Renal Pathology Review Medical Diseases of the Kidney











- Slides: 44
Renal Pathology Review Medical Diseases of the Kidney Karlene Hewan-Lowe, MD Brody School of Medicine at East Carolina University
Renal Pathology The Osler Institute Review Course Normal Histology

Renal Pathology The Osler Institute Review Course Histology Normal Glomerulus • Anastamosing capillary network Architecture is defined with H and E, PAS and Methenamine silver stains • Glomerular capillary wall Fenestrated endothelial cell Glomerular Basement membrane 260 – 340 nm Visceral epithelial cell (Podocyte) • Mesangium Mesangial cells Mesangial matrix
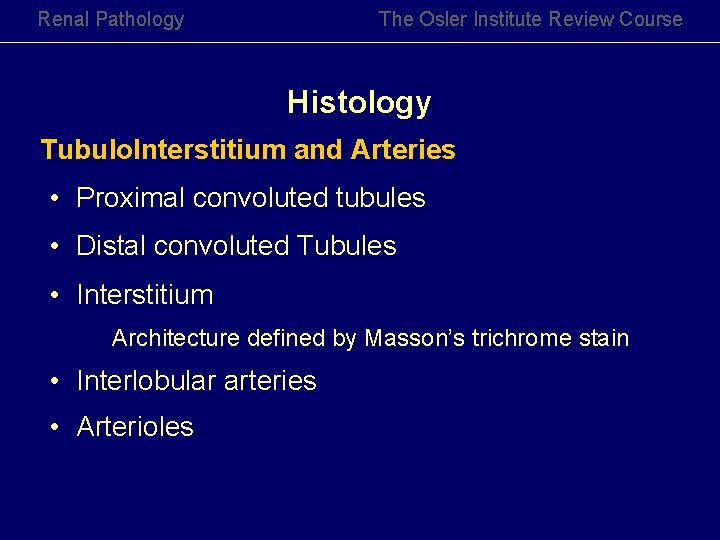
Renal Pathology The Osler Institute Review Course Histology Tubulo. Interstitium and Arteries • Proximal convoluted tubules • Distal convoluted Tubules • Interstitium Architecture defined by Masson’s trichrome stain • Interlobular arteries • Arterioles
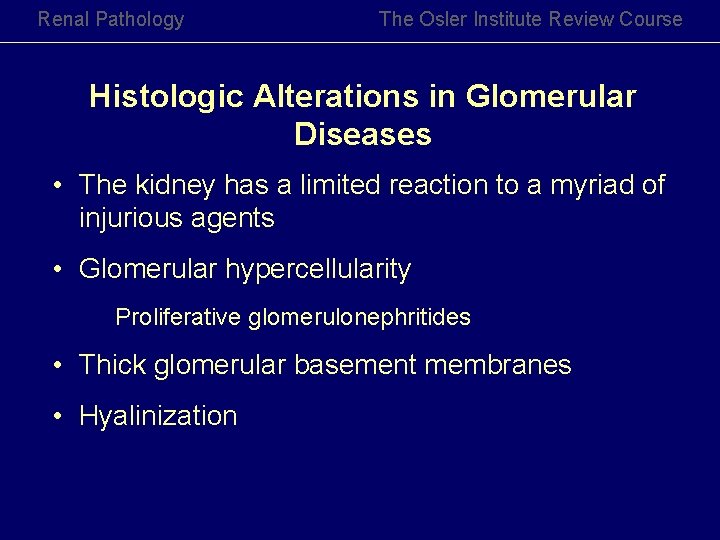
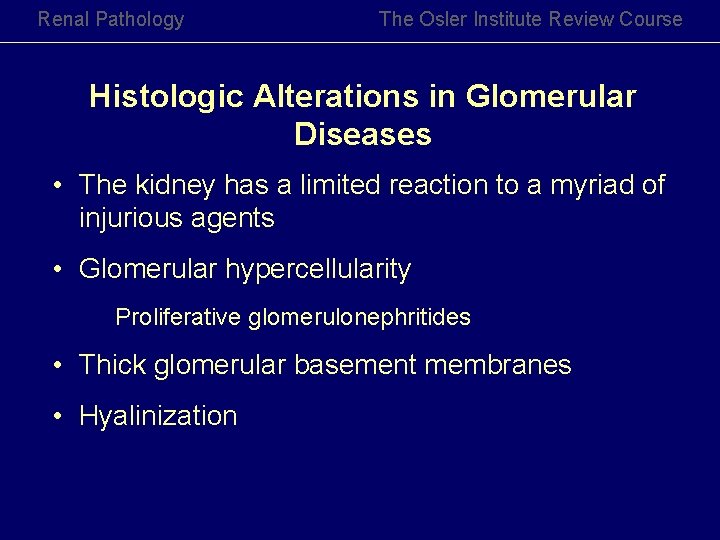
Renal Pathology The Osler Institute Review Course Histologic Alterations in Glomerular Diseases • The kidney has a limited reaction to a myriad of injurious agents • Glomerular hypercellularity Proliferative glomerulonephritides • Thick glomerular basement membranes • Hyalinization

Renal Pathology The Osler Institute Review Course Terms Used in the Evaluation of Glomerular Diseases • Diffuse glomerular changes > 50% • Focal glomerular changes < 50% • Global involvement – single glomerulus • Segmental involvement – single glomerulus
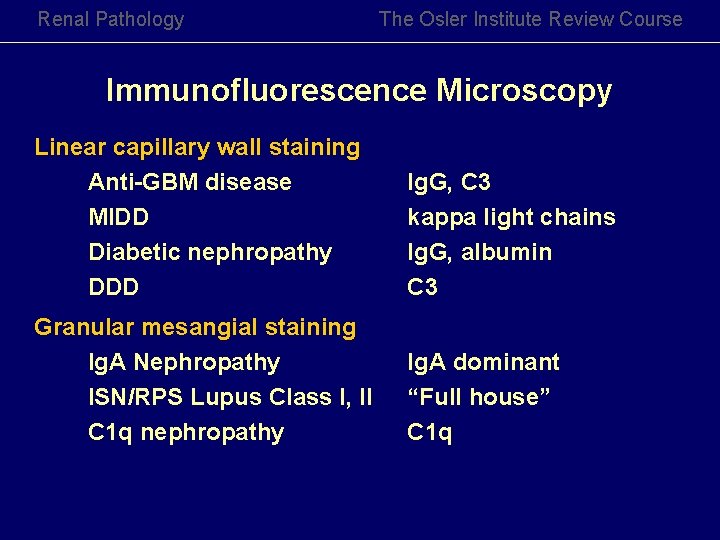
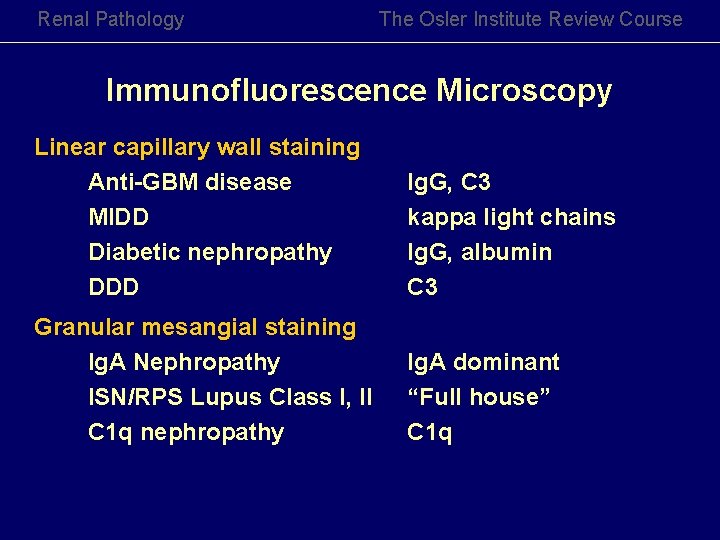
Renal Pathology The Osler Institute Review Course Immunofluorescence Microscopy Linear capillary wall staining Anti-GBM disease MIDD Diabetic nephropathy DDD Ig. G, C 3 kappa light chains Ig. G, albumin C 3 Granular mesangial staining Ig. A Nephropathy ISN/RPS Lupus Class I, II C 1 q nephropathy Ig. A dominant “Full house” C 1 q

