Scottish Patient Safety Programme Paediatric Update Jane Murkin








- Slides: 11

Scottish Patient Safety Programme – Paediatric Update Jane Murkin, National Co-ordinator, Scottish Patient Safety Programme Julie Adams, National Facilitator, Paediatrics National Delivery Plan Implementation Group – 10 th March 2010

Our vision – Scotland leading the way in Patient Safety • Scotland at the forefront - a whole healthcare system approach • A strategic development priority for NHS Scotland • An explicit and tested approach to improving patient safety • Build on foundations laid through audit, clinical effectiveness and clinical governance • Alignment with wider NHS QIS Patient Safety work
Background • • • SPSA launched by CMO March 2007 SPSP first programme of work Strategic priority for all NHS boards Improvement programme – process / outcome Five work streams Designated Board PM and Exec Lead LS 1 Jan 2008, LS 6 May 2010 National Facilitators appointed – Sept 2008 Board trajectories
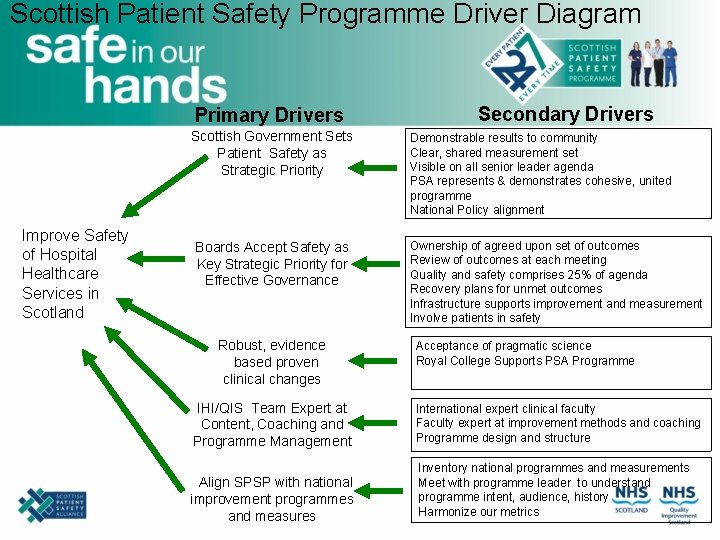
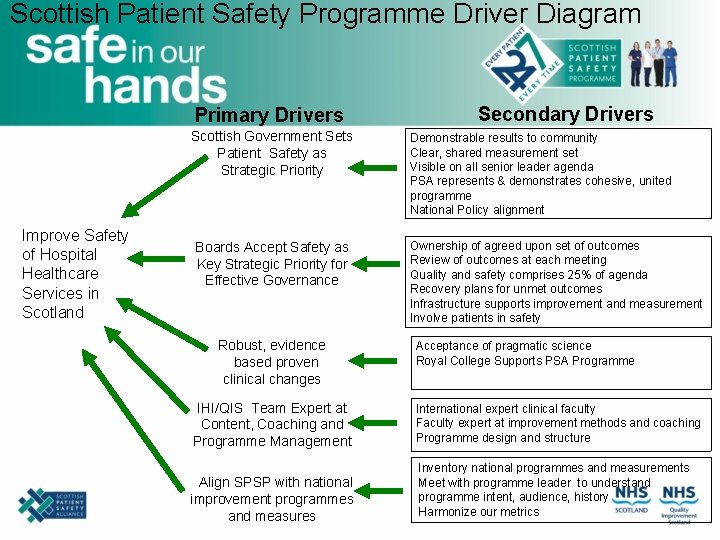
Scottish Patient Safety Programme Driver Diagram Primary Drivers Scottish Government Sets Patient Safety as Strategic Priority Improve Safety of Hospital Healthcare Services in Scotland Boards Accept Safety as Key Strategic Priority for Effective Governance Robust, evidence based proven clinical changes Secondary Drivers Demonstrable results to community Clear, shared measurement set Visible on all senior leader agenda PSA represents & demonstrates cohesive, united programme National Policy alignment Ownership of agreed upon set of outcomes Review of outcomes at each meeting Quality and safety comprises 25% of agenda Recovery plans for unmet outcomes Infrastructure supports improvement and measurement Involve patients in safety Acceptance of pragmatic science Royal College Supports PSA Programme IHI/QIS Team Expert at Content, Coaching and Programme Management International expert clinical faculty Faculty expert at improvement methods and coaching Programme design and structure Align SPSP with national improvement programmes and measures Inventory national programmes and measurements Meet with programme leader to understand programme intent, audience, history Harmonize our metrics

