RISK MANAGEMENT Understanding the risks of clinical practice





- Slides: 43
RISK MANAGEMENT Understanding the risks of clinical practice and overcoming them in a planned and positive way.
BENEFITS OF RISK MANAGEMENT Improved patient care Reduction in risk exposure Closer working relationship inside the dental team Improved patient acceptance at proposed treatment Growth in demand of services
AIMS OF RISK MANAGEMENT • Assess continuously what could go wrong • Determine which risks are important to deal with • Implement strategies to deal with no risks

RISK IDENTIFICATION § Clinical risk § Operational risk § Business risk § Reputation risk
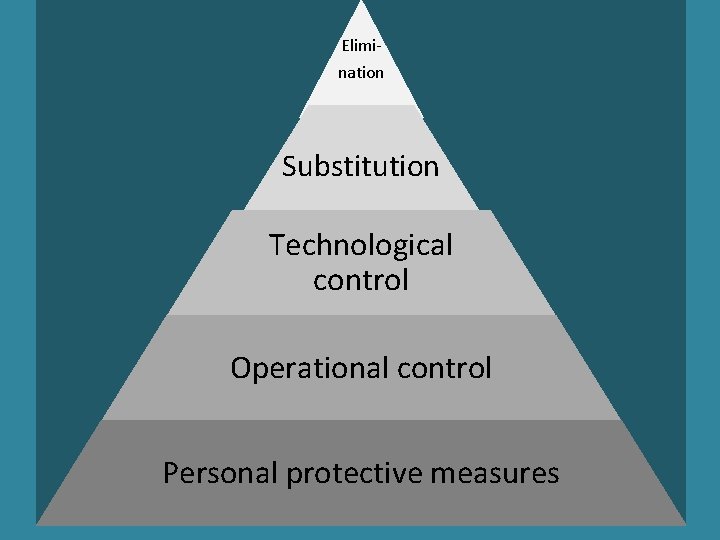
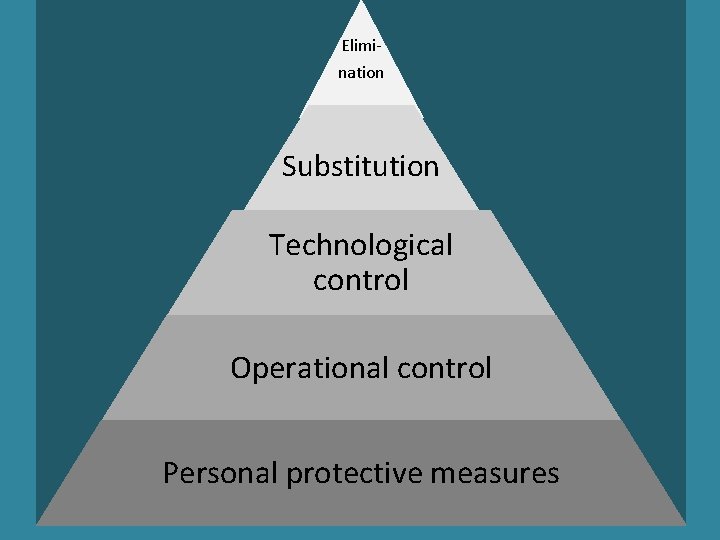
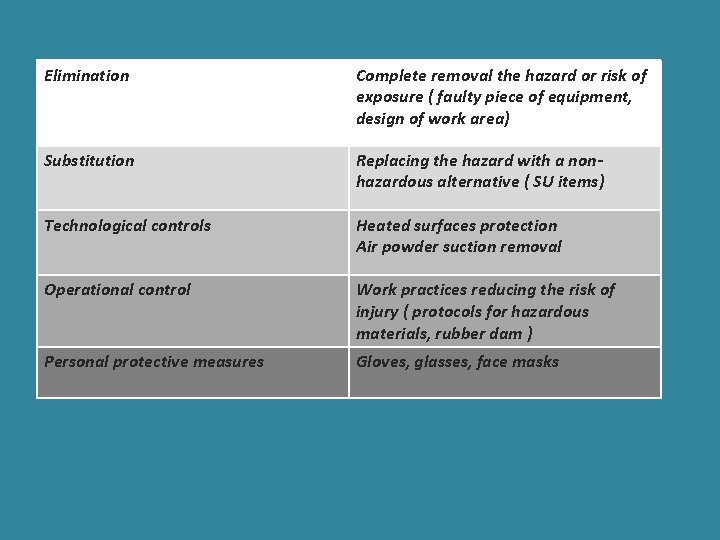
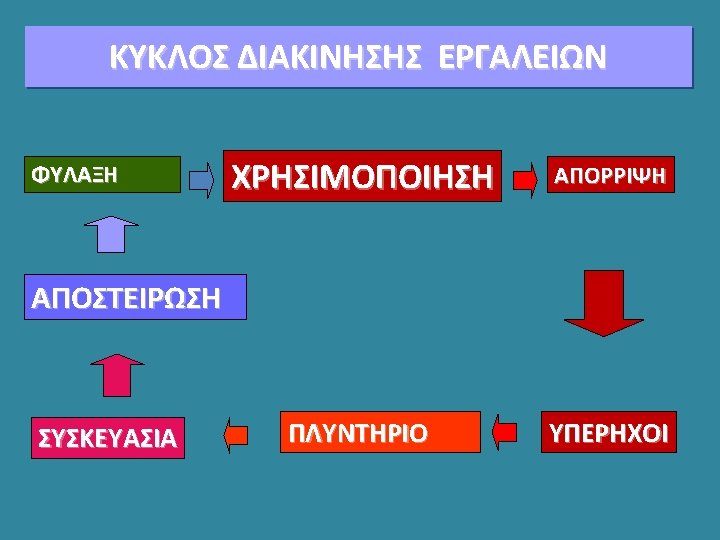
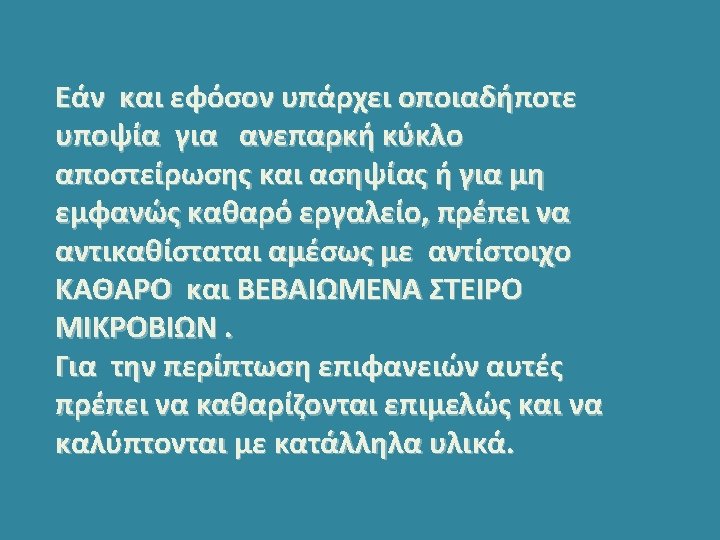
Elimination Substitution Technological control Operational control Personal protective measures
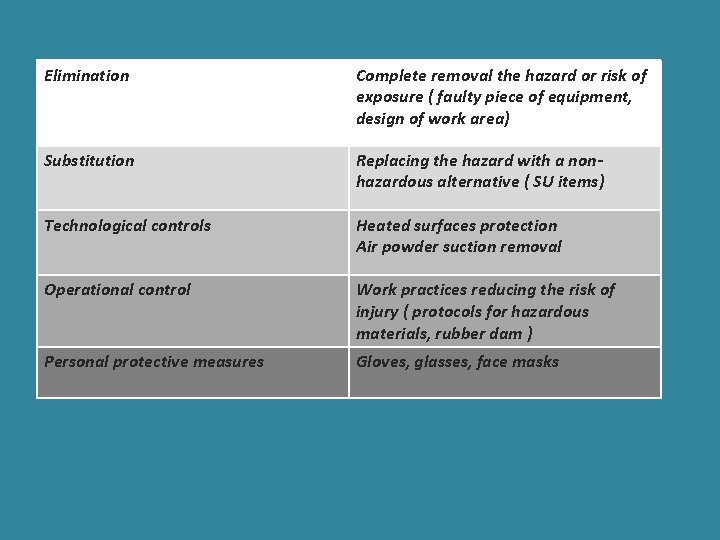
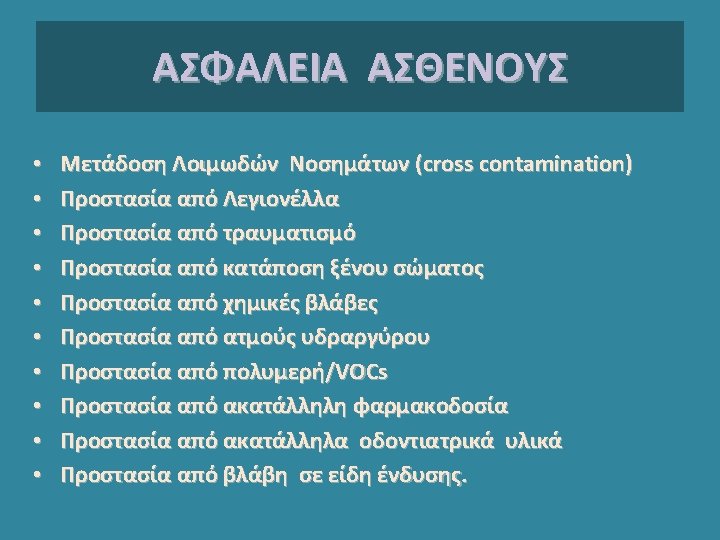
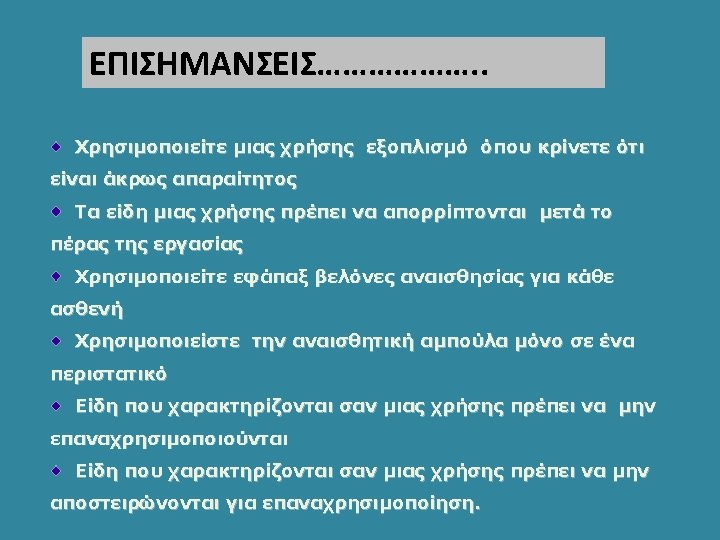
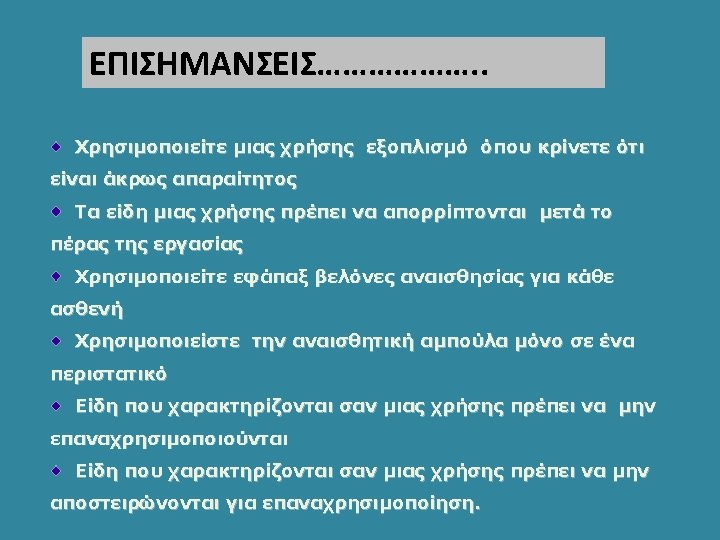
Elimination Complete removal the hazard or risk of exposure ( faulty piece of equipment, design of work area) Substitution Replacing the hazard with a nonhazardous alternative ( SU items) Technological controls Heated surfaces protection Air powder suction removal Operational control Work practices reducing the risk of injury ( protocols for hazardous materials, rubber dam ) Personal protective measures Gloves, glasses, face masks
• CED RECOMMENDATIONS TO ITS MEMBER ORGANISATIONS • The CED recommends that its member organisations: • Seek to ensure that patient safety is part of undergraduate and post-graduate dental training curricula, to strengthen further the patient safety culture in healthcare. • Encourage their dentists to be actively aware of the various elements of their professional practice where patient safety can be compromised. • Encourage their dentists and the rest of the dental team to participate in continuing professional development relating to patient safety, to keep knowledge and skills up to date. • Ensure that dentists have a knowledge of languages necessary for practising in their country, in particular in order that they be able to communicate with patients and other