Renal Pathology The Osler Institute Review Course Immunofluorescence Microscopy Granular mesangial and capillary wall staining Membranous GN Ig. G, C 3 MPGN C 3 WHO Lupus III, IV Full house Post infectious GN Diffuse smudgy mesangial and capillary wall staining Amyloidosis lambda light chains Fibrillary GN Ig. G, C 3, kappa > lambda MIDD kappa light chains

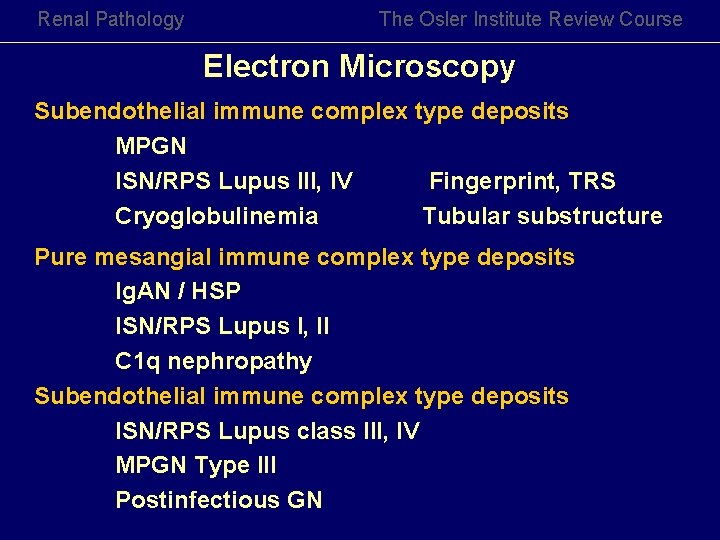
Renal Pathology The Osler Institute Review Course Electron Microscopy Subepithelial immune complex type dense deposits Membranous GN Stage I - IV MPGN WHO Lupus IV Post infectious GN “Humps” Intramembranous (often with mesangial) immune complex type deposits Dense deposit Disease
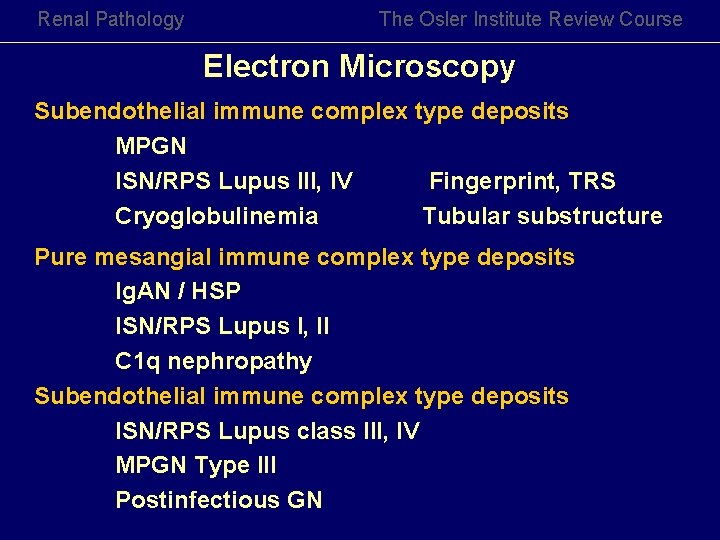
Renal Pathology The Osler Institute Review Course Electron Microscopy Subendothelial immune complex type deposits MPGN ISN/RPS Lupus III, IV Fingerprint, TRS Cryoglobulinemia Tubular substructure Pure mesangial immune complex type deposits Ig. AN / HSP ISN/RPS Lupus I, II C 1 q nephropathy Subendothelial immune complex type deposits ISN/RPS Lupus class III, IV MPGN Type III Postinfectious GN

Renal Pathology The Osler Institute Review Course Clinical Patterns of Glomerular Disease
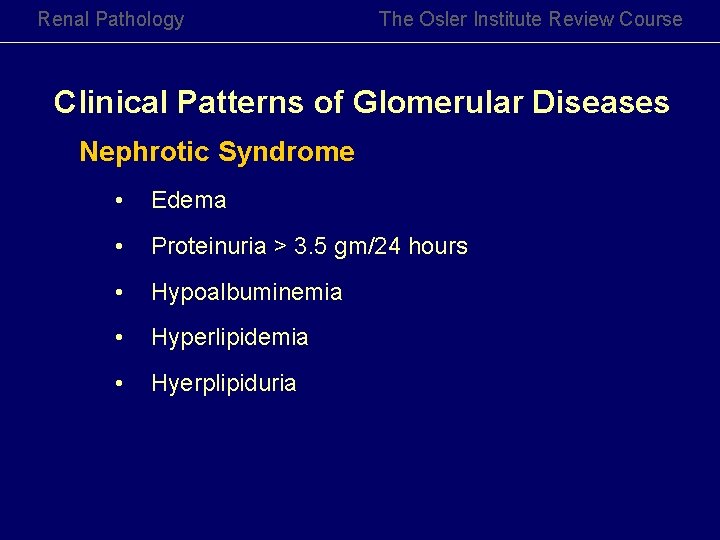
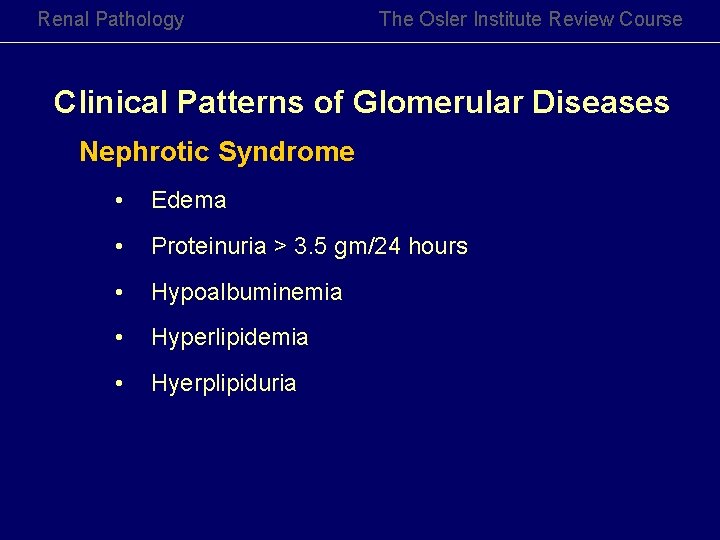
Renal Pathology The Osler Institute Review Course Clinical Patterns of Glomerular Diseases Nephrotic Syndrome • Edema • Proteinuria > 3. 5 gm/24 hours • Hypoalbuminemia • Hyperlipidemia • Hyerplipiduria
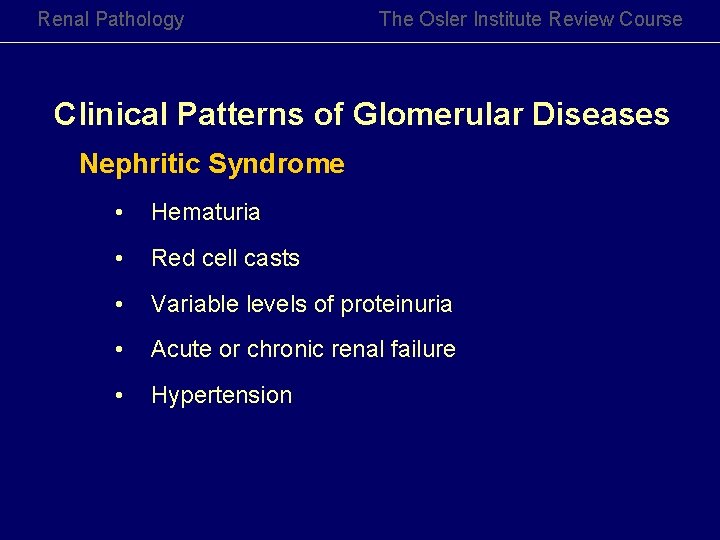
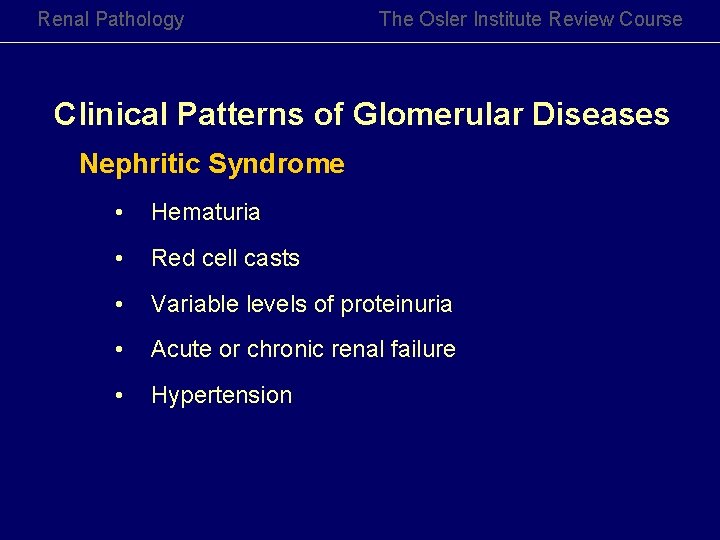
Renal Pathology The Osler Institute Review Course Clinical Patterns of Glomerular Diseases Nephritic Syndrome • Hematuria • Red cell casts • Variable levels of proteinuria • Acute or chronic renal failure • Hypertension
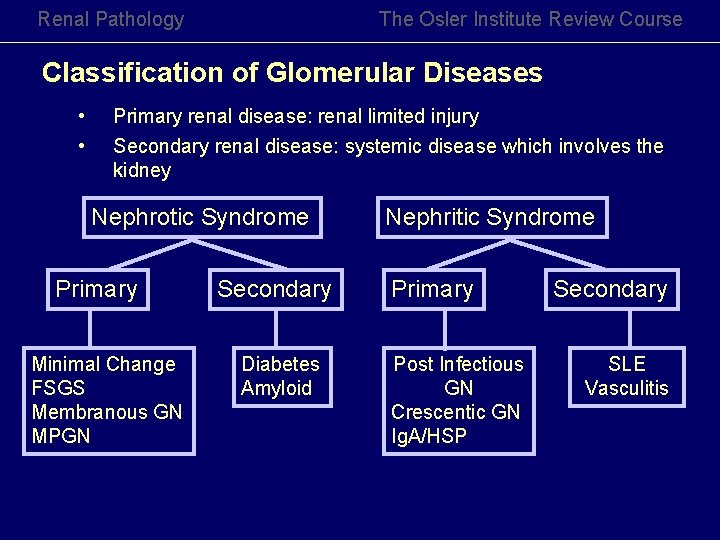
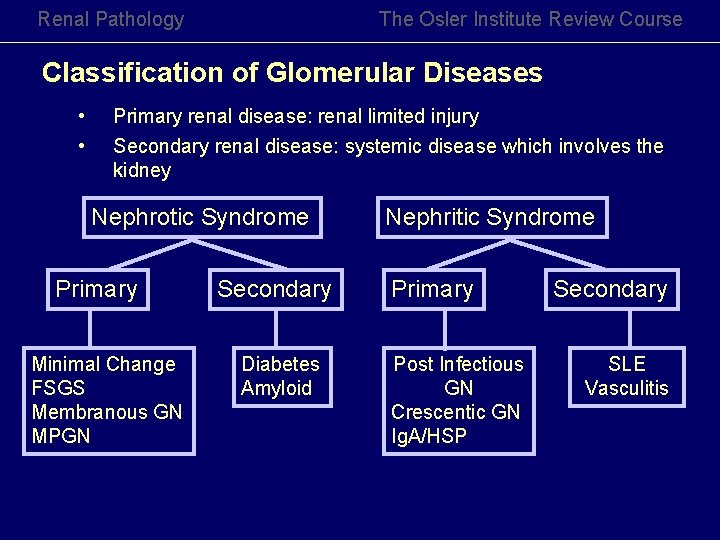
Renal Pathology The Osler Institute Review Course Classification of Glomerular Diseases • • Primary renal disease: renal limited injury Secondary renal disease: systemic disease which involves the kidney Nephrotic Syndrome Primary Minimal Change FSGS Membranous GN MPGN Secondary Diabetes Amyloid Nephritic Syndrome Primary Post Infectious GN Crescentic GN Ig. A/HSP Secondary SLE Vasculitis