Outcome Aims: • 15% reduction in mortality • 30% reduction in adverse events • • • Reduce healthcare associated infections Reduce adverse surgical incidents Reduce adverse drug events Improve critical care outcomes Improve the organisational and leadership culture on safety • Data for improvement
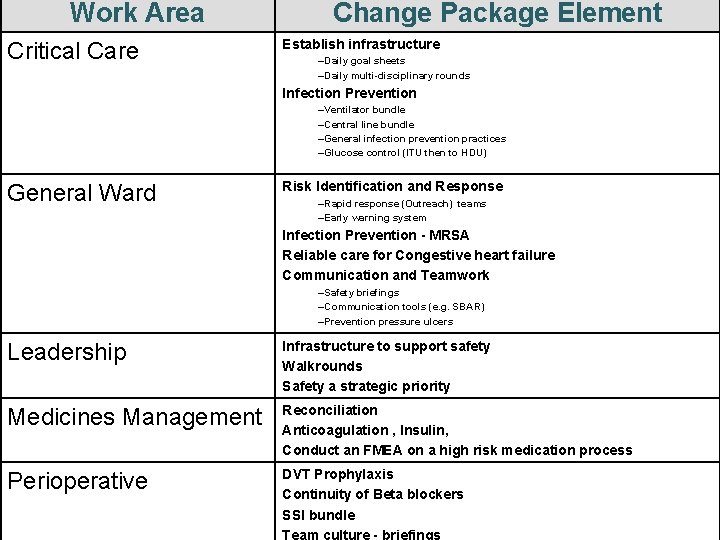
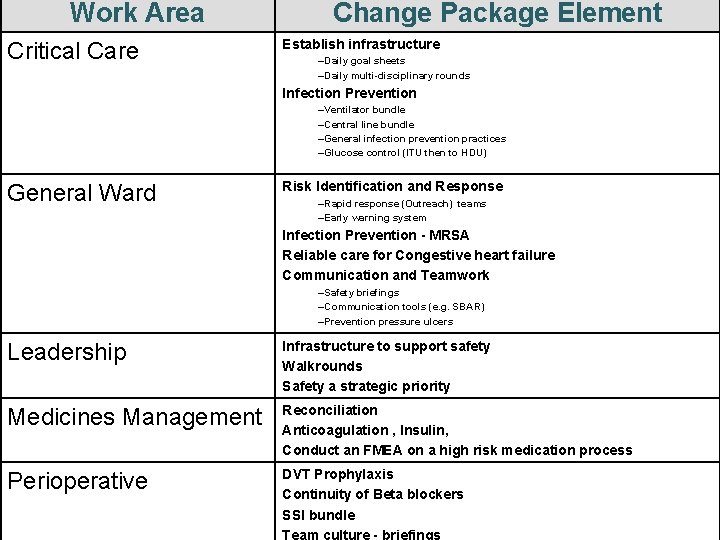
Work Area Critical Care Change Package Element Establish infrastructure –Daily goal sheets –Daily multi-disciplinary rounds Infection Prevention Key objectives General Ward –Ventilator bundle –Central line bundle –General infection prevention practices –Glucose control (ITU then to HDU) Risk Identification and Response –Rapid response (Outreach) teams –Early warning system Infection Prevention - MRSA Reliable care for Congestive heart failure Communication and Teamwork –Safety briefings –Communication tools (e. g. SBAR) –Prevention pressure ulcers Leadership Infrastructure to support safety Walkrounds Safety a strategic priority Medicines Management Reconciliation Anticoagulation , Insulin, Conduct an FMEA on a high risk medication process Perioperative DVT Prophylaxis Continuity of Beta blockers SSI bundle Team culture - briefings

Paediatric Programme • Steering Group established August 2009. • National Facilitator appointed November 2009. • National Event November 2009 – provide access to expert learning: – Cincinnati Children’s Hospital; – Great Ormond Street Hospital.

Develop paediatric aims, goals and measures • Ensure aims are ‘best in class’ • Paediatric evidence-base • Relevance to improving the safety of paediatric hospital healthcare in Scotland; • Same workstream infrastructure as SPSP. • Additional paediatric aims – child protection.

Next Steps…… • Confirm aims, goals and measures: – Steering Group meeting 30 th April 2010. • Launch event June 2010: – publicise the programme; – opportunity for specific paediatric training, i. e. paediatric trigger tool; – capacity building within paediatric community. • Develop strong patient links. • Establish infrastructure to deliver safe and reliable paediatric care.

