Cancer Of The Prostate Prostate cancer is the









- Slides: 36

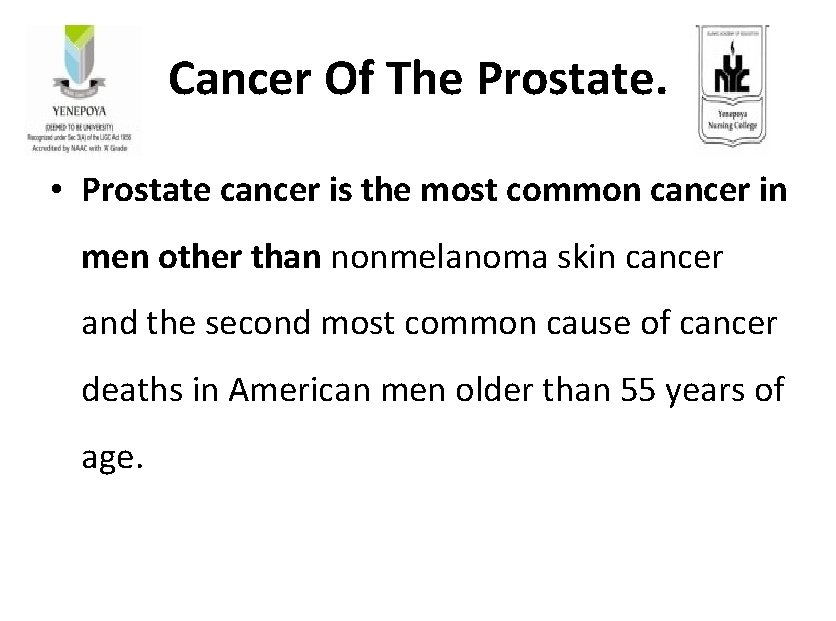
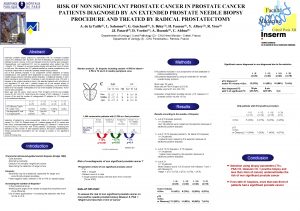
Cancer Of The Prostate. • Prostate cancer is the most common cancer in men other than nonmelanoma skin cancer and the second most common cause of cancer deaths in American men older than 55 years of age.
Risk Factors • • • Increasing age. Race /ethinicity Family history Hereditary breast and ovarian cancer. Other genetic changes Eating habits.
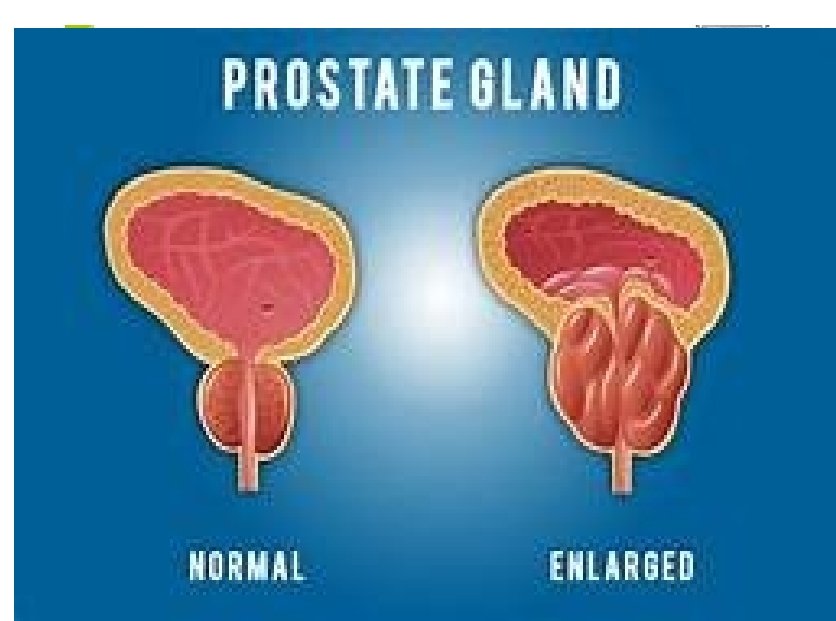
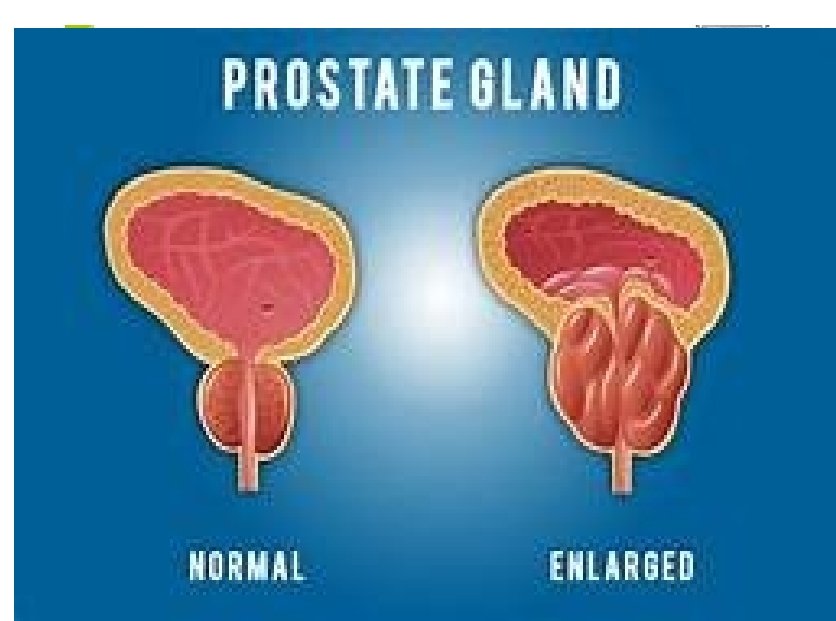
Pathophysiology. • Initially , small clumps of cancer cells remain confined to otherwise normal prostate glands, a condition known as carcinoma in situ or prostatic intraepithelial neoplasia(PIN). Over the time , these cancer cells spread to sorrounding prostate tissue forming a tumour.
• The cancer cells invade nearby organs such as seminal vesicles or rectum or travel in blood stream and lymphatic system.
Clinical Manifestations. • If the neoplasm is large enough to encroach on the bladder neck, signs and symptoms of urinary obstruction occur: difficulty and frequency of urination, urinary retention, and decreased size and force of the urinary stream.
• Hematuria may result if the cancer invades the urethra or bladder, or both. • Symptoms related to metastases include backache, hip pain, perineal and rectal discomfort, anemia, weight loss, weakness, nausea, and oliguria
Assessment and Diagnostic Findings. ü When prostate cancer is detected early, the likelihood of cure is high. Every man older than 40 years of age should have a DRE as part of his regular health checkup. ü Trans rectal ultrasound is also used.