professionals. • Seek to ensure that patient data is safely stored and available to health professionals as and when required, in accordance with national law. • Ensure official registration of qualifications of dentists. • Ensure transparency of the qualifications and competences of all other members of the dental team, as required by national law. • Consider establishing “study groups” to provide a forum for local dentists to discuss experiences openly and learn from each other. • Seek to introduce national systems for voluntarily and anonymously reporting adverse events, near misses and problems with medical devices, to enable all dentists to learn from their own and others’ experiences. • Promote the CED code of ethics and national ethical codes, since strong ethics underpin high quality and safety.
CED WG PATIENT SAFETY SUMMARY OF CED POSITIONS ON PATIENT SAFETY CED-DOC-2011 -013 1. European dentists are committed to providing safe and high quality dental care and minimising risks arising from dental care. While “zero-risk” medical care does not exist, improving patient safety and quality of care is an on-going preoccupation for the dental profession. 2. Action aimed at improving patient safety and quality of care should take into account the various healthcare settings in which patients are treated. The types of patient safety risks and the most appropriate ways of minimising them vary according to the health setting. Most dental care in Europe is provided in liberal practice, in small structures, and in an environment where the dentist generally has complete individual responsibility for the whole procedure. 3. New measures aimed at improving patient safety should not add to the bureaucratic burden in the dental practice to the extent that they would hinder dentists from spending sufficient time with each patient. Devoting sufficient time to each patient is an important parameter of safe and high quality dental care. 4. Reduction of adverse events is most effectively achieved through collaboration and coregulation with dentists, rather than through the threat of outside sanctions. The dental profession in every Member State has self-regulatory functions in promoting high quality and works with its respective government in a co-regulatory context to promote patient safety and quality.
