PROSTATE NORMAL STRUCTURE OF PROSTATE NODULAR HYPERPLASIA CARCINOMA

- Slides: 45
PROSTATE
• NORMAL STRUCTURE OF PROSTATE • NODULAR HYPERPLASIA • CARCINOMA OF PROSTATE
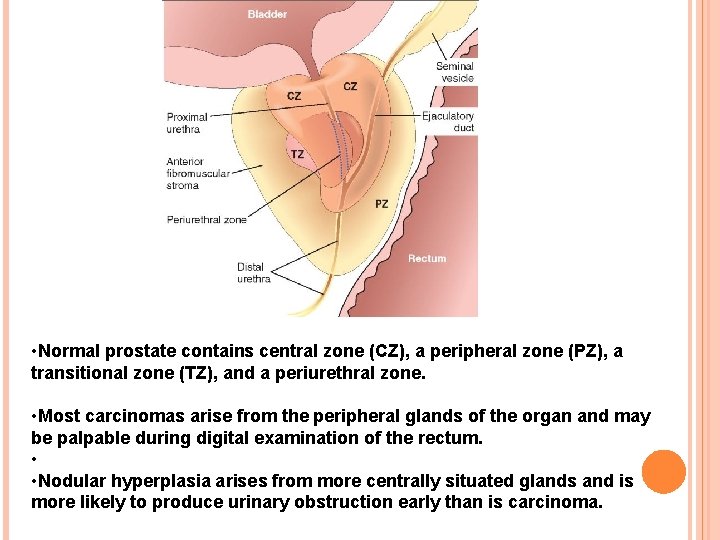
NORMAL STRUCTURE Prostate gland in the normal adult weighs approximately 20 gm. Prostate is a retroperitoneal organ encircling the neck of the bladder and urethra, and is devoid of a distinct capsule. Composed of 5 lobes during embryonic development— anterior, middle, posterior and two lateral lobes.
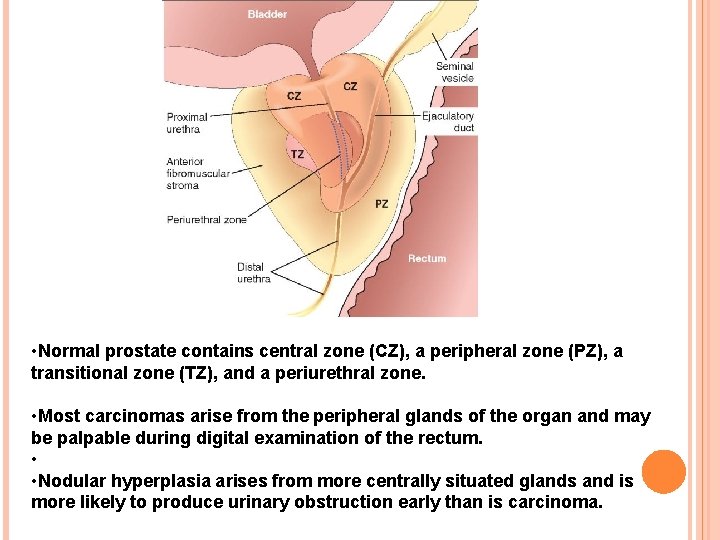
• Normal prostate contains central zone (CZ), a peripheral zone (PZ), a transitional zone (TZ), and a periurethral zone. • Most carcinomas arise from the peripheral glands of the organ and may be palpable during digital examination of the rectum. • • Nodular hyperplasia arises from more centrally situated glands and is more likely to produce urinary obstruction early than is carcinoma.
