Respiratory Failure Zhang Xiaoming Dept pathophysiology 1 3


- Slides: 73
Respiratory Failure Zhang Xiao-ming Dept. pathophysiology 1

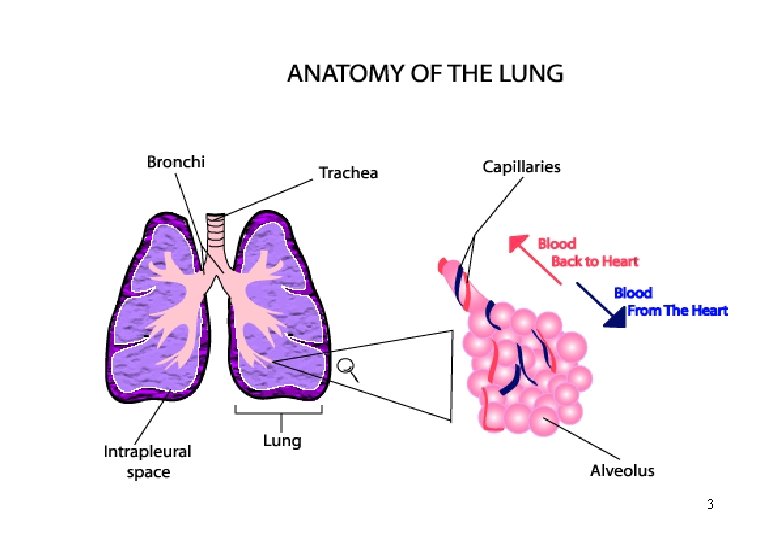
3
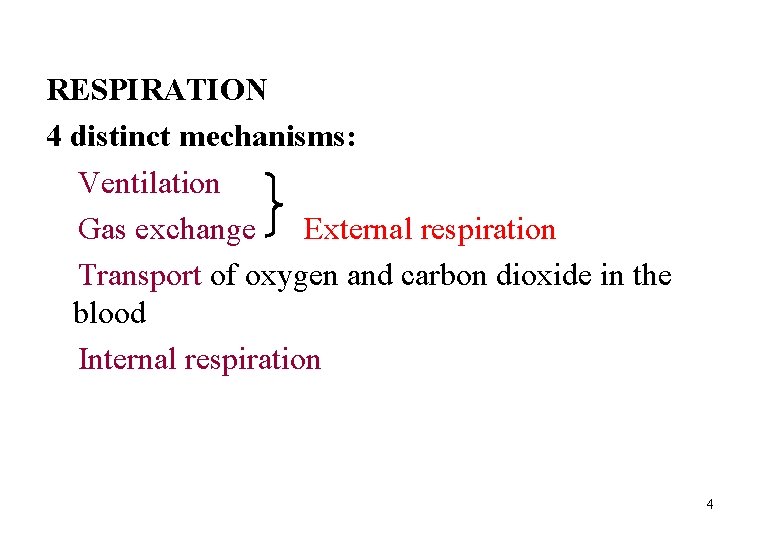
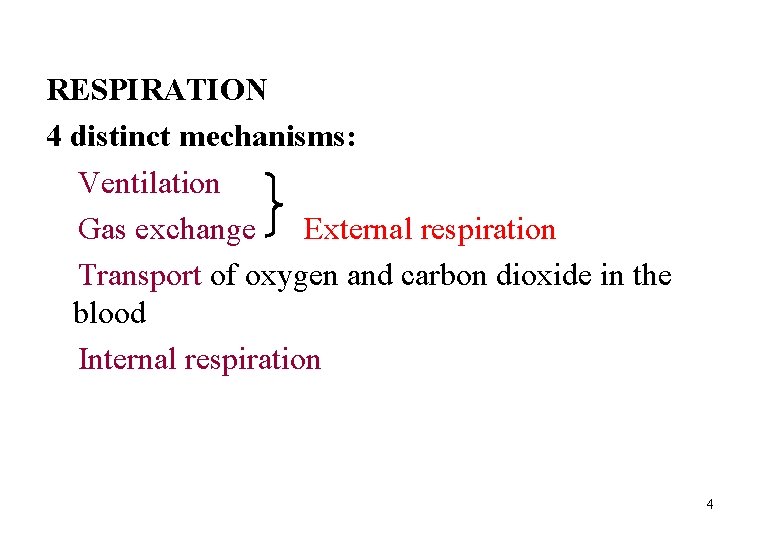
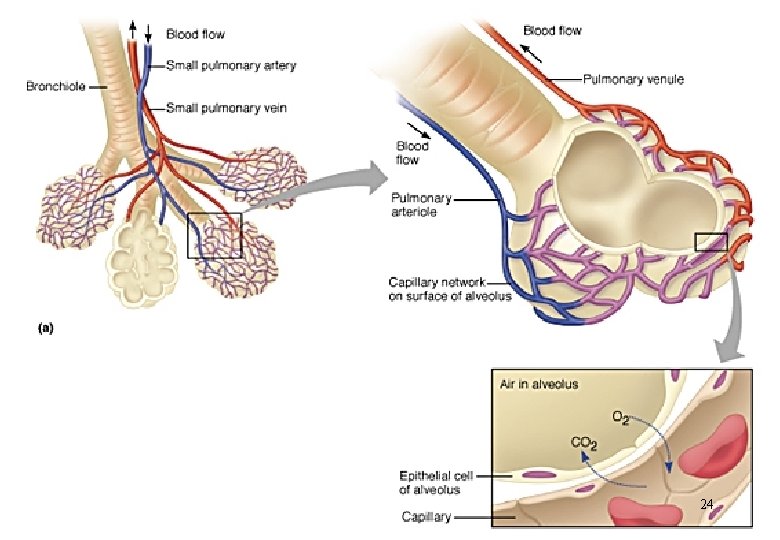
RESPIRATION 4 distinct mechanisms: Ventilation Gas exchange External respiration Transport of oxygen and carbon dioxide in the blood Internal respiration 4
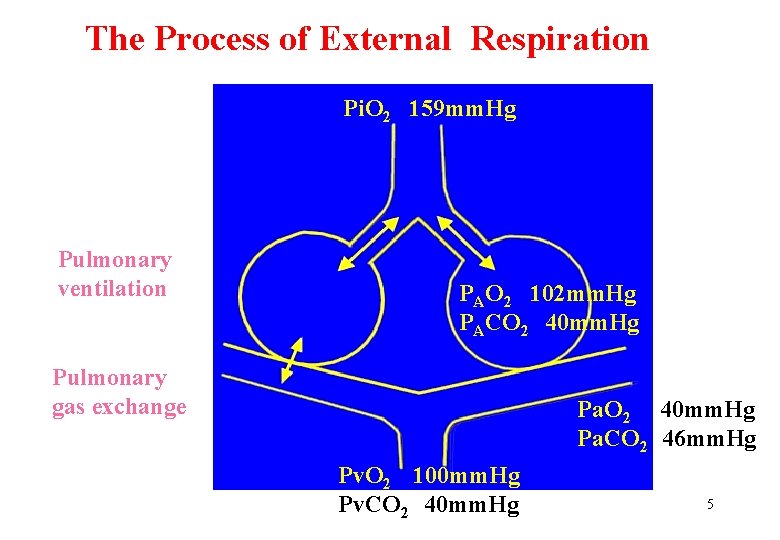
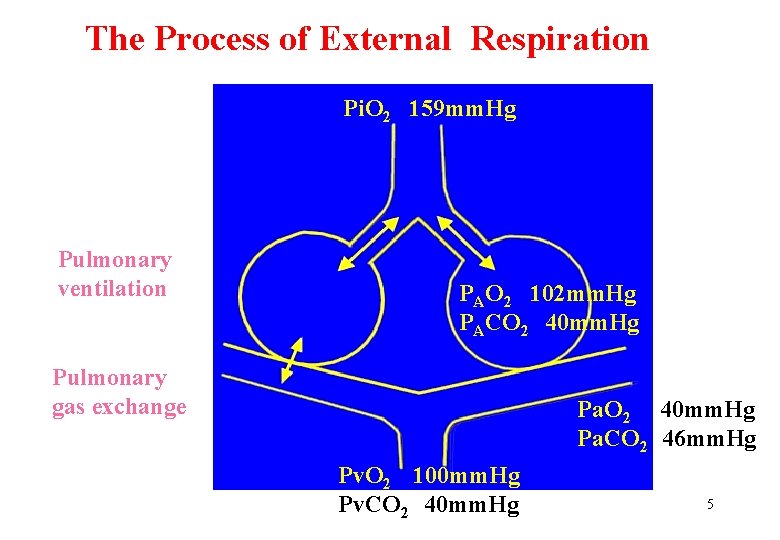
The Process of External Respiration Pi. O 2 159 mm. Hg Pulmonary ventilation PAO 2 102 mm. Hg PACO 2 40 mm. Hg Pulmonary gas exchange Pa. O 2 40 mm. Hg Pa. CO 2 46 mm. Hg Pv. O 2 100 mm. Hg Pv. CO 2 40 mm. Hg 5
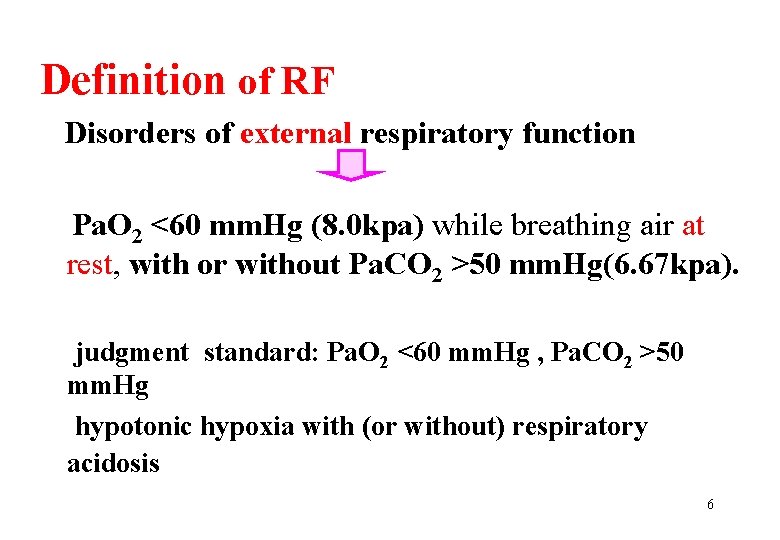
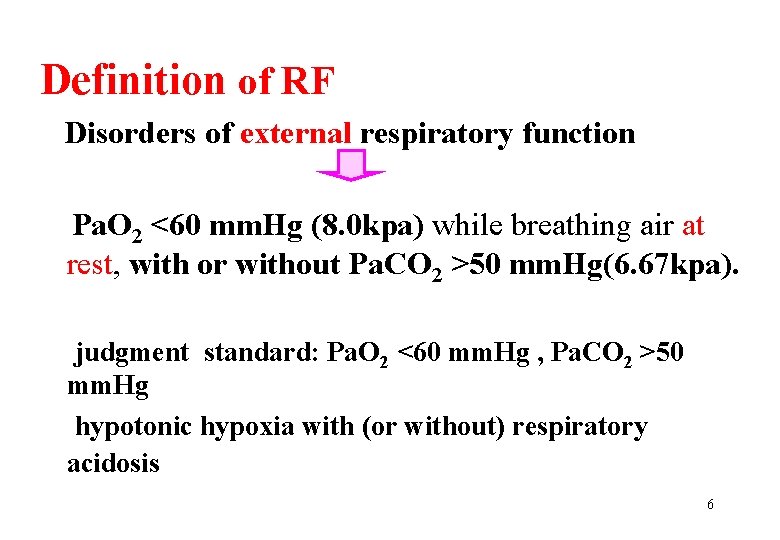
Definition of RF Disorders of external respiratory function Pa. O 2 <60 mm. Hg (8. 0 kpa) while breathing air at rest, with or without Pa. CO 2 >50 mm. Hg(6. 67 kpa). judgment standard: Pa. O 2 <60 mm. Hg , Pa. CO 2 >50 mm. Hg hypotonic hypoxia with (or without) respiratory acidosis 6
respiratory insufficiency: It is a condition in which respiratory function is inadequate to meet body’s needs during exertion. However, respiratory failure does so in rest. a kind of respiratory insufficiency a severe respiratory insufficiency 7
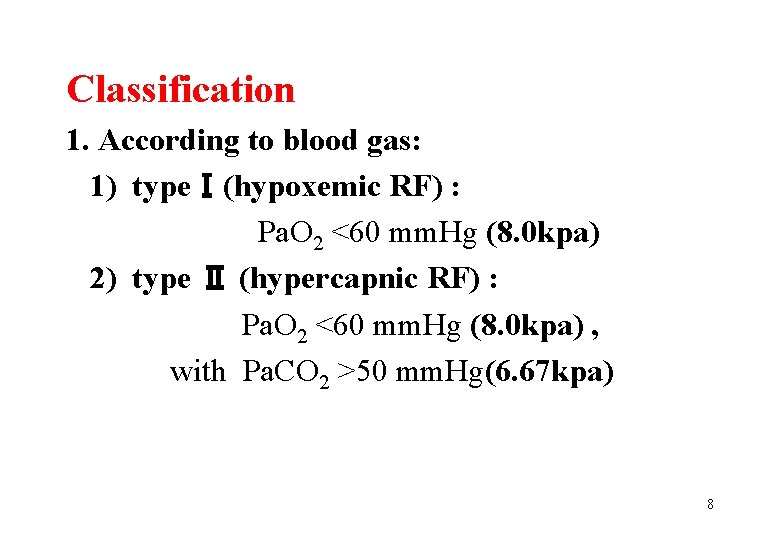
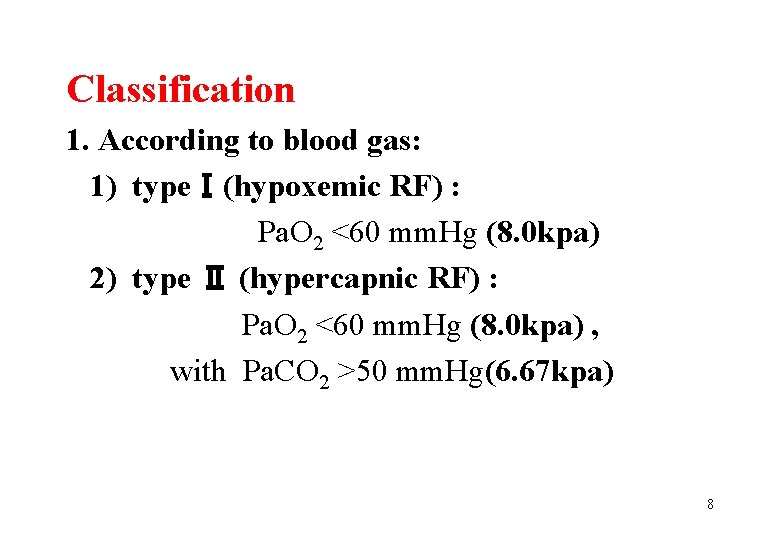
Classification 1. According to blood gas: 1) typeⅠ(hypoxemic RF) : Pa. O 2 <60 mm. Hg (8. 0 kpa) 2) type Ⅱ (hypercapnic RF) : Pa. O 2 <60 mm. Hg (8. 0 kpa) , with Pa. CO 2 >50 mm. Hg(6. 67 kpa) 8
2. According to primary site central peripheral 3. According to duration acute chronic 9
Section 1 Causes and pathogenesis of respiratory failure 10
• Pathogenesis of RF: Disorders of external respiratory function pulmonary ventilation disturbance pulmonary gas exchange disturbance 11
Ⅰ. pulmonary ventilation disturbance i. Types and Causes restrictive hypoventilation obstructive hypoventilation 12
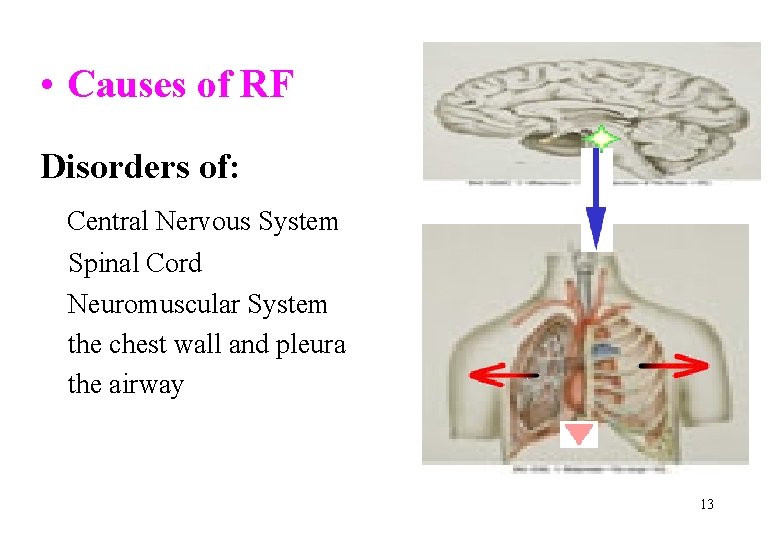
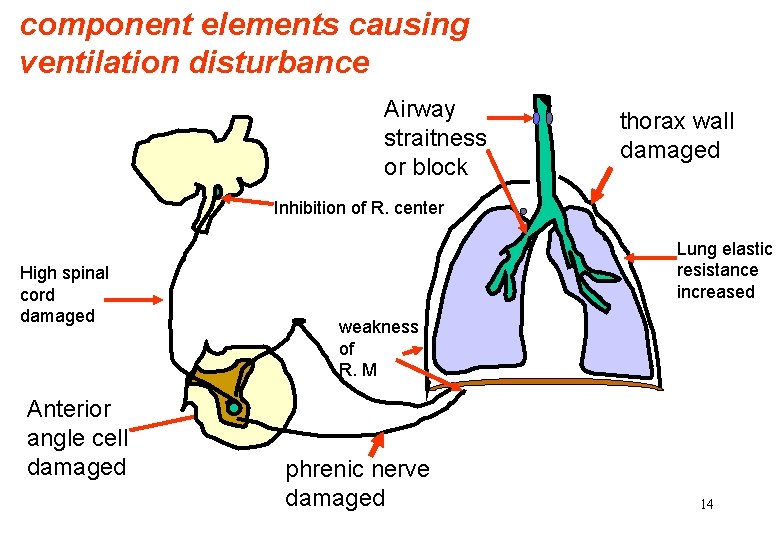
• Causes of RF Disorders of: Central Nervous System Spinal Cord Neuromuscular System the chest wall and pleura the airway 13
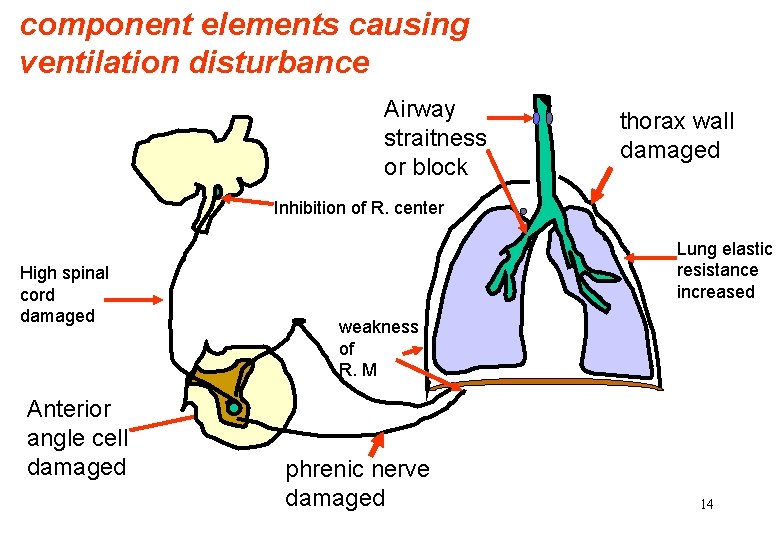
component elements causing ventilation disturbance Airway straitness or block thorax wall damaged Inhibition of R. center High spinal cord damaged Anterior angle cell damaged Lung elastic resistance increased weakness of R. M phrenic nerve damaged 14
