Radiation Therapy for Treatment of Prostate Cancer Stephen



- Slides: 70
Radiation Therapy for Treatment of Prostate Cancer Stephen Ko, M. D. Mayo Clinic Florida August 30, 2010
Overview I. U. S. Epidemiology II. Types of Radiation III. Anatomy IV. Technologic Advances – 2 -Dimensional Planning – Intensity Modulated Radiotherapy – Brachytherapy V. Definition of Risk Categories – Low Risk – Intermediate Risk – High Risk
Overview VI. Dose-escalation Trials – – MSKCC IMRT Dose Escalation Proton Beam Dose Escalation MDACC Randomized Trial (70 Gy vs. 78 Gy) Harvard Randomized Trial (70. 2 Gy. E vs. 79. 2 Gy. E) VII. Low Risk Disease Treatment – IMRT alone – Seeds alone VIII. Intermediate Risk Disease Treatment – IMRT alone – 6 mo Hormone + EBRT – Seeds + EBRT
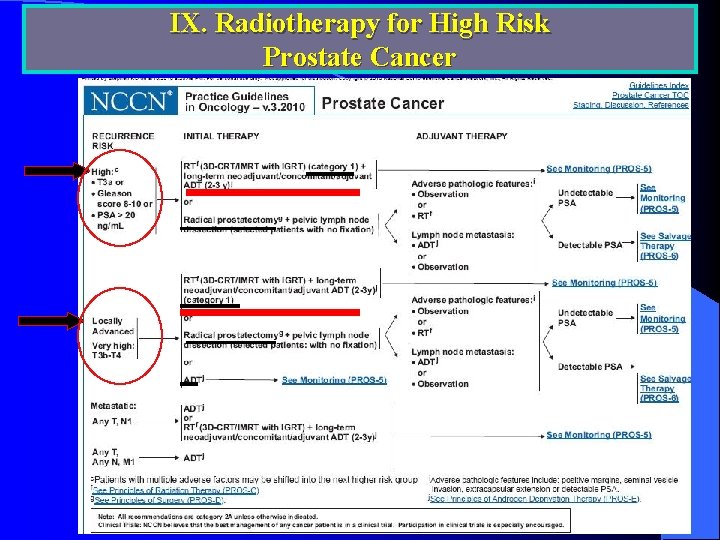
Overview l IX. High Risk Disease Treatment – Long-term Hormonal therapy Randomized Trials l l RTOG randomized Trial EORTC randomized Trial – Seeds + EBRT X. Comparing Modalities (Surgery vs. Radiation) l XI. Quality of Life Comparison l XII. Conclusions l
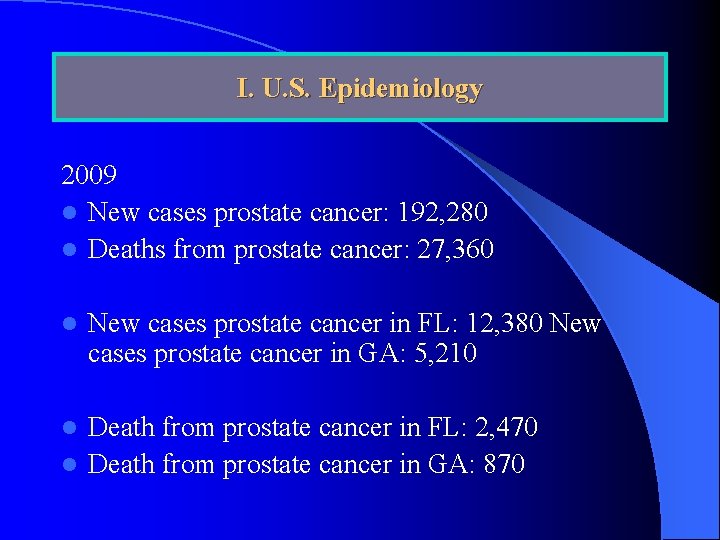
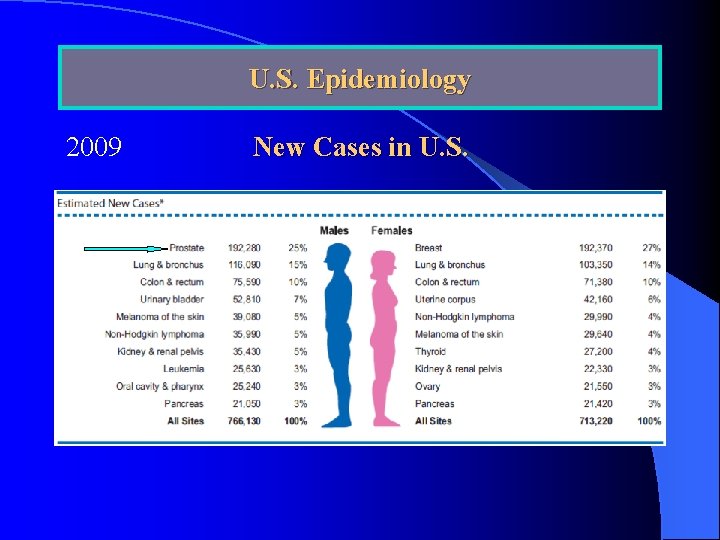
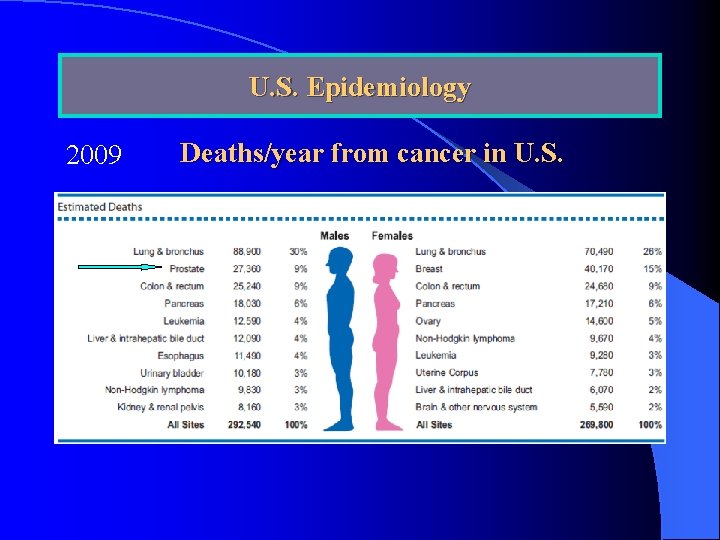
I. U. S. Epidemiology 2009 l New cases prostate cancer: 192, 280 l Deaths from prostate cancer: 27, 360 l New cases prostate cancer in FL: 12, 380 New cases prostate cancer in GA: 5, 210 Death from prostate cancer in FL: 2, 470 l Death from prostate cancer in GA: 870 l
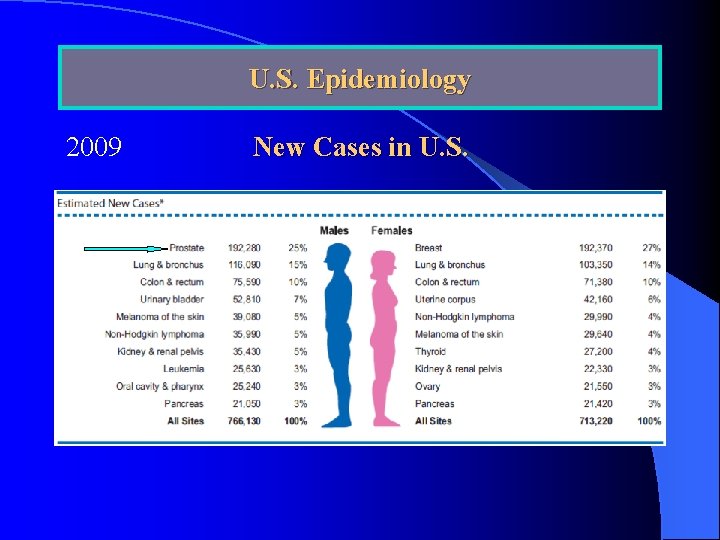
U. S. Epidemiology 2009 New Cases in U. S.
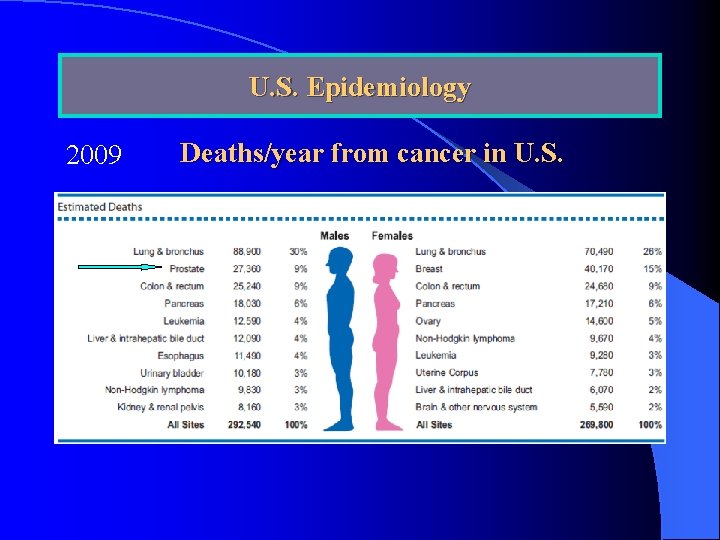
U. S. Epidemiology. 2009 Deaths/year from cancer in U. S.
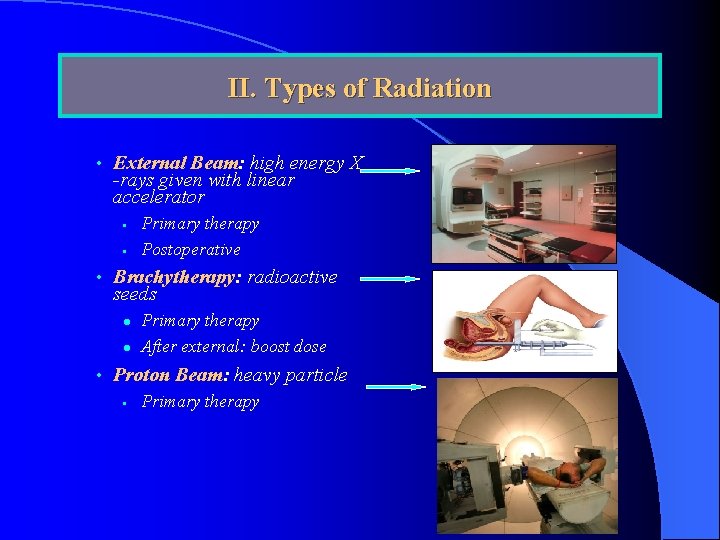
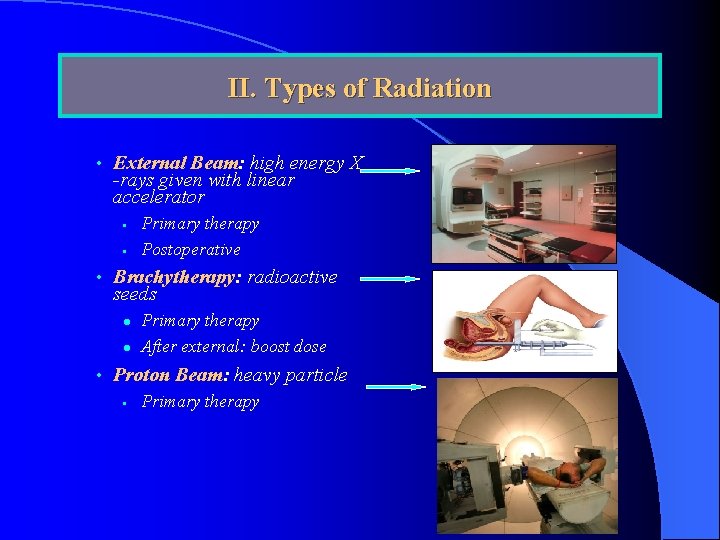
II. Types of Radiation • External Beam: high energy X -rays given with linear accelerator • • Primary therapy Postoperative • Brachytherapy: radioactive seeds l l Primary therapy After external: boost dose • Proton Beam: heavy particle • Primary therapy
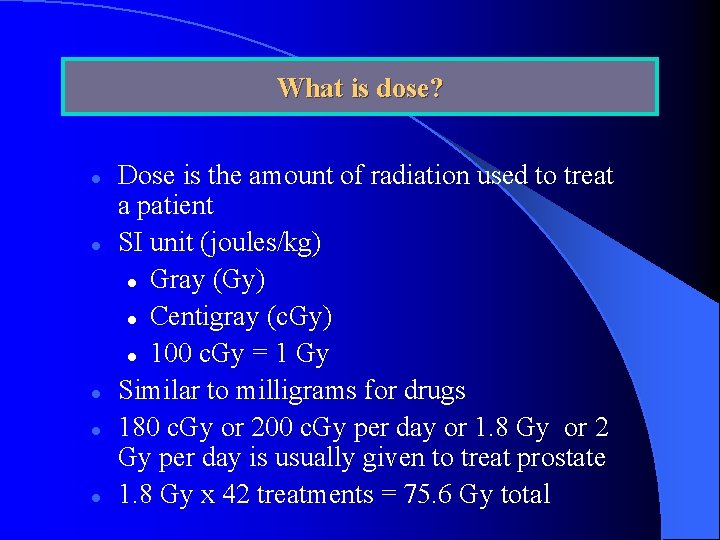
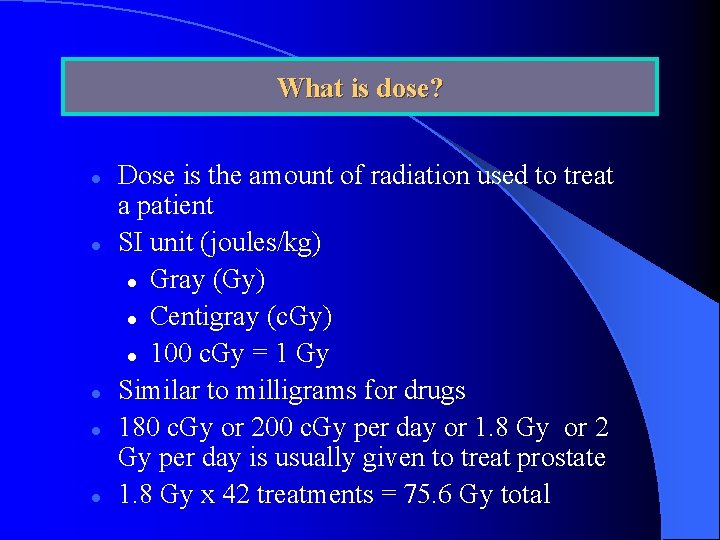
What is dose? l l l Dose is the amount of radiation used to treat a patient SI unit (joules/kg) l Gray (Gy) l Centigray (c. Gy) l 100 c. Gy = 1 Gy Similar to milligrams for drugs 180 c. Gy or 200 c. Gy per day or 1. 8 Gy or 2 Gy per day is usually given to treat prostate 1. 8 Gy x 42 treatments = 75. 6 Gy total