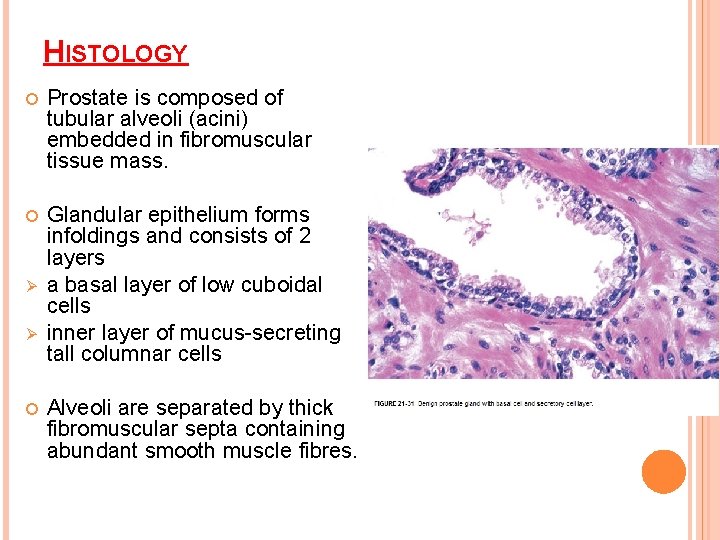
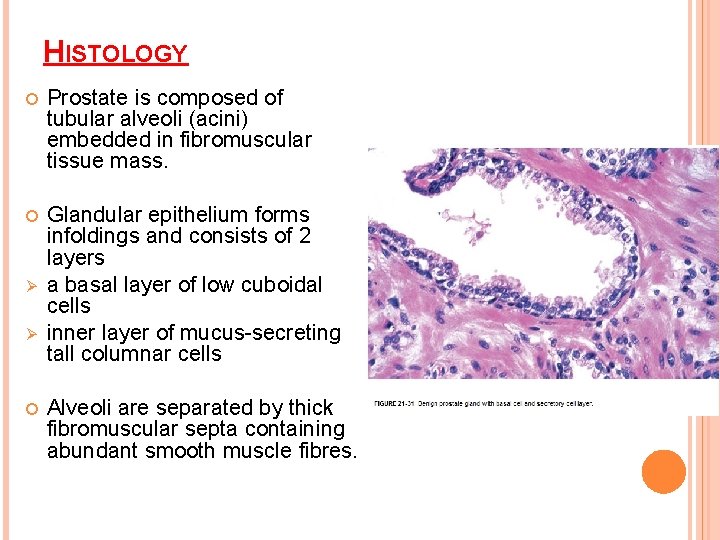
HISTOLOGY Prostate is composed of tubular alveoli (acini) embedded in fibromuscular tissue mass. Glandular epithelium forms infoldings and consists of 2 layers a basal layer of low cuboidal cells inner layer of mucus-secreting tall columnar cells Ø Ø Alveoli are separated by thick fibromuscular septa containing abundant smooth muscle fibres.
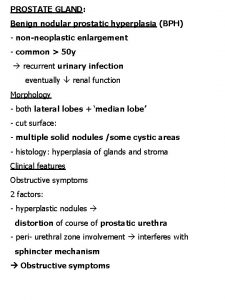
NODULAR HYPERPLASIA Non-neoplastic tumour-like enlargement of the prostate Commonly termed benign nodular hyperplasia (BNH) or benign enlargement of prostate (BEP) Very common condition in men and considered by some as normal ageing process.
More frequent above the age of 50 years and its incidence approaches 75 -80% in men above 80 years. Symptomatic BEP producing urinary tract obstruction and requiring surgical treatment occurs in 5 -10% of cases only.
ETIOLOGY Etiologic factors Endocrinologic Racial Inflammation Arteriosclerosis
ETIOLOGY With advancing age, there is decline in the level of androgen and a corresponding rise of oestrogen in the males. Periurethral inner prostate which is primarily involved in BEP is responsive to the rising level of oestrogen, whereas the outer prostate which is mainly involved in the carcinoma is responsive to androgen. Plausible hypothesis: there is synergistic stimulation of the prostate by both hormones—the oestrogen acting to sensitise the prostatic tissue to the growth promoting effect of dihydroxy-testosterone derived from plasma testosterone.
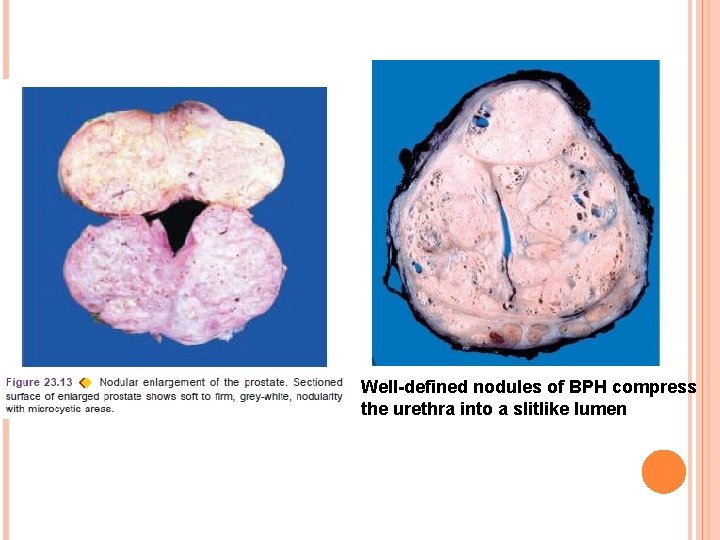
MORPHOLOGIC FEATURES Grossly Enlarged prostate is nodular, smooth and firm and weighs 2 -4 times its normal weight i. e. may weigh up to 40 -80 gm. Cut section varies depending upon whether the hyperplasia is predominantly of the glandular or fibromuscular tissue. In glandular BEP tissue is yellow-pink, soft, honeycombed, and milky fluid exudes In mainly fibromuscular BEP firm, homogeneous and does not exude milky fluid.
