Patient Safety Positioning Patient Safety Patients at risk
- Slides: 19
Patient Safety & Positioning
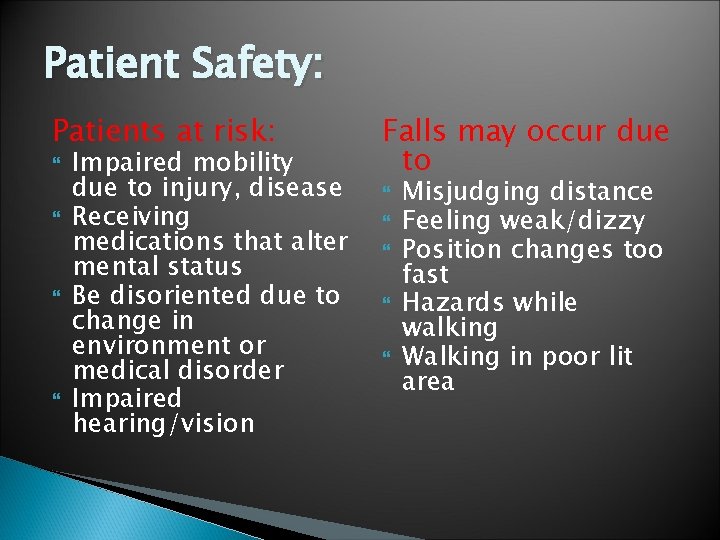
Patient Safety: Patients at risk: Impaired mobility due to injury, disease Receiving medications that alter mental status Be disoriented due to change in environment or medical disorder Impaired hearing/vision Falls may occur due to Misjudging distance Feeling weak/dizzy Position changes too fast Hazards while walking Walking in poor lit area
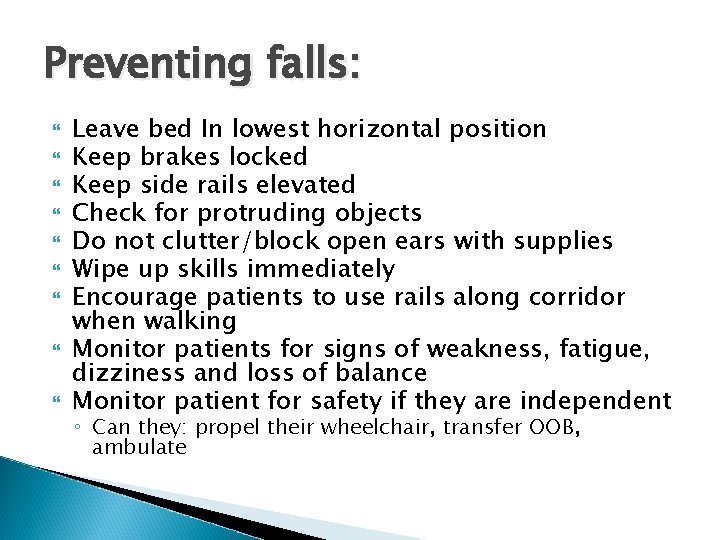
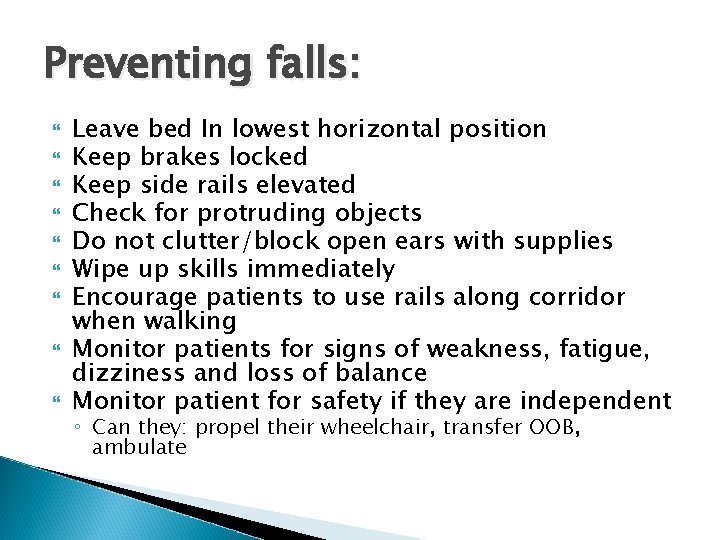
Preventing falls: Leave bed In lowest horizontal position Keep brakes locked Keep side rails elevated Check for protruding objects Do not clutter/block open ears with supplies Wipe up skills immediately Encourage patients to use rails along corridor when walking Monitor patients for signs of weakness, fatigue, dizziness and loss of balance Monitor patient for safety if they are independent ◦ Can they: propel their wheelchair, transfer OOB, ambulate