Renal Pathology The Osler Institute Review Course Nephrotic Syndrome
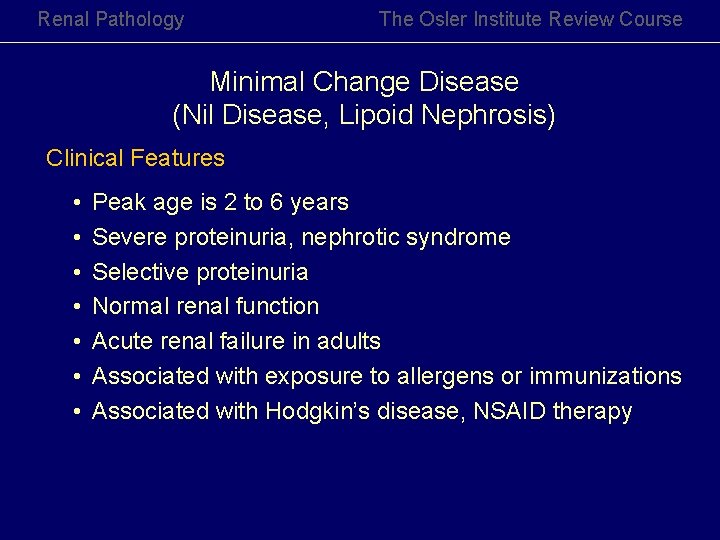
Renal Pathology The Osler Institute Review Course Minimal Change Disease (Nil Disease, Lipoid Nephrosis) Clinical Features • • Peak age is 2 to 6 years Severe proteinuria, nephrotic syndrome Selective proteinuria Normal renal function Acute renal failure in adults Associated with exposure to allergens or immunizations Associated with Hodgkin’s disease, NSAID therapy

Renal Pathology The Osler Institute Review Course Minimal Change Disease (Nil Disease, Lipoid Nephrosis) Pathogenesis • • Immune disorder Circulating permeability factors Loss of fixed, GCW polyanionic charge Decreased and altered distribution of nephrin in podocytes
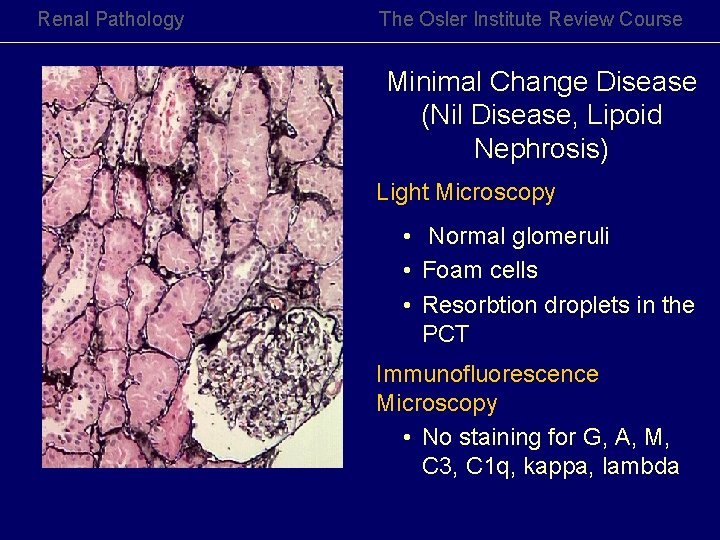
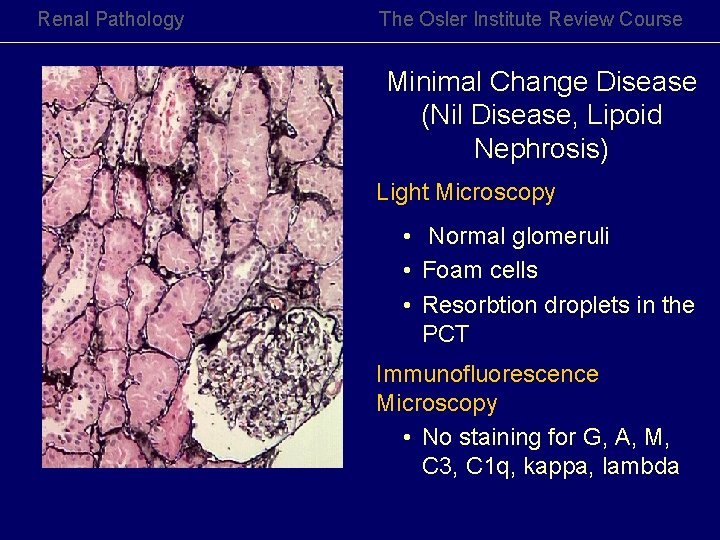
Renal Pathology The Osler Institute Review Course Minimal Change Disease (Nil Disease, Lipoid Nephrosis) Light Microscopy • Normal glomeruli • Foam cells • Resorbtion droplets in the PCT Immunofluorescence Microscopy • No staining for G, A, M, C 3, C 1 q, kappa, lambda

Renal Pathology The Osler Institute Review Course Minimal Change Disease Electron Microscopy • Foot process effacement and microvillous transformation Prognosis • Remission in 8 weeks with steroid therapy • No tendency to progress to chronic renal disease

Renal Pathology The Osler Institute Review Course Focal Segmental Glomerulosclerosis Clinical Features • • • Heavy, non selective proteinuria Nephrotic Syndrome Microhematuria Hypertension Idiopathic FSGS Secondary FSGS HIVAN Heroin abuse Morbid obesity Unilateral renal agenesis Vesicoureteral reflux
Renal Pathology The Osler Institute Review Course Focal Segmental Glomerulosclerosis Pathogenesis of FSGS • • • Hyperfiltration/hyperperfusion injury Circulating permeability factor Most cases are sporadic Few cases are associated with genetic abnormalities Viral infections - HIV, parvovirus B 19