5. The dental profession seeks to improve safety and quality in many ways. This includes: - Continuing professional development to keep skills up to date; - Establishing local study groups for dentists to learn from each others’ experiences; - Developing systems for non-blame, voluntary and anonymous reporting of adverse events or near misses; - Ensuring compliance with infection control and waste management laws. 6. Safe and high quality dental care throughout Europe is underpinned by high standards of professional conduct and ethics. Apart from encouraging dentists to comply with national ethicalcodes, CED members have agreed to a set of general ethical principles and have adopted a Code of Ethics for Dentists in the European Union (first adopted in 1965, last amended in 2007). In the Code of Ethics, European dentists confirmed their commitment to acting always in the best interests of the patients and to respecting their dignity, autonomy and choices, including through good Communication. 7. Ensuring patient safety in cases of patient cross-border mobility can be particularly challenging. The trend of dental tourism, where patients travel long distances for extensive but quick treatment, is where patient safety comes under considerable threat. Pre-treatment planning and post treatment care, which are essential parts of high-quality dental care, cannot easily be undertaken. Also, communication between patient and professional can be hampered due to language difficulties. Better information on the potential risks should be provided to patients in line with the provisions of the Directive on the application of patients’ rights in cross-border healthcare. Dental tourism should not be promoted.
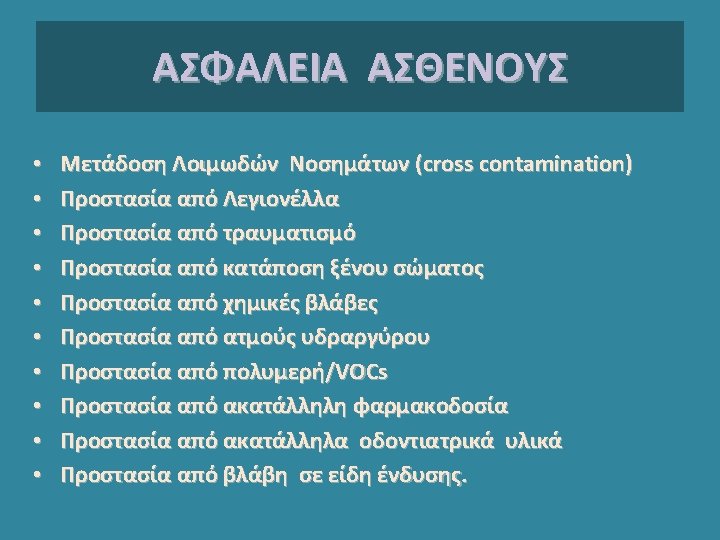

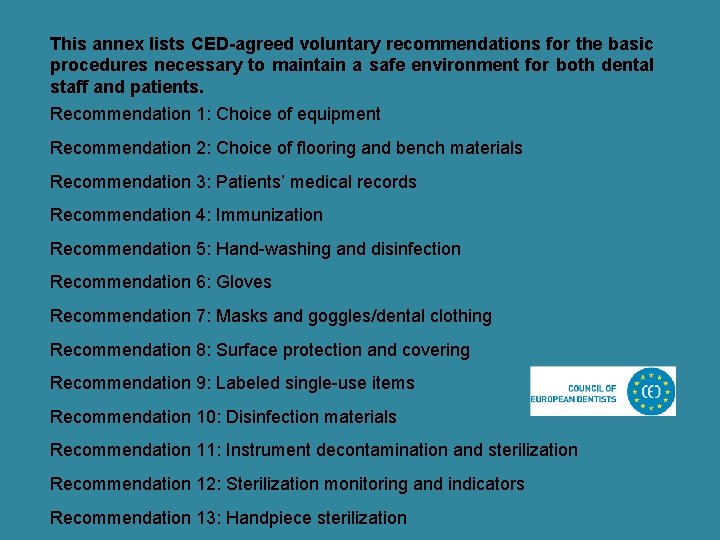
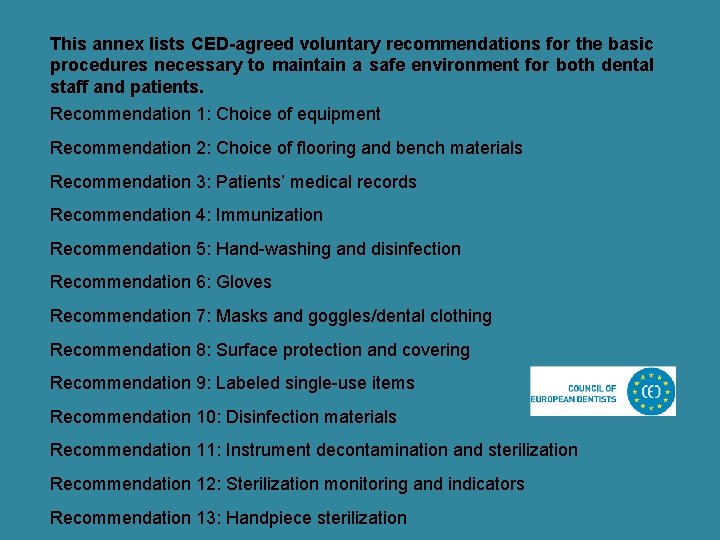
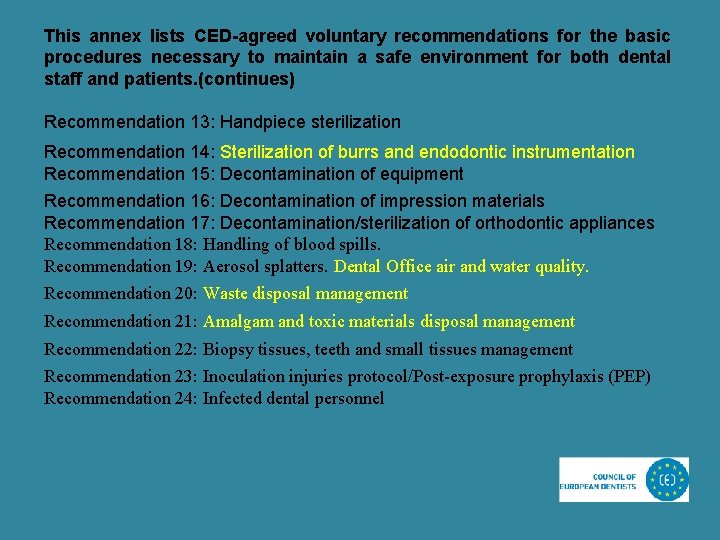
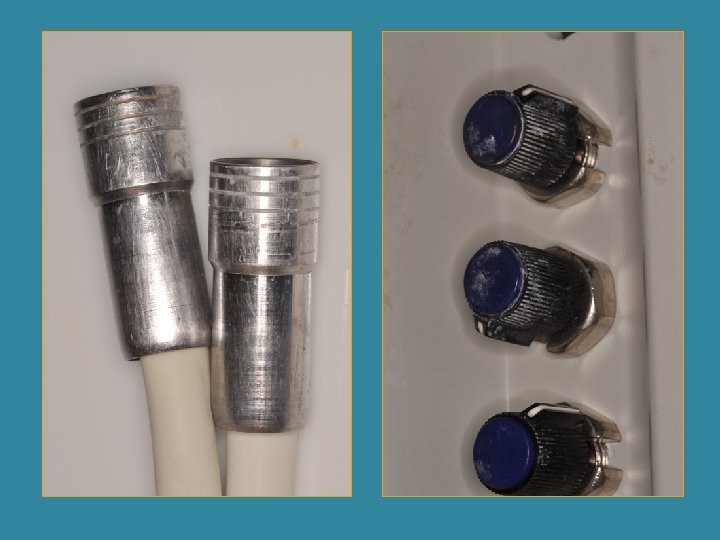
This annex lists CED-agreed voluntary recommendations for the basic procedures necessary to maintain a safe environment for both dental staff and patients. Recommendation 1: Choice of equipment Recommendation 2: Choice of flooring and bench materials Recommendation 3: Patients’ medical records Recommendation 4: Immunization Recommendation 5: Hand-washing and disinfection Recommendation 6: Gloves Recommendation 7: Masks and goggles/dental clothing Recommendation 8: Surface protection and covering Recommendation 9: Labeled single-use items Recommendation 10: Disinfection materials Recommendation 11: Instrument decontamination and sterilization Recommendation 12: Sterilization monitoring and indicators Recommendation 13: Handpiece sterilization
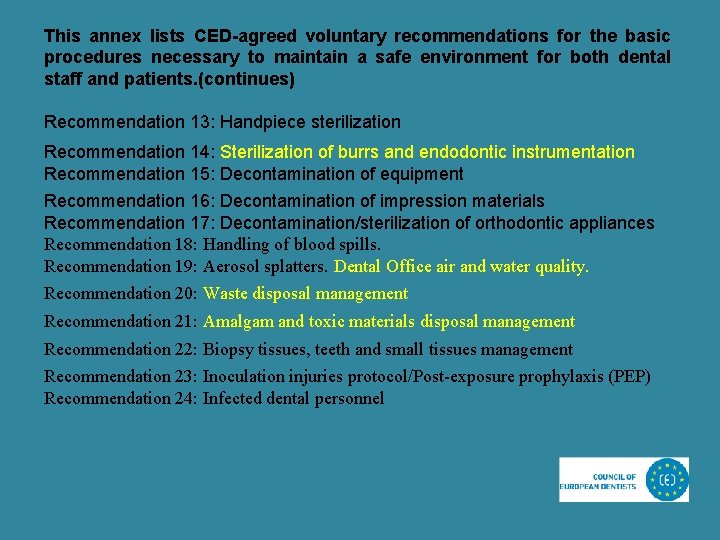
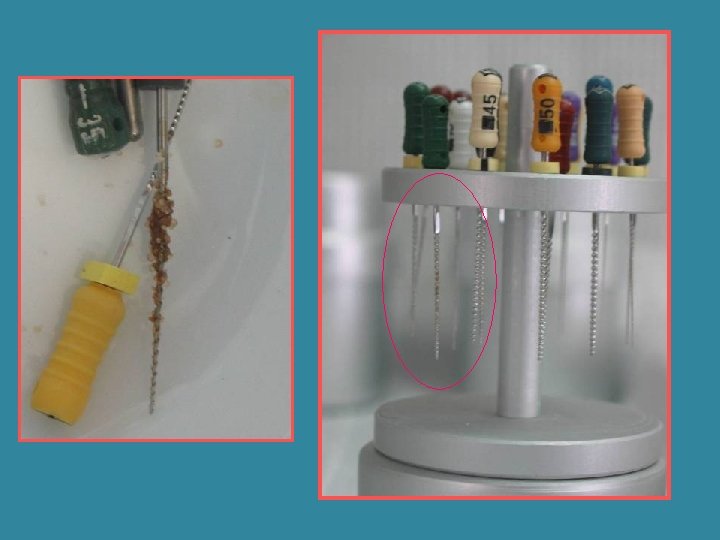
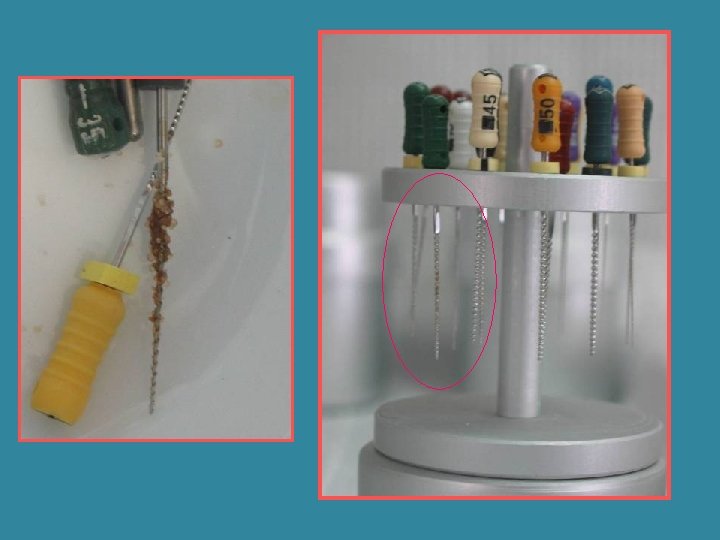