Physical Restraints Research show restraints do NOT necessarily reduce falls or prevent injuries – it may actually cause serious injuries and death
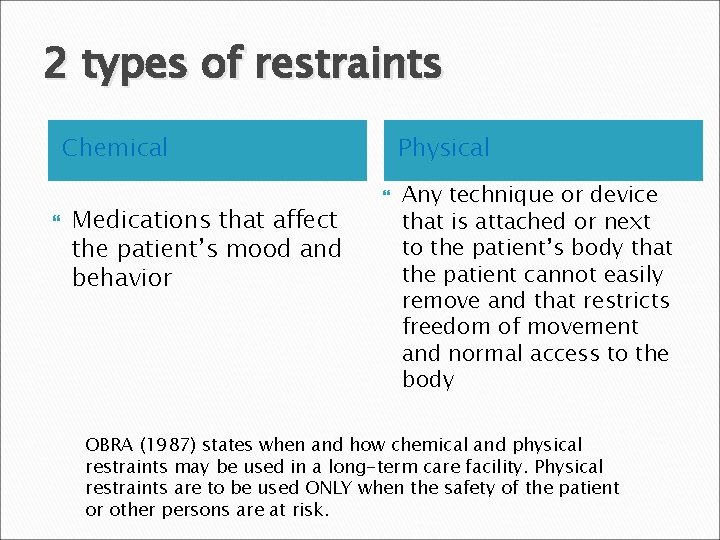
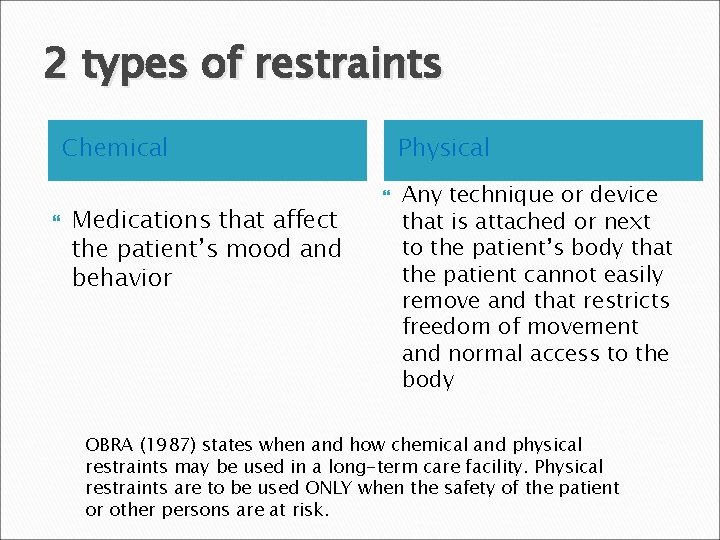
2 types of restraints Chemical Medications that affect the patient’s mood and behavior Physical Any technique or device that is attached or next to the patient’s body that the patient cannot easily remove and that restricts freedom of movement and normal access to the body OBRA (1987) states when and how chemical and physical restraints may be used in a long-term care facility. Physical restraints are to be used ONLY when the safety of the patient or other persons are at risk.
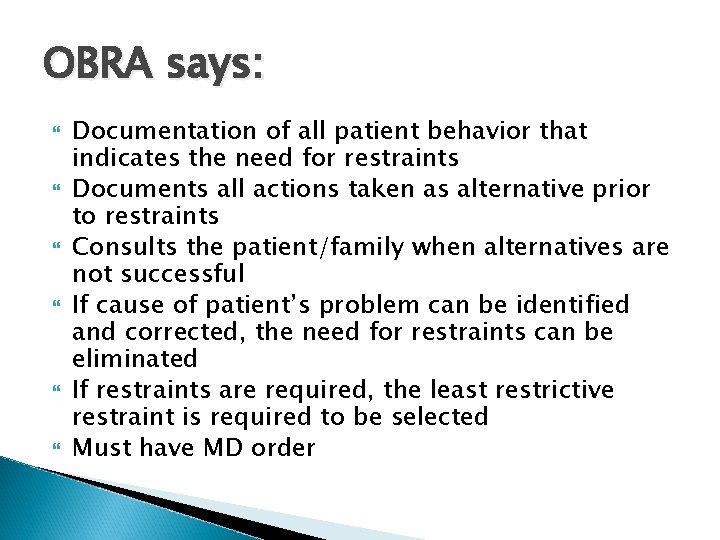