ü Routine repeated rectal palpation of the gland (preferably by the same examiner) is important because early cancer may be detected as a nodule within the substance of the gland or as an extensive hardening in the posterior lobe.
ü The diagnosis of prostate cancer is confirmed by a histologic examination of tissue removed surgically by transurethral resection, open prostatectomy, or transrectal needle biopsy. ü Fine needle aspiration is a quick, painless method of obtaining prostate cells for cytologic examination.
ü PSA, a neutral serine protease, is produced by the normal and neoplastic ductal epithelium of the prostate and secreted into the glandular lumen. A simple blood test can be used to measure PSA levels.

Sexual Complications. • Men with prostate cancer commonly experience sexual dysfunction before the diagnosis is made. Each treatment for prostate cancer further increases the incidence of sexual problems. • With nerve-sparing radical prostatectomy, the chance of recovering erections is better for men who are younger and in whom both neurovascular bundles are spared.
Medical Management. • Treatment is based on the stage of the disease and the patient’s age and symptoms. Partin and associates (1997) combined PSA Level with the clinical stage and pathologic grade of the tumor to create a nomogram to predict the pathologic stage of localized prostate cancer.
• This nomogram can be useful in making treatment decisions and predicting treatment outcomes. Nursing care of the patient with cancer of the prostate is summarized in the Plan of Nursing Care.
Surgical Management. • A radical prostatectomy (removal of the prostate and seminal vesicles) remains the standard surgical procedure for patients who have early-stage, potentially curable disease and a life expectancy of 10 years or more.
Radiation Therapy. • If prostate cancer is detected in its early stage, the treatment may be curative radiation therapy: either teletherapy with a linear accelerator or interstitial irradiation (implantation of radioactive seeds of iodine or palladium),
Hormonal Therapy. • Hormonal therapy is one method used to control rather than cure prostate cancer. • Hormonal therapy for advanced prostate cancer suppresses androgenic stimuli to the prostate by decreasing the circulating plasma testosterone levels or interrupting the conversion to or binding of dihydrotestosterone.
• As a result, the prostatic epithelium atrophies (decreases). This effect is accomplished either by orchiectomy (removal of the testes) or by the administration of medications.
• Estrogen therapy, usually in the form of diethylstilbestrol (DES), has long been used to inhibit the gonadotropins responsible for testicular androgenic activity, thereby removing the androgenic hormone that promotes the growth of the malignancy.
• Cryosurgery of the prostate is used to ablate prostate cancer in patients who could not physically tolerate surgery or in those with recurrent prostate cancer.