This annex lists CED-agreed voluntary recommendations for the basic procedures necessary to maintain a safe environment for both dental staff and patients. (continues) Recommendation 13: Handpiece sterilization Recommendation 14: Sterilization of burrs and endodontic instrumentation Recommendation 15: Decontamination of equipment Recommendation 16: Decontamination of impression materials Recommendation 17: Decontamination/sterilization of orthodontic appliances Recommendation 18: Handling of blood spills. Recommendation 19: Aerosol splatters. Dental Office air and water quality. Recommendation 20: Waste disposal management Recommendation 21: Amalgam and toxic materials disposal management Recommendation 22: Biopsy tissues, teeth and small tissues management Recommendation 23: Inoculation injuries protocol/Post-exposure prophylaxis (PEP) Recommendation 24: Infected dental personnel
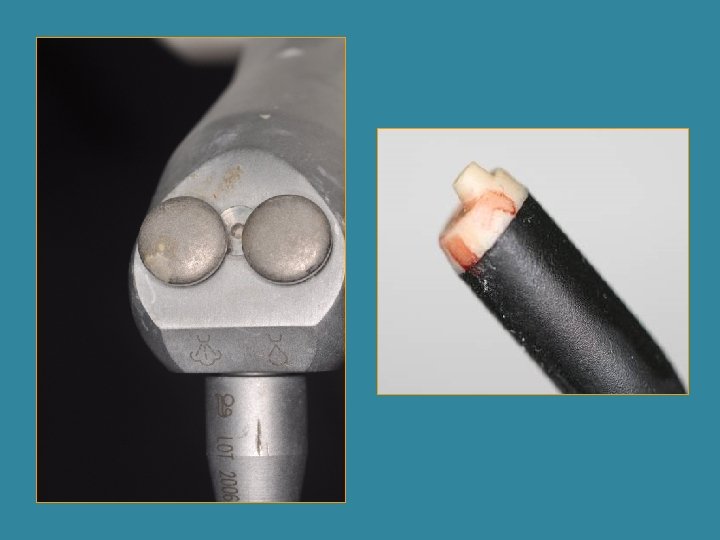


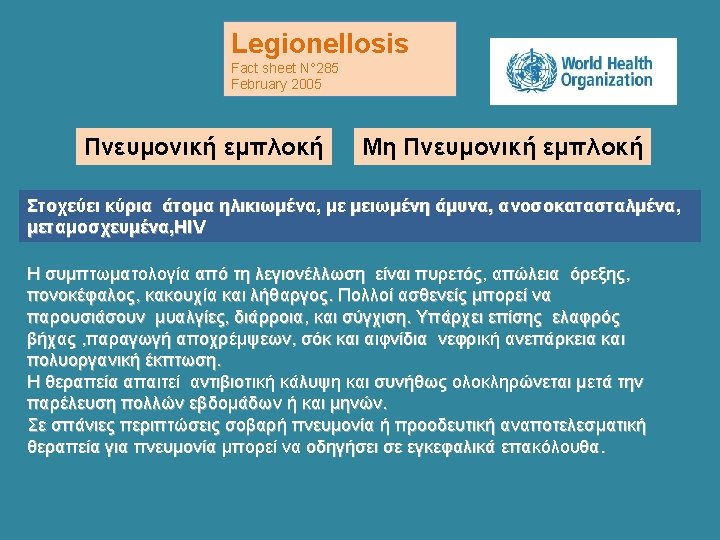
Legionella pneumofila
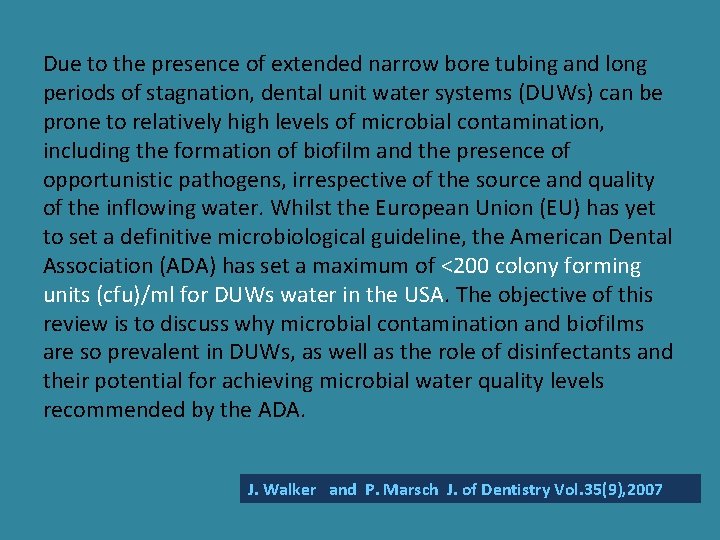
Due to the presence of extended narrow bore tubing and long periods of stagnation, dental unit water systems (DUWs) can be prone to relatively high levels of microbial contamination, including the formation of biofilm and the presence of opportunistic pathogens, irrespective of the source and quality of the inflowing water. Whilst the European Union (EU) has yet to set a definitive microbiological guideline, the American Dental Association (ADA) has set a maximum of <200 colony forming units (cfu)/ml for DUWs water in the USA. The objective of this review is to discuss why microbial contamination and biofilms are so prevalent in DUWs, as well as the role of disinfectants and their potential for achieving microbial water quality levels recommended by the ADA. J. Walker and P. Marsch J. of Dentistry Vol. 35(9), 2007
Legionella pneumophila contamination of a dental unit water line system in a dental teaching centre SY Ma'ayeh AS Al-Hiyasat MY Hindiyeh YS Khader Objective: This study aimed to evaluate the extent of Legionella pneumophila contamination in a dental unit water line (DUWL) at a Dental Teaching Centre in Jordan. Methods: Ten dental units were sampled from each teaching clinic, namely conservative dentistry, periodontology and prosthodontics. Samples were collected from the air/water syringe, high-speed hand piece and water cup filler. Sampling time was at the beginning of the working day (before the dental unit was used), after 2 min of flushing, and at midday. Results: Legionella pneumophila counts ranged between 0 and 8. 35 × 103 (CFU ml− 1). Legionella pneumophila was detected in 86. 7% of the dental units at the beginning of the working day, 40% after 2 min flushing and 53. 3% at midday. The highest L. pneumophila counts were found at the beginning of the working day which were reduced by flushing the waterlines. The conservative dentistry clinic had the highest contamination level followed by the periodontology and prosthodontics clinics (P < 0. 05). The rate of contamination can be ascribed to the dental procedures performed in the clinics, the degree of using the hand pieces, and water softening and heating. Conclusions: The difficulty of completely eliminating micro-organism contaminating water used for dental treatment and the resulting biofilm suggest that flushing of DUWL can be a first solution in reducing L. pneumophila counts, while the incorporation of a disinfection method is highly recommended. Water heating and softening should be considered in practicing dentistry as factors that may aid in L. pneumophila proliferation inside the DUWL.