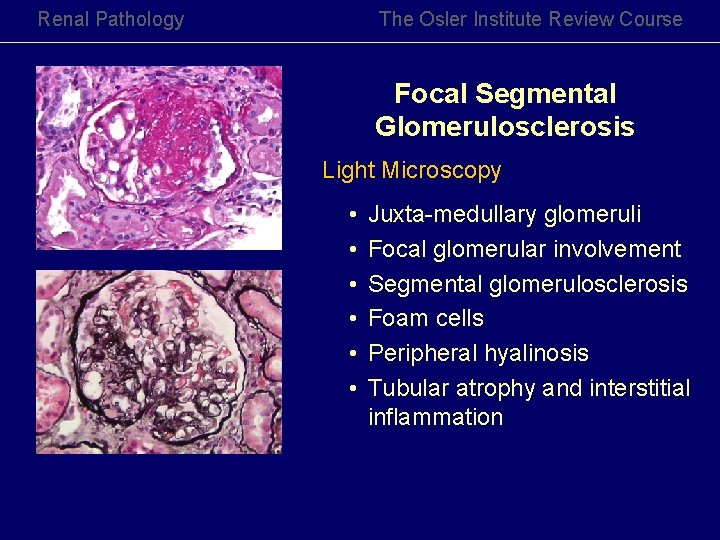
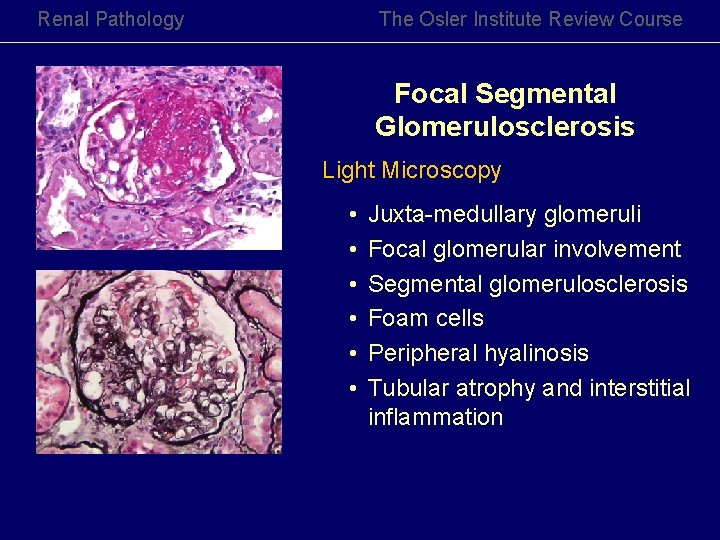
Renal Pathology The Osler Institute Review Course Focal Segmental Glomerulosclerosis Light Microscopy • • • Juxta-medullary glomeruli Focal glomerular involvement Segmental glomerulosclerosis Foam cells Peripheral hyalinosis Tubular atrophy and interstitial inflammation
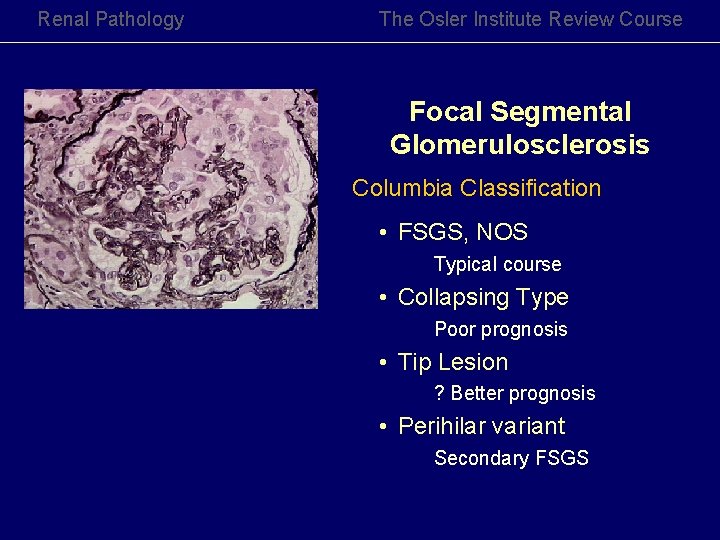
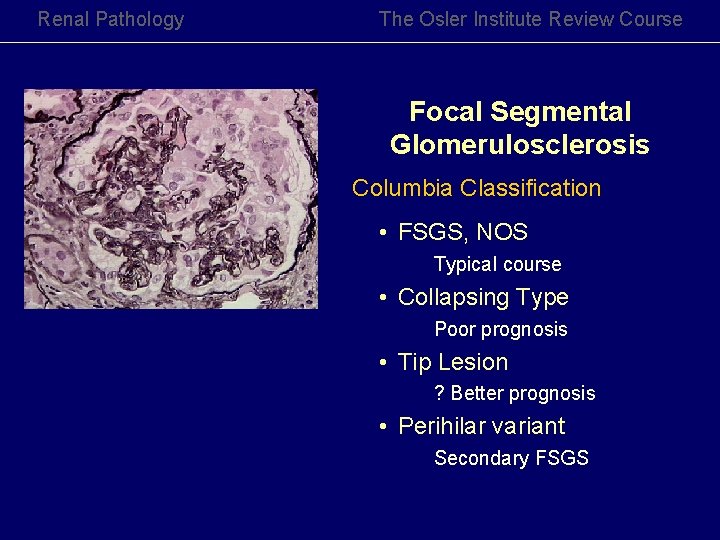
Renal Pathology The Osler Institute Review Course Focal Segmental Glomerulosclerosis Columbia Classification • FSGS, NOS Typical course • Collapsing Type Poor prognosis • Tip Lesion ? Better prognosis • Perihilar variant Secondary FSGS
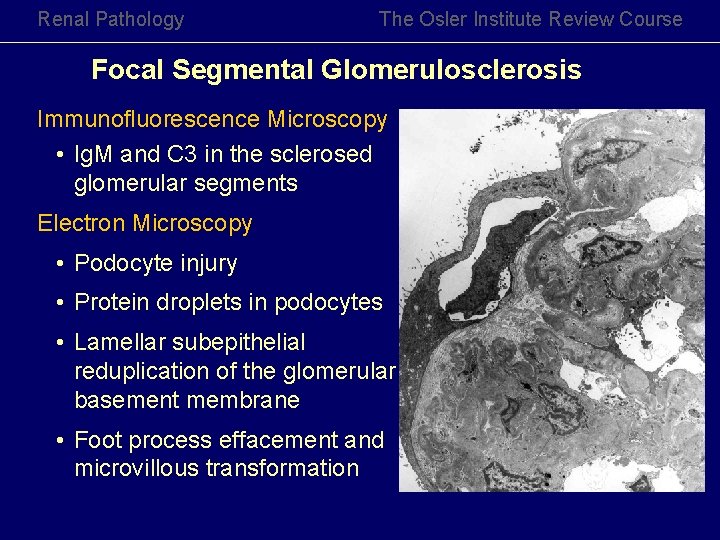
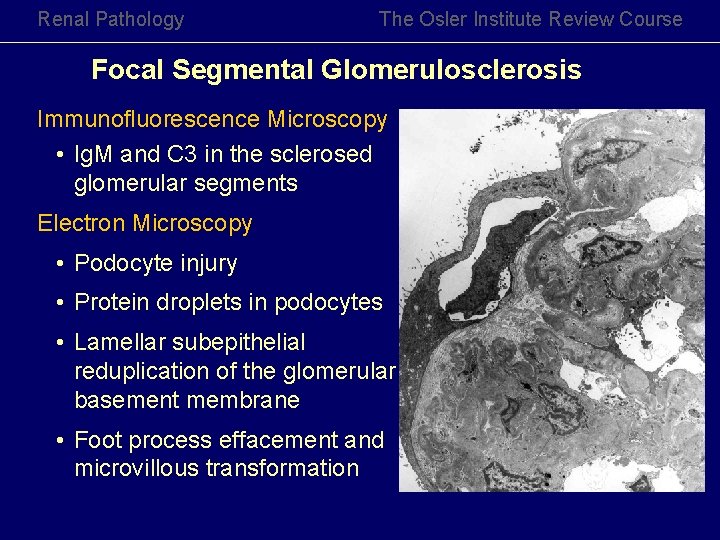
Renal Pathology The Osler Institute Review Course Focal Segmental Glomerulosclerosis Immunofluorescence Microscopy • Ig. M and C 3 in the sclerosed glomerular segments Electron Microscopy • Podocyte injury • Protein droplets in podocytes • Lamellar subepithelial reduplication of the glomerular basement membrane • Foot process effacement and microvillous transformation
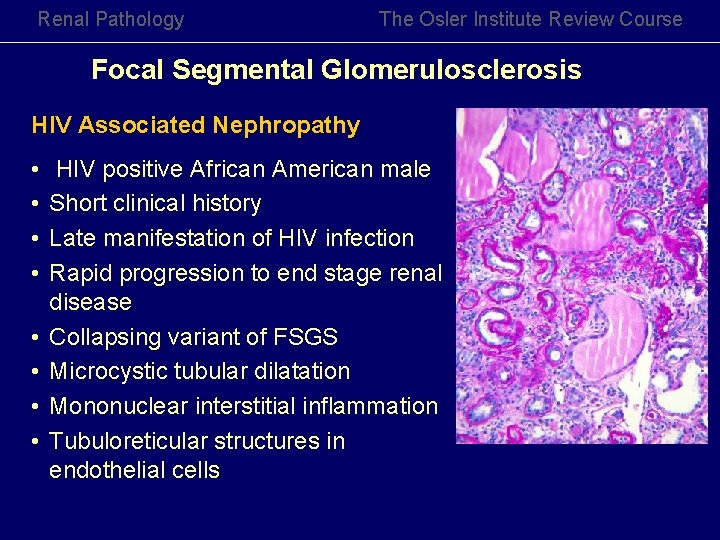
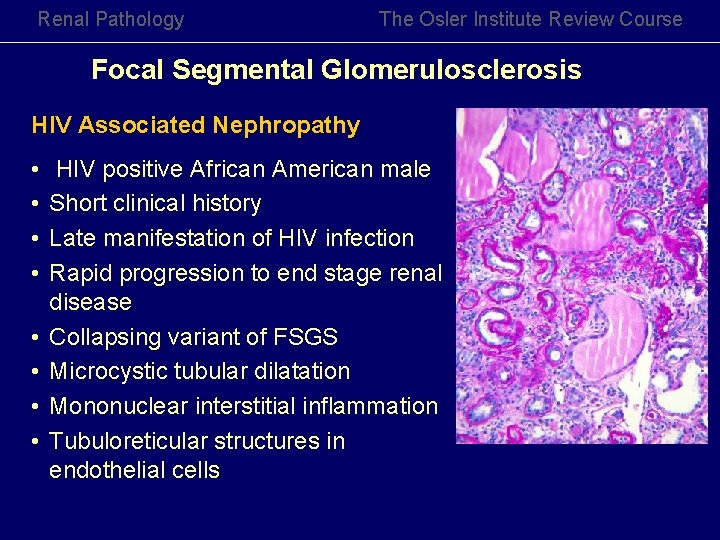
Renal Pathology The Osler Institute Review Course Focal Segmental Glomerulosclerosis HIV Associated Nephropathy • • HIV positive African American male Short clinical history Late manifestation of HIV infection Rapid progression to end stage renal disease Collapsing variant of FSGS Microcystic tubular dilatation Mononuclear interstitial inflammation Tubuloreticular structures in endothelial cells
Renal Pathology The Osler Institute Review Course Membranous Glomerulonephritis Clinical Features • Most common cause of nephrotic syndrome in non-diabetic adults • Insidiuous onset of heavy proteinuria • Most common de novo glomerulonephritis in renal allografts