1. Restrictive hypoventilation: Causes and mechanisms: v impaired activity of respiratory muscle (dysfunction of CNS, neural, muscle etc. ) v decreased compliance of thorax (chest malformation , pleura fibrosis) v decreased compliance of lungs (pulmonary edema , inflammation , fibrosis, insufficient surfactant) v thorax fluidify or pneumothorax 15
2. Obstructive hypoventilation : central airway obstruction peripheral airway obstruction 16
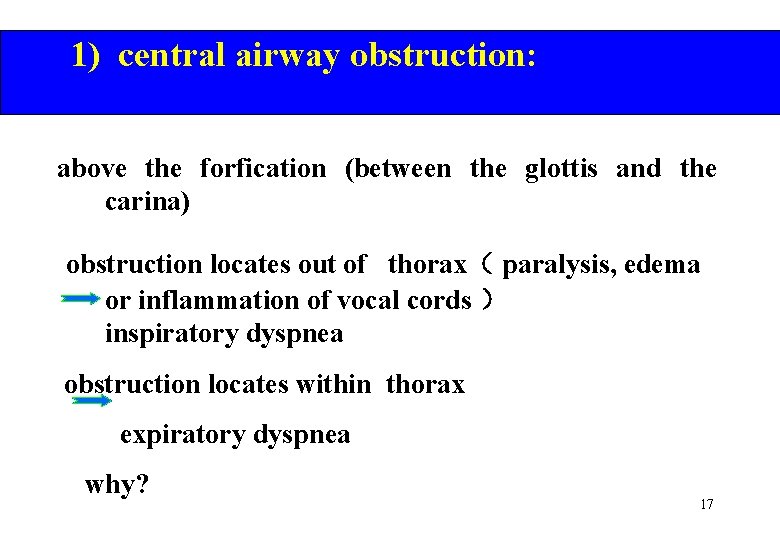
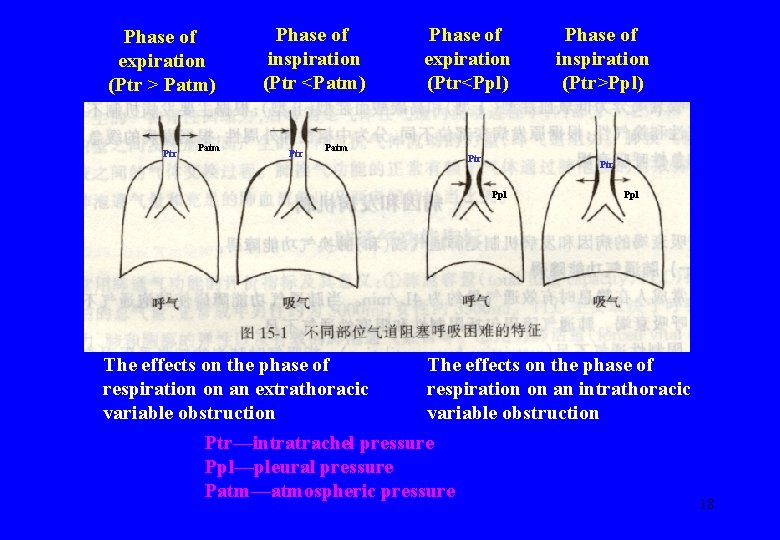
1) central airway obstruction: above the forfication (between the glottis and the carina) obstruction locates out of thorax( paralysis, edema or inflammation of vocal cords ) inspiratory dyspnea obstruction locates within thorax expiratory dyspnea why? 17
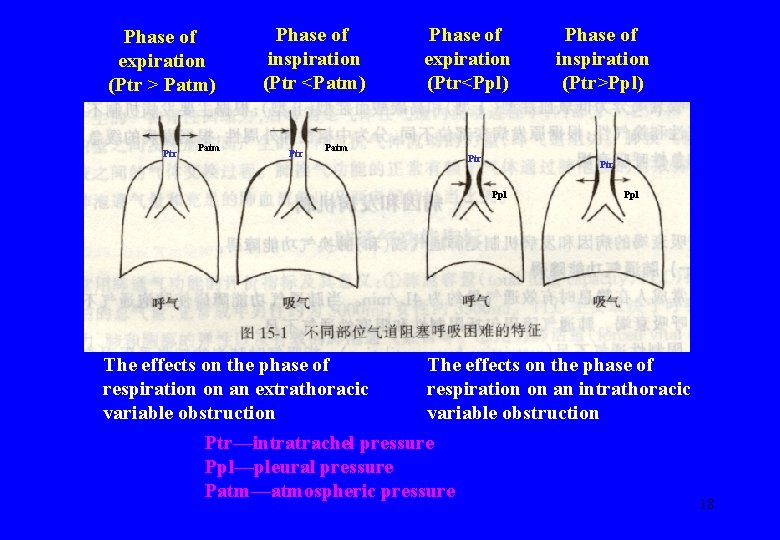
Phase of expiration (Ptr > Patm) Ptr Patm Phase of inspiration (Ptr <Patm) Ptr Phase of expiration (Ptr<Ppl) Patm Ptr Ppl The effects on the phase of respiration on an extrathoracic variable obstruction Phase of inspiration (Ptr>Ppl) Ppl The effects on the phase of respiration on an intrathoracic variable obstruction Ptr—intratrachel pressure Ppl—pleural pressure Patm—atmospheric pressure 18
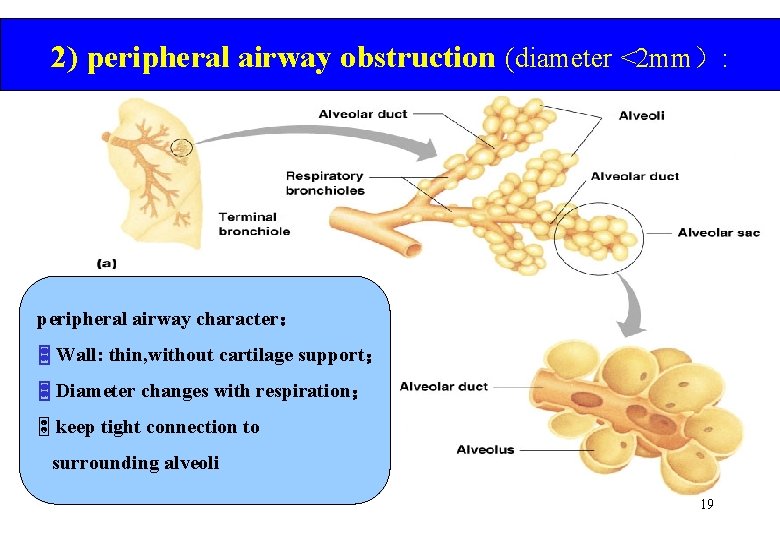
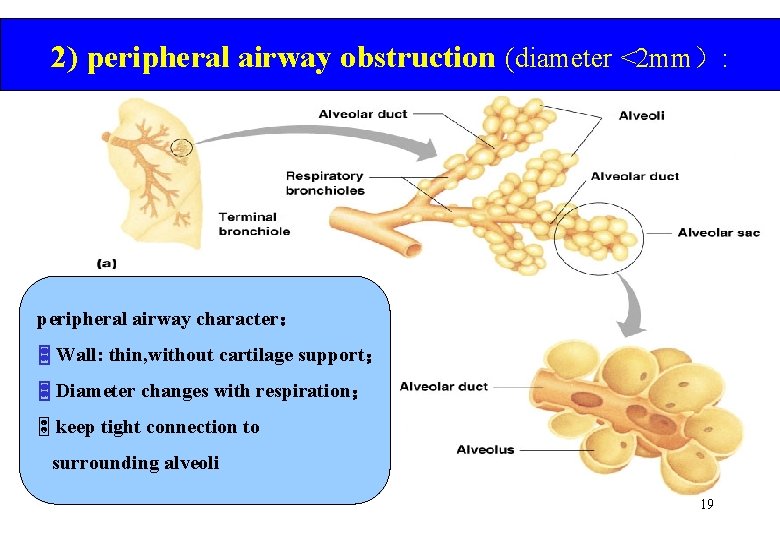
2) peripheral airway obstruction (diameter <2 mm): peripheral airway character: Wall: thin, without cartilage support; Diameter changes with respiration; ½ keep tight connection to surrounding alveoli 19
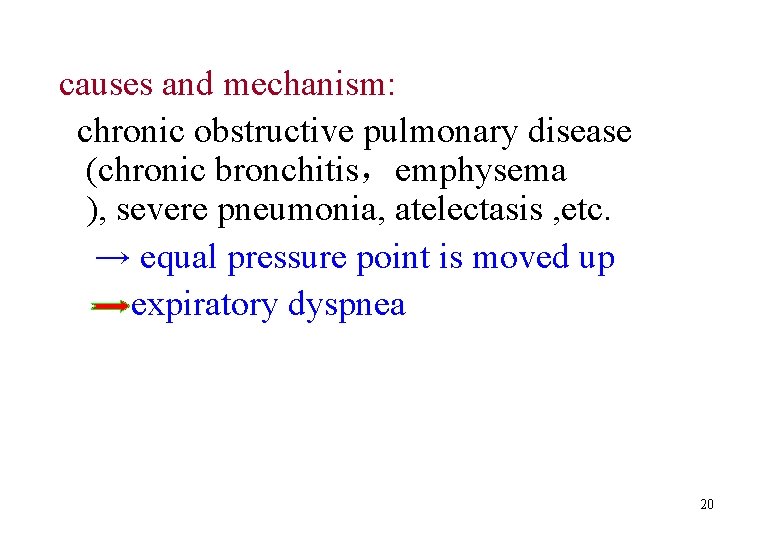
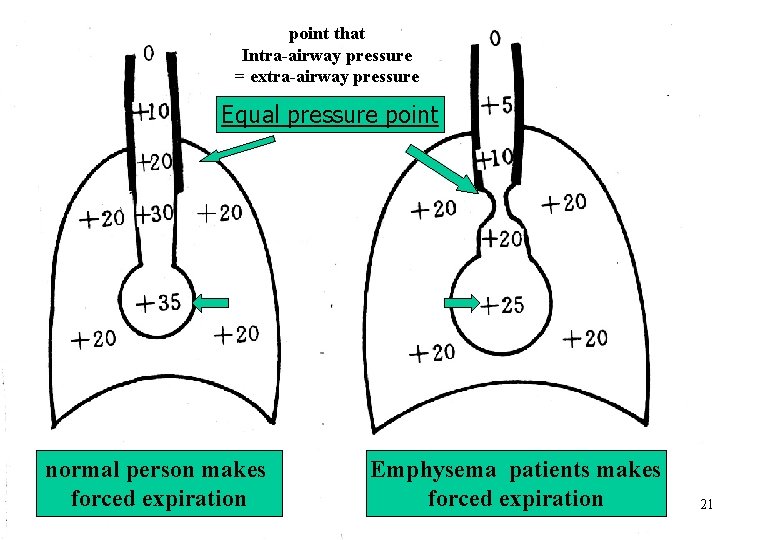
causes and mechanism: chronic obstructive pulmonary disease (chronic bronchitis,emphysema ), severe pneumonia, atelectasis , etc. → equal pressure point is moved up expiratory dyspnea 20
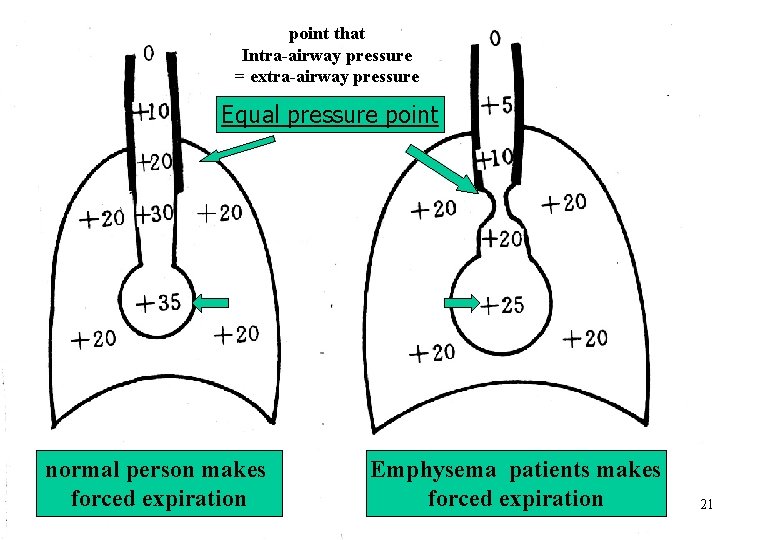
point that Intra-airway pressure = extra-airway pressure Equal pressure point normal person makes forced expiration Emphysema patients makes forced expiration 21
ii. Alteration of Pa. O 2 ,Pa. CO 2 in pulmonary ventilation disturbance Pa. O 2↓ Pa. CO 2↑ ( type II RF) 22
Ⅱ. Pulmonary gas exchange disturbance 23
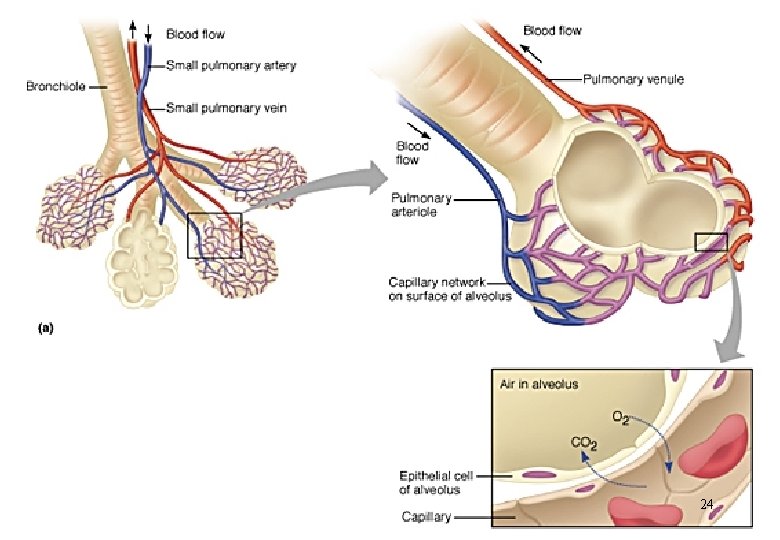
24
Pulmonary gas exchange disturbance diffusion impairment VA / Q mismatch anatomic shunt 25
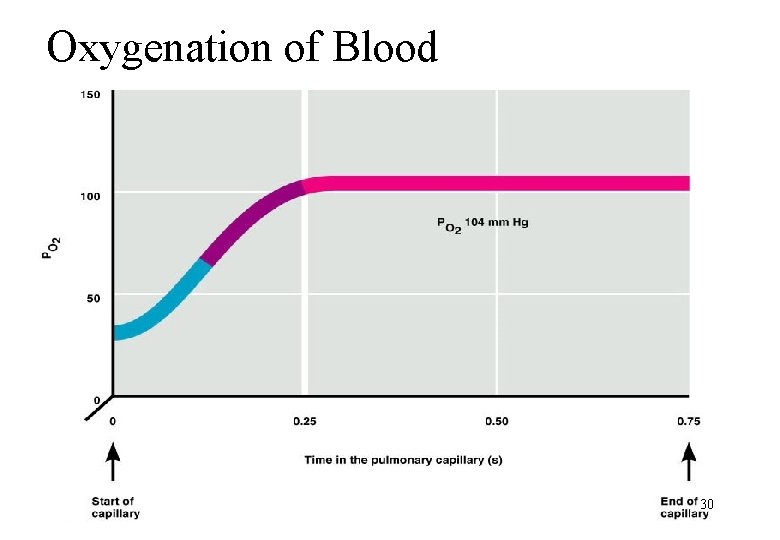
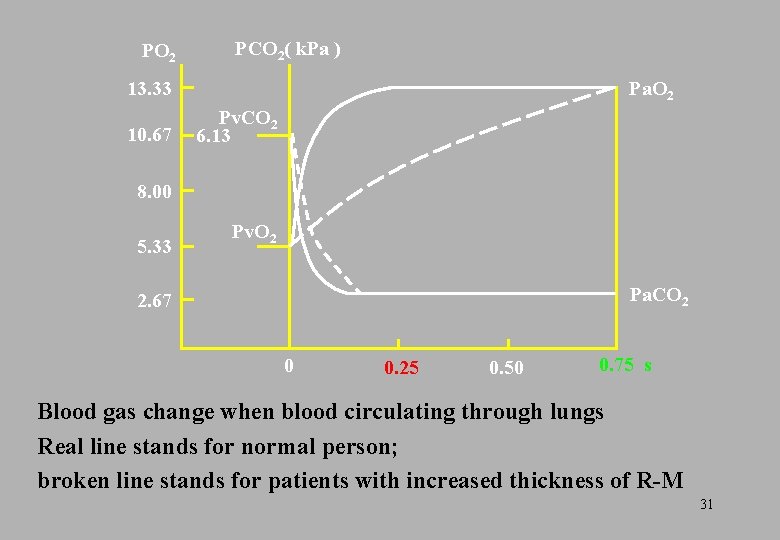
i. Diffusion impairment Causes: area of R-M thickness of R-M diffusion time 26
1. Area of R-M Normal adult R-M: 80 m 2 At rest, used R-M: 35~40 m 2 area of R-M : atelectasis,pulmonary consolidation,lobar resection, emphysema 27