OBRA says: Documentation of all patient behavior that indicates the need for restraints Documents all actions taken as alternative prior to restraints Consults the patient/family when alternatives are not successful If cause of patient’s problem can be identified and corrected, the need for restraints can be eliminated If restraints are required, the least restrictive restraint is required to be selected Must have MD order
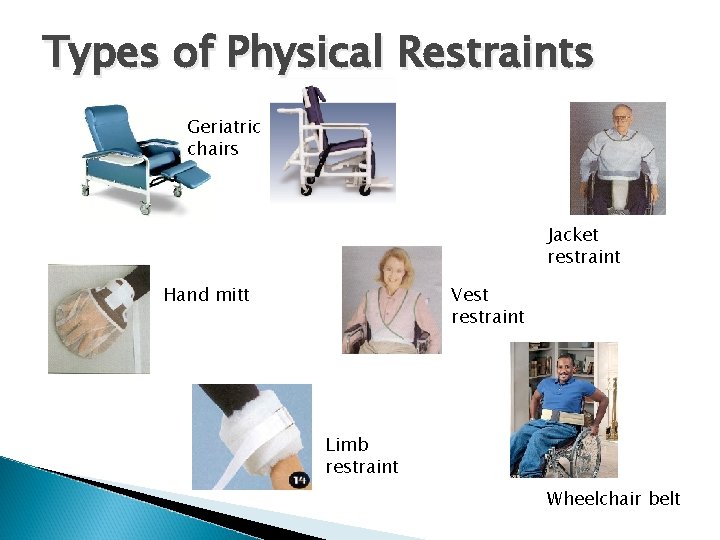
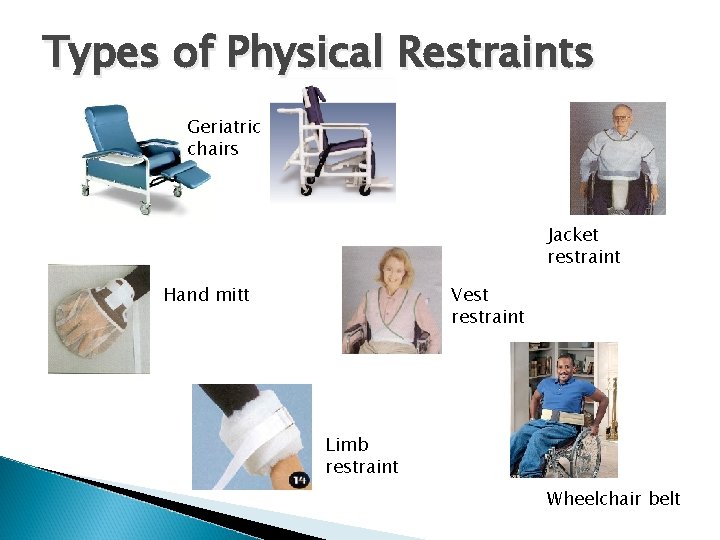
Types of Physical Restraints Geriatric chairs Jacket restraint Hand mitt Vest restraint Limb restraint Wheelchair belt
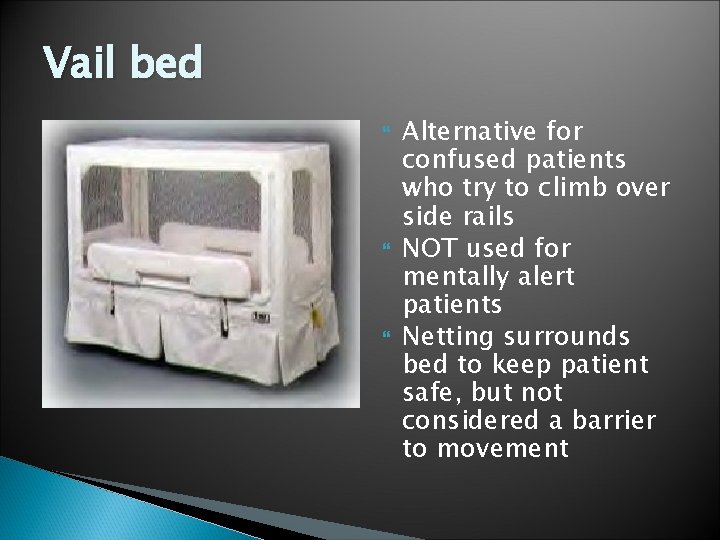
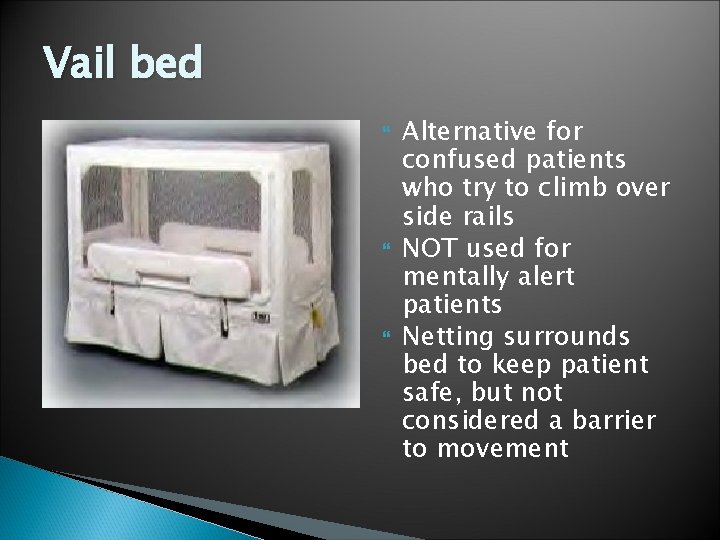
Vail bed Alternative for confused patients who try to climb over side rails NOT used for mentally alert patients Netting surrounds bed to keep patient safe, but not considered a barrier to movement
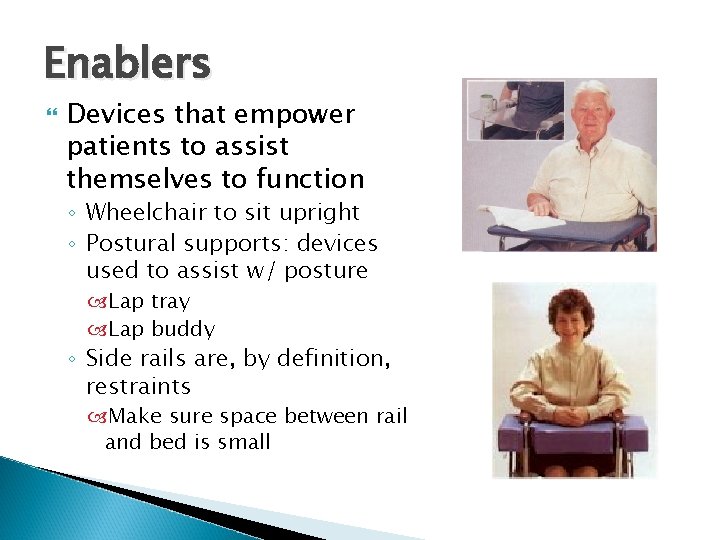
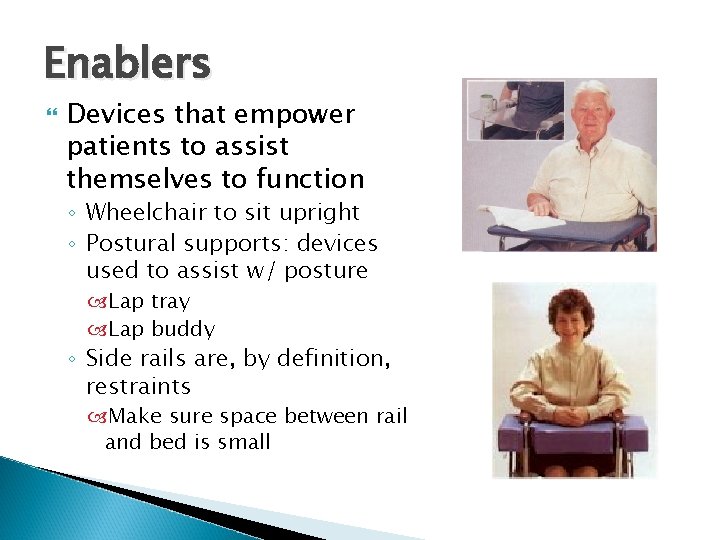