Renal Pathology The Osler Institute Review Course Membranous Glomerulonephritis Secondary MGN Infection Hepatitis B, Hepatitis C, Syphilis, Parastic disease Drugs Mercury, Gold, penicillamine, NSAID, Catopril, formaldehye Neoplasms Renal carcinoma, lung, stomach, breast, Hematolymphoid neoplasms, pancreas, melanoma, seminoma Autoimmune Disease SLE, pemphigoid, MCTD, thyroiditis Others Diabetes, renal vein thrombosis, Sjogren’s, sarcoid, cryoglobulinemia, SCD
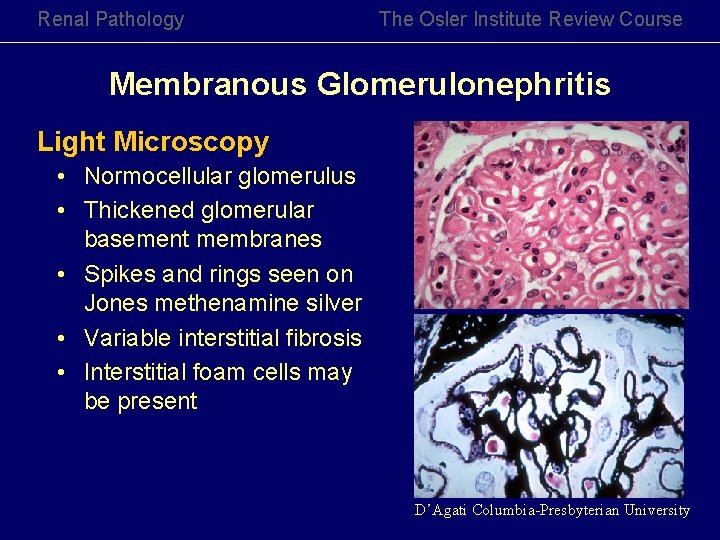
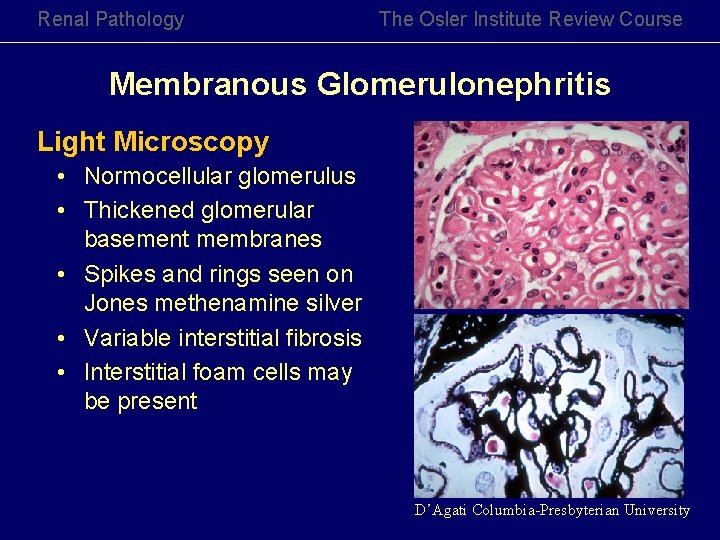
Renal Pathology The Osler Institute Review Course Membranous Glomerulonephritis Light Microscopy • Normocellular glomerulus • Thickened glomerular basement membranes • Spikes and rings seen on Jones methenamine silver • Variable interstitial fibrosis • Interstitial foam cells may be present D’Agati Columbia-Presbyterian University
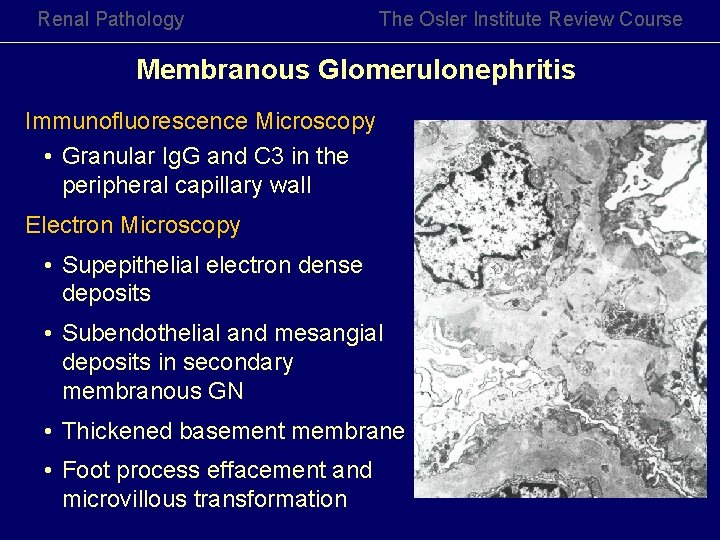
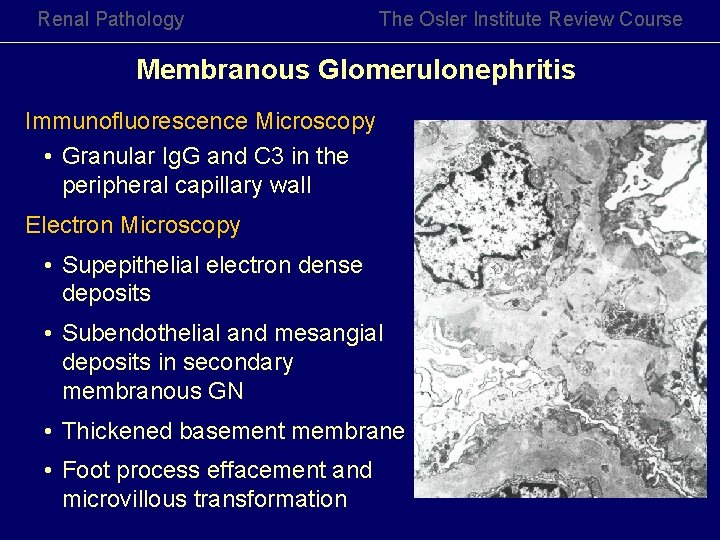
Renal Pathology The Osler Institute Review Course Membranous Glomerulonephritis Immunofluorescence Microscopy • Granular Ig. G and C 3 in the peripheral capillary wall Electron Microscopy • Supepithelial electron dense deposits • Subendothelial and mesangial deposits in secondary membranous GN • Thickened basement membrane • Foot process effacement and microvillous transformation

Renal Pathology The Osler Institute Review Course Membranous Glomerulonephritis Ehrenreich and Churg - Morphologic Classification • Stage I Subepithelial electron dense deposits, normal GBM • Stage II Subepithelial electron dense deposits surrounded by cup-like extensions of the glomerular basement membranes • Stage III Subepithelial deposits, variable electron density, neomembranes are present on the surface of the deposit • Stage IV Irregularly thickened GBM and no deposits
Renal Pathology The Osler Institute Review Course Membranous Glomerulonephritis Prognosis • Slow deterioration to renal failure • Corticosteroids and cytotoxic agents may be beneficial in idiopathic membranous GN • Secondary membranous GN may regress