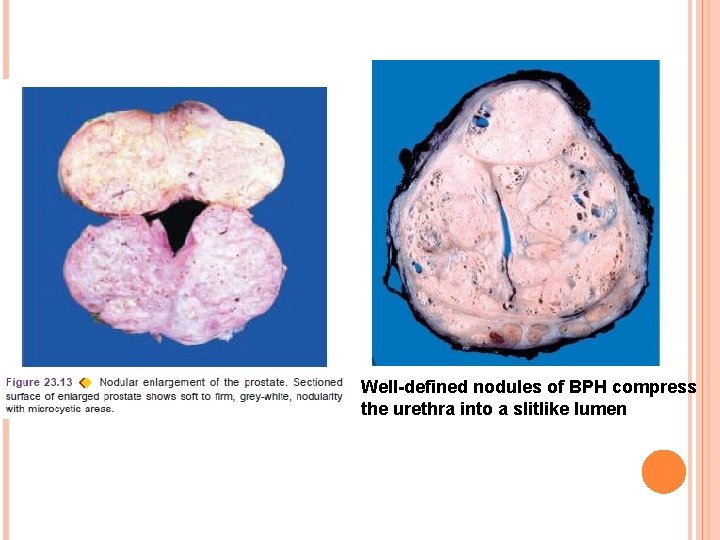
Well-defined nodules of BPH compress the urethra into a slitlike lumen
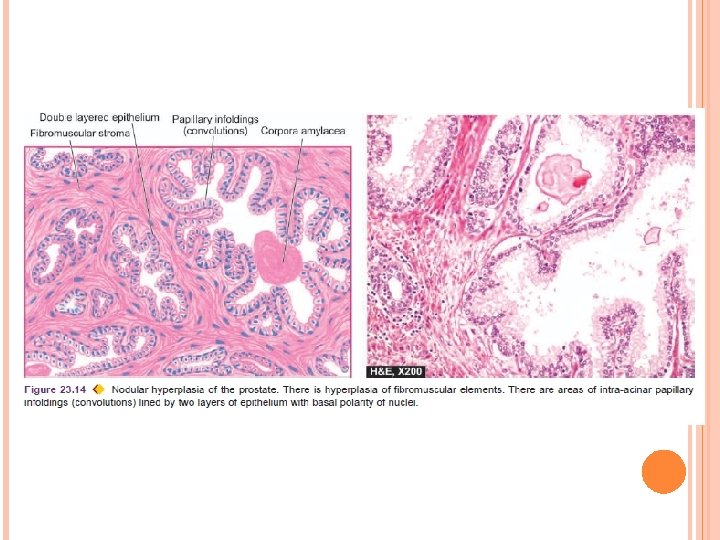
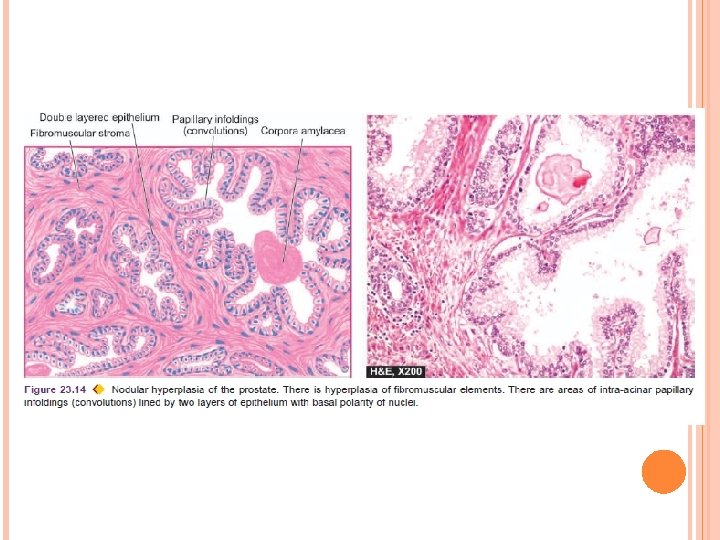
HISTOLOGICALLY Hyperplasia of all three tissue elements in varying proportions—glandular, fibrous and muscular. Glandular hyperplasia is identified by exaggerated intra-acinar papillary infoldings with delicate fibrovascular cores. Lining epithelium is two-layered: the inner tall columnar mucus secreting with poorly-defined borders, and the outer cuboidal to flattened epithelium with basal nuclei.
