global Patient Safety Challenge: Safe Surgery Saves Lives Development of a surgical checklist for patient safety

2 nd GPSC: Safe Surgery Saves Lives Pilot site for surgical checklist
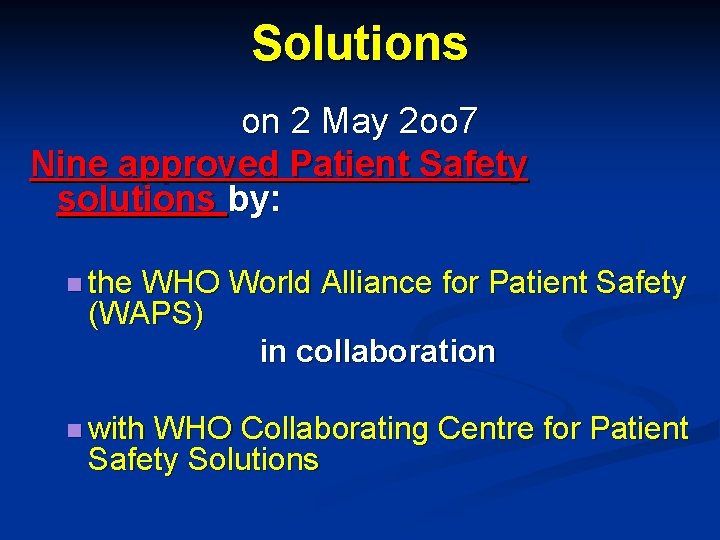
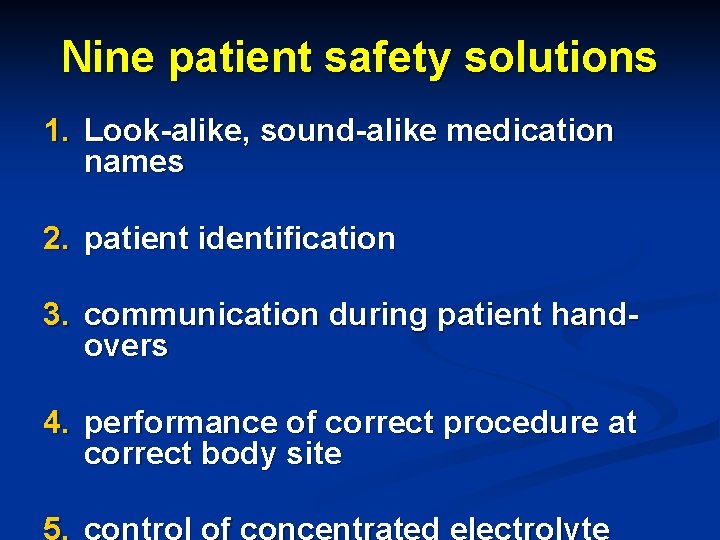
Solutions on 2 May 2 oo 7 Nine approved Patient Safety solutions by: n the WHO World Alliance for Patient Safety (WAPS) in collaboration n with WHO Collaborating Centre for Patient Safety Solutions
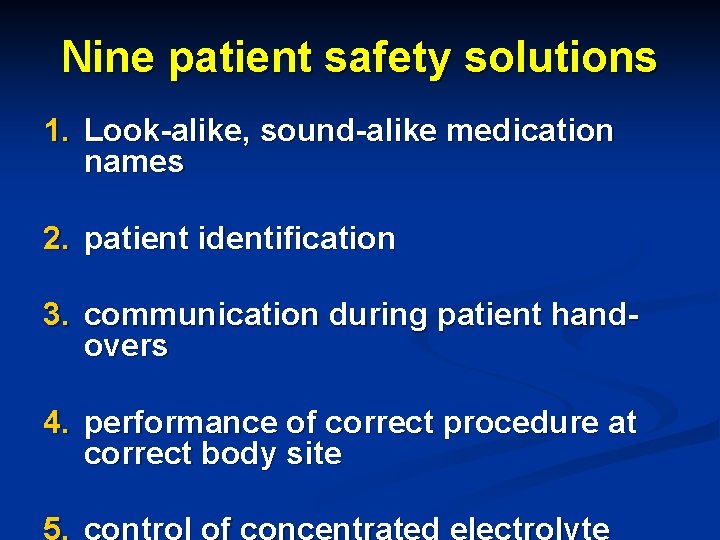
Nine patient safety solutions 1. Look-alike, sound-alike medication names 2. patient identification 3. communication during patient handovers 4. performance of correct procedure at correct body site
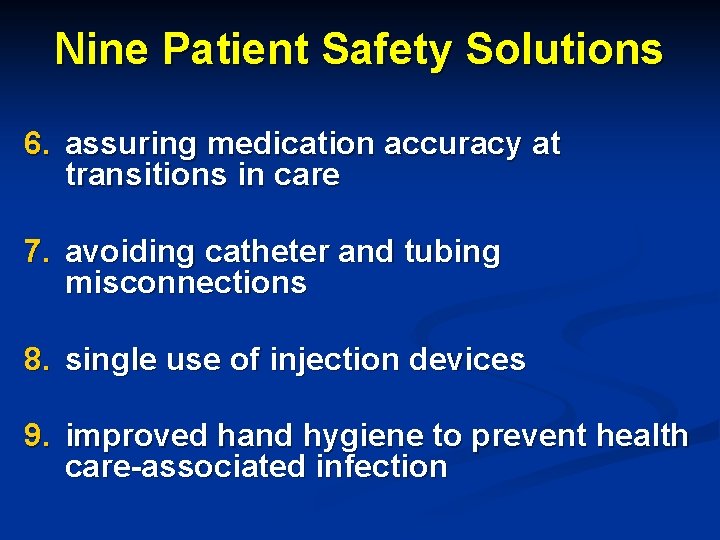
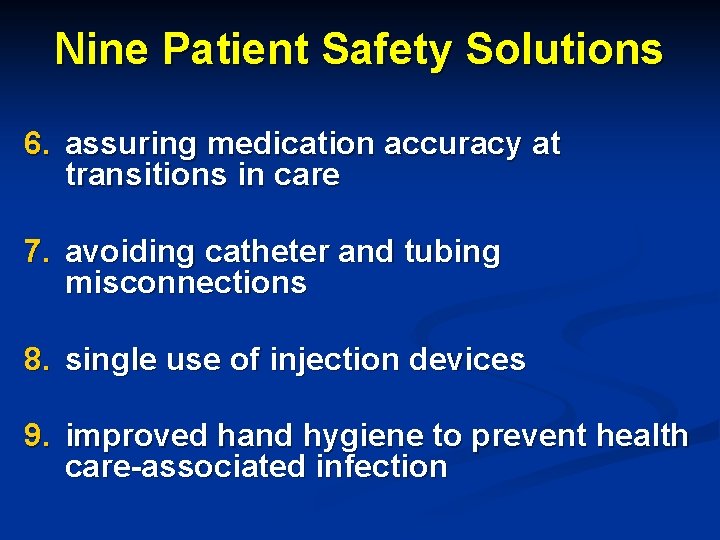
Nine Patient Safety Solutions 6. assuring medication accuracy at transitions in care 7. avoiding catheter and tubing misconnections 8. single use of injection devices 9. improved hand hygiene to prevent health care-associated infection




 Market risk assessment
Market risk assessment Safety incident management system
Safety incident management system Patient 2 patient
Patient 2 patient Key risk indicators template
Key risk indicators template Risk map risk management
Risk map risk management Ccps process safety elements
Ccps process safety elements Safety risk management faa
Safety risk management faa Hamid khattak
Hamid khattak Hamid vakilzadian
Hamid vakilzadian Hamid vakilzadian
Hamid vakilzadian Hamid vazin
Hamid vazin Alia hamid
Alia hamid Hamid rahim
Hamid rahim Hamid sebaly
Hamid sebaly Ashley bucsek
Ashley bucsek Hamid mahini
Hamid mahini Hamid yeşilyayla
Hamid yeşilyayla Hamid d. ismail
Hamid d. ismail Hamid boulares
Hamid boulares Hamid harroud
Hamid harroud Hamid yunis
Hamid yunis Dr hamid rabiee
Dr hamid rabiee Doc zainul abidin hamid
Doc zainul abidin hamid Hamid zolfaghari
Hamid zolfaghari Hamid sebaly
Hamid sebaly Hamid rashid finterra
Hamid rashid finterra Edy suandi hamid
Edy suandi hamid Edy suandi hamid
Edy suandi hamid Rania hamid
Rania hamid Scottish patient safety programme
Scottish patient safety programme Solutions for patient safety bundles
Solutions for patient safety bundles 13 malaysian patient safety goals
13 malaysian patient safety goals National patient safety goals 2012
National patient safety goals 2012 Patient safety incident policy
Patient safety incident policy To err is human to cover up is unforgivable
To err is human to cover up is unforgivable The national patient safety goal 6
The national patient safety goal 6 Chapter 27 patient safety and quality
Chapter 27 patient safety and quality Patient environment and safety
Patient environment and safety Patient safety definition
Patient safety definition Nj patient safety act
Nj patient safety act Patient sitter algorithm
Patient sitter algorithm Dod patient safety program
Dod patient safety program Q2 national patient safety goals
Q2 national patient safety goals Sue sheridan patient safety
Sue sheridan patient safety 13 malaysian safety goals
13 malaysian safety goals National patient safety goals 2017
National patient safety goals 2017 Patient safe solutions