Enablers Devices that empower patients to assist themselves to function ◦ Wheelchair to sit upright ◦ Postural supports: devices used to assist w/ posture Lap tray Lap buddy ◦ Side rails are, by definition, restraints Make sure space between rail and bed is small
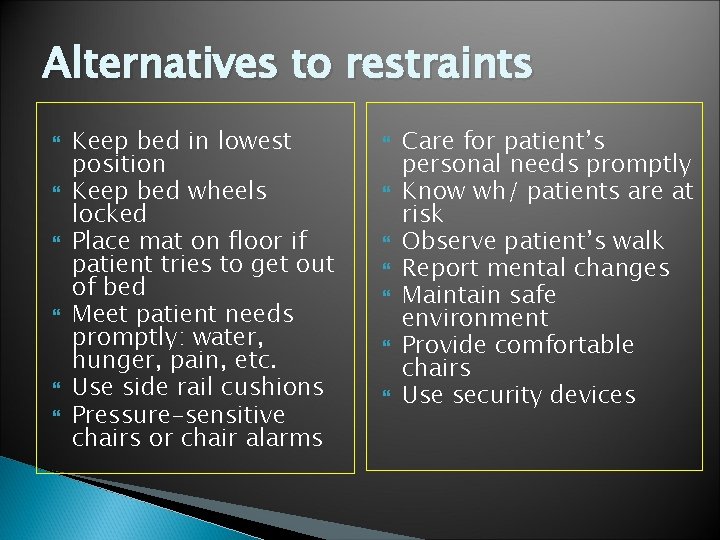
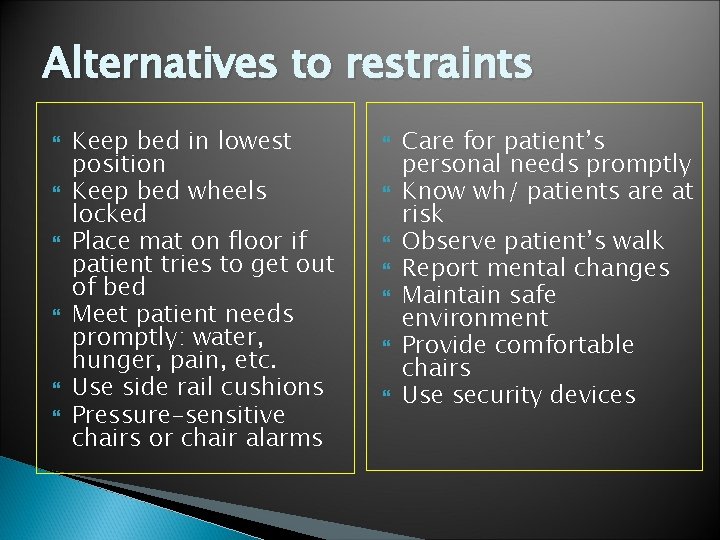
Alternatives to restraints Keep bed in lowest position Keep bed wheels locked Place mat on floor if patient tries to get out of bed Meet patient needs promptly: water, hunger, pain, etc. Use side rail cushions Pressure-sensitive chairs or chair alarms Care for patient’s personal needs promptly Know wh/ patients are at risk Observe patient’s walk Report mental changes Maintain safe environment Provide comfortable chairs Use security devices
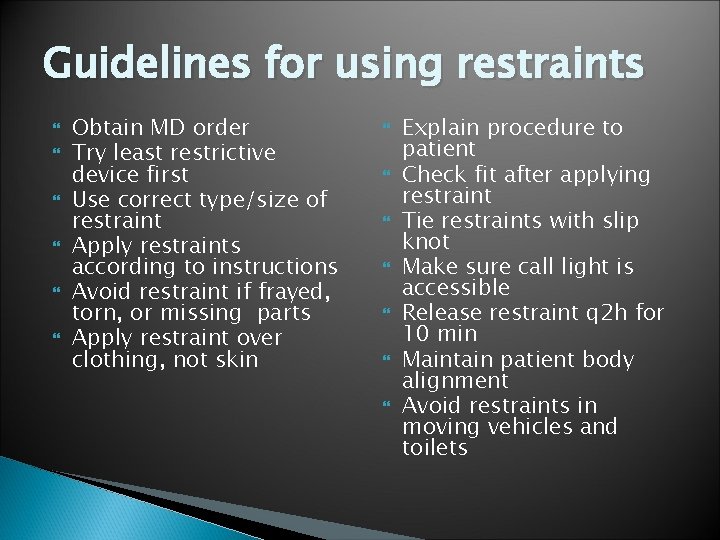
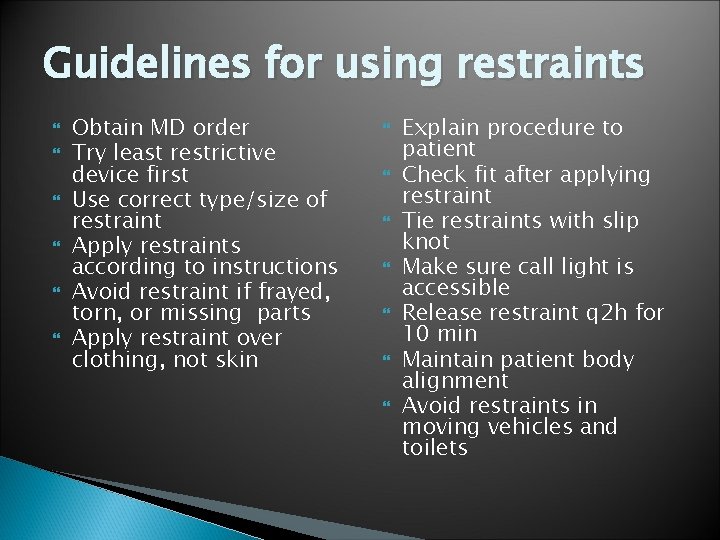
Guidelines for using restraints Obtain MD order Try least restrictive device first Use correct type/size of restraint Apply restraints according to