The presence of Pseudomonas aeruginosa in the dental unit waterline systems of teaching clinics AS Al-Hiyasat, SY Ma'ayeh, MY Hindiyeh and YS Khader Objective: The objective of this study was to evaluate the extent of Pseudomonas aeruginosa contamination of Dental Unit Water (DUW) at a Dental Teaching Center in Jordan. Methods: Water samples were collected from 30 dental units, 10 from each of three teaching clinics, namely conservative dentistry, periodontology, and prosthodontics. Samples were collected from the outlet of the air/water syringe, high-speed handpiece and water cup filler, at the beginning of the working day (before use), after 2 min flushing, and at midday. Results: P. aeruginosa was detected in 86. 7% (26/30) of the dental units at the beginning of the working day, and in 73. 3% (22/30) after 2 min of flushing and at midday. Conservative dentistry units had the highest counts, followed by periodontology and prosthodontics (P < 0. 05). Overall, the highest counts (log 10 count CFU ml− 1) were at the beginning of the working day (1. 38 ± 1. 05), and the lowest counts after flushing for 2 min (1. 10 ± 1. 03), and higher numbers were seen again at midday (1. 15 ± 1. 04) (P < 0. 05). Conclusions: 86. 7% of the dental units were contaminated with P. aeruginosa, the conservative dentistry units had the highest amount of contamination. Flushing the DUW for 2 min significantly reduced the counts of P. aeruginosa
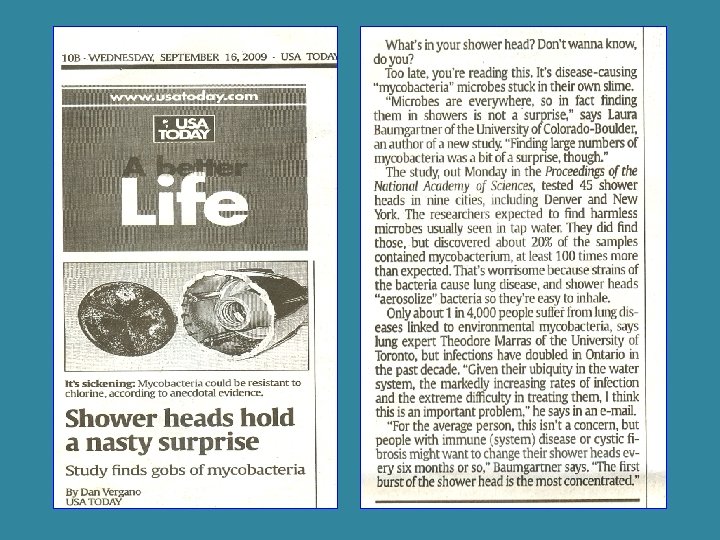
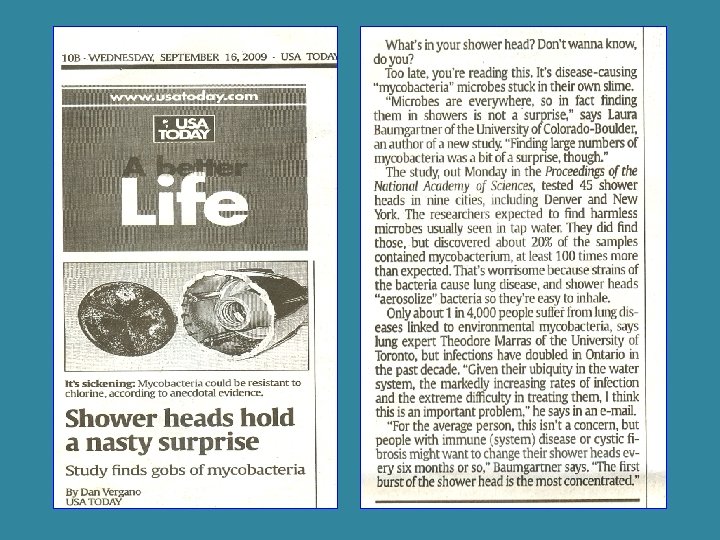
Appl Environ Microbiol. 2003 June; 69(6): 3412– 3420. PMCID: PMC 161485 doi: 10. 1128/AEM. 69. 6. 3412 -3420. 2003. Copyrigh Microbial Diversity of Biofilms in Dental Unit Water Systems Ruby Singh, 1 O. Colin Stine, 2 David L. Smith, 2 John K. Spitznagel, 3 Mohamed E. Labib, 4 and Henry N. Williams 1* Some organisms found in the DUWS may pose a health risk to some patients. Leptospira, the most common organism detected, can invade any susceptible mucosal membrane and cause leptospirosis. Sphingomonas and Legionella, two organisms found in the DUWL, are easily spread via aerosols. Sphingomonas sp. strains secrete viscous polysaccharides (24), which aid in their ability to adhere to and corrode surfaces of pipelines. Legionella species are known to cause respiratory infections (2). Both species have been found in hospital environments, including such devices as mechanical ventilators, catheters, and bronchofiberoscopes (11, 19). Their presence in DUWL is a concern, because studies have shown that aerosols generated from dental handpieces during treatment are sufficient to expose patients and dental personnel to the microorganisms in the DUWS (10).