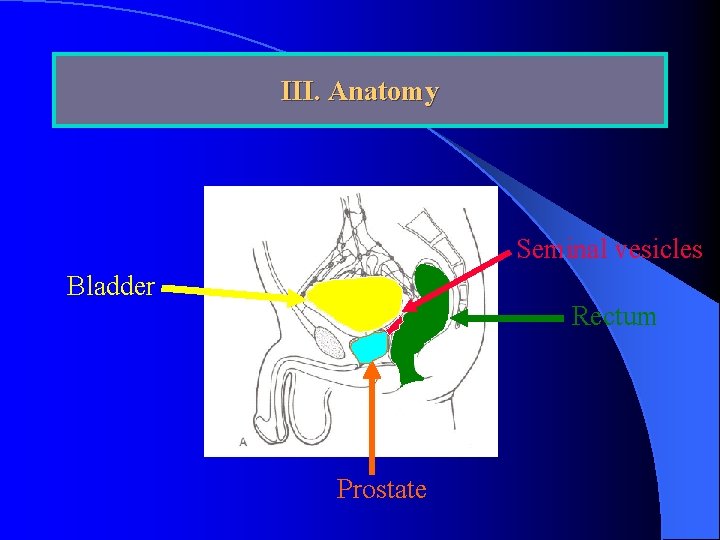
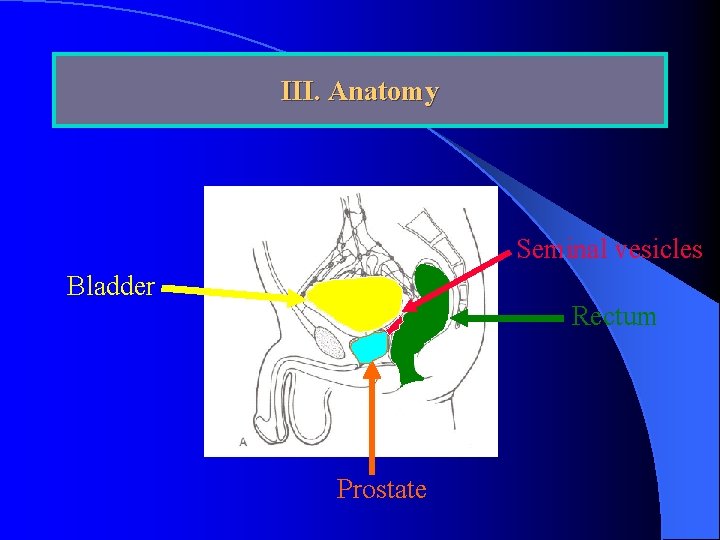
III. Anatomy Seminal vesicles Bladder Rectum Prostate
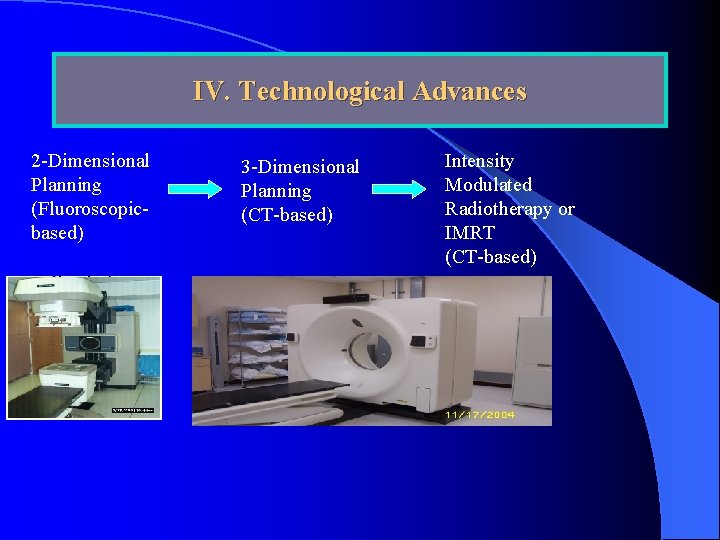
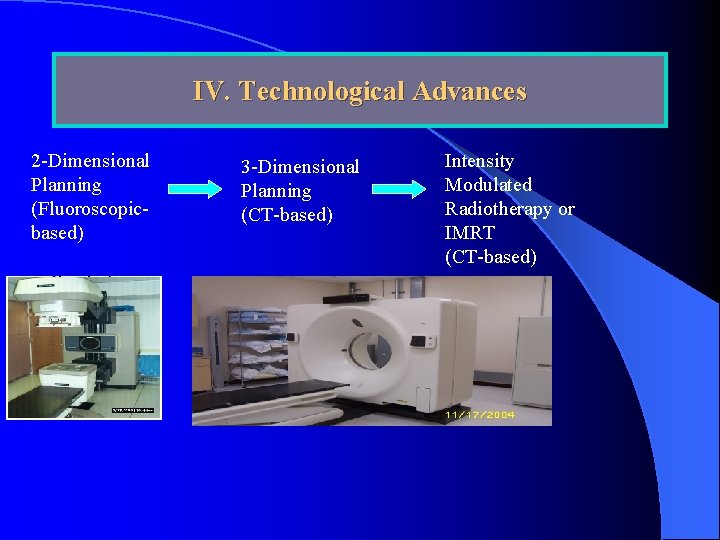
IV. Technological Advances 2 -Dimensional Planning (Fluoroscopicbased) 3 -Dimensional Planning (CT-based) Intensity Modulated Radiotherapy or IMRT (CT-based)
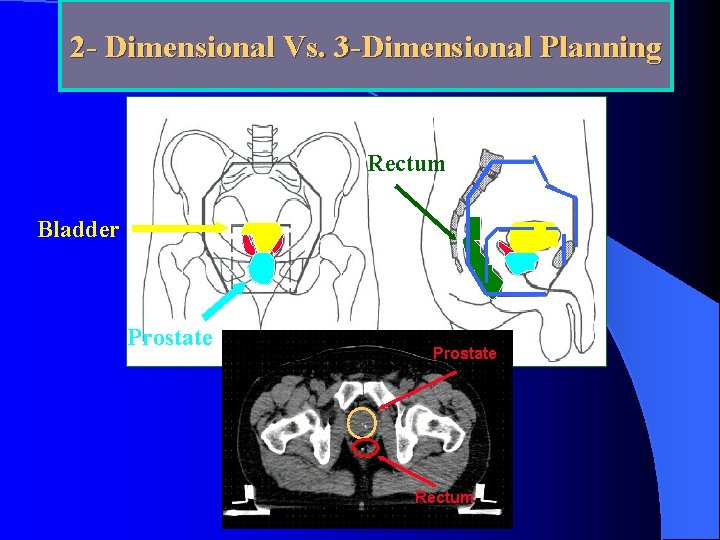
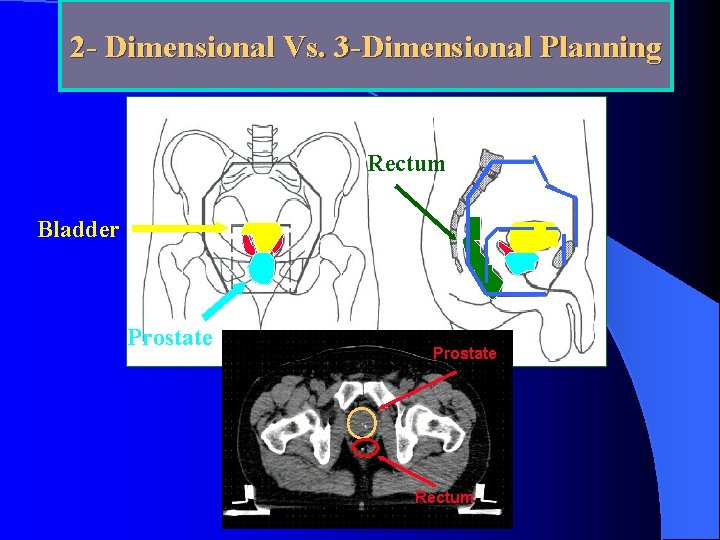
2 - Dimensional Vs. 3 -Dimensional Planning Rectum Bladder Prostate Rectum
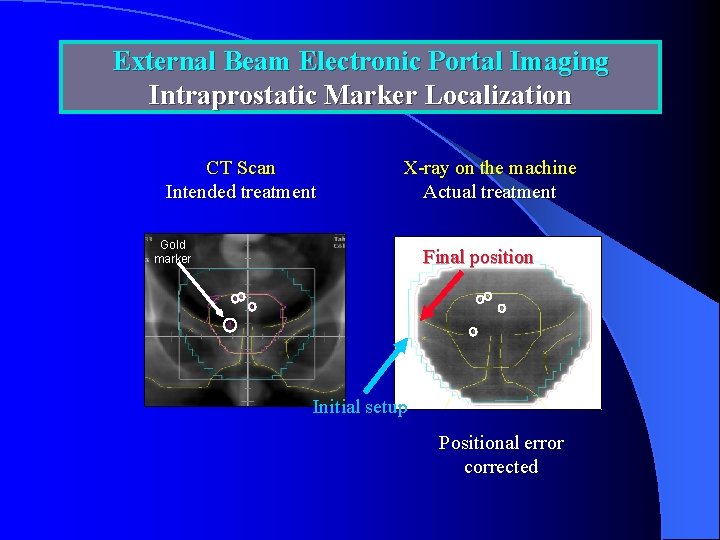
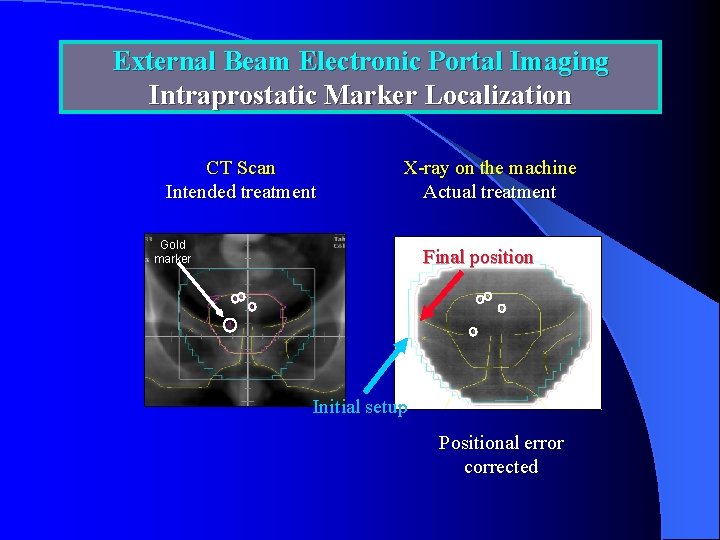
External Beam Electronic Portal Imaging Intraprostatic Marker Localization CT Scan Intended treatment X-ray on the machine Actual treatment Gold marker Final position Initial setup Positional error corrected
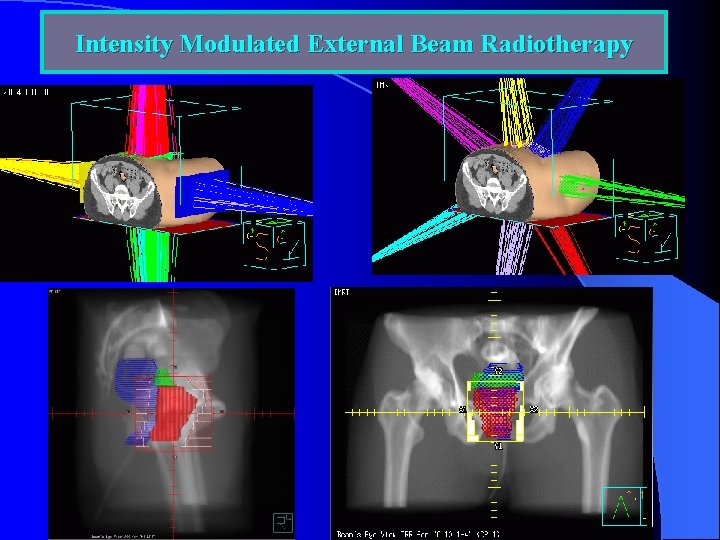
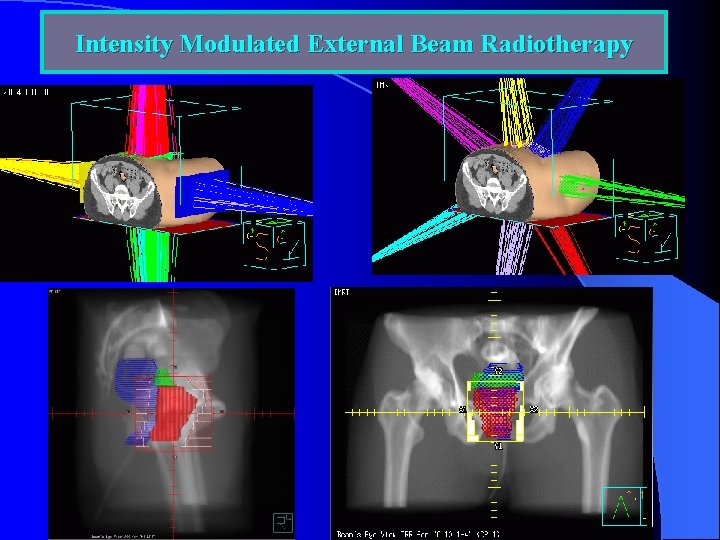
Intensity Modulated External Beam Radiotherapy
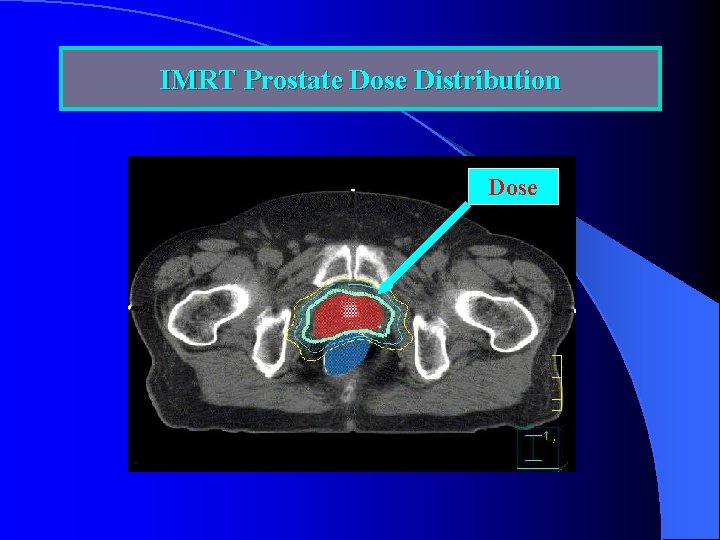
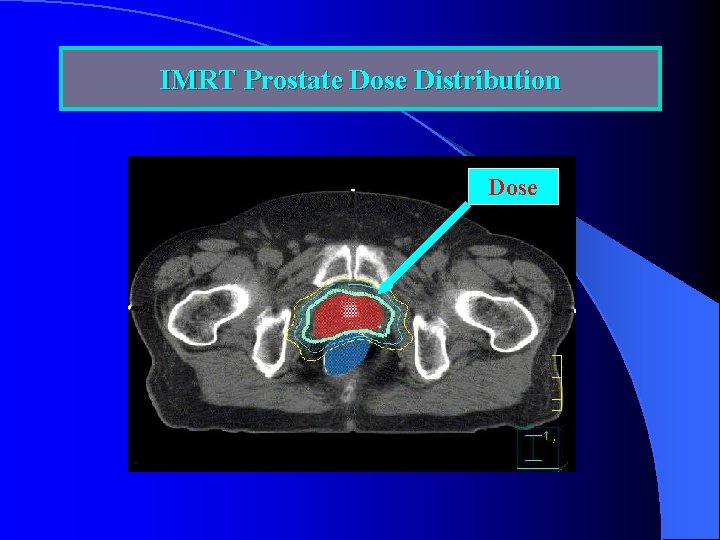
IMRT Prostate Dose Distribution Dose
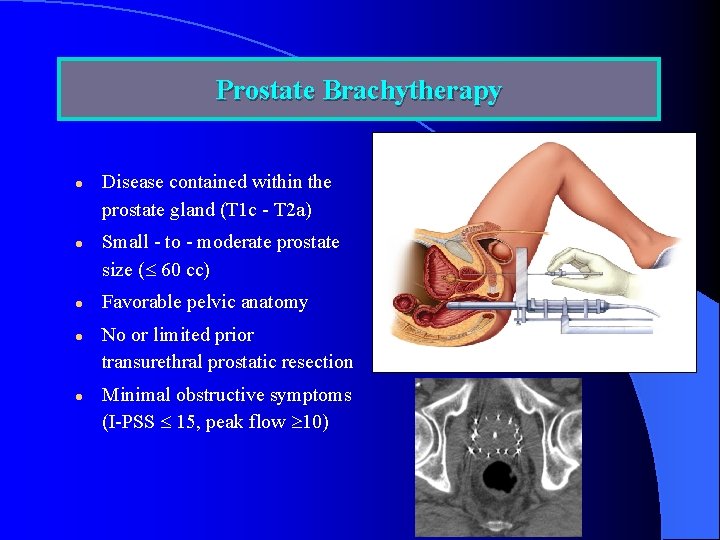
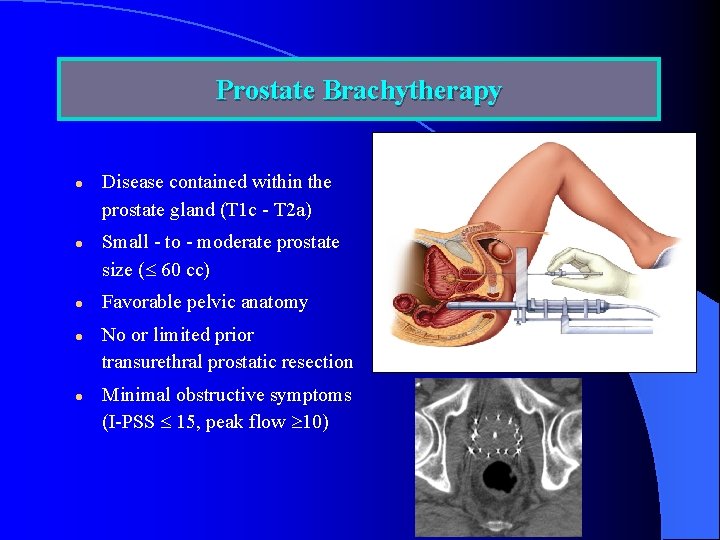
Prostate Brachytherapy l l l Disease contained within the prostate gland (T 1 c - T 2 a) Small - to - moderate prostate size ( 60 cc) Favorable pelvic anatomy No or limited prior transurethral prostatic resection Minimal obstructive symptoms (I-PSS 15, peak flow 10)
V. Definition of Risk Categories -Low Risk -Intermediate Risk -High Risk
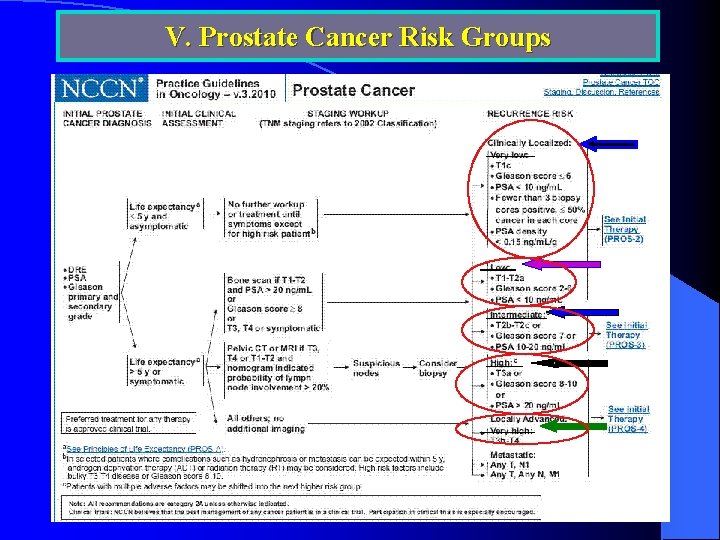
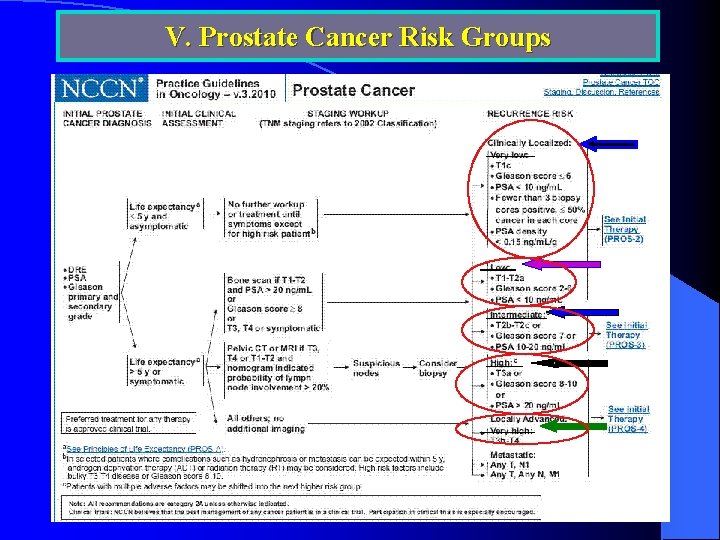
V. Prostate Cancer Risk Groups
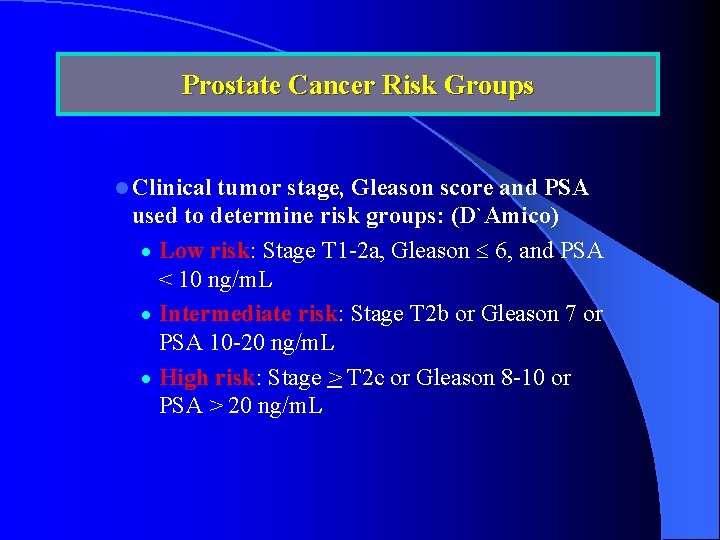
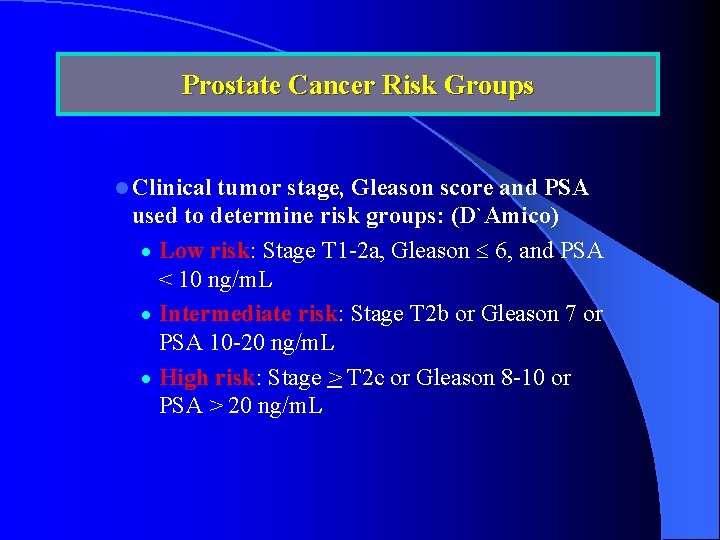
Prostate Cancer Risk Groups l Clinical tumor stage, Gleason score and PSA used to determine risk groups: (D`Amico) · Low risk: Stage T 1 -2 a, Gleason 6, and PSA < 10 ng/m. L · Intermediate risk: Stage T 2 b or Gleason 7 or PSA 10 -20 ng/m. L · High risk: Stage > T 2 c or Gleason 8 -10 or PSA > 20 ng/m. L
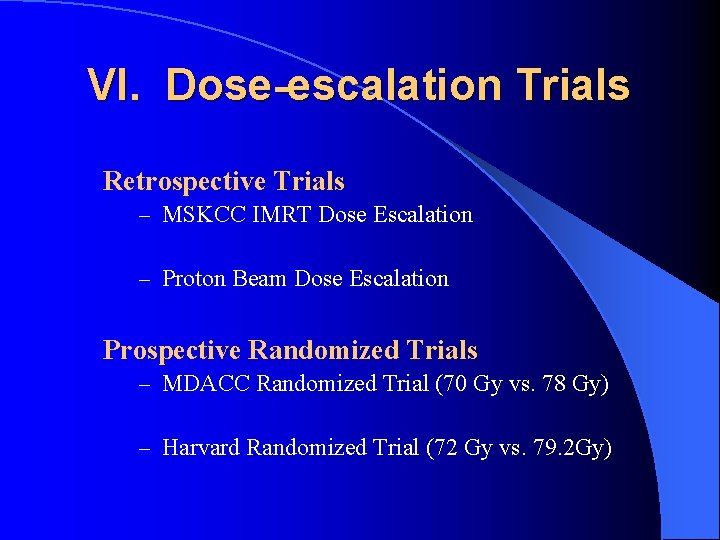
VI. Dose-escalation Trials Retrospective Trials – MSKCC IMRT Dose Escalation – Proton Beam Dose Escalation Prospective Randomized Trials – MDACC Randomized Trial (70 Gy vs. 78 Gy) – Harvard Randomized Trial (72 Gy vs. 79. 2 Gy)
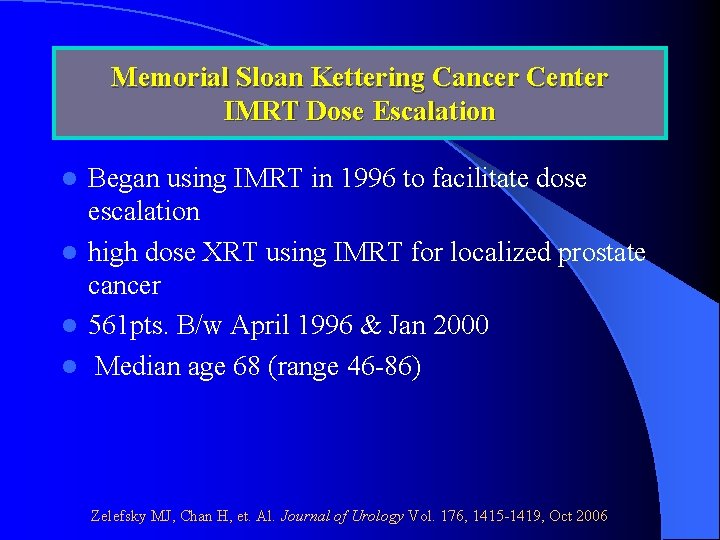
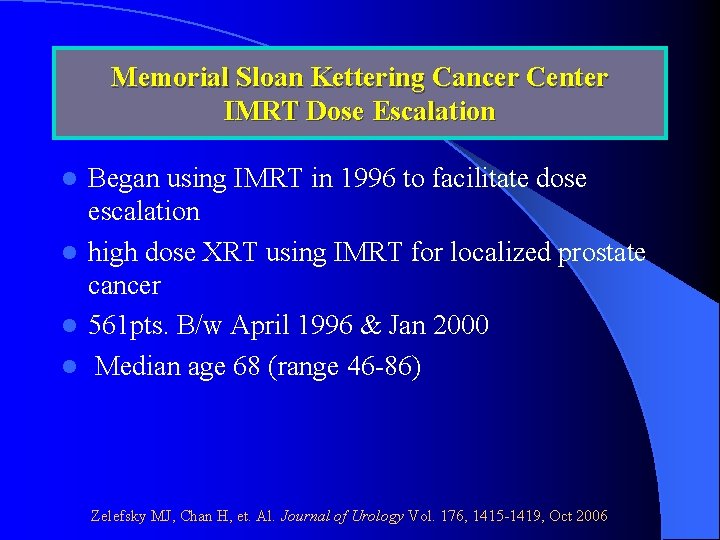
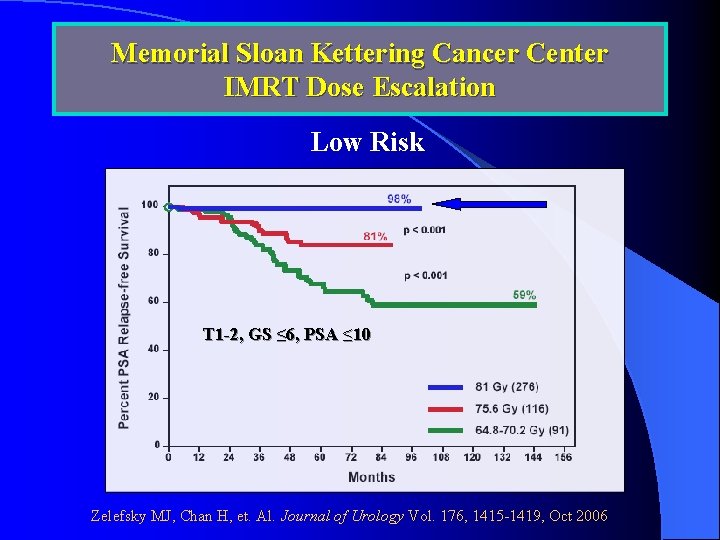