instructions Avoid restraint if frayed, torn, or missing parts Apply restraint over clothing, not skin Explain procedure to patient Check fit after applying restraint Tie restraints with slip knot Make sure call light is accessible Release restraint q 2 h for 10 min Maintain patient body alignment Avoid restraints in moving vehicles and toilets
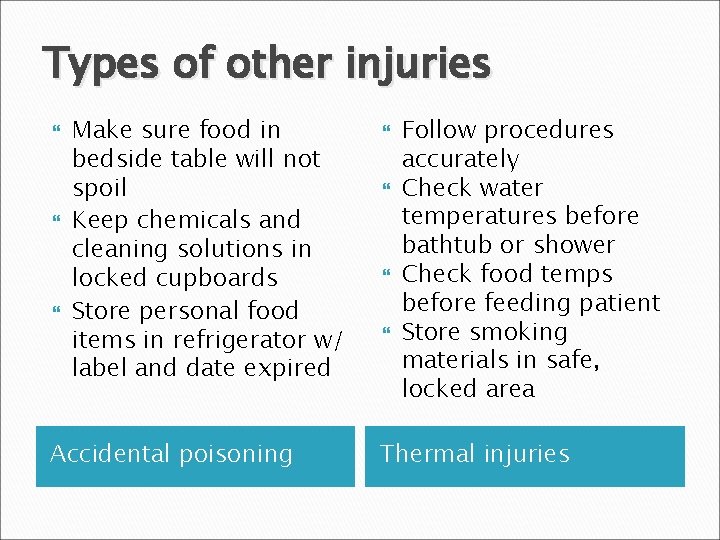
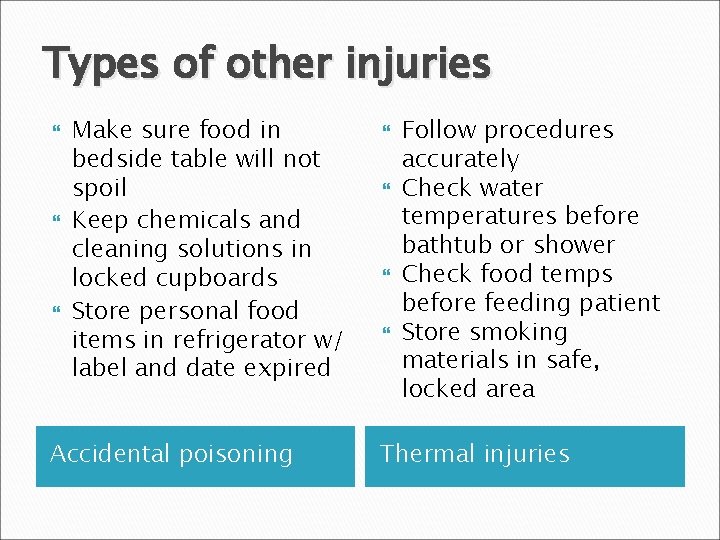
Types of other injuries Make sure food in bedside table will not spoil Keep chemicals and cleaning solutions in locked cupboards Store personal food items in refrigerator w/ label and date expired Accidental poisoning Follow procedures accurately Check water temperatures before bathtub or shower Check food temps before feeding patient Store smoking materials in safe, locked area Thermal injuries
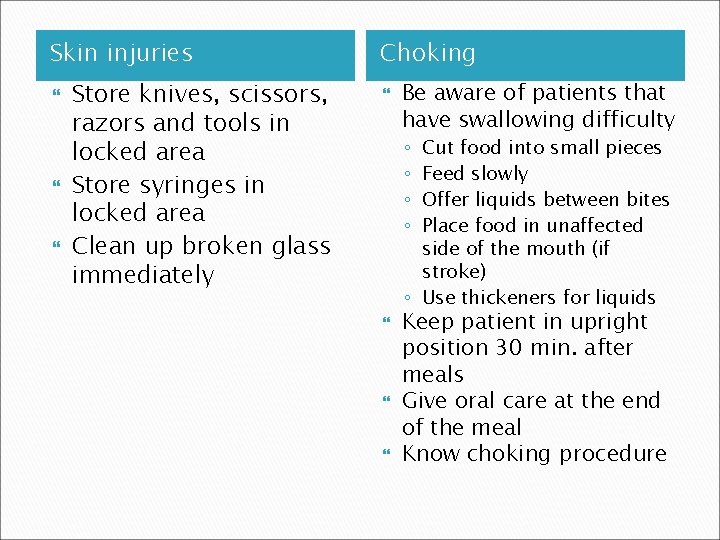
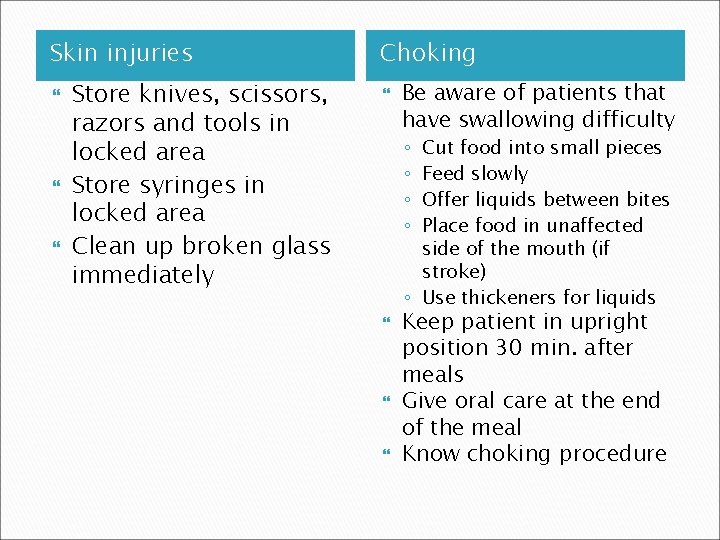