The quality of water passing through the waterlines of the dental units is of primary concern to clinicians because both the patient and the office staff are exposed to the aerosols generated during the various clinical procedures. 1 The concern is related to both the chemical and particle contents of the water as well as the bacterial count in the waterline. 2– 4 For a number of years, it has been ascertained that water delivered from the dental units during routine dental procedures is highly contaminated by numerous species of pathogen and nonpathogen microorganisms, which enter the dental units by being retracted up from the oral cavity of patients undergoing dental treatment. 2 The biofilm, which is derived from bacteria in the incoming water and is intrinsically resistant to most biocides, is the primary reservoir for continued contamination of the system. 1 Biofilm forms a tenacious layer that is strongly adherent to the walls of the tubing and often contains different types of pathogenic bacteria. 3 In 1996, the American Dental Association established a goal for dental water quality and specified that it should not contain more than 200 colony forming units per milliliter (CFU/m. L). 2, 4 On the other hand, Lingr et al found that untreated dental unit waterlines may contain up to 9760 CFU/m. L. 5 Because of such significant levels of contamination, the use of intraoperative antimicrobial agents have been implemented either to be placed in the unit waterline or used topically after cavity preparation. 6 Numerous chemicals for use in disinfecting dental waterlines have been suggested. 7 Lingr et al 5 found that hydrogen peroxide– based dental unit waterline treatment reduced colonization from 9760 CFU/m. L to 200 CFU/m. L in one week. By four weeks, the count was reduced to 0 CFU/m. L. Meiller et al 8 found that the use of Listerine Antiseptic for 18 hours rendered biofilm samples free of recoverable bacteria. Other chemicals for disinfecting dental waterlines have been used, including sodium hypochlorite, glutaraldehyde, chlorhexidine, iodine, and Sterilox, which is superoxidized water. All these chemicals were found to be effective in reducing bacterial biofilm. 9– 11 Mc Fadden et al 6 found that the use of chlorhexidine or glutaraldehyde during the bonding procedure with All-Bond 2 increased its shear bond strength to dentin. Knight et al 7 found no significant difference in shear bond strengths of resin-based composite to tooth structure when rinsed with distilled water as compared with those rinsed with distilled water mixed with mouthwash. On the other hand, Taylor-Hardy et al 12 suggested that dental unit waterline biocides might adversely affect adhesion of resin to enamel. Because of these controversial findings, it is important for the orthodontists to know whether the bond strength will be affected by using water containing an antibacterial agent. The purpose of this study was to determine whether disinfecting the waterlines in the dental units with an iodine compound will affect the shear strength of orthodontic brackets bonded to enamel.