Surgical Procedures. • Transurethral Resection Of The Prostate • TURP, the most common procedure used, can be carried out through endoscopy. The surgical and optical instrument is introduced directly through the urethra to the prostate, which can then be viewed directly. The gland is removed in small chips with an electrical cutting loop.

• Suprapubic Prostatectomy • Suprapubic prostatectomy is one method of removing the gland through an abdominal incision. An incision is made into the bladder, and the prostate gland is removed from above.

• Perineal Prostatectomy • Perineal prostatectomy involves removing the gland through an incision in the perineum
• Retropubic prostatectomy. • The surgeon makes a low abdominal incision and approaches the prostate gland between the pubic arch and the bladder without entering the bladder.
• Transurethral Incision Of The Prostate • Transurethral incision of the prostate (TUIP) is another procedure used in treating BPH. An instrument is passed through the urethra. One or two incisions are made in the prostate and prostate capsule to reduce the prostate’s pressure on the urethra and to reduce urethral constriction.
Laparoscopic Radical Prostatectomy. • The laparoscopic approach provides better visualization of the surgical site and surrounding areas. Preliminary data suggest that patients who undergo this procedure have less bleeding and reduced need for blood transfusion, a shorter hospital stay, less postoperative pain, and more rapid return to normal activity compared to open radical prostatectomy.

Nursing Assessment. Obtain History Collect information from physical examination. Assess the psychological reaction. Assess for signs and symptoms of urinary retention. • Assess the nutritional status. • •

Nursing Diagnosis. • Pain related to progression of disease and treatment modalities. • Urinary retention related to urethral obstruction secondary to prostatic enlargement or tumor and loss of bladder tone due to prolonged distention/retention.
Nursing Diagnosis. • Sexual dysfunction related to effects of therapy: chemotherapy, hormonal therapy, radiation therapy, surgery. • Altered nutrition: less than body requirements related to decreased oral intake because of anorexia, nausea, and vomiting. • Activity intolerance related to tissue hypoxia, malnutrition, and exhaustion
Nursing Interventions. • Assess for factors causing limited mobility (eg, pain, hypercalcemia, limited exercise tolerance). • Provide pain relief by administering prescribed medications. • Encourage use of assistive devices: cane, walker. • Involve significant others in helping patient with range-of-motion exercises, positioning, and walking.
Nursing Interventions. • Evaluate nature of patient’s pain, its location and intensity using pain rating scale. • Avoid activities that aggravate or worsen pain. • Because pain is usually related to bone metastasis, ensure that patient’s bed has a bed board on a firm mattress. Also, protect the patient from falls/injuries.

Nursing interventions. • Inform patient of the effects of prostate surgery, orchiectomy (when applicable), chemotherapy, irradiation, and hormonal therapy on sexual function. • Include his partner in developing understanding and in discovering alternative, satisfying close relations with each other.
THANK YOU.
 Mdv3100 prostate cancer
Mdv3100 prostate cancer Quel taux de psa pour un cancer de la prostate ?
Quel taux de psa pour un cancer de la prostate ? Prostate
Prostate Laprp
Laprp Prostate cancer staging
Prostate cancer staging Prostate cancer tnm classification
Prostate cancer tnm classification Irm prostate
Irm prostate Normal weight of prostate
Normal weight of prostate Pi-rads v
Pi-rads v Prostatic adenocarcinoma
Prostatic adenocarcinoma Prostate organ
Prostate organ Base of prostate gland
Base of prostate gland Prostate
Prostate Celine duperron
Celine duperron Male urethra anatomy
Male urethra anatomy Irm de prostate
Irm de prostate Adenocarcinome prostate
Adenocarcinome prostate Function of prostate gland
Function of prostate gland Base of prostate gland
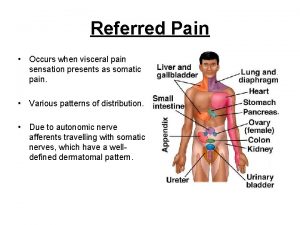
Base of prostate gland Viscerosomatic reflex
Viscerosomatic reflex Prostate
Prostate Prostate histology
Prostate histology Prostate pathology
Prostate pathology Istilah berarti absennya satu atau kedua buah zakar disebut
Istilah berarti absennya satu atau kedua buah zakar disebut Prostate referred pain
Prostate referred pain Prostate pathology
Prostate pathology Prostatakreft symptomer
Prostatakreft symptomer Lobes of prostate
Lobes of prostate Tuip prostate
Tuip prostate Frameset trong html5
Frameset trong html5 Hệ hô hấp
Hệ hô hấp Số nguyên tố là số gì
Số nguyên tố là số gì Tư thế ngồi viết
Tư thế ngồi viết đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Tư thế worm breton là gì
Tư thế worm breton là gì ưu thế lai là gì
ưu thế lai là gì