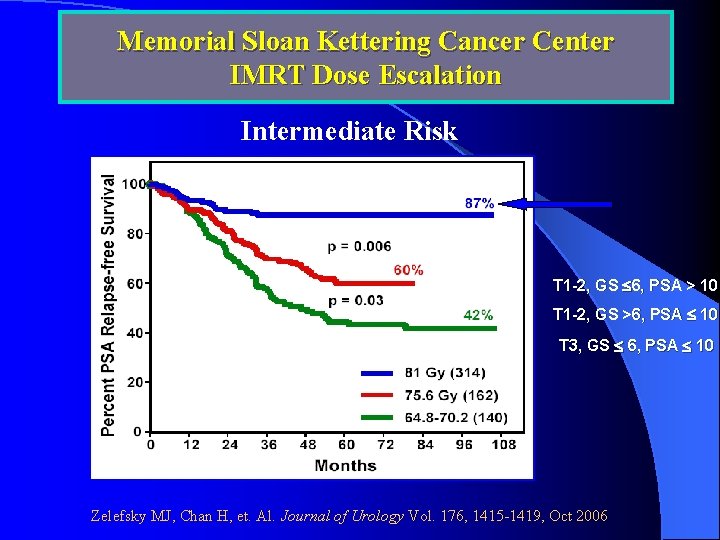
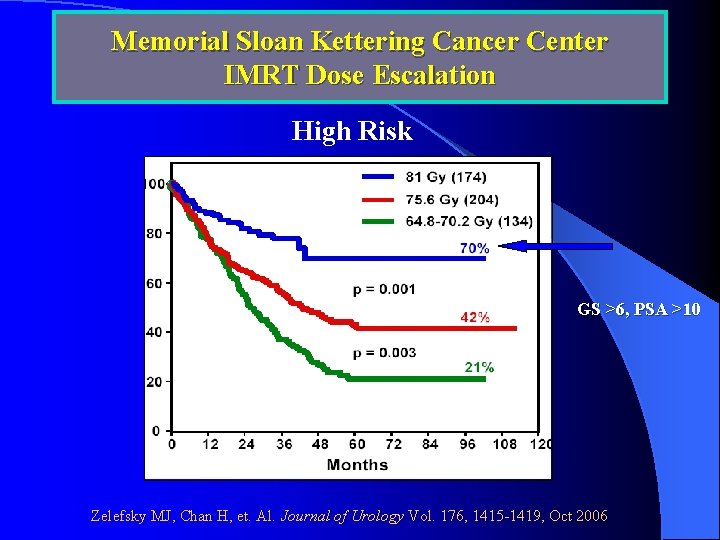
Memorial Sloan Kettering Cancer Center IMRT Dose Escalation Began using IMRT in 1996 to facilitate dose escalation l high dose XRT using IMRT for localized prostate cancer l 561 pts. B/w April 1996 & Jan 2000 l Median age 68 (range 46 -86) l Zelefsky MJ, Chan H, et. Al. Journal of Urology Vol. 176, 1415 -1419, Oct 2006
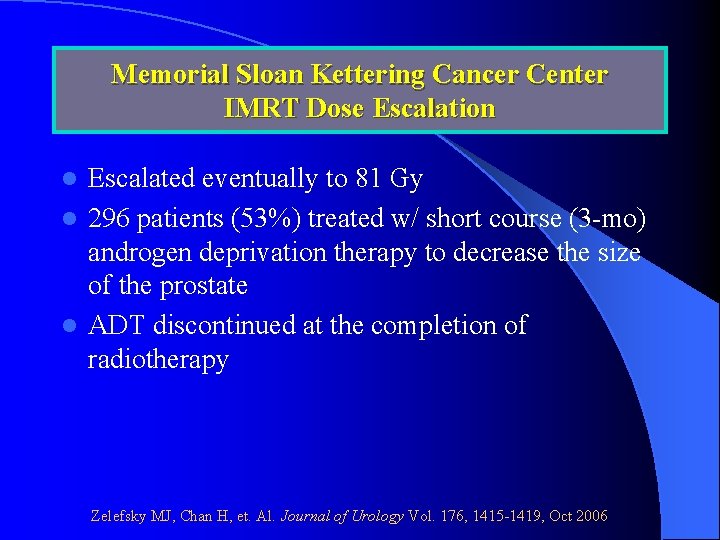
Memorial Sloan Kettering Cancer Center IMRT Dose Escalation Escalated eventually to 81 Gy l 296 patients (53%) treated w/ short course (3 -mo) androgen deprivation therapy to decrease the size of the prostate l ADT discontinued at the completion of radiotherapy l Zelefsky MJ, Chan H, et. Al. Journal of Urology Vol. 176, 1415 -1419, Oct 2006
Memorial Sloan Kettering Cancer Center IMRT Dose Escalation Median f/u: 7 years (range 5 to 9) l PSA relapse: – ASTRO definition: 3 consecutive rises after nadir – Houston definition: nadir + 2 l None received post-irradiation androgen deprivation or other anti-cancer therapy before documentation of a PSA relapse l Zelefsky MJ, Chan H, et. Al. Journal of Urology Vol. 176, 1415 -1419, Oct 2006
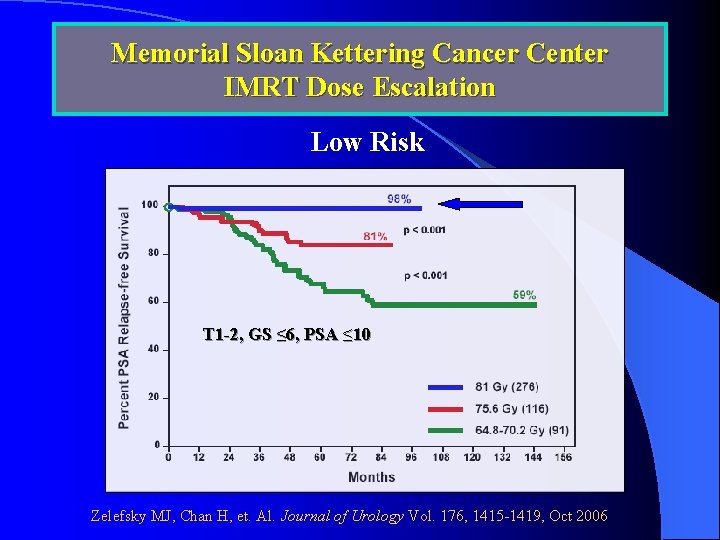
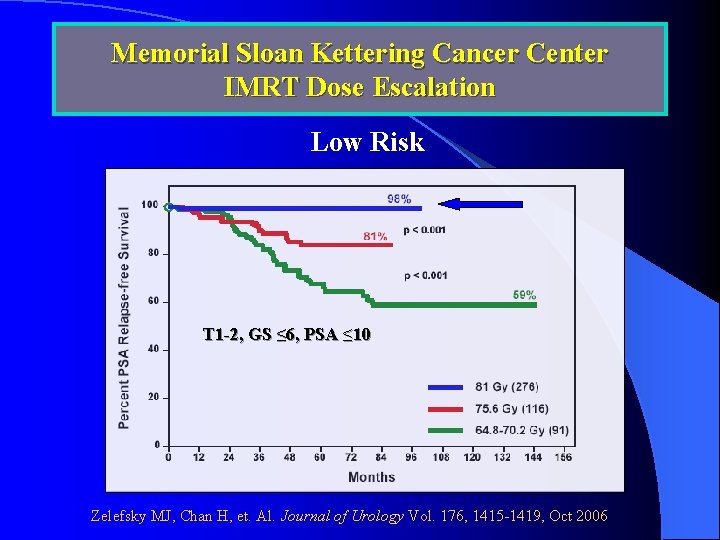
Memorial Sloan Kettering Cancer Center IMRT Dose Escalation Low Risk T 1 -2, GS ≤ 6, PSA ≤ 10 Zelefsky MJ, Chan H, et. Al. Journal of Urology Vol. 176, 1415 -1419, Oct 2006
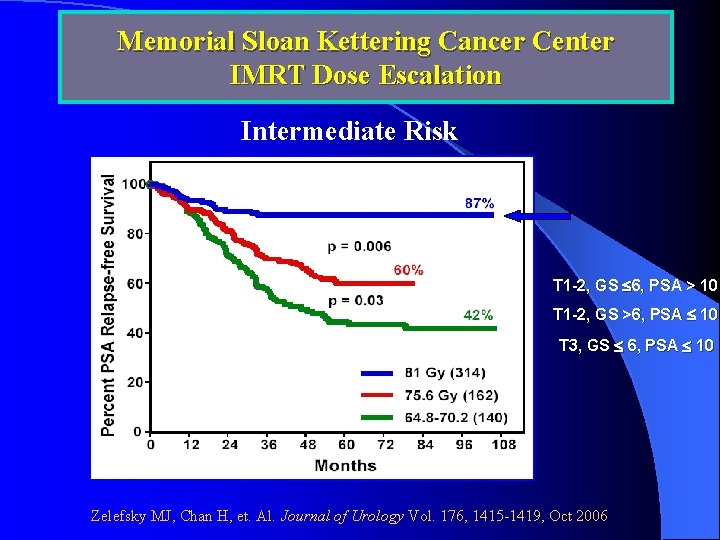
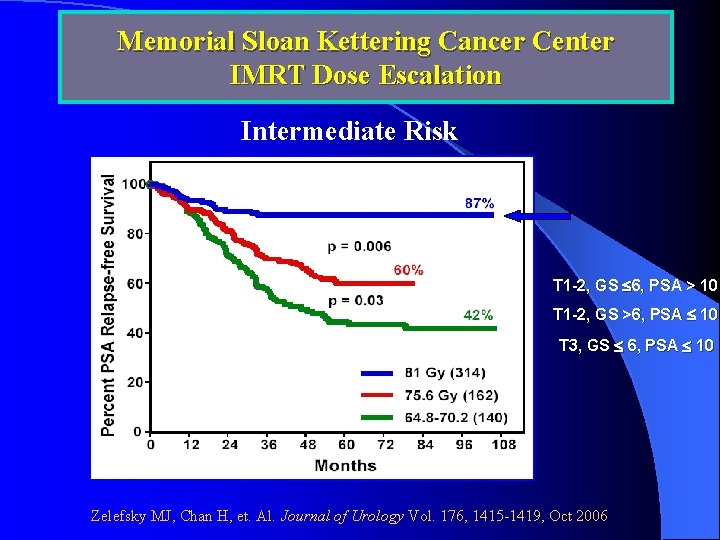
Memorial Sloan Kettering Cancer Center IMRT Dose Escalation Intermediate Risk T 1 -2, GS 6, PSA > 10 T 1 -2, GS >6, PSA 10 T 3, GS 6, PSA 10 Zelefsky MJ, Chan H, et. Al. Journal of Urology Vol. 176, 1415 -1419, Oct 2006
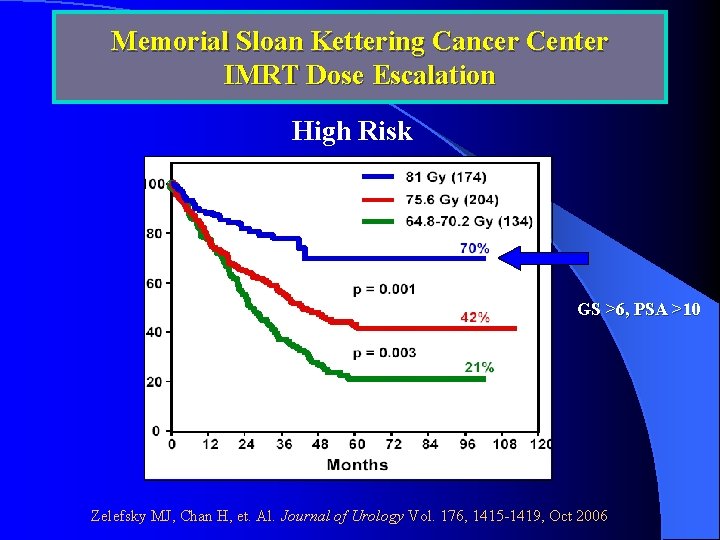
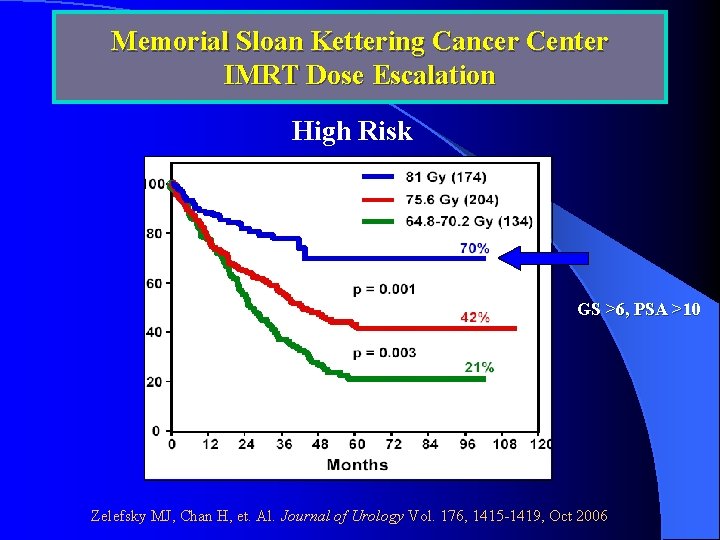
Memorial Sloan Kettering Cancer Center IMRT Dose Escalation High Risk GS >6, PSA >10 Zelefsky MJ, Chan H, et. Al. Journal of Urology Vol. 176, 1415 -1419, Oct 2006
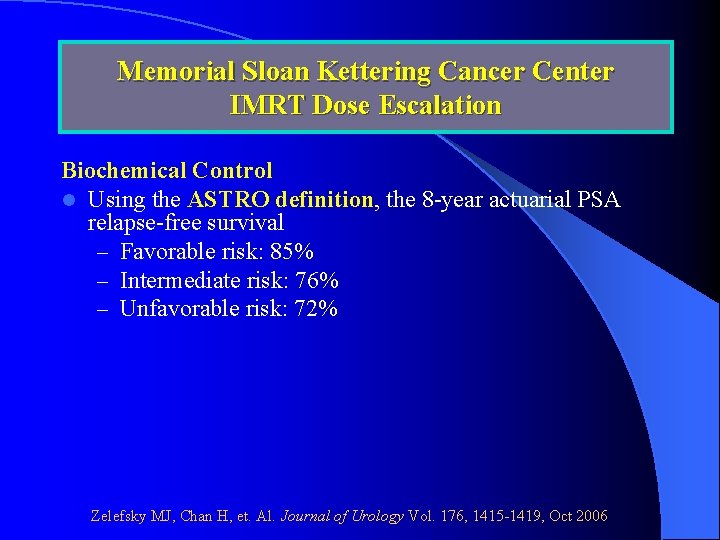
Memorial Sloan Kettering Cancer Center IMRT Dose Escalation Biochemical Control l Using the ASTRO definition, the 8 -year actuarial PSA relapse-free survival – Favorable risk: 85% – Intermediate risk: 76% – Unfavorable risk: 72% Zelefsky MJ, Chan H, et. Al. Journal of Urology Vol. 176, 1415 -1419, Oct 2006
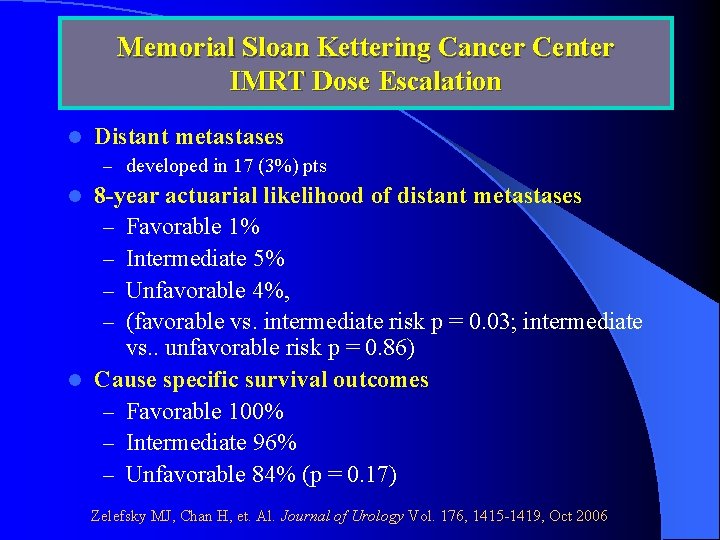