Skin injuries Store knives, scissors, razors and tools in locked area Store syringes in locked area Clean up broken glass immediately Choking Be aware of patients that have swallowing difficulty Cut food into small pieces Feed slowly Offer liquids between bites Place food in unaffected side of the mouth (if stroke) ◦ Use thickeners for liquids ◦ ◦ Keep patient in upright position 30 min. after meals Give oral care at the end of the meal Know choking procedure
Positioning Body alignment: ◦ Maintaining a person in a position in which the body can properly function
Complications Occurs when body alignment is not maintained or when the patient’s position is not changed often enough ◦ Pressure ulcer (bedsores) result when unrelieved pressure on a bony prominence interferes with blood flow to the area ◦ Contractures occurs when a joint is allowed to remain in the same position for too long
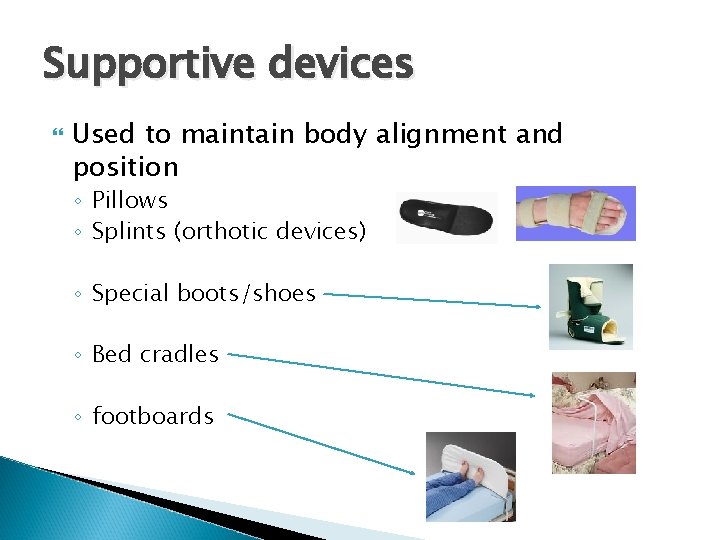
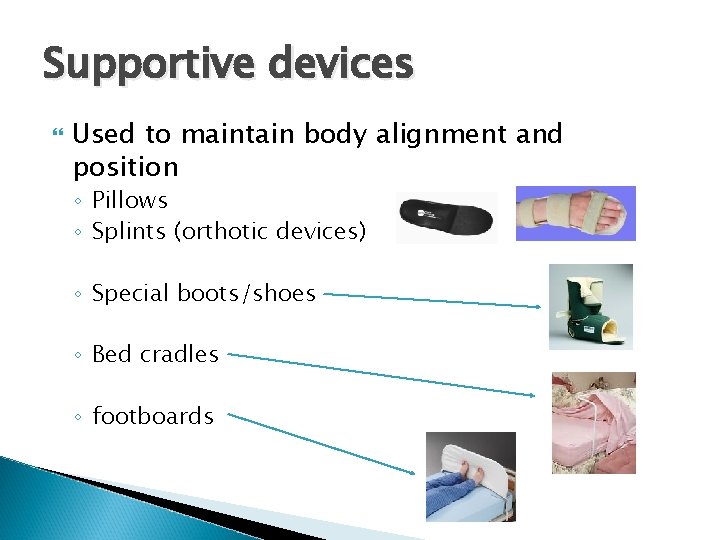