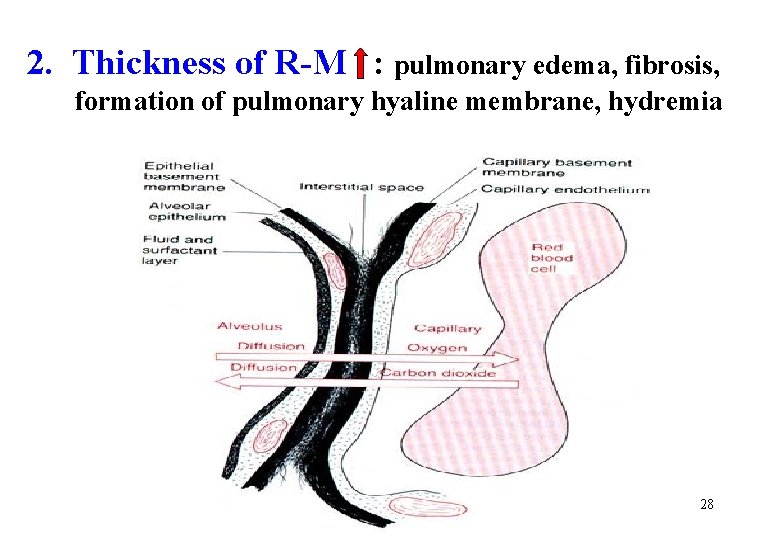
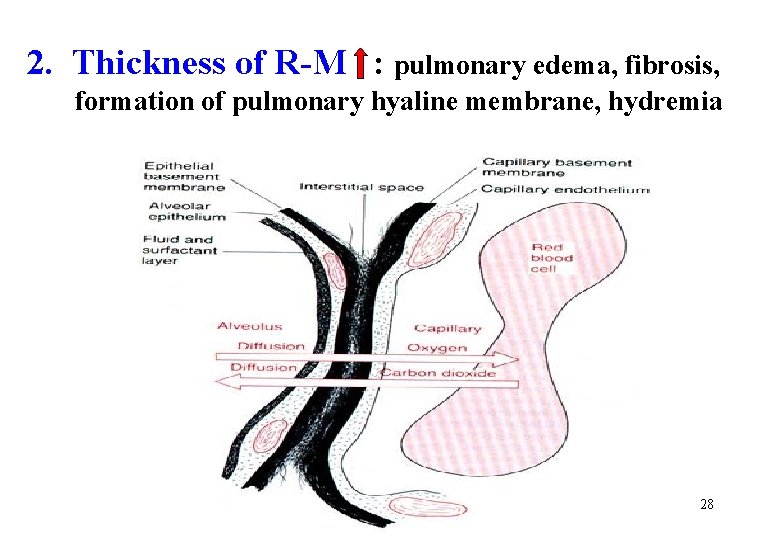
2. Thickness of R-M : pulmonary edema, fibrosis, formation of pulmonary hyaline membrane, hydremia 28
Alteration of Pa. O 2 , Pa. CO 2 Pa. O 2↓ Pa. CO 2 : N or ↓ according to compensatory ventilation why? 29
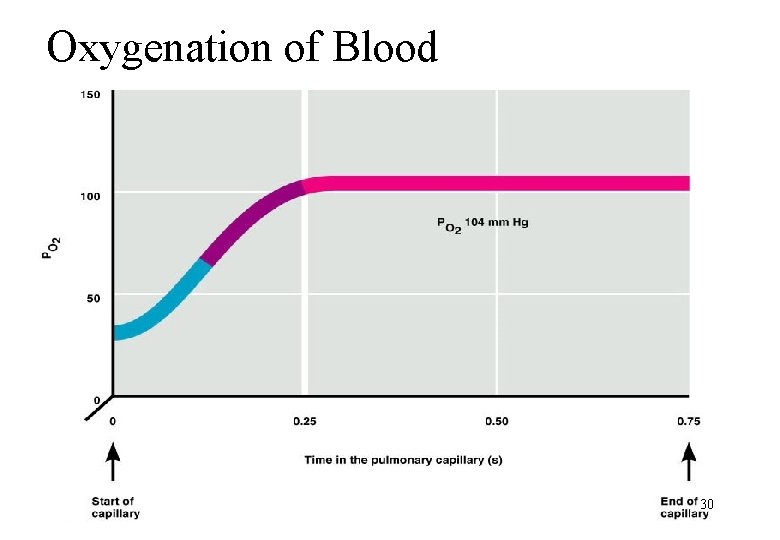
Oxygenation of Blood 30
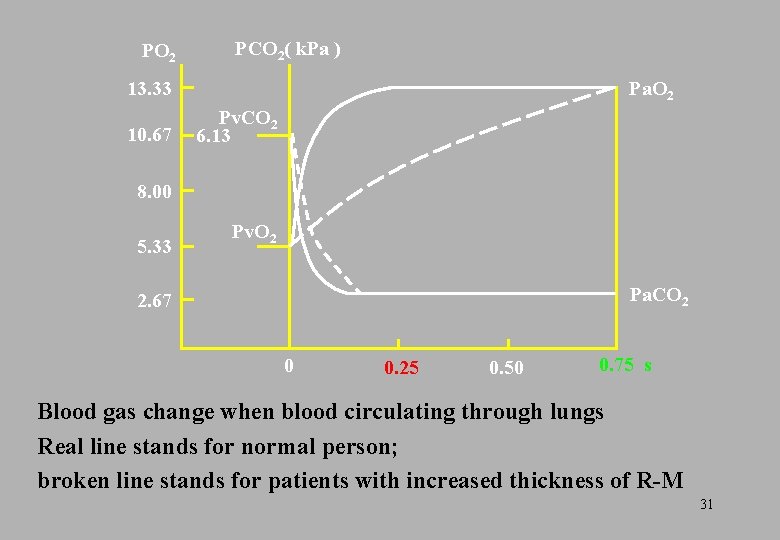
PO 2 PCO 2( k. Pa ) 13. 33 10. 67 Pa. O 2 Pv. CO 2 6. 13 8. 00 5. 33 Pv. O 2 Pa. CO 2 2. 67 0 0. 25 0. 50 0. 75 s Blood gas change when blood circulating through lungs Real line stands for normal person; broken line stands for patients with increased thickness of R-M 31
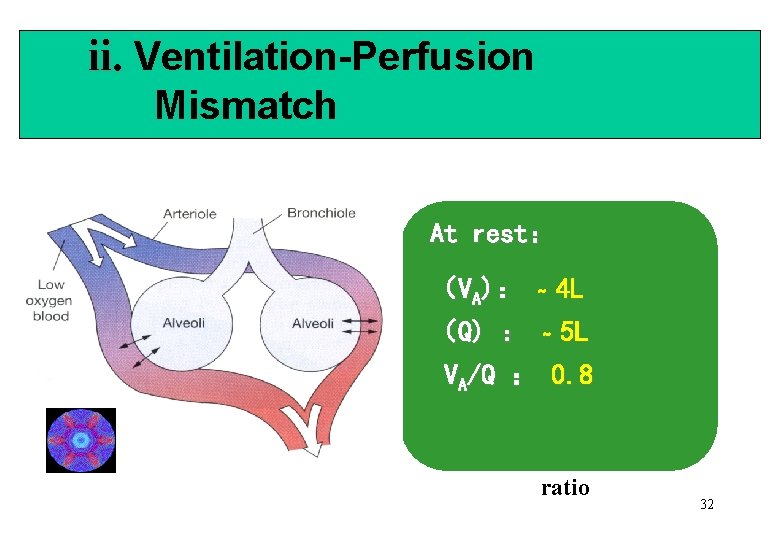
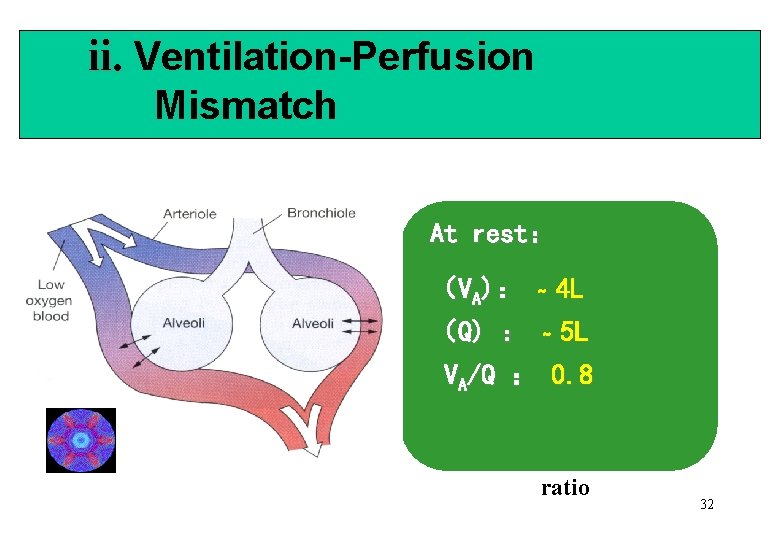
ii. Ventilation-Perfusion Mismatch At rest: (VA): ~ 4 L (Q) : ~ 5 L VA/Q : 0. 8 ratio 32
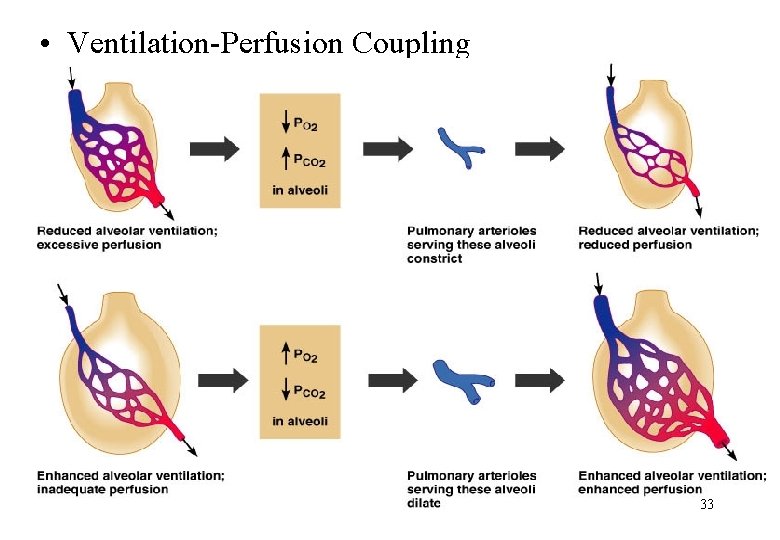
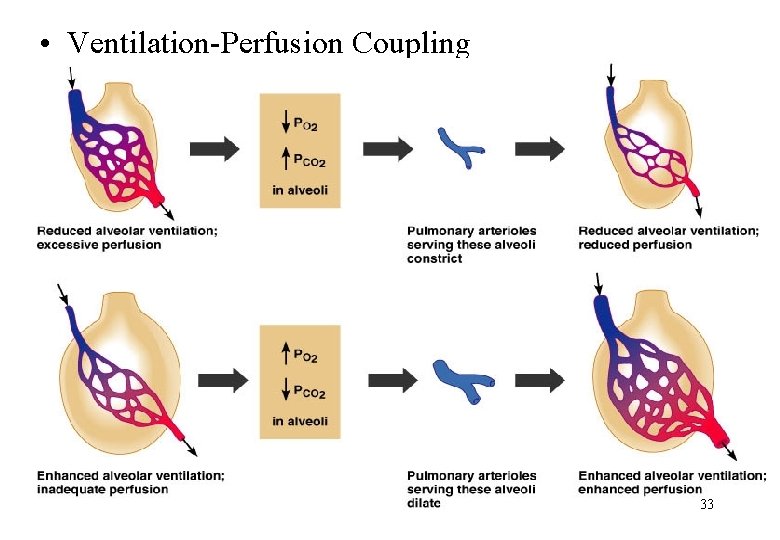
• Ventilation-Perfusion Coupling 33
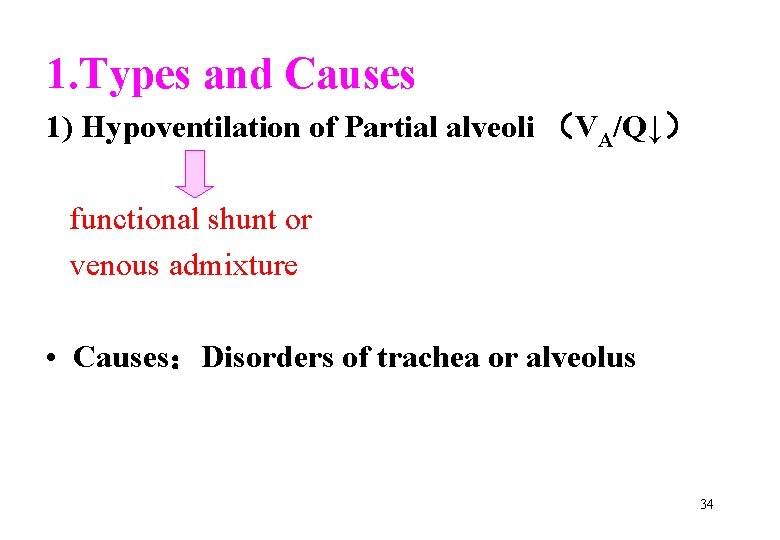
1. Types and Causes 1) Hypoventilation of Partial alveoli (VA/Q↓) functional shunt or venous admixture • Causes:Disorders of trachea or alveolus 34
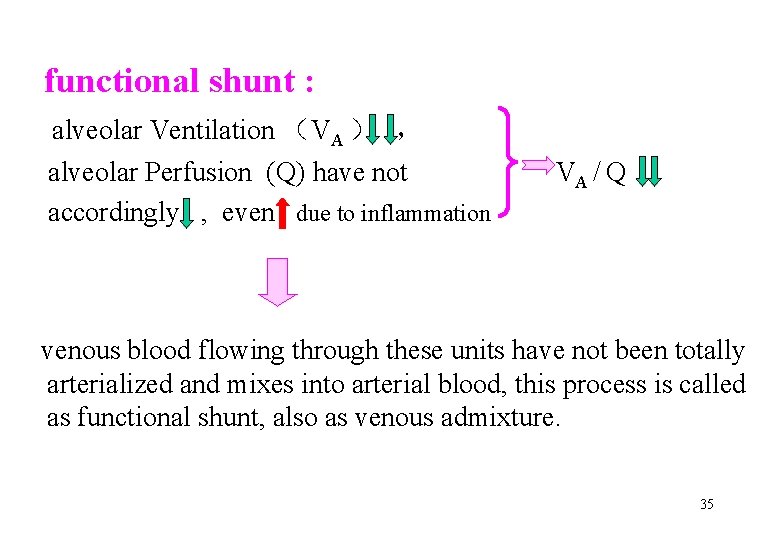
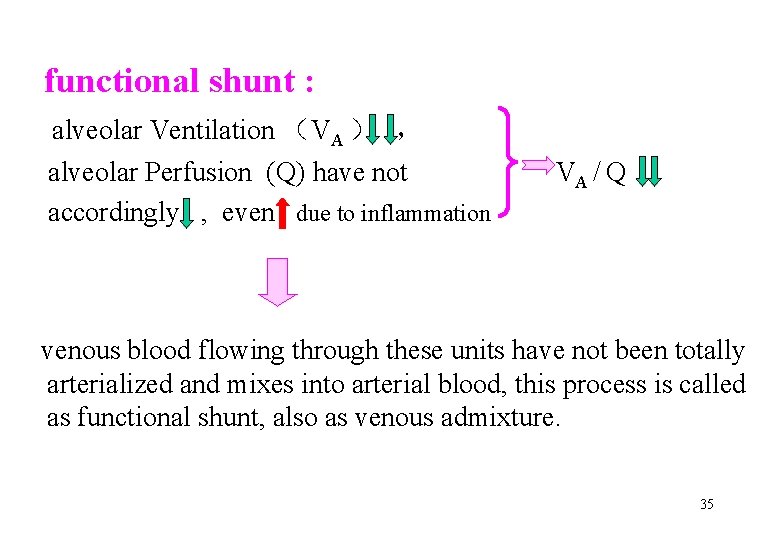
functional shunt : alveolar Ventilation (VA ) , alveolar Perfusion (Q) have not accordingly , even due to inflammation VA / Q venous blood flowing through these units have not been totally arterialized and mixes into arterial blood, this process is called as functional shunt, also as venous admixture. 35
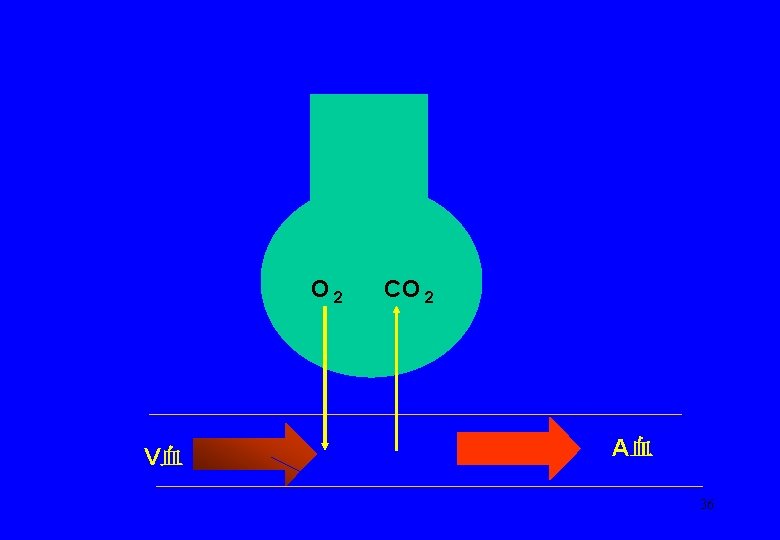
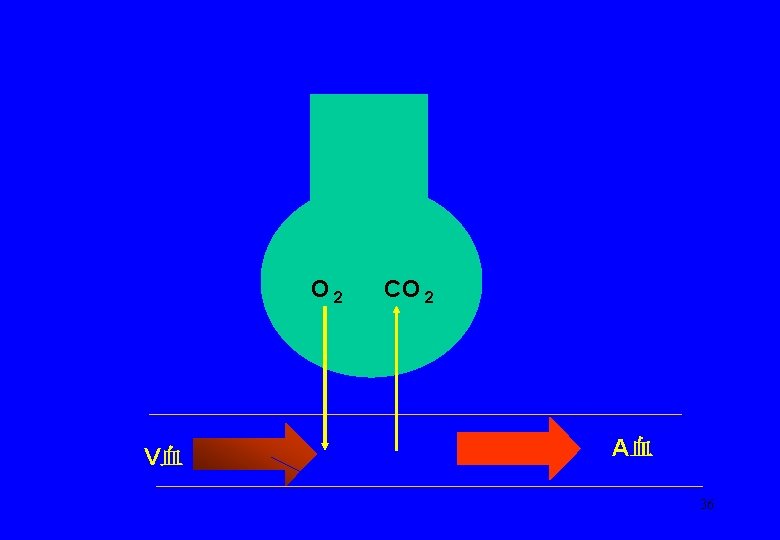
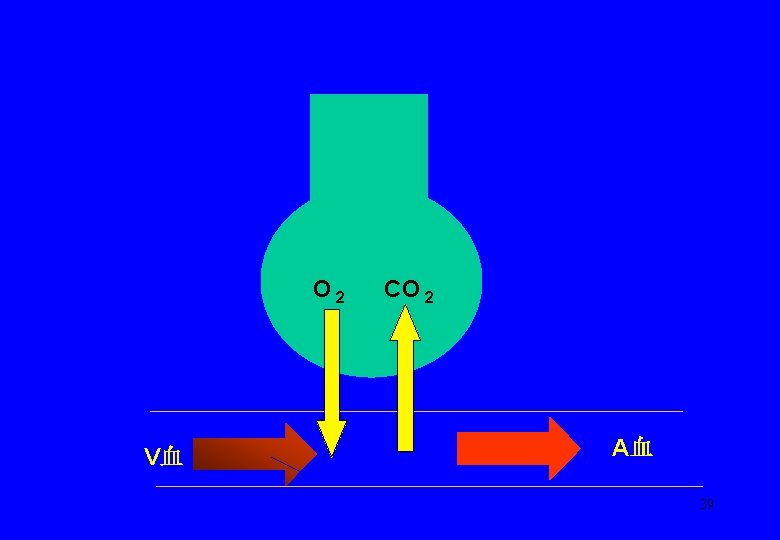
O 2 V血 CO 2 A血 36
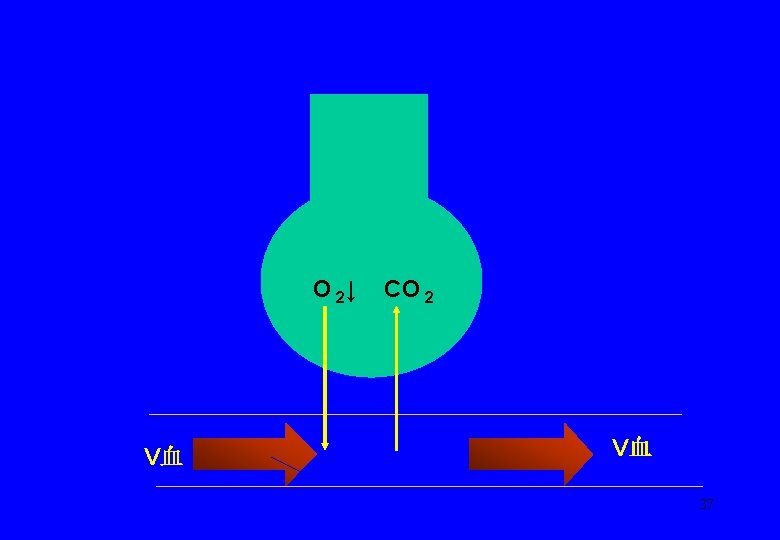
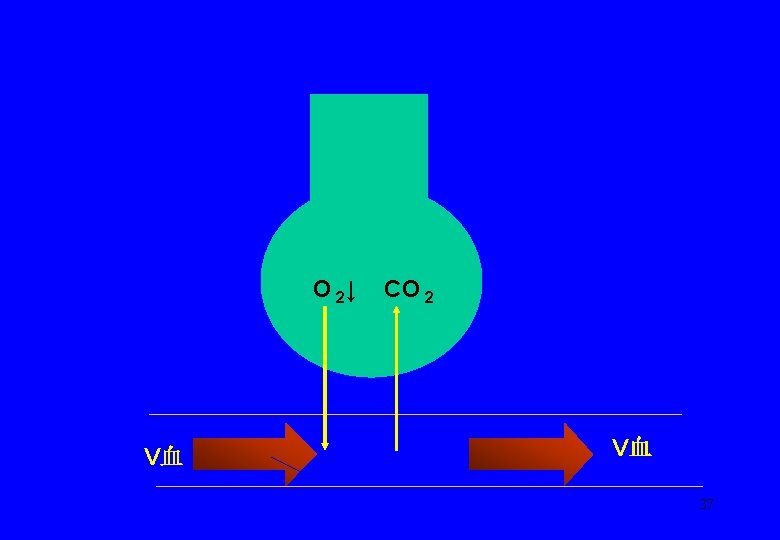
O 2↓ V血 CO 2 V血 37
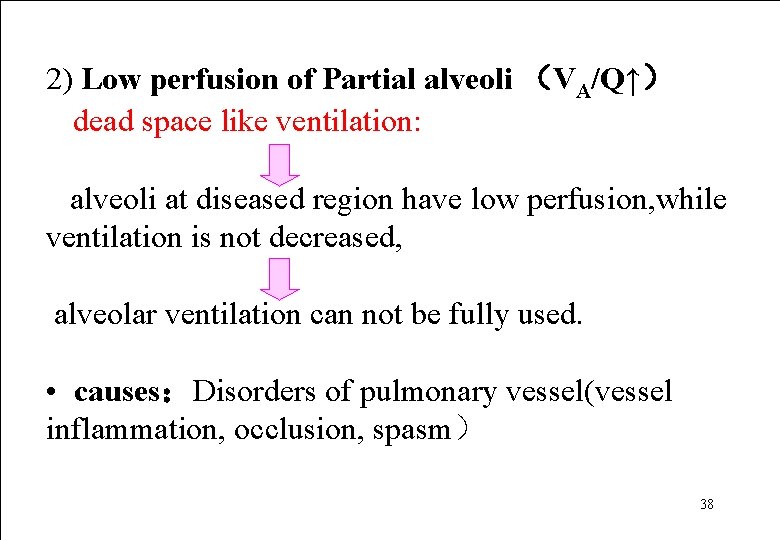
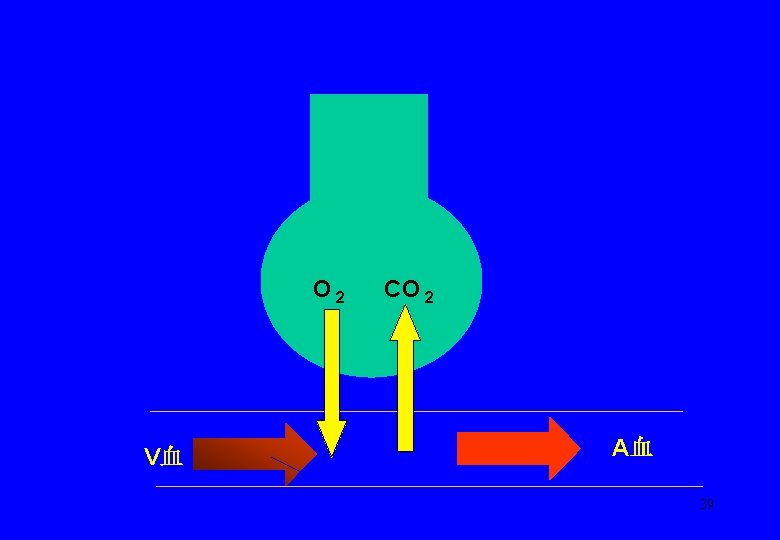
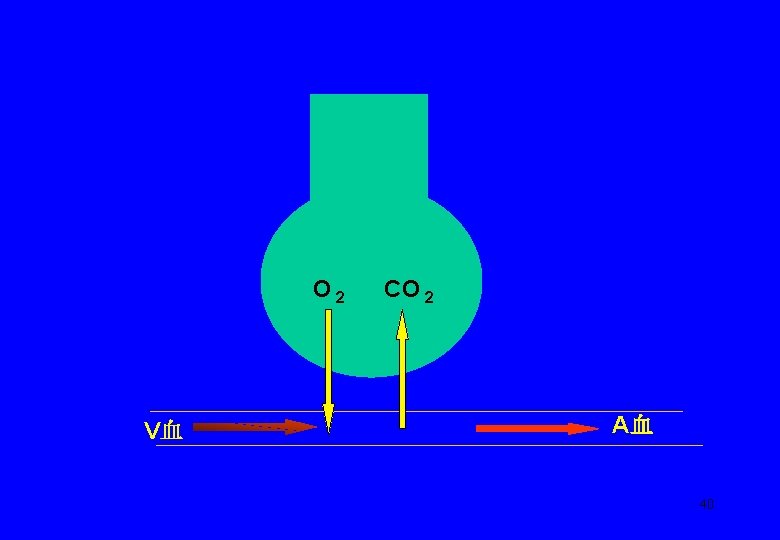
2) Low perfusion of Partial alveoli (VA/Q↑) dead space like ventilation: alveoli at diseased region have low perfusion, while ventilation is not decreased, alveolar ventilation can not be fully used. • causes:Disorders of pulmonary vessel(vessel inflammation, occlusion, spasm) 38
O 2 V血 CO 2 A血 39
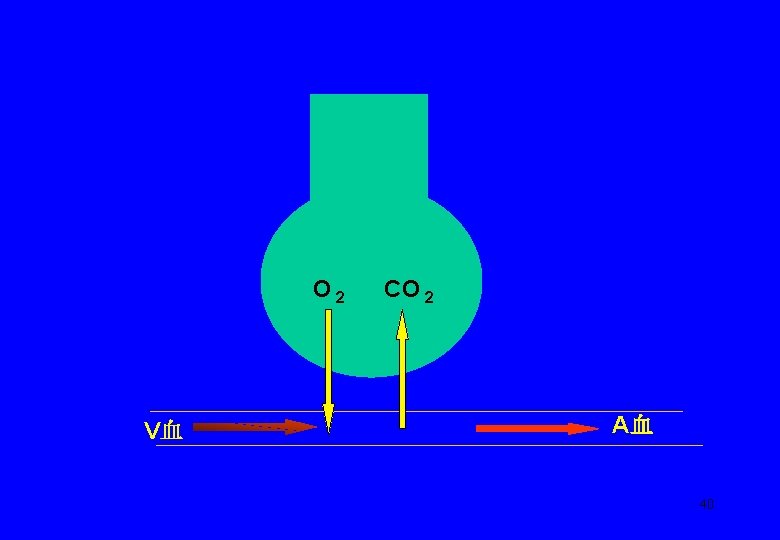
O 2 V血 CO 2 A血 40
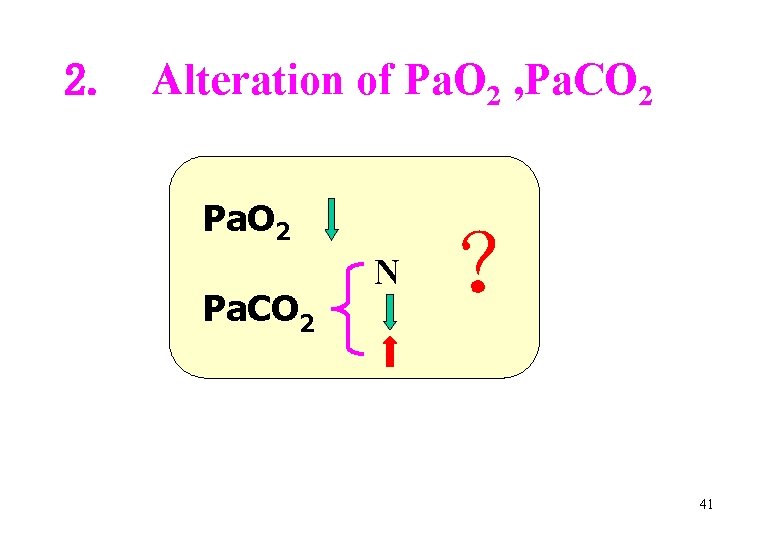
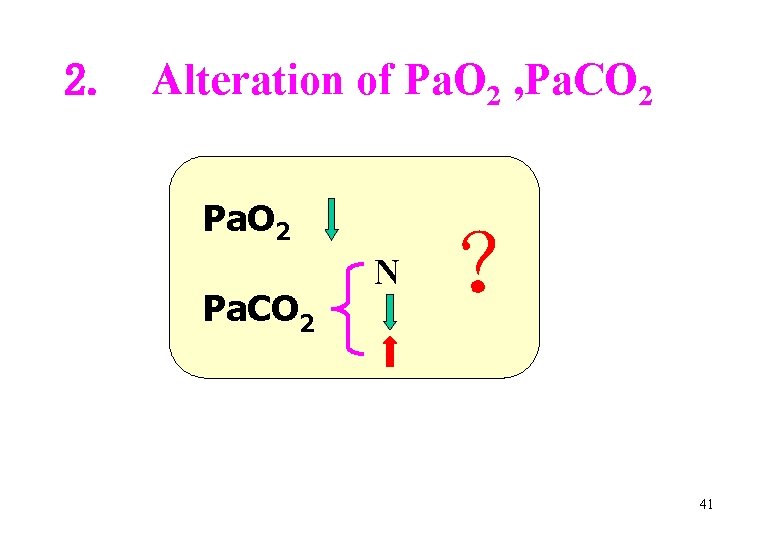
2. Alteration of Pa. O 2 , Pa. CO 2 N ? 41
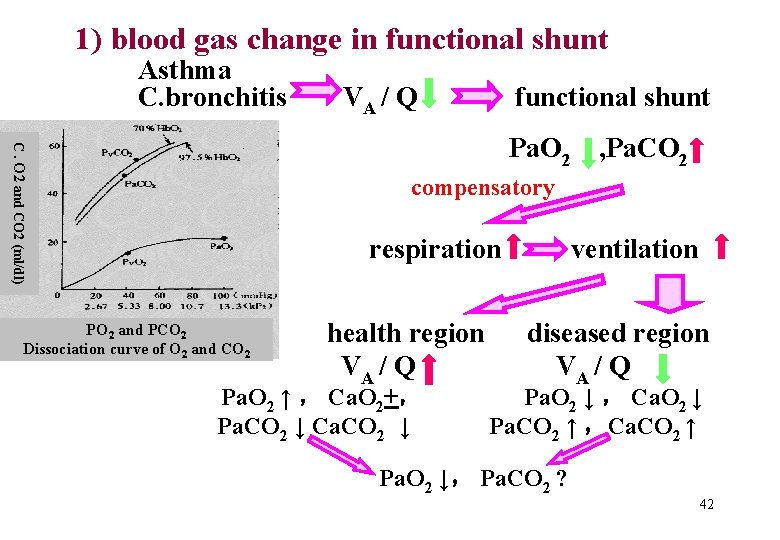
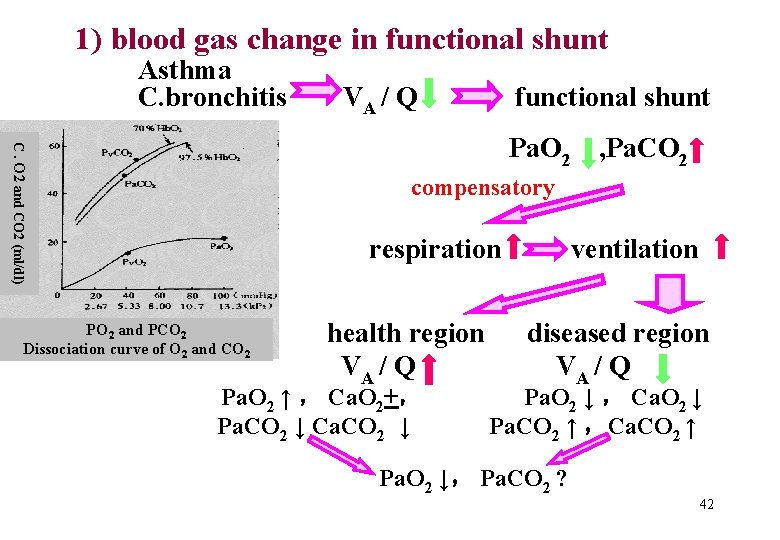