Fibromuscular hyperplasia when present appears as aggregates of spindle cells forming an appearance akin to fibromyoma of the uterus. Other histologic features include foci of lymphocytic aggregates small areas of infarction corpora amylacea foci of squamous metaplasia Ø Ø
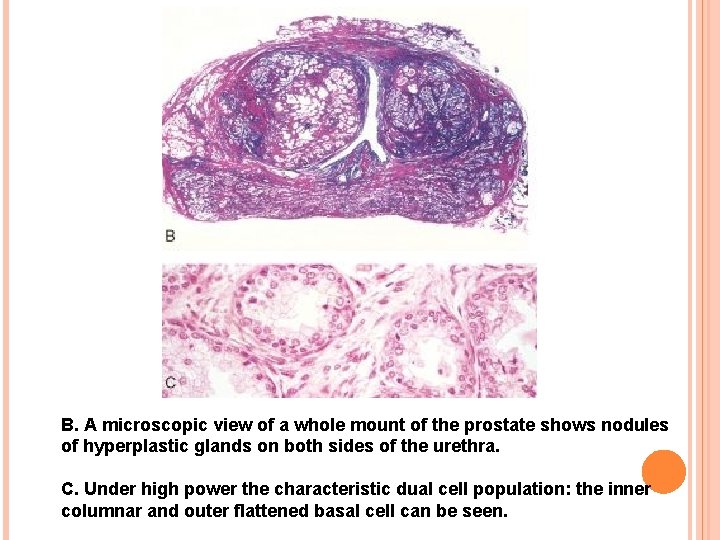
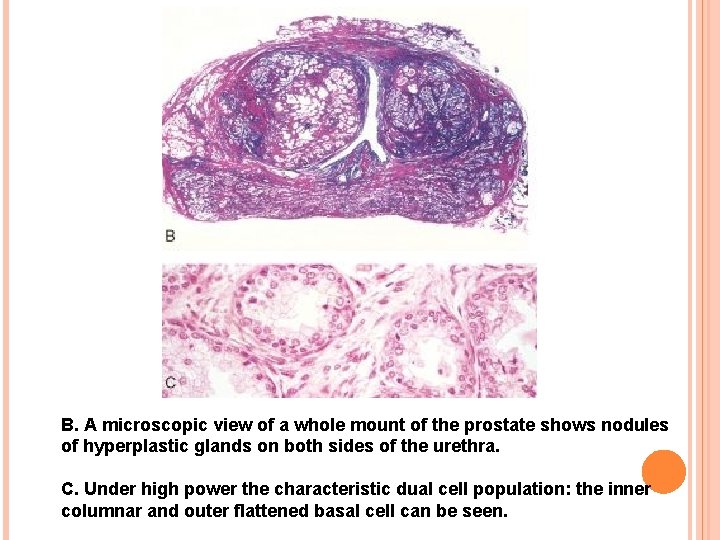
B. A microscopic view of a whole mount of the prostate shows nodules of hyperplastic glands on both sides of the urethra. C. Under high power the characteristic dual cell population: the inner columnar and outer flattened basal cell can be seen.
CLINICAL FEATURES Symptomatic cases develop symptoms due to complications such as urethral obstruction and secondary effects on the bladder (e. g. hypertrophy, cystitis), ureter (e. g. hydroureter) and kidneys (e. g. hydronephrosis). Presenting features include Frequency Nocturia difficulty in micturition Pain haematuria Sometimes present with acute retention of urine requiring immediate catheterisation. Ø Ø Ø
CARCINOMA OF PROSTATE Second most common form of cancer in males, followed in frequency by lung cancer. Disease of men above the age of 50 years Its prevalence increases with increasing age so that more than 50% of men 80 years old have asymptomatic (latent) carcinoma of the prostate. Many a times, carcinoma of the prostate is small and detected as microscopic foci in a prostate removed for BEP or found incidentally at autopsy.
4 TYPES: 1. Latent carcinoma. Found unexpectedly as a small focus of carcinoma in the prostate during autopsy studies in men dying of other causes. Incidence in autopsies - 25 -35%. 2. Incidental carcinoma. About 15 -20% of prostatectomies done for BEP reveal incidental carcinoma of the prostate. 3. Occult carcinoma. Patient has no symptoms of prostatic carcinoma but shows evidence of metastases on clinical examination and investigations. 4. Clinical carcinoma. Detected by rectal examination and other investigations and confirmed by pathologic examination of biopsy of the prostate.
ETIOLOGY 1. Endocrinologic factors 2. Racial and geographic influences 3. Environmental influences 4. Nodular hyperplasia 5. Heredity
1. Endocrinologic factors. Androgens are considered essential for development and maintenance of prostatic epithelium and are responsible for causing malignant transformation. Etiologic role of androgens is supported by the following indirect evidences: i) Orchiectomy causes arrest of metastatic prostatic cancer disease. ii) Administration of oestrogen causes regression of prostatic carcinoma. iii) Cancer of the prostate is extremely rare in eunuchs and in patients with Klinefelter’s syndrome. iv) Cancer of the prostate begins at the stage of life when androgen levels are high.
2. Racial and geographic influences. It is uncommon in Japanese and Chinese, while the prevalence is high in Americans. African Americans have a markedly higher incidence as compared to whites which may be related to genetic variation in androgen receptor gene.
3. Environmental influences. High dietary fat, and exposure to polycyclic aromatic hydrocarbons increase risk. Flavonoids, antioxidants and selenium may reduce the risk.
4. Nodular hyperplasia. Though nodular prostatic hyperplasia has been suggested by some as precursor for development of prostatic cancer, it is considered unlikely. Approximately 15 -20% of nodular hyperplastic prostates harbour carcinoma.