Supportive devices Used to maintain body alignment and position ◦ Pillows ◦ Splints (orthotic devices) ◦ Special boots/shoes ◦ Bed cradles ◦ footboards
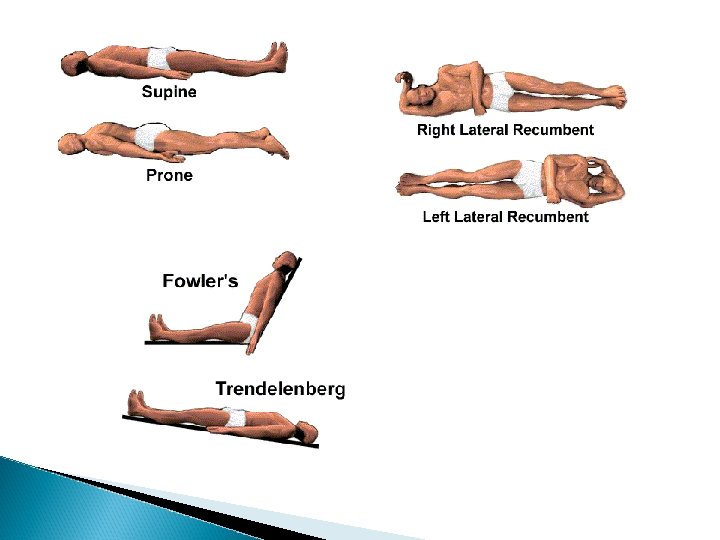
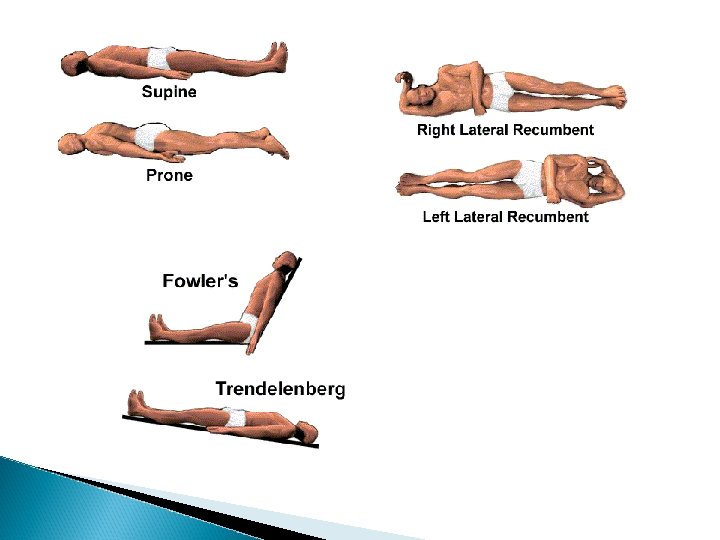
Positioning Prone – on the abdomen Supine – on the back Lateral – on either side Sims’s – left lateral (slight variation) Fowlers – upright; variation include high fowlers (90°) and semi-fowlers (45°)
Moving/Lifting Major responsibility of the CNA Use turning sheet/draw sheet to assist in lifting and make moving easier ◦ Sheet must extend from above the shoulders to below the hip Remember body mechanics rules
 Type of position
Type of position Market risk credit risk operational risk
Market risk credit risk operational risk Horizontal recumbent position
Horizontal recumbent position Ventral decubitus position
Ventral decubitus position Dorsal recumbent position
Dorsal recumbent position 13 malaysian safety goals
13 malaysian safety goals Food safety for immunocompromised patients
Food safety for immunocompromised patients Patient 2 patient
Patient 2 patient Draw rmmm plan
Draw rmmm plan Avoidance risk
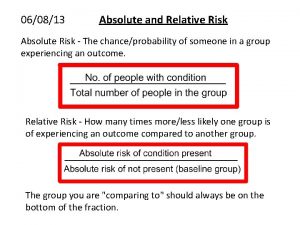
Avoidance risk How to calculate relative risk
How to calculate relative risk Residual risk and secondary risk pmp
Residual risk and secondary risk pmp Inherent risk vs control risk
Inherent risk vs control risk Absolute risk vs relative risk
Absolute risk vs relative risk Thinking algebraically stock market game answer key
Thinking algebraically stock market game answer key Classification of risk
Classification of risk Risk financing transfer adalah
Risk financing transfer adalah The biggest risk is not taking any risks
The biggest risk is not taking any risks Fiduciary investment risk management association
Fiduciary investment risk management association Business risk audit
Business risk audit