1) blood gas change in functional shunt Asthma C. bronchitis VA / Q functional shunt C. O 2 and CO 2 (ml/dl) Pa. O 2 , Pa. CO 2 compensatory respiration PO 2 and PCO 2 Dissociation curve of O 2 and CO 2 health region VA / Q Pa. O 2 ↑ , Ca. O 2+, Pa. CO 2 ↓ Ca. CO 2 ↓ ventilation diseased region VA / Q Pa. O 2 ↓ , Ca. O 2 ↓ Pa. CO 2 ↑ ,Ca. CO 2 ↑ Pa. O 2 ↓, Pa. CO 2 ? 42
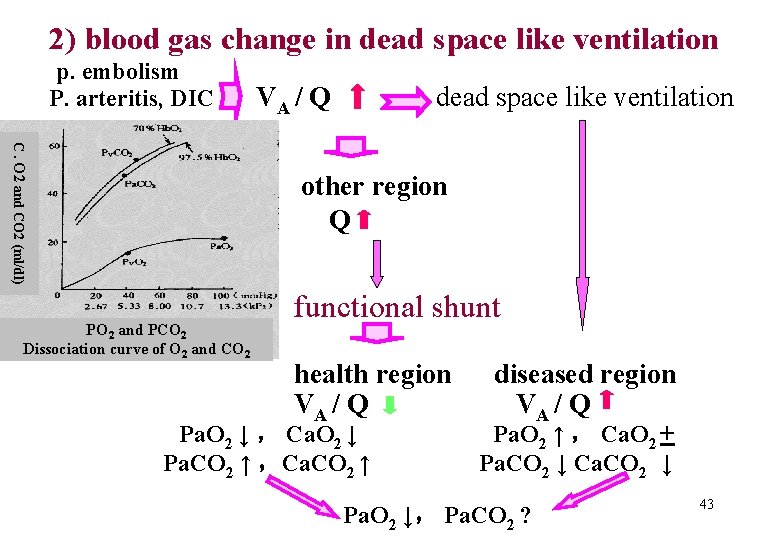
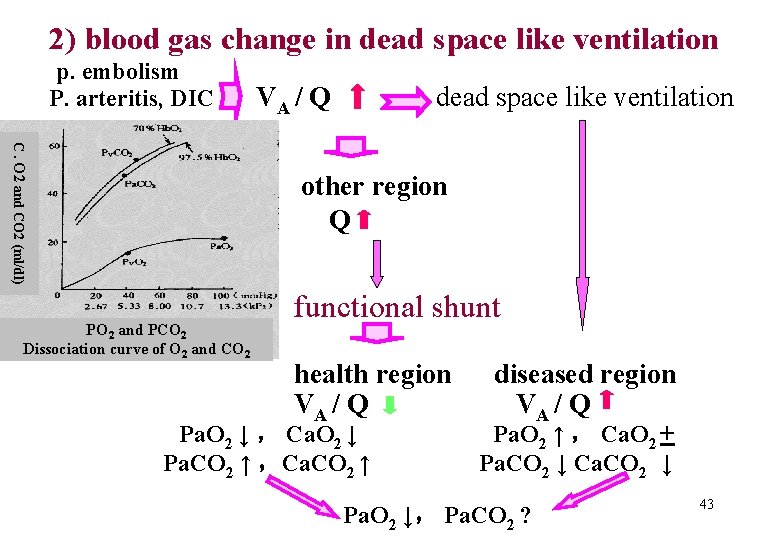
2) blood gas change in dead space like ventilation p. embolism P. arteritis, DIC VA / Q dead space like ventilation C. O 2 and CO 2 (ml/dl) other region Q PO 2 and PCO 2 Dissociation curve of O 2 and CO 2 functional shunt health region VA / Q Pa. O 2 ↓ , Ca. O 2 ↓ Pa. CO 2 ↑ ,Ca. CO 2 ↑ diseased region VA / Q Pa. O 2 ↑ , Ca. O 2 + Pa. CO 2 ↓ Ca. CO 2 ↓ Pa. O 2 ↓, Pa. CO 2 ? 43
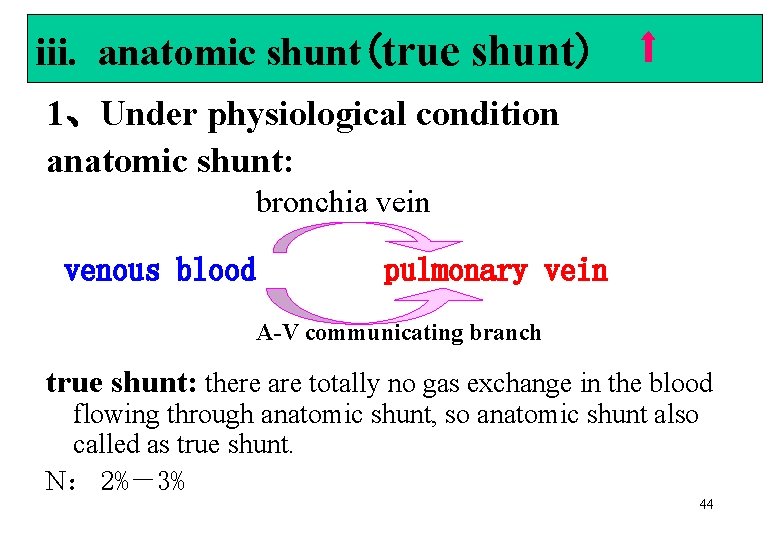
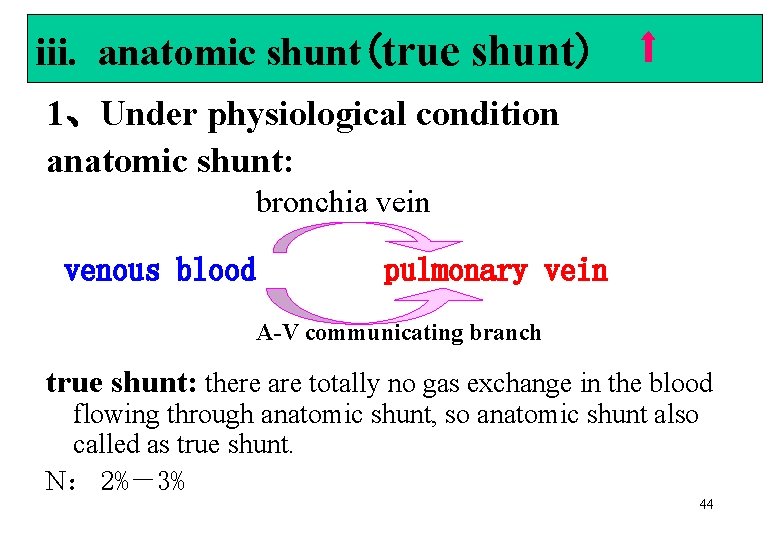
iii. anatomic shunt(true shunt) 1、Under physiological condition anatomic shunt: bronchia vein venous blood pulmonary vein A-V communicating branch true shunt: there are totally no gas exchange in the blood flowing through anatomic shunt, so anatomic shunt also called as true shunt. N: 2%-3% 44
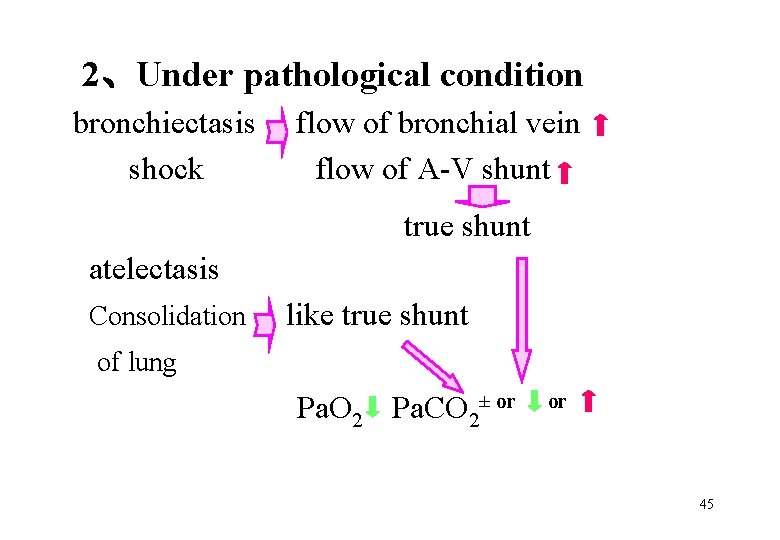
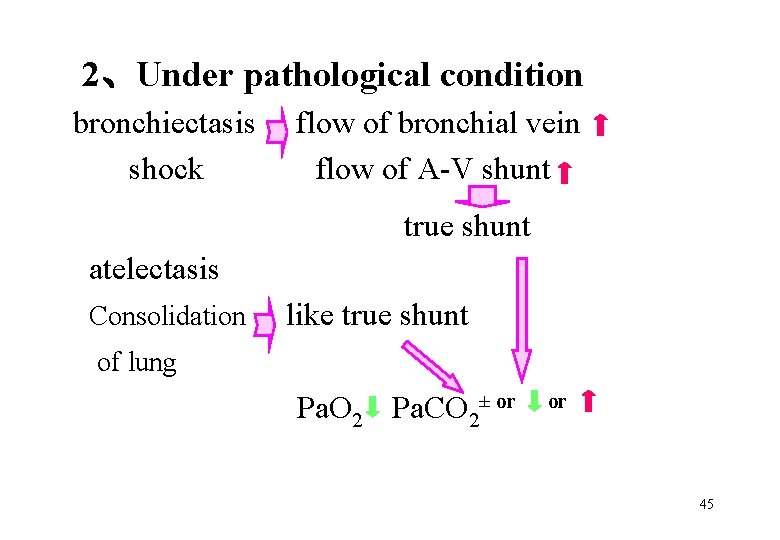
2、Under pathological condition bronchiectasis shock flow of bronchial vein flow of A-V shunt true shunt atelectasis Consolidation like true shunt of lung Pa. O 2 Pa. CO 2± or or 45
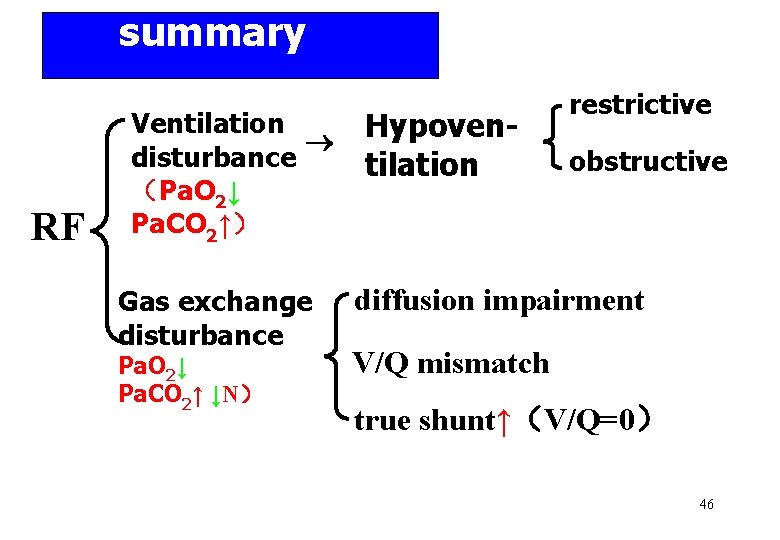
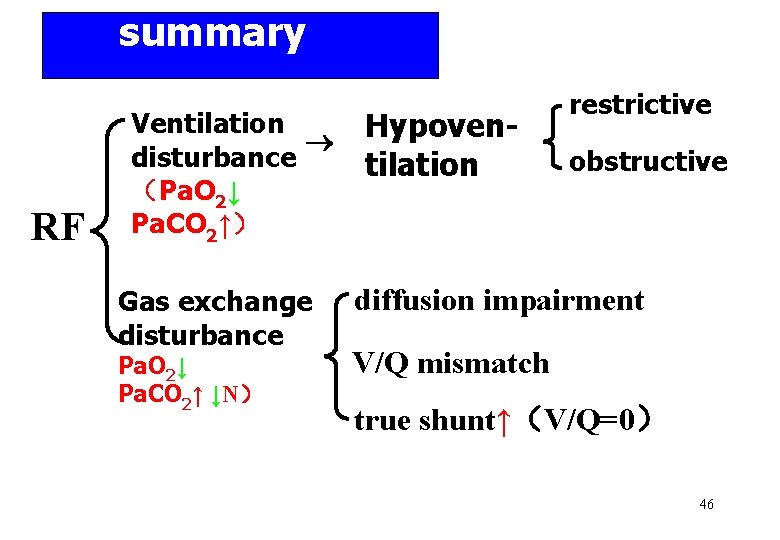
summary RF Ventilation disturbance (Pa. O 2↓ Pa. CO 2↑) Gas exchange disturbance Pa. O 2↓ Pa. CO 2↑ ↓N) Hypoventilation restrictive obstructive diffusion impairment V/Q mismatch true shunt↑(V/Q=0) 46
Section 2 The functional and metabolic changes in RF 47
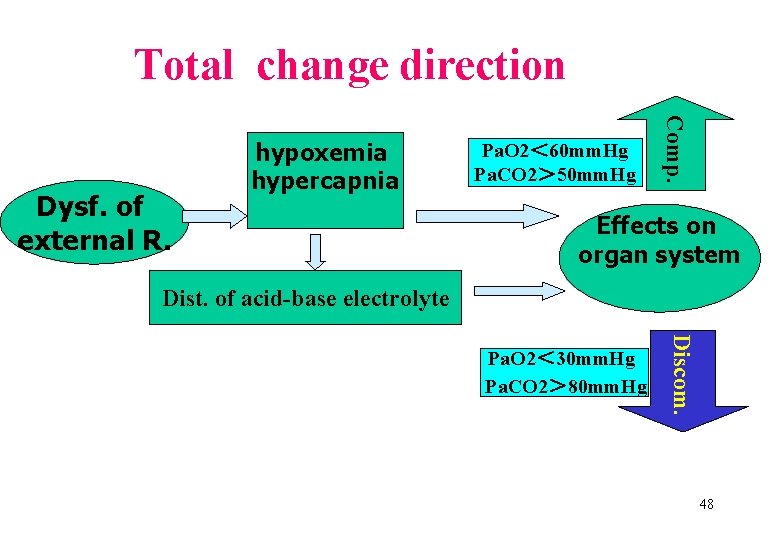
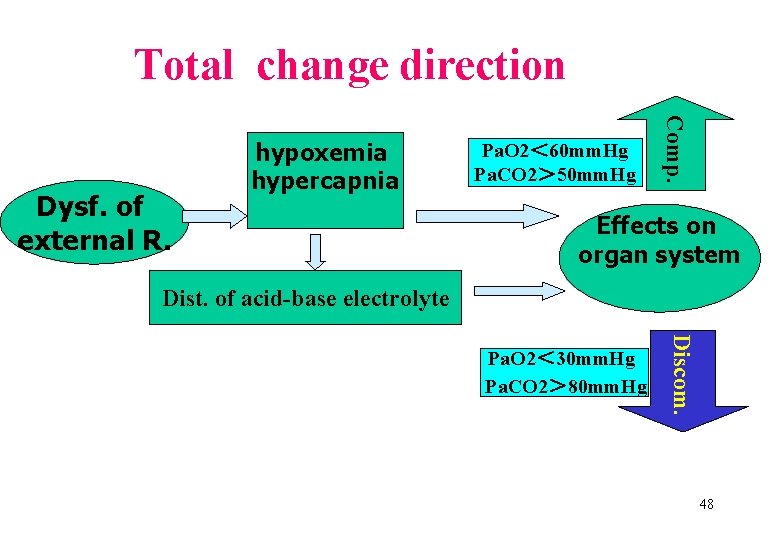
Total change direction Pa. O 2< 60 mm. Hg Pa. CO 2> 50 mm. Hg Comp. Dysf. of external R. hypoxemia hypercapnia Effects on organ system Dist. of acid-base electrolyte Discom. Pa. O 2< 30 mm. Hg Pa. CO 2> 80 mm. Hg 48
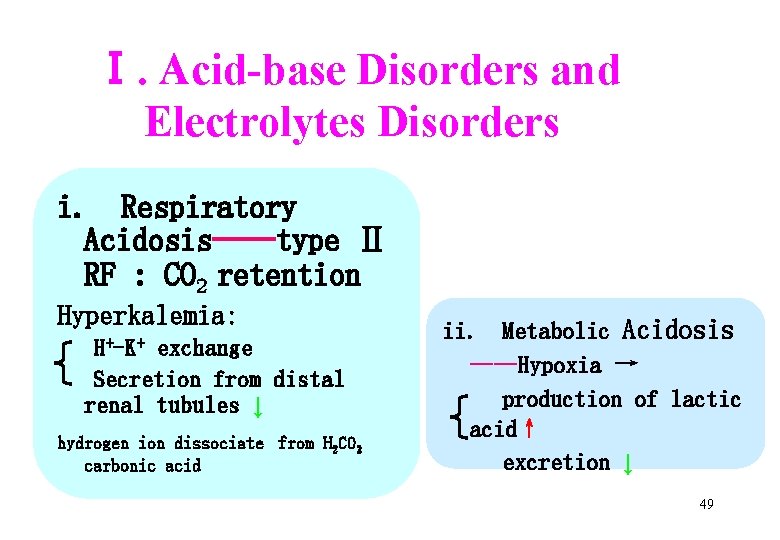
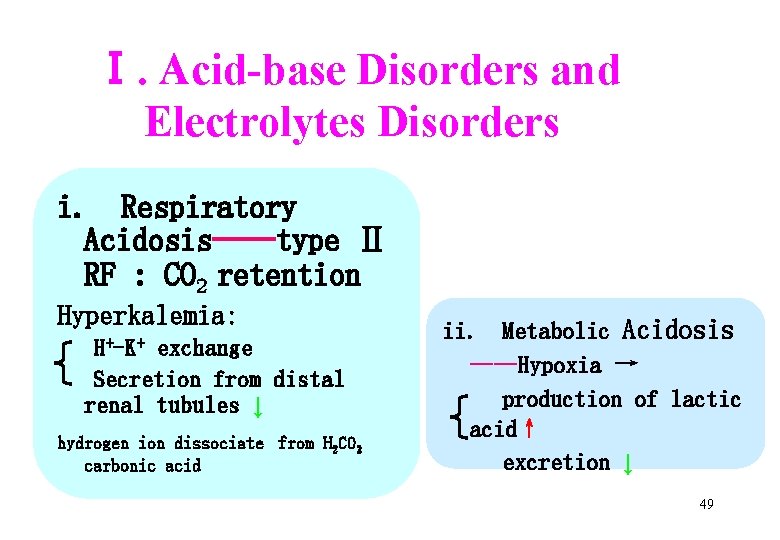
Ⅰ. Acid-base Disorders and Electrolytes Disorders i. Respiratory Acidosis——type Ⅱ RF : CO 2 retention Hyperkalemia: H+-K+ exchange Secretion from distal renal tubules ↓ hydrogen ion dissociate from H 2 CO 3 carbonic acid ii. Metabolic Acidosis ——Hypoxia → production of lactic acid↑ excretion ↓ 49
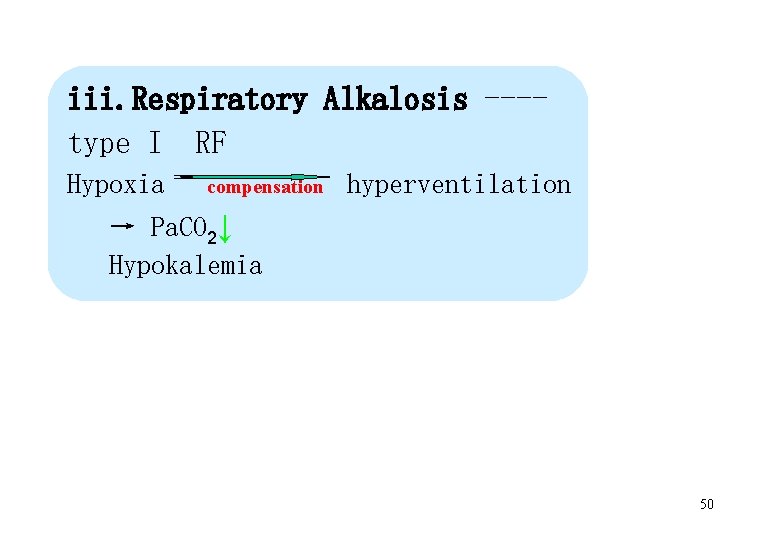
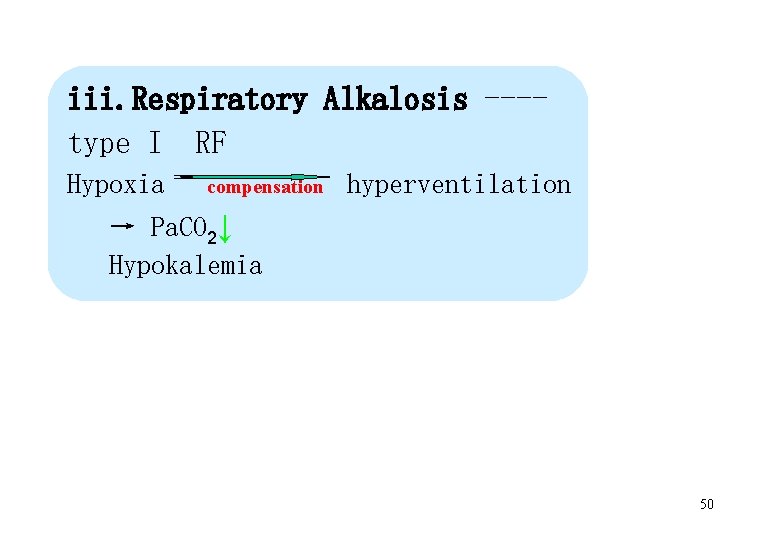