Renal Pathology The Osler Institute Review Course Membranoproliferative GN Type I Clinical Features • • • More common in children Uncommon in adults > 60 years of age Prodrome of an upper respiratory infection Hypertension Proteinuria - always present, moderate to heavy , poorly selective Hematuria - macroscopic hematuria is uncommon Nephritic Syndrome Nephrotic Syndrome Altered renal function - decrease GFR, Elevated BUN, Creatinine Hypocomplimentemia Circulating immune complexes (20%)

Renal Pathology The Osler Institute Review Course Membranoproliferative GN Type I Glomeruli Enlarged, hypercellular tuft Lobular accentuation Infiltrating monocytes and neutrophils Crescents (2 - 10%) Thick peripheral glomerular membranes Silver stain - Double contours Tubules Hyaline (protein and lipid) droplets in tubular epithelium Tubular atrophy Interstitium Interstitial fibrosis, foam cells Iflammatory cells Vessels Arteriosclerosis Vasculitis (Cryoglobulinemia)
Renal Pathology The Osler Institute Review Course MPGN Type II – Dense Deposit Disease Clinical Features • • • Children and young adults URI prodrome in ~50% of patients Proteinuria with hematuria Nephrotic syndrome is the most common presentation Acute nephritic syndrome (16 – 38%) Partial lipodystrophy C 3 – low, fluctuating, normal C 1 q, C 4 – normal C 3 Ne. F - Ig. G autoantibody against complement inhibitory proteins • Factor B, Properdin – low
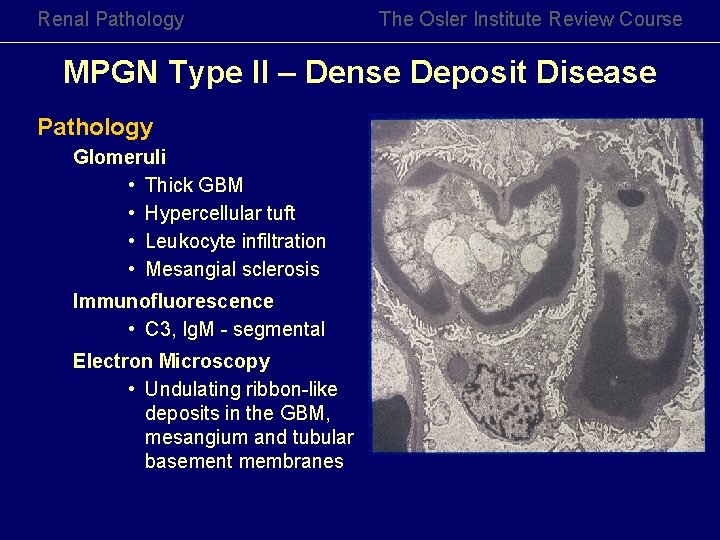
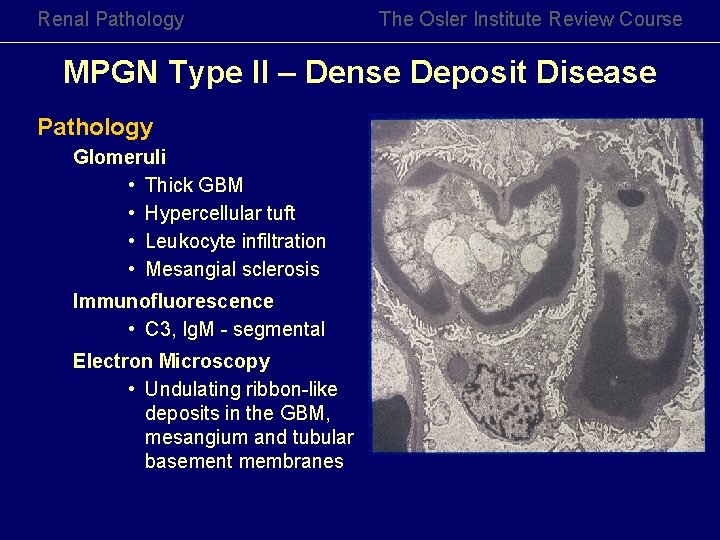
Renal Pathology The Osler Institute Review Course MPGN Type II – Dense Deposit Disease Pathology Glomeruli • Thick GBM • Hypercellular tuft • Leukocyte infiltration • Mesangial sclerosis Immunofluorescence • C 3, Ig. M - segmental Electron Microscopy • Undulating ribbon-like deposits in the GBM, mesangium and tubular basement membranes
Renal Pathology The Osler Institute Review Course Membranoproliferative GN Prognosis • Uniformly poor • Prognosis for Type II is generally worse than Type I • Response to alpha interferon - MPGN associated with Hepatitis C • Type II MPGN has 90% recurrence rate in allograft kidney