Memorial Sloan Kettering Cancer Center IMRT Dose Escalation l Distant metastases – developed in 17 (3%) pts 8 -year actuarial likelihood of distant metastases – Favorable 1% – Intermediate 5% – Unfavorable 4%, – (favorable vs. intermediate risk p = 0. 03; intermediate vs. . unfavorable risk p = 0. 86) l Cause specific survival outcomes – Favorable 100% – Intermediate 96% – Unfavorable 84% (p = 0. 17) l Zelefsky MJ, Chan H, et. Al. Journal of Urology Vol. 176, 1415 -1419, Oct 2006
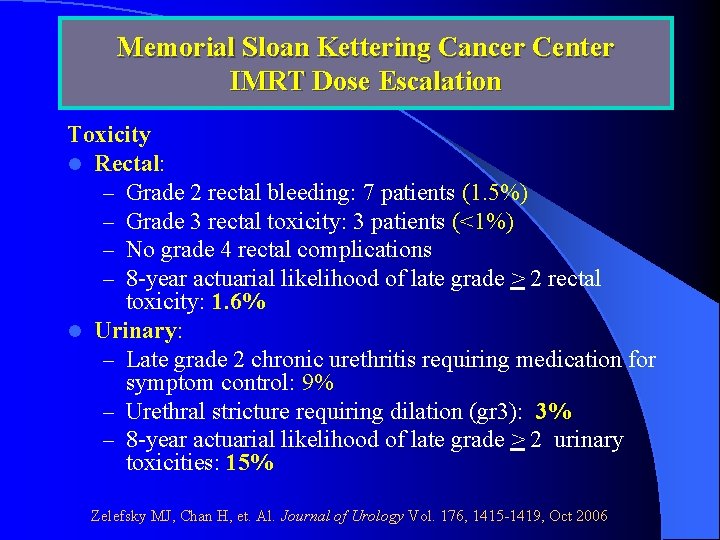
Memorial Sloan Kettering Cancer Center IMRT Dose Escalation Toxicity l Rectal: – Grade 2 rectal bleeding: 7 patients (1. 5%) – Grade 3 rectal toxicity: 3 patients (<1%) – No grade 4 rectal complications – 8 -year actuarial likelihood of late grade > 2 rectal toxicity: 1. 6% l Urinary: – Late grade 2 chronic urethritis requiring medication for symptom control: 9% – Urethral stricture requiring dilation (gr 3): 3% – 8 -year actuarial likelihood of late grade > 2 urinary toxicities: 15% Zelefsky MJ, Chan H, et. Al. Journal of Urology Vol. 176, 1415 -1419, Oct 2006
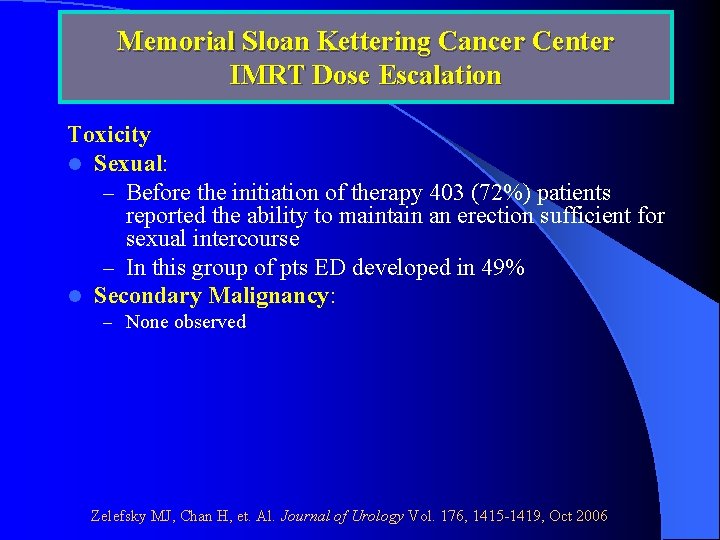
Memorial Sloan Kettering Cancer Center IMRT Dose Escalation Toxicity l Sexual: – Before the initiation of therapy 403 (72%) patients reported the ability to maintain an erection sufficient for sexual intercourse – In this group of pts ED developed in 49% l Secondary Malignancy: – None observed Zelefsky MJ, Chan H, et. Al. Journal of Urology Vol. 176, 1415 -1419, Oct 2006
Loma Linda Proton Beam Experience Dose Escalation. B/w Oct 1991 & Dec 1997, l 1255 pts with Stages Ia-III prostate cancer l No prior surgery, hormonal therapy, or distant mets l Treated with protons alone or in combination with photon-beam XRT l Slater JD, Rossi CJ, et. Al. IJROBP Vol 59, No. 2, 348 -352, 2004.
Loma Linda Proton Beam Experience Dose Escalation. Freedom from biochemical evidence of disease (b. NED) used ASTRO consensus definition ( 3 consecutive PSA rises after reaching a nadir) l Mean duration f/u: 63 months l Median age: 69 years l Slater JD, Rossi CJ, et. Al. IJROBP Vol 59, No. 2, 348 -352, 2004.
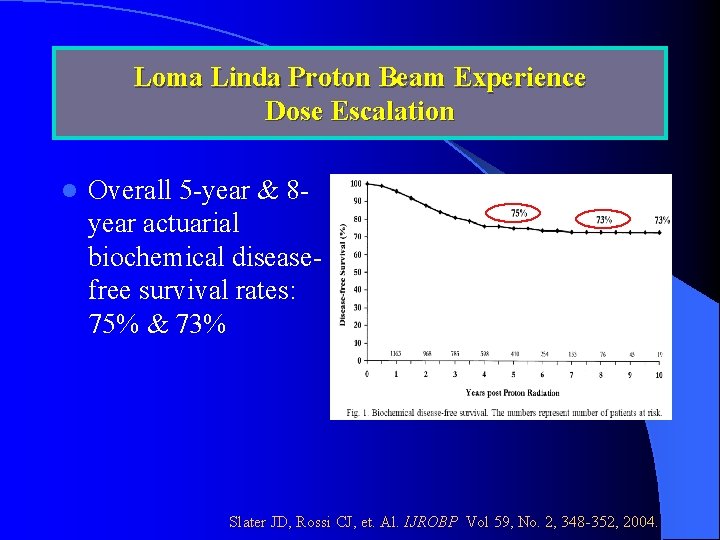
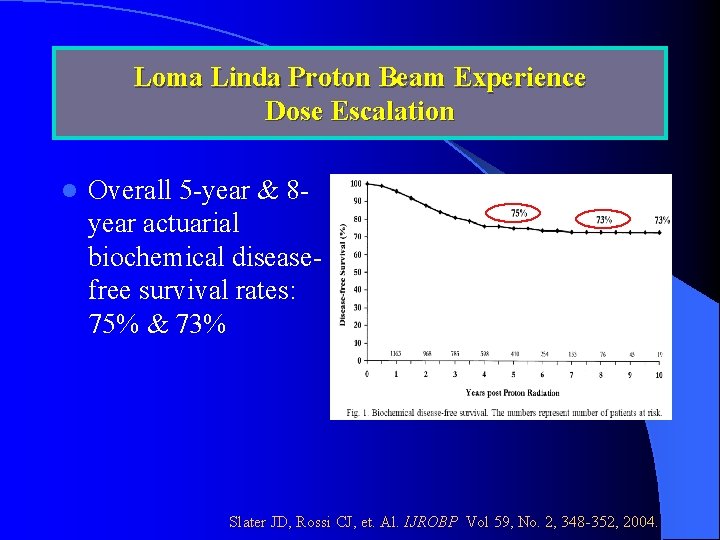
Loma Linda Proton Beam Experience Dose Escalation l Overall 5 -year & 8 year actuarial biochemical diseasefree survival rates: 75% & 73% Slater JD, Rossi CJ, et. Al. IJROBP Vol 59, No. 2, 348 -352, 2004.