iii. Respiratory Alkalosis ---type I RF Hypoxia compensation hyperventilation → Pa. CO 2↓ Hypokalemia 50

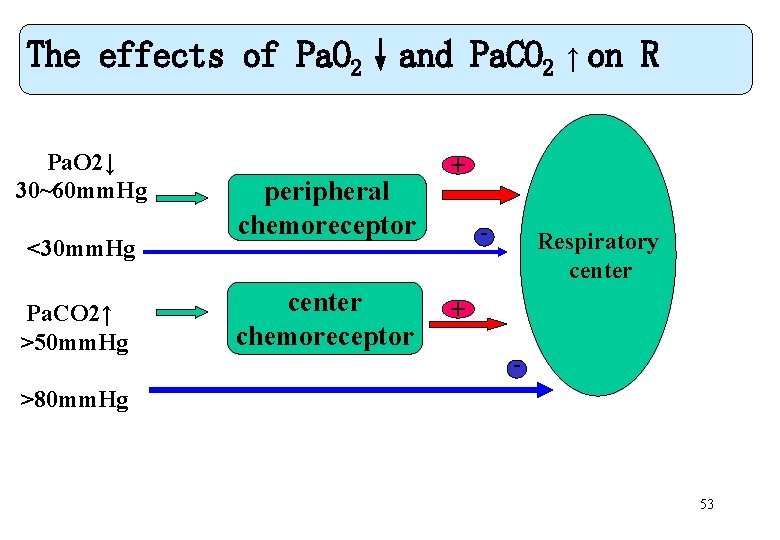
Ⅱ. Respiratory system 1、Effects of Pa. O 2↓and Pa. CO 2↑ (1) Pa. O 2↓ Pa. O 2 ↓ stimulate peripheral chemoreceptor excite respiration inhibit respiratory center inhibit respiration 30 mm. Hg<Pa. O 2<60 mm. Hg: excite respiration Pa. O 2<30 mm. Hg: inhibit respiration 51
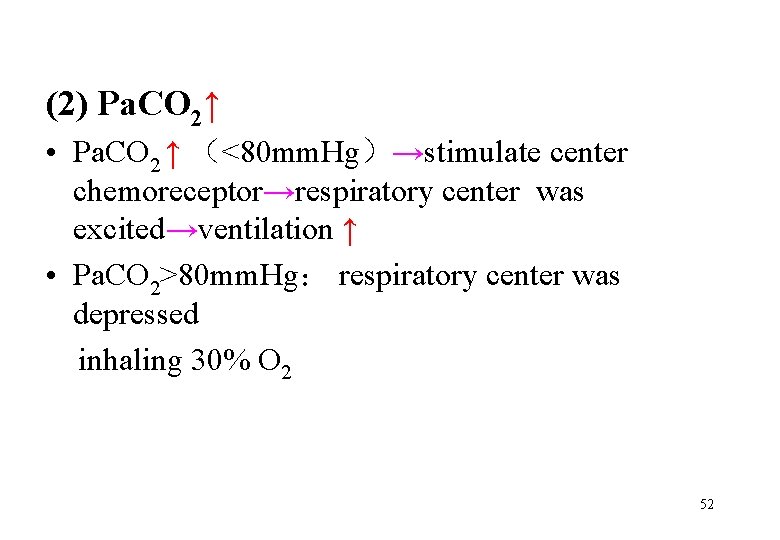
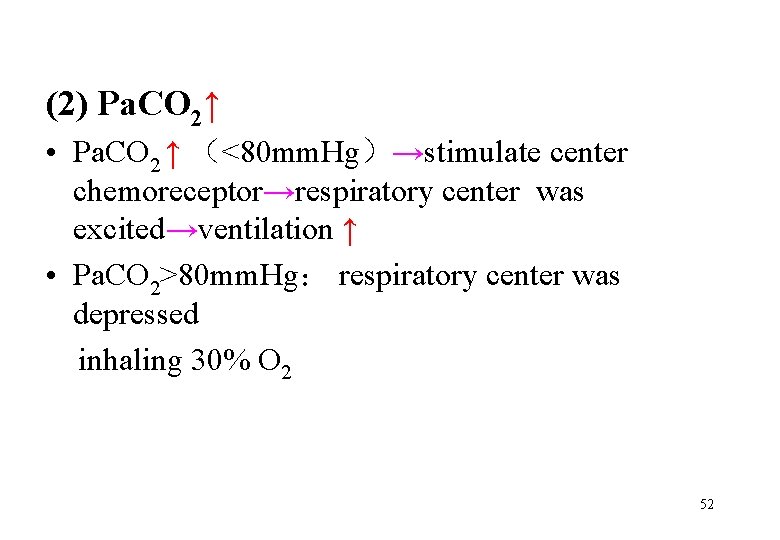
(2) Pa. CO 2↑ • Pa. CO 2 ↑ (<80 mm. Hg)→stimulate center chemoreceptor→respiratory center was excited→ventilation ↑ • Pa. CO 2>80 mm. Hg: respiratory center was depressed inhaling 30% O 2 52
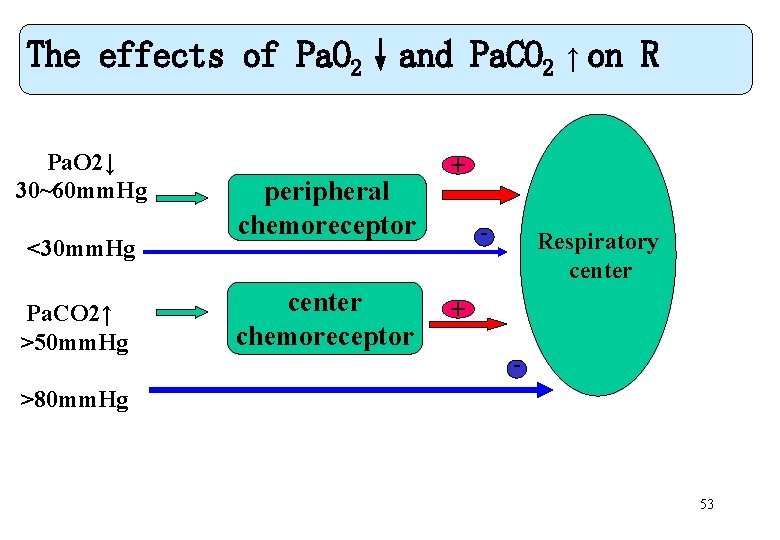
The effects of Pa. O 2↓and Pa. CO 2 ↑ on R <30 mm. Hg Pa. CO 2↑ >50 mm. Hg peripheral chemoreceptor center chemoreceptor + - Pa. O 2↓ 30~60 mm. Hg Respiratory center + - >80 mm. Hg 53
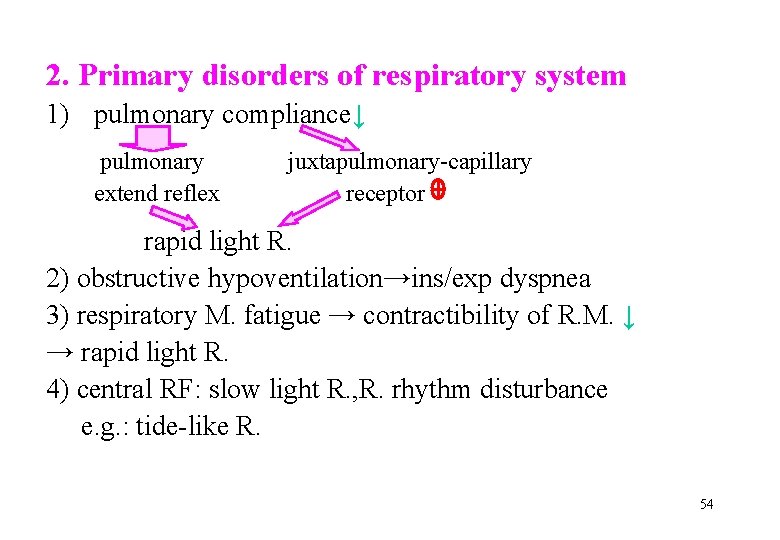
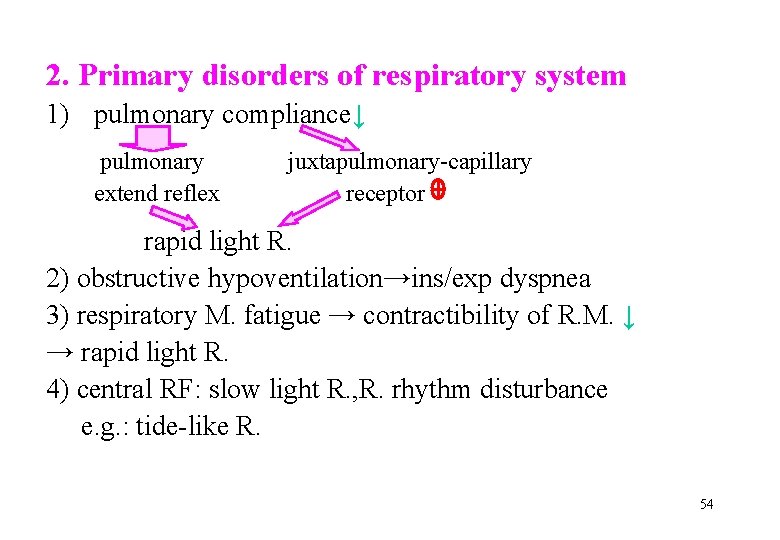
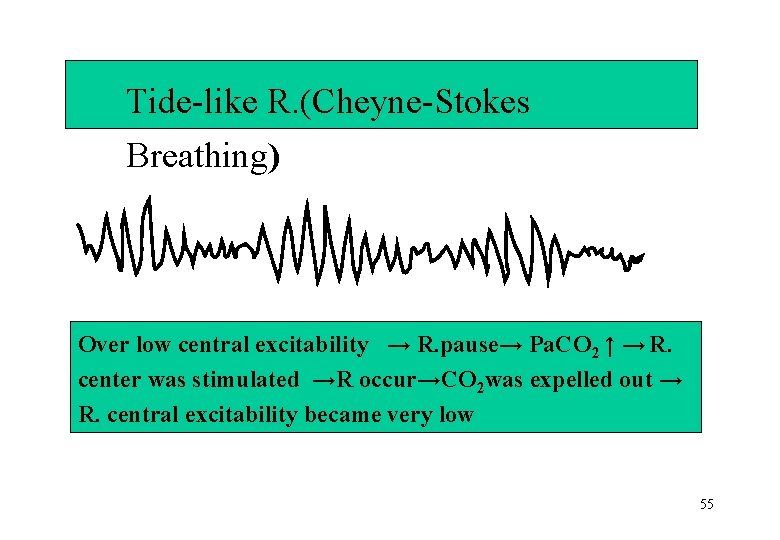
2. Primary disorders of respiratory system 1) pulmonary compliance↓ pulmonary extend reflex juxtapulmonary-capillary receptor rapid light R. 2) obstructive hypoventilation→ins/exp dyspnea 3) respiratory M. fatigue → contractibility of R. M. ↓ → rapid light R. 4) central RF: slow light R. , R. rhythm disturbance e. g. : tide-like R. 54
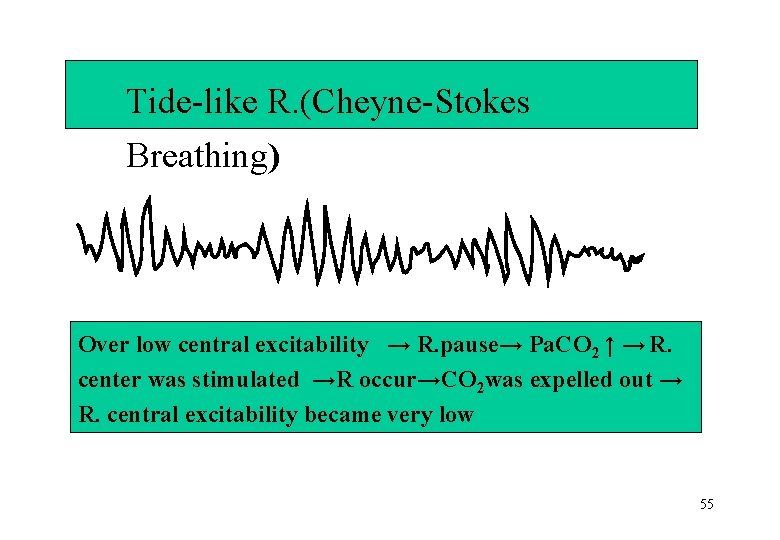
Tide-like R. (Cheyne-Stokes Breathing) Over low central excitability → R. pause→ Pa. CO 2 ↑ → R. center was stimulated →R occur→CO 2 was expelled out → R. central excitability became very low 55
Ⅲ. cardiovascular system mild Pa. O 2 ↓and Pa. CO 2 ↑can excite cardiovascular center Severe Pa. O 2 ↓and Pa. CO 2 ↑can inhibit 56
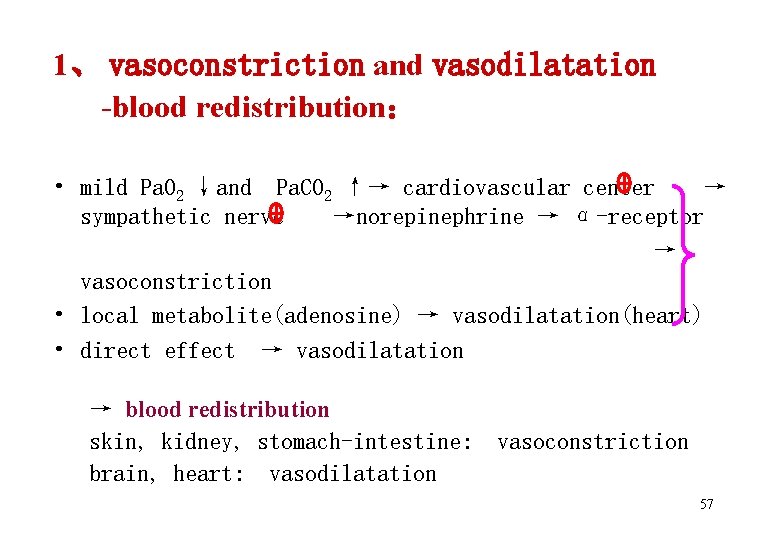
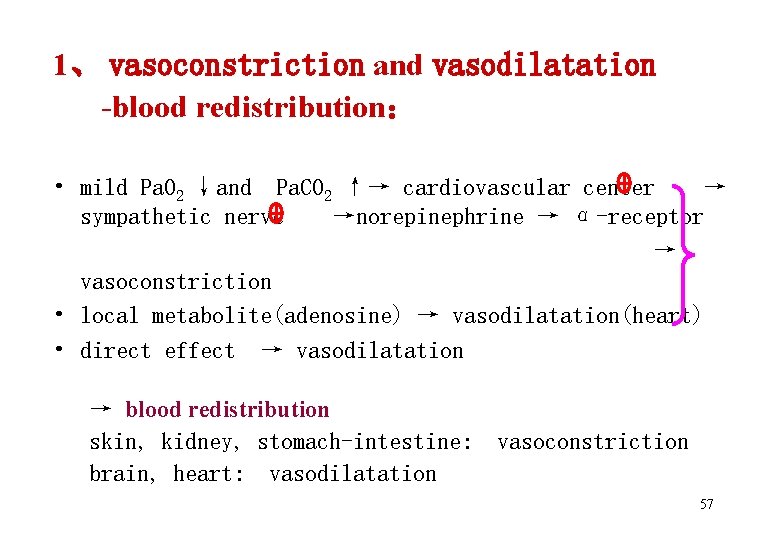
1、 vasoconstriction and vasodilatation -blood redistribution: • mild Pa. O 2 ↓and Pa. CO 2 ↑→ cardiovascular center → sympathetic nerve →norepinephrine → α-receptor → vasoconstriction • local metabolite(adenosine) → vasodilatation(heart) • direct effect → vasodilatation → blood redistribution skin, kidney, stomach-intestine: brain, heart: vasodilatation vasoconstriction 57
2、Heart: mild :heart rate ↑, myocardium contraction force ↑, CO↑ severe: heart rate ↓, myocardium contraction, force ↓, CO↓ , blood pressure↓ right heart failure 58
3. Cor pulmonale • concept: Cor pulmonale is right heart hypertrophy and even failure, which is caused by RF. • Mechanism of Cor pulmonale : 59