5. Heredity. The possibility of genetic basis of prostatic cancer has been suggested by the observations of familial clustering and 2 -fold higher frequency in firstdegree relatives. Prostatic cancer susceptibility gene has been identified in familial cases.
HISTOGENESIS Mutistep process arising from premalignant stage of prostatic intraepithelial neoplasia (PIN). PIN refers to multiple foci of cytologically atypical luminal cells overlying diminished number of basal cells in prostatic ducts and is a forerunner of invasive prostatic carcinoma. Based on cytologic atypia, PIN may be low grade to high grade. PIN of high-grade progresses to prostatic adenocarcinoma.
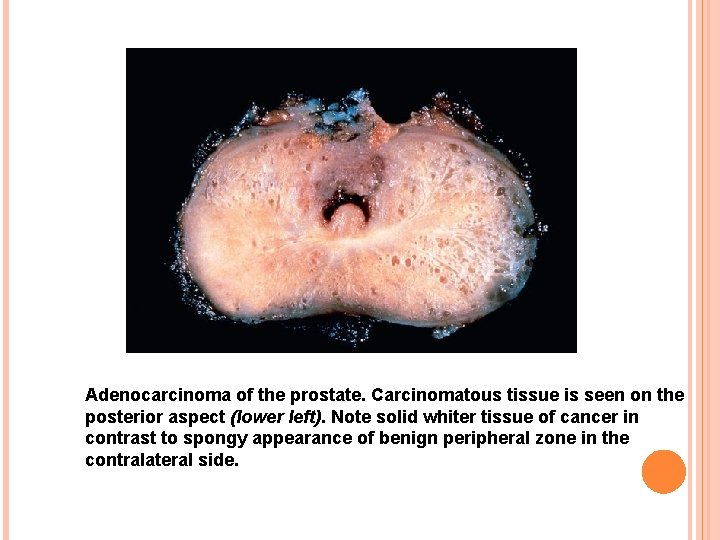
MORPHOLOGIC FEATURES Grossly Prostate may be enlarged, normal in size or smaller than normal. In 95% of cases, prostatic carcinoma is located in the peripheral zone, especially in the posterior lobe. Malignant prostate is firm and fibrous. Cut section is homogeneous and contains irregular yellowish areas.
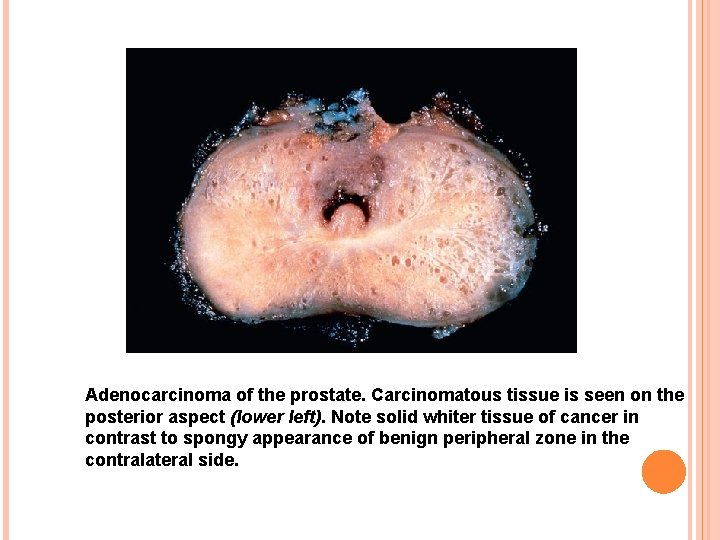
Adenocarcinoma of the prostate. Carcinomatous tissue is seen on the posterior aspect (lower left). Note solid whiter tissue of cancer in contrast to spongy appearance of benign peripheral zone in the contralateral side.
MICROSCOPICALLY Ø Ø 4 histologic types are described— Adenocarcinoma Transitional cell carcinoma Squamous cell carcinoma undifferentiated carcinoma Adenocarcinoma is the most common type found in 96% of cases and is the one generally referred to as carcinoma of the prostate.