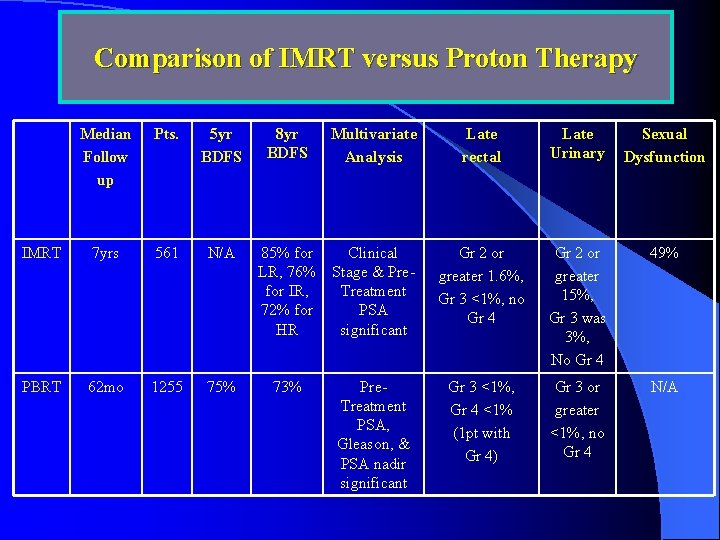
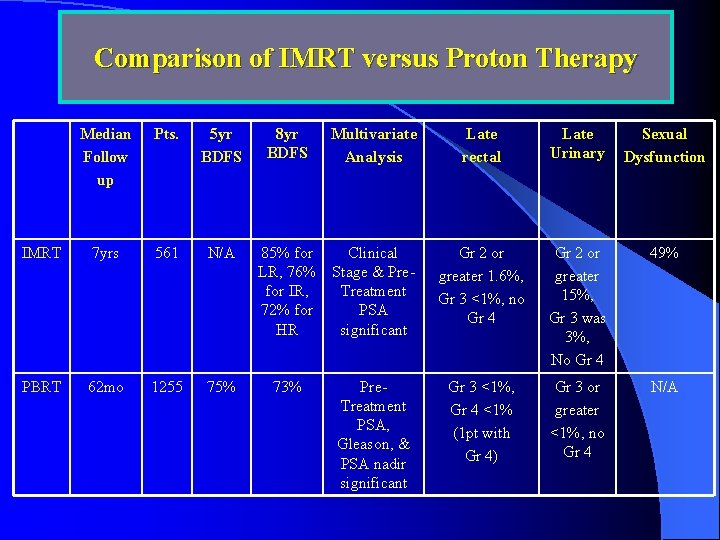
Comparison of IMRT versus Proton Therapy Median Follow up Pts. 5 yr BDFS 8 yr BDFS Multivariate Analysis Late rectal Late Urinary Sexual Dysfunction IMRT 7 yrs 561 N/A 85% for LR, 76% for IR, 72% for HR Clinical Stage & Pre. Treatment PSA significant Gr 2 or greater 1. 6%, Gr 3 <1%, no Gr 4 Gr 2 or greater 15%, Gr 3 was 3%, No Gr 4 49% PBRT 62 mo 1255 75% 73% Pre. Treatment PSA, Gleason, & PSA nadir significant Gr 3 <1%, Gr 4 <1% (1 pt with Gr 4) Gr 3 or greater <1%, no Gr 4 N/A
MDACC Randomized Dose Escalation Trial Results Of A Randomized Dose-Escalation Study Comparing 70 Gy To 78 Gy(isocenter) For The Treatment Of Prostate Cancer Pollack IJROBP 2002
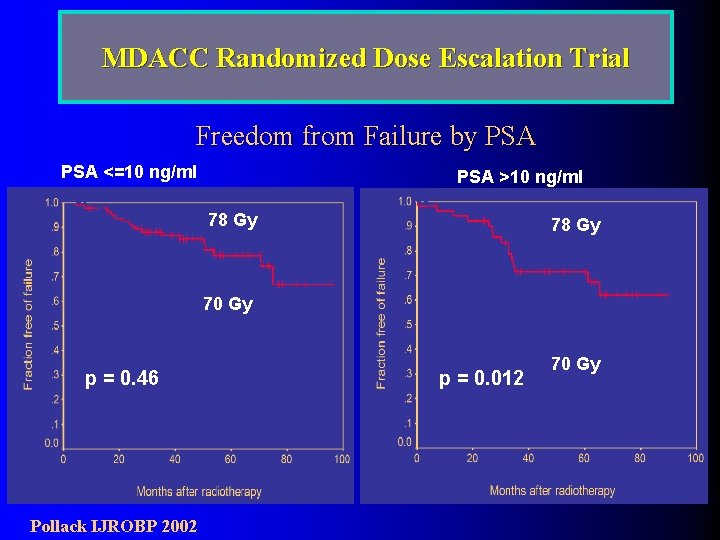
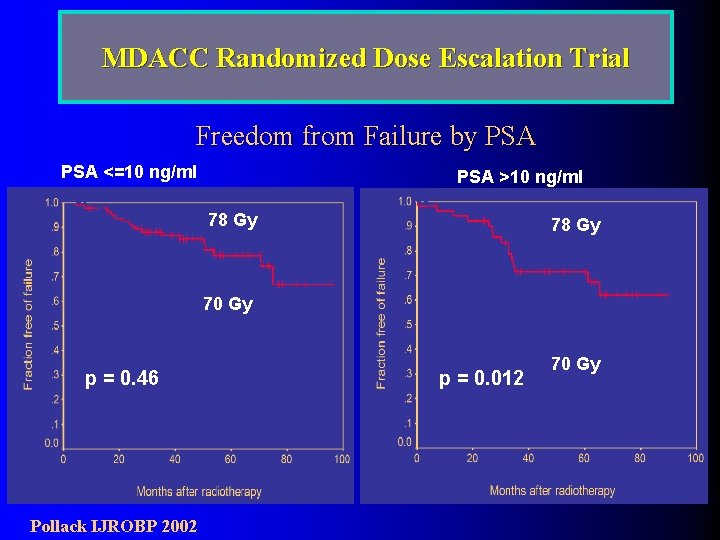
MDACC Randomized Dose Escalation Trial Freedom from Failure by PSA <=10 ng/ml PSA >10 ng/ml 78 Gy 70 Gy p = 0. 46 Pollack IJROBP 2002 p = 0. 012 70 Gy
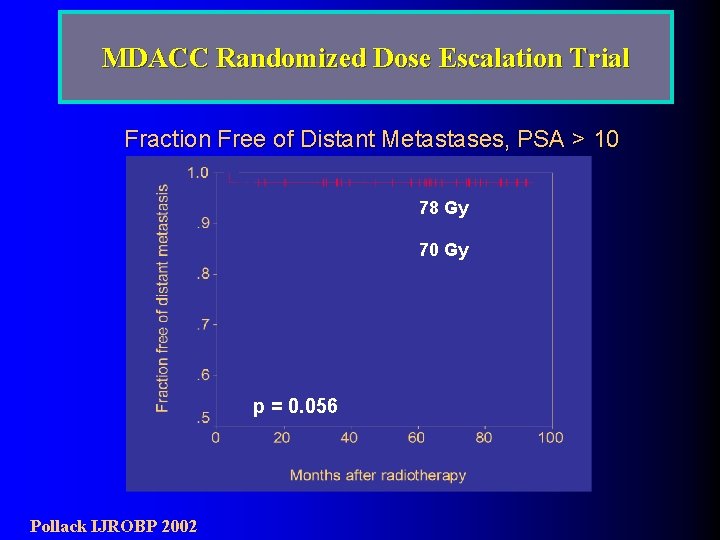
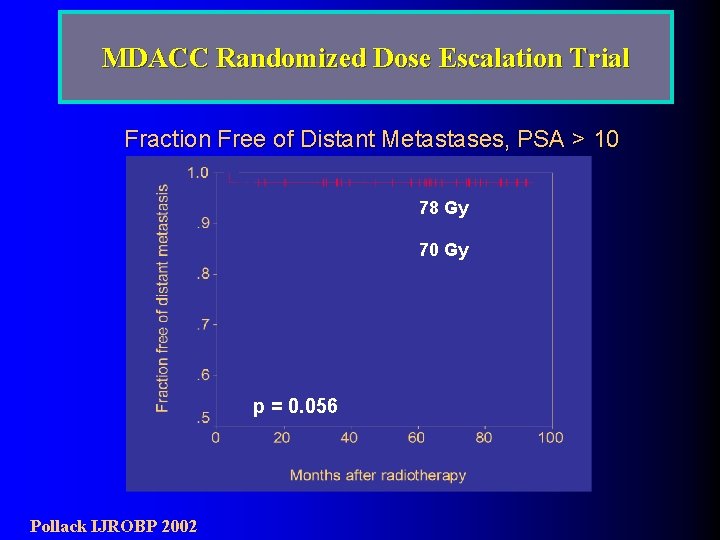
MDACC Randomized Dose Escalation Trial Fraction Free of Distant Metastases, PSA > 10 78 Gy 70 Gy p = 0. 056 Pollack IJROBP 2002
Harvard Randomized Dose Escalation Trial Phase III trial comparing conventional dose with high dose radiation in early stage prostate cancer: results of PROG 95 -09 Zietman A, et. al. JAMA, 2005, 294 (10): 1233
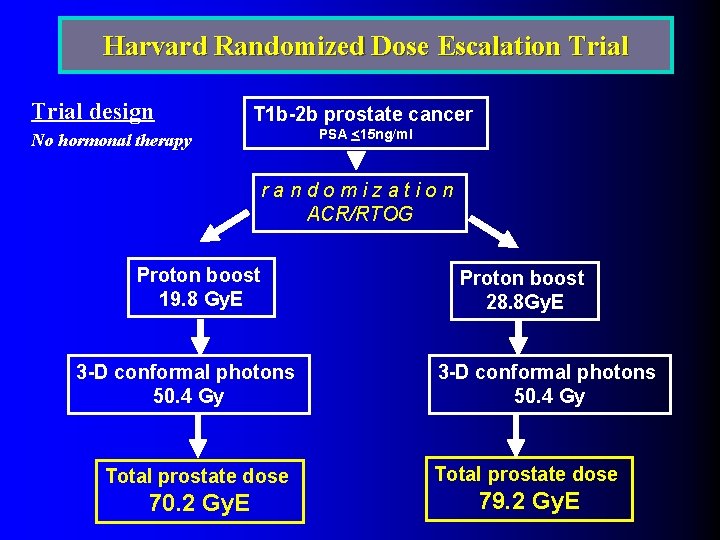
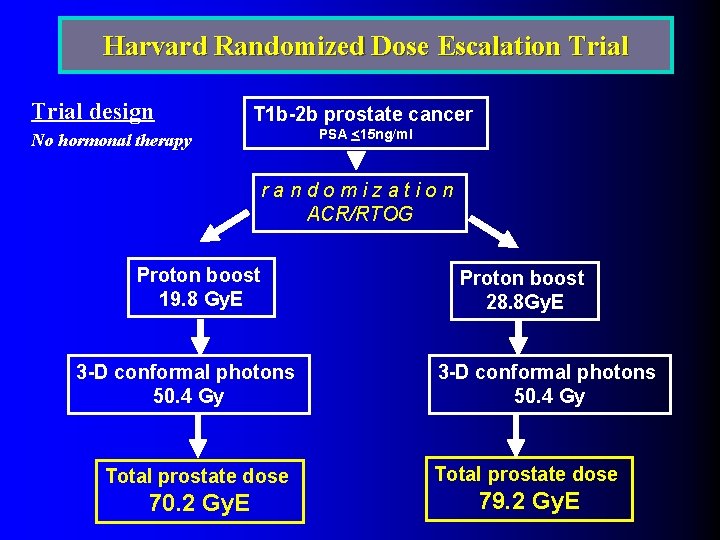
Harvard Randomized Dose Escalation Trial design T 1 b-2 b prostate cancer PSA <15 ng/ml No hormonal therapy randomization ACR/RTOG Proton boost 19. 8 Gy. E 3 -D conformal photons 50. 4 Gy Total prostate dose 70. 2 Gy. E Proton boost 28. 8 Gy. E 3 -D conformal photons 50. 4 Gy Total prostate dose 79. 2 Gy. E
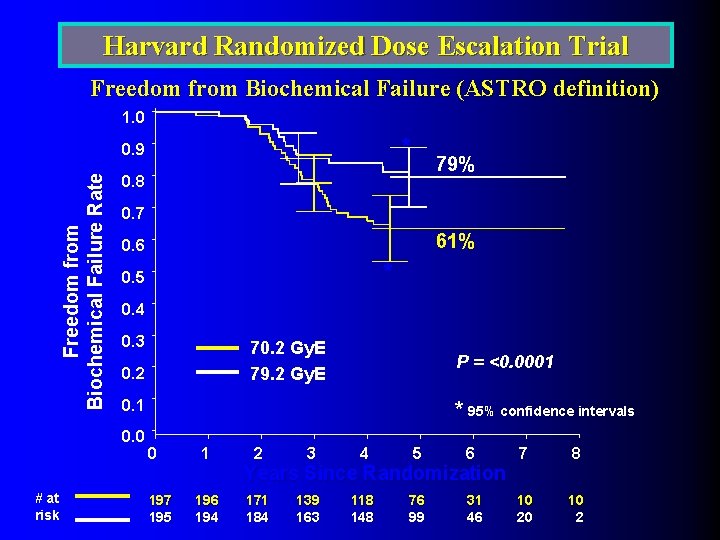
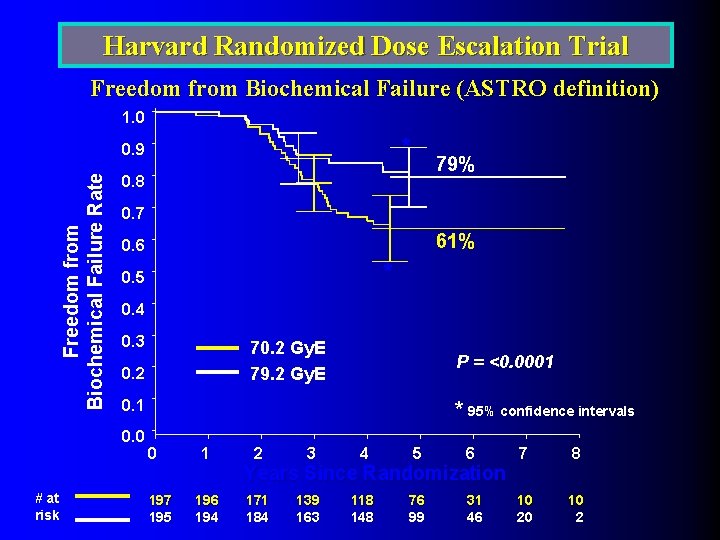
Harvard Randomized Dose Escalation Trial Freedom from Biochemical Failure (ASTRO definition) 1. 0 * Freedom from Biochemical Failure Rate 0. 9 0. 8 0. 7 61% 0. 6 * 0. 5 0. 4 0. 3 70. 2 Gy. E 79. 2 Gy. E 0. 2 P = <0. 0001 0. 0 # at risk 79% * 95% confidence intervals 0 197 195 1 196 194 2 3 4 5 6 7 8 171 184 139 163 118 148 76 99 31 46 10 20 10 2 Years Since Randomization
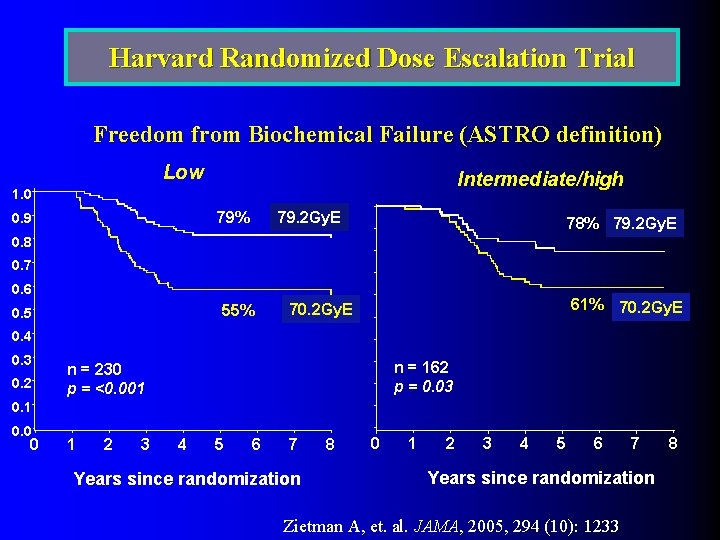
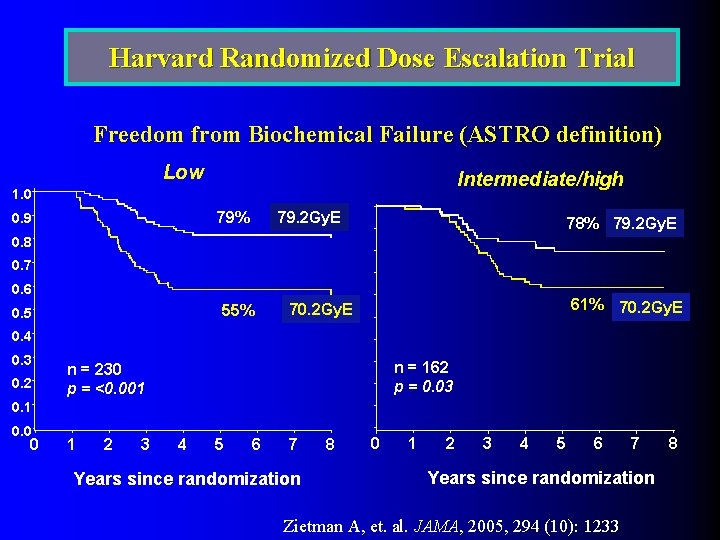