1) pulmonary hypertension : • pulmonary arteriole contraction: hypoxemia ,hypercapnia →blood hydrogen ion [H+ ] ↑ →chemoreceptor → pulmonary artery contraction • Pulmonary vessel becomes sclerosis, stegnosis: chronic RF → pulmonary arteriole contracts long-standing and oxygen deficit long-term → pulmonary vessel’s smooth muscle cell and fibroblast become hypertrophy and proliferation. • Some pulmonary disorders effects: pneumonia,pulmonary fibrosis → pulmonary vessel became twist 60
2) cardiac diastole and contraction were confined : intrathoracic pressure ↑; hypoxemia, acidosis 3) resistance of blood flow is increased: Hypoxemia compensation RBC increased →blood became ropiness 61
Ⅳ. CNS 1. Pa. O 2 ↓ : • Pa. O 2 decreased to 60 mm. Hg →intelligence and eyesight slight impairment • Pa. O 2 decreased to below 40~50 mm. Hg →a series symptom of nerve and consciousness. • Pa. O 2 decreased to 20 mm. Hg → nerve cell will become irreversible damaged 62
2. Pa. CO 2 ↑ : Pa. CO 2 is higher than 80 mm. Hg→ carbon dioxide narcosis: headache, dizziness, dysphoria, flapping tremor, mental disorder , drowsiness, hyperspasmia, respiratory depression , coma, even death 63
3. pulmonary encephalopathy: a kind of brain dysfunction caused by RF. Mechanism: 1) brain vessel : • hypoxia→ brain vessel dilation, blood flow↑ →brain congestion • acidosis → blood vessel endothelium(BVE) permeability↑ → brain interstitial tissue edema → intracranial pressure ↑, to oppress brain vessel →ischemia, hypoxia, acidosis became severe 64
2) brain cell: • hypoxia → ATP↓, Na+-K+-ATPase↓→ brain cell edema • acidosis → glutamic acid decarboxylase (GAD ) activity ↑ → GABA↑ • acidosis → phospholipase ↑ → lysosome enzyme release → nerve cell and tissue damage 65
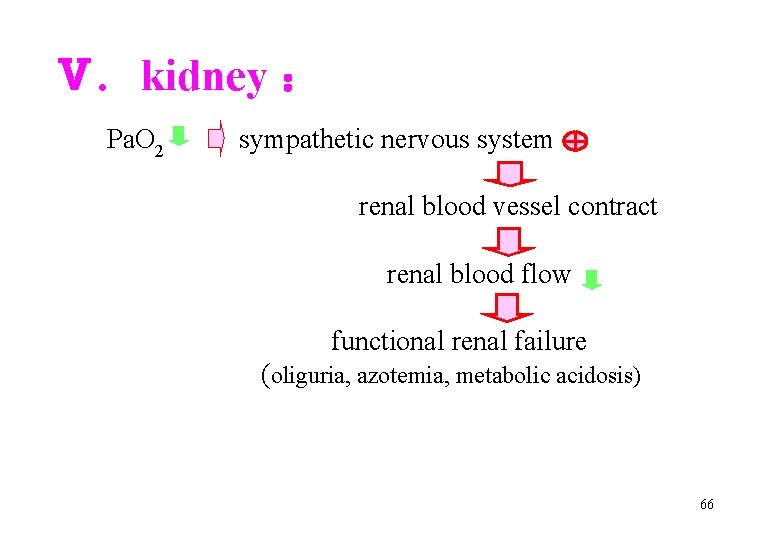
Ⅴ. kidney : Pa. O 2 sympathetic nervous system renal blood vessel contract renal blood flow functional renal failure (oliguria, azotemia, metabolic acidosis) 66
Ⅵ. gastrointestinal tract : hypoxia and acidosis → excitation of sympathetic nerve → gastrointestinal tract wall vessel contraction (large amount of receptor) → ischemia CO 2 retention→↑activity of carbonic anhydrase (CA) in acid cell in stomach →secrete more acid → p. H of gastric juice ↓ → gastrointestinal mucous membrane erosion, necrosis, bleeding ulcer 67
Section 3 Treatment Principle 68
1. Etiology treatment Correcting the cause and relieving the hypoxia and hypercapnia e. g. use of bronchodilators, antibiotics for respiratory infections, establishment of airway (using endotracheal tube ) 69