Patient safe solutions Solutions for patient safety bundles
Solutions for patient safety bundles 2013 hospital national patient safety goals
2013 hospital national patient safety goals Patient safety goals
Patient safety goals Patient safety and quality care movement
Patient safety and quality care movement National patient safety framework
National patient safety framework Npsg 8
Npsg 8 Scottish patient safety programme
Scottish patient safety programme Canadian patient safety officer course
Canadian patient safety officer course Patient safety evaluation system
Patient safety evaluation system Ahrq patient safety survey
Ahrq patient safety survey Risk projection attempts to rate each risk in two ways
Risk projection attempts to rate each risk in two ways Risk avoidance
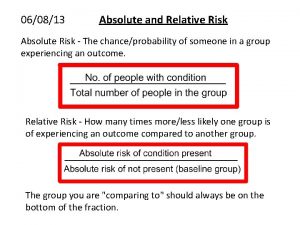
Risk avoidance Absolute risk vs relative risk
Absolute risk vs relative risk Residual risk and secondary risk pmp
Residual risk and secondary risk pmp Ar = ir x cr x dr
Ar = ir x cr x dr Absolute risk vs relative risk
Absolute risk vs relative risk Activity sheet 2: stock market calculations
Activity sheet 2: stock market calculations Pestle risk classification system
Pestle risk classification system Pembelanjaan risiko
Pembelanjaan risiko The biggest risk is not taking any risks
The biggest risk is not taking any risks Ir x cr x dr
Ir x cr x dr Business risk and financial risk leverage
Business risk and financial risk leverage Relative risk calculation
Relative risk calculation Measure of association formula
Measure of association formula Hierarchy risk assessment
Hierarchy risk assessment Health and safety risk assessment template
Health and safety risk assessment template Freedom from danger
Freedom from danger Safety depth formula in ecdis
Safety depth formula in ecdis Safety care training
Safety care training Personal safety vs process safety
Personal safety vs process safety Safety assessment for ind safety reporting
Safety assessment for ind safety reporting 00101-15 basic safety
00101-15 basic safety 00101-15 basic safety
00101-15 basic safety Sap patient management
Sap patient management Obsessive compulsive disorder nursing care plan
Obsessive compulsive disorder nursing care plan The process of classifying and reviewing past due accounts
The process of classifying and reviewing past due accounts Resource patient management system
Resource patient management system Cataract nursing diagnosis
Cataract nursing diagnosis Patient management problem
Patient management problem Patient blood management definition
Patient blood management definition Padded tongue blade
Padded tongue blade Hospital management system patient registration form
Hospital management system patient registration form Skeletal traction vs skin traction
Skeletal traction vs skin traction Top management and middle management
Top management and middle management Management pyramid
Management pyramid Middle level management
Middle level management Wvu risk management
Wvu risk management Risk management cook county
Risk management cook county Uaf risk management
Uaf risk management Wharton insurance and risk management
Wharton insurance and risk management Cal state