Harvard Randomized Dose Escalation Trial Freedom from Biochemical Failure (ASTRO definition) Low Intermediate/high 1. 0 79% 0. 9 79. 2 Gy. E 78% 79. 2 Gy. E 0. 8 0. 7 0. 6 55% 0. 5 61% 70. 2 Gy. E 0. 4 0. 3 0. 2 n = 162 p = 0. 03 n = 230 p = <0. 001 0. 0 0 1 2 3 4 5 6 7 Years since randomization 8 0 1 2 3 4 5 6 7 Years since randomization Zietman A, et. al. JAMA, 2005, 294 (10): 1233 8

VII. Low Risk Disease Treatment -IMRT alone -Seeds alone
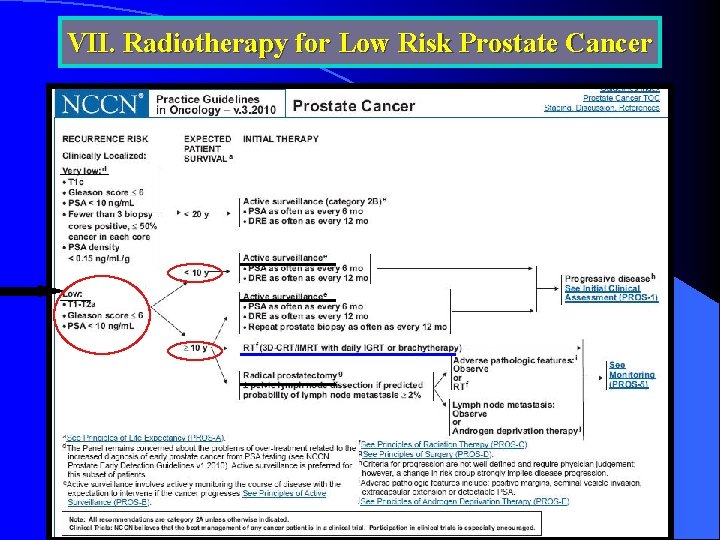
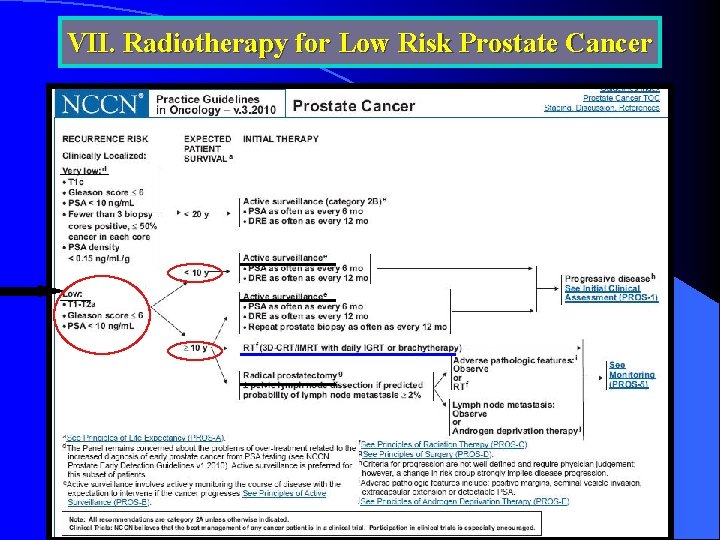
VII. Radiotherapy for Low Risk Prostate Cancer
Treatment Options for Low- Risk Group Watchful waiting vs. active surveillance l Radical prostatectomy l IMRT l Interstitial brachytherapy l
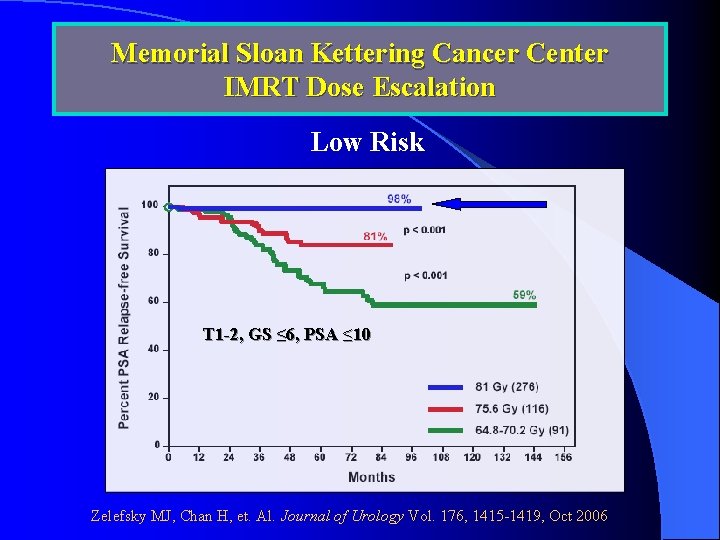
Memorial Sloan Kettering Cancer Center IMRT Dose Escalation Low Risk T 1 -2, GS ≤ 6, PSA ≤ 10 Zelefsky MJ, Chan H, et. Al. Journal of Urology Vol. 176, 1415 -1419, Oct 2006
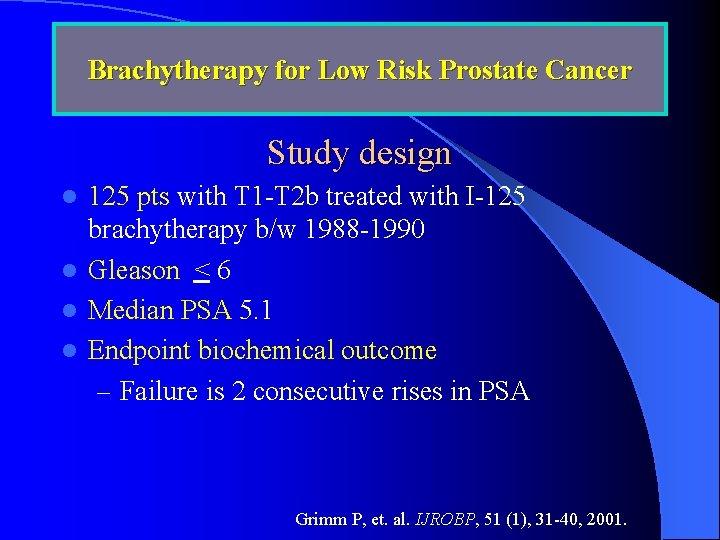
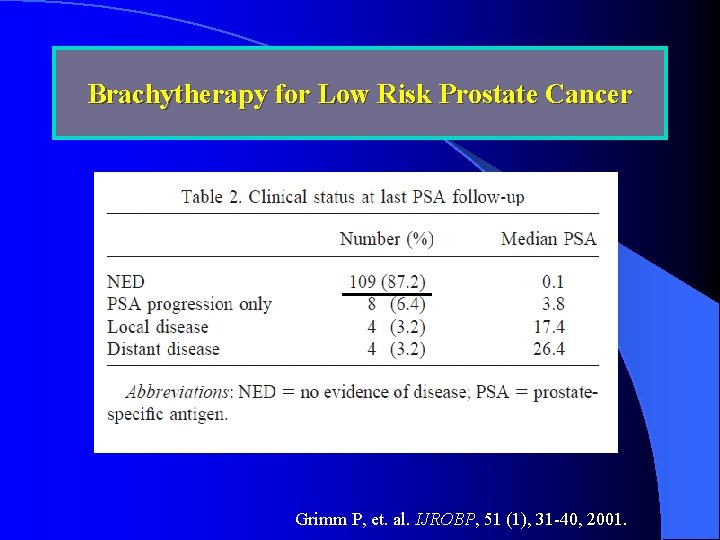
Brachytherapy for Low Risk Prostate Cancer Study design 125 pts with T 1 -T 2 b treated with I-125 brachytherapy b/w 1988 -1990 l Gleason < 6 l Median PSA 5. 1 l Endpoint biochemical outcome – Failure is 2 consecutive rises in PSA l Grimm P, et. al. IJROBP, 51 (1), 31 -40, 2001.
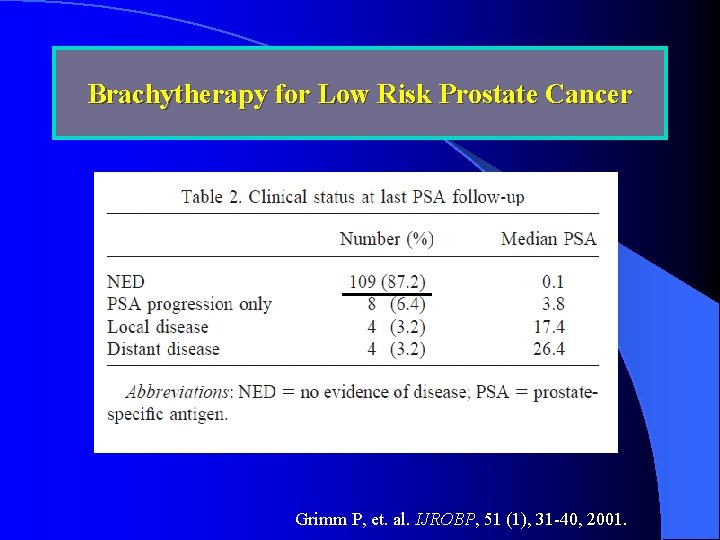
Brachytherapy for Low Risk Prostate Cancer Grimm P, et. al. IJROBP, 51 (1), 31 -40, 2001.

VIII. Intermediate Risk Disease Treatment -IMRT alone -6 mo Hormone + EBRT -Seeds + EBRT
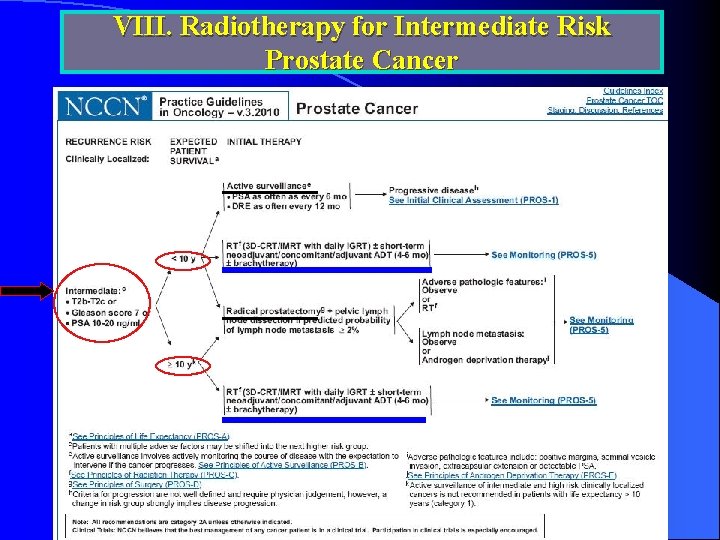
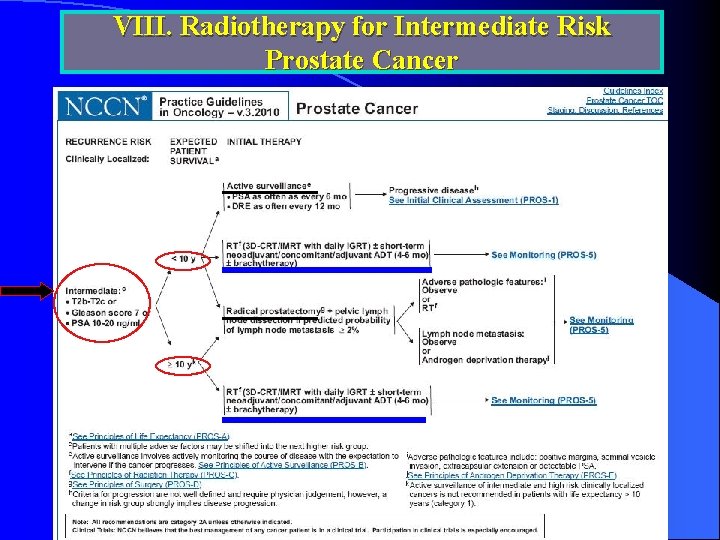
VIII. Radiotherapy for Intermediate Risk Prostate Cancer
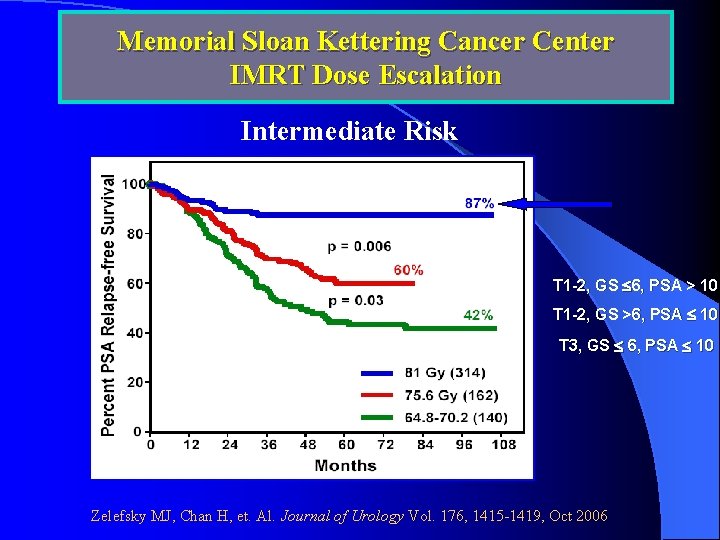
Memorial Sloan Kettering Cancer Center IMRT Dose Escalation Intermediate Risk T 1 -2, GS 6, PSA > 10 T 1 -2, GS >6, PSA 10 T 3, GS 6, PSA 10 Zelefsky MJ, Chan H, et. Al. Journal of Urology Vol. 176, 1415 -1419, Oct 2006
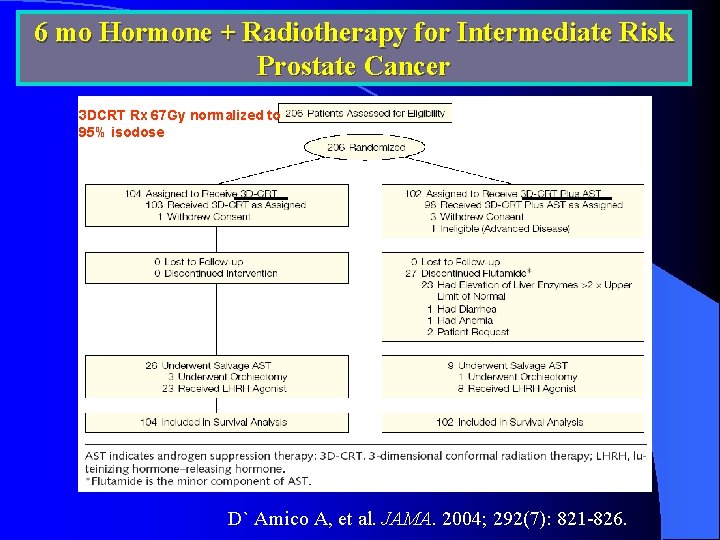
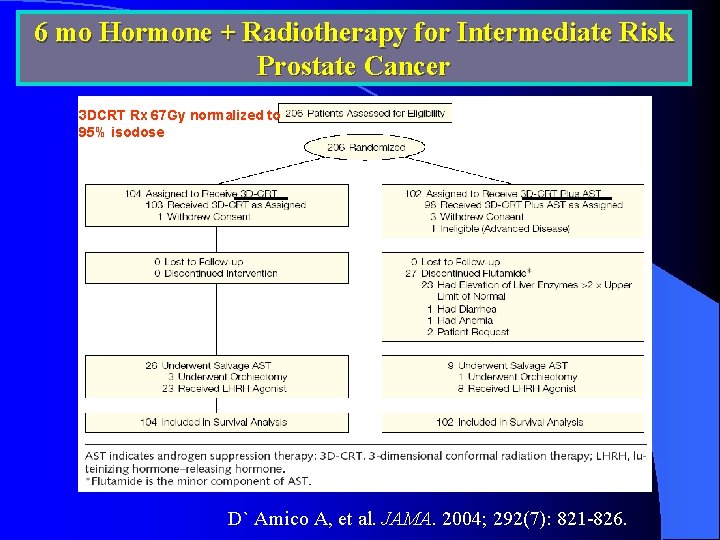
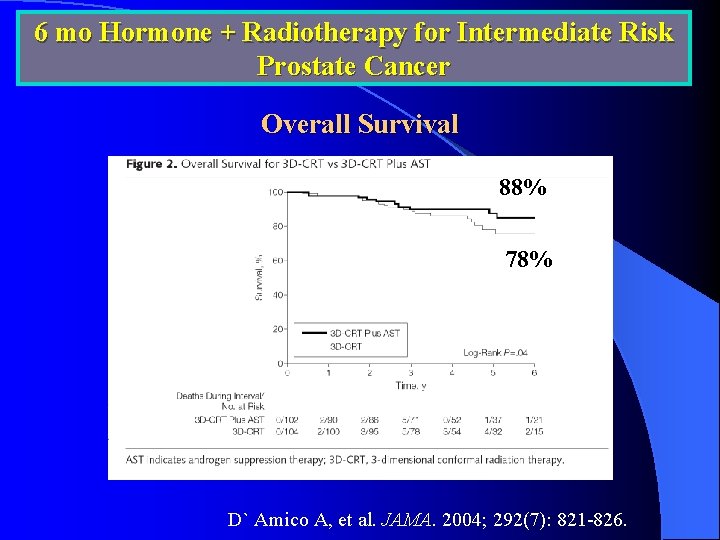
6 mo Hormone + Radiotherapy for Intermediate Risk Prostate Cancer 3 DCRT Rx 67 Gy normalized to 95% isodose D` Amico A, et al. JAMA. 2004; 292(7): 821 -826.
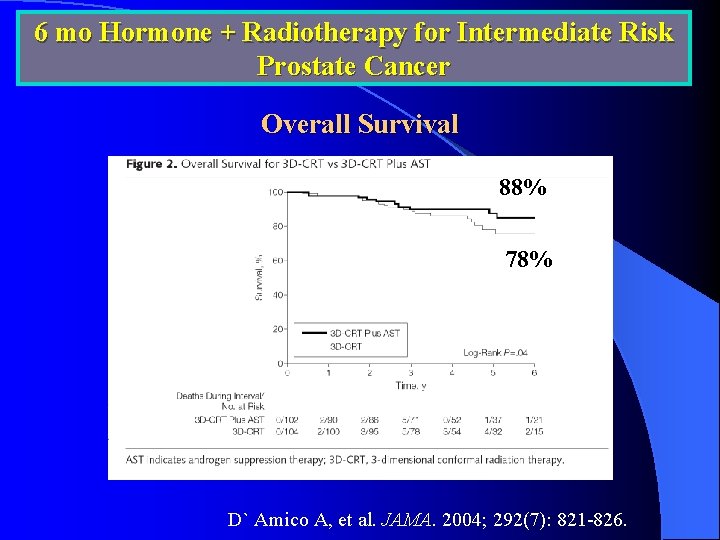
6 mo Hormone + Radiotherapy for Intermediate Risk Prostate Cancer Overall Survival 88% 78% D` Amico A, et al. JAMA. 2004; 292(7): 821 -826.