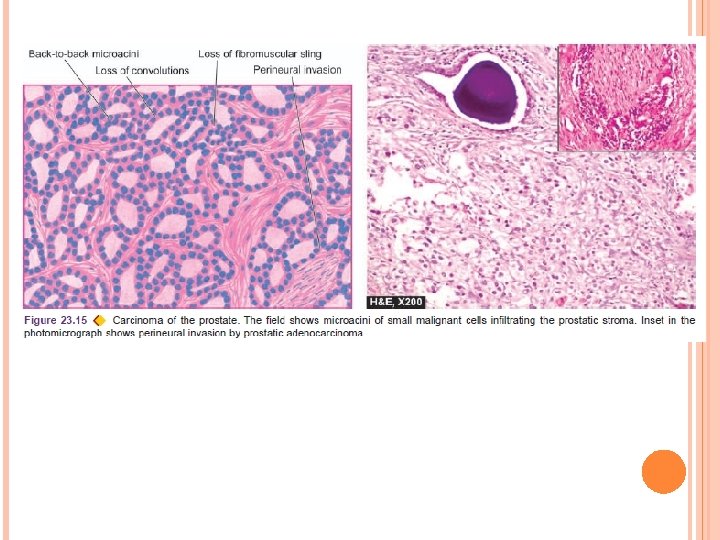
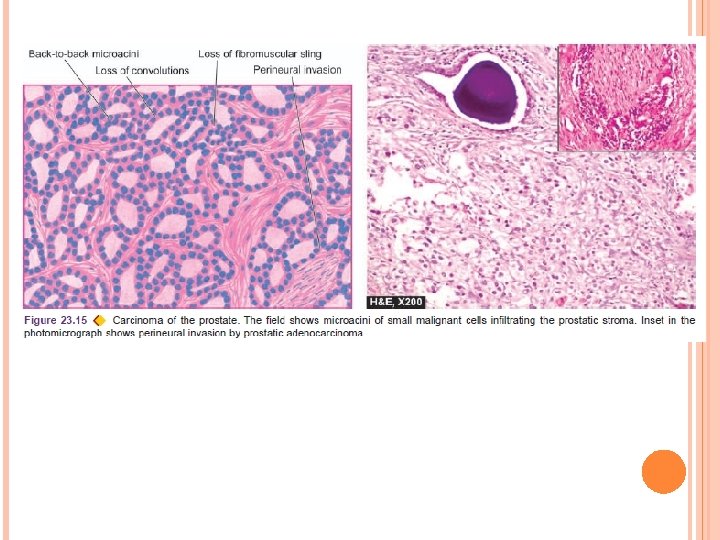
Histologic characteristics of adenocarcinoma of the prostate are: 1. Architectural disturbance. There is loss of intra-acinar papillary convolutions. Groups of acini are either closely packed in back-to-back arrangement without intervening stroma or are haphazardly distributed. 2. Stroma. Normally, fibromuscular sling surrounds the acini, whereas malignant acini have little or no stroma between them. Tumour cells may penetrate and replace the fibromuscular stroma.
3. Gland pattern. Glands in welldifferentiated prostatic adenocarcinoma are small or medium-sized, lined by a single layer of cuboidal or low columnar cells. Moderately-differentiated tumours have cribriform or fenestrated glandular appearance. Poorlydifferentiated tumours have little or no glandular arrangement but instead show solid or trabecular pattern.
4. Tumour cells. Individual tumour cells in prostatic carcinoma do not show usual morphologic features of malignancy. Tumour cells may be clear, dark and eosinophilic cells. Clear cells have foamy cytoplasm, dark cells have homogeneous basophilic cytoplasm, and eosinophilic cells have granular cytoplasm. Cells may show varying degree of anaplasia and nuclear atypia but is generally slight.
5. Invasion. One of the important diagnostic features of malignancy in prostate is the early and frequent occurrence of invasion of intra-prostatic perineural spaces. Lymphatic and vascular invasion may be present but are difficult to detect.
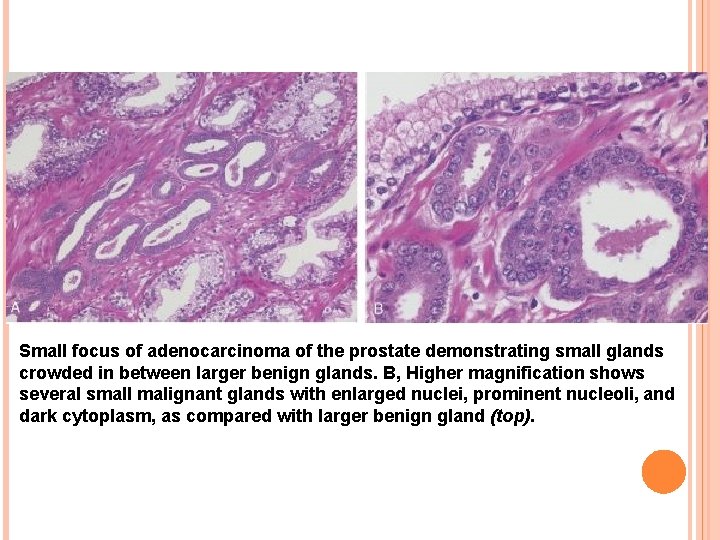
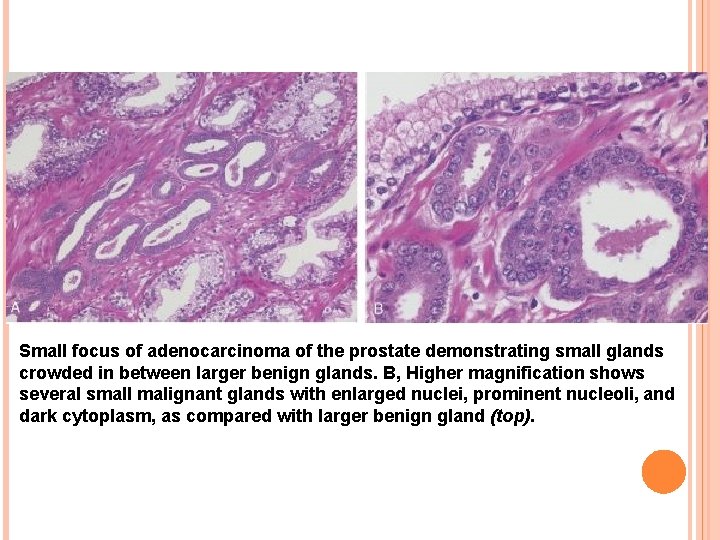
Small focus of adenocarcinoma of the prostate demonstrating small glands crowded in between larger benign glands. B, Higher magnification shows several small malignant glands with enlarged nuclei, prominent nucleoli, and dark cytoplasm, as compared with larger benign gland (top).