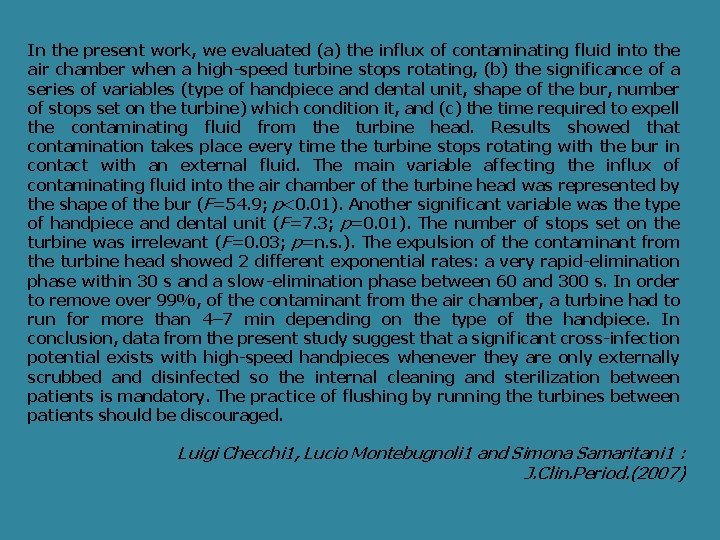
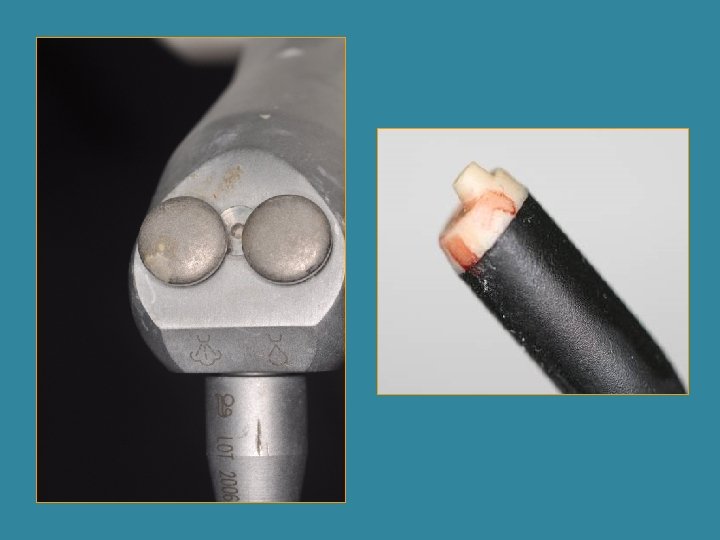
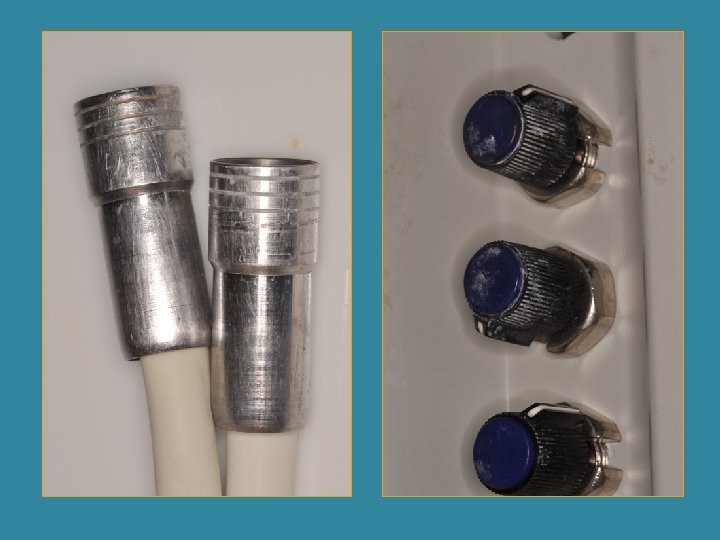
In the present work, we evaluated (a) the influx of contaminating fluid into the air chamber when a high-speed turbine stops rotating, (b) the significance of a series of variables (type of handpiece and dental unit, shape of the bur, number of stops set on the turbine) which condition it, and (c) the time required to expell the contaminating fluid from the turbine head. Results showed that contamination takes place every time the turbine stops rotating with the bur in contact with an external fluid. The main variable affecting the influx of contaminating fluid into the air chamber of the turbine head was represented by the shape of the bur (F=54. 9; p<0. 01). Another significant variable was the type of handpiece and dental unit (F=7. 3; p=0. 01). The number of stops set on the turbine was irrelevant (F=0. 03; p=n. s. ). The expulsion of the contaminant from the turbine head showed 2 different exponential rates: a very rapid-elimination phase within 30 s and a slow-elimination phase between 60 and 300 s. In order to remove over 99%, of the contaminant from the air chamber, a turbine had to run for more than 4– 7 min depending on the type of the handpiece. In conclusion, data from the present study suggest that a significant cross-infection potential exists with high-speed handpieces whenever they are only externally scrubbed and disinfected so the internal cleaning and sterilization between patients is mandatory. The practice of flushing by running the turbines between patients should be discouraged. Luigi Checchi 1, Lucio Montebugnoli 1 and Simona Samaritani 1 : J. Clin. Period. (2007)
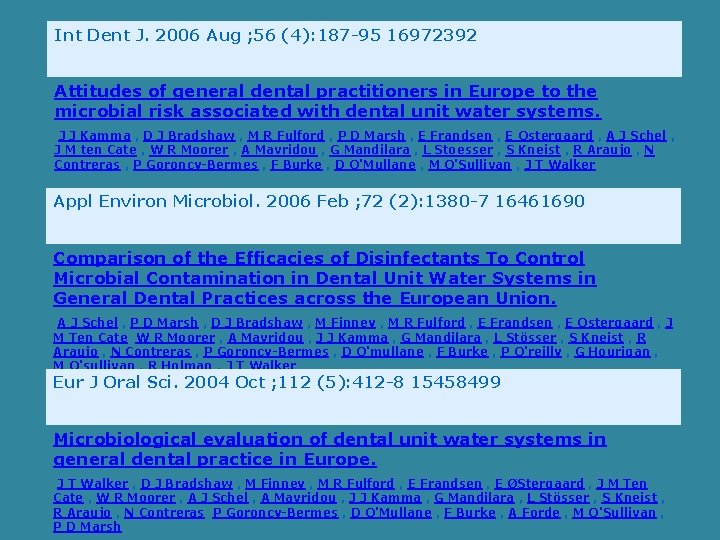
Int Dent J. 2006 Aug ; 56 (4): 187 -95 16972392 Attitudes of general dental practitioners in Europe to the microbial risk associated with dental unit water systems. J J Kamma , D J Bradshaw , M R Fulford , P D Marsh , E Frandsen , E Ostergaard , A J Schel , J M ten Cate , W R Moorer , A Mavridou , G Mandilara , L Stoesser , S Kneist , R Araujo , N Contreras , P Goroncy-Bermes , F Burke , D O'Mullane , M O'Sullivan , J T Walker Appl Environ Microbiol. 2006 Feb ; 72 (2): 1380 -7 16461690 Comparison of the Efficacies of Disinfectants To Control Microbial Contamination in Dental Unit Water Systems in General Dental Practices across the European Union. A J Schel , P D Marsh , D J Bradshaw , M Finney , M R Fulford , E Frandsen , E Ostergaard , J M Ten Cate W R Moorer , A Mavridou , J J Kamma , G Mandilara , L Stösser , S Kneist , R Araujo , N Contreras , P Goroncy-Bermes , D O'mullane , F Burke , P O'reilly , G Hourigan , M O'sullivan , R Holman , J T Walker Eur J Oral Sci. 2004 Oct ; 112 (5): 412 -8 15458499 Microbiological evaluation of dental unit water systems in general dental practice in Europe. J T Walker , D J Bradshaw , M Finney , M R Fulford , E Frandsen , E ØStergaard , J M Ten Cate , W R Moorer , A J Schel , A Mavridou , J J Kamma , G Mandilara , L Stösser , S Kneist , R Araujo , N Contreras P Goroncy-Bermes , D O'Mullane , F Burke , A Forde , M O'Sullivan , P D Marsh
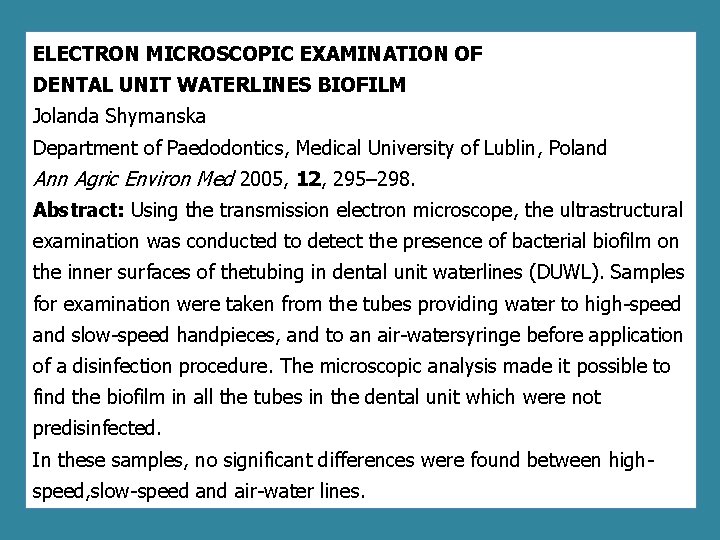
ELECTRON MICROSCOPIC EXAMINATION OF DENTAL UNIT WATERLINES BIOFILM Jolanda Shymanska Department of Paedodontics, Medical University of Lublin, Poland Ann Agric Environ Med 2005, 12, 295– 298. Abstract: Using the transmission electron microscope, the ultrastructural examination was conducted to detect the presence of bacterial biofilm on the inner surfaces of thetubing in dental unit waterlines (DUWL). Samples for examination were taken from the tubes providing water to high-speed and slow-speed handpieces, and to an air-watersyringe before application of a disinfection procedure. The microscopic analysis made it possible to find the biofilm in all the tubes in the dental unit which were not predisinfected. In these samples, no significant differences were found between highspeed, slow-speed and air-water lines.