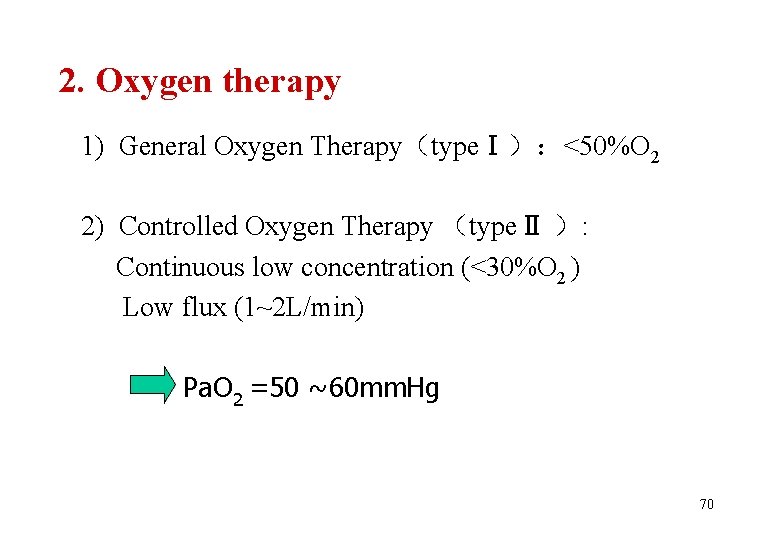
2. Oxygen therapy 1) General Oxygen Therapy(typeⅠ):<50%O 2 2) Controlled Oxygen Therapy (typeⅡ ): Continuous low concentration (<30%O 2 ) Low flux (1~2 L/min) Pa. O 2 =50 ~60 mm. Hg 70
3. To decrease Pa. CO 2 1) To unblock airway 2) To strengthen respiratory driving force 3) Artificial assisted respiration (mechanical ventilator) 4) To add nutrition 4. Treating the consequences of hypoxemia and hypercapnia e. g. acidosis, heart failure. 71
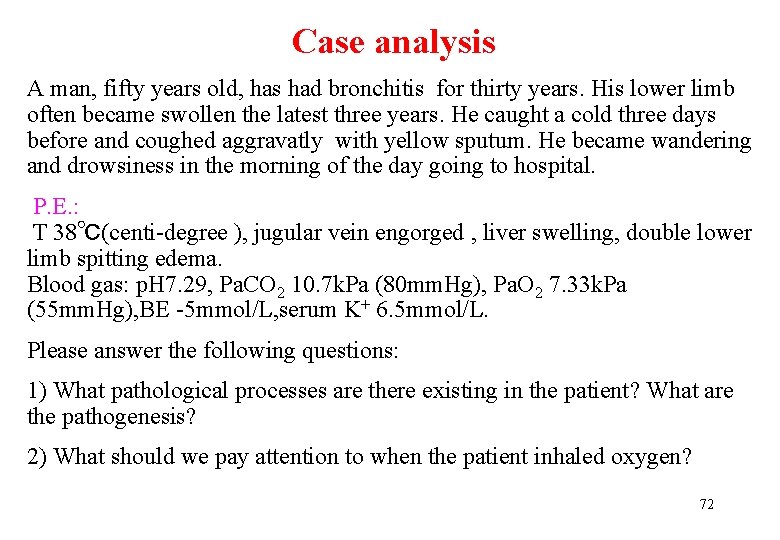
Case analysis A man, fifty years old, has had bronchitis for thirty years. His lower limb often became swollen the latest three years. He caught a cold three days before and coughed aggravatly with yellow sputum. He became wandering and drowsiness in the morning of the day going to hospital. P. E. : T 38℃(centi-degree ), jugular vein engorged , liver swelling, double lower limb spitting edema. Blood gas: p. H 7. 29, Pa. CO 2 10. 7 k. Pa (80 mm. Hg), Pa. O 2 7. 33 k. Pa (55 mm. Hg), BE -5 mmol/L, serum K+ 6. 5 mmol/L. Please answer the following questions: 1) What pathological processes are there existing in the patient? What are the pathogenesis? 2) What should we pay attention to when the patient inhaled oxygen? 72
To grasp Demands 1. the concept and pathogenesis of RF 2. the concept and pathogenesis of Cor pulmonale, and pulmonary encephalopathy To be familiar with 1. The functional and metabolic changes in RF 2. principle of inhaling Oxygen for type II RF To learn Treatment Principle of RF 73
 Xiaoming gao
Xiaoming gao Failure to sense
Failure to sense Failure to capture vs failure to sense
Failure to capture vs failure to sense Brittle failure vs ductile failure
Brittle failure vs ductile failure Primary ciliary dyskinesia
Primary ciliary dyskinesia Types of respiratory failure
Types of respiratory failure Pink puffer
Pink puffer Nursing management of dyspnea ppt
Nursing management of dyspnea ppt Patm disease
Patm disease Type 1 respiratory failure
Type 1 respiratory failure Conducting zone and respiratory zone
Conducting zone and respiratory zone Albany county dept of social services
Albany county dept of social services Nebraska dept of agriculture
Nebraska dept of agriculture Dept of education
Dept of education Gome dept
Gome dept Dept. name of organization
Dept. name of organization La dept of revenue
La dept of revenue Dept a
Dept a Dept of education
Dept of education Gome dept
Gome dept Dept. name of organization
Dept. name of organization Florida department of agriculture and consumer services