SPREAD Tumour spreads within the gland by direct extension, and to distant sites by metastases. Direct spread. Direct extension of the tumour occurs into the prostatic capsule and beyond. In late stage, the tumour may extend into the bladder neck, seminal vesicles, trigone and ureteral openings.
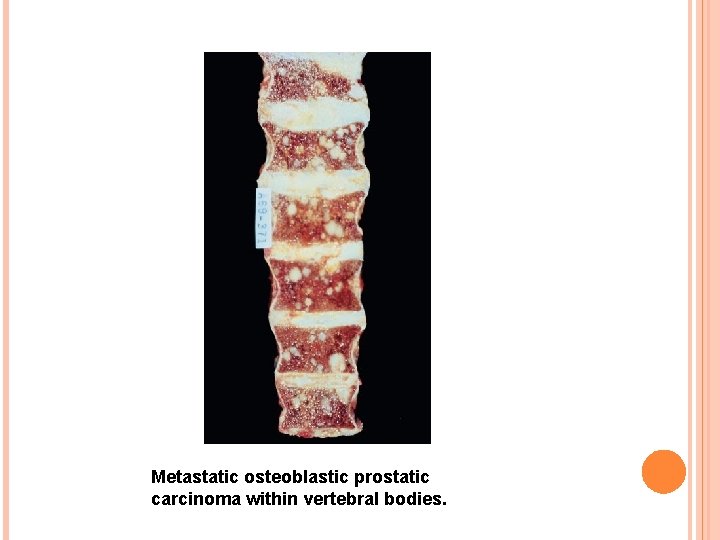
Metastases. Distant spread occurs by both lymphatic and haematogenous routes. Rich lymphatic network surrounding the prostate is the main mode of spread to the sacral, iliac and para-aortic lymph nodes. Earliest metastasis occur to the obturator lymph node. Haematogenous spread leads most often to characteristic osteoblastic osseous metastases, especially to pelvis, and lumbar spine; other sites of metastases are lungs, kidneys, breast and brain. Route of blood-borne metastases may be retrograde spread by prostatic venous plexus or via systemic circulation.
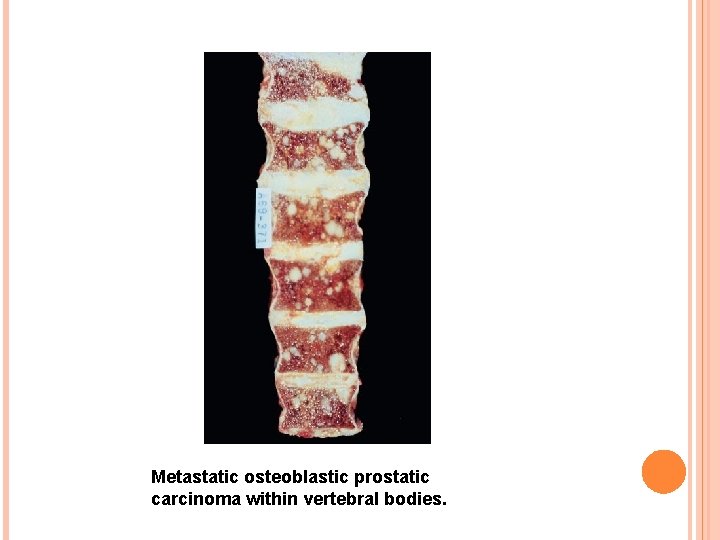
Metastatic osteoblastic prostatic carcinoma within vertebral bodies.
CLINICAL FEATURES By the time symptoms appear, the carcinoma of prostate is usually palpable on rectal examination as a hard and nodular gland fixed to the surrounding tissues. In symptomatic cases, clinical features are: Urinary obstruction with dysuria Frequency Retention of urine Haematuria In 10% of cases pain in the back due to skeletal metastases. Ø Ø Ø
STAGING OF CARCINOMA PROSTATE Clinical staging of carcinoma prostate takes into account the following: Ø Tumour found incidentally or a clinically unsuspected cancer in prostate removed for benign disorder (Stage A). Ø Tumour palpable by rectal digital examination but confined to the prostate (Stage B). Ø Ttumour has extended locally beyond the prostate into the surrounding tissues (Stage C). Ø Tumour is associated with distant metastases (Stage D).