Cal state Ibm smarter supply chain
Ibm smarter supply chain Data governance and risk management
Data governance and risk management Internal audit definition
Internal audit definition Risk management in telecommunication projects
Risk management in telecommunication projects Supply chain risk management framework
Supply chain risk management framework Supply chain risk management framework
Supply chain risk management framework Cisco supply chain risk management
Cisco supply chain risk management Wichtiger chain
Wichtiger chain Steps in risk management process
Steps in risk management process Software project risk
Software project risk Proactive risk management in software engineering
Proactive risk management in software engineering Clinical risk management in dentistry
Clinical risk management in dentistry Risk management plus online
Risk management plus online Risk projection
Risk projection Risk management for water and wastewater utilities
Risk management for water and wastewater utilities Risk register hse
Risk register hse Civil engineering risk assessment example
Civil engineering risk assessment example Risk management for enterprises and individuals
Risk management for enterprises and individuals Risk management in industrial engineering
Risk management in industrial engineering Anz credit risk
Anz credit risk Four stages of risk management
Four stages of risk management Risk management references
Risk management references Pmbok risk management definition
Pmbok risk management definition Avoidance risk
Avoidance risk Operational risk assessment worksheet
Operational risk assessment worksheet Orca risk management
Orca risk management First step in orm process
First step in orm process Swot analysis risk management
Swot analysis risk management Certification course in risk management nibm
Certification course in risk management nibm Literature review on enterprise risk management
Literature review on enterprise risk management Rmf process
Rmf process Reactive risk strategies in software engineering
Reactive risk strategies in software engineering Risk separation
Risk separation Introduction to financial risk management
Introduction to financial risk management Federal flood risk management standard ffrms
Federal flood risk management standard ffrms Fatality risk management
Fatality risk management Framp falls risk
Framp falls risk Risk management ucsf
Risk management ucsf Inherent risks examples
Inherent risks examples Vertical slice architecture
Vertical slice architecture Risk management report geotab
Risk management report geotab Risk management dynamics
Risk management dynamics Dynamic risk assessment training
Dynamic risk assessment training Disaster equation examples
Disaster equation examples Data risk framework
Data risk framework Contract risk management process
Contract risk management process Goldman sachs risk management framework
Goldman sachs risk management framework Sands of iwo jima life is tough
Sands of iwo jima life is tough Citigroup risk management framework
Citigroup risk management framework Financial management chapter 8 risk and return
Financial management chapter 8 risk and return