Renal Pathology The Osler Institute Review Course Glomerular Diseases with a Membranoproliferative Pattern • • Diabetic glomerulosclerosis Cryoglobulinemic Glomerulonephritis Systemic Lupus nephritis (WHO Class IV) Fibrillary glomerulonephritis Hepatitis viral infection Chronic liver disease Light chain deposition disease Lecithin-cholesterol acyltransferase deficiency
Renal Pathology The Osler Institute Review Course Diabetic Nephropathy Clinical Features • Ten year or more history of diabetes mellitus • Microalbuminuria is an early clinical feature • Type I diabetes mellitus has good correlation between renal disease and severity of fundoscopic findings • Hypertension is common
Renal Pathology The Osler Institute Review Course Diabetic Nephropathy Etiology and Pathogenesis • Irreversible glycosylation of the glomerular basement membranes • Growth factors • Genetic susceptibility • Glomerular hyperperfusion or hyperfiltation injury
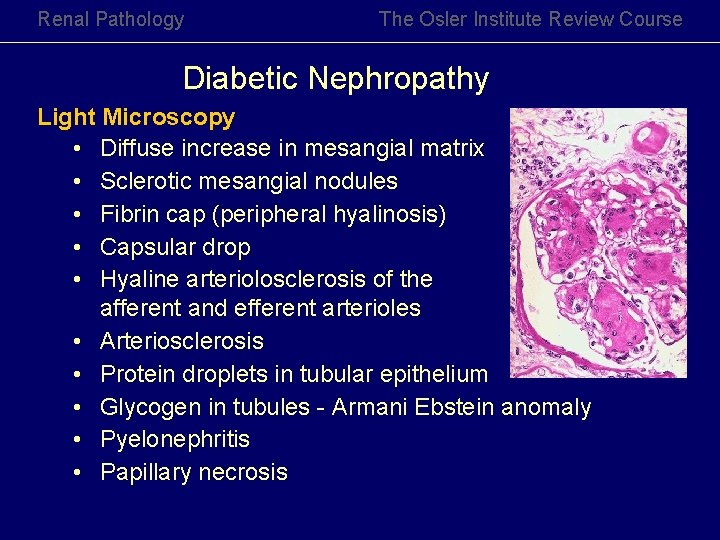
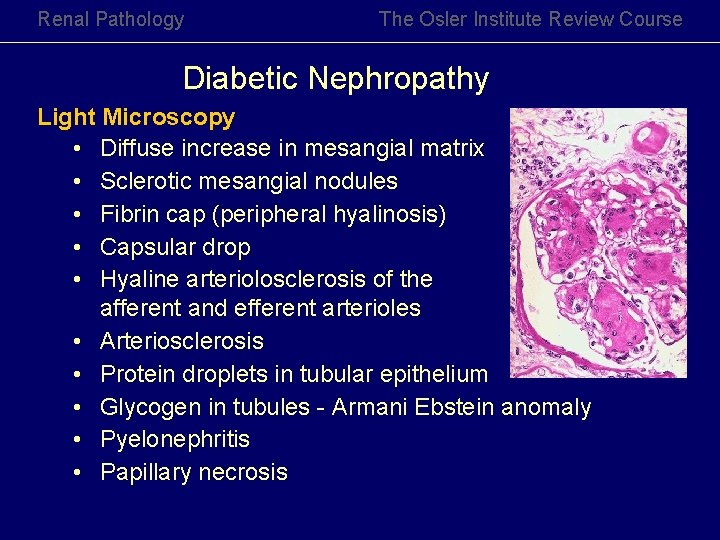
Renal Pathology The Osler Institute Review Course Diabetic Nephropathy Light Microscopy • Diffuse increase in mesangial matrix • Sclerotic mesangial nodules • Fibrin cap (peripheral hyalinosis) • Capsular drop • Hyaline arteriolosclerosis of the afferent and efferent arterioles • Arteriosclerosis • Protein droplets in tubular epithelium • Glycogen in tubules - Armani Ebstein anomaly • Pyelonephritis • Papillary necrosis
Renal Pathology The Osler Institute Review Course Diabetic Nephropathy Immunofluorescence Microscopy • Ig. G - low intensity linear accentuation of the glomerular basement membrane • Albumin - low intensity linear accentuation of the glomerular basement membrane • Ig. M and C 3 in sclerosed glomerular segments Electron Microscopy • Podocytes show foot process effacement • Uniformly thick glomerular basement membrane • Expanded mesangial matrix
Renal Pathology The Osler Institute Review Course Diabetic Nephropathy Prognosis • Progression to end stage renal failure ranges from 3 to 20 years • Renal failure 40% of Type I diabetics 20% Type II diabetics • Recurs in allograft kidney • Control of hyperglycemia and hypertension delays the progression of diabetic nephropathy