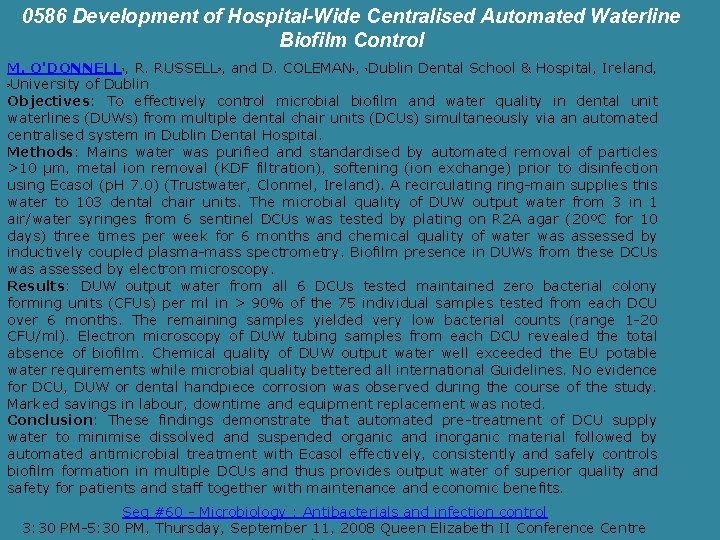
0586 Development of Hospital-Wide Centralised Automated Waterline Biofilm Control M. O'DONNELL , R. RUSSELL , and D. COLEMAN , Dublin Dental School & Hospital, Ireland, University of Dublin Objectives: To effectively control microbial biofilm and water quality in dental unit waterlines (DUWs) from multiple dental chair units (DCUs) simultaneously via an automated centralised system in Dublin Dental Hospital. Methods: Mains water was purified and standardised by automated removal of particles >10 µm, metal ion removal (KDF filtration), softening (ion exchange) prior to disinfection using Ecasol (p. H 7. 0) (Trustwater, Clonmel, Ireland). A recirculating ring-main supplies this water to 103 dental chair units. The microbial quality of DUW output water from 3 in 1 air/water syringes from 6 sentinel DCUs was tested by plating on R 2 A agar (20ºC for 10 days) three times per week for 6 months and chemical quality of water was assessed by inductively coupled plasma-mass spectrometry. Biofilm presence in DUWs from these DCUs was assessed by electron microscopy. Results: DUW output water from all 6 DCUs tested maintained zero bacterial colony forming units (CFUs) per ml in > 90% of the 75 individual samples tested from each DCU over 6 months. The remaining samples yielded very low bacterial counts (range 1 -20 CFU/ml). Electron microscopy of DUW tubing samples from each DCU revealed the total absence of biofilm. Chemical quality of DUW output water well exceeded the EU potable water requirements while microbial quality bettered all international Guidelines. No evidence for DCU, DUW or dental handpiece corrosion was observed during the course of the study. Marked savings in labour, downtime and equipment replacement was noted. Conclusion: These findings demonstrate that automated pre-treatment of DCU supply water to minimise dissolved and suspended organic and inorganic material followed by automated antimicrobial treatment with Ecasol effectively, consistently and safely controls biofilm formation in multiple DCUs and thus provides output water of superior quality and safety for patients and staff together with maintenance and economic benefits. 1 2 1 1 2 Seq #60 - Microbiology : Antibacterials and infection control 3: 30 PM-5: 30 PM, Thursday, September 11, 2008 Queen Elizabeth II Conference Centre
Sacchetti R, Baldissarri A, De Luca G, Lucca P, Stampi S, Zanetti F: Microbial contamination in dental unit waterlines: comparison between Er: YAG laser and turbine lines. Ann Agric Environ Med 2006, 13, 275– 279. Abstract: The investigation was carried out by evaluating the microbiological characteristics of the water before and after treatment with Er: YAG laser and turbine. The study was carried out in 2 dental surgeries. In both cases the laser and dental units were served by two independent circuits, fed by the same potable tap water. Samples were taken from the water supplying and the water leaving the turbine and laser before and after treatment on the same patient. Total heterotrophic plate count was measured at 36ºC and at 22ºC, and the presence of Staphylococcus species and non-fermenting Gram negative bacteria was investigated. Bacterial contamination was found within the circuit, especially in the laser device. Pseudomonas aeruginosa was detected in only 1 sample of supply water, in 11. 1% and in 19. 4% of the samples from the turbine and the laser respectively. No evidence of Staphylococcus aureus was found. The contamination of supply water was low, whereas that of the water leaving the handpieces of the 2 devices was high, especially in the laser. Attention should be paid to the control of the water leaving laser devices, given the increasingly wide use of such instruments indental treatment exposed to risk of infection.
Prevention Preventing Legionella pneumophila from living in all water supplies would be the first method of preventing the spread of this bacteria. This, however, is an extremely difficult task. The reason why it is so difficult is because the bacteria live inside amoebae as well as inside biofilms. Hence it is difficult to kill the bacteria because of their increased resistance to many toxic substances while inside the amoebae. Recent methods for destroying the bacteria, such as passing UV light as well as hot water through pipes, has been found to be very successful but expensive. It especially becomes expensive when treating large amounts of water. Scientists are also trying to discover biocides that are toxic to the bacteria, but safe for humans. This research, however, is in its early stages and so far no biocides have been uncovered. Finally there has been talk of developing a vaccine, but that too is in its early stages.

Journal of the American Dental Association, Vol 126, Issue 5, 603 -608 Copyright © 1995 by American Dental Association Detecting Legionella pneumophila in water systems: a comparison of various dental units SJ Challacombe and LL Fernandes Department of Oral Medicine and Pathology, United Medical School, University of London. The authors sampled 194 dental units over a 44 -month period to detect the presence of Legionella pneumophila. They found L. pneumophila, usually in very low numbers, in 25 percent of the units over this time. However, higher counts were collected from 4 percent of the units, primarily from one model. The authors document colony counts collected from nine different models and those collected from air/water syringes vs. high-speed outlets, and they describe the effectiveness of disinfection.
It will be useful to summarise what the general dental practitioner needs to do to reduce the problem in his dental unit. According to BDA recommendations, the following measures should be implemented: § Flushing of the water lines for 2 minutes every morning before treating the first patient. § Flushing of the water lines for 30 seconds between each two patients. § The use of independent water system. § The use of disinfectants such as H 2 O 2 and Na. Cl. O. § Avoidance the use of warm water in the DUWLs as the water should be kept below 20° C. § Draining of the DUWLs at the end of each day. § Making sure that the anti-retraction valve in the handpiece is functional by regular maintenance.