HISTOLOGIC GRADING Ø Ø Ø Mostofi’s (WHO) histologic grading categorising prostate cancer into grade I (well-differentiated) grade II (moderately differentiated) grade III (poorly differentiated) Replaced with Gleason’s microscopic grading system which is based on two features: i) Degree of glandular differentiation. ii) Growth pattern of the tumour in relation to the stroma.
For clinical staging of prostate cancer, TNM system is considered international standard. Diagnosis of prostatic carcinoma is made by cytologic, biochemical, radiologic ultrasonographic and pathologic methods. Definite diagnosis is established by histopathologic examination of transrectal ultrasound (TRUS)guided core needle biopsy.
DIAGNOSIS Two serum tumour markers employed commonly for diagnosis and monitoring the prognosis of prostatic carcinoma are: 1. Prostatic acid phosphatase (PAP) Secreted by prostatic epithelium. Elevation of serum level of PAP is found in cases of prostatic cancer which have extended beyond the capsule or have metastasised. PAP can also be demonstrated in the normal prostatic tissues.
2. Prostate-specific antigen (PSA) Detected by immunohistochemical method in the malignant prostatic epithelium as well as estimated in the serum. A reading between 4 and 10 (normal 0 -4 ng/ml) is highly suspicious (10% risk) but value above 10 is diagnostic of prostatic carcinoma. PSA assay is useful in deciding whether the metastasis originated from the prostate or not. PSA assay is also helpful in distinguishing high-grade prostatic cancer from urothelial carcinoma, colonic carcinoma, lymphoma and prostatitis. PSA level is generally higher in low-grade tumours than in high-grade tumours.
TREATMENT Treatment of prostatic carcinoma consists of surgery, radiotherapy and hormonal therapy. Hormonal dependence of prostate cancer consists of depriving the tumour cells of growth-promoting influence of testosterone. Achieved by bilateral orchiectomy followed by administration of oestrogen. Surgical approaches for prostate cancer include transurethral resection (TUR), radical prostatectomy and transurethral US-guided laser-induced prostatectomy (TULIP).

 Nodular hyperplasia
Nodular hyperplasia Normal weight of prostate
Normal weight of prostate Normal prostate mri images
Normal prostate mri images Non classical adrenal hyperplasia
Non classical adrenal hyperplasia Congenital adrenal hyperplasia characteristics
Congenital adrenal hyperplasia characteristics 17 hydroxyprogesterone levels
17 hydroxyprogesterone levels Virilisation in females
Virilisation in females Projektov�� mana����r
Projektov�� mana����r Sebaceous hyperplasia
Sebaceous hyperplasia Fundus mirigy hyperplasia
Fundus mirigy hyperplasia Congenital adrenal hyperplasia genitalia
Congenital adrenal hyperplasia genitalia Intimal hyperplasia
Intimal hyperplasia Hyperplasia
Hyperplasia Intimal hyperplasia
Intimal hyperplasia Dianne zwicke
Dianne zwicke Gingival hyperplasia
Gingival hyperplasia Intimal hyperplasia
Intimal hyperplasia Mineralocorticoid function
Mineralocorticoid function Gallbladder histology drawing
Gallbladder histology drawing Example of physiological hyperplasia
Example of physiological hyperplasia Hyperplasia and hypertrophy difference
Hyperplasia and hypertrophy difference Nodular melanoma
Nodular melanoma Nodular melanoma
Nodular melanoma Melanoma texture
Melanoma texture Fonte cenusii
Fonte cenusii Gastrite nodular antral
Gastrite nodular antral Enlarged thyroid gland
Enlarged thyroid gland Enlarged thyroid gland
Enlarged thyroid gland Nodular fasciitis
Nodular fasciitis Nodular fasciitis
Nodular fasciitis Nodular fasciitis
Nodular fasciitis Nodular fasciitis
Nodular fasciitis Quiste sebaceo ecografia
Quiste sebaceo ecografia Escabiose nodular
Escabiose nodular Giriniforme
Giriniforme Oil droplet reflex
Oil droplet reflex Aspiration biopsy
Aspiration biopsy Cervix carcinoma
Cervix carcinoma Renal cell carcinoma
Renal cell carcinoma Carcinoma in situ
Carcinoma in situ Md frcpc definition
Md frcpc definition Invasive ductal carcinoma with medullary features
Invasive ductal carcinoma with medullary features Manchester staging of breast cancer
Manchester staging of breast cancer Carcinoma de mama
Carcinoma de mama Carcinoma in situ
Carcinoma in situ Breast cancer biopsy
Breast cancer biopsy