Renal Pathology The Osler Institute Review Course Amyloidosis Clinical Features • AL Type amyloid - Plasma cell dyscrasia Most common is AL monoclonal light chain, l > k Overt myeloma is present in 10 – 20% • AA Type amyloid - Chronic inflammatory diseases Osteomyelitis, TB, leprosy, rheumatoid arthritis • Neoplasms - Renal cell carcinoma • Familial Mediterranean Fever • Severe proteinuria • Nephrotic syndrome

Renal Pathology The Osler Institute Review Course Amyloidosis Light Microscopy • Smudgy, homogenous deposits in glomeruli, tubular basement membranes, peritubular capillaries and blood vessels • Deposits are weakly PAS positive and silver negative • Detection: Congo Red, antibody to AA, Thioflavine T
 Res extra commercium
Res extra commercium Ira pré renal renal e pós renal
Ira pré renal renal e pós renal Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Tronsmo plant pathology and plant diseases download
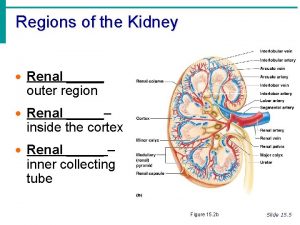
Tronsmo plant pathology and plant diseases download Inside a kidney the ureter expands as a renal pyramid
Inside a kidney the ureter expands as a renal pyramid Acute tubular necrosis
Acute tubular necrosis Distinguish between renal corpuscle and renal tubule
Distinguish between renal corpuscle and renal tubule Ajkd atlas
Ajkd atlas Ajkd atlas of renal pathology
Ajkd atlas of renal pathology Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases Milady chapter 10 review questions
Milady chapter 10 review questions Megalocephalitis prefix root and suffix
Megalocephalitis prefix root and suffix Pathology lectures for medical students
Pathology lectures for medical students Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Tư thế worms-breton
Tư thế worms-breton Chúa yêu trần thế
Chúa yêu trần thế Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Giọng cùng tên là
Giọng cùng tên là Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là