IX. High Risk Disease Treatment -Long-term Hormonal therapy Randomized Trials -RTOG randomized Trial -EORTC randomized Trial -Seeds + EBRT
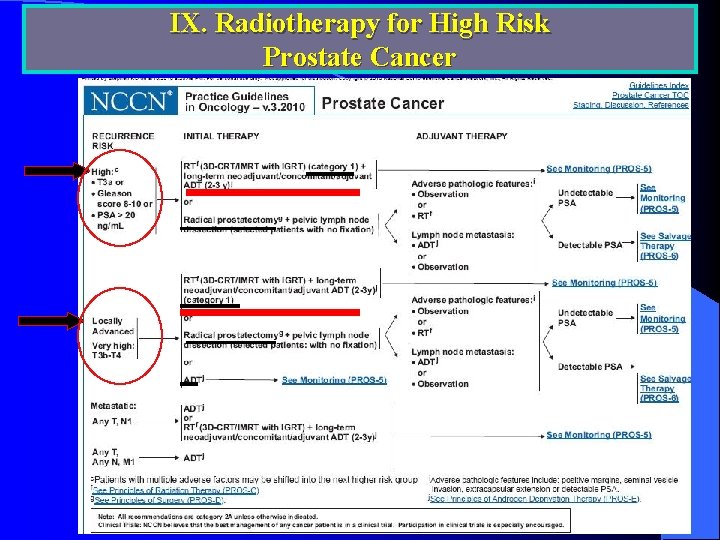
IX. Radiotherapy for High Risk Prostate Cancer
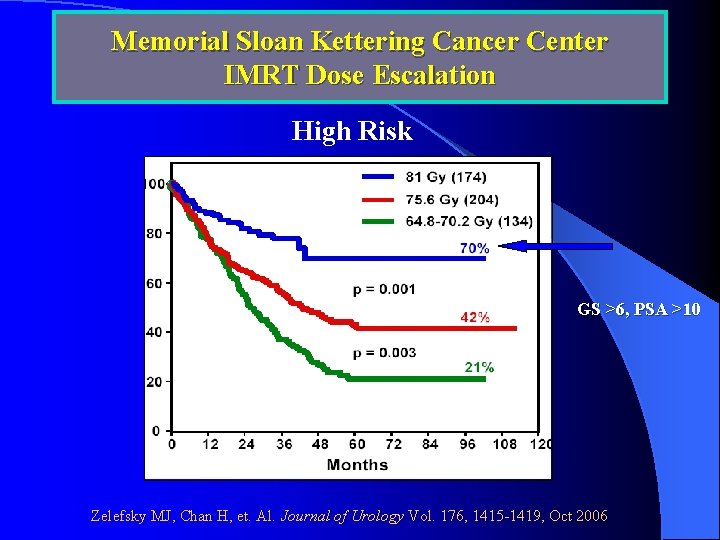
Memorial Sloan Kettering Cancer Center IMRT Dose Escalation High Risk GS >6, PSA >10 Zelefsky MJ, Chan H, et. Al. Journal of Urology Vol. 176, 1415 -1419, Oct 2006
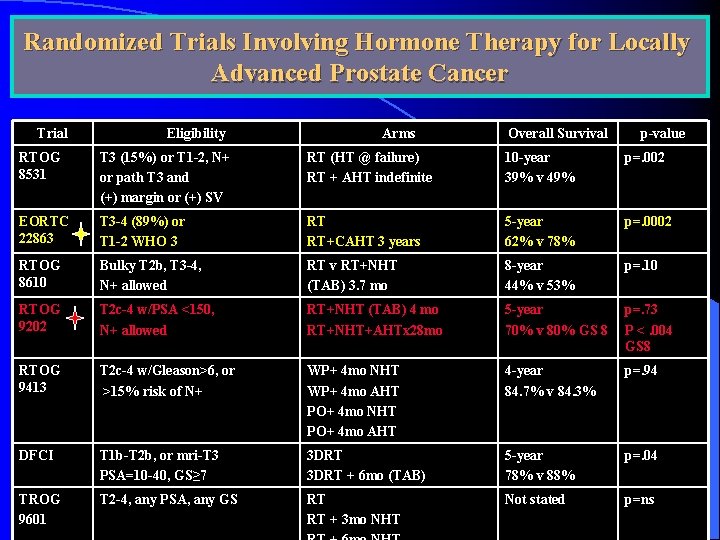
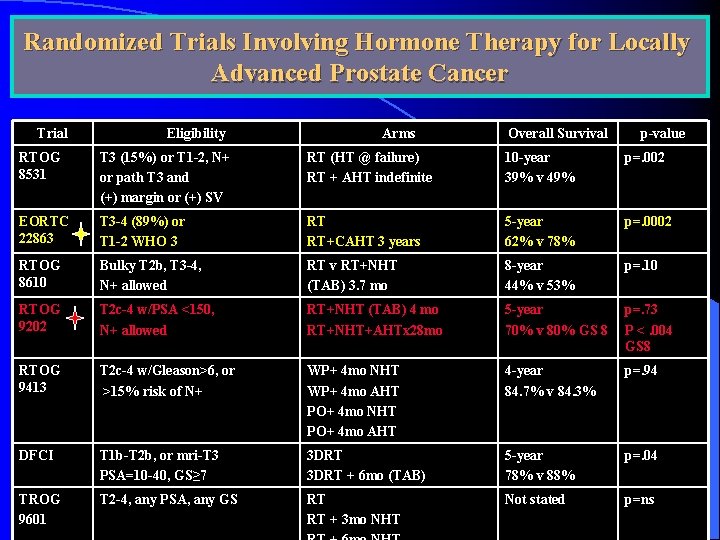
Randomized Trials Involving Hormone Therapy for Locally Advanced Prostate Cancer Trial Eligibility Arms Overall Survival p-value RTOG 8531 T 3 (15%) or T 1 -2, N+ or path T 3 and (+) margin or (+) SV RT (HT @ failure) RT + AHT indefinite 10 -year 39% v 49% p=. 002 EORTC 22863 T 3 -4 (89%) or T 1 -2 WHO 3 RT RT+CAHT 3 years 5 -year 62% v 78% p=. 0002 RTOG 8610 Bulky T 2 b, T 3 -4, N+ allowed RT v RT+NHT (TAB) 3. 7 mo 8 -year 44% v 53% p=. 10 RTOG 9202 T 2 c-4 w/PSA <150, N+ allowed RT+NHT (TAB) 4 mo RT+NHT+AHTx 28 mo 5 -year 70% v 80% GS 8 p=. 73 P <. 004 GS 8 RTOG 9413 T 2 c-4 w/Gleason>6, or >15% risk of N+ WP+ 4 mo NHT WP+ 4 mo AHT PO+ 4 mo NHT PO+ 4 mo AHT 4 -year 84. 7% v 84. 3% p=. 94 DFCI T 1 b-T 2 b, or mri-T 3 PSA=10 -40, GS≥ 7 3 DRT + 6 mo (TAB) 5 -year 78% v 88% p=. 04 TROG 9601 T 2 -4, any PSA, any GS RT RT + 3 mo NHT Not stated p=ns
X. Comparing Modalities
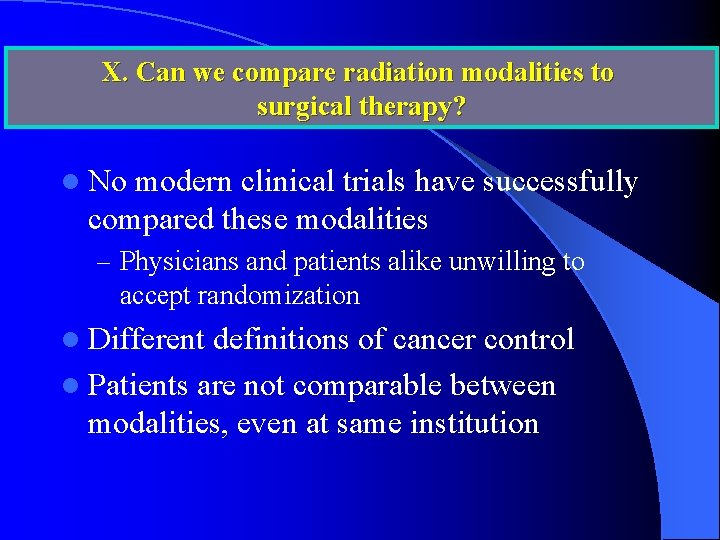
X. Can we compare radiation modalities to surgical therapy? l No modern clinical trials have successfully compared these modalities – Physicians and patients alike unwilling to accept randomization l Different definitions of cancer control l Patients are not comparable between modalities, even at same institution
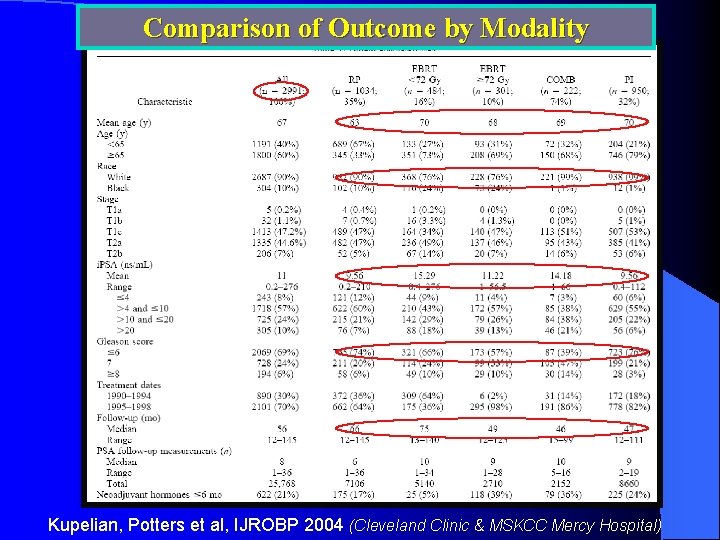
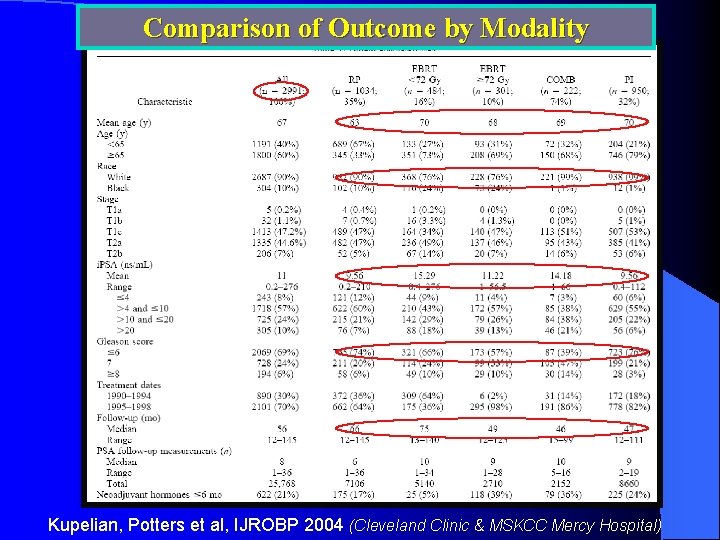
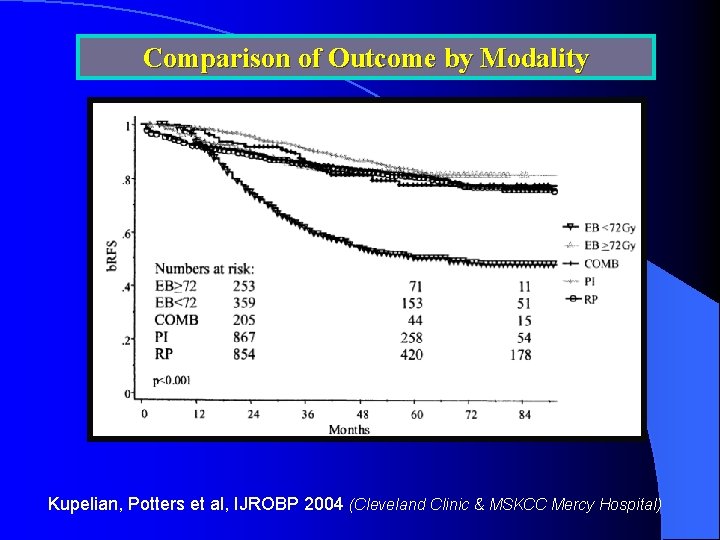
Comparison of Outcome by Modality Kupelian, Potters et al, IJROBP 2004 (Cleveland Clinic & MSKCC Mercy Hospital)
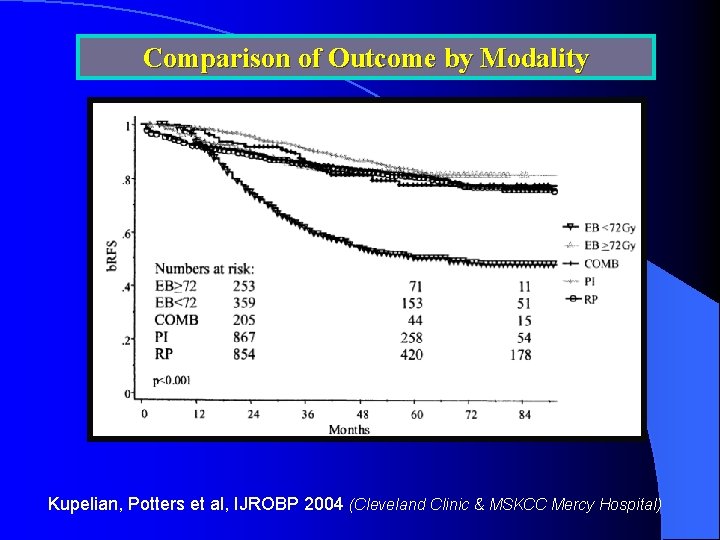
Comparison of Outcome by Modality Kupelian, Potters et al, IJROBP 2004 (Cleveland Clinic & MSKCC Mercy Hospital)
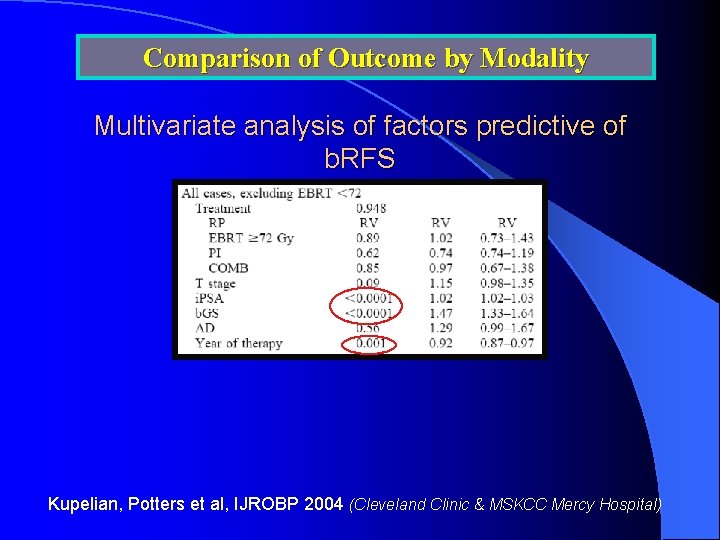
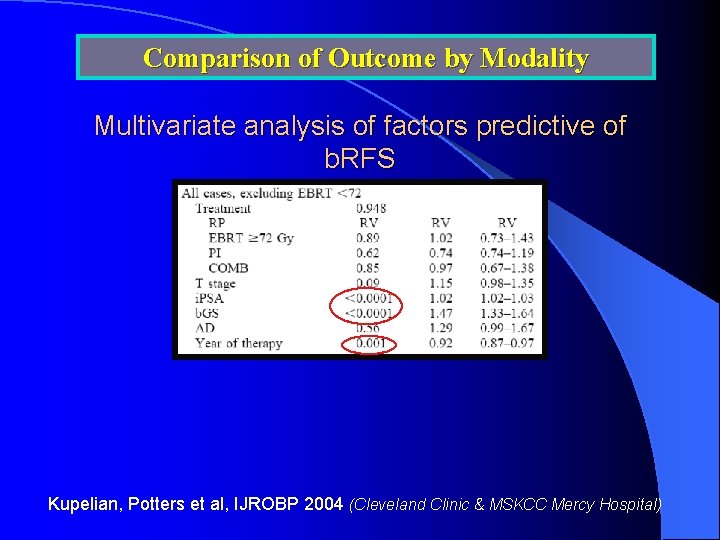
Comparison of Outcome by Modality Multivariate analysis of factors predictive of b. RFS Kupelian, Potters et al, IJROBP 2004 (Cleveland Clinic & MSKCC Mercy Hospital)
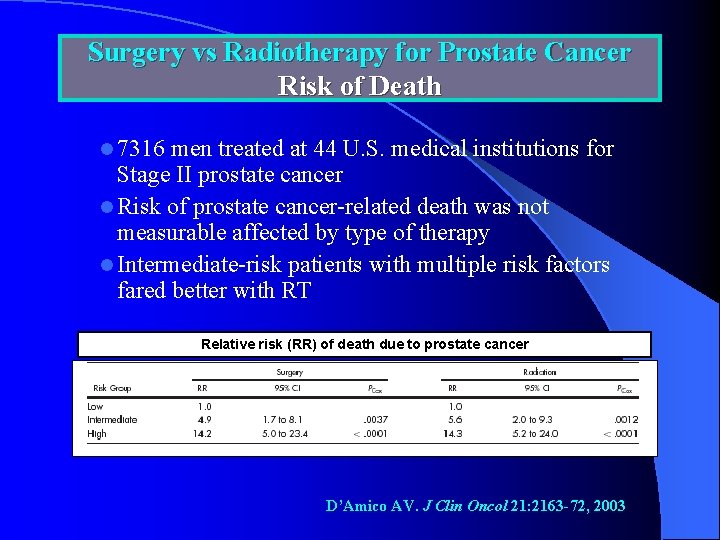
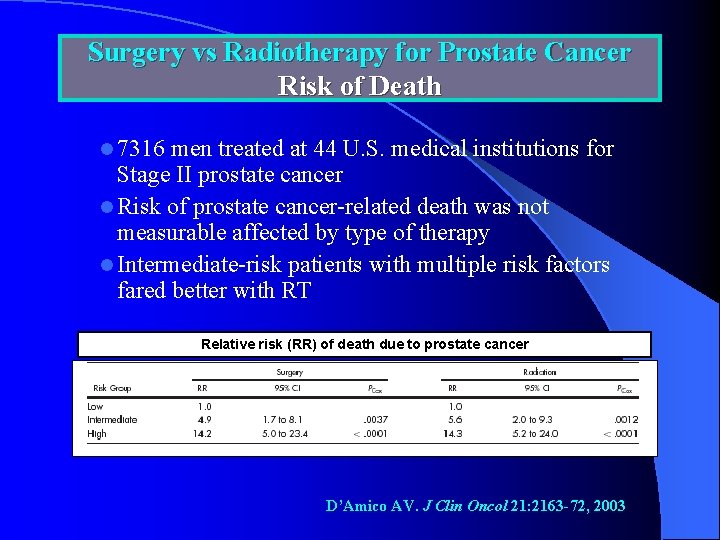
Surgery vs Radiotherapy for Prostate Cancer Risk of Death l 7316 men treated at 44 U. S. medical institutions for Stage II prostate cancer l Risk of prostate cancer-related death was not measurable affected by type of therapy l Intermediate-risk patients with multiple risk factors fared better with RT Relative risk (RR) of death due to prostate cancer D’Amico AV. J Clin Oncol 21: 2163 -72, 2003
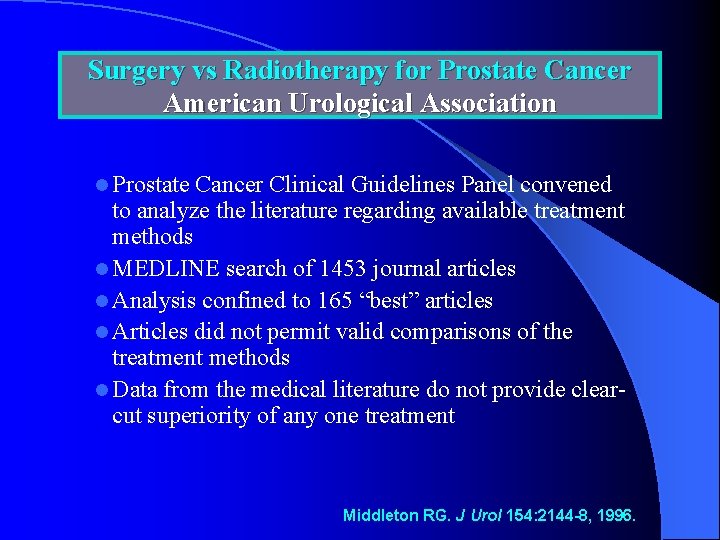
Surgery vs Radiotherapy for Prostate Cancer American Urological Association l Prostate Cancer Clinical Guidelines Panel convened to analyze the literature regarding available treatment methods l MEDLINE search of 1453 journal articles l Analysis confined to 165 “best” articles l Articles did not permit valid comparisons of the treatment methods l Data from the medical literature do not provide clearcut superiority of any one treatment Middleton RG. J Urol 154: 2144 -8, 1996.