Florida department of agriculture and consumer services Ee dept iitb
Ee dept iitb Bromocicloesano
Bromocicloesano Hoe dept
Hoe dept Ohio dept of developmental disabilities
Ohio dept of developmental disabilities Geaux biz login
Geaux biz login Central islip fire dept
Central islip fire dept Gome dept
Gome dept Mn dept of education
Mn dept of education Finance department organizational chart
Finance department organizational chart Dept ind onegov
Dept ind onegov Pt dept logistik
Pt dept logistik Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Fire dept interview questions
Fire dept interview questions Poster affiliation
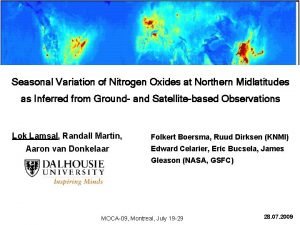
Poster affiliation Continuing education library oxford
Continuing education library oxford Rowan county dss
Rowan county dss Horizontal
Horizontal Dept of finance and administration
Dept of finance and administration Worcester building department
Worcester building department Nys dept of homeland security
Nys dept of homeland security Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Oviposition
Oviposition Vaginal dept
Vaginal dept Dept nmr spectroscopy
Dept nmr spectroscopy Pain pathophysiology
Pain pathophysiology Co2 narcosis
Co2 narcosis 3392chest
3392chest Aplastic anemia lab findings
Aplastic anemia lab findings Egfr calculation formula
Egfr calculation formula Uterine bleeding
Uterine bleeding Shock
Shock Nursing management of pancreatitis
Nursing management of pancreatitis Pathophysiology of asthm
Pathophysiology of asthm Stent graft
Stent graft Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Pathogenesis of cholecystitis
Pathogenesis of cholecystitis Site:slidetodoc.com
Site:slidetodoc.com Magic box respiratory
Magic box respiratory Tonsillitis pathophysiology
Tonsillitis pathophysiology Joffroys sign
Joffroys sign Case mysteries in pathophysiology (doc or html) file
Case mysteries in pathophysiology (doc or html) file Centriacinar
Centriacinar Reactive arthritis pathophysiology
Reactive arthritis pathophysiology Primary complex
Primary complex Acute dystonia pathophysiology
Acute dystonia pathophysiology Cholecystitis pathophysiology
Cholecystitis pathophysiology Pathophysiology of cholelithiasis ppt
Pathophysiology of cholelithiasis ppt Hellp syndrome pathophysiology
Hellp syndrome pathophysiology Tanda ruptur bulbi
Tanda ruptur bulbi Angina pathophysiology
Angina pathophysiology Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Pathophysiology of migraine
Pathophysiology of migraine