XI. Quality of Life Comparison
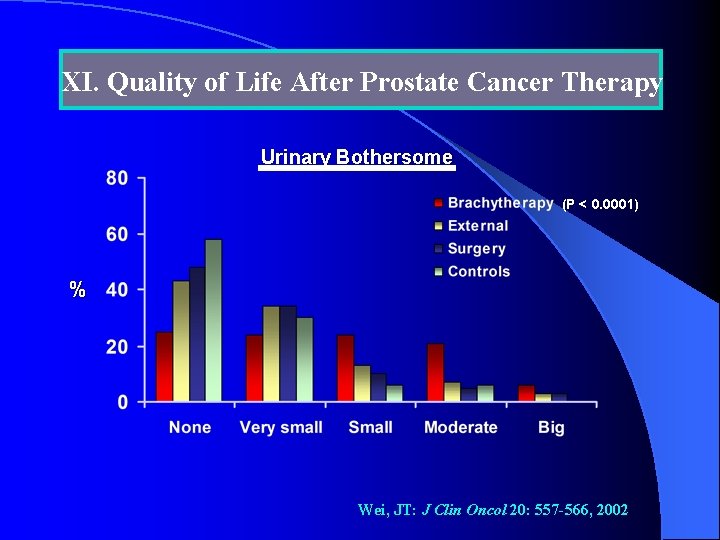
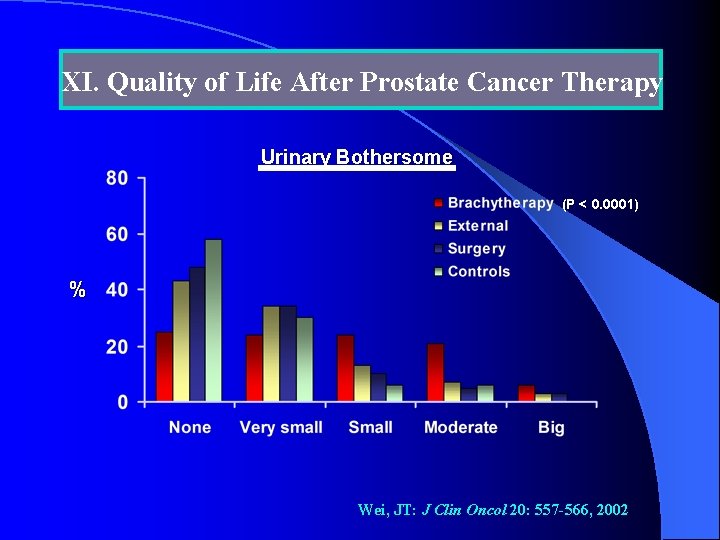
XI. Quality of Life After Prostate Cancer Therapy Urinary Bothersome (P < 0. 0001) % Wei, JT: J Clin Oncol 20: 557 -566, 2002
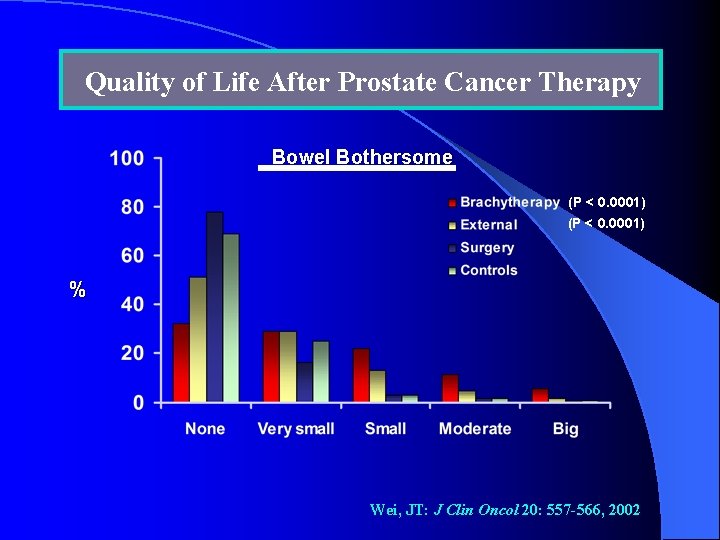
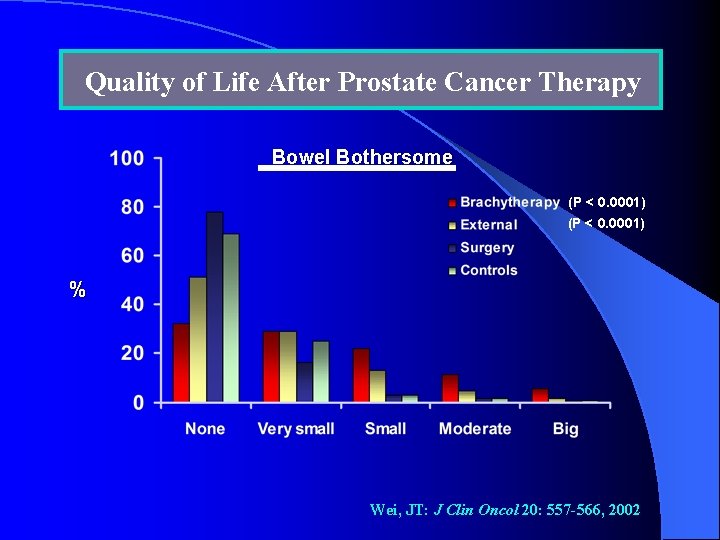
Quality of Life After Prostate Cancer Therapy Bowel Bothersome (P < 0. 0001) % Wei, JT: J Clin Oncol 20: 557 -566, 2002
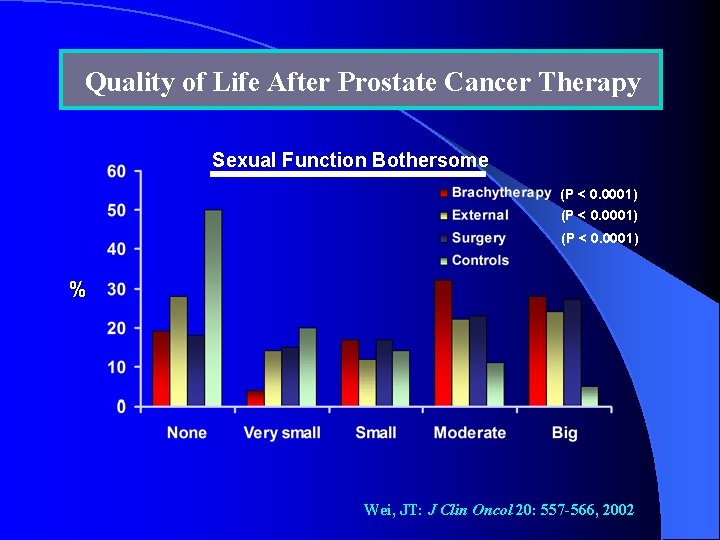
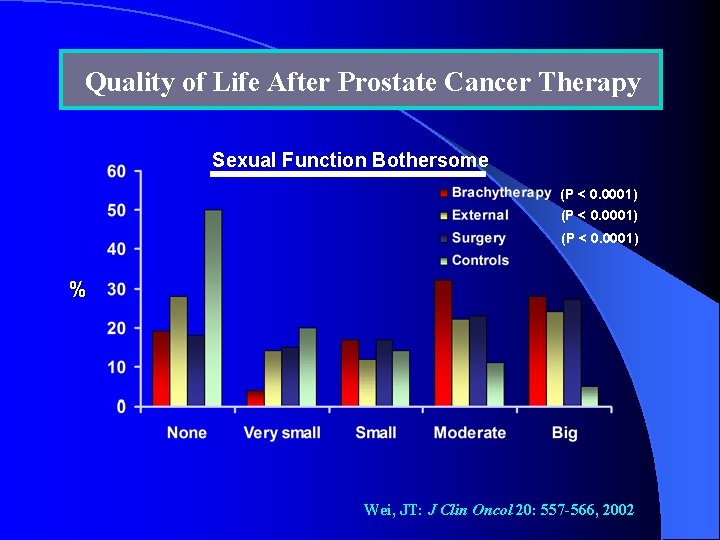
Quality of Life After Prostate Cancer Therapy Sexual Function Bothersome (P < 0. 0001) % Wei, JT: J Clin Oncol 20: 557 -566, 2002
XII. Conclusions
Factors Influencing Management Approach l l Patient expectations of medical care Patient understanding of & engagement in management of condition Patient preference for type of treatment Access of patient to each member of a multispecialty team
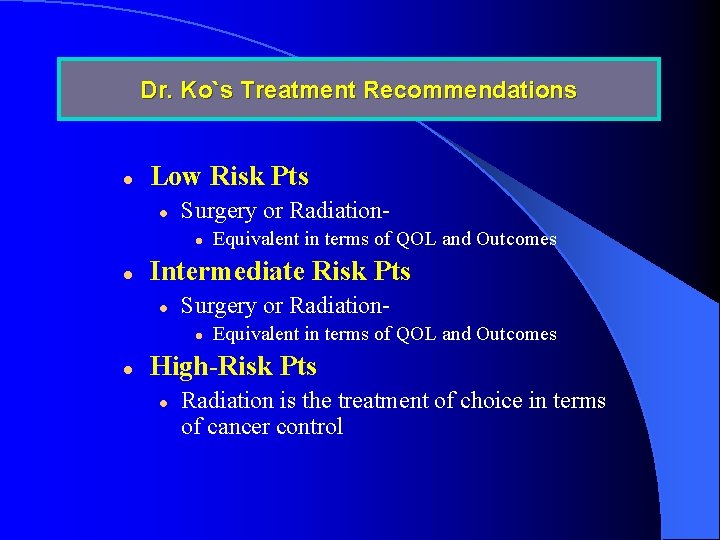
Dr. Ko`s Treatment Recommendations l Low Risk Pts l Surgery or Radiationl l Intermediate Risk Pts l Surgery or Radiationl l Equivalent in terms of QOL and Outcomes High-Risk Pts l Radiation is the treatment of choice in terms of cancer control
 Prostate
Prostate The new prostate cancer infolink
The new prostate cancer infolink Prostate cancer staging
Prostate cancer staging Prostate cancer tnm classification
Prostate cancer tnm classification Mdv3100 prostate cancer
Mdv3100 prostate cancer Espérance de vie après récidive cancer prostate
Espérance de vie après récidive cancer prostate Kolposkopi px
Kolposkopi px Treatment of inflammatory breast cancer
Treatment of inflammatory breast cancer Radiation therapy side effects
Radiation therapy side effects Proton therapy for breast cancer after mastectomy
Proton therapy for breast cancer after mastectomy Nhti radiation therapy
Nhti radiation therapy Intensity modulated radiation therapy
Intensity modulated radiation therapy Gvsu radiation therapy
Gvsu radiation therapy Reality therapy
Reality therapy Bioness integrated therapy system price
Bioness integrated therapy system price Psychoanalytic vs humanistic
Psychoanalytic vs humanistic Humanistic therapy aims to
Humanistic therapy aims to Function of the ductus deferens
Function of the ductus deferens Protocole irm prostate
Protocole irm prostate Alfazusin
Alfazusin Hypointenz
Hypointenz Viscerosomatic reflex
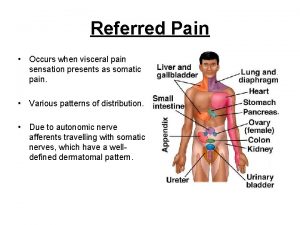
Viscerosomatic reflex Prostate glands
Prostate glands Prostate pathology
Prostate pathology Prostate referred pain
Prostate referred pain Cystocatheter
Cystocatheter Primary sex organ of the male reproductive system? *
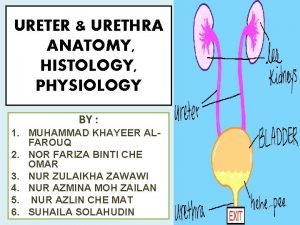
Primary sex organ of the male reproductive system? * Ureter physiology
Ureter physiology Eduard baco
Eduard baco Score de gleason
Score de gleason Prostate histology
Prostate histology Normal weight of prostate
Normal weight of prostate Prostate
Prostate Prostatic adenocarcinoma
Prostatic adenocarcinoma Inguinocele
Inguinocele Prostate pathology
Prostate pathology Tuip prostate
Tuip prostate Prostate
Prostate Dorsal vein of the penis
Dorsal vein of the penis Anatomie zonale de mac neal
Anatomie zonale de mac neal Inköpsprocessen steg för steg
Inköpsprocessen steg för steg Påbyggnader för flakfordon
Påbyggnader för flakfordon Egg för emanuel
Egg för emanuel Sura för anatom
Sura för anatom Formel gruplar
Formel gruplar Rutin för avvikelsehantering
Rutin för avvikelsehantering Trög för kemist
Trög för kemist Presentera för publik crossboss
Presentera för publik crossboss Treserva lathund
Treserva lathund Tack för att ni lyssnade
Tack för att ni lyssnade Debattartikel mall
Debattartikel mall Tack för att ni lyssnade bild
Tack för att ni lyssnade bild En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Mall för referat
Mall för referat Tack för att ni har lyssnat
Tack för att ni har lyssnat Bris för vuxna
Bris för vuxna Programskede byggprocessen
Programskede byggprocessen Gumman cirkel sång
Gumman cirkel sång Rbk mätning
Rbk mätning Arkimedes princip formel
Arkimedes princip formel Vad är densitet
Vad är densitet Elektronik för barn
Elektronik för barn Var 1721 för stormaktssverige
Var 1721 för stormaktssverige Tack för att ni har lyssnat
Tack för att ni har lyssnat Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Sju principer för tillitsbaserad styrning
Sju principer för tillitsbaserad styrning Luftstrupen för medicinare
Luftstrupen för medicinare Vilket tal pekar pilen på
Vilket tal pekar pilen på Autokratiskt ledarskap
Autokratiskt ledarskap Returpilarna
Returpilarna